User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


CBSM phone app eases anxiety, depression in cancer patients
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
AT ASCO 2023
T-DXd active in many solid tumors; ‘shift in thinking’
CHICAGO – Trastuzumab deruxtecan (T-DXd) (Enhertu) already has proven efficacy against HER2-expressing metastatic breast, gastroesophageal, and lung cancers.
including malignancies of the cervix, endometrium, ovaries, bladder, and other sites.
The findings come from the ongoing DESTINY-PanTumor02 trial. Among 267 patients with solid tumors at various organ sites, the investigator-assessed objective response rate among all patients was 37.1%, and ranged from as high as 57.5% for patients with endometrial cancers to as low as 4% for patients with pancreatic cancer, reported Funda Meric-Bernstam, MD, from the University of Texas MD Anderson Cancer Center, Houston.
For patients with tumors that had HER2 immunohistochemistry (IHC) scores of 3+, the highest level of HER2 expression, the overall response rate was 61.3%..
The responses were also durable, with a median duration of 11.8 months among all patients and 22.1 months among patients with IHC 3+ scores.
“Our data to date showed that T-DXd had clinically meaningful activity across a variety of tumor types,” she said in a briefing held prior to her presentation of the data at the annual meeting of the American Society of Clinical Oncology.
“HER2 expression has been around a long time. We think about this all the time in breast cancer and drugs are approved there, but HER2 is expressed in other tumors as well, and that really represents an unmet need, because we have limited options in this situation” commented ASCO expert Bradley Alexander McGregor, MD, from the Dana-Farber Cancer Institute, Boston, an invited discussant at the briefing.
“Aside from pancreatic cancer we saw really, really encouraging results with no new safety signals, so while early I think this really exciting and represents a shift in how we think about cancer care,” he added.
After the presentation, invited discussant Kohei Shitara, MD, of National Cancer Center Hospital East, Kashiwa, Japan, said that he agrees with authors that T-DXd is a potential new treatment option for patients with HER2-expressing solid tumors, and that the evidence suggests the potential for further tumor-agnostic development of the agent.
He cautioned, however, that there is a lack of concordance between local and central assessment of HER2 IHC, and that quality assurance will be required to ensure that the HER2 status of solid tumors is accurately characterized.
At a press briefing, Dr. Meric-Bernstam was asked how she envisioned using T-DXd in therapy for various HER2-expressing tumors.
“I think the activity we’ve seen is quite compelling, and one hopes that eventually this will be a drug that’s accessible for patients that are HER2-expressing across tumor types. Clearly, the activity is very compelling in some of the diseases to think about doing studies for earlier lines,” she said.
“The data indicate that there is tumor-agnostic activity across the board,” she said, but noted that tumors with epithelial components such as ovarian and breast cancers appear to have the highest responses to T-DXd therapy.
Briefing moderator Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, asked Dr. McGregor whether, in the light of this new data, oncologists should test more patients for HER2 expression.
“We have some cancers where we know HER2 expression is there. I think the good thing about HER2 testing is that it’s an IHC test, so this is something that can be easily done in local pathology [labs],” he said. As more evidence mounts of potential benefit of T-DXd in HER2 expressing tumors, clinicians will need to consider more routine HER2 testing.
A rendezvous with DESTINY
The DESTINY-PanTumor02 trial is a phase 2, open-label, multicenter study looking at T-DXd in patients with advanced solid tumors who are not eligible for therapy with curative intent.
All patients had disease progression after at least two prior lines of therapy, and had tumors with HER2 expression of IHC 3+ or 2+ either by local or central testing. Patients were allowed to have previously received HER2-targeting therapy. Patients also had to have good performance status (Eastern Cooperative Oncology Group/World Health Organization performance status 0 or 1).
The investigators planned to enroll 40 patients in each cohort, including patients with cervical, endometrial, ovarian, biliary tract, pancreatic, or bladder cancers, as well those with other tumors expressing HER2 who were not included in the other cohorts.
Under the protocol, cohorts in which none of the first 15 patients had objective responses would be closed, as happened with the pancreatic cancer cohort.
At a median follow-up of 9.7 months, an objective response was seen in 99 patients out of the 267 in the entire study population (ORR, 37.1%). This ORR consisted of 15 complete responses and 84 partial responses. An additional 123 patients had stable disease.
An analysis of ORR by HER2 expression showed that IHC 3+ expressing tumors had rates ranging from 84.6% in endometrial cancers, 75% in cervical cancer, 63.6% in ovarian cancers, and 56.3% in bladder cancers, down to zero in IHC 3+ expressing pancreatic cancer.
The T-DXd safety profile was consistent with that seen in other clinical trials, with most common adverse events being nausea, fatigue, neutropenia, anemia, diarrhea, and thrombocytopenia. There were 20 cases of interstitial lung disease, one of which was fatal.
The trial is ongoing, and investigators plan to report overall survival and progression-free survival results with additional follow-up.
DESTINY-PanTumor02 is funded by Daiichi Sankyo. Dr. Meric-Bernstam disclosed a consulting/advisory role with multiple pharmaceutical companies, research funding to her institution from Daiichi Sankyo and others, and travel expenses from ESMO and EORTC. Dr. McGregor disclosed a consulting/advisory role and institutional research funding with multiple companies, not including the study’s funder. Dr. Gralow disclosed a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
CHICAGO – Trastuzumab deruxtecan (T-DXd) (Enhertu) already has proven efficacy against HER2-expressing metastatic breast, gastroesophageal, and lung cancers.
including malignancies of the cervix, endometrium, ovaries, bladder, and other sites.
The findings come from the ongoing DESTINY-PanTumor02 trial. Among 267 patients with solid tumors at various organ sites, the investigator-assessed objective response rate among all patients was 37.1%, and ranged from as high as 57.5% for patients with endometrial cancers to as low as 4% for patients with pancreatic cancer, reported Funda Meric-Bernstam, MD, from the University of Texas MD Anderson Cancer Center, Houston.
For patients with tumors that had HER2 immunohistochemistry (IHC) scores of 3+, the highest level of HER2 expression, the overall response rate was 61.3%..
The responses were also durable, with a median duration of 11.8 months among all patients and 22.1 months among patients with IHC 3+ scores.
“Our data to date showed that T-DXd had clinically meaningful activity across a variety of tumor types,” she said in a briefing held prior to her presentation of the data at the annual meeting of the American Society of Clinical Oncology.
“HER2 expression has been around a long time. We think about this all the time in breast cancer and drugs are approved there, but HER2 is expressed in other tumors as well, and that really represents an unmet need, because we have limited options in this situation” commented ASCO expert Bradley Alexander McGregor, MD, from the Dana-Farber Cancer Institute, Boston, an invited discussant at the briefing.
“Aside from pancreatic cancer we saw really, really encouraging results with no new safety signals, so while early I think this really exciting and represents a shift in how we think about cancer care,” he added.
After the presentation, invited discussant Kohei Shitara, MD, of National Cancer Center Hospital East, Kashiwa, Japan, said that he agrees with authors that T-DXd is a potential new treatment option for patients with HER2-expressing solid tumors, and that the evidence suggests the potential for further tumor-agnostic development of the agent.
He cautioned, however, that there is a lack of concordance between local and central assessment of HER2 IHC, and that quality assurance will be required to ensure that the HER2 status of solid tumors is accurately characterized.
At a press briefing, Dr. Meric-Bernstam was asked how she envisioned using T-DXd in therapy for various HER2-expressing tumors.
“I think the activity we’ve seen is quite compelling, and one hopes that eventually this will be a drug that’s accessible for patients that are HER2-expressing across tumor types. Clearly, the activity is very compelling in some of the diseases to think about doing studies for earlier lines,” she said.
“The data indicate that there is tumor-agnostic activity across the board,” she said, but noted that tumors with epithelial components such as ovarian and breast cancers appear to have the highest responses to T-DXd therapy.
Briefing moderator Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, asked Dr. McGregor whether, in the light of this new data, oncologists should test more patients for HER2 expression.
“We have some cancers where we know HER2 expression is there. I think the good thing about HER2 testing is that it’s an IHC test, so this is something that can be easily done in local pathology [labs],” he said. As more evidence mounts of potential benefit of T-DXd in HER2 expressing tumors, clinicians will need to consider more routine HER2 testing.
A rendezvous with DESTINY
The DESTINY-PanTumor02 trial is a phase 2, open-label, multicenter study looking at T-DXd in patients with advanced solid tumors who are not eligible for therapy with curative intent.
All patients had disease progression after at least two prior lines of therapy, and had tumors with HER2 expression of IHC 3+ or 2+ either by local or central testing. Patients were allowed to have previously received HER2-targeting therapy. Patients also had to have good performance status (Eastern Cooperative Oncology Group/World Health Organization performance status 0 or 1).
The investigators planned to enroll 40 patients in each cohort, including patients with cervical, endometrial, ovarian, biliary tract, pancreatic, or bladder cancers, as well those with other tumors expressing HER2 who were not included in the other cohorts.
Under the protocol, cohorts in which none of the first 15 patients had objective responses would be closed, as happened with the pancreatic cancer cohort.
At a median follow-up of 9.7 months, an objective response was seen in 99 patients out of the 267 in the entire study population (ORR, 37.1%). This ORR consisted of 15 complete responses and 84 partial responses. An additional 123 patients had stable disease.
An analysis of ORR by HER2 expression showed that IHC 3+ expressing tumors had rates ranging from 84.6% in endometrial cancers, 75% in cervical cancer, 63.6% in ovarian cancers, and 56.3% in bladder cancers, down to zero in IHC 3+ expressing pancreatic cancer.
The T-DXd safety profile was consistent with that seen in other clinical trials, with most common adverse events being nausea, fatigue, neutropenia, anemia, diarrhea, and thrombocytopenia. There were 20 cases of interstitial lung disease, one of which was fatal.
The trial is ongoing, and investigators plan to report overall survival and progression-free survival results with additional follow-up.
DESTINY-PanTumor02 is funded by Daiichi Sankyo. Dr. Meric-Bernstam disclosed a consulting/advisory role with multiple pharmaceutical companies, research funding to her institution from Daiichi Sankyo and others, and travel expenses from ESMO and EORTC. Dr. McGregor disclosed a consulting/advisory role and institutional research funding with multiple companies, not including the study’s funder. Dr. Gralow disclosed a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
CHICAGO – Trastuzumab deruxtecan (T-DXd) (Enhertu) already has proven efficacy against HER2-expressing metastatic breast, gastroesophageal, and lung cancers.
including malignancies of the cervix, endometrium, ovaries, bladder, and other sites.
The findings come from the ongoing DESTINY-PanTumor02 trial. Among 267 patients with solid tumors at various organ sites, the investigator-assessed objective response rate among all patients was 37.1%, and ranged from as high as 57.5% for patients with endometrial cancers to as low as 4% for patients with pancreatic cancer, reported Funda Meric-Bernstam, MD, from the University of Texas MD Anderson Cancer Center, Houston.
For patients with tumors that had HER2 immunohistochemistry (IHC) scores of 3+, the highest level of HER2 expression, the overall response rate was 61.3%..
The responses were also durable, with a median duration of 11.8 months among all patients and 22.1 months among patients with IHC 3+ scores.
“Our data to date showed that T-DXd had clinically meaningful activity across a variety of tumor types,” she said in a briefing held prior to her presentation of the data at the annual meeting of the American Society of Clinical Oncology.
“HER2 expression has been around a long time. We think about this all the time in breast cancer and drugs are approved there, but HER2 is expressed in other tumors as well, and that really represents an unmet need, because we have limited options in this situation” commented ASCO expert Bradley Alexander McGregor, MD, from the Dana-Farber Cancer Institute, Boston, an invited discussant at the briefing.
“Aside from pancreatic cancer we saw really, really encouraging results with no new safety signals, so while early I think this really exciting and represents a shift in how we think about cancer care,” he added.
After the presentation, invited discussant Kohei Shitara, MD, of National Cancer Center Hospital East, Kashiwa, Japan, said that he agrees with authors that T-DXd is a potential new treatment option for patients with HER2-expressing solid tumors, and that the evidence suggests the potential for further tumor-agnostic development of the agent.
He cautioned, however, that there is a lack of concordance between local and central assessment of HER2 IHC, and that quality assurance will be required to ensure that the HER2 status of solid tumors is accurately characterized.
At a press briefing, Dr. Meric-Bernstam was asked how she envisioned using T-DXd in therapy for various HER2-expressing tumors.
“I think the activity we’ve seen is quite compelling, and one hopes that eventually this will be a drug that’s accessible for patients that are HER2-expressing across tumor types. Clearly, the activity is very compelling in some of the diseases to think about doing studies for earlier lines,” she said.
“The data indicate that there is tumor-agnostic activity across the board,” she said, but noted that tumors with epithelial components such as ovarian and breast cancers appear to have the highest responses to T-DXd therapy.
Briefing moderator Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, asked Dr. McGregor whether, in the light of this new data, oncologists should test more patients for HER2 expression.
“We have some cancers where we know HER2 expression is there. I think the good thing about HER2 testing is that it’s an IHC test, so this is something that can be easily done in local pathology [labs],” he said. As more evidence mounts of potential benefit of T-DXd in HER2 expressing tumors, clinicians will need to consider more routine HER2 testing.
A rendezvous with DESTINY
The DESTINY-PanTumor02 trial is a phase 2, open-label, multicenter study looking at T-DXd in patients with advanced solid tumors who are not eligible for therapy with curative intent.
All patients had disease progression after at least two prior lines of therapy, and had tumors with HER2 expression of IHC 3+ or 2+ either by local or central testing. Patients were allowed to have previously received HER2-targeting therapy. Patients also had to have good performance status (Eastern Cooperative Oncology Group/World Health Organization performance status 0 or 1).
The investigators planned to enroll 40 patients in each cohort, including patients with cervical, endometrial, ovarian, biliary tract, pancreatic, or bladder cancers, as well those with other tumors expressing HER2 who were not included in the other cohorts.
Under the protocol, cohorts in which none of the first 15 patients had objective responses would be closed, as happened with the pancreatic cancer cohort.
At a median follow-up of 9.7 months, an objective response was seen in 99 patients out of the 267 in the entire study population (ORR, 37.1%). This ORR consisted of 15 complete responses and 84 partial responses. An additional 123 patients had stable disease.
An analysis of ORR by HER2 expression showed that IHC 3+ expressing tumors had rates ranging from 84.6% in endometrial cancers, 75% in cervical cancer, 63.6% in ovarian cancers, and 56.3% in bladder cancers, down to zero in IHC 3+ expressing pancreatic cancer.
The T-DXd safety profile was consistent with that seen in other clinical trials, with most common adverse events being nausea, fatigue, neutropenia, anemia, diarrhea, and thrombocytopenia. There were 20 cases of interstitial lung disease, one of which was fatal.
The trial is ongoing, and investigators plan to report overall survival and progression-free survival results with additional follow-up.
DESTINY-PanTumor02 is funded by Daiichi Sankyo. Dr. Meric-Bernstam disclosed a consulting/advisory role with multiple pharmaceutical companies, research funding to her institution from Daiichi Sankyo and others, and travel expenses from ESMO and EORTC. Dr. McGregor disclosed a consulting/advisory role and institutional research funding with multiple companies, not including the study’s funder. Dr. Gralow disclosed a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
AT ASCO 2023
Comorbid respiratory disease key predictor of NTM-PD
(NTM-PD), data from a systematic review of 99 studies indicate.
NTM-PD is frequently underdiagnosed, and data on specific risk factors are lacking, especially for high-risk individuals with preexisting respiratory diseases, wrote Michael R. Loebinger, PhD, of Imperial College London, and colleagues.
“NTM-PD can be a substantial burden for patients, contributing to lung function decline and reduced health-related quality of life, and is associated with significant morbidity and mortality,” they said.
In a study published in the journal Chest, the researchers identified 99 studies published between 2011 and 2021. Of these, 24 reported an association between risk factors and NTM-PD among patients with respiratory disease compared with patients without NTM-PD and with healthy control persons without NTM-PD; these studies were included in the meta-analysis.
Overall, comorbid respiratory disease was significantly associated with an increased risk of NTM-PD, with odds ratios ranging from 4.15 for asthma to 21.43 for bronchiectasis. Other conditions significantly associated with NTM-PD risk included history of tuberculosis (odds ratio, 12.69), interstitial lung disease (OR, 6.39), and chronic obstructive pulmonary disease (COPD) (OR, 6.63).
Other factors associated with increased NTM-PD risk included inhaled corticosteroids (OR, 4.46), oral corticosteroids (OR, 3.37), and other immunosuppressants (OR, 2.60). Additional risk factors were use of anti–tumor necrosis factor-alpha for rheumatoid arthritis (OR, 2.13), solid tumors (OR, 4.66), current pneumonia (OR, 5.54), cardiovascular disease (OR, 1.73), and low body mass index (OR, 3.04).
Additional marginal or nonsignificant associations with NTM-PD risk were found for lung function, diabetes, renal disease, cancer, healthy weight, and infection with either Pseudomonas aeruginosa or Staphylococcus aureus.
Possible protective factors, though not significant, included increasing or high BMI and long-term macrolide use.
Bronchiectasis, which is associated with the highest risk of NTM-PD, was assessed in four studies. It was evaluated less frequently because it was often considered a reason for study exclusion, the researchers wrote in their discussion.
“However, many studies report high numbers of patients with nodular bronchiectatic NTM-PD and is suggested to be almost universal in patients with noncavitary NTM-PD,” they said.
The most common risk factors for NTM-PD in the included studies were the use of immunosuppressants, female sex, COPD comorbidity, and history of suspected tuberculosis.
The findings were limited by several factors, including the high level of heterogeneity among the included studies, the lack of data on attributable risk, and inconsistent definitions of NTM-PD, the researchers noted. However, the results may be useful for highlighting risk factors that could be used to identify high-risk patients and to promote early diagnosis and treatment, they said. In addition, long-term studies are needed regarding the impact of multiple potential risk factors on individual risk for NTM-PD among patients with respiratory disease, they concluded.
The study was supported by Insmed BV. Dr. Loebinger has relationships with Insmed, AstraZeneca, Chiesi, Savara, Parion, Zambon, 30T, Electromed, Recode, AN2 Therapeutics, and Armata.
A version of this article first appeared on Medscape.com.
(NTM-PD), data from a systematic review of 99 studies indicate.
NTM-PD is frequently underdiagnosed, and data on specific risk factors are lacking, especially for high-risk individuals with preexisting respiratory diseases, wrote Michael R. Loebinger, PhD, of Imperial College London, and colleagues.
“NTM-PD can be a substantial burden for patients, contributing to lung function decline and reduced health-related quality of life, and is associated with significant morbidity and mortality,” they said.
In a study published in the journal Chest, the researchers identified 99 studies published between 2011 and 2021. Of these, 24 reported an association between risk factors and NTM-PD among patients with respiratory disease compared with patients without NTM-PD and with healthy control persons without NTM-PD; these studies were included in the meta-analysis.
Overall, comorbid respiratory disease was significantly associated with an increased risk of NTM-PD, with odds ratios ranging from 4.15 for asthma to 21.43 for bronchiectasis. Other conditions significantly associated with NTM-PD risk included history of tuberculosis (odds ratio, 12.69), interstitial lung disease (OR, 6.39), and chronic obstructive pulmonary disease (COPD) (OR, 6.63).
Other factors associated with increased NTM-PD risk included inhaled corticosteroids (OR, 4.46), oral corticosteroids (OR, 3.37), and other immunosuppressants (OR, 2.60). Additional risk factors were use of anti–tumor necrosis factor-alpha for rheumatoid arthritis (OR, 2.13), solid tumors (OR, 4.66), current pneumonia (OR, 5.54), cardiovascular disease (OR, 1.73), and low body mass index (OR, 3.04).
Additional marginal or nonsignificant associations with NTM-PD risk were found for lung function, diabetes, renal disease, cancer, healthy weight, and infection with either Pseudomonas aeruginosa or Staphylococcus aureus.
Possible protective factors, though not significant, included increasing or high BMI and long-term macrolide use.
Bronchiectasis, which is associated with the highest risk of NTM-PD, was assessed in four studies. It was evaluated less frequently because it was often considered a reason for study exclusion, the researchers wrote in their discussion.
“However, many studies report high numbers of patients with nodular bronchiectatic NTM-PD and is suggested to be almost universal in patients with noncavitary NTM-PD,” they said.
The most common risk factors for NTM-PD in the included studies were the use of immunosuppressants, female sex, COPD comorbidity, and history of suspected tuberculosis.
The findings were limited by several factors, including the high level of heterogeneity among the included studies, the lack of data on attributable risk, and inconsistent definitions of NTM-PD, the researchers noted. However, the results may be useful for highlighting risk factors that could be used to identify high-risk patients and to promote early diagnosis and treatment, they said. In addition, long-term studies are needed regarding the impact of multiple potential risk factors on individual risk for NTM-PD among patients with respiratory disease, they concluded.
The study was supported by Insmed BV. Dr. Loebinger has relationships with Insmed, AstraZeneca, Chiesi, Savara, Parion, Zambon, 30T, Electromed, Recode, AN2 Therapeutics, and Armata.
A version of this article first appeared on Medscape.com.
(NTM-PD), data from a systematic review of 99 studies indicate.
NTM-PD is frequently underdiagnosed, and data on specific risk factors are lacking, especially for high-risk individuals with preexisting respiratory diseases, wrote Michael R. Loebinger, PhD, of Imperial College London, and colleagues.
“NTM-PD can be a substantial burden for patients, contributing to lung function decline and reduced health-related quality of life, and is associated with significant morbidity and mortality,” they said.
In a study published in the journal Chest, the researchers identified 99 studies published between 2011 and 2021. Of these, 24 reported an association between risk factors and NTM-PD among patients with respiratory disease compared with patients without NTM-PD and with healthy control persons without NTM-PD; these studies were included in the meta-analysis.
Overall, comorbid respiratory disease was significantly associated with an increased risk of NTM-PD, with odds ratios ranging from 4.15 for asthma to 21.43 for bronchiectasis. Other conditions significantly associated with NTM-PD risk included history of tuberculosis (odds ratio, 12.69), interstitial lung disease (OR, 6.39), and chronic obstructive pulmonary disease (COPD) (OR, 6.63).
Other factors associated with increased NTM-PD risk included inhaled corticosteroids (OR, 4.46), oral corticosteroids (OR, 3.37), and other immunosuppressants (OR, 2.60). Additional risk factors were use of anti–tumor necrosis factor-alpha for rheumatoid arthritis (OR, 2.13), solid tumors (OR, 4.66), current pneumonia (OR, 5.54), cardiovascular disease (OR, 1.73), and low body mass index (OR, 3.04).
Additional marginal or nonsignificant associations with NTM-PD risk were found for lung function, diabetes, renal disease, cancer, healthy weight, and infection with either Pseudomonas aeruginosa or Staphylococcus aureus.
Possible protective factors, though not significant, included increasing or high BMI and long-term macrolide use.
Bronchiectasis, which is associated with the highest risk of NTM-PD, was assessed in four studies. It was evaluated less frequently because it was often considered a reason for study exclusion, the researchers wrote in their discussion.
“However, many studies report high numbers of patients with nodular bronchiectatic NTM-PD and is suggested to be almost universal in patients with noncavitary NTM-PD,” they said.
The most common risk factors for NTM-PD in the included studies were the use of immunosuppressants, female sex, COPD comorbidity, and history of suspected tuberculosis.
The findings were limited by several factors, including the high level of heterogeneity among the included studies, the lack of data on attributable risk, and inconsistent definitions of NTM-PD, the researchers noted. However, the results may be useful for highlighting risk factors that could be used to identify high-risk patients and to promote early diagnosis and treatment, they said. In addition, long-term studies are needed regarding the impact of multiple potential risk factors on individual risk for NTM-PD among patients with respiratory disease, they concluded.
The study was supported by Insmed BV. Dr. Loebinger has relationships with Insmed, AstraZeneca, Chiesi, Savara, Parion, Zambon, 30T, Electromed, Recode, AN2 Therapeutics, and Armata.
A version of this article first appeared on Medscape.com.
CDC signs off on RSV vaccine for older adults
The Centers for Disease Control and Prevention has given a green light to two new vaccines to protect against respiratory syncytial virus, or RSV, in older adults.
CDC Director Rochelle P. Walensky, MD, MPH, agreed with and endorsed the recommendations made earlier by CDC advisors that people age 60 and over may get one of two new vaccines for RSV. Decisions should be made based on discussions with one’s health care provider about whether the vaccine is right for them, the federal health agency said.
The new vaccines, the first licensed in the United States to protect against the respiratory illness, are expected to be available this fall.
On June 21, the CDC’s Advisory Committee on Immunization Practices (ACIP), an independent panel, stopped short of recommending the vaccines for everyone age 65 and above, which was the original question the committee was to consider. The experts amended that question, changing it to whether the panel should recommend the vaccine for those 65 and above if the person and their doctor agreed. The committee voted 9 to 5 in favor.
RSV vaccines
RSV leads to 6,000 to 10,000 deaths a year in the United States among those age 65 and older and 60,000 to 160,000 hospitalizations in that group. Seniors and infants are among the most vulnerable to the lower respiratory infection, marked by runny nose, wheezing, sneezing, decreased appetite, and fever.
The FDA in May approved two vaccines — GSK’s Arexvy and Pfizer’s Abrysvo — for adults age 60 and above.
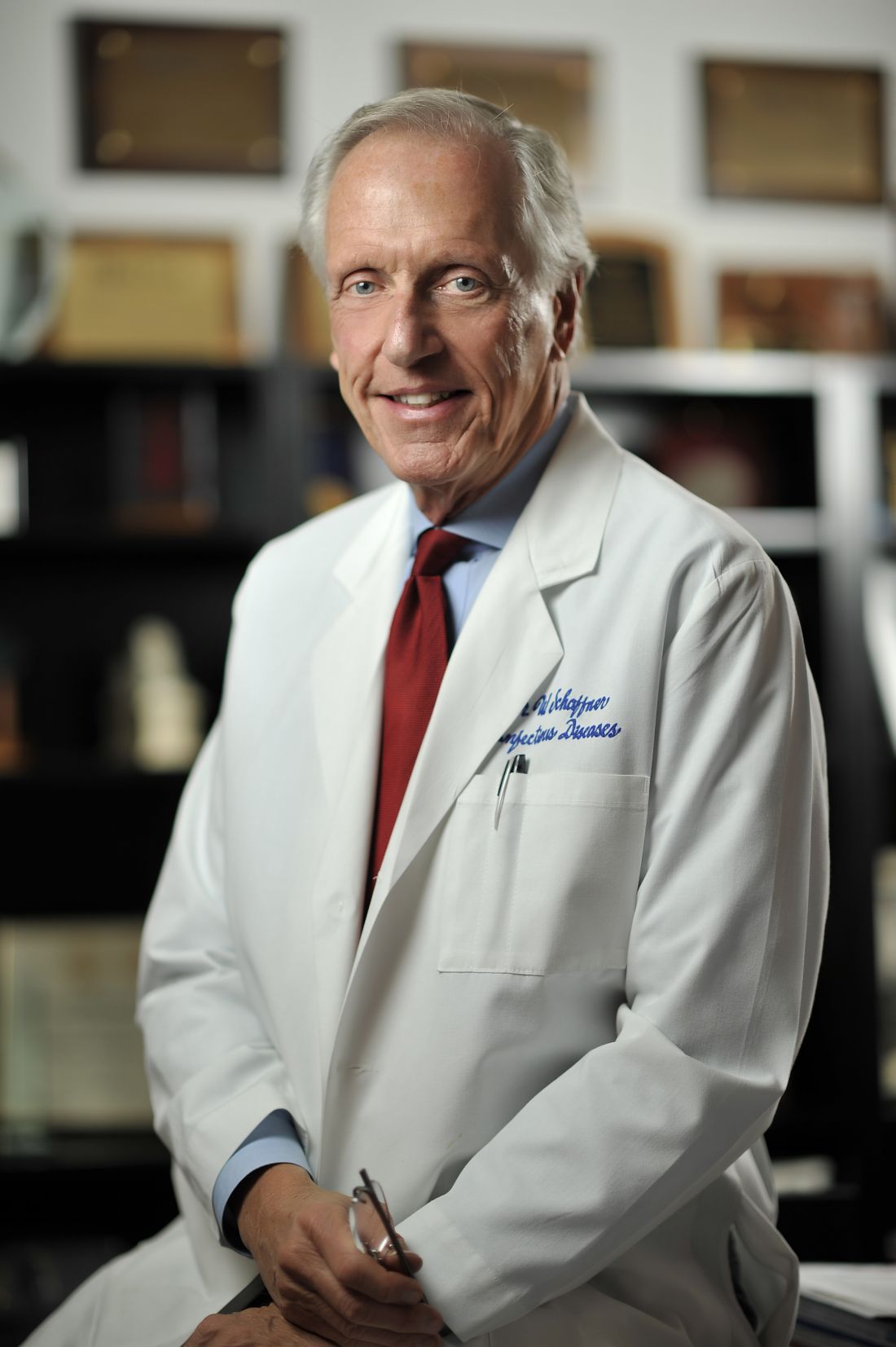
The vote recommending shared decision-making about the vaccine, instead of a routine vaccination recommended for all, “is a weaker recommendation,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University Medical Center in Nashville and medical director of the National Foundation for Infectious Diseases. Dr. Schaffner is a non-voting member of ACIP. He attended the meeting.
He said the experts voiced concern about a number of issues, including what some saw as a lack of sufficient data from trials on the most vulnerable groups, such as nursing home residents.
Experts also wanted more information about the duration of protection and exactly when a second dose might be needed. At the meeting, a GSK official said its vaccine was 84.6% effective after one and a half seasons, down from 94.1% after one season. A Pfizer official said its vaccine decreased the risk of RSV with three or more symptoms by 78.6% after a season and a half, down from 88.9% after one season.
The panel also wanted more data on whether the RSV vaccines could be administered at the same time as other vaccines recommended for adults.
Both companies gave a range of cost estimates. Pfizer expects its vaccine to cost $180 to $270 but said it could not guarantee that range. GSK said it expects a price of $200 to $295. Under the Inflation Reduction Act, recommended vaccines are covered under Medicare for those with Part D plans, which 51 million of 65 million Medicare patients have. Commercial insurance is likely to cover the vaccines if the CDC recommends them.
A version of this article first appeared on WebMD.com.
This article was updated 7/5/23.
The Centers for Disease Control and Prevention has given a green light to two new vaccines to protect against respiratory syncytial virus, or RSV, in older adults.
CDC Director Rochelle P. Walensky, MD, MPH, agreed with and endorsed the recommendations made earlier by CDC advisors that people age 60 and over may get one of two new vaccines for RSV. Decisions should be made based on discussions with one’s health care provider about whether the vaccine is right for them, the federal health agency said.
The new vaccines, the first licensed in the United States to protect against the respiratory illness, are expected to be available this fall.
On June 21, the CDC’s Advisory Committee on Immunization Practices (ACIP), an independent panel, stopped short of recommending the vaccines for everyone age 65 and above, which was the original question the committee was to consider. The experts amended that question, changing it to whether the panel should recommend the vaccine for those 65 and above if the person and their doctor agreed. The committee voted 9 to 5 in favor.
RSV vaccines
RSV leads to 6,000 to 10,000 deaths a year in the United States among those age 65 and older and 60,000 to 160,000 hospitalizations in that group. Seniors and infants are among the most vulnerable to the lower respiratory infection, marked by runny nose, wheezing, sneezing, decreased appetite, and fever.
The FDA in May approved two vaccines — GSK’s Arexvy and Pfizer’s Abrysvo — for adults age 60 and above.
The vote recommending shared decision-making about the vaccine, instead of a routine vaccination recommended for all, “is a weaker recommendation,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University Medical Center in Nashville and medical director of the National Foundation for Infectious Diseases. Dr. Schaffner is a non-voting member of ACIP. He attended the meeting.
He said the experts voiced concern about a number of issues, including what some saw as a lack of sufficient data from trials on the most vulnerable groups, such as nursing home residents.
Experts also wanted more information about the duration of protection and exactly when a second dose might be needed. At the meeting, a GSK official said its vaccine was 84.6% effective after one and a half seasons, down from 94.1% after one season. A Pfizer official said its vaccine decreased the risk of RSV with three or more symptoms by 78.6% after a season and a half, down from 88.9% after one season.
The panel also wanted more data on whether the RSV vaccines could be administered at the same time as other vaccines recommended for adults.
Both companies gave a range of cost estimates. Pfizer expects its vaccine to cost $180 to $270 but said it could not guarantee that range. GSK said it expects a price of $200 to $295. Under the Inflation Reduction Act, recommended vaccines are covered under Medicare for those with Part D plans, which 51 million of 65 million Medicare patients have. Commercial insurance is likely to cover the vaccines if the CDC recommends them.
A version of this article first appeared on WebMD.com.
This article was updated 7/5/23.
The Centers for Disease Control and Prevention has given a green light to two new vaccines to protect against respiratory syncytial virus, or RSV, in older adults.
CDC Director Rochelle P. Walensky, MD, MPH, agreed with and endorsed the recommendations made earlier by CDC advisors that people age 60 and over may get one of two new vaccines for RSV. Decisions should be made based on discussions with one’s health care provider about whether the vaccine is right for them, the federal health agency said.
The new vaccines, the first licensed in the United States to protect against the respiratory illness, are expected to be available this fall.
On June 21, the CDC’s Advisory Committee on Immunization Practices (ACIP), an independent panel, stopped short of recommending the vaccines for everyone age 65 and above, which was the original question the committee was to consider. The experts amended that question, changing it to whether the panel should recommend the vaccine for those 65 and above if the person and their doctor agreed. The committee voted 9 to 5 in favor.
RSV vaccines
RSV leads to 6,000 to 10,000 deaths a year in the United States among those age 65 and older and 60,000 to 160,000 hospitalizations in that group. Seniors and infants are among the most vulnerable to the lower respiratory infection, marked by runny nose, wheezing, sneezing, decreased appetite, and fever.
The FDA in May approved two vaccines — GSK’s Arexvy and Pfizer’s Abrysvo — for adults age 60 and above.
The vote recommending shared decision-making about the vaccine, instead of a routine vaccination recommended for all, “is a weaker recommendation,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University Medical Center in Nashville and medical director of the National Foundation for Infectious Diseases. Dr. Schaffner is a non-voting member of ACIP. He attended the meeting.
He said the experts voiced concern about a number of issues, including what some saw as a lack of sufficient data from trials on the most vulnerable groups, such as nursing home residents.
Experts also wanted more information about the duration of protection and exactly when a second dose might be needed. At the meeting, a GSK official said its vaccine was 84.6% effective after one and a half seasons, down from 94.1% after one season. A Pfizer official said its vaccine decreased the risk of RSV with three or more symptoms by 78.6% after a season and a half, down from 88.9% after one season.
The panel also wanted more data on whether the RSV vaccines could be administered at the same time as other vaccines recommended for adults.
Both companies gave a range of cost estimates. Pfizer expects its vaccine to cost $180 to $270 but said it could not guarantee that range. GSK said it expects a price of $200 to $295. Under the Inflation Reduction Act, recommended vaccines are covered under Medicare for those with Part D plans, which 51 million of 65 million Medicare patients have. Commercial insurance is likely to cover the vaccines if the CDC recommends them.
A version of this article first appeared on WebMD.com.
This article was updated 7/5/23.
Low-dose colchicine approved for CVD: Now what?
The recent U.S. approval of a new low dose of colchicine 0.5 mg (Lodoco; Agepha Pharma) with a broad indication for use in atherosclerotic cardiovascular disease (ASCVD) represents a completely new approach to treatment, specifically targeting inflammation as a driver of atherosclerosis.
The Food and Drug Administration granted colchicine a very broad label: to reduce the risk for cardiovascular events in adult patients with established ASCVD or with multiple risk factors for cardiovascular disease. But how will the drug be used in clinical practice?
“The idea of inflammation as a driver of atherosclerosis and cardiovascular risk has been around for decades, and it is very well known that atherosclerosis is an inflammatory process. However, treating inflammation is new as we haven’t had a specific agent targeting inflammation before, noted Michael Joseph Blaha, MD, director of clinical research, Ciccarone Center for the Prevention of Cardiovascular Disease at Johns Hopkins Hospital, Baltimore.
Dr. Blaha, who has been an unpaid scientific adviser to Agepha, added that the approval of low-dose colchicine “will open the door toward having a routine conversation about residual inflammatory risk in our patients; and we need to work out exactly how we do that.”
Dr. Blaha is not surprised by the FDA-approved indication for colchicine, pointing out that the main large-scale trial supporting its use in ASCVD, the LoDoCo-2 trial, included a similar broad population.
“I think the approval was appropriate as the indication should always follow the data. But I think how the drug will actually be used will depend on the context for different individual patients,” he said.
“The paradigm coming forward is the idea of residual risk that patients have after they been treated with the standard of care – which in most cases is a statin and blood pressure control – and what is driving that residual risk,” he noted. “If we think patients are still at high risk of recurrent cardiovascular events, we have to think what we will do next. This is where this drug will come in.”
Dr. Blaha pointed out that there are now multiple options for reducing residual risk; he believes that it will depend on the profile of the patient as to which of those options is chosen first.
“If after high-dose statin treatment they still have raised LDL, then we can add another LDL lowering drug; or it might be diabetes and obesity that we want to address first; or elevated triglycerides. But now, we can also consider residual inflammatory risk if we think the patient has residual plaque inflammation,” he said. “So, colchicine will be one of several choices beyond a statin that we can think about as the next step for treating residual risk.”
Is CRP measurement necessary?
Though elevated levels of high-sensitivity C-reactive protein (hsCRP) is a marker of inflammation in ASCVD, the two main trials of colchicine in ASCVD, both of which showed large benefits of the drug, did not measure hsCRP, leading to questions as to whether measurement of this biomarker is necessary to select patients for colchicine treatment.
“Some clinicians will favor testing hsCRP and treating those with levels above 2 mg/L. I think that’s very reasonable,” Dr. Blaha said. “However, because hsCRP was not measured in the trials, I don’t think testing for this biomarker is mandatory to establish that there is inflammation,” he added.
“The label does not stipulate that CRP has to be measured. It is giving physicians latitude; they can measure CRP, or they don’t have to.”
Dr. Blaha added that clinicians need to think about what is driving residual risk in each individual patient: “If you think their other risk factors are well controlled but they are still having recurrent events, then we can consider colchicine as a way of reducing their residual risk which is likely being caused by inflammation.
“We are at a great place in cardiovascular medicine as we have several different options to use after a statin, and now we have this new therapy targeted at inflammation as well. While we can use all these options together, I think most clinicians will want to prioritize therapies by using the ones that they believe will reduce the residual risk the most in each individual patient,” Dr. Blaha explained.
‘An entire other axis driving atherosclerosis’
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, is one of the major players in the cardiovascular inflammation field and has helped develop hsCRP testing. He has similar views.
“This FDA approval is extremely important, as it will draw attention to the role of inflammation in atherosclerosis and the need to treat it,” he said.
“Physicians need to be aware that, yes, we need to lower cholesterol aggressively, but they also need to know that there is an entire other axis driving atherosclerosis – and that is inflammation. And until now, we haven’t had an FDA-approved drug to treat inflammation.”
Dr. Ridker stressed that he doesn’t want to undermine lowering lipids: “Therapies aimed at inflammation are not in competition with those aimed at lipid lowering. We know lipid lowering works. But now we have another approach as well. The challenge here is educating physicians on this new approach.”
Dr. Ridker said he already uses low-dose colchicine for patients whom he refers to as “frequent flyers”; those who keep coming back despite aggressive lipid lowering. “They have multiple angioplasties, bypass surgery, etc.”
Like Dr. Blaha, Dr. Ridker thinks that doctors should start using this drug in high-risk patients who are already on a statin and who have residual inflammatory risk: “[The] patient whose underlying biologic problem is inflammation [is whom] we really want to treat with this drug. That is where it is most likely to be highly effective and where the comfort level will be the greatest.”
He said that measurement of hsCRP is an appropriate way to select these patients.
“I think this is a great impetus to start having much wider CRP measurement so we can actually target this anti-inflammatory drug to the patients with residual inflammatory risk – those with hsCRP level above 2 mg/L,” he said, estimating that this could apply to around 30%-40% of patients with ASCVD who are already taking a statin.
A second pillar of ASCVD treatment?
A somewhat different view is held by Jean-Claude Tardif, MD, director of the Research Centre at the Montréal Heart Institute, Canada, who was the lead investigator of the other randomized controlled trial of colchicine in heart disease, the COLCOT trial.
He said that colchicine should become the “second pillar” of ASCVD treatment, along with statins, for almost all patients.
Tardif referred to the recent study (led by Dr. Ridker) in The Lancet, which showed that among patients who are already on a statin, those with high inflammation levels had the highest risk for future events.
“So, the next step after a statin has to be to consider inflammation reduction,” he said.
“Despite all the drugs we have, ASCVD remains the leading cause of death in the Western world. What drives these events is largely inflammation, so it makes sense to directly tackle reduction of inflammation in the vessel, with a drug like colchicine,” he noted.
“I would say all patients with coronary atherosclerosis are potential candidates for low-dose colchicine as long as they do not have severe kidney disease, which is a contraindication,” Dr. Tardif said.
“If you want to fine tune this a bit more, those that are at particular risk are those that have recurrent events, those with multiple risk factors, and those with a recent [myocardial infarction]. In these patients, it would make a lot of sense to add low-dose colchicine to high-dose statins,” he added.
Dr. Tardif said he is not going to use CRP measurements to select patients for colchicine treatment: “Although measuring CRP may make sense intuitively, both large, randomized trials of colchicine did not select patients based on raised CRP, and they showed a benefit across the board.
If I consider a patient with ASCVD to be at high risk of future events and they are already on a statin I’m going to consider colchicine in all these patients, as long as they don’t have severe kidney disease.”
Dr. Tardif said that ASCVD needs to follow the model of heart failure which has several pillars of treatment directed at different targets that are all used together.
“I think we should apply the same approach to patients with ASCVD,” he added. “Yes, we need to hit the cholesterol with a statin, but we can now also hit the inflammation with colchicine.”
Polypharmacy concerns
Steve Nissen, MD, professor of medicine at the Cleveland Clinic, who was not involved in the colchicine trials, is also enthusiastic about use of colchicine. But like Dr. Ridker and Dr. Blaha, he favors selecting patients who are likely to benefit the most.
“I have been an advocate of the inflammatory hypothesis for many years, and we have been on a quest for a pure anti-inflammatory therapy that we can add to the standard treatment of patients with coronary disease. And colchicine has the safety and efficacy to do this,” Dr. Nissen said.
“What colchicine offers here is an inexpensive drug with pretty good data on reduction in morbidity from coronary disease. It has a completely different mechanism, so its benefit is likely to be additive to statins. I think we could probably do a lot of good at very little expense by just using these two therapies,” he said.
“But at present my preference will be to use colchicine selectively in those with raised CRP. I think that’s logical. I’m just worried about polypharmacy. Some of my patients are already on five, six, or seven meds. I need to have a reason to add an additional drug, and I’m not sure if we really analyze this carefully that patients with a low CRP would derive the same benefit. They might do, but I doubt it,” he noted.
“There may be further research and analyses that help us understand the relationship between CRP and efficacy of colchicine, and that may help us figure this out,” he added.
Safety is reassuring
In terms of safety and tolerability of the 0.5-mg colchicine dose, the experts seem to think that this is very manageable.
“When used for gout or pericarditis, colchicine is generally given at a dose of 0.6 mg twice a day and this can cause a lot of gastrointestinal [GI] side effects,” Dr. Nissen said. “But the low dose approved for ASCVD – 0.5 mg once a day – appears to be much better tolerated. There are some GI side effects, but these are not intolerable, and they generally go away with time.”
Dr. Ridker added that in the randomized trials, the adverse effects were “quite minimal,” but, “that being said, this drug is not to be used in severe kidney or liver disease, and there are some drug interactions that we need to be aware of. But in general, side effects are rare with the low dose. There may be some GI effects but they are mainly mild and you can generally treat through them.”
Dr. Blaha agreed that this is not a drug for patients with advanced kidney disease, “and there are some drug interactions that we have to be mindful of, but the list is not so long. There is a signal of modest gastrointestinal and muscle side effects, but most patients will be able to take it without issues. Because it’s already used in gout, physicians are already quite comfortable with its use.”
Part of the backbone of CV treatment?
Concluding, Dr. Blaha said he believes that prescribing of colchicine will start with cardiologists who will use it in their highest-risk patients first.
“But as we become comfortable with it, I think we will start using it in a broader range of patients and eventually primary care doctors will start prescribing it – much like what has happened with the statins,” he suggested.
“Where it sits along with statins in the future will be very interesting to see, but I think some people can envision it being up there with statins as part of the backbone of cardiovascular treatment in future.”
Dr. Tardif holds patents on methods for using low-dose colchicine after myocardial infarction, licensed to Montreal Heart Institute. Dr. Ridker is a consultant to Agepha and has research grants from Novo Nordisk related to the development of alternative anti-inflammatory therapies for atherosclerotic disease. Dr. Blaha reports being an unpaid scientific adviser to Agepha Pharma.
A version of this article first appeared on Medscape.com.
The recent U.S. approval of a new low dose of colchicine 0.5 mg (Lodoco; Agepha Pharma) with a broad indication for use in atherosclerotic cardiovascular disease (ASCVD) represents a completely new approach to treatment, specifically targeting inflammation as a driver of atherosclerosis.
The Food and Drug Administration granted colchicine a very broad label: to reduce the risk for cardiovascular events in adult patients with established ASCVD or with multiple risk factors for cardiovascular disease. But how will the drug be used in clinical practice?
“The idea of inflammation as a driver of atherosclerosis and cardiovascular risk has been around for decades, and it is very well known that atherosclerosis is an inflammatory process. However, treating inflammation is new as we haven’t had a specific agent targeting inflammation before, noted Michael Joseph Blaha, MD, director of clinical research, Ciccarone Center for the Prevention of Cardiovascular Disease at Johns Hopkins Hospital, Baltimore.
Dr. Blaha, who has been an unpaid scientific adviser to Agepha, added that the approval of low-dose colchicine “will open the door toward having a routine conversation about residual inflammatory risk in our patients; and we need to work out exactly how we do that.”
Dr. Blaha is not surprised by the FDA-approved indication for colchicine, pointing out that the main large-scale trial supporting its use in ASCVD, the LoDoCo-2 trial, included a similar broad population.
“I think the approval was appropriate as the indication should always follow the data. But I think how the drug will actually be used will depend on the context for different individual patients,” he said.
“The paradigm coming forward is the idea of residual risk that patients have after they been treated with the standard of care – which in most cases is a statin and blood pressure control – and what is driving that residual risk,” he noted. “If we think patients are still at high risk of recurrent cardiovascular events, we have to think what we will do next. This is where this drug will come in.”
Dr. Blaha pointed out that there are now multiple options for reducing residual risk; he believes that it will depend on the profile of the patient as to which of those options is chosen first.
“If after high-dose statin treatment they still have raised LDL, then we can add another LDL lowering drug; or it might be diabetes and obesity that we want to address first; or elevated triglycerides. But now, we can also consider residual inflammatory risk if we think the patient has residual plaque inflammation,” he said. “So, colchicine will be one of several choices beyond a statin that we can think about as the next step for treating residual risk.”
Is CRP measurement necessary?
Though elevated levels of high-sensitivity C-reactive protein (hsCRP) is a marker of inflammation in ASCVD, the two main trials of colchicine in ASCVD, both of which showed large benefits of the drug, did not measure hsCRP, leading to questions as to whether measurement of this biomarker is necessary to select patients for colchicine treatment.
“Some clinicians will favor testing hsCRP and treating those with levels above 2 mg/L. I think that’s very reasonable,” Dr. Blaha said. “However, because hsCRP was not measured in the trials, I don’t think testing for this biomarker is mandatory to establish that there is inflammation,” he added.
“The label does not stipulate that CRP has to be measured. It is giving physicians latitude; they can measure CRP, or they don’t have to.”
Dr. Blaha added that clinicians need to think about what is driving residual risk in each individual patient: “If you think their other risk factors are well controlled but they are still having recurrent events, then we can consider colchicine as a way of reducing their residual risk which is likely being caused by inflammation.
“We are at a great place in cardiovascular medicine as we have several different options to use after a statin, and now we have this new therapy targeted at inflammation as well. While we can use all these options together, I think most clinicians will want to prioritize therapies by using the ones that they believe will reduce the residual risk the most in each individual patient,” Dr. Blaha explained.
‘An entire other axis driving atherosclerosis’
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, is one of the major players in the cardiovascular inflammation field and has helped develop hsCRP testing. He has similar views.
“This FDA approval is extremely important, as it will draw attention to the role of inflammation in atherosclerosis and the need to treat it,” he said.
“Physicians need to be aware that, yes, we need to lower cholesterol aggressively, but they also need to know that there is an entire other axis driving atherosclerosis – and that is inflammation. And until now, we haven’t had an FDA-approved drug to treat inflammation.”
Dr. Ridker stressed that he doesn’t want to undermine lowering lipids: “Therapies aimed at inflammation are not in competition with those aimed at lipid lowering. We know lipid lowering works. But now we have another approach as well. The challenge here is educating physicians on this new approach.”
Dr. Ridker said he already uses low-dose colchicine for patients whom he refers to as “frequent flyers”; those who keep coming back despite aggressive lipid lowering. “They have multiple angioplasties, bypass surgery, etc.”
Like Dr. Blaha, Dr. Ridker thinks that doctors should start using this drug in high-risk patients who are already on a statin and who have residual inflammatory risk: “[The] patient whose underlying biologic problem is inflammation [is whom] we really want to treat with this drug. That is where it is most likely to be highly effective and where the comfort level will be the greatest.”
He said that measurement of hsCRP is an appropriate way to select these patients.
“I think this is a great impetus to start having much wider CRP measurement so we can actually target this anti-inflammatory drug to the patients with residual inflammatory risk – those with hsCRP level above 2 mg/L,” he said, estimating that this could apply to around 30%-40% of patients with ASCVD who are already taking a statin.
A second pillar of ASCVD treatment?
A somewhat different view is held by Jean-Claude Tardif, MD, director of the Research Centre at the Montréal Heart Institute, Canada, who was the lead investigator of the other randomized controlled trial of colchicine in heart disease, the COLCOT trial.
He said that colchicine should become the “second pillar” of ASCVD treatment, along with statins, for almost all patients.
Tardif referred to the recent study (led by Dr. Ridker) in The Lancet, which showed that among patients who are already on a statin, those with high inflammation levels had the highest risk for future events.
“So, the next step after a statin has to be to consider inflammation reduction,” he said.
“Despite all the drugs we have, ASCVD remains the leading cause of death in the Western world. What drives these events is largely inflammation, so it makes sense to directly tackle reduction of inflammation in the vessel, with a drug like colchicine,” he noted.
“I would say all patients with coronary atherosclerosis are potential candidates for low-dose colchicine as long as they do not have severe kidney disease, which is a contraindication,” Dr. Tardif said.
“If you want to fine tune this a bit more, those that are at particular risk are those that have recurrent events, those with multiple risk factors, and those with a recent [myocardial infarction]. In these patients, it would make a lot of sense to add low-dose colchicine to high-dose statins,” he added.
Dr. Tardif said he is not going to use CRP measurements to select patients for colchicine treatment: “Although measuring CRP may make sense intuitively, both large, randomized trials of colchicine did not select patients based on raised CRP, and they showed a benefit across the board.
If I consider a patient with ASCVD to be at high risk of future events and they are already on a statin I’m going to consider colchicine in all these patients, as long as they don’t have severe kidney disease.”
Dr. Tardif said that ASCVD needs to follow the model of heart failure which has several pillars of treatment directed at different targets that are all used together.
“I think we should apply the same approach to patients with ASCVD,” he added. “Yes, we need to hit the cholesterol with a statin, but we can now also hit the inflammation with colchicine.”
Polypharmacy concerns
Steve Nissen, MD, professor of medicine at the Cleveland Clinic, who was not involved in the colchicine trials, is also enthusiastic about use of colchicine. But like Dr. Ridker and Dr. Blaha, he favors selecting patients who are likely to benefit the most.
“I have been an advocate of the inflammatory hypothesis for many years, and we have been on a quest for a pure anti-inflammatory therapy that we can add to the standard treatment of patients with coronary disease. And colchicine has the safety and efficacy to do this,” Dr. Nissen said.
“What colchicine offers here is an inexpensive drug with pretty good data on reduction in morbidity from coronary disease. It has a completely different mechanism, so its benefit is likely to be additive to statins. I think we could probably do a lot of good at very little expense by just using these two therapies,” he said.
“But at present my preference will be to use colchicine selectively in those with raised CRP. I think that’s logical. I’m just worried about polypharmacy. Some of my patients are already on five, six, or seven meds. I need to have a reason to add an additional drug, and I’m not sure if we really analyze this carefully that patients with a low CRP would derive the same benefit. They might do, but I doubt it,” he noted.
“There may be further research and analyses that help us understand the relationship between CRP and efficacy of colchicine, and that may help us figure this out,” he added.
Safety is reassuring
In terms of safety and tolerability of the 0.5-mg colchicine dose, the experts seem to think that this is very manageable.
“When used for gout or pericarditis, colchicine is generally given at a dose of 0.6 mg twice a day and this can cause a lot of gastrointestinal [GI] side effects,” Dr. Nissen said. “But the low dose approved for ASCVD – 0.5 mg once a day – appears to be much better tolerated. There are some GI side effects, but these are not intolerable, and they generally go away with time.”
Dr. Ridker added that in the randomized trials, the adverse effects were “quite minimal,” but, “that being said, this drug is not to be used in severe kidney or liver disease, and there are some drug interactions that we need to be aware of. But in general, side effects are rare with the low dose. There may be some GI effects but they are mainly mild and you can generally treat through them.”
Dr. Blaha agreed that this is not a drug for patients with advanced kidney disease, “and there are some drug interactions that we have to be mindful of, but the list is not so long. There is a signal of modest gastrointestinal and muscle side effects, but most patients will be able to take it without issues. Because it’s already used in gout, physicians are already quite comfortable with its use.”
Part of the backbone of CV treatment?
Concluding, Dr. Blaha said he believes that prescribing of colchicine will start with cardiologists who will use it in their highest-risk patients first.
“But as we become comfortable with it, I think we will start using it in a broader range of patients and eventually primary care doctors will start prescribing it – much like what has happened with the statins,” he suggested.
“Where it sits along with statins in the future will be very interesting to see, but I think some people can envision it being up there with statins as part of the backbone of cardiovascular treatment in future.”
Dr. Tardif holds patents on methods for using low-dose colchicine after myocardial infarction, licensed to Montreal Heart Institute. Dr. Ridker is a consultant to Agepha and has research grants from Novo Nordisk related to the development of alternative anti-inflammatory therapies for atherosclerotic disease. Dr. Blaha reports being an unpaid scientific adviser to Agepha Pharma.
A version of this article first appeared on Medscape.com.
The recent U.S. approval of a new low dose of colchicine 0.5 mg (Lodoco; Agepha Pharma) with a broad indication for use in atherosclerotic cardiovascular disease (ASCVD) represents a completely new approach to treatment, specifically targeting inflammation as a driver of atherosclerosis.
The Food and Drug Administration granted colchicine a very broad label: to reduce the risk for cardiovascular events in adult patients with established ASCVD or with multiple risk factors for cardiovascular disease. But how will the drug be used in clinical practice?
“The idea of inflammation as a driver of atherosclerosis and cardiovascular risk has been around for decades, and it is very well known that atherosclerosis is an inflammatory process. However, treating inflammation is new as we haven’t had a specific agent targeting inflammation before, noted Michael Joseph Blaha, MD, director of clinical research, Ciccarone Center for the Prevention of Cardiovascular Disease at Johns Hopkins Hospital, Baltimore.
Dr. Blaha, who has been an unpaid scientific adviser to Agepha, added that the approval of low-dose colchicine “will open the door toward having a routine conversation about residual inflammatory risk in our patients; and we need to work out exactly how we do that.”
Dr. Blaha is not surprised by the FDA-approved indication for colchicine, pointing out that the main large-scale trial supporting its use in ASCVD, the LoDoCo-2 trial, included a similar broad population.
“I think the approval was appropriate as the indication should always follow the data. But I think how the drug will actually be used will depend on the context for different individual patients,” he said.
“The paradigm coming forward is the idea of residual risk that patients have after they been treated with the standard of care – which in most cases is a statin and blood pressure control – and what is driving that residual risk,” he noted. “If we think patients are still at high risk of recurrent cardiovascular events, we have to think what we will do next. This is where this drug will come in.”
Dr. Blaha pointed out that there are now multiple options for reducing residual risk; he believes that it will depend on the profile of the patient as to which of those options is chosen first.
“If after high-dose statin treatment they still have raised LDL, then we can add another LDL lowering drug; or it might be diabetes and obesity that we want to address first; or elevated triglycerides. But now, we can also consider residual inflammatory risk if we think the patient has residual plaque inflammation,” he said. “So, colchicine will be one of several choices beyond a statin that we can think about as the next step for treating residual risk.”
Is CRP measurement necessary?
Though elevated levels of high-sensitivity C-reactive protein (hsCRP) is a marker of inflammation in ASCVD, the two main trials of colchicine in ASCVD, both of which showed large benefits of the drug, did not measure hsCRP, leading to questions as to whether measurement of this biomarker is necessary to select patients for colchicine treatment.
“Some clinicians will favor testing hsCRP and treating those with levels above 2 mg/L. I think that’s very reasonable,” Dr. Blaha said. “However, because hsCRP was not measured in the trials, I don’t think testing for this biomarker is mandatory to establish that there is inflammation,” he added.
“The label does not stipulate that CRP has to be measured. It is giving physicians latitude; they can measure CRP, or they don’t have to.”
Dr. Blaha added that clinicians need to think about what is driving residual risk in each individual patient: “If you think their other risk factors are well controlled but they are still having recurrent events, then we can consider colchicine as a way of reducing their residual risk which is likely being caused by inflammation.
“We are at a great place in cardiovascular medicine as we have several different options to use after a statin, and now we have this new therapy targeted at inflammation as well. While we can use all these options together, I think most clinicians will want to prioritize therapies by using the ones that they believe will reduce the residual risk the most in each individual patient,” Dr. Blaha explained.
‘An entire other axis driving atherosclerosis’
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, is one of the major players in the cardiovascular inflammation field and has helped develop hsCRP testing. He has similar views.
“This FDA approval is extremely important, as it will draw attention to the role of inflammation in atherosclerosis and the need to treat it,” he said.
“Physicians need to be aware that, yes, we need to lower cholesterol aggressively, but they also need to know that there is an entire other axis driving atherosclerosis – and that is inflammation. And until now, we haven’t had an FDA-approved drug to treat inflammation.”
Dr. Ridker stressed that he doesn’t want to undermine lowering lipids: “Therapies aimed at inflammation are not in competition with those aimed at lipid lowering. We know lipid lowering works. But now we have another approach as well. The challenge here is educating physicians on this new approach.”
Dr. Ridker said he already uses low-dose colchicine for patients whom he refers to as “frequent flyers”; those who keep coming back despite aggressive lipid lowering. “They have multiple angioplasties, bypass surgery, etc.”
Like Dr. Blaha, Dr. Ridker thinks that doctors should start using this drug in high-risk patients who are already on a statin and who have residual inflammatory risk: “[The] patient whose underlying biologic problem is inflammation [is whom] we really want to treat with this drug. That is where it is most likely to be highly effective and where the comfort level will be the greatest.”
He said that measurement of hsCRP is an appropriate way to select these patients.
“I think this is a great impetus to start having much wider CRP measurement so we can actually target this anti-inflammatory drug to the patients with residual inflammatory risk – those with hsCRP level above 2 mg/L,” he said, estimating that this could apply to around 30%-40% of patients with ASCVD who are already taking a statin.
A second pillar of ASCVD treatment?
A somewhat different view is held by Jean-Claude Tardif, MD, director of the Research Centre at the Montréal Heart Institute, Canada, who was the lead investigator of the other randomized controlled trial of colchicine in heart disease, the COLCOT trial.
He said that colchicine should become the “second pillar” of ASCVD treatment, along with statins, for almost all patients.
Tardif referred to the recent study (led by Dr. Ridker) in The Lancet, which showed that among patients who are already on a statin, those with high inflammation levels had the highest risk for future events.
“So, the next step after a statin has to be to consider inflammation reduction,” he said.
“Despite all the drugs we have, ASCVD remains the leading cause of death in the Western world. What drives these events is largely inflammation, so it makes sense to directly tackle reduction of inflammation in the vessel, with a drug like colchicine,” he noted.
“I would say all patients with coronary atherosclerosis are potential candidates for low-dose colchicine as long as they do not have severe kidney disease, which is a contraindication,” Dr. Tardif said.
“If you want to fine tune this a bit more, those that are at particular risk are those that have recurrent events, those with multiple risk factors, and those with a recent [myocardial infarction]. In these patients, it would make a lot of sense to add low-dose colchicine to high-dose statins,” he added.
Dr. Tardif said he is not going to use CRP measurements to select patients for colchicine treatment: “Although measuring CRP may make sense intuitively, both large, randomized trials of colchicine did not select patients based on raised CRP, and they showed a benefit across the board.
If I consider a patient with ASCVD to be at high risk of future events and they are already on a statin I’m going to consider colchicine in all these patients, as long as they don’t have severe kidney disease.”
Dr. Tardif said that ASCVD needs to follow the model of heart failure which has several pillars of treatment directed at different targets that are all used together.
“I think we should apply the same approach to patients with ASCVD,” he added. “Yes, we need to hit the cholesterol with a statin, but we can now also hit the inflammation with colchicine.”
Polypharmacy concerns
Steve Nissen, MD, professor of medicine at the Cleveland Clinic, who was not involved in the colchicine trials, is also enthusiastic about use of colchicine. But like Dr. Ridker and Dr. Blaha, he favors selecting patients who are likely to benefit the most.
“I have been an advocate of the inflammatory hypothesis for many years, and we have been on a quest for a pure anti-inflammatory therapy that we can add to the standard treatment of patients with coronary disease. And colchicine has the safety and efficacy to do this,” Dr. Nissen said.
“What colchicine offers here is an inexpensive drug with pretty good data on reduction in morbidity from coronary disease. It has a completely different mechanism, so its benefit is likely to be additive to statins. I think we could probably do a lot of good at very little expense by just using these two therapies,” he said.
“But at present my preference will be to use colchicine selectively in those with raised CRP. I think that’s logical. I’m just worried about polypharmacy. Some of my patients are already on five, six, or seven meds. I need to have a reason to add an additional drug, and I’m not sure if we really analyze this carefully that patients with a low CRP would derive the same benefit. They might do, but I doubt it,” he noted.
“There may be further research and analyses that help us understand the relationship between CRP and efficacy of colchicine, and that may help us figure this out,” he added.
Safety is reassuring
In terms of safety and tolerability of the 0.5-mg colchicine dose, the experts seem to think that this is very manageable.
“When used for gout or pericarditis, colchicine is generally given at a dose of 0.6 mg twice a day and this can cause a lot of gastrointestinal [GI] side effects,” Dr. Nissen said. “But the low dose approved for ASCVD – 0.5 mg once a day – appears to be much better tolerated. There are some GI side effects, but these are not intolerable, and they generally go away with time.”
Dr. Ridker added that in the randomized trials, the adverse effects were “quite minimal,” but, “that being said, this drug is not to be used in severe kidney or liver disease, and there are some drug interactions that we need to be aware of. But in general, side effects are rare with the low dose. There may be some GI effects but they are mainly mild and you can generally treat through them.”
Dr. Blaha agreed that this is not a drug for patients with advanced kidney disease, “and there are some drug interactions that we have to be mindful of, but the list is not so long. There is a signal of modest gastrointestinal and muscle side effects, but most patients will be able to take it without issues. Because it’s already used in gout, physicians are already quite comfortable with its use.”
Part of the backbone of CV treatment?
Concluding, Dr. Blaha said he believes that prescribing of colchicine will start with cardiologists who will use it in their highest-risk patients first.
“But as we become comfortable with it, I think we will start using it in a broader range of patients and eventually primary care doctors will start prescribing it – much like what has happened with the statins,” he suggested.
“Where it sits along with statins in the future will be very interesting to see, but I think some people can envision it being up there with statins as part of the backbone of cardiovascular treatment in future.”
Dr. Tardif holds patents on methods for using low-dose colchicine after myocardial infarction, licensed to Montreal Heart Institute. Dr. Ridker is a consultant to Agepha and has research grants from Novo Nordisk related to the development of alternative anti-inflammatory therapies for atherosclerotic disease. Dr. Blaha reports being an unpaid scientific adviser to Agepha Pharma.
A version of this article first appeared on Medscape.com.
Drugmakers are abandoning cheap generics, and now U.S. cancer patients can’t get meds
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Observation recommended as first-line therapy in select cases of primary spontaneous pneumothorax
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
Observation should be considered the first-line treatment of choice in appropriately selected primary spontaneous pneumothorax patients, according to a review comparing observation alone with aspiration or chest tube placement.
Observation was the dominant choice, based on economic modeling showing it to offer both the highest utility and the lowest cost, according to the review, published in CHEST, which encompassed 20 years of relevant publications.
, Gilgamesh Eamer, MD, MSc, FRCSC, of Children’s Hospital of Eastern Ontario, Ottawa, and colleagues wrote. They pointed to recent studies suggesting equivalent or improved outcomes with simple observation in appropriately selected patients. The authors asked, “What management strategy derives the most utility for patients given the cost and morbidity of chest tube placement, hospital admission, surgical intervention and the risk of recurrence of primary spontaneous pneumothorax.”
Primary spontaneous pneumothorax, which leads to progressive pulmonary collapse and respiratory compromise, is thought to be attributable to rupture of air-containing blisters (or bullae) formed under the visceral pleura of the lung, according to the researchers. They stated that, while prior systematic reviews have examined various primary spontaneous pneumothorax management techniques, no reviews encompass more recently published high-quality studies comparing aspiration to other interventions such as observation or Heimlich valve devices.
The authors identified 22 articles for systematic review and meta-analysis after screening an initial list of 5,179 potentially relevant articles (Jan. 1, 2000 to April 10, 2020). They compared observation, needle aspiration, and chest tube placement, and created an economic model for these three treatment pathways based on Canadian medical cost data. The primary outcome measure was resolution following the initial intervention. Secondary outcomes included primary spontaneous pneumothorax recurrence, length of hospital stay, and treatment complications.
The analysis revealed that, compared with observation, chest tube and aspiration had higher resolution without additional intervention (relative risk for chest tube, 0.81; P < .01; RR for aspiration, 0.73; P < .01). Compared with a chest tube, observation and aspiration had shorter length of stay (mean difference for observation, 5.17; P < .01): (MD for aspiration, 2.72; P < .01).
Two-year recurrence rates did not differ between management strategies. Cost utility modeling found a cost of $14,658 (Canadian dollars [CAD] with 1.2535 = 1 US dollar) for chest tube placement, $13,126 CAD for aspiration, and $6,408 CAD for observation.
The utility (a measure including both quantity and quality of life) for each management arm was 0.77 for CT placement, 0.79 for aspiration, and 0.82 for observation. “The observation arm dominates the other two arms meaning it results in a more desirable (higher) utility with lower cost and results in a negative ICER [incremental cost-effectiveness ratio],” the authors stated.
They observed further that it is not typical for a medical intervention to improve patient outcomes, compared with standard care, and at the same time to bring costs down. “Given this, and the increasing evidence that observation is safe and effective in appropriately selected patients presenting with primary spontaneous pneumothorax,” they concluded that “observation should be considered in all patients presenting with primary spontaneous pneumothorax who meet predefined criteria.” They added that, because aspiration is favored over chest tube placement, it should be considered second-line therapy in well-selected primary spontaneous pneumothorax patients presenting with recurrence or who have failed a trial of observation.
“This review sheds light on ‘less is better’ for primary spontaneous pneumothorax management,” commented Dharani K. Narendra, MD, of the department of medicine, Baylor College of Medicine, Houston. “It allows clinicians to utilize a ‘wait approach’ versus invasive treatment. Interestingly, recurrence was lower in the observation group.” She said further, in an interview, “In general we assume that if no intervention is done, there is higher chance of recurrence. However, this meta-analysis reveals that is not the case; there is no difference in recurrence of pneumothorax in all groups and fewer complications in the observation group. The invasive treatments such as aspiration or chest tube are risky as they have more complications like pain, bleeding, injury to surrounding structures, etc.”
Neither Dr. Eamer nor Dr. Narendra reported any conflicts of interest. The study was self-funded.
FROM CHEST
Proteomics reveals potential targets for drug-resistant TB
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
TOPLINE:
Downregulation of plasma exosome-derived apolipoproteins APOA1, APOB, and APOC1 indicates DR-TB status and lipid metabolism regulation in pathogenesis.
METHODOLOGY:
Group case-controlled study assessed 17 drug resistant tuberculosis (DR-TB) and 33 non–drug resistant TB (NDR-TB) patients at The Fourth People’s Hospital of Taiyuan, China, from November 2018 to March 2019.
Plasma exosome purity and quality was determined by transmission electron microscopy, nanoparticle tracking analysis, and Western blot markers.
Proteins purified from plasma exosomes were characterized by SDS-Page with Western blotting and liquid chromatography coupled with tandem mass spectrometry techniques.
Functional proteomic differential analysis was achieved using the UniProt-GOA, Kyoto Encyclopedia of Genes and Genomes (KEGG), and STRING databases.
TAKEAWAYS:
DR-TB patients tended to be older than NDR-TB patients.
Isolated plasma exosomes were morphologically characterized as being “close to pure.”
Differential gene expression analysis revealed 16 upregulated and 10 downregulated proteins from DR-TB compared with NDR-TB patient-derived plasma exosomes.
through their functions in lipid metabolism and protein transport.
IN PRACTICE:
Key apolipoproteins “may be involved in the pathogenesis of DR-TB via accelerating the formation of foamy macrophages and reducing the cellular uptake of anti-TB drugs.”
STUDY DETAILS:
The study led by Mingrui Wu of Shanxi (China) Medical University and colleagues was published in the July 2023 issue of Tuberculosis.
LIMITATIONS:
This study is limited by an enrollment bias of at least twice as many men to women patients for both DR-TB and NDR-TB categories, reporting of some incomplete data collection characterizing the study population, and small sample size, which did not permit stratified analysis of the five types of DR-TB.
DISCLOSURES:
The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New tool uses nanotechnology to speed up diagnostic testing of infectious disease
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new tool promises to expedite detection of infectious disease, according to researchers from McGill University, Montreal.
The diagnostic platform, called The device was tested for several respiratory viruses and bacteria, including the H1N1 influenza virus and SARS-CoV-2. It achieved 95% accuracy at identifying COVID-19 and its variants in 48 human saliva samples.
“COVID was something that opened our eyes, and now we have to think more seriously about point-of-care diagnostics,” Sara Mahshid, PhD, assistant professor of biomedical engineering and Canada Research Chair in Nano-Biosensing Devices at McGill University, said in an interview. The technology could become important for a range of medical applications, especially in low-resource areas.
The development was detailed in an article in Nature Nanotechnology.
Nonclinical setting
The COVID-19 pandemic has demonstrated the need for fast and accurate testing that can be used outside of a clinical setting. The gold-standard diagnostic method is PCR testing, but its accuracy comes with a trade-off. PCR testing involves a lengthy protocol and requires a centralized testing facility.
With QolorEX, the investigators aimed to develop a new test that achieves the accuracy of PCR in an automated tool that can be used outside of a testing facility or hospital setting. Dr. Mahshid noted a particular need for a tool that could be used in congregate settings, such as airports, schools, or restaurants.
The device is compact enough to sit on a tabletop or bench and can be used easily in group settings, according to Dr. Mahshid. In the future, she hopes to further miniaturize the device to make it more scalable for widespread use.
Requiring only a saliva sample, the tool is easy to use. Unlike current COVID-19 rapid tests, which involve several steps, the system is automated and does not require manually mixing reagents. After collecting a sample, a user taps a button in a smartphone or computer application. The device handles the rest.
“We’re not chemists who understand how to mix these solutions,” Dr. Mahshid said. Avoiding those extra steps may reduce the false positives and false negatives caused by user error.
Fast results
QolorEX can return results in 13 minutes, like a rapid antigen test does. Like a PCR test, the device uses nucleic acid amplification. But PCR tests typically take much longer. The sample analysis alone takes 1.5-2 hours.
The new test accelerates the reaction by injecting light-excited “hot” electrons from the surface of a nanoplasmonic sensor. The device then uses imaging and a machine learning algorithm to quantify a color transformation that occurs when a pathogen is present.
The fast, reliable results make the system potentially appropriate for use in places such as airports. Previously, passengers had to wait 24 hours for a negative COVID test before boarding a plane. A device such as QolorEX would allow screening on site.
The ability of the tool to distinguish between bacterial and viral infections so quickly is “an application that is both important and extremely difficult to achieve,” according to Nikhil Bhalla, PhD, in a research briefing. Dr. Bhalla is a lecturer in electronic engineering at Ulster University, Belfast, Ireland.
The researchers hope that by delivering results quickly, the device will help reduce the spread of respiratory diseases and possibly save lives.
‘Sensitive and specific’
The primary benefit of the tool is its ability to return results quickly while having low false positive and false negative rates, according to Leyla Soleymani, PhD, of McMaster University, Hamilton, Ont. “It is hard to come by rapid tests that are both sensitive and specific, compared to PCR,” Dr. Soleymani told this news organization.
Although QolorEX was developed to detect COVID-19 and other infectious diseases, the uses of the device are not limited to the pathogens tested. The tool can be applied to a range of tests that currently use PCR technology. Dr. Mahshid and her team are considering several other applications of the technology, such as analyzing therapeutics for antimicrobial-resistant pathogens prioritized by the World Health Organization. The technology may also have potential for detecting cancer and bacterial infections, Dr. Mahshid said in an interview.
But to Dr. Soleymani, the most exciting application remains its use in diagnosing infectious diseases. She noted, however, that it’s unclear whether the price of the device will be too high for widespread home use. It may be more practical for family physician clinics and other facilities.
Before the device becomes commercially available, more testing is needed to validate the results, which are based on a limited number of samples that were available in a research setting.
The study was supported by the MI4 Emergency COVID-19 Research Funding, Natural Sciences and Engineering Research Council of Canada, Canadian Institutes of Health Research, Canada Foundation for Innovation, and McGill University. Dr. Mahshid and Dr. Soleymani reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NATURE NANOTECHNOLOGY