User login
Endometrial scratching doesn’t lead to higher live birth rate for IVF patients
Endometrial scratching prior to a fresh embryo or frozen embryo transfer did not result in a higher rate of live births for women undergoing in vitro fertilization (IVF), according to results from a recent randomized controlled trial published in the New England Journal of Medicine.
Sarah Lensen, PhD, of the University of Auckland in New Zealand, and her colleagues recruited 1,364 women from 13 sites in 5 countries in 2014-2017 who did not have a recent history of disruptive intrauterine instrumentation such as hysteroscopy or endometrial biopsy and were planning an IVF cycle with a fresh or frozen embryo transfer. The women were randomized to receive endometrial scratching through pipelle biopsy between day 3 of the cycle prior to IVF and day 3 of the IVF cycle. Live birth was the primary outcome, while secondary outcomes measured included ongoing pregnancy, clinical pregnancy, multiple pregnancy, ectopic pregnancy, and biochemical pregnancy, as well as miscarriage, termination of pregnancy, stillbirth, and other maternal and neonatal outcomes.
For the endometrial scratch group, the rate of live birth was 26% (180 of 690 women), compared with 26% (176 of 674 women) in the control group (adjusted odds ratio, 1.00; 95% confidence interval, 0.78-1.27, P = .97). The rate of ongoing pregnancy, clinical pregnancy, ectopic pregnancy, and miscarriage also did not significantly differ between groups.
Among women who underwent endometrial scratching, there was a median pain score of 3.5 points from a range of 0-10 points; 37 women reported a pain scale score of 0, while 6 said their pain score was a 10. Adverse reactions to endometrial scratching included fainting, dizziness and/or nausea (7 women); excessive pain (5 women), including 1 woman who went to the emergency department after a concurrent endometrial scratch and sonohysterogram procedure; and excessive bleeding (2 women).
The researchers noted several limitations in their study, including its unblinded design; tracking of adverse outcomes in the endometrial scratch group only; and a definition of implantation failure not based on embryo or transfer quality, but on the number of previous unsuccessful transfers. There were also “imbalances favoring the endometrial scratch group” based on the number of available oocytes per participant and willingness to begin their IVF cycle.
“Women in the endometrial scratch group may have been more likely to start their cycle in order to capitalize on their exposure to the endometrial scratch. However, results were materially unchanged in a per-protocol analysis,” the researchers said.
This study was funded in part by the University of Auckland, the A+ Trust, Auckland District Health Board, the Nurture Foundation, and the Maurice and Phyllis Paykel Trust. Dr. Priya Bhide received personal fees from Ferring Pharmaceuticals, and grants from Bart’s Charity, Pharmasure Pharmaceuticals, and Finox Pharmaceuticals. The other authors reported no relevant financial disclosures.
SOURCE: Lensen S et al. N Engl J Med. 2019. doi: 10.1056/NEJMoa1808737.
The results of a large, pragmatic trial by Lensen et al., examining the effects of endometrial scratching, which used current standards of care for in vitro fertilization (IVF) and included women undergoing treatment for the first time in addition to those who have had previously failed cycles, should be trusted despite contrary data from other studies, Ben W. Mol, MD, PhD, and Kurt T. Barnhart, MD, MSCE, wrote in a related editorial.
Although a Cochrane systematic review of 14 randomized controlled trials found evidence of an increased live birth rate for women undergoing IVF after an endometrial scratch procedure (risk ratio, 1.42; 95% confidence interval, 1.08-1.85), many trials in the meta-analysis had “unrealistic” large effect sizes within limited sample sizes, were not optimally randomized, were stopped prematurely, or were not prospectively registered, they noted.
“Rigorous synthesis of bad data cannot overcome bias from uncontrolled or poorly conducted studies; it may result only in tighter confidence around a spurious conclusion, an answer that is precisely wrong,” they said.
However, as the results from Lensen et al. show, there were a low number of reported adverse events, and “on the basis of the current report, the IVF community can take solace in the observation that ‘scratching’ apparently caused no harm, other than some procedure-associated pain and bleeding.”
Any adjuvant to IVF should be “evaluated carefully before being offered to infertility couples” and it is still an unanswered question as to whether IVF doctors should continue to offer unevaluated adjuvants to their patients, Dr. Mol and Dr. Barnhart said.
“The population affected by infertility has been described as vulnerable. The goals of reproductive medicine are the same as those of other fields of medicine: Provide compassionate and effective care, do no harm, and do not offer false hope or sell snake oil,” the authors concluded.
Dr. Mol is at Monash University in Clayton, Australia, and Dr. Barnhart is at the University of Pennsylvania in Philadelphia. This commentary summarizes their editorial on the study by Lensen et al. (N Eng J Med. 2019. doi: 10.1056/NEJMe1815042 ). Dr. Mol disclosed ties with Merck, Guerbet, and ObsEva, outside the submitted work. Dr. Barnhart had no relevant disclosures.
The results of a large, pragmatic trial by Lensen et al., examining the effects of endometrial scratching, which used current standards of care for in vitro fertilization (IVF) and included women undergoing treatment for the first time in addition to those who have had previously failed cycles, should be trusted despite contrary data from other studies, Ben W. Mol, MD, PhD, and Kurt T. Barnhart, MD, MSCE, wrote in a related editorial.
Although a Cochrane systematic review of 14 randomized controlled trials found evidence of an increased live birth rate for women undergoing IVF after an endometrial scratch procedure (risk ratio, 1.42; 95% confidence interval, 1.08-1.85), many trials in the meta-analysis had “unrealistic” large effect sizes within limited sample sizes, were not optimally randomized, were stopped prematurely, or were not prospectively registered, they noted.
“Rigorous synthesis of bad data cannot overcome bias from uncontrolled or poorly conducted studies; it may result only in tighter confidence around a spurious conclusion, an answer that is precisely wrong,” they said.
However, as the results from Lensen et al. show, there were a low number of reported adverse events, and “on the basis of the current report, the IVF community can take solace in the observation that ‘scratching’ apparently caused no harm, other than some procedure-associated pain and bleeding.”
Any adjuvant to IVF should be “evaluated carefully before being offered to infertility couples” and it is still an unanswered question as to whether IVF doctors should continue to offer unevaluated adjuvants to their patients, Dr. Mol and Dr. Barnhart said.
“The population affected by infertility has been described as vulnerable. The goals of reproductive medicine are the same as those of other fields of medicine: Provide compassionate and effective care, do no harm, and do not offer false hope or sell snake oil,” the authors concluded.
Dr. Mol is at Monash University in Clayton, Australia, and Dr. Barnhart is at the University of Pennsylvania in Philadelphia. This commentary summarizes their editorial on the study by Lensen et al. (N Eng J Med. 2019. doi: 10.1056/NEJMe1815042 ). Dr. Mol disclosed ties with Merck, Guerbet, and ObsEva, outside the submitted work. Dr. Barnhart had no relevant disclosures.
The results of a large, pragmatic trial by Lensen et al., examining the effects of endometrial scratching, which used current standards of care for in vitro fertilization (IVF) and included women undergoing treatment for the first time in addition to those who have had previously failed cycles, should be trusted despite contrary data from other studies, Ben W. Mol, MD, PhD, and Kurt T. Barnhart, MD, MSCE, wrote in a related editorial.
Although a Cochrane systematic review of 14 randomized controlled trials found evidence of an increased live birth rate for women undergoing IVF after an endometrial scratch procedure (risk ratio, 1.42; 95% confidence interval, 1.08-1.85), many trials in the meta-analysis had “unrealistic” large effect sizes within limited sample sizes, were not optimally randomized, were stopped prematurely, or were not prospectively registered, they noted.
“Rigorous synthesis of bad data cannot overcome bias from uncontrolled or poorly conducted studies; it may result only in tighter confidence around a spurious conclusion, an answer that is precisely wrong,” they said.
However, as the results from Lensen et al. show, there were a low number of reported adverse events, and “on the basis of the current report, the IVF community can take solace in the observation that ‘scratching’ apparently caused no harm, other than some procedure-associated pain and bleeding.”
Any adjuvant to IVF should be “evaluated carefully before being offered to infertility couples” and it is still an unanswered question as to whether IVF doctors should continue to offer unevaluated adjuvants to their patients, Dr. Mol and Dr. Barnhart said.
“The population affected by infertility has been described as vulnerable. The goals of reproductive medicine are the same as those of other fields of medicine: Provide compassionate and effective care, do no harm, and do not offer false hope or sell snake oil,” the authors concluded.
Dr. Mol is at Monash University in Clayton, Australia, and Dr. Barnhart is at the University of Pennsylvania in Philadelphia. This commentary summarizes their editorial on the study by Lensen et al. (N Eng J Med. 2019. doi: 10.1056/NEJMe1815042 ). Dr. Mol disclosed ties with Merck, Guerbet, and ObsEva, outside the submitted work. Dr. Barnhart had no relevant disclosures.
Endometrial scratching prior to a fresh embryo or frozen embryo transfer did not result in a higher rate of live births for women undergoing in vitro fertilization (IVF), according to results from a recent randomized controlled trial published in the New England Journal of Medicine.
Sarah Lensen, PhD, of the University of Auckland in New Zealand, and her colleagues recruited 1,364 women from 13 sites in 5 countries in 2014-2017 who did not have a recent history of disruptive intrauterine instrumentation such as hysteroscopy or endometrial biopsy and were planning an IVF cycle with a fresh or frozen embryo transfer. The women were randomized to receive endometrial scratching through pipelle biopsy between day 3 of the cycle prior to IVF and day 3 of the IVF cycle. Live birth was the primary outcome, while secondary outcomes measured included ongoing pregnancy, clinical pregnancy, multiple pregnancy, ectopic pregnancy, and biochemical pregnancy, as well as miscarriage, termination of pregnancy, stillbirth, and other maternal and neonatal outcomes.
For the endometrial scratch group, the rate of live birth was 26% (180 of 690 women), compared with 26% (176 of 674 women) in the control group (adjusted odds ratio, 1.00; 95% confidence interval, 0.78-1.27, P = .97). The rate of ongoing pregnancy, clinical pregnancy, ectopic pregnancy, and miscarriage also did not significantly differ between groups.
Among women who underwent endometrial scratching, there was a median pain score of 3.5 points from a range of 0-10 points; 37 women reported a pain scale score of 0, while 6 said their pain score was a 10. Adverse reactions to endometrial scratching included fainting, dizziness and/or nausea (7 women); excessive pain (5 women), including 1 woman who went to the emergency department after a concurrent endometrial scratch and sonohysterogram procedure; and excessive bleeding (2 women).
The researchers noted several limitations in their study, including its unblinded design; tracking of adverse outcomes in the endometrial scratch group only; and a definition of implantation failure not based on embryo or transfer quality, but on the number of previous unsuccessful transfers. There were also “imbalances favoring the endometrial scratch group” based on the number of available oocytes per participant and willingness to begin their IVF cycle.
“Women in the endometrial scratch group may have been more likely to start their cycle in order to capitalize on their exposure to the endometrial scratch. However, results were materially unchanged in a per-protocol analysis,” the researchers said.
This study was funded in part by the University of Auckland, the A+ Trust, Auckland District Health Board, the Nurture Foundation, and the Maurice and Phyllis Paykel Trust. Dr. Priya Bhide received personal fees from Ferring Pharmaceuticals, and grants from Bart’s Charity, Pharmasure Pharmaceuticals, and Finox Pharmaceuticals. The other authors reported no relevant financial disclosures.
SOURCE: Lensen S et al. N Engl J Med. 2019. doi: 10.1056/NEJMoa1808737.
Endometrial scratching prior to a fresh embryo or frozen embryo transfer did not result in a higher rate of live births for women undergoing in vitro fertilization (IVF), according to results from a recent randomized controlled trial published in the New England Journal of Medicine.
Sarah Lensen, PhD, of the University of Auckland in New Zealand, and her colleagues recruited 1,364 women from 13 sites in 5 countries in 2014-2017 who did not have a recent history of disruptive intrauterine instrumentation such as hysteroscopy or endometrial biopsy and were planning an IVF cycle with a fresh or frozen embryo transfer. The women were randomized to receive endometrial scratching through pipelle biopsy between day 3 of the cycle prior to IVF and day 3 of the IVF cycle. Live birth was the primary outcome, while secondary outcomes measured included ongoing pregnancy, clinical pregnancy, multiple pregnancy, ectopic pregnancy, and biochemical pregnancy, as well as miscarriage, termination of pregnancy, stillbirth, and other maternal and neonatal outcomes.
For the endometrial scratch group, the rate of live birth was 26% (180 of 690 women), compared with 26% (176 of 674 women) in the control group (adjusted odds ratio, 1.00; 95% confidence interval, 0.78-1.27, P = .97). The rate of ongoing pregnancy, clinical pregnancy, ectopic pregnancy, and miscarriage also did not significantly differ between groups.
Among women who underwent endometrial scratching, there was a median pain score of 3.5 points from a range of 0-10 points; 37 women reported a pain scale score of 0, while 6 said their pain score was a 10. Adverse reactions to endometrial scratching included fainting, dizziness and/or nausea (7 women); excessive pain (5 women), including 1 woman who went to the emergency department after a concurrent endometrial scratch and sonohysterogram procedure; and excessive bleeding (2 women).
The researchers noted several limitations in their study, including its unblinded design; tracking of adverse outcomes in the endometrial scratch group only; and a definition of implantation failure not based on embryo or transfer quality, but on the number of previous unsuccessful transfers. There were also “imbalances favoring the endometrial scratch group” based on the number of available oocytes per participant and willingness to begin their IVF cycle.
“Women in the endometrial scratch group may have been more likely to start their cycle in order to capitalize on their exposure to the endometrial scratch. However, results were materially unchanged in a per-protocol analysis,” the researchers said.
This study was funded in part by the University of Auckland, the A+ Trust, Auckland District Health Board, the Nurture Foundation, and the Maurice and Phyllis Paykel Trust. Dr. Priya Bhide received personal fees from Ferring Pharmaceuticals, and grants from Bart’s Charity, Pharmasure Pharmaceuticals, and Finox Pharmaceuticals. The other authors reported no relevant financial disclosures.
SOURCE: Lensen S et al. N Engl J Med. 2019. doi: 10.1056/NEJMoa1808737.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: The live birth rate for women in the endometrial scratch group was 26% of 690 participants, compared with 26% of 674 women in the control group, a nonsignificant difference.
Study details: A multicenter, open-label, randomized controlled trial of 1,364 women undergoing IVF at 13 different sites in 5 countries.
Disclosures: This study was funded in part by the University of Auckland, the A+ Trust, Auckland District Health Board, the Nurture Foundation, and the Maurice and Phyllis Paykel Trust. Dr. Priya Bhide received personal fees from Ferring Pharmaceuticals, and grants from Bart’s Charity, Pharmasure Pharmaceuticals, and Finox Pharmaceuticals. The other authors reported no relevant financial disclosures.
Source: Lensen S et al. N Engl J Med. 2019. doi: 10.1056/NEJMoa1808737.
FDA: Benefits still outweigh risks from paclitaxel-coated devices for PAD
The Food and Drug Administration has issued a letter alerting health care providers that it is aware of and examining recent data on an increase in long-term mortality rates for patients receiving paclitaxel-coated balloons and paclitaxel-eluting stents for treatment of peripheral artery disease.
“Currently, the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use,” William Maisel, MD, MPH, chief medical officer of the Center for Devices and Radiological Health at the FDA, wrote in a letter to health care providers.
The FDA letter was in response to a recent systematic review of paclitaxel-coated balloons and stents recently published in the Journal of the American Heart Association. Konstantinos Katsanos, MD, PhD, from Patras University Hospital in Rion, Greece, and colleagues performed the systematic review and meta-analysis of 28 randomized controlled trials with 4,663 patients who received paclitaxel-coated devices in the femoral and/or popliteal arteries and found similar 1-year risk of all-cause patient mortality (2.3%; risk ratio, 1.08; 95% confidence interval, 0.72-1.61). However, there was an increased risk of all-cause mortality for patients with paclitaxel-coated devices at 2 years (7.2% vs. 3.8%; RR, 1.68; 95% CI, 1.15-2.47) and at 5 years (14.7% vs. 8.1%; RR, 1.93; 95% CI, 1.27-2.93), compared with control groups. The number needed to harm at 2 years was 29 patients (95% CI, 19-59) and 14 patients (95% CI, 9-32) at 5 years. Their meta regression analysis found a significant link between paclitaxel exposure and absolute risk of death.
“Actual causes for this serious late side effect remain unknown, and further investigations with longer-term follow-up are urgently warranted,” Dr. Katsanos and colleagues wrote in their review.
The FDA told health care providers of patients with paclitaxel-coated balloons and paclitaxel-eluting stents to continue surveillance of these patients per standard of care, to discuss the risks and benefits of PAD treatment options with patients, and to report any adverse or suspected adverse events to MedWatch.
The FDA said they are currently evaluating long-term data on paclitaxel-coated products to determine whether the devices carry an increased risk of death or other long-term risks, and noted there were several paclitaxel-coated balloons or paclitaxel-eluting stents that have either been approved or are under study in the United States.
SOURCE: Katsanos K et al. J Am Heart Assoc. 2018. doi: 10.1161/JAHA.118.011245.
The Food and Drug Administration has issued a letter alerting health care providers that it is aware of and examining recent data on an increase in long-term mortality rates for patients receiving paclitaxel-coated balloons and paclitaxel-eluting stents for treatment of peripheral artery disease.
“Currently, the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use,” William Maisel, MD, MPH, chief medical officer of the Center for Devices and Radiological Health at the FDA, wrote in a letter to health care providers.
The FDA letter was in response to a recent systematic review of paclitaxel-coated balloons and stents recently published in the Journal of the American Heart Association. Konstantinos Katsanos, MD, PhD, from Patras University Hospital in Rion, Greece, and colleagues performed the systematic review and meta-analysis of 28 randomized controlled trials with 4,663 patients who received paclitaxel-coated devices in the femoral and/or popliteal arteries and found similar 1-year risk of all-cause patient mortality (2.3%; risk ratio, 1.08; 95% confidence interval, 0.72-1.61). However, there was an increased risk of all-cause mortality for patients with paclitaxel-coated devices at 2 years (7.2% vs. 3.8%; RR, 1.68; 95% CI, 1.15-2.47) and at 5 years (14.7% vs. 8.1%; RR, 1.93; 95% CI, 1.27-2.93), compared with control groups. The number needed to harm at 2 years was 29 patients (95% CI, 19-59) and 14 patients (95% CI, 9-32) at 5 years. Their meta regression analysis found a significant link between paclitaxel exposure and absolute risk of death.
“Actual causes for this serious late side effect remain unknown, and further investigations with longer-term follow-up are urgently warranted,” Dr. Katsanos and colleagues wrote in their review.
The FDA told health care providers of patients with paclitaxel-coated balloons and paclitaxel-eluting stents to continue surveillance of these patients per standard of care, to discuss the risks and benefits of PAD treatment options with patients, and to report any adverse or suspected adverse events to MedWatch.
The FDA said they are currently evaluating long-term data on paclitaxel-coated products to determine whether the devices carry an increased risk of death or other long-term risks, and noted there were several paclitaxel-coated balloons or paclitaxel-eluting stents that have either been approved or are under study in the United States.
SOURCE: Katsanos K et al. J Am Heart Assoc. 2018. doi: 10.1161/JAHA.118.011245.
The Food and Drug Administration has issued a letter alerting health care providers that it is aware of and examining recent data on an increase in long-term mortality rates for patients receiving paclitaxel-coated balloons and paclitaxel-eluting stents for treatment of peripheral artery disease.
“Currently, the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use,” William Maisel, MD, MPH, chief medical officer of the Center for Devices and Radiological Health at the FDA, wrote in a letter to health care providers.
The FDA letter was in response to a recent systematic review of paclitaxel-coated balloons and stents recently published in the Journal of the American Heart Association. Konstantinos Katsanos, MD, PhD, from Patras University Hospital in Rion, Greece, and colleagues performed the systematic review and meta-analysis of 28 randomized controlled trials with 4,663 patients who received paclitaxel-coated devices in the femoral and/or popliteal arteries and found similar 1-year risk of all-cause patient mortality (2.3%; risk ratio, 1.08; 95% confidence interval, 0.72-1.61). However, there was an increased risk of all-cause mortality for patients with paclitaxel-coated devices at 2 years (7.2% vs. 3.8%; RR, 1.68; 95% CI, 1.15-2.47) and at 5 years (14.7% vs. 8.1%; RR, 1.93; 95% CI, 1.27-2.93), compared with control groups. The number needed to harm at 2 years was 29 patients (95% CI, 19-59) and 14 patients (95% CI, 9-32) at 5 years. Their meta regression analysis found a significant link between paclitaxel exposure and absolute risk of death.
“Actual causes for this serious late side effect remain unknown, and further investigations with longer-term follow-up are urgently warranted,” Dr. Katsanos and colleagues wrote in their review.
The FDA told health care providers of patients with paclitaxel-coated balloons and paclitaxel-eluting stents to continue surveillance of these patients per standard of care, to discuss the risks and benefits of PAD treatment options with patients, and to report any adverse or suspected adverse events to MedWatch.
The FDA said they are currently evaluating long-term data on paclitaxel-coated products to determine whether the devices carry an increased risk of death or other long-term risks, and noted there were several paclitaxel-coated balloons or paclitaxel-eluting stents that have either been approved or are under study in the United States.
SOURCE: Katsanos K et al. J Am Heart Assoc. 2018. doi: 10.1161/JAHA.118.011245.
Key clinical point: In a letter to health care providers, FDA said it was investigating data from a recent meta-analysis of increased long-term mortality risk from paclitaxel-coated balloons and paclitaxel-eluting stents for treatment of peripheral artery disease.
Major finding: All-cause mortality increased significantly after 2 years (7.2% vs. 3.8%) and 5 years (14.7% vs. 8.1%) compared with control groups.
Study details: A systematic review and meta-analysis of 28 randomized controlled trials with 4,663 patients.
Source: Katsanos K et al. J Am Heart Assoc. 2018. doi: 10.1161/JAHA.118.011245.
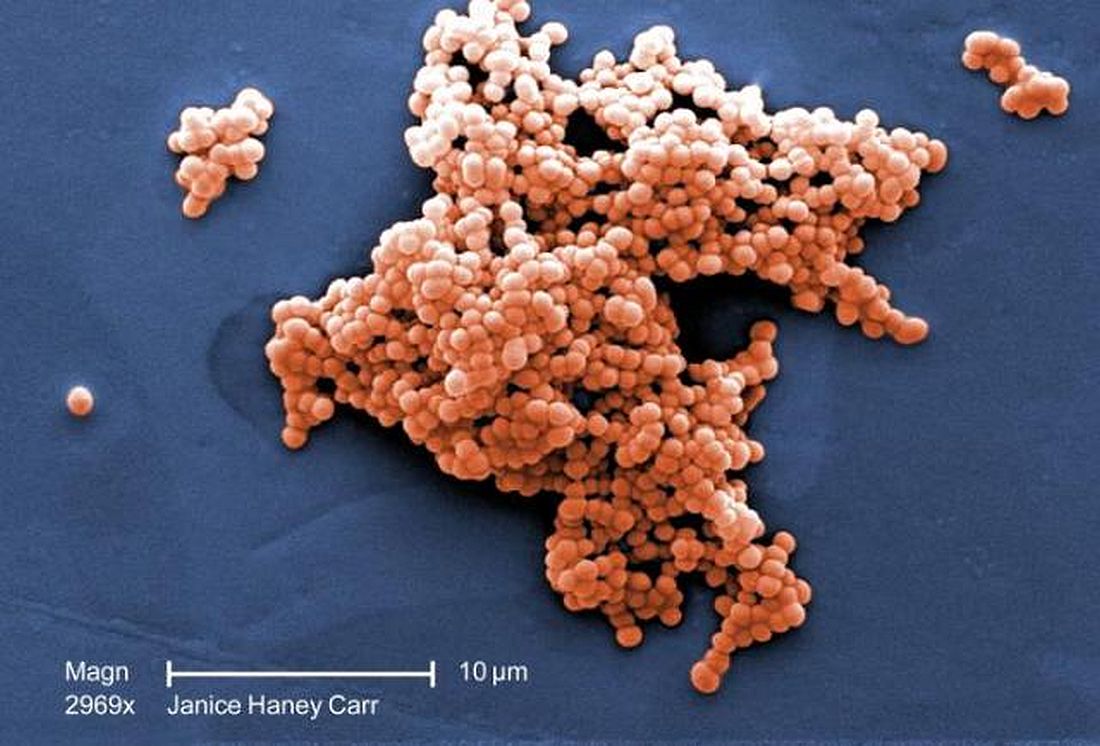
Intrapartum molecular GBS screening reduced newborn early-onset disease, antibiotic use
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: The rate of early-onset disease group B Streptococcus decreased from 1.01/1,000 cases to 0.21/1,000 cases across the antenatal and intrapartum periods.
Study details: A single-center study of antenatal culture screening for 11,226 deliveries during 2006-2009 and intrapartum PCR screening for 18,835 deliveries during 2010-2015.
Disclosures: The authors reported no relevant conflicts of interest.
Source: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Treat-to-target approach for CVD risk factors decreased atherosclerosis in RA patients
Researchers from the Netherlands found that a treat-to-target approach for cardiovascular risk factors in patients with rheumatoid arthritis was effective in reducing clinical and subclinical atherosclerosis; however, the researchers noted there was a “considerable” dropout in the study that could have limited the results, according to data recently published in Annals of the Rheumatic Diseases.
Benjamin Burggraaf, MD, and his associates at Franciscus Gasthuis & Vlietland Hospital in Rotterdam, the Netherlands, performed an open-label, randomized, controlled trial of 320 patients with rheumatoid arthritis (RA) who were younger than 70 years old (mean age, 52.4 years) without a prior history of cardiovascular disease (CVD) and diabetes mellitus. The patients received either usual care for traditional CVD risk factors or a treat-to-target approach using a prespecified protocol for treating hypertension, hyperlipidemia and hypertriglyceridemia, as well hemoglobin A1c greater than 48 mmol/mol. A total of 219 patients (68.4%) finished the study after 5 years. The two groups were similar at baseline, but the treat-to-target group had significantly more women (77.2%) compared with the usual care group (62.0%).
The researchers compared the progression of carotid intima media thickness (cIMT) at baseline and 5 years, with secondary outcomes of nonfatal myocardial infarction, nonfatal stroke, coronary artery bypass grafting, percutaneous coronary intervention, peripheral atherosclerotic arterial disease–related amputation, peripheral atherosclerotic arterial disease revascularization, and death due to cardiovascular causes.
“To account for the high dropout, all missing cIMT values after 5 years of follow-up were imputed with all available cIMT values (baseline, years 1-4) and treatment group as covariate,” the researchers said. “Assuming that unobserved cIMT values were missing at random, missing data were imputed with multiple imputation using the fully conditional specification method for seven cycles.”
Dr. Burggraaf and his colleagues found the treat-to-target group had lower mean cIMT progression (0.023 mm; 95% confidence interval, 0.011-0.036) at 5-year follow-up than did the group that received usual care for CVD risk factors (0.045 mm; 95% CI, 0.030-0.059; P = .028). At 5 years, there were no significant differences between treat-to-target and usual care groups regarding mean systolic blood pressure (124.6 mm Hg vs. 124.7 mm Hg, respectively; P = .97), treat-to-target treatment targets for blood pressure (72.4% for usual care vs. 75.9% for treat-to-target; P = .56) and mean HbA1c (37.6 mmol/mol for treat-to-target vs. 37.0 mmol/mol for usual care; P = .39). The treat-to-target group also had fewer cardiovascular events (two events, 1.3%) compared with the usual care group (seven events, 4.7%; P = .048). There were five patients in the treat-to-target group who died during the study (4.7%), compared with seven patients (3.2%) in the usual care group (P = .51).
“Although the difference in cIMT progression between the groups was relatively small in absolute terms, the relative reduction in progression was almost 50% in favor of the treat-to-target group,” they noted. “In light of the reduction of cardiovascular events, these effects are, in our opinion, clinically relevant.”
Other limitations of the study included the use of cIMT as a “soft endpoint” for modern cardiovascular trials and the use of unblinded cIMT progression measurement. In addition, the researchers noted the study was underpowered, and they used data from a type 2 diabetes mellitus cohort to perform the power calculation, which carried a 50% reduction in CVD risk factors. “We had doubts whether this high risk would apply to patients with RA and therefore used a more conservative target of 20% reduction for cIMT progression,” the researchers said.
This study was funded by the Franciscus Gasthuis & Vlietland Hospital, the Foundation for Research and Development of the Department of Internal Medicine, and the Coolsingel Foundation, Rotterdam. One author reported being a consultant for and receiving lecture honoraria from Merck.
SOURCE: Burggraaf B et al. Ann Rheum Dis. 2019 Jan 4. doi: 10.1136/annrheumdis-2018-214075.
It is well recognized that traditional cardiovascular disease (CVD) risk factors contribute to atherogenesis and CVD events in rheumatoid arthritis (RA) patients at least as much as inflammatory risk factors, and traditional risk factors and inflammatory risk factors may interact (i.e. inflammatory risk factors have a greater impact in the setting of higher number of traditional risk factors).
There is documented reluctance among many rheumatologists to take on the additional burden of screening and managing hyperlipidemia, hypertension, diabetes, weight management, diet, and so on in addition to all the other aspects of managing these patients that take a lot of time. Research is needed on how to efficiently streamline measurement and management of CVD risk in these patients to optimize outcomes.
Jon T. Giles, MD , is a rheumatologist in the division of rheumatology at Columbia University in New York. He was not involved in the study by Burggraaf et al. and reported no relevant conflicts of interest.
It is well recognized that traditional cardiovascular disease (CVD) risk factors contribute to atherogenesis and CVD events in rheumatoid arthritis (RA) patients at least as much as inflammatory risk factors, and traditional risk factors and inflammatory risk factors may interact (i.e. inflammatory risk factors have a greater impact in the setting of higher number of traditional risk factors).
There is documented reluctance among many rheumatologists to take on the additional burden of screening and managing hyperlipidemia, hypertension, diabetes, weight management, diet, and so on in addition to all the other aspects of managing these patients that take a lot of time. Research is needed on how to efficiently streamline measurement and management of CVD risk in these patients to optimize outcomes.
Jon T. Giles, MD , is a rheumatologist in the division of rheumatology at Columbia University in New York. He was not involved in the study by Burggraaf et al. and reported no relevant conflicts of interest.
It is well recognized that traditional cardiovascular disease (CVD) risk factors contribute to atherogenesis and CVD events in rheumatoid arthritis (RA) patients at least as much as inflammatory risk factors, and traditional risk factors and inflammatory risk factors may interact (i.e. inflammatory risk factors have a greater impact in the setting of higher number of traditional risk factors).
There is documented reluctance among many rheumatologists to take on the additional burden of screening and managing hyperlipidemia, hypertension, diabetes, weight management, diet, and so on in addition to all the other aspects of managing these patients that take a lot of time. Research is needed on how to efficiently streamline measurement and management of CVD risk in these patients to optimize outcomes.
Jon T. Giles, MD , is a rheumatologist in the division of rheumatology at Columbia University in New York. He was not involved in the study by Burggraaf et al. and reported no relevant conflicts of interest.
Researchers from the Netherlands found that a treat-to-target approach for cardiovascular risk factors in patients with rheumatoid arthritis was effective in reducing clinical and subclinical atherosclerosis; however, the researchers noted there was a “considerable” dropout in the study that could have limited the results, according to data recently published in Annals of the Rheumatic Diseases.
Benjamin Burggraaf, MD, and his associates at Franciscus Gasthuis & Vlietland Hospital in Rotterdam, the Netherlands, performed an open-label, randomized, controlled trial of 320 patients with rheumatoid arthritis (RA) who were younger than 70 years old (mean age, 52.4 years) without a prior history of cardiovascular disease (CVD) and diabetes mellitus. The patients received either usual care for traditional CVD risk factors or a treat-to-target approach using a prespecified protocol for treating hypertension, hyperlipidemia and hypertriglyceridemia, as well hemoglobin A1c greater than 48 mmol/mol. A total of 219 patients (68.4%) finished the study after 5 years. The two groups were similar at baseline, but the treat-to-target group had significantly more women (77.2%) compared with the usual care group (62.0%).
The researchers compared the progression of carotid intima media thickness (cIMT) at baseline and 5 years, with secondary outcomes of nonfatal myocardial infarction, nonfatal stroke, coronary artery bypass grafting, percutaneous coronary intervention, peripheral atherosclerotic arterial disease–related amputation, peripheral atherosclerotic arterial disease revascularization, and death due to cardiovascular causes.
“To account for the high dropout, all missing cIMT values after 5 years of follow-up were imputed with all available cIMT values (baseline, years 1-4) and treatment group as covariate,” the researchers said. “Assuming that unobserved cIMT values were missing at random, missing data were imputed with multiple imputation using the fully conditional specification method for seven cycles.”
Dr. Burggraaf and his colleagues found the treat-to-target group had lower mean cIMT progression (0.023 mm; 95% confidence interval, 0.011-0.036) at 5-year follow-up than did the group that received usual care for CVD risk factors (0.045 mm; 95% CI, 0.030-0.059; P = .028). At 5 years, there were no significant differences between treat-to-target and usual care groups regarding mean systolic blood pressure (124.6 mm Hg vs. 124.7 mm Hg, respectively; P = .97), treat-to-target treatment targets for blood pressure (72.4% for usual care vs. 75.9% for treat-to-target; P = .56) and mean HbA1c (37.6 mmol/mol for treat-to-target vs. 37.0 mmol/mol for usual care; P = .39). The treat-to-target group also had fewer cardiovascular events (two events, 1.3%) compared with the usual care group (seven events, 4.7%; P = .048). There were five patients in the treat-to-target group who died during the study (4.7%), compared with seven patients (3.2%) in the usual care group (P = .51).
“Although the difference in cIMT progression between the groups was relatively small in absolute terms, the relative reduction in progression was almost 50% in favor of the treat-to-target group,” they noted. “In light of the reduction of cardiovascular events, these effects are, in our opinion, clinically relevant.”
Other limitations of the study included the use of cIMT as a “soft endpoint” for modern cardiovascular trials and the use of unblinded cIMT progression measurement. In addition, the researchers noted the study was underpowered, and they used data from a type 2 diabetes mellitus cohort to perform the power calculation, which carried a 50% reduction in CVD risk factors. “We had doubts whether this high risk would apply to patients with RA and therefore used a more conservative target of 20% reduction for cIMT progression,” the researchers said.
This study was funded by the Franciscus Gasthuis & Vlietland Hospital, the Foundation for Research and Development of the Department of Internal Medicine, and the Coolsingel Foundation, Rotterdam. One author reported being a consultant for and receiving lecture honoraria from Merck.
SOURCE: Burggraaf B et al. Ann Rheum Dis. 2019 Jan 4. doi: 10.1136/annrheumdis-2018-214075.
Researchers from the Netherlands found that a treat-to-target approach for cardiovascular risk factors in patients with rheumatoid arthritis was effective in reducing clinical and subclinical atherosclerosis; however, the researchers noted there was a “considerable” dropout in the study that could have limited the results, according to data recently published in Annals of the Rheumatic Diseases.
Benjamin Burggraaf, MD, and his associates at Franciscus Gasthuis & Vlietland Hospital in Rotterdam, the Netherlands, performed an open-label, randomized, controlled trial of 320 patients with rheumatoid arthritis (RA) who were younger than 70 years old (mean age, 52.4 years) without a prior history of cardiovascular disease (CVD) and diabetes mellitus. The patients received either usual care for traditional CVD risk factors or a treat-to-target approach using a prespecified protocol for treating hypertension, hyperlipidemia and hypertriglyceridemia, as well hemoglobin A1c greater than 48 mmol/mol. A total of 219 patients (68.4%) finished the study after 5 years. The two groups were similar at baseline, but the treat-to-target group had significantly more women (77.2%) compared with the usual care group (62.0%).
The researchers compared the progression of carotid intima media thickness (cIMT) at baseline and 5 years, with secondary outcomes of nonfatal myocardial infarction, nonfatal stroke, coronary artery bypass grafting, percutaneous coronary intervention, peripheral atherosclerotic arterial disease–related amputation, peripheral atherosclerotic arterial disease revascularization, and death due to cardiovascular causes.
“To account for the high dropout, all missing cIMT values after 5 years of follow-up were imputed with all available cIMT values (baseline, years 1-4) and treatment group as covariate,” the researchers said. “Assuming that unobserved cIMT values were missing at random, missing data were imputed with multiple imputation using the fully conditional specification method for seven cycles.”
Dr. Burggraaf and his colleagues found the treat-to-target group had lower mean cIMT progression (0.023 mm; 95% confidence interval, 0.011-0.036) at 5-year follow-up than did the group that received usual care for CVD risk factors (0.045 mm; 95% CI, 0.030-0.059; P = .028). At 5 years, there were no significant differences between treat-to-target and usual care groups regarding mean systolic blood pressure (124.6 mm Hg vs. 124.7 mm Hg, respectively; P = .97), treat-to-target treatment targets for blood pressure (72.4% for usual care vs. 75.9% for treat-to-target; P = .56) and mean HbA1c (37.6 mmol/mol for treat-to-target vs. 37.0 mmol/mol for usual care; P = .39). The treat-to-target group also had fewer cardiovascular events (two events, 1.3%) compared with the usual care group (seven events, 4.7%; P = .048). There were five patients in the treat-to-target group who died during the study (4.7%), compared with seven patients (3.2%) in the usual care group (P = .51).
“Although the difference in cIMT progression between the groups was relatively small in absolute terms, the relative reduction in progression was almost 50% in favor of the treat-to-target group,” they noted. “In light of the reduction of cardiovascular events, these effects are, in our opinion, clinically relevant.”
Other limitations of the study included the use of cIMT as a “soft endpoint” for modern cardiovascular trials and the use of unblinded cIMT progression measurement. In addition, the researchers noted the study was underpowered, and they used data from a type 2 diabetes mellitus cohort to perform the power calculation, which carried a 50% reduction in CVD risk factors. “We had doubts whether this high risk would apply to patients with RA and therefore used a more conservative target of 20% reduction for cIMT progression,” the researchers said.
This study was funded by the Franciscus Gasthuis & Vlietland Hospital, the Foundation for Research and Development of the Department of Internal Medicine, and the Coolsingel Foundation, Rotterdam. One author reported being a consultant for and receiving lecture honoraria from Merck.
SOURCE: Burggraaf B et al. Ann Rheum Dis. 2019 Jan 4. doi: 10.1136/annrheumdis-2018-214075.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: The treat-to-target group had greater mean carotid intima media thickness progression (0.023 mm; 95% confidence interval, 0.011-0.036) at 5-year follow-up compared with the group that received usual care for cardiovascular disease risk factors (0.045 mm; 95% CI, 0.030-0.059; P = .028).
Study details: An open-label, randomized, controlled trial of 320 RA patients who received a treat-to-target intervention or usual care for cardiovascular disease risk factors.
Disclosures: This study was funded by the Franciscus Gasthuis & Vlietland Hospital, the Foundation for Research and Development of the Department of Internal Medicine, and the Coolsingel Foundation, Rotterdam. One author reported being a consultant for and receiving lecture honoraria from Merck.
Source: Burggraaf B et al. Ann Rheum Dis. 2019 Jan 4. doi: 10.1136/annrheumdis-2018-214075.
Incidence of late-onset GBS cases are higher than early-onset disease
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
FROM JAMA PEDIATRICS
Key clinical point: Between 2006 and 2015, early-onset disease cases of group B Streptococcus (GBS) declined, while the incidence of late-onset cases did not change.
Major finding: The rate of early-onset GBS declined from 0.37 to 0.23 per 1,000 live births and the rate of late-onset GBS cases remained at a mean 0.31 per 1,000 live births.
Study details: A population-based study of infants with early-onset disease and late-onset disease GBS from 10 different states in the Active Bacterial Core surveillance program between 2006 and 2015.
Disclosures: This study was funded in part by the Centers for Disease Control and Prevention. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
Source: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
ACOG updates guidance on chronic hypertension in pregnancy, gestational hypertension
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
FROM OBSTETRICS & GYNECOLOGY
Postdiagnosis statin use lowers mortality rate for patients with HCC
Statin use after a diagnosis of hepatocellular carcinoma (HCC) was associated with a reduced risk of all-cause and cancer-specific mortality, according to recent research published in Clinical Gastroenterology and Hepatology.
“Our current findings are biologically plausible since statins inhibit not only cholesterol synthesis but also reduce other important downstream products, including membrane integrity maintenance, cell signaling, protein synthesis, and cell-cycle progression,” wrote Aaron P. Thrift, PhD, of the section of epidemiology and population sciences and department of medicine at Baylor College of Medicine in Houston, and his colleagues. “Not only can statins have a direct impact on cancer cells through inhibition of the mevalonate pathway within the cancer cells, but the reduction of circulating cholesterol levels through hepatic pathways is indeed considered important.”
Dr. Thrift and his colleagues performed a retrospective cohort analysis of data from 15,422 patients with HCC in the VA Central Cancer Registry who were diagnosed between 2002 and 2016 and filled a prescription for statins. The researchers looked at statin prescriptions filled prior to and after diagnosis, following patients from diagnosis up to a 3-month lag period. The statins analyzed included atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin.
Overall, 78.8% of patients died during 26,680 person-years of follow-up and the median survival time was 17.24 months. The researchers found 14.9% of patients (2,293 patients) with HCC filled prescriptions for statins after their cancer diagnosis. The median time to begin statins after diagnosis was 2.37 months, and patients who used statins after diagnosis had a median survival time of 26.38 months compared with 15.67 months for patients who did not use statins after diagnosis. For HCC patients who used statins, there was a decreased risk of all-cause mortality (hazard ratio, 0.89; 95% confidence interval, 0.83-0.95) and cancer-specific mortality (adjusted HR, 0.85; 95% CI, 0.77-0.93), which was consistent for both high-dose and low-dose statins and for lag periods between 0 months and 12 months after diagnosis.
Limitations in the study were the exclusion of any statins filled at non-VA pharmacies, baseline differences in statin users and nonstatin users that could have affected results, potential misclassification of cirrhosis in the registry, and the lack of generalization to other populations due to a veteran-specific patient cohort.
This study was funded by the National Institutes of Health and VA Health Services Research and Development Service Center for Innovations in Quality, Effectiveness, and Safety. The authors report having no conflicts of interest.
SOURCE: Thrift AP et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2018.12.046.
Statin use after a diagnosis of hepatocellular carcinoma (HCC) was associated with a reduced risk of all-cause and cancer-specific mortality, according to recent research published in Clinical Gastroenterology and Hepatology.
“Our current findings are biologically plausible since statins inhibit not only cholesterol synthesis but also reduce other important downstream products, including membrane integrity maintenance, cell signaling, protein synthesis, and cell-cycle progression,” wrote Aaron P. Thrift, PhD, of the section of epidemiology and population sciences and department of medicine at Baylor College of Medicine in Houston, and his colleagues. “Not only can statins have a direct impact on cancer cells through inhibition of the mevalonate pathway within the cancer cells, but the reduction of circulating cholesterol levels through hepatic pathways is indeed considered important.”
Dr. Thrift and his colleagues performed a retrospective cohort analysis of data from 15,422 patients with HCC in the VA Central Cancer Registry who were diagnosed between 2002 and 2016 and filled a prescription for statins. The researchers looked at statin prescriptions filled prior to and after diagnosis, following patients from diagnosis up to a 3-month lag period. The statins analyzed included atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin.
Overall, 78.8% of patients died during 26,680 person-years of follow-up and the median survival time was 17.24 months. The researchers found 14.9% of patients (2,293 patients) with HCC filled prescriptions for statins after their cancer diagnosis. The median time to begin statins after diagnosis was 2.37 months, and patients who used statins after diagnosis had a median survival time of 26.38 months compared with 15.67 months for patients who did not use statins after diagnosis. For HCC patients who used statins, there was a decreased risk of all-cause mortality (hazard ratio, 0.89; 95% confidence interval, 0.83-0.95) and cancer-specific mortality (adjusted HR, 0.85; 95% CI, 0.77-0.93), which was consistent for both high-dose and low-dose statins and for lag periods between 0 months and 12 months after diagnosis.
Limitations in the study were the exclusion of any statins filled at non-VA pharmacies, baseline differences in statin users and nonstatin users that could have affected results, potential misclassification of cirrhosis in the registry, and the lack of generalization to other populations due to a veteran-specific patient cohort.
This study was funded by the National Institutes of Health and VA Health Services Research and Development Service Center for Innovations in Quality, Effectiveness, and Safety. The authors report having no conflicts of interest.
SOURCE: Thrift AP et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2018.12.046.
Statin use after a diagnosis of hepatocellular carcinoma (HCC) was associated with a reduced risk of all-cause and cancer-specific mortality, according to recent research published in Clinical Gastroenterology and Hepatology.
“Our current findings are biologically plausible since statins inhibit not only cholesterol synthesis but also reduce other important downstream products, including membrane integrity maintenance, cell signaling, protein synthesis, and cell-cycle progression,” wrote Aaron P. Thrift, PhD, of the section of epidemiology and population sciences and department of medicine at Baylor College of Medicine in Houston, and his colleagues. “Not only can statins have a direct impact on cancer cells through inhibition of the mevalonate pathway within the cancer cells, but the reduction of circulating cholesterol levels through hepatic pathways is indeed considered important.”
Dr. Thrift and his colleagues performed a retrospective cohort analysis of data from 15,422 patients with HCC in the VA Central Cancer Registry who were diagnosed between 2002 and 2016 and filled a prescription for statins. The researchers looked at statin prescriptions filled prior to and after diagnosis, following patients from diagnosis up to a 3-month lag period. The statins analyzed included atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin.
Overall, 78.8% of patients died during 26,680 person-years of follow-up and the median survival time was 17.24 months. The researchers found 14.9% of patients (2,293 patients) with HCC filled prescriptions for statins after their cancer diagnosis. The median time to begin statins after diagnosis was 2.37 months, and patients who used statins after diagnosis had a median survival time of 26.38 months compared with 15.67 months for patients who did not use statins after diagnosis. For HCC patients who used statins, there was a decreased risk of all-cause mortality (hazard ratio, 0.89; 95% confidence interval, 0.83-0.95) and cancer-specific mortality (adjusted HR, 0.85; 95% CI, 0.77-0.93), which was consistent for both high-dose and low-dose statins and for lag periods between 0 months and 12 months after diagnosis.
Limitations in the study were the exclusion of any statins filled at non-VA pharmacies, baseline differences in statin users and nonstatin users that could have affected results, potential misclassification of cirrhosis in the registry, and the lack of generalization to other populations due to a veteran-specific patient cohort.
This study was funded by the National Institutes of Health and VA Health Services Research and Development Service Center for Innovations in Quality, Effectiveness, and Safety. The authors report having no conflicts of interest.
SOURCE: Thrift AP et al. Clin Gastroenterol Hepatol. 2019. doi: 10.1016/j.cgh.2018.12.046.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The use of statins after diagnosis of hepatocellular carcinoma was associated with a lower risk of death.
Major finding: In 14.9% of patients who used statins after diagnosis, the rate of all-cause mortality (hazard ratio, 0.89; 95% confidence interval, 0.83-0.95) and cancer-specific mortality (adjusted HR, 0.85; 95% CI, 0.77-0.93) was lower, and was consistent for both high-dose and low-dose statins.
Study details: A retrospective analysis of 15,422 patients with hepatocellular carcinoma in the VA Central Cancer Registry between 2002 and 2016.
Disclosures: This study was funded by the National Institutes of Health and VA Health Services Research and Development Service Center for Innovations in Quality, Effectiveness, and Safety. The authors report having no conflicts of interest.
Source: Thrift AP et al. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.12.046.
LAIV4 was less effective for children than IIV against influenza A/H1N1pdm09
The live attenuated influenza vaccine was less effective against the influenza A/H1N1pdm09 virus in children and adolescents across multiple influenza seasons between 2013 and 2016, compared with the inactivated influenza vaccine, according to research published in the journal Pediatrics.
Jessie R. Chung, MPH, from the influenza division at the Centers for Disease Control and Prevention in Atlanta, and her colleagues performed an analysis of five different studies where vaccine effectiveness (VE) was examined for quadrivalent live attenuated vaccine (LAIV4) and inactivated influenza vaccine (IIV) in children and adolescents aged 2-17 years from 42 states.
The analysis included data from the U.S. Influenza Vaccine Effectiveness Network (6,793 patients), a study from the Louisiana State University Health Sciences Center (3,822 patients), the Influenza Clinical Investigation for Children (3,521 patients), Department of Defense Global, Laboratory-based, Influenza Surveillance Program (1,935 patients), and the Influenza Incidence Surveillance Project (1,102 patients) between the periods of 2013-2014 and 2015-2016. The researchers sourced current and previous season vaccination history from electronic medical records and immunization registries.
Of patients who were vaccinated across all seasons, there was 67% effectiveness against influenza A/H1N1pdm09 (95% confidence interval, 62%-72%) for those who received the IIV and 20% (95% CI, −6%-39%) for LAIV4. Among patients who received the LAIV4 vaccination, there was a significantly higher likelihood of developing influenza A/H1N1pdm09 (odds ratio, 2.66; 95% CI, 2.06-3.44) compared with patients who received the IIV vaccination.
With regard to other strains, there was similar effectiveness against influenza A/H3N2 and influenza B with LAIV4 and IIV vaccinations.
“In contrast to findings of reduced LAIV4 effectiveness against influenza A/H1N1pdm09 viruses, our results suggest a possible but nonsignificant benefit of LAIV4 over IIV against influenza B viruses, which has been described previously,” the investigators wrote.
Limitations of the study included having data only one season prior to enrollment and little available demographic information beyond age, gender, and geographic location.
The Influenza Clinical Investigation for Children was funded by MedImmune, a member of the AstraZeneca Group. Two of the researchers are employees of AstraZeneca. The other authors reported having no conflicts of interest. The U.S. Influenza Vaccine Effectiveness Network was supported by the CDC through cooperative agreements with the University of Michigan, Kaiser Permanente Washington Health Research Institute, Marshfield Clinic Research Institute, University of Pittsburgh, and Baylor Scott & White Health. At the University of Pittsburgh, the project also was supported by the National Institutes of Health.
SOURCE: Chung JR et al. Pediatrics. 2018. doi: 10.1542/peds.2018-2094.
There are many explanations for the decline in effectiveness of the live attenuated influenza vaccine (LAIV4), but the data are complicated by conflicting information from studies outside the United States indicating “reasonable protection” against influenza A/H1N1pdm09, A/H3N2, and influenza B, compared with the inactivated influenza virus (IIV), Pedro A. Piedra, MD, wrote in an accompanying editorial.
In 2016, the World Health Organization met to discuss LAIV effectiveness and highlighted factors such as methodological study differences, inadequate vaccine handling at distribution centers, intrinsic virological differences of the A/H1N1pdm09 virus, and increased preexisting population immunity in the United States since 2010 as potential explanations. During the transition from LAIV3 to LAIV4 for the 2013-2014 influenza season, viral interference may have also occurred when the influenza B strain was introduced into the vaccine, he added.
According to the CDC’s Advisory Committee on Immunization Practices (ACIP), viral growth properties of A/H1N1pdm09 has improved in LAIV4, and viral shedding also has improved for children between 2 years and 4 years of age. Although effectiveness numbers were not available for the ACIP recommendation, an interim analysis from Public Health England for the 2017-2018 influenza season found a vaccine effectiveness of 90.3% (95% confidence interval, 16.4%-98.9%).
“This early result is encouraging and supports the reintroduction of LAIV4 in the United States as an option for the control of seasonal influenza,” he said. “It also highlights the need for annual influenza vaccine effectiveness estimates and the importance of the U.S. Influenza Vaccine Effectiveness Network in providing updated information for ACIP recommendations.”
Dr. Piedra is from the departments of molecular virology and microbiology and pediatrics, Baylor College of Medicine, Houston. He reports being a consultant for AstraZeneca, Sanofi Pasteur, GlaxoSmithKline, and Merck Sharp and Dohme, and he has received travel support to present at an influenza seminar supported by Seqirus. His comments are from an editorial accompanying the article by Chung and colleagues ( Pediatrics. 2019. doi: 10.1542/peds.2018- 3290 ).
There are many explanations for the decline in effectiveness of the live attenuated influenza vaccine (LAIV4), but the data are complicated by conflicting information from studies outside the United States indicating “reasonable protection” against influenza A/H1N1pdm09, A/H3N2, and influenza B, compared with the inactivated influenza virus (IIV), Pedro A. Piedra, MD, wrote in an accompanying editorial.
In 2016, the World Health Organization met to discuss LAIV effectiveness and highlighted factors such as methodological study differences, inadequate vaccine handling at distribution centers, intrinsic virological differences of the A/H1N1pdm09 virus, and increased preexisting population immunity in the United States since 2010 as potential explanations. During the transition from LAIV3 to LAIV4 for the 2013-2014 influenza season, viral interference may have also occurred when the influenza B strain was introduced into the vaccine, he added.
According to the CDC’s Advisory Committee on Immunization Practices (ACIP), viral growth properties of A/H1N1pdm09 has improved in LAIV4, and viral shedding also has improved for children between 2 years and 4 years of age. Although effectiveness numbers were not available for the ACIP recommendation, an interim analysis from Public Health England for the 2017-2018 influenza season found a vaccine effectiveness of 90.3% (95% confidence interval, 16.4%-98.9%).
“This early result is encouraging and supports the reintroduction of LAIV4 in the United States as an option for the control of seasonal influenza,” he said. “It also highlights the need for annual influenza vaccine effectiveness estimates and the importance of the U.S. Influenza Vaccine Effectiveness Network in providing updated information for ACIP recommendations.”
Dr. Piedra is from the departments of molecular virology and microbiology and pediatrics, Baylor College of Medicine, Houston. He reports being a consultant for AstraZeneca, Sanofi Pasteur, GlaxoSmithKline, and Merck Sharp and Dohme, and he has received travel support to present at an influenza seminar supported by Seqirus. His comments are from an editorial accompanying the article by Chung and colleagues ( Pediatrics. 2019. doi: 10.1542/peds.2018- 3290 ).
There are many explanations for the decline in effectiveness of the live attenuated influenza vaccine (LAIV4), but the data are complicated by conflicting information from studies outside the United States indicating “reasonable protection” against influenza A/H1N1pdm09, A/H3N2, and influenza B, compared with the inactivated influenza virus (IIV), Pedro A. Piedra, MD, wrote in an accompanying editorial.
In 2016, the World Health Organization met to discuss LAIV effectiveness and highlighted factors such as methodological study differences, inadequate vaccine handling at distribution centers, intrinsic virological differences of the A/H1N1pdm09 virus, and increased preexisting population immunity in the United States since 2010 as potential explanations. During the transition from LAIV3 to LAIV4 for the 2013-2014 influenza season, viral interference may have also occurred when the influenza B strain was introduced into the vaccine, he added.
According to the CDC’s Advisory Committee on Immunization Practices (ACIP), viral growth properties of A/H1N1pdm09 has improved in LAIV4, and viral shedding also has improved for children between 2 years and 4 years of age. Although effectiveness numbers were not available for the ACIP recommendation, an interim analysis from Public Health England for the 2017-2018 influenza season found a vaccine effectiveness of 90.3% (95% confidence interval, 16.4%-98.9%).
“This early result is encouraging and supports the reintroduction of LAIV4 in the United States as an option for the control of seasonal influenza,” he said. “It also highlights the need for annual influenza vaccine effectiveness estimates and the importance of the U.S. Influenza Vaccine Effectiveness Network in providing updated information for ACIP recommendations.”
Dr. Piedra is from the departments of molecular virology and microbiology and pediatrics, Baylor College of Medicine, Houston. He reports being a consultant for AstraZeneca, Sanofi Pasteur, GlaxoSmithKline, and Merck Sharp and Dohme, and he has received travel support to present at an influenza seminar supported by Seqirus. His comments are from an editorial accompanying the article by Chung and colleagues ( Pediatrics. 2019. doi: 10.1542/peds.2018- 3290 ).
The live attenuated influenza vaccine was less effective against the influenza A/H1N1pdm09 virus in children and adolescents across multiple influenza seasons between 2013 and 2016, compared with the inactivated influenza vaccine, according to research published in the journal Pediatrics.
Jessie R. Chung, MPH, from the influenza division at the Centers for Disease Control and Prevention in Atlanta, and her colleagues performed an analysis of five different studies where vaccine effectiveness (VE) was examined for quadrivalent live attenuated vaccine (LAIV4) and inactivated influenza vaccine (IIV) in children and adolescents aged 2-17 years from 42 states.
The analysis included data from the U.S. Influenza Vaccine Effectiveness Network (6,793 patients), a study from the Louisiana State University Health Sciences Center (3,822 patients), the Influenza Clinical Investigation for Children (3,521 patients), Department of Defense Global, Laboratory-based, Influenza Surveillance Program (1,935 patients), and the Influenza Incidence Surveillance Project (1,102 patients) between the periods of 2013-2014 and 2015-2016. The researchers sourced current and previous season vaccination history from electronic medical records and immunization registries.
Of patients who were vaccinated across all seasons, there was 67% effectiveness against influenza A/H1N1pdm09 (95% confidence interval, 62%-72%) for those who received the IIV and 20% (95% CI, −6%-39%) for LAIV4. Among patients who received the LAIV4 vaccination, there was a significantly higher likelihood of developing influenza A/H1N1pdm09 (odds ratio, 2.66; 95% CI, 2.06-3.44) compared with patients who received the IIV vaccination.
With regard to other strains, there was similar effectiveness against influenza A/H3N2 and influenza B with LAIV4 and IIV vaccinations.
“In contrast to findings of reduced LAIV4 effectiveness against influenza A/H1N1pdm09 viruses, our results suggest a possible but nonsignificant benefit of LAIV4 over IIV against influenza B viruses, which has been described previously,” the investigators wrote.
Limitations of the study included having data only one season prior to enrollment and little available demographic information beyond age, gender, and geographic location.
The Influenza Clinical Investigation for Children was funded by MedImmune, a member of the AstraZeneca Group. Two of the researchers are employees of AstraZeneca. The other authors reported having no conflicts of interest. The U.S. Influenza Vaccine Effectiveness Network was supported by the CDC through cooperative agreements with the University of Michigan, Kaiser Permanente Washington Health Research Institute, Marshfield Clinic Research Institute, University of Pittsburgh, and Baylor Scott & White Health. At the University of Pittsburgh, the project also was supported by the National Institutes of Health.
SOURCE: Chung JR et al. Pediatrics. 2018. doi: 10.1542/peds.2018-2094.
The live attenuated influenza vaccine was less effective against the influenza A/H1N1pdm09 virus in children and adolescents across multiple influenza seasons between 2013 and 2016, compared with the inactivated influenza vaccine, according to research published in the journal Pediatrics.
Jessie R. Chung, MPH, from the influenza division at the Centers for Disease Control and Prevention in Atlanta, and her colleagues performed an analysis of five different studies where vaccine effectiveness (VE) was examined for quadrivalent live attenuated vaccine (LAIV4) and inactivated influenza vaccine (IIV) in children and adolescents aged 2-17 years from 42 states.
The analysis included data from the U.S. Influenza Vaccine Effectiveness Network (6,793 patients), a study from the Louisiana State University Health Sciences Center (3,822 patients), the Influenza Clinical Investigation for Children (3,521 patients), Department of Defense Global, Laboratory-based, Influenza Surveillance Program (1,935 patients), and the Influenza Incidence Surveillance Project (1,102 patients) between the periods of 2013-2014 and 2015-2016. The researchers sourced current and previous season vaccination history from electronic medical records and immunization registries.
Of patients who were vaccinated across all seasons, there was 67% effectiveness against influenza A/H1N1pdm09 (95% confidence interval, 62%-72%) for those who received the IIV and 20% (95% CI, −6%-39%) for LAIV4. Among patients who received the LAIV4 vaccination, there was a significantly higher likelihood of developing influenza A/H1N1pdm09 (odds ratio, 2.66; 95% CI, 2.06-3.44) compared with patients who received the IIV vaccination.
With regard to other strains, there was similar effectiveness against influenza A/H3N2 and influenza B with LAIV4 and IIV vaccinations.
“In contrast to findings of reduced LAIV4 effectiveness against influenza A/H1N1pdm09 viruses, our results suggest a possible but nonsignificant benefit of LAIV4 over IIV against influenza B viruses, which has been described previously,” the investigators wrote.
Limitations of the study included having data only one season prior to enrollment and little available demographic information beyond age, gender, and geographic location.
The Influenza Clinical Investigation for Children was funded by MedImmune, a member of the AstraZeneca Group. Two of the researchers are employees of AstraZeneca. The other authors reported having no conflicts of interest. The U.S. Influenza Vaccine Effectiveness Network was supported by the CDC through cooperative agreements with the University of Michigan, Kaiser Permanente Washington Health Research Institute, Marshfield Clinic Research Institute, University of Pittsburgh, and Baylor Scott & White Health. At the University of Pittsburgh, the project also was supported by the National Institutes of Health.
SOURCE: Chung JR et al. Pediatrics. 2018. doi: 10.1542/peds.2018-2094.
FROM PEDIATRICS
Key clinical point: The live attenuated influenza vaccine (LAIV4) was significantly less effective than was the inactivated influenza vaccine (IIV) for children against the influenza A/H1N1pdm09 virus across multiple flu seasons.
Major finding:
Study details: A combined analysis of five studies in the United States between the periods of 2013-2014 and 2015-2016 from the U.S. Influenza Vaccine Effectiveness Network.
Disclosures: The Influenza Clinical Investigation for Children was funded by MedImmune, a member of the AstraZeneca Group. Two of the researchers are employees of AstraZeneca. The other authors reported having no conflicts of interest. The U.S. Influenza Vaccine Effectiveness Network was supported by the CDC through cooperative agreements with the University of Michigan, Kaiser Permanente Washington Health Research Institute, Marshfield Clinic Research Institute, University of Pittsburgh, and Baylor Scott & White Health. At the University of Pittsburgh, the project also was supported by the National Institutes of Health.
Source: Chung JR et al. Pediatrics. 2018. doi: 10.1542/peds.2018-2094.
Antidepressants tied to greater hip fracture incidence in older adults
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
In many cases where an adverse event is linked to a medication, such as in the case of gastrointestinal bleeds and blood thinners, the adverse event is not linked to the medication. However, this is not the case with antidepressants and hip fracture, Andrea Iaboni, MD, DPhil, and Donovan T. Maust, MD, wrote in a related editorial (JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3632).
“Patients are routinely prescribed antidepressants following a fracture,” the authors wrote, noting that depression can occur for patients who do not have a history of depression and can last as long as 1 year after hip fracture. The reasons for depression after hip fracture are possibly caused by the consequences of the event or a comorbid condition, such as cerebrovascular disease burden, cognitive impairment, frailty, and impaired functional status. In addition, new antidepressant prescriptions are 10 times the normal rate for older adults in the months after a hip fracture.
Many older users of antidepressants have a hip fracture event in their past, which could be caused by an untreated case of depression and an elevated risk of elevated fall or fracture, as suggested by Brännström et al., while other reasons could include off-label indications such as insomnia, poor motivation during rehabilitation therapy, pain, or hyperactive delirium.
“If individuals with untreated depression are at risk of falls and fractures, it follows that there would be an elevated rate of fractures before antidepressant use,” the authors wrote. “However, as discussed earlier, it is also important to recognize that, during the postfracture period, rightly or wrongly, antidepressants are prescribed at a high rate.”
Clinicians who treat these patients should not stop all antidepressant prescribing to this population. Instead, “a pragmatic preventive approach is warranted, starting with selecting the antidepressant, a cautious initial dose and dose-escalation schedule, a review of potentially interacting therapies ... and referral to fall prevention programs for patients with other risk factors for falls,” they wrote.
“For most older adults, the toll of untreated depression will likely outweigh the potential risks associated with antidepressant use.”
Dr. Iabroni is with the Toronto Rehabilitation Institute and the University of Toronto. He reported receiving fees from serving as a scientific adviser for Winterlight Labs. Dr. Maust is with the department of psychiatry at the University of Michigan, Ann Arbor. He reported no relevant conflicts of interest.
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
Older patients in a Swedish registry who took antidepressants had a greater incidence of hip fracture the year before beginning antidepressant therapy and the year after starting therapy, compared with individuals in a matched control group.
The use of antidepressants is associated with adverse events such as a higher risk of falls, wrote Jon Brännström, MD, and his colleagues in JAMA Psychiatry. Some evidence also suggests that antidepressants “might affect bone metabolism, thereby increasing the risk of hip fracture.”
To examine the relationship between antidepressants and hip fracture, Dr. Brännström and his colleagues performed a nationwide cohort study of 204,072 individuals in the Prescribed Drug Register of Sweden’s National Board of Health and Welfare. All of the individuals were aged at least 65 years (mean age, 80.1 years; 63.1% women) and filled a prescription for an antidepressant between July 2006 and December 2011. Selective serotonin reuptake inhibitors made up 62.6% of the antidepressants used.
Patients who filled an antidepressant prescription during that time period were matched with a control group of individuals by birth year and gender and were studied the year before and after beginning antidepressant therapy.
In the year after initiating antidepressant therapy, there was a 3.5% incidence rate for hip fractures, compared with 1.3% in the control group.
After adjusting the results using a conditional logistic regression model, the highest rate of hip fracture among antidepressant users occurred between 16 days and 30 days prior to filling the prescription (odds ratio, 5.76; 95% confidence interval, 4.73-7.01); this association persisted in further subgroup analyses based on age, reported Dr. Brännström, who is affiliated with the department of community medicine and rehabilitation and geriatric medicine at Umeå University (Sweden), and his colleagues.
They noted that, although the study included all Swedish individuals who filled prescriptions for antidepressants during the study period, there is an absence of primary care comorbidity data and indications for antidepressant use. In addition, the definition of high- and low-medication doses does not always match what is considered high and low therapeutically and the information that can be gleaned from merging data from several different registries was limited.
“These findings raise questions about associations between antidepressant use and hip fracture seen in previous observational studies,” Dr. Brännström and his colleagues wrote. “Further analysis of this association in treatment studies and examination of the incidence of hip fracture before and after the discontinuation of treatment is required and may shed further light on the possible residual risk associated with treatment.”
This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
SOURCE: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
FROM JAMA PSYCHIATRY
Key clinical point: An association was found between greater hip fracture incidence for older individuals taking antidepressants in the year before beginning therapy and the year after starting therapy.
Major finding: Individuals who took antidepressants had a greater incidence of hip fractures in the year before (2.8% vs. 1.1%) and the year after (3.5% vs. 1.3%) beginning antidepressants, compared with individuals in a matched control group.
Study details: A nationwide cohort study of 408,144 individuals in the Prescribed Drugs Register of Sweden’s National Board of Health and Welfare who were aged 65 years or older.
Disclosures: This study was funded by the Swedish Research Council. The authors reported no relevant conflicts of interest.
Source: Brännström J et al. JAMA Psychiatry. 2019 Jan 2. doi: 10.1001/jamapsychiatry.2018.3679.
Review looks at effectiveness of isotretinoin for acne
There is when based on reductions in inflammatory lesion counts, according to a recent Cochrane Review.
“The current recommendation of clinical guidelines that oral isotretinoin should be the first-line treatment for moderate to severe acne unresponsive to previous therapies, being more effective than the use of oral antibiotics plus topical agents, underpins current dermatological practice,” Caroline S. Costa, MD, from the Emergency Medicine and Evidence-Based Medicine department at Universidade Federal de São Paulo and her colleagues wrote in their review. “The recommendation cannot be fully supported with certainty by the finding of this review; however, neither does this review challenge it.”
Dr. Costa and her colleagues identified 31 randomized, controlled trials in the Cochrane Skin Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, and LILACS databases up to July 2017, which altogether included 3,836 participants with mild to severe acne who were aged 12-55 years. The patients received treatment with oral isotretinoin versus placebo or other treatments, such as antibiotics.
In 3 studies that altogether included 400 participants and compared isotretinoin with oral antibiotics plus topical treatments, there was no significant difference with isotretinoin in decreases in the investigator-assessed inflammatory lesion count in participants with moderate to severe acne after 20-24 weeks (risk ratio, 1.01; 95% confidence interval, 0.96-1.06). One serious side effect – Stevens-Johnson syndrome – was noted in the isotretinoin-treated group (RR, 3.00; 95% CI, 0.12-72.98). These results were based on “very-low-quality evidence,” the authors noted.
Two studies also comparing isotretinoin with oral antibiotics and topical treatments in a total of 351 participants showed a 15% improvement in acne severity (RR, 1.15; 95% CI, 1.00-1.32) as assessed by physician’s global evaluation but with a greater number of adverse events considered less severe (RR, 1.67; 95% CI, 1.42-1.98), such as vomiting, nausea, dry lips and skin, and cheilitis.
With regard to dosing, one study with 154 participants with severe acne showed 0.05 mg/kg per day of isotretinoin reduced inflammatory lesion count by 79% after 20 weeks, while 0.1 mg/kg per day and 0.2 mg/kg per day reduced inflammatory lesion counts by 80% and 84%, respectively, after 20 weeks. A different study of 150 participants with severe acne found a 95% decrease in inflammatory lesion counts for 58% of participants receiving 0.1 mg/kg per day, 80% of participants receiving 0.5 mg/kg per day, and 90% of participants receiving 1 mg/kg per day of oral isotretinoin after 20 weeks.
In a randomized, controlled trial with 40 participants with moderate acne comparing intermittent dosing (0.5-0.7 mg/kg per day for 1 week per month), continuous conventional dosing (0.5-0.7 mg/kg per day), and continuous low dosing (0.25-0.4 mg/kg per day) of oral isotretinoin found greater differences in mean decreased numbers of inflammatory lesions among participants in the continuous low dose (a decrease of 3.72 lesions; 95% CI, 2.13-5.31) and continuous conventional dose (a decrease of 3.87 lesions; 95% CI, 2.31-5.43) groups. The authors noted they were unable to perform a meta-analysis because of study heterogeneity in the three studies examining the primary outcome.
In 14 studies with a total of 906 participants who had moderate and severe acne, the authors noted there were no severe adverse events with different doses and regimens of isotretinoin treatment from 12 weeks to 32 weeks or at follow-up at the end of treatment at up to 48 weeks. There were some adverse events, such as skin dryness, hair loss, and itching in 13 studies with a total of 858 participants.
No birth defects were reported in the studies.
The authors took special note of the low-quality evidence in the review, and said that future studies should include larger sample sizes to observe more rare adverse events, as well as create subgroups with results based on acne severity, longer duration and follow-up, standardization of primary outcomes, and adherence to the 2010 CONSORT statement for reporting parallel-group randomized trials.
“With the aim of providing reliable physician guidelines and a robust evidence-based support for daily clinical practice in acne therapy, future randomized clinical trials on oral isotretinoin for acne should focus on treatment of acne when there is insufficient response to therapy with oral antibiotics plus topical agents,” Dr. Costa and her colleagues wrote.
Dr. Costa reports receiving a grant from the Brazilian government granting agency Coordenação de Aperfeicoamento de Pessoal de Nivel Superior. Another author reported a board membership with Bayer for studies and research and is a paid lecturer for a continuing medical education program on adult female acne. The remaining five authors reported no relevant conflicts of interest.
SOURCE: Costa CS et al. Cochrane Database Syst Rev. 2018. doi: 10.1002/14651858.CD009435.pub2.
I think dermatologists would agree with the assertions of the Cochrane Review that there is limited evidence according to today’s standards of quality evidence. The Cochrane Review process examines available data, ranking it by the quality of the data. The paper by Costa et al. shows where the Cochrane Review process is fatally flawed. It assumes that, where the highest quality data is lacking, the medication in question must be ineffective or that this at least casts doubt on its efficacy.
Isotretinoin was approved for use in acne in the 1980s. If you look at one initial report by Peck et al. examining the efficacy of isotretinoin versus placebo in patients with very severe nodulocystic acne, the isotretinoin group was so effective that half of the patients in the placebo arm broke code because of a 57% worsening of their acne and went to the treatment arm. Overall, there was a 95% improvement in the isotretinoin-treated group at the end of treatment (J Am Acad Dermatol. 1982 Apr;6[4 Pt 2 Suppl]:735-45). This study truly reflects how effective isotretinoin is in the treatment of severe acne, and any dermatologist who uses isotretinoin knows that for a fact. I suspect that, if someone applied the Cochrane Review process to insulin, they also would question its efficacy.
I agree there are questionable data on high versus standard versus low dosing. For most patients, standard dosing of 1.0 mg/kg per day over 20-24 weeks will result in complete and sustained clearance. There are always outliers, however, and alternative dosing may be needed – either higher cumulative dosing to achieve clearance or longer lower dosing to manage side effects.
The authors clearly have limited experience in treating acne, or the aim of the article was simply a review of available data with no consideration of actual clinical usage. However, if patients see this report, it could undermine dermatologists’ efforts to care for their patients with acne. It is rather irresponsible to publish these types of reviews, in which the efficacy of the medication in question was established long ago and is clearly without question, and it really discredits the integrity of the Cochrane Review.
Andrea L. Zaenglein, MD , is professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey, Penn., and is a cochair of the American Academy of Dermatology’s most recent acne management guidelines ( J Am Acad Dermatol. 2016 May;74[5]:945-73.e33 ). She reports being a consultant for Sun Pharmaceutical Industries.
I think dermatologists would agree with the assertions of the Cochrane Review that there is limited evidence according to today’s standards of quality evidence. The Cochrane Review process examines available data, ranking it by the quality of the data. The paper by Costa et al. shows where the Cochrane Review process is fatally flawed. It assumes that, where the highest quality data is lacking, the medication in question must be ineffective or that this at least casts doubt on its efficacy.
Isotretinoin was approved for use in acne in the 1980s. If you look at one initial report by Peck et al. examining the efficacy of isotretinoin versus placebo in patients with very severe nodulocystic acne, the isotretinoin group was so effective that half of the patients in the placebo arm broke code because of a 57% worsening of their acne and went to the treatment arm. Overall, there was a 95% improvement in the isotretinoin-treated group at the end of treatment (J Am Acad Dermatol. 1982 Apr;6[4 Pt 2 Suppl]:735-45). This study truly reflects how effective isotretinoin is in the treatment of severe acne, and any dermatologist who uses isotretinoin knows that for a fact. I suspect that, if someone applied the Cochrane Review process to insulin, they also would question its efficacy.
I agree there are questionable data on high versus standard versus low dosing. For most patients, standard dosing of 1.0 mg/kg per day over 20-24 weeks will result in complete and sustained clearance. There are always outliers, however, and alternative dosing may be needed – either higher cumulative dosing to achieve clearance or longer lower dosing to manage side effects.
The authors clearly have limited experience in treating acne, or the aim of the article was simply a review of available data with no consideration of actual clinical usage. However, if patients see this report, it could undermine dermatologists’ efforts to care for their patients with acne. It is rather irresponsible to publish these types of reviews, in which the efficacy of the medication in question was established long ago and is clearly without question, and it really discredits the integrity of the Cochrane Review.
Andrea L. Zaenglein, MD , is professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey, Penn., and is a cochair of the American Academy of Dermatology’s most recent acne management guidelines ( J Am Acad Dermatol. 2016 May;74[5]:945-73.e33 ). She reports being a consultant for Sun Pharmaceutical Industries.
I think dermatologists would agree with the assertions of the Cochrane Review that there is limited evidence according to today’s standards of quality evidence. The Cochrane Review process examines available data, ranking it by the quality of the data. The paper by Costa et al. shows where the Cochrane Review process is fatally flawed. It assumes that, where the highest quality data is lacking, the medication in question must be ineffective or that this at least casts doubt on its efficacy.
Isotretinoin was approved for use in acne in the 1980s. If you look at one initial report by Peck et al. examining the efficacy of isotretinoin versus placebo in patients with very severe nodulocystic acne, the isotretinoin group was so effective that half of the patients in the placebo arm broke code because of a 57% worsening of their acne and went to the treatment arm. Overall, there was a 95% improvement in the isotretinoin-treated group at the end of treatment (J Am Acad Dermatol. 1982 Apr;6[4 Pt 2 Suppl]:735-45). This study truly reflects how effective isotretinoin is in the treatment of severe acne, and any dermatologist who uses isotretinoin knows that for a fact. I suspect that, if someone applied the Cochrane Review process to insulin, they also would question its efficacy.
I agree there are questionable data on high versus standard versus low dosing. For most patients, standard dosing of 1.0 mg/kg per day over 20-24 weeks will result in complete and sustained clearance. There are always outliers, however, and alternative dosing may be needed – either higher cumulative dosing to achieve clearance or longer lower dosing to manage side effects.
The authors clearly have limited experience in treating acne, or the aim of the article was simply a review of available data with no consideration of actual clinical usage. However, if patients see this report, it could undermine dermatologists’ efforts to care for their patients with acne. It is rather irresponsible to publish these types of reviews, in which the efficacy of the medication in question was established long ago and is clearly without question, and it really discredits the integrity of the Cochrane Review.
Andrea L. Zaenglein, MD , is professor of dermatology and pediatric dermatology at Pennsylvania State University, Hershey, Penn., and is a cochair of the American Academy of Dermatology’s most recent acne management guidelines ( J Am Acad Dermatol. 2016 May;74[5]:945-73.e33 ). She reports being a consultant for Sun Pharmaceutical Industries.
There is when based on reductions in inflammatory lesion counts, according to a recent Cochrane Review.
“The current recommendation of clinical guidelines that oral isotretinoin should be the first-line treatment for moderate to severe acne unresponsive to previous therapies, being more effective than the use of oral antibiotics plus topical agents, underpins current dermatological practice,” Caroline S. Costa, MD, from the Emergency Medicine and Evidence-Based Medicine department at Universidade Federal de São Paulo and her colleagues wrote in their review. “The recommendation cannot be fully supported with certainty by the finding of this review; however, neither does this review challenge it.”
Dr. Costa and her colleagues identified 31 randomized, controlled trials in the Cochrane Skin Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, and LILACS databases up to July 2017, which altogether included 3,836 participants with mild to severe acne who were aged 12-55 years. The patients received treatment with oral isotretinoin versus placebo or other treatments, such as antibiotics.
In 3 studies that altogether included 400 participants and compared isotretinoin with oral antibiotics plus topical treatments, there was no significant difference with isotretinoin in decreases in the investigator-assessed inflammatory lesion count in participants with moderate to severe acne after 20-24 weeks (risk ratio, 1.01; 95% confidence interval, 0.96-1.06). One serious side effect – Stevens-Johnson syndrome – was noted in the isotretinoin-treated group (RR, 3.00; 95% CI, 0.12-72.98). These results were based on “very-low-quality evidence,” the authors noted.
Two studies also comparing isotretinoin with oral antibiotics and topical treatments in a total of 351 participants showed a 15% improvement in acne severity (RR, 1.15; 95% CI, 1.00-1.32) as assessed by physician’s global evaluation but with a greater number of adverse events considered less severe (RR, 1.67; 95% CI, 1.42-1.98), such as vomiting, nausea, dry lips and skin, and cheilitis.
With regard to dosing, one study with 154 participants with severe acne showed 0.05 mg/kg per day of isotretinoin reduced inflammatory lesion count by 79% after 20 weeks, while 0.1 mg/kg per day and 0.2 mg/kg per day reduced inflammatory lesion counts by 80% and 84%, respectively, after 20 weeks. A different study of 150 participants with severe acne found a 95% decrease in inflammatory lesion counts for 58% of participants receiving 0.1 mg/kg per day, 80% of participants receiving 0.5 mg/kg per day, and 90% of participants receiving 1 mg/kg per day of oral isotretinoin after 20 weeks.
In a randomized, controlled trial with 40 participants with moderate acne comparing intermittent dosing (0.5-0.7 mg/kg per day for 1 week per month), continuous conventional dosing (0.5-0.7 mg/kg per day), and continuous low dosing (0.25-0.4 mg/kg per day) of oral isotretinoin found greater differences in mean decreased numbers of inflammatory lesions among participants in the continuous low dose (a decrease of 3.72 lesions; 95% CI, 2.13-5.31) and continuous conventional dose (a decrease of 3.87 lesions; 95% CI, 2.31-5.43) groups. The authors noted they were unable to perform a meta-analysis because of study heterogeneity in the three studies examining the primary outcome.
In 14 studies with a total of 906 participants who had moderate and severe acne, the authors noted there were no severe adverse events with different doses and regimens of isotretinoin treatment from 12 weeks to 32 weeks or at follow-up at the end of treatment at up to 48 weeks. There were some adverse events, such as skin dryness, hair loss, and itching in 13 studies with a total of 858 participants.
No birth defects were reported in the studies.
The authors took special note of the low-quality evidence in the review, and said that future studies should include larger sample sizes to observe more rare adverse events, as well as create subgroups with results based on acne severity, longer duration and follow-up, standardization of primary outcomes, and adherence to the 2010 CONSORT statement for reporting parallel-group randomized trials.
“With the aim of providing reliable physician guidelines and a robust evidence-based support for daily clinical practice in acne therapy, future randomized clinical trials on oral isotretinoin for acne should focus on treatment of acne when there is insufficient response to therapy with oral antibiotics plus topical agents,” Dr. Costa and her colleagues wrote.
Dr. Costa reports receiving a grant from the Brazilian government granting agency Coordenação de Aperfeicoamento de Pessoal de Nivel Superior. Another author reported a board membership with Bayer for studies and research and is a paid lecturer for a continuing medical education program on adult female acne. The remaining five authors reported no relevant conflicts of interest.
SOURCE: Costa CS et al. Cochrane Database Syst Rev. 2018. doi: 10.1002/14651858.CD009435.pub2.
There is when based on reductions in inflammatory lesion counts, according to a recent Cochrane Review.
“The current recommendation of clinical guidelines that oral isotretinoin should be the first-line treatment for moderate to severe acne unresponsive to previous therapies, being more effective than the use of oral antibiotics plus topical agents, underpins current dermatological practice,” Caroline S. Costa, MD, from the Emergency Medicine and Evidence-Based Medicine department at Universidade Federal de São Paulo and her colleagues wrote in their review. “The recommendation cannot be fully supported with certainty by the finding of this review; however, neither does this review challenge it.”
Dr. Costa and her colleagues identified 31 randomized, controlled trials in the Cochrane Skin Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, and LILACS databases up to July 2017, which altogether included 3,836 participants with mild to severe acne who were aged 12-55 years. The patients received treatment with oral isotretinoin versus placebo or other treatments, such as antibiotics.
In 3 studies that altogether included 400 participants and compared isotretinoin with oral antibiotics plus topical treatments, there was no significant difference with isotretinoin in decreases in the investigator-assessed inflammatory lesion count in participants with moderate to severe acne after 20-24 weeks (risk ratio, 1.01; 95% confidence interval, 0.96-1.06). One serious side effect – Stevens-Johnson syndrome – was noted in the isotretinoin-treated group (RR, 3.00; 95% CI, 0.12-72.98). These results were based on “very-low-quality evidence,” the authors noted.
Two studies also comparing isotretinoin with oral antibiotics and topical treatments in a total of 351 participants showed a 15% improvement in acne severity (RR, 1.15; 95% CI, 1.00-1.32) as assessed by physician’s global evaluation but with a greater number of adverse events considered less severe (RR, 1.67; 95% CI, 1.42-1.98), such as vomiting, nausea, dry lips and skin, and cheilitis.
With regard to dosing, one study with 154 participants with severe acne showed 0.05 mg/kg per day of isotretinoin reduced inflammatory lesion count by 79% after 20 weeks, while 0.1 mg/kg per day and 0.2 mg/kg per day reduced inflammatory lesion counts by 80% and 84%, respectively, after 20 weeks. A different study of 150 participants with severe acne found a 95% decrease in inflammatory lesion counts for 58% of participants receiving 0.1 mg/kg per day, 80% of participants receiving 0.5 mg/kg per day, and 90% of participants receiving 1 mg/kg per day of oral isotretinoin after 20 weeks.
In a randomized, controlled trial with 40 participants with moderate acne comparing intermittent dosing (0.5-0.7 mg/kg per day for 1 week per month), continuous conventional dosing (0.5-0.7 mg/kg per day), and continuous low dosing (0.25-0.4 mg/kg per day) of oral isotretinoin found greater differences in mean decreased numbers of inflammatory lesions among participants in the continuous low dose (a decrease of 3.72 lesions; 95% CI, 2.13-5.31) and continuous conventional dose (a decrease of 3.87 lesions; 95% CI, 2.31-5.43) groups. The authors noted they were unable to perform a meta-analysis because of study heterogeneity in the three studies examining the primary outcome.
In 14 studies with a total of 906 participants who had moderate and severe acne, the authors noted there were no severe adverse events with different doses and regimens of isotretinoin treatment from 12 weeks to 32 weeks or at follow-up at the end of treatment at up to 48 weeks. There were some adverse events, such as skin dryness, hair loss, and itching in 13 studies with a total of 858 participants.
No birth defects were reported in the studies.
The authors took special note of the low-quality evidence in the review, and said that future studies should include larger sample sizes to observe more rare adverse events, as well as create subgroups with results based on acne severity, longer duration and follow-up, standardization of primary outcomes, and adherence to the 2010 CONSORT statement for reporting parallel-group randomized trials.
“With the aim of providing reliable physician guidelines and a robust evidence-based support for daily clinical practice in acne therapy, future randomized clinical trials on oral isotretinoin for acne should focus on treatment of acne when there is insufficient response to therapy with oral antibiotics plus topical agents,” Dr. Costa and her colleagues wrote.
Dr. Costa reports receiving a grant from the Brazilian government granting agency Coordenação de Aperfeicoamento de Pessoal de Nivel Superior. Another author reported a board membership with Bayer for studies and research and is a paid lecturer for a continuing medical education program on adult female acne. The remaining five authors reported no relevant conflicts of interest.
SOURCE: Costa CS et al. Cochrane Database Syst Rev. 2018. doi: 10.1002/14651858.CD009435.pub2.
FROM COCHRANE DATABASE OF SYSTEMATIC REVIEWS
Key clinical point: A Cochrane Review found low quality of evidence surrounding oral isotretinoin’s effectiveness for acne.
Major finding: Isotretinoin did not decrease inflammatory lesion count, compared with (risk ratio, 1.01; 95% confidence interval, 0.96-1.06), in 3 studies, and there was low evidence to suggest daily treatment was more effective than treatment for 1 week per month.
Study details: A Cochrane Review of 31 studies that altogether included 3,836 patients with mild to severe acne who received oral isotretinoin, placebo, or other treatments such as antibiotics.
Disclosures: Dr. Costa reported receiving a grant from the Brazilian government granting agency Coordenação de Aperfeicoamento de Pessoal de Nivel Superior. Dr. Bagatin reported a board membership with Bayer for studies and research and is a paid lecturer for a continuing medical education program on adult female acne. The other authors report no relevant conflicts of interest.
Source: Costa CS et al. Cochrane Database Syst Rev. 2018. doi: 10.1002/14651858.CD009435.pub2.