User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Intermittent fasting plus exercise a good option for fatty liver
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the combined approach did not give significantly added benefit, compared with fasting alone, the researchers report.
Eighty patients with NAFLD were randomized to one of four lifestyle strategies (alternate-day fasting, aerobic exercise, both, or neither) for 3 months.
The primary outcome was change in intrahepatic triglyceride (IHTG) content from baseline to study end, measured by magnetic resonance imaging proton density fat fraction.
The results suggest that “combining intermittent fasting with exercise is effective for reducing hepatic steatosis [fatty liver] in patients with NAFLD but may offer no additional benefit versus fasting alone,” Mark Ezpeleta, PhD, formerly at the University of Illinois, Chicago, and now at the University of Colorado Anschutz Medical Campus, and colleagues conclude.
“Our findings also indicate that the combination intervention was effective for reducing body weight, fat mass, waist circumference, [the liver enzyme alanine transaminase (ALT)], fasting insulin, [and] insulin resistance and increasing insulin sensitivity, among patients with obesity and NAFLD versus controls,” the group reports.
“When we compared the results of our study groups, we saw clearly that the most improved patients were in the group that followed the alternate-day fasting diet and exercised 5 days a week,” senior author Krista A. Varady, PhD, professor of nutrition, University of Illinois, said in a press release from the university.
“The people who only dieted or only exercised did not see the same improvements,” she added, “which reinforces the importance of these two relatively inexpensive lifestyle modifications on overall health and on combating chronic diseases like fatty liver disease.”
Moreover, “alternate-day fasting and exercise interventions can be difficult for people to stick to, and in prior studies we have seen significant dropout,” she noted. “It was very interesting to see that in this trial we had very high adherence to the interventions.”
The study was recently published in Cell Metabolism.
An estimated 65% of people with obesity have NAFLD, or fat in the liver that is not the result of excessive alcohol consumption, which is strongly related to the development of insulin resistance and type 2 diabetes, the group writes.
Thiazolidinediones such as pioglitazone reduce hepatic steatosis, but there is mounting concern about the weight-gaining effect of these compounds.
Recent attention has focused on lifestyle interventions to resolve hepatic steatosis, and previous trials showed that alternate-day fasting was effective for certain outcomes in NAFLD, but those studies did not measure changes in IHTG content or include an exercise intervention.
The researchers enrolled 80 adults with obesity and NAFLD and randomized them to one of four groups for 3 months:
- Alternate day fasting group: Participants were instructed to consume 600 kcal at dinner between 5 PM and 8 PM on a fasting day alternating with food as desired on a feasting day.
- Exercise group: A 60-minute moderate-intensity aerobic exercise session 5 times a week.
- Fasting plus exercise group.
- Control group (no intervention).
Participants were age 23-65 (mean age, 44) and 81% were women.
Half were Hispanic, and the rest were Black (30%), White (11%), or Asian (9%).
They had a mean weight of 99 kg (218 lb) and a mean body mass index of 36 kg/m2.
Dropout rates were minimal in the combination group (0%) and fasting groups (5%) and moderately high in the exercise group (25%).
IHTG content was reduced by a significantly greater amount in the combination group (–5.48%) than in the exercise alone group (–1.30%; P = .02) or in the control group (–0.17%; P < .01) and by a greater amount than in the fasting alone group, although this was not significant (–2.25%; P = .05).
Lean mass, aspartate transaminase (AST), A1c, blood pressure, plasma lipids, liver fibrosis score, and hepatokines (fetuin-A, FGF-21, and selenoprotein P) did not differ between groups.
Researchers acknowledge that although the combination intervention resulted in improved NAFLD parameters, IHTG and ALT did not reach the normal range.
Participants likely had early stage NAFLD (their baseline IHTG was in the 16% to 18% range, where 5% to 33% is mild steatosis) and they were likely highly motivated (indicated by the low dropout rate), so the findings may not be generalizable.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. Dr. Varady has reported receiving author fees from the Hachette Book Group for the book entitled “The Every Other Day Diet.” The other authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CELL METABOLISM
Metformin linked to reductions in COVID-19 viral load
These findings add to a multitude of benefits the drug has been shown to have in COVID infection.
COVID-OUT did not meet its primary endpoint, but it did show important secondary outcomes including a 42% reduction in ED visits and in hospitalizations and/or deaths by day 14, and a 58% reduction in hospitalizations/death by day 28. A further subanalysis has shown a 42% reduction in long COVID, compared with placebo.
“In this phase 3 randomized controlled trial, metformin showed prevention of severe COVID, prevention of long COVID, and an antiviral effect, and this is consistent with other data,” said coauthor Carolyn Bramante, MD, University of Minnesota, Minneapolis, in presenting the findings at the Conference on Retroviruses & Opportunistic Infections.
Study details
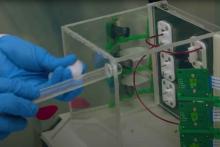
For the new subanalysis, the authors further evaluated the effects of metformin treatment on SARS-CoV-2 viral load.
A total of 1,323 patients in the study, enrolled at six centers, were randomized to treatment either with metformin 1,000 mg per day on days 2-5 and 1,500 mg per day on days 6 to 14 (n = 187), or to ivermectin 390-470 mcg/kg per day for 3 days (n = 187), fluvoxamine 50 mg twice daily for 14 days, and/or an exact-matching placebo in a 2 x 3 factorial trial design.
The subanalysis on viral load included 483 patients from the trial who were treated with metformin versus 462 who received placebo, who were all enrolled within 3 days of a documented SARS-CoV-2 infection and less than 7 days after symptom onset.
The patients had a median age of 46 years, and all had either overweight or obesity. Only about 2% had diabetes, and only patients considered low-risk were excluded from the trial, including those under age 30 and those with a body mass index under 25.
About half of patients had received a primary vaccine and about 5% had received a vaccine booster. SARS-CoV-2 variants that were prominent during the study included Alpha, Delta, and Omicron.
The viral samples available on days 1, 5, and 10 showed a mean change in viral load from baseline to follow-up; the viral load was significantly lower with metformin versus placebo (–0.64 log10 copies/mL), representing a 4.4-fold greater decrease in viral load with metformin.
The mean rate of undetectable SARS-CoV-2 viral load at day 5 was 49.9% in the metformin group versus 54.6% in the placebo group (odds ratio, 1.235), and the undetectable rate at day 10 was 14.3% in the metformin group and 22.6% in the placebo group (OR, 1.663; P = .003).
An increased antiviral effect corresponded with increases in metformin dosing on days 6 through 14. Furthermore, the antiviral effect became stronger when metformin was started earlier in the course of infection.
Of note, the antiviral effect was more pronounced among those who were not vaccinated (mean, –0.95 log copies/mL), compared with the vaccinated (mean, –0.39 log copies/mL).
The antiviral effect with metformin was similar to that seen with nirmatrelvir at day 5 and was greater than nirmatrelvir at day 10.
No similar relationships in SARS-CoV-2 viral load were observed between ivermectin or fluvoxamine and placebo.
The findings are consistent with results of other recent observational studies, including research showing metformin to be associated with reductions in COVID-19 severity in patients with prediabetes, Dr. Bramante noted.
The authors’ previous analysis looking at long COVID in the COVID-OUT study showed that metformin treatment during acute COVID significantly reduced the risk for a diagnosis of long COVID versus placebo at 300 days following randomization, with a hazard ratio of 0.59 after adjustment for the study drug and vaccination at baseline.
Dr. Bramante noted that metformin’s potential antiviral properties have long been speculated, with some of the earliest research on the drug suggesting less severe outcomes in influenza, and more recently, RNA assays suggesting effects against other RNA viruses, including the Zika virus.
In terms of COVID, Dr. Bramante noted that the drug has plenty of potentially favorable benefits.
“Metformin is very safe and is known to have very few contraindications, so the next steps could be to consider looking at this in terms of a combination therapy,” she said.
‘Data from other studies are conflicting’
Commenting on the study, Diane V. Havlir, MD, cautioned that “metformin is currently not recommended in treatment guidelines, [and] data from other studies are conflicting; side effects can be an issue, and the study presented here was in a select population,” she said in an interview.
However, “what is both new and interesting in this presentation is the reduction of viral load, which [was observed] in the samples collected not only on days 1-5, but also days 6-14,” said Dr. Havlir, who is professor and associate chair of clinical research, department of medicine, and chief of the division of HIV, infectious diseases and global medicine and director of the AIDS Research Institute at the University of California, San Francisco.
Key questions the findings raise include whether the results correlate with clinical outcomes or transmission, and whether the findings are generalizable to other populations and settings, Dr. Havlir said.
Ultimately, “we need to continue to pursue all aspects of outpatient treatments for COVID to address questions like these for new and existing agents,” she added.
The trial received funding from the Parsemus Foundation, the Rainwater Charitable Foundation, Fast Grants, and the United Health Group. The authors and Dr. Havlir disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
These findings add to a multitude of benefits the drug has been shown to have in COVID infection.
COVID-OUT did not meet its primary endpoint, but it did show important secondary outcomes including a 42% reduction in ED visits and in hospitalizations and/or deaths by day 14, and a 58% reduction in hospitalizations/death by day 28. A further subanalysis has shown a 42% reduction in long COVID, compared with placebo.
“In this phase 3 randomized controlled trial, metformin showed prevention of severe COVID, prevention of long COVID, and an antiviral effect, and this is consistent with other data,” said coauthor Carolyn Bramante, MD, University of Minnesota, Minneapolis, in presenting the findings at the Conference on Retroviruses & Opportunistic Infections.
Study details
For the new subanalysis, the authors further evaluated the effects of metformin treatment on SARS-CoV-2 viral load.
A total of 1,323 patients in the study, enrolled at six centers, were randomized to treatment either with metformin 1,000 mg per day on days 2-5 and 1,500 mg per day on days 6 to 14 (n = 187), or to ivermectin 390-470 mcg/kg per day for 3 days (n = 187), fluvoxamine 50 mg twice daily for 14 days, and/or an exact-matching placebo in a 2 x 3 factorial trial design.
The subanalysis on viral load included 483 patients from the trial who were treated with metformin versus 462 who received placebo, who were all enrolled within 3 days of a documented SARS-CoV-2 infection and less than 7 days after symptom onset.
The patients had a median age of 46 years, and all had either overweight or obesity. Only about 2% had diabetes, and only patients considered low-risk were excluded from the trial, including those under age 30 and those with a body mass index under 25.
About half of patients had received a primary vaccine and about 5% had received a vaccine booster. SARS-CoV-2 variants that were prominent during the study included Alpha, Delta, and Omicron.
The viral samples available on days 1, 5, and 10 showed a mean change in viral load from baseline to follow-up; the viral load was significantly lower with metformin versus placebo (–0.64 log10 copies/mL), representing a 4.4-fold greater decrease in viral load with metformin.
The mean rate of undetectable SARS-CoV-2 viral load at day 5 was 49.9% in the metformin group versus 54.6% in the placebo group (odds ratio, 1.235), and the undetectable rate at day 10 was 14.3% in the metformin group and 22.6% in the placebo group (OR, 1.663; P = .003).
An increased antiviral effect corresponded with increases in metformin dosing on days 6 through 14. Furthermore, the antiviral effect became stronger when metformin was started earlier in the course of infection.
Of note, the antiviral effect was more pronounced among those who were not vaccinated (mean, –0.95 log copies/mL), compared with the vaccinated (mean, –0.39 log copies/mL).
The antiviral effect with metformin was similar to that seen with nirmatrelvir at day 5 and was greater than nirmatrelvir at day 10.
No similar relationships in SARS-CoV-2 viral load were observed between ivermectin or fluvoxamine and placebo.
The findings are consistent with results of other recent observational studies, including research showing metformin to be associated with reductions in COVID-19 severity in patients with prediabetes, Dr. Bramante noted.
The authors’ previous analysis looking at long COVID in the COVID-OUT study showed that metformin treatment during acute COVID significantly reduced the risk for a diagnosis of long COVID versus placebo at 300 days following randomization, with a hazard ratio of 0.59 after adjustment for the study drug and vaccination at baseline.
Dr. Bramante noted that metformin’s potential antiviral properties have long been speculated, with some of the earliest research on the drug suggesting less severe outcomes in influenza, and more recently, RNA assays suggesting effects against other RNA viruses, including the Zika virus.
In terms of COVID, Dr. Bramante noted that the drug has plenty of potentially favorable benefits.
“Metformin is very safe and is known to have very few contraindications, so the next steps could be to consider looking at this in terms of a combination therapy,” she said.
‘Data from other studies are conflicting’
Commenting on the study, Diane V. Havlir, MD, cautioned that “metformin is currently not recommended in treatment guidelines, [and] data from other studies are conflicting; side effects can be an issue, and the study presented here was in a select population,” she said in an interview.
However, “what is both new and interesting in this presentation is the reduction of viral load, which [was observed] in the samples collected not only on days 1-5, but also days 6-14,” said Dr. Havlir, who is professor and associate chair of clinical research, department of medicine, and chief of the division of HIV, infectious diseases and global medicine and director of the AIDS Research Institute at the University of California, San Francisco.
Key questions the findings raise include whether the results correlate with clinical outcomes or transmission, and whether the findings are generalizable to other populations and settings, Dr. Havlir said.
Ultimately, “we need to continue to pursue all aspects of outpatient treatments for COVID to address questions like these for new and existing agents,” she added.
The trial received funding from the Parsemus Foundation, the Rainwater Charitable Foundation, Fast Grants, and the United Health Group. The authors and Dr. Havlir disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
These findings add to a multitude of benefits the drug has been shown to have in COVID infection.
COVID-OUT did not meet its primary endpoint, but it did show important secondary outcomes including a 42% reduction in ED visits and in hospitalizations and/or deaths by day 14, and a 58% reduction in hospitalizations/death by day 28. A further subanalysis has shown a 42% reduction in long COVID, compared with placebo.
“In this phase 3 randomized controlled trial, metformin showed prevention of severe COVID, prevention of long COVID, and an antiviral effect, and this is consistent with other data,” said coauthor Carolyn Bramante, MD, University of Minnesota, Minneapolis, in presenting the findings at the Conference on Retroviruses & Opportunistic Infections.
Study details
For the new subanalysis, the authors further evaluated the effects of metformin treatment on SARS-CoV-2 viral load.
A total of 1,323 patients in the study, enrolled at six centers, were randomized to treatment either with metformin 1,000 mg per day on days 2-5 and 1,500 mg per day on days 6 to 14 (n = 187), or to ivermectin 390-470 mcg/kg per day for 3 days (n = 187), fluvoxamine 50 mg twice daily for 14 days, and/or an exact-matching placebo in a 2 x 3 factorial trial design.
The subanalysis on viral load included 483 patients from the trial who were treated with metformin versus 462 who received placebo, who were all enrolled within 3 days of a documented SARS-CoV-2 infection and less than 7 days after symptom onset.
The patients had a median age of 46 years, and all had either overweight or obesity. Only about 2% had diabetes, and only patients considered low-risk were excluded from the trial, including those under age 30 and those with a body mass index under 25.
About half of patients had received a primary vaccine and about 5% had received a vaccine booster. SARS-CoV-2 variants that were prominent during the study included Alpha, Delta, and Omicron.
The viral samples available on days 1, 5, and 10 showed a mean change in viral load from baseline to follow-up; the viral load was significantly lower with metformin versus placebo (–0.64 log10 copies/mL), representing a 4.4-fold greater decrease in viral load with metformin.
The mean rate of undetectable SARS-CoV-2 viral load at day 5 was 49.9% in the metformin group versus 54.6% in the placebo group (odds ratio, 1.235), and the undetectable rate at day 10 was 14.3% in the metformin group and 22.6% in the placebo group (OR, 1.663; P = .003).
An increased antiviral effect corresponded with increases in metformin dosing on days 6 through 14. Furthermore, the antiviral effect became stronger when metformin was started earlier in the course of infection.
Of note, the antiviral effect was more pronounced among those who were not vaccinated (mean, –0.95 log copies/mL), compared with the vaccinated (mean, –0.39 log copies/mL).
The antiviral effect with metformin was similar to that seen with nirmatrelvir at day 5 and was greater than nirmatrelvir at day 10.
No similar relationships in SARS-CoV-2 viral load were observed between ivermectin or fluvoxamine and placebo.
The findings are consistent with results of other recent observational studies, including research showing metformin to be associated with reductions in COVID-19 severity in patients with prediabetes, Dr. Bramante noted.
The authors’ previous analysis looking at long COVID in the COVID-OUT study showed that metformin treatment during acute COVID significantly reduced the risk for a diagnosis of long COVID versus placebo at 300 days following randomization, with a hazard ratio of 0.59 after adjustment for the study drug and vaccination at baseline.
Dr. Bramante noted that metformin’s potential antiviral properties have long been speculated, with some of the earliest research on the drug suggesting less severe outcomes in influenza, and more recently, RNA assays suggesting effects against other RNA viruses, including the Zika virus.
In terms of COVID, Dr. Bramante noted that the drug has plenty of potentially favorable benefits.
“Metformin is very safe and is known to have very few contraindications, so the next steps could be to consider looking at this in terms of a combination therapy,” she said.
‘Data from other studies are conflicting’
Commenting on the study, Diane V. Havlir, MD, cautioned that “metformin is currently not recommended in treatment guidelines, [and] data from other studies are conflicting; side effects can be an issue, and the study presented here was in a select population,” she said in an interview.
However, “what is both new and interesting in this presentation is the reduction of viral load, which [was observed] in the samples collected not only on days 1-5, but also days 6-14,” said Dr. Havlir, who is professor and associate chair of clinical research, department of medicine, and chief of the division of HIV, infectious diseases and global medicine and director of the AIDS Research Institute at the University of California, San Francisco.
Key questions the findings raise include whether the results correlate with clinical outcomes or transmission, and whether the findings are generalizable to other populations and settings, Dr. Havlir said.
Ultimately, “we need to continue to pursue all aspects of outpatient treatments for COVID to address questions like these for new and existing agents,” she added.
The trial received funding from the Parsemus Foundation, the Rainwater Charitable Foundation, Fast Grants, and the United Health Group. The authors and Dr. Havlir disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM CROI 2023
How to get started with prescribing and advising on CGM
Continuous glucose monitoring (CGM) is gaining ground with both patients and providers because of an array of driving forces, including broadening eligibility, insulin price caps, public awareness, and an increasing number of educational initiatives for doctors.
While professional organizations aim to familiarize doctors with this relatively new technology, more patients are learning independently that finger sticks may be optional, leading them to request CGM from their provider, according to Neil Skolnik, MD.
“We in primary care are being shepherded into this space by our patients who have seen an advertisement or talked to a friend about the benefits of CGM, and then asked us to prescribe it,” said Dr. Skolnik, professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health.
Systemic factors are also accelerating CGM uptake, he added, highlighting recent Medicare rule changes to expand eligibility, with insurance companies beginning to follow suit.
Warren A. Jones, MD, FAAFP, professor emeritus at the University of Mississippi, Jackson, and past president of the AAFP, said that insulin price regulations have also opened doors to CGM.
“When you had patients trying to determine whether they were going to buy food or pay for high-priced insulin, that was a big challenge,” Dr. Jones said in an interview. “But that barrier has recently been removed, so we’re at the dawn of a new era.”
Like any paradigm shift, however,
Overview of online resources and navigating coverage
The latest learning resource on CGM for physicians comes from the American Academy of Family Physicians in the form of a new online educational hub with a 2-credit, ACCME-accredited course. It offers comprehensive guidance for employing CGM in daily practice. Topics include both medical and practical considerations, from interpretation of curves and glucose goal-setting to choosing a device and navigating coverage.
The AAFP’s new offering joins a growing number of similar educational efforts launched over the past few years by the Association of Diabetes Care & Education Specialists, the American Pharmacists Association, the American Diabetes Association, and the American Association of Clinical Endocrinologists.
Checking for coverage is a key first step when considering CGM for a particular patient, Dr. Jones said, noting that CGM, like any new form of care, presents unique challenges with coding and claims that must be overcome to get reimbursed.
“No margin, no mission,” Dr. Jones said. “If you are not able to pay your bills, you can’t be available for your patients. Our goal at the AAFP is to make sure that physicians get this knowledge [about reimbursement].”
To this end, the AAFP’s new online educational hub and the guide provided by APhA present CGM eligibility criteria for various patient groups, including those with Medicare, Medicaid, private insurance, and without coverage.
Medicare criteria include a diagnosis of diabetes, treatment with three or more daily administrations of insulin or continuous infusion via a pump, frequent adjustment to insulin treatment based on glucose readings, and presentation for diabetes in the past 6 months.
Once these requirements are clearly documented in the patient’s record, providers need to write the script, complete a certificate of medical necessity, and choose a supplier. Medicare covers CGM as a durable medical equipment benefit instead of a pharmacy benefit, according to the AAFP and APhA.
Exact coverage criteria and reimbursement processes for non-Medicare patients follow similar paths, although details vary by state and insurer, so personalized investigation is required.
When exploring coverage, the AAFP recommends paying attention to information needed for prior authorization, the patient’s diabetes type and age, and other medical requirements, such as minimum number of daily finger sticks or insulin doses per day.
Looking ahead, Dr. Jones predicted that authorization obstacles stemming from short-term cost concerns are going to fade as long-term savings are uncovered.
“I think pharmacy benefit managers and payers are going to recognize that we have better patient compliance, and that continuous glucose monitoring is going to bring the cost of care down and decrease the rate of hospitalizations,” Dr. Jones said. “So I think they’re going to be willing to pay clinicians to engage in this more readily over time.”
Patients who fail to qualify for personal CGM can still benefit from professional CGM, in which they borrow necessary equipment on a short-term basis. This avenue typically requires minimal or no insurance authorization. In addition, providers have the “opportunity to cover/exceed expenses by enhancing revenue with separately billable procedures, which can be billed in addition to [evaluation and management] if done on same day,” according to the AAFP guide, which goes on to provide appropriate codes.
Learning CGM through first-hand experience
Getting started with CGM can be intimidating for providers, Dr. Skolnik said, although he offered some reassurance, suggesting that the learning process may be more forgiving than prescribing a new drug for the first time.
“I think the best way to figure out CGM is to prescribe it to a couple of patients and learn with them,” Dr. Skolnik said. “You can’t do that with medicines. With medicines, you need to know what you’re doing before you choose who to give a medicine to.”
Instead of “reading everything under the sun” about CGM, he recommends starting with several of the ADA’s resources focusing on time in range, including an article, webinar, and podcast.
After that, physicians can learn on the job. A beginner’s mindset to CGM is well received by patients, he said, especially if you share your natural curiosity with them.
“Share your patients’ wonder at what they see,” Dr. Skolnik said. “They’ll open the app and you’ll look at their time and range and together you’ll go, ‘Wow, isn’t that something? I wonder why?’ ”
With this approach, providers and patients can join forces to explore trends and troubleshoot anomalous readings.
“Together you’ll go: ‘Hmm, I wonder why on Thursday, that graph is looking so far off from the other days? Wow. And then the patient remembers: they ate out on Thursday. They had a big pasta meal, perhaps. Everyone’s different in how they respond to different carbs. And you’ll both have this epiphany together about: ‘Wow, what I do matters.’ And I think that’s actually the best way to jump in.”
According to the AAFP, ADCES, and APhA resources, providers should first address time below range, as hypoglycemia can be imminently dangerous.
Next, providers should consider time in range, average glucose, and glucose management indicator, the latter of which acts as a surrogate for HbA1c. The first couple weeks of monitoring should be viewed as an information gathering phase, after which specific targets can be addressed through behavioral modifications and insulin adjustments, the AAFP advises.
The ADA guide highlights CGM usage, glucose variability, time in range, time above range, and average glucose as key metrics to monitor and offers corresponding actions when targets are unmet.
Encouraging patients to start CGM
Like providers, patients may also be intimidated by CGM, Dr. Jones said, typically because they don’t know how it works, or it seems complicated. Fortunately, he said, these fears are easily overcome when patients learn that they don’t need to stick themselves, record any of their readings, or really do anything at all for the first few weeks.
“You don’t even worry about it,” Dr. Jones tells his patients, who typically feel “more in control and engaged in their own care” after experiencing CGM for themselves.
Dr. Jones speaks from both professional and personal experience. A member of his family recently started CGM after being discharged from the hospital, and the benefits have been significant for everyone involved.
“I see how effectively we can control [my family member’s] blood pressure and insulin requirements, as opposed to several months ago when we didn’t have it,” Dr. Jones said. “So I’m giving it to you from two perspectives: one, of the clinician who knows, intellectually, what should go on, and two, experientially, from a family trying to take care of someone they love.”
Dr. Skolnik disclosed relationships with AstraZeneca, Teva, Lilly, Boehringer Ingelheim, Sanofi, GSK, Bayer, Genentech, Abbott, Idorsia, Merck, Novartis, Heartland, and Novo Nordisk. Dr Jones disclosed no relevant conflicts of interest.
Continuous glucose monitoring (CGM) is gaining ground with both patients and providers because of an array of driving forces, including broadening eligibility, insulin price caps, public awareness, and an increasing number of educational initiatives for doctors.
While professional organizations aim to familiarize doctors with this relatively new technology, more patients are learning independently that finger sticks may be optional, leading them to request CGM from their provider, according to Neil Skolnik, MD.
“We in primary care are being shepherded into this space by our patients who have seen an advertisement or talked to a friend about the benefits of CGM, and then asked us to prescribe it,” said Dr. Skolnik, professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health.
Systemic factors are also accelerating CGM uptake, he added, highlighting recent Medicare rule changes to expand eligibility, with insurance companies beginning to follow suit.
Warren A. Jones, MD, FAAFP, professor emeritus at the University of Mississippi, Jackson, and past president of the AAFP, said that insulin price regulations have also opened doors to CGM.
“When you had patients trying to determine whether they were going to buy food or pay for high-priced insulin, that was a big challenge,” Dr. Jones said in an interview. “But that barrier has recently been removed, so we’re at the dawn of a new era.”
Like any paradigm shift, however,
Overview of online resources and navigating coverage
The latest learning resource on CGM for physicians comes from the American Academy of Family Physicians in the form of a new online educational hub with a 2-credit, ACCME-accredited course. It offers comprehensive guidance for employing CGM in daily practice. Topics include both medical and practical considerations, from interpretation of curves and glucose goal-setting to choosing a device and navigating coverage.
The AAFP’s new offering joins a growing number of similar educational efforts launched over the past few years by the Association of Diabetes Care & Education Specialists, the American Pharmacists Association, the American Diabetes Association, and the American Association of Clinical Endocrinologists.
Checking for coverage is a key first step when considering CGM for a particular patient, Dr. Jones said, noting that CGM, like any new form of care, presents unique challenges with coding and claims that must be overcome to get reimbursed.
“No margin, no mission,” Dr. Jones said. “If you are not able to pay your bills, you can’t be available for your patients. Our goal at the AAFP is to make sure that physicians get this knowledge [about reimbursement].”
To this end, the AAFP’s new online educational hub and the guide provided by APhA present CGM eligibility criteria for various patient groups, including those with Medicare, Medicaid, private insurance, and without coverage.
Medicare criteria include a diagnosis of diabetes, treatment with three or more daily administrations of insulin or continuous infusion via a pump, frequent adjustment to insulin treatment based on glucose readings, and presentation for diabetes in the past 6 months.
Once these requirements are clearly documented in the patient’s record, providers need to write the script, complete a certificate of medical necessity, and choose a supplier. Medicare covers CGM as a durable medical equipment benefit instead of a pharmacy benefit, according to the AAFP and APhA.
Exact coverage criteria and reimbursement processes for non-Medicare patients follow similar paths, although details vary by state and insurer, so personalized investigation is required.
When exploring coverage, the AAFP recommends paying attention to information needed for prior authorization, the patient’s diabetes type and age, and other medical requirements, such as minimum number of daily finger sticks or insulin doses per day.
Looking ahead, Dr. Jones predicted that authorization obstacles stemming from short-term cost concerns are going to fade as long-term savings are uncovered.
“I think pharmacy benefit managers and payers are going to recognize that we have better patient compliance, and that continuous glucose monitoring is going to bring the cost of care down and decrease the rate of hospitalizations,” Dr. Jones said. “So I think they’re going to be willing to pay clinicians to engage in this more readily over time.”
Patients who fail to qualify for personal CGM can still benefit from professional CGM, in which they borrow necessary equipment on a short-term basis. This avenue typically requires minimal or no insurance authorization. In addition, providers have the “opportunity to cover/exceed expenses by enhancing revenue with separately billable procedures, which can be billed in addition to [evaluation and management] if done on same day,” according to the AAFP guide, which goes on to provide appropriate codes.
Learning CGM through first-hand experience
Getting started with CGM can be intimidating for providers, Dr. Skolnik said, although he offered some reassurance, suggesting that the learning process may be more forgiving than prescribing a new drug for the first time.
“I think the best way to figure out CGM is to prescribe it to a couple of patients and learn with them,” Dr. Skolnik said. “You can’t do that with medicines. With medicines, you need to know what you’re doing before you choose who to give a medicine to.”
Instead of “reading everything under the sun” about CGM, he recommends starting with several of the ADA’s resources focusing on time in range, including an article, webinar, and podcast.
After that, physicians can learn on the job. A beginner’s mindset to CGM is well received by patients, he said, especially if you share your natural curiosity with them.
“Share your patients’ wonder at what they see,” Dr. Skolnik said. “They’ll open the app and you’ll look at their time and range and together you’ll go, ‘Wow, isn’t that something? I wonder why?’ ”
With this approach, providers and patients can join forces to explore trends and troubleshoot anomalous readings.
“Together you’ll go: ‘Hmm, I wonder why on Thursday, that graph is looking so far off from the other days? Wow. And then the patient remembers: they ate out on Thursday. They had a big pasta meal, perhaps. Everyone’s different in how they respond to different carbs. And you’ll both have this epiphany together about: ‘Wow, what I do matters.’ And I think that’s actually the best way to jump in.”
According to the AAFP, ADCES, and APhA resources, providers should first address time below range, as hypoglycemia can be imminently dangerous.
Next, providers should consider time in range, average glucose, and glucose management indicator, the latter of which acts as a surrogate for HbA1c. The first couple weeks of monitoring should be viewed as an information gathering phase, after which specific targets can be addressed through behavioral modifications and insulin adjustments, the AAFP advises.
The ADA guide highlights CGM usage, glucose variability, time in range, time above range, and average glucose as key metrics to monitor and offers corresponding actions when targets are unmet.
Encouraging patients to start CGM
Like providers, patients may also be intimidated by CGM, Dr. Jones said, typically because they don’t know how it works, or it seems complicated. Fortunately, he said, these fears are easily overcome when patients learn that they don’t need to stick themselves, record any of their readings, or really do anything at all for the first few weeks.
“You don’t even worry about it,” Dr. Jones tells his patients, who typically feel “more in control and engaged in their own care” after experiencing CGM for themselves.
Dr. Jones speaks from both professional and personal experience. A member of his family recently started CGM after being discharged from the hospital, and the benefits have been significant for everyone involved.
“I see how effectively we can control [my family member’s] blood pressure and insulin requirements, as opposed to several months ago when we didn’t have it,” Dr. Jones said. “So I’m giving it to you from two perspectives: one, of the clinician who knows, intellectually, what should go on, and two, experientially, from a family trying to take care of someone they love.”
Dr. Skolnik disclosed relationships with AstraZeneca, Teva, Lilly, Boehringer Ingelheim, Sanofi, GSK, Bayer, Genentech, Abbott, Idorsia, Merck, Novartis, Heartland, and Novo Nordisk. Dr Jones disclosed no relevant conflicts of interest.
Continuous glucose monitoring (CGM) is gaining ground with both patients and providers because of an array of driving forces, including broadening eligibility, insulin price caps, public awareness, and an increasing number of educational initiatives for doctors.
While professional organizations aim to familiarize doctors with this relatively new technology, more patients are learning independently that finger sticks may be optional, leading them to request CGM from their provider, according to Neil Skolnik, MD.
“We in primary care are being shepherded into this space by our patients who have seen an advertisement or talked to a friend about the benefits of CGM, and then asked us to prescribe it,” said Dr. Skolnik, professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health.
Systemic factors are also accelerating CGM uptake, he added, highlighting recent Medicare rule changes to expand eligibility, with insurance companies beginning to follow suit.
Warren A. Jones, MD, FAAFP, professor emeritus at the University of Mississippi, Jackson, and past president of the AAFP, said that insulin price regulations have also opened doors to CGM.
“When you had patients trying to determine whether they were going to buy food or pay for high-priced insulin, that was a big challenge,” Dr. Jones said in an interview. “But that barrier has recently been removed, so we’re at the dawn of a new era.”
Like any paradigm shift, however,
Overview of online resources and navigating coverage
The latest learning resource on CGM for physicians comes from the American Academy of Family Physicians in the form of a new online educational hub with a 2-credit, ACCME-accredited course. It offers comprehensive guidance for employing CGM in daily practice. Topics include both medical and practical considerations, from interpretation of curves and glucose goal-setting to choosing a device and navigating coverage.
The AAFP’s new offering joins a growing number of similar educational efforts launched over the past few years by the Association of Diabetes Care & Education Specialists, the American Pharmacists Association, the American Diabetes Association, and the American Association of Clinical Endocrinologists.
Checking for coverage is a key first step when considering CGM for a particular patient, Dr. Jones said, noting that CGM, like any new form of care, presents unique challenges with coding and claims that must be overcome to get reimbursed.
“No margin, no mission,” Dr. Jones said. “If you are not able to pay your bills, you can’t be available for your patients. Our goal at the AAFP is to make sure that physicians get this knowledge [about reimbursement].”
To this end, the AAFP’s new online educational hub and the guide provided by APhA present CGM eligibility criteria for various patient groups, including those with Medicare, Medicaid, private insurance, and without coverage.
Medicare criteria include a diagnosis of diabetes, treatment with three or more daily administrations of insulin or continuous infusion via a pump, frequent adjustment to insulin treatment based on glucose readings, and presentation for diabetes in the past 6 months.
Once these requirements are clearly documented in the patient’s record, providers need to write the script, complete a certificate of medical necessity, and choose a supplier. Medicare covers CGM as a durable medical equipment benefit instead of a pharmacy benefit, according to the AAFP and APhA.
Exact coverage criteria and reimbursement processes for non-Medicare patients follow similar paths, although details vary by state and insurer, so personalized investigation is required.
When exploring coverage, the AAFP recommends paying attention to information needed for prior authorization, the patient’s diabetes type and age, and other medical requirements, such as minimum number of daily finger sticks or insulin doses per day.
Looking ahead, Dr. Jones predicted that authorization obstacles stemming from short-term cost concerns are going to fade as long-term savings are uncovered.
“I think pharmacy benefit managers and payers are going to recognize that we have better patient compliance, and that continuous glucose monitoring is going to bring the cost of care down and decrease the rate of hospitalizations,” Dr. Jones said. “So I think they’re going to be willing to pay clinicians to engage in this more readily over time.”
Patients who fail to qualify for personal CGM can still benefit from professional CGM, in which they borrow necessary equipment on a short-term basis. This avenue typically requires minimal or no insurance authorization. In addition, providers have the “opportunity to cover/exceed expenses by enhancing revenue with separately billable procedures, which can be billed in addition to [evaluation and management] if done on same day,” according to the AAFP guide, which goes on to provide appropriate codes.
Learning CGM through first-hand experience
Getting started with CGM can be intimidating for providers, Dr. Skolnik said, although he offered some reassurance, suggesting that the learning process may be more forgiving than prescribing a new drug for the first time.
“I think the best way to figure out CGM is to prescribe it to a couple of patients and learn with them,” Dr. Skolnik said. “You can’t do that with medicines. With medicines, you need to know what you’re doing before you choose who to give a medicine to.”
Instead of “reading everything under the sun” about CGM, he recommends starting with several of the ADA’s resources focusing on time in range, including an article, webinar, and podcast.
After that, physicians can learn on the job. A beginner’s mindset to CGM is well received by patients, he said, especially if you share your natural curiosity with them.
“Share your patients’ wonder at what they see,” Dr. Skolnik said. “They’ll open the app and you’ll look at their time and range and together you’ll go, ‘Wow, isn’t that something? I wonder why?’ ”
With this approach, providers and patients can join forces to explore trends and troubleshoot anomalous readings.
“Together you’ll go: ‘Hmm, I wonder why on Thursday, that graph is looking so far off from the other days? Wow. And then the patient remembers: they ate out on Thursday. They had a big pasta meal, perhaps. Everyone’s different in how they respond to different carbs. And you’ll both have this epiphany together about: ‘Wow, what I do matters.’ And I think that’s actually the best way to jump in.”
According to the AAFP, ADCES, and APhA resources, providers should first address time below range, as hypoglycemia can be imminently dangerous.
Next, providers should consider time in range, average glucose, and glucose management indicator, the latter of which acts as a surrogate for HbA1c. The first couple weeks of monitoring should be viewed as an information gathering phase, after which specific targets can be addressed through behavioral modifications and insulin adjustments, the AAFP advises.
The ADA guide highlights CGM usage, glucose variability, time in range, time above range, and average glucose as key metrics to monitor and offers corresponding actions when targets are unmet.
Encouraging patients to start CGM
Like providers, patients may also be intimidated by CGM, Dr. Jones said, typically because they don’t know how it works, or it seems complicated. Fortunately, he said, these fears are easily overcome when patients learn that they don’t need to stick themselves, record any of their readings, or really do anything at all for the first few weeks.
“You don’t even worry about it,” Dr. Jones tells his patients, who typically feel “more in control and engaged in their own care” after experiencing CGM for themselves.
Dr. Jones speaks from both professional and personal experience. A member of his family recently started CGM after being discharged from the hospital, and the benefits have been significant for everyone involved.
“I see how effectively we can control [my family member’s] blood pressure and insulin requirements, as opposed to several months ago when we didn’t have it,” Dr. Jones said. “So I’m giving it to you from two perspectives: one, of the clinician who knows, intellectually, what should go on, and two, experientially, from a family trying to take care of someone they love.”
Dr. Skolnik disclosed relationships with AstraZeneca, Teva, Lilly, Boehringer Ingelheim, Sanofi, GSK, Bayer, Genentech, Abbott, Idorsia, Merck, Novartis, Heartland, and Novo Nordisk. Dr Jones disclosed no relevant conflicts of interest.
Rucaparib benefit in BRCA+ prostate cancer confirmed
The finding, which comes from the TRITON3 clinical trial, provides evidence of clinical benefit for an indication for rucaparib that was granted an accelerated approval in May 2020.
“Rucaparib reduced the risk of progression or death by half in patients with BRCA alterations,” said lead author Alan H. Bryce, MD, medical director of the Genomic Oncology Clinic at Mayo Clinic Arizona, in Phoenix.
For the subgroup of patients with BRCA alterations, the median PFS was 11.2 months with rucaparib vs. 6.4 months (hazard ratio, 0.50; P < .001) among those who received physician’s choice of therapy, which included docetaxel or a second-generation ARPI, such as abiraterone or enzalutamide.
In another subgroup of patients whose disease had ATM alterations, the median PFS was 8.1 months with rucaparib vs. 6.8 months with physician’s choice of drug. The difference was not statistically significant.
However, the difference was significant in the intention-to-treat (ITT) population (comprising both subgroups), for whom the median PFS was 10.2 months with rucaparib vs. 6.4 months with physician’s choice of drug (HR, 0.61; P < .001 by log-rank test).
Dr. Bryce pointed out that three-quarters of the patients in the physician’s-choice arm who had progressive disease crossed over to rucaparib upon progression and that overall survival (OS) results are immature. At 62 months, median OS did not significantly differ in the BRCA subgroup (24.3 vs. 20.8 months favoring rucaparib; P = .21) or in the ITT group (23.6 vs. 20.9 months; P = .67).
Importantly, rucaparib was well tolerated. In all treatment groups, the most frequent adverse events were asthenia and fatigue, Bryce said. “There were no cases of myelodysplastic syndrome or acute myeloid leukemia reported.”
These results from the TRITON3 trial were presented at the 2023 ASCO Genitourinary Cancers Symposium and were published simultaneously in the New England Journal of Medicine.
Suggested benefit
Rucaparib is the first PARP inhibitor approved for use in patients with mCRPC that harbors deleterious BRCA mutations (germline and/or somatic) who have already been treated with androgen receptor–directed therapy and a taxane-based chemotherapy. This prostate cancer indication was granted an accelerated approval in May 2020 by the U.S. Food and Drug Administration on the basis of response rates and effect on levels of prostate-specific antigen (PSA) from the TRITON2 clinical trial, the forerunner of the current study.
The TRITON2 study was a single-arm clinical trial that involved three cohorts: 62 patients with a BRCA mutation (germline and/or somatic) and measurable disease; 115 patients with a BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease; and 209 patients with homologous recombination deficiency–positive mCRPC.
In an analysis of 115 patients with a deleterious BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease, the confirmed PSA response rate was 55%. For the patients with measurable disease and a BRCA mutation, the objective response rate was 44%. The objective response rate was similar for those with a germline BRCA mutation.
Study details
The current phase 3 randomized TRITON3 clinical trial was conducted to confirm the earlier findings and to expand upon the data in mCRPC. The participants in this trial were patients with mCRPC who had specific gene alterations, including BRCA and ATM alterations, who had experienced disease progression after androgen receptor–directed therapy but who had not yet received chemotherapy.
A total of 270 men were assigned to receive rucaparib (600 mg twice daily); 135 patients received their physician’s choice of medication. Within the two study arms, 302 patients had a BRCA alteration, and 103 patients had an ATM alteration. The ITT population consisted of all the patients who had been randomly assigned to either of the two groups. A prespecified subgroup included patients with a BRCA alteration.
The primary outcome was the median duration of imaging-based PSF, as determined through independent review. Key secondary outcomes were overall survival and objective response rate.
The most common adverse events in the rucaparib group were fatigue, nausea, and anemia or decreased hemoglobin. In the control group, the most common adverse events were fatigue, diarrhea, and neuropathy. The most common events of grade 3 or higher were anemia or decreased hemoglobin, neutropenia or a decreased neutrophil count, and fatigue in the rucaparib group, and fatigue and neutropenia or a decreased neutrophil count among control patients.
No changes in standard of care
In a discussion of the study, Elena Castro, MD, PhD, of the Instituto de Investigación Biomédica de Málaga, Campanillas, Spain, emphasized that there is a clear benefit from the use of PARP inhibitors (such as rucaparib) for patients with BRCA alterations.
However, she highlighted the absence of convincing overall survival data and the absence of a clear benefit on PFS in the subgroup of patients with ATM alterations.
“These data raise several questions,” she noted, “such as, do patients with ATM alterations benefit at all? And should PARP inhibitors [such as rucaparib] precede or follow docetaxel therapy?”
Because of the high crossover rate, it may be possible to evaluate the directionality of docetaxel followed by PARP inhibitors and the other way around, she suggested.
Dr. Castro said that patients with BRCA alterations benefit from PARP inhibitors and are likely to derive more benefit from them than from taxanes.
“But those with ATM alterations are unlikely to benefit from rucaparib more than from taxanes,” she said.
In a comment, Hank Ng, MD, medical oncologist, NYU Langone Perlmutter Cancer Center, New York, said he is not convinced that the findings from TRITON 3 represent a new standard of care in BRCA 1/2 mutations or ATM.
“Currently, we know that, for patients with prostate cancer with BRCA1/2 or ATM, the standard of care is an androgen receptor pathway inhibitor (ARPI), such as abiraterone or enzalutamide, then docetaxel, and then a PARP inhibitor like rucaparib,” he said.
(Currently, rucaparib is indicated for use in patients with mCRPC with BRCA alterations after they have already received an ARPI and taxane-based chemotherapy.)
Dr. Ng also questioned the control arm of the TRITON 3 trial. All the participants in the trial had already experienced disease progression after treatment with a second-generation ARPI. But the physician’s choice of therapy allowed them to move on to another ARPI or to docetaxel.
Dr. NG commented that, “in almost all cases, after progression of one ARPI, switching to another ARPI does not provide much benefit – from what is visible from this abstract – and only 56% patients received docetaxel, and thus 44% received a not-beneficial treatment,” he said.
“I am not sure what the docetaxel subgroup showed, but potentially, if those numbers are convincing, we could move this [rucaparib] ahead of docetaxel,” he speculated.
However, he also pointed out that an overall survival benefit has not yet been shown; so far, the benefit that has been shown is with respect to imaging-based PFS.
Dr. Ng does agree that rucaparib is indicated in the second line after progression with one ARPI for patients who are not candidates for chemotherapy. “But this has not yet shown me that we should absolutely be offering rucaparib before docetaxel,” he said.
TRITON3 was supported by Clovis Oncology, manufacturer of rucaparib. Dr. Bryce has relationships with Bayer, Foundation Medicine, Janssen, Merck, Myovant Sciences, and Novartis and holds a patent for therapeutic targeting of cancer patients with NRG1 rearrangements. Dr. Castro has relationships with Astellas Pharma, AstraZeneca, Bayer, Clovis Oncology, Janssen-Cilag, Merck, MSD Oncology, Novartis, Pfizer, and Roche.
A version of this article first appeared on Medscape.com.
The finding, which comes from the TRITON3 clinical trial, provides evidence of clinical benefit for an indication for rucaparib that was granted an accelerated approval in May 2020.
“Rucaparib reduced the risk of progression or death by half in patients with BRCA alterations,” said lead author Alan H. Bryce, MD, medical director of the Genomic Oncology Clinic at Mayo Clinic Arizona, in Phoenix.
For the subgroup of patients with BRCA alterations, the median PFS was 11.2 months with rucaparib vs. 6.4 months (hazard ratio, 0.50; P < .001) among those who received physician’s choice of therapy, which included docetaxel or a second-generation ARPI, such as abiraterone or enzalutamide.
In another subgroup of patients whose disease had ATM alterations, the median PFS was 8.1 months with rucaparib vs. 6.8 months with physician’s choice of drug. The difference was not statistically significant.
However, the difference was significant in the intention-to-treat (ITT) population (comprising both subgroups), for whom the median PFS was 10.2 months with rucaparib vs. 6.4 months with physician’s choice of drug (HR, 0.61; P < .001 by log-rank test).
Dr. Bryce pointed out that three-quarters of the patients in the physician’s-choice arm who had progressive disease crossed over to rucaparib upon progression and that overall survival (OS) results are immature. At 62 months, median OS did not significantly differ in the BRCA subgroup (24.3 vs. 20.8 months favoring rucaparib; P = .21) or in the ITT group (23.6 vs. 20.9 months; P = .67).
Importantly, rucaparib was well tolerated. In all treatment groups, the most frequent adverse events were asthenia and fatigue, Bryce said. “There were no cases of myelodysplastic syndrome or acute myeloid leukemia reported.”
These results from the TRITON3 trial were presented at the 2023 ASCO Genitourinary Cancers Symposium and were published simultaneously in the New England Journal of Medicine.
Suggested benefit
Rucaparib is the first PARP inhibitor approved for use in patients with mCRPC that harbors deleterious BRCA mutations (germline and/or somatic) who have already been treated with androgen receptor–directed therapy and a taxane-based chemotherapy. This prostate cancer indication was granted an accelerated approval in May 2020 by the U.S. Food and Drug Administration on the basis of response rates and effect on levels of prostate-specific antigen (PSA) from the TRITON2 clinical trial, the forerunner of the current study.
The TRITON2 study was a single-arm clinical trial that involved three cohorts: 62 patients with a BRCA mutation (germline and/or somatic) and measurable disease; 115 patients with a BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease; and 209 patients with homologous recombination deficiency–positive mCRPC.
In an analysis of 115 patients with a deleterious BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease, the confirmed PSA response rate was 55%. For the patients with measurable disease and a BRCA mutation, the objective response rate was 44%. The objective response rate was similar for those with a germline BRCA mutation.
Study details
The current phase 3 randomized TRITON3 clinical trial was conducted to confirm the earlier findings and to expand upon the data in mCRPC. The participants in this trial were patients with mCRPC who had specific gene alterations, including BRCA and ATM alterations, who had experienced disease progression after androgen receptor–directed therapy but who had not yet received chemotherapy.
A total of 270 men were assigned to receive rucaparib (600 mg twice daily); 135 patients received their physician’s choice of medication. Within the two study arms, 302 patients had a BRCA alteration, and 103 patients had an ATM alteration. The ITT population consisted of all the patients who had been randomly assigned to either of the two groups. A prespecified subgroup included patients with a BRCA alteration.
The primary outcome was the median duration of imaging-based PSF, as determined through independent review. Key secondary outcomes were overall survival and objective response rate.
The most common adverse events in the rucaparib group were fatigue, nausea, and anemia or decreased hemoglobin. In the control group, the most common adverse events were fatigue, diarrhea, and neuropathy. The most common events of grade 3 or higher were anemia or decreased hemoglobin, neutropenia or a decreased neutrophil count, and fatigue in the rucaparib group, and fatigue and neutropenia or a decreased neutrophil count among control patients.
No changes in standard of care
In a discussion of the study, Elena Castro, MD, PhD, of the Instituto de Investigación Biomédica de Málaga, Campanillas, Spain, emphasized that there is a clear benefit from the use of PARP inhibitors (such as rucaparib) for patients with BRCA alterations.
However, she highlighted the absence of convincing overall survival data and the absence of a clear benefit on PFS in the subgroup of patients with ATM alterations.
“These data raise several questions,” she noted, “such as, do patients with ATM alterations benefit at all? And should PARP inhibitors [such as rucaparib] precede or follow docetaxel therapy?”
Because of the high crossover rate, it may be possible to evaluate the directionality of docetaxel followed by PARP inhibitors and the other way around, she suggested.
Dr. Castro said that patients with BRCA alterations benefit from PARP inhibitors and are likely to derive more benefit from them than from taxanes.
“But those with ATM alterations are unlikely to benefit from rucaparib more than from taxanes,” she said.
In a comment, Hank Ng, MD, medical oncologist, NYU Langone Perlmutter Cancer Center, New York, said he is not convinced that the findings from TRITON 3 represent a new standard of care in BRCA 1/2 mutations or ATM.
“Currently, we know that, for patients with prostate cancer with BRCA1/2 or ATM, the standard of care is an androgen receptor pathway inhibitor (ARPI), such as abiraterone or enzalutamide, then docetaxel, and then a PARP inhibitor like rucaparib,” he said.
(Currently, rucaparib is indicated for use in patients with mCRPC with BRCA alterations after they have already received an ARPI and taxane-based chemotherapy.)
Dr. Ng also questioned the control arm of the TRITON 3 trial. All the participants in the trial had already experienced disease progression after treatment with a second-generation ARPI. But the physician’s choice of therapy allowed them to move on to another ARPI or to docetaxel.
Dr. NG commented that, “in almost all cases, after progression of one ARPI, switching to another ARPI does not provide much benefit – from what is visible from this abstract – and only 56% patients received docetaxel, and thus 44% received a not-beneficial treatment,” he said.
“I am not sure what the docetaxel subgroup showed, but potentially, if those numbers are convincing, we could move this [rucaparib] ahead of docetaxel,” he speculated.
However, he also pointed out that an overall survival benefit has not yet been shown; so far, the benefit that has been shown is with respect to imaging-based PFS.
Dr. Ng does agree that rucaparib is indicated in the second line after progression with one ARPI for patients who are not candidates for chemotherapy. “But this has not yet shown me that we should absolutely be offering rucaparib before docetaxel,” he said.
TRITON3 was supported by Clovis Oncology, manufacturer of rucaparib. Dr. Bryce has relationships with Bayer, Foundation Medicine, Janssen, Merck, Myovant Sciences, and Novartis and holds a patent for therapeutic targeting of cancer patients with NRG1 rearrangements. Dr. Castro has relationships with Astellas Pharma, AstraZeneca, Bayer, Clovis Oncology, Janssen-Cilag, Merck, MSD Oncology, Novartis, Pfizer, and Roche.
A version of this article first appeared on Medscape.com.
The finding, which comes from the TRITON3 clinical trial, provides evidence of clinical benefit for an indication for rucaparib that was granted an accelerated approval in May 2020.
“Rucaparib reduced the risk of progression or death by half in patients with BRCA alterations,” said lead author Alan H. Bryce, MD, medical director of the Genomic Oncology Clinic at Mayo Clinic Arizona, in Phoenix.
For the subgroup of patients with BRCA alterations, the median PFS was 11.2 months with rucaparib vs. 6.4 months (hazard ratio, 0.50; P < .001) among those who received physician’s choice of therapy, which included docetaxel or a second-generation ARPI, such as abiraterone or enzalutamide.
In another subgroup of patients whose disease had ATM alterations, the median PFS was 8.1 months with rucaparib vs. 6.8 months with physician’s choice of drug. The difference was not statistically significant.
However, the difference was significant in the intention-to-treat (ITT) population (comprising both subgroups), for whom the median PFS was 10.2 months with rucaparib vs. 6.4 months with physician’s choice of drug (HR, 0.61; P < .001 by log-rank test).
Dr. Bryce pointed out that three-quarters of the patients in the physician’s-choice arm who had progressive disease crossed over to rucaparib upon progression and that overall survival (OS) results are immature. At 62 months, median OS did not significantly differ in the BRCA subgroup (24.3 vs. 20.8 months favoring rucaparib; P = .21) or in the ITT group (23.6 vs. 20.9 months; P = .67).
Importantly, rucaparib was well tolerated. In all treatment groups, the most frequent adverse events were asthenia and fatigue, Bryce said. “There were no cases of myelodysplastic syndrome or acute myeloid leukemia reported.”
These results from the TRITON3 trial were presented at the 2023 ASCO Genitourinary Cancers Symposium and were published simultaneously in the New England Journal of Medicine.
Suggested benefit
Rucaparib is the first PARP inhibitor approved for use in patients with mCRPC that harbors deleterious BRCA mutations (germline and/or somatic) who have already been treated with androgen receptor–directed therapy and a taxane-based chemotherapy. This prostate cancer indication was granted an accelerated approval in May 2020 by the U.S. Food and Drug Administration on the basis of response rates and effect on levels of prostate-specific antigen (PSA) from the TRITON2 clinical trial, the forerunner of the current study.
The TRITON2 study was a single-arm clinical trial that involved three cohorts: 62 patients with a BRCA mutation (germline and/or somatic) and measurable disease; 115 patients with a BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease; and 209 patients with homologous recombination deficiency–positive mCRPC.
In an analysis of 115 patients with a deleterious BRCA mutation (germline and/or somatic) and measurable or nonmeasurable disease, the confirmed PSA response rate was 55%. For the patients with measurable disease and a BRCA mutation, the objective response rate was 44%. The objective response rate was similar for those with a germline BRCA mutation.
Study details
The current phase 3 randomized TRITON3 clinical trial was conducted to confirm the earlier findings and to expand upon the data in mCRPC. The participants in this trial were patients with mCRPC who had specific gene alterations, including BRCA and ATM alterations, who had experienced disease progression after androgen receptor–directed therapy but who had not yet received chemotherapy.
A total of 270 men were assigned to receive rucaparib (600 mg twice daily); 135 patients received their physician’s choice of medication. Within the two study arms, 302 patients had a BRCA alteration, and 103 patients had an ATM alteration. The ITT population consisted of all the patients who had been randomly assigned to either of the two groups. A prespecified subgroup included patients with a BRCA alteration.
The primary outcome was the median duration of imaging-based PSF, as determined through independent review. Key secondary outcomes were overall survival and objective response rate.
The most common adverse events in the rucaparib group were fatigue, nausea, and anemia or decreased hemoglobin. In the control group, the most common adverse events were fatigue, diarrhea, and neuropathy. The most common events of grade 3 or higher were anemia or decreased hemoglobin, neutropenia or a decreased neutrophil count, and fatigue in the rucaparib group, and fatigue and neutropenia or a decreased neutrophil count among control patients.
No changes in standard of care
In a discussion of the study, Elena Castro, MD, PhD, of the Instituto de Investigación Biomédica de Málaga, Campanillas, Spain, emphasized that there is a clear benefit from the use of PARP inhibitors (such as rucaparib) for patients with BRCA alterations.
However, she highlighted the absence of convincing overall survival data and the absence of a clear benefit on PFS in the subgroup of patients with ATM alterations.
“These data raise several questions,” she noted, “such as, do patients with ATM alterations benefit at all? And should PARP inhibitors [such as rucaparib] precede or follow docetaxel therapy?”
Because of the high crossover rate, it may be possible to evaluate the directionality of docetaxel followed by PARP inhibitors and the other way around, she suggested.
Dr. Castro said that patients with BRCA alterations benefit from PARP inhibitors and are likely to derive more benefit from them than from taxanes.
“But those with ATM alterations are unlikely to benefit from rucaparib more than from taxanes,” she said.
In a comment, Hank Ng, MD, medical oncologist, NYU Langone Perlmutter Cancer Center, New York, said he is not convinced that the findings from TRITON 3 represent a new standard of care in BRCA 1/2 mutations or ATM.
“Currently, we know that, for patients with prostate cancer with BRCA1/2 or ATM, the standard of care is an androgen receptor pathway inhibitor (ARPI), such as abiraterone or enzalutamide, then docetaxel, and then a PARP inhibitor like rucaparib,” he said.
(Currently, rucaparib is indicated for use in patients with mCRPC with BRCA alterations after they have already received an ARPI and taxane-based chemotherapy.)
Dr. Ng also questioned the control arm of the TRITON 3 trial. All the participants in the trial had already experienced disease progression after treatment with a second-generation ARPI. But the physician’s choice of therapy allowed them to move on to another ARPI or to docetaxel.
Dr. NG commented that, “in almost all cases, after progression of one ARPI, switching to another ARPI does not provide much benefit – from what is visible from this abstract – and only 56% patients received docetaxel, and thus 44% received a not-beneficial treatment,” he said.
“I am not sure what the docetaxel subgroup showed, but potentially, if those numbers are convincing, we could move this [rucaparib] ahead of docetaxel,” he speculated.
However, he also pointed out that an overall survival benefit has not yet been shown; so far, the benefit that has been shown is with respect to imaging-based PFS.
Dr. Ng does agree that rucaparib is indicated in the second line after progression with one ARPI for patients who are not candidates for chemotherapy. “But this has not yet shown me that we should absolutely be offering rucaparib before docetaxel,” he said.
TRITON3 was supported by Clovis Oncology, manufacturer of rucaparib. Dr. Bryce has relationships with Bayer, Foundation Medicine, Janssen, Merck, Myovant Sciences, and Novartis and holds a patent for therapeutic targeting of cancer patients with NRG1 rearrangements. Dr. Castro has relationships with Astellas Pharma, AstraZeneca, Bayer, Clovis Oncology, Janssen-Cilag, Merck, MSD Oncology, Novartis, Pfizer, and Roche.
A version of this article first appeared on Medscape.com.
AT ASCO GU 2023
Diabetes drug tied to lower dementia risk
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
‘Only a sociopath could work for a large health system,’ doc says sardonically
A frustrated physician recently voiced some strong words in Medscape’s US Physician Burnout & Depression Report: “Only a sociopath could work for a large health system and not be burned out. Anyone who cares about patients is doomed to burnout.”
Medscape’s report showed that 53% of physicians feel burned out by job requirements; 65% say that burnout has impacted their relationships, and other statistics say that physicians are leaving clinical medicine because of all this pressure.
What is it about being employed by large organizations that can be so negative? In another study, MEMO – Minimizing Error, Maximizing Outcomes – researchers at the University of Wisconsin surveyed more than 400 doctors to learn about how their working environments corresponded with medical errors. More than half of the physicians reported time pressures when conducting physical examinations. Nearly a third felt they needed at least 50% more time than was allotted for this patient care function, and nearly a quarter said they needed at least 50% more time for follow-up appointments.
Some have asked: Can anyone, then, thrive in today’s health care environment and avoid burnout?
Although the frustrated physician noted above may sardonically say that a doctor needs to be sociopathic to enjoy it – lacking in feelings for others – “It’s a very small number of doctors who get in it for the wrong reasons and therefore care about their own benefit and not their patients,” said psychiatrist Wendy Dean, MD, CEO and cofounder of Moral Injury of Healthcare, a nonprofit organization addressing workforce distress in health care. “Those are the outliers.”
The vast majority of physicians do care about their patients – deeply, said Dr. Dean. They struggle under the weight of the health care system and yet must find ways to get through. Today, thriving in an imperfect system requires honing new skills, asking for help when needed, and pushing for systemic and cultural change.
“We’ve been assessing and trying to address burnout for half a century,” said Dr. Dean. “Despite all the good intentions, and people dedicating their entire careers to solving the issue, we’ve barely made a dent.”
With the advent of new technological requirements on the job and more demands from increasingly larger health care organizations, the risk for burnout is higher than ever before. “There’s an increased burden of regulatory-mandated and cumbersome administrative workload per patient,” said Shomron Ben-Horin, MD, cofounder of Evinature. “Often the computer/paperwork before and after a procedure is much longer than the procedure itself.”
Meeting insurance requirements is increasingly cumbersome, too, and preauthorizations and debates with payers over medical approval may put physicians frustratingly in the middle.
“This increases the psychological burden for physicians who may feel responsible for wrongdoing no matter which option they deem better,” Dr. Ben-Horin said. “Add in physician accessibility around the clock via mobile phones, emails, and apps, and you end up on call even if you’re not officially on call.”
Why some physicians suffer more
Some physicians are more likely to suffer burnout than others, said Jessi Gold, MD, assistant professor in the department of psychiatry at Washington University in St. Louis. “The self-valuation concept comes into play here,” she said. “If you make a mistake, do you blame yourself or see it as a growth opportunity? If it’s the former, you’re more likely to burn out.”
Dr. Ben-Horin added that the most patient-centric doctors are the ones who struggle most. “These are the doctors we’d all love to have as a patient,” he said. “But they are burdened by the extra tasks of the job, and they are the most stressed by the environment.”
So too are those physicians who never master compartmentalizing their feelings and emotions. “We learn in training to compartmentalize our emotions,” said Dr. Dean. “You can’t allow yourself to get emotional while performing chest compressions on an 18-year-old kid. So you shut it all away; otherwise, you might lose the patient.”
This turn-off switch becomes automatic, but it also comes at a cost. “When doctors were interviewed about [Buffalo Bills player] Damar Hamlin going into cardiac arrest on the football field, they talked about how a life-and-death situation is so common that they have to put the emotions away, work on the patient, and move onto the next,” said Dr. Dean. “The next patient needs you just as much. We must lock away our feelings and manage the situation.”
Dr. Gold explained that burying feelings, however, is a symptom of burnout. “We have to remove ourselves from the situation to protect ourselves,” she said. “We can’t cry in these situations, but we can’t bury our feelings either.”
Instead, Dr. Gold suggested, a good medium may exist. “You may not be able to address them in the moment, but you should sometime after,” she said.
This is just a starting point on how to remain a dedicated, caring physician without burning out. “The system is pretty broken, and to survive it first means wanting to survive it,” Dr. Gold said. “There’s a lot of focus on resiliency and lack thereof if a physician expresses burnout, but that’s a false notion. Doctors are a resilient bunch but even they get burned out.”
Change for the better must come from several places. One is asking for help, something that can be hard for a group conditioned to keeping a stiff upper lip. “Just because your peers might look healthy (emotionally) doesn’t mean they are,” said Dr. Gold. “We’ve normalized this culture of burying feelings, but that doesn’t mean it’s right.”
Dr. Ben-Horin also advocates diversifying your work. This might include engaging in research and academics, for instance. “This not only makes you a better broad-perspective doctor but allows you to psychologically switch gears on research days,” he said.
The biggest place to make change, however, is within the health care system culture itself. The AMA created a series of recommendations to address burnout at the resident and fellow level, a good starting point to carry through into staff work. The steps include creating a well-being framework, gathering a team to support a well-being program, developing the program in a way to foster fun and connectivity among the staff, fostering individual well-being that addresses emotional and physical well-being, and confronting burnout and creating a sustainable culture of well-being.
On a personal level, it’s essential that physicians keep close tabs on themselves and peers. “Understand the signs and symptoms of burnout by taking stock of where you are emotionally,” said Dr. Gold. “Have a place and time at the end of a hard day to reflect or find a ritual that helps you and stay with it.”
You might also reach out to a therapist or a peer when you’re struggling. Having honest conversations with peers can go a long way. “Find a confidant that allows you to be vulnerable,” Dr. Gold recommended. “Acknowledge that this is hard and that you might need help taking care of yourself. The system needs to change, but we can also learn to survive in the meantime. You don’t have to be a sociopath to make it.”
A version of this article originally appeared on Medscape.com.
A frustrated physician recently voiced some strong words in Medscape’s US Physician Burnout & Depression Report: “Only a sociopath could work for a large health system and not be burned out. Anyone who cares about patients is doomed to burnout.”
Medscape’s report showed that 53% of physicians feel burned out by job requirements; 65% say that burnout has impacted their relationships, and other statistics say that physicians are leaving clinical medicine because of all this pressure.
What is it about being employed by large organizations that can be so negative? In another study, MEMO – Minimizing Error, Maximizing Outcomes – researchers at the University of Wisconsin surveyed more than 400 doctors to learn about how their working environments corresponded with medical errors. More than half of the physicians reported time pressures when conducting physical examinations. Nearly a third felt they needed at least 50% more time than was allotted for this patient care function, and nearly a quarter said they needed at least 50% more time for follow-up appointments.
Some have asked: Can anyone, then, thrive in today’s health care environment and avoid burnout?
Although the frustrated physician noted above may sardonically say that a doctor needs to be sociopathic to enjoy it – lacking in feelings for others – “It’s a very small number of doctors who get in it for the wrong reasons and therefore care about their own benefit and not their patients,” said psychiatrist Wendy Dean, MD, CEO and cofounder of Moral Injury of Healthcare, a nonprofit organization addressing workforce distress in health care. “Those are the outliers.”
The vast majority of physicians do care about their patients – deeply, said Dr. Dean. They struggle under the weight of the health care system and yet must find ways to get through. Today, thriving in an imperfect system requires honing new skills, asking for help when needed, and pushing for systemic and cultural change.
“We’ve been assessing and trying to address burnout for half a century,” said Dr. Dean. “Despite all the good intentions, and people dedicating their entire careers to solving the issue, we’ve barely made a dent.”
With the advent of new technological requirements on the job and more demands from increasingly larger health care organizations, the risk for burnout is higher than ever before. “There’s an increased burden of regulatory-mandated and cumbersome administrative workload per patient,” said Shomron Ben-Horin, MD, cofounder of Evinature. “Often the computer/paperwork before and after a procedure is much longer than the procedure itself.”
Meeting insurance requirements is increasingly cumbersome, too, and preauthorizations and debates with payers over medical approval may put physicians frustratingly in the middle.
“This increases the psychological burden for physicians who may feel responsible for wrongdoing no matter which option they deem better,” Dr. Ben-Horin said. “Add in physician accessibility around the clock via mobile phones, emails, and apps, and you end up on call even if you’re not officially on call.”
Why some physicians suffer more
Some physicians are more likely to suffer burnout than others, said Jessi Gold, MD, assistant professor in the department of psychiatry at Washington University in St. Louis. “The self-valuation concept comes into play here,” she said. “If you make a mistake, do you blame yourself or see it as a growth opportunity? If it’s the former, you’re more likely to burn out.”
Dr. Ben-Horin added that the most patient-centric doctors are the ones who struggle most. “These are the doctors we’d all love to have as a patient,” he said. “But they are burdened by the extra tasks of the job, and they are the most stressed by the environment.”
So too are those physicians who never master compartmentalizing their feelings and emotions. “We learn in training to compartmentalize our emotions,” said Dr. Dean. “You can’t allow yourself to get emotional while performing chest compressions on an 18-year-old kid. So you shut it all away; otherwise, you might lose the patient.”
This turn-off switch becomes automatic, but it also comes at a cost. “When doctors were interviewed about [Buffalo Bills player] Damar Hamlin going into cardiac arrest on the football field, they talked about how a life-and-death situation is so common that they have to put the emotions away, work on the patient, and move onto the next,” said Dr. Dean. “The next patient needs you just as much. We must lock away our feelings and manage the situation.”
Dr. Gold explained that burying feelings, however, is a symptom of burnout. “We have to remove ourselves from the situation to protect ourselves,” she said. “We can’t cry in these situations, but we can’t bury our feelings either.”
Instead, Dr. Gold suggested, a good medium may exist. “You may not be able to address them in the moment, but you should sometime after,” she said.
This is just a starting point on how to remain a dedicated, caring physician without burning out. “The system is pretty broken, and to survive it first means wanting to survive it,” Dr. Gold said. “There’s a lot of focus on resiliency and lack thereof if a physician expresses burnout, but that’s a false notion. Doctors are a resilient bunch but even they get burned out.”
Change for the better must come from several places. One is asking for help, something that can be hard for a group conditioned to keeping a stiff upper lip. “Just because your peers might look healthy (emotionally) doesn’t mean they are,” said Dr. Gold. “We’ve normalized this culture of burying feelings, but that doesn’t mean it’s right.”
Dr. Ben-Horin also advocates diversifying your work. This might include engaging in research and academics, for instance. “This not only makes you a better broad-perspective doctor but allows you to psychologically switch gears on research days,” he said.
The biggest place to make change, however, is within the health care system culture itself. The AMA created a series of recommendations to address burnout at the resident and fellow level, a good starting point to carry through into staff work. The steps include creating a well-being framework, gathering a team to support a well-being program, developing the program in a way to foster fun and connectivity among the staff, fostering individual well-being that addresses emotional and physical well-being, and confronting burnout and creating a sustainable culture of well-being.
On a personal level, it’s essential that physicians keep close tabs on themselves and peers. “Understand the signs and symptoms of burnout by taking stock of where you are emotionally,” said Dr. Gold. “Have a place and time at the end of a hard day to reflect or find a ritual that helps you and stay with it.”
You might also reach out to a therapist or a peer when you’re struggling. Having honest conversations with peers can go a long way. “Find a confidant that allows you to be vulnerable,” Dr. Gold recommended. “Acknowledge that this is hard and that you might need help taking care of yourself. The system needs to change, but we can also learn to survive in the meantime. You don’t have to be a sociopath to make it.”
A version of this article originally appeared on Medscape.com.
A frustrated physician recently voiced some strong words in Medscape’s US Physician Burnout & Depression Report: “Only a sociopath could work for a large health system and not be burned out. Anyone who cares about patients is doomed to burnout.”
Medscape’s report showed that 53% of physicians feel burned out by job requirements; 65% say that burnout has impacted their relationships, and other statistics say that physicians are leaving clinical medicine because of all this pressure.
What is it about being employed by large organizations that can be so negative? In another study, MEMO – Minimizing Error, Maximizing Outcomes – researchers at the University of Wisconsin surveyed more than 400 doctors to learn about how their working environments corresponded with medical errors. More than half of the physicians reported time pressures when conducting physical examinations. Nearly a third felt they needed at least 50% more time than was allotted for this patient care function, and nearly a quarter said they needed at least 50% more time for follow-up appointments.
Some have asked: Can anyone, then, thrive in today’s health care environment and avoid burnout?
Although the frustrated physician noted above may sardonically say that a doctor needs to be sociopathic to enjoy it – lacking in feelings for others – “It’s a very small number of doctors who get in it for the wrong reasons and therefore care about their own benefit and not their patients,” said psychiatrist Wendy Dean, MD, CEO and cofounder of Moral Injury of Healthcare, a nonprofit organization addressing workforce distress in health care. “Those are the outliers.”
The vast majority of physicians do care about their patients – deeply, said Dr. Dean. They struggle under the weight of the health care system and yet must find ways to get through. Today, thriving in an imperfect system requires honing new skills, asking for help when needed, and pushing for systemic and cultural change.
“We’ve been assessing and trying to address burnout for half a century,” said Dr. Dean. “Despite all the good intentions, and people dedicating their entire careers to solving the issue, we’ve barely made a dent.”
With the advent of new technological requirements on the job and more demands from increasingly larger health care organizations, the risk for burnout is higher than ever before. “There’s an increased burden of regulatory-mandated and cumbersome administrative workload per patient,” said Shomron Ben-Horin, MD, cofounder of Evinature. “Often the computer/paperwork before and after a procedure is much longer than the procedure itself.”
Meeting insurance requirements is increasingly cumbersome, too, and preauthorizations and debates with payers over medical approval may put physicians frustratingly in the middle.
“This increases the psychological burden for physicians who may feel responsible for wrongdoing no matter which option they deem better,” Dr. Ben-Horin said. “Add in physician accessibility around the clock via mobile phones, emails, and apps, and you end up on call even if you’re not officially on call.”
Why some physicians suffer more
Some physicians are more likely to suffer burnout than others, said Jessi Gold, MD, assistant professor in the department of psychiatry at Washington University in St. Louis. “The self-valuation concept comes into play here,” she said. “If you make a mistake, do you blame yourself or see it as a growth opportunity? If it’s the former, you’re more likely to burn out.”
Dr. Ben-Horin added that the most patient-centric doctors are the ones who struggle most. “These are the doctors we’d all love to have as a patient,” he said. “But they are burdened by the extra tasks of the job, and they are the most stressed by the environment.”
So too are those physicians who never master compartmentalizing their feelings and emotions. “We learn in training to compartmentalize our emotions,” said Dr. Dean. “You can’t allow yourself to get emotional while performing chest compressions on an 18-year-old kid. So you shut it all away; otherwise, you might lose the patient.”
This turn-off switch becomes automatic, but it also comes at a cost. “When doctors were interviewed about [Buffalo Bills player] Damar Hamlin going into cardiac arrest on the football field, they talked about how a life-and-death situation is so common that they have to put the emotions away, work on the patient, and move onto the next,” said Dr. Dean. “The next patient needs you just as much. We must lock away our feelings and manage the situation.”
Dr. Gold explained that burying feelings, however, is a symptom of burnout. “We have to remove ourselves from the situation to protect ourselves,” she said. “We can’t cry in these situations, but we can’t bury our feelings either.”
Instead, Dr. Gold suggested, a good medium may exist. “You may not be able to address them in the moment, but you should sometime after,” she said.
This is just a starting point on how to remain a dedicated, caring physician without burning out. “The system is pretty broken, and to survive it first means wanting to survive it,” Dr. Gold said. “There’s a lot of focus on resiliency and lack thereof if a physician expresses burnout, but that’s a false notion. Doctors are a resilient bunch but even they get burned out.”
Change for the better must come from several places. One is asking for help, something that can be hard for a group conditioned to keeping a stiff upper lip. “Just because your peers might look healthy (emotionally) doesn’t mean they are,” said Dr. Gold. “We’ve normalized this culture of burying feelings, but that doesn’t mean it’s right.”
Dr. Ben-Horin also advocates diversifying your work. This might include engaging in research and academics, for instance. “This not only makes you a better broad-perspective doctor but allows you to psychologically switch gears on research days,” he said.
The biggest place to make change, however, is within the health care system culture itself. The AMA created a series of recommendations to address burnout at the resident and fellow level, a good starting point to carry through into staff work. The steps include creating a well-being framework, gathering a team to support a well-being program, developing the program in a way to foster fun and connectivity among the staff, fostering individual well-being that addresses emotional and physical well-being, and confronting burnout and creating a sustainable culture of well-being.
On a personal level, it’s essential that physicians keep close tabs on themselves and peers. “Understand the signs and symptoms of burnout by taking stock of where you are emotionally,” said Dr. Gold. “Have a place and time at the end of a hard day to reflect or find a ritual that helps you and stay with it.”
You might also reach out to a therapist or a peer when you’re struggling. Having honest conversations with peers can go a long way. “Find a confidant that allows you to be vulnerable,” Dr. Gold recommended. “Acknowledge that this is hard and that you might need help taking care of yourself. The system needs to change, but we can also learn to survive in the meantime. You don’t have to be a sociopath to make it.”
A version of this article originally appeared on Medscape.com.
Not always implemented or enforced: Harassment policies at work
Many companies, government agencies, and organizations have implemented policies and procedures to shield employees from sexual and other forms of harassment. The U.S. Department of Health & Human Services and the American Medical Association are just two examples.
Employers can tap a rich lode of guidance and resources to craft these antiharassment policies. The National Institutes of Health’s resource page is a good site for hospitals to check out.
But how effective have official policies proved in deterring harassment in medical workplaces? After all, in a study by the American Association of Medical Colleges, 34% of female faculty said they had experienced sexual harassment irrespective of such policies. And in a recent Medscape survey of more than 3,000 physicians, 27% reported that they had either witnessed or been subjected to sexual harassment or misconduct at work during the past 4 years.
When policies are absent or unenforced
She believes employer rules and policies generally are helpful in establishing who fields harassment complaints and in creating at least some accountability.
On the other hand, policies that don’t recognize anonymous complaints effectively discourage harassment victims from coming forward, Dr. Rohr-Kirchgraber argues. Even those policies that do allow anonymous complaints may have limitations.
For example, the NIH policy on reporting harassment acknowledges that “officials must follow up on all allegations of harassment and cannot guarantee that your identity will not become apparent during the process. Please note that if you remain anonymous, key details about the allegation or concern [may] be omitted. This will limit the NIH’s ability to conduct an inquiry and take corrective action as warranted.”
Risks in pressing a harassment case
A complainant whose name becomes public risks getting a reputation as a problem employee or suffering workplace retaliation, according to Dr. Rohr-Kirchgraber. She recalls a colleague who was on a clinical education track until she lodged a harassment complaint. Abruptly, she was told she was needed on a service with fewer teaching opportunities.
With such risks in mind, respondents to the Medscape survey advised employees in medical workplaces to familiarize themselves with policies and procedures before pressing a case.
“Document everything,” an ophthalmologist urged, including time, place, offender, and witnesses. Present that information to your supervisor, and if nothing is done, hire a lawyer, a gastroenterologist suggested.
But taking the situation to the Equal Employment Opportunity Commission can be complicated, Roberta Gebhard, DO, past AMWA president and founder of its Gender Equity Task Force, told this news organization.
“They talk to the employer and get the employer’s side of the story and eventually render a decision about whether you have a case you can put through and file a lawsuit,” she said. “I don’t know of any other situation in which you need ‘permission’ to file a lawsuit.”
Nevertheless, an attorney can be helpful with cases, and when someone is terminated, a lawyer can possibly have it overturned or converted to a resignation, Dr. Gebhard said.
“And always have a lawyer review your contract before you take the job,” she advised. The lawyer might adjust the contract’s verbiage in ways that can protect one down the road in the event of a potential termination. “It’s money very well spent.”
More education needed
Dr. Rohr-Kirchgraber said that protection against harassment goes beyond the employer’s policies and procedures. Building an overall consciousness of what harassment is should begin with employee onboarding, she said.
“The harasser may not even recognize that what they’re doing or saying is a form of harassment, so we need better education,” Dr. Rohr-Kirchgraber emphasized.
A version of this article originally appeared on Medscape.com.
Many companies, government agencies, and organizations have implemented policies and procedures to shield employees from sexual and other forms of harassment. The U.S. Department of Health & Human Services and the American Medical Association are just two examples.
Employers can tap a rich lode of guidance and resources to craft these antiharassment policies. The National Institutes of Health’s resource page is a good site for hospitals to check out.
But how effective have official policies proved in deterring harassment in medical workplaces? After all, in a study by the American Association of Medical Colleges, 34% of female faculty said they had experienced sexual harassment irrespective of such policies. And in a recent Medscape survey of more than 3,000 physicians, 27% reported that they had either witnessed or been subjected to sexual harassment or misconduct at work during the past 4 years.
When policies are absent or unenforced
She believes employer rules and policies generally are helpful in establishing who fields harassment complaints and in creating at least some accountability.
On the other hand, policies that don’t recognize anonymous complaints effectively discourage harassment victims from coming forward, Dr. Rohr-Kirchgraber argues. Even those policies that do allow anonymous complaints may have limitations.
For example, the NIH policy on reporting harassment acknowledges that “officials must follow up on all allegations of harassment and cannot guarantee that your identity will not become apparent during the process. Please note that if you remain anonymous, key details about the allegation or concern [may] be omitted. This will limit the NIH’s ability to conduct an inquiry and take corrective action as warranted.”
Risks in pressing a harassment case
A complainant whose name becomes public risks getting a reputation as a problem employee or suffering workplace retaliation, according to Dr. Rohr-Kirchgraber. She recalls a colleague who was on a clinical education track until she lodged a harassment complaint. Abruptly, she was told she was needed on a service with fewer teaching opportunities.
With such risks in mind, respondents to the Medscape survey advised employees in medical workplaces to familiarize themselves with policies and procedures before pressing a case.
“Document everything,” an ophthalmologist urged, including time, place, offender, and witnesses. Present that information to your supervisor, and if nothing is done, hire a lawyer, a gastroenterologist suggested.
But taking the situation to the Equal Employment Opportunity Commission can be complicated, Roberta Gebhard, DO, past AMWA president and founder of its Gender Equity Task Force, told this news organization.
“They talk to the employer and get the employer’s side of the story and eventually render a decision about whether you have a case you can put through and file a lawsuit,” she said. “I don’t know of any other situation in which you need ‘permission’ to file a lawsuit.”
Nevertheless, an attorney can be helpful with cases, and when someone is terminated, a lawyer can possibly have it overturned or converted to a resignation, Dr. Gebhard said.
“And always have a lawyer review your contract before you take the job,” she advised. The lawyer might adjust the contract’s verbiage in ways that can protect one down the road in the event of a potential termination. “It’s money very well spent.”
More education needed
Dr. Rohr-Kirchgraber said that protection against harassment goes beyond the employer’s policies and procedures. Building an overall consciousness of what harassment is should begin with employee onboarding, she said.
“The harasser may not even recognize that what they’re doing or saying is a form of harassment, so we need better education,” Dr. Rohr-Kirchgraber emphasized.
A version of this article originally appeared on Medscape.com.
Many companies, government agencies, and organizations have implemented policies and procedures to shield employees from sexual and other forms of harassment. The U.S. Department of Health & Human Services and the American Medical Association are just two examples.
Employers can tap a rich lode of guidance and resources to craft these antiharassment policies. The National Institutes of Health’s resource page is a good site for hospitals to check out.
But how effective have official policies proved in deterring harassment in medical workplaces? After all, in a study by the American Association of Medical Colleges, 34% of female faculty said they had experienced sexual harassment irrespective of such policies. And in a recent Medscape survey of more than 3,000 physicians, 27% reported that they had either witnessed or been subjected to sexual harassment or misconduct at work during the past 4 years.
When policies are absent or unenforced
She believes employer rules and policies generally are helpful in establishing who fields harassment complaints and in creating at least some accountability.
On the other hand, policies that don’t recognize anonymous complaints effectively discourage harassment victims from coming forward, Dr. Rohr-Kirchgraber argues. Even those policies that do allow anonymous complaints may have limitations.
For example, the NIH policy on reporting harassment acknowledges that “officials must follow up on all allegations of harassment and cannot guarantee that your identity will not become apparent during the process. Please note that if you remain anonymous, key details about the allegation or concern [may] be omitted. This will limit the NIH’s ability to conduct an inquiry and take corrective action as warranted.”
Risks in pressing a harassment case
A complainant whose name becomes public risks getting a reputation as a problem employee or suffering workplace retaliation, according to Dr. Rohr-Kirchgraber. She recalls a colleague who was on a clinical education track until she lodged a harassment complaint. Abruptly, she was told she was needed on a service with fewer teaching opportunities.
With such risks in mind, respondents to the Medscape survey advised employees in medical workplaces to familiarize themselves with policies and procedures before pressing a case.
“Document everything,” an ophthalmologist urged, including time, place, offender, and witnesses. Present that information to your supervisor, and if nothing is done, hire a lawyer, a gastroenterologist suggested.
But taking the situation to the Equal Employment Opportunity Commission can be complicated, Roberta Gebhard, DO, past AMWA president and founder of its Gender Equity Task Force, told this news organization.
“They talk to the employer and get the employer’s side of the story and eventually render a decision about whether you have a case you can put through and file a lawsuit,” she said. “I don’t know of any other situation in which you need ‘permission’ to file a lawsuit.”
Nevertheless, an attorney can be helpful with cases, and when someone is terminated, a lawyer can possibly have it overturned or converted to a resignation, Dr. Gebhard said.
“And always have a lawyer review your contract before you take the job,” she advised. The lawyer might adjust the contract’s verbiage in ways that can protect one down the road in the event of a potential termination. “It’s money very well spent.”
More education needed
Dr. Rohr-Kirchgraber said that protection against harassment goes beyond the employer’s policies and procedures. Building an overall consciousness of what harassment is should begin with employee onboarding, she said.
“The harasser may not even recognize that what they’re doing or saying is a form of harassment, so we need better education,” Dr. Rohr-Kirchgraber emphasized.
A version of this article originally appeared on Medscape.com.
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
COVID-19 shot appears to reduce diabetes risk, even after Omicron
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Genomic clues to poor outcomes in young breast cancer patients
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
and offer clues about molecular targets for future trials.
Compared with older women with early stage HR-positive breast cancer, women under 40 years of age had significantly higher frequencies of certain mutations, such as GATA3, as well as genomic features associated with a poor prognosis. Notably, the researchers found that women with such poor prognostic features vs. those with none had a significantly worse 8-year distant recurrence-free interval and overall survival.
“We have demonstrated age-related differences in genomic profiles with enrichment of genomic features associated with poor prognosis in these younger premenopausal women compared with older premenopausal and postmenopausal women,” the authors wrote in the study, published in the Annals of Oncology. Importantly, the genomic features highlight “the potential for age-focused treatment strategies.”
Charis Eng, MD, PhD, of the Cleveland Clinic Genomic Medicine Institute, Ohio, noted that the findings are promising but need further validation.
“With time and the appropriate clinical trials in place, I envision that these findings will enable the personalized genomics-driven management of these cancers – not only treatment, but also toward prevention,” said Dr. Eng, who was not involved in the study.
Young premenopausal women, particularly those with HR-positive, luminal breast cancer, are known to have significantly higher recurrence rates and worse survival, compared with older women, but the reasons have remained unclear.
Although previous studies have identified key gene expression signatures linked to worse outcomes in younger patients with breast cancer, there are limited data on this younger patient population, especially by breast cancer subtype. Given that breast cancer treatment strategies are often similar across age groups, such evidence gaps could represent missed opportunities for developing more targeted treatment strategies for this high-risk population of young women.
To further investigate the cancer-specific genetic profiles in younger women, Sherene Loi, MD, PhD, of the Peter MacCallum Cancer Centre, University of Melbourne, and colleagues turned to data from the pivotal, multicenter Suppression of Ovarian Function Trial (SOFT).
Using next-generation sequencing, Dr. Loi and colleagues evaluated HR-positive, HER2-negative tumors among a subset of 1,276 premenopausal women who were diagnosed with early stage breast cancer. The study employed deep-targeted sequencing for most patients (n = 1,258) as well as whole-exome sequencing in a matched case-control subsample of young women with a median age of 38 years (n = 82).
Compared with women aged 40 and older, those under 40 years of age (n = 359) had significantly higher frequencies of mutations in GATA3 (19% vs. 16%) and copy number-amplifications (47% vs. 26%).
Younger women also had significantly higher features suggestive of homologous recombination deficiency (27% vs. 21% in older women), and a higher proportion of PIK3CA mutations with concurrent copy number-amplifications (23% vs. 11%, respectively), all considered to be poor prognostic features.
In addition, younger women had significantly lower frequencies of certain mutations, including PIK3CA (32% vs. 47%), CDH1 (3% vs. 9%), and MAP3K1 (7% vs. 12%), compared with older women.
Overall, 46% of women had poor prognostic features. These poor prognostic features were observed in 72% of patients under age 35, compared with 54% aged 35-39, and 40% of those 40 and over.
Compared with women without those features, women with poor prognostic features had a lower 8-year distant recurrence-free interval of 84% vs. 94% (hazard ratio, 1.85), and worse 8-year overall survival of 88% vs. 96%, respectively (HR, 2.20). Notably, younger women under age 40 had the poorest outcomes, with an 8-year distant recurrence-free interval rate of 74% vs. 85% in older women, and an 8-year overall survival of 80% vs. 93%, respectively.
How might these results inform potential therapeutics?
Drugs targeting the homologous recombination deficiency pathway are well established, and up to 36% of very young patients in the study showed genomic features of homologous recombination deficiency, the authors noted.
In addition, Dr. Eng explained, there are other Food and Drug Administration–approved treatments that can target the copy number amplified, PIK3CA-mutated tumors, including therapies that target PIK3CA itself, or proteins downstream of it. However, use of such therapies would need “to be tested experimentally, especially since pathway inhibition sometimes may result in rebound signaling to promote tumor growth,” Dr. Eng said.
An important caveat is that patients with germline BRCA1 or BRCA2 mutations may be underrepresented in the SOFT clinical trial, as the trial excluded patients who already had bilateral oophorectomy or planned to within 5 years, the authors noted.
Nevertheless, Dr. Loi said that the study is important because “there are no other datasets as large or with this long follow-up for very young women with breast cancer.”
Furthermore, “the SOFT clinical trial was practice-changing, so using the tumor samples associated with this study is more impactful than smaller cohorts with no outcome data or institutional retrospective cohorts,” she said.
Dr. Eng agreed that the study’s size is an important attribute, allowing the authors to “identify differences that would have been missed in a smaller and more heterogeneous series.”
She added that future research should also include ancestry and racial diversity.
“While young women have higher occurrences of aggressive breast cancers, mortality is twice as likely in young Black women, compared to young White women,” Dr. Eng said.
The study received funding from a Susan G. Komen for the Cure Promise Grant, the National Health and Research Council of Australia, the Breast Cancer Research Foundation, and the National Breast Cancer Foundation of Australia, and support from the family of Judy Eisman in Australia. Dr. Loi and Dr. Eng report no relevant financial disclosures.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF ONCOLOGY