User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
CDC reports first human case of H5 bird flu in the U.S.
A man who worked on a commercial poultry farm in Colorado has tested positive for avian influenza A(H5) virus, better known as H5 bird flu, the CDC announced on April 28.
This is the first case of H5 bird flu in humans in the United States and only the second case in the world, the CDC said in a news release. The first case was detected last December in a man who raised birds in the United Kingdom. That man had no symptoms.
The only symptom the man in Colorado reported was fatigue, the Colorado Department of Public Health and Environment (CDPHE) reported. He has recovered and is isolating and being treated with oseltamivir, an antiviral drug.
The CDC said the man was helping kill poultry that likely had the H5N1 bird flu.
He is a state prison inmate who was working on a commercial poultry farm in Montrose County in a prerelease employment program, the CDPHE said. The flock he was working with has been euthanized, and the response team and other inmates working on the farm were given protective equipment, the CDPHE said.
“Repeat testing on the person was negative for influenza,” the department said. “Because the person was in close contact with infected poultry, the virus may have been in the person’s nose without causing infection.”
This CDC said the case does not change the risk of bird flu for the general public, which is considered low. People who work with birds should continue to take safety precautions, such as wearing gloves when handling birds and avoiding birds that appear to be dead or ill, the CDC said.
“We want to reassure Coloradans that the risk to them is low,” said Rachel Herlihy, MD, state epidemiologist with the CDPHE. “I am grateful for the seamless collaboration between CDC, Department of Corrections, Department of Agriculture, and CDPHE, as we continue to monitor this virus and protect all Coloradans.”
The federal government says the H5N1 virus has been found in commercial and backyard birds in 29 states and in wild birds in 34 states since the first cases were detected in late 2021.
The CDC says it has tracked the health of 2,500 people exposed to birds infected with H5N1 and only found one case of human infection, in Colorado.
A version of this article first appeared on WebMD.com.
A man who worked on a commercial poultry farm in Colorado has tested positive for avian influenza A(H5) virus, better known as H5 bird flu, the CDC announced on April 28.
This is the first case of H5 bird flu in humans in the United States and only the second case in the world, the CDC said in a news release. The first case was detected last December in a man who raised birds in the United Kingdom. That man had no symptoms.
The only symptom the man in Colorado reported was fatigue, the Colorado Department of Public Health and Environment (CDPHE) reported. He has recovered and is isolating and being treated with oseltamivir, an antiviral drug.
The CDC said the man was helping kill poultry that likely had the H5N1 bird flu.
He is a state prison inmate who was working on a commercial poultry farm in Montrose County in a prerelease employment program, the CDPHE said. The flock he was working with has been euthanized, and the response team and other inmates working on the farm were given protective equipment, the CDPHE said.
“Repeat testing on the person was negative for influenza,” the department said. “Because the person was in close contact with infected poultry, the virus may have been in the person’s nose without causing infection.”
This CDC said the case does not change the risk of bird flu for the general public, which is considered low. People who work with birds should continue to take safety precautions, such as wearing gloves when handling birds and avoiding birds that appear to be dead or ill, the CDC said.
“We want to reassure Coloradans that the risk to them is low,” said Rachel Herlihy, MD, state epidemiologist with the CDPHE. “I am grateful for the seamless collaboration between CDC, Department of Corrections, Department of Agriculture, and CDPHE, as we continue to monitor this virus and protect all Coloradans.”
The federal government says the H5N1 virus has been found in commercial and backyard birds in 29 states and in wild birds in 34 states since the first cases were detected in late 2021.
The CDC says it has tracked the health of 2,500 people exposed to birds infected with H5N1 and only found one case of human infection, in Colorado.
A version of this article first appeared on WebMD.com.
A man who worked on a commercial poultry farm in Colorado has tested positive for avian influenza A(H5) virus, better known as H5 bird flu, the CDC announced on April 28.
This is the first case of H5 bird flu in humans in the United States and only the second case in the world, the CDC said in a news release. The first case was detected last December in a man who raised birds in the United Kingdom. That man had no symptoms.
The only symptom the man in Colorado reported was fatigue, the Colorado Department of Public Health and Environment (CDPHE) reported. He has recovered and is isolating and being treated with oseltamivir, an antiviral drug.
The CDC said the man was helping kill poultry that likely had the H5N1 bird flu.
He is a state prison inmate who was working on a commercial poultry farm in Montrose County in a prerelease employment program, the CDPHE said. The flock he was working with has been euthanized, and the response team and other inmates working on the farm were given protective equipment, the CDPHE said.
“Repeat testing on the person was negative for influenza,” the department said. “Because the person was in close contact with infected poultry, the virus may have been in the person’s nose without causing infection.”
This CDC said the case does not change the risk of bird flu for the general public, which is considered low. People who work with birds should continue to take safety precautions, such as wearing gloves when handling birds and avoiding birds that appear to be dead or ill, the CDC said.
“We want to reassure Coloradans that the risk to them is low,” said Rachel Herlihy, MD, state epidemiologist with the CDPHE. “I am grateful for the seamless collaboration between CDC, Department of Corrections, Department of Agriculture, and CDPHE, as we continue to monitor this virus and protect all Coloradans.”
The federal government says the H5N1 virus has been found in commercial and backyard birds in 29 states and in wild birds in 34 states since the first cases were detected in late 2021.
The CDC says it has tracked the health of 2,500 people exposed to birds infected with H5N1 and only found one case of human infection, in Colorado.
A version of this article first appeared on WebMD.com.
Traumatic brain injury linked to ‘striking’ risk for CVD, diabetes, brain disorders
Mild traumatic brain injury (TBI) is linked to a significantly increased risk for a host of subsequent cardiovascular, endocrine, neurologic, and psychiatric disorders, new research shows.
Incidence of hypertension, coronary heart disease, diabetes, stroke, depression, and dementia all began to increase soon after the brain injury and persisted over a decade in both mild and moderate to severe TBI.
Researchers found the multisystem comorbidities in all age groups, including in patients as young as 18. They also found that patients who developed multiple postinjury problems had higher mortality during the decade-long follow-up.
The findings suggest patients with TBI may require longer follow-up and proactive screening for multisystem disease, regardless of age or injury severity.
“The fact that both patients with mild and moderate to severe injuries both had long-term ongoing associations with comorbidities that continued over time and that they are cardiovascular, endocrine, neurologic, and behavioral health oriented was pretty striking,” study author Ross Zafonte, DO, PhD, president of Spaulding Rehab Hospital and professor and chair of physical medicine and rehab at Harvard Medical School, both in Boston, told this news organization.
The study was published online in JAMA Network Open.
Injury severity not a factor
An estimated 2.8 million individuals in the United States experience TBI every year. Worldwide, the figure may be as high as 74 million.
Studies have long suggested a link between brain injury and subsequent neurologic disorders, but research suggesting a possible link to cardiovascular and endocrine problems has recently gained attention.
Building on a 2021 study that showed increased incidence of cardiovascular issues following a concussion, the researchers examined medical records of previously healthy patients treated for TBI between 2000 and 2015 who also had at least 1 follow-up visit between 6 months and 10 years after the initial injury.
Researchers analyzed data from 13,053 individuals – 4,351 with mild injury (mTBI), 4351 with moderate to severe injury (msTBI), and 4351 with no TBI. The most common cause of injury was a fall. Patients with sports-related injuries were excluded.
Incidence of hypertension was significantly higher among patients with mTBI (hazard ratio, 2.5; 95% confidence interval, 2.1-2.9) and msTBI (HR, 2.4; 95% CI, 2.0-2.9), compared with the unaffected group. Risk for other cardiovascular problems, including hyperlipidemia, obesity, and coronary artery disease, were also higher in the affected groups.
TBI patients also reported higher incidence of endocrine diseases, including diabetes (mTBI: HR, 1.9; 95% CI, 1.4-2.7; msTBI: HR, 1.9; 95% CI, 1.4-2.6). Elevated risk for ischemic stroke or transient ischemic attack was also increased (mTBI: HR, 2.2; 95% CI, 1.4-3.3; msTBI: HR, 3.6; 95% CI, 2.4-5.3).
Regardless of injury severity, patients with TBI had a higher risk for neurologic and psychiatric diseases, particularly depression, dementia, and psychotic disorders. “This tells us that mild TBI is not clean of events,” Dr. Zafonte said.
Surprising rate of comorbidity in youth
Investigators found increased risk for posttrauma comorbidities in all age groups, but researchers were struck by the high rates in younger patients, aged 18-40. Compared with age-matched individuals with no TBI history, hypertension risk was nearly six times higher in those with mTBI (HR, 5.9; 95% CI, 3.9-9.1) and nearly four times higher in patients with msTBI (HR, 3.9; 95% CI, 2.5-6.1).
Rates of hyperlipidemia and diabetes were also higher in younger patients in the mTBI group and posttraumatic seizures and psychiatric disorders were elevated regardless of TBI severity.
Overall, patients with msTBI, but not those with mTBI, were at higher risk for mortality, compared with the unexposed group (432 deaths [9.9%] vs. 250 deaths [5.7%]; P < .001).
“It’s clear that what we may be dealing with is that it holds up even for the younger people,” Dr. Zafonte said. “We used to think brain injury risk is worse in the severe cases, which it is, and it’s worse later on among those who are older, which it is. But our younger folks don’t get away either.”
While the study offers associations between TBI and multisystem health problems, Dr. Zafonte said it’s impossible to say at this point whether the brain injury caused the increased risk for cardiovascular or endocrine problems. Other organ injuries sustained in the trauma may be a contributing factor.
“Further data is needed to elucidate the mechanism and the causative relationships, which we do not have here,” he said.
Many of the postinjury comorbidities emerged a median of 3.5 years after TBI, regardless of severity. But some of the cardiovascular and psychiatric conditions emerged far sooner than that.
That’s important because research suggests less than half of patients with TBI receive follow-up care.
“It does make sense for folks who are interacting with people who’ve had a TBI to be suspicious of medical comorbidities relatively early on, within the first couple of years,” Dr. Zafonte said.
In an invited commentary, Vijay Krishnamoorthy, MD, MPH, PhD, Duke University, Durham, N.C., and Monica S. Vavilala, MD, University of Washington, Seattle, highlight some of the study’s limitations, including a lack of information on comorbidity severity and the lack of a matched group of patients who experienced non-head trauma.
Despite those limitations, the study offers important information on how TBI may affect organs beyond the brain, they noted.
“These observations, if replicated in future studies, raise intriguing implications in the future care of patients with TBI, including heightened chronic disease-screening measures and possibly enhanced guidelines for chronic extracranial organ system care for patients who experience TBI,” Dr. Krishnamoorthy and Dr. Vavilala wrote.
The study received no specific funding. Dr. Zafonte reported having received personal fees from Springer/Demos, serving on scientific advisory boards for Myomo and OnCare and has received funding from the Football Players Health Study at Harvard, funded in part by the National Football League Players Association. Dr. Krishnamoorthy and Dr. Vavilala disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mild traumatic brain injury (TBI) is linked to a significantly increased risk for a host of subsequent cardiovascular, endocrine, neurologic, and psychiatric disorders, new research shows.
Incidence of hypertension, coronary heart disease, diabetes, stroke, depression, and dementia all began to increase soon after the brain injury and persisted over a decade in both mild and moderate to severe TBI.
Researchers found the multisystem comorbidities in all age groups, including in patients as young as 18. They also found that patients who developed multiple postinjury problems had higher mortality during the decade-long follow-up.
The findings suggest patients with TBI may require longer follow-up and proactive screening for multisystem disease, regardless of age or injury severity.
“The fact that both patients with mild and moderate to severe injuries both had long-term ongoing associations with comorbidities that continued over time and that they are cardiovascular, endocrine, neurologic, and behavioral health oriented was pretty striking,” study author Ross Zafonte, DO, PhD, president of Spaulding Rehab Hospital and professor and chair of physical medicine and rehab at Harvard Medical School, both in Boston, told this news organization.
The study was published online in JAMA Network Open.
Injury severity not a factor
An estimated 2.8 million individuals in the United States experience TBI every year. Worldwide, the figure may be as high as 74 million.
Studies have long suggested a link between brain injury and subsequent neurologic disorders, but research suggesting a possible link to cardiovascular and endocrine problems has recently gained attention.
Building on a 2021 study that showed increased incidence of cardiovascular issues following a concussion, the researchers examined medical records of previously healthy patients treated for TBI between 2000 and 2015 who also had at least 1 follow-up visit between 6 months and 10 years after the initial injury.
Researchers analyzed data from 13,053 individuals – 4,351 with mild injury (mTBI), 4351 with moderate to severe injury (msTBI), and 4351 with no TBI. The most common cause of injury was a fall. Patients with sports-related injuries were excluded.
Incidence of hypertension was significantly higher among patients with mTBI (hazard ratio, 2.5; 95% confidence interval, 2.1-2.9) and msTBI (HR, 2.4; 95% CI, 2.0-2.9), compared with the unaffected group. Risk for other cardiovascular problems, including hyperlipidemia, obesity, and coronary artery disease, were also higher in the affected groups.
TBI patients also reported higher incidence of endocrine diseases, including diabetes (mTBI: HR, 1.9; 95% CI, 1.4-2.7; msTBI: HR, 1.9; 95% CI, 1.4-2.6). Elevated risk for ischemic stroke or transient ischemic attack was also increased (mTBI: HR, 2.2; 95% CI, 1.4-3.3; msTBI: HR, 3.6; 95% CI, 2.4-5.3).
Regardless of injury severity, patients with TBI had a higher risk for neurologic and psychiatric diseases, particularly depression, dementia, and psychotic disorders. “This tells us that mild TBI is not clean of events,” Dr. Zafonte said.
Surprising rate of comorbidity in youth
Investigators found increased risk for posttrauma comorbidities in all age groups, but researchers were struck by the high rates in younger patients, aged 18-40. Compared with age-matched individuals with no TBI history, hypertension risk was nearly six times higher in those with mTBI (HR, 5.9; 95% CI, 3.9-9.1) and nearly four times higher in patients with msTBI (HR, 3.9; 95% CI, 2.5-6.1).
Rates of hyperlipidemia and diabetes were also higher in younger patients in the mTBI group and posttraumatic seizures and psychiatric disorders were elevated regardless of TBI severity.
Overall, patients with msTBI, but not those with mTBI, were at higher risk for mortality, compared with the unexposed group (432 deaths [9.9%] vs. 250 deaths [5.7%]; P < .001).
“It’s clear that what we may be dealing with is that it holds up even for the younger people,” Dr. Zafonte said. “We used to think brain injury risk is worse in the severe cases, which it is, and it’s worse later on among those who are older, which it is. But our younger folks don’t get away either.”
While the study offers associations between TBI and multisystem health problems, Dr. Zafonte said it’s impossible to say at this point whether the brain injury caused the increased risk for cardiovascular or endocrine problems. Other organ injuries sustained in the trauma may be a contributing factor.
“Further data is needed to elucidate the mechanism and the causative relationships, which we do not have here,” he said.
Many of the postinjury comorbidities emerged a median of 3.5 years after TBI, regardless of severity. But some of the cardiovascular and psychiatric conditions emerged far sooner than that.
That’s important because research suggests less than half of patients with TBI receive follow-up care.
“It does make sense for folks who are interacting with people who’ve had a TBI to be suspicious of medical comorbidities relatively early on, within the first couple of years,” Dr. Zafonte said.
In an invited commentary, Vijay Krishnamoorthy, MD, MPH, PhD, Duke University, Durham, N.C., and Monica S. Vavilala, MD, University of Washington, Seattle, highlight some of the study’s limitations, including a lack of information on comorbidity severity and the lack of a matched group of patients who experienced non-head trauma.
Despite those limitations, the study offers important information on how TBI may affect organs beyond the brain, they noted.
“These observations, if replicated in future studies, raise intriguing implications in the future care of patients with TBI, including heightened chronic disease-screening measures and possibly enhanced guidelines for chronic extracranial organ system care for patients who experience TBI,” Dr. Krishnamoorthy and Dr. Vavilala wrote.
The study received no specific funding. Dr. Zafonte reported having received personal fees from Springer/Demos, serving on scientific advisory boards for Myomo and OnCare and has received funding from the Football Players Health Study at Harvard, funded in part by the National Football League Players Association. Dr. Krishnamoorthy and Dr. Vavilala disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mild traumatic brain injury (TBI) is linked to a significantly increased risk for a host of subsequent cardiovascular, endocrine, neurologic, and psychiatric disorders, new research shows.
Incidence of hypertension, coronary heart disease, diabetes, stroke, depression, and dementia all began to increase soon after the brain injury and persisted over a decade in both mild and moderate to severe TBI.
Researchers found the multisystem comorbidities in all age groups, including in patients as young as 18. They also found that patients who developed multiple postinjury problems had higher mortality during the decade-long follow-up.
The findings suggest patients with TBI may require longer follow-up and proactive screening for multisystem disease, regardless of age or injury severity.
“The fact that both patients with mild and moderate to severe injuries both had long-term ongoing associations with comorbidities that continued over time and that they are cardiovascular, endocrine, neurologic, and behavioral health oriented was pretty striking,” study author Ross Zafonte, DO, PhD, president of Spaulding Rehab Hospital and professor and chair of physical medicine and rehab at Harvard Medical School, both in Boston, told this news organization.
The study was published online in JAMA Network Open.
Injury severity not a factor
An estimated 2.8 million individuals in the United States experience TBI every year. Worldwide, the figure may be as high as 74 million.
Studies have long suggested a link between brain injury and subsequent neurologic disorders, but research suggesting a possible link to cardiovascular and endocrine problems has recently gained attention.
Building on a 2021 study that showed increased incidence of cardiovascular issues following a concussion, the researchers examined medical records of previously healthy patients treated for TBI between 2000 and 2015 who also had at least 1 follow-up visit between 6 months and 10 years after the initial injury.
Researchers analyzed data from 13,053 individuals – 4,351 with mild injury (mTBI), 4351 with moderate to severe injury (msTBI), and 4351 with no TBI. The most common cause of injury was a fall. Patients with sports-related injuries were excluded.
Incidence of hypertension was significantly higher among patients with mTBI (hazard ratio, 2.5; 95% confidence interval, 2.1-2.9) and msTBI (HR, 2.4; 95% CI, 2.0-2.9), compared with the unaffected group. Risk for other cardiovascular problems, including hyperlipidemia, obesity, and coronary artery disease, were also higher in the affected groups.
TBI patients also reported higher incidence of endocrine diseases, including diabetes (mTBI: HR, 1.9; 95% CI, 1.4-2.7; msTBI: HR, 1.9; 95% CI, 1.4-2.6). Elevated risk for ischemic stroke or transient ischemic attack was also increased (mTBI: HR, 2.2; 95% CI, 1.4-3.3; msTBI: HR, 3.6; 95% CI, 2.4-5.3).
Regardless of injury severity, patients with TBI had a higher risk for neurologic and psychiatric diseases, particularly depression, dementia, and psychotic disorders. “This tells us that mild TBI is not clean of events,” Dr. Zafonte said.
Surprising rate of comorbidity in youth
Investigators found increased risk for posttrauma comorbidities in all age groups, but researchers were struck by the high rates in younger patients, aged 18-40. Compared with age-matched individuals with no TBI history, hypertension risk was nearly six times higher in those with mTBI (HR, 5.9; 95% CI, 3.9-9.1) and nearly four times higher in patients with msTBI (HR, 3.9; 95% CI, 2.5-6.1).
Rates of hyperlipidemia and diabetes were also higher in younger patients in the mTBI group and posttraumatic seizures and psychiatric disorders were elevated regardless of TBI severity.
Overall, patients with msTBI, but not those with mTBI, were at higher risk for mortality, compared with the unexposed group (432 deaths [9.9%] vs. 250 deaths [5.7%]; P < .001).
“It’s clear that what we may be dealing with is that it holds up even for the younger people,” Dr. Zafonte said. “We used to think brain injury risk is worse in the severe cases, which it is, and it’s worse later on among those who are older, which it is. But our younger folks don’t get away either.”
While the study offers associations between TBI and multisystem health problems, Dr. Zafonte said it’s impossible to say at this point whether the brain injury caused the increased risk for cardiovascular or endocrine problems. Other organ injuries sustained in the trauma may be a contributing factor.
“Further data is needed to elucidate the mechanism and the causative relationships, which we do not have here,” he said.
Many of the postinjury comorbidities emerged a median of 3.5 years after TBI, regardless of severity. But some of the cardiovascular and psychiatric conditions emerged far sooner than that.
That’s important because research suggests less than half of patients with TBI receive follow-up care.
“It does make sense for folks who are interacting with people who’ve had a TBI to be suspicious of medical comorbidities relatively early on, within the first couple of years,” Dr. Zafonte said.
In an invited commentary, Vijay Krishnamoorthy, MD, MPH, PhD, Duke University, Durham, N.C., and Monica S. Vavilala, MD, University of Washington, Seattle, highlight some of the study’s limitations, including a lack of information on comorbidity severity and the lack of a matched group of patients who experienced non-head trauma.
Despite those limitations, the study offers important information on how TBI may affect organs beyond the brain, they noted.
“These observations, if replicated in future studies, raise intriguing implications in the future care of patients with TBI, including heightened chronic disease-screening measures and possibly enhanced guidelines for chronic extracranial organ system care for patients who experience TBI,” Dr. Krishnamoorthy and Dr. Vavilala wrote.
The study received no specific funding. Dr. Zafonte reported having received personal fees from Springer/Demos, serving on scientific advisory boards for Myomo and OnCare and has received funding from the Football Players Health Study at Harvard, funded in part by the National Football League Players Association. Dr. Krishnamoorthy and Dr. Vavilala disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Sexually transmitted infections on a 30-year rise worldwide
The incidence of sexually transmitted infection (STI) as well as disability-adjusted life-years (DALYs) increased worldwide over 30 years, according to an observational trend study from China.
“Most countries had a decrease in age-standardized rates of incidence and DALY for STIs, whereas the absolute incident cases and DALYs increased from 1990 to 2019,” the authors write in The Lancet Infectious Diseases. “Therefore, STIs still represent a global public health challenge, especially in sub-Saharan Africa and Latin America, where more attention and health prevention services are warranted.”
“Our study also suggested an upward trend of age-standardized incidence rates among young populations, especially for syphilis, after 2010,” they add.
STIs are a major worldwide public health challenge
To assess global STI burden and trends, co–lead study author Yang Zheng, MD, of Zhejiang University School of Medicine in Hangzhou, China, and colleagues analyzed data from the Global Burden of Disease (GBD) study 2019.
They calculated incidence and DALYs of STIs in the general population at national, regional, and global levels over 30 years. They also calculated annual percentage changes in the age-standardized incidence rate and the age-standardized DALY rate of the five STIs included in the GBD study.
Of 204 countries in GBD 2019, 161 provided data on syphilis, 64 on gonorrhea, 94 on chlamydia, 56 on trichomonas, and 77 on genital herpes. The authors included 95% uncertainty intervals (UIs) and used Bayesian meta-regression to model the data.
- Overall, they found that the global age-standardized incidence rate of STIs trended downward, with an estimated annual percentage change of –0.04 (95% UI, –0.08 to 0.00) from 1990 to 2019, reaching 9,535.71 per 100,000 person-years (8,169.73-11,054.76) in 2019.
- The age-standardized DALY rate decreased with an estimated annual percentage change of –0.92 (–1.01 to –0.84) and reached 22.74 per 100,000 person-years (14.37-37.11) in 2019.
- Sub-Saharan Africa, one of the hotspots, had the highest age-standardized incidence rate (19,973.12 per 100,000 person-years, 17,382.69-23,001.57) and age-standardized DALY rate (389.32 per 100,000 person-years, 154.27-769.74).
- The highest incidence rate was among adolescents (18,377.82 per 100,000 person-years, 14,040.38-23,443.31), with stable total STI trends except for an increase in syphilis between 2010 (347.65 per 100,000 person-years, 203.58-590.69) and 2019 (423.16 per 100,000 person-years, 235.70-659.01).
- The age-standardized incidence rate was higher among males (10,471.63 per 100,000 person-years, 8,892.20-12,176.10) than females (8,602.40 per 100,000 person-years, 7,358.00-10,001.18), whereas the age-standardized DALY rate was higher among females (33.31 per 100,000 person-years, 21.05-55.25) than males (12.11 per 100,000 person-years, 7.63-18.93).
The authors deliver a call to action
“This paper is a call to action to focus on the STI pandemic with granular data on key target populations,” Yukari C. Manabe, MD, FIDSA, FRCP, who was not involved in the study, told this news organization. “If behavioral messaging and testing in adolescents is not improved, HIV incidence rates will be impacted, and the gains that have been made in this area will be threatened.”
“Although the number of countries from which data could be culled was limited, the change in incident cases is particularly striking, with most countries showing an increase and with African countries showing the largest rise,” said Dr. Manabe, professor of medicine, international health, and molecular microbiology and immunology at Johns Hopkins Medicine and director of the Johns Hopkins Center for Innovative Diagnostics for Infectious Diseases, Baltimore.
“The increase in syphilis incidence rates, particularly in younger people, including men who have sex with men, is also alarming,” she added in an email. “It is interesting to see the gender gap grow as more countries adopt antenatal syphilis screening.”
Ken S. Ho, MD, MPH, infectious diseases specialist and medical director of the Pitt Men’s Study at the University of Pittsburgh School of Medicine, Pennsylvania, called the study’s findings a wake-up call for clinicians to discuss sexual health and wellness with their patients, to increase STI screening, and to address STI stigma.
“Overall, STI rates in most countries have trended down, but paradoxically, the number of cases may be going up, because we have more younger, sexually actively people,” Dr. Ho said in an email.
“The study helps us understand the populations most impacted by STIs and allows us to design and create public health interventions that target the most impacted communities and demographic groups,” Dr. Ho, who also was not involved in the study, added. “It allows us to reflect on how we address disparities. For example, the greater burden of disease seen in women may be due to the fact that women may not be screened and are diagnosed later.”
Dr. Ho explained that the high STI rates in sub-Saharan Africa and Latin America are thought to be due to factors such as poverty and limited access to health care, known drivers of health care disparities.
The 2016 global incidence of common STIs was estimated to be up to 563.3 million, including 6.3 million cases of syphilis, 86.9 million cases of gonorrhea, 127.2 million cases of chlamydia, 156.0 million cases of trichomonas, and 186.9 million cases of genital herpes, the authors write.
The World Health Organization aims to end the STI epidemic by 2030, they note.
The study was funded by Mega-Project of National Science and Technology for the 13th Five-Year Plan of China and the National Natural Science Foundation of China. The authors, Dr. Manabe, and Dr. Ho have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of sexually transmitted infection (STI) as well as disability-adjusted life-years (DALYs) increased worldwide over 30 years, according to an observational trend study from China.
“Most countries had a decrease in age-standardized rates of incidence and DALY for STIs, whereas the absolute incident cases and DALYs increased from 1990 to 2019,” the authors write in The Lancet Infectious Diseases. “Therefore, STIs still represent a global public health challenge, especially in sub-Saharan Africa and Latin America, where more attention and health prevention services are warranted.”
“Our study also suggested an upward trend of age-standardized incidence rates among young populations, especially for syphilis, after 2010,” they add.
STIs are a major worldwide public health challenge
To assess global STI burden and trends, co–lead study author Yang Zheng, MD, of Zhejiang University School of Medicine in Hangzhou, China, and colleagues analyzed data from the Global Burden of Disease (GBD) study 2019.
They calculated incidence and DALYs of STIs in the general population at national, regional, and global levels over 30 years. They also calculated annual percentage changes in the age-standardized incidence rate and the age-standardized DALY rate of the five STIs included in the GBD study.
Of 204 countries in GBD 2019, 161 provided data on syphilis, 64 on gonorrhea, 94 on chlamydia, 56 on trichomonas, and 77 on genital herpes. The authors included 95% uncertainty intervals (UIs) and used Bayesian meta-regression to model the data.
- Overall, they found that the global age-standardized incidence rate of STIs trended downward, with an estimated annual percentage change of –0.04 (95% UI, –0.08 to 0.00) from 1990 to 2019, reaching 9,535.71 per 100,000 person-years (8,169.73-11,054.76) in 2019.
- The age-standardized DALY rate decreased with an estimated annual percentage change of –0.92 (–1.01 to –0.84) and reached 22.74 per 100,000 person-years (14.37-37.11) in 2019.
- Sub-Saharan Africa, one of the hotspots, had the highest age-standardized incidence rate (19,973.12 per 100,000 person-years, 17,382.69-23,001.57) and age-standardized DALY rate (389.32 per 100,000 person-years, 154.27-769.74).
- The highest incidence rate was among adolescents (18,377.82 per 100,000 person-years, 14,040.38-23,443.31), with stable total STI trends except for an increase in syphilis between 2010 (347.65 per 100,000 person-years, 203.58-590.69) and 2019 (423.16 per 100,000 person-years, 235.70-659.01).
- The age-standardized incidence rate was higher among males (10,471.63 per 100,000 person-years, 8,892.20-12,176.10) than females (8,602.40 per 100,000 person-years, 7,358.00-10,001.18), whereas the age-standardized DALY rate was higher among females (33.31 per 100,000 person-years, 21.05-55.25) than males (12.11 per 100,000 person-years, 7.63-18.93).
The authors deliver a call to action
“This paper is a call to action to focus on the STI pandemic with granular data on key target populations,” Yukari C. Manabe, MD, FIDSA, FRCP, who was not involved in the study, told this news organization. “If behavioral messaging and testing in adolescents is not improved, HIV incidence rates will be impacted, and the gains that have been made in this area will be threatened.”
“Although the number of countries from which data could be culled was limited, the change in incident cases is particularly striking, with most countries showing an increase and with African countries showing the largest rise,” said Dr. Manabe, professor of medicine, international health, and molecular microbiology and immunology at Johns Hopkins Medicine and director of the Johns Hopkins Center for Innovative Diagnostics for Infectious Diseases, Baltimore.
“The increase in syphilis incidence rates, particularly in younger people, including men who have sex with men, is also alarming,” she added in an email. “It is interesting to see the gender gap grow as more countries adopt antenatal syphilis screening.”
Ken S. Ho, MD, MPH, infectious diseases specialist and medical director of the Pitt Men’s Study at the University of Pittsburgh School of Medicine, Pennsylvania, called the study’s findings a wake-up call for clinicians to discuss sexual health and wellness with their patients, to increase STI screening, and to address STI stigma.
“Overall, STI rates in most countries have trended down, but paradoxically, the number of cases may be going up, because we have more younger, sexually actively people,” Dr. Ho said in an email.
“The study helps us understand the populations most impacted by STIs and allows us to design and create public health interventions that target the most impacted communities and demographic groups,” Dr. Ho, who also was not involved in the study, added. “It allows us to reflect on how we address disparities. For example, the greater burden of disease seen in women may be due to the fact that women may not be screened and are diagnosed later.”
Dr. Ho explained that the high STI rates in sub-Saharan Africa and Latin America are thought to be due to factors such as poverty and limited access to health care, known drivers of health care disparities.
The 2016 global incidence of common STIs was estimated to be up to 563.3 million, including 6.3 million cases of syphilis, 86.9 million cases of gonorrhea, 127.2 million cases of chlamydia, 156.0 million cases of trichomonas, and 186.9 million cases of genital herpes, the authors write.
The World Health Organization aims to end the STI epidemic by 2030, they note.
The study was funded by Mega-Project of National Science and Technology for the 13th Five-Year Plan of China and the National Natural Science Foundation of China. The authors, Dr. Manabe, and Dr. Ho have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of sexually transmitted infection (STI) as well as disability-adjusted life-years (DALYs) increased worldwide over 30 years, according to an observational trend study from China.
“Most countries had a decrease in age-standardized rates of incidence and DALY for STIs, whereas the absolute incident cases and DALYs increased from 1990 to 2019,” the authors write in The Lancet Infectious Diseases. “Therefore, STIs still represent a global public health challenge, especially in sub-Saharan Africa and Latin America, where more attention and health prevention services are warranted.”
“Our study also suggested an upward trend of age-standardized incidence rates among young populations, especially for syphilis, after 2010,” they add.
STIs are a major worldwide public health challenge
To assess global STI burden and trends, co–lead study author Yang Zheng, MD, of Zhejiang University School of Medicine in Hangzhou, China, and colleagues analyzed data from the Global Burden of Disease (GBD) study 2019.
They calculated incidence and DALYs of STIs in the general population at national, regional, and global levels over 30 years. They also calculated annual percentage changes in the age-standardized incidence rate and the age-standardized DALY rate of the five STIs included in the GBD study.
Of 204 countries in GBD 2019, 161 provided data on syphilis, 64 on gonorrhea, 94 on chlamydia, 56 on trichomonas, and 77 on genital herpes. The authors included 95% uncertainty intervals (UIs) and used Bayesian meta-regression to model the data.
- Overall, they found that the global age-standardized incidence rate of STIs trended downward, with an estimated annual percentage change of –0.04 (95% UI, –0.08 to 0.00) from 1990 to 2019, reaching 9,535.71 per 100,000 person-years (8,169.73-11,054.76) in 2019.
- The age-standardized DALY rate decreased with an estimated annual percentage change of –0.92 (–1.01 to –0.84) and reached 22.74 per 100,000 person-years (14.37-37.11) in 2019.
- Sub-Saharan Africa, one of the hotspots, had the highest age-standardized incidence rate (19,973.12 per 100,000 person-years, 17,382.69-23,001.57) and age-standardized DALY rate (389.32 per 100,000 person-years, 154.27-769.74).
- The highest incidence rate was among adolescents (18,377.82 per 100,000 person-years, 14,040.38-23,443.31), with stable total STI trends except for an increase in syphilis between 2010 (347.65 per 100,000 person-years, 203.58-590.69) and 2019 (423.16 per 100,000 person-years, 235.70-659.01).
- The age-standardized incidence rate was higher among males (10,471.63 per 100,000 person-years, 8,892.20-12,176.10) than females (8,602.40 per 100,000 person-years, 7,358.00-10,001.18), whereas the age-standardized DALY rate was higher among females (33.31 per 100,000 person-years, 21.05-55.25) than males (12.11 per 100,000 person-years, 7.63-18.93).
The authors deliver a call to action
“This paper is a call to action to focus on the STI pandemic with granular data on key target populations,” Yukari C. Manabe, MD, FIDSA, FRCP, who was not involved in the study, told this news organization. “If behavioral messaging and testing in adolescents is not improved, HIV incidence rates will be impacted, and the gains that have been made in this area will be threatened.”
“Although the number of countries from which data could be culled was limited, the change in incident cases is particularly striking, with most countries showing an increase and with African countries showing the largest rise,” said Dr. Manabe, professor of medicine, international health, and molecular microbiology and immunology at Johns Hopkins Medicine and director of the Johns Hopkins Center for Innovative Diagnostics for Infectious Diseases, Baltimore.
“The increase in syphilis incidence rates, particularly in younger people, including men who have sex with men, is also alarming,” she added in an email. “It is interesting to see the gender gap grow as more countries adopt antenatal syphilis screening.”
Ken S. Ho, MD, MPH, infectious diseases specialist and medical director of the Pitt Men’s Study at the University of Pittsburgh School of Medicine, Pennsylvania, called the study’s findings a wake-up call for clinicians to discuss sexual health and wellness with their patients, to increase STI screening, and to address STI stigma.
“Overall, STI rates in most countries have trended down, but paradoxically, the number of cases may be going up, because we have more younger, sexually actively people,” Dr. Ho said in an email.
“The study helps us understand the populations most impacted by STIs and allows us to design and create public health interventions that target the most impacted communities and demographic groups,” Dr. Ho, who also was not involved in the study, added. “It allows us to reflect on how we address disparities. For example, the greater burden of disease seen in women may be due to the fact that women may not be screened and are diagnosed later.”
Dr. Ho explained that the high STI rates in sub-Saharan Africa and Latin America are thought to be due to factors such as poverty and limited access to health care, known drivers of health care disparities.
The 2016 global incidence of common STIs was estimated to be up to 563.3 million, including 6.3 million cases of syphilis, 86.9 million cases of gonorrhea, 127.2 million cases of chlamydia, 156.0 million cases of trichomonas, and 186.9 million cases of genital herpes, the authors write.
The World Health Organization aims to end the STI epidemic by 2030, they note.
The study was funded by Mega-Project of National Science and Technology for the 13th Five-Year Plan of China and the National Natural Science Foundation of China. The authors, Dr. Manabe, and Dr. Ho have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET INFECTIOUS DISEASES
Antibiotic prescriptions to Black and Hispanic/Latinx patients in the U.S. are often inappropriate
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Two-thirds of antibiotic prescriptions written for Black patients and more than half of antibiotic prescriptions for Hispanic/Latinx patients are inappropriate, according to data from a study of antibiotic prescribing habits in U.S. doctors’ offices, hospital clinics, and emergency departments.
Eric Young, PharmD, PhD, from the University of Texas at Austin, and UT Health, San Antonio, presented his work as a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022.
“We were really surprised mainly by the racial findings, because Black patients have the highest overall and the highest inappropriate prescribing of antibiotics,” he told this news organization. “There was also a difference seen for age [across all ethnicities].”
Pediatric patients were found to have high overall prescribing but, notably, the lowest inappropriate prescribing among all the patient groups, reported Dr. Young. “This is interesting because oftentimes we think the more antibiotics are prescribed, then surely the greater the inappropriate prescribing would be too, but pediatricians actually have one of the lowest rates of inappropriate antibiotic prescribing. They do a great job.”
The study included more than 7 billion patient visits, 11.3% of which involved an antibiotic prescription.
The rate of antibiotic prescribing was 122 per 1,000 visits in Black patients and 139 per 1,000 visits in Hispanic patients, while in White patients, the rate was 109 per 1,000 visits. The rate was 114 per 1,000 visits in patients younger than 18 years and 170 per 1,000 visits in females.
Dr. Young found that almost 64% of antibiotic prescriptions written for Black patients and 58% for Hispanic patients were inappropriate. For White patients, the rate of inappropriate antibiotic prescribing was 56%. Similarly, 74% of prescriptions dispensed to patients aged 65 years and older and 58% to males were deemed inappropriate.
Kajal Bhakta, PharmD, BCACP, ambulatory care clinical pharmacist, University Health System, UT Health Science Center San Antonio, who was not involved in the study, pointed out that antibiotics are frequently prescribed without confirmation of an infection, owing to the fact that the verification process may delay care, especially in the outpatient setting.
Dr. Bhakta said that overprescribing in the elderly population and in certain ethnic groups was “likely due to socioeconomic and cultural factors. These prescribing methods may lead to unnecessary drug side effects and/or antimicrobial resistance.”
Regarding the patient-doctor consultation process, she pointed out that “older patients may have trouble describing their symptoms, and when those symptoms remain unresolved, providers may be more inclined to prescribe antibiotics to help.”
Sometimes overprescribing can occur because of the logistics involved in getting to the doctor’s office in the outpatient setting. “Sometimes patients struggle with transportation, as two separate trips to the doctor and pharmacy may not be feasible. Additionally, these same patients may have limited access to health care and therefore may use an urgent care facility for their acute infection–like symptoms,” Dr. Bhakta explained.
Dr. Young, who is of Asian descent, first became interested in disparities in health care when he noticed that ethnic minority groups showed greater hesitancy toward COVID-19 vaccination. “I noticed that there weren’t many Asians involved in previous trials and realized at this point that disparities were rampant.”
Dr. Young had been involved in investigating the overall use and the inappropriate use of antibiotics across the whole U.S. population when his interest in health disparities prompted him to study these patterns in specific demographic groups.
“Most previous data are derived from inpatient studies where the physician is giving the antibiotics,” said Dr. Young, who looked specifically at outpatient prescribing.
Dr. Young used prescribing data from the Centers for Disease Control and Prevention’s National Ambulatory Medical Care Survey, which covers more than 5.7 billion adult (aged 18 and older) and 1.3 billion child visits to outpatient practices between 2009 and 2016 across all 50 U.S. states and Washington, D.C.
He gathered patient data on ICD-9-CM and ICD-10 diagnostic codes for infections and for diagnoses that “appeared like infections.” All of the patients who were included had received at least one oral antibiotic. Antibiotic prescribing was defined as visits that included an antibiotic per 1,000 total patient visits.
On the basis of previous research, Dr. Young and his colleagues then determined whether each antibiotic prescription was appropriate, possibly appropriate, or inappropriate. Patient demographics included age (younger than 18 years, 18-64 years, and older than 64 years), sex (male or female), race, and ethnicity (White, Black, more than one race, Hispanic/Latinx, and other). These data were used to evaluate overall and inappropriate use.
“The health care community needs to be really careful with the judicious use of antibiotics,” Dr. Young said. “We have good guidelines on antimicrobial stewardship both in the inpatient and outpatient settings, but sometimes we overlook the disparities and cultural implications held by some patients.”
Typical examples of socioeconomic and cultural factors at play included patients not being able to afford the antibiotics, having limited access to care, or not returning for a follow-up visit for whatever reason.
“Patients of Black and Hispanic descent often don’t have the same degree of established care that many White patients have,” Dr. Young noted.
In the future, Dr. Young wants to conduct research into whether patients are actually taking their prescribed antibiotics, as well as their outcomes. For example, he would like to investigate whether rates of antibiotic resistance or Clostridioides difficile infection are higher among Black patients.
Dr. Young and Dr. Bhakta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ECCMID 2022
The woman who kept passing out
CASE An apparent code blue
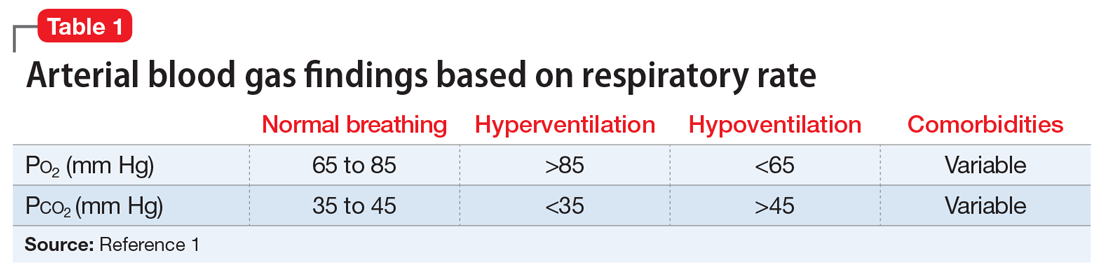
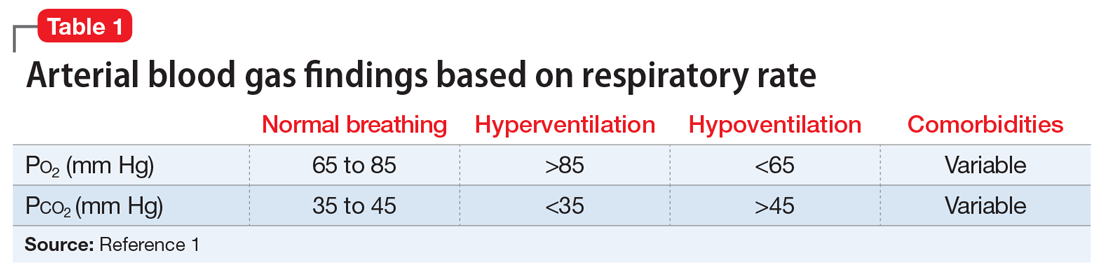
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
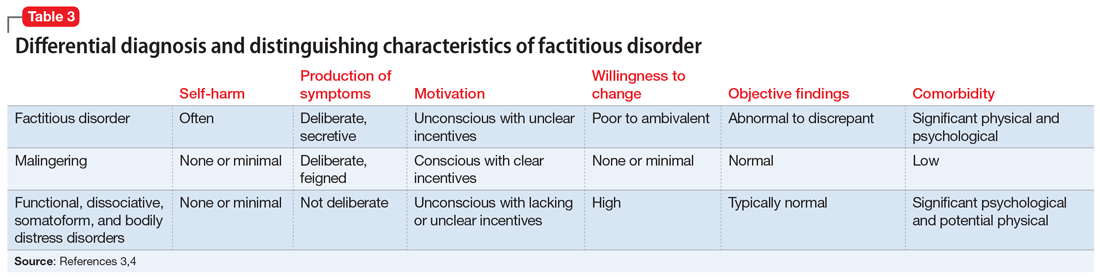
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
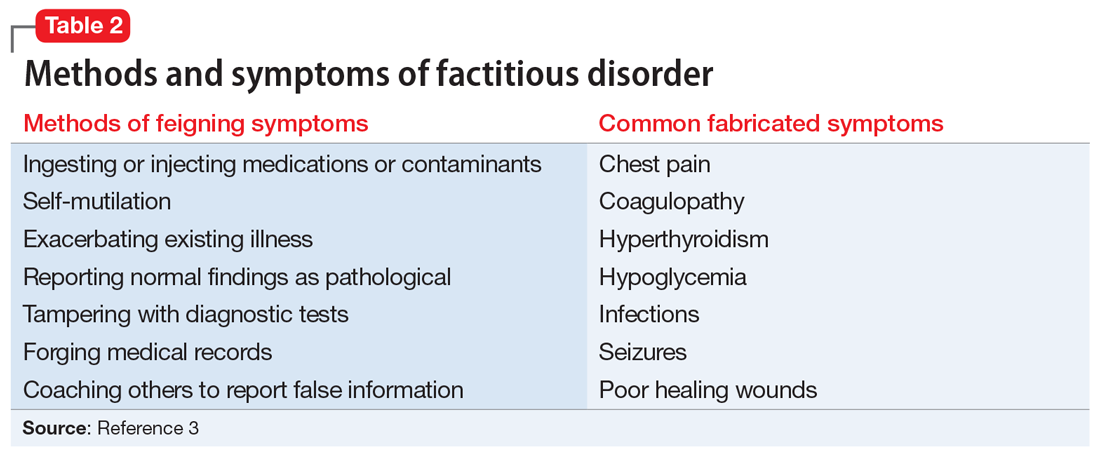
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
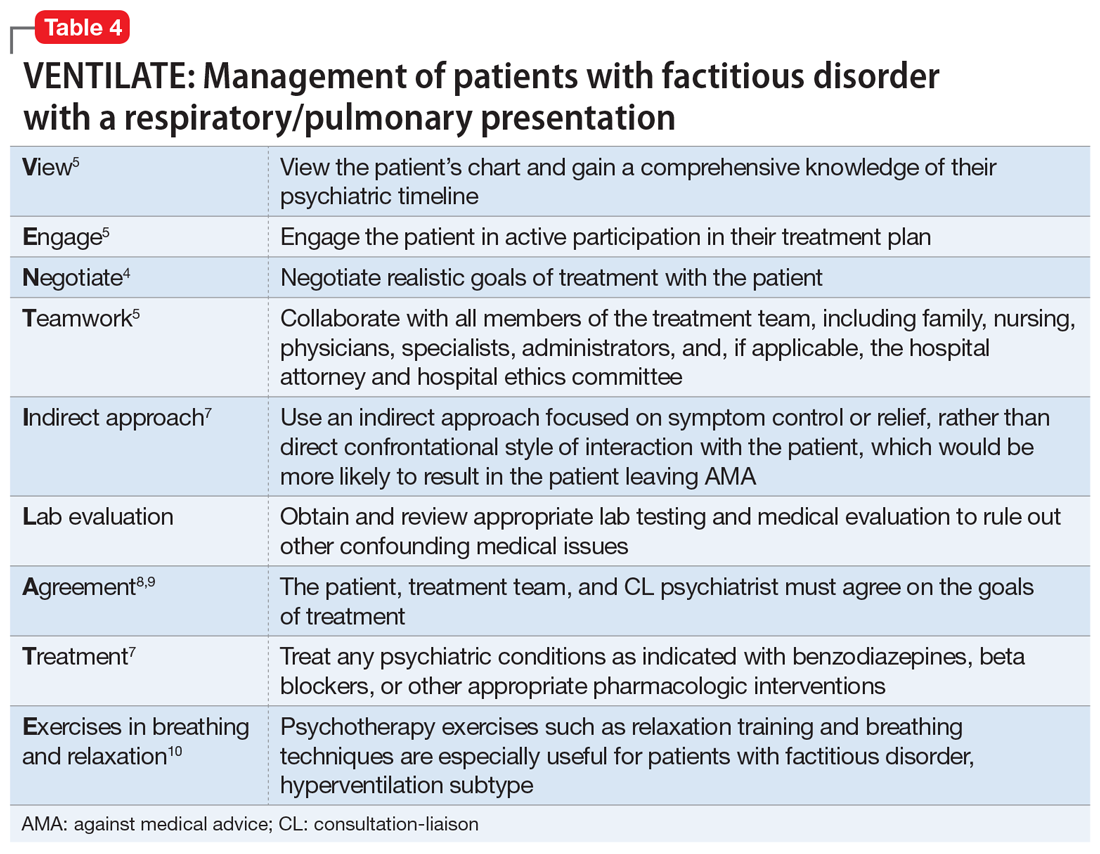
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
CASE An apparent code blue
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
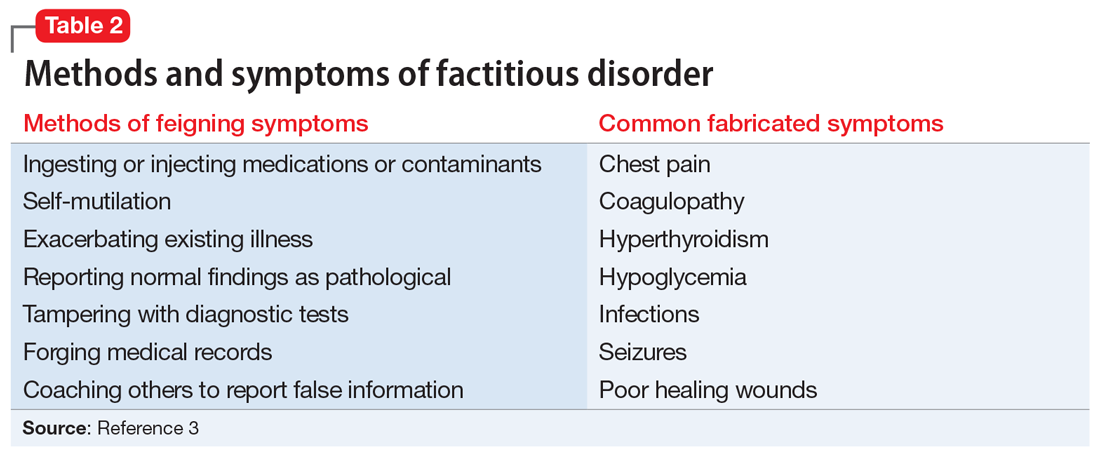
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
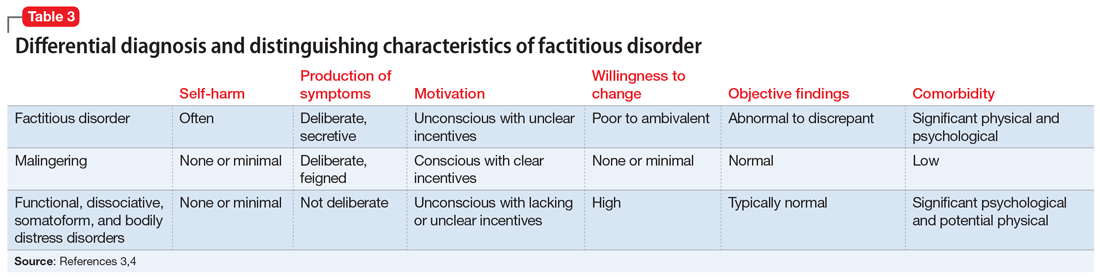
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
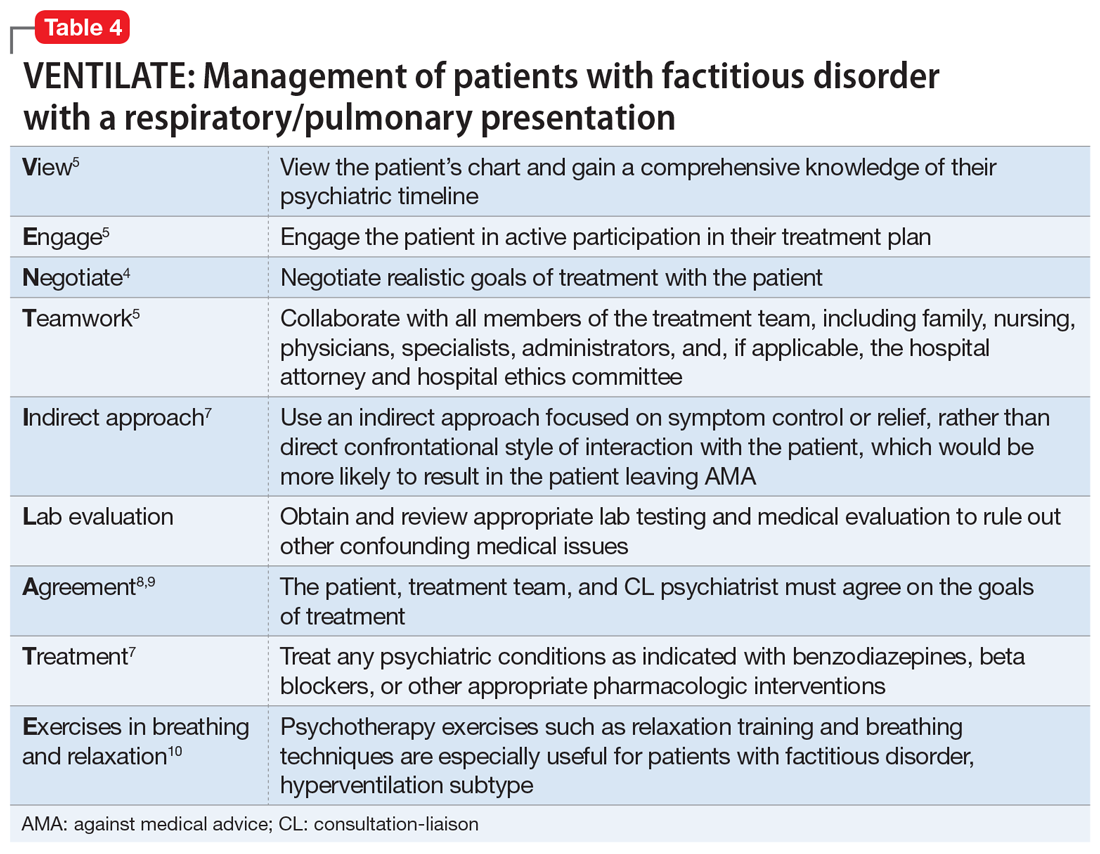
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
CASE An apparent code blue
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
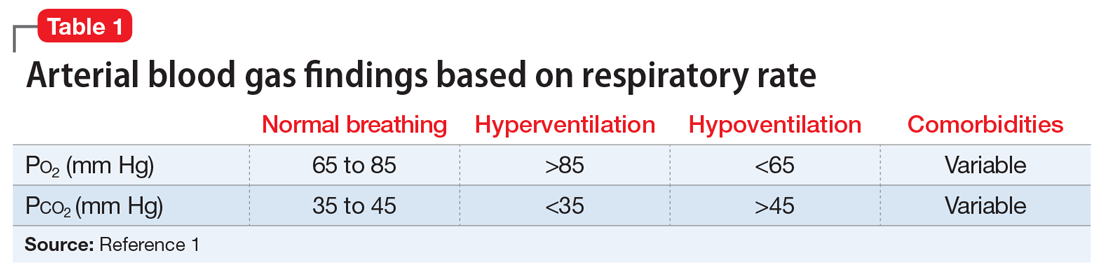
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
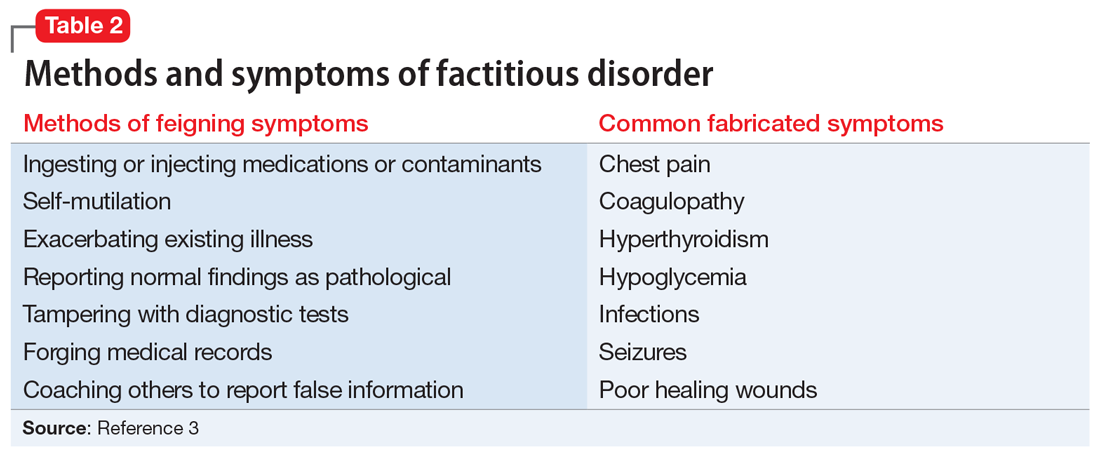
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
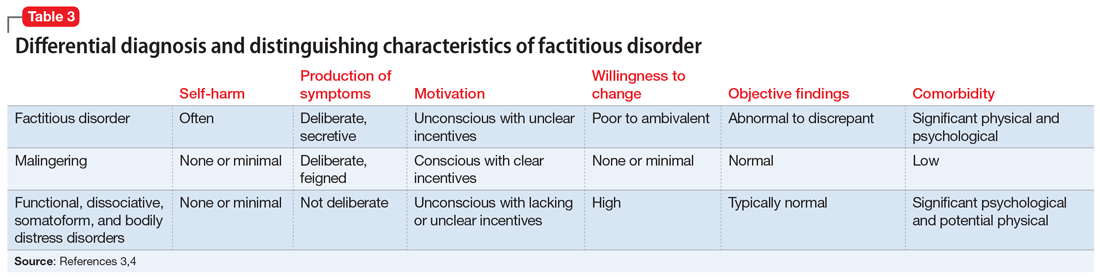
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
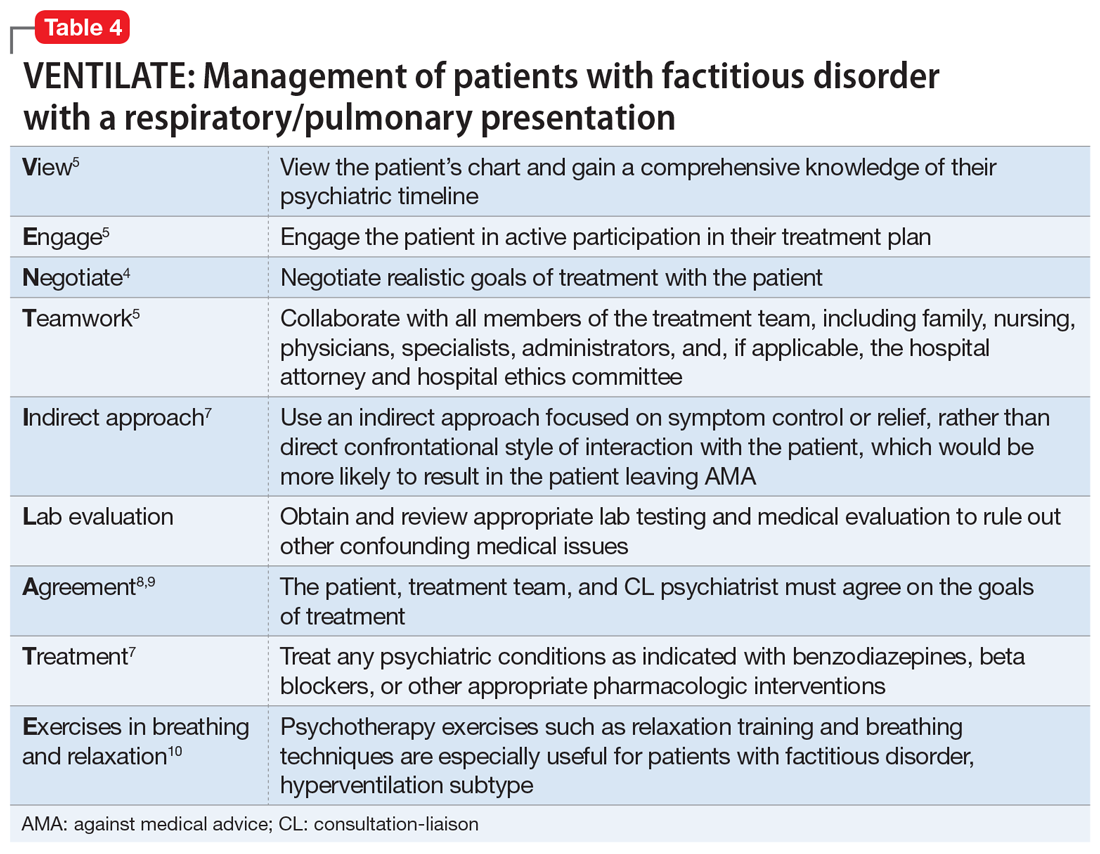
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
‘Where does it hurt?’: Primary care tips for common ortho problems
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2022
How to communicate effectively with patients when tension is high
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Homelessness seems to have greater link to death than common diseases, says physician
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
On a return visit about 10 years later, Dr. Perri went to the park and inquired about the men.
“I came to the horrible realization that all of these people were dead. All of them in 10 years,” he continued, speaking to an audience at the annual meeting of the American College of Physicians.
People experiencing homelessness don’t have to have such a grim health outlook, said Dr. Perri, who is medical director of the Center for Inclusion Health at the Allegheny Health Network in Pittsburgh.
During his talk, filled with jarring statistics on the health plight of those who struggle to stay sheltered, Dr. Perri said that many of the things that sicken and kill these people are the same things that sicken and kill others – liver disease, congestive heart failure, substance abuse. But the system isn’t equipped to handle the problems.
“Their needs are actually straightforward, they’re easy to describe,” he declared. “They’re known quantities. But the way that our systems respond, or don’t respond, to that creates the complexity. It’s the systems that are complex.”
Morbidity, mortality rates ‘go off a cliff’
A 2017 study in The Lancet compared morbidity and mortality in high-income countries, grouping people by their “level of deprivation.” The morbidity and mortality ticked higher with each deprivation level, but skyrocketed – nearly 10 times higher – for the group that included those experiencing homelessness or imprisonment, sex workers, and those with substance use disorders. As Dr. Perri put it, the rates “go off a cliff.”
Studies by the Boston Healthcare for the Homeless program have tracked mortality, and from 1988 to 1993 the average age at death was 47, so, “if you died while homeless, you probably died young.” Moreover, from their first contact to receive care through the program, to their death, only 25 months had elapsed.
“If there’s going to be an effective health care intervention, an acute one at least, you’ve got to get cracking,” Dr. Perri said.
Age at death has improved somewhat over time but drug overdose has become a much more common cause, Dr. Perri noted.
“There is utilitarian value in learning from people experiencing homelessness,” he said.
The same program looked at a high-risk cohort of 199 – those who went unsheltered for more than 6 months,were age 60 or older, or had certain serious health conditions, such as cirrhosis, substance abuse, and AIDS. A third of these people died within 5 years.
“There aren’t any other common diseases that I’m aware of that have statistics like that,” he said.
These people had an average of 31 emergency department visits a year and accounted for 871 hospitalizations. The estimated cost per-person, per-year was $22,000, while the average annual rent for a one-bedroom in Boston was $10,000.
“We’re hemorrhaging utilization around this population,” Dr. Perri said. “Maybe it makes sense to invest in something else other than acute health care. It’s not really yielding very much return on investment.”
Street medicine could be the answer
Housing First, a program to provide housing without the need to meet preconditions such as sobriety or passing background checks, has had a nonsignificant effect on mortality, substance use disorders, and mental health but has improved self-reported health status and quality of life. Analyses of the program suggest that better interventions are needed, Dr. Perri said.
Street medicine could be an answer, he said. Teams of medical staff go to where the people are, and the concept is intended as a continuous, cost-effective, flexible approach to care. Lehigh Valley Street Medicine in Pennsylvania has reported a reduction in emergency department visits and hospitalizations, Dr. Perri said. The programs are still too new to gauge the effect on actual health outcomes, but they hold the promise of being able to do so, he continued.
Curiosity about those experiencing homeless is a key first step in improving care, he said. The HOUSED BEDS tool, developed in Los Angeles, can help guide clinicians through their interactions with patients who do not have homes.
Dr. Perri said it is “enlightening” when you “express interest, genuine curiosity, about other people’s experiences.”
Catherine Kiley, MD, a retired internal medicine physician who volunteers as a preceptor for medical students in Cincinnati, said there is a void when it comes to teaching students about those experiencing homelessness.
“I don’t think there’s much of this type of discussion that they’re exposed to as part of medical education,” Dr. Kiley said. “Their experiences over time, as with most of medicine, will inform them.”
But the findings shared in the session show “how great the need is to speak out, speak up, about patients as people, and what they have to teach us.”
Dr. Perri disclosed no relevant financial relationships.
REPORTING FROM INTERNAL MEDICINE 2022
FDA clears mavacamten (Camzyos) for obstructive hypertrophic cardiomyopathy
The U.S. Food and Drug Administration has approved mavacamten (Camzyos, Bristol Myers Squibb) to improve functional capacity and symptoms in adults with symptomatic New York Heart Association (NYHA) class II-III obstructive hypertrophic cardiomyopathy (oHCM).
Mavacamten is the first FDA-approved allosteric and reversible inhibitor selective for cardiac myosin that targets the underlying pathophysiology of the genetic disorder. It’s available in 2.5-mg, 5-mg, 10-mg, and 15-mg capsules.
“The approval of Camzyos represents a significant milestone for appropriate symptomatic obstructive HCM patients and their families, who have long awaited a new treatment option for this chronic and progressive disease,” Anjali T. Owens, MD, medical director of the Center for Inherited Cardiac Disease and assistant professor of medicine, University of Pennsylvania, Philadelphia, said in a news release.
‘Revolutionary’ change
The approval of mavacamten was based on data from the pivotal EXPLORER-HCM and EXPLORER-LTE (long-term extension) trial of adults with symptomatic NYHA class II-III oHCM.
In EXPLORER-HCM, treatment with mavacamten over 30 weeks led to significant improvement in exercise capacity, left ventricular outflow tract (LVOT) obstruction, NYHA functional class, and health status, as reported by this news organization.
The safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase of EXPLORER-LTE were maintained in patients who continued treatment for a median of about 62 weeks.
Mavacamten represents “an almost revolutionary change” for the treatment of oHCM, Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis, said during a press briefing earlier this month at the American College of Cardiology 2022 Scientific Session earlier this month.
“Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” Dr. Guglin said.
The product information for mavacamten includes a boxed warning citing a risk for heart failure.
Echocardiogram assessments of left ventricular ejection fraction (LVEF) are required before and during treatment.
Starting mavacamten in patients with LVEF below 55% is not recommended and the drug should be interrupted if LVEF falls below 50% at any visit or if the patient experiences heart failure symptoms or worsening clinical status.
Concomitant use of mavacamten with certain cytochrome P450 inhibitors or discontinuation of certain cytochrome P450 inducers can increase the risk for heart failure attributable to systolic dysfunction. Therefore, its use is contraindicated in patients using moderate to strong CYP2C19 inhibitors or strong CYP3A4 inhibitors, and moderate to strong CYP2C19 inducers or moderate to strong CYP3A4 inducers.
Because of the risk for heart failure attributable to systolic dysfunction, mavacamten is only available through the Camzyos Risk Evaluation and Mitigation Strategy (REMS) Program.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved mavacamten (Camzyos, Bristol Myers Squibb) to improve functional capacity and symptoms in adults with symptomatic New York Heart Association (NYHA) class II-III obstructive hypertrophic cardiomyopathy (oHCM).
Mavacamten is the first FDA-approved allosteric and reversible inhibitor selective for cardiac myosin that targets the underlying pathophysiology of the genetic disorder. It’s available in 2.5-mg, 5-mg, 10-mg, and 15-mg capsules.
“The approval of Camzyos represents a significant milestone for appropriate symptomatic obstructive HCM patients and their families, who have long awaited a new treatment option for this chronic and progressive disease,” Anjali T. Owens, MD, medical director of the Center for Inherited Cardiac Disease and assistant professor of medicine, University of Pennsylvania, Philadelphia, said in a news release.
‘Revolutionary’ change
The approval of mavacamten was based on data from the pivotal EXPLORER-HCM and EXPLORER-LTE (long-term extension) trial of adults with symptomatic NYHA class II-III oHCM.
In EXPLORER-HCM, treatment with mavacamten over 30 weeks led to significant improvement in exercise capacity, left ventricular outflow tract (LVOT) obstruction, NYHA functional class, and health status, as reported by this news organization.
The safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase of EXPLORER-LTE were maintained in patients who continued treatment for a median of about 62 weeks.
Mavacamten represents “an almost revolutionary change” for the treatment of oHCM, Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis, said during a press briefing earlier this month at the American College of Cardiology 2022 Scientific Session earlier this month.
“Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” Dr. Guglin said.
The product information for mavacamten includes a boxed warning citing a risk for heart failure.
Echocardiogram assessments of left ventricular ejection fraction (LVEF) are required before and during treatment.
Starting mavacamten in patients with LVEF below 55% is not recommended and the drug should be interrupted if LVEF falls below 50% at any visit or if the patient experiences heart failure symptoms or worsening clinical status.
Concomitant use of mavacamten with certain cytochrome P450 inhibitors or discontinuation of certain cytochrome P450 inducers can increase the risk for heart failure attributable to systolic dysfunction. Therefore, its use is contraindicated in patients using moderate to strong CYP2C19 inhibitors or strong CYP3A4 inhibitors, and moderate to strong CYP2C19 inducers or moderate to strong CYP3A4 inducers.
Because of the risk for heart failure attributable to systolic dysfunction, mavacamten is only available through the Camzyos Risk Evaluation and Mitigation Strategy (REMS) Program.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved mavacamten (Camzyos, Bristol Myers Squibb) to improve functional capacity and symptoms in adults with symptomatic New York Heart Association (NYHA) class II-III obstructive hypertrophic cardiomyopathy (oHCM).
Mavacamten is the first FDA-approved allosteric and reversible inhibitor selective for cardiac myosin that targets the underlying pathophysiology of the genetic disorder. It’s available in 2.5-mg, 5-mg, 10-mg, and 15-mg capsules.
“The approval of Camzyos represents a significant milestone for appropriate symptomatic obstructive HCM patients and their families, who have long awaited a new treatment option for this chronic and progressive disease,” Anjali T. Owens, MD, medical director of the Center for Inherited Cardiac Disease and assistant professor of medicine, University of Pennsylvania, Philadelphia, said in a news release.
‘Revolutionary’ change
The approval of mavacamten was based on data from the pivotal EXPLORER-HCM and EXPLORER-LTE (long-term extension) trial of adults with symptomatic NYHA class II-III oHCM.
In EXPLORER-HCM, treatment with mavacamten over 30 weeks led to significant improvement in exercise capacity, left ventricular outflow tract (LVOT) obstruction, NYHA functional class, and health status, as reported by this news organization.
The safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase of EXPLORER-LTE were maintained in patients who continued treatment for a median of about 62 weeks.
Mavacamten represents “an almost revolutionary change” for the treatment of oHCM, Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis, said during a press briefing earlier this month at the American College of Cardiology 2022 Scientific Session earlier this month.
“Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” Dr. Guglin said.
The product information for mavacamten includes a boxed warning citing a risk for heart failure.
Echocardiogram assessments of left ventricular ejection fraction (LVEF) are required before and during treatment.
Starting mavacamten in patients with LVEF below 55% is not recommended and the drug should be interrupted if LVEF falls below 50% at any visit or if the patient experiences heart failure symptoms or worsening clinical status.
Concomitant use of mavacamten with certain cytochrome P450 inhibitors or discontinuation of certain cytochrome P450 inducers can increase the risk for heart failure attributable to systolic dysfunction. Therefore, its use is contraindicated in patients using moderate to strong CYP2C19 inhibitors or strong CYP3A4 inhibitors, and moderate to strong CYP2C19 inducers or moderate to strong CYP3A4 inducers.
Because of the risk for heart failure attributable to systolic dysfunction, mavacamten is only available through the Camzyos Risk Evaluation and Mitigation Strategy (REMS) Program.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
FDA warns of pump defect with Medtronic HVAD system
Patients implanted with the Medtronic HeartWare ventricular assist device (HVAD) System who develop pump thrombosis could have a welding defect in the internal pump causing the pump to malfunction, the Food and Drug Administration said in a letter to health care professionals.
Medtronic has sent providers an urgent medical device notice about the pump weld defect and is trying to identify which HVAD pumps are affected.
The Medtronic HVAD System was approved as a bridge to heart transplantation in 2012. Since then, it has been fraught with problems.
This past June, the company announced it was stopping all sales of the device and advised physicians to stop implanting it, as reported by this news organization.
Pump thrombosis
Medtronic has received complaints of suspected pump thrombosis in three patients with the HVAD System.
All three patients presented with one or more of the following signs or symptoms: grinding sound, transient power spikes on log files and high watt alarms, elevated lactate dehydrogenase, and low motor speed resulting in low perfusion or dizziness or lightheadedness.
Inspection of the returned pumps in these three cases identified a malfunction of the internal pump. The pumps were exchanged in all three patients. Two patients died after the pump exchange.
The FDA does not recommend the elective removal of properly functioning systems.
“Decisions about removing or exchanging the Medtronic HVAD System should be made by health care providers and patients on a case-by-case basis, considering the patient’s clinical status and surgical risks,” the agency advised.
Patients who present with one or more of the signs or symptoms of pump thrombosis should be first treated for pump thrombosis.
If symptoms fail to resolve, providers may consider whether the patient is a candidate for pump exchange, heart transplant, or pump explant for recovery, taking into account the patient’s clinical condition and surgical risks.
For patients with any of the signs and symptoms of pump thrombosis, logfiles from the controller should be uploaded to Medtronic.
The FDA is working with Medtronic to monitor for any adverse events related to pump weld defects and ensure patients with the HVAD implant continue to receive appropriate follow-up monitoring.
Problems related to the Medtronic HVAD System should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Patients implanted with the Medtronic HeartWare ventricular assist device (HVAD) System who develop pump thrombosis could have a welding defect in the internal pump causing the pump to malfunction, the Food and Drug Administration said in a letter to health care professionals.
Medtronic has sent providers an urgent medical device notice about the pump weld defect and is trying to identify which HVAD pumps are affected.
The Medtronic HVAD System was approved as a bridge to heart transplantation in 2012. Since then, it has been fraught with problems.
This past June, the company announced it was stopping all sales of the device and advised physicians to stop implanting it, as reported by this news organization.
Pump thrombosis
Medtronic has received complaints of suspected pump thrombosis in three patients with the HVAD System.
All three patients presented with one or more of the following signs or symptoms: grinding sound, transient power spikes on log files and high watt alarms, elevated lactate dehydrogenase, and low motor speed resulting in low perfusion or dizziness or lightheadedness.
Inspection of the returned pumps in these three cases identified a malfunction of the internal pump. The pumps were exchanged in all three patients. Two patients died after the pump exchange.
The FDA does not recommend the elective removal of properly functioning systems.
“Decisions about removing or exchanging the Medtronic HVAD System should be made by health care providers and patients on a case-by-case basis, considering the patient’s clinical status and surgical risks,” the agency advised.
Patients who present with one or more of the signs or symptoms of pump thrombosis should be first treated for pump thrombosis.
If symptoms fail to resolve, providers may consider whether the patient is a candidate for pump exchange, heart transplant, or pump explant for recovery, taking into account the patient’s clinical condition and surgical risks.
For patients with any of the signs and symptoms of pump thrombosis, logfiles from the controller should be uploaded to Medtronic.
The FDA is working with Medtronic to monitor for any adverse events related to pump weld defects and ensure patients with the HVAD implant continue to receive appropriate follow-up monitoring.
Problems related to the Medtronic HVAD System should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Patients implanted with the Medtronic HeartWare ventricular assist device (HVAD) System who develop pump thrombosis could have a welding defect in the internal pump causing the pump to malfunction, the Food and Drug Administration said in a letter to health care professionals.
Medtronic has sent providers an urgent medical device notice about the pump weld defect and is trying to identify which HVAD pumps are affected.
The Medtronic HVAD System was approved as a bridge to heart transplantation in 2012. Since then, it has been fraught with problems.
This past June, the company announced it was stopping all sales of the device and advised physicians to stop implanting it, as reported by this news organization.
Pump thrombosis
Medtronic has received complaints of suspected pump thrombosis in three patients with the HVAD System.
All three patients presented with one or more of the following signs or symptoms: grinding sound, transient power spikes on log files and high watt alarms, elevated lactate dehydrogenase, and low motor speed resulting in low perfusion or dizziness or lightheadedness.
Inspection of the returned pumps in these three cases identified a malfunction of the internal pump. The pumps were exchanged in all three patients. Two patients died after the pump exchange.
The FDA does not recommend the elective removal of properly functioning systems.
“Decisions about removing or exchanging the Medtronic HVAD System should be made by health care providers and patients on a case-by-case basis, considering the patient’s clinical status and surgical risks,” the agency advised.
Patients who present with one or more of the signs or symptoms of pump thrombosis should be first treated for pump thrombosis.
If symptoms fail to resolve, providers may consider whether the patient is a candidate for pump exchange, heart transplant, or pump explant for recovery, taking into account the patient’s clinical condition and surgical risks.
For patients with any of the signs and symptoms of pump thrombosis, logfiles from the controller should be uploaded to Medtronic.
The FDA is working with Medtronic to monitor for any adverse events related to pump weld defects and ensure patients with the HVAD implant continue to receive appropriate follow-up monitoring.
Problems related to the Medtronic HVAD System should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.





