User login
In Brazil, few patients get second- and third-line treatment for metastatic RCC
, a retrospective study showed.
Of 3,990 patients with metastatic renal cell carcinoma (mRCC), 79% received an appropriate first-line treatment – mainly a vascular endothelial growth factor agent. But only 20% went on to get a second-line agent, and just 5% received a third-line agent, Paulo G. Bergerot, MD, and his colleagues reported in the Journal of Global Oncology.
Patients in private institutions were significantly more likely to receive appropriate first- and second-line treatment than those in public institutions, although the numbers receiving third-line agents were similarly low, reported Dr. Bergerot of the Federal University of São Paulo and his coauthors.
The study highlights sharp discrepancies between treatment in Brazil and more developed countries, the team noted.
“Previous reports from the International Metastatic Renal Cell Carcinoma Database Consortium suggest that approximately 48% of patients who receive first-line therapy proceed to second-line therapy. In addition, among patients who received first-line therapy in this experience, approximately 21% received third-line therapy,” the investigators wrote.
The reasons behind the differences aren’t entirely clear, but cost and clinicians’ knowledge of emerging study data could be major factors, they suggested.
“In particular, we suspect limited availability and cost of second-line treatments to be a barrier, although our data set did not have the capability of confirming this. Another barrier to receipt of second-line therapy might be educational gaps among practitioners. Emerging data from phase 3 studies supporting the use of agents in the refractory setting may not be widely broadcast. The discordance in receipt of therapies in private and public settings is perhaps the greatest indication that financial and social barriers likely affect treatment paradigms in Brazil,” the authors wrote.
Slow dissemination of clinical knowledge may also be reflected in another of the team’s findings: 240 patients received “nontraditional” first-line cytotoxic treatments, which lacked regulatory approval and had little supporting evidence for treating mRCC, the investigators reported.
Dr. Bergerot had no relevant financial disclosures, although several of his coauthors reported financial relationships with various pharmaceutical companies.
SOURCE: Bergerot et al. J Glob Oncol. 2017 Dec 27. doi: 10.1200/JGO.17.00113.
, a retrospective study showed.
Of 3,990 patients with metastatic renal cell carcinoma (mRCC), 79% received an appropriate first-line treatment – mainly a vascular endothelial growth factor agent. But only 20% went on to get a second-line agent, and just 5% received a third-line agent, Paulo G. Bergerot, MD, and his colleagues reported in the Journal of Global Oncology.
Patients in private institutions were significantly more likely to receive appropriate first- and second-line treatment than those in public institutions, although the numbers receiving third-line agents were similarly low, reported Dr. Bergerot of the Federal University of São Paulo and his coauthors.
The study highlights sharp discrepancies between treatment in Brazil and more developed countries, the team noted.
“Previous reports from the International Metastatic Renal Cell Carcinoma Database Consortium suggest that approximately 48% of patients who receive first-line therapy proceed to second-line therapy. In addition, among patients who received first-line therapy in this experience, approximately 21% received third-line therapy,” the investigators wrote.
The reasons behind the differences aren’t entirely clear, but cost and clinicians’ knowledge of emerging study data could be major factors, they suggested.
“In particular, we suspect limited availability and cost of second-line treatments to be a barrier, although our data set did not have the capability of confirming this. Another barrier to receipt of second-line therapy might be educational gaps among practitioners. Emerging data from phase 3 studies supporting the use of agents in the refractory setting may not be widely broadcast. The discordance in receipt of therapies in private and public settings is perhaps the greatest indication that financial and social barriers likely affect treatment paradigms in Brazil,” the authors wrote.
Slow dissemination of clinical knowledge may also be reflected in another of the team’s findings: 240 patients received “nontraditional” first-line cytotoxic treatments, which lacked regulatory approval and had little supporting evidence for treating mRCC, the investigators reported.
Dr. Bergerot had no relevant financial disclosures, although several of his coauthors reported financial relationships with various pharmaceutical companies.
SOURCE: Bergerot et al. J Glob Oncol. 2017 Dec 27. doi: 10.1200/JGO.17.00113.
, a retrospective study showed.
Of 3,990 patients with metastatic renal cell carcinoma (mRCC), 79% received an appropriate first-line treatment – mainly a vascular endothelial growth factor agent. But only 20% went on to get a second-line agent, and just 5% received a third-line agent, Paulo G. Bergerot, MD, and his colleagues reported in the Journal of Global Oncology.
Patients in private institutions were significantly more likely to receive appropriate first- and second-line treatment than those in public institutions, although the numbers receiving third-line agents were similarly low, reported Dr. Bergerot of the Federal University of São Paulo and his coauthors.
The study highlights sharp discrepancies between treatment in Brazil and more developed countries, the team noted.
“Previous reports from the International Metastatic Renal Cell Carcinoma Database Consortium suggest that approximately 48% of patients who receive first-line therapy proceed to second-line therapy. In addition, among patients who received first-line therapy in this experience, approximately 21% received third-line therapy,” the investigators wrote.
The reasons behind the differences aren’t entirely clear, but cost and clinicians’ knowledge of emerging study data could be major factors, they suggested.
“In particular, we suspect limited availability and cost of second-line treatments to be a barrier, although our data set did not have the capability of confirming this. Another barrier to receipt of second-line therapy might be educational gaps among practitioners. Emerging data from phase 3 studies supporting the use of agents in the refractory setting may not be widely broadcast. The discordance in receipt of therapies in private and public settings is perhaps the greatest indication that financial and social barriers likely affect treatment paradigms in Brazil,” the authors wrote.
Slow dissemination of clinical knowledge may also be reflected in another of the team’s findings: 240 patients received “nontraditional” first-line cytotoxic treatments, which lacked regulatory approval and had little supporting evidence for treating mRCC, the investigators reported.
Dr. Bergerot had no relevant financial disclosures, although several of his coauthors reported financial relationships with various pharmaceutical companies.
SOURCE: Bergerot et al. J Glob Oncol. 2017 Dec 27. doi: 10.1200/JGO.17.00113.
FROM THE JOURNAL OF GLOBAL ONCOLOGY
Key clinical point: Few Brazilians with mRCC receive anything after their first-line treatment.
Major finding: First-line agents were used in 79% of the cohort, but only 20% got second-line treatments and just 5%, third-line treatment.
Study details: A retrospective database study involving 3,990 patients with mRCC.
Disclosures: Dr. Bergerot had no relevant financial disclosures, although several of his coauthors disclosed financial relationships with pharmaceutical companies.
Source: Bergerot et al. J Glob Oncol. 2017 Dec 27. doi: 10.1200/JGO.17.00113.
Idalopirdine falls short in three phase 3 Alzheimer’s trials
Idalopirdine suffered the final nail in its coffin with the complete release of its phase 3 data detailing its failure to improve cognitive outcomes in patients with mild to moderate Alzheimer’s disease.
The 5-HT6 receptor antagonist idalopirdine was given on a background of stable cholinesterase inhibitor therapy in three Lundbeck-sponsored phase 3 trials: STARSHINE, STARBEAM, and STARBRIGHT. But none of the STAR studies reproduced the results of idalopirdine’s modestly successful phase 2 study, LADDER, wrote Alireza Atri, MD, PhD, and his colleagues. The report appears Jan. 9 in JAMA.
STARSHINE, STARBEAM, and STARBRIGHT were all 24-week, fixed-dose, randomized placebo-controlled studies with the same endpoint: change on the Alzheimer’s Disease Cooperative Scale–cognitive (ADAS-cog) measure. Together, they enrolled 2,525 patients with mild to moderate AD. Patients were a mean of 74 years old, with a mean Mini Mental State Exam Score of 17-18 and a mean baseline ADAS-cog of 26.
Study 1 (STARSHINE) randomized patients to background donepezil plus placebo, or idalopirdine 30 mg or 60 mg. Study 2 (STARBEAM) randomized patients to background donepezil plus placebo or idalopirdine 10 mg or 30 mg. Study 3 (STARBRIGHT) randomized patients to background donepezil, rivastigmine, or galantamine plus placebo or 60 mg idalopirdine.
Cohort retention was good in all three studies, with about a 9% dropout rate for those taking placebo, 10% for those taking 10 mg or 30 mg idalopirdine, and 11% for those taking the 60-mg dose. The adverse event profile was also acceptable. However, there were no statistically significant cognitive improvements in any study.
In study 1, the mean 24-week change in ADAS-cog total score was 0.37 for the 60-mg group, 0.61 for the 30-mg group, and 0.41 for the placebo group. Compared with placebo, the mean difference in ADAS-cog score change was 0.05 for the 60-mg dose group and 0.33 for the 30-mg group.
In study 2, the mean 24-week change in ADAS-cog score was 1.01 for the 30-mg group, 0.53 for the 10-mg group, and 0.56 for the placebo group. Compared with placebo, the adjusted mean difference in ADAS-cog was 0.63 for the 30-mg group and −0.09 for the 10-mg group.
In study 3, the mean ADAS-cog change was 0.38 for the 60-mg group and 0.82 for the placebo group. Compared with placebo, the mean difference was –0.55.
Adverse events were similar across the studies. The most common treatment-related adverse events were accidental overdose (idalopirdine treatment groups: 5%-11%; placebo: 9%-12%). Falls were the next most common (idalopirdine treatment groups: 4%-6%; placebo: 3%-6%). Cholinergic adverse events were also more common among those taking the study drug, with nausea and vomiting occurring in up to 4% of patients. About 5%-7% of patients taking idalopirdine discontinued because of a treatment-emergent adverse event, compared with 3%-5% of those taking placebo.
Five patients taking idalopirdine and three taking placebo died during the study; no death was related to the study drug. There was no indication of suicidal ideation or behavior associated with idalopirdine.
One striking difference between the modestly successful phase 2 and the clearly negative phase 3 studies was dosage, Dr. Atri noted. LADDER tested 90 mg of idalopirdine, split into three 30-mg doses each day. The STAR-series opted for a lower dose because PET studies on healthy volunteers showed high binding on the 5-HT6 receptors (more than 80%) at both the 30- and 60-mg doses.
“Although there is an approximate 40% decrease in 5-HT6 receptor expression among patients with Alzheimer disease compared with healthy individuals, there are also potential limitations in translating occupancy data from healthy individuals to those with a diseased brain,” the authors noted.
Based on the soundly negative data, and disappointing results with idalopirdine’s close competitor, intepirdine, it may be time to retire this area of investigation entirely, Dr. Atri concluded.
“Placing the results of this study in the broader context of the 5-HT6 antagonism adjunctive to cholinesterase inhibitor therapy mechanism of action suggests a lack of efficacy for this approach in the treatment of Alzheimer disease. In the phase 3 MINDSET study, intepirdine (another 5-HT6 antagonist) was administered at a dose of 35 mg daily added to background donepezil therapy in patients with mild to moderate Alzheimer disease and it failed to meet cognitive and functional efficacy outcomes.”
As if on cue with the idalopirdine data, Axovant Life Sciences, the New York company developing intepirdine, announced on Jan. 8 that it would shelve that drug. The announcement came on the heels of negative findings in its last best-hope studies aimed at patients with Lewy body dementia.
In the HEADWAY Lewy body dementia study, neither 35 mg nor 70 mg of intepirdine significantly improved cognition, compared with placebo. The 70-mg dose was associated with a small but insignificant improvement in motor function, but the 35-mg dose was associated with a 2-point worsening.
In a phase 2 study of intepirdine in patients with dementia and gait impairment, 35 mg of intepirdine did not improve gait speed.
“Based on the totality of intepirdine data to date, there is no evidence to support its further development. We are incredibly disappointed and saddened for the millions of people living with these difficult conditions, and are deeply grateful to the patients, caregivers and investigators who participated in our trials,” David Hung, MD, chief executive officer of Axovant, said in a press statement.
Dr. Atri reported financial relationships with numerous pharmaceutical companies, including Lundbeck, which sponsored the STAR trials.
This article was updated 1/12/18.
Idalopirdine’s failure is an all-too-familiar theme in Alzheimer’s research: a drug with a rational therapeutic target, which performed reasonable well in early clinical trials, but fell apart in large phase 3 studies, David Bennett, MD, wrote in an accompanying editorial (JAMA. 2018;319:123-4).
“Over the past 15 years, more than 400 clinical trials of therapeutics for Alzheimer’s disease have been registered, with a failure rate of nearly 100%. ... The lack of progress in the treatment and prevention of Alzheimer disease is frustrating for patients, families, physicians, researchers, industry, funders, and policy makers. Understanding the causes for these failures is essential for informing future trials.”
This task, however, is daunting. Researchers continue to unfold the complexity of Alzheimer’s disease, which is increasingly acknowledged as much more than a load of sticky protein in the brain, Dr. Bennett wrote.
“Clinical and pathological findings from community-based studies that incorporate brain autopsy find that clinically evident Alzheimer disease dementia is a function of multiple pathological abnormalities adding to and interacting with multiple resilience factors (e.g., synaptic proteins), further complicating strategies for clinical trial design and drug discovery. Some studies suggest that the comorbid pathological abnormalities account for an equal amount of dementia, perhaps even more than Alzheimer disease pathology, collectively ... These data suggest that much of the age-related loss of cognition and dementia is unexplained. Thus, treatments that affect any single pathology are unlikely to have a major effect on the occurrence of clinically diagnosed Alzheimer disease dementia.”
Nevertheless, Dr. Bennett predicts that researchers will ultimately succeed in finding an effective treatment for Alzheimer’s.
“Given the series of failures in rigorous attempts to develop an effective treatment for Alzheimer disease, it may seem difficult to be optimistic, yet lessons from the past century paint a different picture.”
He likened the current research situation to the early days of President Nixon’s “War on Cancer,” launched in the early 1970s. Once that public commitment was made, funding opportunities followed, research surged, and successes followed.
“Since then, numerous treatments for cancer are now available that were unimaginable 45 years ago.”
The 2011 National Alzheimer’s Project Act is even now fostering a similar research environment, Dr. Bennett said. Federal funding for Alzheimer’s research topped out at $1.4 billion in 2017 – a new high.
“This is a worldwide effort with many countries creating plans to counteract dementia and both governments and industry increasing research funding in this area. In addition, despite the complexity of the disease, the field is generating new knowledge at an unprecedented pace. It is just a matter of time before that knowledge is translated into effective strategies for the treatment and prevention of Alzheimer disease dementia.”
Dr. Bennett is the Robert C. Borwell Professor of Neurological Science and director of the Rush Alzheimer’s Disease Center, Rush University, Chicago. He reported serving on study committees for Takeda and AbbVie.
Idalopirdine’s failure is an all-too-familiar theme in Alzheimer’s research: a drug with a rational therapeutic target, which performed reasonable well in early clinical trials, but fell apart in large phase 3 studies, David Bennett, MD, wrote in an accompanying editorial (JAMA. 2018;319:123-4).
“Over the past 15 years, more than 400 clinical trials of therapeutics for Alzheimer’s disease have been registered, with a failure rate of nearly 100%. ... The lack of progress in the treatment and prevention of Alzheimer disease is frustrating for patients, families, physicians, researchers, industry, funders, and policy makers. Understanding the causes for these failures is essential for informing future trials.”
This task, however, is daunting. Researchers continue to unfold the complexity of Alzheimer’s disease, which is increasingly acknowledged as much more than a load of sticky protein in the brain, Dr. Bennett wrote.
“Clinical and pathological findings from community-based studies that incorporate brain autopsy find that clinically evident Alzheimer disease dementia is a function of multiple pathological abnormalities adding to and interacting with multiple resilience factors (e.g., synaptic proteins), further complicating strategies for clinical trial design and drug discovery. Some studies suggest that the comorbid pathological abnormalities account for an equal amount of dementia, perhaps even more than Alzheimer disease pathology, collectively ... These data suggest that much of the age-related loss of cognition and dementia is unexplained. Thus, treatments that affect any single pathology are unlikely to have a major effect on the occurrence of clinically diagnosed Alzheimer disease dementia.”
Nevertheless, Dr. Bennett predicts that researchers will ultimately succeed in finding an effective treatment for Alzheimer’s.
“Given the series of failures in rigorous attempts to develop an effective treatment for Alzheimer disease, it may seem difficult to be optimistic, yet lessons from the past century paint a different picture.”
He likened the current research situation to the early days of President Nixon’s “War on Cancer,” launched in the early 1970s. Once that public commitment was made, funding opportunities followed, research surged, and successes followed.
“Since then, numerous treatments for cancer are now available that were unimaginable 45 years ago.”
The 2011 National Alzheimer’s Project Act is even now fostering a similar research environment, Dr. Bennett said. Federal funding for Alzheimer’s research topped out at $1.4 billion in 2017 – a new high.
“This is a worldwide effort with many countries creating plans to counteract dementia and both governments and industry increasing research funding in this area. In addition, despite the complexity of the disease, the field is generating new knowledge at an unprecedented pace. It is just a matter of time before that knowledge is translated into effective strategies for the treatment and prevention of Alzheimer disease dementia.”
Dr. Bennett is the Robert C. Borwell Professor of Neurological Science and director of the Rush Alzheimer’s Disease Center, Rush University, Chicago. He reported serving on study committees for Takeda and AbbVie.
Idalopirdine’s failure is an all-too-familiar theme in Alzheimer’s research: a drug with a rational therapeutic target, which performed reasonable well in early clinical trials, but fell apart in large phase 3 studies, David Bennett, MD, wrote in an accompanying editorial (JAMA. 2018;319:123-4).
“Over the past 15 years, more than 400 clinical trials of therapeutics for Alzheimer’s disease have been registered, with a failure rate of nearly 100%. ... The lack of progress in the treatment and prevention of Alzheimer disease is frustrating for patients, families, physicians, researchers, industry, funders, and policy makers. Understanding the causes for these failures is essential for informing future trials.”
This task, however, is daunting. Researchers continue to unfold the complexity of Alzheimer’s disease, which is increasingly acknowledged as much more than a load of sticky protein in the brain, Dr. Bennett wrote.
“Clinical and pathological findings from community-based studies that incorporate brain autopsy find that clinically evident Alzheimer disease dementia is a function of multiple pathological abnormalities adding to and interacting with multiple resilience factors (e.g., synaptic proteins), further complicating strategies for clinical trial design and drug discovery. Some studies suggest that the comorbid pathological abnormalities account for an equal amount of dementia, perhaps even more than Alzheimer disease pathology, collectively ... These data suggest that much of the age-related loss of cognition and dementia is unexplained. Thus, treatments that affect any single pathology are unlikely to have a major effect on the occurrence of clinically diagnosed Alzheimer disease dementia.”
Nevertheless, Dr. Bennett predicts that researchers will ultimately succeed in finding an effective treatment for Alzheimer’s.
“Given the series of failures in rigorous attempts to develop an effective treatment for Alzheimer disease, it may seem difficult to be optimistic, yet lessons from the past century paint a different picture.”
He likened the current research situation to the early days of President Nixon’s “War on Cancer,” launched in the early 1970s. Once that public commitment was made, funding opportunities followed, research surged, and successes followed.
“Since then, numerous treatments for cancer are now available that were unimaginable 45 years ago.”
The 2011 National Alzheimer’s Project Act is even now fostering a similar research environment, Dr. Bennett said. Federal funding for Alzheimer’s research topped out at $1.4 billion in 2017 – a new high.
“This is a worldwide effort with many countries creating plans to counteract dementia and both governments and industry increasing research funding in this area. In addition, despite the complexity of the disease, the field is generating new knowledge at an unprecedented pace. It is just a matter of time before that knowledge is translated into effective strategies for the treatment and prevention of Alzheimer disease dementia.”
Dr. Bennett is the Robert C. Borwell Professor of Neurological Science and director of the Rush Alzheimer’s Disease Center, Rush University, Chicago. He reported serving on study committees for Takeda and AbbVie.
Idalopirdine suffered the final nail in its coffin with the complete release of its phase 3 data detailing its failure to improve cognitive outcomes in patients with mild to moderate Alzheimer’s disease.
The 5-HT6 receptor antagonist idalopirdine was given on a background of stable cholinesterase inhibitor therapy in three Lundbeck-sponsored phase 3 trials: STARSHINE, STARBEAM, and STARBRIGHT. But none of the STAR studies reproduced the results of idalopirdine’s modestly successful phase 2 study, LADDER, wrote Alireza Atri, MD, PhD, and his colleagues. The report appears Jan. 9 in JAMA.
STARSHINE, STARBEAM, and STARBRIGHT were all 24-week, fixed-dose, randomized placebo-controlled studies with the same endpoint: change on the Alzheimer’s Disease Cooperative Scale–cognitive (ADAS-cog) measure. Together, they enrolled 2,525 patients with mild to moderate AD. Patients were a mean of 74 years old, with a mean Mini Mental State Exam Score of 17-18 and a mean baseline ADAS-cog of 26.
Study 1 (STARSHINE) randomized patients to background donepezil plus placebo, or idalopirdine 30 mg or 60 mg. Study 2 (STARBEAM) randomized patients to background donepezil plus placebo or idalopirdine 10 mg or 30 mg. Study 3 (STARBRIGHT) randomized patients to background donepezil, rivastigmine, or galantamine plus placebo or 60 mg idalopirdine.
Cohort retention was good in all three studies, with about a 9% dropout rate for those taking placebo, 10% for those taking 10 mg or 30 mg idalopirdine, and 11% for those taking the 60-mg dose. The adverse event profile was also acceptable. However, there were no statistically significant cognitive improvements in any study.
In study 1, the mean 24-week change in ADAS-cog total score was 0.37 for the 60-mg group, 0.61 for the 30-mg group, and 0.41 for the placebo group. Compared with placebo, the mean difference in ADAS-cog score change was 0.05 for the 60-mg dose group and 0.33 for the 30-mg group.
In study 2, the mean 24-week change in ADAS-cog score was 1.01 for the 30-mg group, 0.53 for the 10-mg group, and 0.56 for the placebo group. Compared with placebo, the adjusted mean difference in ADAS-cog was 0.63 for the 30-mg group and −0.09 for the 10-mg group.
In study 3, the mean ADAS-cog change was 0.38 for the 60-mg group and 0.82 for the placebo group. Compared with placebo, the mean difference was –0.55.
Adverse events were similar across the studies. The most common treatment-related adverse events were accidental overdose (idalopirdine treatment groups: 5%-11%; placebo: 9%-12%). Falls were the next most common (idalopirdine treatment groups: 4%-6%; placebo: 3%-6%). Cholinergic adverse events were also more common among those taking the study drug, with nausea and vomiting occurring in up to 4% of patients. About 5%-7% of patients taking idalopirdine discontinued because of a treatment-emergent adverse event, compared with 3%-5% of those taking placebo.
Five patients taking idalopirdine and three taking placebo died during the study; no death was related to the study drug. There was no indication of suicidal ideation or behavior associated with idalopirdine.
One striking difference between the modestly successful phase 2 and the clearly negative phase 3 studies was dosage, Dr. Atri noted. LADDER tested 90 mg of idalopirdine, split into three 30-mg doses each day. The STAR-series opted for a lower dose because PET studies on healthy volunteers showed high binding on the 5-HT6 receptors (more than 80%) at both the 30- and 60-mg doses.
“Although there is an approximate 40% decrease in 5-HT6 receptor expression among patients with Alzheimer disease compared with healthy individuals, there are also potential limitations in translating occupancy data from healthy individuals to those with a diseased brain,” the authors noted.
Based on the soundly negative data, and disappointing results with idalopirdine’s close competitor, intepirdine, it may be time to retire this area of investigation entirely, Dr. Atri concluded.
“Placing the results of this study in the broader context of the 5-HT6 antagonism adjunctive to cholinesterase inhibitor therapy mechanism of action suggests a lack of efficacy for this approach in the treatment of Alzheimer disease. In the phase 3 MINDSET study, intepirdine (another 5-HT6 antagonist) was administered at a dose of 35 mg daily added to background donepezil therapy in patients with mild to moderate Alzheimer disease and it failed to meet cognitive and functional efficacy outcomes.”
As if on cue with the idalopirdine data, Axovant Life Sciences, the New York company developing intepirdine, announced on Jan. 8 that it would shelve that drug. The announcement came on the heels of negative findings in its last best-hope studies aimed at patients with Lewy body dementia.
In the HEADWAY Lewy body dementia study, neither 35 mg nor 70 mg of intepirdine significantly improved cognition, compared with placebo. The 70-mg dose was associated with a small but insignificant improvement in motor function, but the 35-mg dose was associated with a 2-point worsening.
In a phase 2 study of intepirdine in patients with dementia and gait impairment, 35 mg of intepirdine did not improve gait speed.
“Based on the totality of intepirdine data to date, there is no evidence to support its further development. We are incredibly disappointed and saddened for the millions of people living with these difficult conditions, and are deeply grateful to the patients, caregivers and investigators who participated in our trials,” David Hung, MD, chief executive officer of Axovant, said in a press statement.
Dr. Atri reported financial relationships with numerous pharmaceutical companies, including Lundbeck, which sponsored the STAR trials.
This article was updated 1/12/18.
Idalopirdine suffered the final nail in its coffin with the complete release of its phase 3 data detailing its failure to improve cognitive outcomes in patients with mild to moderate Alzheimer’s disease.
The 5-HT6 receptor antagonist idalopirdine was given on a background of stable cholinesterase inhibitor therapy in three Lundbeck-sponsored phase 3 trials: STARSHINE, STARBEAM, and STARBRIGHT. But none of the STAR studies reproduced the results of idalopirdine’s modestly successful phase 2 study, LADDER, wrote Alireza Atri, MD, PhD, and his colleagues. The report appears Jan. 9 in JAMA.
STARSHINE, STARBEAM, and STARBRIGHT were all 24-week, fixed-dose, randomized placebo-controlled studies with the same endpoint: change on the Alzheimer’s Disease Cooperative Scale–cognitive (ADAS-cog) measure. Together, they enrolled 2,525 patients with mild to moderate AD. Patients were a mean of 74 years old, with a mean Mini Mental State Exam Score of 17-18 and a mean baseline ADAS-cog of 26.
Study 1 (STARSHINE) randomized patients to background donepezil plus placebo, or idalopirdine 30 mg or 60 mg. Study 2 (STARBEAM) randomized patients to background donepezil plus placebo or idalopirdine 10 mg or 30 mg. Study 3 (STARBRIGHT) randomized patients to background donepezil, rivastigmine, or galantamine plus placebo or 60 mg idalopirdine.
Cohort retention was good in all three studies, with about a 9% dropout rate for those taking placebo, 10% for those taking 10 mg or 30 mg idalopirdine, and 11% for those taking the 60-mg dose. The adverse event profile was also acceptable. However, there were no statistically significant cognitive improvements in any study.
In study 1, the mean 24-week change in ADAS-cog total score was 0.37 for the 60-mg group, 0.61 for the 30-mg group, and 0.41 for the placebo group. Compared with placebo, the mean difference in ADAS-cog score change was 0.05 for the 60-mg dose group and 0.33 for the 30-mg group.
In study 2, the mean 24-week change in ADAS-cog score was 1.01 for the 30-mg group, 0.53 for the 10-mg group, and 0.56 for the placebo group. Compared with placebo, the adjusted mean difference in ADAS-cog was 0.63 for the 30-mg group and −0.09 for the 10-mg group.
In study 3, the mean ADAS-cog change was 0.38 for the 60-mg group and 0.82 for the placebo group. Compared with placebo, the mean difference was –0.55.
Adverse events were similar across the studies. The most common treatment-related adverse events were accidental overdose (idalopirdine treatment groups: 5%-11%; placebo: 9%-12%). Falls were the next most common (idalopirdine treatment groups: 4%-6%; placebo: 3%-6%). Cholinergic adverse events were also more common among those taking the study drug, with nausea and vomiting occurring in up to 4% of patients. About 5%-7% of patients taking idalopirdine discontinued because of a treatment-emergent adverse event, compared with 3%-5% of those taking placebo.
Five patients taking idalopirdine and three taking placebo died during the study; no death was related to the study drug. There was no indication of suicidal ideation or behavior associated with idalopirdine.
One striking difference between the modestly successful phase 2 and the clearly negative phase 3 studies was dosage, Dr. Atri noted. LADDER tested 90 mg of idalopirdine, split into three 30-mg doses each day. The STAR-series opted for a lower dose because PET studies on healthy volunteers showed high binding on the 5-HT6 receptors (more than 80%) at both the 30- and 60-mg doses.
“Although there is an approximate 40% decrease in 5-HT6 receptor expression among patients with Alzheimer disease compared with healthy individuals, there are also potential limitations in translating occupancy data from healthy individuals to those with a diseased brain,” the authors noted.
Based on the soundly negative data, and disappointing results with idalopirdine’s close competitor, intepirdine, it may be time to retire this area of investigation entirely, Dr. Atri concluded.
“Placing the results of this study in the broader context of the 5-HT6 antagonism adjunctive to cholinesterase inhibitor therapy mechanism of action suggests a lack of efficacy for this approach in the treatment of Alzheimer disease. In the phase 3 MINDSET study, intepirdine (another 5-HT6 antagonist) was administered at a dose of 35 mg daily added to background donepezil therapy in patients with mild to moderate Alzheimer disease and it failed to meet cognitive and functional efficacy outcomes.”
As if on cue with the idalopirdine data, Axovant Life Sciences, the New York company developing intepirdine, announced on Jan. 8 that it would shelve that drug. The announcement came on the heels of negative findings in its last best-hope studies aimed at patients with Lewy body dementia.
In the HEADWAY Lewy body dementia study, neither 35 mg nor 70 mg of intepirdine significantly improved cognition, compared with placebo. The 70-mg dose was associated with a small but insignificant improvement in motor function, but the 35-mg dose was associated with a 2-point worsening.
In a phase 2 study of intepirdine in patients with dementia and gait impairment, 35 mg of intepirdine did not improve gait speed.
“Based on the totality of intepirdine data to date, there is no evidence to support its further development. We are incredibly disappointed and saddened for the millions of people living with these difficult conditions, and are deeply grateful to the patients, caregivers and investigators who participated in our trials,” David Hung, MD, chief executive officer of Axovant, said in a press statement.
Dr. Atri reported financial relationships with numerous pharmaceutical companies, including Lundbeck, which sponsored the STAR trials.
This article was updated 1/12/18.
FROM JAMA
Key clinical point:
Major finding: None of the trio of phase 3 trials showed any cognitive benefit associated with the drug.
Study details: The studies randomized more than 2,000 patients to placebo plus idalopirdine 10, 30, or 60 mg on background cholinesterase inhibitor medication.
Disclosures: Dr. Atri disclosed financial relationships with numerous pharmaceutical companies, including Lundbeck, which sponsored the trials.
Source: Atri A et al., JAMA. 2018;319(2):130-42
FDA cites manufacturer of autologous stem cells for regulatory, manufacturing missteps
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
for manufacturing processes that may compromise its safety and for failing to toe the regulatory line in marketing.
American CryoStem received an FDA warning letter Jan. 3 demanding that the company comply with best-manufacturing processes and obtain an investigational new drug application if it wishes to continue marketing ATCELL for its currently advertised clinical indications and administration routes. These include intravenous, intrathecal, or aerosol inhalation of the product for anoxic brain injury, Parkinson’s disease, amyotrophic lateral sclerosis, stroke, and multiple sclerosis.
“Please be advised that, to lawfully market a drug that is a biological product, a valid biologics license must be in effect,” noted the letter. “Such licenses are issued only after a showing that the product is safe, pure, and potent. While in the development stage, such products may be distributed for clinical use in humans only if the sponsor has an investigational new drug application (IND) in effect as specified by FDA regulations. ATCELL is not the subject of an approved biologics license application nor is there an IND in effect. Based on this information, we have determined that your actions have violated the Food, Drug, and Cosmetic Act and the Public Health Service Act.”
FDA inspectors conducted a site inspection of American CryoStem in Eatontown, N.J., last summer, during which they “documented evidence of significant deviations from current good manufacturing practice.” The agency then provided the company a chance to respond to these issues. The new warning letter discussed each complaint, noting that some were inadequately addressed, and demanded that the company take action within 15 working days or face potential legal process, including seizure and/or injunction.
American CryoStem is one of the first companies to experience increased scrutiny under FDA’s new commitment to regulate the rapid growth and development of regenerative medicine products, which include novel cellular therapies, with the aim of ensuring their safety and effectiveness.
The new policy is designed to support the potential of cellular rejuvenation medicine, while protecting patients from “unscrupulous actors” who might endanger public health with untested products, according to FDA Commissioner Scott Gottlieb, MD. As enthusiasm for stem cell treatments surges, so are reports of adverse events. The New England Journal of Medicine recently reported on three patients with age-related macular degeneration who were blinded by intravitreal injection of autologous adipose-derived stem cells (N Engl J Med. 2017;376:1047-53).
Under the new policy, cell- and tissue-based products could be exempt from FDA premarket review only if they are removed from and implanted back into the same patient in their original form, or if the products are “minimally manipulated.” ATCELL fulfills neither qualification, the FDA warning letter said.
“You process adipose tissue ... to isolate cellular components of adipose tissue, commonly referred to as stromal vascular fraction [SVF]. Such processing is more than minimal manipulation because [it alters] the original relevant characteristics of the [tissue] relating to its utility for reconstruction, repair, or replacement. Then you process the SVF by expanding it in cell culture to manufacture ATCELL. Such expansion also is more than minimal manipulation because it alters the original relevant characteristics of the tissue.”
Furthermore, the letter noted, at least one of the components used in the clonal expansion process is investigational and not intended for human use. The manufacturer of that component, which was not named, “indicates the following: ‘Unless otherwise stated in our catalog or other company documentation accompanying the product(s), our products are intended for research use only and are not to be used for any other purpose, which includes but is not limited to, unauthorized commercial uses, in vitro diagnostic uses, ex vivo or in vivo therapeutic uses or any type of consumption or application to human and animals.”
The FDA also took exception with several equipment and lab safety issues. ATCELL was being created in areas that had no clean space designation – a serious concern, the letter said.
“American CryoStem’s unvalidated processes, inadequately controlled environment, lack of control of components used in production, and lack of sufficient and validated product testing ... pose a significant risk that ATCELL may be contaminated with microorganisms or have other serious product quality defects ... Because the product is administered to humans by various higher risk routes of administration, including intravenously, intrathecally, and by aerosol inhalation, if contaminated, its use could cause a range of adverse events, from infections to death.”
FDA also expressed concerns over a lack of consistent quality control testing of each batch and questioned whether the company’s method of shipping ATCELL to clinicians had been adequately validated.
Finally, the agency raised concerns that ATCELL, while it is labeled as being for research purposes only, may harm patients indirectly by preventing them from seeking timely treatment with proven therapies.
“ATCELL is intended to treat a variety of serious or life-threatening diseases or conditions, all of which are non-homologous uses,” the warning letter noted. “Such uses raise potential significant safety concerns because there is less basis on which to predict the product’s behavior in the recipient, and use of these unapproved products may cause users to delay or discontinue medical treatments that have been found safe and effective.”
SOURCE: FDA warning letter
Tau imaging predicts looming cognitive decline in cognitively normal elderly
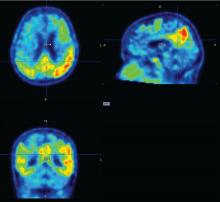
BOSTON – Progressive tau accumulation in the temporal lobe of cognitively normal older adults was associated with cognitive decline over time in a prospective, longitudinal study presented at the Clinical Trials on Alzheimer’s Disease conference.
This track of cognitive impairment following tau pathology in a preclinical Alzheimer’s disease (AD) population suggests two roles for serial positron emission tomography (PET) scans with a tau binding agent, Bernard Hanseeuw, MD, PhD, said at the meeting. In the near future, they could be used to track therapeutic response in clinical trials. Farther out, if future validation studies confirm these preliminary results, they might be a useful clinical tool for predicting how fast an individual Alzheimer’s patient will progress, he said in an interview.
Serial tau scans, however, would, he said.
“Every patient with Alzheimer’s disease is different, with a different disease course. Amyloid scans can tell us if someone is on the wrong path, but tau scans could tell us how fast they are going. If you have Alzheimer’s, it’s important to know if you may not be able to live in your own home in a year. With tau PET, we could track the disease and predict how fast it might evolve. That is very clinically relevant,” said Dr. Hanseeuw.
Tau imaging remains investigational only. Several tau imaging agents are being developed, but none has yet been approved in the United States or in Europe.
To investigate the correlation of tau and cognitive decline in preclinical Alzheimer’s, Dr. Hanseeuw examined serial tau and amyloid PET scans conducted on 60 clinically normal older adults with a mean age of 75 years. About one-third of the cohort was positive for the APOE4 allele. All of them had a baseline Clinical Dementia Rating (CDR) score of 0 and a mean Mini-Mental State Exam score of at least 27. They also scored in the normal range on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the WAIS-R Digit Symbol Substitution Test, Mini-Mental State Exam, Free and Cued Selective Reminding Test, and Logical Memory IIA Delayed Recall, and correlates well with amyloid accumulation in the brain.
The study included up to 4 years of data on cognition and amyloid PET imaging, and up to 3 years of tau PET imaging data. The investigators assessed amyloid as a whole-brain aggregate and tau in the bilateral inferior temporal neocortex. “This is where the change is most happening in patients, and it’s a place where relatively few normal elderly would have tau,” Dr. Hanseeuw said. All of the analyses controlled for age, sex, and years of education.
Baseline amyloid levels were low in 36 participants and high in 24. At least some tau was present in all of the subjects. This is not an unexpected finding, since tau accumulates with age, Dr. Hanseeuw said. Over the study period, six subjects progressed to a CDR of 0.5 – a rating consistent with mild cognitive impairment. At baseline, high tau and high amyloid levels were both associated with a progressive decline in PACC scores in the following years. However, the rate of change in tau predicted change in cognition better than did the baseline measurements. In contrast, the rate of change in amyloid was not associated with cognitive decline.
“What is interesting here is that tau changed four times faster than amyloid,” Dr. Hanseeuw said. “The average subject needed 5 years to change 1 standard deviation in tau, but would have needed 20 years to change 1 standard deviation in amyloid.”
Fast-changing outcomes are important to accelerate drug assessment in clinical trials. Currently, it takes 3-5 years to conduct most anti-AD trials, he added.
Dr. Hanseeuw had no relevant financial disclosures.
BOSTON – Progressive tau accumulation in the temporal lobe of cognitively normal older adults was associated with cognitive decline over time in a prospective, longitudinal study presented at the Clinical Trials on Alzheimer’s Disease conference.
This track of cognitive impairment following tau pathology in a preclinical Alzheimer’s disease (AD) population suggests two roles for serial positron emission tomography (PET) scans with a tau binding agent, Bernard Hanseeuw, MD, PhD, said at the meeting. In the near future, they could be used to track therapeutic response in clinical trials. Farther out, if future validation studies confirm these preliminary results, they might be a useful clinical tool for predicting how fast an individual Alzheimer’s patient will progress, he said in an interview.
Serial tau scans, however, would, he said.
“Every patient with Alzheimer’s disease is different, with a different disease course. Amyloid scans can tell us if someone is on the wrong path, but tau scans could tell us how fast they are going. If you have Alzheimer’s, it’s important to know if you may not be able to live in your own home in a year. With tau PET, we could track the disease and predict how fast it might evolve. That is very clinically relevant,” said Dr. Hanseeuw.
Tau imaging remains investigational only. Several tau imaging agents are being developed, but none has yet been approved in the United States or in Europe.
To investigate the correlation of tau and cognitive decline in preclinical Alzheimer’s, Dr. Hanseeuw examined serial tau and amyloid PET scans conducted on 60 clinically normal older adults with a mean age of 75 years. About one-third of the cohort was positive for the APOE4 allele. All of them had a baseline Clinical Dementia Rating (CDR) score of 0 and a mean Mini-Mental State Exam score of at least 27. They also scored in the normal range on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the WAIS-R Digit Symbol Substitution Test, Mini-Mental State Exam, Free and Cued Selective Reminding Test, and Logical Memory IIA Delayed Recall, and correlates well with amyloid accumulation in the brain.
The study included up to 4 years of data on cognition and amyloid PET imaging, and up to 3 years of tau PET imaging data. The investigators assessed amyloid as a whole-brain aggregate and tau in the bilateral inferior temporal neocortex. “This is where the change is most happening in patients, and it’s a place where relatively few normal elderly would have tau,” Dr. Hanseeuw said. All of the analyses controlled for age, sex, and years of education.
Baseline amyloid levels were low in 36 participants and high in 24. At least some tau was present in all of the subjects. This is not an unexpected finding, since tau accumulates with age, Dr. Hanseeuw said. Over the study period, six subjects progressed to a CDR of 0.5 – a rating consistent with mild cognitive impairment. At baseline, high tau and high amyloid levels were both associated with a progressive decline in PACC scores in the following years. However, the rate of change in tau predicted change in cognition better than did the baseline measurements. In contrast, the rate of change in amyloid was not associated with cognitive decline.
“What is interesting here is that tau changed four times faster than amyloid,” Dr. Hanseeuw said. “The average subject needed 5 years to change 1 standard deviation in tau, but would have needed 20 years to change 1 standard deviation in amyloid.”
Fast-changing outcomes are important to accelerate drug assessment in clinical trials. Currently, it takes 3-5 years to conduct most anti-AD trials, he added.
Dr. Hanseeuw had no relevant financial disclosures.
BOSTON – Progressive tau accumulation in the temporal lobe of cognitively normal older adults was associated with cognitive decline over time in a prospective, longitudinal study presented at the Clinical Trials on Alzheimer’s Disease conference.
This track of cognitive impairment following tau pathology in a preclinical Alzheimer’s disease (AD) population suggests two roles for serial positron emission tomography (PET) scans with a tau binding agent, Bernard Hanseeuw, MD, PhD, said at the meeting. In the near future, they could be used to track therapeutic response in clinical trials. Farther out, if future validation studies confirm these preliminary results, they might be a useful clinical tool for predicting how fast an individual Alzheimer’s patient will progress, he said in an interview.
Serial tau scans, however, would, he said.
“Every patient with Alzheimer’s disease is different, with a different disease course. Amyloid scans can tell us if someone is on the wrong path, but tau scans could tell us how fast they are going. If you have Alzheimer’s, it’s important to know if you may not be able to live in your own home in a year. With tau PET, we could track the disease and predict how fast it might evolve. That is very clinically relevant,” said Dr. Hanseeuw.
Tau imaging remains investigational only. Several tau imaging agents are being developed, but none has yet been approved in the United States or in Europe.
To investigate the correlation of tau and cognitive decline in preclinical Alzheimer’s, Dr. Hanseeuw examined serial tau and amyloid PET scans conducted on 60 clinically normal older adults with a mean age of 75 years. About one-third of the cohort was positive for the APOE4 allele. All of them had a baseline Clinical Dementia Rating (CDR) score of 0 and a mean Mini-Mental State Exam score of at least 27. They also scored in the normal range on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the WAIS-R Digit Symbol Substitution Test, Mini-Mental State Exam, Free and Cued Selective Reminding Test, and Logical Memory IIA Delayed Recall, and correlates well with amyloid accumulation in the brain.
The study included up to 4 years of data on cognition and amyloid PET imaging, and up to 3 years of tau PET imaging data. The investigators assessed amyloid as a whole-brain aggregate and tau in the bilateral inferior temporal neocortex. “This is where the change is most happening in patients, and it’s a place where relatively few normal elderly would have tau,” Dr. Hanseeuw said. All of the analyses controlled for age, sex, and years of education.
Baseline amyloid levels were low in 36 participants and high in 24. At least some tau was present in all of the subjects. This is not an unexpected finding, since tau accumulates with age, Dr. Hanseeuw said. Over the study period, six subjects progressed to a CDR of 0.5 – a rating consistent with mild cognitive impairment. At baseline, high tau and high amyloid levels were both associated with a progressive decline in PACC scores in the following years. However, the rate of change in tau predicted change in cognition better than did the baseline measurements. In contrast, the rate of change in amyloid was not associated with cognitive decline.
“What is interesting here is that tau changed four times faster than amyloid,” Dr. Hanseeuw said. “The average subject needed 5 years to change 1 standard deviation in tau, but would have needed 20 years to change 1 standard deviation in amyloid.”
Fast-changing outcomes are important to accelerate drug assessment in clinical trials. Currently, it takes 3-5 years to conduct most anti-AD trials, he added.
Dr. Hanseeuw had no relevant financial disclosures.
REPORTING FROM CTAD
Key clinical point:
Major finding: Tau levels changed twice as fast as cognition, suggesting that the protein is a significant marker of future cognitive change.
Data source: A prospective, longitudinal study of 60 cognitively normal subjects.
Disclosures: Dr. Hanseeuw had no relevant financial disclosures.
Source: Hanseeuw B et al. CTAD 2017 Abstract OC2.
Think before you Tweet: Social media guidelines for surgeons aim to prevent Internet regret
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
As Editor of the ACS Communities, I am thrilled to see the RAS paper of social media recommendations. We who did not grow up with a keyboard in our hands can learn valuable and career-saving lessons from our younger colleagues who have had a lifetime of experience with social media.
There’s nothing like social media to get your thoughts “out there,” but the other side of the sword is excellently described in this article. I have seen or had to intervene on each of the subjects mentioned in it while reading through the thousands of posts that the ACS Communities’ users have generated over the last three-and-a-half years. When sitting in front of a screen, we can easily lose sight of the fact that our comments are going out into the real world and how rapidly they might reflect back on us and affect friends, relatives, employers, patients, foreign governments, cultures vastly different from our own, and other breathing, feeling human beings – in short, the entire universe hears regardless of whether the site is “password protected.”
I urge everyone using social media to read these guidelines, laminate them, and put them in their wallets, purses, or somewhere else that’s handy. Being self-aware and insightful in your posts can do a world of good, but a lack thereof can result in an avalanche of harm to yourself or others.
Tyler G. Hughes, MD, FACS, is a clinical professor in the department of surgery and the director of medical education at the Kansas University in Salina, Kan., as well as a Co-Editor of ACS Surgery News.
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
Think before you tweet. That’s what surgeons should remember before they express themselves on social media.
Anger and frustration can prompt ill-advised social media postings that have a big potential for blowback, Heather J. Logghe, MD, FACS, and her colleagues wrote in the Journal of the American College of Surgeons. But so can enthusiasm about posting about a new device or procedure, a fascination with a difficult case, the sense of relief that a patient made it though a harrowing period, or even just the simple joy of tossing back a beer or two with pals at the local watering hole (J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022).
“In a survey of 48 state medical boards, 44 (92%) reported online-related misbehavior with serious disciplinary consequences leading to license restriction, suspension, or revocation. A 2011 study of ‘Physicians on Twitter’ revealed that 10% of the physicians sampled had tweeted potential patient privacy violations. A 2014 study of publicly available Facebook profiles of 319 Midwest residents found 14% had ‘potentially unprofessional content’ and 12.2% had ‘clearly unprofessional’ content, the latter including references to binge drinking, sexually suggestive photos, and HIPAA violations.”
Dr. Logghe, of Thomas Jefferson University, Philadelphia, is a member of the American College of Surgeons’ (ACS’s) social media committee tasked with creating practice recommendations for clinicians’ use of social media. Conducting a literature review was the first step to creating a surgeon-specific document, and the team found seven online behavior guidelines directed at physicians. Groups authoring these papers included the American Medical Association, the Federation of State Medical Boards, the American Congress of Obstetricians and Gynecologists, and several international groups.
Dr. Logghe and her colleagues reviewed each one, synthesized the information, and created a practice recommendation statement specific to the ACS. While not encoded in any professional ethics requirements, “Best Practices for Surgeons’ Social Media Use: Statement of the Resident and Associate Society of the American College of Surgeons” does lay out some common, potentially problematic scenarios and offers some suggestions about how to avoid Internet regret.
Everything discussed in the paper revolves around maintaining a decorous public persona. Professionalism on and off the clock is a key tenet of the recommendations. Definitions of key terms like “professionalism” are an important basis for any practice guideline, but sometimes concepts are not easy to define, the team wrote. “Perhaps the limitation most difficult to address in any formalized guideline is the necessary subjectivity in interpreting what is ‘appropriate’ or ‘professional’ online – or in any other setting,” the authors wrote. The ACS Code of Professional Conduct does not explicitly define either of those terms or discuss the appearance of unprofessional behavior.
In the absence of a plain-and-simple definition, the authors attempted to couch the social media recommendations in terms of ACS’s commitment to maintaining the patient trust. It urges surgeons to “avoid even the appearance of impropriety.”
The practice recommendations touch on a number of areas that are potentially problematic for surgeons, including confidentiality, financial conflicts, collegial support, and general social responsibility.
Confidentiality
Maintaining privacy is more than a courtesy to patients: It’s a federally mandated law with serious punitive repercussions if violated. Blogs, YouTube, Twitter, and Facebook offer a vast potential for sharing information with and educating the public, but postings can also easily violate HIPPA standards, the team wrote.
“In general, most social media platforms are not HIPPA-compliant,” no matter how the privacy settings are adjusted. These modes of communication are never appropriate for patient-physician communication: They can’t be archived in an electronic health record, and it is ill advised to give any medical advice by using these channels.
Discussing a particular case online, even with the usual defining details omitted, can be a bad idea.“Simply de-identifying patient information may not be sufficient. When posting information online, one must be cognizant of the context of other information available online. Such information includes the poster’s place of employment, news media, and publicly available vital statistics. Therefore even when posting general comments about hospital events, surgical cases, or patients under one’s care, it is essential to consider the sum of information available to the reader, rather than simply the information shared in the isolated post.”
Employment
Most employers have social media guidelines and don’t take kindly to violations – which can affect both current and future job postings. “A strong social media presence can be of benefit to one’s employer, [but] content that portrays a surgeon in an unprofessional or controversial light can be detrimental and even career-damaging.”
This reaches beyond professional communications online and deep into a surgeon’s personal life, the team noted, so exercise caution when “friending.”
“While this practice is inevitable, surgeons should be aware of potential conflicts. Connecting with or accepting friend requests from some but not all coworkers or coresidents could be interpreted as favoritism and may create a problematic work relationship. … Surgeons should consider primarily connecting with coworkers on professional websites if they have little contact with them outside the workplace.”
As for friending patients – just don’t, for both your sake and theirs. “Accepting a patient’s Facebook friend request may allow them access to events, details, and commentary not traditionally appropriate for the patient-physician relationship. Accepting such requests is strongly discouraged. If concerned about appearing rude or rejecting a patient’s request to be Facebook friends, the patient can be referred to society guidelines or best practices such as these.” One helpful alternative to such a request may be to invite patients to follow a practice website or other professional page.
Conflicts of interest
Online friends might not require disclosures when a surgeon posts about an exciting procedure or piece of equipment, such as whether there is a financial interest in doing so, but it’s important to be proactive. “As always, it is the physician’s responsibility to avoid even the appearance of impropriety. If it is not feasible to include a relevant conflict of interest within a post, the post should not be made.”
Defamation
Irritated about a colleague? Keep it to yourself – especially if you’ve had a beer. “It is never appropriate to post derogatory comments about patients or colleagues. Surgeons should be careful not to post in anger or under the influence of any substance. Statements about a colleague’s abilities, experience, or outcomes intended in jest may be appropriate for the surgeon’s lounge, yet entirely inappropriate for public consumption. Again, the ‘pause-before-posting’ practice is likely to prevent regretful posts in this vein.”
Privacy and Permanence
The Internet goes everywhere and lasts forever. A snappy quote that’s funny at 2 a.m. might not seem so hilarious in the light of day – or even in the light of a day 5 years yet to come.
The delete key is a false friend, and that clever pseudonym you dreamed up is probably as crackable as the classic “Pa55word” password. “One should presume that all content posted online will remain there forever and may be seen by anyone. Again, ‘pause-before-posting’ is a recommended practice.”
Privacy settings should be viewed as an illusion, the team noted. In this era of face recognition and tagging, images carry just as much risk as words.
Collegial support
Maybe your mother was right when she said, “This is for your own good.” If a colleague’s postings are getting out of hand, a tactful heart-to-heart might be the best course of action. “As coined by Dr. Sarah Mansfield, ‘Looking after colleagues is an integral element of professional conduct.’ Surgeons who notice colleagues posting unprofessional content that could be damaging to both the colleague and the public’s trust in the profession should discreetly express their concern to the individual, who should then take any appropriate corrective actions. … If the action is in violation of the law or medical board regulations, it should be reported to the appropriate governing bodies.”
Physician, Google Thyself
The team acknowledged that an online presence is virtually a must for professional development. And even if you don’t create a web page, chances are your university or hospital has done it for you. The media is interested in your life, too, and may make mention of your activities – both positive or negative.
“To better understand and control this publicly accessible information, surgeons are encouraged to periodically self-audit themselves online and taking measures to ensure that the information present is accurate and professional.” Some professional service websites are more trustworthy than others. The team encouraged physicians to participate in the ACS professional pages, LinkedIn, Doximity, and ResearchGate.
Not rules – just recommendations
The team stressed that their recommendations aren’t meant to stifle personal expression. Instead, their aim is to prompt a more conscious use of what can be a very powerful tool for both self-expression and professional development.
“The authors recommend no punitive action based on a perceived ‘violation’ of these recommendations alone. While they refer to other guidelines, including laws such as HIPAA, that must be appropriately enforced, these best practices are intended to guide the practicing surgeon in the use of social media rather than act as regulations or encourage reprimand. Rather than encouraging a social media landscape as sterile as the operating theater, the authors hope these recommendations lead to conscious consideration of online behavior, to avoidance of preventable harm, and to recognition of others’ views of their posts.”
None of the authors reported any financial disclosures.
SOURCE: Logghe HJ et al. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.11.022.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
FDA: Laparoscopic power morcellators can spread malignant cells when used in women with occult uterine cancers*
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
Laparoscopic power morcellation appears capable of spreading fulminant uterine malignancies when used to remove uterine fibroids from women who have unsuspected uterine cancers.
A new Food and Drug Administration literature review of 23 studies found consistent evidence that women who undergo surgery using laparoscopic power morcellators (LPMs) for fibroids that were assumed to be benign may have an occult uterine sarcoma or leiomyosarcoma. In the FDA’s literature review of 12 studies from 2014 to 2016, women who received power morcellation were at a significantly increased risk of death, compared with those whose fibroids were removed by other methods.
The findings reaffirm the agency’s 2014 warnings about LPMs:
• LPMs are contraindicated in gynecologic surgery in which the tissue to be morcellated is known or suspected to contain malignancy.
• LPMs are contraindicated for removal of uterine tissue containing suspected fibroids in patients who are peri- or postmenopausal, or in candidates for en bloc tissue removal.
• Boxed warning: Uterine tissue may contain unsuspected cancer. The use of LPMs during fibroid surgery may spread cancer and decrease long-term survival of patients. This information should be shared with patients when considering surgery with the use of these devices.
“We recognize that some health organizations have reported a lower estimate of risk and that some groups continue to request that we scale back our recommendations. However, after looking at all the relevant data, we believe our estimates remain accurate, and our recommendation against the use of this device to remove fibroids in the vast majority of women is appropriate and critical to better protecting these women. We are committed to continuing to review new relevant data to assure patient safety.”
The review determined that 1 in 350 women undergoing hysterectomy or myomectomy for fibroids may have an occult uterine sarcoma, and that 1 in about 500 have an unsuspected leiomyosarcoma. The literature review clearly identified increased risk of uterine cancers and decreased survival when these women are treated with an LPM, as opposed to manual morcellation or en bloc removal.
Twelve studies of women with uterine cancers examined this outcome in comparison groups. LPMs were associated with a 2- to 3-times increased risk of disease recurrence, compared with manual morcellation or other fibroid removal methods. In some studies, disease-free survival was significantly shorter among those who had undergone an LPM procedure; others found a higher risk of death – including, in one study, almost a quintupling of mortality risk by 1 year (crude risk ratio, 4.75).
Device-related malignancies began appearing in 2013; since then, 262 cases have been reported. But after the 2014 warning, use of LPMs in this application has decreased sharply. Two studies examined this, one finding that LPM use in fibroid surgery dropped from 14% to 3% and the other, that it dropped from 11% to 0.02%.
“The agency also continues to recommend that the advantages and risks of using LPMs during fibroid surgery be thoroughly discussed between the patient and physician before surgery,” the paper concluded. “FDA continues to actively encourage and engage in research to evaluate outcomes for a range of treatment options for fibroids and support the development of safer alternatives for providing a minimally invasive approach.”
[email protected]
ADA guidelines embrace heart health
Recent studies that confirm the cardiovascular benefit of some antihyperglycemic agents are shaping the newest therapeutic recommendations for patients with type 2 diabetes and comorbid atherosclerotic cardiovascular disease (ASCVD).
Treatment for these patients – as all with diabetes – should start with lifestyle modifications and metformin. But in its new position statement, the American Diabetes Association now recommends that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the sodium glucose cotransporter-2 (SGLT2) inhibitor empagliflozin or the glucagon-like peptide 1 (GLP-1) agonist liraglutide – to the regimens of patients with diabetes and ASCVD (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
The medications are indicated if, after being treated with lifestyle and metformin therapy, the patient isn’t meeting hemoglobin A1c goals, said Rita R. Kalyani, MD, who led the ADA’s 12-member writing committee. But clinicians may also consider adding these agents for cardiovascular benefit alone, even when glucose control is adequate on a regimen of lifestyle modification and metformin, with dose adjustments as appropriate, she said in an interview.
“A1c remains the main target of sequencing antihyperglycemic therapies, if it’s not reached after 3 months,” said Dr. Kalyani of Johns Hopkins University, Baltimore. “But, it could also be that the provider, after consulting with the patient, feels it’s appropriate to add one of these agents solely for cardioprotective benefit in patients with ASCVD.”
The recommendation to incorporate agents with cardiovascular benefit is related directly to data from two trials, LEADER and EMPA-REG, which support this recommendation. All of these cardiovascular outcome trials included a majority of patients who were already on metformin. “We developed these evidence-based recommendations based on these trials and to appropriately reflect the populations studied,” said Dr. Kalyani.
The 2018 update contains a number of new recommendations; more will be added as new data emerge, since the ADA intends it to be a continuously refreshed “living document.” This makes it especially clinically useful, Paul S. Jellinger, MD, said in an interview. A member of the writing committee of the American Association of Clinical Endocrinologists’ diabetes management guidelines, Dr. Jellinger feels ADA’s previous versions have not been as targeted as this new one and, he hopes, its subsequent iterations.
“This is a nice enhancement of previously published guidelines for diabetes therapy,” said Dr. Jellinger, professor of clinical medicine at the University of Miami. “For the first time, ADA is providing some guidance in terms of which agents to use. It’s definitely more prescriptive than it was in the past, when, unlike the AACE Diabetes Guidelines, it was a palette of choice for clinicians, but with very little guidance about which agent to pick. The guidance for patients with cardiovascular disease in particular is big news because these antihyperglycemic agents showed such a significant cardiovascular benefit in the trials.”
While the document gives a detailed algorithm of advancing therapy in patients with ASCVD, it doesn’t specify a preference for a specific drug class after metformin therapy in patients without ASCVD. Instead, it provides a detailed table listing the drug-specific effects and patient factors to consider when selecting from different classes of antihyperglycemic agents ( SGLT2 inhibitors, GLP-1 agonists, DPP-4 inhibitors, thiazolidinones, sulfonylureas, and insulins). The table notes the drugs’ general efficacy in diabetes, and their impact on hypoglycemia, weight gain, and cardiovascular and renal health. The table also includes the Food and Drug Administration black box warnings that are on some of these medications.
Another helpful feature is a cost comparison of antidiabetic agents, Dr. Kalyani noted. “Last year we added comprehensive cost tables for all the different insulins and noninsulins, and this year we added a second data set of cost information, to assist the provider when prescribing these agents.”
The pricing information is a very important addition to this guideline, and one that clinicians will appreciate, said Richard Hellman, MD, clinical professor of medicine at the University of Missouri–Kansas City.
“In this document, ADA is urging providers of care to ask about whether the cost of their diabetes care is more than they can deal with. They present tables which compare the costs of the current blood glucose lowering agents used in the U.S., and it is plain to see that many patients, without insurance coverage, will find some of the medications unaffordable,” said Dr. Hellman, a past president of AACE. “They also provide data that show half of all patients with diabetes have financial problems,” and he suspects that medication costs are an important component of their financial insecurity.
The document also notes data from the 2017 National Health and Nutrition Examination Survey, which found that 10% of people with diabetes have severe food insecurity and 20% have mild food insecurity (Diabetes Educ. 2017;43:260-71. doi: 10.1177/0145721717699890).
“Another thing the document points out is that two-thirds of the patients who don’t take all their medications due to cost don’t tell their doctor,” Dr. Hellman said. “The ADA is making the point that providers have a responsibility to ask if a patient is not taking certain medications because of the cost. We have so many better tools to manage this disease, but so many of these tools are unaffordable.”
While the treatment algorithm for patients with ASCVD will likely be embraced, another new recommendation may stir the pot a bit, Dr. Hellman noted. The section on cardiovascular disease and risk management sticks to a definition of hypertension as 140/90 mm Hg or higher – a striking diversion from the new 130/80 mm Hg limit set this fall by both the American Heart Association and the American College of Cardiology.
“This difference in recommendations is very important and will be controversial,” Dr. Hellman said, adding that he agrees with this clinical point.
Again, this recommendation is grounded in clinical trials, which suggest that people with diabetes don’t benefit from overly strict blood pressure control. The new AHA/ACC recommendations largely drew on data from the SPRINT trial, which was conducted in an entirely nondiabetic population. “These gave a clear signal that a lower BP target is beneficial to that group,” Dr. Hellman said.
But large well-designed randomized controlled trials of intensive blood pressure lowering in people with diabetes, such as ACCORD-BP, did not demonstrate that intensive blood-pressure lowering targeting a systolic less than120 mm Hg had a significant benefit on the composite primary cardiovascular endpoint. And while the ADVANCE BP trial found that the composite endpoint was improved with intensive blood pressure lowering, the blood pressure level achieved in the intervention group was 136/73 mm Hg.
“This recommendation is based on current evidence for people with diabetes,” Dr. Kalyani said. “We maintain our definition of hypertension as 140/90 mm Hg or higher based on the results of large clinical trials specifically in people with diabetes but emphasize that intensification of antihypertensive therapy to target lower blood pressures (less than 130/80 mm Hg) may be beneficial for high-risk patients with diabetes such as those with cardiovascular disease. We are constantly assessing the evidence and will continue to review the results of new studies for potential incorporation into recommendations in the future.”
Dr. Kalyani and Dr. Hellman had no financial disclosures. Dr. Jellinger has been a speaker for several pharmaceutical companies.
SOURCE: Kalyani R et al. Diabetes Care 2018;41(Suppl. 1):S86-S104 doi: 10.2337/dc18-S009
This article was updated 12/21/17.
Recent studies that confirm the cardiovascular benefit of some antihyperglycemic agents are shaping the newest therapeutic recommendations for patients with type 2 diabetes and comorbid atherosclerotic cardiovascular disease (ASCVD).
Treatment for these patients – as all with diabetes – should start with lifestyle modifications and metformin. But in its new position statement, the American Diabetes Association now recommends that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the sodium glucose cotransporter-2 (SGLT2) inhibitor empagliflozin or the glucagon-like peptide 1 (GLP-1) agonist liraglutide – to the regimens of patients with diabetes and ASCVD (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
The medications are indicated if, after being treated with lifestyle and metformin therapy, the patient isn’t meeting hemoglobin A1c goals, said Rita R. Kalyani, MD, who led the ADA’s 12-member writing committee. But clinicians may also consider adding these agents for cardiovascular benefit alone, even when glucose control is adequate on a regimen of lifestyle modification and metformin, with dose adjustments as appropriate, she said in an interview.
“A1c remains the main target of sequencing antihyperglycemic therapies, if it’s not reached after 3 months,” said Dr. Kalyani of Johns Hopkins University, Baltimore. “But, it could also be that the provider, after consulting with the patient, feels it’s appropriate to add one of these agents solely for cardioprotective benefit in patients with ASCVD.”
The recommendation to incorporate agents with cardiovascular benefit is related directly to data from two trials, LEADER and EMPA-REG, which support this recommendation. All of these cardiovascular outcome trials included a majority of patients who were already on metformin. “We developed these evidence-based recommendations based on these trials and to appropriately reflect the populations studied,” said Dr. Kalyani.
The 2018 update contains a number of new recommendations; more will be added as new data emerge, since the ADA intends it to be a continuously refreshed “living document.” This makes it especially clinically useful, Paul S. Jellinger, MD, said in an interview. A member of the writing committee of the American Association of Clinical Endocrinologists’ diabetes management guidelines, Dr. Jellinger feels ADA’s previous versions have not been as targeted as this new one and, he hopes, its subsequent iterations.
“This is a nice enhancement of previously published guidelines for diabetes therapy,” said Dr. Jellinger, professor of clinical medicine at the University of Miami. “For the first time, ADA is providing some guidance in terms of which agents to use. It’s definitely more prescriptive than it was in the past, when, unlike the AACE Diabetes Guidelines, it was a palette of choice for clinicians, but with very little guidance about which agent to pick. The guidance for patients with cardiovascular disease in particular is big news because these antihyperglycemic agents showed such a significant cardiovascular benefit in the trials.”
While the document gives a detailed algorithm of advancing therapy in patients with ASCVD, it doesn’t specify a preference for a specific drug class after metformin therapy in patients without ASCVD. Instead, it provides a detailed table listing the drug-specific effects and patient factors to consider when selecting from different classes of antihyperglycemic agents ( SGLT2 inhibitors, GLP-1 agonists, DPP-4 inhibitors, thiazolidinones, sulfonylureas, and insulins). The table notes the drugs’ general efficacy in diabetes, and their impact on hypoglycemia, weight gain, and cardiovascular and renal health. The table also includes the Food and Drug Administration black box warnings that are on some of these medications.
Another helpful feature is a cost comparison of antidiabetic agents, Dr. Kalyani noted. “Last year we added comprehensive cost tables for all the different insulins and noninsulins, and this year we added a second data set of cost information, to assist the provider when prescribing these agents.”
The pricing information is a very important addition to this guideline, and one that clinicians will appreciate, said Richard Hellman, MD, clinical professor of medicine at the University of Missouri–Kansas City.
“In this document, ADA is urging providers of care to ask about whether the cost of their diabetes care is more than they can deal with. They present tables which compare the costs of the current blood glucose lowering agents used in the U.S., and it is plain to see that many patients, without insurance coverage, will find some of the medications unaffordable,” said Dr. Hellman, a past president of AACE. “They also provide data that show half of all patients with diabetes have financial problems,” and he suspects that medication costs are an important component of their financial insecurity.
The document also notes data from the 2017 National Health and Nutrition Examination Survey, which found that 10% of people with diabetes have severe food insecurity and 20% have mild food insecurity (Diabetes Educ. 2017;43:260-71. doi: 10.1177/0145721717699890).
“Another thing the document points out is that two-thirds of the patients who don’t take all their medications due to cost don’t tell their doctor,” Dr. Hellman said. “The ADA is making the point that providers have a responsibility to ask if a patient is not taking certain medications because of the cost. We have so many better tools to manage this disease, but so many of these tools are unaffordable.”
While the treatment algorithm for patients with ASCVD will likely be embraced, another new recommendation may stir the pot a bit, Dr. Hellman noted. The section on cardiovascular disease and risk management sticks to a definition of hypertension as 140/90 mm Hg or higher – a striking diversion from the new 130/80 mm Hg limit set this fall by both the American Heart Association and the American College of Cardiology.
“This difference in recommendations is very important and will be controversial,” Dr. Hellman said, adding that he agrees with this clinical point.
Again, this recommendation is grounded in clinical trials, which suggest that people with diabetes don’t benefit from overly strict blood pressure control. The new AHA/ACC recommendations largely drew on data from the SPRINT trial, which was conducted in an entirely nondiabetic population. “These gave a clear signal that a lower BP target is beneficial to that group,” Dr. Hellman said.
But large well-designed randomized controlled trials of intensive blood pressure lowering in people with diabetes, such as ACCORD-BP, did not demonstrate that intensive blood-pressure lowering targeting a systolic less than120 mm Hg had a significant benefit on the composite primary cardiovascular endpoint. And while the ADVANCE BP trial found that the composite endpoint was improved with intensive blood pressure lowering, the blood pressure level achieved in the intervention group was 136/73 mm Hg.
“This recommendation is based on current evidence for people with diabetes,” Dr. Kalyani said. “We maintain our definition of hypertension as 140/90 mm Hg or higher based on the results of large clinical trials specifically in people with diabetes but emphasize that intensification of antihypertensive therapy to target lower blood pressures (less than 130/80 mm Hg) may be beneficial for high-risk patients with diabetes such as those with cardiovascular disease. We are constantly assessing the evidence and will continue to review the results of new studies for potential incorporation into recommendations in the future.”
Dr. Kalyani and Dr. Hellman had no financial disclosures. Dr. Jellinger has been a speaker for several pharmaceutical companies.
SOURCE: Kalyani R et al. Diabetes Care 2018;41(Suppl. 1):S86-S104 doi: 10.2337/dc18-S009
This article was updated 12/21/17.
Recent studies that confirm the cardiovascular benefit of some antihyperglycemic agents are shaping the newest therapeutic recommendations for patients with type 2 diabetes and comorbid atherosclerotic cardiovascular disease (ASCVD).
Treatment for these patients – as all with diabetes – should start with lifestyle modifications and metformin. But in its new position statement, the American Diabetes Association now recommends that clinicians consider adding agents proved to reduce major cardiovascular events and cardiovascular death – such as the sodium glucose cotransporter-2 (SGLT2) inhibitor empagliflozin or the glucagon-like peptide 1 (GLP-1) agonist liraglutide – to the regimens of patients with diabetes and ASCVD (Diabetes Care 2018;41(Suppl. 1):S86-S104. doi: 10.2337/dc18-S009).
The medications are indicated if, after being treated with lifestyle and metformin therapy, the patient isn’t meeting hemoglobin A1c goals, said Rita R. Kalyani, MD, who led the ADA’s 12-member writing committee. But clinicians may also consider adding these agents for cardiovascular benefit alone, even when glucose control is adequate on a regimen of lifestyle modification and metformin, with dose adjustments as appropriate, she said in an interview.
“A1c remains the main target of sequencing antihyperglycemic therapies, if it’s not reached after 3 months,” said Dr. Kalyani of Johns Hopkins University, Baltimore. “But, it could also be that the provider, after consulting with the patient, feels it’s appropriate to add one of these agents solely for cardioprotective benefit in patients with ASCVD.”
The recommendation to incorporate agents with cardiovascular benefit is related directly to data from two trials, LEADER and EMPA-REG, which support this recommendation. All of these cardiovascular outcome trials included a majority of patients who were already on metformin. “We developed these evidence-based recommendations based on these trials and to appropriately reflect the populations studied,” said Dr. Kalyani.
The 2018 update contains a number of new recommendations; more will be added as new data emerge, since the ADA intends it to be a continuously refreshed “living document.” This makes it especially clinically useful, Paul S. Jellinger, MD, said in an interview. A member of the writing committee of the American Association of Clinical Endocrinologists’ diabetes management guidelines, Dr. Jellinger feels ADA’s previous versions have not been as targeted as this new one and, he hopes, its subsequent iterations.
“This is a nice enhancement of previously published guidelines for diabetes therapy,” said Dr. Jellinger, professor of clinical medicine at the University of Miami. “For the first time, ADA is providing some guidance in terms of which agents to use. It’s definitely more prescriptive than it was in the past, when, unlike the AACE Diabetes Guidelines, it was a palette of choice for clinicians, but with very little guidance about which agent to pick. The guidance for patients with cardiovascular disease in particular is big news because these antihyperglycemic agents showed such a significant cardiovascular benefit in the trials.”
While the document gives a detailed algorithm of advancing therapy in patients with ASCVD, it doesn’t specify a preference for a specific drug class after metformin therapy in patients without ASCVD. Instead, it provides a detailed table listing the drug-specific effects and patient factors to consider when selecting from different classes of antihyperglycemic agents ( SGLT2 inhibitors, GLP-1 agonists, DPP-4 inhibitors, thiazolidinones, sulfonylureas, and insulins). The table notes the drugs’ general efficacy in diabetes, and their impact on hypoglycemia, weight gain, and cardiovascular and renal health. The table also includes the Food and Drug Administration black box warnings that are on some of these medications.
Another helpful feature is a cost comparison of antidiabetic agents, Dr. Kalyani noted. “Last year we added comprehensive cost tables for all the different insulins and noninsulins, and this year we added a second data set of cost information, to assist the provider when prescribing these agents.”
The pricing information is a very important addition to this guideline, and one that clinicians will appreciate, said Richard Hellman, MD, clinical professor of medicine at the University of Missouri–Kansas City.
“In this document, ADA is urging providers of care to ask about whether the cost of their diabetes care is more than they can deal with. They present tables which compare the costs of the current blood glucose lowering agents used in the U.S., and it is plain to see that many patients, without insurance coverage, will find some of the medications unaffordable,” said Dr. Hellman, a past president of AACE. “They also provide data that show half of all patients with diabetes have financial problems,” and he suspects that medication costs are an important component of their financial insecurity.
The document also notes data from the 2017 National Health and Nutrition Examination Survey, which found that 10% of people with diabetes have severe food insecurity and 20% have mild food insecurity (Diabetes Educ. 2017;43:260-71. doi: 10.1177/0145721717699890).
“Another thing the document points out is that two-thirds of the patients who don’t take all their medications due to cost don’t tell their doctor,” Dr. Hellman said. “The ADA is making the point that providers have a responsibility to ask if a patient is not taking certain medications because of the cost. We have so many better tools to manage this disease, but so many of these tools are unaffordable.”
While the treatment algorithm for patients with ASCVD will likely be embraced, another new recommendation may stir the pot a bit, Dr. Hellman noted. The section on cardiovascular disease and risk management sticks to a definition of hypertension as 140/90 mm Hg or higher – a striking diversion from the new 130/80 mm Hg limit set this fall by both the American Heart Association and the American College of Cardiology.
“This difference in recommendations is very important and will be controversial,” Dr. Hellman said, adding that he agrees with this clinical point.
Again, this recommendation is grounded in clinical trials, which suggest that people with diabetes don’t benefit from overly strict blood pressure control. The new AHA/ACC recommendations largely drew on data from the SPRINT trial, which was conducted in an entirely nondiabetic population. “These gave a clear signal that a lower BP target is beneficial to that group,” Dr. Hellman said.
But large well-designed randomized controlled trials of intensive blood pressure lowering in people with diabetes, such as ACCORD-BP, did not demonstrate that intensive blood-pressure lowering targeting a systolic less than120 mm Hg had a significant benefit on the composite primary cardiovascular endpoint. And while the ADVANCE BP trial found that the composite endpoint was improved with intensive blood pressure lowering, the blood pressure level achieved in the intervention group was 136/73 mm Hg.
“This recommendation is based on current evidence for people with diabetes,” Dr. Kalyani said. “We maintain our definition of hypertension as 140/90 mm Hg or higher based on the results of large clinical trials specifically in people with diabetes but emphasize that intensification of antihypertensive therapy to target lower blood pressures (less than 130/80 mm Hg) may be beneficial for high-risk patients with diabetes such as those with cardiovascular disease. We are constantly assessing the evidence and will continue to review the results of new studies for potential incorporation into recommendations in the future.”
Dr. Kalyani and Dr. Hellman had no financial disclosures. Dr. Jellinger has been a speaker for several pharmaceutical companies.
SOURCE: Kalyani R et al. Diabetes Care 2018;41(Suppl. 1):S86-S104 doi: 10.2337/dc18-S009
This article was updated 12/21/17.
EXPERT ANALYSIS FROM DIABETES CARE
Up to 47 million Americans may have “preclinical” Alzheimer’s disease, study estimates
A treatment that would cut the risk of developing amyloid plaques in the brain by 50% could save more than 4 million U.S. residents from mild cognitive impairment and 2.5 million from Alzheimer’s disease by 2060.
The conclusion that even modestly effective preventive therapy could vastly improve the Alzheimer’s outlook is especially important given another startling finding in a new mathematical modeling study by Ron Brookmeyer, PhD, and his colleagues: Right now, they assert, .
“This is the first major attempt to forecast these proposed preclinical Alzheimer’s disease and [mild cognitive impairment] due to Alzheimer’s disease numbers. If confirmed, these data provide essential information for public health planning, and for informing and guiding the public and private investment in Alzheimer’s and dementia research. We need more research to confirm the findings from this model, and more Alzheimer’s and dementia research that includes diverse populations.”
In an interview, Dr. Brookmeyer, a biostatistician at the University of California, Los Angeles, attempted to put those numbers into perspective.
“I want to emphasize that of the 47 million with these Alzheimer’s brain changes, but without clinical symptoms, most will not progress to clinical disease during their lifetimes. In fact, perhaps only 1 in 7 will progress to full-blown dementia.”
Nevertheless, the numbers are disturbing and represent a reality that must be confronted and managed proactively if at all possible, Dr. Brookmeyer said.
“The numbers are what they are,” he said. “They may sound alarmist, but I have every confidence in them. And they’re important because they allow us to understand how many people could potentially benefit from treatment, at what point on the disease continuum it would be useful to implement treatment, and how those treatments could impact public health.”
To carry out the modeling, Dr. Brookmeyer extrapolated from data in two prospective longitudinal cohort studies: the Mayo Clinic Study of Aging, and one by Stephanie J. Vos, PhD, of Maastricht (the Netherlands) University.
The Mayo study followed 1,541 cognitively normal older adults and provided data on the rate of transition from normal cognition to mild cognitive impairment (MCI). The study by Dr. Vos and her associates followed 353 subjects with MCI and brain amyloid, and 222 with late MCI as they progressed. It’s the largest prospective study of progression from MCI to AD that also contains data on baseline neurodegeneration and amyloid burden (Brain. 2015;138[5]:1327-38).
“These studies gave us the rates of transition from one state to another,” Dr. Brookmeyer said. “For example; the Mayo study gave us rates of transition from normal to amyloidosis: 3% of normal 60-year-olds will convert to this state every year.”
The Vos study, Dr. Brookmeyer said, determined rates of progression from MCI to Alzheimer’s dementia, given two preclinical states: asymptomatic amyloid brain plaques alone, or plaques with evidence of neurodegeneration and cognitive signs. Both of these transitional states were first defined in 2011 in a joint paper by the Alzheimer’s Association and the National Institute on Aging (Alzheimers Dement. 2011;7[3]:280-92). While acknowledging that the root causes of Alzheimer’s are unknown, and probably multifactorial, the paper hypothesized a pathophysiologic time line beginning with a three-stage preclinical phase:
• Stage 1: Asymptomatic cerebral amyloidosis: amyloid-positive PET brain imaging with an amyloid-binding ligand and/or a cerebrospinal fluid assay with low amyloid-beta 42 in the presence of normal cognition.
• Stage 2: Amyloid positivity and evidence of synaptic dysfunction and/or early neurodegeneration in the presence of normal cognition.
• Stage 3: Amyloid positivity with evidence of neurodegeneration in the presence of subtle cognitive decline.
“Using those definitions, and piecing together the numbers from these studies, we constructed a computer model based on U.S. census population projections to simulate how many people might be in these different states of disease,” Dr. Brookmeyer said.
In 2017, 6 million Americans were in one of the clinical disease states (MCI due to AD, early clinical AD, or late clinical AD). Dr. Brookmeyer and his colleagues predicted that number will grow to 15 million by 2060. Similarly, in 2017, about 47 million Americans were in one of the preclinical AD states: 22 million with amyloidosis, 8.3 million with only neurodegeneration, and 16.2 million with both. He projects that number will increase to 75.7 million by 2060.
The team then remodeled those numbers in three hypothetical intervention scenarios. In general, Alzheimer’s researchers say a treatment that slows decline by at least 30% would have a meaningful clinical, financial, and societal impact. However, Dr. Brookmeyer modeled treatment scenarios with a greater effect than that.
A primary prevention that reduced the annual risk of new amyloidosis by 50% could decrease the prevalence of MCI by about 700,000 in 2060. A secondary prevention strategy that reduced the annual risk progression to MCI by 50% would decrease the prevalence of MCI by more than 2 million and the prevalence of AD by about 3.8 million.
The results were more complicated with a secondary prevention strategy that would reduce annual risk of MCI-AD conversion by 50%. In this scenario, the prevalence of MCI in 2060 would actually increase by 2.8 million, but the prevalence of AD would decrease by 2.5 million.
These scenarios also developed over different time courses, the researchers wrote.
“We find that the highly effective primary prevention strategy resulted in the lowest AD prevalence by the year 2060. However, [it] was associated with the largest AD prevalence in the 15 years immediately after its introduction ... The explanation for this finding is that the full benefits of delaying amyloidosis in terms of reduced AD prevalence are not realized for many years because of the long lag time between amyloidosis and clinical AD. A take-home message is that the full impact on disease burden of primary prevention that targets the early stages of the pathogenesis of AD on clinical disease burden may not be realized for decades.”
Decreasing preclinical conversion to MCI with a secondary prevention strategy would result in the highest AD prevalence reduction for most of the period. But by 2054, the primary prevention strategy would surpass it.
The intervention targeting MCI-AD conversion would reduce AD prevalence the quickest, with a slight decrease in the first 3 years after introduction. “The explanation for this finding is that MCI is proximate to clinical AD diagnosis, and thus, the impact of delaying progression of MCI will be seen relatively quickly on AD prevalence compared to interventions that delay onset of amyloidosis or MCI.”
The study sharply illustrates two futures: one with an unimpeded tsunami of Alzheimer’s cases, and one in which prevention strategies, while not a floodgate, at least stem the tide somewhat. And while researchers hold out hope for the primary and secondary treatments currently in clinical trials, the AD community is nowhere close to finding even a modestly effective therapy.
Seen in this light, Dr. Brookmeyer’s projections are a cry for action, the Alzheimer’s Association statement proclaimed.
“By focusing attention on a concerning reality – that tens of millions of American adults may face the possibility of dementia due to Alzheimer’s disease – the results reported in this new article, if confirmed, illustrate and greatly amplify the need for more research to develop effective treatments and proven prevention strategies for Alzheimer’s disease. This is especially true as we get better at early detection, and are able to more accurately identify people who have the early brain changes associated with Alzheimer’s disease and other dementias.”
Dr. Brookmeyer reported receiving fees from Takeda for serving as a member of a data safety monitoring board.
SOURCE: Brookemeyer R et al. Alzheimers Dement. 2017 Dec 6. doi: 10.1016/j.jalz.2017.10.009
The study by Brookmeyer and colleagues is a logical and thoughtful attempt to “size” the potential impact of Alzheimer’s disease now and in the future, updating “old technology” estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
The attention paid by the Alzheimer’s Association is understandable given its mission of increasing awareness and supporting more funding, but it omits mention of another important article that is showing that dementia rates are actually declining (JAMA Neurol. 2017;74[11]:1345-51) when adjusted for our aging population (observed vs. expected).
In my opinion, we need some rational balance between maintaining public awareness without creating unnecessary panic. There is no question that AD is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises in my mind.
Richard J. Caselli, MD, is professor of neurology at the Mayo Clinic Arizona in Scottsdale. He is also associate director and clinical core director of the Arizona Alzheimer’s Disease Center. He has no relevant disclosures.
The study by Brookmeyer and colleagues is a logical and thoughtful attempt to “size” the potential impact of Alzheimer’s disease now and in the future, updating “old technology” estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
The attention paid by the Alzheimer’s Association is understandable given its mission of increasing awareness and supporting more funding, but it omits mention of another important article that is showing that dementia rates are actually declining (JAMA Neurol. 2017;74[11]:1345-51) when adjusted for our aging population (observed vs. expected).
In my opinion, we need some rational balance between maintaining public awareness without creating unnecessary panic. There is no question that AD is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises in my mind.
Richard J. Caselli, MD, is professor of neurology at the Mayo Clinic Arizona in Scottsdale. He is also associate director and clinical core director of the Arizona Alzheimer’s Disease Center. He has no relevant disclosures.
The study by Brookmeyer and colleagues is a logical and thoughtful attempt to “size” the potential impact of Alzheimer’s disease now and in the future, updating “old technology” estimates based on actual diagnoses with new technologically derived diagnoses of preclinical neurodegenerative states. They acknowledge that the uncertainty in the actual disease burden we will face is centered on the question of conversion rates, which vary between studies and are far less certain in the preclinical stages than the symptomatic ones.
The attention paid by the Alzheimer’s Association is understandable given its mission of increasing awareness and supporting more funding, but it omits mention of another important article that is showing that dementia rates are actually declining (JAMA Neurol. 2017;74[11]:1345-51) when adjusted for our aging population (observed vs. expected).
In my opinion, we need some rational balance between maintaining public awareness without creating unnecessary panic. There is no question that AD is a major public health issue that warrants all the funding we can provide to researchers seeking a cure. How to balance that need with the need to give our population hope that all is not lost when they misplace their keys is the challenge this article raises in my mind.
Richard J. Caselli, MD, is professor of neurology at the Mayo Clinic Arizona in Scottsdale. He is also associate director and clinical core director of the Arizona Alzheimer’s Disease Center. He has no relevant disclosures.
A treatment that would cut the risk of developing amyloid plaques in the brain by 50% could save more than 4 million U.S. residents from mild cognitive impairment and 2.5 million from Alzheimer’s disease by 2060.
The conclusion that even modestly effective preventive therapy could vastly improve the Alzheimer’s outlook is especially important given another startling finding in a new mathematical modeling study by Ron Brookmeyer, PhD, and his colleagues: Right now, they assert, .
“This is the first major attempt to forecast these proposed preclinical Alzheimer’s disease and [mild cognitive impairment] due to Alzheimer’s disease numbers. If confirmed, these data provide essential information for public health planning, and for informing and guiding the public and private investment in Alzheimer’s and dementia research. We need more research to confirm the findings from this model, and more Alzheimer’s and dementia research that includes diverse populations.”
In an interview, Dr. Brookmeyer, a biostatistician at the University of California, Los Angeles, attempted to put those numbers into perspective.
“I want to emphasize that of the 47 million with these Alzheimer’s brain changes, but without clinical symptoms, most will not progress to clinical disease during their lifetimes. In fact, perhaps only 1 in 7 will progress to full-blown dementia.”
Nevertheless, the numbers are disturbing and represent a reality that must be confronted and managed proactively if at all possible, Dr. Brookmeyer said.
“The numbers are what they are,” he said. “They may sound alarmist, but I have every confidence in them. And they’re important because they allow us to understand how many people could potentially benefit from treatment, at what point on the disease continuum it would be useful to implement treatment, and how those treatments could impact public health.”
To carry out the modeling, Dr. Brookmeyer extrapolated from data in two prospective longitudinal cohort studies: the Mayo Clinic Study of Aging, and one by Stephanie J. Vos, PhD, of Maastricht (the Netherlands) University.
The Mayo study followed 1,541 cognitively normal older adults and provided data on the rate of transition from normal cognition to mild cognitive impairment (MCI). The study by Dr. Vos and her associates followed 353 subjects with MCI and brain amyloid, and 222 with late MCI as they progressed. It’s the largest prospective study of progression from MCI to AD that also contains data on baseline neurodegeneration and amyloid burden (Brain. 2015;138[5]:1327-38).
“These studies gave us the rates of transition from one state to another,” Dr. Brookmeyer said. “For example; the Mayo study gave us rates of transition from normal to amyloidosis: 3% of normal 60-year-olds will convert to this state every year.”
The Vos study, Dr. Brookmeyer said, determined rates of progression from MCI to Alzheimer’s dementia, given two preclinical states: asymptomatic amyloid brain plaques alone, or plaques with evidence of neurodegeneration and cognitive signs. Both of these transitional states were first defined in 2011 in a joint paper by the Alzheimer’s Association and the National Institute on Aging (Alzheimers Dement. 2011;7[3]:280-92). While acknowledging that the root causes of Alzheimer’s are unknown, and probably multifactorial, the paper hypothesized a pathophysiologic time line beginning with a three-stage preclinical phase:
• Stage 1: Asymptomatic cerebral amyloidosis: amyloid-positive PET brain imaging with an amyloid-binding ligand and/or a cerebrospinal fluid assay with low amyloid-beta 42 in the presence of normal cognition.
• Stage 2: Amyloid positivity and evidence of synaptic dysfunction and/or early neurodegeneration in the presence of normal cognition.
• Stage 3: Amyloid positivity with evidence of neurodegeneration in the presence of subtle cognitive decline.
“Using those definitions, and piecing together the numbers from these studies, we constructed a computer model based on U.S. census population projections to simulate how many people might be in these different states of disease,” Dr. Brookmeyer said.
In 2017, 6 million Americans were in one of the clinical disease states (MCI due to AD, early clinical AD, or late clinical AD). Dr. Brookmeyer and his colleagues predicted that number will grow to 15 million by 2060. Similarly, in 2017, about 47 million Americans were in one of the preclinical AD states: 22 million with amyloidosis, 8.3 million with only neurodegeneration, and 16.2 million with both. He projects that number will increase to 75.7 million by 2060.
The team then remodeled those numbers in three hypothetical intervention scenarios. In general, Alzheimer’s researchers say a treatment that slows decline by at least 30% would have a meaningful clinical, financial, and societal impact. However, Dr. Brookmeyer modeled treatment scenarios with a greater effect than that.
A primary prevention that reduced the annual risk of new amyloidosis by 50% could decrease the prevalence of MCI by about 700,000 in 2060. A secondary prevention strategy that reduced the annual risk progression to MCI by 50% would decrease the prevalence of MCI by more than 2 million and the prevalence of AD by about 3.8 million.
The results were more complicated with a secondary prevention strategy that would reduce annual risk of MCI-AD conversion by 50%. In this scenario, the prevalence of MCI in 2060 would actually increase by 2.8 million, but the prevalence of AD would decrease by 2.5 million.
These scenarios also developed over different time courses, the researchers wrote.
“We find that the highly effective primary prevention strategy resulted in the lowest AD prevalence by the year 2060. However, [it] was associated with the largest AD prevalence in the 15 years immediately after its introduction ... The explanation for this finding is that the full benefits of delaying amyloidosis in terms of reduced AD prevalence are not realized for many years because of the long lag time between amyloidosis and clinical AD. A take-home message is that the full impact on disease burden of primary prevention that targets the early stages of the pathogenesis of AD on clinical disease burden may not be realized for decades.”
Decreasing preclinical conversion to MCI with a secondary prevention strategy would result in the highest AD prevalence reduction for most of the period. But by 2054, the primary prevention strategy would surpass it.
The intervention targeting MCI-AD conversion would reduce AD prevalence the quickest, with a slight decrease in the first 3 years after introduction. “The explanation for this finding is that MCI is proximate to clinical AD diagnosis, and thus, the impact of delaying progression of MCI will be seen relatively quickly on AD prevalence compared to interventions that delay onset of amyloidosis or MCI.”
The study sharply illustrates two futures: one with an unimpeded tsunami of Alzheimer’s cases, and one in which prevention strategies, while not a floodgate, at least stem the tide somewhat. And while researchers hold out hope for the primary and secondary treatments currently in clinical trials, the AD community is nowhere close to finding even a modestly effective therapy.
Seen in this light, Dr. Brookmeyer’s projections are a cry for action, the Alzheimer’s Association statement proclaimed.
“By focusing attention on a concerning reality – that tens of millions of American adults may face the possibility of dementia due to Alzheimer’s disease – the results reported in this new article, if confirmed, illustrate and greatly amplify the need for more research to develop effective treatments and proven prevention strategies for Alzheimer’s disease. This is especially true as we get better at early detection, and are able to more accurately identify people who have the early brain changes associated with Alzheimer’s disease and other dementias.”
Dr. Brookmeyer reported receiving fees from Takeda for serving as a member of a data safety monitoring board.
SOURCE: Brookemeyer R et al. Alzheimers Dement. 2017 Dec 6. doi: 10.1016/j.jalz.2017.10.009
A treatment that would cut the risk of developing amyloid plaques in the brain by 50% could save more than 4 million U.S. residents from mild cognitive impairment and 2.5 million from Alzheimer’s disease by 2060.
The conclusion that even modestly effective preventive therapy could vastly improve the Alzheimer’s outlook is especially important given another startling finding in a new mathematical modeling study by Ron Brookmeyer, PhD, and his colleagues: Right now, they assert, .
“This is the first major attempt to forecast these proposed preclinical Alzheimer’s disease and [mild cognitive impairment] due to Alzheimer’s disease numbers. If confirmed, these data provide essential information for public health planning, and for informing and guiding the public and private investment in Alzheimer’s and dementia research. We need more research to confirm the findings from this model, and more Alzheimer’s and dementia research that includes diverse populations.”
In an interview, Dr. Brookmeyer, a biostatistician at the University of California, Los Angeles, attempted to put those numbers into perspective.
“I want to emphasize that of the 47 million with these Alzheimer’s brain changes, but without clinical symptoms, most will not progress to clinical disease during their lifetimes. In fact, perhaps only 1 in 7 will progress to full-blown dementia.”
Nevertheless, the numbers are disturbing and represent a reality that must be confronted and managed proactively if at all possible, Dr. Brookmeyer said.
“The numbers are what they are,” he said. “They may sound alarmist, but I have every confidence in them. And they’re important because they allow us to understand how many people could potentially benefit from treatment, at what point on the disease continuum it would be useful to implement treatment, and how those treatments could impact public health.”
To carry out the modeling, Dr. Brookmeyer extrapolated from data in two prospective longitudinal cohort studies: the Mayo Clinic Study of Aging, and one by Stephanie J. Vos, PhD, of Maastricht (the Netherlands) University.
The Mayo study followed 1,541 cognitively normal older adults and provided data on the rate of transition from normal cognition to mild cognitive impairment (MCI). The study by Dr. Vos and her associates followed 353 subjects with MCI and brain amyloid, and 222 with late MCI as they progressed. It’s the largest prospective study of progression from MCI to AD that also contains data on baseline neurodegeneration and amyloid burden (Brain. 2015;138[5]:1327-38).
“These studies gave us the rates of transition from one state to another,” Dr. Brookmeyer said. “For example; the Mayo study gave us rates of transition from normal to amyloidosis: 3% of normal 60-year-olds will convert to this state every year.”
The Vos study, Dr. Brookmeyer said, determined rates of progression from MCI to Alzheimer’s dementia, given two preclinical states: asymptomatic amyloid brain plaques alone, or plaques with evidence of neurodegeneration and cognitive signs. Both of these transitional states were first defined in 2011 in a joint paper by the Alzheimer’s Association and the National Institute on Aging (Alzheimers Dement. 2011;7[3]:280-92). While acknowledging that the root causes of Alzheimer’s are unknown, and probably multifactorial, the paper hypothesized a pathophysiologic time line beginning with a three-stage preclinical phase:
• Stage 1: Asymptomatic cerebral amyloidosis: amyloid-positive PET brain imaging with an amyloid-binding ligand and/or a cerebrospinal fluid assay with low amyloid-beta 42 in the presence of normal cognition.
• Stage 2: Amyloid positivity and evidence of synaptic dysfunction and/or early neurodegeneration in the presence of normal cognition.
• Stage 3: Amyloid positivity with evidence of neurodegeneration in the presence of subtle cognitive decline.
“Using those definitions, and piecing together the numbers from these studies, we constructed a computer model based on U.S. census population projections to simulate how many people might be in these different states of disease,” Dr. Brookmeyer said.
In 2017, 6 million Americans were in one of the clinical disease states (MCI due to AD, early clinical AD, or late clinical AD). Dr. Brookmeyer and his colleagues predicted that number will grow to 15 million by 2060. Similarly, in 2017, about 47 million Americans were in one of the preclinical AD states: 22 million with amyloidosis, 8.3 million with only neurodegeneration, and 16.2 million with both. He projects that number will increase to 75.7 million by 2060.
The team then remodeled those numbers in three hypothetical intervention scenarios. In general, Alzheimer’s researchers say a treatment that slows decline by at least 30% would have a meaningful clinical, financial, and societal impact. However, Dr. Brookmeyer modeled treatment scenarios with a greater effect than that.
A primary prevention that reduced the annual risk of new amyloidosis by 50% could decrease the prevalence of MCI by about 700,000 in 2060. A secondary prevention strategy that reduced the annual risk progression to MCI by 50% would decrease the prevalence of MCI by more than 2 million and the prevalence of AD by about 3.8 million.
The results were more complicated with a secondary prevention strategy that would reduce annual risk of MCI-AD conversion by 50%. In this scenario, the prevalence of MCI in 2060 would actually increase by 2.8 million, but the prevalence of AD would decrease by 2.5 million.
These scenarios also developed over different time courses, the researchers wrote.
“We find that the highly effective primary prevention strategy resulted in the lowest AD prevalence by the year 2060. However, [it] was associated with the largest AD prevalence in the 15 years immediately after its introduction ... The explanation for this finding is that the full benefits of delaying amyloidosis in terms of reduced AD prevalence are not realized for many years because of the long lag time between amyloidosis and clinical AD. A take-home message is that the full impact on disease burden of primary prevention that targets the early stages of the pathogenesis of AD on clinical disease burden may not be realized for decades.”
Decreasing preclinical conversion to MCI with a secondary prevention strategy would result in the highest AD prevalence reduction for most of the period. But by 2054, the primary prevention strategy would surpass it.
The intervention targeting MCI-AD conversion would reduce AD prevalence the quickest, with a slight decrease in the first 3 years after introduction. “The explanation for this finding is that MCI is proximate to clinical AD diagnosis, and thus, the impact of delaying progression of MCI will be seen relatively quickly on AD prevalence compared to interventions that delay onset of amyloidosis or MCI.”
The study sharply illustrates two futures: one with an unimpeded tsunami of Alzheimer’s cases, and one in which prevention strategies, while not a floodgate, at least stem the tide somewhat. And while researchers hold out hope for the primary and secondary treatments currently in clinical trials, the AD community is nowhere close to finding even a modestly effective therapy.
Seen in this light, Dr. Brookmeyer’s projections are a cry for action, the Alzheimer’s Association statement proclaimed.
“By focusing attention on a concerning reality – that tens of millions of American adults may face the possibility of dementia due to Alzheimer’s disease – the results reported in this new article, if confirmed, illustrate and greatly amplify the need for more research to develop effective treatments and proven prevention strategies for Alzheimer’s disease. This is especially true as we get better at early detection, and are able to more accurately identify people who have the early brain changes associated with Alzheimer’s disease and other dementias.”
Dr. Brookmeyer reported receiving fees from Takeda for serving as a member of a data safety monitoring board.
SOURCE: Brookemeyer R et al. Alzheimers Dement. 2017 Dec 6. doi: 10.1016/j.jalz.2017.10.009
FROM ALZHEIMER’S & DEMENTIA
Key clinical point: Preventing amyloid accumulation would save millions from MCI and later AD.
Major finding: A treatment that decreased the risk of amyloidosis by 50% would prevent 4 million MCI cases and 2 million AD cases in the United States by 2060.
Study details: A computer modeling study based on two prospective longitudinal studies of aging.
Disclosures: This research was funded by a grant from the National Institutes of Health. Dr. Brookmeyer reported remuneration from Takeda as part of a data safety monitoring board.
Source: Brookemeyer R et al. Alzheimers Dement. 2017 Dec 6. doi: 10.1016/j.jalz.2017.10.009
Psychotic symptoms predict persistent problems in adolescents
BERLIN – Teens who reported psychotic symptoms – especially hallucinations – on a baseline mental health screening were twice as likely to develop persistent psychiatric symptoms over the next year as were those without such experiences.
Hallucinations in particular predicted a persistent course, nearly tripling the risk (odds ratio, 2.74), Saliha El-Bouhaddani said at the meeting of the World Psychiatric Association.
“This is quite informative and quite clinically relevant,” said Ms. El-Bouhaddani, a doctoral student in psychology at the Parnassia Group, Rotterdam, the Netherlands. Because mental health symptoms in young people may be self-limiting, it’s not easy to identify which teens are at high risk for developing persistent problems that can predispose them to a full-blown mental disorder. “But we can see here that psychotic experiences may be very useful in detecting which adolescents may have persistency of symptoms. I believe that screening tools for teenagers should involve questions about psychotic symptoms, because the answer may help us discriminate who will have a self-limiting course and who will have a persistent course.”
Ms. El-Bouhaddani described MasterMind, a longitudinal cohort study of adolescents drawn from the general population. Each teen completed self-report questionnaires on psychotic experiences and psychosocial problems at two time points over a 2-year period. The study was divided into two phases: a 1-year observational period, followed by an intervention for those at risk, and then a 1-year treatment and follow-up period. She reported only the results of the observational phase.
The study enrolled 1,827 young people, who completed four questionnaires: the Strengths & Difficulties Questionnaire, and questionnaires about psychotic experiences, trauma, and self-esteem. One year later, 1,521 of the participants returned and completed the same surveys.
Ms. El-Bouhaddani constructed four potential pathways from baseline to follow-up: no psychiatric symptoms, remitting symptoms (baseline psychosocial symptoms that remitted by 1 year), incident symptoms (symptoms that appeared only at 1 year), and persistent symptoms (symptoms at both baseline and 1 year). Her goal was to identify any baseline characteristics that might predict a persistent course.
At the 1-year point, the cohort was a mean of 13.5 years old. Most subjects (1,134) had no symptoms at either time point. Incident symptoms were present in 151, remitting symptoms in 181, and persistent symptoms in 46.
Several baseline characteristics significantly separated the group with remitting symptoms from all other groups: They were significantly more likely to have a low education level (61%), to have divorced parents (38%), to report frequent household moves (22%), to have repeated a grade (31%), to report low self-esteem (15%), and to have somatic symptoms (3%). Teens with persistent symptoms also reported more somatic symptoms (3%), but they were significantly more likely than any of the other groups to report having had at least one traumatic event (45%).
At follow-up, psychotic incidents were significantly more common in the remitting and persistent groups (40% and 62%, respectively) than in the nonsymptomatic and incident groups (10% and 11%).
Ms. El-Bouhaddani then broke psychotic experiences down into hallucinations and delusions, and examined their relationships to symptom course. Hallucinations were significantly more common than delusions among those with a persistent course (58% vs. 42%).
She conducted a logistic regression analysis, which determined that any psychotic experience nearly doubled the risk of a persistent course of psychiatric symptoms (OR, 1.92). Hallucinations nearly tripled the risk (OR, 2.74), as did traumatic experiences (OR, 3.0). Delusions increased the risk by close to 60% (OR, 1.59).
The SDQ does not contain questions about psychotic experiences or trauma – the two most powerful predictors of persistent symptoms. It’s time to change this, Ms. El-Bouhaddani said.
“From these results it seems as though we should be asking adolescents about psychotic experiences and trauma. Perhaps it’s time for a new version of the SDQ.”
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
SOURCE: El-Bouhaddani S et al. WPA 2017 Abstract S-023 002.
BERLIN – Teens who reported psychotic symptoms – especially hallucinations – on a baseline mental health screening were twice as likely to develop persistent psychiatric symptoms over the next year as were those without such experiences.
Hallucinations in particular predicted a persistent course, nearly tripling the risk (odds ratio, 2.74), Saliha El-Bouhaddani said at the meeting of the World Psychiatric Association.
“This is quite informative and quite clinically relevant,” said Ms. El-Bouhaddani, a doctoral student in psychology at the Parnassia Group, Rotterdam, the Netherlands. Because mental health symptoms in young people may be self-limiting, it’s not easy to identify which teens are at high risk for developing persistent problems that can predispose them to a full-blown mental disorder. “But we can see here that psychotic experiences may be very useful in detecting which adolescents may have persistency of symptoms. I believe that screening tools for teenagers should involve questions about psychotic symptoms, because the answer may help us discriminate who will have a self-limiting course and who will have a persistent course.”
Ms. El-Bouhaddani described MasterMind, a longitudinal cohort study of adolescents drawn from the general population. Each teen completed self-report questionnaires on psychotic experiences and psychosocial problems at two time points over a 2-year period. The study was divided into two phases: a 1-year observational period, followed by an intervention for those at risk, and then a 1-year treatment and follow-up period. She reported only the results of the observational phase.
The study enrolled 1,827 young people, who completed four questionnaires: the Strengths & Difficulties Questionnaire, and questionnaires about psychotic experiences, trauma, and self-esteem. One year later, 1,521 of the participants returned and completed the same surveys.
Ms. El-Bouhaddani constructed four potential pathways from baseline to follow-up: no psychiatric symptoms, remitting symptoms (baseline psychosocial symptoms that remitted by 1 year), incident symptoms (symptoms that appeared only at 1 year), and persistent symptoms (symptoms at both baseline and 1 year). Her goal was to identify any baseline characteristics that might predict a persistent course.
At the 1-year point, the cohort was a mean of 13.5 years old. Most subjects (1,134) had no symptoms at either time point. Incident symptoms were present in 151, remitting symptoms in 181, and persistent symptoms in 46.
Several baseline characteristics significantly separated the group with remitting symptoms from all other groups: They were significantly more likely to have a low education level (61%), to have divorced parents (38%), to report frequent household moves (22%), to have repeated a grade (31%), to report low self-esteem (15%), and to have somatic symptoms (3%). Teens with persistent symptoms also reported more somatic symptoms (3%), but they were significantly more likely than any of the other groups to report having had at least one traumatic event (45%).
At follow-up, psychotic incidents were significantly more common in the remitting and persistent groups (40% and 62%, respectively) than in the nonsymptomatic and incident groups (10% and 11%).
Ms. El-Bouhaddani then broke psychotic experiences down into hallucinations and delusions, and examined their relationships to symptom course. Hallucinations were significantly more common than delusions among those with a persistent course (58% vs. 42%).
She conducted a logistic regression analysis, which determined that any psychotic experience nearly doubled the risk of a persistent course of psychiatric symptoms (OR, 1.92). Hallucinations nearly tripled the risk (OR, 2.74), as did traumatic experiences (OR, 3.0). Delusions increased the risk by close to 60% (OR, 1.59).
The SDQ does not contain questions about psychotic experiences or trauma – the two most powerful predictors of persistent symptoms. It’s time to change this, Ms. El-Bouhaddani said.
“From these results it seems as though we should be asking adolescents about psychotic experiences and trauma. Perhaps it’s time for a new version of the SDQ.”
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
SOURCE: El-Bouhaddani S et al. WPA 2017 Abstract S-023 002.
BERLIN – Teens who reported psychotic symptoms – especially hallucinations – on a baseline mental health screening were twice as likely to develop persistent psychiatric symptoms over the next year as were those without such experiences.
Hallucinations in particular predicted a persistent course, nearly tripling the risk (odds ratio, 2.74), Saliha El-Bouhaddani said at the meeting of the World Psychiatric Association.
“This is quite informative and quite clinically relevant,” said Ms. El-Bouhaddani, a doctoral student in psychology at the Parnassia Group, Rotterdam, the Netherlands. Because mental health symptoms in young people may be self-limiting, it’s not easy to identify which teens are at high risk for developing persistent problems that can predispose them to a full-blown mental disorder. “But we can see here that psychotic experiences may be very useful in detecting which adolescents may have persistency of symptoms. I believe that screening tools for teenagers should involve questions about psychotic symptoms, because the answer may help us discriminate who will have a self-limiting course and who will have a persistent course.”
Ms. El-Bouhaddani described MasterMind, a longitudinal cohort study of adolescents drawn from the general population. Each teen completed self-report questionnaires on psychotic experiences and psychosocial problems at two time points over a 2-year period. The study was divided into two phases: a 1-year observational period, followed by an intervention for those at risk, and then a 1-year treatment and follow-up period. She reported only the results of the observational phase.
The study enrolled 1,827 young people, who completed four questionnaires: the Strengths & Difficulties Questionnaire, and questionnaires about psychotic experiences, trauma, and self-esteem. One year later, 1,521 of the participants returned and completed the same surveys.
Ms. El-Bouhaddani constructed four potential pathways from baseline to follow-up: no psychiatric symptoms, remitting symptoms (baseline psychosocial symptoms that remitted by 1 year), incident symptoms (symptoms that appeared only at 1 year), and persistent symptoms (symptoms at both baseline and 1 year). Her goal was to identify any baseline characteristics that might predict a persistent course.
At the 1-year point, the cohort was a mean of 13.5 years old. Most subjects (1,134) had no symptoms at either time point. Incident symptoms were present in 151, remitting symptoms in 181, and persistent symptoms in 46.
Several baseline characteristics significantly separated the group with remitting symptoms from all other groups: They were significantly more likely to have a low education level (61%), to have divorced parents (38%), to report frequent household moves (22%), to have repeated a grade (31%), to report low self-esteem (15%), and to have somatic symptoms (3%). Teens with persistent symptoms also reported more somatic symptoms (3%), but they were significantly more likely than any of the other groups to report having had at least one traumatic event (45%).
At follow-up, psychotic incidents were significantly more common in the remitting and persistent groups (40% and 62%, respectively) than in the nonsymptomatic and incident groups (10% and 11%).
Ms. El-Bouhaddani then broke psychotic experiences down into hallucinations and delusions, and examined their relationships to symptom course. Hallucinations were significantly more common than delusions among those with a persistent course (58% vs. 42%).
She conducted a logistic regression analysis, which determined that any psychotic experience nearly doubled the risk of a persistent course of psychiatric symptoms (OR, 1.92). Hallucinations nearly tripled the risk (OR, 2.74), as did traumatic experiences (OR, 3.0). Delusions increased the risk by close to 60% (OR, 1.59).
The SDQ does not contain questions about psychotic experiences or trauma – the two most powerful predictors of persistent symptoms. It’s time to change this, Ms. El-Bouhaddani said.
“From these results it seems as though we should be asking adolescents about psychotic experiences and trauma. Perhaps it’s time for a new version of the SDQ.”
She had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
SOURCE: El-Bouhaddani S et al. WPA 2017 Abstract S-023 002.
REPORTING FROM WPA 2017
Key clinical point: Among teens, psychotic symptoms predicted a persistent course of psychosocial problems.
Major finding: Psychotic experiences at baseline doubled the risk of a persistent course of psychosocial problems (odds ratio, 1.94).
Study details: A prospective longitudinal cohort study of 1,521 teens.
Disclosures: Ms. El-Bouhaddani had no relevant financial disclosures.
Source: El-Bouhaddani S et al. WPA 2017 Abstract S-023 002.
Gene silencer reduces mutant huntingtin protein in early-stage Huntington’s patients
An investigational gene-silencing molecule safely and dose-dependently reduced production of the mutant huntingtin protein in people with early-stage Huntington’s disease in a small, early-phase study, according to an announcement from the drug’s developer, Ionis Pharmaceuticals.
The antisense oligonucleotide IONIS-HTTRx – the first potentially disease-modifying drug for Huntington’s – will now go forward in a larger study to determine whether lowering mutant huntingtin protein (mHTT) confers any clinical benefits upon patients with the fatal neurodegenerative disease.
IONIS-HTTRx reduced mHTT by fractions that “exceeded expectations” set for the 46-person trial, C. Frank Bennett, PhD, senior vice president of research at Ionis, said in a press statement.
“The results of this trial are of groundbreaking importance for Huntington’s disease patients and families,” said Dr. Tabrizi, director of the Huntington’s Disease Centre at University College London. “For the first time a drug has lowered the level of the toxic disease-causing protein in the nervous system, and the drug was safe and well tolerated. The key now is to move quickly to a larger trial to test whether the drug slows disease progression.”
Upon receiving the positive data, Roche Pharma exercised its $45 million option to license the molecule. Roche now takes all regulatory and clinical development responsibility for IONIS-HTTRx.
There are few publicly available data on the IONIS-HTTRx study. It enrolled 46 patients with early-stage Huntington’s who were recruited from nine sites in the United Kingdom, Germany, and Canada. They were randomized to placebo or to four ascending doses of IONIS-HTTRx. The primary outcomes were mHTT levels in spinal fluid, safety, and tolerability. It produced significant, dose-dependent reductions of mHTT without concerning or dose-limiting safety signals, the press statement noted.
A larger study with clinical endpoints is next up, according to a statement Ionis and Roche jointly issued to the Huntington’s Disease Society of America.
“The next step for this program will be to conduct a safety and efficacy study to investigate if decreasing mutant huntingtin protein with IONIS-HTTRx can benefit people with Huntington’s disease,” the statement noted. “Future studies for the program will be conducted globally, including in the U.S. Roche will announce details about future studies, including eligibility criteria and planned start dates, as this information becomes available. All relevant information on upcoming studies will also be posted on HDTrialFinder.org and ClinicalTrials.gov.”
Huntington’s disease is caused by an expansion of at least 36 repeats of the CAG trinucleotide sequence in the huntingtin gene. The resulting mHTT is toxic and gradually damages neurons. IONIS-HTTRx interrupts the messenger RNA that fuels this toxic protein buildup, and it is the only drug that has ever attacked the disease at this level. This development is “a historic moment in the fight against Huntington’s, as it represents the successful completion of the first trial to treat the underlying cause of Huntington’s disease, the genetic mutation itself,” according to a statement by Louise Vetter, president of the Huntington’s Disease Society of America.
“The fact that levels of mutant huntingtin were reduced in correlation to the dose of IONIS-HTTRx that was given is significant, and the fact that participants in this first Phase 1/2a study are able to continue on the drug through an open-label extension gives us optimism regarding its safety,” Ms. Vetter said.
In January 2016, the Food and Drug Administration granted orphan drug status to IONIS-HTTRX; the European Medicines Agency had previously granted it similar status.
The press release from Ionis Pharmaceuticals sounds very promising. There is reason to believe that lowering mHTT protein might prevent or delay Huntington’s disease, and this antisense molecule appears to be safe and to lower mHTT in cerebrospinal fluid. However, there are several caveats.
First, it is unclear whether lowering mHTT protein might help those who already have clinical Huntington’s disease.
Third, no information is given in the press release about the degree of reduction of mHTT observed and whether there is evidence that this lowering might be sufficient for a therapeutic effect.
Fourth, neurotoxicity may not only result from the mHTT protein but also directly from the mRNA itself. The contribution of mutant mRNA to pathogenesis is a key open question in the study of Huntington’s disease and other related “repeat disorders.”
Michael Wolfe, PhD , is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. He has no relevant disclosures.
The press release from Ionis Pharmaceuticals sounds very promising. There is reason to believe that lowering mHTT protein might prevent or delay Huntington’s disease, and this antisense molecule appears to be safe and to lower mHTT in cerebrospinal fluid. However, there are several caveats.
First, it is unclear whether lowering mHTT protein might help those who already have clinical Huntington’s disease.
Third, no information is given in the press release about the degree of reduction of mHTT observed and whether there is evidence that this lowering might be sufficient for a therapeutic effect.
Fourth, neurotoxicity may not only result from the mHTT protein but also directly from the mRNA itself. The contribution of mutant mRNA to pathogenesis is a key open question in the study of Huntington’s disease and other related “repeat disorders.”
Michael Wolfe, PhD , is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. He has no relevant disclosures.
The press release from Ionis Pharmaceuticals sounds very promising. There is reason to believe that lowering mHTT protein might prevent or delay Huntington’s disease, and this antisense molecule appears to be safe and to lower mHTT in cerebrospinal fluid. However, there are several caveats.
First, it is unclear whether lowering mHTT protein might help those who already have clinical Huntington’s disease.
Third, no information is given in the press release about the degree of reduction of mHTT observed and whether there is evidence that this lowering might be sufficient for a therapeutic effect.
Fourth, neurotoxicity may not only result from the mHTT protein but also directly from the mRNA itself. The contribution of mutant mRNA to pathogenesis is a key open question in the study of Huntington’s disease and other related “repeat disorders.”
Michael Wolfe, PhD , is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. He has no relevant disclosures.
An investigational gene-silencing molecule safely and dose-dependently reduced production of the mutant huntingtin protein in people with early-stage Huntington’s disease in a small, early-phase study, according to an announcement from the drug’s developer, Ionis Pharmaceuticals.
The antisense oligonucleotide IONIS-HTTRx – the first potentially disease-modifying drug for Huntington’s – will now go forward in a larger study to determine whether lowering mutant huntingtin protein (mHTT) confers any clinical benefits upon patients with the fatal neurodegenerative disease.
IONIS-HTTRx reduced mHTT by fractions that “exceeded expectations” set for the 46-person trial, C. Frank Bennett, PhD, senior vice president of research at Ionis, said in a press statement.
“The results of this trial are of groundbreaking importance for Huntington’s disease patients and families,” said Dr. Tabrizi, director of the Huntington’s Disease Centre at University College London. “For the first time a drug has lowered the level of the toxic disease-causing protein in the nervous system, and the drug was safe and well tolerated. The key now is to move quickly to a larger trial to test whether the drug slows disease progression.”
Upon receiving the positive data, Roche Pharma exercised its $45 million option to license the molecule. Roche now takes all regulatory and clinical development responsibility for IONIS-HTTRx.
There are few publicly available data on the IONIS-HTTRx study. It enrolled 46 patients with early-stage Huntington’s who were recruited from nine sites in the United Kingdom, Germany, and Canada. They were randomized to placebo or to four ascending doses of IONIS-HTTRx. The primary outcomes were mHTT levels in spinal fluid, safety, and tolerability. It produced significant, dose-dependent reductions of mHTT without concerning or dose-limiting safety signals, the press statement noted.
A larger study with clinical endpoints is next up, according to a statement Ionis and Roche jointly issued to the Huntington’s Disease Society of America.
“The next step for this program will be to conduct a safety and efficacy study to investigate if decreasing mutant huntingtin protein with IONIS-HTTRx can benefit people with Huntington’s disease,” the statement noted. “Future studies for the program will be conducted globally, including in the U.S. Roche will announce details about future studies, including eligibility criteria and planned start dates, as this information becomes available. All relevant information on upcoming studies will also be posted on HDTrialFinder.org and ClinicalTrials.gov.”
Huntington’s disease is caused by an expansion of at least 36 repeats of the CAG trinucleotide sequence in the huntingtin gene. The resulting mHTT is toxic and gradually damages neurons. IONIS-HTTRx interrupts the messenger RNA that fuels this toxic protein buildup, and it is the only drug that has ever attacked the disease at this level. This development is “a historic moment in the fight against Huntington’s, as it represents the successful completion of the first trial to treat the underlying cause of Huntington’s disease, the genetic mutation itself,” according to a statement by Louise Vetter, president of the Huntington’s Disease Society of America.
“The fact that levels of mutant huntingtin were reduced in correlation to the dose of IONIS-HTTRx that was given is significant, and the fact that participants in this first Phase 1/2a study are able to continue on the drug through an open-label extension gives us optimism regarding its safety,” Ms. Vetter said.
In January 2016, the Food and Drug Administration granted orphan drug status to IONIS-HTTRX; the European Medicines Agency had previously granted it similar status.
An investigational gene-silencing molecule safely and dose-dependently reduced production of the mutant huntingtin protein in people with early-stage Huntington’s disease in a small, early-phase study, according to an announcement from the drug’s developer, Ionis Pharmaceuticals.
The antisense oligonucleotide IONIS-HTTRx – the first potentially disease-modifying drug for Huntington’s – will now go forward in a larger study to determine whether lowering mutant huntingtin protein (mHTT) confers any clinical benefits upon patients with the fatal neurodegenerative disease.
IONIS-HTTRx reduced mHTT by fractions that “exceeded expectations” set for the 46-person trial, C. Frank Bennett, PhD, senior vice president of research at Ionis, said in a press statement.
“The results of this trial are of groundbreaking importance for Huntington’s disease patients and families,” said Dr. Tabrizi, director of the Huntington’s Disease Centre at University College London. “For the first time a drug has lowered the level of the toxic disease-causing protein in the nervous system, and the drug was safe and well tolerated. The key now is to move quickly to a larger trial to test whether the drug slows disease progression.”
Upon receiving the positive data, Roche Pharma exercised its $45 million option to license the molecule. Roche now takes all regulatory and clinical development responsibility for IONIS-HTTRx.
There are few publicly available data on the IONIS-HTTRx study. It enrolled 46 patients with early-stage Huntington’s who were recruited from nine sites in the United Kingdom, Germany, and Canada. They were randomized to placebo or to four ascending doses of IONIS-HTTRx. The primary outcomes were mHTT levels in spinal fluid, safety, and tolerability. It produced significant, dose-dependent reductions of mHTT without concerning or dose-limiting safety signals, the press statement noted.
A larger study with clinical endpoints is next up, according to a statement Ionis and Roche jointly issued to the Huntington’s Disease Society of America.
“The next step for this program will be to conduct a safety and efficacy study to investigate if decreasing mutant huntingtin protein with IONIS-HTTRx can benefit people with Huntington’s disease,” the statement noted. “Future studies for the program will be conducted globally, including in the U.S. Roche will announce details about future studies, including eligibility criteria and planned start dates, as this information becomes available. All relevant information on upcoming studies will also be posted on HDTrialFinder.org and ClinicalTrials.gov.”
Huntington’s disease is caused by an expansion of at least 36 repeats of the CAG trinucleotide sequence in the huntingtin gene. The resulting mHTT is toxic and gradually damages neurons. IONIS-HTTRx interrupts the messenger RNA that fuels this toxic protein buildup, and it is the only drug that has ever attacked the disease at this level. This development is “a historic moment in the fight against Huntington’s, as it represents the successful completion of the first trial to treat the underlying cause of Huntington’s disease, the genetic mutation itself,” according to a statement by Louise Vetter, president of the Huntington’s Disease Society of America.
“The fact that levels of mutant huntingtin were reduced in correlation to the dose of IONIS-HTTRx that was given is significant, and the fact that participants in this first Phase 1/2a study are able to continue on the drug through an open-label extension gives us optimism regarding its safety,” Ms. Vetter said.
In January 2016, the Food and Drug Administration granted orphan drug status to IONIS-HTTRX; the European Medicines Agency had previously granted it similar status.