User login
Rotavirus vaccine again linked to small increase in risk of intussusception hospitalization
The first dose of rotavirus vaccine was again linked to a small, short-term increase in the risk of hospitalization for intussusception, but the benefits of the vaccine exceed this risk, according to a report.
In absolute numbers, there were an estimated 7 to 26 more intussusception cases per year among U.S. children aged 8-11 weeks during the postvaccine era, compared with the prevaccine era, said Jacqueline E. Tate, PhD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, and her associates.
The increased risk did not extend to older children, which “is consistent with other U.S. studies,” the investigators said. “[Given] the magnitude of the declines in rotavirus disease compared with the small increased risk of intussusception, the public health benefits of rotavirus vaccination far exceed the increased risk of intussusception.”
Human rotavirus vaccines have been linked to rare events of intussusception since at least 1999, when Rotashield was withdrawn from the market for this reason. The next two rotavirus vaccines to receive Food and Drug Administration approval, RotaTeq and Rotarix, were not linked to intussusception in large trials or early postmarketing studies, but were estimated to cause 1-5 excess cases of intussusception per 100,000 population in more recent studies. Furthermore, a prior analysis of U.S. hospital discharge data found a small increase in the risk of intussusception hospitalization among 8- to 11-week-olds between 2007 to 2009, compared with baseline data from the prevaccine era, the investigators noted (Pediatrics. 2016 Aug 24. doi: 10.1542/peds.2016-1082).
To build on that analysis, they calculated rates of intussusception between 2000 and 2013 overall and among recommended age windows for rotavirus vaccination, which are 6-14 weeks for the first dose, 15-24 weeks for the second dose, and 25-34 weeks for the third dose. For consistency, they also looked at hospitalization rates among children aged 8-11 weeks.
The investigators identified 15,231 intussusception hospitalizations among children under 1 year of age during the study from 2000-2013. There were no overall trends in intussusception hospitalizations for all children under 1 year of age or subgroups of children aged 15-24 weeks or 25-34 weeks. Among children aged 8-11 weeks, intussusception hospitalization rates did rise significantly during the postvaccine era, compared with the prevaccine era for all years except 2011 and 2013. Excluding those two years, annual rates of intussusception hospitalizations among 8- to 11-week-olds were 46%-101% higher (16.7 to 22.9 hospitalizations per 100,000 population) during the postvaccine era than during the prevaccine era (11.4 hospitalizations per 100,000 population).
These results are “consistent with other U.S. studies that have been able to associate an increased risk of intussusception in the first week after the first dose of vaccine,” the researchers concluded. The advent of rotavirus vaccination prevented more than 176,000 hospitalizations, 242,000 emergency department visits, and 1.1 million outpatient visits from 2007 to 2011 (JAMA. 2015;313(22):2282-4), they noted.
The investigators reported no external funding sources and had no disclosures.
The first dose of rotavirus vaccine was again linked to a small, short-term increase in the risk of hospitalization for intussusception, but the benefits of the vaccine exceed this risk, according to a report.
In absolute numbers, there were an estimated 7 to 26 more intussusception cases per year among U.S. children aged 8-11 weeks during the postvaccine era, compared with the prevaccine era, said Jacqueline E. Tate, PhD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, and her associates.
The increased risk did not extend to older children, which “is consistent with other U.S. studies,” the investigators said. “[Given] the magnitude of the declines in rotavirus disease compared with the small increased risk of intussusception, the public health benefits of rotavirus vaccination far exceed the increased risk of intussusception.”
Human rotavirus vaccines have been linked to rare events of intussusception since at least 1999, when Rotashield was withdrawn from the market for this reason. The next two rotavirus vaccines to receive Food and Drug Administration approval, RotaTeq and Rotarix, were not linked to intussusception in large trials or early postmarketing studies, but were estimated to cause 1-5 excess cases of intussusception per 100,000 population in more recent studies. Furthermore, a prior analysis of U.S. hospital discharge data found a small increase in the risk of intussusception hospitalization among 8- to 11-week-olds between 2007 to 2009, compared with baseline data from the prevaccine era, the investigators noted (Pediatrics. 2016 Aug 24. doi: 10.1542/peds.2016-1082).
To build on that analysis, they calculated rates of intussusception between 2000 and 2013 overall and among recommended age windows for rotavirus vaccination, which are 6-14 weeks for the first dose, 15-24 weeks for the second dose, and 25-34 weeks for the third dose. For consistency, they also looked at hospitalization rates among children aged 8-11 weeks.
The investigators identified 15,231 intussusception hospitalizations among children under 1 year of age during the study from 2000-2013. There were no overall trends in intussusception hospitalizations for all children under 1 year of age or subgroups of children aged 15-24 weeks or 25-34 weeks. Among children aged 8-11 weeks, intussusception hospitalization rates did rise significantly during the postvaccine era, compared with the prevaccine era for all years except 2011 and 2013. Excluding those two years, annual rates of intussusception hospitalizations among 8- to 11-week-olds were 46%-101% higher (16.7 to 22.9 hospitalizations per 100,000 population) during the postvaccine era than during the prevaccine era (11.4 hospitalizations per 100,000 population).
These results are “consistent with other U.S. studies that have been able to associate an increased risk of intussusception in the first week after the first dose of vaccine,” the researchers concluded. The advent of rotavirus vaccination prevented more than 176,000 hospitalizations, 242,000 emergency department visits, and 1.1 million outpatient visits from 2007 to 2011 (JAMA. 2015;313(22):2282-4), they noted.
The investigators reported no external funding sources and had no disclosures.
The first dose of rotavirus vaccine was again linked to a small, short-term increase in the risk of hospitalization for intussusception, but the benefits of the vaccine exceed this risk, according to a report.
In absolute numbers, there were an estimated 7 to 26 more intussusception cases per year among U.S. children aged 8-11 weeks during the postvaccine era, compared with the prevaccine era, said Jacqueline E. Tate, PhD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, and her associates.
The increased risk did not extend to older children, which “is consistent with other U.S. studies,” the investigators said. “[Given] the magnitude of the declines in rotavirus disease compared with the small increased risk of intussusception, the public health benefits of rotavirus vaccination far exceed the increased risk of intussusception.”
Human rotavirus vaccines have been linked to rare events of intussusception since at least 1999, when Rotashield was withdrawn from the market for this reason. The next two rotavirus vaccines to receive Food and Drug Administration approval, RotaTeq and Rotarix, were not linked to intussusception in large trials or early postmarketing studies, but were estimated to cause 1-5 excess cases of intussusception per 100,000 population in more recent studies. Furthermore, a prior analysis of U.S. hospital discharge data found a small increase in the risk of intussusception hospitalization among 8- to 11-week-olds between 2007 to 2009, compared with baseline data from the prevaccine era, the investigators noted (Pediatrics. 2016 Aug 24. doi: 10.1542/peds.2016-1082).
To build on that analysis, they calculated rates of intussusception between 2000 and 2013 overall and among recommended age windows for rotavirus vaccination, which are 6-14 weeks for the first dose, 15-24 weeks for the second dose, and 25-34 weeks for the third dose. For consistency, they also looked at hospitalization rates among children aged 8-11 weeks.
The investigators identified 15,231 intussusception hospitalizations among children under 1 year of age during the study from 2000-2013. There were no overall trends in intussusception hospitalizations for all children under 1 year of age or subgroups of children aged 15-24 weeks or 25-34 weeks. Among children aged 8-11 weeks, intussusception hospitalization rates did rise significantly during the postvaccine era, compared with the prevaccine era for all years except 2011 and 2013. Excluding those two years, annual rates of intussusception hospitalizations among 8- to 11-week-olds were 46%-101% higher (16.7 to 22.9 hospitalizations per 100,000 population) during the postvaccine era than during the prevaccine era (11.4 hospitalizations per 100,000 population).
These results are “consistent with other U.S. studies that have been able to associate an increased risk of intussusception in the first week after the first dose of vaccine,” the researchers concluded. The advent of rotavirus vaccination prevented more than 176,000 hospitalizations, 242,000 emergency department visits, and 1.1 million outpatient visits from 2007 to 2011 (JAMA. 2015;313(22):2282-4), they noted.
The investigators reported no external funding sources and had no disclosures.
FROM PEDIATRICS
Key clinical point: The first dose of rotavirus vaccination is associated with a slight increase in risk of hospitalization for intussusception.
Major finding: Among 8-week-old infants to 11-week-old infants, rates of intussusception hospitalizations were significantly (46% to 101%) higher than in the prevaccine era for all postvaccine years except 2011 and 2013.
Data source: An analysis of hospitalization data from 2000 through 2013 from the State Inpatient Database, which covers 26 U.S. states.
Disclosures: The investigators had no external funding sources and no disclosures.
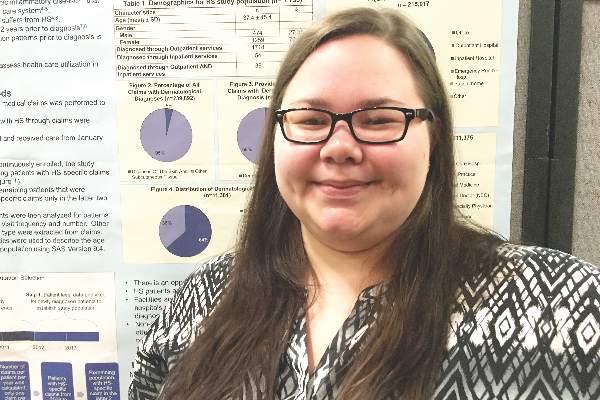
Healthy donor stool safe, effective for recurrent CDI
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
Kelly and her colleagues demonstrate that rigorous controlled trials are valuable even when we think we know the answer. Their results prompt us to ask again whether microbial manipulation has any as-yet unappreciated health benefits or risks and whether there are preferred microbiomes for specific human populations or locales.
Careful review of reported adverse events in the current trial is instructive. One participant reported a 9.1-kg weight gain (donor details were not provided), a problem previously described in a separate case report. There is great interest in understanding whether the microbiome can be manipulated to modify weight in humans, as has been clearly shown in mice. In addition, patients receiving donor stool more frequently reported chills. In my own practice, I have rarely observed transient fever after healthy donor FMT delivered orally in encapsulated form, and I hypothesize that this may be due to an immune reaction to a new microbial ecosystem. Patients considering FMT should be informed of both of these possible adverse events.
Elizabeth L. Hohmann, MD, is at Massachusetts General Hospital, Boston. She reported grant support and personal fees from Seres Therapeutics outside the submitted work. These comments are from an editorial accompanying the article (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-1784).
AGA Resource
The AGA Center for Gut Microbiome Research and Education was created to serve as a virtual ‘home’ for AGA activities related to the gut microbiome with a mission to advance research and education on the gut microbiome with the goal of improving human health. Learn more at www.gastro.org/microbiome.
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
For patients with recurrent Clostridium difficile infection (CDI), donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT), based on a small trial reported online in Annals of Internal Medicine.
In all, 20 of 22 patients (91%) achieved cure with donor FMT, compared with 63% of patients who received their own markedly dysbiotic stool (P = .04), reported Colleen Kelly, MD, of The Miriam Hospital, Providence, R.I., together with her associates. “Differences in efficacy between sites suggest that some patients with lower risk for CDI recurrence may not benefit from FMT. Further research may help determine the best candidates,” the researchers wrote.
FMT corrects the dysbiosis associated with CDI and is recommended in the event of failed antibiotic therapy leading to a third episode of infection. But this advice is based mainly on case series and open-label trials, the researchers noted. Their dual-center, randomized, controlled, double-blinded study included 46 patients with at least three recurrences of CDI who had completed a course of vancomycin during their most recent episode of infection. Patients older than age 75 years or who were immunocompromised were excluded (Ann Intern Med. 2016 Aug 22. doi: 10.7326/M16-0271).
The overall clinical cure rates reflected the literature, the researchers reported, and all nine patients who developed CDI after autologous FMT were subsequently cured by donor FMT. Indeed, donor FMT “restored normal microbial community structure, with reductions in Proteobacteria and Verrucomicrobia and increases in Bacteroidetes and Firmicutes. In contrast, microbial diversity did not improve after autologous FMT.”
Notably, however, 90% of autologous FMT patients at the center in New York achieved clinical cure, compared with 43% of patients at the center in Rhode Island. Further analyses revealed differences between patients and fecal microbiota at the two sites, the investigators said. Patients in New York typically had CDI for longer, with more recurrences and up to 148 weeks of vancomycin and other antibiotics. Thus, they might have been cured before enrollment. But “autologous FMT patients at the New York site [also] had greater abundances of Clostridia, raising the possibility of emergence of microbial community assemblages inhibitory to C. difficile via competitive niche exclusion, or possibly by emergence of nontoxigenic organisms,” the researchers wrote.
There were no serious adverse effects associated with either type of FMT, they noted.
Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Donor stool administered via colonoscopy seemed safe and achieved clinical cure significantly more often than autologous fecal microbiota transplantation (FMT) in patients with recurrent Clostridium difficile infection (CDI).
Major finding: In all, 91% of donor FMT patients and 63% of autologous FMT patients achieved clinical cure stool (P = .04).
Data source: A prospective, double-blind, randomized trial of 46 patients with at least three episodes of CDI, who had completed a full course of vancomycin during the most recent episode.
Disclosures: Dr. Kelly disclosed ties to Seres Health outside the submitted work. Two coauthors had patents or patents pending for “compositions and methods for transplantation of colon microbiota.” A third coauthor disclosed ties to OpenBiome and personal fees from CIPAC/Crestovo outside the submitted work. The remaining coauthors had no conflicts of interest.
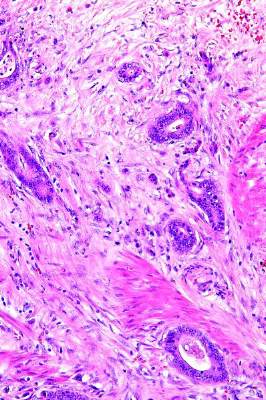
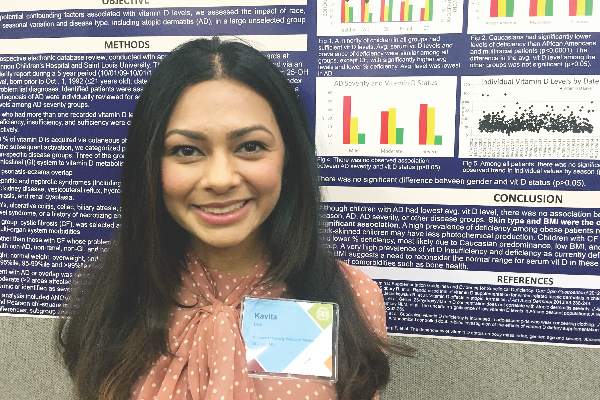
Inflammatory markers did not significantly predict colorectal cancer risk in men
Colorectal cancer in men was not significantly associated with baseline plasma levels of three inflammatory markers – C-reactive protein, interleukin-6, and tumor necrosis factor receptor 2 (TNFR-2), investigators reported online in Cancer Epidemiology.
The nested case-control study included 268 colorectal cancer (CRC) cases and 446 controls matched by age and smoking status from the Physician’s Health Study, a prospective, randomized, placebo-controlled aspirin trial. High TNFR-2 levels were significantly linked with CRC risk in the placebo arm (relative risk, 1.77; 95% confidence interval, 1.02-3.06; P = .02) of the study, and not in the aspirin arm (P = .72), Chul Kim, MD, of University of Minnesota, Minneapolis, and his associates noted. “This may suggest that aspirin exerts its carcinoprotective effect by blocking the TNF-alpha pathway,” they added, noting that in mice, blocking this pathway helps prevent CRC secondary to chronic colitis. However, a test for interactions yielded no evidence that aspirin significantly modifies the relationship between TNFR-2 and CRC, they said (Cancer Epidemiol. 2016;44:65-70).
Chronic inflammation is thought to promote carcinogenesis, including CRC, which is associated with inflammatory bowel disease. Studies have shown that long-term nonsteroidal anti-inflammatory and aspirin therapy attenuates CRC risk, but have not clarified the relationship between baseline plasma inflammatory markers and CRC. Dr. Kim and associates controlled for known CRC risk factors, including body mass index, alcohol consumption, physical activity level, multivitamin use, and dairy intake. In contrast to their findings in men, the Nurses’ Health Study did find a significant link between TNFR-2 levels and CRC risk in women, they noted (RR, 1.67; 95% CI, 1.05-2.68; P = .03).
They acknowledged several limitations. A single inflammatory marker test “may not represent a person’s inflammatory status during the development of colorectal cancer,” and marker levels were assayed during the run-in period of the trial, when all participants received aspirin, they said. Furthermore, the trial only ran for 5 years, after which more than 70% of patients took aspirin, which “would have significantly attenuated the true association that we would observe in this study.”
The National Cancer Institute, National Heart, Lung, and Blood Institute, National Cancer Institute of Canada, and National Institutes of Health provided funding. The authors had no disclosures.
Colorectal cancer in men was not significantly associated with baseline plasma levels of three inflammatory markers – C-reactive protein, interleukin-6, and tumor necrosis factor receptor 2 (TNFR-2), investigators reported online in Cancer Epidemiology.
The nested case-control study included 268 colorectal cancer (CRC) cases and 446 controls matched by age and smoking status from the Physician’s Health Study, a prospective, randomized, placebo-controlled aspirin trial. High TNFR-2 levels were significantly linked with CRC risk in the placebo arm (relative risk, 1.77; 95% confidence interval, 1.02-3.06; P = .02) of the study, and not in the aspirin arm (P = .72), Chul Kim, MD, of University of Minnesota, Minneapolis, and his associates noted. “This may suggest that aspirin exerts its carcinoprotective effect by blocking the TNF-alpha pathway,” they added, noting that in mice, blocking this pathway helps prevent CRC secondary to chronic colitis. However, a test for interactions yielded no evidence that aspirin significantly modifies the relationship between TNFR-2 and CRC, they said (Cancer Epidemiol. 2016;44:65-70).
Chronic inflammation is thought to promote carcinogenesis, including CRC, which is associated with inflammatory bowel disease. Studies have shown that long-term nonsteroidal anti-inflammatory and aspirin therapy attenuates CRC risk, but have not clarified the relationship between baseline plasma inflammatory markers and CRC. Dr. Kim and associates controlled for known CRC risk factors, including body mass index, alcohol consumption, physical activity level, multivitamin use, and dairy intake. In contrast to their findings in men, the Nurses’ Health Study did find a significant link between TNFR-2 levels and CRC risk in women, they noted (RR, 1.67; 95% CI, 1.05-2.68; P = .03).
They acknowledged several limitations. A single inflammatory marker test “may not represent a person’s inflammatory status during the development of colorectal cancer,” and marker levels were assayed during the run-in period of the trial, when all participants received aspirin, they said. Furthermore, the trial only ran for 5 years, after which more than 70% of patients took aspirin, which “would have significantly attenuated the true association that we would observe in this study.”
The National Cancer Institute, National Heart, Lung, and Blood Institute, National Cancer Institute of Canada, and National Institutes of Health provided funding. The authors had no disclosures.
Colorectal cancer in men was not significantly associated with baseline plasma levels of three inflammatory markers – C-reactive protein, interleukin-6, and tumor necrosis factor receptor 2 (TNFR-2), investigators reported online in Cancer Epidemiology.
The nested case-control study included 268 colorectal cancer (CRC) cases and 446 controls matched by age and smoking status from the Physician’s Health Study, a prospective, randomized, placebo-controlled aspirin trial. High TNFR-2 levels were significantly linked with CRC risk in the placebo arm (relative risk, 1.77; 95% confidence interval, 1.02-3.06; P = .02) of the study, and not in the aspirin arm (P = .72), Chul Kim, MD, of University of Minnesota, Minneapolis, and his associates noted. “This may suggest that aspirin exerts its carcinoprotective effect by blocking the TNF-alpha pathway,” they added, noting that in mice, blocking this pathway helps prevent CRC secondary to chronic colitis. However, a test for interactions yielded no evidence that aspirin significantly modifies the relationship between TNFR-2 and CRC, they said (Cancer Epidemiol. 2016;44:65-70).
Chronic inflammation is thought to promote carcinogenesis, including CRC, which is associated with inflammatory bowel disease. Studies have shown that long-term nonsteroidal anti-inflammatory and aspirin therapy attenuates CRC risk, but have not clarified the relationship between baseline plasma inflammatory markers and CRC. Dr. Kim and associates controlled for known CRC risk factors, including body mass index, alcohol consumption, physical activity level, multivitamin use, and dairy intake. In contrast to their findings in men, the Nurses’ Health Study did find a significant link between TNFR-2 levels and CRC risk in women, they noted (RR, 1.67; 95% CI, 1.05-2.68; P = .03).
They acknowledged several limitations. A single inflammatory marker test “may not represent a person’s inflammatory status during the development of colorectal cancer,” and marker levels were assayed during the run-in period of the trial, when all participants received aspirin, they said. Furthermore, the trial only ran for 5 years, after which more than 70% of patients took aspirin, which “would have significantly attenuated the true association that we would observe in this study.”
The National Cancer Institute, National Heart, Lung, and Blood Institute, National Cancer Institute of Canada, and National Institutes of Health provided funding. The authors had no disclosures.
FROM CANCER EPIDEMIOLOGY
Key clinical point: Baseline levels of C-reactive protein, TNFR-2, and interleukin-6 were not significantly associated with colorectal cancer risk among men.
Major finding: There was a significant link between high TNFR-2 levels and CRC risk in the placebo arm (RR, 1.77; 95% CI, 1.02-3.06; P = .02) of the trial, and not in the aspirin arm (P = .72). But there was no significant interaction between TNFR-2 and aspirin, making their relationship unclear.
Data source: A nested case-control study of 268 colorectal cancer patients and 446 age- and smoking-matched controls from a prospective randomized aspirin trial.
Disclosures: The National Cancer Institute, National Heart, Lung, and Blood Institute, National Cancer Institute of Canada, and National Institutes of Health provided funding. The authors had no disclosures.
Lentinan missed primary endpoint in gastric cancer trial
A shiitake mushroom extract called lentinan did not improve overall survival in advanced gastric cancer when added to the oral fluoropyrimidine S-1 in a randomized, controlled phase III trial.
Patients also experienced treatment failure significantly earlier on lentinan/S-1 than on S-1 monotherapy, Shigefumi Yoshino, MD, of Yamaguchi University Graduate School of Medicine in Ube, Japan, and his associates reported online August 5 in the European Journal of Cancer. “The present study showed no efficacy of lentinan administration combined with S-1 treatment in patients with unresectable or recurrent gastric cancer,” they concluded.
Lentinan, a purified beta-1, 3-glucan from Lentinus edodes (shiitake mushroom) has been shown to boost immune response and humoral antitumor immunity in mice and humans. S-1, a combination of tegafur, gimeracil, and potassium oxonate, is the most widely used therapy for unresectable or recurrent gastric cancer in Japan, the researchers noted. Based on promising results from a pilot trial, they conducted a prospective, multicenter, open-label phase III trial of 309 adults with unresectable or recurrent gastric cancer who were randomly assigned to receive S-1 with lentinan or S-1 alone. “S-1 was given orally twice daily for the first 4 weeks of a 6-week cycle,” they noted. “The dose of S-1 administered was calculated according to the patient’s body surface area as follows: less than 1.25 m2, 40 mg; 1.25-1.5 m2, 50 mg; and greater than 1.5 m2, 60 mg.” Lentinan was given intravenously at a dose of 2 mg weekly. Patients continued treatment until progressive disease, unacceptable toxicity, withdrawal of consent, or a decision to stop treatment by the treating physician (Eur J Cancer. 2016;65:164-71). The S-1 group received a median of three treatment cycles, while the S-1/lentinan group received a median of two S-1 cycles and 22 lentinan infusions, the investigators reported. Median overall survival was statistically similar between the arms (13.8 months with S-1 monotherapy and 9.9 months with combination therapy; P = 0.21). Median time to treatment failure was significantly longer with S-1 alone than with S-1 plus lentinan (4.3 and 2.6 months (P less than 0.001). Overall response rates were 22.3% with S-1 alone and 18.7% with S-1/lentinan combination therapy.
Lentinan did not yield significant safety signals, nor did it seem to affect quality of life, the researchers noted. Patients with relatively higher percentages of lentinan-binding monocytes (that is, at least 2%) who received more than two cycles of chemotherapy did survive significantly longer with lentinan plus S-1 than with S-1 alone, they reported. Within this subgroup, 24% of lentinan/S-1 patients were still alive at 3 years, compared with 3% of patients given S-1 monotherapy. Thus, a patient’s percentage of lentinan-binding monocytes might help predict response to lentinan, the researchers concluded.
The Japanese Foundation for Multidisciplinary Treatment of Cancer funded the study. Dr. Yoshino disclosed personal fees outside the current study from MSD, Taiho, and Chugai.
A shiitake mushroom extract called lentinan did not improve overall survival in advanced gastric cancer when added to the oral fluoropyrimidine S-1 in a randomized, controlled phase III trial.
Patients also experienced treatment failure significantly earlier on lentinan/S-1 than on S-1 monotherapy, Shigefumi Yoshino, MD, of Yamaguchi University Graduate School of Medicine in Ube, Japan, and his associates reported online August 5 in the European Journal of Cancer. “The present study showed no efficacy of lentinan administration combined with S-1 treatment in patients with unresectable or recurrent gastric cancer,” they concluded.
Lentinan, a purified beta-1, 3-glucan from Lentinus edodes (shiitake mushroom) has been shown to boost immune response and humoral antitumor immunity in mice and humans. S-1, a combination of tegafur, gimeracil, and potassium oxonate, is the most widely used therapy for unresectable or recurrent gastric cancer in Japan, the researchers noted. Based on promising results from a pilot trial, they conducted a prospective, multicenter, open-label phase III trial of 309 adults with unresectable or recurrent gastric cancer who were randomly assigned to receive S-1 with lentinan or S-1 alone. “S-1 was given orally twice daily for the first 4 weeks of a 6-week cycle,” they noted. “The dose of S-1 administered was calculated according to the patient’s body surface area as follows: less than 1.25 m2, 40 mg; 1.25-1.5 m2, 50 mg; and greater than 1.5 m2, 60 mg.” Lentinan was given intravenously at a dose of 2 mg weekly. Patients continued treatment until progressive disease, unacceptable toxicity, withdrawal of consent, or a decision to stop treatment by the treating physician (Eur J Cancer. 2016;65:164-71). The S-1 group received a median of three treatment cycles, while the S-1/lentinan group received a median of two S-1 cycles and 22 lentinan infusions, the investigators reported. Median overall survival was statistically similar between the arms (13.8 months with S-1 monotherapy and 9.9 months with combination therapy; P = 0.21). Median time to treatment failure was significantly longer with S-1 alone than with S-1 plus lentinan (4.3 and 2.6 months (P less than 0.001). Overall response rates were 22.3% with S-1 alone and 18.7% with S-1/lentinan combination therapy.
Lentinan did not yield significant safety signals, nor did it seem to affect quality of life, the researchers noted. Patients with relatively higher percentages of lentinan-binding monocytes (that is, at least 2%) who received more than two cycles of chemotherapy did survive significantly longer with lentinan plus S-1 than with S-1 alone, they reported. Within this subgroup, 24% of lentinan/S-1 patients were still alive at 3 years, compared with 3% of patients given S-1 monotherapy. Thus, a patient’s percentage of lentinan-binding monocytes might help predict response to lentinan, the researchers concluded.
The Japanese Foundation for Multidisciplinary Treatment of Cancer funded the study. Dr. Yoshino disclosed personal fees outside the current study from MSD, Taiho, and Chugai.
A shiitake mushroom extract called lentinan did not improve overall survival in advanced gastric cancer when added to the oral fluoropyrimidine S-1 in a randomized, controlled phase III trial.
Patients also experienced treatment failure significantly earlier on lentinan/S-1 than on S-1 monotherapy, Shigefumi Yoshino, MD, of Yamaguchi University Graduate School of Medicine in Ube, Japan, and his associates reported online August 5 in the European Journal of Cancer. “The present study showed no efficacy of lentinan administration combined with S-1 treatment in patients with unresectable or recurrent gastric cancer,” they concluded.
Lentinan, a purified beta-1, 3-glucan from Lentinus edodes (shiitake mushroom) has been shown to boost immune response and humoral antitumor immunity in mice and humans. S-1, a combination of tegafur, gimeracil, and potassium oxonate, is the most widely used therapy for unresectable or recurrent gastric cancer in Japan, the researchers noted. Based on promising results from a pilot trial, they conducted a prospective, multicenter, open-label phase III trial of 309 adults with unresectable or recurrent gastric cancer who were randomly assigned to receive S-1 with lentinan or S-1 alone. “S-1 was given orally twice daily for the first 4 weeks of a 6-week cycle,” they noted. “The dose of S-1 administered was calculated according to the patient’s body surface area as follows: less than 1.25 m2, 40 mg; 1.25-1.5 m2, 50 mg; and greater than 1.5 m2, 60 mg.” Lentinan was given intravenously at a dose of 2 mg weekly. Patients continued treatment until progressive disease, unacceptable toxicity, withdrawal of consent, or a decision to stop treatment by the treating physician (Eur J Cancer. 2016;65:164-71). The S-1 group received a median of three treatment cycles, while the S-1/lentinan group received a median of two S-1 cycles and 22 lentinan infusions, the investigators reported. Median overall survival was statistically similar between the arms (13.8 months with S-1 monotherapy and 9.9 months with combination therapy; P = 0.21). Median time to treatment failure was significantly longer with S-1 alone than with S-1 plus lentinan (4.3 and 2.6 months (P less than 0.001). Overall response rates were 22.3% with S-1 alone and 18.7% with S-1/lentinan combination therapy.
Lentinan did not yield significant safety signals, nor did it seem to affect quality of life, the researchers noted. Patients with relatively higher percentages of lentinan-binding monocytes (that is, at least 2%) who received more than two cycles of chemotherapy did survive significantly longer with lentinan plus S-1 than with S-1 alone, they reported. Within this subgroup, 24% of lentinan/S-1 patients were still alive at 3 years, compared with 3% of patients given S-1 monotherapy. Thus, a patient’s percentage of lentinan-binding monocytes might help predict response to lentinan, the researchers concluded.
The Japanese Foundation for Multidisciplinary Treatment of Cancer funded the study. Dr. Yoshino disclosed personal fees outside the current study from MSD, Taiho, and Chugai.
FROM EUROPEAN JOURNAL OF CANCER
Key clinical point: A shiitake mushroom extract called lentinan was ineffective in treating advanced gastric cancer when added to the oral fluoropyrimidine S-1.
Major finding: The primary endpoint, median overall survival, was 13.8 months with S-1 monotherapy and 9.9 months with lentinan/S-1 combination therapy (P = 0.21).
Data source: A prospective, multicenter, open-label, randomized phase III trial of 309 adults with unresectable or recurrent gastric cancer.
Disclosures: The Japanese Foundation for Multidisciplinary Treatment of Cancer funded the study. Dr. Yoshino disclosed personal fees outside the current study from MSD, Taiho, and Chugai.
AGA Clinical Practice Update: Experts carve pathway for celiac trials
Celiac disease’s only treatment is far from ideal. Not only is the gluten-free diet hard to follow, costly, and socially isolating, but even adherent patients can suffer persistent and disabling symptoms, Daniel A. Leffler, MD, MS, of Beth Israel Deaconess Medical Center in Boston, and his associates noted. This “high unmet medical need” inspired their discussion of clinical trials in celiac disease at the third Gastroenterology Regulatory Endpoints and Advancement of Therapeutics (GREAT 3). A summary appears as a Clinical Practice Update in Gastroenterology (2016 Jul 22. doi: 10.1053/j.gastro.2016.07.025).
Celiac is the “outlier among intestinal diseases,” the experts noted. Few randomized trials have assessed nondietary celiac disease therapies, drug developers lack a precedent approval to clarify a “guiding regulatory pathway.” The first step toward bridging these gaps is to better define target populations for clinical trials, meeting attendees agreed. Such groups might include patients with diet-refractory symptoms; newly diagnosed patients who need pharmacologic support for symptom resolution and duodenal healing; patients with asymptomatic mucosal damage, if such damage is shown to cause malignancy; and patients with neurobehavioral disorders that impede gluten avoidance. Medications that enable patients to safely consume gluten could benefit even more, including those who already face “arduous” dietary controls from comorbidities such as type 1 diabetes, the experts added.
Defining “clinical benefit” in pivotal trials of celiac disease also poses a challenge. “While every patient might desire something slightly different, the overarching theme of clinical benefit from the patient’s perspective appears to be quality of life – free of symptoms and inflammation without worry about [gluten] contamination,” attendees emphasized. Indeed, one recent survey found that patients prioritized protection against cross-contamination over being able to consume gluten at will. But initial trials should focus on gastrointestinal symptoms, which are common, affect patients of all ages, and “can be measured in a reasonable time frame,” they concluded.
Unfortunately, defining and measuring atypical symptoms can be difficult, particularly in children and adolescents. In an unpublished study at the Nationwide Children’s Hospital, gastrointestinal symptoms affected 77% of celiac patients, while only about 5% experienced atypical or nongastrointestinal symptoms, the experts noted. Such low percentages could make it difficult to adequately power studies of these nongastrointestinal outcomes. Furthermore, measuring sequelae such as osteoporosis or anemia “would require longer studies, as these conditions do not resolve quickly.”
Phase II and III trials cannot secure marketing approvals without clearly defining and measuring “clinical benefit,” Food and Drug Administration representatives at the meeting noted. Accordingly, diarrhea and abdominal pain will be key patient-reported outcome measures, and pivotal trials of young children with celiac disease will require observer-reported outcomes, attendees agreed. Although both celiac disease and the gluten-free diet profoundly undercut health-related quality of life, this measure is too broad and easily confounded to be a good endpoint in pivotal trials of celiac therapies. Likewise, histology is valuable for relating symptoms to active disease, but mucosal healing is too variable and unpredictable to serve as a primary endpoint, experts noted.
In contrast, serologic tests could serve as enrollment criteria, stratification measures, and endpoints if these tests received the appropriate FDA approvals, experts asserted. The endomysial antibody, tissue transglutaminase antibody, and deamidated gliadin peptide tests are most often used in practice, but have only been approved for diagnosing celiac disease – not as a replacement for biopsy or as a measure of disease progression or therapeutic response, FDA representatives noted. Although drug developers need tools to measure therapeutic efficacy in celiac disease, FDA recommended soliciting advice from its Center for Drug Evaluation and Research before testing these tools or kicking off monitoring studies.
The meeting was supported by the Celiac Disease Foundation and Beyond Celiac, and was sponsored by the FDA Center for Drug Evaluation and Research; the American Gastroenterological Association; the American College of Gastroenterology; the American Society for Pediatric Gastroenterology, Hepatology, and Nutrition; and the North American Society for the Study of Celiac Disease. Dr. Leffler disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, INOVA Diagnostics, Coronado Biosciences, Pfizer, and GI Supply. One coauthor and senior author, Dr. Sheila Crowe, disclosed ties to Alvine Pharmaceuticals, Ferring, and Celimmune.
Celiac disease’s only treatment is far from ideal. Not only is the gluten-free diet hard to follow, costly, and socially isolating, but even adherent patients can suffer persistent and disabling symptoms, Daniel A. Leffler, MD, MS, of Beth Israel Deaconess Medical Center in Boston, and his associates noted. This “high unmet medical need” inspired their discussion of clinical trials in celiac disease at the third Gastroenterology Regulatory Endpoints and Advancement of Therapeutics (GREAT 3). A summary appears as a Clinical Practice Update in Gastroenterology (2016 Jul 22. doi: 10.1053/j.gastro.2016.07.025).
Celiac is the “outlier among intestinal diseases,” the experts noted. Few randomized trials have assessed nondietary celiac disease therapies, drug developers lack a precedent approval to clarify a “guiding regulatory pathway.” The first step toward bridging these gaps is to better define target populations for clinical trials, meeting attendees agreed. Such groups might include patients with diet-refractory symptoms; newly diagnosed patients who need pharmacologic support for symptom resolution and duodenal healing; patients with asymptomatic mucosal damage, if such damage is shown to cause malignancy; and patients with neurobehavioral disorders that impede gluten avoidance. Medications that enable patients to safely consume gluten could benefit even more, including those who already face “arduous” dietary controls from comorbidities such as type 1 diabetes, the experts added.
Defining “clinical benefit” in pivotal trials of celiac disease also poses a challenge. “While every patient might desire something slightly different, the overarching theme of clinical benefit from the patient’s perspective appears to be quality of life – free of symptoms and inflammation without worry about [gluten] contamination,” attendees emphasized. Indeed, one recent survey found that patients prioritized protection against cross-contamination over being able to consume gluten at will. But initial trials should focus on gastrointestinal symptoms, which are common, affect patients of all ages, and “can be measured in a reasonable time frame,” they concluded.
Unfortunately, defining and measuring atypical symptoms can be difficult, particularly in children and adolescents. In an unpublished study at the Nationwide Children’s Hospital, gastrointestinal symptoms affected 77% of celiac patients, while only about 5% experienced atypical or nongastrointestinal symptoms, the experts noted. Such low percentages could make it difficult to adequately power studies of these nongastrointestinal outcomes. Furthermore, measuring sequelae such as osteoporosis or anemia “would require longer studies, as these conditions do not resolve quickly.”
Phase II and III trials cannot secure marketing approvals without clearly defining and measuring “clinical benefit,” Food and Drug Administration representatives at the meeting noted. Accordingly, diarrhea and abdominal pain will be key patient-reported outcome measures, and pivotal trials of young children with celiac disease will require observer-reported outcomes, attendees agreed. Although both celiac disease and the gluten-free diet profoundly undercut health-related quality of life, this measure is too broad and easily confounded to be a good endpoint in pivotal trials of celiac therapies. Likewise, histology is valuable for relating symptoms to active disease, but mucosal healing is too variable and unpredictable to serve as a primary endpoint, experts noted.
In contrast, serologic tests could serve as enrollment criteria, stratification measures, and endpoints if these tests received the appropriate FDA approvals, experts asserted. The endomysial antibody, tissue transglutaminase antibody, and deamidated gliadin peptide tests are most often used in practice, but have only been approved for diagnosing celiac disease – not as a replacement for biopsy or as a measure of disease progression or therapeutic response, FDA representatives noted. Although drug developers need tools to measure therapeutic efficacy in celiac disease, FDA recommended soliciting advice from its Center for Drug Evaluation and Research before testing these tools or kicking off monitoring studies.
The meeting was supported by the Celiac Disease Foundation and Beyond Celiac, and was sponsored by the FDA Center for Drug Evaluation and Research; the American Gastroenterological Association; the American College of Gastroenterology; the American Society for Pediatric Gastroenterology, Hepatology, and Nutrition; and the North American Society for the Study of Celiac Disease. Dr. Leffler disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, INOVA Diagnostics, Coronado Biosciences, Pfizer, and GI Supply. One coauthor and senior author, Dr. Sheila Crowe, disclosed ties to Alvine Pharmaceuticals, Ferring, and Celimmune.
Celiac disease’s only treatment is far from ideal. Not only is the gluten-free diet hard to follow, costly, and socially isolating, but even adherent patients can suffer persistent and disabling symptoms, Daniel A. Leffler, MD, MS, of Beth Israel Deaconess Medical Center in Boston, and his associates noted. This “high unmet medical need” inspired their discussion of clinical trials in celiac disease at the third Gastroenterology Regulatory Endpoints and Advancement of Therapeutics (GREAT 3). A summary appears as a Clinical Practice Update in Gastroenterology (2016 Jul 22. doi: 10.1053/j.gastro.2016.07.025).
Celiac is the “outlier among intestinal diseases,” the experts noted. Few randomized trials have assessed nondietary celiac disease therapies, drug developers lack a precedent approval to clarify a “guiding regulatory pathway.” The first step toward bridging these gaps is to better define target populations for clinical trials, meeting attendees agreed. Such groups might include patients with diet-refractory symptoms; newly diagnosed patients who need pharmacologic support for symptom resolution and duodenal healing; patients with asymptomatic mucosal damage, if such damage is shown to cause malignancy; and patients with neurobehavioral disorders that impede gluten avoidance. Medications that enable patients to safely consume gluten could benefit even more, including those who already face “arduous” dietary controls from comorbidities such as type 1 diabetes, the experts added.
Defining “clinical benefit” in pivotal trials of celiac disease also poses a challenge. “While every patient might desire something slightly different, the overarching theme of clinical benefit from the patient’s perspective appears to be quality of life – free of symptoms and inflammation without worry about [gluten] contamination,” attendees emphasized. Indeed, one recent survey found that patients prioritized protection against cross-contamination over being able to consume gluten at will. But initial trials should focus on gastrointestinal symptoms, which are common, affect patients of all ages, and “can be measured in a reasonable time frame,” they concluded.
Unfortunately, defining and measuring atypical symptoms can be difficult, particularly in children and adolescents. In an unpublished study at the Nationwide Children’s Hospital, gastrointestinal symptoms affected 77% of celiac patients, while only about 5% experienced atypical or nongastrointestinal symptoms, the experts noted. Such low percentages could make it difficult to adequately power studies of these nongastrointestinal outcomes. Furthermore, measuring sequelae such as osteoporosis or anemia “would require longer studies, as these conditions do not resolve quickly.”
Phase II and III trials cannot secure marketing approvals without clearly defining and measuring “clinical benefit,” Food and Drug Administration representatives at the meeting noted. Accordingly, diarrhea and abdominal pain will be key patient-reported outcome measures, and pivotal trials of young children with celiac disease will require observer-reported outcomes, attendees agreed. Although both celiac disease and the gluten-free diet profoundly undercut health-related quality of life, this measure is too broad and easily confounded to be a good endpoint in pivotal trials of celiac therapies. Likewise, histology is valuable for relating symptoms to active disease, but mucosal healing is too variable and unpredictable to serve as a primary endpoint, experts noted.
In contrast, serologic tests could serve as enrollment criteria, stratification measures, and endpoints if these tests received the appropriate FDA approvals, experts asserted. The endomysial antibody, tissue transglutaminase antibody, and deamidated gliadin peptide tests are most often used in practice, but have only been approved for diagnosing celiac disease – not as a replacement for biopsy or as a measure of disease progression or therapeutic response, FDA representatives noted. Although drug developers need tools to measure therapeutic efficacy in celiac disease, FDA recommended soliciting advice from its Center for Drug Evaluation and Research before testing these tools or kicking off monitoring studies.
The meeting was supported by the Celiac Disease Foundation and Beyond Celiac, and was sponsored by the FDA Center for Drug Evaluation and Research; the American Gastroenterological Association; the American College of Gastroenterology; the American Society for Pediatric Gastroenterology, Hepatology, and Nutrition; and the North American Society for the Study of Celiac Disease. Dr. Leffler disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, INOVA Diagnostics, Coronado Biosciences, Pfizer, and GI Supply. One coauthor and senior author, Dr. Sheila Crowe, disclosed ties to Alvine Pharmaceuticals, Ferring, and Celimmune.
FROM GASTROENTEROLOGY
European Commission’s Proposed Criteria for Endocrine Disruptors Trigger Multiple Concerns
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
European Commission’s proposed criteria for endocrine disruptors trigger multiple concerns
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
The European Commission has proposed regulatory criteria on endocrine-disrupting chemicals that are too strict and so fall short of protecting the public, as they were intended to do, experts contend.
Endocrine-disrupting chemicals cost Europe billions in health care costs each year (Andrology. 2016 Jul;4[4]:565-72).
Published in June, the criteria would require proof that chemicals harm human endocrine health to define them as endocrine-disrupting chemicals (EDCs) – even if data from animal and in vitro studies already suggest so. “Because health effects can take years or even generations to become apparent, this proposal will not protect public health,” the Endocrine Society noted in a sharp formal critique.
Endocrine-disrupting chemicals mimic or block hormones central to brain development, reproduction, metabolism, growth, and other key physiologic processes. The European Union is the largest single economy to regulate EDCs specifically, which more than 1,300 studies have linked to health problems such as infertility, diabetes, obesity, hormone-related cancers, and neurological disorders, the Endocrine Society concluded in a 2015 scientific statement.
Exposure to even low doses of EDCs such as bisphenol A (BPA) can cause adverse effects. But to fulfill the regulatory definition of the European Commission, EDCs would have to meet an even greater burden of proof than carcinogens – a backward step that “defeats the purpose of the regulations – to shield the public from EDCs that pose a threat to human health,” Rémy Slama, PhD, a member of the Society’s European Union Endocrine-Disrupting Chemicals Task Force, stated in an Endocrine Society news release. Of particular concern is the proposal that EDCs must have a single known “mode of action,” which “represents a fundamental misunderstanding of how endocrine signaling works by connecting different organ systems within the body,” said Dr. Slama, senior investigator at Inserm (the National Institute of Health and Medical Research) in Paris.
Deborah M. Kurrasch, PhD, assistant professor and principal investigator at the University of Calgary (Alta.), agreed. The “mode of action” criterion misses the point that EDCs are “messy” compounds that target various proteins and elicit a range of potential cellular responses based on dose, target tissue, and age, she said in an interview. An EDC may lack a single mode of action, or its mode of action may be far harder to pinpoint than its effects on processes such as reproduction, sleep, mood, and growth, she added. “In my opinion, an endocrine-disrupting chemical is one that disrupts the endocrine system. Despite some internal dialogue, the name for this broad and diverse group of chemicals is, and likely will remain, EDCs because the name so accurately describes their one unifying effect – they all perturb normal endocrine function.”
Ultimately, enacting such tight criteria would tie the hands of regulators with regard to newly recognized and even some well-studied EDCs, “despite evidence that they affect endocrine signaling, because their mode of action is not yet known,” Dr. Kurrasch said.
Experts also noted that the EC criteria would keep regulatory bodies from ranking chemicals based on the strength of evidence that they disrupt endocrine function. Instead, the Endocrine Society advocates for a tiered ranking system based on available data. “As the European Parliament and member countries consider whether to implement the European Commission’s criteria, the Society will continue to advocate for criteria that reflect the state of the science,” the organization emphasized.
Dr. Kurrasch is a member of the Endocrine Society and had no other disclosures.
New EULAR gout guidelines garner praise, criticism
The European League Against Rheumatism’s updated recommendations on gout generally resemble those from the American College of Rheumatology, but with several important caveats, two prominent U.S. rheumatologists said in interviews.
First came the praise. “Both ACR and EULAR are sending a consistent message that gout needs more attention and improvement in the quality of care that’s being provided,” said John FitzGerald, MD, PhD, who coauthored the 2012 ACR guidelines and is a professor of medicine and rheumatology at the University of California, Los Angeles.
EULAR also strengthened its advice to start urate-lowering therapy (ULT) early (Ann Rheum Dis. 2016 Jul 25. doi: 10.1136/annrheumdis-2016-209707). This choice reflects “the opinion of many gout experts, that delaying treatment only allows for further accumulation of monosodium urate deposition around the body, which promotes inflammation and tissue destruction and makes it harder to achieve clinical and biologic remission,” said N. Lawrence Edwards, MD, who also helped write the ACR guidelines and is a vice chairman of the department of medicine at the University of Florida, Gainesville.
Finally, EULAR again emphasized treating to a target serum urate level of less than 6.0 mg/dL. “That is definitely consistent with the current recommendations from ACR, and with the way most rheumatologists think,” Dr. FitzGerald said. “The recommendations for future research are also very good and should be commended.”
But several other points depart from the ACR guidance and have prompted critiques.
Allopurinol
Perhaps most strikingly, EULAR now recommends adjusting maximum allopurinol dose based on creatinine clearance if patients have renal impairment. “This modification is very surprising, since [it has] never been shown to affect the incidence of severe allopurinol hypersensitivity reactions,” Dr. Edwards said. “Instead, these antiquated treatment schedules have only added to the epidemic of underdosing of allopurinol by both general practitioners and rheumatologists alike.”
Indeed, requiring clinicians to consider creatinine clearance when using allopurinol in many of their gout patients might push them toward other drugs and their accompanying side effects, “without first trying a slow, safe titration” of allopurinol, Dr. FitzGerald said.
Instead, both he and Dr. Edwards recommended following the gradual allopurinol dose escalation detailed in the 2012 ACR recommendations. “The biggest risk of adverse effects with allopurinol is during the initial treatment period, whereas there is little data about maximum dose,” Dr. FitzGerald emphasized. “I think the starting dose should be 50 mg every day, or even 50 mg every other day – the latter if patients have stage 4 chronic kidney disease.”
Serum urate
EULAR also advises against letting serum urate fall below 3.0 mg/dL “in the long term” – that is, over several years. This guidance stems from reports that hyperuricemia could help prevent neurodegenerative diseases, Dr. Edwards said. But studies have never clearly linked serum urate to neurologic processes, nor have they shown that low serum urate triggers or worsens disease, he added. “The harm of this EULAR recommendation comes from the chilling effect it might have on getting internists and general practitioners to more fully engage in urate lowering in subjects with gout. They could view a therapeutic serum urate window of 3.0 mg/dL to 6.0 mg/dL as too narrow and requiring too much oversight – leading once again to undertreatment.”
Comorbidities
ACR already had recommended ULT for gout patients with chronic kidney disease or urate renoliths, but EULAR expanded this list to include not only renal impairment, but also hypertension, ischemic heart disease, and heart failure, Dr. FitzGerald pointed out. “The recommendation for hypertension was based on a systematic literature review, but hypertension is so prevalent that this additional recommendation really expands the number of patients that would be treated with ULT,” he added. “If it is a patient’s first attack of gout, I think a lot of primary care providers would be uncomfortable starting patients on ULT.”
EULAR and ACR have always diverged in their recommendations about who should receive ULT, and widening these criteria further without direct supporting evidence from a clinical trial will provoke concerns, according to Dr. FitzGerald. “The EULAR authors lay out the logic for it, but without direct evidence it will be controversial, and the risk-benefit ratio of treating this expanded list of patients is unclear.”
Febuxostat
Dr. FitzGerald also recommended starting the xanthine oxidase inhibitor febuxostat (Uloric) at 40 mg, rather than 80 mg as recommended by EULAR. “This is based on a similar logic, that starting lower and titrating up has less risks than starting at a higher dose.”
Dr. Pascal Richette, first author of the updated EULAR recommendations, disclosed fees from Ipsen Pharma/Menarini, AstraZeneca, and Savient. Dr. FitzGerald and Dr. Edwards were coauthors of the 2012 ACR guidelines on gout, part 1 and part 2.
The European League Against Rheumatism’s updated recommendations on gout generally resemble those from the American College of Rheumatology, but with several important caveats, two prominent U.S. rheumatologists said in interviews.
First came the praise. “Both ACR and EULAR are sending a consistent message that gout needs more attention and improvement in the quality of care that’s being provided,” said John FitzGerald, MD, PhD, who coauthored the 2012 ACR guidelines and is a professor of medicine and rheumatology at the University of California, Los Angeles.
EULAR also strengthened its advice to start urate-lowering therapy (ULT) early (Ann Rheum Dis. 2016 Jul 25. doi: 10.1136/annrheumdis-2016-209707). This choice reflects “the opinion of many gout experts, that delaying treatment only allows for further accumulation of monosodium urate deposition around the body, which promotes inflammation and tissue destruction and makes it harder to achieve clinical and biologic remission,” said N. Lawrence Edwards, MD, who also helped write the ACR guidelines and is a vice chairman of the department of medicine at the University of Florida, Gainesville.
Finally, EULAR again emphasized treating to a target serum urate level of less than 6.0 mg/dL. “That is definitely consistent with the current recommendations from ACR, and with the way most rheumatologists think,” Dr. FitzGerald said. “The recommendations for future research are also very good and should be commended.”
But several other points depart from the ACR guidance and have prompted critiques.
Allopurinol
Perhaps most strikingly, EULAR now recommends adjusting maximum allopurinol dose based on creatinine clearance if patients have renal impairment. “This modification is very surprising, since [it has] never been shown to affect the incidence of severe allopurinol hypersensitivity reactions,” Dr. Edwards said. “Instead, these antiquated treatment schedules have only added to the epidemic of underdosing of allopurinol by both general practitioners and rheumatologists alike.”
Indeed, requiring clinicians to consider creatinine clearance when using allopurinol in many of their gout patients might push them toward other drugs and their accompanying side effects, “without first trying a slow, safe titration” of allopurinol, Dr. FitzGerald said.
Instead, both he and Dr. Edwards recommended following the gradual allopurinol dose escalation detailed in the 2012 ACR recommendations. “The biggest risk of adverse effects with allopurinol is during the initial treatment period, whereas there is little data about maximum dose,” Dr. FitzGerald emphasized. “I think the starting dose should be 50 mg every day, or even 50 mg every other day – the latter if patients have stage 4 chronic kidney disease.”
Serum urate
EULAR also advises against letting serum urate fall below 3.0 mg/dL “in the long term” – that is, over several years. This guidance stems from reports that hyperuricemia could help prevent neurodegenerative diseases, Dr. Edwards said. But studies have never clearly linked serum urate to neurologic processes, nor have they shown that low serum urate triggers or worsens disease, he added. “The harm of this EULAR recommendation comes from the chilling effect it might have on getting internists and general practitioners to more fully engage in urate lowering in subjects with gout. They could view a therapeutic serum urate window of 3.0 mg/dL to 6.0 mg/dL as too narrow and requiring too much oversight – leading once again to undertreatment.”
Comorbidities
ACR already had recommended ULT for gout patients with chronic kidney disease or urate renoliths, but EULAR expanded this list to include not only renal impairment, but also hypertension, ischemic heart disease, and heart failure, Dr. FitzGerald pointed out. “The recommendation for hypertension was based on a systematic literature review, but hypertension is so prevalent that this additional recommendation really expands the number of patients that would be treated with ULT,” he added. “If it is a patient’s first attack of gout, I think a lot of primary care providers would be uncomfortable starting patients on ULT.”
EULAR and ACR have always diverged in their recommendations about who should receive ULT, and widening these criteria further without direct supporting evidence from a clinical trial will provoke concerns, according to Dr. FitzGerald. “The EULAR authors lay out the logic for it, but without direct evidence it will be controversial, and the risk-benefit ratio of treating this expanded list of patients is unclear.”
Febuxostat
Dr. FitzGerald also recommended starting the xanthine oxidase inhibitor febuxostat (Uloric) at 40 mg, rather than 80 mg as recommended by EULAR. “This is based on a similar logic, that starting lower and titrating up has less risks than starting at a higher dose.”
Dr. Pascal Richette, first author of the updated EULAR recommendations, disclosed fees from Ipsen Pharma/Menarini, AstraZeneca, and Savient. Dr. FitzGerald and Dr. Edwards were coauthors of the 2012 ACR guidelines on gout, part 1 and part 2.
The European League Against Rheumatism’s updated recommendations on gout generally resemble those from the American College of Rheumatology, but with several important caveats, two prominent U.S. rheumatologists said in interviews.
First came the praise. “Both ACR and EULAR are sending a consistent message that gout needs more attention and improvement in the quality of care that’s being provided,” said John FitzGerald, MD, PhD, who coauthored the 2012 ACR guidelines and is a professor of medicine and rheumatology at the University of California, Los Angeles.
EULAR also strengthened its advice to start urate-lowering therapy (ULT) early (Ann Rheum Dis. 2016 Jul 25. doi: 10.1136/annrheumdis-2016-209707). This choice reflects “the opinion of many gout experts, that delaying treatment only allows for further accumulation of monosodium urate deposition around the body, which promotes inflammation and tissue destruction and makes it harder to achieve clinical and biologic remission,” said N. Lawrence Edwards, MD, who also helped write the ACR guidelines and is a vice chairman of the department of medicine at the University of Florida, Gainesville.
Finally, EULAR again emphasized treating to a target serum urate level of less than 6.0 mg/dL. “That is definitely consistent with the current recommendations from ACR, and with the way most rheumatologists think,” Dr. FitzGerald said. “The recommendations for future research are also very good and should be commended.”
But several other points depart from the ACR guidance and have prompted critiques.
Allopurinol
Perhaps most strikingly, EULAR now recommends adjusting maximum allopurinol dose based on creatinine clearance if patients have renal impairment. “This modification is very surprising, since [it has] never been shown to affect the incidence of severe allopurinol hypersensitivity reactions,” Dr. Edwards said. “Instead, these antiquated treatment schedules have only added to the epidemic of underdosing of allopurinol by both general practitioners and rheumatologists alike.”
Indeed, requiring clinicians to consider creatinine clearance when using allopurinol in many of their gout patients might push them toward other drugs and their accompanying side effects, “without first trying a slow, safe titration” of allopurinol, Dr. FitzGerald said.
Instead, both he and Dr. Edwards recommended following the gradual allopurinol dose escalation detailed in the 2012 ACR recommendations. “The biggest risk of adverse effects with allopurinol is during the initial treatment period, whereas there is little data about maximum dose,” Dr. FitzGerald emphasized. “I think the starting dose should be 50 mg every day, or even 50 mg every other day – the latter if patients have stage 4 chronic kidney disease.”
Serum urate
EULAR also advises against letting serum urate fall below 3.0 mg/dL “in the long term” – that is, over several years. This guidance stems from reports that hyperuricemia could help prevent neurodegenerative diseases, Dr. Edwards said. But studies have never clearly linked serum urate to neurologic processes, nor have they shown that low serum urate triggers or worsens disease, he added. “The harm of this EULAR recommendation comes from the chilling effect it might have on getting internists and general practitioners to more fully engage in urate lowering in subjects with gout. They could view a therapeutic serum urate window of 3.0 mg/dL to 6.0 mg/dL as too narrow and requiring too much oversight – leading once again to undertreatment.”
Comorbidities
ACR already had recommended ULT for gout patients with chronic kidney disease or urate renoliths, but EULAR expanded this list to include not only renal impairment, but also hypertension, ischemic heart disease, and heart failure, Dr. FitzGerald pointed out. “The recommendation for hypertension was based on a systematic literature review, but hypertension is so prevalent that this additional recommendation really expands the number of patients that would be treated with ULT,” he added. “If it is a patient’s first attack of gout, I think a lot of primary care providers would be uncomfortable starting patients on ULT.”
EULAR and ACR have always diverged in their recommendations about who should receive ULT, and widening these criteria further without direct supporting evidence from a clinical trial will provoke concerns, according to Dr. FitzGerald. “The EULAR authors lay out the logic for it, but without direct evidence it will be controversial, and the risk-benefit ratio of treating this expanded list of patients is unclear.”
Febuxostat
Dr. FitzGerald also recommended starting the xanthine oxidase inhibitor febuxostat (Uloric) at 40 mg, rather than 80 mg as recommended by EULAR. “This is based on a similar logic, that starting lower and titrating up has less risks than starting at a higher dose.”
Dr. Pascal Richette, first author of the updated EULAR recommendations, disclosed fees from Ipsen Pharma/Menarini, AstraZeneca, and Savient. Dr. FitzGerald and Dr. Edwards were coauthors of the 2012 ACR guidelines on gout, part 1 and part 2.
FROM ANNALS OF THE RHEUMATIC DISEASES
Studies highlight diagnostic and treatment challenges in hidradenitis suppurativa
SCOTTSDALE, ARIZ. – Patients with hidradenitis suppurativa (HS) may be misdiagnosed when they see providers who are not dermatologists – as is usually the case during the initial years of their disease, according to a large analysis of medical claims data.
The findings highlight the need for visual diagnostic aids and specific guidelines for treating HS that target nondermatologists, Melissa Butt, MPH, of Penn State Hershey (Pa.) Medical Center, said during an interview at the annual meeting of the Society for Investigative Dermatology. She presented the findings during a poster session at the meeting.
HS is a chronic inflammatory disease of the hair follicles that affects 0.5%-4% of people in the United States. In past studies, up to 12 years elapsed between disease onset and diagnosis, in part because patients often cannot readily access dermatologists, Ms. Butt said. To better understand patterns of health care use during the years leading up to HS diagnosis, she and her colleagues used MarketScan data to identify 1,733 patients with HS-specific medical care claims filed in 2012 and 2013. Then they looked back at medical claims for these patients during 2008 through 2011, before the patients were diagnosed with HS. The cohort averaged 37 years of age (standard deviation, 15 years), and 73% were female.
Among 239,892 claims filed before patients were diagnosed with HS, 11,381 (4.7%) included codes for other diseases of the skin and subcutaneous tissues, Ms. Butt said. Dermatologists filed only 31% of these skin-specific claims, while 69% were filed by other providers, such as family practitioners, internists, emergency department physicians, and acute care hospitalists.
Notably, about two-thirds of the skin-specific diagnostic codes could have represented a misdiagnosis of HS. These codes included conditions such as abscesses, carbuncles, local infections, ulcers, and diseases of the sebaceous glands.
The fact that 78% of visits occurred in offices and other outpatient settings further underscores the need to improve the detection and care of HS in these environments, Ms. Butt said. Given current national shortages of dermatologists, visual HS diagnostic aids and “detailed, multistep clinical practice guidelines” for nondermatologists could help improve care of HS while patients wait to see the specialists, she added.
A second poster presented at the meeting provided results of a study on the use and impact of antibiotics in the treatment of HS. Alexander Fischer of Johns Hopkins University, Baltimore, and his associates studied antibiotic prescriptions and bacterial cultures from the lesions of 239 patients with HS who were treated at Johns Hopkins medical facilities between 2010 and 2015. Not only were 51% of HS patients on antibiotics at the time of culture, but these patients’ lesions were significantly more likely to contain antibiotic-resistant bacteria than were those of patients not on antibiotics.
Strikingly, Proteus species were isolated from nearly half of patients on trimethoprim-sulfamethoxazole (TMP/SMX), and 88% of colonies were resistant to TMP/SMX, while only 13% of cultures from untreated patients grew Proteus (P less than .001) and all were TMP/SMX-susceptible (P less than .001). Likewise, 100% of methicillin-resistant Staphylococcus aureus (MRSA) strains from patients prescribed ciprofloxacin were resistant to it, compared with a 10% background rate of ciprofloxacin resistance among MRSA from patients not taking antibiotics (P = .04). In addition, the proportion of other S. aureus strains that were clindamycin-resistant was higher when patients were taking this antibiotic than when they were not (63% versus 17%; P = .03).
The results “raise questions” about whether antibiotics should be used in HS patients who are not clearly benefiting from them, according to the researchers.
The authors of both studies reported no funding sources and had no disclosures.
SCOTTSDALE, ARIZ. – Patients with hidradenitis suppurativa (HS) may be misdiagnosed when they see providers who are not dermatologists – as is usually the case during the initial years of their disease, according to a large analysis of medical claims data.
The findings highlight the need for visual diagnostic aids and specific guidelines for treating HS that target nondermatologists, Melissa Butt, MPH, of Penn State Hershey (Pa.) Medical Center, said during an interview at the annual meeting of the Society for Investigative Dermatology. She presented the findings during a poster session at the meeting.
HS is a chronic inflammatory disease of the hair follicles that affects 0.5%-4% of people in the United States. In past studies, up to 12 years elapsed between disease onset and diagnosis, in part because patients often cannot readily access dermatologists, Ms. Butt said. To better understand patterns of health care use during the years leading up to HS diagnosis, she and her colleagues used MarketScan data to identify 1,733 patients with HS-specific medical care claims filed in 2012 and 2013. Then they looked back at medical claims for these patients during 2008 through 2011, before the patients were diagnosed with HS. The cohort averaged 37 years of age (standard deviation, 15 years), and 73% were female.
Among 239,892 claims filed before patients were diagnosed with HS, 11,381 (4.7%) included codes for other diseases of the skin and subcutaneous tissues, Ms. Butt said. Dermatologists filed only 31% of these skin-specific claims, while 69% were filed by other providers, such as family practitioners, internists, emergency department physicians, and acute care hospitalists.
Notably, about two-thirds of the skin-specific diagnostic codes could have represented a misdiagnosis of HS. These codes included conditions such as abscesses, carbuncles, local infections, ulcers, and diseases of the sebaceous glands.
The fact that 78% of visits occurred in offices and other outpatient settings further underscores the need to improve the detection and care of HS in these environments, Ms. Butt said. Given current national shortages of dermatologists, visual HS diagnostic aids and “detailed, multistep clinical practice guidelines” for nondermatologists could help improve care of HS while patients wait to see the specialists, she added.
A second poster presented at the meeting provided results of a study on the use and impact of antibiotics in the treatment of HS. Alexander Fischer of Johns Hopkins University, Baltimore, and his associates studied antibiotic prescriptions and bacterial cultures from the lesions of 239 patients with HS who were treated at Johns Hopkins medical facilities between 2010 and 2015. Not only were 51% of HS patients on antibiotics at the time of culture, but these patients’ lesions were significantly more likely to contain antibiotic-resistant bacteria than were those of patients not on antibiotics.
Strikingly, Proteus species were isolated from nearly half of patients on trimethoprim-sulfamethoxazole (TMP/SMX), and 88% of colonies were resistant to TMP/SMX, while only 13% of cultures from untreated patients grew Proteus (P less than .001) and all were TMP/SMX-susceptible (P less than .001). Likewise, 100% of methicillin-resistant Staphylococcus aureus (MRSA) strains from patients prescribed ciprofloxacin were resistant to it, compared with a 10% background rate of ciprofloxacin resistance among MRSA from patients not taking antibiotics (P = .04). In addition, the proportion of other S. aureus strains that were clindamycin-resistant was higher when patients were taking this antibiotic than when they were not (63% versus 17%; P = .03).
The results “raise questions” about whether antibiotics should be used in HS patients who are not clearly benefiting from them, according to the researchers.
The authors of both studies reported no funding sources and had no disclosures.
SCOTTSDALE, ARIZ. – Patients with hidradenitis suppurativa (HS) may be misdiagnosed when they see providers who are not dermatologists – as is usually the case during the initial years of their disease, according to a large analysis of medical claims data.
The findings highlight the need for visual diagnostic aids and specific guidelines for treating HS that target nondermatologists, Melissa Butt, MPH, of Penn State Hershey (Pa.) Medical Center, said during an interview at the annual meeting of the Society for Investigative Dermatology. She presented the findings during a poster session at the meeting.
HS is a chronic inflammatory disease of the hair follicles that affects 0.5%-4% of people in the United States. In past studies, up to 12 years elapsed between disease onset and diagnosis, in part because patients often cannot readily access dermatologists, Ms. Butt said. To better understand patterns of health care use during the years leading up to HS diagnosis, she and her colleagues used MarketScan data to identify 1,733 patients with HS-specific medical care claims filed in 2012 and 2013. Then they looked back at medical claims for these patients during 2008 through 2011, before the patients were diagnosed with HS. The cohort averaged 37 years of age (standard deviation, 15 years), and 73% were female.
Among 239,892 claims filed before patients were diagnosed with HS, 11,381 (4.7%) included codes for other diseases of the skin and subcutaneous tissues, Ms. Butt said. Dermatologists filed only 31% of these skin-specific claims, while 69% were filed by other providers, such as family practitioners, internists, emergency department physicians, and acute care hospitalists.
Notably, about two-thirds of the skin-specific diagnostic codes could have represented a misdiagnosis of HS. These codes included conditions such as abscesses, carbuncles, local infections, ulcers, and diseases of the sebaceous glands.
The fact that 78% of visits occurred in offices and other outpatient settings further underscores the need to improve the detection and care of HS in these environments, Ms. Butt said. Given current national shortages of dermatologists, visual HS diagnostic aids and “detailed, multistep clinical practice guidelines” for nondermatologists could help improve care of HS while patients wait to see the specialists, she added.
A second poster presented at the meeting provided results of a study on the use and impact of antibiotics in the treatment of HS. Alexander Fischer of Johns Hopkins University, Baltimore, and his associates studied antibiotic prescriptions and bacterial cultures from the lesions of 239 patients with HS who were treated at Johns Hopkins medical facilities between 2010 and 2015. Not only were 51% of HS patients on antibiotics at the time of culture, but these patients’ lesions were significantly more likely to contain antibiotic-resistant bacteria than were those of patients not on antibiotics.
Strikingly, Proteus species were isolated from nearly half of patients on trimethoprim-sulfamethoxazole (TMP/SMX), and 88% of colonies were resistant to TMP/SMX, while only 13% of cultures from untreated patients grew Proteus (P less than .001) and all were TMP/SMX-susceptible (P less than .001). Likewise, 100% of methicillin-resistant Staphylococcus aureus (MRSA) strains from patients prescribed ciprofloxacin were resistant to it, compared with a 10% background rate of ciprofloxacin resistance among MRSA from patients not taking antibiotics (P = .04). In addition, the proportion of other S. aureus strains that were clindamycin-resistant was higher when patients were taking this antibiotic than when they were not (63% versus 17%; P = .03).
The results “raise questions” about whether antibiotics should be used in HS patients who are not clearly benefiting from them, according to the researchers.
The authors of both studies reported no funding sources and had no disclosures.
AT THE 2016 SID ANNUAL MEETING
Key clinical point: Two studies underscored current challenges in diagnosing and treating hidradenitis suppurativa (HS).
Major finding: HS was usually diagnosed in outpatient settings by nondermatologists who often initially filed claims for carbuncles, ulcers, and other conditions that are confused with HS. In a separate study, antibiotic-resistant bacteria were significantly more prevalent in the lesions of HS patients who were receiving antibiotics than in patients who were not taking antibiotics.
Data source: A medical claims analysis of 1,733 patients with HS, and a study of antibiotic prescriptions and bacterial cultures from 239 patients with HS.
Disclosures: The authors of both studies reported no funding sources and had no disclosures.
Serum Vitamin D Levels, Atopy Not Significantly Linked
SCOTTSDALE, ARIZ. – Serum vitamin D level was not significantly associated with atopic dermatitis or disease severity in a single-center study of more than 600 children and adolescents.
However, “we did observe a strong correlation between average serum vitamin D levels and skin type, as well as body mass index,” said Kavita Darji, a medical student at Saint Louis (Mo.) University, who presented the findings in a poster at the annual meeting of the Society for Investigative Dermatology. Those findings challenge the logic of following universal definitions of vitamin D deficiency, especially given the phenotypic heterogeneity of patients in the United States, she added in an interview.
Serum vitamin D testing is one of most common laboratory assays in this country, but clinicians still debate the risks and benefits of supplementing children and adolescents who test below the Endocrine Society’s threshold for sufficiency (30.0 ng/mL).
To identify factors affecting vitamin D levels, Ms. Darji and her associates reviewed electronic medical charts for patients under age 22 years at Saint Louis University medical centers between 2009 and 2014. The cohort of 655 patients was primarily white (64%) or black (29%), and was nearly equally balanced by gender; their average age was 10 years. The researchers analyzed only the first vitamin D serum measurement for each patient, and defined deficiency as a level under 20 ng/mL, insufficiency as a level between 20 and 29.9 ng/mL, and sufficiency as a level of at least 30 ng/mL.
Serum vitamin D levels were slightly lower among atopic patients, compared with those without atopy, but the difference did not reach statistical significance (about 25 ng/mL vs. about 38 ng/mL; P greater than .05). “We also did not find an association between AD severity and vitamin D level,” Ms. Darji reported. Instead, race and body mass index were the most significant predictors of vitamin D deficiency, probably because these factors directly affect cutaneous photo-induced vitamin D synthesis and the sequestration of fat-soluble vitamins in adipose tissue, she said.
Using the standard definitions, more than 50% of black patients were vitamin D deficient, while less than 30% had sufficient vitamin D levels. In contrast, about 25% of white patients were vitamin D deficient, while nearly 40% had sufficient vitamin D levels (P less than .0001 for proportions of deficiency by race). Furthermore, only about 10% of obese children (those who exceeded the 99th percentile of BMI for age) had sufficient vitamin D levels, compared with more than 40% of underweight children and about 30% of normal-weight children (P less than .00001).
Since vitamin D deficiency was more common among black and obese patients, “maybe they could benefit from a different cut-off value than the standard 30 ng per mL that we used,” Ms. Darji said. “The question is, do they really require these supplements? It may be beneficial to look at the unique characteristics of each patient before supplementing, because the risks of supplementation are considerable in terms of bone health and cardiovascular disease.”
Vitamin D levels did not vary significantly by gender or by month or season measured, Ms. Darji noted. She reported no funding sources and had no disclosures.
SCOTTSDALE, ARIZ. – Serum vitamin D level was not significantly associated with atopic dermatitis or disease severity in a single-center study of more than 600 children and adolescents.
However, “we did observe a strong correlation between average serum vitamin D levels and skin type, as well as body mass index,” said Kavita Darji, a medical student at Saint Louis (Mo.) University, who presented the findings in a poster at the annual meeting of the Society for Investigative Dermatology. Those findings challenge the logic of following universal definitions of vitamin D deficiency, especially given the phenotypic heterogeneity of patients in the United States, she added in an interview.
Serum vitamin D testing is one of most common laboratory assays in this country, but clinicians still debate the risks and benefits of supplementing children and adolescents who test below the Endocrine Society’s threshold for sufficiency (30.0 ng/mL).
To identify factors affecting vitamin D levels, Ms. Darji and her associates reviewed electronic medical charts for patients under age 22 years at Saint Louis University medical centers between 2009 and 2014. The cohort of 655 patients was primarily white (64%) or black (29%), and was nearly equally balanced by gender; their average age was 10 years. The researchers analyzed only the first vitamin D serum measurement for each patient, and defined deficiency as a level under 20 ng/mL, insufficiency as a level between 20 and 29.9 ng/mL, and sufficiency as a level of at least 30 ng/mL.
Serum vitamin D levels were slightly lower among atopic patients, compared with those without atopy, but the difference did not reach statistical significance (about 25 ng/mL vs. about 38 ng/mL; P greater than .05). “We also did not find an association between AD severity and vitamin D level,” Ms. Darji reported. Instead, race and body mass index were the most significant predictors of vitamin D deficiency, probably because these factors directly affect cutaneous photo-induced vitamin D synthesis and the sequestration of fat-soluble vitamins in adipose tissue, she said.
Using the standard definitions, more than 50% of black patients were vitamin D deficient, while less than 30% had sufficient vitamin D levels. In contrast, about 25% of white patients were vitamin D deficient, while nearly 40% had sufficient vitamin D levels (P less than .0001 for proportions of deficiency by race). Furthermore, only about 10% of obese children (those who exceeded the 99th percentile of BMI for age) had sufficient vitamin D levels, compared with more than 40% of underweight children and about 30% of normal-weight children (P less than .00001).
Since vitamin D deficiency was more common among black and obese patients, “maybe they could benefit from a different cut-off value than the standard 30 ng per mL that we used,” Ms. Darji said. “The question is, do they really require these supplements? It may be beneficial to look at the unique characteristics of each patient before supplementing, because the risks of supplementation are considerable in terms of bone health and cardiovascular disease.”
Vitamin D levels did not vary significantly by gender or by month or season measured, Ms. Darji noted. She reported no funding sources and had no disclosures.
SCOTTSDALE, ARIZ. – Serum vitamin D level was not significantly associated with atopic dermatitis or disease severity in a single-center study of more than 600 children and adolescents.
However, “we did observe a strong correlation between average serum vitamin D levels and skin type, as well as body mass index,” said Kavita Darji, a medical student at Saint Louis (Mo.) University, who presented the findings in a poster at the annual meeting of the Society for Investigative Dermatology. Those findings challenge the logic of following universal definitions of vitamin D deficiency, especially given the phenotypic heterogeneity of patients in the United States, she added in an interview.
Serum vitamin D testing is one of most common laboratory assays in this country, but clinicians still debate the risks and benefits of supplementing children and adolescents who test below the Endocrine Society’s threshold for sufficiency (30.0 ng/mL).
To identify factors affecting vitamin D levels, Ms. Darji and her associates reviewed electronic medical charts for patients under age 22 years at Saint Louis University medical centers between 2009 and 2014. The cohort of 655 patients was primarily white (64%) or black (29%), and was nearly equally balanced by gender; their average age was 10 years. The researchers analyzed only the first vitamin D serum measurement for each patient, and defined deficiency as a level under 20 ng/mL, insufficiency as a level between 20 and 29.9 ng/mL, and sufficiency as a level of at least 30 ng/mL.
Serum vitamin D levels were slightly lower among atopic patients, compared with those without atopy, but the difference did not reach statistical significance (about 25 ng/mL vs. about 38 ng/mL; P greater than .05). “We also did not find an association between AD severity and vitamin D level,” Ms. Darji reported. Instead, race and body mass index were the most significant predictors of vitamin D deficiency, probably because these factors directly affect cutaneous photo-induced vitamin D synthesis and the sequestration of fat-soluble vitamins in adipose tissue, she said.
Using the standard definitions, more than 50% of black patients were vitamin D deficient, while less than 30% had sufficient vitamin D levels. In contrast, about 25% of white patients were vitamin D deficient, while nearly 40% had sufficient vitamin D levels (P less than .0001 for proportions of deficiency by race). Furthermore, only about 10% of obese children (those who exceeded the 99th percentile of BMI for age) had sufficient vitamin D levels, compared with more than 40% of underweight children and about 30% of normal-weight children (P less than .00001).
Since vitamin D deficiency was more common among black and obese patients, “maybe they could benefit from a different cut-off value than the standard 30 ng per mL that we used,” Ms. Darji said. “The question is, do they really require these supplements? It may be beneficial to look at the unique characteristics of each patient before supplementing, because the risks of supplementation are considerable in terms of bone health and cardiovascular disease.”
Vitamin D levels did not vary significantly by gender or by month or season measured, Ms. Darji noted. She reported no funding sources and had no disclosures.
AT THE 2016 SID ANNUAL MEETING