User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Words, now actions: How medical associations try to fulfill pledges to combat racism in health care
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
– from health care outcomes, from the level and quality of patient treatment, from their own memberships. How have those pronouncements translated into programs that could have, or even have had, positive impacts?
For this article, this news organization asked several associations about tangible actions behind their vows to combat racism in health care. Meanwhile, a recent Medscape report focused on the degree to which physicians prioritize racial disparities as a leading social issue.
American Academy of Family Physicians
The American Academy of Family Physicians’ approach is to integrate diversity, equity, and inclusion (DEI) efforts into all existing and new projects rather than tackle racial disparities as a discrete problem.
“Our policies, our advocacy efforts, everything our commissions and staff do ... is through a lens of diversity, equity, and inclusiveness,” said AAFP Board Chair Ada D. Stewart, MD, FAAP.
That lens is ground by a DEI center the AAFP created in 2017. Run by AAFP staff, members, and chapters, the center focuses on five areas: policy, education and training, practice, diversifying the workplace, and strategic partnerships.
The center has established a special project called EveryONE to provide AAFP members with relevant research, policy templates, and other resources to address patient needs. One example is the Neighborhood Navigator, an online tool that shows food, housing, transportation, and other needs in a patient’s neighborhood.
Meanwhile, the DEI center has created training programs for AAFP members on topics like unconscious and implicit racial biases. And the AAFP has implemented several relevant governing policies regarding pushes to improve childbirth conditions and limit race-based treatment, among other areas.
In January, the AAFP established a new DEI commission for family medicine to set the academy’s agenda on racial issues moving forward. “We only had 10 physician positions available on the commission, and over 100 individuals applied, which gave us comfort that we were going in the right direction,” Dr. Stewart said.
Association of American Medical Colleges
The Association of American Medical Colleges, which represents nearly 600 U.S. and Canadian medical schools and teaching hospitals, has a “longstanding” focus on racial equity, said Philip Alberti, founder of the AAMC Center for Health Justice. However, in 2020 that focus became more detailed and layered.
Those layers include:
- Encouraging self-reflection by members on how personal racial biases and stereotypes can lead to systemic racism in health care.
- Working on the AAMC organizational structure. Priorities range from hiring a consultant to help guide antiracism efforts, to establishing a DEI council and advisors, to regularly seeking input from staff. In 2021, the AAMC launched a Center for Health Justice to work more closely with communities.
- Ramping up collaboration with national and local academic medicine organizations and partners. As one example, the AAMC and American Medical Association released a guide for physicians and health care professionals on language that could be interpreted as racist or disrespectful.
- Continuing to be outspoken about racial disparities in health care in society generally.
Meanwhile, the AAMC is supporting more specific, localized health equity efforts in cities such as Cincinnati and Boston.
Cincinnati Children’s Hospital research has found that children in poor neighborhoods are five times more likely to need hospital stays. AAMC members have helped identify “hot spots” for social needs among children and focused specifically on two neighborhoods in the city. The initiative has roped in partnerships with community and social service organizations as well as health care providers, and proponents say the number of child hospital stays in those neighborhoods has dropped by 20%.
Boston Medical Center researchers learned that Black and Latino patients experiencing problems with heart failure were less likely to be referred to a cardiologist. AAMC members assisted with a program to encourage physicians to make medically necessary referrals more often.
National Health Council
The National Health Council, an umbrella association of health organizations, similarly has made a “commitment, not just around policy work but anytime and anything the NHC is doing, to build around trying to identify and solve issues of health equity,” CEO Randall Rutta said.
The NHC has identified four strategic policy areas including race and in 2021 issued a statement signed by 45 other health care organizations vowing to take on systemic racism and advance equity, through public policy and law.
In relation to policy, Mr. Rutta said his organization is lobbying Congress and federal agencies to diversify clinical trials.
“We want to make sure that clinical trials are inclusive of people from different racial and ethnic groups, in order to understand how [they are] affected by a particular condition,” he said. “As you would imagine, some conditions hit certain groups harder than others for genetic or other reasons, or it may just be a reflection of other disparities that occur across health care.”
The organization has issued suggestions for policy change in the Food and Drug Administration’s clinical trial policy and separately targeted telemedicine policy to promote equity and greater patient access. For example, one initiative aims to ensure patients’ privacy and civil rights as telemedicine’s popularity grows after the COVID-19 pandemic. The NHC presented the initiative in a congressional briefing last year.
American Public Health Association
The American Public Health Association says it started focusing on racial disparities in health care in 2015, following a series of racially fueled violent acts. The APHA started with a four-part webinar series on racism in health (more than 10,000 live participants and 40,000 replays to date).
Shortly afterward, then-APHA President Camara Jones, MD, MPH, PhD, launched a national campaign encouraging APHA members, affiliates, and partners to name and address racism as a determinant of health.
More recently in 2021, the APHA adopted a “Truth, Racial Healing & Transformation” guiding framework and “Healing Through Policy” initiative that offer local leaders policy templates and best practices.
“We have identified a suite of policies that have actually been implemented successfully and are advancing racial equity,” said Regina Davis Moss, APHA’s associate executive director of health policy and practice. “You can’t advance health without having a policy that supports it.”
Montgomery County, Md., is one community that has used the framework (for racial equity training of county employees). Leaders in Evanston, Ill., also used it in crafting a resolution to end structural racism in the city.
A version of this article first appeared on Medscape.com.
Stop smoking and reduce death risk from pneumonia?
; the risk decreased even more with added years of not smoking, according to data from nearly 95,000 individuals.
Smoking is associated with an increased risk for pneumonia, but the extent to which smoking cessation reduces this risk long-term has not been explored, wrote Tomomi Kihara, MD, PhD, of the University of Tsukuba, Japan, and colleagues on behalf of the Japan Collaborative Cohort.
In the Japan Collaborative Cohort Study for Evaluation of Cancer Risk, known as the JACC Study, a community-based cohort of 110,585 individuals aged 40-79 years participated in health screening exams and self-administered questionnaires that included information about smoking. Other findings from the study have been previously published.
In the current study published in Preventive Medicine, the researchers reviewed data from 94,972 JACC participants who provided data about smoking status, including 59,514 never-smokers, 10,554 former smokers, and 24,904 current smokers. The mean age of the participants was 57 years; 57% were women.
The respondents were divided into groups based on years of smoking cessation: 0-1 year, 2-4 years, 5-9 years, 10-14 years, and 15 or more years. The primary endpoint was an underlying cause of death from pneumonia.
Over a median follow-up period of 19 years, 1,806 participants (1,115 men and 691 women) died of pneumonia.
In a multivariate analysis, the hazard ratio for those who quit smoking, compared with current smokers, was 1.02 for 0-1 year of smoking cessation, 0.92 for 2-4 years, 0.95 for 5-9 years, 0.71 for 10-14 years, and 0.63 (0.48-0.83) for 15 or more years. The HR for never smokers was 0.50. The analysis adjusted for competing risk for death without pneumonia in the study population.
Most of the benefits of smoking cessation occurred after 10-14 years, the researchers wrote in their discussion of the findings, and smoking cessation of 10 years or more resulted in risk for death from pneumonia similar to that of never-smokers.
“To our knowledge, no previous studies have examined the association between years of smoking cessation and pneumonia in a general population,” they added.
The study findings were limited by several factors, including the use of data on smoking and smoking cessation at baseline as well as a lack of data on the use of tobacco products other than cigarettes, although alternative tobacco products are rarely used in Japan, the researchers noted. Other limitations include the use of pneumonia mortality as an endpoint, which could have ignored the impact of smoking cessation on less severe pneumonia, and the inability to clarify the association between smoking cessation and pneumonia mortality by sex because of the small number of female former smokers. However, the results were strengthened by the large sample size and long observation period, they said.
“The present study provides empirical evidence that smoking cessation may lead to a decline in the risk of mortality from pneumonia,” and supports smoking cessation as a preventive measure, the researchers concluded.
The study was supported by the Japanese Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare, Health and Labor Sciences; and an Intramural Research Fund for Cardiovascular Diseases of National Cerebral and Cardiovascular Center. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
; the risk decreased even more with added years of not smoking, according to data from nearly 95,000 individuals.
Smoking is associated with an increased risk for pneumonia, but the extent to which smoking cessation reduces this risk long-term has not been explored, wrote Tomomi Kihara, MD, PhD, of the University of Tsukuba, Japan, and colleagues on behalf of the Japan Collaborative Cohort.
In the Japan Collaborative Cohort Study for Evaluation of Cancer Risk, known as the JACC Study, a community-based cohort of 110,585 individuals aged 40-79 years participated in health screening exams and self-administered questionnaires that included information about smoking. Other findings from the study have been previously published.
In the current study published in Preventive Medicine, the researchers reviewed data from 94,972 JACC participants who provided data about smoking status, including 59,514 never-smokers, 10,554 former smokers, and 24,904 current smokers. The mean age of the participants was 57 years; 57% were women.
The respondents were divided into groups based on years of smoking cessation: 0-1 year, 2-4 years, 5-9 years, 10-14 years, and 15 or more years. The primary endpoint was an underlying cause of death from pneumonia.
Over a median follow-up period of 19 years, 1,806 participants (1,115 men and 691 women) died of pneumonia.
In a multivariate analysis, the hazard ratio for those who quit smoking, compared with current smokers, was 1.02 for 0-1 year of smoking cessation, 0.92 for 2-4 years, 0.95 for 5-9 years, 0.71 for 10-14 years, and 0.63 (0.48-0.83) for 15 or more years. The HR for never smokers was 0.50. The analysis adjusted for competing risk for death without pneumonia in the study population.
Most of the benefits of smoking cessation occurred after 10-14 years, the researchers wrote in their discussion of the findings, and smoking cessation of 10 years or more resulted in risk for death from pneumonia similar to that of never-smokers.
“To our knowledge, no previous studies have examined the association between years of smoking cessation and pneumonia in a general population,” they added.
The study findings were limited by several factors, including the use of data on smoking and smoking cessation at baseline as well as a lack of data on the use of tobacco products other than cigarettes, although alternative tobacco products are rarely used in Japan, the researchers noted. Other limitations include the use of pneumonia mortality as an endpoint, which could have ignored the impact of smoking cessation on less severe pneumonia, and the inability to clarify the association between smoking cessation and pneumonia mortality by sex because of the small number of female former smokers. However, the results were strengthened by the large sample size and long observation period, they said.
“The present study provides empirical evidence that smoking cessation may lead to a decline in the risk of mortality from pneumonia,” and supports smoking cessation as a preventive measure, the researchers concluded.
The study was supported by the Japanese Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare, Health and Labor Sciences; and an Intramural Research Fund for Cardiovascular Diseases of National Cerebral and Cardiovascular Center. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
; the risk decreased even more with added years of not smoking, according to data from nearly 95,000 individuals.
Smoking is associated with an increased risk for pneumonia, but the extent to which smoking cessation reduces this risk long-term has not been explored, wrote Tomomi Kihara, MD, PhD, of the University of Tsukuba, Japan, and colleagues on behalf of the Japan Collaborative Cohort.
In the Japan Collaborative Cohort Study for Evaluation of Cancer Risk, known as the JACC Study, a community-based cohort of 110,585 individuals aged 40-79 years participated in health screening exams and self-administered questionnaires that included information about smoking. Other findings from the study have been previously published.
In the current study published in Preventive Medicine, the researchers reviewed data from 94,972 JACC participants who provided data about smoking status, including 59,514 never-smokers, 10,554 former smokers, and 24,904 current smokers. The mean age of the participants was 57 years; 57% were women.
The respondents were divided into groups based on years of smoking cessation: 0-1 year, 2-4 years, 5-9 years, 10-14 years, and 15 or more years. The primary endpoint was an underlying cause of death from pneumonia.
Over a median follow-up period of 19 years, 1,806 participants (1,115 men and 691 women) died of pneumonia.
In a multivariate analysis, the hazard ratio for those who quit smoking, compared with current smokers, was 1.02 for 0-1 year of smoking cessation, 0.92 for 2-4 years, 0.95 for 5-9 years, 0.71 for 10-14 years, and 0.63 (0.48-0.83) for 15 or more years. The HR for never smokers was 0.50. The analysis adjusted for competing risk for death without pneumonia in the study population.
Most of the benefits of smoking cessation occurred after 10-14 years, the researchers wrote in their discussion of the findings, and smoking cessation of 10 years or more resulted in risk for death from pneumonia similar to that of never-smokers.
“To our knowledge, no previous studies have examined the association between years of smoking cessation and pneumonia in a general population,” they added.
The study findings were limited by several factors, including the use of data on smoking and smoking cessation at baseline as well as a lack of data on the use of tobacco products other than cigarettes, although alternative tobacco products are rarely used in Japan, the researchers noted. Other limitations include the use of pneumonia mortality as an endpoint, which could have ignored the impact of smoking cessation on less severe pneumonia, and the inability to clarify the association between smoking cessation and pneumonia mortality by sex because of the small number of female former smokers. However, the results were strengthened by the large sample size and long observation period, they said.
“The present study provides empirical evidence that smoking cessation may lead to a decline in the risk of mortality from pneumonia,” and supports smoking cessation as a preventive measure, the researchers concluded.
The study was supported by the Japanese Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare, Health and Labor Sciences; and an Intramural Research Fund for Cardiovascular Diseases of National Cerebral and Cardiovascular Center. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
‘Medical Methuselahs’: Treating the growing population of centenarians
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
For about the past year, Priya Goel, MD, can be seen cruising around the island of Manhattan as she makes her way between visits to some of New York City’s most treasured residents: a small but essential group of patients born before the Empire State Building scraped the sky and the old Yankee Stadium had become the House That Ruth Built.
– the oldest is a 108-year-old man – whom she visits monthly.
The gray wave
Dr. Goel’s charges are among America’s latest baby boom – babies born a century ago, that is.
Between 1980 and 2019, the share of American centenarians, those aged 100 and up, grew faster than the total population. In 2019, 100,322 persons in the United States were at least 100 years old – more than triple the 1980 figure of 32,194, according to the U.S. Administration on Aging. By 2060, experts predict, the U.S. centenarian population will reach nearly 600,000.
Although some of the ultra-aged live in nursing homes, many continue to live independently. They require both routine and acute medical care. So, what does it take to be a physician for a centenarian?
Dr. Goel, who is in her mid-30s and could well be the great-granddaughter of some of her patients, urged her colleagues not to stereotype patients on the basis of age.
“You have to consider their functional and cognitive abilities, their ability to understand disease processes and make decisions for themselves,” Dr. Goel said. “Age is just one factor in the grand scheme of things.”
Visiting patients in their homes provides her with insights into how well they’re doing, including the safety of their environments and the depth of their social networks.
New York City has its peculiar demands. Heal provides Dr. Goel with a driver who chauffeurs her to her patient visits. She takes notes between stops.
“The idea is to have these patients remain in an environment where they’re comfortable, in surroundings where they’ve grown up or lived for many years,” she said. “A lot of them are in elevator buildings and they are wheelchair-bound or bed-bound and they physically can’t leave.”
She said she gets a far different view of the patient than does an office-based physician.
“When you go into their home, it’s very personal. You’re seeing what their daily environment is like, what their diet is like. You can see their food on the counter. You can see the level of hygiene,” Dr. Goel said. “You get to see their social support. Are their kids involved? Are they hoarding? Stuff that they wouldn’t just necessarily disclose but on a visit you get to see going into the home. It’s an extra layer of understanding that patient.”
Dr. Goel contrasted home care from care in a nursing home, where the patients are seen daily. On the basis of her observations, she decides whether to see her patients every month or every 3 months.
She applies this strategy to everyone from age 60 to over 100.
Tracking a growing group
Since 1995, geriatrician Thomas Perls, MD, has directed the New England Centenarian Study at Boston University. The study, largely funded by the National Institute on Aging, has enrolled 2,599 centenarian persons and 700 of their offspring. At any given time in the study, about 10% of the centenarians are alive. The study has a high mortality rate.
The people in Dr. Perls’s study range in age, but they top out at 119, the third oldest person ever in the world. Most centenarians are women.
“When we first began the study in 1995, the prevalence of centenarians in the United States was about 1 per 10,000 in the population,” Perls told this news organization. “And now, that prevalence has doubled to 1 per 5,000.”
Even if no one has achieved the record of Methuselah, the Biblical patriarch who was purported to have lived to the age of 969, some people always have lived into their 90s and beyond. Dr. Perls attributed the increase in longevity to control at the turn of the 20th century of typhoid fever, diphtheria, and other infectious diseases with effective public health measures, including the availability of clean water and improvement in socioeconomic conditions.
“Infant mortality just plummeted. So, come around 1915, 1920, we were no longer losing a quarter of our population to these diseases. That meant a quarter more of the population could age into adulthood and middle age,” he said. “A certain component of that group was, therefore, able to continue to age to a very, very old age.”
Other advances, such as antibiotics and vaccinations in the 1960s; the availability in the 1970s of much better detection and effective treatment of high blood pressure; the recognition of the harms of smoking; and much more effective treatment of cardiovascular disease and cancer have allowed many people who would have otherwise died in their 70s and 80s to live much longer. “I think what this means is that there is a substantial proportion of the population that has the biology to get to 100,” Dr. Perls said.
Perls said the Latino population and Blacks have a better track record than Whites in reaching the 100-year milestone. “The average life expectancy might be lower in these populations because of socioeconomic factors, but if they are able to get to around their early 80s, compared to Whites, their ability to get to 100 is actually better,” he said.
Asians fare best when it comes to longevity. While around 1% of White women in the United States live to 100, 10% of Asian women in Hong Kong hit that mark.
“I think some of that is better environment and health habits in Hong Kong than in the United States,” Dr. Perls said. “I think another piece may be a genetic advantage in East Asians. We’re looking into that.”
Dr. Perls said he agreed with Dr. Goel that health care providers and the lay public should not make assumptions on the basis of age alone as to how a person is doing. “People can age so very differently from one another,” he said.
Up to about age 90, the vast majority of those differences are determined by our health behaviors, such as smoking, alcohol use, exercise, sleep, the effect of our diets on weight, and access to good health care, including regular screening for problems such as high blood pressure, diabetes, and cancer. “People who are able to do everything right generally add healthy years to their lives, while those who do not have shorter life expectancies and longer periods of chronic diseases,” Dr. Perls said.
Paying diligent attention to these behaviors over the long run can have a huge payoff.
Dr. Perls’s team has found that to live beyond age 90 and on into the early 100s, protective genes can play a strong role. These genes help slow aging and decrease one’s risk for aging-related diseases. Centenarians usually have a history of aging very slowly and greatly delaying aging-related diseases and disability toward the ends of their lives.
Centenarians are the antithesis of the misguided belief that the older you get, the sicker you get. Quite the opposite occurs. For Dr. Perls, “the older you get, the healthier you’ve been.”
MD bias against the elderly?
Care of elderly patients is becoming essential in the practice of primary care physicians – but not all of them enjoy the work.
To be effective, physicians who treat centenarians must get a better idea of the individual patient’s functional status and comorbidities. “You absolutely cannot make assumptions on age alone,” Dr. Perls said.
The so-called “normal” temperature, 98.6° F, can spell trouble for centenarians and other very old patients, warned Natalie Baker, DNP, CRNP, an associate professor of nursing at the University of Alabama, Birmingham, and president of the 3,000-member Gerontological Advanced Practice Nurses Association.
“We have to be very cognizant of what we call a typical presentation of disease or illness and that a very subtle change in an older adult can signal a serious infection or illness,” Dr. Baker said. “If your patient has a high fever, that is a potential problem.”
The average temperature of an older adult is lower than the accepted 98.6° F, and their body’s response to an infection is slow to exhibit an increase in temperature, Dr. Baker said. “When treating centenarians, clinicians must be cognizant of other subtle signs of infection, such as decreased appetite or change in mentation,” she cautioned.
A decline in appetite or insomnia may be a subtle sign that these patients need to be evaluated, she added.
COVID-19 and centenarians
Three-quarters of the 1 million U.S. deaths from COVID-19 occurred in people aged 65 and older. However, Dr. Perls said centenarians may be a special subpopulation when it comes to COVID.
The Japanese Health Ministry, which follows the large centenarian population in that country, noted a marked jump in the number of centenarians during the pandemic – although the reasons for the increase aren’t clear.
Centenarians may be a bit different. Dr. Perls said some evidence suggests that the over-100 crowd may have better immune systems than younger people. “Part of the trick of getting to 100 is having a pretty good immune system,” he said.
Don’t mess with success
“There is no need at that point for us to try to alter their diet to what we think it might be,” Dr. Baker said. “There’s no need to start with diabetic education. They may tell you their secret is a shot of vodka every day. Why should we stop it at that age? Accept their lifestyles, because they’ve done something right to get to that age.”
Opinions differ on how to approach screening for centenarians.
Dr. Goel said guidelines for routine screening, such as colonoscopies, mammograms, and PAP smears, drop off for patients starting at 75. Dr. Perls said this strategy stems from the belief that people will die from other things first, so screening is no longer needed. Dr. Perls said he disagrees with this approach.
“Again, we can’t base our screening and health care decisions on age alone. If I have an independently functioning and robust 95-year-old man in my office, you can be sure I am going to continue recommending regular screening for colon cancer and other screenings that are normal for people who are 30 years younger,” he said.
Justin Zaghi, MD, chief medical officer at Heal, said screening patients in their late 90s and 100s for cancer generally doesn’t make sense except in some rare circumstances in which the cancer would be unlikely to be a cause of death. “However, if we are talking about screening for fall risks, hearing difficulties, poor vision, pain, and malnutrition, those screenings still absolutely make sense for patients in their late 90s and 100s,” Dr. Zaghi said.
One high-functioning 104-year-old patient of Dr. Perls underwent a total hip replacement for a hip fracture and is faring well. “Obviously, if she had end-stage dementia, we’d do everything to keep the person comfortable, or if they had medical problems that made surgery too high risk, then you don’t do it,” he said. “But if they’re otherwise, I would proceed.”
Avoid the ED
Dr. Goel said doctors should avoid sending patients to the emergency department, an often chaotic place that is especially unfriendly to centenarians and the very old. “Sometimes I’ve seen older patients who are being rushed to the ER, and I ask, What are the goals of care?” she said.
Clinicians caring for seniors should keep in mind that infections can cause seniors to appear confused – and this may lead the clinician to think the patient has dementia. Or, Dr. Goel said, a patient with dementia may suddenly experience much worse dementia.
“In either case, you want to make sure you’re not dealing with any underlying infection, like urinary tract infection, or pneumonia brewing, or skin infections,” she said. “Their skin is so much frailer. You want to make sure there are no bedsores.”
She has had patients whose children report that their usually placid centenarian parents are suddenly acting out. “We’ll do a urinary test and it definitely shows a urinary tract infection. You want to make sure you’re not missing out on something else before you attribute it to dementia,” she said.
Environmental changes, such as moving a patient to a new room in a hospital setting, can trigger an acute mental status change, such as delirium, she added. Helping older patients feel in control as much as possible is important.
“You want to make sure you’re orienting them to the time of day. Make sure they get up at the same time, go to bed at the same time, have clocks and calendars present – just making sure that they feel like they’re still in control of their body and their day,” she said.
Physicians should be aware of potential depression in these patients, whose experience of loss – an unavoidable consequence of outliving family and friends – can result in problems with sleep and diet, as well as a sense of social isolation.
Neal Flomenbaum, MD, professor and emergency physician-in-chief emeritus, New York–Presbyterian/Weill Cornell Medical Center in New York, said sometimes the best thing for these very elderly patients is to “get them in and out of ED as quickly as possible, and do what you can diagnostically.”
He noted that EDs have been making accommodations to serve the elderly, such as using LEDs that replicate outdoor lighting conditions, as well as providing seniors with separate rooms with glass doors to protect them from noise, separate air handlers to prevent infections, and adequate space for visitors.
These patients often are subject to trauma from falls.
“The bones don’t heal as well as in younger people, and treating their comorbidities is essential. Once they have trouble with one area and they’re lying in bed and can’t move much, they can get bedsores,” Dr. Flomenbaum said. “In the hospital, they are vulnerable to infections. So, you’re thinking of all of these things at the same time and how to treat them appropriately and then get them out of the hospital as soon as possible with whatever care that they need in their own homes if at all possible.”
“I always err on the side of less is more,” Dr. Goel said. “Obviously, if there is something – if they have a cough, they need an x-ray. That’s very basic. We want to take care of that. Give them the antibiotic if they need that. But rushing them in and out of the hospital doesn’t add to their quality of life.”
Dr. Flomenbaum, a pioneer in geriatric emergency medicine, says physicians need to be aware that centenarians and other very old patients don’t present the same way as younger adults.
He began to notice more than 20 years ago that every night, patients would turn up in his ED who were in their late 90s into their 100s. Some would come in with what their children identified as sudden-onset dementia – they didn’t know their own names and couldn’t identify their kids. They didn’t know the time or day. Dr. Flomenbaum said the children often asked whether their parents should enter a nursing home.
“And I’d say, ‘Not so fast. Well, let’s take a look at this.’ You don’t develop that kind of dementia overnight. It usually takes a while,” he said.
He said he ordered complete blood cell counts and oxygen saturation tests that frequently turned out to be abnormal. They didn’t have a fever, and infiltrates initially weren’t seen on chest x-rays.
With rehydration and supplemental oxygen, their symptoms started to improve, and it became obvious that the symptoms were not of dementia but of pneumonia, and that they required antibiotics, Dr. Flomenbaum said.
Dementia dilemma
Too often, on the basis of age, doctors assume patients have dementia or other cognitive impairments.
“What a shock and a surprise when doctors actually talk to folks and do a neurocognitive screen and find they’re just fine,” Dr. Perls said.
The decline in hearing and vision can lead to a misdiagnosis of cognitive impairment because the patients are not able to hear what you’re asking them. “It’s really important that the person can hear you – whether you use an amplifying device or they have hearing aids, that’s critical,” he said. “You just have to be a good doctor.”
Often the physical toll of aging exacerbates social difficulties. Poor hearing, for example, can accelerate cognitive impairment and cause people to interact less often, and less meaningfully, with their environment. For some, wearing hearing aids seems demeaning – until they hear what they’ve been missing.
“I get them to wear their hearing aids and, lo and behold, they’re a whole new person because they’re now able to take in their environment and interact with others,” Dr. Perls said.
Dr. Flomenbaum said alcohol abuse and drug reactions can cause delirium, which, unlike dementia, is potentially reversible. Yet many physicians cannot reliably differentiate between dementia and delirium, he added.
The geriatric specialists talk about the lessons they’ve learned and the gratification they get from caring for centenarians.
“I have come to realize the importance of family, of having a close circle, whether that’s through friends or neighbors,” Dr. Goel said. “This work is very rewarding because, if it wasn’t for homebound organizations, how would these people get care or get access to care?”
For Dr. Baker, a joy of the job is hearing centenarians share their life stories.
“I love to hear their stories about how they’ve overcome adversity, living through the depression and living through different wars,” she said. “I love talking to veterans, and I think that oftentimes, we do not value our older adults in our society as we should. Sometimes they are dismissed because they move slowly or are hard to communicate with due to hearing deficits. But they are, I think, a very important part of our lives.”
‘They’ve already won’
Most centenarians readily offer the secrets to their longevity. Aline Jacobsohn, of Boca Raton, Fla., is no different.
Ms. Jacobsohn, who will be 101 in October, thinks a diet of small portions of fish, vegetables, and fruit, which she has followed since her husband Leo died in 1982, has helped keep her healthy. She eats lots of salmon and herring and is a fan of spinach sautéed with olive oil. “The only thing I don’t eat is meat,” the trim and active Ms. Jacobsohn said in a recent interview over Zoom.
Her other secret: “Doctors. I like to stay away from them as much as possible.”
Shari Rosenbaum, MD, Jacobsohn’s internist, doesn’t dismiss that approach. She uses a version of it when managing her three centenarian patients, the oldest of whom is 103.
“Let them smoke! Let them drink! They’re happy. It’s not causing harm. Let them eat cake! They’ve already won,” said Dr. Rosenbaum, who is affiliated with Boca Raton–based MDVIP, a national membership-based network of 1,100 primary care physicians serving 368,000 patients. Of those, nearly 460 are centenarians.
“You’re not preventing those problems in this population,” she said. “They’re here to enjoy every moment that they have, and they might as well.”
Dr. Rosenbaum sees a divergence in her patients – those who will reach very old age, and those who won’t – starting in their 60s.
“The centenarians don’t have medical problems,” she said. “They don’t get cancer. They don’t get diabetes. Some of them take good care of themselves. Some don’t take such good care of themselves. But they are all optimists. They all see the glass half full. They all participate in life. They all have excellent support systems. They have good genes, a positive attitude toward life, and a strong social network.”
Ms. Jacobsohn – whose surname at the time was Bakst – grew up in Frankfurt am Main, Germany, during the rise of the Nazi regime. The family fled to Columbia in 1938, where she met and eventually married her husband, Leo, who ran a business importing clocks and watches in Cali.
In 1989, the Jacobsohns and their three children moved to south Florida to escape the dangers of kidnappings and ransoms posed by the drug cartels.
Ms. Jacobsohn agreed that she appears to have longevity genes – “good stock,” she calls it. “My mother died 23 days before she was 100. My grandmother lived till 99, almost 100,” she said.
Two years ago, she donated her car to a charity and stopped driving in the interest of her own safety and that of other drivers and pedestrians.
Ms. Jacobsohn has a strong support system. Two of her children live nearby and visit her nearly every day. A live-in companion helps her with the activities of daily life, including preparing meals.
Ms. Jacobsohn plays bridge regularly, and well. “I’m sorry to say that I’m a very good bridge player,” she said, frankly. “How is it possible that I’ve played bridge so well and then I don’t remember what I had for lunch yesterday?”
She reads, mainly a diet of history but occasionally novels, too. “They have to be engaging,” she said.
The loss of loved ones is an inevitable part of very old age. Her husband of 47 years died of emphysema, and one of her sons died in his 70s of prostate cancer.
She knows well the fate that awaits us all and accepts it philosophically.
“It’s a very normal thing that people die. You don’t live forever. So, whenever it comes, it’s okay. Enough is enough. Dayenu,” she said, using the Hebrew word for, “It would have been enough” – a favorite in the Passover Seder celebrating the ancient Jews’ liberation from slavery in Egypt.
Ms. Jacobsohn sang the song and then took a reporter on a Zoom tour of her tidy home and her large flower garden featuring Cattleya orchids from Colombia.
A version of this article first appeared on Medscape.com.
Exercise limitations in COPD – not everyone needs more inhalers
Chronic obstructive pulmonary disease (COPD) is defined by airway obstruction and alveolar damage caused by exposure to noxious air particles. The physiologic results include varying degrees of gas-exchange abnormality and mechanical respiratory limitation, often in the form of dynamic hyperinflation. There’s a third major contributor, though – skeletal muscle deconditioning. Only one of these abnormalities responds to inhalers.
When your patients with COPD report dyspnea or exercise intolerance, what do you do? Do you attempt to determine its character to pinpoint its origin? Do you quiz them about their baseline activity levels to quantify their conditioning? I bet you get right to the point and order a cardiopulmonary exercise test (CPET). That way you’ll be able to tease out all the contributors. Nah. Most likely you add an inhaler before continuing to rush through your COPD quality metrics: Vaccines? Check. Lung cancer screening? Check. Smoking cessation? Check.
The physiology of dyspnea and exercise limitation in COPD has been extensively studied. Work-of-breathing, dynamic hyperinflation, and gas-exchange inefficiencies interact with each other in complex ways to produce symptoms. The presence of deconditioning simply magnifies the existing abnormalities within the respiratory system by creating more strain at lower work rates. Acute exacerbations (AECOPD) and oral corticosteroids further aggravate skeletal muscle dysfunction.
The Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) Report directs clinicians to use inhalers to manage dyspnea. If they’re already on one inhaler, they get another. This continues until they’re stabilized on a long-acting beta-agonist (LABA), long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid (ICS). The GOLD report also advises pulmonary rehabilitation for any patient with grade B through D disease. Unfortunately, the pulmonary rehabilitation recommendation is buried in the text and doesn’t appear within the popularized pharmacologic algorithms in the report’s figures.
The data for adding inhalers on top of each other to reduce AECOPD and improve overall quality of life (QOL) are good. However, although GOLD tells us to keep adding inhalers for the dyspneic patient with COPD, the authors acknowledge that this hasn’t been systematically tested. The difference? A statement doesn’t require the same formal, rigorous scientific analysis known as the GRADE approach. Using this kind of analysis, a recent clinical practice guideline by the American Thoracic Society found no benefit in dyspnea or respiratory QOL with step-up from inhaler monotherapy.
Inhalers won’t do anything for gas-exchange inefficiencies and deconditioning, at least not directly. A recent CPET study from the CanCOLD network found ventilatory inefficiency in 23% of GOLD 1 and 26% of GOLD 2-4 COPD patients. The numbers were higher for those who reported dyspnea. Skeletal muscle dysfunction rates are equally high.
Thus, dyspnea and exercise intolerance are major determinants of QOL in COPD, but inhalers will only get you so far. At a minimum, make sure you get an activity/exercise history from your patients with COPD. For those who are sedentary, provide an exercise prescription (really, it’s not that hard to do). If dyspnea persists despite LABA or LAMA monotherapy, clarify the complaint before doubling down. Finally, try to get the patient into a good pulmonary rehabilitation program. They’ll thank you afterwards.
Dr. Holley is Associate Professor, department of medicine, Uniformed Services University of the Health Sciences and Program Director, Pulmonary and Critical Care Medical Fellowship, department of medicine, Walter Reed National Military Medical Center, both in Bethesda, Md. He reported receiving research grants from Fisher-Paykel and receiving income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Chronic obstructive pulmonary disease (COPD) is defined by airway obstruction and alveolar damage caused by exposure to noxious air particles. The physiologic results include varying degrees of gas-exchange abnormality and mechanical respiratory limitation, often in the form of dynamic hyperinflation. There’s a third major contributor, though – skeletal muscle deconditioning. Only one of these abnormalities responds to inhalers.
When your patients with COPD report dyspnea or exercise intolerance, what do you do? Do you attempt to determine its character to pinpoint its origin? Do you quiz them about their baseline activity levels to quantify their conditioning? I bet you get right to the point and order a cardiopulmonary exercise test (CPET). That way you’ll be able to tease out all the contributors. Nah. Most likely you add an inhaler before continuing to rush through your COPD quality metrics: Vaccines? Check. Lung cancer screening? Check. Smoking cessation? Check.
The physiology of dyspnea and exercise limitation in COPD has been extensively studied. Work-of-breathing, dynamic hyperinflation, and gas-exchange inefficiencies interact with each other in complex ways to produce symptoms. The presence of deconditioning simply magnifies the existing abnormalities within the respiratory system by creating more strain at lower work rates. Acute exacerbations (AECOPD) and oral corticosteroids further aggravate skeletal muscle dysfunction.
The Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) Report directs clinicians to use inhalers to manage dyspnea. If they’re already on one inhaler, they get another. This continues until they’re stabilized on a long-acting beta-agonist (LABA), long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid (ICS). The GOLD report also advises pulmonary rehabilitation for any patient with grade B through D disease. Unfortunately, the pulmonary rehabilitation recommendation is buried in the text and doesn’t appear within the popularized pharmacologic algorithms in the report’s figures.
The data for adding inhalers on top of each other to reduce AECOPD and improve overall quality of life (QOL) are good. However, although GOLD tells us to keep adding inhalers for the dyspneic patient with COPD, the authors acknowledge that this hasn’t been systematically tested. The difference? A statement doesn’t require the same formal, rigorous scientific analysis known as the GRADE approach. Using this kind of analysis, a recent clinical practice guideline by the American Thoracic Society found no benefit in dyspnea or respiratory QOL with step-up from inhaler monotherapy.
Inhalers won’t do anything for gas-exchange inefficiencies and deconditioning, at least not directly. A recent CPET study from the CanCOLD network found ventilatory inefficiency in 23% of GOLD 1 and 26% of GOLD 2-4 COPD patients. The numbers were higher for those who reported dyspnea. Skeletal muscle dysfunction rates are equally high.
Thus, dyspnea and exercise intolerance are major determinants of QOL in COPD, but inhalers will only get you so far. At a minimum, make sure you get an activity/exercise history from your patients with COPD. For those who are sedentary, provide an exercise prescription (really, it’s not that hard to do). If dyspnea persists despite LABA or LAMA monotherapy, clarify the complaint before doubling down. Finally, try to get the patient into a good pulmonary rehabilitation program. They’ll thank you afterwards.
Dr. Holley is Associate Professor, department of medicine, Uniformed Services University of the Health Sciences and Program Director, Pulmonary and Critical Care Medical Fellowship, department of medicine, Walter Reed National Military Medical Center, both in Bethesda, Md. He reported receiving research grants from Fisher-Paykel and receiving income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Chronic obstructive pulmonary disease (COPD) is defined by airway obstruction and alveolar damage caused by exposure to noxious air particles. The physiologic results include varying degrees of gas-exchange abnormality and mechanical respiratory limitation, often in the form of dynamic hyperinflation. There’s a third major contributor, though – skeletal muscle deconditioning. Only one of these abnormalities responds to inhalers.
When your patients with COPD report dyspnea or exercise intolerance, what do you do? Do you attempt to determine its character to pinpoint its origin? Do you quiz them about their baseline activity levels to quantify their conditioning? I bet you get right to the point and order a cardiopulmonary exercise test (CPET). That way you’ll be able to tease out all the contributors. Nah. Most likely you add an inhaler before continuing to rush through your COPD quality metrics: Vaccines? Check. Lung cancer screening? Check. Smoking cessation? Check.
The physiology of dyspnea and exercise limitation in COPD has been extensively studied. Work-of-breathing, dynamic hyperinflation, and gas-exchange inefficiencies interact with each other in complex ways to produce symptoms. The presence of deconditioning simply magnifies the existing abnormalities within the respiratory system by creating more strain at lower work rates. Acute exacerbations (AECOPD) and oral corticosteroids further aggravate skeletal muscle dysfunction.
The Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (GOLD) Report directs clinicians to use inhalers to manage dyspnea. If they’re already on one inhaler, they get another. This continues until they’re stabilized on a long-acting beta-agonist (LABA), long-acting muscarinic antagonist (LAMA), and an inhaled corticosteroid (ICS). The GOLD report also advises pulmonary rehabilitation for any patient with grade B through D disease. Unfortunately, the pulmonary rehabilitation recommendation is buried in the text and doesn’t appear within the popularized pharmacologic algorithms in the report’s figures.
The data for adding inhalers on top of each other to reduce AECOPD and improve overall quality of life (QOL) are good. However, although GOLD tells us to keep adding inhalers for the dyspneic patient with COPD, the authors acknowledge that this hasn’t been systematically tested. The difference? A statement doesn’t require the same formal, rigorous scientific analysis known as the GRADE approach. Using this kind of analysis, a recent clinical practice guideline by the American Thoracic Society found no benefit in dyspnea or respiratory QOL with step-up from inhaler monotherapy.
Inhalers won’t do anything for gas-exchange inefficiencies and deconditioning, at least not directly. A recent CPET study from the CanCOLD network found ventilatory inefficiency in 23% of GOLD 1 and 26% of GOLD 2-4 COPD patients. The numbers were higher for those who reported dyspnea. Skeletal muscle dysfunction rates are equally high.
Thus, dyspnea and exercise intolerance are major determinants of QOL in COPD, but inhalers will only get you so far. At a minimum, make sure you get an activity/exercise history from your patients with COPD. For those who are sedentary, provide an exercise prescription (really, it’s not that hard to do). If dyspnea persists despite LABA or LAMA monotherapy, clarify the complaint before doubling down. Finally, try to get the patient into a good pulmonary rehabilitation program. They’ll thank you afterwards.
Dr. Holley is Associate Professor, department of medicine, Uniformed Services University of the Health Sciences and Program Director, Pulmonary and Critical Care Medical Fellowship, department of medicine, Walter Reed National Military Medical Center, both in Bethesda, Md. He reported receiving research grants from Fisher-Paykel and receiving income from the American College of Chest Physicians.
A version of this article first appeared on Medscape.com.
Lung adverse effects in patients taking trastuzumab deruxtecan
although the benefit-to-risk relationship with use of the drug is still positive, say researchers who report a review of early clinical trials with the drug.
T-DXd is a monoclonal antibody that targets HER2. It is approved for use in HER2-positive breast, gastric, and lung cancers.
In the new study, investigators analyzed data from early clinical trials that involved patients with advanced cancers who had been heavily pretreated. They found an incidence of just over 15% for interstitial lung disease (ILD)/pneumonitis associated with the drug. Most patients (77.4%) had grade 1 or 2 ILD, but 2.2% of patients had grade 5 ILD.
“Interstitial lung disease is a known risk factor in patients treated with antibody conjugates for cancer,” commented lead author Charles Powell, MD, Icahn School of Medicine at Mount Sinai, New York. This adverse effect can lead to lung fibrosis and can become severe, life threatening, and even fatal, the authors warned.
The authors also discussed management of the event, which involves corticosteroids, and recommended that any patient who develops ILD of grade 3 or higher be hospitalized.
Close monitoring and proactive management may reduce the risk of ILD, they suggested.
Indeed, the incidence of this adverse effect was lower in a later phase 3 trial of the drug (10.5% in the DESTINY-Breast03 trial) and that the adverse events were less severe in this patient population (none of these events were of grade 4 or 5).
“Increased knowledge ... and implementation of ILD/pneumonitis monitoring, diagnosis, and management guidelines” may have resulted in this adverse effect being identified early and treated before it progressed, they commented.
ILD is highlighted in a boxed warning on the product label.
The study was published online in ESMO Open.
In their review, the investigators evaluated nine early-stage monotherapy clinical trials (phases 1 and 2) involving a total of 1,150 patients (breast cancer, 44.3%; gastric cancer, 25.6%; lung cancer, 17.7%; colorectal cancer, 9.3%, other cancers, 3.0%).
These patients had advanced cancer and had been heavily pretreated with a median of four prior lines of therapy. They received one or more doses of at least 5.4 mg/kg of T-DXd.
Nearly half of the cohort were treated for more than 6 months. A total of 276 potential ILD/pneumonitis events were sent for adjudication; of those, 85% were adjudicated as ILD/pneumonitis.
The overall incidence of adjudicated ILD/pneumonitis events was 15.4%; most were low-grade events. Some 87% of patients experienced their first ILD event within 12 months of treatment. The median time to experiencing an ILD/pneumonitis event was 5.4 months.
Some of the patients who developed grade 1 ILD/pneumonitis were treated and the adverse event resolved. These patients were then rechallenged with the drug. Only 3 of the 47 rechallenged patients experienced recurrence of ILD/pneumonitis, the authors noted.
“Rechallenge with T-DXd after complete resolution of grade 1 events is possible and warrants further investigation,” they commented. They cautioned, however, that rechallenge is not recommended for all patients, at least not for those with grade 2 or higher ILD/pneumonitis.
Overall, the authors concluded that the “benefit-risk of T-DXd treatment is positive,” but they warned that some patients may be at increased risk of developing ILD/pneumonitis
Baseline factors that increase the risk of developing an ILD/pneumonitis event include the following: being younger than 65 years, receiving a T-DXd dose of more than6.4 mg/kg, having a baseline oxygen saturation level of less than 95%, having moderate to severe renal impairment, and having lung comorbidities. In addition, patients who had initially been diagnosed with cancer more than 4 years before receiving the drug were at higher risk of developing ILD/pneumonitis.
“Using learnings from the early clinical trials experience, physician education and patient management protocols were revised and disseminated by the study sponsors [and] more recent trial data in earlier lines of therapy has demonstrated lower rates of ILD events, suggesting close monitoring and proactive management of ILD/pneumonitis is warranted for all patients,” Dr. Powell said in a statement.
The T-DXd clinical trials were sponsored by AstraZeneca and Daiichi Sankyo. Dr. Powell has received fees from Daiichi Sankyo, AstraZeneca, and Voluntis.
A version of this article first appeared on Medscape.com.
although the benefit-to-risk relationship with use of the drug is still positive, say researchers who report a review of early clinical trials with the drug.
T-DXd is a monoclonal antibody that targets HER2. It is approved for use in HER2-positive breast, gastric, and lung cancers.
In the new study, investigators analyzed data from early clinical trials that involved patients with advanced cancers who had been heavily pretreated. They found an incidence of just over 15% for interstitial lung disease (ILD)/pneumonitis associated with the drug. Most patients (77.4%) had grade 1 or 2 ILD, but 2.2% of patients had grade 5 ILD.
“Interstitial lung disease is a known risk factor in patients treated with antibody conjugates for cancer,” commented lead author Charles Powell, MD, Icahn School of Medicine at Mount Sinai, New York. This adverse effect can lead to lung fibrosis and can become severe, life threatening, and even fatal, the authors warned.
The authors also discussed management of the event, which involves corticosteroids, and recommended that any patient who develops ILD of grade 3 or higher be hospitalized.
Close monitoring and proactive management may reduce the risk of ILD, they suggested.
Indeed, the incidence of this adverse effect was lower in a later phase 3 trial of the drug (10.5% in the DESTINY-Breast03 trial) and that the adverse events were less severe in this patient population (none of these events were of grade 4 or 5).
“Increased knowledge ... and implementation of ILD/pneumonitis monitoring, diagnosis, and management guidelines” may have resulted in this adverse effect being identified early and treated before it progressed, they commented.
ILD is highlighted in a boxed warning on the product label.
The study was published online in ESMO Open.
In their review, the investigators evaluated nine early-stage monotherapy clinical trials (phases 1 and 2) involving a total of 1,150 patients (breast cancer, 44.3%; gastric cancer, 25.6%; lung cancer, 17.7%; colorectal cancer, 9.3%, other cancers, 3.0%).
These patients had advanced cancer and had been heavily pretreated with a median of four prior lines of therapy. They received one or more doses of at least 5.4 mg/kg of T-DXd.
Nearly half of the cohort were treated for more than 6 months. A total of 276 potential ILD/pneumonitis events were sent for adjudication; of those, 85% were adjudicated as ILD/pneumonitis.
The overall incidence of adjudicated ILD/pneumonitis events was 15.4%; most were low-grade events. Some 87% of patients experienced their first ILD event within 12 months of treatment. The median time to experiencing an ILD/pneumonitis event was 5.4 months.
Some of the patients who developed grade 1 ILD/pneumonitis were treated and the adverse event resolved. These patients were then rechallenged with the drug. Only 3 of the 47 rechallenged patients experienced recurrence of ILD/pneumonitis, the authors noted.
“Rechallenge with T-DXd after complete resolution of grade 1 events is possible and warrants further investigation,” they commented. They cautioned, however, that rechallenge is not recommended for all patients, at least not for those with grade 2 or higher ILD/pneumonitis.
Overall, the authors concluded that the “benefit-risk of T-DXd treatment is positive,” but they warned that some patients may be at increased risk of developing ILD/pneumonitis
Baseline factors that increase the risk of developing an ILD/pneumonitis event include the following: being younger than 65 years, receiving a T-DXd dose of more than6.4 mg/kg, having a baseline oxygen saturation level of less than 95%, having moderate to severe renal impairment, and having lung comorbidities. In addition, patients who had initially been diagnosed with cancer more than 4 years before receiving the drug were at higher risk of developing ILD/pneumonitis.
“Using learnings from the early clinical trials experience, physician education and patient management protocols were revised and disseminated by the study sponsors [and] more recent trial data in earlier lines of therapy has demonstrated lower rates of ILD events, suggesting close monitoring and proactive management of ILD/pneumonitis is warranted for all patients,” Dr. Powell said in a statement.
The T-DXd clinical trials were sponsored by AstraZeneca and Daiichi Sankyo. Dr. Powell has received fees from Daiichi Sankyo, AstraZeneca, and Voluntis.
A version of this article first appeared on Medscape.com.
although the benefit-to-risk relationship with use of the drug is still positive, say researchers who report a review of early clinical trials with the drug.
T-DXd is a monoclonal antibody that targets HER2. It is approved for use in HER2-positive breast, gastric, and lung cancers.
In the new study, investigators analyzed data from early clinical trials that involved patients with advanced cancers who had been heavily pretreated. They found an incidence of just over 15% for interstitial lung disease (ILD)/pneumonitis associated with the drug. Most patients (77.4%) had grade 1 or 2 ILD, but 2.2% of patients had grade 5 ILD.
“Interstitial lung disease is a known risk factor in patients treated with antibody conjugates for cancer,” commented lead author Charles Powell, MD, Icahn School of Medicine at Mount Sinai, New York. This adverse effect can lead to lung fibrosis and can become severe, life threatening, and even fatal, the authors warned.
The authors also discussed management of the event, which involves corticosteroids, and recommended that any patient who develops ILD of grade 3 or higher be hospitalized.
Close monitoring and proactive management may reduce the risk of ILD, they suggested.
Indeed, the incidence of this adverse effect was lower in a later phase 3 trial of the drug (10.5% in the DESTINY-Breast03 trial) and that the adverse events were less severe in this patient population (none of these events were of grade 4 or 5).
“Increased knowledge ... and implementation of ILD/pneumonitis monitoring, diagnosis, and management guidelines” may have resulted in this adverse effect being identified early and treated before it progressed, they commented.
ILD is highlighted in a boxed warning on the product label.
The study was published online in ESMO Open.
In their review, the investigators evaluated nine early-stage monotherapy clinical trials (phases 1 and 2) involving a total of 1,150 patients (breast cancer, 44.3%; gastric cancer, 25.6%; lung cancer, 17.7%; colorectal cancer, 9.3%, other cancers, 3.0%).
These patients had advanced cancer and had been heavily pretreated with a median of four prior lines of therapy. They received one or more doses of at least 5.4 mg/kg of T-DXd.
Nearly half of the cohort were treated for more than 6 months. A total of 276 potential ILD/pneumonitis events were sent for adjudication; of those, 85% were adjudicated as ILD/pneumonitis.
The overall incidence of adjudicated ILD/pneumonitis events was 15.4%; most were low-grade events. Some 87% of patients experienced their first ILD event within 12 months of treatment. The median time to experiencing an ILD/pneumonitis event was 5.4 months.
Some of the patients who developed grade 1 ILD/pneumonitis were treated and the adverse event resolved. These patients were then rechallenged with the drug. Only 3 of the 47 rechallenged patients experienced recurrence of ILD/pneumonitis, the authors noted.
“Rechallenge with T-DXd after complete resolution of grade 1 events is possible and warrants further investigation,” they commented. They cautioned, however, that rechallenge is not recommended for all patients, at least not for those with grade 2 or higher ILD/pneumonitis.
Overall, the authors concluded that the “benefit-risk of T-DXd treatment is positive,” but they warned that some patients may be at increased risk of developing ILD/pneumonitis
Baseline factors that increase the risk of developing an ILD/pneumonitis event include the following: being younger than 65 years, receiving a T-DXd dose of more than6.4 mg/kg, having a baseline oxygen saturation level of less than 95%, having moderate to severe renal impairment, and having lung comorbidities. In addition, patients who had initially been diagnosed with cancer more than 4 years before receiving the drug were at higher risk of developing ILD/pneumonitis.
“Using learnings from the early clinical trials experience, physician education and patient management protocols were revised and disseminated by the study sponsors [and] more recent trial data in earlier lines of therapy has demonstrated lower rates of ILD events, suggesting close monitoring and proactive management of ILD/pneumonitis is warranted for all patients,” Dr. Powell said in a statement.
The T-DXd clinical trials were sponsored by AstraZeneca and Daiichi Sankyo. Dr. Powell has received fees from Daiichi Sankyo, AstraZeneca, and Voluntis.
A version of this article first appeared on Medscape.com.
FROM ESMO OPEN
Primary care now offering physicians the 26.7-hour day
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Doctors using fake positive reviews to boost business
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Children and COVID: ED visits and new admissions change course
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).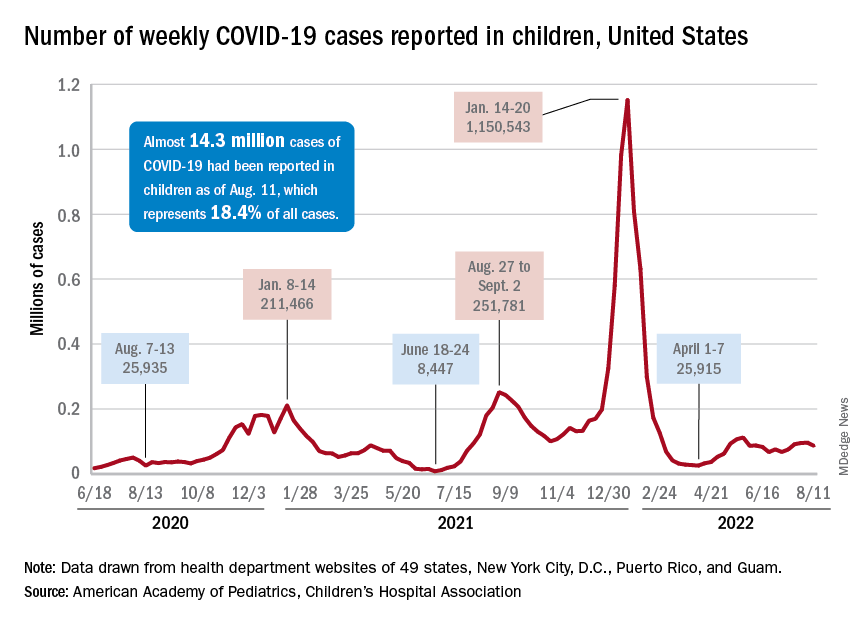
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).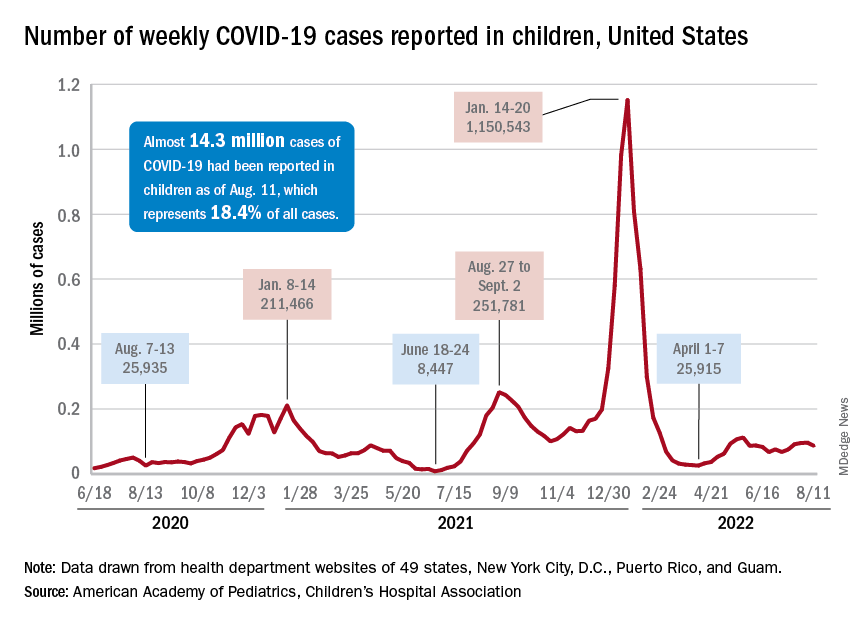
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
New child cases of COVID-19 made at least a temporary transition from slow increase to decrease, and emergency department visits and new admissions seem to be following a downward trend.
, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. For some historical perspective, the latest weekly count falls below last year’s Delta surge figure of 121,000 (Aug. 6-12) but above the summer 2020 total of 26,000 (Aug. 7-13).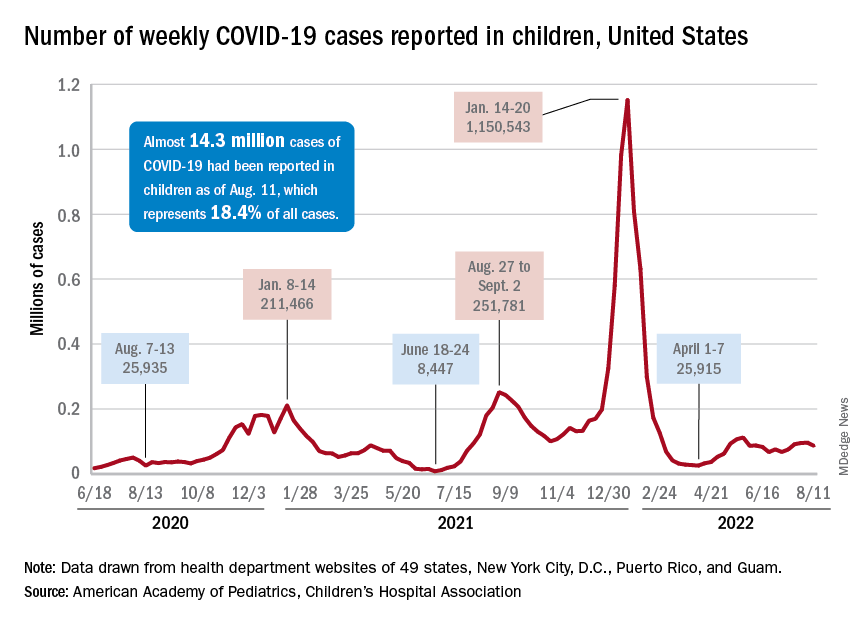
Measures of serious illness finally head downward
The prolonged rise in ED visits and new admissions over the last 5 months, which continued even through late spring when cases were declining, seems to have peaked, CDC data suggest.
That upward trend, driven largely by continued increases among younger children, peaked in late July, when 6.7% of all ED visits for children aged 0-11 years involved diagnosed COVID-19. The corresponding peaks for older children occurred around the same time but were only about half as high: 3.4% for 12- to 15-year-olds and 3.6% for those aged 16-17, the CDC reported.
The data for new admissions present a similar scenario: an increase starting in mid-April that continued unabated into late July despite the decline in new cases. By the time admissions among children aged 0-17 years peaked at 0.46 per 100,000 population in late July, they had reached the same level seen during the Delta surge. By Aug. 7, the rate of new hospitalizations was down to 0.42 per 100,000, the CDC said on its COVID Data Tracker.
The vaccine is ready for all students, but …
As children all over the country start or get ready to start a new school year, the only large-scale student vaccine mandate belongs to the District of Columbia. California has a mandate pending, but it will not go into effect until after July 1, 2023. There are, however, 20 states that have banned vaccine mandates for students, according to the National Academy for State Health Policy.
Nonmandated vaccination of the youngest children against COVID-19 continues to be slow. In the approximately 7 weeks (June 19 to Aug. 9) since the vaccine was approved for use in children younger than 5 years, just 4.4% of that age group has received at least one dose and 0.7% are fully vaccinated. Among those aged 5-11 years, who have been vaccine-eligible since early November of last year, 37.6% have received at least one dose and 30.2% are fully vaccinated, the CDC said.
Diagnosing children with long COVID can be tricky: Experts
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
When Spencer Siedlecki got COVID-19 in March 2021, he was sick for weeks with extreme fatigue, fevers, a sore throat, bad headaches, nausea, and eventually, pneumonia.
That was scary enough for the then-13-year-old and his parents, who live in Ohio. More than a year later, Spencer still had many of the symptoms and, more alarming, the once-healthy teen had postural orthostatic tachycardia syndrome, a condition that has caused dizziness, a racing heart when he stands, and fainting. Spencer missed most of the last few months of eighth grade because of long COVID.
“He gets sick very easily,” said his mother, Melissa Siedlecki, who works in technology sales. “The common cold that he would shake off in a few days takes weeks for him to feel better.”
The transformation from regular teen life to someone with a chronic illness “sucked,” said Spencer, who will turn 15 in August. “I felt like I was never going to get better.” Fortunately, after some therapy at a specialized clinic, Spencer is back to playing baseball and golf.
Spencer’s journey to better health was difficult; his regular pediatrician told the family at first that there were no treatments to help him – a reaction that is not uncommon. “I still get a lot of parents who heard of me through the grapevine,” said Amy Edwards, MD, director of the pediatric COVID clinic at University Hospitals Rainbow Babies & Children’s and an assistant professor of pediatrics at Case Western Reserve University, both in Cleveland. “The pediatricians either are unsure of what is wrong, or worse, tell children ‘there is nothing wrong with you. Stop faking it.’ ” Dr. Edwards treated Spencer after his mother found the clinic through an internet search.
Alexandra Yonts, MD, a pediatric infectious diseases doctor and director of the post-COVID program clinic at Children’s National Medical Center in Washington, has seen this too. she said.
But those who do get attention tend to be White and affluent, something Dr. Yonts said “doesn’t jibe with the epidemiologic data of who COVID has affected the most.” Black, Latino, and American Indian and Alaska Native children are more likely to be infected with COVID than White children, and have higher rates of hospitalization and death than White children.
It’s not clear whether these children have a particular risk factor, or if they are just the ones who have the resources to get to the clinics. But Dr. Yonts and Dr. Edwards believe many children are not getting the help they need. High-performing kids are coming in “because they are the ones whose symptoms are most obvious,” said Dr. Edwards. “I think there are kids out there who are getting missed because they’re already struggling because of socioeconomic reasons.”
Spencer is one of 14 million children who have tested positive for SARS-CoV-2 since the start of the pandemic. Many pediatricians are still grappling with how to address cases like Spencer’s. The American Academy of Pediatrics has issued only brief guidance on long COVID in children, in part because there have been so few studies to use as a basis for guidance.
The federal government is aiming to change that with a newly launched National Research Action Plan on Long COVID that includes speeding up research on how the condition affects children and youths, including their ability to learn and thrive.
A CDC study found children with COVID were significantly more likely to have smell and taste disturbances, circulatory system problems, fatigue and malaise, and pain. Those who had been infected had higher rates of acute blockage of a lung artery, myocarditis and weakening of the heart, kidney failure, and type 1 diabetes.
Difficult to diagnose
Even with increased media attention and more published studies on pediatric long COVID, it’s still hard for a busy primary care doctor “to sort through what could just be a cold or what could be a series of colds and trying to look at the bigger picture of what’s been going on in a 1- to 3-month period with a kid,” Dr. Yonts said.
Most children with potential or definite long COVID are still being seen by individual pediatricians, not in a specialized clinic with easy access to an army of specialists. It’s not clear how many of those pediatric clinics exist. Survivor Corps, an advocacy group for people with long COVID, has posted a map of locations providing care, but few are specialized or focus on pediatric long COVID.
Long COVID is different from multisystem inflammatory syndrome in children (MIS-C), which occurs within a month or so of infection, triggers high fevers and severe symptoms in the gut, and often results in hospitalization. MIS-C “is not subtle,” said Dr. Edwards.
The long COVID clinic doctors said most of their patients were not very sick at first. “Anecdotally, of the 83 kids that we’ve seen, most have had mild, very mild, or even asymptomatic infections initially,” and then went on to have long COVID, said Dr. Yonts.
“We see it even in children who have very mild disease or even are asymptomatic,” agreed Allison Eckard, MD, director of pediatric infectious diseases at the Medical University of South Carolina, Charleston.
Fatigue, mood problems
Dr. Yonts said 90% of her patients have fatigue, and many also have severe symptoms in their gut. Those and other long COVID symptoms will be looked at more closely in a 3-year study the Children’s National Medical Center is doing along with the National Institute of Allergy and Infectious Diseases.
There are no treatments for long COVID itself.
“Management is probably more the correct term for what we do in our clinic at this point,” said Dr. Yonts. That means dealing with fatigue and managing headache and digestive symptoms with medications or coping strategies. Guidelines from the American Academy of Physical Medicine and Rehabilitation help inform how to help kids safely resume exercise.
At the Children’s National Medical Center clinic, children will typically meet with a team of specialists including infectious diseases doctors on the same day, said Dr. Yonts. Psychologists help children with coping skills. Dr. Yonts is careful not to imply that long COVID is a psychological illness. Parents “will just shut down, because for so long, they’ve been told this is all a mental thing.”
In about a third of children, symptoms get better on their own, and most kids get better over time. But many still struggle. “We don’t talk about cure, because we don’t know what cure looks like,” said Dr. Edwards.
Vaccination may be best protection
Vaccination seems to help reduce the risk of long COVID, perhaps by as much as half. But parents have been slow to vaccinate children, especially the very young. The AAP reported that, as of Aug. 3, just 5% of children under age 5, 37% of those ages 5-11, and 69% of 12- to 17-year-olds have received at least one dose of a COVID-19 vaccine.
“We have tried to really push vaccine as one of the ways to help prevent some of these long COVID syndromes,” said Dr. Eckard. But that advice is not always welcome. Dr. Eckard told the story of a mother who refused to have her autistic son vaccinated, even as she tearfully pleaded for help with his long COVID symptoms, which had also worsened his autism. The woman told Dr. Eckard: “Nothing you can say will convince me to get him vaccinated.” She thought a vaccine could make his symptoms even worse.
The best prevention is to avoid being infected in the first place.
“The more times you get COVID, the more you increase your risk of getting long COVID,” said Dr. Yonts. “The more times you roll the dice, eventually your number could come up.
A version of this article first appeared on WebMD.com.
Patients who won’t pay: What’s your recourse?
Owing to the pandemic, job loss, and the possible loss of health insurance, patients have had more difficulty managing copays, coinsurance, and deductibles, not to mention other out-of-pocket health care charges.
“Many of our patients have lost their jobs or have had their hours cut back, and as a result, they are struggling to make ends meet,” said Ahmad Chaudhry, MD, a cardiothoracic surgeon in Lexington, Ky. “However, we cannot continue to provide care if our patients do not pay their bills.”
This news organization asked physicians what they do when their patients don’t pay. About 43% said that they continue to treat them and develop a payment plan; 13% send their bill to collections; 12% continue their care and write off their balance, and 25% choose other actions. Only 8% of physicians drop patients if they don’t pay.
Because you need to pay your own bills, what can you do about nonpaying patients?
Start with price transparency
In the past, patients never knew what their lab work or a chest EKG would cost because it wasn’t listed anywhere, and it was usually more than expected. Because of new legislation concerning health care price transparency, hospitals, health plans, and insurers must pony up with the actual fees, making them transparent to patients. Physician practices should follow suit and keep prices transparent too. Patients are more likely to pay their bills when prepared for the expense.
Patients with insurance often don’t know what they’ll be paying for their visit or their tests because they don’t know how much insurance will cover and what will be left for them to pay. Also, they may not know if they’ve met their deductible yet so they’re unsure whether insurance will even kick in. And patients without insurance still need to know what their costs will be upfront.
According to 10 insights from the Primary Care Consumer Choice Survey, 74% of health care consumers were willing to pay a $50 out-of-pocket charge to know the cost of their primary care visit.
Provide payment plans
Many patients have always needed payment plans. It’s one thing to post a sign at check-in telling patients that all monies are due at the time of service, but it’s another reality for a patient who can’t fork over the $250 charge they just unexpectedly spent in your office.
Discover Financial Services recently ran a survey, with results presented in the press release Americans are Delaying Non-Emergency Medical Care in Higher Numbers than Last Year, and found that many Americans with medical debt are delaying nonemergency medical care. For example, they put off seeing a specialist (52%), seeing a doctor for sickness (41%), and undergoing treatment plans recommended by their doctor (31%).
Turning an account over to collections should be a last resort. In addition, agencies typically charge 30%-40% of the total collected off the top.
Though collecting that amount is better than nothing, using a collection agency may have unexpected consequences. For instance, you’re trusting the agency you hire to collect to represent you and act on your practice’s behalf. If they’re rude or their tactics are harsh in the eyes of the patient or their relatives, it’s your reputation that is on the line.
Rather than use a collection agency, you could collect the payments yourself. When a patient fails to pay within about 3 months, begin mailing statements from the office, followed by firm but generous phone calls trying to collect. Industry estimates put the average cost of sending an invoice, including staff labor, printing, and postage, at about $35 per mailer. Some practices combat the added costs by offering a 20% prompt-pay discount. Offering payment plans is another option that helps garner eventual payment. Plus, practices should direct patients to third-party lenders such as CareCredit for larger bills.
On occasion, some small practices may allow a swap, such as allowing a patient to provide a service such as plumbing, electrical, or painting in exchange for working off the bill. Though it’s not ideal when it comes to finances, you may find it can work in a pinch for a cash-strapped patient. Make sure to keep records of what bills the patient’s work goes toward.
It often helps to incentivize your billing staff to follow up regularly, with various suggestions and tactics, to get patients to pay their bills. The incentive amount you offer will probably be less than if you had to use a collection agency.
Have a payment policy
Because your practice’s primary job is caring for patients’ physical and emotional needs, payment collection without coming off as insensitive can be tricky. “We understand these are difficult times for everyone, and we are doing our best to work with our patients,” said Dr. Chaudhry. Having a written payment policy can help build the bridge. A policy lets patients know what they can expect and can help prevent surprises over what occurs in the event of nonpayment. Your written policy should include:
- When payment is due.
- How the practice handles copays and deductibles.
- What forms of payment are accepted.
- Your policy regarding nonpayment.
Why patients don’t pay
A 2021 Healthcare Consumer Experience Study from Cedar found that medical bills are a source of anxiety and frustration for most patients, affecting their financial experience. More than half of the respondents said that paying a medical bill is stressful. Complicating matters, many health care practices rely on outdated payment systems, which may not provide patients with a clear view of what they owe and how to pay it.
The study found that 53% of respondents find understanding their plan’s coverage and benefits stressful, and 37% of patients won’t pay their bill if they can’t understand it.
People may think the patient is trying to get out of paying, which, of course, is sometimes true, but most of the time they want to pay, concluded the study. Most patients need a better explanation, communication, and accurate accounting of their out-of-pocket costs.
What can doctors do?
If you’re a physician who regularly sees patients who have problems paying their bills, you can take a few steps to minimize the financial impact on your practice:
- Bill the patient’s insurance directly to ensure you receive at least partial payment.
- Keep adequate records of services in case you need to pursue legal action.
- “Be understanding and flexible when it comes to payment arrangements, as this can often be the difference between getting paid and not getting paid at all,” said Dr. Chaudhry.
Distance yourself
When discussing payment policies, physicians should try to distance themselves from the actual collection process as much as possible. Well-meaning physicians often tell patients things like they can “figure something out “ financially or “work them in” during a scheduling conflict, but that often undermines the authority and credibility of the practice’s office staff. Plus, it teaches patients they can get their way if they work on the doctor’s soft spot – something you don’t want to encourage.
By following some of these measures, you can help ensure that your practice continues to thrive despite the challenges posed by nonpaying patients.
A version of this article first appeared on Medscape.com.
Owing to the pandemic, job loss, and the possible loss of health insurance, patients have had more difficulty managing copays, coinsurance, and deductibles, not to mention other out-of-pocket health care charges.
“Many of our patients have lost their jobs or have had their hours cut back, and as a result, they are struggling to make ends meet,” said Ahmad Chaudhry, MD, a cardiothoracic surgeon in Lexington, Ky. “However, we cannot continue to provide care if our patients do not pay their bills.”
This news organization asked physicians what they do when their patients don’t pay. About 43% said that they continue to treat them and develop a payment plan; 13% send their bill to collections; 12% continue their care and write off their balance, and 25% choose other actions. Only 8% of physicians drop patients if they don’t pay.
Because you need to pay your own bills, what can you do about nonpaying patients?
Start with price transparency
In the past, patients never knew what their lab work or a chest EKG would cost because it wasn’t listed anywhere, and it was usually more than expected. Because of new legislation concerning health care price transparency, hospitals, health plans, and insurers must pony up with the actual fees, making them transparent to patients. Physician practices should follow suit and keep prices transparent too. Patients are more likely to pay their bills when prepared for the expense.
Patients with insurance often don’t know what they’ll be paying for their visit or their tests because they don’t know how much insurance will cover and what will be left for them to pay. Also, they may not know if they’ve met their deductible yet so they’re unsure whether insurance will even kick in. And patients without insurance still need to know what their costs will be upfront.
According to 10 insights from the Primary Care Consumer Choice Survey, 74% of health care consumers were willing to pay a $50 out-of-pocket charge to know the cost of their primary care visit.
Provide payment plans
Many patients have always needed payment plans. It’s one thing to post a sign at check-in telling patients that all monies are due at the time of service, but it’s another reality for a patient who can’t fork over the $250 charge they just unexpectedly spent in your office.
Discover Financial Services recently ran a survey, with results presented in the press release Americans are Delaying Non-Emergency Medical Care in Higher Numbers than Last Year, and found that many Americans with medical debt are delaying nonemergency medical care. For example, they put off seeing a specialist (52%), seeing a doctor for sickness (41%), and undergoing treatment plans recommended by their doctor (31%).
Turning an account over to collections should be a last resort. In addition, agencies typically charge 30%-40% of the total collected off the top.
Though collecting that amount is better than nothing, using a collection agency may have unexpected consequences. For instance, you’re trusting the agency you hire to collect to represent you and act on your practice’s behalf. If they’re rude or their tactics are harsh in the eyes of the patient or their relatives, it’s your reputation that is on the line.
Rather than use a collection agency, you could collect the payments yourself. When a patient fails to pay within about 3 months, begin mailing statements from the office, followed by firm but generous phone calls trying to collect. Industry estimates put the average cost of sending an invoice, including staff labor, printing, and postage, at about $35 per mailer. Some practices combat the added costs by offering a 20% prompt-pay discount. Offering payment plans is another option that helps garner eventual payment. Plus, practices should direct patients to third-party lenders such as CareCredit for larger bills.
On occasion, some small practices may allow a swap, such as allowing a patient to provide a service such as plumbing, electrical, or painting in exchange for working off the bill. Though it’s not ideal when it comes to finances, you may find it can work in a pinch for a cash-strapped patient. Make sure to keep records of what bills the patient’s work goes toward.
It often helps to incentivize your billing staff to follow up regularly, with various suggestions and tactics, to get patients to pay their bills. The incentive amount you offer will probably be less than if you had to use a collection agency.
Have a payment policy
Because your practice’s primary job is caring for patients’ physical and emotional needs, payment collection without coming off as insensitive can be tricky. “We understand these are difficult times for everyone, and we are doing our best to work with our patients,” said Dr. Chaudhry. Having a written payment policy can help build the bridge. A policy lets patients know what they can expect and can help prevent surprises over what occurs in the event of nonpayment. Your written policy should include:
- When payment is due.
- How the practice handles copays and deductibles.
- What forms of payment are accepted.
- Your policy regarding nonpayment.
Why patients don’t pay
A 2021 Healthcare Consumer Experience Study from Cedar found that medical bills are a source of anxiety and frustration for most patients, affecting their financial experience. More than half of the respondents said that paying a medical bill is stressful. Complicating matters, many health care practices rely on outdated payment systems, which may not provide patients with a clear view of what they owe and how to pay it.
The study found that 53% of respondents find understanding their plan’s coverage and benefits stressful, and 37% of patients won’t pay their bill if they can’t understand it.
People may think the patient is trying to get out of paying, which, of course, is sometimes true, but most of the time they want to pay, concluded the study. Most patients need a better explanation, communication, and accurate accounting of their out-of-pocket costs.
What can doctors do?
If you’re a physician who regularly sees patients who have problems paying their bills, you can take a few steps to minimize the financial impact on your practice:
- Bill the patient’s insurance directly to ensure you receive at least partial payment.
- Keep adequate records of services in case you need to pursue legal action.
- “Be understanding and flexible when it comes to payment arrangements, as this can often be the difference between getting paid and not getting paid at all,” said Dr. Chaudhry.
Distance yourself
When discussing payment policies, physicians should try to distance themselves from the actual collection process as much as possible. Well-meaning physicians often tell patients things like they can “figure something out “ financially or “work them in” during a scheduling conflict, but that often undermines the authority and credibility of the practice’s office staff. Plus, it teaches patients they can get their way if they work on the doctor’s soft spot – something you don’t want to encourage.
By following some of these measures, you can help ensure that your practice continues to thrive despite the challenges posed by nonpaying patients.
A version of this article first appeared on Medscape.com.
Owing to the pandemic, job loss, and the possible loss of health insurance, patients have had more difficulty managing copays, coinsurance, and deductibles, not to mention other out-of-pocket health care charges.
“Many of our patients have lost their jobs or have had their hours cut back, and as a result, they are struggling to make ends meet,” said Ahmad Chaudhry, MD, a cardiothoracic surgeon in Lexington, Ky. “However, we cannot continue to provide care if our patients do not pay their bills.”
This news organization asked physicians what they do when their patients don’t pay. About 43% said that they continue to treat them and develop a payment plan; 13% send their bill to collections; 12% continue their care and write off their balance, and 25% choose other actions. Only 8% of physicians drop patients if they don’t pay.
Because you need to pay your own bills, what can you do about nonpaying patients?
Start with price transparency
In the past, patients never knew what their lab work or a chest EKG would cost because it wasn’t listed anywhere, and it was usually more than expected. Because of new legislation concerning health care price transparency, hospitals, health plans, and insurers must pony up with the actual fees, making them transparent to patients. Physician practices should follow suit and keep prices transparent too. Patients are more likely to pay their bills when prepared for the expense.
Patients with insurance often don’t know what they’ll be paying for their visit or their tests because they don’t know how much insurance will cover and what will be left for them to pay. Also, they may not know if they’ve met their deductible yet so they’re unsure whether insurance will even kick in. And patients without insurance still need to know what their costs will be upfront.
According to 10 insights from the Primary Care Consumer Choice Survey, 74% of health care consumers were willing to pay a $50 out-of-pocket charge to know the cost of their primary care visit.
Provide payment plans
Many patients have always needed payment plans. It’s one thing to post a sign at check-in telling patients that all monies are due at the time of service, but it’s another reality for a patient who can’t fork over the $250 charge they just unexpectedly spent in your office.
Discover Financial Services recently ran a survey, with results presented in the press release Americans are Delaying Non-Emergency Medical Care in Higher Numbers than Last Year, and found that many Americans with medical debt are delaying nonemergency medical care. For example, they put off seeing a specialist (52%), seeing a doctor for sickness (41%), and undergoing treatment plans recommended by their doctor (31%).
Turning an account over to collections should be a last resort. In addition, agencies typically charge 30%-40% of the total collected off the top.
Though collecting that amount is better than nothing, using a collection agency may have unexpected consequences. For instance, you’re trusting the agency you hire to collect to represent you and act on your practice’s behalf. If they’re rude or their tactics are harsh in the eyes of the patient or their relatives, it’s your reputation that is on the line.
Rather than use a collection agency, you could collect the payments yourself. When a patient fails to pay within about 3 months, begin mailing statements from the office, followed by firm but generous phone calls trying to collect. Industry estimates put the average cost of sending an invoice, including staff labor, printing, and postage, at about $35 per mailer. Some practices combat the added costs by offering a 20% prompt-pay discount. Offering payment plans is another option that helps garner eventual payment. Plus, practices should direct patients to third-party lenders such as CareCredit for larger bills.
On occasion, some small practices may allow a swap, such as allowing a patient to provide a service such as plumbing, electrical, or painting in exchange for working off the bill. Though it’s not ideal when it comes to finances, you may find it can work in a pinch for a cash-strapped patient. Make sure to keep records of what bills the patient’s work goes toward.
It often helps to incentivize your billing staff to follow up regularly, with various suggestions and tactics, to get patients to pay their bills. The incentive amount you offer will probably be less than if you had to use a collection agency.
Have a payment policy
Because your practice’s primary job is caring for patients’ physical and emotional needs, payment collection without coming off as insensitive can be tricky. “We understand these are difficult times for everyone, and we are doing our best to work with our patients,” said Dr. Chaudhry. Having a written payment policy can help build the bridge. A policy lets patients know what they can expect and can help prevent surprises over what occurs in the event of nonpayment. Your written policy should include:
- When payment is due.
- How the practice handles copays and deductibles.
- What forms of payment are accepted.
- Your policy regarding nonpayment.
Why patients don’t pay
A 2021 Healthcare Consumer Experience Study from Cedar found that medical bills are a source of anxiety and frustration for most patients, affecting their financial experience. More than half of the respondents said that paying a medical bill is stressful. Complicating matters, many health care practices rely on outdated payment systems, which may not provide patients with a clear view of what they owe and how to pay it.
The study found that 53% of respondents find understanding their plan’s coverage and benefits stressful, and 37% of patients won’t pay their bill if they can’t understand it.
People may think the patient is trying to get out of paying, which, of course, is sometimes true, but most of the time they want to pay, concluded the study. Most patients need a better explanation, communication, and accurate accounting of their out-of-pocket costs.
What can doctors do?
If you’re a physician who regularly sees patients who have problems paying their bills, you can take a few steps to minimize the financial impact on your practice:
- Bill the patient’s insurance directly to ensure you receive at least partial payment.
- Keep adequate records of services in case you need to pursue legal action.
- “Be understanding and flexible when it comes to payment arrangements, as this can often be the difference between getting paid and not getting paid at all,” said Dr. Chaudhry.
Distance yourself
When discussing payment policies, physicians should try to distance themselves from the actual collection process as much as possible. Well-meaning physicians often tell patients things like they can “figure something out “ financially or “work them in” during a scheduling conflict, but that often undermines the authority and credibility of the practice’s office staff. Plus, it teaches patients they can get their way if they work on the doctor’s soft spot – something you don’t want to encourage.
By following some of these measures, you can help ensure that your practice continues to thrive despite the challenges posed by nonpaying patients.
A version of this article first appeared on Medscape.com.