User login
These amniotic biomarkers predicted pPROM in women undergoing fetal surgery for spinal cord defect
DALLAS – Two molecular biomarkers in amniotic fluid seem to predict preterm premature rupture of membranes (pPROM) and subsequent premature delivery in women whose fetuses undergo surgical repair of spinal cord defects.
Matrix metalloproteinase–8 (MMP-8) and lactic acid levels were significantly higher in these women than in a comparator group of women who did not deliver a premature infant after the repair, Aikaterini Athanasiou, MD, said at the meeting sponsored by the Society for Maternal Fetal Medicine.
“Based on this pilot study, it appears that elevated amniotic levels of lactic acid and MMP-8 at time of surgery might identify a subset of women with increased susceptibility for pPROM and shorter time to delivery,” said Dr. Athanasiou, a fellow in obstetrics and gynecology at Cornell University, New York. She presented the work on behalf of primary author Antonio Moron, MD, PhD, of the Federal University of São Paulo.
Dr. Athanasiou was part of the Cornell team that conducted molecular assays on amniotic fluid samples drawn from 26 women carrying fetuses about to have corrective surgery for spinal defects in the fetuses. The women were all patients at the Federal Hospital of São Paulo. Samples were drawn immediately before surgery commenced, frozen, and shipped to Cornell for assay.
After surgical repair, 7 of the women (27%) later experienced pPROM and 19 did not.
At baseline, there were no significant differences between the groups. Women were a mean age of 32 years, with a mean of two prior pregnancies. There were no differences in prior cesarean and vaginal births, smoking status, and fetal gender. The defect was most commonly a myelomeningocele (about 70% of each group). Rachischisis was next most common, occurring in 27% of the pPROM group and 21% of the non-pPROM group. There were two cases of encephalocele, both in the non-pPROM group.
The length of surgery was not significantly different between those who experienced pPROM and those who did not (121 vs. 130 minutes). Wound healing time was 7 days for each group, as was the mean length of hospital stay.
Both groups went a mean of 57 days from surgery to delivery, although the fetal gestational age was almost a week younger in the pPROM group (33.7 vs. 34.4 weeks). These infants were also smaller at birth (2,247 g vs. 2,410 g).
The Cornell team examined five potential biomarkers in each amniotic fluid sample: MMP-8, MMP-9, MMP-2, lactic acid, and interleukin-6 (IL-6). The levels of IL-6, MMP-2, and MMP-9 were similar between groups.
However, lactic acid was significantly higher in the pPROM group (7.1 vs. 5.9 mU/mL). MMP-8 was also significantly elevated in the pPROM group (1.7 vs. 0.6 mcg/mL).
Dr. Athanasiou and her colleagues also observed an inverse relationship between MMP-8 levels and gestational age at delivery, which was statistically significant. There was also an inverse relationship between lactic acid levels and gestational age, but this did not reach statistical significance.
“While further investigations are needed to verify our findings, our data suggest that these differences are present before fetal surgery and that an increase in intra-amniotic anaerobic glycolysis as evidenced by elevated lactic acid may enhance MMP-8 production, which will weaken the maternal-fetal membranes,” Dr. Athanasiou said. “The mechanism may not be related to inflammation, as evidenced by the lack of association between pPROM and IL-6.”
She had no financial disclosures.
SOURCE: Moron A et al. Am J Obstet Gynecol. 2018 Jan:218(1);S64.
DALLAS – Two molecular biomarkers in amniotic fluid seem to predict preterm premature rupture of membranes (pPROM) and subsequent premature delivery in women whose fetuses undergo surgical repair of spinal cord defects.
Matrix metalloproteinase–8 (MMP-8) and lactic acid levels were significantly higher in these women than in a comparator group of women who did not deliver a premature infant after the repair, Aikaterini Athanasiou, MD, said at the meeting sponsored by the Society for Maternal Fetal Medicine.
“Based on this pilot study, it appears that elevated amniotic levels of lactic acid and MMP-8 at time of surgery might identify a subset of women with increased susceptibility for pPROM and shorter time to delivery,” said Dr. Athanasiou, a fellow in obstetrics and gynecology at Cornell University, New York. She presented the work on behalf of primary author Antonio Moron, MD, PhD, of the Federal University of São Paulo.
Dr. Athanasiou was part of the Cornell team that conducted molecular assays on amniotic fluid samples drawn from 26 women carrying fetuses about to have corrective surgery for spinal defects in the fetuses. The women were all patients at the Federal Hospital of São Paulo. Samples were drawn immediately before surgery commenced, frozen, and shipped to Cornell for assay.
After surgical repair, 7 of the women (27%) later experienced pPROM and 19 did not.
At baseline, there were no significant differences between the groups. Women were a mean age of 32 years, with a mean of two prior pregnancies. There were no differences in prior cesarean and vaginal births, smoking status, and fetal gender. The defect was most commonly a myelomeningocele (about 70% of each group). Rachischisis was next most common, occurring in 27% of the pPROM group and 21% of the non-pPROM group. There were two cases of encephalocele, both in the non-pPROM group.
The length of surgery was not significantly different between those who experienced pPROM and those who did not (121 vs. 130 minutes). Wound healing time was 7 days for each group, as was the mean length of hospital stay.
Both groups went a mean of 57 days from surgery to delivery, although the fetal gestational age was almost a week younger in the pPROM group (33.7 vs. 34.4 weeks). These infants were also smaller at birth (2,247 g vs. 2,410 g).
The Cornell team examined five potential biomarkers in each amniotic fluid sample: MMP-8, MMP-9, MMP-2, lactic acid, and interleukin-6 (IL-6). The levels of IL-6, MMP-2, and MMP-9 were similar between groups.
However, lactic acid was significantly higher in the pPROM group (7.1 vs. 5.9 mU/mL). MMP-8 was also significantly elevated in the pPROM group (1.7 vs. 0.6 mcg/mL).
Dr. Athanasiou and her colleagues also observed an inverse relationship between MMP-8 levels and gestational age at delivery, which was statistically significant. There was also an inverse relationship between lactic acid levels and gestational age, but this did not reach statistical significance.
“While further investigations are needed to verify our findings, our data suggest that these differences are present before fetal surgery and that an increase in intra-amniotic anaerobic glycolysis as evidenced by elevated lactic acid may enhance MMP-8 production, which will weaken the maternal-fetal membranes,” Dr. Athanasiou said. “The mechanism may not be related to inflammation, as evidenced by the lack of association between pPROM and IL-6.”
She had no financial disclosures.
SOURCE: Moron A et al. Am J Obstet Gynecol. 2018 Jan:218(1);S64.
DALLAS – Two molecular biomarkers in amniotic fluid seem to predict preterm premature rupture of membranes (pPROM) and subsequent premature delivery in women whose fetuses undergo surgical repair of spinal cord defects.
Matrix metalloproteinase–8 (MMP-8) and lactic acid levels were significantly higher in these women than in a comparator group of women who did not deliver a premature infant after the repair, Aikaterini Athanasiou, MD, said at the meeting sponsored by the Society for Maternal Fetal Medicine.
“Based on this pilot study, it appears that elevated amniotic levels of lactic acid and MMP-8 at time of surgery might identify a subset of women with increased susceptibility for pPROM and shorter time to delivery,” said Dr. Athanasiou, a fellow in obstetrics and gynecology at Cornell University, New York. She presented the work on behalf of primary author Antonio Moron, MD, PhD, of the Federal University of São Paulo.
Dr. Athanasiou was part of the Cornell team that conducted molecular assays on amniotic fluid samples drawn from 26 women carrying fetuses about to have corrective surgery for spinal defects in the fetuses. The women were all patients at the Federal Hospital of São Paulo. Samples were drawn immediately before surgery commenced, frozen, and shipped to Cornell for assay.
After surgical repair, 7 of the women (27%) later experienced pPROM and 19 did not.
At baseline, there were no significant differences between the groups. Women were a mean age of 32 years, with a mean of two prior pregnancies. There were no differences in prior cesarean and vaginal births, smoking status, and fetal gender. The defect was most commonly a myelomeningocele (about 70% of each group). Rachischisis was next most common, occurring in 27% of the pPROM group and 21% of the non-pPROM group. There were two cases of encephalocele, both in the non-pPROM group.
The length of surgery was not significantly different between those who experienced pPROM and those who did not (121 vs. 130 minutes). Wound healing time was 7 days for each group, as was the mean length of hospital stay.
Both groups went a mean of 57 days from surgery to delivery, although the fetal gestational age was almost a week younger in the pPROM group (33.7 vs. 34.4 weeks). These infants were also smaller at birth (2,247 g vs. 2,410 g).
The Cornell team examined five potential biomarkers in each amniotic fluid sample: MMP-8, MMP-9, MMP-2, lactic acid, and interleukin-6 (IL-6). The levels of IL-6, MMP-2, and MMP-9 were similar between groups.
However, lactic acid was significantly higher in the pPROM group (7.1 vs. 5.9 mU/mL). MMP-8 was also significantly elevated in the pPROM group (1.7 vs. 0.6 mcg/mL).
Dr. Athanasiou and her colleagues also observed an inverse relationship between MMP-8 levels and gestational age at delivery, which was statistically significant. There was also an inverse relationship between lactic acid levels and gestational age, but this did not reach statistical significance.
“While further investigations are needed to verify our findings, our data suggest that these differences are present before fetal surgery and that an increase in intra-amniotic anaerobic glycolysis as evidenced by elevated lactic acid may enhance MMP-8 production, which will weaken the maternal-fetal membranes,” Dr. Athanasiou said. “The mechanism may not be related to inflammation, as evidenced by the lack of association between pPROM and IL-6.”
She had no financial disclosures.
SOURCE: Moron A et al. Am J Obstet Gynecol. 2018 Jan:218(1);S64.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Lactic acid and MMP-8 in amniotic fluid may have utility as biomarkers predictive of pPROM in women who undergo fetal surgery for spinal cord defects.
Major finding: Women who experienced pPROM had higher amniotic lactic acid (7.1 vs. 5.9 mU/mL) and MMP-8 (1.7 vs. 0.6 mcg/mL) at time of fetal surgery.
Study details: The prospective study comprised 26 women.
Disclosures: Dr. Athanasiou had no financial disclosures.
Source: Moron A et al. Am J Obstet Gynecol. 2018 Jan:218(1);S64.
Ibuprofen appears safe with preeclampsia, study says
DALLAS – Compared to acetaminophen, ibuprofen does not prolong the time needed to control postpartum hypertension in women who experience preeclampsia with severe features, Nathan Blue MD, reported at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine.
Ibuprofen did not exacerbate postpartum hypertension, as some studies have suggested, and women randomized to it for postpartum pain control reached their target blood pressure at a mean of 35 hours after delivery, similar to the 38 hours needed among women receiving acetaminophen.
Dr. Blue’s findings contradict the recommendation by the American College of Obstetricians and Gynecologists to avoid the use of ibuprofen and other nonsteroidal anti-inflammatory drugs (NSAIDs) for pain control in women who experience preeclampsia or other hypertensive disorders of pregnancy.
“While our study was not meant to answer all questions about the potential problems of nonsteroidal anti-inflammatories [in this population], I would conclude from these results that providers and patients can make a decision together and feel good about the use of NSAIDs,” in the presence of postpartum hypertension, said Dr. Blue, a fellow at the University of New Mexico, Albuquerque.
These concerns led ACOG to issue its recommendation in 2013 against the use of NSAIDs in pregnant women with hypertension.
“This is problematic, because NSAIDs are particularly well-suited to address obstetric pain,” Dr. Blue said at the meeting. “They have been shown to be better than acetaminophen for perineal injury and they are associated with a reduced use of opioids after cesarean section.”
To investigate the effect of ibuprofen on postpartum hypertension, Dr. Blue and his colleagues conducted a double-blind randomized controlled trial of 100 women with preeclampsia with severe features. The study population also included women who had chronic hypertension complicated by preeclampsia with severe features, and women with HELLP syndrome – a constellation of hemolysis, elevated liver enzymes, and low platelet count.
Women were randomized to either 600 mg ibuprofen or 650 mg acetaminophen every 6 hours, around the clock, with the first dose delivered within 6 hours of delivery. All patients received at least eight doses of their assigned medication. The primary endpoint was the time required to achieve blood pressure control. “We defined blood pressure control as the number of hours from delivery to the last reading of at least 160/110 mm Hg before discharge,” Dr. Blue said. “Our rationale here was that persistence of a blood pressure of that level would require a delay in discharge of at least 24 hours.”
The study had a number of secondary outcomes, including time from delivery to last blood pressure reading of at least 150/100 mm Hg; postpartum mean arterial pressure; any blood pressure reading of 160/110 mm Hg or higher; need for antihypertensive drugs at discharge; prolongation of hospital stay due to hypertension; and the need for postpartum opioids.
There was a 6-week follow-up assessment, at which time women reported any continued antihypertensive or opioid use, obstetrical triage visits after discharge, and hospital readmission.
The study cohort was well-balanced at baseline. Women were a mean of 30 years old; about a third were nulliparous, and half had a vaginal delivery. Chronic hypertension requiring medication was present in about 15%. The maximum blood pressure before delivery was about 180/107.
There was no significant difference between the ibuprofen group and the acetaminophen group in the primary endpoint of time to blood pressure of 160/110 mm Hg or below (35.3 vs. 38 hours). Nor were there significant differences in any of the secondary endpoints, including time to achieve a blood pressure of less than 150/100 mm Hg (58 vs. 57 hours), postpartum mean arterial pressure, maximum systolic and diastolic blood pressures, or the number of women who needed a short-acting antihypertensive (30 vs. 26) and who went home on an antihypertensive (33 vs. 31).
There were also no significant between-group differences in opioid use, either on postpartum days 0, 1, or 2. The total morphine equivalent dose for each group was likewise not significantly different (77 vs. 88 mg).
Dr. Blue was able to contact 77 women at 6 weeks’ postpartum. He found that 6-week outcomes were also similar. There were no significant differences in the number who required continuing antihypertensive or opioids, no difference in obstetric triage visits, and no difference in hospital readmission.
“Our study does not support the hypothesis that NSAIDs adversely affect blood pressure control in patients with preeclampsia,” he said. “Not only did we not find a difference in the primary outcome, we found not even a suggestion of difference in any measure of blood pressure control.”
The University of New Mexico sponsored the study. Dr. Blue reported having no financial disclosures.
SOURCE: Blue et al. The Pregnancy Meeting 2018 Abstract LB04.
DALLAS – Compared to acetaminophen, ibuprofen does not prolong the time needed to control postpartum hypertension in women who experience preeclampsia with severe features, Nathan Blue MD, reported at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine.
Ibuprofen did not exacerbate postpartum hypertension, as some studies have suggested, and women randomized to it for postpartum pain control reached their target blood pressure at a mean of 35 hours after delivery, similar to the 38 hours needed among women receiving acetaminophen.
Dr. Blue’s findings contradict the recommendation by the American College of Obstetricians and Gynecologists to avoid the use of ibuprofen and other nonsteroidal anti-inflammatory drugs (NSAIDs) for pain control in women who experience preeclampsia or other hypertensive disorders of pregnancy.
“While our study was not meant to answer all questions about the potential problems of nonsteroidal anti-inflammatories [in this population], I would conclude from these results that providers and patients can make a decision together and feel good about the use of NSAIDs,” in the presence of postpartum hypertension, said Dr. Blue, a fellow at the University of New Mexico, Albuquerque.
These concerns led ACOG to issue its recommendation in 2013 against the use of NSAIDs in pregnant women with hypertension.
“This is problematic, because NSAIDs are particularly well-suited to address obstetric pain,” Dr. Blue said at the meeting. “They have been shown to be better than acetaminophen for perineal injury and they are associated with a reduced use of opioids after cesarean section.”
To investigate the effect of ibuprofen on postpartum hypertension, Dr. Blue and his colleagues conducted a double-blind randomized controlled trial of 100 women with preeclampsia with severe features. The study population also included women who had chronic hypertension complicated by preeclampsia with severe features, and women with HELLP syndrome – a constellation of hemolysis, elevated liver enzymes, and low platelet count.
Women were randomized to either 600 mg ibuprofen or 650 mg acetaminophen every 6 hours, around the clock, with the first dose delivered within 6 hours of delivery. All patients received at least eight doses of their assigned medication. The primary endpoint was the time required to achieve blood pressure control. “We defined blood pressure control as the number of hours from delivery to the last reading of at least 160/110 mm Hg before discharge,” Dr. Blue said. “Our rationale here was that persistence of a blood pressure of that level would require a delay in discharge of at least 24 hours.”
The study had a number of secondary outcomes, including time from delivery to last blood pressure reading of at least 150/100 mm Hg; postpartum mean arterial pressure; any blood pressure reading of 160/110 mm Hg or higher; need for antihypertensive drugs at discharge; prolongation of hospital stay due to hypertension; and the need for postpartum opioids.
There was a 6-week follow-up assessment, at which time women reported any continued antihypertensive or opioid use, obstetrical triage visits after discharge, and hospital readmission.
The study cohort was well-balanced at baseline. Women were a mean of 30 years old; about a third were nulliparous, and half had a vaginal delivery. Chronic hypertension requiring medication was present in about 15%. The maximum blood pressure before delivery was about 180/107.
There was no significant difference between the ibuprofen group and the acetaminophen group in the primary endpoint of time to blood pressure of 160/110 mm Hg or below (35.3 vs. 38 hours). Nor were there significant differences in any of the secondary endpoints, including time to achieve a blood pressure of less than 150/100 mm Hg (58 vs. 57 hours), postpartum mean arterial pressure, maximum systolic and diastolic blood pressures, or the number of women who needed a short-acting antihypertensive (30 vs. 26) and who went home on an antihypertensive (33 vs. 31).
There were also no significant between-group differences in opioid use, either on postpartum days 0, 1, or 2. The total morphine equivalent dose for each group was likewise not significantly different (77 vs. 88 mg).
Dr. Blue was able to contact 77 women at 6 weeks’ postpartum. He found that 6-week outcomes were also similar. There were no significant differences in the number who required continuing antihypertensive or opioids, no difference in obstetric triage visits, and no difference in hospital readmission.
“Our study does not support the hypothesis that NSAIDs adversely affect blood pressure control in patients with preeclampsia,” he said. “Not only did we not find a difference in the primary outcome, we found not even a suggestion of difference in any measure of blood pressure control.”
The University of New Mexico sponsored the study. Dr. Blue reported having no financial disclosures.
SOURCE: Blue et al. The Pregnancy Meeting 2018 Abstract LB04.
DALLAS – Compared to acetaminophen, ibuprofen does not prolong the time needed to control postpartum hypertension in women who experience preeclampsia with severe features, Nathan Blue MD, reported at the Pregnancy Meeting, sponsored by the Society for Maternal-Fetal Medicine.
Ibuprofen did not exacerbate postpartum hypertension, as some studies have suggested, and women randomized to it for postpartum pain control reached their target blood pressure at a mean of 35 hours after delivery, similar to the 38 hours needed among women receiving acetaminophen.
Dr. Blue’s findings contradict the recommendation by the American College of Obstetricians and Gynecologists to avoid the use of ibuprofen and other nonsteroidal anti-inflammatory drugs (NSAIDs) for pain control in women who experience preeclampsia or other hypertensive disorders of pregnancy.
“While our study was not meant to answer all questions about the potential problems of nonsteroidal anti-inflammatories [in this population], I would conclude from these results that providers and patients can make a decision together and feel good about the use of NSAIDs,” in the presence of postpartum hypertension, said Dr. Blue, a fellow at the University of New Mexico, Albuquerque.
These concerns led ACOG to issue its recommendation in 2013 against the use of NSAIDs in pregnant women with hypertension.
“This is problematic, because NSAIDs are particularly well-suited to address obstetric pain,” Dr. Blue said at the meeting. “They have been shown to be better than acetaminophen for perineal injury and they are associated with a reduced use of opioids after cesarean section.”
To investigate the effect of ibuprofen on postpartum hypertension, Dr. Blue and his colleagues conducted a double-blind randomized controlled trial of 100 women with preeclampsia with severe features. The study population also included women who had chronic hypertension complicated by preeclampsia with severe features, and women with HELLP syndrome – a constellation of hemolysis, elevated liver enzymes, and low platelet count.
Women were randomized to either 600 mg ibuprofen or 650 mg acetaminophen every 6 hours, around the clock, with the first dose delivered within 6 hours of delivery. All patients received at least eight doses of their assigned medication. The primary endpoint was the time required to achieve blood pressure control. “We defined blood pressure control as the number of hours from delivery to the last reading of at least 160/110 mm Hg before discharge,” Dr. Blue said. “Our rationale here was that persistence of a blood pressure of that level would require a delay in discharge of at least 24 hours.”
The study had a number of secondary outcomes, including time from delivery to last blood pressure reading of at least 150/100 mm Hg; postpartum mean arterial pressure; any blood pressure reading of 160/110 mm Hg or higher; need for antihypertensive drugs at discharge; prolongation of hospital stay due to hypertension; and the need for postpartum opioids.
There was a 6-week follow-up assessment, at which time women reported any continued antihypertensive or opioid use, obstetrical triage visits after discharge, and hospital readmission.
The study cohort was well-balanced at baseline. Women were a mean of 30 years old; about a third were nulliparous, and half had a vaginal delivery. Chronic hypertension requiring medication was present in about 15%. The maximum blood pressure before delivery was about 180/107.
There was no significant difference between the ibuprofen group and the acetaminophen group in the primary endpoint of time to blood pressure of 160/110 mm Hg or below (35.3 vs. 38 hours). Nor were there significant differences in any of the secondary endpoints, including time to achieve a blood pressure of less than 150/100 mm Hg (58 vs. 57 hours), postpartum mean arterial pressure, maximum systolic and diastolic blood pressures, or the number of women who needed a short-acting antihypertensive (30 vs. 26) and who went home on an antihypertensive (33 vs. 31).
There were also no significant between-group differences in opioid use, either on postpartum days 0, 1, or 2. The total morphine equivalent dose for each group was likewise not significantly different (77 vs. 88 mg).
Dr. Blue was able to contact 77 women at 6 weeks’ postpartum. He found that 6-week outcomes were also similar. There were no significant differences in the number who required continuing antihypertensive or opioids, no difference in obstetric triage visits, and no difference in hospital readmission.
“Our study does not support the hypothesis that NSAIDs adversely affect blood pressure control in patients with preeclampsia,” he said. “Not only did we not find a difference in the primary outcome, we found not even a suggestion of difference in any measure of blood pressure control.”
The University of New Mexico sponsored the study. Dr. Blue reported having no financial disclosures.
SOURCE: Blue et al. The Pregnancy Meeting 2018 Abstract LB04.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point:
Major finding: The mean time to achieve postpartum blood pressure control was 35 hours in the ibuprofen group and 38 hours in the acetaminophen group.
Study details: The randomized study comprised 100 women.
Disclosures: The University of New Mexico sponsored the study. Dr. Blue reported having no financial disclosures.
Source: Blue N et al. The Pregnancy Meeting 2018 Abstract LB04.
Is elective induction at 39 weeks a good idea?
DALLAS – Elective inductions at 39 weeks’ gestation were safe for the newborn and conferred dual benefits upon first-time mothers, reducing the risk of cesarean delivery by 16% and pregnancy-related hypertensive disorder by 36%, compared with women managed expectantly.
Infants delivered by elective inductions were smaller than those born to expectantly managed women and experienced a 29% reduction in the need for respiratory support at birth, William A. Grobman, MD, reported at the meeting, sponsored by the Society for Maternal-Fetal Medicine. They were no more likely than infants in the comparator group to experience dangerous perinatal outcomes, including low Apgar scores, meconium inhalation, hypoxia, or birth trauma, said Dr. Grobman, professor of obstetrics and gynecology at Northwestern University, Chicago.
The new data, however, may set a new standard by which to make this decision, Dr. Grobman said.
“I will leave it up to the professional organizations to determine the final outcome of these data, but it’s important to understand that the Choosing Wisely recommendation was based on observational data that essentially used an incorrect clinical comparator” of spontaneous labor, he said. The large study that Dr. Grobman and his colleagues conducted used expectant management (EM) as the comparator, allowing women to continue up to 42 weeks’ gestation. Using this comparator, he said, “Our data are largely with almost every observational study” and with a recently published randomized controlled trial by Kate F. Walker, a clinical research fellow at the University of Nottingham (England).
That study determined that labor induction between 39 weeks and 39 weeks, 6 days, in women older than 35 years had no significant effect on the rate of cesarean section and no adverse short-term effects on maternal or neonatal outcomes.
Dr. Grobman conducted his randomized trial at 41 hospitals in the National Institutes of Health’s Maternal-Fetal Medicine Units Network.
It randomized 6,106 healthy, nulliparous women to either elective induction from 39 weeks to 39 weeks, 4 days, or to EM. These women were asked to forgo elective delivery before 40 weeks, 5 days, but to be delivered by 42 weeks, 2 days.
The primary perinatal outcome was a composite endpoint that included fetal or neonatal death; respiratory support in the first 72 hours; 5-minute Apgar of 3 or lower; hypoxic ischemic encephalopathy; seizure; infection; meconium aspiration syndrome; birth trauma; intracranial or subgaleal hemorrhage; and hypotension requiring vasopressors.
The primary maternal outcome was a composite of cesarean delivery; hypertensive disorder of pregnancy; postpartum hemorrhage; chorioamnionitis; postpartum infection; labor pain; and the Labour Agentry Scale, a midwife-created measure of a laboring woman’s perception of her birth experience.
Women were a mean of 23.5 years old; about 44% of each group was privately insured. Prior pregnancy loss was more common among those randomized to EM (25.6% vs. 22.8%). Just over half were obese, with a body mass index of at least 30 kg/m2. Most (about 63%) had an unfavorable cervix, with a Bishop score of less than 5. The trial specified no particular induction regimen, Dr. Grobman said. “There were a variety of ripening agents and oxytocin regimens used.”
Infants in the elective induction group were born significantly earlier than were those in the EM group (39.3 vs. 40 weeks) and weighed significantly less (3,300 g vs. 3,380 g). Induction was safe for the newborn, with the primary endpoint occurring in 4.4%, compared with 5.4% of those in the EM group – not significantly different.
When investigators examined each outcome in the perinatal composite individually, only one – early respiratory support – was significantly different from the EM group. Infants in the induction group were 29% less likely to need respiratory support in the first 72 hours (3% vs. 4.2%; relative risk, 0.71). The rate of cesarean delivery also was significantly less among the induction group (18.6% vs. 22.2%; RR, 0.84).
None of these outcomes changed when the investigators controlled for race/ethnicity, Bishop score of less than 5, body mass index of 30 kg/m2 or more, or advanced maternal age.
Induction also was safe for mothers, and conferred a significant 36% reduction in the risk of pregnancy-related hypertensive disorders (9.1% vs. 14.1%; RR, 0.64). All other maternal outcomes were similar between the two groups.
The Agentry scale results also showed that women who were induced felt they were more in control of their birth experience, both at delivery and at 6 weeks’ postpartum. They also rated their worst labor pain and overall labor pain as significantly less than did women in the EM group.
“Our result suggest that policies directed toward avoidance of elective labor induction in nulliparous women would be unlikely to reduce the rate of cesarean section on a population level,” Dr. Grobman said. “To the contrary, our data show that, for every 28 nulliparous women to undergo elective induction at 39 weeks, one cesarean section would be avoided. Additionally, the number needed to treat to prevent one case of neonatal respiratory support is 83, and to prevent one case of hypertensive disease of pregnancy, 20. Our results should provide information useful to women as they consider their options, and can be incorporated into shared decision-making discussions with the provider.”
The study was sponsored by the National Institutes of Health. Dr. Grobman had no financial disclosures.
SOURCE: Grobman W. Am J Obstet Gynecol. 2018 Jan;218:S601.
DALLAS – Elective inductions at 39 weeks’ gestation were safe for the newborn and conferred dual benefits upon first-time mothers, reducing the risk of cesarean delivery by 16% and pregnancy-related hypertensive disorder by 36%, compared with women managed expectantly.
Infants delivered by elective inductions were smaller than those born to expectantly managed women and experienced a 29% reduction in the need for respiratory support at birth, William A. Grobman, MD, reported at the meeting, sponsored by the Society for Maternal-Fetal Medicine. They were no more likely than infants in the comparator group to experience dangerous perinatal outcomes, including low Apgar scores, meconium inhalation, hypoxia, or birth trauma, said Dr. Grobman, professor of obstetrics and gynecology at Northwestern University, Chicago.
The new data, however, may set a new standard by which to make this decision, Dr. Grobman said.
“I will leave it up to the professional organizations to determine the final outcome of these data, but it’s important to understand that the Choosing Wisely recommendation was based on observational data that essentially used an incorrect clinical comparator” of spontaneous labor, he said. The large study that Dr. Grobman and his colleagues conducted used expectant management (EM) as the comparator, allowing women to continue up to 42 weeks’ gestation. Using this comparator, he said, “Our data are largely with almost every observational study” and with a recently published randomized controlled trial by Kate F. Walker, a clinical research fellow at the University of Nottingham (England).
That study determined that labor induction between 39 weeks and 39 weeks, 6 days, in women older than 35 years had no significant effect on the rate of cesarean section and no adverse short-term effects on maternal or neonatal outcomes.
Dr. Grobman conducted his randomized trial at 41 hospitals in the National Institutes of Health’s Maternal-Fetal Medicine Units Network.
It randomized 6,106 healthy, nulliparous women to either elective induction from 39 weeks to 39 weeks, 4 days, or to EM. These women were asked to forgo elective delivery before 40 weeks, 5 days, but to be delivered by 42 weeks, 2 days.
The primary perinatal outcome was a composite endpoint that included fetal or neonatal death; respiratory support in the first 72 hours; 5-minute Apgar of 3 or lower; hypoxic ischemic encephalopathy; seizure; infection; meconium aspiration syndrome; birth trauma; intracranial or subgaleal hemorrhage; and hypotension requiring vasopressors.
The primary maternal outcome was a composite of cesarean delivery; hypertensive disorder of pregnancy; postpartum hemorrhage; chorioamnionitis; postpartum infection; labor pain; and the Labour Agentry Scale, a midwife-created measure of a laboring woman’s perception of her birth experience.
Women were a mean of 23.5 years old; about 44% of each group was privately insured. Prior pregnancy loss was more common among those randomized to EM (25.6% vs. 22.8%). Just over half were obese, with a body mass index of at least 30 kg/m2. Most (about 63%) had an unfavorable cervix, with a Bishop score of less than 5. The trial specified no particular induction regimen, Dr. Grobman said. “There were a variety of ripening agents and oxytocin regimens used.”
Infants in the elective induction group were born significantly earlier than were those in the EM group (39.3 vs. 40 weeks) and weighed significantly less (3,300 g vs. 3,380 g). Induction was safe for the newborn, with the primary endpoint occurring in 4.4%, compared with 5.4% of those in the EM group – not significantly different.
When investigators examined each outcome in the perinatal composite individually, only one – early respiratory support – was significantly different from the EM group. Infants in the induction group were 29% less likely to need respiratory support in the first 72 hours (3% vs. 4.2%; relative risk, 0.71). The rate of cesarean delivery also was significantly less among the induction group (18.6% vs. 22.2%; RR, 0.84).
None of these outcomes changed when the investigators controlled for race/ethnicity, Bishop score of less than 5, body mass index of 30 kg/m2 or more, or advanced maternal age.
Induction also was safe for mothers, and conferred a significant 36% reduction in the risk of pregnancy-related hypertensive disorders (9.1% vs. 14.1%; RR, 0.64). All other maternal outcomes were similar between the two groups.
The Agentry scale results also showed that women who were induced felt they were more in control of their birth experience, both at delivery and at 6 weeks’ postpartum. They also rated their worst labor pain and overall labor pain as significantly less than did women in the EM group.
“Our result suggest that policies directed toward avoidance of elective labor induction in nulliparous women would be unlikely to reduce the rate of cesarean section on a population level,” Dr. Grobman said. “To the contrary, our data show that, for every 28 nulliparous women to undergo elective induction at 39 weeks, one cesarean section would be avoided. Additionally, the number needed to treat to prevent one case of neonatal respiratory support is 83, and to prevent one case of hypertensive disease of pregnancy, 20. Our results should provide information useful to women as they consider their options, and can be incorporated into shared decision-making discussions with the provider.”
The study was sponsored by the National Institutes of Health. Dr. Grobman had no financial disclosures.
SOURCE: Grobman W. Am J Obstet Gynecol. 2018 Jan;218:S601.
DALLAS – Elective inductions at 39 weeks’ gestation were safe for the newborn and conferred dual benefits upon first-time mothers, reducing the risk of cesarean delivery by 16% and pregnancy-related hypertensive disorder by 36%, compared with women managed expectantly.
Infants delivered by elective inductions were smaller than those born to expectantly managed women and experienced a 29% reduction in the need for respiratory support at birth, William A. Grobman, MD, reported at the meeting, sponsored by the Society for Maternal-Fetal Medicine. They were no more likely than infants in the comparator group to experience dangerous perinatal outcomes, including low Apgar scores, meconium inhalation, hypoxia, or birth trauma, said Dr. Grobman, professor of obstetrics and gynecology at Northwestern University, Chicago.
The new data, however, may set a new standard by which to make this decision, Dr. Grobman said.
“I will leave it up to the professional organizations to determine the final outcome of these data, but it’s important to understand that the Choosing Wisely recommendation was based on observational data that essentially used an incorrect clinical comparator” of spontaneous labor, he said. The large study that Dr. Grobman and his colleagues conducted used expectant management (EM) as the comparator, allowing women to continue up to 42 weeks’ gestation. Using this comparator, he said, “Our data are largely with almost every observational study” and with a recently published randomized controlled trial by Kate F. Walker, a clinical research fellow at the University of Nottingham (England).
That study determined that labor induction between 39 weeks and 39 weeks, 6 days, in women older than 35 years had no significant effect on the rate of cesarean section and no adverse short-term effects on maternal or neonatal outcomes.
Dr. Grobman conducted his randomized trial at 41 hospitals in the National Institutes of Health’s Maternal-Fetal Medicine Units Network.
It randomized 6,106 healthy, nulliparous women to either elective induction from 39 weeks to 39 weeks, 4 days, or to EM. These women were asked to forgo elective delivery before 40 weeks, 5 days, but to be delivered by 42 weeks, 2 days.
The primary perinatal outcome was a composite endpoint that included fetal or neonatal death; respiratory support in the first 72 hours; 5-minute Apgar of 3 or lower; hypoxic ischemic encephalopathy; seizure; infection; meconium aspiration syndrome; birth trauma; intracranial or subgaleal hemorrhage; and hypotension requiring vasopressors.
The primary maternal outcome was a composite of cesarean delivery; hypertensive disorder of pregnancy; postpartum hemorrhage; chorioamnionitis; postpartum infection; labor pain; and the Labour Agentry Scale, a midwife-created measure of a laboring woman’s perception of her birth experience.
Women were a mean of 23.5 years old; about 44% of each group was privately insured. Prior pregnancy loss was more common among those randomized to EM (25.6% vs. 22.8%). Just over half were obese, with a body mass index of at least 30 kg/m2. Most (about 63%) had an unfavorable cervix, with a Bishop score of less than 5. The trial specified no particular induction regimen, Dr. Grobman said. “There were a variety of ripening agents and oxytocin regimens used.”
Infants in the elective induction group were born significantly earlier than were those in the EM group (39.3 vs. 40 weeks) and weighed significantly less (3,300 g vs. 3,380 g). Induction was safe for the newborn, with the primary endpoint occurring in 4.4%, compared with 5.4% of those in the EM group – not significantly different.
When investigators examined each outcome in the perinatal composite individually, only one – early respiratory support – was significantly different from the EM group. Infants in the induction group were 29% less likely to need respiratory support in the first 72 hours (3% vs. 4.2%; relative risk, 0.71). The rate of cesarean delivery also was significantly less among the induction group (18.6% vs. 22.2%; RR, 0.84).
None of these outcomes changed when the investigators controlled for race/ethnicity, Bishop score of less than 5, body mass index of 30 kg/m2 or more, or advanced maternal age.
Induction also was safe for mothers, and conferred a significant 36% reduction in the risk of pregnancy-related hypertensive disorders (9.1% vs. 14.1%; RR, 0.64). All other maternal outcomes were similar between the two groups.
The Agentry scale results also showed that women who were induced felt they were more in control of their birth experience, both at delivery and at 6 weeks’ postpartum. They also rated their worst labor pain and overall labor pain as significantly less than did women in the EM group.
“Our result suggest that policies directed toward avoidance of elective labor induction in nulliparous women would be unlikely to reduce the rate of cesarean section on a population level,” Dr. Grobman said. “To the contrary, our data show that, for every 28 nulliparous women to undergo elective induction at 39 weeks, one cesarean section would be avoided. Additionally, the number needed to treat to prevent one case of neonatal respiratory support is 83, and to prevent one case of hypertensive disease of pregnancy, 20. Our results should provide information useful to women as they consider their options, and can be incorporated into shared decision-making discussions with the provider.”
The study was sponsored by the National Institutes of Health. Dr. Grobman had no financial disclosures.
SOURCE: Grobman W. Am J Obstet Gynecol. 2018 Jan;218:S601.
AT THE PREGNANCY MEETING
Key clinical point: Induction at 39 weeks conferred some health benefits to nulliparous women and didn’t harm infants.
Major finding: Induction reduced risk of C-section by 16% and risk of pregnancy-related hypertensive disorder by 36%, compared with expectant management.
Study details: The study randomized 6,106 women to elective induction or expectant management with delivery by 42 weeks.
Disclosures: The National Institutes of Health sponsored the study; Dr. Grobman had no financial disclosures.
Source: Grobman W. Am J Obstet Gynecol. 2018 Jan;218:S601.
VIDEO: Cystic fibrosis patients need earlier, more frequent colorectal cancer screening
Adults with cystic fibrosis (CF) should undergo screening colonoscopy for colorectal cancer every 5 years beginning at age 40 years, unless they have had a solid organ transplant – in which case, screening should begin at age 30 years. For both groups, screening intervals should be shortened to 3 years if any adenomatous polyps are recovered.
The new screening recommendation is 1 of 10 set forth by the Cystic Fibrosis Foundation, in conjunction with the American Gastroenterological Association. The document reflects the significantly increased risk of colorectal cancer among adults with the chronic lung disorder, Denis Hadjiliadis, MD, and his colleagues wrote in the February issue of Gastroenterology. ; the risk approaches a 30-fold increase among CF patients who have undergone a lung transplant.
SOURCE: American Gastroenterological Association
In addition to making recommendations on screening intervals and protocols, the document asks clinicians to reframe their thinking of CF as a respiratory-only disease.
“Physicians should recognize that CF is a colon cancer syndrome,” wrote Dr. Hadjiliadis, director of the Adult Cystic Fibrosis Program at the University of Pennsylvania, Philadelphia, and his coauthors.
The increased colorectal cancer risk has become increasingly evident as CF patients live longer, Dr. Hadjiliadis and the panel wrote.
“The current median predicted survival is 41 years, and persons born in 2015 have an estimated average life expectancy of 45 years. The increasing longevity of adults with CF puts them at risk for other diseases, such as gastrointestinal cancer.”
In addition to the normal age-related risk, however, CF patients seem to have an elevated risk profile unique to the disease. The underlying causes have not been fully elucidated but may have to do with mutations in the cystic fibrosis transmembrane conductance regulator (CFTR), which are responsible for the excess thickened mucosal secretions that characterize CF. CFTR also is a tumor-suppressor gene in the intestinal tract of mice, and is important in gastrointestinal epithelial homeostasis. “Absence of CFTR is associated with dysregulation of the immune response, intestinal stem cells, and growth signaling regulators,” the authors noted.
In response to this observed increased risk of colorectal cancers among CF patients, the Cystic Fibrosis Foundation convened an 18-member task force to review the extant literature and compile colorectal cancer screening recommendations for CF patients who show no signs of such malignancies. The team reviewed 1,159 articles and based its findings on the 50 most relevant. The papers comprised observational studies, case-control studies, and case reports; there are no randomized clinical trials of screening for this population.
The American Gastroenterological Association reviewed and approved all of the recommendations:
- Screening decisions should be a collaborative process between the CF patient and clinician, taking into account comorbidities, safety, and quality of life. This should include a discussion of expected lifespan; patients with limited lifespan won’t benefit from screening for a slow-growing cancer. Patients should also consider that the colonoscopy prep for CF patients is somewhat more complex than for non-CF patients. “Given these complexities, the task force agreed that individuals with CF and their providers should … carefully assess the risks and benefits of CRC screening and its impact on the health and quality of life for the adult with CF.”
- The decision team should include an endoscopist. An endoscopist with CF training is preferred, but the panel noted these specialists are rare.
- Colonoscopy is the preferred method of screening for CF patients, since it can both detect and remove polyps. “This is one of the main reasons why colonoscopy is the screening procedure of choice for other high-risk groups,” the panel noted.
- There is insufficient evidence to recommend alternate screening methods in CF patients, including CT scanning, colonography, stool-based tests, or flexible sigmoidoscopy.
- In CF patients without signs of CRC, screening should commence at age 40 years and be repeated every 5 years as long as the results are negative.
- Any CF patient who has had adenomatous polyps on a screening colonoscopy should have a repeat colonoscopy within 3 years, unless clinical findings support more frequent screening.
- For any adult CF patient older than age 30 years who has undergone a solid organ transplant, screening colonoscopy should commence within 2 years of transplantation. “Although the absolute risk of CRC in individuals with CF is extremely low for patients younger than 30 years, the risk … greatly increases after lung transplantation,” to 25-30 times the age-adjusted baseline, the panel wrote. “Increased posttransplantation survival means that many transplant patients will enter older age groups where there is an increased risk of cancer.” Screening should be performed after recovery and within 2 years, unless there was a negative colonoscopy in the 5 years before transplant.
- Thereafter, patients who have had a solid organ transplant should undergo colonoscopy every 5 years, based on their life expectancy. “In cases where the expected survival time is limited (less than 10 years), screening should not be performed. For adults appropriately selected, lung transplantation usually increases survival probability. Therefore, a lung transplantation candidate with a short life expectancy is likely to become a screening candidate before and after transplantation at the appropriate ages described here, because the potential survival increases to approximately 10 years.”
- Colonoscopy should be repeated every 3 years on CF patients with transplants with a history of adenomatous polyps. This interval may be as short as 1 year for patients with high-risk, large, or multiple polyps.
- CF patients should undergo more intense bowel prep for colonoscopy, with three-four washes of a minimum of one liter of purgative per wash; the last wash should occur 4-6 hours before the procedure. Split-prep regimens (several smaller-volume washes) are better than a single larger-volume wash. The panel suggested a sample CF-specific regimen available from the Minnesota Cystic Fibrosis Center.
The new document reflects expert consensus on the currently available data, the panel said. As more data emerge, the recommendations might change.
“It is possible that different subpopulations will need more or less frequent schedules for rescreening and surveillance. Our recommendations are making an effort to balance the risk of missing advanced colorectal cancer and minimizing the burden and risk of too frequent examinations.”
None of the panel members had any financial disclosures.
SOURCE: Hadjiliadis D et al. Gastroenterology. 2017 Dec 28. doi. org/10.1053/j.gastro.2017.12.012
According to the Cystic Fibrosis Foundation Patient Registry, more than 30,000 people are living with cystic fibrosis (CF ) in the United States. More than half of the CF population is over 18 years of age! It is extremely important to talk to patients about preventative medicine which was not a topic of conversation CF healthcare providers were adding to their management plan in the past.
According to the Cystic Fibrosis Foundation Patient Registry, more than 30,000 people are living with cystic fibrosis (CF ) in the United States. More than half of the CF population is over 18 years of age! It is extremely important to talk to patients about preventative medicine which was not a topic of conversation CF healthcare providers were adding to their management plan in the past.
According to the Cystic Fibrosis Foundation Patient Registry, more than 30,000 people are living with cystic fibrosis (CF ) in the United States. More than half of the CF population is over 18 years of age! It is extremely important to talk to patients about preventative medicine which was not a topic of conversation CF healthcare providers were adding to their management plan in the past.
Adults with cystic fibrosis (CF) should undergo screening colonoscopy for colorectal cancer every 5 years beginning at age 40 years, unless they have had a solid organ transplant – in which case, screening should begin at age 30 years. For both groups, screening intervals should be shortened to 3 years if any adenomatous polyps are recovered.
The new screening recommendation is 1 of 10 set forth by the Cystic Fibrosis Foundation, in conjunction with the American Gastroenterological Association. The document reflects the significantly increased risk of colorectal cancer among adults with the chronic lung disorder, Denis Hadjiliadis, MD, and his colleagues wrote in the February issue of Gastroenterology. ; the risk approaches a 30-fold increase among CF patients who have undergone a lung transplant.
SOURCE: American Gastroenterological Association
In addition to making recommendations on screening intervals and protocols, the document asks clinicians to reframe their thinking of CF as a respiratory-only disease.
“Physicians should recognize that CF is a colon cancer syndrome,” wrote Dr. Hadjiliadis, director of the Adult Cystic Fibrosis Program at the University of Pennsylvania, Philadelphia, and his coauthors.
The increased colorectal cancer risk has become increasingly evident as CF patients live longer, Dr. Hadjiliadis and the panel wrote.
“The current median predicted survival is 41 years, and persons born in 2015 have an estimated average life expectancy of 45 years. The increasing longevity of adults with CF puts them at risk for other diseases, such as gastrointestinal cancer.”
In addition to the normal age-related risk, however, CF patients seem to have an elevated risk profile unique to the disease. The underlying causes have not been fully elucidated but may have to do with mutations in the cystic fibrosis transmembrane conductance regulator (CFTR), which are responsible for the excess thickened mucosal secretions that characterize CF. CFTR also is a tumor-suppressor gene in the intestinal tract of mice, and is important in gastrointestinal epithelial homeostasis. “Absence of CFTR is associated with dysregulation of the immune response, intestinal stem cells, and growth signaling regulators,” the authors noted.
In response to this observed increased risk of colorectal cancers among CF patients, the Cystic Fibrosis Foundation convened an 18-member task force to review the extant literature and compile colorectal cancer screening recommendations for CF patients who show no signs of such malignancies. The team reviewed 1,159 articles and based its findings on the 50 most relevant. The papers comprised observational studies, case-control studies, and case reports; there are no randomized clinical trials of screening for this population.
The American Gastroenterological Association reviewed and approved all of the recommendations:
- Screening decisions should be a collaborative process between the CF patient and clinician, taking into account comorbidities, safety, and quality of life. This should include a discussion of expected lifespan; patients with limited lifespan won’t benefit from screening for a slow-growing cancer. Patients should also consider that the colonoscopy prep for CF patients is somewhat more complex than for non-CF patients. “Given these complexities, the task force agreed that individuals with CF and their providers should … carefully assess the risks and benefits of CRC screening and its impact on the health and quality of life for the adult with CF.”
- The decision team should include an endoscopist. An endoscopist with CF training is preferred, but the panel noted these specialists are rare.
- Colonoscopy is the preferred method of screening for CF patients, since it can both detect and remove polyps. “This is one of the main reasons why colonoscopy is the screening procedure of choice for other high-risk groups,” the panel noted.
- There is insufficient evidence to recommend alternate screening methods in CF patients, including CT scanning, colonography, stool-based tests, or flexible sigmoidoscopy.
- In CF patients without signs of CRC, screening should commence at age 40 years and be repeated every 5 years as long as the results are negative.
- Any CF patient who has had adenomatous polyps on a screening colonoscopy should have a repeat colonoscopy within 3 years, unless clinical findings support more frequent screening.
- For any adult CF patient older than age 30 years who has undergone a solid organ transplant, screening colonoscopy should commence within 2 years of transplantation. “Although the absolute risk of CRC in individuals with CF is extremely low for patients younger than 30 years, the risk … greatly increases after lung transplantation,” to 25-30 times the age-adjusted baseline, the panel wrote. “Increased posttransplantation survival means that many transplant patients will enter older age groups where there is an increased risk of cancer.” Screening should be performed after recovery and within 2 years, unless there was a negative colonoscopy in the 5 years before transplant.
- Thereafter, patients who have had a solid organ transplant should undergo colonoscopy every 5 years, based on their life expectancy. “In cases where the expected survival time is limited (less than 10 years), screening should not be performed. For adults appropriately selected, lung transplantation usually increases survival probability. Therefore, a lung transplantation candidate with a short life expectancy is likely to become a screening candidate before and after transplantation at the appropriate ages described here, because the potential survival increases to approximately 10 years.”
- Colonoscopy should be repeated every 3 years on CF patients with transplants with a history of adenomatous polyps. This interval may be as short as 1 year for patients with high-risk, large, or multiple polyps.
- CF patients should undergo more intense bowel prep for colonoscopy, with three-four washes of a minimum of one liter of purgative per wash; the last wash should occur 4-6 hours before the procedure. Split-prep regimens (several smaller-volume washes) are better than a single larger-volume wash. The panel suggested a sample CF-specific regimen available from the Minnesota Cystic Fibrosis Center.
The new document reflects expert consensus on the currently available data, the panel said. As more data emerge, the recommendations might change.
“It is possible that different subpopulations will need more or less frequent schedules for rescreening and surveillance. Our recommendations are making an effort to balance the risk of missing advanced colorectal cancer and minimizing the burden and risk of too frequent examinations.”
None of the panel members had any financial disclosures.
SOURCE: Hadjiliadis D et al. Gastroenterology. 2017 Dec 28. doi. org/10.1053/j.gastro.2017.12.012
Adults with cystic fibrosis (CF) should undergo screening colonoscopy for colorectal cancer every 5 years beginning at age 40 years, unless they have had a solid organ transplant – in which case, screening should begin at age 30 years. For both groups, screening intervals should be shortened to 3 years if any adenomatous polyps are recovered.
The new screening recommendation is 1 of 10 set forth by the Cystic Fibrosis Foundation, in conjunction with the American Gastroenterological Association. The document reflects the significantly increased risk of colorectal cancer among adults with the chronic lung disorder, Denis Hadjiliadis, MD, and his colleagues wrote in the February issue of Gastroenterology. ; the risk approaches a 30-fold increase among CF patients who have undergone a lung transplant.
SOURCE: American Gastroenterological Association
In addition to making recommendations on screening intervals and protocols, the document asks clinicians to reframe their thinking of CF as a respiratory-only disease.
“Physicians should recognize that CF is a colon cancer syndrome,” wrote Dr. Hadjiliadis, director of the Adult Cystic Fibrosis Program at the University of Pennsylvania, Philadelphia, and his coauthors.
The increased colorectal cancer risk has become increasingly evident as CF patients live longer, Dr. Hadjiliadis and the panel wrote.
“The current median predicted survival is 41 years, and persons born in 2015 have an estimated average life expectancy of 45 years. The increasing longevity of adults with CF puts them at risk for other diseases, such as gastrointestinal cancer.”
In addition to the normal age-related risk, however, CF patients seem to have an elevated risk profile unique to the disease. The underlying causes have not been fully elucidated but may have to do with mutations in the cystic fibrosis transmembrane conductance regulator (CFTR), which are responsible for the excess thickened mucosal secretions that characterize CF. CFTR also is a tumor-suppressor gene in the intestinal tract of mice, and is important in gastrointestinal epithelial homeostasis. “Absence of CFTR is associated with dysregulation of the immune response, intestinal stem cells, and growth signaling regulators,” the authors noted.
In response to this observed increased risk of colorectal cancers among CF patients, the Cystic Fibrosis Foundation convened an 18-member task force to review the extant literature and compile colorectal cancer screening recommendations for CF patients who show no signs of such malignancies. The team reviewed 1,159 articles and based its findings on the 50 most relevant. The papers comprised observational studies, case-control studies, and case reports; there are no randomized clinical trials of screening for this population.
The American Gastroenterological Association reviewed and approved all of the recommendations:
- Screening decisions should be a collaborative process between the CF patient and clinician, taking into account comorbidities, safety, and quality of life. This should include a discussion of expected lifespan; patients with limited lifespan won’t benefit from screening for a slow-growing cancer. Patients should also consider that the colonoscopy prep for CF patients is somewhat more complex than for non-CF patients. “Given these complexities, the task force agreed that individuals with CF and their providers should … carefully assess the risks and benefits of CRC screening and its impact on the health and quality of life for the adult with CF.”
- The decision team should include an endoscopist. An endoscopist with CF training is preferred, but the panel noted these specialists are rare.
- Colonoscopy is the preferred method of screening for CF patients, since it can both detect and remove polyps. “This is one of the main reasons why colonoscopy is the screening procedure of choice for other high-risk groups,” the panel noted.
- There is insufficient evidence to recommend alternate screening methods in CF patients, including CT scanning, colonography, stool-based tests, or flexible sigmoidoscopy.
- In CF patients without signs of CRC, screening should commence at age 40 years and be repeated every 5 years as long as the results are negative.
- Any CF patient who has had adenomatous polyps on a screening colonoscopy should have a repeat colonoscopy within 3 years, unless clinical findings support more frequent screening.
- For any adult CF patient older than age 30 years who has undergone a solid organ transplant, screening colonoscopy should commence within 2 years of transplantation. “Although the absolute risk of CRC in individuals with CF is extremely low for patients younger than 30 years, the risk … greatly increases after lung transplantation,” to 25-30 times the age-adjusted baseline, the panel wrote. “Increased posttransplantation survival means that many transplant patients will enter older age groups where there is an increased risk of cancer.” Screening should be performed after recovery and within 2 years, unless there was a negative colonoscopy in the 5 years before transplant.
- Thereafter, patients who have had a solid organ transplant should undergo colonoscopy every 5 years, based on their life expectancy. “In cases where the expected survival time is limited (less than 10 years), screening should not be performed. For adults appropriately selected, lung transplantation usually increases survival probability. Therefore, a lung transplantation candidate with a short life expectancy is likely to become a screening candidate before and after transplantation at the appropriate ages described here, because the potential survival increases to approximately 10 years.”
- Colonoscopy should be repeated every 3 years on CF patients with transplants with a history of adenomatous polyps. This interval may be as short as 1 year for patients with high-risk, large, or multiple polyps.
- CF patients should undergo more intense bowel prep for colonoscopy, with three-four washes of a minimum of one liter of purgative per wash; the last wash should occur 4-6 hours before the procedure. Split-prep regimens (several smaller-volume washes) are better than a single larger-volume wash. The panel suggested a sample CF-specific regimen available from the Minnesota Cystic Fibrosis Center.
The new document reflects expert consensus on the currently available data, the panel said. As more data emerge, the recommendations might change.
“It is possible that different subpopulations will need more or less frequent schedules for rescreening and surveillance. Our recommendations are making an effort to balance the risk of missing advanced colorectal cancer and minimizing the burden and risk of too frequent examinations.”
None of the panel members had any financial disclosures.
SOURCE: Hadjiliadis D et al. Gastroenterology. 2017 Dec 28. doi. org/10.1053/j.gastro.2017.12.012
FROM GASTROENTEROLOGY
Full report confirms solanezumab’s failure to rescue cognition in mild Alzheimer’s
More than a year after the release of EXPEDITION 3’s negative data, a new report is reminding the world once more that antiamyloid antibodies have yet to live up to their promise.
Solanezumab, an antibody that targets soluble amyloid-beta (AB) did nothing to improve cognition in the phase 3, placebo-controlled trial of 2,129 patients with mild Alzheimer’s disease, Lawrence Honig, MD, and his colleagues reported in the Jan. 24 issue of the New England Journal of Medicine. Eli Lilly initially released the disappointing topline data in November 2016. The next month, Lilly detailed the numbers at the Clinical Trials in Alzheimer’s Disease (CTAD) meeting in San Diego.
Dr. Honig of Columbia University Medical Center, New York, presented the data at the San Diego meeting, as well as being primary author of the journal paper. In a nutshell, solanezumab was no better than placebo on any of the primary or secondary endpoints of cognition or function, he and his coinvestigators wrote.
At 80 weeks, scores on the Alzheimer’s Disease Assessment Scale-Cognitive subscale were similar in both treatment arms, with a change of 6.6 points in the solanezumab group and 7.4 in the placebo group. The secondary endpoints were considered descriptive only, but treated patients worsened on all of them: the Mini Mental State Exam, Clinical Dementia Rating Scale Sum of Boxes, Alzheimer’s Disease Cooperative Study Activities of Daily Living Inventory, Functional Activities Questionnaire, and the Integrated Alzheimer’s Disease Rating Scale.
Adverse events were common among both groups, occurring in 84.5% of the active group and 83.4% of the placebo group. However, four categories of events occurred significantly more often among those taking solanezumab: vitamin D deficiency, nasal congestion, spinal osteoarthritis, and dysuria. The placebo group was more likely to experience gait disturbance and somnolence.
Adverse events led to study discontinuation in 4.5% of the solanezumab group and 3.6% of the placebo group. One patient taking solanezumab and two taking placebo developed amyloid-related imaging abnormalities of edema/effusions. These were asymptomatic.
The authors provided several explanations for the negative results. Solanezumab does not attack consolidated amyloid plaques but rather binds to soluble AB. Biomarker studies did indicate that the antibody was hitting this target, but, the team said, “the observed peripheral reductions in soluble-free AB concentrations may not have been sufficient to reduce deposited cerebral amyloid, neuronal atrophy, or the pathobiologic events that lead to clinical decline.”
This observation renders null the peripheral sink hypothesis, which proposes that reducing free AB in plasma should lead to AB clearance from the brain. Despite reducing plasma concentrations of AB by about 90%, there was no obvious clinical impact on cognition, and no evidence of change in existing brain plaques. “Thus, a reduction in peripheral-free AB alone is unlikely to lead to clinically meaningful cognitive benefits,” they noted.
The investigators also suggested that the 400-mg monthly dose was probably much too small. Only about 3% of the antibody crossed the blood-brain barrier – too little to have a clinically meaningful effect, they posited.
Indeed, this idea of ineffective dosing has saved solanezumab from the ever-growing scrap heap of a decade’s worth of failed antiamyloid drugs. Solanezumab is also being investigated in the ongoing Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) prevention study and the Dominantly Inherited Alzheimer Network Trial (DIAN-TU).
Based on a rethinking of the failed EXPEDITION 3 and its likewise negative predecessors (EXPEDITION and EXPEDITION 2), researchers announced at CTAD 2017 that they will quadruple the dose of solanezumab in A4. Patients already enrolled will be titrated up from 400-mg to 1,600-mg infusions every month, principal investigator Reisa A. Sperling, MD, said at the meeting. DIAN-TU follows a dose-escalation pattern with no stated upward limit.
Timing – every AD researcher’s nightmare – also may have been a factor in EXPEDITION 3’s failure, Dr. Honig and his coauthors said. Even though it enrolled only patients with mild AD, they already may have been beyond the critical tipping point of potentially successful cognitive rescue.
“Some data from mouse models suggest that neurodegeneration in Alzheimer’s disease may reach a point at which it becomes self-propagating and not susceptible to intervention,” the team wrote.
At CTAD 2017, Dr. Sperling, director of the Center for Alzheimer’s Research and Treatment at Brigham and Women’s Hospital, Boston, echoed this comment, saying the fear of treating too late “keeps me up at night.” But recent advances in imaging confirm that amyloid pathology begins years, or even decades, before any cognitive changes occur. This gives researchers hope that backing up the treatment timeline even further may interrupt, or at least slow, the pathology that leads to memory loss.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment and prodromal Alzheimer’s,” Dr. Sperling said at the meeting. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Studies of cognitively healthy elderly who are amyloid positive, like A4, and of healthy younger subjects with high genetic risk factors, like DIAN-TU and the Colombian study of those with presenilin-1 mutations, should answer this question.
Finally, Dr. Honig and his colleagues wrote, the amyloid cascade hypothesis – the foundation of all antiamyloid therapies – may itself be flawed.
“Although the amyloid hypothesis is based on considerable genetic and biomarker data, if amyloid is not the cause of the disease, solanezumab would not be expected to slow disease progression. A single study ought not to be viewed as disproving a hypothesis; nevertheless, the amyloid hypothesis will need to be considered in the context of accruing results from this trial and other clinical trials of antiamyloid therapies.”
Eli Lilly sponsored EXPEDITION 3. Dr. Honig reported receiving financial remuneration from the company and financial ties with numerous other pharmaceutical manufacturers.
SOURCE: Honig LS et al. N Engl J Med. 2018;378:321-30.
Antiamyloid therapies may be facing the solemn ticking of time, Michael Paul Murphy, PhD, wrote in an accompanying editorial (N Engl J Med. 378;4;391-2).
It’s still possible that such a treatment might achieve success. The antiamyloid antibody aducanumab, which targets fibrillar amyloid-beta (AB), has shown some evidence of clinical benefit, with cognitive improvement tracking amyloid plaque clearance. While solanezumab was highly effective at clearing soluble AB, however, it did nothing to improve cognition.
“If clearing previously deposited amyloid from the brain is more important than preventing its production, this could also at least partially explain the lack of success with other strategies such as beta-secretase inhibitors that have, after initial promise, proved disappointing,” Dr. Murphy wrote.
Although perhaps too early to abandon AB immunotherapy, however, “it would be foolish to ignore the continued failures of antiamyloid approaches. In spite of the mountain of evidence supporting the primacy of AB in Alzheimer’s disease, many researchers are coming to the realization that our preclinical models of the disease may be missing the mark. Even if there is some future success in a primary prevention trial, there is still little headway being made in improving the treatment of Alzheimer’s disease.”
A multipronged treatment approach that attacks several key players in the AD pathologic parade, including tau, might be more successful.
“There is some hope that a combination of therapeutic approaches might help, since there is evidence that the different pathologic aspects of Alzheimer’s disease are interactive,” Dr. Murphy wrote. But “whether a multifaceted strategy or something entirely unforeseen is the answer, the field is clearly in need of innovative ideas. We may very well be nearing the end of the amyloid hypothesis rope, at which point one or two more failures will cause us to loosen our grip and let go.”
Dr. Murphy is an associate professor of cellular and molecular biochemistry at the University of Kentucky, Lexington. He has no relevant financial disclosures.
Antiamyloid therapies may be facing the solemn ticking of time, Michael Paul Murphy, PhD, wrote in an accompanying editorial (N Engl J Med. 378;4;391-2).
It’s still possible that such a treatment might achieve success. The antiamyloid antibody aducanumab, which targets fibrillar amyloid-beta (AB), has shown some evidence of clinical benefit, with cognitive improvement tracking amyloid plaque clearance. While solanezumab was highly effective at clearing soluble AB, however, it did nothing to improve cognition.
“If clearing previously deposited amyloid from the brain is more important than preventing its production, this could also at least partially explain the lack of success with other strategies such as beta-secretase inhibitors that have, after initial promise, proved disappointing,” Dr. Murphy wrote.
Although perhaps too early to abandon AB immunotherapy, however, “it would be foolish to ignore the continued failures of antiamyloid approaches. In spite of the mountain of evidence supporting the primacy of AB in Alzheimer’s disease, many researchers are coming to the realization that our preclinical models of the disease may be missing the mark. Even if there is some future success in a primary prevention trial, there is still little headway being made in improving the treatment of Alzheimer’s disease.”
A multipronged treatment approach that attacks several key players in the AD pathologic parade, including tau, might be more successful.
“There is some hope that a combination of therapeutic approaches might help, since there is evidence that the different pathologic aspects of Alzheimer’s disease are interactive,” Dr. Murphy wrote. But “whether a multifaceted strategy or something entirely unforeseen is the answer, the field is clearly in need of innovative ideas. We may very well be nearing the end of the amyloid hypothesis rope, at which point one or two more failures will cause us to loosen our grip and let go.”
Dr. Murphy is an associate professor of cellular and molecular biochemistry at the University of Kentucky, Lexington. He has no relevant financial disclosures.
Antiamyloid therapies may be facing the solemn ticking of time, Michael Paul Murphy, PhD, wrote in an accompanying editorial (N Engl J Med. 378;4;391-2).
It’s still possible that such a treatment might achieve success. The antiamyloid antibody aducanumab, which targets fibrillar amyloid-beta (AB), has shown some evidence of clinical benefit, with cognitive improvement tracking amyloid plaque clearance. While solanezumab was highly effective at clearing soluble AB, however, it did nothing to improve cognition.
“If clearing previously deposited amyloid from the brain is more important than preventing its production, this could also at least partially explain the lack of success with other strategies such as beta-secretase inhibitors that have, after initial promise, proved disappointing,” Dr. Murphy wrote.
Although perhaps too early to abandon AB immunotherapy, however, “it would be foolish to ignore the continued failures of antiamyloid approaches. In spite of the mountain of evidence supporting the primacy of AB in Alzheimer’s disease, many researchers are coming to the realization that our preclinical models of the disease may be missing the mark. Even if there is some future success in a primary prevention trial, there is still little headway being made in improving the treatment of Alzheimer’s disease.”
A multipronged treatment approach that attacks several key players in the AD pathologic parade, including tau, might be more successful.
“There is some hope that a combination of therapeutic approaches might help, since there is evidence that the different pathologic aspects of Alzheimer’s disease are interactive,” Dr. Murphy wrote. But “whether a multifaceted strategy or something entirely unforeseen is the answer, the field is clearly in need of innovative ideas. We may very well be nearing the end of the amyloid hypothesis rope, at which point one or two more failures will cause us to loosen our grip and let go.”
Dr. Murphy is an associate professor of cellular and molecular biochemistry at the University of Kentucky, Lexington. He has no relevant financial disclosures.
More than a year after the release of EXPEDITION 3’s negative data, a new report is reminding the world once more that antiamyloid antibodies have yet to live up to their promise.
Solanezumab, an antibody that targets soluble amyloid-beta (AB) did nothing to improve cognition in the phase 3, placebo-controlled trial of 2,129 patients with mild Alzheimer’s disease, Lawrence Honig, MD, and his colleagues reported in the Jan. 24 issue of the New England Journal of Medicine. Eli Lilly initially released the disappointing topline data in November 2016. The next month, Lilly detailed the numbers at the Clinical Trials in Alzheimer’s Disease (CTAD) meeting in San Diego.
Dr. Honig of Columbia University Medical Center, New York, presented the data at the San Diego meeting, as well as being primary author of the journal paper. In a nutshell, solanezumab was no better than placebo on any of the primary or secondary endpoints of cognition or function, he and his coinvestigators wrote.
At 80 weeks, scores on the Alzheimer’s Disease Assessment Scale-Cognitive subscale were similar in both treatment arms, with a change of 6.6 points in the solanezumab group and 7.4 in the placebo group. The secondary endpoints were considered descriptive only, but treated patients worsened on all of them: the Mini Mental State Exam, Clinical Dementia Rating Scale Sum of Boxes, Alzheimer’s Disease Cooperative Study Activities of Daily Living Inventory, Functional Activities Questionnaire, and the Integrated Alzheimer’s Disease Rating Scale.
Adverse events were common among both groups, occurring in 84.5% of the active group and 83.4% of the placebo group. However, four categories of events occurred significantly more often among those taking solanezumab: vitamin D deficiency, nasal congestion, spinal osteoarthritis, and dysuria. The placebo group was more likely to experience gait disturbance and somnolence.
Adverse events led to study discontinuation in 4.5% of the solanezumab group and 3.6% of the placebo group. One patient taking solanezumab and two taking placebo developed amyloid-related imaging abnormalities of edema/effusions. These were asymptomatic.
The authors provided several explanations for the negative results. Solanezumab does not attack consolidated amyloid plaques but rather binds to soluble AB. Biomarker studies did indicate that the antibody was hitting this target, but, the team said, “the observed peripheral reductions in soluble-free AB concentrations may not have been sufficient to reduce deposited cerebral amyloid, neuronal atrophy, or the pathobiologic events that lead to clinical decline.”
This observation renders null the peripheral sink hypothesis, which proposes that reducing free AB in plasma should lead to AB clearance from the brain. Despite reducing plasma concentrations of AB by about 90%, there was no obvious clinical impact on cognition, and no evidence of change in existing brain plaques. “Thus, a reduction in peripheral-free AB alone is unlikely to lead to clinically meaningful cognitive benefits,” they noted.
The investigators also suggested that the 400-mg monthly dose was probably much too small. Only about 3% of the antibody crossed the blood-brain barrier – too little to have a clinically meaningful effect, they posited.
Indeed, this idea of ineffective dosing has saved solanezumab from the ever-growing scrap heap of a decade’s worth of failed antiamyloid drugs. Solanezumab is also being investigated in the ongoing Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) prevention study and the Dominantly Inherited Alzheimer Network Trial (DIAN-TU).
Based on a rethinking of the failed EXPEDITION 3 and its likewise negative predecessors (EXPEDITION and EXPEDITION 2), researchers announced at CTAD 2017 that they will quadruple the dose of solanezumab in A4. Patients already enrolled will be titrated up from 400-mg to 1,600-mg infusions every month, principal investigator Reisa A. Sperling, MD, said at the meeting. DIAN-TU follows a dose-escalation pattern with no stated upward limit.
Timing – every AD researcher’s nightmare – also may have been a factor in EXPEDITION 3’s failure, Dr. Honig and his coauthors said. Even though it enrolled only patients with mild AD, they already may have been beyond the critical tipping point of potentially successful cognitive rescue.
“Some data from mouse models suggest that neurodegeneration in Alzheimer’s disease may reach a point at which it becomes self-propagating and not susceptible to intervention,” the team wrote.
At CTAD 2017, Dr. Sperling, director of the Center for Alzheimer’s Research and Treatment at Brigham and Women’s Hospital, Boston, echoed this comment, saying the fear of treating too late “keeps me up at night.” But recent advances in imaging confirm that amyloid pathology begins years, or even decades, before any cognitive changes occur. This gives researchers hope that backing up the treatment timeline even further may interrupt, or at least slow, the pathology that leads to memory loss.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment and prodromal Alzheimer’s,” Dr. Sperling said at the meeting. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Studies of cognitively healthy elderly who are amyloid positive, like A4, and of healthy younger subjects with high genetic risk factors, like DIAN-TU and the Colombian study of those with presenilin-1 mutations, should answer this question.
Finally, Dr. Honig and his colleagues wrote, the amyloid cascade hypothesis – the foundation of all antiamyloid therapies – may itself be flawed.
“Although the amyloid hypothesis is based on considerable genetic and biomarker data, if amyloid is not the cause of the disease, solanezumab would not be expected to slow disease progression. A single study ought not to be viewed as disproving a hypothesis; nevertheless, the amyloid hypothesis will need to be considered in the context of accruing results from this trial and other clinical trials of antiamyloid therapies.”
Eli Lilly sponsored EXPEDITION 3. Dr. Honig reported receiving financial remuneration from the company and financial ties with numerous other pharmaceutical manufacturers.
SOURCE: Honig LS et al. N Engl J Med. 2018;378:321-30.
More than a year after the release of EXPEDITION 3’s negative data, a new report is reminding the world once more that antiamyloid antibodies have yet to live up to their promise.
Solanezumab, an antibody that targets soluble amyloid-beta (AB) did nothing to improve cognition in the phase 3, placebo-controlled trial of 2,129 patients with mild Alzheimer’s disease, Lawrence Honig, MD, and his colleagues reported in the Jan. 24 issue of the New England Journal of Medicine. Eli Lilly initially released the disappointing topline data in November 2016. The next month, Lilly detailed the numbers at the Clinical Trials in Alzheimer’s Disease (CTAD) meeting in San Diego.
Dr. Honig of Columbia University Medical Center, New York, presented the data at the San Diego meeting, as well as being primary author of the journal paper. In a nutshell, solanezumab was no better than placebo on any of the primary or secondary endpoints of cognition or function, he and his coinvestigators wrote.
At 80 weeks, scores on the Alzheimer’s Disease Assessment Scale-Cognitive subscale were similar in both treatment arms, with a change of 6.6 points in the solanezumab group and 7.4 in the placebo group. The secondary endpoints were considered descriptive only, but treated patients worsened on all of them: the Mini Mental State Exam, Clinical Dementia Rating Scale Sum of Boxes, Alzheimer’s Disease Cooperative Study Activities of Daily Living Inventory, Functional Activities Questionnaire, and the Integrated Alzheimer’s Disease Rating Scale.
Adverse events were common among both groups, occurring in 84.5% of the active group and 83.4% of the placebo group. However, four categories of events occurred significantly more often among those taking solanezumab: vitamin D deficiency, nasal congestion, spinal osteoarthritis, and dysuria. The placebo group was more likely to experience gait disturbance and somnolence.
Adverse events led to study discontinuation in 4.5% of the solanezumab group and 3.6% of the placebo group. One patient taking solanezumab and two taking placebo developed amyloid-related imaging abnormalities of edema/effusions. These were asymptomatic.
The authors provided several explanations for the negative results. Solanezumab does not attack consolidated amyloid plaques but rather binds to soluble AB. Biomarker studies did indicate that the antibody was hitting this target, but, the team said, “the observed peripheral reductions in soluble-free AB concentrations may not have been sufficient to reduce deposited cerebral amyloid, neuronal atrophy, or the pathobiologic events that lead to clinical decline.”
This observation renders null the peripheral sink hypothesis, which proposes that reducing free AB in plasma should lead to AB clearance from the brain. Despite reducing plasma concentrations of AB by about 90%, there was no obvious clinical impact on cognition, and no evidence of change in existing brain plaques. “Thus, a reduction in peripheral-free AB alone is unlikely to lead to clinically meaningful cognitive benefits,” they noted.
The investigators also suggested that the 400-mg monthly dose was probably much too small. Only about 3% of the antibody crossed the blood-brain barrier – too little to have a clinically meaningful effect, they posited.
Indeed, this idea of ineffective dosing has saved solanezumab from the ever-growing scrap heap of a decade’s worth of failed antiamyloid drugs. Solanezumab is also being investigated in the ongoing Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) prevention study and the Dominantly Inherited Alzheimer Network Trial (DIAN-TU).
Based on a rethinking of the failed EXPEDITION 3 and its likewise negative predecessors (EXPEDITION and EXPEDITION 2), researchers announced at CTAD 2017 that they will quadruple the dose of solanezumab in A4. Patients already enrolled will be titrated up from 400-mg to 1,600-mg infusions every month, principal investigator Reisa A. Sperling, MD, said at the meeting. DIAN-TU follows a dose-escalation pattern with no stated upward limit.
Timing – every AD researcher’s nightmare – also may have been a factor in EXPEDITION 3’s failure, Dr. Honig and his coauthors said. Even though it enrolled only patients with mild AD, they already may have been beyond the critical tipping point of potentially successful cognitive rescue.
“Some data from mouse models suggest that neurodegeneration in Alzheimer’s disease may reach a point at which it becomes self-propagating and not susceptible to intervention,” the team wrote.
At CTAD 2017, Dr. Sperling, director of the Center for Alzheimer’s Research and Treatment at Brigham and Women’s Hospital, Boston, echoed this comment, saying the fear of treating too late “keeps me up at night.” But recent advances in imaging confirm that amyloid pathology begins years, or even decades, before any cognitive changes occur. This gives researchers hope that backing up the treatment timeline even further may interrupt, or at least slow, the pathology that leads to memory loss.
“One of the greatest advances in this field over the past 10 years is the recognition that Alzheimer’s disease is a continuum that likely begins well before the stage we recognize as dementia, and even before the stages of mild cognitive impairment and prodromal Alzheimer’s,” Dr. Sperling said at the meeting. “Treating in the presymptomatic phase may be the best opportunity to bend this curve back toward the trajectory of normal aging.”
Studies of cognitively healthy elderly who are amyloid positive, like A4, and of healthy younger subjects with high genetic risk factors, like DIAN-TU and the Colombian study of those with presenilin-1 mutations, should answer this question.
Finally, Dr. Honig and his colleagues wrote, the amyloid cascade hypothesis – the foundation of all antiamyloid therapies – may itself be flawed.
“Although the amyloid hypothesis is based on considerable genetic and biomarker data, if amyloid is not the cause of the disease, solanezumab would not be expected to slow disease progression. A single study ought not to be viewed as disproving a hypothesis; nevertheless, the amyloid hypothesis will need to be considered in the context of accruing results from this trial and other clinical trials of antiamyloid therapies.”
Eli Lilly sponsored EXPEDITION 3. Dr. Honig reported receiving financial remuneration from the company and financial ties with numerous other pharmaceutical manufacturers.
SOURCE: Honig LS et al. N Engl J Med. 2018;378:321-30.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The antiamyloid antibody solanezumab did not improve cognition relative to placebo in patients with mild Alzheimer’s.
Major finding: Scores on the ADAS-Cog14 were similar in the solanezumab and placebo groups (delta, 6.6 vs. 7.4 points).
Study details: The phase 3, randomized placebo-controlled study comprised 2,129 patients.
Disclosures: Eli Lilly sponsored the study. Dr. Honig has served as a consultant for the company and reported financial ties with numerous other pharmaceutical companies.
Source: Honig LS et al. N Engl J Med. 2018;378:321-30.
MGUS progression risk linked to IgM status
The mode and risk of disease progression significantly differs for patients with IgM monoclonal gammopathy of undetermined significance (MGUS) and those with non-IgM MGUS, Robert A. Kyle, MD, and his colleagues reported in the New England Journal of Medicine.
The risk for progression among IgM MGUS patients was 1.1 events/100 person-years, compared with 0.8 events among those with non-IgM MGUS – a significant difference. The researchers also found that risk is related to monoclonal (M) protein level and abnormal serum-free, light-chain assay results for both forms of MGUS.
Further, risk of progression varied with duration of follow-up in IgM MGUS, unlike non-IgM MGUS. However, for MGUS in general, “the risk of progression to myeloma or a related disorder is much less than the competing risk of death due to other causes,” Dr. Kyle, of the Mayo Clinic, Rochester, Minn., and his associates wrote.
The findings should help to determine the appropriate type of monitoring for MGUS patients, the researchers concluded.
The researchers reported results of the longest-yet follow-up study of MGUS patients. The team described median 34-year follow-up data on 1,384 patients with MGUS –70% with IgG type, 12% with IgA type, 15% with IgM type, and 3% with a biclonal gammopathy. (The patients formed the basis of an initial 2002 report.) They were diagnosed during 1960-1994, at a mean age of 72 years. Of these patients, 1,300 (94%) have died.
Among the 210 patients with IgM MGUS, the risk of progression was 2%/year in the first 10 years after diagnosis and 1%/year thereafter. Risk of progression did not vary during the follow-up of patients with non-IgM MGUS.
“The initial concentration of the serum M protein and the serum-free, light-chain ratio were the most important univariate risk factors for progression to a plasma cell disorder among patients with IgM or non-IgM MGUS. Combined, these two variables provided prognostic value in both IgM MGUS and non-IgM types of MGUS,” the authors wrote.
They explained that the difference may lie in the origins of MGUS. “IgM MGUS typically arises from a CD20+ lymphoplasmacytic cell that has not undergone switch recombination. … In contrast, non-IgM MGUS typically arises from mature plasma cells that have undergone switch recombination.”
During follow-up, 11% of the group (147) developed an MGUS-related disorder, including multiple myeloma, lymphoma with an IgM serum M protein, AL amyloidosis, macroglobulinemia, chronic lymphocytic leukemia, or plasmacytoma. This represents a 6.5-fold increased risk compared to the age- and sex-matched background population. Patients with IgM MGUS had a higher risk of progression than did those with non-IgM MGUS (relative risk, 10.8 vs. 5.7).
The overall risk of progression to a plasma cell–related disorder was 10% at 10 years; 18% at 20 years; 28% at 30 years; 36% at 35 years, and 36% at 40 years.
Among patients with IgM MGUS, the presence of high serum M protein (at least 1.5 g/dL) and an abnormal serum-free, light-chain ratio increased the risk of progression to 55% at 20 years, compared with a 41% risk among those patients with one risk factor and 19% among those with neither factor.
Among patients with non-IgM MGUS, the presence of both factors conferred a 30% risk of progression by 20 years. The risk was 20% among those with one factor and 7% among those with neither.
Compared with a control population, patients experienced about a 4-year shorter median survival time (8.1 vs. 12 years). Patients with IgM MGUS had worse 30-year overall survival than those with non-IgM MGUS (4% vs. 7%).
“There were 474 excess deaths in the cohort and 142 persons who had progression to multiple myeloma or a related disorder – findings that indicate that many additional deaths cannot be attributed to disease progression,” the authors noted.
The majority of deceased patients had died from non-plasma cell disorders (87%), including cardiovascular and cerebrovascular events, and nonplasma cell cancers. “In addition to the risk of malignant progression, this finding may be related to potentially serious disorders that led to the initial unexpected diagnosis of MGUS.”
The study was funded in part by the National Cancer Institute.
Dr. Kyle disclosed financial relationships with Celgene, Bristol-Myers Squibb, Amgen, Pharmacyclics, and Pfizer.
SOURCE: Kyle RA et al. N Engl J Med. 2018;378:241-9.
The mode and risk of disease progression significantly differs for patients with IgM monoclonal gammopathy of undetermined significance (MGUS) and those with non-IgM MGUS, Robert A. Kyle, MD, and his colleagues reported in the New England Journal of Medicine.
The risk for progression among IgM MGUS patients was 1.1 events/100 person-years, compared with 0.8 events among those with non-IgM MGUS – a significant difference. The researchers also found that risk is related to monoclonal (M) protein level and abnormal serum-free, light-chain assay results for both forms of MGUS.
Further, risk of progression varied with duration of follow-up in IgM MGUS, unlike non-IgM MGUS. However, for MGUS in general, “the risk of progression to myeloma or a related disorder is much less than the competing risk of death due to other causes,” Dr. Kyle, of the Mayo Clinic, Rochester, Minn., and his associates wrote.
The findings should help to determine the appropriate type of monitoring for MGUS patients, the researchers concluded.
The researchers reported results of the longest-yet follow-up study of MGUS patients. The team described median 34-year follow-up data on 1,384 patients with MGUS –70% with IgG type, 12% with IgA type, 15% with IgM type, and 3% with a biclonal gammopathy. (The patients formed the basis of an initial 2002 report.) They were diagnosed during 1960-1994, at a mean age of 72 years. Of these patients, 1,300 (94%) have died.
Among the 210 patients with IgM MGUS, the risk of progression was 2%/year in the first 10 years after diagnosis and 1%/year thereafter. Risk of progression did not vary during the follow-up of patients with non-IgM MGUS.
“The initial concentration of the serum M protein and the serum-free, light-chain ratio were the most important univariate risk factors for progression to a plasma cell disorder among patients with IgM or non-IgM MGUS. Combined, these two variables provided prognostic value in both IgM MGUS and non-IgM types of MGUS,” the authors wrote.
They explained that the difference may lie in the origins of MGUS. “IgM MGUS typically arises from a CD20+ lymphoplasmacytic cell that has not undergone switch recombination. … In contrast, non-IgM MGUS typically arises from mature plasma cells that have undergone switch recombination.”
During follow-up, 11% of the group (147) developed an MGUS-related disorder, including multiple myeloma, lymphoma with an IgM serum M protein, AL amyloidosis, macroglobulinemia, chronic lymphocytic leukemia, or plasmacytoma. This represents a 6.5-fold increased risk compared to the age- and sex-matched background population. Patients with IgM MGUS had a higher risk of progression than did those with non-IgM MGUS (relative risk, 10.8 vs. 5.7).
The overall risk of progression to a plasma cell–related disorder was 10% at 10 years; 18% at 20 years; 28% at 30 years; 36% at 35 years, and 36% at 40 years.
Among patients with IgM MGUS, the presence of high serum M protein (at least 1.5 g/dL) and an abnormal serum-free, light-chain ratio increased the risk of progression to 55% at 20 years, compared with a 41% risk among those patients with one risk factor and 19% among those with neither factor.
Among patients with non-IgM MGUS, the presence of both factors conferred a 30% risk of progression by 20 years. The risk was 20% among those with one factor and 7% among those with neither.
Compared with a control population, patients experienced about a 4-year shorter median survival time (8.1 vs. 12 years). Patients with IgM MGUS had worse 30-year overall survival than those with non-IgM MGUS (4% vs. 7%).
“There were 474 excess deaths in the cohort and 142 persons who had progression to multiple myeloma or a related disorder – findings that indicate that many additional deaths cannot be attributed to disease progression,” the authors noted.
The majority of deceased patients had died from non-plasma cell disorders (87%), including cardiovascular and cerebrovascular events, and nonplasma cell cancers. “In addition to the risk of malignant progression, this finding may be related to potentially serious disorders that led to the initial unexpected diagnosis of MGUS.”
The study was funded in part by the National Cancer Institute.
Dr. Kyle disclosed financial relationships with Celgene, Bristol-Myers Squibb, Amgen, Pharmacyclics, and Pfizer.
SOURCE: Kyle RA et al. N Engl J Med. 2018;378:241-9.
The mode and risk of disease progression significantly differs for patients with IgM monoclonal gammopathy of undetermined significance (MGUS) and those with non-IgM MGUS, Robert A. Kyle, MD, and his colleagues reported in the New England Journal of Medicine.
The risk for progression among IgM MGUS patients was 1.1 events/100 person-years, compared with 0.8 events among those with non-IgM MGUS – a significant difference. The researchers also found that risk is related to monoclonal (M) protein level and abnormal serum-free, light-chain assay results for both forms of MGUS.
Further, risk of progression varied with duration of follow-up in IgM MGUS, unlike non-IgM MGUS. However, for MGUS in general, “the risk of progression to myeloma or a related disorder is much less than the competing risk of death due to other causes,” Dr. Kyle, of the Mayo Clinic, Rochester, Minn., and his associates wrote.
The findings should help to determine the appropriate type of monitoring for MGUS patients, the researchers concluded.
The researchers reported results of the longest-yet follow-up study of MGUS patients. The team described median 34-year follow-up data on 1,384 patients with MGUS –70% with IgG type, 12% with IgA type, 15% with IgM type, and 3% with a biclonal gammopathy. (The patients formed the basis of an initial 2002 report.) They were diagnosed during 1960-1994, at a mean age of 72 years. Of these patients, 1,300 (94%) have died.
Among the 210 patients with IgM MGUS, the risk of progression was 2%/year in the first 10 years after diagnosis and 1%/year thereafter. Risk of progression did not vary during the follow-up of patients with non-IgM MGUS.
“The initial concentration of the serum M protein and the serum-free, light-chain ratio were the most important univariate risk factors for progression to a plasma cell disorder among patients with IgM or non-IgM MGUS. Combined, these two variables provided prognostic value in both IgM MGUS and non-IgM types of MGUS,” the authors wrote.
They explained that the difference may lie in the origins of MGUS. “IgM MGUS typically arises from a CD20+ lymphoplasmacytic cell that has not undergone switch recombination. … In contrast, non-IgM MGUS typically arises from mature plasma cells that have undergone switch recombination.”
During follow-up, 11% of the group (147) developed an MGUS-related disorder, including multiple myeloma, lymphoma with an IgM serum M protein, AL amyloidosis, macroglobulinemia, chronic lymphocytic leukemia, or plasmacytoma. This represents a 6.5-fold increased risk compared to the age- and sex-matched background population. Patients with IgM MGUS had a higher risk of progression than did those with non-IgM MGUS (relative risk, 10.8 vs. 5.7).
The overall risk of progression to a plasma cell–related disorder was 10% at 10 years; 18% at 20 years; 28% at 30 years; 36% at 35 years, and 36% at 40 years.
Among patients with IgM MGUS, the presence of high serum M protein (at least 1.5 g/dL) and an abnormal serum-free, light-chain ratio increased the risk of progression to 55% at 20 years, compared with a 41% risk among those patients with one risk factor and 19% among those with neither factor.
Among patients with non-IgM MGUS, the presence of both factors conferred a 30% risk of progression by 20 years. The risk was 20% among those with one factor and 7% among those with neither.
Compared with a control population, patients experienced about a 4-year shorter median survival time (8.1 vs. 12 years). Patients with IgM MGUS had worse 30-year overall survival than those with non-IgM MGUS (4% vs. 7%).
“There were 474 excess deaths in the cohort and 142 persons who had progression to multiple myeloma or a related disorder – findings that indicate that many additional deaths cannot be attributed to disease progression,” the authors noted.
The majority of deceased patients had died from non-plasma cell disorders (87%), including cardiovascular and cerebrovascular events, and nonplasma cell cancers. “In addition to the risk of malignant progression, this finding may be related to potentially serious disorders that led to the initial unexpected diagnosis of MGUS.”
The study was funded in part by the National Cancer Institute.
Dr. Kyle disclosed financial relationships with Celgene, Bristol-Myers Squibb, Amgen, Pharmacyclics, and Pfizer.
SOURCE: Kyle RA et al. N Engl J Med. 2018;378:241-9.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Survival is shorter in MGUS patients, but most die of causes unrelated to the disorder.
Major finding: Patients have an overall progression risk of 10% by 10 years, and experience a 4-year shortening of median survival time.
Study details: The 34-year follow-up study comprised 1,384 patients.Disclosures: The study was funded in part by the National Cancer Institute. Dr. Kyle disclosed relationships with several pharmaceutical companies.
Source: Kyle RA et al. N Engl J Med. 2018 Jan 18;378:241-9.
DMARDs may hamper pneumococcal vaccine response in systemic sclerosis patients
Patients taking disease-modifying antirheumatic medications for systemic sclerosis appear to have a decreased response to pneumococcal vaccines, a Swedish study has determined.
Those not taking disease-modifying antirheumatic medications (DMARDs), however, had a normal immune response, suggesting that it’s the immunomodulating medications, not the disease itself, that is affecting antibody levels, Roger Hesselstrand, MD, of Lund (Sweden) University and his colleagues reported online in Rheumatology.
“The currently recommended prime-boost vaccination strategy using a dose of PCV13 [13-valent pneumococcal conjugate vaccine] followed by a dose of PPV23 [23-valent pneumococcal polysaccharide vaccine] might be a possible way of enhancing the vaccine immunogenicity in immunosuppressed patients,” Dr. Hesselstrand and his coauthors wrote.
The study comprised 44 subjects with systemic sclerosis, 12 of whom were taking a DMARD (mycophenolate mofetil, azathioprine, or hydroxychloroquine), and 49 healthy controls; all underwent pneumococcal vaccination. The first 13 got a single dose of PPV23 intramuscularly. PCV13 was then licensed for adults in Sweden, and the remaining 31 patients received this vaccine. The primary outcome was 6-week change from baseline in the level of pneumococcal IgG to Streptococcus pneumoniae serotypes 23F and 6B.
Both vaccines were safe and well-tolerated by all patients, including those taking a DMARD.
Before vaccination, antibody levels to both serotypes were similar between the groups. After vaccination, antibody levels for both serotypes increased significantly in systemic sclerosis patients not taking a DMARD and in controls. However, patients taking a DMARD mounted only an adequate response to serotype 6B.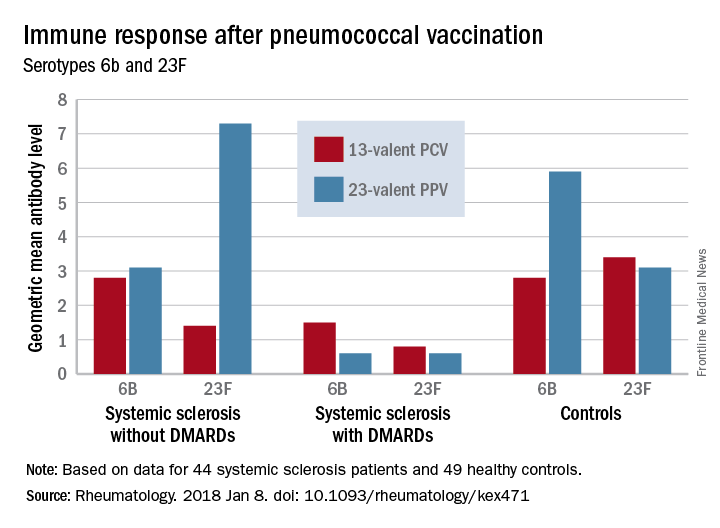
There were fewer responders among those taking DMARDs, whether they received the PCV13 or the PPV23 vaccine. An increase from prevaccination antibody levels of at least twofold occurred in fewer patients taking DMARDs than did in patients not taking DMARDs and in controls, regardless of vaccine type (PPV23, 50% vs. about 55% and 50%, respectively; PCV13, about 17% vs. 57% and 100%, respectively).
“We demonstrated that the antibody response ... as well as functionality of antibodies in [systemic sclerosis] patients not receiving DMARDs was as good as in controls regardless of vaccine type,” the investigators concluded. “Systemic sclerosis patients treated with DMARDs, however, had lower proportion of patients with positive antibody response, although the functionality of the antibodies was preserved. These results suggest that immunomodulating drugs but not systemic sclerosis itself and/or immunological disturbance as a part of this disease affect the ability to produce a sufficient amount of vaccine-specific antibodies, but not their function.”
None of the authors had conflicts of interest to disclose.
SOURCE: Hesselstrand R et al. Rheumatology [Oxford]. 2018 Jan 8. doi: 10.1093/rheumatology/kex471.
Patients taking disease-modifying antirheumatic medications for systemic sclerosis appear to have a decreased response to pneumococcal vaccines, a Swedish study has determined.
Those not taking disease-modifying antirheumatic medications (DMARDs), however, had a normal immune response, suggesting that it’s the immunomodulating medications, not the disease itself, that is affecting antibody levels, Roger Hesselstrand, MD, of Lund (Sweden) University and his colleagues reported online in Rheumatology.
“The currently recommended prime-boost vaccination strategy using a dose of PCV13 [13-valent pneumococcal conjugate vaccine] followed by a dose of PPV23 [23-valent pneumococcal polysaccharide vaccine] might be a possible way of enhancing the vaccine immunogenicity in immunosuppressed patients,” Dr. Hesselstrand and his coauthors wrote.
The study comprised 44 subjects with systemic sclerosis, 12 of whom were taking a DMARD (mycophenolate mofetil, azathioprine, or hydroxychloroquine), and 49 healthy controls; all underwent pneumococcal vaccination. The first 13 got a single dose of PPV23 intramuscularly. PCV13 was then licensed for adults in Sweden, and the remaining 31 patients received this vaccine. The primary outcome was 6-week change from baseline in the level of pneumococcal IgG to Streptococcus pneumoniae serotypes 23F and 6B.
Both vaccines were safe and well-tolerated by all patients, including those taking a DMARD.
Before vaccination, antibody levels to both serotypes were similar between the groups. After vaccination, antibody levels for both serotypes increased significantly in systemic sclerosis patients not taking a DMARD and in controls. However, patients taking a DMARD mounted only an adequate response to serotype 6B.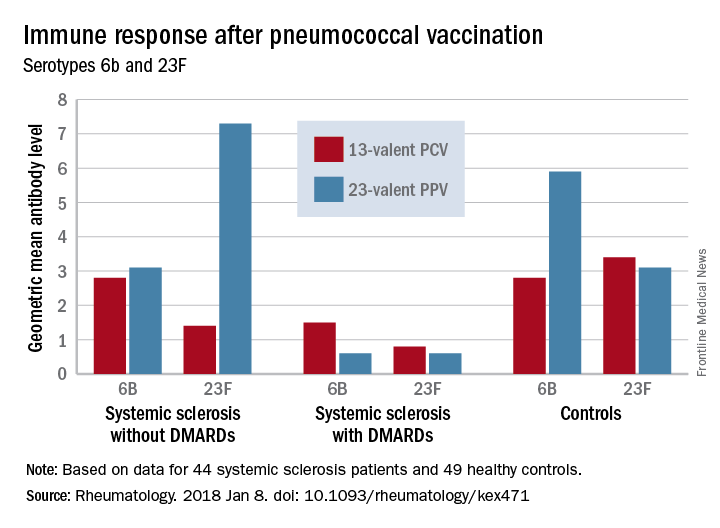
There were fewer responders among those taking DMARDs, whether they received the PCV13 or the PPV23 vaccine. An increase from prevaccination antibody levels of at least twofold occurred in fewer patients taking DMARDs than did in patients not taking DMARDs and in controls, regardless of vaccine type (PPV23, 50% vs. about 55% and 50%, respectively; PCV13, about 17% vs. 57% and 100%, respectively).
“We demonstrated that the antibody response ... as well as functionality of antibodies in [systemic sclerosis] patients not receiving DMARDs was as good as in controls regardless of vaccine type,” the investigators concluded. “Systemic sclerosis patients treated with DMARDs, however, had lower proportion of patients with positive antibody response, although the functionality of the antibodies was preserved. These results suggest that immunomodulating drugs but not systemic sclerosis itself and/or immunological disturbance as a part of this disease affect the ability to produce a sufficient amount of vaccine-specific antibodies, but not their function.”
None of the authors had conflicts of interest to disclose.
SOURCE: Hesselstrand R et al. Rheumatology [Oxford]. 2018 Jan 8. doi: 10.1093/rheumatology/kex471.
Patients taking disease-modifying antirheumatic medications for systemic sclerosis appear to have a decreased response to pneumococcal vaccines, a Swedish study has determined.
Those not taking disease-modifying antirheumatic medications (DMARDs), however, had a normal immune response, suggesting that it’s the immunomodulating medications, not the disease itself, that is affecting antibody levels, Roger Hesselstrand, MD, of Lund (Sweden) University and his colleagues reported online in Rheumatology.
“The currently recommended prime-boost vaccination strategy using a dose of PCV13 [13-valent pneumococcal conjugate vaccine] followed by a dose of PPV23 [23-valent pneumococcal polysaccharide vaccine] might be a possible way of enhancing the vaccine immunogenicity in immunosuppressed patients,” Dr. Hesselstrand and his coauthors wrote.
The study comprised 44 subjects with systemic sclerosis, 12 of whom were taking a DMARD (mycophenolate mofetil, azathioprine, or hydroxychloroquine), and 49 healthy controls; all underwent pneumococcal vaccination. The first 13 got a single dose of PPV23 intramuscularly. PCV13 was then licensed for adults in Sweden, and the remaining 31 patients received this vaccine. The primary outcome was 6-week change from baseline in the level of pneumococcal IgG to Streptococcus pneumoniae serotypes 23F and 6B.
Both vaccines were safe and well-tolerated by all patients, including those taking a DMARD.
Before vaccination, antibody levels to both serotypes were similar between the groups. After vaccination, antibody levels for both serotypes increased significantly in systemic sclerosis patients not taking a DMARD and in controls. However, patients taking a DMARD mounted only an adequate response to serotype 6B.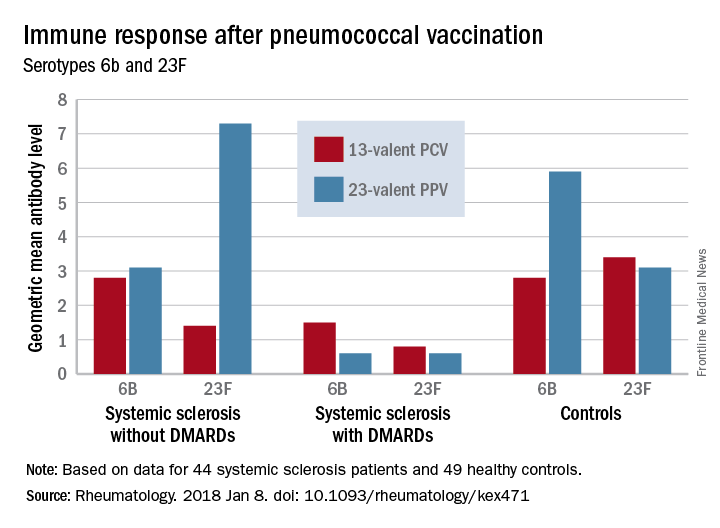
There were fewer responders among those taking DMARDs, whether they received the PCV13 or the PPV23 vaccine. An increase from prevaccination antibody levels of at least twofold occurred in fewer patients taking DMARDs than did in patients not taking DMARDs and in controls, regardless of vaccine type (PPV23, 50% vs. about 55% and 50%, respectively; PCV13, about 17% vs. 57% and 100%, respectively).
“We demonstrated that the antibody response ... as well as functionality of antibodies in [systemic sclerosis] patients not receiving DMARDs was as good as in controls regardless of vaccine type,” the investigators concluded. “Systemic sclerosis patients treated with DMARDs, however, had lower proportion of patients with positive antibody response, although the functionality of the antibodies was preserved. These results suggest that immunomodulating drugs but not systemic sclerosis itself and/or immunological disturbance as a part of this disease affect the ability to produce a sufficient amount of vaccine-specific antibodies, but not their function.”
None of the authors had conflicts of interest to disclose.
SOURCE: Hesselstrand R et al. Rheumatology [Oxford]. 2018 Jan 8. doi: 10.1093/rheumatology/kex471.
FROM RHEUMATOLOGY
Key clinical point:
Major finding: An increase in prevaccination antibody levels of at least twofold occurred in significantly fewer patients taking DMARDs than in patients not taking DMARDs and controls, regardless of vaccine type (PPV23, 50% vs. about 55% and 50%, respectively; PCV13, about 17% vs. 57% and 100%, respectively).
Study details: The prospective study comprised 44 systemic sclerosis patients and 49 healthy controls.
Disclosures: None of the authors had conflicts of interest to disclose.
Source: Hesselstrand R et al. Rheumatology [Oxford]. 2018 Jan 8. doi: 10.1093/rheumatology/kex471
Children with pathogenic TP53 variants face increased risk of hard-to-treat ALL
Pathogenic loss-of-function germline variants in the TP53 gene predispose children to acute lymphoblastic leukemia (ALL), and, later, to solid tumors that may be related to cancer therapy, according to results from a genetic sequencing study.
Researchers at St. Jude Children’s Hospital in Memphis have identified 49 unique variants of the gene among 3,801 children with newly diagnosed B-cell ALL; 22 variants were deemed pathogenic. Children with these variants were at a “dramatically higher risk” of secondary cancers, which occurred in 25% within 5 years of ALL treatment, compared with 0.7% among children without the pathogenic genetic signal, according to Maoxiang Qian, PhD, and colleagues. The report was published in the Journal of Clinical Oncology.
The increased risk of secondary cancers is probably related to a common characteristic of the pathogenic variants: the ablation of the p53-mediated DNA damage response. This increases the risk of the genotoxic therapy given during ALL treatment, according to the researchers.
“In fact, of the five patients with TP53 pathogenic variants who also had second cancers, two received irradiation therapy, including total body irradiation, and both subsequently developed solid tumors,” the researchers wrote. “The exact lifelong risk of second cancer in these patients is difficult to ascertain as many patients might have succumbed to relapsed ALL before they had the chance to develop second cancers.”
The research team conducted targeted sequencing of TP53 coding regions in 3,801 children who were enrolled in two trials sponsored by the Children’s Oncology Group (AALL0232 and P9900). They compared the results to TP53 mutations seen in almost 61,000 children enrolled in the Exome Aggregation Consortium (ExAC) cohort.
The researchers identified nine exonic nonsilent TP53 variants in the ALL cohort, all of which had an allele frequency of less than 0.5%. Of the variants, 22 were deemed pathogenic: Twelve showed a complete loss of transcriptional activity, three showed a partial loss of p53 function, and seven showed loss of the critical core DNA-binding domain in p53. The rest of the variants were deemed of unknown significance (VUS).
Pathogenic variants occurred in 26 children in the ALL cohort – significantly more often than in the control cohort (0.7% vs. 0.1%; odds ratio, 5.2). The VUS risk was not significantly elevated compared to controls, however.
Children with the pathogenic variants were significantly older at ALL diagnosis (15.5 vs. 6.6 years) and had significantly lower leukocyte count. Of the 26 with a pathogenic variant, 17 (65.4%) showed hypodiploidy in ALL blasts.
Pathogenic variants negatively affected ALL treatment outcomes, quadrupling the risk of lower event-free survival and lower overall survival (hazard ratio, 4.2 and 3.9, respectively) in both ALL cohorts.
Of the children with pathogenic variants, 14 experienced a pathological clinical event, including five ALL relapses and five second cancers, each accounting for 36% of all events.
“This pattern of events was dramatically different from that in patients with wild-type TP53 or VUS, for whom ALL relapse accounted for 75% of all events, with only 4% as second cancers,” the researchers wrote. “In fact, within hypodiploid ALL patients who experienced an event, the frequency of second cancer was significantly higher in those with TP53 pathogenic variants than in those without [50% vs. 5%], which additionally suggests that germline TP53 variation, instead of hypodiploid ALL, was the underlying cause of second cancers in these patients.”
The study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. Dr. Qian reported having no financial disclosures. Other researchers reported funding from various pharmaceutical companies.
SOURCE: Qian et al. JCO 2018 Jan 4. doi: 10.1200/JCO.2017.75.5215
Pathogenic loss-of-function germline variants in the TP53 gene predispose children to acute lymphoblastic leukemia (ALL), and, later, to solid tumors that may be related to cancer therapy, according to results from a genetic sequencing study.
Researchers at St. Jude Children’s Hospital in Memphis have identified 49 unique variants of the gene among 3,801 children with newly diagnosed B-cell ALL; 22 variants were deemed pathogenic. Children with these variants were at a “dramatically higher risk” of secondary cancers, which occurred in 25% within 5 years of ALL treatment, compared with 0.7% among children without the pathogenic genetic signal, according to Maoxiang Qian, PhD, and colleagues. The report was published in the Journal of Clinical Oncology.
The increased risk of secondary cancers is probably related to a common characteristic of the pathogenic variants: the ablation of the p53-mediated DNA damage response. This increases the risk of the genotoxic therapy given during ALL treatment, according to the researchers.
“In fact, of the five patients with TP53 pathogenic variants who also had second cancers, two received irradiation therapy, including total body irradiation, and both subsequently developed solid tumors,” the researchers wrote. “The exact lifelong risk of second cancer in these patients is difficult to ascertain as many patients might have succumbed to relapsed ALL before they had the chance to develop second cancers.”
The research team conducted targeted sequencing of TP53 coding regions in 3,801 children who were enrolled in two trials sponsored by the Children’s Oncology Group (AALL0232 and P9900). They compared the results to TP53 mutations seen in almost 61,000 children enrolled in the Exome Aggregation Consortium (ExAC) cohort.
The researchers identified nine exonic nonsilent TP53 variants in the ALL cohort, all of which had an allele frequency of less than 0.5%. Of the variants, 22 were deemed pathogenic: Twelve showed a complete loss of transcriptional activity, three showed a partial loss of p53 function, and seven showed loss of the critical core DNA-binding domain in p53. The rest of the variants were deemed of unknown significance (VUS).
Pathogenic variants occurred in 26 children in the ALL cohort – significantly more often than in the control cohort (0.7% vs. 0.1%; odds ratio, 5.2). The VUS risk was not significantly elevated compared to controls, however.
Children with the pathogenic variants were significantly older at ALL diagnosis (15.5 vs. 6.6 years) and had significantly lower leukocyte count. Of the 26 with a pathogenic variant, 17 (65.4%) showed hypodiploidy in ALL blasts.
Pathogenic variants negatively affected ALL treatment outcomes, quadrupling the risk of lower event-free survival and lower overall survival (hazard ratio, 4.2 and 3.9, respectively) in both ALL cohorts.
Of the children with pathogenic variants, 14 experienced a pathological clinical event, including five ALL relapses and five second cancers, each accounting for 36% of all events.
“This pattern of events was dramatically different from that in patients with wild-type TP53 or VUS, for whom ALL relapse accounted for 75% of all events, with only 4% as second cancers,” the researchers wrote. “In fact, within hypodiploid ALL patients who experienced an event, the frequency of second cancer was significantly higher in those with TP53 pathogenic variants than in those without [50% vs. 5%], which additionally suggests that germline TP53 variation, instead of hypodiploid ALL, was the underlying cause of second cancers in these patients.”
The study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. Dr. Qian reported having no financial disclosures. Other researchers reported funding from various pharmaceutical companies.
SOURCE: Qian et al. JCO 2018 Jan 4. doi: 10.1200/JCO.2017.75.5215
Pathogenic loss-of-function germline variants in the TP53 gene predispose children to acute lymphoblastic leukemia (ALL), and, later, to solid tumors that may be related to cancer therapy, according to results from a genetic sequencing study.
Researchers at St. Jude Children’s Hospital in Memphis have identified 49 unique variants of the gene among 3,801 children with newly diagnosed B-cell ALL; 22 variants were deemed pathogenic. Children with these variants were at a “dramatically higher risk” of secondary cancers, which occurred in 25% within 5 years of ALL treatment, compared with 0.7% among children without the pathogenic genetic signal, according to Maoxiang Qian, PhD, and colleagues. The report was published in the Journal of Clinical Oncology.
The increased risk of secondary cancers is probably related to a common characteristic of the pathogenic variants: the ablation of the p53-mediated DNA damage response. This increases the risk of the genotoxic therapy given during ALL treatment, according to the researchers.
“In fact, of the five patients with TP53 pathogenic variants who also had second cancers, two received irradiation therapy, including total body irradiation, and both subsequently developed solid tumors,” the researchers wrote. “The exact lifelong risk of second cancer in these patients is difficult to ascertain as many patients might have succumbed to relapsed ALL before they had the chance to develop second cancers.”
The research team conducted targeted sequencing of TP53 coding regions in 3,801 children who were enrolled in two trials sponsored by the Children’s Oncology Group (AALL0232 and P9900). They compared the results to TP53 mutations seen in almost 61,000 children enrolled in the Exome Aggregation Consortium (ExAC) cohort.
The researchers identified nine exonic nonsilent TP53 variants in the ALL cohort, all of which had an allele frequency of less than 0.5%. Of the variants, 22 were deemed pathogenic: Twelve showed a complete loss of transcriptional activity, three showed a partial loss of p53 function, and seven showed loss of the critical core DNA-binding domain in p53. The rest of the variants were deemed of unknown significance (VUS).
Pathogenic variants occurred in 26 children in the ALL cohort – significantly more often than in the control cohort (0.7% vs. 0.1%; odds ratio, 5.2). The VUS risk was not significantly elevated compared to controls, however.
Children with the pathogenic variants were significantly older at ALL diagnosis (15.5 vs. 6.6 years) and had significantly lower leukocyte count. Of the 26 with a pathogenic variant, 17 (65.4%) showed hypodiploidy in ALL blasts.
Pathogenic variants negatively affected ALL treatment outcomes, quadrupling the risk of lower event-free survival and lower overall survival (hazard ratio, 4.2 and 3.9, respectively) in both ALL cohorts.
Of the children with pathogenic variants, 14 experienced a pathological clinical event, including five ALL relapses and five second cancers, each accounting for 36% of all events.
“This pattern of events was dramatically different from that in patients with wild-type TP53 or VUS, for whom ALL relapse accounted for 75% of all events, with only 4% as second cancers,” the researchers wrote. “In fact, within hypodiploid ALL patients who experienced an event, the frequency of second cancer was significantly higher in those with TP53 pathogenic variants than in those without [50% vs. 5%], which additionally suggests that germline TP53 variation, instead of hypodiploid ALL, was the underlying cause of second cancers in these patients.”
The study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. Dr. Qian reported having no financial disclosures. Other researchers reported funding from various pharmaceutical companies.
SOURCE: Qian et al. JCO 2018 Jan 4. doi: 10.1200/JCO.2017.75.5215
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: TP53 variants quadrupled the risk of lower event-free survival and lower overall survival (HR 4.2 and 3.9, respectively).
Study details: The genetic sequencing study comprised 3,801 children with newly diagnosed B-cell ALL.
Disclosures: The study was supported by grants from the National Institutes of Health and the American Lebanese Syrian Associated Charities. Dr. Qian reported having no financial disclosures. Other researchers reported funding from various pharmaceutical companies.
Source: Qian et al. JCO 2018 Jan 4. doi: 10.1200/JCO.2017.75.5215.
High levels of neuroinflammatory markers may drive increased Alzheimer’s prevalence among blacks
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
REPORTING FROM FDA GRAND ROUNDS
Mutations on LRRK2 gene modify risks for both Crohn’s and Parkinson’s
Crohn’s and Parkinson’s diseases seem to share a common genetic risk pathway, mediated by mutations in a gene that modify disease risk in both directions.
A multidisciplinary collaboration of researchers have discovered that the Crohn’s risk variant N2081D in the leucine-rich repeat kinase 2 (LRRK2) gene lies close to variant G2019S, the major genetic risk factor for both sporadic and familial Parkinson’s. However, protective mutations also occur in the LRRK2 gene, and Ken Y. Hui, MD, of Yale University, New Haven, Conn., and his associates identified two that, when combined, significantly decrease the risk of Crohn’s.
The team first discovered the association in an exome sequencing study of 50 Crohn’s patients of Ashkenazi Jewish descent. This identified more than 4,000 potentially high-yield mutations, which they then examined in a pure Ashkenazi cohort of 1,477 Crohn’s patients and 2,614 healthy controls.
In this phase, the researchers found that N2081D in LRRK2 was associated with a 73% increased odds of Crohn’s. The LRRK2 N551K variant was associated with protection against Crohn’s, reducing odds for the disease by 35% (odds ratio, 0.65), as was R1398H, which conferred a 29% reduction in the likelihood of developing the disease (OR, 0.71). It has been known that these two mutations can combine to provide a protective genetic signature, and the team investigated this compound interaction as well.
After repeated analyses in large, unique case-control cohorts and tissue samples, they determined that the N2081D allele increased the odds of Crohn’s by 70% in the Ashkenazi subjects and by 60% in non-Ashkenazi subjects. The allele was associated with a 10% increased likelihood of Parkinson’s among the Ashkenazi cohort and a 30% increased likelihood among the non-Ashkenazi cohort.
The researchers also examined the two protective alleles, N551K and R1398H, in these further analyses. In the Ashkenazi cohort, N551K decreased the likelihood of Crohn’s by 33%, and it decreased the likelihood of Parkinson’s by 23% in non-Ashkenazi subjects (OR, 0.67 and 0.77, respectively).
In the Ashkenazi cohort, R1398H reduced the odds of Crohn’s by 29% and the odds of Parkinson’s by 16% (OR, 0.71 and 0.84, respectively). In the non-Ashkenazi cohort, the risk reduction was not significant.
Finally, they examined the effect of the mutations on macrophages isolated from four Crohn’s patients who carried the N2081D allele, as well as five patients with the two protective mutations N551K and R1398H and four patients with no mutation. When the macrophages were put in nutrient starvation, those from the N2081D carriers exhibited impaired resting acetylation of alpha-tubulin and poor response to cellular stress. Decreased alpha-tubulin acetylation is associated with poor protein transport through the cytoskeleton. “In contrast, the highest basal acetylation of alpha-tubulin was detected in macrophages of noncarriers and carriers of the protective N551K + R1398H mutations,” the investigators wrote.
“Our study strongly implicates the contribution of LRRK2 in Crohn’s disease risk,” they concluded. “The LRRK2 N2081D risk allele and the N551K/R1398H protective alleles, as well as numerous other variants within the LRRK2 locus, revealed shared genetic effects between Crohn’s and Parkinson’s risk, providing a potential biological basis for clinical co-occurrence. Our findings suggest that LRRK2 may be a useful target for developing drugs to treat Crohn’s disease.”
The research was supported by a variety of grants from the National Institutes of Health, the National Science Foundation, and various other foundations. Five of the authors reported consulting for various pharmaceutical companies or companies selling genetic information products. None of the other authors had relevant disclosures.
SOURCE: Hui K et al. Sci Transl Med. 2018. doi: 10.1126/scitranslmed.aai7795
Crohn’s and Parkinson’s diseases seem to share a common genetic risk pathway, mediated by mutations in a gene that modify disease risk in both directions.
A multidisciplinary collaboration of researchers have discovered that the Crohn’s risk variant N2081D in the leucine-rich repeat kinase 2 (LRRK2) gene lies close to variant G2019S, the major genetic risk factor for both sporadic and familial Parkinson’s. However, protective mutations also occur in the LRRK2 gene, and Ken Y. Hui, MD, of Yale University, New Haven, Conn., and his associates identified two that, when combined, significantly decrease the risk of Crohn’s.
The team first discovered the association in an exome sequencing study of 50 Crohn’s patients of Ashkenazi Jewish descent. This identified more than 4,000 potentially high-yield mutations, which they then examined in a pure Ashkenazi cohort of 1,477 Crohn’s patients and 2,614 healthy controls.
In this phase, the researchers found that N2081D in LRRK2 was associated with a 73% increased odds of Crohn’s. The LRRK2 N551K variant was associated with protection against Crohn’s, reducing odds for the disease by 35% (odds ratio, 0.65), as was R1398H, which conferred a 29% reduction in the likelihood of developing the disease (OR, 0.71). It has been known that these two mutations can combine to provide a protective genetic signature, and the team investigated this compound interaction as well.
After repeated analyses in large, unique case-control cohorts and tissue samples, they determined that the N2081D allele increased the odds of Crohn’s by 70% in the Ashkenazi subjects and by 60% in non-Ashkenazi subjects. The allele was associated with a 10% increased likelihood of Parkinson’s among the Ashkenazi cohort and a 30% increased likelihood among the non-Ashkenazi cohort.
The researchers also examined the two protective alleles, N551K and R1398H, in these further analyses. In the Ashkenazi cohort, N551K decreased the likelihood of Crohn’s by 33%, and it decreased the likelihood of Parkinson’s by 23% in non-Ashkenazi subjects (OR, 0.67 and 0.77, respectively).
In the Ashkenazi cohort, R1398H reduced the odds of Crohn’s by 29% and the odds of Parkinson’s by 16% (OR, 0.71 and 0.84, respectively). In the non-Ashkenazi cohort, the risk reduction was not significant.
Finally, they examined the effect of the mutations on macrophages isolated from four Crohn’s patients who carried the N2081D allele, as well as five patients with the two protective mutations N551K and R1398H and four patients with no mutation. When the macrophages were put in nutrient starvation, those from the N2081D carriers exhibited impaired resting acetylation of alpha-tubulin and poor response to cellular stress. Decreased alpha-tubulin acetylation is associated with poor protein transport through the cytoskeleton. “In contrast, the highest basal acetylation of alpha-tubulin was detected in macrophages of noncarriers and carriers of the protective N551K + R1398H mutations,” the investigators wrote.
“Our study strongly implicates the contribution of LRRK2 in Crohn’s disease risk,” they concluded. “The LRRK2 N2081D risk allele and the N551K/R1398H protective alleles, as well as numerous other variants within the LRRK2 locus, revealed shared genetic effects between Crohn’s and Parkinson’s risk, providing a potential biological basis for clinical co-occurrence. Our findings suggest that LRRK2 may be a useful target for developing drugs to treat Crohn’s disease.”
The research was supported by a variety of grants from the National Institutes of Health, the National Science Foundation, and various other foundations. Five of the authors reported consulting for various pharmaceutical companies or companies selling genetic information products. None of the other authors had relevant disclosures.
SOURCE: Hui K et al. Sci Transl Med. 2018. doi: 10.1126/scitranslmed.aai7795
Crohn’s and Parkinson’s diseases seem to share a common genetic risk pathway, mediated by mutations in a gene that modify disease risk in both directions.
A multidisciplinary collaboration of researchers have discovered that the Crohn’s risk variant N2081D in the leucine-rich repeat kinase 2 (LRRK2) gene lies close to variant G2019S, the major genetic risk factor for both sporadic and familial Parkinson’s. However, protective mutations also occur in the LRRK2 gene, and Ken Y. Hui, MD, of Yale University, New Haven, Conn., and his associates identified two that, when combined, significantly decrease the risk of Crohn’s.
The team first discovered the association in an exome sequencing study of 50 Crohn’s patients of Ashkenazi Jewish descent. This identified more than 4,000 potentially high-yield mutations, which they then examined in a pure Ashkenazi cohort of 1,477 Crohn’s patients and 2,614 healthy controls.
In this phase, the researchers found that N2081D in LRRK2 was associated with a 73% increased odds of Crohn’s. The LRRK2 N551K variant was associated with protection against Crohn’s, reducing odds for the disease by 35% (odds ratio, 0.65), as was R1398H, which conferred a 29% reduction in the likelihood of developing the disease (OR, 0.71). It has been known that these two mutations can combine to provide a protective genetic signature, and the team investigated this compound interaction as well.
After repeated analyses in large, unique case-control cohorts and tissue samples, they determined that the N2081D allele increased the odds of Crohn’s by 70% in the Ashkenazi subjects and by 60% in non-Ashkenazi subjects. The allele was associated with a 10% increased likelihood of Parkinson’s among the Ashkenazi cohort and a 30% increased likelihood among the non-Ashkenazi cohort.
The researchers also examined the two protective alleles, N551K and R1398H, in these further analyses. In the Ashkenazi cohort, N551K decreased the likelihood of Crohn’s by 33%, and it decreased the likelihood of Parkinson’s by 23% in non-Ashkenazi subjects (OR, 0.67 and 0.77, respectively).
In the Ashkenazi cohort, R1398H reduced the odds of Crohn’s by 29% and the odds of Parkinson’s by 16% (OR, 0.71 and 0.84, respectively). In the non-Ashkenazi cohort, the risk reduction was not significant.
Finally, they examined the effect of the mutations on macrophages isolated from four Crohn’s patients who carried the N2081D allele, as well as five patients with the two protective mutations N551K and R1398H and four patients with no mutation. When the macrophages were put in nutrient starvation, those from the N2081D carriers exhibited impaired resting acetylation of alpha-tubulin and poor response to cellular stress. Decreased alpha-tubulin acetylation is associated with poor protein transport through the cytoskeleton. “In contrast, the highest basal acetylation of alpha-tubulin was detected in macrophages of noncarriers and carriers of the protective N551K + R1398H mutations,” the investigators wrote.
“Our study strongly implicates the contribution of LRRK2 in Crohn’s disease risk,” they concluded. “The LRRK2 N2081D risk allele and the N551K/R1398H protective alleles, as well as numerous other variants within the LRRK2 locus, revealed shared genetic effects between Crohn’s and Parkinson’s risk, providing a potential biological basis for clinical co-occurrence. Our findings suggest that LRRK2 may be a useful target for developing drugs to treat Crohn’s disease.”
The research was supported by a variety of grants from the National Institutes of Health, the National Science Foundation, and various other foundations. Five of the authors reported consulting for various pharmaceutical companies or companies selling genetic information products. None of the other authors had relevant disclosures.
SOURCE: Hui K et al. Sci Transl Med. 2018. doi: 10.1126/scitranslmed.aai7795
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Variant N2081D in LRRK2 was associated with a 73% increased risk of Crohn’s.
Study details: The study comprised data from 30,269 patients and controls.
Disclosures: The research was supported by a variety of grants from the National Institutes of Health, the National Science Foundation, and various other foundations. Five of the authors reported consulting for various pharmaceutical companies or companies selling genetic information products. None of the other authors had relevant disclosures.
Source: Hui K et al. Sci Transl Med. 2018. doi: 10.1126/scitranslmed.aai7795