User login
Extended-release naltrexone competes with buprenorphine-naloxone combo
Improvements in comorbid symptoms result in both treatments
Patients with opioid dependence and anxiety, depression, and insomnia symptoms who receive extended-release naltrexone injections experience similar results to those treated with daily oral buprenorphine-naloxone, research shows. The results suggest that those comorbid symptoms should not prevent a switch from treating patients with an opioid agonist to treating them with extended-release naltrexone, reported Zill-e-Huma Latif, MD, and colleagues.
“Our results showed improvements in anxiety, depression, and insomnia within only a few weeks of beginning either study treatment,” Dr. Latif and colleagues wrote in JAMA Psychiatry. “Our study also showed reductions in the use of opioids and other illegal substances in both treatment groups.”
Dr. Latif and colleagues conducted a prospective, randomized trial of 159 men and women with opioid dependence to receive a 380-mg injectable dose of extended-release naltrexone every 4 weeks or flexible doses (4-24 mg) of daily combined buprenorphine-naloxone for 12 weeks and then a 9-month, open-label period with one of the treatments as chosen by the participant. Of the participants, 105 reached the end of the trial (66%).
The participants were aged 18-60 years and had similar ages, gender distributions, and heroin use duration between treatment groups. The researchers used the 25-item Hopkins Symptom Checklist (HSCL-25) and the Insomnia Severity Index to assess anxiety, depression, and insomnia symptoms every 4 weeks until 48 weeks, reported Dr. Latif, of the department of research and development in mental health at Akershus University Hospital in Norway, and colleagues.
Over 12 weeks of the trial, However, the Insomnia Severity Index score was significantly lower among participants taking extended-release naltrexone (ES, −0.32; 95% CI, −0.65 to 0.02; P = .008). In the 9-month, open-label follow-up period, no significant differences were found in anxiety (ES, 0.04; 95% CI, −0.34 to 0.42), depression (ES, −0.04; 95% CI, −0.42 to 0.33), or insomnia (ES, 0.04; 95% CI, −0.33 to 0.42) among participants who switched to extended-release naltrexone or continued using extended-release naltrexone.
“Because participants receiving treatment with [extended-release naltrexone] or [buprenorphine-naloxone] showed equal improvements in anxiety, depression, and insomnia as assessed by the HSCL-25 and the Insomnia Severity Index, such symptoms should not preclude the choice to leave opioid agonist treatment and to start treatment with [extended-release naltrexone],” Dr. Latif and colleagues wrote.
With regard to study limitations, the researchers noted that they used self-reported questionnaires for anxiety, depression, and insomnia symptoms, did not confirm reported drug use through urine samples, and used the HSCL-25 when it is not a diagnostic tool.
The study was funded by grants from the Research Council of Norway and the Western Norway Regional Health Authority; financial support was provided by the Norwegian Center for Addiction Research, University of Oslo, and Akershus University Hospital. The authors report no relevant conflicts of interest.
SOURCE: Latif Z-H et al. JAMA Psychiatry. 2018 Dec 19. doi: 10.1001/jamapsychiatry.2018.3537.
Improvements in comorbid symptoms result in both treatments
Improvements in comorbid symptoms result in both treatments
Patients with opioid dependence and anxiety, depression, and insomnia symptoms who receive extended-release naltrexone injections experience similar results to those treated with daily oral buprenorphine-naloxone, research shows. The results suggest that those comorbid symptoms should not prevent a switch from treating patients with an opioid agonist to treating them with extended-release naltrexone, reported Zill-e-Huma Latif, MD, and colleagues.
“Our results showed improvements in anxiety, depression, and insomnia within only a few weeks of beginning either study treatment,” Dr. Latif and colleagues wrote in JAMA Psychiatry. “Our study also showed reductions in the use of opioids and other illegal substances in both treatment groups.”
Dr. Latif and colleagues conducted a prospective, randomized trial of 159 men and women with opioid dependence to receive a 380-mg injectable dose of extended-release naltrexone every 4 weeks or flexible doses (4-24 mg) of daily combined buprenorphine-naloxone for 12 weeks and then a 9-month, open-label period with one of the treatments as chosen by the participant. Of the participants, 105 reached the end of the trial (66%).
The participants were aged 18-60 years and had similar ages, gender distributions, and heroin use duration between treatment groups. The researchers used the 25-item Hopkins Symptom Checklist (HSCL-25) and the Insomnia Severity Index to assess anxiety, depression, and insomnia symptoms every 4 weeks until 48 weeks, reported Dr. Latif, of the department of research and development in mental health at Akershus University Hospital in Norway, and colleagues.
Over 12 weeks of the trial, However, the Insomnia Severity Index score was significantly lower among participants taking extended-release naltrexone (ES, −0.32; 95% CI, −0.65 to 0.02; P = .008). In the 9-month, open-label follow-up period, no significant differences were found in anxiety (ES, 0.04; 95% CI, −0.34 to 0.42), depression (ES, −0.04; 95% CI, −0.42 to 0.33), or insomnia (ES, 0.04; 95% CI, −0.33 to 0.42) among participants who switched to extended-release naltrexone or continued using extended-release naltrexone.
“Because participants receiving treatment with [extended-release naltrexone] or [buprenorphine-naloxone] showed equal improvements in anxiety, depression, and insomnia as assessed by the HSCL-25 and the Insomnia Severity Index, such symptoms should not preclude the choice to leave opioid agonist treatment and to start treatment with [extended-release naltrexone],” Dr. Latif and colleagues wrote.
With regard to study limitations, the researchers noted that they used self-reported questionnaires for anxiety, depression, and insomnia symptoms, did not confirm reported drug use through urine samples, and used the HSCL-25 when it is not a diagnostic tool.
The study was funded by grants from the Research Council of Norway and the Western Norway Regional Health Authority; financial support was provided by the Norwegian Center for Addiction Research, University of Oslo, and Akershus University Hospital. The authors report no relevant conflicts of interest.
SOURCE: Latif Z-H et al. JAMA Psychiatry. 2018 Dec 19. doi: 10.1001/jamapsychiatry.2018.3537.
Patients with opioid dependence and anxiety, depression, and insomnia symptoms who receive extended-release naltrexone injections experience similar results to those treated with daily oral buprenorphine-naloxone, research shows. The results suggest that those comorbid symptoms should not prevent a switch from treating patients with an opioid agonist to treating them with extended-release naltrexone, reported Zill-e-Huma Latif, MD, and colleagues.
“Our results showed improvements in anxiety, depression, and insomnia within only a few weeks of beginning either study treatment,” Dr. Latif and colleagues wrote in JAMA Psychiatry. “Our study also showed reductions in the use of opioids and other illegal substances in both treatment groups.”
Dr. Latif and colleagues conducted a prospective, randomized trial of 159 men and women with opioid dependence to receive a 380-mg injectable dose of extended-release naltrexone every 4 weeks or flexible doses (4-24 mg) of daily combined buprenorphine-naloxone for 12 weeks and then a 9-month, open-label period with one of the treatments as chosen by the participant. Of the participants, 105 reached the end of the trial (66%).
The participants were aged 18-60 years and had similar ages, gender distributions, and heroin use duration between treatment groups. The researchers used the 25-item Hopkins Symptom Checklist (HSCL-25) and the Insomnia Severity Index to assess anxiety, depression, and insomnia symptoms every 4 weeks until 48 weeks, reported Dr. Latif, of the department of research and development in mental health at Akershus University Hospital in Norway, and colleagues.
Over 12 weeks of the trial, However, the Insomnia Severity Index score was significantly lower among participants taking extended-release naltrexone (ES, −0.32; 95% CI, −0.65 to 0.02; P = .008). In the 9-month, open-label follow-up period, no significant differences were found in anxiety (ES, 0.04; 95% CI, −0.34 to 0.42), depression (ES, −0.04; 95% CI, −0.42 to 0.33), or insomnia (ES, 0.04; 95% CI, −0.33 to 0.42) among participants who switched to extended-release naltrexone or continued using extended-release naltrexone.
“Because participants receiving treatment with [extended-release naltrexone] or [buprenorphine-naloxone] showed equal improvements in anxiety, depression, and insomnia as assessed by the HSCL-25 and the Insomnia Severity Index, such symptoms should not preclude the choice to leave opioid agonist treatment and to start treatment with [extended-release naltrexone],” Dr. Latif and colleagues wrote.
With regard to study limitations, the researchers noted that they used self-reported questionnaires for anxiety, depression, and insomnia symptoms, did not confirm reported drug use through urine samples, and used the HSCL-25 when it is not a diagnostic tool.
The study was funded by grants from the Research Council of Norway and the Western Norway Regional Health Authority; financial support was provided by the Norwegian Center for Addiction Research, University of Oslo, and Akershus University Hospital. The authors report no relevant conflicts of interest.
SOURCE: Latif Z-H et al. JAMA Psychiatry. 2018 Dec 19. doi: 10.1001/jamapsychiatry.2018.3537.
FROM JAMA PSYCHIATRY
Key clinical point: No significant differences were found in the improvement of anxiety, depression, and insomnia symptoms among individuals with opioid dependence when receiving extended-release naltrexone, compared with combined buprenorphine-naloxone.
Major finding: In the 9-month, open-label follow-up period, there were no significant differences in anxiety (effect size, 0.04; 95% confidence interval, −0.34 to 0.42), depression (ES, −0.04; 95% CI, −0.42 to 0.33), or insomnia (ES, 0.04; 95% CI, −0.33 to 0.42) among participants who switched to extended-release naltrexone or continued using buprenorphine-naloxone.
Study details: A prospective, randomized trial of 159 men and women with opioid dependence who received extended-release naltrexone or combined buprenorphine-naloxone between November 2012 and October 2015.
Disclosures: This study was funded by grants from the Research Council of Norway and the Western Norway Regional Health Authority, and financial support was provided by the Norwegian Center for Addiction Research, University of Oslo, and Akershus University Hospital. The authors reported no relevant conflicts of interest.
Source: Latif Z-H et al. JAMA Psychiatry. 2018 Dec 19. doi: 10.1001/jamapsychiatry.2018.3537.
Active migraine in women linked to lower risk of developing T2DM
Women with active migraines are less likely to have type 2 diabetes mellitus (T2DM) and show a decrease in migraine symptoms prior to diagnosis of T2DM, indicating an inverse relationship between hyperglycemia, hyperinsulinism, and migraines, according to recent research published in JAMA Neurology.
“Because plasma glucose concentration rises with time up to the point of type 2 diabetes occurrence, the prevalence of migraine symptoms may decrease,” Guy Fagherazzi, PhD, at the Center for Research in Epidemiology and Population Health at the Gustave Roussy Institute in Villejuif, France, and his colleagues wrote in their study. “Consequently, tracking the evolution and especially the decrease of migraine frequency in individuals with migraine at high risk of diabetes, such as individuals with obesity, irrespective of age could be the sign of an emerging increased blood glucose levels, prediabetes, or type 2 diabetes.”
The researchers used data from the prospective Etude Epidémiologique Auprès des Femmes de la Mutuelle Générale de l’Education Nationale (E3N) study, initiated in 1990 and identified 74,247 women (mean age, 61 years old) with self-reported migraine in a 2002 follow-up questionnaire who had 10-year follow-up data during 2004-2014. The women in the cohort were born during 1925-1950 and completed biennial questionnaires about their health, including migraine status and medications, since 1992. The participants were divided into groups based on no migraine (49,199 participants), active migraine (7,839 participants), or prior migraine history (17,209 participants), and patients with T2DM at baseline were excluded.
Dr. Fagherazzi and his colleagues found 2,372 cases of type 2 diabetes over the follow-up period. Women who had active migraine status were less likely to have T2DM (hazard ratio, 0.80; 95% confidence interval, 0.67-0.96) than were the participants who did not have migraines, and this inverse association persisted after the researchers adjusted for factors such as myocardial infarction, education level, family history of diabetes, body mass index, smoking status, hypertension, physical activity, oral contraceptive use, menopausal status, menopausal hormone therapy, handedness, antimigraine preparations, and other prescribed migraine drugs (HR, 0.70; 95% CI, 0.58-0.85).
In the participants who developed T2DM, the researchers also found that there was a decrease in the prevalence of active migraine in the 24 years prior to T2DM diagnosis from 22% (95% CI, 16%-27%) to 11% (95% CI, 10%-12%) after adjusting for T2DM risk factors, which was then followed by an up to 22-year plateau in migraine prevalence of 11% for these participants.
“The linear decrease of migraine prevalence long before and the plateau long after type 2 diabetes diagnosis is novel and the association deserves to be studied in other populations,” Dr. Fagherazzi and his colleagues wrote. “The potential beneficial role of both hyperglycemia and hyperinsulinism on migraine occurrence needs to be further explored.”
The researchers noted limitations in the study, such as self-reported migraine by participants in the cohort, exclusion of non–pharmacologically treated T2DM cases, observational nature of the study, and homogenized population in the E3N cohort consisting of mainly women in menopause who were teachers and belonged to the same health insurance plan.
This study was funded by a grant from the French Research agency. The E3N cohort study was funded by the “Mutuelle Générale de l’Education Nationale,” European Community, French League against Cancer, Gustave Roussy, and French Institute of Health and Medical Research. Dr. Kurth is an advisory board member for CoLucid and has received funding for a research project from Amgen, honoraria from Lilly, lecture support from Novartis and Daiichi Sankyo, and travel support from the International Headache Society, as well as provided BMJ with editorial services.
SOURCE: Fagherazzi G et al. JAMA Neurol. 2018. doi: 10.1001/jamaneurol.2018.3960.
Although it has been noted for some time in the clinical setting, researchers are still unsure why there is an inverse association between active migraine and type 2 diabetes mellitus, as noted by Fagherazzi et al. in a recent study.
One explanation is the presence of calcitonin gene–related peptide in both animal models of energy metabolism and the pathophysiology of migraine. It is possible that insulin resistance and hyperglycemia damage the sensory neurons that produce the peptide. If these damaged nerves are soothed, migraine may resolve.
Other silver linings associated with active migraine include an increased likelihood of having a healthy cardiovascular system and decreased alcohol consumption.
The epidemiology of migraine and findings like those in this study prompt the question: What is migraine good for?
Amy A. Gelfand, MD , of the University of California, San Francisco, and Elizabeth Loder, MD , MPH, of Harvard Medical School in Boston made these comments in an editorial accompanying Dr. Fagherazzi’s study. They disclosed a number of financial relationships with companies marketing treatments for migraine.
Although it has been noted for some time in the clinical setting, researchers are still unsure why there is an inverse association between active migraine and type 2 diabetes mellitus, as noted by Fagherazzi et al. in a recent study.
One explanation is the presence of calcitonin gene–related peptide in both animal models of energy metabolism and the pathophysiology of migraine. It is possible that insulin resistance and hyperglycemia damage the sensory neurons that produce the peptide. If these damaged nerves are soothed, migraine may resolve.
Other silver linings associated with active migraine include an increased likelihood of having a healthy cardiovascular system and decreased alcohol consumption.
The epidemiology of migraine and findings like those in this study prompt the question: What is migraine good for?
Amy A. Gelfand, MD , of the University of California, San Francisco, and Elizabeth Loder, MD , MPH, of Harvard Medical School in Boston made these comments in an editorial accompanying Dr. Fagherazzi’s study. They disclosed a number of financial relationships with companies marketing treatments for migraine.
Although it has been noted for some time in the clinical setting, researchers are still unsure why there is an inverse association between active migraine and type 2 diabetes mellitus, as noted by Fagherazzi et al. in a recent study.
One explanation is the presence of calcitonin gene–related peptide in both animal models of energy metabolism and the pathophysiology of migraine. It is possible that insulin resistance and hyperglycemia damage the sensory neurons that produce the peptide. If these damaged nerves are soothed, migraine may resolve.
Other silver linings associated with active migraine include an increased likelihood of having a healthy cardiovascular system and decreased alcohol consumption.
The epidemiology of migraine and findings like those in this study prompt the question: What is migraine good for?
Amy A. Gelfand, MD , of the University of California, San Francisco, and Elizabeth Loder, MD , MPH, of Harvard Medical School in Boston made these comments in an editorial accompanying Dr. Fagherazzi’s study. They disclosed a number of financial relationships with companies marketing treatments for migraine.
Women with active migraines are less likely to have type 2 diabetes mellitus (T2DM) and show a decrease in migraine symptoms prior to diagnosis of T2DM, indicating an inverse relationship between hyperglycemia, hyperinsulinism, and migraines, according to recent research published in JAMA Neurology.
“Because plasma glucose concentration rises with time up to the point of type 2 diabetes occurrence, the prevalence of migraine symptoms may decrease,” Guy Fagherazzi, PhD, at the Center for Research in Epidemiology and Population Health at the Gustave Roussy Institute in Villejuif, France, and his colleagues wrote in their study. “Consequently, tracking the evolution and especially the decrease of migraine frequency in individuals with migraine at high risk of diabetes, such as individuals with obesity, irrespective of age could be the sign of an emerging increased blood glucose levels, prediabetes, or type 2 diabetes.”
The researchers used data from the prospective Etude Epidémiologique Auprès des Femmes de la Mutuelle Générale de l’Education Nationale (E3N) study, initiated in 1990 and identified 74,247 women (mean age, 61 years old) with self-reported migraine in a 2002 follow-up questionnaire who had 10-year follow-up data during 2004-2014. The women in the cohort were born during 1925-1950 and completed biennial questionnaires about their health, including migraine status and medications, since 1992. The participants were divided into groups based on no migraine (49,199 participants), active migraine (7,839 participants), or prior migraine history (17,209 participants), and patients with T2DM at baseline were excluded.
Dr. Fagherazzi and his colleagues found 2,372 cases of type 2 diabetes over the follow-up period. Women who had active migraine status were less likely to have T2DM (hazard ratio, 0.80; 95% confidence interval, 0.67-0.96) than were the participants who did not have migraines, and this inverse association persisted after the researchers adjusted for factors such as myocardial infarction, education level, family history of diabetes, body mass index, smoking status, hypertension, physical activity, oral contraceptive use, menopausal status, menopausal hormone therapy, handedness, antimigraine preparations, and other prescribed migraine drugs (HR, 0.70; 95% CI, 0.58-0.85).
In the participants who developed T2DM, the researchers also found that there was a decrease in the prevalence of active migraine in the 24 years prior to T2DM diagnosis from 22% (95% CI, 16%-27%) to 11% (95% CI, 10%-12%) after adjusting for T2DM risk factors, which was then followed by an up to 22-year plateau in migraine prevalence of 11% for these participants.
“The linear decrease of migraine prevalence long before and the plateau long after type 2 diabetes diagnosis is novel and the association deserves to be studied in other populations,” Dr. Fagherazzi and his colleagues wrote. “The potential beneficial role of both hyperglycemia and hyperinsulinism on migraine occurrence needs to be further explored.”
The researchers noted limitations in the study, such as self-reported migraine by participants in the cohort, exclusion of non–pharmacologically treated T2DM cases, observational nature of the study, and homogenized population in the E3N cohort consisting of mainly women in menopause who were teachers and belonged to the same health insurance plan.
This study was funded by a grant from the French Research agency. The E3N cohort study was funded by the “Mutuelle Générale de l’Education Nationale,” European Community, French League against Cancer, Gustave Roussy, and French Institute of Health and Medical Research. Dr. Kurth is an advisory board member for CoLucid and has received funding for a research project from Amgen, honoraria from Lilly, lecture support from Novartis and Daiichi Sankyo, and travel support from the International Headache Society, as well as provided BMJ with editorial services.
SOURCE: Fagherazzi G et al. JAMA Neurol. 2018. doi: 10.1001/jamaneurol.2018.3960.
Women with active migraines are less likely to have type 2 diabetes mellitus (T2DM) and show a decrease in migraine symptoms prior to diagnosis of T2DM, indicating an inverse relationship between hyperglycemia, hyperinsulinism, and migraines, according to recent research published in JAMA Neurology.
“Because plasma glucose concentration rises with time up to the point of type 2 diabetes occurrence, the prevalence of migraine symptoms may decrease,” Guy Fagherazzi, PhD, at the Center for Research in Epidemiology and Population Health at the Gustave Roussy Institute in Villejuif, France, and his colleagues wrote in their study. “Consequently, tracking the evolution and especially the decrease of migraine frequency in individuals with migraine at high risk of diabetes, such as individuals with obesity, irrespective of age could be the sign of an emerging increased blood glucose levels, prediabetes, or type 2 diabetes.”
The researchers used data from the prospective Etude Epidémiologique Auprès des Femmes de la Mutuelle Générale de l’Education Nationale (E3N) study, initiated in 1990 and identified 74,247 women (mean age, 61 years old) with self-reported migraine in a 2002 follow-up questionnaire who had 10-year follow-up data during 2004-2014. The women in the cohort were born during 1925-1950 and completed biennial questionnaires about their health, including migraine status and medications, since 1992. The participants were divided into groups based on no migraine (49,199 participants), active migraine (7,839 participants), or prior migraine history (17,209 participants), and patients with T2DM at baseline were excluded.
Dr. Fagherazzi and his colleagues found 2,372 cases of type 2 diabetes over the follow-up period. Women who had active migraine status were less likely to have T2DM (hazard ratio, 0.80; 95% confidence interval, 0.67-0.96) than were the participants who did not have migraines, and this inverse association persisted after the researchers adjusted for factors such as myocardial infarction, education level, family history of diabetes, body mass index, smoking status, hypertension, physical activity, oral contraceptive use, menopausal status, menopausal hormone therapy, handedness, antimigraine preparations, and other prescribed migraine drugs (HR, 0.70; 95% CI, 0.58-0.85).
In the participants who developed T2DM, the researchers also found that there was a decrease in the prevalence of active migraine in the 24 years prior to T2DM diagnosis from 22% (95% CI, 16%-27%) to 11% (95% CI, 10%-12%) after adjusting for T2DM risk factors, which was then followed by an up to 22-year plateau in migraine prevalence of 11% for these participants.
“The linear decrease of migraine prevalence long before and the plateau long after type 2 diabetes diagnosis is novel and the association deserves to be studied in other populations,” Dr. Fagherazzi and his colleagues wrote. “The potential beneficial role of both hyperglycemia and hyperinsulinism on migraine occurrence needs to be further explored.”
The researchers noted limitations in the study, such as self-reported migraine by participants in the cohort, exclusion of non–pharmacologically treated T2DM cases, observational nature of the study, and homogenized population in the E3N cohort consisting of mainly women in menopause who were teachers and belonged to the same health insurance plan.
This study was funded by a grant from the French Research agency. The E3N cohort study was funded by the “Mutuelle Générale de l’Education Nationale,” European Community, French League against Cancer, Gustave Roussy, and French Institute of Health and Medical Research. Dr. Kurth is an advisory board member for CoLucid and has received funding for a research project from Amgen, honoraria from Lilly, lecture support from Novartis and Daiichi Sankyo, and travel support from the International Headache Society, as well as provided BMJ with editorial services.
SOURCE: Fagherazzi G et al. JAMA Neurol. 2018. doi: 10.1001/jamaneurol.2018.3960.
FROM JAMA NEUROLOGY
Key clinical point: There was an inverse association between active migraine and type 2 diabetes mellitus in women over 10 years of follow-up.
Major finding: Compared with women who had no history of active migraine, women with active migraine had a lower risk of developing type 2 diabetes (univariate hazard ratio, 0.80; 95% confidence interval, 0.67-0.96).
Study details: Results from a prospective, population-based study of 74,247 women with active migraines in the E3N cohort study in France.
Disclosures: This study was funded by a grant from the French Research agency. The E3N cohort study was funded by the Mutuelle Générale de l’Education Nationale, European Community, French League against Cancer, Gustave Roussy, and French Institute of Health and Medical Research. Dr. Kurth is an advisory board member for CoLucid and has received funding for a research project from Amgen, honoraria from Lilly, lecture support from Novartis and Daiichi Sankyo, and travel support from the International Headache Society, as well as provided the BMJ with editorial services.
Source: Fagherazzi G et al. JAMA Neurol. 2018. doi: 10.1001/jamaneurol.2018.3960.
Motor neuron disease spasticity improved with cannabis-based oral spray, antispasticity drugs
Nabiximols, a cannabis-based oral spray containing delta-9 tetrahydrocannabinol and cannabidiol, significantly improved spasticity symptoms in combination with antispasticity drugs in patients with motor neuron disease in a randomized, double-blind, placebo-controlled, parallel-group, phase 2 clinical trial.
Nabiximols proved superior to a placebo spray when both were given to patients with either amyotrophic lateral sclerosis or primary lateral sclerosis as part of an antispasticity regimen in the 6-week, CANALS (Cannabis Sativa Extract in Amyotrophic Lateral Sclerosis and other Motor Neuron Disease) study at four Italian centers, Nilo Riva, MD, PhD, of the San Raffaele Scientific Institute in Milan and his colleagues reported in The Lancet Neurology. Nabiximols is approved for the treatment of spasticity due to multiple sclerosis in multiple countries, but not in the United States.
“There is no cure for motor neuron disease, so improved symptom control and quality of life are important for patients,” Dr. Riva stated in a press release. “Our proof-of-concept trial showed a beneficial effect of THC-CBD [delta-9 tetrahydrocannabinol and cannabidiol] spray in people on treatment-resistant spasticity and pain.
“Despite these encouraging findings, we must first confirm that THC-CBD spray is effective and safe in larger, longer-term phase 3 trials,” Dr. Riva added.
The patients enrolled in the phase 2 trial between January 2013 and December 2014 and were between 18 and 80 years old with a probable diagnosis of amyotrophic lateral sclerosis or primary lateral sclerosis, were on an antispasticity regimen for at least 30 days, and had a spasticity score of at least 1 in two muscle groups on the 5-point Modified Ashworth Scale. Participants titrated for the first 2 weeks before maintaining their treatment for 4 weeks.
Of 59 participants at final follow-up, Modified Ashworth Scale scores improved in the nabiximols group (29 participants) by a mean of –0.11 points, compared with worsening by a mean of 0.16 points in the placebo group (30 participants). The researchers noted that there were no participants who withdrew from the study, nabiximols was well-tolerated, and there were no serious adverse events in the nabiximols group; however, there were 22 participants in the nabiximols group and 8 participants in the placebo group who experienced an adverse event from any cause.
“This study is, to our knowledge, the first randomized controlled trial of safety and efficacy of a pharmacological treatment for spasticity and the first trial of nabiximols in motor neuron disease,” Dr. Riva and his colleagues wrote. “Our results suggest that the study drug is well tolerated and provides first evidence of efficacy in terms of controlling spasticity in patients with motor neuron disease.”
The study was funded by the Italian Research Foundation for Amyotrophic Lateral Sclerosis. GW Pharma, which developed nabiximols, provided the study drug and placebo. Many of the authors reported financial disclosures with pharmaceutical companies.
SOURCE: Riva N et al. Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422(18)30406-X.
Although the results of Riva et al. are encouraging, the study had several major limitations and future research in the form of larger, multicenter, randomized controlled trials is needed, Marianne de Visser, MD, PhD, wrote in a related editorial.
Dr. de Visser noted a bias in the study as it randomized 16 patients with predominantly upper motor neuron involvement to the nabiximols group. The treatment could potentially have benefited those patients, for whom spasticity is the prevailing symptom, more than the 13 patients randomized to the nabiximols group who had classic amyotrophic lateral sclerosis involving both upper and lower neurons. In addition, Riva et al. did not differentiate between patients with upper and lower limb spasticity or patients with bulbar spasticity and those without, she said.
The use of the Modified Ashworth Scale was also a potential issue, because while it has been used in previous studies examining antispastic treatment efficacy, “it lacked sensitivity in studies of the efficacy of cannabinoids in patients with multiple sclerosis–related spasticity, and new spasticity numeric rating or visual analogue scales are being adopted,” Dr. de Visser wrote.
The number of adverse effects in the treatment group could have also unblinded researchers, which may have affected the significant findings, she said.
“Before asking for approval of cannabinoids for symptomatic treatment of spasticity in patients with amyotrophic lateral sclerosis, further studies are needed to establish the frequency of spasticity in the various presentations of motor neuron disease, and also whether reductions in spasticity improve quality of life,” Dr. de Visser said in a press release. “Natural history studies including all subtypes of motor neuron disease and better outcome measures aimed at assessment of spasticity are required. Dr. Riva and colleagues’ data are encouraging, and larger multicenter, randomized controlled trials should be done to identify which subgroups of patients derive clinically significant benefits from nabiximols.”
Marianne de Visser, MD, PhD, is with the department of neurology at Amsterdam University Medical Center. She reported no relevant conflicts of interest. Her remarks are taken from an editorial accompanying the study by Dr. Riva and associates (Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422[18]30493-9 ).
Although the results of Riva et al. are encouraging, the study had several major limitations and future research in the form of larger, multicenter, randomized controlled trials is needed, Marianne de Visser, MD, PhD, wrote in a related editorial.
Dr. de Visser noted a bias in the study as it randomized 16 patients with predominantly upper motor neuron involvement to the nabiximols group. The treatment could potentially have benefited those patients, for whom spasticity is the prevailing symptom, more than the 13 patients randomized to the nabiximols group who had classic amyotrophic lateral sclerosis involving both upper and lower neurons. In addition, Riva et al. did not differentiate between patients with upper and lower limb spasticity or patients with bulbar spasticity and those without, she said.
The use of the Modified Ashworth Scale was also a potential issue, because while it has been used in previous studies examining antispastic treatment efficacy, “it lacked sensitivity in studies of the efficacy of cannabinoids in patients with multiple sclerosis–related spasticity, and new spasticity numeric rating or visual analogue scales are being adopted,” Dr. de Visser wrote.
The number of adverse effects in the treatment group could have also unblinded researchers, which may have affected the significant findings, she said.
“Before asking for approval of cannabinoids for symptomatic treatment of spasticity in patients with amyotrophic lateral sclerosis, further studies are needed to establish the frequency of spasticity in the various presentations of motor neuron disease, and also whether reductions in spasticity improve quality of life,” Dr. de Visser said in a press release. “Natural history studies including all subtypes of motor neuron disease and better outcome measures aimed at assessment of spasticity are required. Dr. Riva and colleagues’ data are encouraging, and larger multicenter, randomized controlled trials should be done to identify which subgroups of patients derive clinically significant benefits from nabiximols.”
Marianne de Visser, MD, PhD, is with the department of neurology at Amsterdam University Medical Center. She reported no relevant conflicts of interest. Her remarks are taken from an editorial accompanying the study by Dr. Riva and associates (Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422[18]30493-9 ).
Although the results of Riva et al. are encouraging, the study had several major limitations and future research in the form of larger, multicenter, randomized controlled trials is needed, Marianne de Visser, MD, PhD, wrote in a related editorial.
Dr. de Visser noted a bias in the study as it randomized 16 patients with predominantly upper motor neuron involvement to the nabiximols group. The treatment could potentially have benefited those patients, for whom spasticity is the prevailing symptom, more than the 13 patients randomized to the nabiximols group who had classic amyotrophic lateral sclerosis involving both upper and lower neurons. In addition, Riva et al. did not differentiate between patients with upper and lower limb spasticity or patients with bulbar spasticity and those without, she said.
The use of the Modified Ashworth Scale was also a potential issue, because while it has been used in previous studies examining antispastic treatment efficacy, “it lacked sensitivity in studies of the efficacy of cannabinoids in patients with multiple sclerosis–related spasticity, and new spasticity numeric rating or visual analogue scales are being adopted,” Dr. de Visser wrote.
The number of adverse effects in the treatment group could have also unblinded researchers, which may have affected the significant findings, she said.
“Before asking for approval of cannabinoids for symptomatic treatment of spasticity in patients with amyotrophic lateral sclerosis, further studies are needed to establish the frequency of spasticity in the various presentations of motor neuron disease, and also whether reductions in spasticity improve quality of life,” Dr. de Visser said in a press release. “Natural history studies including all subtypes of motor neuron disease and better outcome measures aimed at assessment of spasticity are required. Dr. Riva and colleagues’ data are encouraging, and larger multicenter, randomized controlled trials should be done to identify which subgroups of patients derive clinically significant benefits from nabiximols.”
Marianne de Visser, MD, PhD, is with the department of neurology at Amsterdam University Medical Center. She reported no relevant conflicts of interest. Her remarks are taken from an editorial accompanying the study by Dr. Riva and associates (Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422[18]30493-9 ).
Nabiximols, a cannabis-based oral spray containing delta-9 tetrahydrocannabinol and cannabidiol, significantly improved spasticity symptoms in combination with antispasticity drugs in patients with motor neuron disease in a randomized, double-blind, placebo-controlled, parallel-group, phase 2 clinical trial.
Nabiximols proved superior to a placebo spray when both were given to patients with either amyotrophic lateral sclerosis or primary lateral sclerosis as part of an antispasticity regimen in the 6-week, CANALS (Cannabis Sativa Extract in Amyotrophic Lateral Sclerosis and other Motor Neuron Disease) study at four Italian centers, Nilo Riva, MD, PhD, of the San Raffaele Scientific Institute in Milan and his colleagues reported in The Lancet Neurology. Nabiximols is approved for the treatment of spasticity due to multiple sclerosis in multiple countries, but not in the United States.
“There is no cure for motor neuron disease, so improved symptom control and quality of life are important for patients,” Dr. Riva stated in a press release. “Our proof-of-concept trial showed a beneficial effect of THC-CBD [delta-9 tetrahydrocannabinol and cannabidiol] spray in people on treatment-resistant spasticity and pain.
“Despite these encouraging findings, we must first confirm that THC-CBD spray is effective and safe in larger, longer-term phase 3 trials,” Dr. Riva added.
The patients enrolled in the phase 2 trial between January 2013 and December 2014 and were between 18 and 80 years old with a probable diagnosis of amyotrophic lateral sclerosis or primary lateral sclerosis, were on an antispasticity regimen for at least 30 days, and had a spasticity score of at least 1 in two muscle groups on the 5-point Modified Ashworth Scale. Participants titrated for the first 2 weeks before maintaining their treatment for 4 weeks.
Of 59 participants at final follow-up, Modified Ashworth Scale scores improved in the nabiximols group (29 participants) by a mean of –0.11 points, compared with worsening by a mean of 0.16 points in the placebo group (30 participants). The researchers noted that there were no participants who withdrew from the study, nabiximols was well-tolerated, and there were no serious adverse events in the nabiximols group; however, there were 22 participants in the nabiximols group and 8 participants in the placebo group who experienced an adverse event from any cause.
“This study is, to our knowledge, the first randomized controlled trial of safety and efficacy of a pharmacological treatment for spasticity and the first trial of nabiximols in motor neuron disease,” Dr. Riva and his colleagues wrote. “Our results suggest that the study drug is well tolerated and provides first evidence of efficacy in terms of controlling spasticity in patients with motor neuron disease.”
The study was funded by the Italian Research Foundation for Amyotrophic Lateral Sclerosis. GW Pharma, which developed nabiximols, provided the study drug and placebo. Many of the authors reported financial disclosures with pharmaceutical companies.
SOURCE: Riva N et al. Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422(18)30406-X.
Nabiximols, a cannabis-based oral spray containing delta-9 tetrahydrocannabinol and cannabidiol, significantly improved spasticity symptoms in combination with antispasticity drugs in patients with motor neuron disease in a randomized, double-blind, placebo-controlled, parallel-group, phase 2 clinical trial.
Nabiximols proved superior to a placebo spray when both were given to patients with either amyotrophic lateral sclerosis or primary lateral sclerosis as part of an antispasticity regimen in the 6-week, CANALS (Cannabis Sativa Extract in Amyotrophic Lateral Sclerosis and other Motor Neuron Disease) study at four Italian centers, Nilo Riva, MD, PhD, of the San Raffaele Scientific Institute in Milan and his colleagues reported in The Lancet Neurology. Nabiximols is approved for the treatment of spasticity due to multiple sclerosis in multiple countries, but not in the United States.
“There is no cure for motor neuron disease, so improved symptom control and quality of life are important for patients,” Dr. Riva stated in a press release. “Our proof-of-concept trial showed a beneficial effect of THC-CBD [delta-9 tetrahydrocannabinol and cannabidiol] spray in people on treatment-resistant spasticity and pain.
“Despite these encouraging findings, we must first confirm that THC-CBD spray is effective and safe in larger, longer-term phase 3 trials,” Dr. Riva added.
The patients enrolled in the phase 2 trial between January 2013 and December 2014 and were between 18 and 80 years old with a probable diagnosis of amyotrophic lateral sclerosis or primary lateral sclerosis, were on an antispasticity regimen for at least 30 days, and had a spasticity score of at least 1 in two muscle groups on the 5-point Modified Ashworth Scale. Participants titrated for the first 2 weeks before maintaining their treatment for 4 weeks.
Of 59 participants at final follow-up, Modified Ashworth Scale scores improved in the nabiximols group (29 participants) by a mean of –0.11 points, compared with worsening by a mean of 0.16 points in the placebo group (30 participants). The researchers noted that there were no participants who withdrew from the study, nabiximols was well-tolerated, and there were no serious adverse events in the nabiximols group; however, there were 22 participants in the nabiximols group and 8 participants in the placebo group who experienced an adverse event from any cause.
“This study is, to our knowledge, the first randomized controlled trial of safety and efficacy of a pharmacological treatment for spasticity and the first trial of nabiximols in motor neuron disease,” Dr. Riva and his colleagues wrote. “Our results suggest that the study drug is well tolerated and provides first evidence of efficacy in terms of controlling spasticity in patients with motor neuron disease.”
The study was funded by the Italian Research Foundation for Amyotrophic Lateral Sclerosis. GW Pharma, which developed nabiximols, provided the study drug and placebo. Many of the authors reported financial disclosures with pharmaceutical companies.
SOURCE: Riva N et al. Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422(18)30406-X.
FROM THE LANCET NEUROLOGY
Key clinical point:
Major finding: In the nabiximols group, Modified Ashworth Scale scores improved by mean of –0.11 points, compared with worsening by a mean of 0.16 points in the placebo group.
Study details: A multicenter, double-blinded, randomized, placebo-controlled, phase 2 trial of 59 participants with spasticity symptoms from motor neuron disease from four tertiary motor neuron centers in Italy.
Disclosures: The study was funded by the Italian Research Foundation for Amyotrophic Lateral Sclerosis. GW Pharma, which developed nabiximols, provided the study drug and placebo. Many of the authors reported financial disclosures with pharmaceutical companies.
Source: Riva N et al. Lancet Neurol. 2018 Dec 13. doi: 10.1016/S1474-4422(18)30406-X
Algorithm proposes approach for managing TNF inhibitor–induced psoriasis
Patients with tumor necrosis factor inhibitor–induced psoriasis could potentially be switched to a different drug class if they have moderate to severe skin eruption or mild skin eruption with an uncontrolled underlying disease such as inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis, according to a new treatment algorithm proposed by researchers from Brigham and Women’s Hospital and Harvard Medical School in Boston.
The researchers outlined the prevalence of tumor necrosis factor–alpha inhibitor (TNFi)-induced psoriasis in a literature review of inflammatory bowel disease (IBD), psoriasis, psoriatic arthritis (PsA), and rheumatoid arthritis (RA) and identified an estimated rate of between 2.3% and 5% in patients with RA and between 1.6% and 2.7% in patients with IBD. Although there have been reports of TNFi-induced psoriasis in patients with psoriasis and PsA, the prevalence is unclear, they wrote in the Journal of Psoriasis and Psoriatic Arthritis.
The authors then created an algorithm to manage and treat TNFi-induced psoriasiform skin eruptions with decisions to continue therapy and “treat through” symptoms, switch to a different anti-TNF therapy, or switch to a different drug class based on severity of symptoms, whether the underlying disease is well controlled, and how patients with those underlying diseases have fared with those specific therapies or agents.
“We’ve shifted gears over the past decade, and we’ve gone from having very few agents and trying to keep patients desperately on one or two agents because we didn’t want to have to give up on them for their other comorbid disease, whether it was Crohn’s, colitis, RA, or whatever it may be,” senior author Joseph Merola, MD, director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, said in an interview. “We’re now in an area where we can have an algorithm like this, and we have so many more mechanistic options to move to.”
Dr. Merola, who is board certified in dermatology and rheumatology, said the algorithm is meant to “open a dialogue” with other specialists in different areas and raise awareness of treatments in related but separate fields. For diseases not often seen by more than one specialty, with the exception of psoriasis and PsA, he said that “the idea is to start a dialogue and increase communication between specialists.”
Dr. Merola noted that while the algorithm in many respects is meant to guide a physician in a specialty in appropriate medication decisions, at the same time he hopes that “it opens a dialogue and communication with the other specialty who tends to oversee this particular disease state or class of medicine to really work together to try to find the right drug for the right person.”
For patients with a mild skin eruption and a controlled underlying disease, the algorithm recommends a “treat through” approach by continuing anti-TNF therapy and treating psoriasis symptoms with topical steroids, ultraviolet therapy, methotrexate, cyclosporine, or acitretin, and to consider dapsone in cases of pustular psoriasis. However, the researchers noted that “treat through” studies have reported complete symptom resolution in 26%-41% of patients.
For patients with recalcitrant or worsening TNFi-induced psoriasis or patients with mild skin eruptions with an uncontrolled underlying disease, the researchers proposed considering switching to a different anti-TNF therapy, although studies have shown complete resolution of symptoms in only 5%-37% of patients.
If patients worsen from there, or if they have moderate to-severe skin eruption with uncontrolled underlying disease, they could be considered for switching to a different drug class and treated based on their underlying disease, along with treatment for psoriasis symptoms. This approach has been shown to completely resolve lesions in up to 64% of cases, they said. IBD patients could benefit from ustekinumab, vedolizumab, 6-mercaptopurine, or azathioprine as an alternative to anti-TNF therapy. Those patients with psoriasis should be considered for guselkumab, while ustekinumab, ixekizumab, secukinumab, and apremilast are effective treatments for patients with psoriasis and PsA. Patients with RA could receive treatment with tocilizumab, rituximab, abatacept, and tofacitinib, the authors wrote.
Dr. Merola reported serving as a consultant and/or investigator for Merck Research Laboratories, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Samumed, Celgene, Sanofi Regeneron, GlaxoSmithKline, Almirall, Sun Pharma, Biogen, Pfizer, Incyte, Aclaris, and Leo Pharma.
SOURCE: Li SJ et al. J Psoriasis Psoriatic Arthritis. 2018 Nov 21. doi: 10.1177/2475530318810851.
Patients with tumor necrosis factor inhibitor–induced psoriasis could potentially be switched to a different drug class if they have moderate to severe skin eruption or mild skin eruption with an uncontrolled underlying disease such as inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis, according to a new treatment algorithm proposed by researchers from Brigham and Women’s Hospital and Harvard Medical School in Boston.
The researchers outlined the prevalence of tumor necrosis factor–alpha inhibitor (TNFi)-induced psoriasis in a literature review of inflammatory bowel disease (IBD), psoriasis, psoriatic arthritis (PsA), and rheumatoid arthritis (RA) and identified an estimated rate of between 2.3% and 5% in patients with RA and between 1.6% and 2.7% in patients with IBD. Although there have been reports of TNFi-induced psoriasis in patients with psoriasis and PsA, the prevalence is unclear, they wrote in the Journal of Psoriasis and Psoriatic Arthritis.
The authors then created an algorithm to manage and treat TNFi-induced psoriasiform skin eruptions with decisions to continue therapy and “treat through” symptoms, switch to a different anti-TNF therapy, or switch to a different drug class based on severity of symptoms, whether the underlying disease is well controlled, and how patients with those underlying diseases have fared with those specific therapies or agents.
“We’ve shifted gears over the past decade, and we’ve gone from having very few agents and trying to keep patients desperately on one or two agents because we didn’t want to have to give up on them for their other comorbid disease, whether it was Crohn’s, colitis, RA, or whatever it may be,” senior author Joseph Merola, MD, director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, said in an interview. “We’re now in an area where we can have an algorithm like this, and we have so many more mechanistic options to move to.”
Dr. Merola, who is board certified in dermatology and rheumatology, said the algorithm is meant to “open a dialogue” with other specialists in different areas and raise awareness of treatments in related but separate fields. For diseases not often seen by more than one specialty, with the exception of psoriasis and PsA, he said that “the idea is to start a dialogue and increase communication between specialists.”
Dr. Merola noted that while the algorithm in many respects is meant to guide a physician in a specialty in appropriate medication decisions, at the same time he hopes that “it opens a dialogue and communication with the other specialty who tends to oversee this particular disease state or class of medicine to really work together to try to find the right drug for the right person.”
For patients with a mild skin eruption and a controlled underlying disease, the algorithm recommends a “treat through” approach by continuing anti-TNF therapy and treating psoriasis symptoms with topical steroids, ultraviolet therapy, methotrexate, cyclosporine, or acitretin, and to consider dapsone in cases of pustular psoriasis. However, the researchers noted that “treat through” studies have reported complete symptom resolution in 26%-41% of patients.
For patients with recalcitrant or worsening TNFi-induced psoriasis or patients with mild skin eruptions with an uncontrolled underlying disease, the researchers proposed considering switching to a different anti-TNF therapy, although studies have shown complete resolution of symptoms in only 5%-37% of patients.
If patients worsen from there, or if they have moderate to-severe skin eruption with uncontrolled underlying disease, they could be considered for switching to a different drug class and treated based on their underlying disease, along with treatment for psoriasis symptoms. This approach has been shown to completely resolve lesions in up to 64% of cases, they said. IBD patients could benefit from ustekinumab, vedolizumab, 6-mercaptopurine, or azathioprine as an alternative to anti-TNF therapy. Those patients with psoriasis should be considered for guselkumab, while ustekinumab, ixekizumab, secukinumab, and apremilast are effective treatments for patients with psoriasis and PsA. Patients with RA could receive treatment with tocilizumab, rituximab, abatacept, and tofacitinib, the authors wrote.
Dr. Merola reported serving as a consultant and/or investigator for Merck Research Laboratories, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Samumed, Celgene, Sanofi Regeneron, GlaxoSmithKline, Almirall, Sun Pharma, Biogen, Pfizer, Incyte, Aclaris, and Leo Pharma.
SOURCE: Li SJ et al. J Psoriasis Psoriatic Arthritis. 2018 Nov 21. doi: 10.1177/2475530318810851.
Patients with tumor necrosis factor inhibitor–induced psoriasis could potentially be switched to a different drug class if they have moderate to severe skin eruption or mild skin eruption with an uncontrolled underlying disease such as inflammatory bowel disease, psoriasis, psoriatic arthritis, or rheumatoid arthritis, according to a new treatment algorithm proposed by researchers from Brigham and Women’s Hospital and Harvard Medical School in Boston.
The researchers outlined the prevalence of tumor necrosis factor–alpha inhibitor (TNFi)-induced psoriasis in a literature review of inflammatory bowel disease (IBD), psoriasis, psoriatic arthritis (PsA), and rheumatoid arthritis (RA) and identified an estimated rate of between 2.3% and 5% in patients with RA and between 1.6% and 2.7% in patients with IBD. Although there have been reports of TNFi-induced psoriasis in patients with psoriasis and PsA, the prevalence is unclear, they wrote in the Journal of Psoriasis and Psoriatic Arthritis.
The authors then created an algorithm to manage and treat TNFi-induced psoriasiform skin eruptions with decisions to continue therapy and “treat through” symptoms, switch to a different anti-TNF therapy, or switch to a different drug class based on severity of symptoms, whether the underlying disease is well controlled, and how patients with those underlying diseases have fared with those specific therapies or agents.
“We’ve shifted gears over the past decade, and we’ve gone from having very few agents and trying to keep patients desperately on one or two agents because we didn’t want to have to give up on them for their other comorbid disease, whether it was Crohn’s, colitis, RA, or whatever it may be,” senior author Joseph Merola, MD, director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston, said in an interview. “We’re now in an area where we can have an algorithm like this, and we have so many more mechanistic options to move to.”
Dr. Merola, who is board certified in dermatology and rheumatology, said the algorithm is meant to “open a dialogue” with other specialists in different areas and raise awareness of treatments in related but separate fields. For diseases not often seen by more than one specialty, with the exception of psoriasis and PsA, he said that “the idea is to start a dialogue and increase communication between specialists.”
Dr. Merola noted that while the algorithm in many respects is meant to guide a physician in a specialty in appropriate medication decisions, at the same time he hopes that “it opens a dialogue and communication with the other specialty who tends to oversee this particular disease state or class of medicine to really work together to try to find the right drug for the right person.”
For patients with a mild skin eruption and a controlled underlying disease, the algorithm recommends a “treat through” approach by continuing anti-TNF therapy and treating psoriasis symptoms with topical steroids, ultraviolet therapy, methotrexate, cyclosporine, or acitretin, and to consider dapsone in cases of pustular psoriasis. However, the researchers noted that “treat through” studies have reported complete symptom resolution in 26%-41% of patients.
For patients with recalcitrant or worsening TNFi-induced psoriasis or patients with mild skin eruptions with an uncontrolled underlying disease, the researchers proposed considering switching to a different anti-TNF therapy, although studies have shown complete resolution of symptoms in only 5%-37% of patients.
If patients worsen from there, or if they have moderate to-severe skin eruption with uncontrolled underlying disease, they could be considered for switching to a different drug class and treated based on their underlying disease, along with treatment for psoriasis symptoms. This approach has been shown to completely resolve lesions in up to 64% of cases, they said. IBD patients could benefit from ustekinumab, vedolizumab, 6-mercaptopurine, or azathioprine as an alternative to anti-TNF therapy. Those patients with psoriasis should be considered for guselkumab, while ustekinumab, ixekizumab, secukinumab, and apremilast are effective treatments for patients with psoriasis and PsA. Patients with RA could receive treatment with tocilizumab, rituximab, abatacept, and tofacitinib, the authors wrote.
Dr. Merola reported serving as a consultant and/or investigator for Merck Research Laboratories, AbbVie, Dermavant, Eli Lilly, Novartis, Janssen, UCB, Samumed, Celgene, Sanofi Regeneron, GlaxoSmithKline, Almirall, Sun Pharma, Biogen, Pfizer, Incyte, Aclaris, and Leo Pharma.
SOURCE: Li SJ et al. J Psoriasis Psoriatic Arthritis. 2018 Nov 21. doi: 10.1177/2475530318810851.
FROM JOURNAL OF PSORIASIS AND PSORIATIC ARTHRITIS
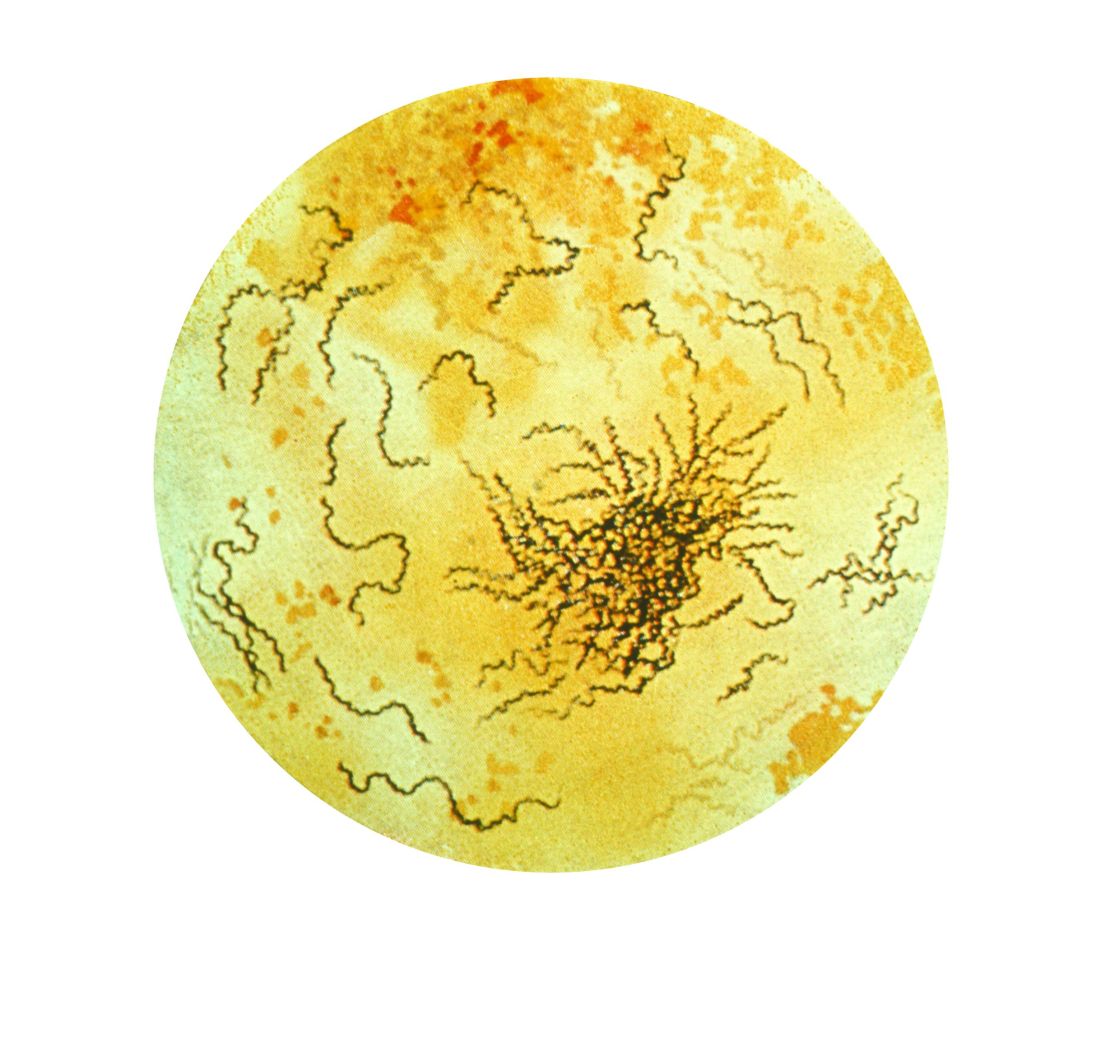
New syphilis cases for pregnant women rose 61% over 5 years
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Syphilis rates rose more in pregnant women between 2012 and 2016, compared with women in the general population.
Major finding: There was an increase of syphilis cases by 61% among pregnant women, compared with a 55% increase among women overall.
Study details: A study of national case report data from 9,883 pregnant women with reported syphilis during 2012-2016.
Disclosures: The authors reported no relevant conflicts of interest.
Source: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
Anticoagulant choice, PPI cotherapy impact risk of upper GI bleeding
Patients receiving oral anticoagulant treatment had the lowest risk of gastrointestinal bleeding when taking apixaban, compared with rivaroxaban, dabigatran, and warfarin, according to a recent study.
Further, patients who received proton pump inhibitor (PPI) cotherapy had a lower overall risk of gastrointestinal bleeding, according to Wayne A. Ray, PhD, from the department of health policy at Vanderbilt University, Nashville, Tenn., and his colleagues.
“These findings indicate the potential benefits of a gastrointestinal bleeding risk assessment before initiating anticoagulant treatment,” Dr. Ray and his colleagues wrote in their study, which was published in JAMA.
Dr. Ray and his colleagues performed a retrospective, population-based study of 1,643,123 Medicare beneficiaries (mean age, 76.4 years) who received 1,713,183 new episodes of oral anticoagulant treatment between January 2011 and September 2015. They analyzed how patients reacted to apixaban, dabigatran, rivaroxaban, or warfarin both with and without PPI cotherapy.
Overall, the risk of gastrointestinal bleeding across 754,389 person-years without PPI therapy was 115 per 10,000 person-years (95% confidence interval, 112-118) in 7,119 patients. The researchers found the risk of gastrointestinal bleeding was highest in patients taking rivaroxaban (1,278 patients; 144 per 10,000 person-years; 95% CI, 136-152) and lowest when taking apixaban (279 patients; 120 per 10,000 person-years; incidence rate ratio, 1,97; 95% CI, 1.73-2.25), compared with dabigatran (629 patients; 120 per 10,000 person-years; IRR, 1.19; 95% CI, 1.08-1.32) and warfarin (4,933 patients; 113 per 10,000 person-years; IRR, 1.27; 95% CI, 1.19-1.35). There was a significantly lower incidence of gastrointestinal bleeding for apixaban, compared with warfarin (IRR, 0.64; 95% CI, 0.57-0.73) and dabigatran (IRR, 0.61; 95% CI, 0.52-0.70).
There was a lower overall incidence of gastrointestinal bleeding when receiving PPI cotherapy (264,447 person-years; 76 per 10,000 person-years), compared with patients who received anticoagulant treatment without PPI cotherapy (IRR, 0.66; 95% CI, 0.62-0.69). This reduced incidence of gastrointestinal bleeding was also seen in patients receiving PPI cotherapy and taking apixaban (IRR, 0.66; 95% CI, 0.52-0.85), dabigatran (IRR, 0.49; 95% CI, 0.41-0.59), rivaroxaban (IRR, 0.75; 95% CI, 0.68-0.84), and warfarin (IRR, 0.65; 95% CI, 0.62-0.69).
The researchers noted that limitations in this study included potential misclassification of anticoagulant treatment, PPI cotherapy, and NSAIDs because of a reliance on filled prescription data; confounding by unmeasured factors such as aspirin exposure or Helicobacter pylori infection; and gastrointestinal bleeding being measured using a disease risk score.
This study was supported by a grant from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Ray WA et al. JAMA. 2018 Dec 4. doi: 10.1001/jama.2018.17242.
Patients receiving oral anticoagulant treatment had the lowest risk of gastrointestinal bleeding when taking apixaban, compared with rivaroxaban, dabigatran, and warfarin, according to a recent study.
Further, patients who received proton pump inhibitor (PPI) cotherapy had a lower overall risk of gastrointestinal bleeding, according to Wayne A. Ray, PhD, from the department of health policy at Vanderbilt University, Nashville, Tenn., and his colleagues.
“These findings indicate the potential benefits of a gastrointestinal bleeding risk assessment before initiating anticoagulant treatment,” Dr. Ray and his colleagues wrote in their study, which was published in JAMA.
Dr. Ray and his colleagues performed a retrospective, population-based study of 1,643,123 Medicare beneficiaries (mean age, 76.4 years) who received 1,713,183 new episodes of oral anticoagulant treatment between January 2011 and September 2015. They analyzed how patients reacted to apixaban, dabigatran, rivaroxaban, or warfarin both with and without PPI cotherapy.
Overall, the risk of gastrointestinal bleeding across 754,389 person-years without PPI therapy was 115 per 10,000 person-years (95% confidence interval, 112-118) in 7,119 patients. The researchers found the risk of gastrointestinal bleeding was highest in patients taking rivaroxaban (1,278 patients; 144 per 10,000 person-years; 95% CI, 136-152) and lowest when taking apixaban (279 patients; 120 per 10,000 person-years; incidence rate ratio, 1,97; 95% CI, 1.73-2.25), compared with dabigatran (629 patients; 120 per 10,000 person-years; IRR, 1.19; 95% CI, 1.08-1.32) and warfarin (4,933 patients; 113 per 10,000 person-years; IRR, 1.27; 95% CI, 1.19-1.35). There was a significantly lower incidence of gastrointestinal bleeding for apixaban, compared with warfarin (IRR, 0.64; 95% CI, 0.57-0.73) and dabigatran (IRR, 0.61; 95% CI, 0.52-0.70).
There was a lower overall incidence of gastrointestinal bleeding when receiving PPI cotherapy (264,447 person-years; 76 per 10,000 person-years), compared with patients who received anticoagulant treatment without PPI cotherapy (IRR, 0.66; 95% CI, 0.62-0.69). This reduced incidence of gastrointestinal bleeding was also seen in patients receiving PPI cotherapy and taking apixaban (IRR, 0.66; 95% CI, 0.52-0.85), dabigatran (IRR, 0.49; 95% CI, 0.41-0.59), rivaroxaban (IRR, 0.75; 95% CI, 0.68-0.84), and warfarin (IRR, 0.65; 95% CI, 0.62-0.69).
The researchers noted that limitations in this study included potential misclassification of anticoagulant treatment, PPI cotherapy, and NSAIDs because of a reliance on filled prescription data; confounding by unmeasured factors such as aspirin exposure or Helicobacter pylori infection; and gastrointestinal bleeding being measured using a disease risk score.
This study was supported by a grant from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Ray WA et al. JAMA. 2018 Dec 4. doi: 10.1001/jama.2018.17242.
Patients receiving oral anticoagulant treatment had the lowest risk of gastrointestinal bleeding when taking apixaban, compared with rivaroxaban, dabigatran, and warfarin, according to a recent study.
Further, patients who received proton pump inhibitor (PPI) cotherapy had a lower overall risk of gastrointestinal bleeding, according to Wayne A. Ray, PhD, from the department of health policy at Vanderbilt University, Nashville, Tenn., and his colleagues.
“These findings indicate the potential benefits of a gastrointestinal bleeding risk assessment before initiating anticoagulant treatment,” Dr. Ray and his colleagues wrote in their study, which was published in JAMA.
Dr. Ray and his colleagues performed a retrospective, population-based study of 1,643,123 Medicare beneficiaries (mean age, 76.4 years) who received 1,713,183 new episodes of oral anticoagulant treatment between January 2011 and September 2015. They analyzed how patients reacted to apixaban, dabigatran, rivaroxaban, or warfarin both with and without PPI cotherapy.
Overall, the risk of gastrointestinal bleeding across 754,389 person-years without PPI therapy was 115 per 10,000 person-years (95% confidence interval, 112-118) in 7,119 patients. The researchers found the risk of gastrointestinal bleeding was highest in patients taking rivaroxaban (1,278 patients; 144 per 10,000 person-years; 95% CI, 136-152) and lowest when taking apixaban (279 patients; 120 per 10,000 person-years; incidence rate ratio, 1,97; 95% CI, 1.73-2.25), compared with dabigatran (629 patients; 120 per 10,000 person-years; IRR, 1.19; 95% CI, 1.08-1.32) and warfarin (4,933 patients; 113 per 10,000 person-years; IRR, 1.27; 95% CI, 1.19-1.35). There was a significantly lower incidence of gastrointestinal bleeding for apixaban, compared with warfarin (IRR, 0.64; 95% CI, 0.57-0.73) and dabigatran (IRR, 0.61; 95% CI, 0.52-0.70).
There was a lower overall incidence of gastrointestinal bleeding when receiving PPI cotherapy (264,447 person-years; 76 per 10,000 person-years), compared with patients who received anticoagulant treatment without PPI cotherapy (IRR, 0.66; 95% CI, 0.62-0.69). This reduced incidence of gastrointestinal bleeding was also seen in patients receiving PPI cotherapy and taking apixaban (IRR, 0.66; 95% CI, 0.52-0.85), dabigatran (IRR, 0.49; 95% CI, 0.41-0.59), rivaroxaban (IRR, 0.75; 95% CI, 0.68-0.84), and warfarin (IRR, 0.65; 95% CI, 0.62-0.69).
The researchers noted that limitations in this study included potential misclassification of anticoagulant treatment, PPI cotherapy, and NSAIDs because of a reliance on filled prescription data; confounding by unmeasured factors such as aspirin exposure or Helicobacter pylori infection; and gastrointestinal bleeding being measured using a disease risk score.
This study was supported by a grant from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Ray WA et al. JAMA. 2018 Dec 4. doi: 10.1001/jama.2018.17242.
FROM JAMA
Key clinical point: In patients receiving oral anticoagulant treatment, risk of gastrointestinal bleeding was highest in patients taking rivaroxaban, lowest when taking apixaban, and there was a lower overall incidence of gastrointestinal bleeding when receiving proton pump inhibitor cotherapy.
Major finding: Per 10,000 person-years, the incidence rate of gastrointestinal bleeding was 144 for rivaroxaban, 73 for apixaban, 120 for dabigatran, and 113 for warfarin; there was a gastrointestinal bleeding incidence rate ratio of 0.66 for patients using protein pump inhibitor cotherapy.
Study details: A retrospective, population-based study of 1,643,123 Medicare beneficiaries who received oral anticoagulant treatment between January 2011 and September 2015.
Disclosures: This study was supported by a grant from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
Source: Ray WA et al. JAMA. 2018 Dec 4. doi: 10.1001/jama.2018.17242.
Nocturnal hypoxemia predicts incident atrial fibrillation in sleep apnea patients
Researchers have found a significant independent association between nocturnal hypoxemia and risk of incident atrial fibrillation (AF) in patients with obstructive sleep apnea (OSA), which they believe may help prevent the development of AF in this population, according to recent research published in the journal CHEST®.
“These findings are consistent with those of previous studies suggesting that these groups, who are typically at somewhat lower risk of [atrial fibrillation], might be especially vulnerable to the effects of [obstructive sleep apnea] and hypoxemia,” Tetyana Kendzerska, MD, PhD, of the University of Ottawa in Ottawa, and her colleagues wrote in their study.
They performed an analysis of 8,256 patients with data linked to a provincial health administrative database who had suspected OSA who underwent a sleep study at a large academic hospital between 1994 and 2010. The patients were median 47 years old; 62% of the cohort were men, 28% had an apnea-hypopnea index (AHI) of greater than 30 events per hour, and 6% spent more than 30% of the time during sleep with less than 90% oxygen saturation.
Overall, 173 of 8,256 patients (2.1%) developed AF during the study period. In patients with suspected OSA and who were arrhythmia free, nocturnal hypoxemia significantly increased the risk of incident hospitalized AF (hazard ratio, 2.47; 95% confidence interval, 1.64-3.71) over median 10 years of follow-up (interquartile range, 7-13 years) after the researchers controlled for age, sex, chronic obstructive pulmonary disease, history of heart failure, smoking status, nocturnal hypoxemia, and pulmonary embolism, and this association remained significant after adjustment for body mass index and hypertension (HR, 1.77; 95% CI, 1.15-2.74).
“These findings support a relationship between OSA, chronic nocturnal hypoxemia, and the development of [atrial fibrillation], and may be used to identify those patients with OSA who are at greatest risk of developing AF.”
Researchers cited the observational design, retrospective data collection, and examining hospitalized AF only as limitations in the study. However, they noted that clinical data was collected prospectively and the inability to adjust to positive airway pressure would push results to the null with regard to unstudied confounders.
The authors reported no relevant conflicts of interest.
SOURCE: Kendzerska T et al. CHEST. 2018;doi:10.1016/j.chest.2018.08.1075.
Researchers have found a significant independent association between nocturnal hypoxemia and risk of incident atrial fibrillation (AF) in patients with obstructive sleep apnea (OSA), which they believe may help prevent the development of AF in this population, according to recent research published in the journal CHEST®.
“These findings are consistent with those of previous studies suggesting that these groups, who are typically at somewhat lower risk of [atrial fibrillation], might be especially vulnerable to the effects of [obstructive sleep apnea] and hypoxemia,” Tetyana Kendzerska, MD, PhD, of the University of Ottawa in Ottawa, and her colleagues wrote in their study.
They performed an analysis of 8,256 patients with data linked to a provincial health administrative database who had suspected OSA who underwent a sleep study at a large academic hospital between 1994 and 2010. The patients were median 47 years old; 62% of the cohort were men, 28% had an apnea-hypopnea index (AHI) of greater than 30 events per hour, and 6% spent more than 30% of the time during sleep with less than 90% oxygen saturation.
Overall, 173 of 8,256 patients (2.1%) developed AF during the study period. In patients with suspected OSA and who were arrhythmia free, nocturnal hypoxemia significantly increased the risk of incident hospitalized AF (hazard ratio, 2.47; 95% confidence interval, 1.64-3.71) over median 10 years of follow-up (interquartile range, 7-13 years) after the researchers controlled for age, sex, chronic obstructive pulmonary disease, history of heart failure, smoking status, nocturnal hypoxemia, and pulmonary embolism, and this association remained significant after adjustment for body mass index and hypertension (HR, 1.77; 95% CI, 1.15-2.74).
“These findings support a relationship between OSA, chronic nocturnal hypoxemia, and the development of [atrial fibrillation], and may be used to identify those patients with OSA who are at greatest risk of developing AF.”
Researchers cited the observational design, retrospective data collection, and examining hospitalized AF only as limitations in the study. However, they noted that clinical data was collected prospectively and the inability to adjust to positive airway pressure would push results to the null with regard to unstudied confounders.
The authors reported no relevant conflicts of interest.
SOURCE: Kendzerska T et al. CHEST. 2018;doi:10.1016/j.chest.2018.08.1075.
Researchers have found a significant independent association between nocturnal hypoxemia and risk of incident atrial fibrillation (AF) in patients with obstructive sleep apnea (OSA), which they believe may help prevent the development of AF in this population, according to recent research published in the journal CHEST®.
“These findings are consistent with those of previous studies suggesting that these groups, who are typically at somewhat lower risk of [atrial fibrillation], might be especially vulnerable to the effects of [obstructive sleep apnea] and hypoxemia,” Tetyana Kendzerska, MD, PhD, of the University of Ottawa in Ottawa, and her colleagues wrote in their study.
They performed an analysis of 8,256 patients with data linked to a provincial health administrative database who had suspected OSA who underwent a sleep study at a large academic hospital between 1994 and 2010. The patients were median 47 years old; 62% of the cohort were men, 28% had an apnea-hypopnea index (AHI) of greater than 30 events per hour, and 6% spent more than 30% of the time during sleep with less than 90% oxygen saturation.
Overall, 173 of 8,256 patients (2.1%) developed AF during the study period. In patients with suspected OSA and who were arrhythmia free, nocturnal hypoxemia significantly increased the risk of incident hospitalized AF (hazard ratio, 2.47; 95% confidence interval, 1.64-3.71) over median 10 years of follow-up (interquartile range, 7-13 years) after the researchers controlled for age, sex, chronic obstructive pulmonary disease, history of heart failure, smoking status, nocturnal hypoxemia, and pulmonary embolism, and this association remained significant after adjustment for body mass index and hypertension (HR, 1.77; 95% CI, 1.15-2.74).
“These findings support a relationship between OSA, chronic nocturnal hypoxemia, and the development of [atrial fibrillation], and may be used to identify those patients with OSA who are at greatest risk of developing AF.”
Researchers cited the observational design, retrospective data collection, and examining hospitalized AF only as limitations in the study. However, they noted that clinical data was collected prospectively and the inability to adjust to positive airway pressure would push results to the null with regard to unstudied confounders.
The authors reported no relevant conflicts of interest.
SOURCE: Kendzerska T et al. CHEST. 2018;doi:10.1016/j.chest.2018.08.1075.
FROM CHEST
Key clinical point: In patients with suspected obstructive sleep apnea and who were arrhythmia free, nocturnal hypoxemia increased the risk of incident hospitalized atrial fibrillation by 77%.
Major finding: Nocturnal hypoxemia significantly predicted atrial fibrillation (hazard ratio, 2.47; 95% confidence interval, 1.64-3.71) and remained significant after adjustment for body mass index and hypertension (HR, 1.77; 95% CI, 1.15-2.74).
Study details: An observational study of 8,256 arrhythmia-free patients with suspected obstructive sleep apnea who underwent a sleep study at a large academic hospital between 1994 and 2010.
Disclosures: The authors report no relevant conflicts of interest.
Source: Kendzerska T et al. CHEST. 2018;doi:10.1016/j.chest.2018.08.1075.
Prenatal, postnatal neuroimaging IDs most Zika-related brain injuries
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
While the study by Mulkey et al. adds to the body of evidence of prenatal and postnatal brain abnormalities, there are still many unanswered questions about the Zika virus and how to handle its unique diagnostic and clinical challenges, Margaret A. Honein, PhD, MPH, and Denise J. Jamieson, MD, MPH, wrote in a related editorial.
For example, Centers for Disease Control and Prevention recommendations state that infants with possible Zika exposure should receive an ophthalmologic and ultrasonographic examination at 1 month, and if the hearing test used otoacoustic emissions methods only, an automated auditory brainstem response test should be administered. While Mulkey et al. examined brain abnormalities in utero and in infants, it is not clear whether all CDC guidelines were followed in these cases.
In addition, because there is no reliable way to determine whether infants acquired Zika virus through the mother or through vertical transmission, assessing the proportion of congenitally infected infants or vertical-transmission infected infants who have neurodevelopmental disabilities and defects is not possible, they said. More longitudinal studies are needed to study the effects of the Zika virus and to prepare for the next outbreak.
“Zika was affecting pregnant women and their infants years before its teratogenic effect was recognized, and Zika will remain a serious risk to pregnant women and their infants until we have a safe vaccine that can fully prevent Zika virus infection during pregnancy,” they said. “Until then, ongoing public health efforts are essential to protect mothers and babies from this threat and ensure all disabilities associated with Zika virus infection are promptly identified, so that timely interventions can be provided.”
Dr. Honein is from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention, and Dr. Jamieson is from the department of gynecology & obstetrics at Emory University School of Medicine, Atlanta. These comments summarize their editorial in response to Mulkey et al. (JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4164). They reported no relevant conflicts of interest.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
Prenatal ultrasound can identify most abnormalities in fetuses exposed to Zika virus during pregnancy, and neuroimaging after birth can detect infant exposure in cases that appeared normal on prenatal ultrasound, according to research published in JAMA Pediatrics.
“Absence of prolonged maternal viremia did not have predictive associations with normal fetal or neonatal brain imaging,” Sarah B. Mulkey, MD, PhD, from the division of fetal and transitional medicine at Children’s National Health System, in Washington, and her colleagues wrote. “Postnatal imaging can detect changes not seen on fetal imaging, supporting the current CDC [Centers for Disease Control and Prevention] recommendation for postnatal cranial [ultrasound].”
Dr. Mulkey and her colleagues performed a prospective cohort analysis of 82 pregnant women from Colombia and the United States who had clinical evidence of probable exposure to the Zika virus through travel (U.S. cases, 2 patients), physician referral, or community cases during June 2016-June 2017. Pregnant women underwent fetal MRI or ultrasound during the second or third trimesters between 4 weeks and 10 weeks after symptom onset, with infants undergoing brain MRI and cranial ultrasound after birth.
Of those 82 pregnancies, there were 80 live births, 1 case of termination because of severe fetal brain abnormalities, and 1 near-term fetal death of unknown cause. There was one death 3 days after birth and one instance of neurosurgical intervention from encephalocele. The researchers found 3 of 82 cases (4%) displayed fetal abnormalities from MRI, which consisted of 2 cases of heterotopias and malformations in cortical development and 1 case with parietal encephalocele, Chiari II malformation, and microcephaly. One infant had a normal ultrasound despite abnormalities displayed on fetal MRI.
After birth, of the 79 infants with normal ultrasound results, 53 infants underwent a postnatal brain MRI and Dr. Mulkey and her associates found 7 cases with mild abnormalities (13%). There were 57 infants who underwent cranial ultrasound, which yielded 21 cases of lenticulostriate vasculopathy, choroid plexus cysts, germinolytic/subependymal cysts, and/or calcification; these were poorly characterized by MRI.
“Normal fetal imaging had predictive associations with normal postnatal imaging or mild postnatal imaging findings unlikely to be of significant clinical consequence,” they said.
Nonetheless, “there is a need for long-term follow-up to assess the neurodevelopmental significance of these early neuroimaging findings, both normal and abnormal; such studies are in progress,” Dr. Mulkey and her colleagues said.
The researchers noted the timing of maternal infections and symptoms as well as the Zika testing, ultrasound, and MRI performance, technique during fetal MRI, and incomplete prenatal testing in the cohort as limitations in the study.
This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr. Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
SOURCE: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26. doi: 10.1001/jamapediatrics.2018.4138.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: In 82 pregnant women, prenatal neuroimaging identified fetal abnormalities in 3 cases, while postnatal neuroimaging in 53 of the remaining 79 cases yielded an additional 7 cases with mild abnormalities.
Study details: A prospective longitudinal cohort study of 82 pregnant women with clinical evidence of probable Zika infection in Colombia and the United States.
Disclosures: This study was funded in part by Children’s National Health System and by a philanthropic gift from the Ikaria Healthcare Fund. Dr Mulkey received research support from the Thrasher Research Fund and is supported by awards from the National Institutes of Health National Center for Advancing Translational Sciences. The other authors reported no relevant conflicts of interest.
Source: Mulkey SB et al. JAMA Pediatr. 2018 Nov. 26; doi: 10.1001/jamapediatrics.2018.4138.
Annual cost of branded topical rosacea therapy is twice that of generics
according to a retrospective analysis of claims data published in the Journal of the American Academy of Dermatology.
“We found the mean annual cost of topical therapy for branded medications per person was nearly twice the cost of generics, despite the rise in generic drug costs,” Hadar Lev-Tov, MD, from the department of dermatology and cutaneous surgery at the University of Miami and his colleagues wrote in their study, published as a letter to the editor. “Thus, there is an opportunity to save healthcare costs, nearly $7.5 million annually, for this cohort.”
Dr. Lev-Tov and his colleagues performed an analysis of the MarketScan Commercial Claims and Encounters database to determine real-world costs and usage of rosacea medication and identified 72,173 adults with two or more claims for rosacea who visited a primary care provider, dermatologist, or ophthalmologist over 18 months, from January 2005 through December 2014. The majority of these patients – 62,074 (86%) – received topical medication therapy, while 4,463 (6%) of patients received oral therapy only. Of the patients who received topical therapy, 47,035 (75.8%) received single agent topical therapy and 15,039 (24.2%) patients used combination topical therapy. Metronidazole and azelaic acid were the most common combination used.
The researchers noted that this was “an important proportion” of patients who used combination topical therapy, despite it not being discussed in most guidelines. In addition, they added, “these medications are thought to work by similar mechanisms (anti-inflammatory, antioxidant, and KLK5 modulation) and to our knowledge have not been studied together.”
More patients were treated with branded topical medications (50,334) than with generics (39,621). With regard to price (calculated as the sum of insurance payments, copay, and deductible for each medication over 1 year), the mean annual cost of the branded topical medication was $308.02, compared with $160.37 for generic medications (P less than .0001). The researchers noted switching to a generic medication for treatment of rosacea would potentially save $147.65 per patient a year. (Costs were reported in 2015 US dollars.)
The researchers said their study was limited by lack of Medicare and Medicaid claims data, the retrospective study design, and dependence on an ICD-9 code only for diagnosis of rosacea, but they noted that 92% of patients received a diagnosis from a dermatologist. In addition, they recommended more studies be conducted on the cost-effectiveness of rosacea therapy when comparing systemic medications and topical therapies.
This study was funded in part by a grant from the American Acne and Rosacea Society. The authors report no relevant conflicts of interest.
SOURCE: Lev-Tov H et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.09.039.
according to a retrospective analysis of claims data published in the Journal of the American Academy of Dermatology.
“We found the mean annual cost of topical therapy for branded medications per person was nearly twice the cost of generics, despite the rise in generic drug costs,” Hadar Lev-Tov, MD, from the department of dermatology and cutaneous surgery at the University of Miami and his colleagues wrote in their study, published as a letter to the editor. “Thus, there is an opportunity to save healthcare costs, nearly $7.5 million annually, for this cohort.”
Dr. Lev-Tov and his colleagues performed an analysis of the MarketScan Commercial Claims and Encounters database to determine real-world costs and usage of rosacea medication and identified 72,173 adults with two or more claims for rosacea who visited a primary care provider, dermatologist, or ophthalmologist over 18 months, from January 2005 through December 2014. The majority of these patients – 62,074 (86%) – received topical medication therapy, while 4,463 (6%) of patients received oral therapy only. Of the patients who received topical therapy, 47,035 (75.8%) received single agent topical therapy and 15,039 (24.2%) patients used combination topical therapy. Metronidazole and azelaic acid were the most common combination used.
The researchers noted that this was “an important proportion” of patients who used combination topical therapy, despite it not being discussed in most guidelines. In addition, they added, “these medications are thought to work by similar mechanisms (anti-inflammatory, antioxidant, and KLK5 modulation) and to our knowledge have not been studied together.”
More patients were treated with branded topical medications (50,334) than with generics (39,621). With regard to price (calculated as the sum of insurance payments, copay, and deductible for each medication over 1 year), the mean annual cost of the branded topical medication was $308.02, compared with $160.37 for generic medications (P less than .0001). The researchers noted switching to a generic medication for treatment of rosacea would potentially save $147.65 per patient a year. (Costs were reported in 2015 US dollars.)
The researchers said their study was limited by lack of Medicare and Medicaid claims data, the retrospective study design, and dependence on an ICD-9 code only for diagnosis of rosacea, but they noted that 92% of patients received a diagnosis from a dermatologist. In addition, they recommended more studies be conducted on the cost-effectiveness of rosacea therapy when comparing systemic medications and topical therapies.
This study was funded in part by a grant from the American Acne and Rosacea Society. The authors report no relevant conflicts of interest.
SOURCE: Lev-Tov H et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.09.039.
according to a retrospective analysis of claims data published in the Journal of the American Academy of Dermatology.
“We found the mean annual cost of topical therapy for branded medications per person was nearly twice the cost of generics, despite the rise in generic drug costs,” Hadar Lev-Tov, MD, from the department of dermatology and cutaneous surgery at the University of Miami and his colleagues wrote in their study, published as a letter to the editor. “Thus, there is an opportunity to save healthcare costs, nearly $7.5 million annually, for this cohort.”
Dr. Lev-Tov and his colleagues performed an analysis of the MarketScan Commercial Claims and Encounters database to determine real-world costs and usage of rosacea medication and identified 72,173 adults with two or more claims for rosacea who visited a primary care provider, dermatologist, or ophthalmologist over 18 months, from January 2005 through December 2014. The majority of these patients – 62,074 (86%) – received topical medication therapy, while 4,463 (6%) of patients received oral therapy only. Of the patients who received topical therapy, 47,035 (75.8%) received single agent topical therapy and 15,039 (24.2%) patients used combination topical therapy. Metronidazole and azelaic acid were the most common combination used.
The researchers noted that this was “an important proportion” of patients who used combination topical therapy, despite it not being discussed in most guidelines. In addition, they added, “these medications are thought to work by similar mechanisms (anti-inflammatory, antioxidant, and KLK5 modulation) and to our knowledge have not been studied together.”
More patients were treated with branded topical medications (50,334) than with generics (39,621). With regard to price (calculated as the sum of insurance payments, copay, and deductible for each medication over 1 year), the mean annual cost of the branded topical medication was $308.02, compared with $160.37 for generic medications (P less than .0001). The researchers noted switching to a generic medication for treatment of rosacea would potentially save $147.65 per patient a year. (Costs were reported in 2015 US dollars.)
The researchers said their study was limited by lack of Medicare and Medicaid claims data, the retrospective study design, and dependence on an ICD-9 code only for diagnosis of rosacea, but they noted that 92% of patients received a diagnosis from a dermatologist. In addition, they recommended more studies be conducted on the cost-effectiveness of rosacea therapy when comparing systemic medications and topical therapies.
This study was funded in part by a grant from the American Acne and Rosacea Society. The authors report no relevant conflicts of interest.
SOURCE: Lev-Tov H et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.09.039.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: Patients used branded topical medications more often than generic medications for treatment of rosacea.
Major finding: About 50,000 patients were treated with branded topical medications than with generics (almost 40,000), at a mean annual cost of $308.02 and $160.37, respectively.
Study details: A retrospective cohort analysis of 72,173 adults with rosacea treated with topical or oral therapy from a commercial claims database between January 2005 and 2014.
Disclosures: This study was funded in part by a grant from the American Acne and Rosacea Society. The authors report no relevant conflicts of interest.
Source: Lev-Tov H et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.09.039.
Gestational, umbilical cord vitamin D levels don’t predict atopic disease in offspring
according to study results published in the journal Allergy.
Áine Hennessy, PhD, from the School of Food and Nutritional Sciences at the University College Cork (Ireland), and her colleagues performed a prospective cohort study of 1,537 women in the Cork BASELINE Birth Cohort Study who underwent measurement of serum 25-hydroxyvitamin D (25[OH]D) from maternal sera followed by measurement of 25(OH)D in umbilical cord blood (1,050 cases). They then measured the prevalence of eczema, food allergy, allergic rhinitis, and asthma in infants at aged 2 and 5 years.
The researchers found at 2 years old, 5% of infants had persistent eczema, 4% of infants had a food allergy and 8% of infants had aeroallergen sensitization. At age 5 years, 15% of infants had asthma, while 5% had allergic rhinitis. Mothers whose children went on to have atopy did not differ in their 25(OH)D levels at 15 weeks’ gestation (mean 58.4 nmol/L vs. 58.5 nmol/L) or in the levels in umbilical cord blood (mean 35.2 nmol/L and 35.4 nmol/L).
Of the women in the cohort, 74% ranged in age from 25 to 34 years; 49% reported a personal history of allergy and 37% reported a paternal allergy. The mean birth weight of the infants was 3,458 g; infants were breastfed for mean 11.9 weeks, 73% of infants were breastfeeding by the time they left the hospital and 45% of infants were breastfeeding by age 2 months.
Limitations of the study included that parental atopy status was self-reported and that the researchers noted they did not examine genetic variants of immunoglobulin E synthesis or vitamin D receptor polymorphisms.
“To fully characterize relationships between intrauterine vitamin D exposure and allergic disease, analysis of well‐constructed, large‐scale prospective cohorts of maternal‐infant dyads, which take due consideration of an individual’s inherited risk, early‐life exposures and environmental confounders, is still needed,” Dr. Hennessy and her colleagues wrote.
The study was funded by grants from the European Commission, Ireland Health Research Board, National Children’s Research Centre, Food Standards Agency and Science Foundation Ireland. The authors report no relevant conflicts of interest.
SOURCE: Hennessy A et al. Allergy. 2018 Aug 7. doi: 10.1111/all.13590.
according to study results published in the journal Allergy.
Áine Hennessy, PhD, from the School of Food and Nutritional Sciences at the University College Cork (Ireland), and her colleagues performed a prospective cohort study of 1,537 women in the Cork BASELINE Birth Cohort Study who underwent measurement of serum 25-hydroxyvitamin D (25[OH]D) from maternal sera followed by measurement of 25(OH)D in umbilical cord blood (1,050 cases). They then measured the prevalence of eczema, food allergy, allergic rhinitis, and asthma in infants at aged 2 and 5 years.
The researchers found at 2 years old, 5% of infants had persistent eczema, 4% of infants had a food allergy and 8% of infants had aeroallergen sensitization. At age 5 years, 15% of infants had asthma, while 5% had allergic rhinitis. Mothers whose children went on to have atopy did not differ in their 25(OH)D levels at 15 weeks’ gestation (mean 58.4 nmol/L vs. 58.5 nmol/L) or in the levels in umbilical cord blood (mean 35.2 nmol/L and 35.4 nmol/L).
Of the women in the cohort, 74% ranged in age from 25 to 34 years; 49% reported a personal history of allergy and 37% reported a paternal allergy. The mean birth weight of the infants was 3,458 g; infants were breastfed for mean 11.9 weeks, 73% of infants were breastfeeding by the time they left the hospital and 45% of infants were breastfeeding by age 2 months.
Limitations of the study included that parental atopy status was self-reported and that the researchers noted they did not examine genetic variants of immunoglobulin E synthesis or vitamin D receptor polymorphisms.
“To fully characterize relationships between intrauterine vitamin D exposure and allergic disease, analysis of well‐constructed, large‐scale prospective cohorts of maternal‐infant dyads, which take due consideration of an individual’s inherited risk, early‐life exposures and environmental confounders, is still needed,” Dr. Hennessy and her colleagues wrote.
The study was funded by grants from the European Commission, Ireland Health Research Board, National Children’s Research Centre, Food Standards Agency and Science Foundation Ireland. The authors report no relevant conflicts of interest.
SOURCE: Hennessy A et al. Allergy. 2018 Aug 7. doi: 10.1111/all.13590.
according to study results published in the journal Allergy.
Áine Hennessy, PhD, from the School of Food and Nutritional Sciences at the University College Cork (Ireland), and her colleagues performed a prospective cohort study of 1,537 women in the Cork BASELINE Birth Cohort Study who underwent measurement of serum 25-hydroxyvitamin D (25[OH]D) from maternal sera followed by measurement of 25(OH)D in umbilical cord blood (1,050 cases). They then measured the prevalence of eczema, food allergy, allergic rhinitis, and asthma in infants at aged 2 and 5 years.
The researchers found at 2 years old, 5% of infants had persistent eczema, 4% of infants had a food allergy and 8% of infants had aeroallergen sensitization. At age 5 years, 15% of infants had asthma, while 5% had allergic rhinitis. Mothers whose children went on to have atopy did not differ in their 25(OH)D levels at 15 weeks’ gestation (mean 58.4 nmol/L vs. 58.5 nmol/L) or in the levels in umbilical cord blood (mean 35.2 nmol/L and 35.4 nmol/L).
Of the women in the cohort, 74% ranged in age from 25 to 34 years; 49% reported a personal history of allergy and 37% reported a paternal allergy. The mean birth weight of the infants was 3,458 g; infants were breastfed for mean 11.9 weeks, 73% of infants were breastfeeding by the time they left the hospital and 45% of infants were breastfeeding by age 2 months.
Limitations of the study included that parental atopy status was self-reported and that the researchers noted they did not examine genetic variants of immunoglobulin E synthesis or vitamin D receptor polymorphisms.
“To fully characterize relationships between intrauterine vitamin D exposure and allergic disease, analysis of well‐constructed, large‐scale prospective cohorts of maternal‐infant dyads, which take due consideration of an individual’s inherited risk, early‐life exposures and environmental confounders, is still needed,” Dr. Hennessy and her colleagues wrote.
The study was funded by grants from the European Commission, Ireland Health Research Board, National Children’s Research Centre, Food Standards Agency and Science Foundation Ireland. The authors report no relevant conflicts of interest.
SOURCE: Hennessy A et al. Allergy. 2018 Aug 7. doi: 10.1111/all.13590.
FROM ALLERGY
Key clinical point: There was no association between prevalence of atopic disease and vitamin D levels measured in maternal sera during pregnancy or in umbilical cord blood.
Major finding: Maternal vitamin D levels at 15 weeks of gestation (mean 58.4 nmol/L vs. 58.5 nmol/L) and concentrations in umbilical cord blood (mean 35.2 nmol/L and 35.4 nmol/L) were not associated with such atopic diseases as eczema, food allergy, asthma, and allergic rhinitis in children.
Study details: A prospective group of 1,537 women and infant pairs from the Cork BASELINE Birth Cohort Study.
Disclosures: This study was funded by grants from the European Commission, Ireland Health Research Board, National Children’s Research Centre, Food Standards Agency and Science Foundation Ireland. The authors report no relevant conflicts of interest.
Source: Hennessy A et al. Allergy 2018 Aug 7. doi:10.1111/all.13590.