User login
Germline genetic testing: Why it matters and where we are failing
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Historically, the role of genetic testing has been to identify familial cancer syndromes and initiate cascade testing. If a germline pathogenic variant is found in an individual, cascade testing involves genetic counseling and testing of blood relatives, starting with those closest in relation to the proband, to identify other family members at high hereditary cancer risk. Once testing identifies those family members at higher cancer risk, these individuals can be referred for risk-reducing procedures. They can undergo screening tests starting at an earlier age and/or increased frequency to help prevent invasive cancer or diagnose it at an earlier stage.
Genetic testing can also inform prognosis. While women with a BRCA1 or BRCA2 mutation are at higher risk of developing ovarian cancer compared with the baseline population, the presence of a germline BRCA mutation has been shown to confer improved survival compared with no BRCA mutation (BRCA wild type). However, more recent data have shown that when long-term survival was analyzed, the prognostic benefit seen in patients with a germline BRCA mutation was lost. The initial survival advantage seen in this population may be related to increased sensitivity to treatment. There appears to be improved response to platinum therapy, which is the standard of care for upfront treatment, in germline BRCA mutation carriers.
Most recently, genetic testing has been used to guide treatment decisions in gynecologic cancers. In 2014, the first poly ADP-ribose polymerase (PARP) inhibitor, olaparib, received Food and Drug Administration approval for the treatment of recurrent ovarian cancer in the presence of a germline BRCA mutation. Now there are multiple PARP inhibitors that have FDA approval for ovarian cancer treatment, some as frontline treatment.
Previous data indicate that 13%-18% of women with ovarian cancer have a germline BRCA mutation that places them at increased risk of hereditary ovarian cancer.1 Current guidelines from the American Society of Clinical Oncology, the U.S. Preventive Services Task Force, the National Comprehensive Cancer Network, the Society of Gynecologic Oncology (SGO), and the American College of Obstetricians and Gynecologists recommend universal genetic counseling and testing for patients diagnosed with epithelial ovarian cancer. Despite these guidelines, rates of referral for genetic counseling and completion of genetic testing are low.
There has been improvement for both referrals and testing since the publication of the 2014 SGO clinical practice statement on genetic testing for ovarian cancer patients, which recommended that all women, even those without any significant family history, should receive genetic counseling and be offered genetic testing.2 When including only studies that collected data after the publication of the 2014 SGO clinical practice statement on genetic testing, a recent systematic review found that 64% of patients were referred for genetic counseling and 63% underwent testing.3
Clinical interventions to target genetic evaluation appear to improve uptake of both counseling and testing. These interventions include using telemedicine to deliver genetic counseling services, mainstreaming (counseling and testing are provided in an oncology clinic by nongenetics specialists), having a genetic counselor within the clinic, and performing reflex testing. With limited numbers of genetic counselors (and even further limited numbers of cancer-specific genetic counselors),4 referral for genetic counseling before testing is often challenging and may not be feasible. There is continued need for strategies to help overcome the barrier to accessing genetic counseling.
While the data are limited, there appear to be significant disparities in rates of genetic testing. Genetic counseling and testing were completed by White (43% and 40%) patients more frequently than by either Black (24% and 26%) or Asian (23% and 14%) patients.4 Uninsured patients were about half as likely (23% vs. 47%) to complete genetic testing as were those with private insurance.4
Genetic testing is an important tool to help identify individuals and families at risk of having hereditary cancer syndromes. This identification allows us to prevent many cancers and identify others while still early stage, significantly decreasing the health care and financial burden on our society and improving outcomes for patients. While we have seen improvement in rates of referral for genetic counseling and testing, we are still falling short. Given the shortage of genetic counselors, it is imperative that we find solutions to ensure continued and improved access to genetic testing for our patients.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Norquist BM et al. JAMA Oncol. 2016;2(4):482-90.
2. SGO Clinical Practice Statement. 2014 Oct 1.
3. Lin J et al. Gynecol Oncol. 2021;162(2):506-16.
4. American Society of Clinical Oncology. J Oncol Pract. 2016 Apr;12(4):339-83.
Rules for performing research with children
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The road to hell is paved with good intentions – especially true in clinical research. A Food and Drug Administration press release notes, “Historically, children were not included in clinical trials because of a misperception that excluding them from research was in fact protecting them. This resulted in many FDA-approved, licensed, cleared, or authorized drugs, biological products, and medical devices lacking pediatric-specific labeling information.” In an effort to improve on this situation, the FDA published in September 2022 a proposed new draft guidance on performing research with children that is open for public comment for 3 months.
There is a long history of government attempts to promote research and development for the benefit of society. Sometimes government succeeds and sometimes not. For instance, when the U.S. federal government funded scientific research in the 1960s, it sought to increase the common good by promulgating those discoveries. The government insisted that all federally funded research be in the public domain. The funding produced a spectacular number of technological advancements that have enriched society. However, a decade later, the government concluded that too many good research ideas were never developed into beneficial products because without the ability to patent the results, the costs and risks of product development were not profitable for industry. By the late 1970s, new laws were enacted to enable universities and their faculty to patent the results of government-funded research and share in any wealth created.
Pharmaceutical research in the 1970s and 1980s was mostly performed on men in order to reduce the risk of giving treatments of unknown safety to pregnant women. The unintended consequence was that the new drugs frequently were less effective for women. This was particularly true for cardiac medications for which lifestyle risk factors differed between the sexes.
Similarly, children were often excluded from research because of the unknown risks of new drugs on growing bodies and brains. Children were also seen as a vulnerable population for whom informed consent was problematic. The result of these well-intentioned restrictions was the creation of new products that did not have pediatric dosing recommendations, pediatric safety assessments, or approval for pediatric indications. To remediate these deficiencies, in 1997 and 2007 the FDA offered a 6-month extension on patent protection as motivation for companies to develop those pediatric recommendations. Alas, those laws were primarily used to extend the profitability of blockbuster products rather than truly benefit children.
Over the past 4 decades, pediatric ethicists proposed and refined rules to govern research on children. The Common Rule used by institutional review boards (IRBs) to protect human research subjects was expanded with guidelines covering children. The new draft guidance is the latest iteration of this effort. Nothing in the 14 pages of draft regulation appears revolutionary to me. The ideas are tweaks, based on theory and experience, of principles agreed upon 30 years ago. Finding the optimal social moral contract involves some empirical assessment of praxis and effectiveness.
I am loathe to summarize this new document, which itself is a summary of a vast body of literature, that supports the Code of Federal Regulations Title 21 Part 50 and 45 CFR Part 46. The draft document is well organized and I recommend it as an excellent primer for the area of pediatric research ethics if the subject is new to you. I also recommend it as required reading for anyone serving on an IRB.
IRBs usually review and approve any research on people. Generally, the selection of people for research should be done equitably. However, children should not be enrolled unless it is necessary to answer an important question relevant to children. For the past 2 decades, there has been an emphasis on obtaining the assent of the child as well as informed consent by the parents.
An important determination is whether the research is likely to help that particular child or whether it is aimed at advancing general knowledge. If there is no prospect of direct benefit, research is still permissible but more restricted for safety and comfort reasons. Next is determining whether the research carries only minimal risk or a minor increase over minimal risk. The draft defines and provides anchor examples of these situations. For instance, oral placebos and single blood draws are typically minimal risk. Multiple injections and blood draws over a year fall into the second category. One MRI is minimal risk but a minor increase in risk if it involves sedation or contrast.
I strongly support the ideals expressed in these guidelines. They represent the best blend of intentions and practical experience. They will become the law of the land. In ethics, there is merit in striving to do things properly, orderly, and enforceably.
The cynic in me sees two weaknesses in the stated approach. First, the volume of harm to children occurring during organized clinical research is extremely small. The greater harms come from off-label use, nonsystematic research, and the ignorance resulting from a lack of research. Second, my observation in all endeavors of morality is, “Raise the bar high enough and people walk under it.”
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Why the 5-day isolation period for COVID makes no sense
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
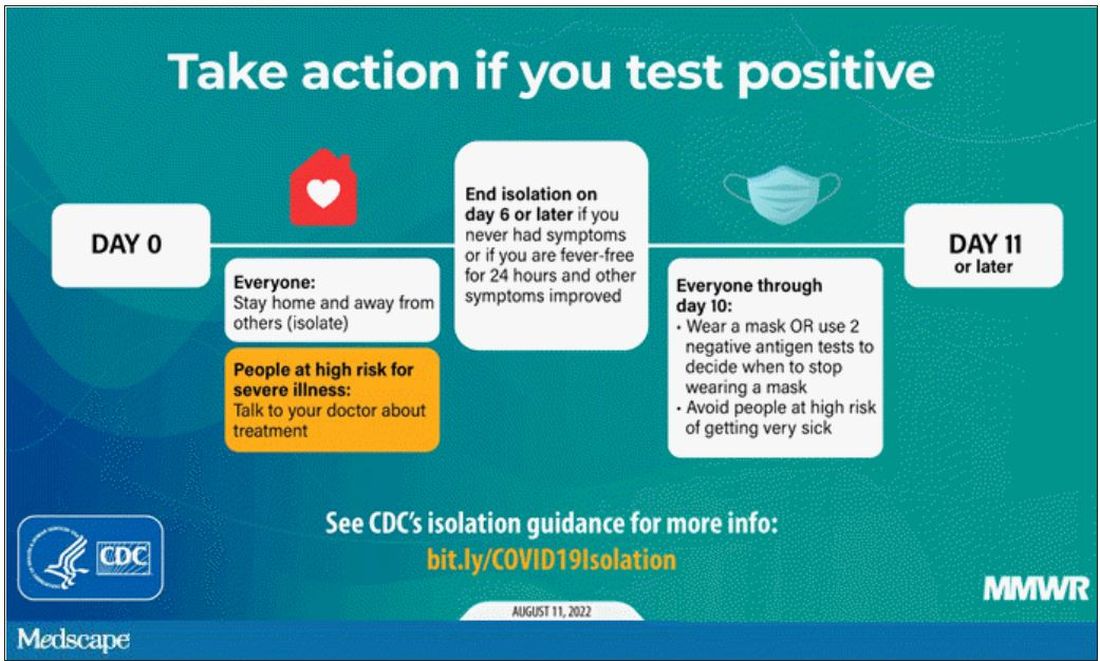
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
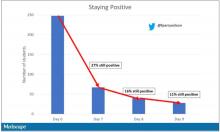
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
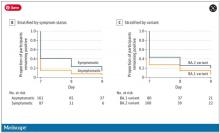
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How to remain apolitical with patients
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
It is assumed that psychiatrists in general, but particularly in academia, are progressive liberals. There is evidence to support this idea, with a survey finding that more than three-quarters of U.S. psychiatrists are registered Democrats.1
Other corroborating factors to our field’s progressive tendency include the publication of pseudo-political books like “The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President” – without a well-known equivalent on the other side.
Additionally, psychiatry has in the recent past, rightfully spent significant effort examining the disproportional trauma faced by patients with underprivileged backgrounds, which is often seen as a political position. The American Psychiatric Association has itself taken a stance on the national debate about abortion to warn against the psychiatric consequences of the Dobbs v. Jackson Supreme Court decision despite the clear political statement it makes.
We understand a likely rationale for psychiatry’s liberal tendency. Most psychiatrists support political objectives that provide resources for the treatment of the severely mentally ill. In general, the psychosocial consequences of mental illness place a downward economic pressure on our patients that leads to poverty and its associated traumas that then tend to feedback to worsen the severity of the illness itself. It is thus natural for psychiatry to promote political causes such as progressivism that focus on the needs of economically and socially struggling communities. If one posits a natural role for psychiatry in promoting the interests of patients, then it is a short leap to psychiatry promoting the political causes of the underprivileged, often in the form of endorsing the Democratic party.
As a result, a proportion of patients come into psychiatric treatment with expectations that their providers will negatively judge them and possibly punish their conservative beliefs or Republican political affiliation. Herein lies a question – “Is psychiatry willing to make 46.9% of Americans uncomfortable?” How should psychiatry address the 46.9% of Americans who voted Republican during the 2020 presidential election? In our desire to support the disadvantaged, how political are we willing to get and at what cost? While we cannot speak for the field as a whole, it is our concern that a vast percentage of Americans feel alienated from talking to us, which is particularly problematic in a field based on mutual trust and understanding.
This problem may be particularly palpable to us, as we are psychiatrists in a large metropolitan area of California who often treat specialty populations like veterans and law enforcement. In one study, law enforcement officers were found to be twice as likely to be Republicans as civilians.2 Michael McHale, the president of the National Association of Police Organizations, spoke at the 2020 Republican Party’s national convention as documented in an article titled “Union leader tells Republican convention why cops back Trump.”3 Similarly, about 60% of veterans identify as Republicans.4
Within the first few sessions, when patients are most vulnerable and sensitive to the perception of being judged, we commonly get asked questions to test our political beliefs. Some patients will display clothing that suggests a political affiliation; those wardrobe arrangements are, at times, an attempt at testing our knowledge of their in-group. While a bright-red cap with a reminder to keep the United States “great” in capital letters may be an overt invitation to address the topic, other patients may have a small symbol of a rattlesnake to test our ability to recognize the “Don’t Tread on Me” Gadsden flag.
Alternatively, other patients will ask our opinion, or bring up news topics, to share their concerns and/or examine our response and reactions. We remember, in particular, a patient who subtly asked if they needed to be vaccinated to attend therapy visits in person as a leading statement into their conservative political beliefs. It is a reminder that many patients fear how we will judge them or where we will draw the line – “Is there something I, the patient, can say that will make him dislike me?”
While the concept of making all patients comfortable may feel abstract or trivial to some, the consequences can be very real. We remember a patient with severe depression and occasional suicidality, who required many months of treatment for him to reveal that he owned a gun. His conservative beliefs made him very resistant to discuss gun ownership with someone who is presumably liberal and has the power to restrict such ownership. However, after a frank discussion that our concerns about his gun were not constitutional or political but medical, the patient agreed to relinquish his gun, at least temporarily, a likely more important intervention than many in psychiatry.
The ramifications are also wider than most imagine. In California, a particularly liberal state, many consistently and reliably liberal patients have some conservative beliefs. Those beliefs are often closeted: a Democratic mother who doesn’t think her 3-year-old daughter should wear a mask in school; a Democratic woman who questioned the veracity of Amber Heard during the Johnny Depp defamation trial and feels guilty about her prior dedication to the #MeToo movement.
Patients may feel torn about those beliefs and may be apprehensive to discuss them despite a nagging need to express or examine them in a place without judgment.
that we attempted to highlight in this article. In particular, a vast proportion of Americans may feel alienated from treatment or may refuse to divulge clinically relevant information, and a large number of patients may enter psychiatric treatment with concerns that they will be judged.
Psychiatry is founded on the honest exchange of thoughts and feelings between patients and providers without the fear of harsh judgment and intellectual retaliation. Psychiatrists would be wise to consider those factors and their repercussions when choosing to take political positions and setting a frame of care with their patients.
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Sanger-Katz M. Your surgeon is probably a Republican, your psychiatrist probably a Democrat. New York Times. 2016 Oct 6.
2. Ba B et al. Who are the police? Descriptive representation in the coercive arm of government. 2022 Mar 21.
3. Rainey J. Union leader tells Republican convention why cops back Trump. Los Angeles Times. 2020 Aug 26.
4. Igielnik R et al. Trump draws stronger support from veterans than from the public on leadership of U.S. military. Pew Research Center. 2019 July 10.
Vision loss may be a risk with PRP facial injections
A systematic review was recently conducted by Wu and colleagues examining the risk of blindness associated with platelet-rich plasma (PRP) injection. In dermatology, PRP is used more commonly now than 5 years ago to promote hair growth with injections on the scalp, as an adjunct to microneedling procedures, and sometimes – in a similar way to facial fillers – to improve volume loss, and skin tone and texture (particularly to the tear trough region).
Total unilateral blindness occurred in all cases. In one of the seven reported cases, the patient experienced recovery of vision after 3 months, but with some residual deficits noted on the ophthalmologist examination. In this case, the patient was evaluated and treated by an ophthalmologist within 3 hours of symptom onset.
In addition, four cases were reported from Venezuela, one from the United States, one from the United Kingdom, and one from Malaysia. Similar to reports of blindness with facial fillers, the most common injection site reported with this adverse effect was the glabella (five cases);
Other reports involved injections of the forehead (two), followed by the nasolabial fold (one), lateral canthus (one), and temporomandibular joint (one). Two of the seven patients received injections at more than one site, resulting in the total number of injections reported (10) being higher than the number of patients.
The risk of blindness is inherent with deep injection into a vessel that anastomoses with the blood supply to the eye. No mention was made as to whether PRP or platelet-rich fibrin was used. Other details are lacking from the original articles as to injection technique and whether or not cannula injection was used. No treatment was attempted in four of seven cases.
As plasma is native to the arteries and dissolves in the blood stream naturally, the mechanism as to why retinal artery occlusion or blindness would occur is not completely clear. One theory is that it is volume related and results from the speed of injection, causing a large rapid bolus that temporarily occludes or compresses an involved vessel.
Another theory is that damage to the vessel results from the injection itself or injection technique, leading to a clotting cascade and clot of the involved vessel with subsequent retrograde flow or blockade of the retinal artery. But if this were the case, we would expect to hear about more cases of clots leading to vascular occlusion or skin necrosis, which does not typically occur or we do not hear about.
Details about proper collection materials and technique or mixing with some other materials are also unknown in these cases, thus leaving the possibility that a more occlusive material may have been injected, as opposed to the fluid-like composition of the typical PRP preparation.With regards to risk with scalp PRP injection, the frontal scalp does receive blood supply from the supratrochlear artery that anastomoses with the angular artery of the face – both of which anastomose with the retinal artery (where occlusion would occur via back flow). The scalp tributaries are small and far enough away from the retina at that point that risk of back flow the to retinal artery should be minimal. Additionally, no reports of vascular occlusion from PRP scalp injection leading to skin necrosis have ever been reported. Of note, this is also not a risk that has been reported with the use of PRP with microneedling procedures, where PRP is placed on top of the skin before, during and after microneedling.
Anything that occludes the blood supply to the eye, whether it be fat, filler, or PRP, has an inherent risk of blindness. As there is no reversal agent or designated treatment for PRP occlusion, care must be taken to minimize risk, including awareness of anatomy and avoidance of injection into high risk areas, and cannula use where appropriate. Gentle, slow, low-volume administration, and when possible, use of a retrograde injection technique, may also be helpful.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
A systematic review was recently conducted by Wu and colleagues examining the risk of blindness associated with platelet-rich plasma (PRP) injection. In dermatology, PRP is used more commonly now than 5 years ago to promote hair growth with injections on the scalp, as an adjunct to microneedling procedures, and sometimes – in a similar way to facial fillers – to improve volume loss, and skin tone and texture (particularly to the tear trough region).
Total unilateral blindness occurred in all cases. In one of the seven reported cases, the patient experienced recovery of vision after 3 months, but with some residual deficits noted on the ophthalmologist examination. In this case, the patient was evaluated and treated by an ophthalmologist within 3 hours of symptom onset.
In addition, four cases were reported from Venezuela, one from the United States, one from the United Kingdom, and one from Malaysia. Similar to reports of blindness with facial fillers, the most common injection site reported with this adverse effect was the glabella (five cases);
Other reports involved injections of the forehead (two), followed by the nasolabial fold (one), lateral canthus (one), and temporomandibular joint (one). Two of the seven patients received injections at more than one site, resulting in the total number of injections reported (10) being higher than the number of patients.
The risk of blindness is inherent with deep injection into a vessel that anastomoses with the blood supply to the eye. No mention was made as to whether PRP or platelet-rich fibrin was used. Other details are lacking from the original articles as to injection technique and whether or not cannula injection was used. No treatment was attempted in four of seven cases.
As plasma is native to the arteries and dissolves in the blood stream naturally, the mechanism as to why retinal artery occlusion or blindness would occur is not completely clear. One theory is that it is volume related and results from the speed of injection, causing a large rapid bolus that temporarily occludes or compresses an involved vessel.
Another theory is that damage to the vessel results from the injection itself or injection technique, leading to a clotting cascade and clot of the involved vessel with subsequent retrograde flow or blockade of the retinal artery. But if this were the case, we would expect to hear about more cases of clots leading to vascular occlusion or skin necrosis, which does not typically occur or we do not hear about.
Details about proper collection materials and technique or mixing with some other materials are also unknown in these cases, thus leaving the possibility that a more occlusive material may have been injected, as opposed to the fluid-like composition of the typical PRP preparation.With regards to risk with scalp PRP injection, the frontal scalp does receive blood supply from the supratrochlear artery that anastomoses with the angular artery of the face – both of which anastomose with the retinal artery (where occlusion would occur via back flow). The scalp tributaries are small and far enough away from the retina at that point that risk of back flow the to retinal artery should be minimal. Additionally, no reports of vascular occlusion from PRP scalp injection leading to skin necrosis have ever been reported. Of note, this is also not a risk that has been reported with the use of PRP with microneedling procedures, where PRP is placed on top of the skin before, during and after microneedling.
Anything that occludes the blood supply to the eye, whether it be fat, filler, or PRP, has an inherent risk of blindness. As there is no reversal agent or designated treatment for PRP occlusion, care must be taken to minimize risk, including awareness of anatomy and avoidance of injection into high risk areas, and cannula use where appropriate. Gentle, slow, low-volume administration, and when possible, use of a retrograde injection technique, may also be helpful.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
A systematic review was recently conducted by Wu and colleagues examining the risk of blindness associated with platelet-rich plasma (PRP) injection. In dermatology, PRP is used more commonly now than 5 years ago to promote hair growth with injections on the scalp, as an adjunct to microneedling procedures, and sometimes – in a similar way to facial fillers – to improve volume loss, and skin tone and texture (particularly to the tear trough region).
Total unilateral blindness occurred in all cases. In one of the seven reported cases, the patient experienced recovery of vision after 3 months, but with some residual deficits noted on the ophthalmologist examination. In this case, the patient was evaluated and treated by an ophthalmologist within 3 hours of symptom onset.
In addition, four cases were reported from Venezuela, one from the United States, one from the United Kingdom, and one from Malaysia. Similar to reports of blindness with facial fillers, the most common injection site reported with this adverse effect was the glabella (five cases);
Other reports involved injections of the forehead (two), followed by the nasolabial fold (one), lateral canthus (one), and temporomandibular joint (one). Two of the seven patients received injections at more than one site, resulting in the total number of injections reported (10) being higher than the number of patients.
The risk of blindness is inherent with deep injection into a vessel that anastomoses with the blood supply to the eye. No mention was made as to whether PRP or platelet-rich fibrin was used. Other details are lacking from the original articles as to injection technique and whether or not cannula injection was used. No treatment was attempted in four of seven cases.
As plasma is native to the arteries and dissolves in the blood stream naturally, the mechanism as to why retinal artery occlusion or blindness would occur is not completely clear. One theory is that it is volume related and results from the speed of injection, causing a large rapid bolus that temporarily occludes or compresses an involved vessel.
Another theory is that damage to the vessel results from the injection itself or injection technique, leading to a clotting cascade and clot of the involved vessel with subsequent retrograde flow or blockade of the retinal artery. But if this were the case, we would expect to hear about more cases of clots leading to vascular occlusion or skin necrosis, which does not typically occur or we do not hear about.
Details about proper collection materials and technique or mixing with some other materials are also unknown in these cases, thus leaving the possibility that a more occlusive material may have been injected, as opposed to the fluid-like composition of the typical PRP preparation.With regards to risk with scalp PRP injection, the frontal scalp does receive blood supply from the supratrochlear artery that anastomoses with the angular artery of the face – both of which anastomose with the retinal artery (where occlusion would occur via back flow). The scalp tributaries are small and far enough away from the retina at that point that risk of back flow the to retinal artery should be minimal. Additionally, no reports of vascular occlusion from PRP scalp injection leading to skin necrosis have ever been reported. Of note, this is also not a risk that has been reported with the use of PRP with microneedling procedures, where PRP is placed on top of the skin before, during and after microneedling.
Anything that occludes the blood supply to the eye, whether it be fat, filler, or PRP, has an inherent risk of blindness. As there is no reversal agent or designated treatment for PRP occlusion, care must be taken to minimize risk, including awareness of anatomy and avoidance of injection into high risk areas, and cannula use where appropriate. Gentle, slow, low-volume administration, and when possible, use of a retrograde injection technique, may also be helpful.
Dr. Wesley and Lily Talakoub, MD, are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
An infant with a tender bump on her ear
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A biopsy of the lesion was performed that showed a well-defined nodulocystic tumor composed of nests of basaloid cells that are undergoing trichilemmal keratinization. Shadow cells are seen as well as small areas of calcification. There is also a histiocytic infiltrate with multinucleated giant cells. The histologic diagnosis is of a pilomatrixoma.
Pilomatrixoma, also known as calcifying epithelioma of Malherbe, was first described in 1880, as a tumor of sebaceous gland origin. Later, in 1961, Robert Forbis Jr, MD, and Elson B. Helwig, MD, coined the term pilomatrixoma to describe the hair follicle matrix as the source of the tumor. Pilomatrixomas are commonly seen in the pediatric population, usually in children between 8 and 13 years of age. Our patient is one of the youngest described. The lesions are commonly seen on the face and neck in about 70% of the cases followed by the upper extremities, back, and legs. Clinically, the lesions appear as a firm dermal papule or nodule, which moves freely and may have associated erythema on the skin surface or a blueish gray hue on the underlying skin.
Most pilomatrixomas that have been studied have shown a mutation in Exon 3 of the beta-catenin gene (CTNNB1). The beta-catenin molecule is a subunit of the cadherin protein, which is part of an important pathway in the terminal hair follicle differentiation. Beta-catenin also plays an important role in the Wnt pathway, which regulates cell fate as well as early embryonic patterning. Beta-catenin is responsible for forming adhesion junctions among cells. There have also been immunohistochemical studies that have shown a BCL2 proto-oncogene overexpression to pilomatrixoma.
There are several genetic syndromes that have been associated with the presence of pilomatrixomas: Turner syndrome (XO chromosome abnormality associated with short stature and cardiac defects), Gardner syndrome (polyposis coli and colon and rectal cancer), myotonic dystrophy, Rubinstein-Taybi syndrome (characterized by broad thumbs and toes, short stature, distinctive facial features, and varying degrees of intellectual disability), and trisomy 9. On physical examination our patient didn’t present with any of the typical features or history that could suggest any of these syndromes. A close follow-up and evaluation by a geneticist was recommended because after the initial visit she developed a second lesion on the forehead.
The differential diagnosis for this lesion includes other cysts that may occur on the ear such as epidermal inclusion cyst or dermoid cysts, though these lesions do not tend to be as firm as pilomatrixomas are, which can help with the diagnosis. Dermoid cysts are made of dermal and epidermal components. They are usually present at birth and are commonly seen on the scalp and the periorbital face.
Keloids are rubbery nodules of scar tissue that can form on sites of trauma, and although the lesion occurred after she had her ears pierced, the consistency and rapid growth of the lesion as well as the pathological description made this benign fibrous growth less likely.
When pilomatrixomas are inflamed they can be confused with vascular growths: in this particular case, a hemangioma or another vascular tumor such as a tufted angioma or kaposiform hemangioendothelioma. An ultrasound of the lesion could have helped in the differential diagnosis of the lesion.
Pilomatrixomas can grow significantly and in some cases get inflamed or infected. Surgical management of pilomatrixomas is often required because the lesions do not regress spontaneously.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Forbis R Jr and Helwig EB. Arch Dermatol 1961;83:606-18.
Schwarz Y et al. Int J Pediatr Otorhinolaryngol. 2016 Jun;85:148-53.
A 4-month-old female was referred to our clinic for evaluation of a bump on the right ear. The lesion was first noted at 2 months of age as a little pimple. She was evaluated by her pediatrician and was treated with topical and oral antibiotics without resolution of the lesion. The bump continued to grow and seemed tender to palpation, so she was referred to dermatology for evaluation.
She was born via normal vaginal delivery at 40 weeks. Her mother has no medical conditions and the pregnancy was uneventful. She has been growing and developing well. She takes vitamin D and is currently breast fed.
There have been no other family members with similar lesions. She had her ears pierced at a month of age without any complications.
On skin examination she has a firm red nodule on the right ear that appears slightly tender to touch. She has no other skin lesions of concern. She has normal muscle tone and there are no other abnormalities noted on the physical exam. She has no hepatomegaly, splenomegaly, or lymphadenopathy.
Vaccinium myrtillus (bilberry seed oil) extract
A member of the Ericaceae family, bilberry (Vaccinium myrtillus) is native to northern Europe and North America, and its fruit is known to contain myriad polyphenols that display potent antioxidant and anti-inflammatory activity.1,2 Also known as European blueberry or whortleberry, this perennial deciduous shrub is also one of the richest sources of the polyphenolic pigments anthocyanins.3-5 Indeed, anthocyanins impart the blue/black color to bilberries and other berries and are thought to be the primary bioactive constituents of berries associated with numerous health benefits.3,6 They are also known to confer anti-allergic, anticancer, and wound healing activity.4 Overall, bilberry has also been reported to exert anti-inflammatory, lipid-lowering, and antimicrobial activity.3 In this column, the focus will be on the chemical constituents and properties of V. myrtillus that indicate potential or applicability for skin care.
Active ingredients of bilberry
Bilberry seed oil contains unsaturated fatty acids such as linoleic acid and alpha-linolenic acid, which exhibit anti-inflammatory activity and contribute to the suppression of tyrosinase. For instance, Ando et al. showed, in 1998, that linoleic and alpha-linolenic acids lighten UV-induced skin hyperpigmentation. Their in vitro experiments using cultured murine melanoma cells and in vivo study of the topical application of either acid to the UV-induced hyperpigmented dorsal skin of guinea pigs revealed pigment-lightening effects that they partly ascribed to inhibited melanin synthesis by active melanocytes and accelerated desquamation of epidermal melanin pigment.7
A 2009 comparative study of the anthocyanin composition as well as antimicrobial and antioxidant activities delivered by bilberry and blueberry fruits and their skins by Burdulis et al. revealed robust functions in both fruits. Cyanidin was found to be an active anthocyanidin in bilberry. Cultivars of both fruits demonstrated antimicrobial and antioxidant activity, with bilberry fruit skin demonstrating potent antiradical activity.8
The anthocyanins of V. myrtillus are reputed to impart protection against cardiovascular disorders, age-induced oxidative stress, inflammatory responses, and various degenerative conditions, as well ameliorate neuronal and cognitive brain functions and ocular health.6
In 2012, Bornsek et al. demonstrated that bilberry (and blueberry) anthocyanins function as potent intracellular antioxidants, which may account for their noted health benefits despite relatively low bioavailability.9
Six years later, a chemical composition study of wild bilberry found in Montenegro, Brasanac-Vukanovic et al. determined that chlorogenic acid was the most prevalent phenolic constituent, followed by protocatechuic acid, with resveratrol, isoquercetin, quercetin, and hyperoside also found to be abundant. In vitro assays indicated significant antioxidant activity exhibited by these compounds.10
Activity against allergic contact dermatitis
Yamaura et al. used a mouse model, in 2011, to determine that the anthocyanins from a bilberry extract attenuated various symptoms of chronic allergic contact dermatitis, particularly alleviating pruritus.8 A year later, Yamaura et al. used a BALB/c mouse model of allergic contact dermatitis to compare the antipruritic effect of anthocyanin-rich quality-controlled bilberry extract and anthocyanidin-rich degraded extract. The investigators found that anthocyanins, but not anthocyanidins, derived from bilberry exert an antipruritic effect, likely through their inhibitory action on mast cell degranulation. They concluded that anthocyanin-rich bilberry extract could act as an effective oral supplement to treat pruritic symptoms of skin disorders such as chronic allergic contact dermatitis and atopic dermatitis.11
Antioxidant and anti-inflammatory activity
Bilberries, consumed since ancient times, are reputed to function as potent antioxidants because of a wide array of phenolic constituents, and this fruit is gaining interest for use in pharmaceuticals.12
In 2008, Svobodová et al. assessed possible UVA preventive properties of V. myrtillus fruit extract in a human keratinocyte cell line (HaCaT), finding that pre- or posttreatment mitigated UVA-induced harm. They also observed a significant decrease in UVA-caused reactive oxygen species (ROS) formation and the prevention or attenuation of UVA-stimulated peroxidation of membrane lipids. Intracellular glutathione was also protected. The investigators attributed the array of cytoprotective effects conferred by V. myrtillus extract primarily to its constituent anthocyanins.2 A year later, they found that the phenolic fraction of V. myrtillus fruits inhibited UVB-induced damage to HaCaT keratinocytes in vitro.13
In 2014, Calò and Marabini used HaCaT keratinocytes to ascertain whether a water-soluble V. myrtillus extract could mitigate UVA- and UVB-induced damage. They found that the extract diminished UVB-induced cytotoxicity and genotoxicity at lower doses, decreasing lipid peroxidation but exerting no effect on reactive oxygen species generated by UVB. The extract attenuated genotoxicity induced by UVA as well as ROS and apoptosis. Overall, the investigators concluded that V. myrtillus extract demonstrated antioxidant activity, particularly against UVA exposure.14
Four years later, Bucci et al. developed nanoberries, an ultradeformable liposome carrying V. myrtillus ethanolic extract, and determined that the preparation could penetrate the stratum corneum safely and suggested potential for yielding protection against photodamage.15
Skin preparations
In 2021, Tadic et al. developed an oil-in-water (O/W) cream containing wild bilberry leaf extracts and seed oil. The leaves contained copious phenolic acids (particularly chlorogenic acid), flavonoids (especially isoquercetin), and resveratrol. The seed oil was rife with alpha-linolenic, linoleic, and oleic acids. The investigators conducted an in vivo study over 30 days in 25 healthy volunteers (20 women, 5 men; mean age 23.36 ± 0.64 years). They found that the O/W cream successfully increased stratum corneum hydration, enhanced skin barrier function, and maintained skin pH after topical application. The cream was also well tolerated. In vitro assays also indicated that the bilberry isolates displayed notable antioxidant capacity (stronger in the case of the leaves). Tadic et al. suggested that skin disorders characterized by oxidative stress and/or xerosis may be appropriate targets for topically applied bilberry cream.1
Early in 2022, Ruscinc et al. reported on their efforts to incorporate V. myrtillus extract into a multifunctional sunscreen. In vitro and in vivo tests revealed that while sun protection factor was lowered in the presence of the extract, the samples were safe and photostable. The researchers concluded that further study is necessary to elucidate the effect of V. myrtillus extract on photoprotection.16
V. myrtillus has been consumed by human beings for many generations. Skin care formulations based on this ingredient have not been associated with adverse events. Notably, the Environmental Working Group has rated V. myrtillus (bilberry seed) oil as very safe.17
Summary
While research, particularly in the form of randomized controlled trials, is called for, because the fatty acids it contains have been shown to suppress tyrosinase. Currently, this botanical agent seems to be most suited for sensitive, aging skin and for skin with an uneven tone, particularly postinflammatory pigmentation and melasma.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, an SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Tadic VM et al. Antioxidants (Basel). 2021 Mar 16;10(3):465.
2. Svobodová A et al. Biofactors. 2008;33(4):249-66.
3. Chu WK et al. Bilberry (Vaccinium myrtillus L.), in Benzie IFF, Wachtel-Galor S, eds., “Herbal Medicine: Biomolecular and Clinical Aspects,” 2nd ed. (Boca Raton, Fla.: CRC Press/Taylor & Francis, 2011, Chapter 4).
4. Yamaura K et al. Pharmacognosy Res. 2011 Jul;3(3):173-7.
5. Stefanescu BE et al. Molecules. 2019 May 29;24(11):2046.
6. Smeriglio A et al. Mini Rev Med Chem. 2014;14(7):567-84.
7. Ando H et al. Arch Dermatol Res. 1998 Jul;290(7):375-81.
8. Burdulis D et al. Acta Pol Pharm. 2009 Jul-Aug;66(4):399-408.
9. Bornsek SM et al. Food Chem. 2012 Oct 15;134(4):1878-84.
10. Brasanac-Vukanovic S et al. Molecules. 2018 Jul 26;23(8):1864.
11. Yamaura K et al. J Food Sci. 2012 Dec;77(12):H262-7.
12. Pires TCSP et al. Curr Pharm Des. 2020;26(16):1917-28.
13. Svobodová A et al. J Dermatol Sci. 2009 Dec;56(3):196-204.
14. Calò R, Marabini L. J Photochem Photobiol B. 2014 Mar 5;132:27-35.
15. Bucci P et al. J Cosmet Dermatol. 2018 Oct;17(5):889-99.
16. Ruscinc N et al. J Cosmet Dermatol. 2022 Jan 13.
17. Environmental Working Group’s Skin Deep website. Vaccinium Myrtillus Bilberry Seed Oil. Accessed October 18, 2022.
A member of the Ericaceae family, bilberry (Vaccinium myrtillus) is native to northern Europe and North America, and its fruit is known to contain myriad polyphenols that display potent antioxidant and anti-inflammatory activity.1,2 Also known as European blueberry or whortleberry, this perennial deciduous shrub is also one of the richest sources of the polyphenolic pigments anthocyanins.3-5 Indeed, anthocyanins impart the blue/black color to bilberries and other berries and are thought to be the primary bioactive constituents of berries associated with numerous health benefits.3,6 They are also known to confer anti-allergic, anticancer, and wound healing activity.4 Overall, bilberry has also been reported to exert anti-inflammatory, lipid-lowering, and antimicrobial activity.3 In this column, the focus will be on the chemical constituents and properties of V. myrtillus that indicate potential or applicability for skin care.
Active ingredients of bilberry
Bilberry seed oil contains unsaturated fatty acids such as linoleic acid and alpha-linolenic acid, which exhibit anti-inflammatory activity and contribute to the suppression of tyrosinase. For instance, Ando et al. showed, in 1998, that linoleic and alpha-linolenic acids lighten UV-induced skin hyperpigmentation. Their in vitro experiments using cultured murine melanoma cells and in vivo study of the topical application of either acid to the UV-induced hyperpigmented dorsal skin of guinea pigs revealed pigment-lightening effects that they partly ascribed to inhibited melanin synthesis by active melanocytes and accelerated desquamation of epidermal melanin pigment.7
A 2009 comparative study of the anthocyanin composition as well as antimicrobial and antioxidant activities delivered by bilberry and blueberry fruits and their skins by Burdulis et al. revealed robust functions in both fruits. Cyanidin was found to be an active anthocyanidin in bilberry. Cultivars of both fruits demonstrated antimicrobial and antioxidant activity, with bilberry fruit skin demonstrating potent antiradical activity.8
The anthocyanins of V. myrtillus are reputed to impart protection against cardiovascular disorders, age-induced oxidative stress, inflammatory responses, and various degenerative conditions, as well ameliorate neuronal and cognitive brain functions and ocular health.6
In 2012, Bornsek et al. demonstrated that bilberry (and blueberry) anthocyanins function as potent intracellular antioxidants, which may account for their noted health benefits despite relatively low bioavailability.9
Six years later, a chemical composition study of wild bilberry found in Montenegro, Brasanac-Vukanovic et al. determined that chlorogenic acid was the most prevalent phenolic constituent, followed by protocatechuic acid, with resveratrol, isoquercetin, quercetin, and hyperoside also found to be abundant. In vitro assays indicated significant antioxidant activity exhibited by these compounds.10
Activity against allergic contact dermatitis
Yamaura et al. used a mouse model, in 2011, to determine that the anthocyanins from a bilberry extract attenuated various symptoms of chronic allergic contact dermatitis, particularly alleviating pruritus.8 A year later, Yamaura et al. used a BALB/c mouse model of allergic contact dermatitis to compare the antipruritic effect of anthocyanin-rich quality-controlled bilberry extract and anthocyanidin-rich degraded extract. The investigators found that anthocyanins, but not anthocyanidins, derived from bilberry exert an antipruritic effect, likely through their inhibitory action on mast cell degranulation. They concluded that anthocyanin-rich bilberry extract could act as an effective oral supplement to treat pruritic symptoms of skin disorders such as chronic allergic contact dermatitis and atopic dermatitis.11
Antioxidant and anti-inflammatory activity
Bilberries, consumed since ancient times, are reputed to function as potent antioxidants because of a wide array of phenolic constituents, and this fruit is gaining interest for use in pharmaceuticals.12
In 2008, Svobodová et al. assessed possible UVA preventive properties of V. myrtillus fruit extract in a human keratinocyte cell line (HaCaT), finding that pre- or posttreatment mitigated UVA-induced harm. They also observed a significant decrease in UVA-caused reactive oxygen species (ROS) formation and the prevention or attenuation of UVA-stimulated peroxidation of membrane lipids. Intracellular glutathione was also protected. The investigators attributed the array of cytoprotective effects conferred by V. myrtillus extract primarily to its constituent anthocyanins.2 A year later, they found that the phenolic fraction of V. myrtillus fruits inhibited UVB-induced damage to HaCaT keratinocytes in vitro.13
In 2014, Calò and Marabini used HaCaT keratinocytes to ascertain whether a water-soluble V. myrtillus extract could mitigate UVA- and UVB-induced damage. They found that the extract diminished UVB-induced cytotoxicity and genotoxicity at lower doses, decreasing lipid peroxidation but exerting no effect on reactive oxygen species generated by UVB. The extract attenuated genotoxicity induced by UVA as well as ROS and apoptosis. Overall, the investigators concluded that V. myrtillus extract demonstrated antioxidant activity, particularly against UVA exposure.14
Four years later, Bucci et al. developed nanoberries, an ultradeformable liposome carrying V. myrtillus ethanolic extract, and determined that the preparation could penetrate the stratum corneum safely and suggested potential for yielding protection against photodamage.15
Skin preparations
In 2021, Tadic et al. developed an oil-in-water (O/W) cream containing wild bilberry leaf extracts and seed oil. The leaves contained copious phenolic acids (particularly chlorogenic acid), flavonoids (especially isoquercetin), and resveratrol. The seed oil was rife with alpha-linolenic, linoleic, and oleic acids. The investigators conducted an in vivo study over 30 days in 25 healthy volunteers (20 women, 5 men; mean age 23.36 ± 0.64 years). They found that the O/W cream successfully increased stratum corneum hydration, enhanced skin barrier function, and maintained skin pH after topical application. The cream was also well tolerated. In vitro assays also indicated that the bilberry isolates displayed notable antioxidant capacity (stronger in the case of the leaves). Tadic et al. suggested that skin disorders characterized by oxidative stress and/or xerosis may be appropriate targets for topically applied bilberry cream.1
Early in 2022, Ruscinc et al. reported on their efforts to incorporate V. myrtillus extract into a multifunctional sunscreen. In vitro and in vivo tests revealed that while sun protection factor was lowered in the presence of the extract, the samples were safe and photostable. The researchers concluded that further study is necessary to elucidate the effect of V. myrtillus extract on photoprotection.16
V. myrtillus has been consumed by human beings for many generations. Skin care formulations based on this ingredient have not been associated with adverse events. Notably, the Environmental Working Group has rated V. myrtillus (bilberry seed) oil as very safe.17
Summary
While research, particularly in the form of randomized controlled trials, is called for, because the fatty acids it contains have been shown to suppress tyrosinase. Currently, this botanical agent seems to be most suited for sensitive, aging skin and for skin with an uneven tone, particularly postinflammatory pigmentation and melasma.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, an SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Tadic VM et al. Antioxidants (Basel). 2021 Mar 16;10(3):465.
2. Svobodová A et al. Biofactors. 2008;33(4):249-66.
3. Chu WK et al. Bilberry (Vaccinium myrtillus L.), in Benzie IFF, Wachtel-Galor S, eds., “Herbal Medicine: Biomolecular and Clinical Aspects,” 2nd ed. (Boca Raton, Fla.: CRC Press/Taylor & Francis, 2011, Chapter 4).
4. Yamaura K et al. Pharmacognosy Res. 2011 Jul;3(3):173-7.
5. Stefanescu BE et al. Molecules. 2019 May 29;24(11):2046.
6. Smeriglio A et al. Mini Rev Med Chem. 2014;14(7):567-84.
7. Ando H et al. Arch Dermatol Res. 1998 Jul;290(7):375-81.
8. Burdulis D et al. Acta Pol Pharm. 2009 Jul-Aug;66(4):399-408.
9. Bornsek SM et al. Food Chem. 2012 Oct 15;134(4):1878-84.
10. Brasanac-Vukanovic S et al. Molecules. 2018 Jul 26;23(8):1864.
11. Yamaura K et al. J Food Sci. 2012 Dec;77(12):H262-7.
12. Pires TCSP et al. Curr Pharm Des. 2020;26(16):1917-28.
13. Svobodová A et al. J Dermatol Sci. 2009 Dec;56(3):196-204.
14. Calò R, Marabini L. J Photochem Photobiol B. 2014 Mar 5;132:27-35.
15. Bucci P et al. J Cosmet Dermatol. 2018 Oct;17(5):889-99.
16. Ruscinc N et al. J Cosmet Dermatol. 2022 Jan 13.
17. Environmental Working Group’s Skin Deep website. Vaccinium Myrtillus Bilberry Seed Oil. Accessed October 18, 2022.
A member of the Ericaceae family, bilberry (Vaccinium myrtillus) is native to northern Europe and North America, and its fruit is known to contain myriad polyphenols that display potent antioxidant and anti-inflammatory activity.1,2 Also known as European blueberry or whortleberry, this perennial deciduous shrub is also one of the richest sources of the polyphenolic pigments anthocyanins.3-5 Indeed, anthocyanins impart the blue/black color to bilberries and other berries and are thought to be the primary bioactive constituents of berries associated with numerous health benefits.3,6 They are also known to confer anti-allergic, anticancer, and wound healing activity.4 Overall, bilberry has also been reported to exert anti-inflammatory, lipid-lowering, and antimicrobial activity.3 In this column, the focus will be on the chemical constituents and properties of V. myrtillus that indicate potential or applicability for skin care.
Active ingredients of bilberry
Bilberry seed oil contains unsaturated fatty acids such as linoleic acid and alpha-linolenic acid, which exhibit anti-inflammatory activity and contribute to the suppression of tyrosinase. For instance, Ando et al. showed, in 1998, that linoleic and alpha-linolenic acids lighten UV-induced skin hyperpigmentation. Their in vitro experiments using cultured murine melanoma cells and in vivo study of the topical application of either acid to the UV-induced hyperpigmented dorsal skin of guinea pigs revealed pigment-lightening effects that they partly ascribed to inhibited melanin synthesis by active melanocytes and accelerated desquamation of epidermal melanin pigment.7
A 2009 comparative study of the anthocyanin composition as well as antimicrobial and antioxidant activities delivered by bilberry and blueberry fruits and their skins by Burdulis et al. revealed robust functions in both fruits. Cyanidin was found to be an active anthocyanidin in bilberry. Cultivars of both fruits demonstrated antimicrobial and antioxidant activity, with bilberry fruit skin demonstrating potent antiradical activity.8
The anthocyanins of V. myrtillus are reputed to impart protection against cardiovascular disorders, age-induced oxidative stress, inflammatory responses, and various degenerative conditions, as well ameliorate neuronal and cognitive brain functions and ocular health.6
In 2012, Bornsek et al. demonstrated that bilberry (and blueberry) anthocyanins function as potent intracellular antioxidants, which may account for their noted health benefits despite relatively low bioavailability.9
Six years later, a chemical composition study of wild bilberry found in Montenegro, Brasanac-Vukanovic et al. determined that chlorogenic acid was the most prevalent phenolic constituent, followed by protocatechuic acid, with resveratrol, isoquercetin, quercetin, and hyperoside also found to be abundant. In vitro assays indicated significant antioxidant activity exhibited by these compounds.10
Activity against allergic contact dermatitis
Yamaura et al. used a mouse model, in 2011, to determine that the anthocyanins from a bilberry extract attenuated various symptoms of chronic allergic contact dermatitis, particularly alleviating pruritus.8 A year later, Yamaura et al. used a BALB/c mouse model of allergic contact dermatitis to compare the antipruritic effect of anthocyanin-rich quality-controlled bilberry extract and anthocyanidin-rich degraded extract. The investigators found that anthocyanins, but not anthocyanidins, derived from bilberry exert an antipruritic effect, likely through their inhibitory action on mast cell degranulation. They concluded that anthocyanin-rich bilberry extract could act as an effective oral supplement to treat pruritic symptoms of skin disorders such as chronic allergic contact dermatitis and atopic dermatitis.11
Antioxidant and anti-inflammatory activity
Bilberries, consumed since ancient times, are reputed to function as potent antioxidants because of a wide array of phenolic constituents, and this fruit is gaining interest for use in pharmaceuticals.12
In 2008, Svobodová et al. assessed possible UVA preventive properties of V. myrtillus fruit extract in a human keratinocyte cell line (HaCaT), finding that pre- or posttreatment mitigated UVA-induced harm. They also observed a significant decrease in UVA-caused reactive oxygen species (ROS) formation and the prevention or attenuation of UVA-stimulated peroxidation of membrane lipids. Intracellular glutathione was also protected. The investigators attributed the array of cytoprotective effects conferred by V. myrtillus extract primarily to its constituent anthocyanins.2 A year later, they found that the phenolic fraction of V. myrtillus fruits inhibited UVB-induced damage to HaCaT keratinocytes in vitro.13
In 2014, Calò and Marabini used HaCaT keratinocytes to ascertain whether a water-soluble V. myrtillus extract could mitigate UVA- and UVB-induced damage. They found that the extract diminished UVB-induced cytotoxicity and genotoxicity at lower doses, decreasing lipid peroxidation but exerting no effect on reactive oxygen species generated by UVB. The extract attenuated genotoxicity induced by UVA as well as ROS and apoptosis. Overall, the investigators concluded that V. myrtillus extract demonstrated antioxidant activity, particularly against UVA exposure.14
Four years later, Bucci et al. developed nanoberries, an ultradeformable liposome carrying V. myrtillus ethanolic extract, and determined that the preparation could penetrate the stratum corneum safely and suggested potential for yielding protection against photodamage.15
Skin preparations
In 2021, Tadic et al. developed an oil-in-water (O/W) cream containing wild bilberry leaf extracts and seed oil. The leaves contained copious phenolic acids (particularly chlorogenic acid), flavonoids (especially isoquercetin), and resveratrol. The seed oil was rife with alpha-linolenic, linoleic, and oleic acids. The investigators conducted an in vivo study over 30 days in 25 healthy volunteers (20 women, 5 men; mean age 23.36 ± 0.64 years). They found that the O/W cream successfully increased stratum corneum hydration, enhanced skin barrier function, and maintained skin pH after topical application. The cream was also well tolerated. In vitro assays also indicated that the bilberry isolates displayed notable antioxidant capacity (stronger in the case of the leaves). Tadic et al. suggested that skin disorders characterized by oxidative stress and/or xerosis may be appropriate targets for topically applied bilberry cream.1
Early in 2022, Ruscinc et al. reported on their efforts to incorporate V. myrtillus extract into a multifunctional sunscreen. In vitro and in vivo tests revealed that while sun protection factor was lowered in the presence of the extract, the samples were safe and photostable. The researchers concluded that further study is necessary to elucidate the effect of V. myrtillus extract on photoprotection.16
V. myrtillus has been consumed by human beings for many generations. Skin care formulations based on this ingredient have not been associated with adverse events. Notably, the Environmental Working Group has rated V. myrtillus (bilberry seed) oil as very safe.17
Summary
While research, particularly in the form of randomized controlled trials, is called for, because the fatty acids it contains have been shown to suppress tyrosinase. Currently, this botanical agent seems to be most suited for sensitive, aging skin and for skin with an uneven tone, particularly postinflammatory pigmentation and melasma.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, an SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Tadic VM et al. Antioxidants (Basel). 2021 Mar 16;10(3):465.
2. Svobodová A et al. Biofactors. 2008;33(4):249-66.
3. Chu WK et al. Bilberry (Vaccinium myrtillus L.), in Benzie IFF, Wachtel-Galor S, eds., “Herbal Medicine: Biomolecular and Clinical Aspects,” 2nd ed. (Boca Raton, Fla.: CRC Press/Taylor & Francis, 2011, Chapter 4).
4. Yamaura K et al. Pharmacognosy Res. 2011 Jul;3(3):173-7.
5. Stefanescu BE et al. Molecules. 2019 May 29;24(11):2046.
6. Smeriglio A et al. Mini Rev Med Chem. 2014;14(7):567-84.
7. Ando H et al. Arch Dermatol Res. 1998 Jul;290(7):375-81.
8. Burdulis D et al. Acta Pol Pharm. 2009 Jul-Aug;66(4):399-408.
9. Bornsek SM et al. Food Chem. 2012 Oct 15;134(4):1878-84.
10. Brasanac-Vukanovic S et al. Molecules. 2018 Jul 26;23(8):1864.
11. Yamaura K et al. J Food Sci. 2012 Dec;77(12):H262-7.
12. Pires TCSP et al. Curr Pharm Des. 2020;26(16):1917-28.
13. Svobodová A et al. J Dermatol Sci. 2009 Dec;56(3):196-204.
14. Calò R, Marabini L. J Photochem Photobiol B. 2014 Mar 5;132:27-35.
15. Bucci P et al. J Cosmet Dermatol. 2018 Oct;17(5):889-99.
16. Ruscinc N et al. J Cosmet Dermatol. 2022 Jan 13.
17. Environmental Working Group’s Skin Deep website. Vaccinium Myrtillus Bilberry Seed Oil. Accessed October 18, 2022.
The ‘root cause’ visit
“How did we miss out on that?” “What?” my physician friend replied as we stood in line at the coffee cart. “Root cause. I mean, we invented this idea and now all these naturopaths and functional medicine quacks are gettin’ rich off it.” “Take it easy,” he says. “Just order a coffee.”
It’s hard not to be indignant. I had a morning clinic with three patients insisting I find the “root cause” of their problem. Now, if one had flagellate dermatitis after eating Asian mushroom soup, I’d have said “Root cause? Shiitake mushrooms!” and walked out like Costanza in Seinfeld, “All right, that’s it for me! Be good everybody!”
Alas no. They had perioral dermatitis, alopecia areata, eczema – no satisfying “roots” for walk-off answers.
There is a universal desire to find the proximal cause for problems. Patients often want to know it so that we address the root of their trouble and not just cut off the branches. This is deeply gratifying for those who want not only to know why, but also to have agency in how to control their disease. For example, if they believe the root cause of perioral dermatitis was excess yeast, then eating a “candida diet’’ should do the trick! Food sensitivities, hormones, and heavy metals round out the top suspects that root cause patients want to talk about.
Of course, patients have been asking about this for a long time, but lately, the root cause visit seems to be on trend. Check out any hip primary care start-up such as One Medical or any hot direct-to-consumer virtual offering such as ParsleyHealth and you will see root-cause everywhere. Our patients are expecting us to address it, or it seems they will find someone cooler who will.
Yet, it wasn’t the slick marketing team at ParsleyHeath who invented the “root cause doctor visit.” We did. It’s an idea that started with our Greek physician ancestors. Breaking from the diviners and priests, we were the first “naturalists” positing that there was a natural, not a divine cause for illness. The cardinal concept in the Hippocratic Corpus was that health was an equilibrium and illness an imbalance. They didn’t have dehydroepiandrosterone tests or mercury levels, but did have bodily fluids. Yellow bile, black bile, blood, and phlegm, were the root of all root causes. A physician simply had to identify which was in excess or deficient and fix that to cure the disease. Interestingly, the word “diagnosis” appears only once in the Corpus. The word “Diagignoskein” appears occasionally but this describes studying thoroughly, not naming a diagnosis as we understand it.
Advances in chemistry in the 17th century meant physicians could add new theories, and new root causes. Now alkaline or other chemical elixirs were added to cure at the source. Since there was no verifiable evidence to prove causes, theories were adopted to provide some rational direction to treatment. In the 18th century, physicians such as Dr. Benjamin Rush, one of the original faculty at the University of Pennsylvania school of medicine, taught that spasms of the arteries were the root cause of illnesses. “Heroic” treatments such as extreme bloodletting were the cure. (Note, those patients who survived us kept coming back to us for more).
Scientific knowledge and diagnostic technologies led to more and more complex and abstruse causes. Yet, as we became more precise and effective, our explanations became less satisfying to our patients. I can diagnose and readily treat perioral dermatitis, yet I’m hard pressed to give an answer to its root cause. “Root cause? Yes. Just apply this pimecrolimus cream for a couple of weeks and it’ll be better! All right, that’s it for me! Be good everybody!”
You’ll have to do better, George.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
“How did we miss out on that?” “What?” my physician friend replied as we stood in line at the coffee cart. “Root cause. I mean, we invented this idea and now all these naturopaths and functional medicine quacks are gettin’ rich off it.” “Take it easy,” he says. “Just order a coffee.”
It’s hard not to be indignant. I had a morning clinic with three patients insisting I find the “root cause” of their problem. Now, if one had flagellate dermatitis after eating Asian mushroom soup, I’d have said “Root cause? Shiitake mushrooms!” and walked out like Costanza in Seinfeld, “All right, that’s it for me! Be good everybody!”
Alas no. They had perioral dermatitis, alopecia areata, eczema – no satisfying “roots” for walk-off answers.
There is a universal desire to find the proximal cause for problems. Patients often want to know it so that we address the root of their trouble and not just cut off the branches. This is deeply gratifying for those who want not only to know why, but also to have agency in how to control their disease. For example, if they believe the root cause of perioral dermatitis was excess yeast, then eating a “candida diet’’ should do the trick! Food sensitivities, hormones, and heavy metals round out the top suspects that root cause patients want to talk about.
Of course, patients have been asking about this for a long time, but lately, the root cause visit seems to be on trend. Check out any hip primary care start-up such as One Medical or any hot direct-to-consumer virtual offering such as ParsleyHealth and you will see root-cause everywhere. Our patients are expecting us to address it, or it seems they will find someone cooler who will.
Yet, it wasn’t the slick marketing team at ParsleyHeath who invented the “root cause doctor visit.” We did. It’s an idea that started with our Greek physician ancestors. Breaking from the diviners and priests, we were the first “naturalists” positing that there was a natural, not a divine cause for illness. The cardinal concept in the Hippocratic Corpus was that health was an equilibrium and illness an imbalance. They didn’t have dehydroepiandrosterone tests or mercury levels, but did have bodily fluids. Yellow bile, black bile, blood, and phlegm, were the root of all root causes. A physician simply had to identify which was in excess or deficient and fix that to cure the disease. Interestingly, the word “diagnosis” appears only once in the Corpus. The word “Diagignoskein” appears occasionally but this describes studying thoroughly, not naming a diagnosis as we understand it.
Advances in chemistry in the 17th century meant physicians could add new theories, and new root causes. Now alkaline or other chemical elixirs were added to cure at the source. Since there was no verifiable evidence to prove causes, theories were adopted to provide some rational direction to treatment. In the 18th century, physicians such as Dr. Benjamin Rush, one of the original faculty at the University of Pennsylvania school of medicine, taught that spasms of the arteries were the root cause of illnesses. “Heroic” treatments such as extreme bloodletting were the cure. (Note, those patients who survived us kept coming back to us for more).
Scientific knowledge and diagnostic technologies led to more and more complex and abstruse causes. Yet, as we became more precise and effective, our explanations became less satisfying to our patients. I can diagnose and readily treat perioral dermatitis, yet I’m hard pressed to give an answer to its root cause. “Root cause? Yes. Just apply this pimecrolimus cream for a couple of weeks and it’ll be better! All right, that’s it for me! Be good everybody!”
You’ll have to do better, George.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
“How did we miss out on that?” “What?” my physician friend replied as we stood in line at the coffee cart. “Root cause. I mean, we invented this idea and now all these naturopaths and functional medicine quacks are gettin’ rich off it.” “Take it easy,” he says. “Just order a coffee.”
It’s hard not to be indignant. I had a morning clinic with three patients insisting I find the “root cause” of their problem. Now, if one had flagellate dermatitis after eating Asian mushroom soup, I’d have said “Root cause? Shiitake mushrooms!” and walked out like Costanza in Seinfeld, “All right, that’s it for me! Be good everybody!”
Alas no. They had perioral dermatitis, alopecia areata, eczema – no satisfying “roots” for walk-off answers.
There is a universal desire to find the proximal cause for problems. Patients often want to know it so that we address the root of their trouble and not just cut off the branches. This is deeply gratifying for those who want not only to know why, but also to have agency in how to control their disease. For example, if they believe the root cause of perioral dermatitis was excess yeast, then eating a “candida diet’’ should do the trick! Food sensitivities, hormones, and heavy metals round out the top suspects that root cause patients want to talk about.
Of course, patients have been asking about this for a long time, but lately, the root cause visit seems to be on trend. Check out any hip primary care start-up such as One Medical or any hot direct-to-consumer virtual offering such as ParsleyHealth and you will see root-cause everywhere. Our patients are expecting us to address it, or it seems they will find someone cooler who will.
Yet, it wasn’t the slick marketing team at ParsleyHeath who invented the “root cause doctor visit.” We did. It’s an idea that started with our Greek physician ancestors. Breaking from the diviners and priests, we were the first “naturalists” positing that there was a natural, not a divine cause for illness. The cardinal concept in the Hippocratic Corpus was that health was an equilibrium and illness an imbalance. They didn’t have dehydroepiandrosterone tests or mercury levels, but did have bodily fluids. Yellow bile, black bile, blood, and phlegm, were the root of all root causes. A physician simply had to identify which was in excess or deficient and fix that to cure the disease. Interestingly, the word “diagnosis” appears only once in the Corpus. The word “Diagignoskein” appears occasionally but this describes studying thoroughly, not naming a diagnosis as we understand it.
Advances in chemistry in the 17th century meant physicians could add new theories, and new root causes. Now alkaline or other chemical elixirs were added to cure at the source. Since there was no verifiable evidence to prove causes, theories were adopted to provide some rational direction to treatment. In the 18th century, physicians such as Dr. Benjamin Rush, one of the original faculty at the University of Pennsylvania school of medicine, taught that spasms of the arteries were the root cause of illnesses. “Heroic” treatments such as extreme bloodletting were the cure. (Note, those patients who survived us kept coming back to us for more).
Scientific knowledge and diagnostic technologies led to more and more complex and abstruse causes. Yet, as we became more precise and effective, our explanations became less satisfying to our patients. I can diagnose and readily treat perioral dermatitis, yet I’m hard pressed to give an answer to its root cause. “Root cause? Yes. Just apply this pimecrolimus cream for a couple of weeks and it’ll be better! All right, that’s it for me! Be good everybody!”
You’ll have to do better, George.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Since when does providing pediatric care require courage?
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
I have been noticing “jokes” lately about doctors. Magazine cartoons depict doctors as conveying a bad prognosis in abrupt, indirect, vague ways. I remember, from medical school, the joke about pediatricians being doctors for patients “from the waist up” – wimps about tough topics such as sexuality. As an inherently shy person, I have appreciated the structure of the contractual relationship with families that both gives me permission and requires me to be direct about topics that would not be socially acceptable to discuss in other relationships.
Examples include our asking about bowel movements, genital symptoms, marital conflict, past abortions, food insecurity, adherence to medication, history of trauma or discrimination, substance use, illegal conduct, and suicidal ideation, among others. By bringing up these topics nonjudgmentally and with skill, we are demonstrating openness and making it safe for the patient/parent to ask questions about their own concerns.
Since these may be topics for which we lack knowledge or have very little power to help, it is far easier to not bring them up. Yet failing to have the courage to elicit sensitive information may delay the correct diagnosis, result in inappropriate tests or treatments, or miss factors critical in either the cause or solution for the patient’s problems.
Historically, being a physician has conveyed a promise of confidentiality and always trying to do what is best for the patient. The fact that we had to swear an oath to do so may also indicate that these things are not easy to do.
Yes, we need a lot of knowledge to know what is truly in the patient’s best interest. But we need to take personal risks to do it as well. There have been times when a parent has shouted “That is none of your business” at me or stormed out. Although only one patient has ever connected when striking out at me, other clinicians have not been as lucky (or had such small patients); some have even been killed.
For those of us in private practice, upsetting a patient with our well-intentioned words may mean losing them from our income stream or having them post negative comments online, which may affect our reputation in the community. Patients may not return for needed follow-up if a conversation was too uncomfortable for them. Current political divisions make this even trickier.
These days anxiety about getting behind in seeing the next patient may be a covert reason for avoiding difficult conversations as tears or anger take extra time. Certainly, fears of these outcomes can make us hold back from talking about important but potentially upsetting topics.
Of course, courage does not just mean being direct with questions, stating your observations, or giving advice. Courage requires thoughtfulness about possible adverse outcomes and their effect on others. It is not just “stupid bravery,” to proceed even when sensing danger. Courage is thus best paired with skill. It is:
- Setting up potentially difficult discussions with privacy (from the child or parent), seating, and enough time to listen.
- Normalizing questions by saying “I ask all my patients about ...” so patients do not feel singled out.
- Asking the patient or family first what they think is going on and how their own culture might regard the issue.
- Using simple language and arranging a translator when needed.
- Not just stating facts but checking “to be sure I explained well enough” rather than setting a patient up to appear ignorant for not understanding.
- Offering to contact the patient or other family member/support soon to review what you said and answer more questions.
- Offering a second opinion option.
- Promising to get more information when you do not know.
- Always leaving room for hope and sharing in that hope with them.
And it is crucial to have a way to keep notes about past trauma or difficult topics for a patient so neither you nor subsequent clinicians unnecessarily ask about sensitive topics.
Courage includes facing difficult situations without undue delay. Making that call about an abnormal test result right away, even when you are tired and upset, takes courage. Each time you overcome your own reluctance it takes moral strength but tends to make future courageous acts easier. Speaking up to a specialist on rounds when you think he or she is incorrect takes courage to serve the patient’s best interest. Being willing to try a new workflow in your office takes the courage to risk looking awkward or being judged by your team, but can be essential to progress. Asking for help or an opinion, sometimes from a medical assistant or student, can take courage but may reduce status barriers and improve relationships. Standing up for your values when they are not popular may take courage in some organizations. It takes courage to admit a mistake, even when your mistake may not otherwise be noticed.
How can we grow in courage? T. Berry Brazelton, MD, was a model of courage for me during my training – able and willing to tell about a child’s delays or ask about a parent’s well-being with empathy and by giving hope. Dr. Brazelton, pediatrician, developer of the Neonatal Behavioral Assessment Scale, professor at Harvard Medical School and founder of its Child Development Unit, was a world-renowned educator about the development of children and founder of the Touchpoints program. Our goal should be to promise to partner with the family in dealing with the problem, no matter how difficult or tender. I hope you had role models who not only said what to do but also demonstrated it with patients.
We had the privilege of hearing stories of difficult situations from hundreds of pediatricians in group sessions over the years in the Collaborative Office Rounds program. What group members often said that they valued most from these sessions was hearing examples of words they might say in these cases, either modeled by the coleaders or suggested by their pediatrician peers. Opportunities to share the tough times with trusted empathic peers is an important resource rarer and thus even more worth securing for yourself.
Being courageous may not be natural part of your personality but Aristotle said, “We become what we repeatedly do.” Even if you do not consider yourself so now, with practice you can become courageous and reap its benefits for your patients and yourself.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Drug abusers will find a way
Recently, when I logged on to see what medication refills had come in, I was greeted with a notice that Walgreens would no longer carry promethazine/codeine cough syrup. It wouldn’t surprise me if other pharmacies follow.
This doesn’t affect me much. As a neurologist I’ve never prescribed it, and as a patient I’ve never used it.
The unwritten reason was likely because of its popularity for abuse. It is often mixed with various beverages and called “purple drank.” It has both social, and legal, consequences that can come back and bite the pharmacy.
A friend of mine commented that if everything that can be abused gets banned, all we’ll be left with are Tylenol and Preparation H. Another friend made the comment that it’s a shame, because codeine is a remarkably effective antitussive.
I agree with both of them, but Walgreens is pulling only the combo preparation off the shelves. Codeine and promethazine are still available. The former is on WHO’s list of essential medications.
They’d still find a way to get the components and whip up some equivalent. Human innovation can be remarkable. All of us who trained in the inner city (which is pretty much all of us at some point) have seen people who drank mouthwash, hairspray, and who knows what else in desperation.
No one believes it’s going to stop drug abuse, but it will make it harder to have purple drank, which is often passed around as a low-level drug at parties. Putting Sudafed behind the counter has reduced, though not stopped, meth. Walter White can tell you that.
A patient of mine who’s a pharmacist also was talking about this. He’s in favor of it, as he’s tired of dealing with people trying to get it through faked prescriptions and bogus visits to urgent care pretending to have a cough, not to mention the additional paperwork and reporting requirements that a controlled drug carries.
I agree with it, mostly, but there are those who truly do need it at times, and who now will have to take it as individual components, or find a pharmacy that does carry it. The issue here becomes that, by punishing the abusers, you’re also punishing the responsible.
The vast majority of alcohol users are responsible drinkers. I have the occasional beer myself. Unfortunately, there are a comparative few who aren’t, and their actions can bring tremendous grief to many others. So we have tougher laws all around that we all have to follow.
I agree with Walgreens actions on this, but still find myself wondering how much of a difference it will make.
Probably not as much as I hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, when I logged on to see what medication refills had come in, I was greeted with a notice that Walgreens would no longer carry promethazine/codeine cough syrup. It wouldn’t surprise me if other pharmacies follow.
This doesn’t affect me much. As a neurologist I’ve never prescribed it, and as a patient I’ve never used it.
The unwritten reason was likely because of its popularity for abuse. It is often mixed with various beverages and called “purple drank.” It has both social, and legal, consequences that can come back and bite the pharmacy.
A friend of mine commented that if everything that can be abused gets banned, all we’ll be left with are Tylenol and Preparation H. Another friend made the comment that it’s a shame, because codeine is a remarkably effective antitussive.
I agree with both of them, but Walgreens is pulling only the combo preparation off the shelves. Codeine and promethazine are still available. The former is on WHO’s list of essential medications.
They’d still find a way to get the components and whip up some equivalent. Human innovation can be remarkable. All of us who trained in the inner city (which is pretty much all of us at some point) have seen people who drank mouthwash, hairspray, and who knows what else in desperation.
No one believes it’s going to stop drug abuse, but it will make it harder to have purple drank, which is often passed around as a low-level drug at parties. Putting Sudafed behind the counter has reduced, though not stopped, meth. Walter White can tell you that.
A patient of mine who’s a pharmacist also was talking about this. He’s in favor of it, as he’s tired of dealing with people trying to get it through faked prescriptions and bogus visits to urgent care pretending to have a cough, not to mention the additional paperwork and reporting requirements that a controlled drug carries.
I agree with it, mostly, but there are those who truly do need it at times, and who now will have to take it as individual components, or find a pharmacy that does carry it. The issue here becomes that, by punishing the abusers, you’re also punishing the responsible.
The vast majority of alcohol users are responsible drinkers. I have the occasional beer myself. Unfortunately, there are a comparative few who aren’t, and their actions can bring tremendous grief to many others. So we have tougher laws all around that we all have to follow.
I agree with Walgreens actions on this, but still find myself wondering how much of a difference it will make.
Probably not as much as I hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, when I logged on to see what medication refills had come in, I was greeted with a notice that Walgreens would no longer carry promethazine/codeine cough syrup. It wouldn’t surprise me if other pharmacies follow.
This doesn’t affect me much. As a neurologist I’ve never prescribed it, and as a patient I’ve never used it.
The unwritten reason was likely because of its popularity for abuse. It is often mixed with various beverages and called “purple drank.” It has both social, and legal, consequences that can come back and bite the pharmacy.
A friend of mine commented that if everything that can be abused gets banned, all we’ll be left with are Tylenol and Preparation H. Another friend made the comment that it’s a shame, because codeine is a remarkably effective antitussive.
I agree with both of them, but Walgreens is pulling only the combo preparation off the shelves. Codeine and promethazine are still available. The former is on WHO’s list of essential medications.
They’d still find a way to get the components and whip up some equivalent. Human innovation can be remarkable. All of us who trained in the inner city (which is pretty much all of us at some point) have seen people who drank mouthwash, hairspray, and who knows what else in desperation.
No one believes it’s going to stop drug abuse, but it will make it harder to have purple drank, which is often passed around as a low-level drug at parties. Putting Sudafed behind the counter has reduced, though not stopped, meth. Walter White can tell you that.
A patient of mine who’s a pharmacist also was talking about this. He’s in favor of it, as he’s tired of dealing with people trying to get it through faked prescriptions and bogus visits to urgent care pretending to have a cough, not to mention the additional paperwork and reporting requirements that a controlled drug carries.
I agree with it, mostly, but there are those who truly do need it at times, and who now will have to take it as individual components, or find a pharmacy that does carry it. The issue here becomes that, by punishing the abusers, you’re also punishing the responsible.
The vast majority of alcohol users are responsible drinkers. I have the occasional beer myself. Unfortunately, there are a comparative few who aren’t, and their actions can bring tremendous grief to many others. So we have tougher laws all around that we all have to follow.
I agree with Walgreens actions on this, but still find myself wondering how much of a difference it will make.
Probably not as much as I hope.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.