User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Metformin fails as early COVID-19 treatment but shows potential
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
Neither metformin, ivermectin, or fluvoxamine had any impact on reducing disease severity, hospitalization, or death from COVID-19, according to results from more than 1,000 overweight or obese adult patients in the COVID-OUT randomized trial.
However, metformin showed some potential in a secondary analysis.
Early treatment to prevent severe disease remains a goal in managing the ongoing COVID-19 pandemic, and biophysical modeling suggested that metformin, ivermectin, and fluvoxamine may serve as antivirals to help reduce severe disease in COVID-19 patients, Carolyn T. Bramante, MD, of the University of Minnesota, Minneapolis, and colleagues wrote.
“We started enrolling patients at the end of December 2020,” Dr. Bramante said in an interview. “At that time, even though vaccine data were coming out, we thought it was important to test early outpatient treatment with widely available safe medications with no interactions, because the virus would evolve and vaccine availability may be limited.”
In a study published in the New England Journal of Medicine, the researchers used a two-by-three factorial design to test the ability of metformin, ivermectin, and fluvoxamine to prevent severe COVID-19 infection in nonhospitalized adults aged 30-85 years. A total of 1,431 patients at six U.S. sites were enrolled within 3 days of a confirmed infection and less than 7 days after the start of symptoms, then randomized to one of six groups: metformin plus fluvoxamine; metformin plus ivermectin; metformin plus placebo; placebo plus fluvoxamine; placebo plus ivermectin; and placebo plus placebo.
A total of 1,323 patients were included in the primary analysis. The median age of the patients was 46 years, 56% were female (of whom 6% were pregnant), and all individuals met criteria for overweight or obesity. About half (52%) of the patients had been vaccinated against COVID-19.
The primary endpoint was a composite of hypoxemia, ED visit, hospitalization, or death. The analyses were adjusted for COVID-19 vaccination and other trial medications. Overall, the adjusted odds ratios of any primary event, compared with placebo, was 0.84 for metformin (P = .19), 1.05 for ivermectin (P = .78), and 0.94 for fluvoxamine (P = .75).
The researchers also conducted a prespecified secondary analysis of components of the primary endpoint. In this analysis, the aORs for an ED visit, hospitalization, or death was 0.58 for metformin, 1.39 for ivermectin, and 1.17 for fluvoxamine. The aORs for hospitalization or death were 0.47, 0.73, and 1.11 for metformin, ivermectin, and fluvoxamine, respectively. No medication-related serious adverse events were reported with any of the drugs during the study period.
The possible benefit for prevention of severe COVID-19 with metformin was a prespecified secondary endpoint, and therefore not definitive until more research has been completed, the researchers said. Metformin has demonstrated anti-inflammatory actions in previous studies, and has shown protective effects against COVID-19 lung injury in animal studies.
Previous observational studies also have shown an association between metformin use and less severe COVID-19 in patients already taking metformin. “The proposed mechanisms of action against COVID-19 for metformin include anti-inflammatory and antiviral activity and the prevention of hyperglycemia during acute illness,” they added.
The study findings were limited by several factors including the population age range and focus on overweight and obese patients, which may limit generalizability, the researchers noted. Other limitations include the disproportionately small percentage of Black and Latino patients and the potential lack of accuracy in identifying hypoxemia via home oxygen monitors.
However, the results demonstrate that none of the three repurposed drugs – metformin, ivermectin, and fluvoxamine – prevented primary events or reduced symptom severity in COVID-19, compared with placebos, the researchers concluded.
“Metformin had several streams of evidence supporting its use: in vitro, in silico [computer modeled], observational, and in tissue. We were not surprised to see that it reduced emergency department visits, hospitalization, and death,” Dr. Bramante said in an interview.
The take-home message for clinicians is to continue to look to guideline committees for direction on COVID-19 treatments, but to continue to consider metformin along with other treatments, she said.
“All research should be replicated, whether the primary outcome is positive or negative,” Dr. Bramante emphasized. “In this case, when our positive outcome was negative and secondary outcome was positive, a confirmatory trial for metformin is particularly important.”
Ineffective drugs are inefficient use of resources
“The results of the COVID-OUT trial provide persuasive additional data that increase the confidence and degree of certainty that fluvoxamine and ivermectin are not effective in preventing progression to severe disease,” wrote Salim S. Abdool Karim, MB, and Nikita Devnarain, PhD, of the Centre for the AIDS Programme of Research in South Africa, Durban, in an accompanying editorial.
At the start of the study, in 2020, data on the use of the three drugs to prevent severe COVID-19 were “either unavailable or equivocal,” they said. Since then, accumulating data support the current study findings of the nonefficacy of ivermectin and fluvoxamine, and the World Health Organization has advised against their use for COVID-19, although the WHO has not provided guidance for the use of metformin.
The authors called on clinicians to stop using ivermectin and fluvoxamine to treat COVID-19 patients.
“With respect to clinical decisions about COVID-19 treatment, some drug choices, especially those that have negative [World Health Organization] recommendations, are clearly wrong,” they wrote. “In keeping with evidence-based medical practice, patients with COVID-19 must be treated with efficacious medications; they deserve nothing less.”
The study was supported by the Parsemus Foundation, Rainwater Charitable Foundation, Fast Grants, and UnitedHealth Group Foundation. The fluvoxamine placebo tablets were donated by Apotex Pharmaceuticals. The ivermectin placebo and active tablets were donated by Edenbridge Pharmaceuticals. Lead author Dr. Bramante was supported the National Center for Advancing Translational Sciences and the National Institute of Diabetes and Digestive and Kidney Diseases. The researchers had no financial conflicts to disclose. Dr. Abdool Karim serves as a member of the World Health Organization Science Council. Dr. Devnarain had no financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
No fish can escape this net ... of COVID testing
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Something about this COVID testing smells fishy
The Chinese have been challenging America’s political and economic hegemony (yes, we did have to look that one up – you’re rude to ask) for some time, but now they’ve gone too far. Are we going to just sit here and let China do something more ridiculous than us in response to COVID? No way!
Here’s the deal: The government of the Chinese coastal city of Xiamen has decided that it’s not just the workers on returning fishing boats who have the potential to introduce COVID to the rest of the population. The fish also present a problem. So when the authorities say that everyone needs to be tested before they can enter the city, they mean everyone.
An employee of the municipal ocean development bureau told local media that “all people in Xiamen City need nucleic acid testing, and the fish catches must be tested as well,” according to the Guardian, which also said that “TV news reports showed officials swabbing the mouths of fish and the underside of crabs.”
In the words of George Takei: “Oh my.”
Hold on there a second, George Takei, because we here in the good old US of A have still got Los Angeles, where COVID testing also has taken a nonhuman turn. The LA County public health department recently announced that pets are now eligible for a free SARS-CoV-2 test through veterinarians and other animal care facilities.
“Our goal is to test many different species of animals including wildlife (deer, bats, raccoons), pets (dogs, cats, hamsters, pocket pets), marine mammals (seals), and more,” Veterinary Public Health announced.
Hegemony restored.
Not even God could save them from worms
The Dark Ages may not have been as dark and violent as many people think, but there’s no denying that life in medieval Europe kind of sucked. The only real alternative to serfdom was a job with the Catholic Church. Medieval friars, for example, lived in stone buildings, had access to fresh fruits and vegetables, and even had latrines and running water. Luxuries compared with the life of the average peasant.
So why then, despite having access to more modern sanitation and amenities, did the friars have so many gut parasites? That’s the question raised by a group of researchers from the University of Cambridge, who conducted a study of 19 medieval friars buried at a local friary (Oh, doesn’t your town have one of those?) and 25 local people buried at a nonreligious cemetery during a similar time period. Of those 19 friars, 11 were infected with worms and parasites, compared with just 8 of 25 townspeople.
This doesn’t make a lot of sense. The friars had a good life by old-time standards: They had basic sanitation down and a solid diet. These things should lead to a healthier population. The problem, the researchers found, is two pronged and a vicious cycle. First off, the friars had plenty of fresh food, but they used human feces to fertilize their produce. There’s a reason modern practice for human waste fertilization is to let the waste compost for 6 months: The waiting period allows the parasites a chance to kindly die off, which prevents reinfection.
Secondly, the friars’ diet of fresh fruits and vegetables mixed together into a salad, while appealing to our modern-day sensibilities, was not a great choice. By comparison, laypeople tended to eat a boiled mishmash of whatever they could find, and while that’s kind of gross, the key here is that their food was cooked. And heat kills parasites. The uncooked salads did no such thing, so the monks ate infected food, expelled infected poop, and grew more infected food with their infected poop.
Once the worms arrived, they never left, making them the worst kind of house guest. Read the room, worms, take your dinner and move on. You don’t have to go home, but you can’t stay here.
What’s a shared genotype between friends?
Do you find it hard to tell the difference between Katy Perry and Zooey Deschanel? They look alike, but they’re not related. Or are they? According to new research, people who look and act very similar but are not related may share DNA.
“Our study provides a rare insight into human likeness by showing that people with extreme look-alike faces share common genotypes, whereas they are discordant at the epigenome and microbiome levels,” senior author Manel Esteller of the Josep Carreras Leukemia Research Institute in Barcelona said in a written statement. “Genomics clusters them together, and the rest sets them apart.”
The Internet has been a great source in being able to find look-alikes. The research team found photos of doppelgangers photographed by François Brunelle, a Canadian artist. Using facial recognition algorithms, the investigators were able to measure likeness between the each pair of look-alikes. The participants also completed a questionnaire about lifestyle and provided a saliva sample.
The results showed that the look-alikes had similar genotypes but different DNA methylation and microbiome landscapes. The look-alikes also seemed to have similarities in weight, height, and behaviors such as smoking, proving that doppelgangers not only look alike but also share common interests.
Next time someone tells you that you look like their best friend Steve, you won’t have to wonder much what Steve is like.
The secret to a good relationship? It’s a secret
Strong relationships are built on honesty and trust, right? Being open with your partner and/or friends is usually a good practice for keeping the relationship healthy, but the latest evidence suggests that maybe you shouldn’t share everything.
According to the first known study on the emotional, behavioral, and relational aspect of consumer behavior, not disclosing certain purchases to your partner can actually be a good thing for the relationship. How? Well, it all has to do with guilt.
In a series of studies, the researchers asked couples about their secret consumptions. The most commonly hidden thing by far was a product (65%).
“We found that 90% of people have recently kept everyday consumer behaviors a secret from a close other – like a friend or spouse – even though they also report that they don’t think their partner would care if they knew about it,” Kelley Gullo Wight, one of the study’s two lead authors, said in a written statement.
Keeping a hidden stash of chocolate produces guilt, which the researchers found to be the key factor, making the perpetrator want to do more in the relationship to ease that sense of betrayal or dishonesty. They called it a “greater relationship investment,” meaning the person is more likely to do a little extra for their partner, like shell out more money for the next anniversary gift or yield to watching their partner’s favorite program.
So don’t feel too bad about that secret Amazon purchase. As long as the other person doesn’t see the box, nobody has to know. Your relationship can only improve.
Are we up the creek without a paddle? What COVID, monkeypox, and nature are trying to tell us
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Monkeypox. Polio. Covid. A quick glance at the news on any given day seems to indicate that outbreaks, epidemics, and perhaps even pandemics are increasing in frequency.
Granted, these types of events are hardly new; from the plagues of the 5th and 13th centuries to the Spanish flu in the 20th century and SARS-CoV-2 today, they’ve been with us from time immemorial.
What appears to be different, however, is not their frequency, but their intensity, with research reinforcing that we may be facing unique challenges and smaller windows to intervene as we move forward.
Findings from a modeling study, published in 2021 in Proceedings of the National Academy of Sciences, underscore that without effective intervention, the probability of extreme events like COVID-19 will likely increase threefold in the coming decades.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, told this news organization.
“It’s all been based on some unusual cluster of cases that were causing severe disease and overwhelming local authorities. So often, like Indiana Jones, somebody got dispatched to deal with an outbreak,” Dr. Adalja said.
In a perfect post-COVID world, government bodies, scientists, clinicians, and others would cross silos to coordinate pandemic prevention, not just preparedness. The public would trust those who carry the title “public health” in their daily responsibilities, and in turn, public health experts would get back to their core responsibility – infectious disease preparedness – the role they were initially assigned following Europe’s Black Death during the 14th century. Instead, the world finds itself at a crossroads, with emerging and reemerging infectious disease outbreaks that on the surface appear to arise haphazardly but in reality are the result of decades of reaction and containment policies aimed at putting out fires, not addressing their cause.
Dr. Adalja noted that only when the threat of biological weapons became a reality in the mid-2000s was there a realization that economies of scale could be exploited by merging interests and efforts to develop health security medical countermeasures. For example, it encouraged governments to more closely integrate agencies like the Biomedical Advanced Research and Development Authority and infectious disease research organizations and individuals.
Still, while significant strides have been made in certain areas, the ongoing COVID-19 pandemic has revealed substantial weaknesses remaining in public and private health systems, as well as major gaps in infectious disease preparedness.
The role of spillover events
No matter whom you ask, scientists, public health and conservation experts, and infectious disease clinicians all point to one of the most important threats to human health. As Walt Kelly’s Pogo famously put it, “We have met the enemy, and he is us.”
“The reason why these outbreaks of novel infectious diseases are increasingly occurring is because of human-driven environmental change, particularly land use, unsafe practices when raising farmed animals, and commercial wildlife markets,” Neil M. Vora, MD, a physician specializing in pandemic prevention at Conservation International and a former Centers for Disease Control and Prevention epidemic intelligence officer, said in an interview.
In fact, more than 60% of emerging infections and diseases are due to these “spillover events” (zoonotic spillover) that occur when pathogens that commonly circulate in wildlife jump over to new, human hosts.
Several examples come to mind.
COVID-19 may have begun as an enzootic virus from two undetermined animals, using the Huanan Seafood Market as a possible intermediate reservoir, according to a July 26 preprint in the journal Science.
Likewise, while the Ebola virus was originally attributed to deforestation efforts to create palm oil (which allowed fruit bat carriers to transfer the virus to humans), recent research suggests that bats dwelling in the walls of human dwellings and hospitals are responsible for the 2018 outbreak in the Democratic Republic of Congo.
(Incidentally, just this week, a new Ebola case was confirmed in Eastern Congo, and it has been genetically linked to the previous outbreak, despite that outbreak having been declared over in early July.)
“When we clear forests, we create opportunities for humans to live alongside the forest edge and displace wildlife. There’s evidence that shows when [these] biodiverse areas are cleared, specialist species that evolved to live in the forests first start to disappear, whereas generalist species – rodents and bats – continue to survive and are able to carry pathogens that can be passed on to humans,” Dr. Vora explained.
So far, China’s outbreak of the novel Langya henipavirus is believed to have spread (either directly or indirectly) by rodents and shrews, according to reports from public health authorities like the European Centre for Disease Prevention and Control, which is currently monitoring the situation.
Yet, an overreliance on surveillance and containment only perpetuates what Dr. Vora says are cycles of panic and neglect.
“We saw it with Ebola in 2015, in 2016 to 2017 with Zika, you see it with tuberculosis, with sexually transmitted infections, and with COVID. You have policymakers working on solutions, and once they think that they’ve fixed the problem, they’re going to move on to the next crisis.”
It’s also a question of equity.
Reports detailing the reemergence of monkeypox in Nigeria in 2017 were largely ignored, despite the fact that the United States assisted in diagnosing an early case in an 11-year-old boy. At the time, it was clear that the virus was spreading by human-to-human transmission versus animal-to-human transmission, something that had not been seen previously.
“The current model [is] waiting for pathogens to spill over and then [continuing] to spread signals that rich countries are tolerant of these outbreaks so long as they don’t grow into epidemics or pandemics,” Dr. Vora said.
This model is clearly broken; roughly 5 years after Nigeria reported the resurgence of monkeypox, the United States has more than 14,000 confirmed cases, which represents more than a quarter of the total number of cases reported worldwide.
Public health on the brink
I’s difficult to imagine a future without outbreaks and more pandemics, and if experts are to be believed, we are ill-prepared.
“I think that we are in a situation where this is a major threat, and people have become complacent about it,” said Dr. Adalja, who noted that we should be asking ourselves if the “government is actually in a position to be able to respond in a way that we need them to or is [that response] tied up in bureaucracy and inefficiency?”
COVID-19 should have been seen as a wake-up call, and many of those deaths were preventable. “With monkeypox, they’re faltering; it should have been a layup, not a disaster,” he emphasized.
Ellen Eaton, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, also pointed to the reality that by the time COVID-19 reached North America, the United States had already moved away from the model of the public health department as the epicenter of knowledge, education, awareness, and, ironically, public health.
“Thinking about my community, very few people knew the face and name of our local and state health officers,” she told this news organization.
“There was just this inherent mistrust of these people. If you add in a lot of talking heads, a lot of politicians and messaging from non-experts that countered what was coming out of our public health agencies early, you had this huge disconnect; in the South, it was the perfect storm for vaccine hesitancy.”
At last count, this perfect storm has led to 1.46 million COVID cases and just over 20,000 deaths – many of which were preventable – in Alabama alone.
“In certain parts of America, we were starting with a broken system with limited resources and few providers,” Dr. Eaton explained.
Dr. Eaton said that a lot of fields, not just medicine and public health, have finite resources that have been stretched to capacity by COVID, and now monkeypox, and wondered what was next as we’re headed into autumn and influenza season. But she also mentioned the tremendous implications of climate change on infectious diseases and community health and wellness.
“There’s a tremendous need to have the ability to survey not just humans but also how the disease burden in our environment that is fluctuating with climate change is going to impact communities in really important ways,” Dr. Eaton said.
Upstream prevention
Dr. Vora said he could not agree more and believes that upstream prevention holds the key.
“We have to make sure while there’s tension on this issue that the right solutions are implemented,” he said.
In coming years, postspillover containment strategies – vaccine research and development and strengthening health care surveillance, for example – are likely to become inadequate.
“We saw it with COVID and we are seeing it again with monkeypox,” Dr. Vora said. “We also have to invest further upstream to prevent spillovers in the first place, for example, by addressing deforestation, commercial wildlife markets and trade, [and] infection control when raising farm animals.”
“The thing is, when you invest in those upstream solutions, you are also mitigating climate change and loss of biodiversity. I’m not saying that we should not invest in postspillover containment efforts; we’re never going to contain every spillover. But we also have to invest in prevention,” he added.
In a piece published in Nature, Dr. Vora and his coauthors acknowledge that several international bodies such as the World Health Organization and G7 have invested in initiatives to facilitate coordinated, global responses to climate change, pandemic preparedness, and response. But they point out that these efforts fail to “explicitly address the negative feedback cycle between environmental degradation, wildlife exploitation, and the emergence of pathogens.”
“Environmental conservation is no longer a left-wing fringe issue, it’s moving into public consciousness, and ... it is public health,” Dr. Vora said. “When we destroy nature, we’re destroying our own ability to survive.”
Dr. Adalja, Dr. Vora, and Dr. Eaton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases fall again, ED rates rebound for some
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.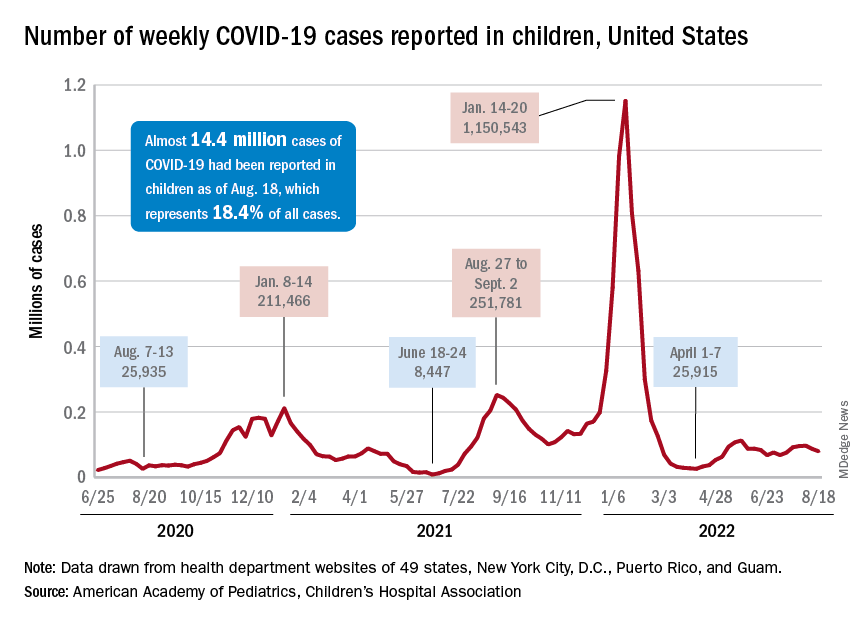
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
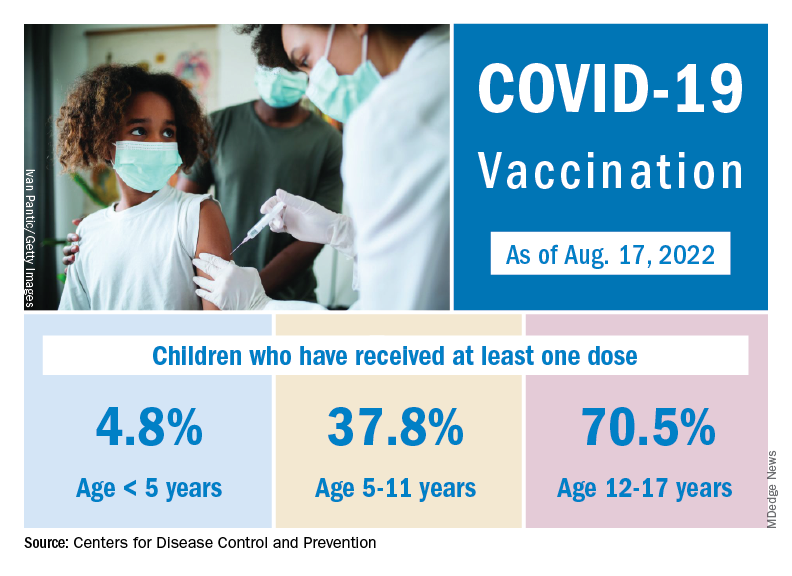
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.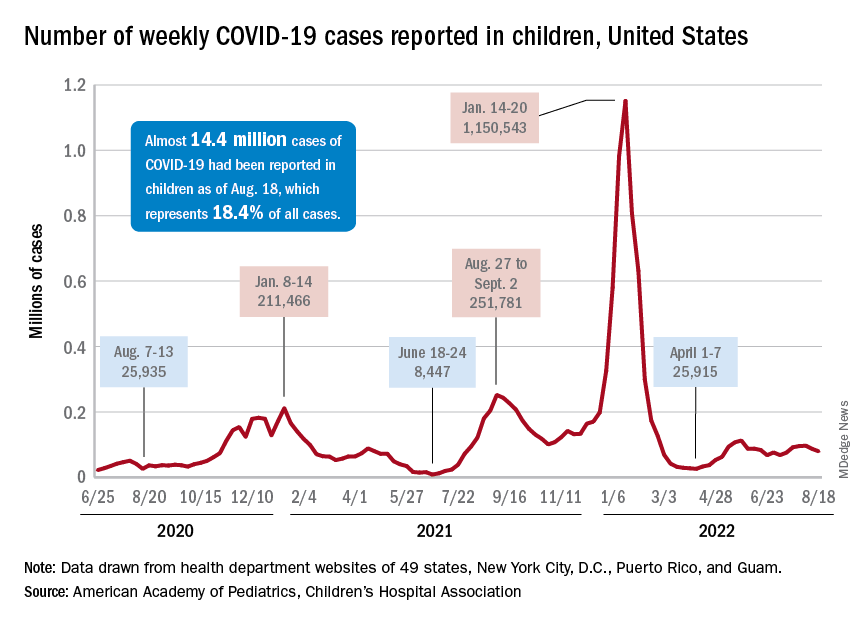
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
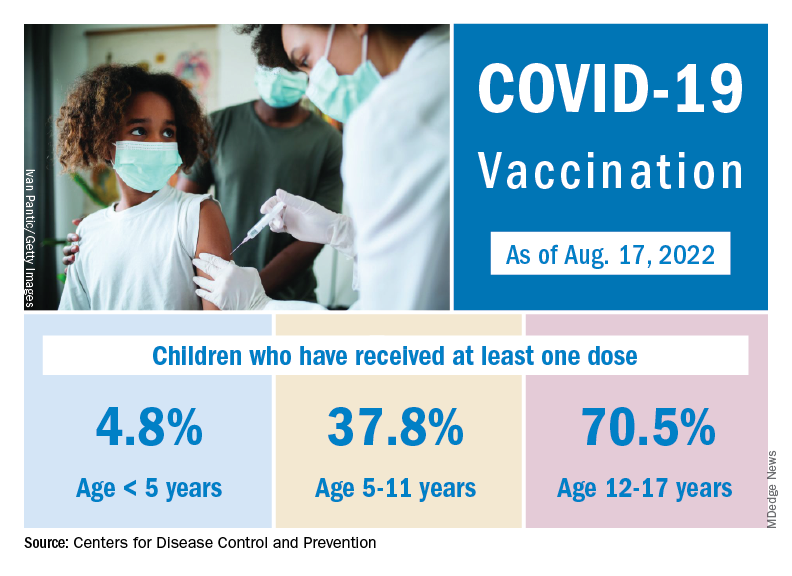
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
The 7-day average percentage of ED visits with diagnosed COVID, which had reached a post-Omicron high of 3.5% in late July for those aged 12-15, began to fall and was down to 3.0% on Aug. 12. That trend reversed, however, and the rate was up to 3.6% on Aug. 19, the last date for which data are available from the Centers for Disease Control and Prevention.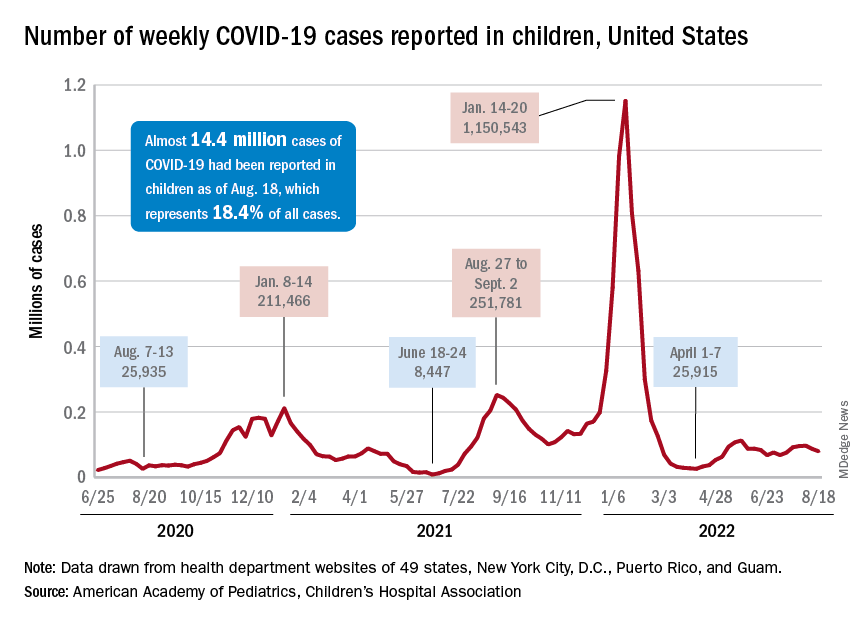
That change of COVID fortunes cannot yet be seen for all children. The 7-day average ED visit rate for those aged 0-11 years peaked at 6.8% during the last week of July and has continued to fall, dropping from 5.7% on Aug. 12 to 5.1% on Aug. 19. Children aged 16-17 years seem to be taking a middle path: Their ED-visit rate declined from late July into mid-August but held steady over the last week, according to the CDC’s COVID Data Tracker.
There is a hint of the same trend regarding new admissions among children aged 0-17 years. The national rate, which had declined in recent weeks, ticked up from 0.42 to 0.43 new admissions per 100,000 population over the last week of available data, the CDC said.
Weekly cases fall below 80,000
New cases in general were down by 8.5% from the previous week, dropping from 87,902 for the week of Aug. 5-11 to 79,525 for Aug. 12-18. That marked the second straight week with fewer cases after a 4-week period that saw weekly totals increase from almost 68,000 to nearly 97,000, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP and CHA put the cumulative number of child COVID-19 cases at just under 14.4 million since the pandemic began, which represents 18.4% of cases among all ages. The CDC estimates that there have been almost 14.7 million cases in children aged 0-17 years, as well as 1,750 deaths, of which 14 were reported in the last week (Aug. 16-22).
The CDC age subgroups indicate that children aged 0-4 years have experienced fewer cases (2.9 million) than children aged 5-11 years (5.6 million cases) and 12-15 (3.0 million cases) but more deaths: 548 so far, versus 432 for 5- to 11-year-olds and 437 for 12- to 15-year-olds, the COVID Data Tracker shows. Those aged 0-4 make up 6% of the total U.S. population, compared with 8.7% and 5.1%, respectively, for the older children.
Most younger children still not vaccinated
Although it may not qualify as a big push to vaccinate children before the start of the new school year, first-time vaccinations did rise somewhat in late July and August for children aged 5-17 years. Among children younger than 5 years, though, initial doses of the vaccine fell during the second full week of August, especially in 2- to 4-year-olds, based on the CDC data.
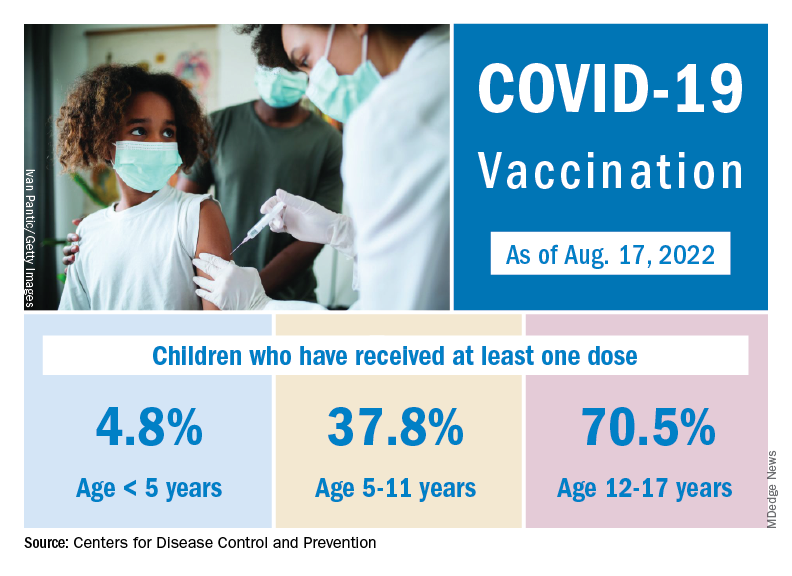
Through almost 2 months of vaccine eligibility, 4.8% of children under age 5 have received at least one dose and 0.9% are fully vaccinated as of Aug. 17. The current rates are 37.8% (one dose) and 30.4% (completed) for those aged 5-11 and 70.5% and 60.3% for 12- to 17-year-olds.
How does not getting enough sleep affect the developing brain?
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
Children who do not get enough sleep for one night can be cranky, groggy, or meltdown prone the next day.
Over time, though, insufficient sleep may impair neurodevelopment in ways that can be measured on brain scans and tests long term, a new study shows.
Research published in The Lancet Child & Adolescent Health found that 9- and 10-year-olds who do not get at least 9 hours of sleep most nights tend to have less gray matter and smaller areas of the brain responsible for attention, memory, and inhibition control, relative to children who do get enough sleep.
The researchers also found a relationship between insufficient sleep and disrupted connections between the basal ganglia and cortical regions of the brain. These disruptions appeared to be linked to depression, thought problems, and impairments in crystallized intelligence, a type of intelligence that depends on memory.
The overall patterns persisted 2 years later, even as those who got enough sleep at baseline gradually slept less over time, while those who were not getting enough sleep to begin with continued to sleep about the same amount, the researchers reported.
The results bolster the case for delaying school start times, as California recently did, according one researcher who was not involved in the study.
The ABCD Study
To examine how insufficient sleep affects children’s mental health, cognition, brain function, and brain structure over 2 years, Ze Wang, PhD, professor of diagnostic radiology and nuclear medicine at the University of Maryland, Baltimore, and colleagues analyzed data from the ongoing Adolescent Brain Cognitive Development (ABCD) Study. The ABCD Study is tracking the biologic and behavioral development of more than 11,000 children in the United States who were recruited for the study when they were 9 or 10 years old.
For their new analysis, Dr. Wang’s group focused on 6,042 participants: 3,021 children with insufficient sleep who were matched with an equal number of participants who were similar in many respects, including sex, socioeconomic status, and puberty status, except they got at least 9 hours of sleep. They also looked at outcomes 2 years later from 749 of the matched pairs who had results available.
The investigators determined sleep duration based on how parents answered the question: “How many hours of sleep does your child get on most nights in the past 6 months?” Possible answers included at least 9 hours, 8-9 hours, 7-8 hours, 5-7 hours, or less than 5 hours. They also looked at functional and structural MRI scans, test results, and responses to questionnaires.
Negative effects of inadequate sleep were spread over “several different domains including brain structure, function, cognition, behavior, and mental health,” Dr. Wang said.
The strength of the relationship between sleep duration and the various outcomes was “modest” and based on group averages, he said. So, a given child who does not sleep for 9 hours most nights won’t necessarily perform worse than a child who gets enough sleep.
Still, modest effects may accumulate and have lasting consequences, Dr. Wang said.
Crystallized intelligence
The researchers looked at 42 behavioral outcomes, 32 of which were significantly different between the groups. Four outcomes in particular – depression, thought problems, performance on a picture-vocabulary test, and crystallized intelligence – were areas where insufficient sleep seemed to have a larger negative effect.
Sleep duration’s relationship with crystallized intelligence was twice that for fluid intelligence, which does not depend on memory.
“Sleep affects memory,” Dr. Wang said. “Crystallized intelligence depends on learned skills and knowledge, which are memory. In this sense, sleep is related to crystallized intelligence.”
One limitation of the study is that some parents may not accurately report how much sleep their child gets, Dr. Wang acknowledged. Children may be awake when parents think they are asleep, for example.
And although the results show getting 9 hours of sleep may help neurocognitive development, it’s also possible that excessive amounts of sleep could be problematic, the study authors wrote.
Further experiments are needed to prove that insufficient sleep – and not some other, unaccounted for factor – causes the observed impairments in neurodevelopment.
To promote healthy sleep, parents should keep a strict routine for their children, such as a regular bedtime and no electronic devices in the bedroom, Dr. Wang suggested. More physical activity during the day also should help.
If children have high levels of stress and depression, “finding the source is critical,” he said. Likewise, clinicians should consider how mental health can affect their patients’ sleep.
More to healthy sleep than duration
“This study both aligns with and advances existing research on the importance of sufficient sleep for child well-being,” said Ariel A. Williamson, PhD, DBSM, a psychologist and pediatric sleep expert in the department of child and adolescent psychiatry and behavioral sciences at Children’s Hospital of Philadelphia and assistant professor of psychiatry and pediatrics at University of Pennsylvania, also in Philadelphia.
The researchers used rigorous propensity score matching, longitudinal data, and brain imaging, which are “innovative methods that provide more evidence on potential mechanisms linking insufficient sleep and child outcomes,” said Dr. Williamson, who was not involved in the study.
While the investigators focused on sleep duration, child sleep health is multidimensional and includes other elements like timing and perception of sleep quality, Dr. Williamson noted. “For example, some research shows that having a sleep schedule that varies night to night is linked to poor child outcomes.”
Dr. Williamson tells families and clinicians that “sleep is a pillar of health,” equal to diet and exercise. That said, sleep recommendations need to fit within a family’s life – taking into account after school activities and late-night homework sessions. But extending sleep by just “20-30 minutes can make a meaningful difference for daytime functioning,” Dr. Williamson said.
Start school later?
Researchers have only relatively recently begun to understand how insufficient sleep affects adolescent neurocognitive development long term, and this study provides “crucial evidence” about the consequences, Lydia Gabriela Speyer, PhD, said in an editorial published with the study. Dr. Speyer is affiliated with the department of psychology at the University of Cambridge (England).
“Given the novel finding that insufficient sleep is associated with changes in brain structure and connectivity that are long-lasting, early intervention is crucial because such neural changes are probably not reversible and might consequently affect adolescents’ development into adulthood,” Dr. Speyer wrote.
Delaying school start times could be one way to help kids get more sleep. The American Academy of Pediatrics and the American Academy of Sleep Medicine recommend that middle schools and high schools start no earlier than 8:30 a.m. to better align with students’ circadian rhythm, Dr. Speyer noted.
As it is in the United States, most schools start closer to 8 a.m. In California, though, a law that went into effect on July 1 prohibits high schools from starting before 8:30 a.m. Other states are weighing similar legislation.
The research was supported by the National Institutes of Health. Dr. Wang and his coauthors and Dr. Speyer had no conflict of interest disclosures. Dr. Williamson is a sleep expert for the Pediatric Sleep Council (www.babysleep.com), which provides free information about early childhood sleep, but she does not receive compensation for this role.
FROM THE LANCET CHILD & ADOLESCENT HEALTH
Regular physical activity may fight infection, illness from COVID: Study
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research suggests that regular physical activity can help lower the risk of COVID-19 infection and its severity, with a weekly tally of 150 minutes of moderate, or 75 minutes of vigorous, physical activity affording the best protection.
“, with potential benefits to reduce the risk of severe COVID-19,” say Antonio García-Hermoso, PhD, Public University of Navarra, Pamplona, Spain, and colleagues.
“Regular physical activity seemed to be related to a lower risk of COVID-19 infection, Dr. García-Hermoso said in an interview. “There is evidence that regular physical activity might contribute to a more effective immune response, providing enhanced protective immunity to infections, which could explain the relationship between exercise consistency with COVID-19 infection.”
Regular exercise may also help to boost the body’s anti-inflammatory responses, as well as cardiorespiratory and muscular fitness, all of which may explain its beneficial effects on COVID-19 severity, the researchers say.
The study was published online in the British Journal of Sports Medicine.
Strong protection from COVID?
A growing body of evidence suggests that increased physical activity may modulate the course of COVID-19 infection and reduce the risk of poor outcomes. The new analysis is the first to systematically evaluate and pool data on the effect of regular physical activity on COVID-19 outcomes.
The findings are based on data from 16 studies with over 1.8 million adults (53% women, mean age 53 years).
Individuals who included regular physical activity in their weekly routine had an 11% lower risk for infection with SARS-CoV-2 (hazard ratio, 0.89; 95% confidence interval, 0.84-0.95), compared with inactive peers.
The physically active adults also had a 36% (HR, 0.64; 95% CI, 0.54-0.76) lower risk of being hospitalized, a 44% (HR, 0.66; 95% CI, 0.58-0.77) lower risk for severe COVID-19 illness, and a 43% (HR, 0.57; 95% CI, 0.46-0.71) lower risk of dying from COVID-19 than their inactive peers.
The greatest protective effect occurs with achieving at least 500 metabolic equivalent of task (MET) minutes per week of physical activity – equivalent to 150 minutes of moderate-intensity or 75 min of vigorous-intensity physical activity per week – with no added benefit beyond this level.
The researchers caution that the analysis included observational studies, differing study designs, subjective assessments of physical activity levels, and concerned only the Beta and Delta variants of SARS-CoV-2, not Omicron.
Despite these limitations, the researchers say their findings “may help guide physicians and health care policymakers in making recommendations and developing guidelines with respect to the degree of physical activity that can help reduce the risk of infectivity, hospitalization, severity, and mortality of COVID-19 at both the individual and the population level, especially in high-risk patients.”
Helpful, but not a panacea
Reached for comment, Sean Heffron, MD, a preventive cardiologist and assistant professor of medicine at NYU Langone Health, New York, said the study “supports the well-established nonlinear association of increasing physical activity with adverse outcomes from a diverse array of diseases, including infectious diseases, such as COVID-19.”
The observation is not particularly surprising, he said.
“It is as I would suspect. They compiled data from a large number of studies published over the past several years that all had consistent findings,” Dr. Heffron said.
“The take-away from a public health standpoint is that being physically active improves health in myriad ways. That being said, it is not a panacea, so additional measures (masking, vaccinations, etc.) are important for everyone,” he said.
Also weighing in, Joseph Herrera, DO, chair of the department of rehabilitation for Mount Sinai Health System, New York, said, “If you are physically fit, your body is more resilient and better prepared to handle the stressors of COVID or any other disease process.”
For now, however, the question of whether physical fitness is actually protective against COVID remains unclear. “I’m just not sure right now,” Dr. Herrera said in an interview.
He said he has treated athletes in professional sports – including the National Football League and Major League Baseball – and some of them have had long COVID and have not returned to play. “These are athletes at the peak of fitness and their career.”
Nonetheless, Dr. Herrera said a good public health message in general is to stay fit or get fit.
“That’s something I preach all the time,” he told this news organization.
Dr. García-Hermoso agreed. “In contrast to the vast majority of drugs, exercise is free of adverse effects. It’s time to consider exercise as medicine. It’s never too late to start being physically active.”
The study had no specific funding. Dr. García-Hermoso, Dr. Heffron, and Dr. Herrera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BRITISH JOURNAL OF SPORTS MEDICINE
Screen COPD patients for peripheral neuropathy
Polyneuropathy (PNP) remains a common comorbidity among patients with chronic obstructive pulmonary disease (COPD), and better screening strategies are needed to identify the condition and improve patients’ quality of life, according to authors of a recent review.
of stroke, dementia, depression, and other neurological and psychiatric conditions, even after controlling for the main confounding risk factors, such as age and smoking,” write Irina Odajiu, MD, of Colentina Clinical Hospital, Bucharest, Romania, and colleagues. However, data on the relationship between COPD and peripheral nervous system pathology are limited.
PNP is distinct from peripheral neuropathy and neuropathy, the researchers emphasize.
“Polyneuropathy implies a homogeneous process affecting peripheral nerves, specifically distal nerves, more severely than proximal ones,” while peripheral neuropathy refers to any disorder of the peripheral nervous system, they explain.
In an article published in Respiratory Medicine, the authors summarize the latest data on the association between COPD and polyneuropathy. They reviewed data from 21 studies published between 1981 and 2021. All studies included adults with COPD. The mean age of the patients was 55-65 years.
Peripheral neuropathy represents a significant comorbidity among patients with COPD. The percentage of cases of peripheral neuropathy among patients in the study populations ranged from 15% to 93.8%. Of these cases, the majority were of axonal sensory polyneuropathy. In most of the studies, the neuropathy affected the lower limbs more than the upper limbs.
“Additionally, in most presented studies, peripheral neuropathy correlated with disease duration and hypoxemia severity; the longer the duration and the more severe hypoxia, the more severe peripheral neuropathy was,” the researchers note.
Overall, potential predisposing factors for PNP among patients with COPD (in addition to chronic hypoxemia) included older age, poor nutrition, systemic inflammation, COPD medications, smoking, and increased partial pressure of carbon dioxide (hypercapnia).
Several strategies for managing peripheral neuropathy for patients with COPD were described. Prophylaxis options include neuroprotection with hormones such as progesterone, neuronal growth factors, and corticosteroids, although none have shown high levels of effectiveness, the researchers write. Topical treatment with muscarinic antagonists has shown some potential and may be a practical therapeutic choice, they say. Oxygen support, including hyperbaric oxygen therapy, has demonstrated healing of diabetic leg ulcers associated with PNP and has led to improvements in pain-related symptoms and quality-of-life scores, they add.
Although PNP is often present in patients with COPD, no association between COPD severity and PNP has been determined, the researchers write in their discussion section.
“Moreover, the current data do not indicate a relationship between COPD stages, GOLD classification, or degree of obstruction and PNP,” they say.
The data support screening of all COPD patients for PNP, both clinically and with electrodiagnostic studies, despite the absence of current specific COPD-related PNP screening tools, they write.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Polyneuropathy (PNP) remains a common comorbidity among patients with chronic obstructive pulmonary disease (COPD), and better screening strategies are needed to identify the condition and improve patients’ quality of life, according to authors of a recent review.
of stroke, dementia, depression, and other neurological and psychiatric conditions, even after controlling for the main confounding risk factors, such as age and smoking,” write Irina Odajiu, MD, of Colentina Clinical Hospital, Bucharest, Romania, and colleagues. However, data on the relationship between COPD and peripheral nervous system pathology are limited.
PNP is distinct from peripheral neuropathy and neuropathy, the researchers emphasize.
“Polyneuropathy implies a homogeneous process affecting peripheral nerves, specifically distal nerves, more severely than proximal ones,” while peripheral neuropathy refers to any disorder of the peripheral nervous system, they explain.
In an article published in Respiratory Medicine, the authors summarize the latest data on the association between COPD and polyneuropathy. They reviewed data from 21 studies published between 1981 and 2021. All studies included adults with COPD. The mean age of the patients was 55-65 years.
Peripheral neuropathy represents a significant comorbidity among patients with COPD. The percentage of cases of peripheral neuropathy among patients in the study populations ranged from 15% to 93.8%. Of these cases, the majority were of axonal sensory polyneuropathy. In most of the studies, the neuropathy affected the lower limbs more than the upper limbs.
“Additionally, in most presented studies, peripheral neuropathy correlated with disease duration and hypoxemia severity; the longer the duration and the more severe hypoxia, the more severe peripheral neuropathy was,” the researchers note.
Overall, potential predisposing factors for PNP among patients with COPD (in addition to chronic hypoxemia) included older age, poor nutrition, systemic inflammation, COPD medications, smoking, and increased partial pressure of carbon dioxide (hypercapnia).
Several strategies for managing peripheral neuropathy for patients with COPD were described. Prophylaxis options include neuroprotection with hormones such as progesterone, neuronal growth factors, and corticosteroids, although none have shown high levels of effectiveness, the researchers write. Topical treatment with muscarinic antagonists has shown some potential and may be a practical therapeutic choice, they say. Oxygen support, including hyperbaric oxygen therapy, has demonstrated healing of diabetic leg ulcers associated with PNP and has led to improvements in pain-related symptoms and quality-of-life scores, they add.
Although PNP is often present in patients with COPD, no association between COPD severity and PNP has been determined, the researchers write in their discussion section.
“Moreover, the current data do not indicate a relationship between COPD stages, GOLD classification, or degree of obstruction and PNP,” they say.
The data support screening of all COPD patients for PNP, both clinically and with electrodiagnostic studies, despite the absence of current specific COPD-related PNP screening tools, they write.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Polyneuropathy (PNP) remains a common comorbidity among patients with chronic obstructive pulmonary disease (COPD), and better screening strategies are needed to identify the condition and improve patients’ quality of life, according to authors of a recent review.
of stroke, dementia, depression, and other neurological and psychiatric conditions, even after controlling for the main confounding risk factors, such as age and smoking,” write Irina Odajiu, MD, of Colentina Clinical Hospital, Bucharest, Romania, and colleagues. However, data on the relationship between COPD and peripheral nervous system pathology are limited.
PNP is distinct from peripheral neuropathy and neuropathy, the researchers emphasize.
“Polyneuropathy implies a homogeneous process affecting peripheral nerves, specifically distal nerves, more severely than proximal ones,” while peripheral neuropathy refers to any disorder of the peripheral nervous system, they explain.
In an article published in Respiratory Medicine, the authors summarize the latest data on the association between COPD and polyneuropathy. They reviewed data from 21 studies published between 1981 and 2021. All studies included adults with COPD. The mean age of the patients was 55-65 years.
Peripheral neuropathy represents a significant comorbidity among patients with COPD. The percentage of cases of peripheral neuropathy among patients in the study populations ranged from 15% to 93.8%. Of these cases, the majority were of axonal sensory polyneuropathy. In most of the studies, the neuropathy affected the lower limbs more than the upper limbs.
“Additionally, in most presented studies, peripheral neuropathy correlated with disease duration and hypoxemia severity; the longer the duration and the more severe hypoxia, the more severe peripheral neuropathy was,” the researchers note.
Overall, potential predisposing factors for PNP among patients with COPD (in addition to chronic hypoxemia) included older age, poor nutrition, systemic inflammation, COPD medications, smoking, and increased partial pressure of carbon dioxide (hypercapnia).
Several strategies for managing peripheral neuropathy for patients with COPD were described. Prophylaxis options include neuroprotection with hormones such as progesterone, neuronal growth factors, and corticosteroids, although none have shown high levels of effectiveness, the researchers write. Topical treatment with muscarinic antagonists has shown some potential and may be a practical therapeutic choice, they say. Oxygen support, including hyperbaric oxygen therapy, has demonstrated healing of diabetic leg ulcers associated with PNP and has led to improvements in pain-related symptoms and quality-of-life scores, they add.
Although PNP is often present in patients with COPD, no association between COPD severity and PNP has been determined, the researchers write in their discussion section.
“Moreover, the current data do not indicate a relationship between COPD stages, GOLD classification, or degree of obstruction and PNP,” they say.
The data support screening of all COPD patients for PNP, both clinically and with electrodiagnostic studies, despite the absence of current specific COPD-related PNP screening tools, they write.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Is it COVID or long COVID? Your organs may know
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
There’s little doubt long COVID is real. The federal government recognizes long COVID as a condition and said in two reports issued in August that one in five adult COVID-19 survivors have a health condition related to their illness.
COVID-19 can damage multiple organs in the body. Sometimes this damage leads to long COVID; sometimes other reasons are at play. Doctors are beginning to sort it out.
“COVID itself can actually cause prolonged illness, and we don’t really call that long COVID,” said Nisha Viswanathan, MD, a doctor at UCLA Health in Los Angeles. But if symptoms extend beyond 12 weeks, that puts patients in the realm of long COVID.
Symptoms can range from mild to severe and can keep people from resuming their normal lives and jobs. Sometimes they last for months, according to the U.S. Department of Health & Human Services.
Multiorgan damage
Lung scarring and other lung problems are common after COVID, said Leora Horwitz, MD, an internal medicine specialist at New York University. Even after a mild case, people can have breathing issues for months, a team at Johns Hopkins Medicine, Baltimore, said in an online briefing. One study published in the journal Radiology found damage in people a full year after a COVID-19 diagnosis.
Some people have persistent heart, kidney, liver, and nervous system problems after COVID-19. A study published in 2020 in JAMA Cardiology found 60% of people who had COVID-19 had ongoing signs of heart inflammation. Nearly a third of people hospitalized for COVID-19 get kidney damage that can become chronic, and some end up needing dialysis or a transplant, said C. John Sperati, MD, a kidney specialist at Johns Hopkins Medicine.
This might be, in part, because SARS-CoV-2, the virus that causes COVID-19, directly infects the cells in many organs.
Nicole Bhave, MD, a cardiologist at University of Michigan Health, Ann Arbor is concerned that COVID-19 appears to increase the risk of heart problems in some people.
“Some of the uptick may just be recognition bias, in that people with symptoms are seeking care,” she said. “But there’s definitely a biological basis by which COVID could tip people over into a new diagnosis of heart failure.”
Inflammation
Inflammation is probably a key part of the long-term effects of COVID-19.
Some people have a serious immune reaction to COVID-19 called a cytokine storm, said Nitra Aggarwal Gilotra, MD, a cardiologist at Johns Hopkins Medicine. This release of inflammation-causing molecules called cytokines is meant to attack the invading virus. But it can be so severe that it wreaks havoc on healthy tissues and organs and causes lasting damage – if patients even survive it.
In some people, inflammation can affect the heart, causing myocarditis. Myocarditis symptoms include chest pain, breathlessness, and heart palpitations. Though rare, it can be serious and can raise the risk of other heart problems, including heart failure, down the line.
Long COVID may also trigger an autoimmune condition, said Eline Luning Prak, MD, PhD, a pathologist at the Hospital of the University of Pennsylvania, Philadelphia. Long COVID can share many hallmark symptoms with autoimmune diseases, including fatigue, widespread pain, memory problems, and mood disorders.
Blood clots
Studies have shown the overcharged inflammatory response to COVID-19 can cause blood clots. This sometimes overwhelming clotting was an early hallmark of COVID-19 infection, and when clots restrict blood flow in the brain, lungs, kidneys, or limbs, they can cause long-term damage. Some can be deadly. Researchers in Sweden found patients were at risk of deep vein thrombosis – a blood clot usually in the leg – up to 3 months after infection and at higher risk of a blood clot in the lung, called pulmonary embolism, for as long as 3 months.
Viral reservoirs
The virus itself may also linger in a patient’s body, causing continued symptoms and, potentially, new flare-ups. Zoe Swank, PhD, of Harvard Medical School, Boston, and colleagues reported in a preprint study that they found pieces of the SARS-CoV-2 virus in the blood of most patients with long COVID symptoms they tested – some as long as a year after infection. The study has not yet been peer reviewed.
Another team found evidence of the virus in stool up to 7 months later, which suggests the virus hides out in the gut. Other early studies have found bits of viral RNA in the appendix, breast tissue, heart, eyes, and brain.
Diabetes
Diabetes is a risk factor for getting severe COVID-19, and multiple studies have shown people can get diabetes both while battling infection and afterward. One study of veterans, published in The Lancet Diabetes and Endocrinology, found COVID-19 survivors were about 40% more likely to get diabetes over the next year.
There are a few ways this might happen. Insulin-producing cells in the pancreas have SARS-CoV-2 receptors – a type of molecular doorway the coronavirus can attach to. Damage to these cells could make the body less able to produce insulin, which in turn can lead to diabetes. The virus could also disrupt the balance in the body or cause inflammation that leads to insulin resistance, which can develop into diabetes, Ziad Al-Aly, MD, of the Veterans Affairs St. Louis Health Care System, and colleagues wrote.
Nervous system issues
People who get COVID-19 are also more vulnerable to postural orthostatic tachycardia syndrome (POTS). This affects what’s known as the autonomic nervous system, which regulates blood circulation, and includes those things that happen in your body without your having to think about them, like breathing, heartbeat, and digestion. POTS can cause common long COVID neurologic symptoms, including headaches, fatigue, brain fog, insomnia, and problems thinking and concentrating. “This was a known condition prior to COVID, but it was incredibly rare,” said Dr. Viswanathan. “After COVID, I’ve seen it with increasing frequency.”
Long-term outlook
Lasting issues after COVID-19 are much more likely after a moderate or severe infection. Still, plenty of people are battling them even after a mild illness. “As for why, that’s the billion-dollar question,” said Dr. Horwitz. “It’s well known that viral infections can cause long-term dysregulation. Why that is, we really just don’t know.”
Whether it’s virus hiding out in the body, long-term organ damage, or an autoimmune reaction likely differs from person to person. “I’m believing, increasingly, that it’s a combination of all of these, just based on how different patients are responding to different medications,” said Dr. Viswanathan. “One patient will respond to something beautifully, and another patient won’t at all.”
But it’s clear a significant number of people are facing long-term health struggles because of COVID-19, which has infected at least 580 million people globally and 92 million – likely many more – in the United States, according to Johns Hopkins University.
Even a small increased risk of conditions like heart disease or diabetes translates to a huge number of people, Dr. Horwitz said. “If even 1% of people getting COVID have long-term symptoms, that’s a major public health crisis, because that’s 1% of pretty much everybody in the country.”
A version of this article first appeared on WebMD.com.
Most people with Omicron don’t know they’re infected
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
Most people with Omicron likely don’t know it.
That’s according to a study in JAMA Network Open, which says 56% of people who have the Omicron variant of the coronavirus are unaware of their infection.
And it has an upside and a downside, depending on how you look at it, according to Time magazine.
“It’s good news, in some ways, since ) in vaccinated people,” Time says. “The downside is that many people are likely spreading the virus unintentionally.”
The study looked at 210 hospital patients and employees in the Los Angeles area. More than half who tested positive didn’t know it – because they had no symptoms, or they assumed they merely had a cold or allergies.
“The findings support early data from around the world suggesting that throughout the pandemic, anywhere from 25% to 40% of SARS-CoV-2 infections have been asymptomatic, which presents challenges for public health officials trying to control the spread of the virus,” Time reports.
The study found that awareness of infection rose after at-home tests became available this year. About three-quarters of people in January and February didn’t know their status, for example.
“Findings of this study suggest that low rates of Omicron variant infection awareness may be a key contributor to rapid transmission of the virus within communities,” the authors wrote. “Given that unawareness of active infection precludes self-initiated interventions, such as testing and self-isolation, even modest levels of undiagnosed infection can contribute to substantial population-level transmission.”
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN
Airway structure in women leads to worse COPD outcomes
A study aimed at determining whether behind some of the sex differences in chronic obstructive airway disease (COPD) prevalence and clinical outcomes lie structural differences in airways found that airway lumen sizes quantified through chest CT were smaller in women than in men.
The findings, published in Radiology, took into account height and lung size. for equivalent changes, compared with men.
Among key findings in a secondary analysis of consecutive participants (9,363 ever-smokers and 420 never-smokers) enrolled in the Genetic Epidemiology of COPD (COPDGene) study, airway lumen dimensions were lower in never-smoker women than in men (segmental lumen diameter, 8.1 mm vs. 9.1 mm; P < .001). Also, ever-smoker women had narrower segmental lumen diameter (7.8 mm ± 0.05 vs. 8.7 mm ± 0.04; P < .001). The investigators found also that a unit change in wall thickness or lumen area resulted in more severe airflow obstruction, more dyspnea, worse respiratory quality of life, lower 6-minute walk distance, and worse survival in women, compared with men.
While COPD is diagnosed more often in men than women, changes in smoking behavior and increasing urbanization have led to COPD prevalence in women fast approaching the rate in men. Although age-adjusted rates for COPD-related deaths have continued to decline in men, in women they have not. Indeed, never-smoking women accounted for two-thirds of COPD in a population-based study.
COPDGene, a prospective, multicenter, observational cohort study, enrolled current and former smokers, as well as never-smokers, aged 45-80 years at 21 clinical centers across the United States from January 2008 to June 2011 with longitudinal follow-up until November 2020. The investigators quantified airway disease through CT imaging using the following metrics: airway wall thickness of segmental airways, wall area percent of segmental airways, the square root of the wall area of a hypothetical airway with 10-mm internal perimeter, total airway count, lumen diameter of segmental airways, airway volume, and airway fractal dimension.
“Not all sex differences in prevalence of COPD have been explained, and structural differences may explain some of these differences. Our findings may have implications for patient selection for clinical trials,” corresponding author Surya P. Bhatt, MD, associate professor of medicine and director of the University of Alabama Imaging Core at Birmingham, said in an interview.
The investigators wrote: “Our findings have implications for airflow limitation and the consequent clinical outcomes. ... We confirmed that men have more emphysema than women with equivalent smoking burden, and our results suggest that the lower reserve conferred by smaller airways predisposes women to develop airflow limitation predominantly through the airway phenotype. All airway remodeling changes were associated with more dyspnea, worse respiratory quality of life, and lower functional capacity in women than in men. The smaller airways in women can result in higher airway resistance and more turbulent airflow, and thus place a higher ventilatory constraint during exertion. Alteration in each airway measure was also associated with worse survival in women than in men, partially explaining the comparable mortality between the sexes for COPD despite the differing degrees of emphysema.”
“I think these findings highlight underappreciated sex differences in the natural history of COPD,” Mohsen Sadatsafavi, MD, PhD, associate professor, faculty of pharmaceutical sciences, at the University of British Columbia, Vancouver, said in an interview. “To me, first and foremost, the Bhatt et al. findings highlight how the ‘one size fits all’ approach to COPD management of using exacerbation history alone to guide preventive therapies is incorrect. These findings have the potential to change the management paradigm of COPD in the long term, but before getting there, I think we need to relate these findings to clinically relevant and patient-reported outcomes.”
Noting study limitations, the authors stated that a higher proportion of men were active smokers, compared with women, and despite adjustments for smoking status, some of the airway wall differences may be from the impact of active cigarette smoking on airway wall thickness.
Five study authors reported receiving support from various government and industry sources and disclosed conflicts of interest based on relationships with industry. The rest reported no conflicts of interest.
A study aimed at determining whether behind some of the sex differences in chronic obstructive airway disease (COPD) prevalence and clinical outcomes lie structural differences in airways found that airway lumen sizes quantified through chest CT were smaller in women than in men.
The findings, published in Radiology, took into account height and lung size. for equivalent changes, compared with men.
Among key findings in a secondary analysis of consecutive participants (9,363 ever-smokers and 420 never-smokers) enrolled in the Genetic Epidemiology of COPD (COPDGene) study, airway lumen dimensions were lower in never-smoker women than in men (segmental lumen diameter, 8.1 mm vs. 9.1 mm; P < .001). Also, ever-smoker women had narrower segmental lumen diameter (7.8 mm ± 0.05 vs. 8.7 mm ± 0.04; P < .001). The investigators found also that a unit change in wall thickness or lumen area resulted in more severe airflow obstruction, more dyspnea, worse respiratory quality of life, lower 6-minute walk distance, and worse survival in women, compared with men.
While COPD is diagnosed more often in men than women, changes in smoking behavior and increasing urbanization have led to COPD prevalence in women fast approaching the rate in men. Although age-adjusted rates for COPD-related deaths have continued to decline in men, in women they have not. Indeed, never-smoking women accounted for two-thirds of COPD in a population-based study.
COPDGene, a prospective, multicenter, observational cohort study, enrolled current and former smokers, as well as never-smokers, aged 45-80 years at 21 clinical centers across the United States from January 2008 to June 2011 with longitudinal follow-up until November 2020. The investigators quantified airway disease through CT imaging using the following metrics: airway wall thickness of segmental airways, wall area percent of segmental airways, the square root of the wall area of a hypothetical airway with 10-mm internal perimeter, total airway count, lumen diameter of segmental airways, airway volume, and airway fractal dimension.
“Not all sex differences in prevalence of COPD have been explained, and structural differences may explain some of these differences. Our findings may have implications for patient selection for clinical trials,” corresponding author Surya P. Bhatt, MD, associate professor of medicine and director of the University of Alabama Imaging Core at Birmingham, said in an interview.
The investigators wrote: “Our findings have implications for airflow limitation and the consequent clinical outcomes. ... We confirmed that men have more emphysema than women with equivalent smoking burden, and our results suggest that the lower reserve conferred by smaller airways predisposes women to develop airflow limitation predominantly through the airway phenotype. All airway remodeling changes were associated with more dyspnea, worse respiratory quality of life, and lower functional capacity in women than in men. The smaller airways in women can result in higher airway resistance and more turbulent airflow, and thus place a higher ventilatory constraint during exertion. Alteration in each airway measure was also associated with worse survival in women than in men, partially explaining the comparable mortality between the sexes for COPD despite the differing degrees of emphysema.”
“I think these findings highlight underappreciated sex differences in the natural history of COPD,” Mohsen Sadatsafavi, MD, PhD, associate professor, faculty of pharmaceutical sciences, at the University of British Columbia, Vancouver, said in an interview. “To me, first and foremost, the Bhatt et al. findings highlight how the ‘one size fits all’ approach to COPD management of using exacerbation history alone to guide preventive therapies is incorrect. These findings have the potential to change the management paradigm of COPD in the long term, but before getting there, I think we need to relate these findings to clinically relevant and patient-reported outcomes.”
Noting study limitations, the authors stated that a higher proportion of men were active smokers, compared with women, and despite adjustments for smoking status, some of the airway wall differences may be from the impact of active cigarette smoking on airway wall thickness.
Five study authors reported receiving support from various government and industry sources and disclosed conflicts of interest based on relationships with industry. The rest reported no conflicts of interest.
A study aimed at determining whether behind some of the sex differences in chronic obstructive airway disease (COPD) prevalence and clinical outcomes lie structural differences in airways found that airway lumen sizes quantified through chest CT were smaller in women than in men.
The findings, published in Radiology, took into account height and lung size. for equivalent changes, compared with men.
Among key findings in a secondary analysis of consecutive participants (9,363 ever-smokers and 420 never-smokers) enrolled in the Genetic Epidemiology of COPD (COPDGene) study, airway lumen dimensions were lower in never-smoker women than in men (segmental lumen diameter, 8.1 mm vs. 9.1 mm; P < .001). Also, ever-smoker women had narrower segmental lumen diameter (7.8 mm ± 0.05 vs. 8.7 mm ± 0.04; P < .001). The investigators found also that a unit change in wall thickness or lumen area resulted in more severe airflow obstruction, more dyspnea, worse respiratory quality of life, lower 6-minute walk distance, and worse survival in women, compared with men.
While COPD is diagnosed more often in men than women, changes in smoking behavior and increasing urbanization have led to COPD prevalence in women fast approaching the rate in men. Although age-adjusted rates for COPD-related deaths have continued to decline in men, in women they have not. Indeed, never-smoking women accounted for two-thirds of COPD in a population-based study.
COPDGene, a prospective, multicenter, observational cohort study, enrolled current and former smokers, as well as never-smokers, aged 45-80 years at 21 clinical centers across the United States from January 2008 to June 2011 with longitudinal follow-up until November 2020. The investigators quantified airway disease through CT imaging using the following metrics: airway wall thickness of segmental airways, wall area percent of segmental airways, the square root of the wall area of a hypothetical airway with 10-mm internal perimeter, total airway count, lumen diameter of segmental airways, airway volume, and airway fractal dimension.
“Not all sex differences in prevalence of COPD have been explained, and structural differences may explain some of these differences. Our findings may have implications for patient selection for clinical trials,” corresponding author Surya P. Bhatt, MD, associate professor of medicine and director of the University of Alabama Imaging Core at Birmingham, said in an interview.
The investigators wrote: “Our findings have implications for airflow limitation and the consequent clinical outcomes. ... We confirmed that men have more emphysema than women with equivalent smoking burden, and our results suggest that the lower reserve conferred by smaller airways predisposes women to develop airflow limitation predominantly through the airway phenotype. All airway remodeling changes were associated with more dyspnea, worse respiratory quality of life, and lower functional capacity in women than in men. The smaller airways in women can result in higher airway resistance and more turbulent airflow, and thus place a higher ventilatory constraint during exertion. Alteration in each airway measure was also associated with worse survival in women than in men, partially explaining the comparable mortality between the sexes for COPD despite the differing degrees of emphysema.”
“I think these findings highlight underappreciated sex differences in the natural history of COPD,” Mohsen Sadatsafavi, MD, PhD, associate professor, faculty of pharmaceutical sciences, at the University of British Columbia, Vancouver, said in an interview. “To me, first and foremost, the Bhatt et al. findings highlight how the ‘one size fits all’ approach to COPD management of using exacerbation history alone to guide preventive therapies is incorrect. These findings have the potential to change the management paradigm of COPD in the long term, but before getting there, I think we need to relate these findings to clinically relevant and patient-reported outcomes.”
Noting study limitations, the authors stated that a higher proportion of men were active smokers, compared with women, and despite adjustments for smoking status, some of the airway wall differences may be from the impact of active cigarette smoking on airway wall thickness.
Five study authors reported receiving support from various government and industry sources and disclosed conflicts of interest based on relationships with industry. The rest reported no conflicts of interest.
FROM RADIOLOGY