User login
Official Newspaper of the American College of Surgeons
Postoperative complications increase risk of death in CRC patients
Patients who develop infectious complications after undergoing curative surgery for colorectal cancer face a significantly increased risk of death, results from a large retrospective study showed.
“The association of postoperative complications with long-term survival after major surgery has been suggested by several studies in mixed populations and is to some degree expected and intuitive,” authors led by Dr. Avo Artinyan, of the surgery department at Baylor College of Medicine, Houston, wrote online Sept. 1 in Annals of Surgery. “It has been difficult, however, to determine a specific cause-effect relationship, particularly because this association is noted even in patients who suffer late mortality, that is, those who presumably recover from postoperative complications.”
In an effort to investigate the effect of postoperative complications on long-term survival after colorectal cancer resection, the researchers evaluated the records of 12,075 patients from the Veterans Affairs Surgical Quality Improvement Program and the Central Cancer Registry databases who underwent resection for nonmetastatic colorectal cancer from 1999 to 2009 (Ann. Surg. 2014 Sept. 1 [doi: 10.1097/SLA.0000000000000854]). They categorized patients by presence of any complication within 30 days and by type of complication (infectious vs. noninfectious); excluded patients who died within 90 days of the procedure; and performed univariate and multivariate analyses adjusted for patient, disease, and treatment factors.
The average age of the cohort was 69 years, 98% were men, more than two-thirds (69%) had an American Society of Anesthesiologists (ASA) classification score of 3, and 61% had stage 1 or 2 disease. Dr. Artinyan and his associates found that the overall morbidity and infectious complication rates were 27.8% and 22.5%, respectively.
Compared with patients who had no postoperative complications, those who did were older and had lower postoperative serum albumin, worse functional status, and higher ASA scores (P less than .001). Multivariate analysis revealed that the presence of any complication was associated with a 24% increased hazard of death (hazard ratio, 1.24; P less that .001). When the analysis was limited to the type of complication, patients with infectious complications (in particular, surgical site infections) had an increased hazard of death (HR, 1.31), predominately those with severe infections (HR, 1.41).
“To our knowledge, this is the largest single study to examine the association of postoperative complications with long-term survival for CRC,” the authors wrote. “Similar to other groups, we have demonstrated that postoperative complications occur in a significant proportion of patients after CRC resection and that most patients with postoperative morbidity have at least one infectious complication.”
They acknowledged certain limitations of the study, including its retrospective design and the potential for selection bias. “Additional limitations include the absence of margin data – which may have a considerable impact on both the risk of organ-space infections and disease recurrence – and the inability to calculate cancer-specific survival and other cancer-specific outcomes,” they wrote.
“Overall all-cause survival, however, is still a commonly used and useful outcome measure, and we have attempted to mitigate the effect of early non–cancer-related mortality with the exclusion of early deaths.”
The authors reported having no financial disclosures.
On Twitter @dougbrunk
Patients who develop infectious complications after undergoing curative surgery for colorectal cancer face a significantly increased risk of death, results from a large retrospective study showed.
“The association of postoperative complications with long-term survival after major surgery has been suggested by several studies in mixed populations and is to some degree expected and intuitive,” authors led by Dr. Avo Artinyan, of the surgery department at Baylor College of Medicine, Houston, wrote online Sept. 1 in Annals of Surgery. “It has been difficult, however, to determine a specific cause-effect relationship, particularly because this association is noted even in patients who suffer late mortality, that is, those who presumably recover from postoperative complications.”
In an effort to investigate the effect of postoperative complications on long-term survival after colorectal cancer resection, the researchers evaluated the records of 12,075 patients from the Veterans Affairs Surgical Quality Improvement Program and the Central Cancer Registry databases who underwent resection for nonmetastatic colorectal cancer from 1999 to 2009 (Ann. Surg. 2014 Sept. 1 [doi: 10.1097/SLA.0000000000000854]). They categorized patients by presence of any complication within 30 days and by type of complication (infectious vs. noninfectious); excluded patients who died within 90 days of the procedure; and performed univariate and multivariate analyses adjusted for patient, disease, and treatment factors.
The average age of the cohort was 69 years, 98% were men, more than two-thirds (69%) had an American Society of Anesthesiologists (ASA) classification score of 3, and 61% had stage 1 or 2 disease. Dr. Artinyan and his associates found that the overall morbidity and infectious complication rates were 27.8% and 22.5%, respectively.
Compared with patients who had no postoperative complications, those who did were older and had lower postoperative serum albumin, worse functional status, and higher ASA scores (P less than .001). Multivariate analysis revealed that the presence of any complication was associated with a 24% increased hazard of death (hazard ratio, 1.24; P less that .001). When the analysis was limited to the type of complication, patients with infectious complications (in particular, surgical site infections) had an increased hazard of death (HR, 1.31), predominately those with severe infections (HR, 1.41).
“To our knowledge, this is the largest single study to examine the association of postoperative complications with long-term survival for CRC,” the authors wrote. “Similar to other groups, we have demonstrated that postoperative complications occur in a significant proportion of patients after CRC resection and that most patients with postoperative morbidity have at least one infectious complication.”
They acknowledged certain limitations of the study, including its retrospective design and the potential for selection bias. “Additional limitations include the absence of margin data – which may have a considerable impact on both the risk of organ-space infections and disease recurrence – and the inability to calculate cancer-specific survival and other cancer-specific outcomes,” they wrote.
“Overall all-cause survival, however, is still a commonly used and useful outcome measure, and we have attempted to mitigate the effect of early non–cancer-related mortality with the exclusion of early deaths.”
The authors reported having no financial disclosures.
On Twitter @dougbrunk
Patients who develop infectious complications after undergoing curative surgery for colorectal cancer face a significantly increased risk of death, results from a large retrospective study showed.
“The association of postoperative complications with long-term survival after major surgery has been suggested by several studies in mixed populations and is to some degree expected and intuitive,” authors led by Dr. Avo Artinyan, of the surgery department at Baylor College of Medicine, Houston, wrote online Sept. 1 in Annals of Surgery. “It has been difficult, however, to determine a specific cause-effect relationship, particularly because this association is noted even in patients who suffer late mortality, that is, those who presumably recover from postoperative complications.”
In an effort to investigate the effect of postoperative complications on long-term survival after colorectal cancer resection, the researchers evaluated the records of 12,075 patients from the Veterans Affairs Surgical Quality Improvement Program and the Central Cancer Registry databases who underwent resection for nonmetastatic colorectal cancer from 1999 to 2009 (Ann. Surg. 2014 Sept. 1 [doi: 10.1097/SLA.0000000000000854]). They categorized patients by presence of any complication within 30 days and by type of complication (infectious vs. noninfectious); excluded patients who died within 90 days of the procedure; and performed univariate and multivariate analyses adjusted for patient, disease, and treatment factors.
The average age of the cohort was 69 years, 98% were men, more than two-thirds (69%) had an American Society of Anesthesiologists (ASA) classification score of 3, and 61% had stage 1 or 2 disease. Dr. Artinyan and his associates found that the overall morbidity and infectious complication rates were 27.8% and 22.5%, respectively.
Compared with patients who had no postoperative complications, those who did were older and had lower postoperative serum albumin, worse functional status, and higher ASA scores (P less than .001). Multivariate analysis revealed that the presence of any complication was associated with a 24% increased hazard of death (hazard ratio, 1.24; P less that .001). When the analysis was limited to the type of complication, patients with infectious complications (in particular, surgical site infections) had an increased hazard of death (HR, 1.31), predominately those with severe infections (HR, 1.41).
“To our knowledge, this is the largest single study to examine the association of postoperative complications with long-term survival for CRC,” the authors wrote. “Similar to other groups, we have demonstrated that postoperative complications occur in a significant proportion of patients after CRC resection and that most patients with postoperative morbidity have at least one infectious complication.”
They acknowledged certain limitations of the study, including its retrospective design and the potential for selection bias. “Additional limitations include the absence of margin data – which may have a considerable impact on both the risk of organ-space infections and disease recurrence – and the inability to calculate cancer-specific survival and other cancer-specific outcomes,” they wrote.
“Overall all-cause survival, however, is still a commonly used and useful outcome measure, and we have attempted to mitigate the effect of early non–cancer-related mortality with the exclusion of early deaths.”
The authors reported having no financial disclosures.
On Twitter @dougbrunk
FROM ANNALS OF SURGERY
Key clinical point: Postoperative complications after colorectal cancer surgery are associated with decreased long-term survival.
Major finding: The presence of any complication after CRC surgery was associated with a 24% increased hazard of death (hazard ratio, 1.24; P less than .001).
Data source: A retrospective evaluation of 12,075 patients who underwent resection for nonmetastatic CRC from 1999-2009.
Disclosures: The authors reported having no financial disclosures.
Survey: Many physicians plan to reduce their workload
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
IOM calls for pay for end-of-life planning
Physicians should be compensated for counseling patients on end-of-life planning, according to recommendations from the Institute of Medicine, and the health care delivery and payment system should be realigned to encourage and financially reward higher-quality, more comprehensive, more efficient, and more humane care for those with serious illnesses.
“Individuals should have time with their doctors to talk about end-of-life issues, and clinicians should receive the training and financial incentives for such discussions,” said David Walker, the former comptroller general of the United States, who was the cochair of the IOM committee that created the report published Sept. 17.
Dying in America calls on health care providers, payers, policy makers, and the American public to have a more open discourse about death and dying.
End-of-life care was caught up in a political firestorm in 2009 when the Obama administration proposed to pay for advanced care conversations under the Affordable Care Act, Dr. Harvey Fineberg, former IOM president, noted in a video message at a briefing to release the report. Such efforts were construed as “death panels,” and the administration withdrew its proposal within days of it going into effect in 2011, said Dr. Fineberg, who is now at the University of California, San Francisco.
“The controversy on this topic and the political desire to avoid it do not alter the fact that every person will face the end of life one day, and many have had hard experience with the final days of a parent, a spouse, a child, a sibling, another relative, or a dear friend,” Dr. Fineberg said.
The report focuses on three areas: what individuals and their families can do to take more control over their own life and their health care throughout their life; what clinicians and other professionals can do; and what policy makers and payers need to do to try to effectuate change. The 21-member IOM committee spent 2 years developing the consensus report, Mr. Walker said.
“For most people, death does not come suddenly,” said Dr. Philip Pizzo, committee cochair. “Instead, dying is a result of one or more diseases that must be managed carefully and compassionately over weeks, months, or even years, through many ups and downs,” said Dr. Pizzo of Stanford (Calif.) University.
The committee made five broad recommendations:
• Comprehensive care for patients with advanced, serious illness who are nearing the end of life should be covered by public and private payers.
• Evidence-based standards for clinician-patient communication and advanced care planning should be developed by professional societies; such standards should be used as measures for payment, licensing, and credentialing.
• Standardized training and requirements should be developed and implemented.
• Care standards should seek to avoid unnecessary emergency department or acute care services; care should be coordinated across settings and providers by using tools such as interoperable electronic health records and physician orders for life-sustaining treatment programs.
• Fact-based information on end-of-life care planning should be developed and disseminated broadly through public health and other governmental agencies, community-based organizations, and faith-based organizations, as well as through health care providers and payers.
More needs to be done to educate physicians, other health care providers, and patients about the differences between hospice care and palliative care, and the potential they have for improving quality of life and reducing potentially unnecessary – and costly – medical services, according to the committee report.
Dr. Pizzo noted that many physicians, when asked in surveys, have said that they would personally prefer less-aggressive care at the end of life, and if possible, having the patient receive care at home. Yet, when it comes to their patients, they tend to pull out the stops.
He said that was being driven by a lack of understanding of patients’ individual needs and preferences, and by what he and the committee called the “perverse incentives” of the health care system.
The system rewards more care, not less, and acute care more so than palliative or supportive care, Mr. Walker noted. “Our current system is broken. It does not result in the honoring of individual preferences as much as it should.”
The IOM report was financed by an anonymous donor, Dr. Fineberg said.
The donor made money available for the IOM to continue for at least a year, disseminating the findings and encouraging adoption of its recommendations, Mr. Walker said.
On Twitter @aliciaault
This recommendation for end-of-life discussions is long overdue. Physicians have been providing these services for years, and it is appropriate that they be encouraged to provide such care both in and out of the hospital. The impact can be significant for this time-consuming and emotion-consuming practice. Referrals to palliative care will likely increase, as will patient satisfaction scores. Use of hospital resources and their cost are likely to decrease as patients and their families request that nonessential treatment be decreased or stopped. Only good can come from this, once the process has been fully developed by the CMS.
This recommendation for end-of-life discussions is long overdue. Physicians have been providing these services for years, and it is appropriate that they be encouraged to provide such care both in and out of the hospital. The impact can be significant for this time-consuming and emotion-consuming practice. Referrals to palliative care will likely increase, as will patient satisfaction scores. Use of hospital resources and their cost are likely to decrease as patients and their families request that nonessential treatment be decreased or stopped. Only good can come from this, once the process has been fully developed by the CMS.
This recommendation for end-of-life discussions is long overdue. Physicians have been providing these services for years, and it is appropriate that they be encouraged to provide such care both in and out of the hospital. The impact can be significant for this time-consuming and emotion-consuming practice. Referrals to palliative care will likely increase, as will patient satisfaction scores. Use of hospital resources and their cost are likely to decrease as patients and their families request that nonessential treatment be decreased or stopped. Only good can come from this, once the process has been fully developed by the CMS.
Physicians should be compensated for counseling patients on end-of-life planning, according to recommendations from the Institute of Medicine, and the health care delivery and payment system should be realigned to encourage and financially reward higher-quality, more comprehensive, more efficient, and more humane care for those with serious illnesses.
“Individuals should have time with their doctors to talk about end-of-life issues, and clinicians should receive the training and financial incentives for such discussions,” said David Walker, the former comptroller general of the United States, who was the cochair of the IOM committee that created the report published Sept. 17.
Dying in America calls on health care providers, payers, policy makers, and the American public to have a more open discourse about death and dying.
End-of-life care was caught up in a political firestorm in 2009 when the Obama administration proposed to pay for advanced care conversations under the Affordable Care Act, Dr. Harvey Fineberg, former IOM president, noted in a video message at a briefing to release the report. Such efforts were construed as “death panels,” and the administration withdrew its proposal within days of it going into effect in 2011, said Dr. Fineberg, who is now at the University of California, San Francisco.
“The controversy on this topic and the political desire to avoid it do not alter the fact that every person will face the end of life one day, and many have had hard experience with the final days of a parent, a spouse, a child, a sibling, another relative, or a dear friend,” Dr. Fineberg said.
The report focuses on three areas: what individuals and their families can do to take more control over their own life and their health care throughout their life; what clinicians and other professionals can do; and what policy makers and payers need to do to try to effectuate change. The 21-member IOM committee spent 2 years developing the consensus report, Mr. Walker said.
“For most people, death does not come suddenly,” said Dr. Philip Pizzo, committee cochair. “Instead, dying is a result of one or more diseases that must be managed carefully and compassionately over weeks, months, or even years, through many ups and downs,” said Dr. Pizzo of Stanford (Calif.) University.
The committee made five broad recommendations:
• Comprehensive care for patients with advanced, serious illness who are nearing the end of life should be covered by public and private payers.
• Evidence-based standards for clinician-patient communication and advanced care planning should be developed by professional societies; such standards should be used as measures for payment, licensing, and credentialing.
• Standardized training and requirements should be developed and implemented.
• Care standards should seek to avoid unnecessary emergency department or acute care services; care should be coordinated across settings and providers by using tools such as interoperable electronic health records and physician orders for life-sustaining treatment programs.
• Fact-based information on end-of-life care planning should be developed and disseminated broadly through public health and other governmental agencies, community-based organizations, and faith-based organizations, as well as through health care providers and payers.
More needs to be done to educate physicians, other health care providers, and patients about the differences between hospice care and palliative care, and the potential they have for improving quality of life and reducing potentially unnecessary – and costly – medical services, according to the committee report.
Dr. Pizzo noted that many physicians, when asked in surveys, have said that they would personally prefer less-aggressive care at the end of life, and if possible, having the patient receive care at home. Yet, when it comes to their patients, they tend to pull out the stops.
He said that was being driven by a lack of understanding of patients’ individual needs and preferences, and by what he and the committee called the “perverse incentives” of the health care system.
The system rewards more care, not less, and acute care more so than palliative or supportive care, Mr. Walker noted. “Our current system is broken. It does not result in the honoring of individual preferences as much as it should.”
The IOM report was financed by an anonymous donor, Dr. Fineberg said.
The donor made money available for the IOM to continue for at least a year, disseminating the findings and encouraging adoption of its recommendations, Mr. Walker said.
On Twitter @aliciaault
Physicians should be compensated for counseling patients on end-of-life planning, according to recommendations from the Institute of Medicine, and the health care delivery and payment system should be realigned to encourage and financially reward higher-quality, more comprehensive, more efficient, and more humane care for those with serious illnesses.
“Individuals should have time with their doctors to talk about end-of-life issues, and clinicians should receive the training and financial incentives for such discussions,” said David Walker, the former comptroller general of the United States, who was the cochair of the IOM committee that created the report published Sept. 17.
Dying in America calls on health care providers, payers, policy makers, and the American public to have a more open discourse about death and dying.
End-of-life care was caught up in a political firestorm in 2009 when the Obama administration proposed to pay for advanced care conversations under the Affordable Care Act, Dr. Harvey Fineberg, former IOM president, noted in a video message at a briefing to release the report. Such efforts were construed as “death panels,” and the administration withdrew its proposal within days of it going into effect in 2011, said Dr. Fineberg, who is now at the University of California, San Francisco.
“The controversy on this topic and the political desire to avoid it do not alter the fact that every person will face the end of life one day, and many have had hard experience with the final days of a parent, a spouse, a child, a sibling, another relative, or a dear friend,” Dr. Fineberg said.
The report focuses on three areas: what individuals and their families can do to take more control over their own life and their health care throughout their life; what clinicians and other professionals can do; and what policy makers and payers need to do to try to effectuate change. The 21-member IOM committee spent 2 years developing the consensus report, Mr. Walker said.
“For most people, death does not come suddenly,” said Dr. Philip Pizzo, committee cochair. “Instead, dying is a result of one or more diseases that must be managed carefully and compassionately over weeks, months, or even years, through many ups and downs,” said Dr. Pizzo of Stanford (Calif.) University.
The committee made five broad recommendations:
• Comprehensive care for patients with advanced, serious illness who are nearing the end of life should be covered by public and private payers.
• Evidence-based standards for clinician-patient communication and advanced care planning should be developed by professional societies; such standards should be used as measures for payment, licensing, and credentialing.
• Standardized training and requirements should be developed and implemented.
• Care standards should seek to avoid unnecessary emergency department or acute care services; care should be coordinated across settings and providers by using tools such as interoperable electronic health records and physician orders for life-sustaining treatment programs.
• Fact-based information on end-of-life care planning should be developed and disseminated broadly through public health and other governmental agencies, community-based organizations, and faith-based organizations, as well as through health care providers and payers.
More needs to be done to educate physicians, other health care providers, and patients about the differences between hospice care and palliative care, and the potential they have for improving quality of life and reducing potentially unnecessary – and costly – medical services, according to the committee report.
Dr. Pizzo noted that many physicians, when asked in surveys, have said that they would personally prefer less-aggressive care at the end of life, and if possible, having the patient receive care at home. Yet, when it comes to their patients, they tend to pull out the stops.
He said that was being driven by a lack of understanding of patients’ individual needs and preferences, and by what he and the committee called the “perverse incentives” of the health care system.
The system rewards more care, not less, and acute care more so than palliative or supportive care, Mr. Walker noted. “Our current system is broken. It does not result in the honoring of individual preferences as much as it should.”
The IOM report was financed by an anonymous donor, Dr. Fineberg said.
The donor made money available for the IOM to continue for at least a year, disseminating the findings and encouraging adoption of its recommendations, Mr. Walker said.
On Twitter @aliciaault
Few risks seen with initial ultrasonography in nephrolithiasis
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Ultrasonography may be preferable to computed tomography in initial imaging to diagnose kidney stones.
Major finding: Initial ultrasound, followed by CT if indicated, did not increase incidence of high-risk diagnoses with complications or adverse outcomes compared with initial CT; patients also saw lower cumulative radiation compared with initial CT.
Data source: Study of 2,759 patients with suspected nephrolithiasis enrolled from 15 U.S. hospital emergency departments between October 2011 and February 2013, randomized to initial screening with CT or ultrasonography, and followed up for 6 months.
Disclosures: None of the study authors declared financial conflicts of interest.
FDA approves drug for opioid-induced constipation in chronic noncancer pain population
Naloxegol, an orally administered peripherally acting mu-opioid receptor antagonist, has been approved by the Food and Drug Administration as a treatment for opioid-induced constipation in adults with chronic noncancer pain, the agency announced on Sept. 17.
The drug will be marketed by AstraZeneca Pharmaceuticals as Movantik and is expected to be available during the first half of 2015, according to a company statement. A company petition for the drug to be descheduled is under review at the US Drug Enforcement Administration. Because the drug is structurally related to noroxymorphone, naloxegol is considered a schedule II drug, but the FDA-approved labeling states that it has “no risk of abuse or dependency,” the company statement said.
Approval of the drug, which is taken once a day in a tablet formulation, was based on two 12-week studies of 1,352 patients who had taken opioids for noncancer related pain for at least 4 weeks and had opioid-induced constipation, according to a FDA statement. The two studies, KODIAC-04 and KODIAC-05, were published in June (N. Engl. J. Med. 2014;370:2387-96).
Patients with noncancer-related pain and opioid-induced constipation were randomized to receive one of two doses of naloxegol or placebo, once a day for 12 weeks. The 12-week endpoint was at least three spontaneous bowel movements per week and an increase of at least one spontaneous bowel movement per week from baseline for at least 9 of the 12 weeks and for at least 3 of the final 4 weeks of the study. In one study, 44% of those on the 25-mg dose and 41% of those on the lower dose met this endpoint, vs. 29% of those on placebo. In the second study, 40% of those on the higher dose and 35% of those on the lower dose met this endpoint, vs. 29% of those on placebo.
Abdominal pain, diarrhea, headache, and flatulence were among the common side effects of the drug, according to the FDA.
The manufacturer is required to conduct a postmarketing study to evaluate the possible cardiovascular risks of the drug in patients, according to the agency.
Naloxegol is under review by the European Medicines Agency in Europe, according to the company.
Naloxegol, an orally administered peripherally acting mu-opioid receptor antagonist, has been approved by the Food and Drug Administration as a treatment for opioid-induced constipation in adults with chronic noncancer pain, the agency announced on Sept. 17.
The drug will be marketed by AstraZeneca Pharmaceuticals as Movantik and is expected to be available during the first half of 2015, according to a company statement. A company petition for the drug to be descheduled is under review at the US Drug Enforcement Administration. Because the drug is structurally related to noroxymorphone, naloxegol is considered a schedule II drug, but the FDA-approved labeling states that it has “no risk of abuse or dependency,” the company statement said.
Approval of the drug, which is taken once a day in a tablet formulation, was based on two 12-week studies of 1,352 patients who had taken opioids for noncancer related pain for at least 4 weeks and had opioid-induced constipation, according to a FDA statement. The two studies, KODIAC-04 and KODIAC-05, were published in June (N. Engl. J. Med. 2014;370:2387-96).
Patients with noncancer-related pain and opioid-induced constipation were randomized to receive one of two doses of naloxegol or placebo, once a day for 12 weeks. The 12-week endpoint was at least three spontaneous bowel movements per week and an increase of at least one spontaneous bowel movement per week from baseline for at least 9 of the 12 weeks and for at least 3 of the final 4 weeks of the study. In one study, 44% of those on the 25-mg dose and 41% of those on the lower dose met this endpoint, vs. 29% of those on placebo. In the second study, 40% of those on the higher dose and 35% of those on the lower dose met this endpoint, vs. 29% of those on placebo.
Abdominal pain, diarrhea, headache, and flatulence were among the common side effects of the drug, according to the FDA.
The manufacturer is required to conduct a postmarketing study to evaluate the possible cardiovascular risks of the drug in patients, according to the agency.
Naloxegol is under review by the European Medicines Agency in Europe, according to the company.
Naloxegol, an orally administered peripherally acting mu-opioid receptor antagonist, has been approved by the Food and Drug Administration as a treatment for opioid-induced constipation in adults with chronic noncancer pain, the agency announced on Sept. 17.
The drug will be marketed by AstraZeneca Pharmaceuticals as Movantik and is expected to be available during the first half of 2015, according to a company statement. A company petition for the drug to be descheduled is under review at the US Drug Enforcement Administration. Because the drug is structurally related to noroxymorphone, naloxegol is considered a schedule II drug, but the FDA-approved labeling states that it has “no risk of abuse or dependency,” the company statement said.
Approval of the drug, which is taken once a day in a tablet formulation, was based on two 12-week studies of 1,352 patients who had taken opioids for noncancer related pain for at least 4 weeks and had opioid-induced constipation, according to a FDA statement. The two studies, KODIAC-04 and KODIAC-05, were published in June (N. Engl. J. Med. 2014;370:2387-96).
Patients with noncancer-related pain and opioid-induced constipation were randomized to receive one of two doses of naloxegol or placebo, once a day for 12 weeks. The 12-week endpoint was at least three spontaneous bowel movements per week and an increase of at least one spontaneous bowel movement per week from baseline for at least 9 of the 12 weeks and for at least 3 of the final 4 weeks of the study. In one study, 44% of those on the 25-mg dose and 41% of those on the lower dose met this endpoint, vs. 29% of those on placebo. In the second study, 40% of those on the higher dose and 35% of those on the lower dose met this endpoint, vs. 29% of those on placebo.
Abdominal pain, diarrhea, headache, and flatulence were among the common side effects of the drug, according to the FDA.
The manufacturer is required to conduct a postmarketing study to evaluate the possible cardiovascular risks of the drug in patients, according to the agency.
Naloxegol is under review by the European Medicines Agency in Europe, according to the company.
Most acute VTE therapies yield similar outcomes
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
For patients with acute venous thromboembolism, both clinical and safety outcomes were similar among seven of eight possible treatment strategies assessed in a network meta-analysis published online Sept. 16 in JAMA.
Clinicians have several treatment options but little guidance for choosing among them when managing acute VTE. Many strategies have shown promising results when assessed in single studies, but there have been few direct comparison studies. So investigators performed a network meta-analysis of 45 articles involving 44,989 patients, which enabled them to compare the safety and efficacy of eight possible approaches. The sample sizes of these studies ranged from 60 to 8,240 participants, with a median of 298. The median follow-up period was 3 months, with a range of 3-8 months.
The currently accepted standard treatment for acute VTE is the use of parenteral low-molecular-weight heparin (LMWH) for a minimum of 5 days, followed by transition to a vitamin K antagonist. This approach was compared against parenteral unfractionated heparin followed by a vitamin K antagonist; parenteral fondaparinux followed by a vitamin K antagonist; parenteral LMWH combined with dabigatran; parenteral LMWH combined with edoxaban; oral rivaroxaban; oral apixaban; and parenteral LMWH alone, said Dr. Lana A. Castellucci of the Ottawa Hospital Research Institute, University of Ottawa, and her associates.
Compared with standard parenteral LMWH plus a vitamin K antagonist, six of these approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding, the investigators said (JAMA 2014 September 16 [doi:10.1001/jama.2014.10538]).
The only strategy that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist. However, “there are clinical circumstances that necessitate the use of unfractionated heparin, including for patients with severe renal insufficiency and those with massive or submassive pulmonary embolism who are potential candidates for thrombolysis or thrombectomy,” Dr. Castellucci and her associates noted.
Oral rivaroxaban and oral apixaban appeared to be associated with the lowest risk of major bleeding. “Future direct comparison trials, patient-level network meta-analyses, or high-quality nonrandomized studies are required to confirm our findings,” they added.
This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
*Correction, 9/17/2014: An earlier version of this article misstated the Key Clinical Point in the Vitals section.
FROM JAMA
Key clinical point: Seven of the eight available VTE therapies are equally safe and effective.*
Major finding: Compared with standard parenteral LMWH plus a vitamin K antagonist, six treatment approaches yielded comparable reductions in recurrent VTE and induced comparable rates of major bleeding; the only approach that was less effective at reducing the rate of recurrent VTE was parenteral unfractionated heparin plus a vitamin K antagonist.
Data source: A network meta-analysis of 45 articles on studies involving 44,989 patients with acute VTE who were treated using any of eight strategies and followed for a median of 3 months.
Disclosures: This study was supported by the Heart and Stroke Foundation of Canada, the University of Ottawa, the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and the Heart and Stroke Foundation of Ontario. Dr. Castellucci reported no financial conflicts of interest; some of her associates reported ties to Bayer, Biomerieux, Boehringer Ingelheim, Bristol-Myers Squibb, Leo Pharma, Pfizer, and Sanofi.
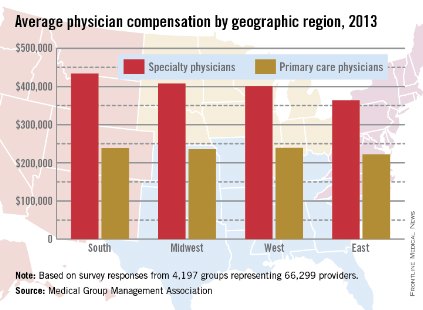
Physician income in 2013: The East earned least
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
Redundant antibiotics used at 80% of hospitals
Redundant combinations of intravenous antibiotics are used in nearly 8 of 10 hospitals, even though they are very infrequently indicated, said a group of researchers working to promote antimicrobial stewardship in hospitals.
In an article published in the October issue of Infection Control and Hospital Epidemiology, Leslie Schultz, R.N., Ph.D., of Premier Safety Institute in Charlotte, N.C., and colleagues reported that a review of cases from more than 500 U.S. hospitals revealed that about 150,000 days of inappropriate antibiotic therapy were prescribed, at an estimated excess cost of more than $12 million over the 4-year study period. Some 78% of hospitals in the study used the unnecessary drug combinations, they said.
The combination of metronidazole and piperacillin-tazobactam accounted for more than half of the redundant treatments detected in the study, with some 32,500 cases receiving this combination for 2 days or more. Other commonly seen redundant treatments included metronidazole and ampicillin-sulbactam, along with metronidazole and ertapenem, which, together with the metronidazole and piperacillin-tazobactam combination, were seen as responsible for 70% of redundant treatments administered to patients (Infect. Control Hosp. Epidemiol. 2014; 35:1229-35).
In a telephone press conference on Sept. 10, one of Dr. Schultz’s coauthors on the paper, Dr. Arjun Srinivasan of the Centers for Disease Control and Prevention, Atlanta, said that, while concerns about antimicrobial stewardship are not new, the findings came as a surprise. "We would expect the use of these combinations to be vanishingly rare given how often they’re indicated," Dr. Srinivasan said, citing a lack of training in antibiotics as a contributing factor.
"We’ve heard from a lot of clinicians that providers don’t know that piperacillin-tazobactam very effectively kills anaerobic bacteria – but they do know that metronidazole is effective," Dr. Srinivasan said. "People are not as aware as they need to be about what antibiotics kill what bacteria, and we need to make sure people know which antibiotics need to be combined and when – and that with some, you don’t gain anything by adding the second drug. You only increase the risk of side effects."
Another physician taking part in the press conference, Dr. Sara Cosgrove of Johns Hopkins Hospital, Baltimore, agreed. "We have suboptimal training among medical students and house staff about what antibiotics cover what bugs," she said. "We have seen publications suggesting that medical students and residents want more info on antibiotics."
Dr. Cosgrove also noted that changes in hospital work practices may have contributed to the problem. "More people are working in hospitals on shorter shifts, and there are communication issues from one physician to the next. One physician may start an antibiotic and a second physician starts a second. There are many ways we can address the problem of unintended duplicate therapy," she said, including the use of alerts generated when pharmacy receives a request for a redundant drug.
Dr. Srinivasan said that hospitals that have implemented alerts have found them effective. Still, both physicians stressed that whatever the methods used, dedicated antimicrobial stewardship teams in hospitals were essential to ensuring the avoidance of redundant treatments.
"Many hospitals report that they are thinking about having an antimicrobial stewardship program. We’d like to nudge them to actually have one," said Dr. Cosgrove, who is chair of the antimicrobial stewardship committee for the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
Though Johns Hopkins has had an antimicrobial stewardship team since 2002, most hospitals do not have formal groups in place, she said. The Society for Healthcare Epidemiology of America will publish checklists and guidelines in 2015 to help hospitals set up teams, Dr. Cosgrove said, noting that California has recently passed legislation mandating their creation in all hospitals in that state.
All the coauthors of Dr. Schultz’s study except Dr. Srinivasan are employees of Premier Inc., which is a for-profit research corporation. Dr. Srinivasan reported having no conflicts of interest.
To be honest, before reading this article, I expected the study to find problems with prolonged coverage for presumed MRSA with vancomycin or linezolid, or double anti-pseudomonal coverage when it is not necessary. I was not expecting such a basic mistake as failure to recognize that penicillins and carbapenems provide excellent anaerobic coverage. Clearly, the medical students are correct in wanting more antibiotic training, and practicing physicians throughout the United States should follow suit with CME. Fortunately, antibiotic charts are readily available from a variety of reliable Internet resources, making this information easy to find and to use.
To be honest, before reading this article, I expected the study to find problems with prolonged coverage for presumed MRSA with vancomycin or linezolid, or double anti-pseudomonal coverage when it is not necessary. I was not expecting such a basic mistake as failure to recognize that penicillins and carbapenems provide excellent anaerobic coverage. Clearly, the medical students are correct in wanting more antibiotic training, and practicing physicians throughout the United States should follow suit with CME. Fortunately, antibiotic charts are readily available from a variety of reliable Internet resources, making this information easy to find and to use.
To be honest, before reading this article, I expected the study to find problems with prolonged coverage for presumed MRSA with vancomycin or linezolid, or double anti-pseudomonal coverage when it is not necessary. I was not expecting such a basic mistake as failure to recognize that penicillins and carbapenems provide excellent anaerobic coverage. Clearly, the medical students are correct in wanting more antibiotic training, and practicing physicians throughout the United States should follow suit with CME. Fortunately, antibiotic charts are readily available from a variety of reliable Internet resources, making this information easy to find and to use.
Redundant combinations of intravenous antibiotics are used in nearly 8 of 10 hospitals, even though they are very infrequently indicated, said a group of researchers working to promote antimicrobial stewardship in hospitals.
In an article published in the October issue of Infection Control and Hospital Epidemiology, Leslie Schultz, R.N., Ph.D., of Premier Safety Institute in Charlotte, N.C., and colleagues reported that a review of cases from more than 500 U.S. hospitals revealed that about 150,000 days of inappropriate antibiotic therapy were prescribed, at an estimated excess cost of more than $12 million over the 4-year study period. Some 78% of hospitals in the study used the unnecessary drug combinations, they said.
The combination of metronidazole and piperacillin-tazobactam accounted for more than half of the redundant treatments detected in the study, with some 32,500 cases receiving this combination for 2 days or more. Other commonly seen redundant treatments included metronidazole and ampicillin-sulbactam, along with metronidazole and ertapenem, which, together with the metronidazole and piperacillin-tazobactam combination, were seen as responsible for 70% of redundant treatments administered to patients (Infect. Control Hosp. Epidemiol. 2014; 35:1229-35).
In a telephone press conference on Sept. 10, one of Dr. Schultz’s coauthors on the paper, Dr. Arjun Srinivasan of the Centers for Disease Control and Prevention, Atlanta, said that, while concerns about antimicrobial stewardship are not new, the findings came as a surprise. "We would expect the use of these combinations to be vanishingly rare given how often they’re indicated," Dr. Srinivasan said, citing a lack of training in antibiotics as a contributing factor.
"We’ve heard from a lot of clinicians that providers don’t know that piperacillin-tazobactam very effectively kills anaerobic bacteria – but they do know that metronidazole is effective," Dr. Srinivasan said. "People are not as aware as they need to be about what antibiotics kill what bacteria, and we need to make sure people know which antibiotics need to be combined and when – and that with some, you don’t gain anything by adding the second drug. You only increase the risk of side effects."
Another physician taking part in the press conference, Dr. Sara Cosgrove of Johns Hopkins Hospital, Baltimore, agreed. "We have suboptimal training among medical students and house staff about what antibiotics cover what bugs," she said. "We have seen publications suggesting that medical students and residents want more info on antibiotics."
Dr. Cosgrove also noted that changes in hospital work practices may have contributed to the problem. "More people are working in hospitals on shorter shifts, and there are communication issues from one physician to the next. One physician may start an antibiotic and a second physician starts a second. There are many ways we can address the problem of unintended duplicate therapy," she said, including the use of alerts generated when pharmacy receives a request for a redundant drug.
Dr. Srinivasan said that hospitals that have implemented alerts have found them effective. Still, both physicians stressed that whatever the methods used, dedicated antimicrobial stewardship teams in hospitals were essential to ensuring the avoidance of redundant treatments.
"Many hospitals report that they are thinking about having an antimicrobial stewardship program. We’d like to nudge them to actually have one," said Dr. Cosgrove, who is chair of the antimicrobial stewardship committee for the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
Though Johns Hopkins has had an antimicrobial stewardship team since 2002, most hospitals do not have formal groups in place, she said. The Society for Healthcare Epidemiology of America will publish checklists and guidelines in 2015 to help hospitals set up teams, Dr. Cosgrove said, noting that California has recently passed legislation mandating their creation in all hospitals in that state.
All the coauthors of Dr. Schultz’s study except Dr. Srinivasan are employees of Premier Inc., which is a for-profit research corporation. Dr. Srinivasan reported having no conflicts of interest.
Redundant combinations of intravenous antibiotics are used in nearly 8 of 10 hospitals, even though they are very infrequently indicated, said a group of researchers working to promote antimicrobial stewardship in hospitals.
In an article published in the October issue of Infection Control and Hospital Epidemiology, Leslie Schultz, R.N., Ph.D., of Premier Safety Institute in Charlotte, N.C., and colleagues reported that a review of cases from more than 500 U.S. hospitals revealed that about 150,000 days of inappropriate antibiotic therapy were prescribed, at an estimated excess cost of more than $12 million over the 4-year study period. Some 78% of hospitals in the study used the unnecessary drug combinations, they said.
The combination of metronidazole and piperacillin-tazobactam accounted for more than half of the redundant treatments detected in the study, with some 32,500 cases receiving this combination for 2 days or more. Other commonly seen redundant treatments included metronidazole and ampicillin-sulbactam, along with metronidazole and ertapenem, which, together with the metronidazole and piperacillin-tazobactam combination, were seen as responsible for 70% of redundant treatments administered to patients (Infect. Control Hosp. Epidemiol. 2014; 35:1229-35).
In a telephone press conference on Sept. 10, one of Dr. Schultz’s coauthors on the paper, Dr. Arjun Srinivasan of the Centers for Disease Control and Prevention, Atlanta, said that, while concerns about antimicrobial stewardship are not new, the findings came as a surprise. "We would expect the use of these combinations to be vanishingly rare given how often they’re indicated," Dr. Srinivasan said, citing a lack of training in antibiotics as a contributing factor.
"We’ve heard from a lot of clinicians that providers don’t know that piperacillin-tazobactam very effectively kills anaerobic bacteria – but they do know that metronidazole is effective," Dr. Srinivasan said. "People are not as aware as they need to be about what antibiotics kill what bacteria, and we need to make sure people know which antibiotics need to be combined and when – and that with some, you don’t gain anything by adding the second drug. You only increase the risk of side effects."
Another physician taking part in the press conference, Dr. Sara Cosgrove of Johns Hopkins Hospital, Baltimore, agreed. "We have suboptimal training among medical students and house staff about what antibiotics cover what bugs," she said. "We have seen publications suggesting that medical students and residents want more info on antibiotics."
Dr. Cosgrove also noted that changes in hospital work practices may have contributed to the problem. "More people are working in hospitals on shorter shifts, and there are communication issues from one physician to the next. One physician may start an antibiotic and a second physician starts a second. There are many ways we can address the problem of unintended duplicate therapy," she said, including the use of alerts generated when pharmacy receives a request for a redundant drug.
Dr. Srinivasan said that hospitals that have implemented alerts have found them effective. Still, both physicians stressed that whatever the methods used, dedicated antimicrobial stewardship teams in hospitals were essential to ensuring the avoidance of redundant treatments.
"Many hospitals report that they are thinking about having an antimicrobial stewardship program. We’d like to nudge them to actually have one," said Dr. Cosgrove, who is chair of the antimicrobial stewardship committee for the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
Though Johns Hopkins has had an antimicrobial stewardship team since 2002, most hospitals do not have formal groups in place, she said. The Society for Healthcare Epidemiology of America will publish checklists and guidelines in 2015 to help hospitals set up teams, Dr. Cosgrove said, noting that California has recently passed legislation mandating their creation in all hospitals in that state.
All the coauthors of Dr. Schultz’s study except Dr. Srinivasan are employees of Premier Inc., which is a for-profit research corporation. Dr. Srinivasan reported having no conflicts of interest.
FROM INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY
EHRs rob physicians of 4 hours of free time per week
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Physicians may balk at using EHR systems because they consume rather than save time.
Major finding: EHR usage is accounting for 48 minutes of lost free time per day.
Data source: An analysis of 411 responses to a survey.
Disclosures: The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
E-order sets for Vitamin D testing cut deficiency among elderly
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
Making physicians aware of their track record assessing vitamin D deficiency and adding computerized order sets to check vitamin D levels and initiate vitamin D supplementation led to "significant improvement" in assessment and treatment of vitamin D deficiency in elderly patients with hip fracture at a North Carolina hospital, according to a study published online in the Journal of Hospital Medicine.
After these interventions, the percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5% (P less than .001), and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68% (P = .008), Dr. John R. Stephens of the University of North Carolina Hospitals and his colleagues reported (J. Hosp. Med. 2014 Sept. 5 [doi:10.1002/jhm.2255]).
The study authors reviewed the literature on the prevalence of vitamin D deficiency in elderly patients and used Endocrine Society guidelines "to define vitamin D deficiency, insufficiency, and recommended treatment dosing for each condition." They presented this information along with a review of data from their hospitalist group practice at a staff meeting.
They also revised the computerized physician order entry (CPOE) set for patients with hip fractures to include two new orders: an automatic order for 25-OH vitamin D level to be drawn the morning after admission and an order for initiation of 1,000 IU daily of vitamin D at admission.
They compared records of 196 patients (mean age 80), with hip fracture treated in the 28 months before these interventions and 107 similar patients treated in the 12 months following the interventions.
Three-quarters of the patients were female and at least 81% of the patients in both the intervention and preintervention groups were white in the single-center study.
"Our study demonstrates a systematic method groups may use to adopt and reliably implement practice guidelines," the authors wrote.
"With safeguards in the electronic system to flag duplicate medications, low toxicity of standard doses of vitamin D, and minimal economic harm with duplicate laboratory therapy in the context of a hospitalization for hip fracture," the researchers wrote, any possible risks "are outweighed by the benefits of screening."
They reported no conflicts of interest.
FROM THE JOURNAL OF HOSPITAL MEDICINE
Key clinical point: Having CPOE prompt screening can help reduce vitamin D deficiency in elderly inpatients.
Major finding: The percentage of patients screened for vitamin D deficiency improved from 37.2% to 93.5%, and the percentage of deficient or insufficient patients discharged on the recommended vitamin D dose improved from 40.9% to 68%.
Data source: An internal review of hospital records for 196 patients treated before CPOE set interventions and 107 patients treated after interventions.
Disclosures: The authors reported no conflicts of interest.