User login
Official Newspaper of the American College of Surgeons
VIDEO: Complications increase with bilateral mastectomy and reconstruction
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO – Women undergoing mastectomy and breast reconstruction for the treatment of breast cancer are more likely to develop perioperative complications if they opt for prophylactic mastectomy of the other breast at the same time, a study of 18,229 cases found.
Compared with women who had a unilateral mastectomy and reconstruction, the 36% of patients who chose bilateral mastectomy and reconstruction were 55% more likely to lose a breast implant (if implants were used for reconstruction), twice as likely to need a transfusion regardless of whether the reconstruction used implants or autologous material, and twice as likely to remain hospitalized for at least 2 days regardless of reconstruction method, Dr. Amanda K. Silva and her associates reported in a poster presentation at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
The reconstruction used implants in 89% of women undergoing bilateral mastectomy and 79% of those getting unilateral mastectomy, Dr. Silva and her colleagues reported.
The overall rate of complications was low, however, averaging 5%, said Dr. Silva, a surgeon at the University of Chicago, and her associates.
In this video interview, Dr. Silva discusses factors that physicians and patients should consider when choosing unilateral or bilateral mastectomy and reconstruction.
Previous studies have compared the risks of unilateral versus bilateral mastectomy without reconstruction, she said, and this study provides some of the first data of risks from either type of mastectomy with reconstruction.
Dr. Silva reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ASCO BREAST CANCER SYMPOSIUM
Quick tips for taming toxic feelings
Our team has been involved with a patient whose hospital stay is measured not in days, weeks, or months but in years. The scope of the problems surrounding not only the medical issues but also the family dynamic, out-of-hospital support system, and social situation can easily make the most seasoned providers feel paralyzed. It is fair to use words such as helpless, hopeless, overwhelmed, angry, confused, and conflicted for how the dozens of team members caring for this patient feel on a regular basis.
While the details of this case would eat up multiple columns, it might better for the reader to recall when a patient whose case you’ve been involved in has brought out strong, and often times, negative emotions from the faculty and staff that resulted in conflict. Finding a path to resolve conflict can be one of the most rewarding aspects of working within a system that relies on teamwork for desired, successful outcomes.
Toxic feelings build up easily in cases in which it seems like there is no end, no chance for our good intentions and hard work to salvage a patient’s spiraling course. Conflict with those we work with is almost inevitable. Hospitalists disagree with the surgeons, nursing staff and the pain team aren’t on the same page, hospital administration might seem to have the C-suite agenda. It is in times like this that conflict resolution smarts can preserve the peace. While maintaining a collegial attitude might not ultimately transform the patient’s outcome, the presence of on-going conflict amongst health care professionals is well studied and studded with unwanted outcomes.
There are conflict resolution books, courses, and even graduate degrees. For the hospitalist on the run, what principles can be applied immediately?
• Don’t react. Think it through. Emotions are strong and feelings differ. This is the crucible for doing something we might later regret. If you hear or read something that makes you upset, then first assume that your colleague has attempted to craft the absolute best plan for the patient. Before making statements or casting judgment, ask many questions. Never send a text or e-mail, make a phone call, or approach someone when you’re having trouble suppressing strong emotions.
• Practice active listening. This takes concentration, so rid yourself of distractions while engaging in listening. Use body language such as smiling or nodding to acknowledge the other person’s message. Pay attention to their gesticulations and nonverbal cues to their position. Avoid interruptions and defer judgment until they have finished. Summarize what you’ve heard from them to demonstrate that their message has been received. Even when you heartily disagree, show respect. We have the ability to find ways of being both candid and kind in our responses.
• Always go after the problem. It is too easy to attack a person rather than the underlying issue. Everyone involved in the care of a patient has the potential to contribute to the solution. By staying focused on the problem and not the people, you are building trust with your colleagues.
• Continue to show up. We all tire and become jaded with these marathon cases. Throwing your hands up in surrender and failing to remain a participating member of the team will send a message that you are not accepting responsibility. Showing up shouts that you’re committed.
• Be mindful of the words used in communication. Focus on "I" statements rather than "You" statements.As in "I need feedback on the plan of care I’ve proposed," rather than "You haven’t provided me with feedback on my plan." ... "I need more information before deciding on whether this procedure would be beneficial," rather than, "You haven’t told me why the procedure needs to be done now."
• Find common goals. Don’t spend time picking apart a nurse’s point of view or your consultant’s idea to work-up diagnoses that seem farfetched. Instead agree upon a goal or two and ask how we can get there together.
• Look toward tomorrow. Focusing on what has happened in the past leads only to war, litigation, or stagnation. Talking about how you can go forward from here can help reset the dynamic.
Like negotiation tools we’ve previously written about conflict resolution skills have broad applicability outside the work place and can make life better in a variety of situations.
As always if you’d like suggested readings or resources please contact us.
Dr. Bekanich and Dr. Leigh A. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern residency programs in Austin. They alternate contributions to the monthly Palliatively Speaking blog.
Our team has been involved with a patient whose hospital stay is measured not in days, weeks, or months but in years. The scope of the problems surrounding not only the medical issues but also the family dynamic, out-of-hospital support system, and social situation can easily make the most seasoned providers feel paralyzed. It is fair to use words such as helpless, hopeless, overwhelmed, angry, confused, and conflicted for how the dozens of team members caring for this patient feel on a regular basis.
While the details of this case would eat up multiple columns, it might better for the reader to recall when a patient whose case you’ve been involved in has brought out strong, and often times, negative emotions from the faculty and staff that resulted in conflict. Finding a path to resolve conflict can be one of the most rewarding aspects of working within a system that relies on teamwork for desired, successful outcomes.
Toxic feelings build up easily in cases in which it seems like there is no end, no chance for our good intentions and hard work to salvage a patient’s spiraling course. Conflict with those we work with is almost inevitable. Hospitalists disagree with the surgeons, nursing staff and the pain team aren’t on the same page, hospital administration might seem to have the C-suite agenda. It is in times like this that conflict resolution smarts can preserve the peace. While maintaining a collegial attitude might not ultimately transform the patient’s outcome, the presence of on-going conflict amongst health care professionals is well studied and studded with unwanted outcomes.
There are conflict resolution books, courses, and even graduate degrees. For the hospitalist on the run, what principles can be applied immediately?
• Don’t react. Think it through. Emotions are strong and feelings differ. This is the crucible for doing something we might later regret. If you hear or read something that makes you upset, then first assume that your colleague has attempted to craft the absolute best plan for the patient. Before making statements or casting judgment, ask many questions. Never send a text or e-mail, make a phone call, or approach someone when you’re having trouble suppressing strong emotions.
• Practice active listening. This takes concentration, so rid yourself of distractions while engaging in listening. Use body language such as smiling or nodding to acknowledge the other person’s message. Pay attention to their gesticulations and nonverbal cues to their position. Avoid interruptions and defer judgment until they have finished. Summarize what you’ve heard from them to demonstrate that their message has been received. Even when you heartily disagree, show respect. We have the ability to find ways of being both candid and kind in our responses.
• Always go after the problem. It is too easy to attack a person rather than the underlying issue. Everyone involved in the care of a patient has the potential to contribute to the solution. By staying focused on the problem and not the people, you are building trust with your colleagues.
• Continue to show up. We all tire and become jaded with these marathon cases. Throwing your hands up in surrender and failing to remain a participating member of the team will send a message that you are not accepting responsibility. Showing up shouts that you’re committed.
• Be mindful of the words used in communication. Focus on "I" statements rather than "You" statements.As in "I need feedback on the plan of care I’ve proposed," rather than "You haven’t provided me with feedback on my plan." ... "I need more information before deciding on whether this procedure would be beneficial," rather than, "You haven’t told me why the procedure needs to be done now."
• Find common goals. Don’t spend time picking apart a nurse’s point of view or your consultant’s idea to work-up diagnoses that seem farfetched. Instead agree upon a goal or two and ask how we can get there together.
• Look toward tomorrow. Focusing on what has happened in the past leads only to war, litigation, or stagnation. Talking about how you can go forward from here can help reset the dynamic.
Like negotiation tools we’ve previously written about conflict resolution skills have broad applicability outside the work place and can make life better in a variety of situations.
As always if you’d like suggested readings or resources please contact us.
Dr. Bekanich and Dr. Leigh A. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern residency programs in Austin. They alternate contributions to the monthly Palliatively Speaking blog.
Our team has been involved with a patient whose hospital stay is measured not in days, weeks, or months but in years. The scope of the problems surrounding not only the medical issues but also the family dynamic, out-of-hospital support system, and social situation can easily make the most seasoned providers feel paralyzed. It is fair to use words such as helpless, hopeless, overwhelmed, angry, confused, and conflicted for how the dozens of team members caring for this patient feel on a regular basis.
While the details of this case would eat up multiple columns, it might better for the reader to recall when a patient whose case you’ve been involved in has brought out strong, and often times, negative emotions from the faculty and staff that resulted in conflict. Finding a path to resolve conflict can be one of the most rewarding aspects of working within a system that relies on teamwork for desired, successful outcomes.
Toxic feelings build up easily in cases in which it seems like there is no end, no chance for our good intentions and hard work to salvage a patient’s spiraling course. Conflict with those we work with is almost inevitable. Hospitalists disagree with the surgeons, nursing staff and the pain team aren’t on the same page, hospital administration might seem to have the C-suite agenda. It is in times like this that conflict resolution smarts can preserve the peace. While maintaining a collegial attitude might not ultimately transform the patient’s outcome, the presence of on-going conflict amongst health care professionals is well studied and studded with unwanted outcomes.
There are conflict resolution books, courses, and even graduate degrees. For the hospitalist on the run, what principles can be applied immediately?
• Don’t react. Think it through. Emotions are strong and feelings differ. This is the crucible for doing something we might later regret. If you hear or read something that makes you upset, then first assume that your colleague has attempted to craft the absolute best plan for the patient. Before making statements or casting judgment, ask many questions. Never send a text or e-mail, make a phone call, or approach someone when you’re having trouble suppressing strong emotions.
• Practice active listening. This takes concentration, so rid yourself of distractions while engaging in listening. Use body language such as smiling or nodding to acknowledge the other person’s message. Pay attention to their gesticulations and nonverbal cues to their position. Avoid interruptions and defer judgment until they have finished. Summarize what you’ve heard from them to demonstrate that their message has been received. Even when you heartily disagree, show respect. We have the ability to find ways of being both candid and kind in our responses.
• Always go after the problem. It is too easy to attack a person rather than the underlying issue. Everyone involved in the care of a patient has the potential to contribute to the solution. By staying focused on the problem and not the people, you are building trust with your colleagues.
• Continue to show up. We all tire and become jaded with these marathon cases. Throwing your hands up in surrender and failing to remain a participating member of the team will send a message that you are not accepting responsibility. Showing up shouts that you’re committed.
• Be mindful of the words used in communication. Focus on "I" statements rather than "You" statements.As in "I need feedback on the plan of care I’ve proposed," rather than "You haven’t provided me with feedback on my plan." ... "I need more information before deciding on whether this procedure would be beneficial," rather than, "You haven’t told me why the procedure needs to be done now."
• Find common goals. Don’t spend time picking apart a nurse’s point of view or your consultant’s idea to work-up diagnoses that seem farfetched. Instead agree upon a goal or two and ask how we can get there together.
• Look toward tomorrow. Focusing on what has happened in the past leads only to war, litigation, or stagnation. Talking about how you can go forward from here can help reset the dynamic.
Like negotiation tools we’ve previously written about conflict resolution skills have broad applicability outside the work place and can make life better in a variety of situations.
As always if you’d like suggested readings or resources please contact us.
Dr. Bekanich and Dr. Leigh A. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern residency programs in Austin. They alternate contributions to the monthly Palliatively Speaking blog.
Open Payments may help drive malpractice claims; review period closes Sept. 11
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
NHLBI expert panel issues guideline on sickle cell disease
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
FROM JAMA
Major finding: The two most widely available disease-modifying therapies for SCD, hydroxyurea and long-term transfusions, are underused, in large part because no evidence-based treatment protocols have been devised until now.
Data source: A review of the literature and compilation of management guidelines "to assist health care professionals in the management of common issues of sickle cell disease."
Disclosures: The National Heart, Lung, and Blood Institute sponsored the development of this guideline. All expert panel members served voluntarily. Many reported numerous ties to industry sources.
High-dose statins don’t prevent postop AF
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
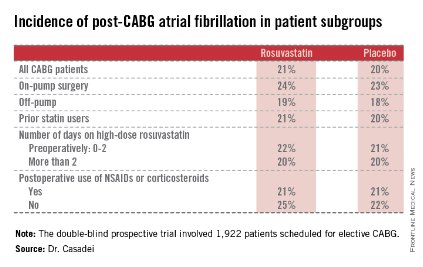
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.
AT THE ESC CONGRESS 2014
Key clinical point: Perioperative statin therapy in patients undergoing CABG failed to protect against new-onset postop atrial fibrillation.
Major finding: The incidence of postop atrial fibrillation within 5 days post-CABG was 21% in patients randomized to 20 mg/day of rosuvastatin and 20% in placebo-treated controls.
Data source: The multicenter STICS trial included 1,922 randomized patients scheduled for elective CABG.
Disclosures: STICS was funded by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. The presenter reported having received a research grant from AstraZeneca.
Risk of multidrug-resistant gram-negative infections rose 1% per day of hospitalization
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
WASHINGTON – With each day of hospitalization, the risk rises by 1% for contracting an infection with a gram-negative, multidrug-resistant organism, based on results from a single-hospital retrospective study.
While conventional wisdom holds that infection risk increases with duration of hospitalization, the study is the first to quantify the potential risk of contracting a multidrug-resistant infection based on length of stay. And while the results may not be applicable to all patients at all hospitals, the findings do give clinicians a sense of the risk posed by a prolonged stay, according to John A. Bosso, Pharm.D., a professor in the College of Pharmacy at the Medical University of South Carolina, Charleston.
Dr. Bosso and his colleagues focused on gram-negative organisms because a colleague had compiled data for 949 episodes of documented gram-negative infections that occurred between 1998 and 2011 at the university hospital. A statement issued at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy noted that the Centers for Disease Control and Prevention has estimated that on any given day, 1 in 25 hospitalized patients has at least one health care–associated infection, and about a third of these are caused by gram-negative bacteria.
The study defined drug-resistant organisms as those that did not respond to treatment with one or more agents in three or more antibiotic classes. The five classes of antibiotics used in the cases studied included aminoglycosides, penicillins, cephalosporins, fluoroquinolones, and folic acid inhibitors. The largest percentage of isolates (38%) was taken from patients with blood stream infections; 29% had pneumonia, 23% had surgical site infections, 6% had urinary tract infections, and 4% had other infections.
Of the 949 organisms reviewed, 251 (26%) were determined to be multidrug resistant.
Ultimately, the type of infection was found to be unrelated to whether a patient had a multidrug-resistant infection. Certain pathogens were more likely to be multidrug resistant. About 56% of Enterobacter isolates, for example, were multidrug resistant as compared with 20% of all other organisms. Alternatively, Pseudomonas isolates were 44% less likely than other isolates to be multidrug resistant.
Length of stay seemed to have the greatest impact on contracting multidrug-resistant strains of gram-negative organisms, with risk maximizing at 10 days of hospitalization. Each day of hospitalization increased the likelihood of multidrug resistance by 1%, Dr. Bosso said.
The researchers were unable to determine the proportion of patients who were already colonized with a multidrug-resistant strain at admission from those who acquired their infections while hospitalized, said Dr. Bosso.
Dr. Bosso reported no financial conflicts of interest.
On Twitter @aliciaault
AT ICAAC 2014
Key clinical point: Risk of multidrug-resistant gram-negative infections rise with length of stay.
Major finding: With each day of hospitalization, the risk of a multidrug resistant gram-negative infection rose by 1%.
Data source: A single-hospital review of 949 documented cases of gram-negative infections from 1998 to 2011.
Disclosures: The authors reported no financial conflicts.
Health care coverage down for 26- to 34-year-olds
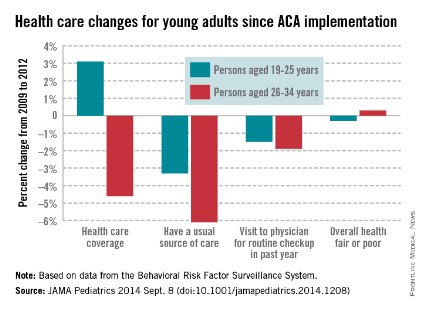
Health care coverage has increased for Americans aged 19-25 years but decreased for those aged 26-34 years since implementation of the Affordable Care Act in 2010, according to a study published online Sept. 8 in JAMA Pediatrics.
From 2009 to 2012, health care coverage rose 3.1% for 19- to 25-year-olds but decreased 4.6% among those aged 26-34. Both groups were less likely to have a usual source of care, but the decrease was larger for the older age group (–6.1% vs. –3.3%), Dr. Meera Kotagal of the University of Washington, Seattle, and her associates reported.
There was, however, no significant difference between the age groups for visits to a physician for a routine checkup in the past year, with 19- to 25-year-olds down 1.5% and 26- to 34-year-olds down 1.9%. The investigators noted that, despite these largely negative changes, there was no significant change in self-reported health status: –0.3% for those aged 19-25 and 0.3% for those aged 26-34.
"Young adults, given their overall healthy status, may not desire regular primary care, and thus an expansion in coverage may not lead these individuals to have a usual source. The proportion of young adults who reported a recent physician’s visit ... has declined yearly since 2003," Dr. Kotagal and her associates wrote (JAMA Pediatr. 2014 Sept. 8 (doi:10.1001/jamapediatrics.2014.1208).
This analysis was based on data for 2009 and 2012 from the Behavioral Risk Factor Surveillance System. The investigators did not report any conflicts of interest.

Health care coverage has increased for Americans aged 19-25 years but decreased for those aged 26-34 years since implementation of the Affordable Care Act in 2010, according to a study published online Sept. 8 in JAMA Pediatrics.
From 2009 to 2012, health care coverage rose 3.1% for 19- to 25-year-olds but decreased 4.6% among those aged 26-34. Both groups were less likely to have a usual source of care, but the decrease was larger for the older age group (–6.1% vs. –3.3%), Dr. Meera Kotagal of the University of Washington, Seattle, and her associates reported.
There was, however, no significant difference between the age groups for visits to a physician for a routine checkup in the past year, with 19- to 25-year-olds down 1.5% and 26- to 34-year-olds down 1.9%. The investigators noted that, despite these largely negative changes, there was no significant change in self-reported health status: –0.3% for those aged 19-25 and 0.3% for those aged 26-34.
"Young adults, given their overall healthy status, may not desire regular primary care, and thus an expansion in coverage may not lead these individuals to have a usual source. The proportion of young adults who reported a recent physician’s visit ... has declined yearly since 2003," Dr. Kotagal and her associates wrote (JAMA Pediatr. 2014 Sept. 8 (doi:10.1001/jamapediatrics.2014.1208).
This analysis was based on data for 2009 and 2012 from the Behavioral Risk Factor Surveillance System. The investigators did not report any conflicts of interest.

Health care coverage has increased for Americans aged 19-25 years but decreased for those aged 26-34 years since implementation of the Affordable Care Act in 2010, according to a study published online Sept. 8 in JAMA Pediatrics.
From 2009 to 2012, health care coverage rose 3.1% for 19- to 25-year-olds but decreased 4.6% among those aged 26-34. Both groups were less likely to have a usual source of care, but the decrease was larger for the older age group (–6.1% vs. –3.3%), Dr. Meera Kotagal of the University of Washington, Seattle, and her associates reported.
There was, however, no significant difference between the age groups for visits to a physician for a routine checkup in the past year, with 19- to 25-year-olds down 1.5% and 26- to 34-year-olds down 1.9%. The investigators noted that, despite these largely negative changes, there was no significant change in self-reported health status: –0.3% for those aged 19-25 and 0.3% for those aged 26-34.
"Young adults, given their overall healthy status, may not desire regular primary care, and thus an expansion in coverage may not lead these individuals to have a usual source. The proportion of young adults who reported a recent physician’s visit ... has declined yearly since 2003," Dr. Kotagal and her associates wrote (JAMA Pediatr. 2014 Sept. 8 (doi:10.1001/jamapediatrics.2014.1208).
This analysis was based on data for 2009 and 2012 from the Behavioral Risk Factor Surveillance System. The investigators did not report any conflicts of interest.

FROM JAMA PEDIATRICS
Federation finalizes telemedicine compact for legislative review
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
The Federation of State Medical Boards has completed the drafting of its interstate medical licensure compact and is ready for state legislatures to consider the proposal.
The proposed interstate compact would expedite the process of multistate physician licensure and help expand the practice of telemedicine. In a Sept. 5 statement, Dr. Humayun J. Chaudhry, CEO of the Federation of State Medical Boards (FSMB), said the compact’s language design is finished and that state legislatures and medical boards can now weigh adoption of the model legislation.
"The FSMB is pleased to have supported the state medical board community as it developed this compact to streamline licensure, while maintaining patient protection as a top priority," Dr. Chaudhry said in the statement.
The FSMB House of Delegates unanimously approved the development of an interstate compact to streamline medical licensure and facilitate multistate practice at its 2013 annual meeting. Under the proposed system, states and doctors would voluntarily enter into the compact, and approved physicians would be under the jurisdiction of the state medical board in which the patient was located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight, according to the proposed compact. The compact system is expected to significantly reduce barriers to the process of gaining licensure in multiple states, while helping to facilitate licensure portability and telemedicine.
The American Medical Association said the interstate compact aligns with its efforts to modernize state medical licensure and allow for an expedited pathway in participating states.
"State-based licensure is an important tenet of accountability, ensuring that physicians are qualified through the review of their education, training, character, and professional disciplinary histories," AMA President Dr. Robert M. Wah said in a statement. "We applaud the FSMB for developing the interstate compact and other reforms designed to simplify and improve the licensure process for physicians practicing across state lines as well as providing telemedicine services in multiple states."
Each individual state board will now work with their state legislators and stakeholder community to determine whether participation in the compact is ideal for their jurisdiction. The FSMB will continue to serve as a resource for interested states, the federation said. Four state boards have endorsed the compact thus far, and several more states have begun discussions with state legislators and other stakeholders in anticipation of introducing the model compact during the 2015 legislative session.
On Twitter @legal_med
Young adults using emergency departments less in post-ACA world
Young adults are using emergency departments less following the implementation of expanded coverage under the Affordable Care Act, though the number of patients from this population has not significantly changed.
According to new research published in Health Affairs, ED visits by young adults increased by 3.8 visits/1,000 people between pre-ACA implementation (Sept. 1, 2009-Aug. 31, 2010) and post-ACA implementation (2011 calendar year), while the control group of adults ages 26-31 [years] increased by 6.5/1,000 people. "The difference-in-differences analysis estimated an absolute difference of –2.7%/1,000 people among the younger group, compared to the older group. After regression adjustment ... the difference-in-differences analysis estimated a reduction of 2.1% in young adults ages 19-25 [years], compared to people ages 26-31 [years]."
Researchers analyzed data from three states – California, Florida, and New York – and also found that among people aged 26-31 years, the probability of an ED visit between pre-and post-ACA implementation increased by 2.2%, while young adults aged 19-25 years had a smaller increase of 1.9%.
Findings were published online Sept. 8 and are scheduled to appear in the September issue of Health Affairs (2014 [doi:10.1377/hthaff.2014.0103]).
"Our results suggest that the ACA’s dependent coverage provision is associated with a relative decrease in the number of ED visits for young adults but a minimum relative decrease in the rate at which they ever used the ED," reported Tina Hernandez-Boussard of the departments of surgery and biomedical informatics at Stanford (Calif.) University, and her associates.
The authors state that the research and analysis showed that "ED use by young adults ages 19-25 expanded by a modest amount after the implementation of the ACA insurance expansion but that ED use by people ages 26-31, who were not including in the ACA expansion, grew faster. Relatively slower growth in use by the younger group is consistent with the view that the ACA decreased ED use in this age group."
Dr. Hernandez-Boussard and her associates suggest that better coverage of young adults "could have facilitated better access to health care in non-ED settings such as doctors’ offices, which could have reduced the use of ED care."
Young adults are using emergency departments less following the implementation of expanded coverage under the Affordable Care Act, though the number of patients from this population has not significantly changed.
According to new research published in Health Affairs, ED visits by young adults increased by 3.8 visits/1,000 people between pre-ACA implementation (Sept. 1, 2009-Aug. 31, 2010) and post-ACA implementation (2011 calendar year), while the control group of adults ages 26-31 [years] increased by 6.5/1,000 people. "The difference-in-differences analysis estimated an absolute difference of –2.7%/1,000 people among the younger group, compared to the older group. After regression adjustment ... the difference-in-differences analysis estimated a reduction of 2.1% in young adults ages 19-25 [years], compared to people ages 26-31 [years]."
Researchers analyzed data from three states – California, Florida, and New York – and also found that among people aged 26-31 years, the probability of an ED visit between pre-and post-ACA implementation increased by 2.2%, while young adults aged 19-25 years had a smaller increase of 1.9%.
Findings were published online Sept. 8 and are scheduled to appear in the September issue of Health Affairs (2014 [doi:10.1377/hthaff.2014.0103]).
"Our results suggest that the ACA’s dependent coverage provision is associated with a relative decrease in the number of ED visits for young adults but a minimum relative decrease in the rate at which they ever used the ED," reported Tina Hernandez-Boussard of the departments of surgery and biomedical informatics at Stanford (Calif.) University, and her associates.
The authors state that the research and analysis showed that "ED use by young adults ages 19-25 expanded by a modest amount after the implementation of the ACA insurance expansion but that ED use by people ages 26-31, who were not including in the ACA expansion, grew faster. Relatively slower growth in use by the younger group is consistent with the view that the ACA decreased ED use in this age group."
Dr. Hernandez-Boussard and her associates suggest that better coverage of young adults "could have facilitated better access to health care in non-ED settings such as doctors’ offices, which could have reduced the use of ED care."
Young adults are using emergency departments less following the implementation of expanded coverage under the Affordable Care Act, though the number of patients from this population has not significantly changed.
According to new research published in Health Affairs, ED visits by young adults increased by 3.8 visits/1,000 people between pre-ACA implementation (Sept. 1, 2009-Aug. 31, 2010) and post-ACA implementation (2011 calendar year), while the control group of adults ages 26-31 [years] increased by 6.5/1,000 people. "The difference-in-differences analysis estimated an absolute difference of –2.7%/1,000 people among the younger group, compared to the older group. After regression adjustment ... the difference-in-differences analysis estimated a reduction of 2.1% in young adults ages 19-25 [years], compared to people ages 26-31 [years]."
Researchers analyzed data from three states – California, Florida, and New York – and also found that among people aged 26-31 years, the probability of an ED visit between pre-and post-ACA implementation increased by 2.2%, while young adults aged 19-25 years had a smaller increase of 1.9%.
Findings were published online Sept. 8 and are scheduled to appear in the September issue of Health Affairs (2014 [doi:10.1377/hthaff.2014.0103]).
"Our results suggest that the ACA’s dependent coverage provision is associated with a relative decrease in the number of ED visits for young adults but a minimum relative decrease in the rate at which they ever used the ED," reported Tina Hernandez-Boussard of the departments of surgery and biomedical informatics at Stanford (Calif.) University, and her associates.
The authors state that the research and analysis showed that "ED use by young adults ages 19-25 expanded by a modest amount after the implementation of the ACA insurance expansion but that ED use by people ages 26-31, who were not including in the ACA expansion, grew faster. Relatively slower growth in use by the younger group is consistent with the view that the ACA decreased ED use in this age group."
Dr. Hernandez-Boussard and her associates suggest that better coverage of young adults "could have facilitated better access to health care in non-ED settings such as doctors’ offices, which could have reduced the use of ED care."
FROM HEALTH AFFAIRS
Right-sided living donor kidney transplant found safe
SAN FRANCISCO – The practice of preferentially using left instead of right kidneys in living donor kidney transplantation may no longer be justified in the era of contemporary laparoscopic surgery, suggests a national study reported at the 2014 World Transplant Congress.
"The current approach in many centers is to prefer left living donor nephrectomy due to longer vessel length...Right donor nephrectomy, at least in our center and I think in most centers, has generally been reserved for cases of multiple or complex vessels on the left or incidental anatomical abnormalities on the right like cysts or stones," commented presenting author Dr. Tim E. Taber of Indiana University in Indianapolis.
Only one in seven of the roughly 59,000 living donor kidney transplants studied was performed using a right kidney. However, most short- and long-term outcomes were statistically indistinguishable between recipients of left and right kidneys, and the differences that were significant were small, he reported at the congress sponsored by the American Society of Transplant Surgeons.
"Our [study] is the largest national analysis or most recent large data analysis done on this subject in today’s surgical era of established laparoscopic living donor nephrectomies. There may be a minor risk for slightly inferior outcomes with right versus left kidneys," Dr. Taber concluded.
"Right-donor nephrectomy continues to be performed with great reluctance," he added. Yet, "under the accepted principles of live-donor nephrectomy, with enough surgical expertise, right-donor nephrectomy can be performed successfully. Right kidneys seem to have a very small difference, if any, in outcomes as compared to left kidneys. Surgical expertise and experience should be tailored toward this aspect."
A session attendee from Brazil commented, "We [prefer] to choose the right kidney in situations where we have one artery on the right side and multiple arteries on the left side." In these cases, his group uses an approach to the vasculature adopted from pancreas transplantation. "We have identical results with the right and left side," he reported.
Dr. Lloyd E. Ratner, director of renal and pancreatic transplantation at Columbia University Medical Center in New York, who also attended the session, said, "I feel somewhat responsible for causing this problem with the right kidney because we were the ones that originally described the higher thrombosis rate with the right kidney with the laparoscopic donor nephrectomies. And I think it scared everyone off from this topic."
As several attendees noted, "there are surgical ways of getting around this," he agreed, offering two more options. "The first is that if we get a short vein, we’re not reluctant at all to put a piece of Dacron onto it, so you don’t even need to dig out the saphenous and cause additional time or morbidity to the patient. And the nice thing about the Dacron grafts is that they are corrugated and they don’t collapse. They also stretch, so you don’t need to cut them exactly precisely," he said.
"And number two is when you are stapling ... it’s often useful to be able to staple onto the cava and not get the vein in one staple byte." By using two passes in the appropriate configuration, "you actually get a cuff of cava, then you have plenty of vein," he explained.
In the study, Dr. Taber and colleagues retrospectively analyzed data from 58,599 adult living donor kidney transplants performed during 2000-2009 and captured in the United Network for Organ Sharing (UNOS) database. In 86% of cases, surgeons used the donor’s left kidney.
Recipients of left and right kidneys were statistically indistinguishable with respect to hospital length of stay, treatment for acute rejection within 6 months, acute rejection as a cause of graft failure, inadequate urine production in the first 24 hours, primary graft failure, graft thrombosis or surgical complication as a contributory cause of graft failure, and 1-year graft survival.
Those receiving a right kidney did have significant but small increases in rates of delayed graft function, as defined by the need for dialysis within 7 days of transplantation (5.7% vs. 4.2%), lack of decline in serum creatinine in the first 24 hours (19.7% vs. 16.4%), treatment for acute rejection within 1 year (12.7% vs. 11.8%), and graft thrombosis as the cause of graft failure (1.1% vs. 0.8%).
The Kaplan-Meier cumulative rate of graft survival was better for left kidneys than for right kidneys (P = .006), but "these are essentially superimposed numbers," said Dr. Taber, who disclosed no conflicts of interest related to the research.
The study had limitations, such as its retrospective design, lack of more detailed information about donor and recipient outcomes, and reliance on data as reported by centers, he acknowledged. Also, such large studies may pick up small differences that are not clinically meaningful.
"With ever-increasing demands for living donor transplantation, right-donor nephrectomies are being considered more often. Every effort should be made to leave the donor with the higher-functioning kidney, but at the same time maximizing the living donor pool," Dr. Taber concluded.
Dr. Taber disclosed no relevant conflicts of interest.
SAN FRANCISCO – The practice of preferentially using left instead of right kidneys in living donor kidney transplantation may no longer be justified in the era of contemporary laparoscopic surgery, suggests a national study reported at the 2014 World Transplant Congress.
"The current approach in many centers is to prefer left living donor nephrectomy due to longer vessel length...Right donor nephrectomy, at least in our center and I think in most centers, has generally been reserved for cases of multiple or complex vessels on the left or incidental anatomical abnormalities on the right like cysts or stones," commented presenting author Dr. Tim E. Taber of Indiana University in Indianapolis.
Only one in seven of the roughly 59,000 living donor kidney transplants studied was performed using a right kidney. However, most short- and long-term outcomes were statistically indistinguishable between recipients of left and right kidneys, and the differences that were significant were small, he reported at the congress sponsored by the American Society of Transplant Surgeons.
"Our [study] is the largest national analysis or most recent large data analysis done on this subject in today’s surgical era of established laparoscopic living donor nephrectomies. There may be a minor risk for slightly inferior outcomes with right versus left kidneys," Dr. Taber concluded.
"Right-donor nephrectomy continues to be performed with great reluctance," he added. Yet, "under the accepted principles of live-donor nephrectomy, with enough surgical expertise, right-donor nephrectomy can be performed successfully. Right kidneys seem to have a very small difference, if any, in outcomes as compared to left kidneys. Surgical expertise and experience should be tailored toward this aspect."
A session attendee from Brazil commented, "We [prefer] to choose the right kidney in situations where we have one artery on the right side and multiple arteries on the left side." In these cases, his group uses an approach to the vasculature adopted from pancreas transplantation. "We have identical results with the right and left side," he reported.
Dr. Lloyd E. Ratner, director of renal and pancreatic transplantation at Columbia University Medical Center in New York, who also attended the session, said, "I feel somewhat responsible for causing this problem with the right kidney because we were the ones that originally described the higher thrombosis rate with the right kidney with the laparoscopic donor nephrectomies. And I think it scared everyone off from this topic."
As several attendees noted, "there are surgical ways of getting around this," he agreed, offering two more options. "The first is that if we get a short vein, we’re not reluctant at all to put a piece of Dacron onto it, so you don’t even need to dig out the saphenous and cause additional time or morbidity to the patient. And the nice thing about the Dacron grafts is that they are corrugated and they don’t collapse. They also stretch, so you don’t need to cut them exactly precisely," he said.
"And number two is when you are stapling ... it’s often useful to be able to staple onto the cava and not get the vein in one staple byte." By using two passes in the appropriate configuration, "you actually get a cuff of cava, then you have plenty of vein," he explained.
In the study, Dr. Taber and colleagues retrospectively analyzed data from 58,599 adult living donor kidney transplants performed during 2000-2009 and captured in the United Network for Organ Sharing (UNOS) database. In 86% of cases, surgeons used the donor’s left kidney.
Recipients of left and right kidneys were statistically indistinguishable with respect to hospital length of stay, treatment for acute rejection within 6 months, acute rejection as a cause of graft failure, inadequate urine production in the first 24 hours, primary graft failure, graft thrombosis or surgical complication as a contributory cause of graft failure, and 1-year graft survival.
Those receiving a right kidney did have significant but small increases in rates of delayed graft function, as defined by the need for dialysis within 7 days of transplantation (5.7% vs. 4.2%), lack of decline in serum creatinine in the first 24 hours (19.7% vs. 16.4%), treatment for acute rejection within 1 year (12.7% vs. 11.8%), and graft thrombosis as the cause of graft failure (1.1% vs. 0.8%).
The Kaplan-Meier cumulative rate of graft survival was better for left kidneys than for right kidneys (P = .006), but "these are essentially superimposed numbers," said Dr. Taber, who disclosed no conflicts of interest related to the research.
The study had limitations, such as its retrospective design, lack of more detailed information about donor and recipient outcomes, and reliance on data as reported by centers, he acknowledged. Also, such large studies may pick up small differences that are not clinically meaningful.
"With ever-increasing demands for living donor transplantation, right-donor nephrectomies are being considered more often. Every effort should be made to leave the donor with the higher-functioning kidney, but at the same time maximizing the living donor pool," Dr. Taber concluded.
Dr. Taber disclosed no relevant conflicts of interest.
SAN FRANCISCO – The practice of preferentially using left instead of right kidneys in living donor kidney transplantation may no longer be justified in the era of contemporary laparoscopic surgery, suggests a national study reported at the 2014 World Transplant Congress.
"The current approach in many centers is to prefer left living donor nephrectomy due to longer vessel length...Right donor nephrectomy, at least in our center and I think in most centers, has generally been reserved for cases of multiple or complex vessels on the left or incidental anatomical abnormalities on the right like cysts or stones," commented presenting author Dr. Tim E. Taber of Indiana University in Indianapolis.
Only one in seven of the roughly 59,000 living donor kidney transplants studied was performed using a right kidney. However, most short- and long-term outcomes were statistically indistinguishable between recipients of left and right kidneys, and the differences that were significant were small, he reported at the congress sponsored by the American Society of Transplant Surgeons.
"Our [study] is the largest national analysis or most recent large data analysis done on this subject in today’s surgical era of established laparoscopic living donor nephrectomies. There may be a minor risk for slightly inferior outcomes with right versus left kidneys," Dr. Taber concluded.
"Right-donor nephrectomy continues to be performed with great reluctance," he added. Yet, "under the accepted principles of live-donor nephrectomy, with enough surgical expertise, right-donor nephrectomy can be performed successfully. Right kidneys seem to have a very small difference, if any, in outcomes as compared to left kidneys. Surgical expertise and experience should be tailored toward this aspect."
A session attendee from Brazil commented, "We [prefer] to choose the right kidney in situations where we have one artery on the right side and multiple arteries on the left side." In these cases, his group uses an approach to the vasculature adopted from pancreas transplantation. "We have identical results with the right and left side," he reported.
Dr. Lloyd E. Ratner, director of renal and pancreatic transplantation at Columbia University Medical Center in New York, who also attended the session, said, "I feel somewhat responsible for causing this problem with the right kidney because we were the ones that originally described the higher thrombosis rate with the right kidney with the laparoscopic donor nephrectomies. And I think it scared everyone off from this topic."
As several attendees noted, "there are surgical ways of getting around this," he agreed, offering two more options. "The first is that if we get a short vein, we’re not reluctant at all to put a piece of Dacron onto it, so you don’t even need to dig out the saphenous and cause additional time or morbidity to the patient. And the nice thing about the Dacron grafts is that they are corrugated and they don’t collapse. They also stretch, so you don’t need to cut them exactly precisely," he said.
"And number two is when you are stapling ... it’s often useful to be able to staple onto the cava and not get the vein in one staple byte." By using two passes in the appropriate configuration, "you actually get a cuff of cava, then you have plenty of vein," he explained.
In the study, Dr. Taber and colleagues retrospectively analyzed data from 58,599 adult living donor kidney transplants performed during 2000-2009 and captured in the United Network for Organ Sharing (UNOS) database. In 86% of cases, surgeons used the donor’s left kidney.
Recipients of left and right kidneys were statistically indistinguishable with respect to hospital length of stay, treatment for acute rejection within 6 months, acute rejection as a cause of graft failure, inadequate urine production in the first 24 hours, primary graft failure, graft thrombosis or surgical complication as a contributory cause of graft failure, and 1-year graft survival.
Those receiving a right kidney did have significant but small increases in rates of delayed graft function, as defined by the need for dialysis within 7 days of transplantation (5.7% vs. 4.2%), lack of decline in serum creatinine in the first 24 hours (19.7% vs. 16.4%), treatment for acute rejection within 1 year (12.7% vs. 11.8%), and graft thrombosis as the cause of graft failure (1.1% vs. 0.8%).
The Kaplan-Meier cumulative rate of graft survival was better for left kidneys than for right kidneys (P = .006), but "these are essentially superimposed numbers," said Dr. Taber, who disclosed no conflicts of interest related to the research.
The study had limitations, such as its retrospective design, lack of more detailed information about donor and recipient outcomes, and reliance on data as reported by centers, he acknowledged. Also, such large studies may pick up small differences that are not clinically meaningful.
"With ever-increasing demands for living donor transplantation, right-donor nephrectomies are being considered more often. Every effort should be made to leave the donor with the higher-functioning kidney, but at the same time maximizing the living donor pool," Dr. Taber concluded.
Dr. Taber disclosed no relevant conflicts of interest.
FROM THE 2014 WORLD TRANSPLANT CONGRESS
Key clinical point: Choices of kidney to transplant may not need to hinge on left or right donor organ as a deciding factor.
Major Finding: Recipients of left and right kidneys were statistically indistinguishable with respect to hospital length of stay, treatment for acute rejection within 6 months, acute rejection as a cause of graft failure, inadequate urine production in the first 24 hours, and primary graft failure for acute rejection.
Data Source: A national retrospective cohort study of 58,599 adult living donor kidney transplants done during 2000-2009
Disclosures: Dr. Taber disclosed no relevant conflicts of interest.