User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Medicaid coverage of HPV vaccine in adults: Implications in dermatology
, according to the authors of a review of Medicaid policies across all 50 states.
The human papillomavirus (HPV) vaccine is approved for people aged 9-45 years, for preventing genital, cervical, anal, and oropharyngeal cancers, and genital warts. And the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices recommends routine vaccination with the HPV vaccine for individuals aged 9-26 years, with “shared clinical decision-making” recommended for vaccination of those aged 27-45 years, wrote Nathaniel Goldman of New York Medical College, Valhalla, and coauthors, from the University of Missouri–Kansas City and Harvard Medical School, Boston.
A total of 33 states offered formal statewide Medicaid coverage policies that were accessible online or through the state’s Medicaid office. Another 11 states provided coverage through Medicaid managed care organizations, and 4 states had HPV vaccination as part of their formal Medicaid adult vaccination programs.
Overall, 43 states covered HPV vaccination through age 45 years with no need for prior authorization, and another 4 states (Ohio, Maine, Nebraska, and New York) provided coverage with prior authorization for adults older than 26 years.
The study findings were limited by the use of Medicaid coverage only, the researchers noted. Consequently, patients eligible for HPV vaccination who are uninsured or have other types of insurance may face additional barriers in the form of high costs, given that the current retail price is $250-$350 per shot for the three-shot series, the researchers noted.
However, the results suggest that Medicaid coverage for HPV vaccination may inform dermatologists’ recommendations for patients at increased risk, they said. More research is needed to “better identify dermatology patients at risk for new HPV infection and ways to improve vaccination rates in these vulnerable individuals,” they added.
Vaccine discussions are important in dermatology
“Dermatologists care for patients who may be an increased risk of vaccine-preventable illnesses, either from a skin disease or a dermatology medication,” corresponding author Megan H. Noe, MD, a dermatologist at Brigham and Women’s Hospital, and assistant professor of dermatology, Harvard Medical School, Boston, said in an interview. “Over the last several years, we have seen that all physicians, whether they provide vaccinations or not, can play an important role in discussing vaccines with their patients,” she said.
“Vaccines can be cost-prohibitive for patients without insurance coverage, so we hope that dermatologists will be more likely to recommend the HPV vaccine to patients 27-45 years of age if they know that it is likely covered by insurance,” Dr. Noe noted.
However, “time may be a barrier for many dermatologists who have many important things to discuss with patients during their appointments,” she said. “We are currently working on developing educational information to help facilitate this conversation,” she added.
Looking ahead, she said that “additional research is necessary to create vaccine guidelines specific to dermatology patients and dermatology medications, so we can provide clear recommendations to our patients and ensure appropriate insurance coverage for all necessary vaccines.”
Vaccine discussions
“I think it’s great that many Medicaid plans are covering HPV vaccination,” said Karl Saardi, MD, of the department of dermatology, George Washington University, Washington, who was asked to comment on the study. “I routinely recommend [vaccination] for patients who have viral warts, since it does lead to improvement in some cases,” Dr. Saardi, who was not involved in the current study, said in an interview. “Although we don’t have the HPV vaccines in our clinic for administration, my experience has been that patients are very open to discussing it with their primary care doctors.”
Although the upper age range continues to rise, “I think getting younger people vaccinated will also prove to be important,” said Dr. Saardi, director of the inpatient dermatology service at the George Washington University Hospital.
The point made in the current study about the importance of HPV vaccination in patients with hidradenitis suppurativa is also crucial, he added. “Since chronic skin inflammation in hidradenitis drives squamous cell carcinoma, reducing the impact of HPV on such cancers makes perfect sense.”
The study received no outside funding. Dr. Noe disclosed grants from Boehringer Ingelheim unrelated to the current study. Dr. Saardi had no financial conflicts to disclose.
, according to the authors of a review of Medicaid policies across all 50 states.
The human papillomavirus (HPV) vaccine is approved for people aged 9-45 years, for preventing genital, cervical, anal, and oropharyngeal cancers, and genital warts. And the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices recommends routine vaccination with the HPV vaccine for individuals aged 9-26 years, with “shared clinical decision-making” recommended for vaccination of those aged 27-45 years, wrote Nathaniel Goldman of New York Medical College, Valhalla, and coauthors, from the University of Missouri–Kansas City and Harvard Medical School, Boston.
A total of 33 states offered formal statewide Medicaid coverage policies that were accessible online or through the state’s Medicaid office. Another 11 states provided coverage through Medicaid managed care organizations, and 4 states had HPV vaccination as part of their formal Medicaid adult vaccination programs.
Overall, 43 states covered HPV vaccination through age 45 years with no need for prior authorization, and another 4 states (Ohio, Maine, Nebraska, and New York) provided coverage with prior authorization for adults older than 26 years.
The study findings were limited by the use of Medicaid coverage only, the researchers noted. Consequently, patients eligible for HPV vaccination who are uninsured or have other types of insurance may face additional barriers in the form of high costs, given that the current retail price is $250-$350 per shot for the three-shot series, the researchers noted.
However, the results suggest that Medicaid coverage for HPV vaccination may inform dermatologists’ recommendations for patients at increased risk, they said. More research is needed to “better identify dermatology patients at risk for new HPV infection and ways to improve vaccination rates in these vulnerable individuals,” they added.
Vaccine discussions are important in dermatology
“Dermatologists care for patients who may be an increased risk of vaccine-preventable illnesses, either from a skin disease or a dermatology medication,” corresponding author Megan H. Noe, MD, a dermatologist at Brigham and Women’s Hospital, and assistant professor of dermatology, Harvard Medical School, Boston, said in an interview. “Over the last several years, we have seen that all physicians, whether they provide vaccinations or not, can play an important role in discussing vaccines with their patients,” she said.
“Vaccines can be cost-prohibitive for patients without insurance coverage, so we hope that dermatologists will be more likely to recommend the HPV vaccine to patients 27-45 years of age if they know that it is likely covered by insurance,” Dr. Noe noted.
However, “time may be a barrier for many dermatologists who have many important things to discuss with patients during their appointments,” she said. “We are currently working on developing educational information to help facilitate this conversation,” she added.
Looking ahead, she said that “additional research is necessary to create vaccine guidelines specific to dermatology patients and dermatology medications, so we can provide clear recommendations to our patients and ensure appropriate insurance coverage for all necessary vaccines.”
Vaccine discussions
“I think it’s great that many Medicaid plans are covering HPV vaccination,” said Karl Saardi, MD, of the department of dermatology, George Washington University, Washington, who was asked to comment on the study. “I routinely recommend [vaccination] for patients who have viral warts, since it does lead to improvement in some cases,” Dr. Saardi, who was not involved in the current study, said in an interview. “Although we don’t have the HPV vaccines in our clinic for administration, my experience has been that patients are very open to discussing it with their primary care doctors.”
Although the upper age range continues to rise, “I think getting younger people vaccinated will also prove to be important,” said Dr. Saardi, director of the inpatient dermatology service at the George Washington University Hospital.
The point made in the current study about the importance of HPV vaccination in patients with hidradenitis suppurativa is also crucial, he added. “Since chronic skin inflammation in hidradenitis drives squamous cell carcinoma, reducing the impact of HPV on such cancers makes perfect sense.”
The study received no outside funding. Dr. Noe disclosed grants from Boehringer Ingelheim unrelated to the current study. Dr. Saardi had no financial conflicts to disclose.
, according to the authors of a review of Medicaid policies across all 50 states.
The human papillomavirus (HPV) vaccine is approved for people aged 9-45 years, for preventing genital, cervical, anal, and oropharyngeal cancers, and genital warts. And the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices recommends routine vaccination with the HPV vaccine for individuals aged 9-26 years, with “shared clinical decision-making” recommended for vaccination of those aged 27-45 years, wrote Nathaniel Goldman of New York Medical College, Valhalla, and coauthors, from the University of Missouri–Kansas City and Harvard Medical School, Boston.
A total of 33 states offered formal statewide Medicaid coverage policies that were accessible online or through the state’s Medicaid office. Another 11 states provided coverage through Medicaid managed care organizations, and 4 states had HPV vaccination as part of their formal Medicaid adult vaccination programs.
Overall, 43 states covered HPV vaccination through age 45 years with no need for prior authorization, and another 4 states (Ohio, Maine, Nebraska, and New York) provided coverage with prior authorization for adults older than 26 years.
The study findings were limited by the use of Medicaid coverage only, the researchers noted. Consequently, patients eligible for HPV vaccination who are uninsured or have other types of insurance may face additional barriers in the form of high costs, given that the current retail price is $250-$350 per shot for the three-shot series, the researchers noted.
However, the results suggest that Medicaid coverage for HPV vaccination may inform dermatologists’ recommendations for patients at increased risk, they said. More research is needed to “better identify dermatology patients at risk for new HPV infection and ways to improve vaccination rates in these vulnerable individuals,” they added.
Vaccine discussions are important in dermatology
“Dermatologists care for patients who may be an increased risk of vaccine-preventable illnesses, either from a skin disease or a dermatology medication,” corresponding author Megan H. Noe, MD, a dermatologist at Brigham and Women’s Hospital, and assistant professor of dermatology, Harvard Medical School, Boston, said in an interview. “Over the last several years, we have seen that all physicians, whether they provide vaccinations or not, can play an important role in discussing vaccines with their patients,” she said.
“Vaccines can be cost-prohibitive for patients without insurance coverage, so we hope that dermatologists will be more likely to recommend the HPV vaccine to patients 27-45 years of age if they know that it is likely covered by insurance,” Dr. Noe noted.
However, “time may be a barrier for many dermatologists who have many important things to discuss with patients during their appointments,” she said. “We are currently working on developing educational information to help facilitate this conversation,” she added.
Looking ahead, she said that “additional research is necessary to create vaccine guidelines specific to dermatology patients and dermatology medications, so we can provide clear recommendations to our patients and ensure appropriate insurance coverage for all necessary vaccines.”
Vaccine discussions
“I think it’s great that many Medicaid plans are covering HPV vaccination,” said Karl Saardi, MD, of the department of dermatology, George Washington University, Washington, who was asked to comment on the study. “I routinely recommend [vaccination] for patients who have viral warts, since it does lead to improvement in some cases,” Dr. Saardi, who was not involved in the current study, said in an interview. “Although we don’t have the HPV vaccines in our clinic for administration, my experience has been that patients are very open to discussing it with their primary care doctors.”
Although the upper age range continues to rise, “I think getting younger people vaccinated will also prove to be important,” said Dr. Saardi, director of the inpatient dermatology service at the George Washington University Hospital.
The point made in the current study about the importance of HPV vaccination in patients with hidradenitis suppurativa is also crucial, he added. “Since chronic skin inflammation in hidradenitis drives squamous cell carcinoma, reducing the impact of HPV on such cancers makes perfect sense.”
The study received no outside funding. Dr. Noe disclosed grants from Boehringer Ingelheim unrelated to the current study. Dr. Saardi had no financial conflicts to disclose.
FROM JAMA DERMATOLOGY
Physicians react: Climate change and other social issues
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
The danger when doctors don’t get mental health help
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
Med students dismayed that residency match process won’t change
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
Lego introduces first character with vitiligo
The
The character appears with the customizable array of players to assemble for a table football team.
It’s the latest representation of the disease as toymakers diversify their lines.
In May 2022, Mattel released a Ken doll with vitiligo after a Barbie with vitiligo was released in 2020. Rainbow High and other toy makers also have character versions.
The Lego addition follows a big summer medically for vitiligo as the first treatment was approved for repigmentation. In July, a cream formulation of ruxolitinib (Opzelura), a Janus kinase inhibitor, became the first repigmentation treatment approved by the Food and Drug Administration for nonsegmental vitiligo, the most common form of the disease.
Vitiligo is estimated to affect 1.9 million–2.8 million adults in the United States and more than 100 million people worldwide. It cuts across races and genders and can be psychologically painful for many who live with it.
John E. Harris, MD, director of the Vitiligo Clinic and Research Center at the University of Massachusetts, Worcester, wrote about the Lego character in his blog “Speaking of Vitiligo ...” saying: “I could not be more excited. This new minifigure also serves as a way to educate both children and adults who are not familiar with vitiligo about the disease.”
He noted that until recently vitiligo representation in kids’ toys has been limited. “By adding diversity such as representations of vitiligo in toys, it can help remove stigmas associated with vitiligo and give children more options that they can relate to.”
Erika Page of Richmond, Va., who founded and edits the vitiligo blog “Living Dappled,” told this news organization she was thrilled to see the new Lego character.
“Growing up I didn’t know anyone who looked like me, let alone a toy or a character,” she said. The message the representations send is important not just for the kids but for the parents of kids with vitiligo who want to help their kids in any way they can.
Ms. Page was diagnosed with vitiligo at age 7 and struggled emotionally in her high school and college years when she often looked in the mirror, saw “giraffe-like” spots, and cried. Over time she lost 100% of her pigment to the condition and today at age 33, lives with universal vitiligo or overall very pale skin.
She founded the Living Dappled blog 6 years ago to help people with the disease feel less alone. The Lego character will also help with that, she said.
“Growing up with vitiligo was so isolating and you felt so different,” Ms. Page said. “Today we see billboards and models and dolls and now Legos that look like us. I hope this is a first of many to come for Lego.”
Dr. Harris and Ms. Page declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The
The character appears with the customizable array of players to assemble for a table football team.
It’s the latest representation of the disease as toymakers diversify their lines.
In May 2022, Mattel released a Ken doll with vitiligo after a Barbie with vitiligo was released in 2020. Rainbow High and other toy makers also have character versions.
The Lego addition follows a big summer medically for vitiligo as the first treatment was approved for repigmentation. In July, a cream formulation of ruxolitinib (Opzelura), a Janus kinase inhibitor, became the first repigmentation treatment approved by the Food and Drug Administration for nonsegmental vitiligo, the most common form of the disease.
Vitiligo is estimated to affect 1.9 million–2.8 million adults in the United States and more than 100 million people worldwide. It cuts across races and genders and can be psychologically painful for many who live with it.
John E. Harris, MD, director of the Vitiligo Clinic and Research Center at the University of Massachusetts, Worcester, wrote about the Lego character in his blog “Speaking of Vitiligo ...” saying: “I could not be more excited. This new minifigure also serves as a way to educate both children and adults who are not familiar with vitiligo about the disease.”
He noted that until recently vitiligo representation in kids’ toys has been limited. “By adding diversity such as representations of vitiligo in toys, it can help remove stigmas associated with vitiligo and give children more options that they can relate to.”
Erika Page of Richmond, Va., who founded and edits the vitiligo blog “Living Dappled,” told this news organization she was thrilled to see the new Lego character.
“Growing up I didn’t know anyone who looked like me, let alone a toy or a character,” she said. The message the representations send is important not just for the kids but for the parents of kids with vitiligo who want to help their kids in any way they can.
Ms. Page was diagnosed with vitiligo at age 7 and struggled emotionally in her high school and college years when she often looked in the mirror, saw “giraffe-like” spots, and cried. Over time she lost 100% of her pigment to the condition and today at age 33, lives with universal vitiligo or overall very pale skin.
She founded the Living Dappled blog 6 years ago to help people with the disease feel less alone. The Lego character will also help with that, she said.
“Growing up with vitiligo was so isolating and you felt so different,” Ms. Page said. “Today we see billboards and models and dolls and now Legos that look like us. I hope this is a first of many to come for Lego.”
Dr. Harris and Ms. Page declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The
The character appears with the customizable array of players to assemble for a table football team.
It’s the latest representation of the disease as toymakers diversify their lines.
In May 2022, Mattel released a Ken doll with vitiligo after a Barbie with vitiligo was released in 2020. Rainbow High and other toy makers also have character versions.
The Lego addition follows a big summer medically for vitiligo as the first treatment was approved for repigmentation. In July, a cream formulation of ruxolitinib (Opzelura), a Janus kinase inhibitor, became the first repigmentation treatment approved by the Food and Drug Administration for nonsegmental vitiligo, the most common form of the disease.
Vitiligo is estimated to affect 1.9 million–2.8 million adults in the United States and more than 100 million people worldwide. It cuts across races and genders and can be psychologically painful for many who live with it.
John E. Harris, MD, director of the Vitiligo Clinic and Research Center at the University of Massachusetts, Worcester, wrote about the Lego character in his blog “Speaking of Vitiligo ...” saying: “I could not be more excited. This new minifigure also serves as a way to educate both children and adults who are not familiar with vitiligo about the disease.”
He noted that until recently vitiligo representation in kids’ toys has been limited. “By adding diversity such as representations of vitiligo in toys, it can help remove stigmas associated with vitiligo and give children more options that they can relate to.”
Erika Page of Richmond, Va., who founded and edits the vitiligo blog “Living Dappled,” told this news organization she was thrilled to see the new Lego character.
“Growing up I didn’t know anyone who looked like me, let alone a toy or a character,” she said. The message the representations send is important not just for the kids but for the parents of kids with vitiligo who want to help their kids in any way they can.
Ms. Page was diagnosed with vitiligo at age 7 and struggled emotionally in her high school and college years when she often looked in the mirror, saw “giraffe-like” spots, and cried. Over time she lost 100% of her pigment to the condition and today at age 33, lives with universal vitiligo or overall very pale skin.
She founded the Living Dappled blog 6 years ago to help people with the disease feel less alone. The Lego character will also help with that, she said.
“Growing up with vitiligo was so isolating and you felt so different,” Ms. Page said. “Today we see billboards and models and dolls and now Legos that look like us. I hope this is a first of many to come for Lego.”
Dr. Harris and Ms. Page declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Practical pearls guide treatment of psoriasis in tricky areas
LAS VEGAS – With the right regimen, a majority of patients with psoriasis can achieve at least a Psoriasis Area and Severity Index (PASI) 75 score, Jennifer Soung, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
The array of treatment options includes mainstay topicals, new nonsteroidals, traditional oral systemics, new oral systemics, biologics, and light therapy, said Dr. Soung, director of clinical research at Harbor-UCLA Medical Center, Santa Ana, Calif. However, she said.
For these areas, make sure the diagnosis of psoriasis is correct, to avoid wasting time on the wrong course of treatment, Dr. Soung emphasized.
Scalp strategies
The scalp is often the first area of the body affected by psoriasis, and patients with severe scalp psoriasis may have minimal plaques on the body, Dr. Soung said. However, a differential diagnosis should include seborrheic dermatitis, she noted.
For most cases of scalp psoriasis, “start with localized topical treatment,” such as vitamin D and corticosteroid combination therapy, or excimer laser, Dr. Soung advised.
Systemic treatments with demonstrated effectiveness on scalp psoriasis in post hoc analyses of patients with moderate to severe plaque psoriasis include adalimumab, etanercept, ixekizumab, and secukinumab. Studies specifically focused on treatment of scalp psoriasis have shown success with secukinumab and apremilast, she noted.
Roflumilast foam, 0.3%, is in development and is an emerging option for scalp psoriasis. (A cream formulation of roflumilast, a topical phosphodiesterase 4 inhibitor, was approved for treatment of plaque psoriasis in July 2022.) A phase 2b study of roflumilast foam showed that approximately one-third of patients with scalp psoriasis achieved a status of clear based on scalp-investigator global assessment, compared with approximately 3% of those on vehicle, and similar results were seen in a recently completed phase 3 trial for scalp and body psoriasis, she added.
Facial psoriasis
Patients with facial psoriasis tend to be younger, and they may have more severe disease overall, Dr. Soung said. Given the sensitivity of facial skin, “it is nice to have a nonsteroidal option,” she noted. Current novel nonsteroidal therapies include a cream formulation of tapinarof, an aryl hydrocarbon receptor agonist, which was approved earlier this year for plaque psoriasis in adults, and roflumilast cream. Vitamin D and topical calcineurin inhibitors are options as well, she said.
Intertriginous tricks
Intertriginous (inverse) psoriasis is distinct from other areas in that the plaques are usually smooth and well-demarcated, with little or no scaling, Dr. Soung said. Erosions or signs of maceration may be present. The prevalence of inverse psoriasis is approximately 30%, but the prevalence on external genitalia is 80%, she noted. For inverse psoriasis, topical corticosteroids can result in adverse events such as poor wound healing and skin fragility, and some patients resist the idea of a steroid and don’t adhere to the medication, she added. Dr. Soung recommended topical corticosteroids for the short term, and topical calcineurin inhibitors or calcipotriol for the long term.
New topical options for inverse psoriasis include tapinarof and roflumilast, Dr. Soung said. For tapinarof, the phase 3 PSOARING program included assessment of tolerability in sensitive skin areas and found little to no irritation. Similarly, treatment with roflumilast cream was effective and well tolerated by patients with intertriginous plaque psoriasis in the DERMIS-1 and DERMIS-2 studies, she said.
Genital psoriasis
Ask patients with psoriasis about genital psoriasis, because they often are too embarrassed to provide that information on their own, said Dr. Soung. In fact, 63% of patients with psoriasis report ever experiencing genital psoriasis, but it often goes undiagnosed and undertreated, which has a significant impact on patient quality of life and sexual health.
A differential diagnosis of genital psoriasis should include dermatitis, tinea or candidiasis, and even squamous cell carcinoma, she noted. Other considerations include fixed drug eruption, lichen nitidus, lichen sclerosus, and scabies.
Dr. Soung’s first line of treatment for genital psoriasis is low-potency topical corticosteroids for 2-4 weeks. If long-term topical therapy is needed, alternatives include calcineurin inhibitors and vitamin D analogs, she said. The new topicals roflumilast and tapinarof are options as well, she said.
For those patients with severe and extensive genital psoriasis, consider systemic therapy, possibly with ixekizumab or secukinumab, she added. Patients with moderate to severe genital psoriasis treated with apremilast have shown improvement at week 16, in an ongoing clinical trial, she noted.
Palmoplantar involvement
For patients with palmar plantar psoriasis, “don’t underestimate the impact on quality of life,” said Dr. Soung. Approximately 12%-16% of patients with psoriasis report palmoplantar involvement, she noted.
Palmoplantar psoriasis can be stubborn, and many patients will need combination therapy with topicals and systemics, she said. “I am very curious about how well our new topical nonsteroidals will work in these areas,” she added.
Dr. Soung starts patients with palmoplantar psoriasis with a “potent to super-potent” twice daily topical corticosteroid, with or without occlusion. Her first-line systemic therapy is acitretin, 10-50 mg daily. However, keep in mind that acitretin is contraindicated in pregnancy, and also may cause side effects including cheilitis, alopecia, and peeling skin, she cautioned.
During the question and answer session, Dr. Soung was asked whether she routinely biopsies patients with palmoplantar psoriasis. “Not always,” was her answer. Instead, she looks for clues elsewhere on the body to confirm the diagnosis.
Nail know-how
Approximately 23%-27% of patients with psoriasis experience nail involvement, said Dr. Soung. Nail psoriasis can appear on the nail plate as pitting, onycholysis, or subungual hyperkeratosis, or in the nail bed as splinter hemorrhages or oil spots, she said.
For patients with psoriasis of the nails only, Dr. Soung described the use of high-potency topical corticosteroids, with or without calcipotriol. In her experience, she said that intralesional steroids for nail psoriasis are torturous to patients. For patients who have failed topical therapy or have psoriasis in other areas, with or without psoriatic arthritis, she advised the use of either IL-17 antagonists (secukinumab, ixekizumab, brodalumab) or IL-23 antagonists (risankizumab, guselkumab).
Dr. Soung disclosed serving as a consultant or advisor for Arcutis, Bristol Myers Squibb Company, Dermavant, and Novartis. She also disclosed serving as a speaker or member of the speakers’ bureau for AbbVie, Amgen, Arcutis, Bristol Myers Squibb Company, Celgene, Leo Pharma, Eli Lilly, Novartis, Ortho Dermatologics, Pfizer, Regeneron, and Sanofi, as well as research funding from AbbVie, Amgen, Arcutis, Castle Biosciences, Dermavant, KoBio, Kyowa Kirin, Leo Pharma, Eli Lilly, Novartis, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – With the right regimen, a majority of patients with psoriasis can achieve at least a Psoriasis Area and Severity Index (PASI) 75 score, Jennifer Soung, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
The array of treatment options includes mainstay topicals, new nonsteroidals, traditional oral systemics, new oral systemics, biologics, and light therapy, said Dr. Soung, director of clinical research at Harbor-UCLA Medical Center, Santa Ana, Calif. However, she said.
For these areas, make sure the diagnosis of psoriasis is correct, to avoid wasting time on the wrong course of treatment, Dr. Soung emphasized.
Scalp strategies
The scalp is often the first area of the body affected by psoriasis, and patients with severe scalp psoriasis may have minimal plaques on the body, Dr. Soung said. However, a differential diagnosis should include seborrheic dermatitis, she noted.
For most cases of scalp psoriasis, “start with localized topical treatment,” such as vitamin D and corticosteroid combination therapy, or excimer laser, Dr. Soung advised.
Systemic treatments with demonstrated effectiveness on scalp psoriasis in post hoc analyses of patients with moderate to severe plaque psoriasis include adalimumab, etanercept, ixekizumab, and secukinumab. Studies specifically focused on treatment of scalp psoriasis have shown success with secukinumab and apremilast, she noted.
Roflumilast foam, 0.3%, is in development and is an emerging option for scalp psoriasis. (A cream formulation of roflumilast, a topical phosphodiesterase 4 inhibitor, was approved for treatment of plaque psoriasis in July 2022.) A phase 2b study of roflumilast foam showed that approximately one-third of patients with scalp psoriasis achieved a status of clear based on scalp-investigator global assessment, compared with approximately 3% of those on vehicle, and similar results were seen in a recently completed phase 3 trial for scalp and body psoriasis, she added.
Facial psoriasis
Patients with facial psoriasis tend to be younger, and they may have more severe disease overall, Dr. Soung said. Given the sensitivity of facial skin, “it is nice to have a nonsteroidal option,” she noted. Current novel nonsteroidal therapies include a cream formulation of tapinarof, an aryl hydrocarbon receptor agonist, which was approved earlier this year for plaque psoriasis in adults, and roflumilast cream. Vitamin D and topical calcineurin inhibitors are options as well, she said.
Intertriginous tricks
Intertriginous (inverse) psoriasis is distinct from other areas in that the plaques are usually smooth and well-demarcated, with little or no scaling, Dr. Soung said. Erosions or signs of maceration may be present. The prevalence of inverse psoriasis is approximately 30%, but the prevalence on external genitalia is 80%, she noted. For inverse psoriasis, topical corticosteroids can result in adverse events such as poor wound healing and skin fragility, and some patients resist the idea of a steroid and don’t adhere to the medication, she added. Dr. Soung recommended topical corticosteroids for the short term, and topical calcineurin inhibitors or calcipotriol for the long term.
New topical options for inverse psoriasis include tapinarof and roflumilast, Dr. Soung said. For tapinarof, the phase 3 PSOARING program included assessment of tolerability in sensitive skin areas and found little to no irritation. Similarly, treatment with roflumilast cream was effective and well tolerated by patients with intertriginous plaque psoriasis in the DERMIS-1 and DERMIS-2 studies, she said.
Genital psoriasis
Ask patients with psoriasis about genital psoriasis, because they often are too embarrassed to provide that information on their own, said Dr. Soung. In fact, 63% of patients with psoriasis report ever experiencing genital psoriasis, but it often goes undiagnosed and undertreated, which has a significant impact on patient quality of life and sexual health.
A differential diagnosis of genital psoriasis should include dermatitis, tinea or candidiasis, and even squamous cell carcinoma, she noted. Other considerations include fixed drug eruption, lichen nitidus, lichen sclerosus, and scabies.
Dr. Soung’s first line of treatment for genital psoriasis is low-potency topical corticosteroids for 2-4 weeks. If long-term topical therapy is needed, alternatives include calcineurin inhibitors and vitamin D analogs, she said. The new topicals roflumilast and tapinarof are options as well, she said.
For those patients with severe and extensive genital psoriasis, consider systemic therapy, possibly with ixekizumab or secukinumab, she added. Patients with moderate to severe genital psoriasis treated with apremilast have shown improvement at week 16, in an ongoing clinical trial, she noted.
Palmoplantar involvement
For patients with palmar plantar psoriasis, “don’t underestimate the impact on quality of life,” said Dr. Soung. Approximately 12%-16% of patients with psoriasis report palmoplantar involvement, she noted.
Palmoplantar psoriasis can be stubborn, and many patients will need combination therapy with topicals and systemics, she said. “I am very curious about how well our new topical nonsteroidals will work in these areas,” she added.
Dr. Soung starts patients with palmoplantar psoriasis with a “potent to super-potent” twice daily topical corticosteroid, with or without occlusion. Her first-line systemic therapy is acitretin, 10-50 mg daily. However, keep in mind that acitretin is contraindicated in pregnancy, and also may cause side effects including cheilitis, alopecia, and peeling skin, she cautioned.
During the question and answer session, Dr. Soung was asked whether she routinely biopsies patients with palmoplantar psoriasis. “Not always,” was her answer. Instead, she looks for clues elsewhere on the body to confirm the diagnosis.
Nail know-how
Approximately 23%-27% of patients with psoriasis experience nail involvement, said Dr. Soung. Nail psoriasis can appear on the nail plate as pitting, onycholysis, or subungual hyperkeratosis, or in the nail bed as splinter hemorrhages or oil spots, she said.
For patients with psoriasis of the nails only, Dr. Soung described the use of high-potency topical corticosteroids, with or without calcipotriol. In her experience, she said that intralesional steroids for nail psoriasis are torturous to patients. For patients who have failed topical therapy or have psoriasis in other areas, with or without psoriatic arthritis, she advised the use of either IL-17 antagonists (secukinumab, ixekizumab, brodalumab) or IL-23 antagonists (risankizumab, guselkumab).
Dr. Soung disclosed serving as a consultant or advisor for Arcutis, Bristol Myers Squibb Company, Dermavant, and Novartis. She also disclosed serving as a speaker or member of the speakers’ bureau for AbbVie, Amgen, Arcutis, Bristol Myers Squibb Company, Celgene, Leo Pharma, Eli Lilly, Novartis, Ortho Dermatologics, Pfizer, Regeneron, and Sanofi, as well as research funding from AbbVie, Amgen, Arcutis, Castle Biosciences, Dermavant, KoBio, Kyowa Kirin, Leo Pharma, Eli Lilly, Novartis, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – With the right regimen, a majority of patients with psoriasis can achieve at least a Psoriasis Area and Severity Index (PASI) 75 score, Jennifer Soung, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
The array of treatment options includes mainstay topicals, new nonsteroidals, traditional oral systemics, new oral systemics, biologics, and light therapy, said Dr. Soung, director of clinical research at Harbor-UCLA Medical Center, Santa Ana, Calif. However, she said.
For these areas, make sure the diagnosis of psoriasis is correct, to avoid wasting time on the wrong course of treatment, Dr. Soung emphasized.
Scalp strategies
The scalp is often the first area of the body affected by psoriasis, and patients with severe scalp psoriasis may have minimal plaques on the body, Dr. Soung said. However, a differential diagnosis should include seborrheic dermatitis, she noted.
For most cases of scalp psoriasis, “start with localized topical treatment,” such as vitamin D and corticosteroid combination therapy, or excimer laser, Dr. Soung advised.
Systemic treatments with demonstrated effectiveness on scalp psoriasis in post hoc analyses of patients with moderate to severe plaque psoriasis include adalimumab, etanercept, ixekizumab, and secukinumab. Studies specifically focused on treatment of scalp psoriasis have shown success with secukinumab and apremilast, she noted.
Roflumilast foam, 0.3%, is in development and is an emerging option for scalp psoriasis. (A cream formulation of roflumilast, a topical phosphodiesterase 4 inhibitor, was approved for treatment of plaque psoriasis in July 2022.) A phase 2b study of roflumilast foam showed that approximately one-third of patients with scalp psoriasis achieved a status of clear based on scalp-investigator global assessment, compared with approximately 3% of those on vehicle, and similar results were seen in a recently completed phase 3 trial for scalp and body psoriasis, she added.
Facial psoriasis
Patients with facial psoriasis tend to be younger, and they may have more severe disease overall, Dr. Soung said. Given the sensitivity of facial skin, “it is nice to have a nonsteroidal option,” she noted. Current novel nonsteroidal therapies include a cream formulation of tapinarof, an aryl hydrocarbon receptor agonist, which was approved earlier this year for plaque psoriasis in adults, and roflumilast cream. Vitamin D and topical calcineurin inhibitors are options as well, she said.
Intertriginous tricks
Intertriginous (inverse) psoriasis is distinct from other areas in that the plaques are usually smooth and well-demarcated, with little or no scaling, Dr. Soung said. Erosions or signs of maceration may be present. The prevalence of inverse psoriasis is approximately 30%, but the prevalence on external genitalia is 80%, she noted. For inverse psoriasis, topical corticosteroids can result in adverse events such as poor wound healing and skin fragility, and some patients resist the idea of a steroid and don’t adhere to the medication, she added. Dr. Soung recommended topical corticosteroids for the short term, and topical calcineurin inhibitors or calcipotriol for the long term.
New topical options for inverse psoriasis include tapinarof and roflumilast, Dr. Soung said. For tapinarof, the phase 3 PSOARING program included assessment of tolerability in sensitive skin areas and found little to no irritation. Similarly, treatment with roflumilast cream was effective and well tolerated by patients with intertriginous plaque psoriasis in the DERMIS-1 and DERMIS-2 studies, she said.
Genital psoriasis
Ask patients with psoriasis about genital psoriasis, because they often are too embarrassed to provide that information on their own, said Dr. Soung. In fact, 63% of patients with psoriasis report ever experiencing genital psoriasis, but it often goes undiagnosed and undertreated, which has a significant impact on patient quality of life and sexual health.
A differential diagnosis of genital psoriasis should include dermatitis, tinea or candidiasis, and even squamous cell carcinoma, she noted. Other considerations include fixed drug eruption, lichen nitidus, lichen sclerosus, and scabies.
Dr. Soung’s first line of treatment for genital psoriasis is low-potency topical corticosteroids for 2-4 weeks. If long-term topical therapy is needed, alternatives include calcineurin inhibitors and vitamin D analogs, she said. The new topicals roflumilast and tapinarof are options as well, she said.
For those patients with severe and extensive genital psoriasis, consider systemic therapy, possibly with ixekizumab or secukinumab, she added. Patients with moderate to severe genital psoriasis treated with apremilast have shown improvement at week 16, in an ongoing clinical trial, she noted.
Palmoplantar involvement
For patients with palmar plantar psoriasis, “don’t underestimate the impact on quality of life,” said Dr. Soung. Approximately 12%-16% of patients with psoriasis report palmoplantar involvement, she noted.
Palmoplantar psoriasis can be stubborn, and many patients will need combination therapy with topicals and systemics, she said. “I am very curious about how well our new topical nonsteroidals will work in these areas,” she added.
Dr. Soung starts patients with palmoplantar psoriasis with a “potent to super-potent” twice daily topical corticosteroid, with or without occlusion. Her first-line systemic therapy is acitretin, 10-50 mg daily. However, keep in mind that acitretin is contraindicated in pregnancy, and also may cause side effects including cheilitis, alopecia, and peeling skin, she cautioned.
During the question and answer session, Dr. Soung was asked whether she routinely biopsies patients with palmoplantar psoriasis. “Not always,” was her answer. Instead, she looks for clues elsewhere on the body to confirm the diagnosis.
Nail know-how
Approximately 23%-27% of patients with psoriasis experience nail involvement, said Dr. Soung. Nail psoriasis can appear on the nail plate as pitting, onycholysis, or subungual hyperkeratosis, or in the nail bed as splinter hemorrhages or oil spots, she said.
For patients with psoriasis of the nails only, Dr. Soung described the use of high-potency topical corticosteroids, with or without calcipotriol. In her experience, she said that intralesional steroids for nail psoriasis are torturous to patients. For patients who have failed topical therapy or have psoriasis in other areas, with or without psoriatic arthritis, she advised the use of either IL-17 antagonists (secukinumab, ixekizumab, brodalumab) or IL-23 antagonists (risankizumab, guselkumab).
Dr. Soung disclosed serving as a consultant or advisor for Arcutis, Bristol Myers Squibb Company, Dermavant, and Novartis. She also disclosed serving as a speaker or member of the speakers’ bureau for AbbVie, Amgen, Arcutis, Bristol Myers Squibb Company, Celgene, Leo Pharma, Eli Lilly, Novartis, Ortho Dermatologics, Pfizer, Regeneron, and Sanofi, as well as research funding from AbbVie, Amgen, Arcutis, Castle Biosciences, Dermavant, KoBio, Kyowa Kirin, Leo Pharma, Eli Lilly, Novartis, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
AT INNOVATIONS IN DERMATOLOGY
What does it take for men to embrace cosmetic treatments?
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
HPV vaccine effectiveness dependent on age at receipt
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Academic dermatology: Gender diversity advances as some gaps persist
, according to a recent cross-sectional study.
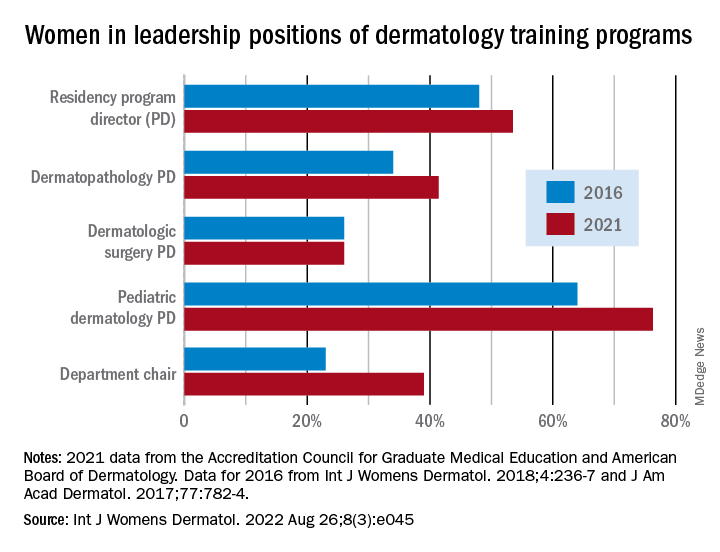
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
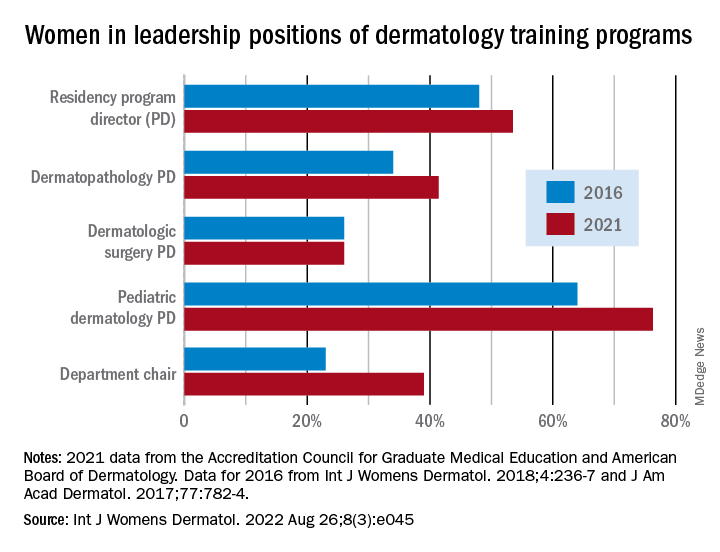
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
FROM INTERNATIONAL JOURNAL OF WOMEN’S DERMATOLOGY
Surgical site dressing turns blue when it needs changing
Surgical site infections are one of the top causes of postoperative morbidity and death worldwide, but there is little agreement and much debate over the most effective wound dressing to improve outcomes and reduce the health care burden.
Recent clinical trials have indicated that transparent, semiocclusive films have advantages over gauze held by adhesive tape.
But current transparent film bandages may become dislodged during activities such as showering, say authors of a pilot study published in the Journal of Wound Care. Patients may not realize the bandage has been disrupted, which can lead to infection.
.
“Clinicians, patients, and caregivers are alerted to the loss of dressing integrity and can replace the dressing when any portion of the perimeter changes to a blue [color],” the authors explain. “In addition, the dressing turns blue when the central pad is saturated with fluid, allowing the patient or provider to change the dressing.”
DSD is indicated for wounds that have low levels of exudate.
Two transparent film dressings compared
Researchers recruited 20 patients from the general population in Pittsburgh, for a small pilot study to test DSD against a comparator film dressing (3M Tegaderm + Pad). The volunteers received “a small stipend,” according to the paper.
A 1.5-centimeter incision was made in both forearms of each volunteer. The forearms were randomized regarding which got which bandage. Both bandages have been cleared by the U.S. Food and Drug Administration as nonsignificant-risk devices.
Volunteers were instructed to wear the dressing and continue their typical activities of daily living.
The average age of the volunteers was 52 years (range, 20-80 years). Among the 20 volunteers, 11 reported no comorbidities, and 45% reported at least one comorbidity.
Most of the volunteers favored DSD over the comparator in a postoperative survey – 75% to 25%, according to the report.
The wear time between the two transparent dressings across all subjects was 1.4 days. There was no difference in wear time, logged by the volunteers, between the two groups.
There were no infectious complications, the paper states.
The maker, DrySee (Houston), which holds three patents on the product, supported the research with an unrestricted grant.
DrySee CEO Brad Greer told this news organization, “With DrySee, you know when to change your dressing. All other dressings look the same wet, saturated, or dry.”
He said the study confirms what they have seen in practice, adding that the product is unique.
“No one else in the world has this technology,” Mr. Greer said.
Surgeons want to see more data
Heather Evans, MD, a general surgeon with the Medical University of South Carolina, MUSC Health, Charleston, who was not involved with the study, praised the color-indicator design and said she liked the bandage’s narrow indication for low-exudate wounds.
She said in an interview, “It’s a lot to put on a layperson to suddenly know how to take care of wounds when you leave the hospital.”
Giving them the confidence that their wound is safe if the blue doesn’t appear “is a really cool concept,” she said.
She said that, although the volunteers included some elderly people and people with conditions such as diabetes that could affect wound healing, the bandage needs to be tested with a bigger trial to see if it is effective outside controlled conditions.
She also said that some occlusive dressings will be more durable and stay on days longer than DSD or the comparator, which may affect the choice for some.
“The average length of dressing time in this study was less than 2 days,” she pointed out.
Jim Rickert, MD, an orthopedic surgeon with Indiana University Health Bedford, who was not involved with the study, agreed that any surgical or wound dressing, including transparent films, can become dislodged, and said, “This type of product has promise but this is a small pilot study. I would want to see results from a trial of actual surgical patients to see if this type of dressing did indeed decrease post-op infections compared to standard dressing materials.”
Not all are convinced either that there is a need to be filled or that DSD will be the right solution.
Therese Duane, MD, a general surgeon with Texas Health Harris Methodist Fort Worth, who was not part of the study, said in an interview that she “has no issues with the current products.”
She added that more information is needed before considering DSD a better solution, including animal studies and use “on very sick patients.”
“Twenty volunteers with cuts on their arm is barely a start for comparison,” she said.
The authors, led by Kristy Breisinger, a research analyst with the SerenaGroup Research Foundation in Cambridge, Mass., acknowledged the limitations, including the small sample size and that the trial was conducted at only one institution. Additionally, the analysis is based on descriptive statistics.
They write that the trial design was chosen “to simulate a real-world setting that is not always achievable in animal studies.”
The research was sponsored by an unrestricted grant from the maker of DSD, DrySee Inc., in Houston.
Mr. Greer is DrySee’s CEO. The authors and Dr. Duane, Dr. Rickert, and Dr. Evans declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Surgical site infections are one of the top causes of postoperative morbidity and death worldwide, but there is little agreement and much debate over the most effective wound dressing to improve outcomes and reduce the health care burden.
Recent clinical trials have indicated that transparent, semiocclusive films have advantages over gauze held by adhesive tape.
But current transparent film bandages may become dislodged during activities such as showering, say authors of a pilot study published in the Journal of Wound Care. Patients may not realize the bandage has been disrupted, which can lead to infection.
.
“Clinicians, patients, and caregivers are alerted to the loss of dressing integrity and can replace the dressing when any portion of the perimeter changes to a blue [color],” the authors explain. “In addition, the dressing turns blue when the central pad is saturated with fluid, allowing the patient or provider to change the dressing.”
DSD is indicated for wounds that have low levels of exudate.
Two transparent film dressings compared
Researchers recruited 20 patients from the general population in Pittsburgh, for a small pilot study to test DSD against a comparator film dressing (3M Tegaderm + Pad). The volunteers received “a small stipend,” according to the paper.
A 1.5-centimeter incision was made in both forearms of each volunteer. The forearms were randomized regarding which got which bandage. Both bandages have been cleared by the U.S. Food and Drug Administration as nonsignificant-risk devices.
Volunteers were instructed to wear the dressing and continue their typical activities of daily living.
The average age of the volunteers was 52 years (range, 20-80 years). Among the 20 volunteers, 11 reported no comorbidities, and 45% reported at least one comorbidity.
Most of the volunteers favored DSD over the comparator in a postoperative survey – 75% to 25%, according to the report.
The wear time between the two transparent dressings across all subjects was 1.4 days. There was no difference in wear time, logged by the volunteers, between the two groups.
There were no infectious complications, the paper states.
The maker, DrySee (Houston), which holds three patents on the product, supported the research with an unrestricted grant.
DrySee CEO Brad Greer told this news organization, “With DrySee, you know when to change your dressing. All other dressings look the same wet, saturated, or dry.”
He said the study confirms what they have seen in practice, adding that the product is unique.
“No one else in the world has this technology,” Mr. Greer said.
Surgeons want to see more data
Heather Evans, MD, a general surgeon with the Medical University of South Carolina, MUSC Health, Charleston, who was not involved with the study, praised the color-indicator design and said she liked the bandage’s narrow indication for low-exudate wounds.
She said in an interview, “It’s a lot to put on a layperson to suddenly know how to take care of wounds when you leave the hospital.”
Giving them the confidence that their wound is safe if the blue doesn’t appear “is a really cool concept,” she said.
She said that, although the volunteers included some elderly people and people with conditions such as diabetes that could affect wound healing, the bandage needs to be tested with a bigger trial to see if it is effective outside controlled conditions.
She also said that some occlusive dressings will be more durable and stay on days longer than DSD or the comparator, which may affect the choice for some.
“The average length of dressing time in this study was less than 2 days,” she pointed out.
Jim Rickert, MD, an orthopedic surgeon with Indiana University Health Bedford, who was not involved with the study, agreed that any surgical or wound dressing, including transparent films, can become dislodged, and said, “This type of product has promise but this is a small pilot study. I would want to see results from a trial of actual surgical patients to see if this type of dressing did indeed decrease post-op infections compared to standard dressing materials.”
Not all are convinced either that there is a need to be filled or that DSD will be the right solution.
Therese Duane, MD, a general surgeon with Texas Health Harris Methodist Fort Worth, who was not part of the study, said in an interview that she “has no issues with the current products.”
She added that more information is needed before considering DSD a better solution, including animal studies and use “on very sick patients.”
“Twenty volunteers with cuts on their arm is barely a start for comparison,” she said.
The authors, led by Kristy Breisinger, a research analyst with the SerenaGroup Research Foundation in Cambridge, Mass., acknowledged the limitations, including the small sample size and that the trial was conducted at only one institution. Additionally, the analysis is based on descriptive statistics.
They write that the trial design was chosen “to simulate a real-world setting that is not always achievable in animal studies.”
The research was sponsored by an unrestricted grant from the maker of DSD, DrySee Inc., in Houston.
Mr. Greer is DrySee’s CEO. The authors and Dr. Duane, Dr. Rickert, and Dr. Evans declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Surgical site infections are one of the top causes of postoperative morbidity and death worldwide, but there is little agreement and much debate over the most effective wound dressing to improve outcomes and reduce the health care burden.
Recent clinical trials have indicated that transparent, semiocclusive films have advantages over gauze held by adhesive tape.
But current transparent film bandages may become dislodged during activities such as showering, say authors of a pilot study published in the Journal of Wound Care. Patients may not realize the bandage has been disrupted, which can lead to infection.
.
“Clinicians, patients, and caregivers are alerted to the loss of dressing integrity and can replace the dressing when any portion of the perimeter changes to a blue [color],” the authors explain. “In addition, the dressing turns blue when the central pad is saturated with fluid, allowing the patient or provider to change the dressing.”
DSD is indicated for wounds that have low levels of exudate.
Two transparent film dressings compared
Researchers recruited 20 patients from the general population in Pittsburgh, for a small pilot study to test DSD against a comparator film dressing (3M Tegaderm + Pad). The volunteers received “a small stipend,” according to the paper.
A 1.5-centimeter incision was made in both forearms of each volunteer. The forearms were randomized regarding which got which bandage. Both bandages have been cleared by the U.S. Food and Drug Administration as nonsignificant-risk devices.
Volunteers were instructed to wear the dressing and continue their typical activities of daily living.
The average age of the volunteers was 52 years (range, 20-80 years). Among the 20 volunteers, 11 reported no comorbidities, and 45% reported at least one comorbidity.
Most of the volunteers favored DSD over the comparator in a postoperative survey – 75% to 25%, according to the report.
The wear time between the two transparent dressings across all subjects was 1.4 days. There was no difference in wear time, logged by the volunteers, between the two groups.
There were no infectious complications, the paper states.
The maker, DrySee (Houston), which holds three patents on the product, supported the research with an unrestricted grant.
DrySee CEO Brad Greer told this news organization, “With DrySee, you know when to change your dressing. All other dressings look the same wet, saturated, or dry.”
He said the study confirms what they have seen in practice, adding that the product is unique.
“No one else in the world has this technology,” Mr. Greer said.
Surgeons want to see more data
Heather Evans, MD, a general surgeon with the Medical University of South Carolina, MUSC Health, Charleston, who was not involved with the study, praised the color-indicator design and said she liked the bandage’s narrow indication for low-exudate wounds.
She said in an interview, “It’s a lot to put on a layperson to suddenly know how to take care of wounds when you leave the hospital.”
Giving them the confidence that their wound is safe if the blue doesn’t appear “is a really cool concept,” she said.
She said that, although the volunteers included some elderly people and people with conditions such as diabetes that could affect wound healing, the bandage needs to be tested with a bigger trial to see if it is effective outside controlled conditions.
She also said that some occlusive dressings will be more durable and stay on days longer than DSD or the comparator, which may affect the choice for some.
“The average length of dressing time in this study was less than 2 days,” she pointed out.
Jim Rickert, MD, an orthopedic surgeon with Indiana University Health Bedford, who was not involved with the study, agreed that any surgical or wound dressing, including transparent films, can become dislodged, and said, “This type of product has promise but this is a small pilot study. I would want to see results from a trial of actual surgical patients to see if this type of dressing did indeed decrease post-op infections compared to standard dressing materials.”
Not all are convinced either that there is a need to be filled or that DSD will be the right solution.
Therese Duane, MD, a general surgeon with Texas Health Harris Methodist Fort Worth, who was not part of the study, said in an interview that she “has no issues with the current products.”
She added that more information is needed before considering DSD a better solution, including animal studies and use “on very sick patients.”
“Twenty volunteers with cuts on their arm is barely a start for comparison,” she said.
The authors, led by Kristy Breisinger, a research analyst with the SerenaGroup Research Foundation in Cambridge, Mass., acknowledged the limitations, including the small sample size and that the trial was conducted at only one institution. Additionally, the analysis is based on descriptive statistics.
They write that the trial design was chosen “to simulate a real-world setting that is not always achievable in animal studies.”
The research was sponsored by an unrestricted grant from the maker of DSD, DrySee Inc., in Houston.
Mr. Greer is DrySee’s CEO. The authors and Dr. Duane, Dr. Rickert, and Dr. Evans declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF WOUND CARE