User login
PET-CT better predicted follicular lymphoma survival
F-18 positron emission tomography combined with low-dose computed tomography was more effective than conventional CT or the Follicular Lymphoma International Prognostic Index for predicting treatment response in patients with advanced follicular lymphoma, authors of a pooled analysis reported online in the Lancet Haemotology.
“Although these results are reassuring for patients who have a negative PET [positron emission tomography] scan, those who have a positive PET scan after first-line therapy can no longer be regarded as having an indolent disease and should be closely monitored,” wrote Dr. Judith Trotman at the University of Sydney, Australia, and her associates.
Follicular lymphoma often recurs after treatment, but predicting early relapsers has been a challenge, the investigators noted. They performed a masked review of three prospective, multicenter studies of 246 patients with follicular lymphoma, finding that patients with negative postinduction PET-CT scans (scores of less than four on the five-point Deauville scale) had median progression-free survival (PFS) of more than 6 years, compared with a median PFS of only 16.9 months for PET-positive patients (P = .0001). The markedly shorter PFS occurred even though most patients received anthracycline (CHOP/FM), the researchers said (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/ S2352-3026(14)70008-0]).
Four years after induction, 63.4% of PET-negative patients were progression free, compared with only 23.2% of PET-positive patients (P less than .0001), the investigators added. And 4-year overall survival in PET-negative patients also was significantly higher than in PET-negative patients (97.1% vs. 87.2%; P less than .0001), they reported.PET status also was “much stronger” than the Follicular Lymphoma International Prognostic Index, FLIPI2, or contrast-enhanced CT for predicting outcomes in conventional responders, Dr. Trotman and her associates said. Conventional CT response only weakly predicted progression-free survival (P = .017), while a FLIPI2 score of 3-5 predicted progression-free survival (P = .011) but not overall survival. For this reason, responders historically have faced “an uncertain remission” and need close clinical follow-up, they pointed out.
The study was funded by the Lymphoma Study Association, Direction de la Recherche Clinique de l’Assistance Publique–Hôpitaux de Paris, Fondazione Italiana Linfomi, and the Italian Ministry of Health. Dr. Trotman reported uncompensated advisory relationships with Roche and Janssen, and three of 18 coauthors reported financial relationships with Merck, Celgene, Roche, Takeda, Janssen, and Spectrum. The rest reported having no conflicts of interest.
That patient outcome can be predicted with molecular imaging is good news: The question is, what should be done with this information? In clinical practice, patients with a positive scan could be followed up more closely. No data yet show that intervention with treatment after a positive PET result in patients with follicular lymphoma will improve outcome.
The results from Dr. Trotman and her colleagues might lead to several clinical research opportunities. One such possibility would be to assess if an early reaction to the PET scan result improves patient outcome. Thus, patients with a positive PET scan after induction therapy could be randomly assigned to either deferred treatment until disease progression or immediate intervention. A preferable alternative would be to introduce a unique agent at that time, such as the newly developed small molecules (including idelalisib, ibrutinib, or ABT-199) in a novel combination.
The most crucial need is to identify biomarkers that distinguish this group of patients from those whose PET scans become negative. Once that goal is achieved, that information could be used to develop new, targeted induction regimens that improve initial treatment of the disease and, as a result, increase the number of patients with negative PET scans.
Dr. Bruce Cheson is professor of medicine and director of hematology research at Georgetown University Hospital, Washington. He reported research funding from Pharmacyclics, Gilead, Celgene, Roche-Genentech, and AbbVie, and paid consulting relationships with Pharmacyclics, Seattle Genetics, Gilead, Celgene, Roche-Genentech, Spectrum, and Mundipharma. These remarks are taken from his accompanying editorial (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/S2352-3026(14)70015-8]).
That patient outcome can be predicted with molecular imaging is good news: The question is, what should be done with this information? In clinical practice, patients with a positive scan could be followed up more closely. No data yet show that intervention with treatment after a positive PET result in patients with follicular lymphoma will improve outcome.
The results from Dr. Trotman and her colleagues might lead to several clinical research opportunities. One such possibility would be to assess if an early reaction to the PET scan result improves patient outcome. Thus, patients with a positive PET scan after induction therapy could be randomly assigned to either deferred treatment until disease progression or immediate intervention. A preferable alternative would be to introduce a unique agent at that time, such as the newly developed small molecules (including idelalisib, ibrutinib, or ABT-199) in a novel combination.
The most crucial need is to identify biomarkers that distinguish this group of patients from those whose PET scans become negative. Once that goal is achieved, that information could be used to develop new, targeted induction regimens that improve initial treatment of the disease and, as a result, increase the number of patients with negative PET scans.
Dr. Bruce Cheson is professor of medicine and director of hematology research at Georgetown University Hospital, Washington. He reported research funding from Pharmacyclics, Gilead, Celgene, Roche-Genentech, and AbbVie, and paid consulting relationships with Pharmacyclics, Seattle Genetics, Gilead, Celgene, Roche-Genentech, Spectrum, and Mundipharma. These remarks are taken from his accompanying editorial (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/S2352-3026(14)70015-8]).
That patient outcome can be predicted with molecular imaging is good news: The question is, what should be done with this information? In clinical practice, patients with a positive scan could be followed up more closely. No data yet show that intervention with treatment after a positive PET result in patients with follicular lymphoma will improve outcome.
The results from Dr. Trotman and her colleagues might lead to several clinical research opportunities. One such possibility would be to assess if an early reaction to the PET scan result improves patient outcome. Thus, patients with a positive PET scan after induction therapy could be randomly assigned to either deferred treatment until disease progression or immediate intervention. A preferable alternative would be to introduce a unique agent at that time, such as the newly developed small molecules (including idelalisib, ibrutinib, or ABT-199) in a novel combination.
The most crucial need is to identify biomarkers that distinguish this group of patients from those whose PET scans become negative. Once that goal is achieved, that information could be used to develop new, targeted induction regimens that improve initial treatment of the disease and, as a result, increase the number of patients with negative PET scans.
Dr. Bruce Cheson is professor of medicine and director of hematology research at Georgetown University Hospital, Washington. He reported research funding from Pharmacyclics, Gilead, Celgene, Roche-Genentech, and AbbVie, and paid consulting relationships with Pharmacyclics, Seattle Genetics, Gilead, Celgene, Roche-Genentech, Spectrum, and Mundipharma. These remarks are taken from his accompanying editorial (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/S2352-3026(14)70015-8]).
F-18 positron emission tomography combined with low-dose computed tomography was more effective than conventional CT or the Follicular Lymphoma International Prognostic Index for predicting treatment response in patients with advanced follicular lymphoma, authors of a pooled analysis reported online in the Lancet Haemotology.
“Although these results are reassuring for patients who have a negative PET [positron emission tomography] scan, those who have a positive PET scan after first-line therapy can no longer be regarded as having an indolent disease and should be closely monitored,” wrote Dr. Judith Trotman at the University of Sydney, Australia, and her associates.
Follicular lymphoma often recurs after treatment, but predicting early relapsers has been a challenge, the investigators noted. They performed a masked review of three prospective, multicenter studies of 246 patients with follicular lymphoma, finding that patients with negative postinduction PET-CT scans (scores of less than four on the five-point Deauville scale) had median progression-free survival (PFS) of more than 6 years, compared with a median PFS of only 16.9 months for PET-positive patients (P = .0001). The markedly shorter PFS occurred even though most patients received anthracycline (CHOP/FM), the researchers said (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/ S2352-3026(14)70008-0]).
Four years after induction, 63.4% of PET-negative patients were progression free, compared with only 23.2% of PET-positive patients (P less than .0001), the investigators added. And 4-year overall survival in PET-negative patients also was significantly higher than in PET-negative patients (97.1% vs. 87.2%; P less than .0001), they reported.PET status also was “much stronger” than the Follicular Lymphoma International Prognostic Index, FLIPI2, or contrast-enhanced CT for predicting outcomes in conventional responders, Dr. Trotman and her associates said. Conventional CT response only weakly predicted progression-free survival (P = .017), while a FLIPI2 score of 3-5 predicted progression-free survival (P = .011) but not overall survival. For this reason, responders historically have faced “an uncertain remission” and need close clinical follow-up, they pointed out.
The study was funded by the Lymphoma Study Association, Direction de la Recherche Clinique de l’Assistance Publique–Hôpitaux de Paris, Fondazione Italiana Linfomi, and the Italian Ministry of Health. Dr. Trotman reported uncompensated advisory relationships with Roche and Janssen, and three of 18 coauthors reported financial relationships with Merck, Celgene, Roche, Takeda, Janssen, and Spectrum. The rest reported having no conflicts of interest.
F-18 positron emission tomography combined with low-dose computed tomography was more effective than conventional CT or the Follicular Lymphoma International Prognostic Index for predicting treatment response in patients with advanced follicular lymphoma, authors of a pooled analysis reported online in the Lancet Haemotology.
“Although these results are reassuring for patients who have a negative PET [positron emission tomography] scan, those who have a positive PET scan after first-line therapy can no longer be regarded as having an indolent disease and should be closely monitored,” wrote Dr. Judith Trotman at the University of Sydney, Australia, and her associates.
Follicular lymphoma often recurs after treatment, but predicting early relapsers has been a challenge, the investigators noted. They performed a masked review of three prospective, multicenter studies of 246 patients with follicular lymphoma, finding that patients with negative postinduction PET-CT scans (scores of less than four on the five-point Deauville scale) had median progression-free survival (PFS) of more than 6 years, compared with a median PFS of only 16.9 months for PET-positive patients (P = .0001). The markedly shorter PFS occurred even though most patients received anthracycline (CHOP/FM), the researchers said (Lancet Haematol. 2014 Sept. 18 [doi:10.1016/ S2352-3026(14)70008-0]).
Four years after induction, 63.4% of PET-negative patients were progression free, compared with only 23.2% of PET-positive patients (P less than .0001), the investigators added. And 4-year overall survival in PET-negative patients also was significantly higher than in PET-negative patients (97.1% vs. 87.2%; P less than .0001), they reported.PET status also was “much stronger” than the Follicular Lymphoma International Prognostic Index, FLIPI2, or contrast-enhanced CT for predicting outcomes in conventional responders, Dr. Trotman and her associates said. Conventional CT response only weakly predicted progression-free survival (P = .017), while a FLIPI2 score of 3-5 predicted progression-free survival (P = .011) but not overall survival. For this reason, responders historically have faced “an uncertain remission” and need close clinical follow-up, they pointed out.
The study was funded by the Lymphoma Study Association, Direction de la Recherche Clinique de l’Assistance Publique–Hôpitaux de Paris, Fondazione Italiana Linfomi, and the Italian Ministry of Health. Dr. Trotman reported uncompensated advisory relationships with Roche and Janssen, and three of 18 coauthors reported financial relationships with Merck, Celgene, Roche, Takeda, Janssen, and Spectrum. The rest reported having no conflicts of interest.
Key clinical point: In patients with follicular lymphoma, PET-CT was better than conventional CT for assessing response and survival after first-line chemoimmunotherapy.
Major finding: Patients with positive postinduction PET scans were significantly less likely to be progression free at 4 years, compared with PET-negative patients (23.2% vs. 63.4%, P less than .0001), and had significantly lower 4-year overall survival (87.2% vs. 97.1%; P less than .0001).
Data source: Masked review of three multicenter prospective studies of 246 patients with follicular lymphoma who underwent postinduction PET-CT according to the five-point Deauville scale.
Disclosures: The study was funded by the Lymphoma Study Association, Direction de la Recherche Clinique de l’Assistance Publique–Hôpitaux de Paris, Fondazione Italiana Linfomi, and the Italian Ministry of Health. Dr. Trotman reported uncompensated advisory relationships with Roche and Janssen, and three of 18 coauthors reported financial relationships with Merck, Celgene, Roche, Takeda, Janssen, and Spectrum. The rest reported having no conflicts of interest.
Laparoscopic resection improved short-term outcomes in patients with cirrhotic liver cancer
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resection had fewer complications, shorter hospital stays, no port site recurrences, and no significant difference in survival, compared with patients who had open resections, according to a single-center, 10-year study published online in the Journal of the American College of Surgeons.
The study is the first to report long-term favorable results of laparoscopic hepatic resection for liver cancer in patients with cirrhosis, said Dr. Yo-ichi Yamashita and associates at Kyushu University, Fukuoka, Japan. Based on the data, laparoscopic instead of open resection should be considered for patients with cirrhosis whose hepatocellular carcinomas fall within the Milan criteria, the investigators said (J. Am. Coll. Surg. 2014 Sept. 9 [doi: 10.1016/j.jamcollsurg.2014.09.003]).
The retrospective study included 162 patients with cirrhosis and hepatocellular carcinoma within the Milan criteria. In all, 99 patients had open hepatic resections, while 63 underwent laparoscopic resections, the investigators said. Only 10% of laparoscopy patients had complications of grade 2 or higher, compared with 26% of open surgery cases (P = .0459), they reported. And while 7% of the open surgery patients developed ascites after surgery, none of the laparoscopy patients did (P = .0077), possibly because they experienced less tissue damage and because the deliberate induction of carbon dioxide pneumoperitoneum during laparoscopy can reduce local inflammatory responses, the researchers said. Laparoscopy patients also averaged 6 fewer days in the hospital after their procedures, Dr. Yamashita and associates reported (median length of stay, 10 vs. 16 days; P = .0008).
The laparoscopy group had no port site recurrences or peritoneal seeding of hepatocellular carcinoma, the investigators noted. Rates of disease-free and overall survival were similar between the two groups (P = .5196 and P = .6791, respectively), they added. Five-year and 10-year overall survival rates were 78% and 69% for laparoscopy patients, and were 77% and 57% for open resection patients, they said.
The authors disclosed no funding sources and reported having no conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Patients with liver cancer and cirrhosis who underwent laparoscopic hepatic resections had lower postoperative morbidity and shorter hospital stays than patients who had open resections.
Major finding: Laparoscopy patients had significantly less postoperative morbidity (10% vs. 26%; P = .0459) and shorter hospital stays (10 vs. 16 days; P = .0008), compared with patients who underwent open resection, with no port site recurrences and no significant differences in long-term survival.
Data source:Retrospective, single-center study of 162 patients with cirrhosis and primary hepatocellular carcinoma who underwent curative hepatic resections, of whom 99 underwent open procedures and 63 underwent laparoscopies.
Disclosures: The authors disclosed no funding sources and reported having no conflicts of interest.
ACIP Recommends PCV13 for All Adults 65 and Up
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
ACIP recommends PCV13 for all adults 65 and up
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
|
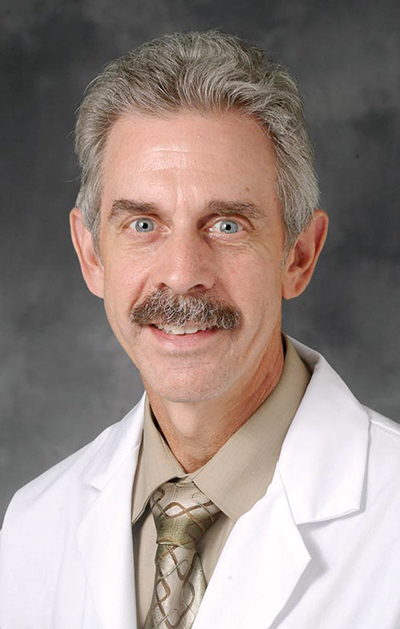
| Dr. Dan Ouellette |
Dr. Dan Ouellette, FCCP, comments: Every year in the fall, I recommend to my patients with respiratory disease that they receive the influenza vaccine. Often, they ask me "what about the pneumonia vaccine"? We then have a conversation about what the "pneumonia vaccine" is. I review their immunization record with them to try and figure out if they have received this vaccine before, and if so, when. This year, the situation is both complicated and clear in my patients over 65 years of age. It is more complicated because the 13-valent pneumococcal vaccine must be administered in addition to the 23-valent pneumococcal vaccine, with those patients who have not received the PCV23 having to receive both. It is clearer, because all of my older patients must receive the PCV13. It is better for my patients, because they will have increased immunity to the pneumococcus.
Dr. Ouellette is a specialist in pulmonary disease at Henry Ford Hospital in Detroit, Michigan.
|
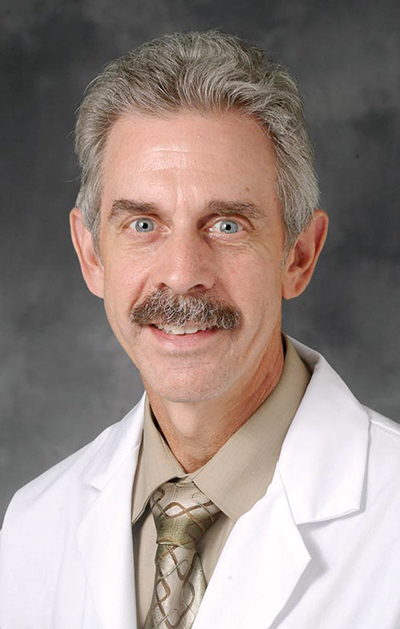
| Dr. Dan Ouellette |
Dr. Dan Ouellette, FCCP, comments: Every year in the fall, I recommend to my patients with respiratory disease that they receive the influenza vaccine. Often, they ask me "what about the pneumonia vaccine"? We then have a conversation about what the "pneumonia vaccine" is. I review their immunization record with them to try and figure out if they have received this vaccine before, and if so, when. This year, the situation is both complicated and clear in my patients over 65 years of age. It is more complicated because the 13-valent pneumococcal vaccine must be administered in addition to the 23-valent pneumococcal vaccine, with those patients who have not received the PCV23 having to receive both. It is clearer, because all of my older patients must receive the PCV13. It is better for my patients, because they will have increased immunity to the pneumococcus.
Dr. Ouellette is a specialist in pulmonary disease at Henry Ford Hospital in Detroit, Michigan.
|
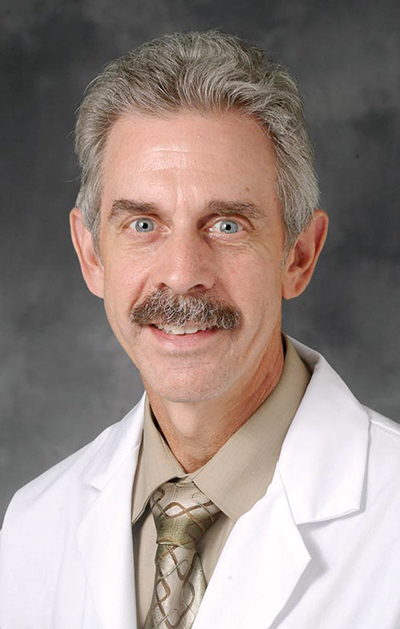
| Dr. Dan Ouellette |
Dr. Dan Ouellette, FCCP, comments: Every year in the fall, I recommend to my patients with respiratory disease that they receive the influenza vaccine. Often, they ask me "what about the pneumonia vaccine"? We then have a conversation about what the "pneumonia vaccine" is. I review their immunization record with them to try and figure out if they have received this vaccine before, and if so, when. This year, the situation is both complicated and clear in my patients over 65 years of age. It is more complicated because the 13-valent pneumococcal vaccine must be administered in addition to the 23-valent pneumococcal vaccine, with those patients who have not received the PCV23 having to receive both. It is clearer, because all of my older patients must receive the PCV13. It is better for my patients, because they will have increased immunity to the pneumococcus.
Dr. Ouellette is a specialist in pulmonary disease at Henry Ford Hospital in Detroit, Michigan.
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
All adults who are 65 years or older should receive 13-valent pneumococcal conjugate vaccine (PCV13) routinely in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23), according to a new recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP). The recommendation appears in the Sept. 19 issue of Morbidity and Mortality Weekly Report.
The ACIP recommendation calls for pneumococcal vaccine-naive adults aged 65 and older to receive one dose of PCV13 vaccine, followed by a dose of PPSV23 6-12 months later (MMWR 2014:63;822-5). Older adults who have previously received only PPSV23 should receive a dose of PCV13 at least 12 months later, wrote Sara Tomczyk of the CDC and her associates.
ACIP has recommended PPSV23 for older adults since 2010. In 2012, the committee made its first recommendation for PCV13, targeting patients 19 years and older who have immunocompromising conditions, functional or anatomic asplenia, cerebrospinal fluid leak, or cochlear implants. The new PCV13 recommendation for all older adults is based on a randomized, placebo-controlled trial of the vaccine in about 85,000 adults aged 65 years and older in the Netherlands who had no prior pneumococcal vaccine exposure. The vaccine showed a moderate level of evidence for efficacy against community-acquired pneumonia in this cohort, ACIP determined. Efficacy against nonbacteremic vaccine-type pneumococcal pneumonia was about 45%, while efficacy against vaccine-type invasive pneumococcal disease was about 75%, the reviewers wrote.
ACIP will reevaluate the recommendations in 2018.
Ms. Tomczyk and her colleagues disclosed no funding sources or conflicts of interest.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Key clinical point: Adults who are 65 years and older should routinely receive 13-valent pneumococcal conjugate vaccine (PCV13) in series with 23-valent pneumococcal polysaccharide vaccine (PPSV23).
Major finding: A review by ACIP identified a moderate level of evidence for PCV13 in preventing community-acquired pneumonia in older adults.
Data source: Randomized, placebo-controlled trial of PCV13 in about 85,000 adults aged 65 years and up who had no prior pneumococcal vaccine exposure.
Disclosures: The authors made no disclosures.
FDG-PET no help in differentiating cancer from benign lung nodules in infection-endemic regions
In geographic regions of endemic granulomatous lung infections, positron emission tomography combined with fludeoxyglucose F18 did not reliably differentiate benign lung disease from lung cancer, according to a meta-analysis published online Sept. 23 in JAMA.
The average adjusted specificity of FDG-PET was only 61% in regions of endemic infections – 16% lower than in nonendemic regions, reported Stephen A. Deppen, Ph.D., of Vanderbilt University Medical Center, Nashville, Tenn., and his associates. “The accuracy of FDG-PET for diagnosing lung nodules was extremely heterogeneous,” Dr. Deppen and his associates said. “These data do not support the use of FDG-PET to diagnose lung cancer in endemic regions unless an institution achieves test performance accuracy similar to that found in nonendemic regions.”
Several guidelines recommend FDG-PET to noninvasively evaluate patients with lung disease, depending on cancer risk. But granulomas caused by pulmonary tuberculosis, blastomycosis, histoplasmosis, and coccidioidomycosis can challenge diagnosticians by mimicking lung cancer. To assess the ability of FDG-PET to distinguish malignant and benign nodules, the researchers reviewed 70 studies of 8,511 lesions carried out between 2000 and 2014, including 10 studies from regions of endemic lung infections. These studies reported lung infections in the population from which participants were recruited or reported that at least half of benign lesions were infection-related granulomas, the researchers reported (JAMA 2014;312:1227-36).
The average adjusted estimate of specificity in regions with endemic disease was 61% (95% confidence interval, 49%-72%), compared with 77% (95% CI, 73%-80%) for nonendemic regions, the researchers reported.
The study received funding support from the Agency for Healthcare Research and Quality, Veterans Health Administration, National Institutes of Health, and National Cancer Institute. The authors reported having no relevant financial conflicts.
In geographic regions of endemic granulomatous lung infections, positron emission tomography combined with fludeoxyglucose F18 did not reliably differentiate benign lung disease from lung cancer, according to a meta-analysis published online Sept. 23 in JAMA.
The average adjusted specificity of FDG-PET was only 61% in regions of endemic infections – 16% lower than in nonendemic regions, reported Stephen A. Deppen, Ph.D., of Vanderbilt University Medical Center, Nashville, Tenn., and his associates. “The accuracy of FDG-PET for diagnosing lung nodules was extremely heterogeneous,” Dr. Deppen and his associates said. “These data do not support the use of FDG-PET to diagnose lung cancer in endemic regions unless an institution achieves test performance accuracy similar to that found in nonendemic regions.”
Several guidelines recommend FDG-PET to noninvasively evaluate patients with lung disease, depending on cancer risk. But granulomas caused by pulmonary tuberculosis, blastomycosis, histoplasmosis, and coccidioidomycosis can challenge diagnosticians by mimicking lung cancer. To assess the ability of FDG-PET to distinguish malignant and benign nodules, the researchers reviewed 70 studies of 8,511 lesions carried out between 2000 and 2014, including 10 studies from regions of endemic lung infections. These studies reported lung infections in the population from which participants were recruited or reported that at least half of benign lesions were infection-related granulomas, the researchers reported (JAMA 2014;312:1227-36).
The average adjusted estimate of specificity in regions with endemic disease was 61% (95% confidence interval, 49%-72%), compared with 77% (95% CI, 73%-80%) for nonendemic regions, the researchers reported.
The study received funding support from the Agency for Healthcare Research and Quality, Veterans Health Administration, National Institutes of Health, and National Cancer Institute. The authors reported having no relevant financial conflicts.
In geographic regions of endemic granulomatous lung infections, positron emission tomography combined with fludeoxyglucose F18 did not reliably differentiate benign lung disease from lung cancer, according to a meta-analysis published online Sept. 23 in JAMA.
The average adjusted specificity of FDG-PET was only 61% in regions of endemic infections – 16% lower than in nonendemic regions, reported Stephen A. Deppen, Ph.D., of Vanderbilt University Medical Center, Nashville, Tenn., and his associates. “The accuracy of FDG-PET for diagnosing lung nodules was extremely heterogeneous,” Dr. Deppen and his associates said. “These data do not support the use of FDG-PET to diagnose lung cancer in endemic regions unless an institution achieves test performance accuracy similar to that found in nonendemic regions.”
Several guidelines recommend FDG-PET to noninvasively evaluate patients with lung disease, depending on cancer risk. But granulomas caused by pulmonary tuberculosis, blastomycosis, histoplasmosis, and coccidioidomycosis can challenge diagnosticians by mimicking lung cancer. To assess the ability of FDG-PET to distinguish malignant and benign nodules, the researchers reviewed 70 studies of 8,511 lesions carried out between 2000 and 2014, including 10 studies from regions of endemic lung infections. These studies reported lung infections in the population from which participants were recruited or reported that at least half of benign lesions were infection-related granulomas, the researchers reported (JAMA 2014;312:1227-36).
The average adjusted estimate of specificity in regions with endemic disease was 61% (95% confidence interval, 49%-72%), compared with 77% (95% CI, 73%-80%) for nonendemic regions, the researchers reported.
The study received funding support from the Agency for Healthcare Research and Quality, Veterans Health Administration, National Institutes of Health, and National Cancer Institute. The authors reported having no relevant financial conflicts.
FROM JAMA
Key clinical point: Combined FDG-PET did not reliably distinguish benign lung disease from lung cancer in areas of endemic lung infection.
Major finding: The average adjusted specificity of FDG-PET was only 61% in endemic regions, which was 16% lower than in nonendemic regions.
Data source: A meta-analysis of 70 studies of FDG-PET used to evaluate 8,511 lung nodules.
Disclosures: The study received funding support from the Agency for Healthcare Research and Quality, Veterans Health Administration, National Institutes of Health, and National Cancer Institute. The authors reported having no relevant financial conflicts.
Adult diabetes leveled off in United States
The occurrence of diabetes has leveled off among U.S. adults in general, but has continued to rise among non-Hispanic blacks, Hispanics, and adults who did not study past high school, researchers from the Centers for Disease Control and Prevention reported Sept. 23 in JAMA.
In 2012, the estimated diabetes incidence was 7.1 cases per 1,000 adults (95% confidence interval, 6.1-8.2), and the prevalence was 8.3% (95% CI, 7.9%-8.7%), with no significant changes in either rate since 2008, said Linda Geiss and her associates at the CDC. The plateau could reflect stabilizations in U.S. obesity rates since 2003, and “appears to be concurrent with declines in overall caloric intake, food purchases, and energy intake,” the researchers said.
The study included National Health Interview Survey data collected between 1980 and 2012 from 664,969 U.S. adults aged 20-79 years old. Rates of type 1 and 2 diabetes rose by about 4.5% per year between 1990 and 2008, the researchers said. During that period, the estimated incidence of diabetes more than doubled from 3.1 to 8.8 cases per 1,000 persons, while prevalence climbed from 3.5% to 7.9%.
Changes in diagnostic practices could have fueled the increase, but were unlikely to fully explain the “strong and steady 15- to 20-year increase in diabetes prevalence and incidence,” Ms. Geiss and her associates added (JAMA 2014 Sept. 23;312:1218-26).
Despite the recent overall plateau, diabetes incidence continued to climb among Hispanics and non-Hispanic blacks between 2008 and 2012, while prevalence rose among adult Americans who had a high school education or less, said the investigators. “This threatens to exacerbate racial/ethnic and socioeconomic disparities in diabetes prevalence and incidence,” the researchers wrote. “Furthermore, in light of the well-known excess risk of amputation, blindness, end-stage renal disease, disability, mortality, and health care costs associated with diabetes, the doubling of diabetes incidence and prevalence ensures that diabetes will remain a major public health problem that demands effective prevention and management programs.”
The Centers for Disease Control National Center for Health Statistics collected the data. The authors reported having no relevant financial conflicts.
The occurrence of diabetes has leveled off among U.S. adults in general, but has continued to rise among non-Hispanic blacks, Hispanics, and adults who did not study past high school, researchers from the Centers for Disease Control and Prevention reported Sept. 23 in JAMA.
In 2012, the estimated diabetes incidence was 7.1 cases per 1,000 adults (95% confidence interval, 6.1-8.2), and the prevalence was 8.3% (95% CI, 7.9%-8.7%), with no significant changes in either rate since 2008, said Linda Geiss and her associates at the CDC. The plateau could reflect stabilizations in U.S. obesity rates since 2003, and “appears to be concurrent with declines in overall caloric intake, food purchases, and energy intake,” the researchers said.
The study included National Health Interview Survey data collected between 1980 and 2012 from 664,969 U.S. adults aged 20-79 years old. Rates of type 1 and 2 diabetes rose by about 4.5% per year between 1990 and 2008, the researchers said. During that period, the estimated incidence of diabetes more than doubled from 3.1 to 8.8 cases per 1,000 persons, while prevalence climbed from 3.5% to 7.9%.
Changes in diagnostic practices could have fueled the increase, but were unlikely to fully explain the “strong and steady 15- to 20-year increase in diabetes prevalence and incidence,” Ms. Geiss and her associates added (JAMA 2014 Sept. 23;312:1218-26).
Despite the recent overall plateau, diabetes incidence continued to climb among Hispanics and non-Hispanic blacks between 2008 and 2012, while prevalence rose among adult Americans who had a high school education or less, said the investigators. “This threatens to exacerbate racial/ethnic and socioeconomic disparities in diabetes prevalence and incidence,” the researchers wrote. “Furthermore, in light of the well-known excess risk of amputation, blindness, end-stage renal disease, disability, mortality, and health care costs associated with diabetes, the doubling of diabetes incidence and prevalence ensures that diabetes will remain a major public health problem that demands effective prevention and management programs.”
The Centers for Disease Control National Center for Health Statistics collected the data. The authors reported having no relevant financial conflicts.
The occurrence of diabetes has leveled off among U.S. adults in general, but has continued to rise among non-Hispanic blacks, Hispanics, and adults who did not study past high school, researchers from the Centers for Disease Control and Prevention reported Sept. 23 in JAMA.
In 2012, the estimated diabetes incidence was 7.1 cases per 1,000 adults (95% confidence interval, 6.1-8.2), and the prevalence was 8.3% (95% CI, 7.9%-8.7%), with no significant changes in either rate since 2008, said Linda Geiss and her associates at the CDC. The plateau could reflect stabilizations in U.S. obesity rates since 2003, and “appears to be concurrent with declines in overall caloric intake, food purchases, and energy intake,” the researchers said.
The study included National Health Interview Survey data collected between 1980 and 2012 from 664,969 U.S. adults aged 20-79 years old. Rates of type 1 and 2 diabetes rose by about 4.5% per year between 1990 and 2008, the researchers said. During that period, the estimated incidence of diabetes more than doubled from 3.1 to 8.8 cases per 1,000 persons, while prevalence climbed from 3.5% to 7.9%.
Changes in diagnostic practices could have fueled the increase, but were unlikely to fully explain the “strong and steady 15- to 20-year increase in diabetes prevalence and incidence,” Ms. Geiss and her associates added (JAMA 2014 Sept. 23;312:1218-26).
Despite the recent overall plateau, diabetes incidence continued to climb among Hispanics and non-Hispanic blacks between 2008 and 2012, while prevalence rose among adult Americans who had a high school education or less, said the investigators. “This threatens to exacerbate racial/ethnic and socioeconomic disparities in diabetes prevalence and incidence,” the researchers wrote. “Furthermore, in light of the well-known excess risk of amputation, blindness, end-stage renal disease, disability, mortality, and health care costs associated with diabetes, the doubling of diabetes incidence and prevalence ensures that diabetes will remain a major public health problem that demands effective prevention and management programs.”
The Centers for Disease Control National Center for Health Statistics collected the data. The authors reported having no relevant financial conflicts.
FROM JAMA
Key clinical point: Diabetes plateaued among U.S. adults between 2008 and 2012.
Major finding: Between 1990 and 2012 in the United States, the incidence of diabetes rose from 3.1 to 8.8 cases per 1,000 adults, and prevalence increased from 3.5% to 7.9%, after which rates plateaued overall between 2008 and 2012.
Data source: Analysis of data from 664,969 U.S. adults from the National Health Interview Survey.
Disclosures: The Centers for Disease Control National Center for Health Statistics collected the data. The authors reported having no relevant financial conflicts.
Women who were better informed chose fewer prenatal genetic tests
Pregnant women who used an interactive computer program to help them decide whether to undergo prenatal testing were 55% less likely to choose invasive testing than women who received standard prenatal care, even when they were offered free testing, researchers reported online Sept. 23 in JAMA.
Women who used the computer program also were more likely to correctly estimate the risks of amniocentesis-related miscarriage and fetal trisomy 21, said Miriam Kuppermann, Ph.D., of the University of California, San Francisco, and her associates. “
If validated in additional populations, this approach may result in more informed and preference-based prenatal testing decision making and fewer women undergoing testing,” the investigators said.
The multicenter study included 710 English- or Spanish-speaking women who were at 20 weeks’ gestation or less.
A bilingual actress narrated the computer program, emulating a “warm and knowledgeable friend” and emphasizing “the personal nature of prenatal testing decisions,” said the researchers.
The control group received prenatal care based on current guidelines, and did not receive financial support for prenatal tests beyond their own insurance plans, the investigators added (JAMA 2014 Sept. 23 [doi:10.1001/jama.2014.11479]).
Medical record reviews showed that the intervention group was significantly less likely to pursue amniocentesis or chorionic villi sampling than was the control group (5.9% vs. 12.3%; odds ratio, 0.45; 95% confidence interval, 0.25 to 0.80). In addition, computer program users were more than three times as likely to forego testing altogether and more than twice as likely to elect screening alone than to choose screening followed by invasive testing.
Although the computer program did not address cell-free DNA testing, the findings should extend to these tests because they cover the same conditions, the researchers said.
The intervention group also was more likely to correctly estimate the risk of amniocentesis-related miscarriage (73.8% vs. 59.0%; OR, 1.95 [95% CI, 1.39-2.75]) and the age-adjusted chance of fetal trisomy 21 (58.7% vs. 46.1%; OR, 1.66 [95% CI, 1.22-2.28]) than the control group, Dr. Kuppermann and her associates reported.
The National Institutes of Health and the March of Dimes Foundation funded the study. Dr. Kuppermann reported receiving research support from Ariosa Diagnostics, Verinata Health, and Natera. Two coauthors reported receiving funding or stock options from Verinata Health, Natera, Ariosa Diagnostics, and Cellscape. The authors disclosed no other financial conflicts.
“The finding that women who were fully informed about various prenatal testing options were less likely to undertake invasive testing is important, and contradicts the notion that more information is always desired. It is possible that the nature of prenatal testing is different than other health care decisions, but the public may be increasingly aware that the numerous medical advances of the last decade also have created greater complexity in decision making. This finding also suggests that prenatal genetic testing decisions require a complex calculus that considers the timing of the testing, the certainty of the results, and the risks of invasive genetic testing during pregnancy.
“Most women are somewhere between wanting the most sophisticated testing and declining all testing. While seeking reassurance through prenatal testing, they acknowledge that difficult information may be revealed. Many admit not knowing exactly what decisions might be made based on receiving difficult information until they have it. For these women, providing information about testing options, with scenarios that illustrate the risks and benefits of each test as well as assisting with values clarification, is important before embarking on any particular testing strategy,” according to Dr. Siobhan M. Dolan.
Dr. Dolan is a professor of obstetrics and gynecology specializing in reproductive genetics at the Albert Einstein College of Medicine in New York. She gave her comments in an editorial to Dr. Kuppermann’s report (JAMA 2014;312:1203-5). She reported no relevant financial conflicts.
“The finding that women who were fully informed about various prenatal testing options were less likely to undertake invasive testing is important, and contradicts the notion that more information is always desired. It is possible that the nature of prenatal testing is different than other health care decisions, but the public may be increasingly aware that the numerous medical advances of the last decade also have created greater complexity in decision making. This finding also suggests that prenatal genetic testing decisions require a complex calculus that considers the timing of the testing, the certainty of the results, and the risks of invasive genetic testing during pregnancy.
“Most women are somewhere between wanting the most sophisticated testing and declining all testing. While seeking reassurance through prenatal testing, they acknowledge that difficult information may be revealed. Many admit not knowing exactly what decisions might be made based on receiving difficult information until they have it. For these women, providing information about testing options, with scenarios that illustrate the risks and benefits of each test as well as assisting with values clarification, is important before embarking on any particular testing strategy,” according to Dr. Siobhan M. Dolan.
Dr. Dolan is a professor of obstetrics and gynecology specializing in reproductive genetics at the Albert Einstein College of Medicine in New York. She gave her comments in an editorial to Dr. Kuppermann’s report (JAMA 2014;312:1203-5). She reported no relevant financial conflicts.
“The finding that women who were fully informed about various prenatal testing options were less likely to undertake invasive testing is important, and contradicts the notion that more information is always desired. It is possible that the nature of prenatal testing is different than other health care decisions, but the public may be increasingly aware that the numerous medical advances of the last decade also have created greater complexity in decision making. This finding also suggests that prenatal genetic testing decisions require a complex calculus that considers the timing of the testing, the certainty of the results, and the risks of invasive genetic testing during pregnancy.
“Most women are somewhere between wanting the most sophisticated testing and declining all testing. While seeking reassurance through prenatal testing, they acknowledge that difficult information may be revealed. Many admit not knowing exactly what decisions might be made based on receiving difficult information until they have it. For these women, providing information about testing options, with scenarios that illustrate the risks and benefits of each test as well as assisting with values clarification, is important before embarking on any particular testing strategy,” according to Dr. Siobhan M. Dolan.
Dr. Dolan is a professor of obstetrics and gynecology specializing in reproductive genetics at the Albert Einstein College of Medicine in New York. She gave her comments in an editorial to Dr. Kuppermann’s report (JAMA 2014;312:1203-5). She reported no relevant financial conflicts.
Pregnant women who used an interactive computer program to help them decide whether to undergo prenatal testing were 55% less likely to choose invasive testing than women who received standard prenatal care, even when they were offered free testing, researchers reported online Sept. 23 in JAMA.
Women who used the computer program also were more likely to correctly estimate the risks of amniocentesis-related miscarriage and fetal trisomy 21, said Miriam Kuppermann, Ph.D., of the University of California, San Francisco, and her associates. “
If validated in additional populations, this approach may result in more informed and preference-based prenatal testing decision making and fewer women undergoing testing,” the investigators said.
The multicenter study included 710 English- or Spanish-speaking women who were at 20 weeks’ gestation or less.
A bilingual actress narrated the computer program, emulating a “warm and knowledgeable friend” and emphasizing “the personal nature of prenatal testing decisions,” said the researchers.
The control group received prenatal care based on current guidelines, and did not receive financial support for prenatal tests beyond their own insurance plans, the investigators added (JAMA 2014 Sept. 23 [doi:10.1001/jama.2014.11479]).
Medical record reviews showed that the intervention group was significantly less likely to pursue amniocentesis or chorionic villi sampling than was the control group (5.9% vs. 12.3%; odds ratio, 0.45; 95% confidence interval, 0.25 to 0.80). In addition, computer program users were more than three times as likely to forego testing altogether and more than twice as likely to elect screening alone than to choose screening followed by invasive testing.
Although the computer program did not address cell-free DNA testing, the findings should extend to these tests because they cover the same conditions, the researchers said.
The intervention group also was more likely to correctly estimate the risk of amniocentesis-related miscarriage (73.8% vs. 59.0%; OR, 1.95 [95% CI, 1.39-2.75]) and the age-adjusted chance of fetal trisomy 21 (58.7% vs. 46.1%; OR, 1.66 [95% CI, 1.22-2.28]) than the control group, Dr. Kuppermann and her associates reported.
The National Institutes of Health and the March of Dimes Foundation funded the study. Dr. Kuppermann reported receiving research support from Ariosa Diagnostics, Verinata Health, and Natera. Two coauthors reported receiving funding or stock options from Verinata Health, Natera, Ariosa Diagnostics, and Cellscape. The authors disclosed no other financial conflicts.
Pregnant women who used an interactive computer program to help them decide whether to undergo prenatal testing were 55% less likely to choose invasive testing than women who received standard prenatal care, even when they were offered free testing, researchers reported online Sept. 23 in JAMA.
Women who used the computer program also were more likely to correctly estimate the risks of amniocentesis-related miscarriage and fetal trisomy 21, said Miriam Kuppermann, Ph.D., of the University of California, San Francisco, and her associates. “
If validated in additional populations, this approach may result in more informed and preference-based prenatal testing decision making and fewer women undergoing testing,” the investigators said.
The multicenter study included 710 English- or Spanish-speaking women who were at 20 weeks’ gestation or less.
A bilingual actress narrated the computer program, emulating a “warm and knowledgeable friend” and emphasizing “the personal nature of prenatal testing decisions,” said the researchers.
The control group received prenatal care based on current guidelines, and did not receive financial support for prenatal tests beyond their own insurance plans, the investigators added (JAMA 2014 Sept. 23 [doi:10.1001/jama.2014.11479]).
Medical record reviews showed that the intervention group was significantly less likely to pursue amniocentesis or chorionic villi sampling than was the control group (5.9% vs. 12.3%; odds ratio, 0.45; 95% confidence interval, 0.25 to 0.80). In addition, computer program users were more than three times as likely to forego testing altogether and more than twice as likely to elect screening alone than to choose screening followed by invasive testing.
Although the computer program did not address cell-free DNA testing, the findings should extend to these tests because they cover the same conditions, the researchers said.
The intervention group also was more likely to correctly estimate the risk of amniocentesis-related miscarriage (73.8% vs. 59.0%; OR, 1.95 [95% CI, 1.39-2.75]) and the age-adjusted chance of fetal trisomy 21 (58.7% vs. 46.1%; OR, 1.66 [95% CI, 1.22-2.28]) than the control group, Dr. Kuppermann and her associates reported.
The National Institutes of Health and the March of Dimes Foundation funded the study. Dr. Kuppermann reported receiving research support from Ariosa Diagnostics, Verinata Health, and Natera. Two coauthors reported receiving funding or stock options from Verinata Health, Natera, Ariosa Diagnostics, and Cellscape. The authors disclosed no other financial conflicts.
FROM JAMA
Key clinical point: Pregnant women who received interactive computerized guidance on prenatal testing were better informed, but less likely to choose invasive testing than women who received typical prenatal care.
Major finding: Women who received computerized guidance on prenatal testing were 55% less likely to choose invasive testing than women who received usual care, even when tests were offered without cost.
Data source: A randomized multicenter trial of 710 pregnant women in the San Francisco Bay area.
Disclosures: The National Institutes of Health and the March of Dimes Foundation funded the study. Dr. Kuppermann reported past research support from Ariosa Diagnostics, Verinata Health, and Natera. Two coauthors reported advisory or financial relationships with Verinata Health, Natera, Ariosa Diagnostics, and Cellscape. The authors disclosed no other financial conflicts.
Adjunctive VNS therapy helps children with drug-resistant epilepsy
Adjunctive vagus nerve stimulation therapy significantly reduced seizure activity for more than a third of children with drug-resistant epilepsy in the largest retrospective, multicenter study of the therapy to date.
Dr. Iren Orosz of Medical University of Lübeck, Germany, and her colleagues at 11 medical centers across Europe found that 130 (37.6%) of 346 patients with drug-resistant epilepsy had at least a 50% reduction in seizures 12 months after being implanted with a vagus nerve stimulation (VNS) device. This included 19 (5.5%) who were rendered seizure free and 111 (32.1%) who achieved a 50%-99% reduction in seizure frequency. A total of 59 patients (17.1%) had a 25%-49% reduction in seizures and 136 patients (39.3%) had a seizure reduction of 25% or less.
The authors reviewed medical records of children who were implanted with a VNS Therapy device during April 1995-April 2010. The children were aged 6 months to 17.9 years at implantation. All patients had a mean of 6.9 antiepileptic drugs (AEDs) prior to implantation; 45% had predominantly generalized seizures. The investigators assessed the change in frequency of the children’s predominant seizure type from baseline, defined as the 3 months prior to device implantation to 12 months after. They defined response as a reduction in baseline seizure frequency of at least 50%. Authors also assessed the incidence of adverse events, and noted clinicians’ assessments of the patients’ health outcomes, quality of life, and seizures (Epilepsia 2014 Sept. 17 [doi:10.1111/epi.12762]).
The rate of reduction in baseline seizure frequency of at least 50% increased over time from 32.5% at 6 months to 37.6% at 12 months to 43.8% at 24 months and “was higher in a subgroup of patients who had no change in antiepileptic drugs during the study,” wrote Dr. Orosz and her coauthors. Dr. Orosz currently works as a visiting assistant professor in the department of radiological sciences at the University of California, Los Angeles.
Responder rates were “comparable to rates from randomized controlled trials of new AEDs in adult and pediatric patients with drug-resistant epilepsy,” the authors wrote.
The study was supported by Cyberonics, the manufacturer of VNS Therapy. Some of the authors are employees of, or have received grant support, consultant fees, or speaker honoraria from, the company.
Adjunctive vagus nerve stimulation therapy significantly reduced seizure activity for more than a third of children with drug-resistant epilepsy in the largest retrospective, multicenter study of the therapy to date.
Dr. Iren Orosz of Medical University of Lübeck, Germany, and her colleagues at 11 medical centers across Europe found that 130 (37.6%) of 346 patients with drug-resistant epilepsy had at least a 50% reduction in seizures 12 months after being implanted with a vagus nerve stimulation (VNS) device. This included 19 (5.5%) who were rendered seizure free and 111 (32.1%) who achieved a 50%-99% reduction in seizure frequency. A total of 59 patients (17.1%) had a 25%-49% reduction in seizures and 136 patients (39.3%) had a seizure reduction of 25% or less.
The authors reviewed medical records of children who were implanted with a VNS Therapy device during April 1995-April 2010. The children were aged 6 months to 17.9 years at implantation. All patients had a mean of 6.9 antiepileptic drugs (AEDs) prior to implantation; 45% had predominantly generalized seizures. The investigators assessed the change in frequency of the children’s predominant seizure type from baseline, defined as the 3 months prior to device implantation to 12 months after. They defined response as a reduction in baseline seizure frequency of at least 50%. Authors also assessed the incidence of adverse events, and noted clinicians’ assessments of the patients’ health outcomes, quality of life, and seizures (Epilepsia 2014 Sept. 17 [doi:10.1111/epi.12762]).
The rate of reduction in baseline seizure frequency of at least 50% increased over time from 32.5% at 6 months to 37.6% at 12 months to 43.8% at 24 months and “was higher in a subgroup of patients who had no change in antiepileptic drugs during the study,” wrote Dr. Orosz and her coauthors. Dr. Orosz currently works as a visiting assistant professor in the department of radiological sciences at the University of California, Los Angeles.
Responder rates were “comparable to rates from randomized controlled trials of new AEDs in adult and pediatric patients with drug-resistant epilepsy,” the authors wrote.
The study was supported by Cyberonics, the manufacturer of VNS Therapy. Some of the authors are employees of, or have received grant support, consultant fees, or speaker honoraria from, the company.
Adjunctive vagus nerve stimulation therapy significantly reduced seizure activity for more than a third of children with drug-resistant epilepsy in the largest retrospective, multicenter study of the therapy to date.
Dr. Iren Orosz of Medical University of Lübeck, Germany, and her colleagues at 11 medical centers across Europe found that 130 (37.6%) of 346 patients with drug-resistant epilepsy had at least a 50% reduction in seizures 12 months after being implanted with a vagus nerve stimulation (VNS) device. This included 19 (5.5%) who were rendered seizure free and 111 (32.1%) who achieved a 50%-99% reduction in seizure frequency. A total of 59 patients (17.1%) had a 25%-49% reduction in seizures and 136 patients (39.3%) had a seizure reduction of 25% or less.
The authors reviewed medical records of children who were implanted with a VNS Therapy device during April 1995-April 2010. The children were aged 6 months to 17.9 years at implantation. All patients had a mean of 6.9 antiepileptic drugs (AEDs) prior to implantation; 45% had predominantly generalized seizures. The investigators assessed the change in frequency of the children’s predominant seizure type from baseline, defined as the 3 months prior to device implantation to 12 months after. They defined response as a reduction in baseline seizure frequency of at least 50%. Authors also assessed the incidence of adverse events, and noted clinicians’ assessments of the patients’ health outcomes, quality of life, and seizures (Epilepsia 2014 Sept. 17 [doi:10.1111/epi.12762]).
The rate of reduction in baseline seizure frequency of at least 50% increased over time from 32.5% at 6 months to 37.6% at 12 months to 43.8% at 24 months and “was higher in a subgroup of patients who had no change in antiepileptic drugs during the study,” wrote Dr. Orosz and her coauthors. Dr. Orosz currently works as a visiting assistant professor in the department of radiological sciences at the University of California, Los Angeles.
Responder rates were “comparable to rates from randomized controlled trials of new AEDs in adult and pediatric patients with drug-resistant epilepsy,” the authors wrote.
The study was supported by Cyberonics, the manufacturer of VNS Therapy. Some of the authors are employees of, or have received grant support, consultant fees, or speaker honoraria from, the company.
FROM EPILEPSIA
Key clinical point: Adjunctive vagus nerve stimulation therapy in children with drug-resistant epilepsy reduces seizures.
Major finding: At 12 months after implantation of a VNS Therapy device, 130 (37.6%) of 346 patients were considered responders, including 19 (5.5%) who were rendered seizure free and 111 (32.1%) who achieved a 50%-99% reduction in seizure frequency.
Data source: A review of medical records of 347 European children implanted with a VNS Therapy device because of drug-resistant epilepsy.
Disclosures: Some of the authors are employees of, or have received grant support, consultant fees, or speaker honoraria from Cyberonics, which supported the study and manufactures VNS Therapy.
Adding MRI bone marrow edema improved diagnosis of early rheumatoid arthritis
In patients with early rheumatoid arthritis, combining the 2010 RA classification criteria with bone marrow edema as seen on MRI was a more sensitive and accurate diagnostic approach than using the 2010 criteria alone, researchers reported in Annals of the Rheumatic Diseases.
"The present findings are the first evidence that the diagnostic probability of early RA using the 2010 RA classification criteria is improved by combining these criteria with MRI-detected bone marrow edema of the wrist and finger joints," said Dr. Mami Tamai at Nagasaki University in Japan and associates.
The investigators studied 166 patients with early arthritis and a median disease duration of 2 months. They defined RA as using disease-modifying antirheumatic drugs (DMARDs) within the first year or as fulfilling the 1987 RA criteria at 1 year, they said (Ann. Rheum. Dis. 2014 [doi:10.1136/annrheumdis-2013-205074]).
Combining the 2010 criteria with bone marrow edema of the wrists or finger joints on MRI yielded a higher sensitivity (76.3%), negative predictive value (69.3%), and accuracy (75.9%) than did using the 2010 criteria alone with the DMARD-based definition as the reference standard. Applied alone, the 2010 RA classification had a sensitivity of only 61.9%, a negative predictive value of 60.6%, and an accuracy of 70.5%. Results were similar when they used the 1987 definition as the reference standard, the investigators said.
Bone marrow edema had a higher positive predictive value than did MRI-detected bone erosion or symmetrical synovitis when added to the 2010 RA classification criteria. "Our study may strengthen the statements of the European League Against Rheumatism recommendations for the use of imaging," they added.
Funding information for the study was not available. The authors reported no conflicts of interest.
In patients with early rheumatoid arthritis, combining the 2010 RA classification criteria with bone marrow edema as seen on MRI was a more sensitive and accurate diagnostic approach than using the 2010 criteria alone, researchers reported in Annals of the Rheumatic Diseases.
"The present findings are the first evidence that the diagnostic probability of early RA using the 2010 RA classification criteria is improved by combining these criteria with MRI-detected bone marrow edema of the wrist and finger joints," said Dr. Mami Tamai at Nagasaki University in Japan and associates.
The investigators studied 166 patients with early arthritis and a median disease duration of 2 months. They defined RA as using disease-modifying antirheumatic drugs (DMARDs) within the first year or as fulfilling the 1987 RA criteria at 1 year, they said (Ann. Rheum. Dis. 2014 [doi:10.1136/annrheumdis-2013-205074]).
Combining the 2010 criteria with bone marrow edema of the wrists or finger joints on MRI yielded a higher sensitivity (76.3%), negative predictive value (69.3%), and accuracy (75.9%) than did using the 2010 criteria alone with the DMARD-based definition as the reference standard. Applied alone, the 2010 RA classification had a sensitivity of only 61.9%, a negative predictive value of 60.6%, and an accuracy of 70.5%. Results were similar when they used the 1987 definition as the reference standard, the investigators said.
Bone marrow edema had a higher positive predictive value than did MRI-detected bone erosion or symmetrical synovitis when added to the 2010 RA classification criteria. "Our study may strengthen the statements of the European League Against Rheumatism recommendations for the use of imaging," they added.
Funding information for the study was not available. The authors reported no conflicts of interest.
In patients with early rheumatoid arthritis, combining the 2010 RA classification criteria with bone marrow edema as seen on MRI was a more sensitive and accurate diagnostic approach than using the 2010 criteria alone, researchers reported in Annals of the Rheumatic Diseases.
"The present findings are the first evidence that the diagnostic probability of early RA using the 2010 RA classification criteria is improved by combining these criteria with MRI-detected bone marrow edema of the wrist and finger joints," said Dr. Mami Tamai at Nagasaki University in Japan and associates.
The investigators studied 166 patients with early arthritis and a median disease duration of 2 months. They defined RA as using disease-modifying antirheumatic drugs (DMARDs) within the first year or as fulfilling the 1987 RA criteria at 1 year, they said (Ann. Rheum. Dis. 2014 [doi:10.1136/annrheumdis-2013-205074]).
Combining the 2010 criteria with bone marrow edema of the wrists or finger joints on MRI yielded a higher sensitivity (76.3%), negative predictive value (69.3%), and accuracy (75.9%) than did using the 2010 criteria alone with the DMARD-based definition as the reference standard. Applied alone, the 2010 RA classification had a sensitivity of only 61.9%, a negative predictive value of 60.6%, and an accuracy of 70.5%. Results were similar when they used the 1987 definition as the reference standard, the investigators said.
Bone marrow edema had a higher positive predictive value than did MRI-detected bone erosion or symmetrical synovitis when added to the 2010 RA classification criteria. "Our study may strengthen the statements of the European League Against Rheumatism recommendations for the use of imaging," they added.
Funding information for the study was not available. The authors reported no conflicts of interest.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: In patients with early rheumatoid arthritis, combining the 2010 RA classification criteria with MRI-detected bone marrow edema was a more sensitive and accurate diagnostic approach than using the 2010 criteria alone.
Major finding: With disease-modifying antirheumatic drugs at year 1 as the reference standard, using the combined approach yielded higher sensitivity (76.3%), negative predictive value (69.3%), and accuracy (75.9%) than applying the 2010 criteria alone.
Data source: Cohort study of 166 patients with early arthritis and a median disease duration of 2 months.
Disclosures: Funding information was not available. The authors reported no conflicts of interest.
Sleeping on Animal Skins Might Protect Against Childhood Asthma, Hay Fever
Babies who slept on animal skins during their first 3 months of life were almost 40% less likely to have asthma by the time they were 10 years old, according to a population-based cohort study.
Sleeping on animal skins during infancy also was linked to lower odds of wheezing and hay fever, but did not seem to affect eczema or sensitivity to airborne antigens, Dr. Christina Tischer reported at the annual meeting of the European Respiratory Society.
"Early exposure to animal fur could be a simple, cheap, and effective way to resemble an environment with higher microbial exposure," said Dr. Tischer, a researcher at the German Institute for Environmental Health in Neuherberg, Germany. "It might follow similar protective mechanisms in relation to asthma and allergy as it has been observed in farm and rural environments."
The investigators studied 2,441 children in Germany who were up to 10 years old; parents answered a series of questionnaires about asthma and respiratory risk factors and health outcomes. In all, 55% of the children slept on animal skins or animal furs during their first 3 months of life, Dr. Tischer and her associates reported.
By age 10 years, children who slept on animal skins or animal fur as infants had a 25% lower odds of ever having wheezed (adjusted odds ratio, 0.75), a 38% lower odds of having been diagnosed with asthma (aOR, 0.62), and a 35% lower odds of having been diagnosed with hay fever (aOR, 0.65) compared with children who did not sleep on animals skins or furs as infants, the investigators reported.
Funding information for the study was not available. Dr. Tischer reported no conflicts of interest.
Babies who slept on animal skins during their first 3 months of life were almost 40% less likely to have asthma by the time they were 10 years old, according to a population-based cohort study.
Sleeping on animal skins during infancy also was linked to lower odds of wheezing and hay fever, but did not seem to affect eczema or sensitivity to airborne antigens, Dr. Christina Tischer reported at the annual meeting of the European Respiratory Society.
"Early exposure to animal fur could be a simple, cheap, and effective way to resemble an environment with higher microbial exposure," said Dr. Tischer, a researcher at the German Institute for Environmental Health in Neuherberg, Germany. "It might follow similar protective mechanisms in relation to asthma and allergy as it has been observed in farm and rural environments."
The investigators studied 2,441 children in Germany who were up to 10 years old; parents answered a series of questionnaires about asthma and respiratory risk factors and health outcomes. In all, 55% of the children slept on animal skins or animal furs during their first 3 months of life, Dr. Tischer and her associates reported.
By age 10 years, children who slept on animal skins or animal fur as infants had a 25% lower odds of ever having wheezed (adjusted odds ratio, 0.75), a 38% lower odds of having been diagnosed with asthma (aOR, 0.62), and a 35% lower odds of having been diagnosed with hay fever (aOR, 0.65) compared with children who did not sleep on animals skins or furs as infants, the investigators reported.
Funding information for the study was not available. Dr. Tischer reported no conflicts of interest.
Babies who slept on animal skins during their first 3 months of life were almost 40% less likely to have asthma by the time they were 10 years old, according to a population-based cohort study.
Sleeping on animal skins during infancy also was linked to lower odds of wheezing and hay fever, but did not seem to affect eczema or sensitivity to airborne antigens, Dr. Christina Tischer reported at the annual meeting of the European Respiratory Society.
"Early exposure to animal fur could be a simple, cheap, and effective way to resemble an environment with higher microbial exposure," said Dr. Tischer, a researcher at the German Institute for Environmental Health in Neuherberg, Germany. "It might follow similar protective mechanisms in relation to asthma and allergy as it has been observed in farm and rural environments."
The investigators studied 2,441 children in Germany who were up to 10 years old; parents answered a series of questionnaires about asthma and respiratory risk factors and health outcomes. In all, 55% of the children slept on animal skins or animal furs during their first 3 months of life, Dr. Tischer and her associates reported.
By age 10 years, children who slept on animal skins or animal fur as infants had a 25% lower odds of ever having wheezed (adjusted odds ratio, 0.75), a 38% lower odds of having been diagnosed with asthma (aOR, 0.62), and a 35% lower odds of having been diagnosed with hay fever (aOR, 0.65) compared with children who did not sleep on animals skins or furs as infants, the investigators reported.
Funding information for the study was not available. Dr. Tischer reported no conflicts of interest.
FROM THE EUROPEAN RESPIRATORY SOCIETY INTERNATIONAL CONGRESS