User login
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care. “An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care. “An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
Earlier diagnostic screening, routine and emerging therapies, and increased awareness are helping people with the lysosomal storage disorder Fabry disease lead longer, healthier lives. Because Fabry disease is rare, however, it can be misdiagnosed and treated incorrectly – for years and by various providers – while the patient’s health declines.
Four Fabry disease experts shared their perspectives, and recommendations, with Neurology Reviews 2023 Rare Neurological Disease Special Report.
What is Fabry disease?
Fabry disease is an X-linked lysosomal storage disorder caused by mutations in the galactosidase alpha (GLA) gene that causes reduced or absent alpha-galactosidase A (alpha-Gal A) enzyme activity. As a result, globotriaosylceramide (Gb3) accumulates, leading to cell, tissue, and organ damage in a range of systems. People with Fabry disease can develop progressive renal and cardiovascular dysfunction, neuropathy, and psychiatric disorders. They can experience cerebrovascular events; have eye, skin, gastrointestinal, and neuro-otologic involvement; and die prematurely.
Estimates of Fabry disease prevalence in the general population range from approximately 1 in 40,000 to 1 in 117,000 people. As an X-linked disorder, Fabry disease has been considered a disease mainly of males; however, affected females who are heterozygous for GLA mutations can remain asymptomatic through a normal lifespan or be as severely affected as a male would be.
Generally speaking, for every Fabry patient whose disease is diagnosed, there are five undiagnosed family members. Fabry disease affects future generations: Many patients are in their reproductive years; they want to have children and are therefore concerned about passing down the disease.
Symptoms of classic Fabry disease tend to appear during childhood or adolescence, often, and as early as 2 years of age, as acroparesthesias that intensify over time. In late-onset Fabry disease, symptoms might begin with renal failure or heart disease in the patient’s 30s, or later.
“Patients with classic Fabry disease commonly complain of acroparesthesias or whole-body pain,” said Anjay Rastogi, MD, PhD, professor of clinical medicine, clinical chief of nephrology, and director of the Fabry Disease Program at UCLA Health, Los Angeles. “With neuropathic pain, drugs like nonsteroidal anti-inflammatory drugs will probably not lessen the pain and might cause further cardiovascular, kidney, and other problems. So much of this pain is controlled by medications that are specific for nerves, including phenytoin, carbamazepine, and gabapentin.”
How do patients with Fabry disease typically present?
“Typically, with classic Fabry, young men visit the neurologist in their teenage years or later due to acroparesthesias – burning and tingling of the hands and feet,” further explained Gerald Vincent Raymond, MD, professor of genetic medicine and neurology and director of the Lysosomal Storage Disease Center at Johns Hopkins Medicine in Baltimore. “Sometimes they come to the attention of neurologists as 20- to 30-year-old men with strokes.
“These patients often undergo a long diagnostic odyssey of being misdiagnosed and treated incorrectly,” Dr. Raymond said. “Only years later, when they develop renal disease, cardiomyopathy, throw emboli, or have large- and small-vessel strokes, does a provider connect the dots.
“Neurologists should consider Fabry disease with any young patient with stroke, history of cardiomyopathy, renal disease, small-fiber peripheral neuropathy, tinnitus, hearing loss, unusual corneal whorls, or gastrointestinal issues. Because Fabry is an X-linked disease, women are usually less affected, but women can have the full manifestations of this disease.”
Who oversees the care of patients with Fabry disease?
“As a multisystem disease, Fabry disease must be managed by a multidisciplinary team, including genetics, neurology, nephrology, cardiology, psychiatry, ophthalmology, and otolaryngology,” explained Lizbeth Mellin, MD, assistant professor of pediatrics and clinical geneticist at University of Florida Health Jacksonville.
At what point does a neurologist encounter patients with Fabry disease? “Patients with Fabry disease are usually treated by rheumatologists and other specialists before they find a neurologist,” Dr. Mellin said. “Or they may see the neurologist for transient ischemic attacks or stroke, or for treatment of headaches, vascular dementia, dizziness or vertigo, hearing loss, seizures, hemiplegia, or aphasia.
“Almost 80% of adults with Fabry disease have distal neuropathic pain characterized by acroparesthesias and sensory loss starting in the palms of the hands or the soles of the feet, spreading to the entire body, and lasting for hours or days.
Dr. Mellin continued: “Neurologists play a critical role in treating manifestations such as neuropathic pain, stroke, and seizure. Without a current curative treatment for Fabry disease, the goals of its management are focused on treating manifestations and maintaining organ function, optimizing quality of life, and preserving life expectancy.”
What role does the neurologist play in ongoing management of Fabry disease? “Neurologists are involved in primary and secondary stroke prevention and pain management,” Dr. Rastogi explained, “and in diagnosing possible Fabry disease when they find cryptogenic stroke, especially in younger patients; when screening family members; and when reaching out to other appropriate Fabry providers.
“Primary care providers, geneticists, and, sometimes, nephrologists may manage the patient’s overall care. We send our patients to neurologists to evaluate and manage neuropathic pain, stroke, white-matter lesions, and cerebrovascular disease. After a stroke, a support team cares for the patient and manages the rehab.
“Neurologists tend to have organ-specific involvement, and they may treat pain. They may have their first encounter with the patient when they do nerve testing, brain scans, or other tests, or when they diagnose nervous system problems that they may continue to treat.”
How does the role of the neurologist complement others on the interdisciplinary care team? “Fabry requires management by specialists familiar with the multiple aspects of the disorder,” Dr. Raymond said. “As a geneticist and neurologist, I care for a broad portfolio of lysosomal storage diseases. Usually, a metabolic genetics center or a Fabry center will handle the therapy. Fabry requires a multidisciplinary approach, and someone needs to be quarterbacking the patient’s overall management.”
“Teamwork is about patient well-being and empowerment,” Dr. Mellin pointed out. “Patients with Fabry disease require multidisciplinary care to reduce their morbidity and improve their health-related quality of life. Early diagnosis and treatment are critical to preventing irreversible organ damage and failure. Patients with stroke are usually evaluated in a hospital setting. To protect major organs from progressive damage, the differential diagnosis must include Fabry disease.”
“It’s important to provide coordinated care to the entire patient, not only the affected organ,” Dr. Rastogi pointed out. “Taking care of patients with Fabry disease is difficult, complicated, and time-consuming. Academic programs have various specialties under the same umbrella, so it’s easier to coordinate care than in private practice. In private practice, the neurologist needs to reach out to other specialists to coordinate care. “An interdisciplinary team approach, with integrative care in which the team members communicate with each other, is very important. The team may include geneticists, pediatricians, nephrologists, cardiologists, neurologists, gastroenterologists, and a pain management team that may use biofeedback and other non-opioid approaches. The interdisciplinary UCLA Fabry Disease Program addresses almost every aspect of Fabry. As a nephrologist, I oversee the entire care of the patient, not just the kidneys.
“Some medical practices may have only three to five patients, with a geneticist leading the care team. In others, the primary care physician oversees and coordinates care with a neurologist, nephrologist, cardiologist, pain specialist, and other specialists. Patients are often anxious and depressed, so a psychologist and psychiatrist should also be involved.
“A neurologist who diagnoses a patient with Fabry disease should contact their local Fabry disease experts. If none are available, they should refer their patients to geneticists to oversee their care. At-risk family members also need to be screened.”
Monroe Carell Jr. Children’s Hospital at Vanderbilt, in Nashville, Tenn., has a multidisciplinary Fabry Disease Clinic with specialists in genetics, neurology, and cardiology. Chelsea J. Lauderdale, DNP, MPH, APRN, CPNP-PC, in the division of medical genetics and genomic medicine, helps screen and diagnose patients with Fabry disease.
“A nurse practitioner in this setting may work closely with newborn screening and be involved in infant and adult diagnosis,” Ms. Lauderdale said. “They may identify the onset of new symptoms and aid specialists in their evaluations. Nurse practitioners may be involved throughout Fabry disease patients’ care, monitoring labs, ensuring they are treated by the appropriate specialists, and initiating treatment when indicated.”
What recent research and advances should neurologists be aware of?
Diagnostics. Tests for Fabry disease now include an enzyme assay to measure alpha-galactosidase activity in the blood of males and genetic testing in males and females to identify GLA mutations. Several states now test newborns for Fabry disease, enabling earlier diagnosis and treatment, Dr. Raymond said. Identifying Fabry disease in a boy by enzyme assay sometimes leads to identifying an uncle, a grandfather, or others in the family who have Fabry. Fabry is sometimes discovered from genetic panels to help diagnose peripheral neuropathy and from prenatal genetic testing.
“Genetic screening of at-risk family members, of any degree, in various generations, is important,” Dr. Rastogi emphasized, “so we construct a family tree to find everyone at risk. Genetic testing is much easier and more widespread than it was even 5 years ago. It’s more accessible and you don’t need to go through a geneticist to diagnose Fabry disease.
“Some patients first come to us for dialysis in their 40s or 50s, but people are being tested and treated at younger ages now, and we also have newborn screening. Genetic testing for Fabry is not common, but in several states, every newborn is tested for Fabry. And, if parents have Fabry, we test their children.”
Therapeutics. “Available and emerging therapies make the field exciting,” Dr. Raymond said. “Some current gene therapy trials look promising, and preliminary evidence suggests that gene therapy may stabilize kidney and heart function.”
“Although Fabry disease does not have a cure,” Dr. Rastogi pointed out, “two treatments for Fabry disease appear to help prevent life-threatening complications: enzyme replacement therapy (ERT) and chaperone therapy.”
Replacing enzymes. “In Fabry disease, the enzyme alpha-galactosidase A is deficient,” Dr. Rastogi explained, “causing build-up of sphingolipids in blood vessels and tissues. ERT, a great advance that we’ve had for over 20 years, replenishes that deficiency. ERT has some challenges: It’s an infusion every 2 weeks for life, and it can have infusion reactions and other complications.
“Newer, second-generation, versions of ERT are being developed, including pegunigalsidase alfa (Elfabrio, Chiesi Global Rare Diseases, Protalix Biotherapeutics), recently approved by the U.S. Food and Drug Administration to treat adults with Fabry disease.”
Chaperone therapy. “The oral drug migalastat (Galafold, Fabrazyme) is a small-molecule chaperone therapy that stabilizes the faulty alpha-galactosidase A enzyme,” Dr. Rastogi explained. “It is easier to take, every other day for life, than [undergoing] infusion. Limitations include that it is available only to patients who have the amenable mutations, and whose estimated glomerular filtration rate is greater than 30 [mL/min/1.73 m2], and they may have some adverse events including nausea or vomiting.”
On the horizon: substrate reduction, gene therapy. “[These] are also exciting avenues of research,” said Dr. Rastogi. “Substrate reduction therapy aims to reduce glycosphingolipid accumulation, and lucerastat [Idorsia Pharmaceutical]1,2 and venglustat [Sanofi Genzyme]3,4 are in active clinical trials or trials that have been completed.
Gene therapy “delivers a healthy gene that helps the body produce a previously deficient enzyme,” Dr. Rastogi explained. “This is an early, very promising field in need of more research, with many challenges involving the vector and complications.
“While it is still too early to predict how effective gene therapy will be, research is encouraging. Another promising therapy is modulation of gene expression, which changes the activity of a gene.”
“Gene therapy may potentially offer an alternative to typical ERT, which some patients find burdensome,” Ms. Lauderdale added. “If a neurologist has a patient who may be a good candidate for a gene therapy clinical trial that is recruiting participants, I encourage them to learn more about the study and its requirements.”
Dr. Mellin concurred: “Several gene therapy clinical trials show promise, but further information and evidence are required.”
How might these advances affect the trajectory of Fabry disease?
“Untreated Fabry compromises quality of life and may shorten the lifespan,” Dr. Raymond said. “I’m aware of individuals and their family members who died in their 60s. In the past, individuals would develop renal failure, stroke, or cardiomyopathy before being diagnosed and treated, but now we can begin treating them earlier and head off those outcomes.
“We have many options, and their number is increasing. We now diagnose patients when they are younger and maybe presymptomatic, when therapies have much greater potential to ameliorate their lives.”
Dr. Raymond spoke hopefully: “With gene therapy, people with Fabry disease will no longer need enzyme replacement or chaperone therapy. Ultimately, if gene therapy proves to be as efficacious as we hope, without big downsides, we will, essentially, be curing Fabry.”
Concluding remarks
In summing up, the four experts quoted in this article offered the following observations and advice for neurologists:
Dr. Mellin. “Pain has a significant impact on quality of life for patients with Fabry disease. Identifying and adequately treating neuropathic pain can be life-changing.”
Ms. Lauderdale. “Reach out to geneticists and other appropriate specialists. We all need to communicate the needs of our patients to ensure they receive the best possible patient-centered care.”
Dr. Rastogi. “Fabry disease is an area of active research that can be a prototype for, and affect the outcomes of, other genetic disorders. I expect to see more centers of excellence for the study and treatment of Fabry disease.”
Dr. Raymond. “With therapies rapidly evolving, neurologists need to consider rare diseases and think about how to build them into their diagnostic schemes.”
Dr. Raymond, Dr. Mellin, and Ms. Lauderdale, have nothing to disclose. Dr. Rastogi discloses a financial relationship with several pharmaceutical and biopharmaceutical companies involved in Fabry disease therapeutics research and development, including Amicus Therapeutics, Chiesi Global Rare Diseases, Genzyme Sanofi, Sanofi S.A., Idorsia Pharmaceuticals Ltd., and Protalix Biotherapeutics.
Additional recommended reading
Beck M et al. Twenty years of the Fabry Outcome Survey (FOS): Insights, achievements, and lessons learned from a global patient registry. Orphanet J Rare Dis. 2022;17(1):238. doi: 10.1186/s13023-022-02392-9.
Beraza-Millor M et al. Novel golden lipid nanoparticles with small interference ribonucleic acid for substrate reduction therapy in Fabry disease. Pharmaceutics. 2023;15(7):1936. doi: 10.3390/pharmaceutics15071936.
Ezgu F et al. Expert opinion on the recognition, diagnosis and management of children and adults with Fabry disease: A multidisciplinary Turkey perspective. Orphanet J Rare Dis. 2022;17(1):90. doi: 10.1186/s13023-022-02215-x.
Fabry disease registry & pregnancy sub-registry. ClinicalTrials.gov Identifier: NCT00196742. Updated July 13, 2023. Accessed Sept. 13, 2023. https://www.clinicaltrials.gov/study/NCT00196742?term=Fabry%20Disease%20Registry%20%26%20Pregnancy%20Sub-registry&rank=1.
Umer M and Kalra DK. Treatment of Fabry disease: established and emerging therapies. Pharmaceuticals. 2023;16(2):320. doi: 10.3390/ph16020320.
Weidemann F et al. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887. doi: 10.3390/ijms23031887.
References
1. Efficacy and safety of lucerastat oral monotherapy in adult subjects with Fabry disease (MODIFY). ClinicalTrials.gov Identifier: NCT03425539. Updated Aug. 9, 2022. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03425539?term=NCT03425539&rank=1.
2. A study to evaluate the long-term safety and tolerability of lucerastat in adult subjects with Fabry disease. ClinicalTrials.gov Identifier: NCT03737214. Updated Aug. 16, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT03737214?term=NCT03737214&rank=1.
3. Evaluate the safety, pharmacodynamics, pharmacokinetics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02228460. Updated Dec. 17, 2019. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02228460?term=NCT02228460&rank=1.
4. Evaluation of the long-term safety, pharmacodynamics, and exploratory efficacy of GZ/SAR402671 in treatment-naive adult male patients with Fabry disease. ClinicalTrials.gov Identifier: NCT02489344. Updated March 23, 2023. Accessed Sept. 18, 2023. https://www.clinicaltrials.gov/study/NCT02489344?term=NC
The dawning age of therapy for Friedreich ataxia
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
It took 160 years but, in February 2023, the Food and Drug Administration approved the first drug specifically designed to treat the rare neuromuscular disease Friedreich ataxia (FA). The disease, first described in 1863 by German physician Nikolaus Friedreich, has an estimated incidence of 1 in 50,000 worldwide. It is the most common form of hereditary ataxia, accounting for approximately 50% of all cases of ataxia and approximately 75% of cases among patients younger than 25 years in the United States.1
FA typically presents in childhood or early adolescence; in some patients, symptoms manifest in the middle of the third decade of life. Patients exhibit symptoms such as ataxia that becomes worse over time, gait ataxia, impaired sensation in the extremities that can spread centrally, loss of normal reflexes, especially in the knees, speech disorders (dysarthria), muscle spasticity, scoliosis, and dysphagia.
Severity of disease ranges from relatively mild to completely disabling. Symptoms are progressive; patients almost inevitably require ambulatory support or a wheelchair. They might develop diabetes mellitus and can lose hearing and vision as the disease progresses. Hypertrophic cardiomyopathy is the most common cause of death among FA patients. Some patients who have less severe features might live into their 60s – even beyond that age.2There is no cure for FA. Until recently, no therapy was available other than supportive care to address associated neuromuscular, cardiovascular, and metabolic complications.
Making the diagnosis
Genetic testing can provide a definitive diagnosis of FA. (The genetic etiology of the disease is described later in this article.)
In addition to genetic screening, the workup includes a thorough medical history and physical examination that focuses on problems with balance, proprioception, absence of reflexes, and neurological signs. Tests include electromyography, nerve-conduction studies, electrocardiography, a metabolic profile, and MRI of the brain and spinal cord.
MRI utility in FA. In a paper published in July 2023 in Brain Communications, investigators from the University of Minnesota, Minneapolis, reported that various MRI techniques can be combined to detect early-stage alterations and disease progression in patients with FA.3 The researchers compared images taken at baseline and at 1, 2, and 3 years in 28 FA patients and 20 age- and gender-matched controls.
They observed that, compared with controls, patients with FA had lower cerebellar white matter volume but not lower cerebellar gray matter volume; larger cerebellar peduncle, thalamus, and brain stem structures; and a higher volume of the fourth ventricle. Using diffusion-tensor imaging and fixel-based analysis of diffusion MRI metrics, they also detected microstructural differences in several brain regions – especially in the cerebellum and corticospinal tract.
“Over time, many of these macrostructural and microstructural alterations progressed, especially cerebellar gray- and white-matter volume and microstructures of the superior cerebellar peduncle, the posterior limb of the internal capsule, and the superior corona radiata,” the investigators reported. In addition, “linear regressions showed significant associations between many of those imaging metrics and clinical scales.”
Pathophysiological basis of FA
The underlying genetic pathology of FA was first described in 1996 by investigators from the University of Valencia (Spain). They reported that FA is caused by a mutation in FXN (formerly X25), a gene that encodes for the protein frataxin, which is important for producing mitochondrial adenosine triphosphate and managing iron stores.4
The mutation results in multiple guanine-adenine-adenine repeats in FXN, or, in a few cases, a point mutation or deletion in 1 allele of FXN, with multiple GAA repeats in the other allele. A hallmark of FA is impairment of cellular antioxidative defense mechanisms – a major cause of disease progression.
The GAA repeat leads to methylation of the promoter region of FXN. This results in production and accumulation in cells of an abnormal, ineffective form of frataxin and oxidative damage to cells, particularly those that require larger amounts of energy, such as cells in the brain, heart, and pancreas.
“You would expect that the cells would be revving up all of their endogenous defenses,” David Lynch, MD, PhD, director of the Friedreich ataxia program at Children’s Hospital of Philadelphia, explained in an interview. “These oxidative damage responses are controlled by a DNA response element called the antioxidant response element, and it’s activated by the transcription factor Nrf2 [nuclear factor erythroid 2–related factor 2].”
Treatment options have been limited
Omaveloxolone. Dr. Lynch is principal investigator for the MOXIe trial of the safety, pharmacodynamics, and efficacy of omaveloxolone (marketed as Skyclarys [Reata Pharmaceuticals]),5 which received FDA orphan drug, fast track, priority review, and rare pediatric disease designations for the treatment of FA and, in February 2023, formal FDA approval.6 Development of this drug, which activates Nrf2 and induces antioxidant target genes, arose from basic science investigation into mechanisms by which cells respond to stresses.
“Omaveloxolone works on the Nrf2 pathway, which is, paradoxically, deficient in FA,” Dr. Lynch said. “This pathway should be active all the time. You would expect that, in cells from Friedreich ataxia in a person or an animal model of the disease, you’d see that Nrf2 would be very active but, in fact, what you find is the opposite,” Dr. Lynch explained. “It’s relatively inefficient, it’s localized in the cell, and the antioxidant response element genes – the things we all use to protect ourselves from mitochondrial damage – are all relatively turned off.”
In the first phase of MOXIe, 103 patients with FA were randomly assigned to receive either omaveloxolone, 15 mg orally (51 patients), or placebo (52 patients) for 48 weeks.
The primary endpoint was change in the modified Friedreich’s Ataxia Rating Scale (mFARS) score at 48 weeks. The scale is a clinically validated neurological instrument that evaluates upper- and lower-limb coordination, upright stability, and bulbar function.
Patients assigned to placebo had worsening of function at 48 weeks (mean increase in mFARS score, 0.85). In contrast, patients assigned to omaveloxolone had a mean decrease in the mFARS score of –1.56, indicating improvement. The between-group difference of –2.41 points was statistically significant in favor of omaveloxolone (P = .038).
In a 3-year, post hoc, propensity-matched analysis, patients assigned to omaveloxolone had lower mFARS scores than a matched set of untreated patients in a study of the natural history of FA.7Dimethyl fumarate (marketed as Tecfidera [Biogen]), approved in the United States and other countries for the treatment of patients with relapsing forms of multiple sclerosis, also has Nrf2 as a therapeutic target, although its precise mechanism of action is unclear. Clinical trials of this agent for the treatment of FA are under consideration in Europe, Dr. Lynch said.
Apart from these agents, treatment of patients with FA largely centers on management of metabolic and cardiac complications; physical and occupational therapy; devices such as orthopedic shoes, canes, and wheelchairs; and, when indicated, surgery to correct skeletal problems or for implantation of a cardiac-assist device.
The FA therapeutic pipeline
According to the Friedreich’s Ataxia Research Alliance, other approaches to improving mitochondrial function and reducing oxidative stress in FA are under investigation or awaiting approval, including elamipretide, for which FDA approval is pending for Barth syndrome (a rare, X-linked disorder) and for primary mitochondrial myopathy; nicotinamide adenine dinucleotide (NAD+, a coenzyme for redox reactions) plus exercise; and MIB-626, a crystalline form of nicotinamide mononucleotide, a precursor of NAD+.
Vatiquinone, an investigational inhibitor of 15-lipoxygenase, a regulator of energetic and oxidative stress pathways, failed to meet its primary endpoint of significant improvement on the mFARS score at 72 weeks of follow-up in the MOVE-FA trial, according to the manufacturer, PTC Therapeutics.8Another therapeutic approach under investigation is modulation of frataxin-controlled metabolic pathways with leriglitazone, an orally available selective peroxisome proliferator-activated receptor gamma agonist,9 or with the prodrug precursor of monomethyl fumarate plus dimethyl fumarate.
CTI-1601, a recombinant fusion protein intended to deliver human frataxin into the mitochondria of patients with FA, is in phase 1 trials. This compound has been granted rare pediatric disease designation, fast track designation, and orphan drug status by the FDA, according to the manufacturer, Larimar Therapeutics.10Etravirine, a nonnucleoside reverse transcriptase inhibitor approved for treating HIV infection, has been demonstrated to increase the frataxin protein in cells derived from FA patients and in the heart and skeletal muscle of frataxin-deficient YG8 mice. This agent recently completed a phase 2 trial in patients with FA.11
Gene therapy: Promising
Given the genetic etiology of FA, gene therapy strategies aimed at either increasing FA gene expression or editing the genome to replace defective FXN are under active investigation.
Increasing FA gene expression. DT-216 (Design Therapeutics) is a novel, gene-targeted chimera small molecule designed to target the GAA repeat expansion mutation and restore FXN expression. This agent completed phase 1 dosing studies in 2022.
Oligonucleotides, which are nucleic acid polymers primarily used for gene silencing, are also being explored for increasing the expression of FXN, in research at the University of Texas Southwestern Medical Center, Dallas, and the University of Massachusetts, Worcester.
Gene replacement strategies under investigation to treat FA include LX2006 (Lexeo Therapeutics), a gene replacement therapy using an adeno-associated viral vector to deliver FXN intravenously, with the goal of getting the gene into myocardial cells and increasing the frataxin level in mitochondria.
A similar approach is being taken by Ronald G. Crystal, MD, and colleagues at Weill Cornell Medicine, New York. The group is designing phase 1 studies of AAVrh.10hFXN, a serotype rh.10 adeno-associated virus coding for human frataxin, with the goal of treating cardiac manifestations of FA.12FA researcher Arnulf H. Koeppen, MD, from the Samuel S. Stratton Department of Veterans Affairs Medical Center, Albany, N.Y., and Albany Medical College, said in an interview that gene replacement therapy in FA is focused on the heart “because there is no blood-heart barrier, but there is a blood-brain barrier that makes it more complicated for gene therapy to reach the brain.”
Future directions
Dr. Koeppen, Dr. Lynch, and colleagues Ian H. Harding, PhD, from Monash University, Melbourne, and Massimo Pandolfo, MD, McGill University, Montreal, conducted an extensive review of FA with a focus on challenges that researchers and drug developers face crafting therapies for this complex disorder.13
They noted that FA is “characterized by marked differences in the vulnerability of neuronal systems. In general, the proprioceptive system appears to be affected early, while later in the disease, the dentate nucleus of the cerebellum and, to some degree, the corticospinal tracts degenerate.”
The authors took a deep dive into the evidence, old and new, to evaluate the effects of FA on the central and peripheral nervous systems and to look at the course of neuropathologic changes associated with the disease. They propose a comprehensive approach to identify nervous system locations that are likely to be most successfully targeted at different disease time points.
“The proprioceptive system, usually considered a major target for frataxin-restoring treatments, shows substantial evidence of hypoplasia and/or early developmental loss, with minimal evidence of progression over time,” they wrote. “It seems likely that this system is not an ideal target for therapies given after early childhood. Targeting the [dentate nucleus] of the cerebellum is likely to be most effective early in the course of the disease, when it is functionally affected, but still shows limited atrophy. The corticospinal tract degenerates over time contributing to disease progression throughout its late stages and may be considered a target.”
David Lynch, MD, PhD, and Arnulf Koeppen, MD, disclose support from the Friedreich’s Ataxia Research Alliance. Dr. Lynch also discloses support from the National Institutes of Health, U.S. Food and Drug Administration, Muscular Dystrophy Association, Reata Pharmaceuticals, and Retrotope.
References
1. Williams CT and De Jesus O. Friedreich ataxia. StatPearls. 2023 Jun 27. https://www.ncbi.nlm.nih.gov/books/NBK563199/.
2. National Institute of Neurological Disorders and Stroke. Friedreich ataxia. 2023 Sep 2. https://www.ninds.nih.gov/health-information/disorders/friedreich-ataxia.
3. Adanyeguh IM et al. Brain Commun. 2023;5(4):fcad196. doi: 10.1093/braincomms/fcad196.
4. Camapuzano V et al. Science. 1996;271(5254):1423-7. doi: 10.1126/science.271.5254.1423.
5. RTA 408 capsules in patients with Friedreich’s ataxia–MOXIe. ClinicalTrials. gov Identifier: NCT02255435. 2022 Dec 6. https://clinicaltrials.gov/study/NCT02255435.
6. Food and Drug Administration. FDA approves first treatment for Friedreich’s ataxia. 2023 Feb 28. www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-friedreichs-ataxia#.
7. Lynch DR et al. Ann Clin Transl Neurol. 2023 Sep 10. doi: 10.1002/acn3.51897
8. PTC Therapeutics. PTC Therapeutics announces topline results from vatiquinone MOVE-FA registration-directed trial. 2023 May 23. https://ir.ptcbio.com/news-releases/news-release-details/ptc-therapeutics-announces-topline-results-vatiquinone-move-fa.
9. Minoryx Therapeutics. The FRAMES Clinical Study in FRDA. https://www.minoryx.com/clinical-studies/clinical-study-frames/.
10. Larimar Therapeutics. CTI-1601 for Friedreich’s ataxia. https://larimartx.com/our-programs/cti-1601/.
11. Safety and efficacy of etravirine in Friedreich ataxia patients (FAEST1). ClinicalTrials.gov Identifier: NCT04273165. 2023 Mar 20. https://clinicaltrials.gov/study/NCT04273165.
12. Phase IA study of AAVrh.10hFXN gene therapy for the cardiomyopathy of Friedreich’s ataxia. ClinicalTrials.gov Identifier: NCT05302271. https://clinicaltrials.gov/study/NCT05302271.
13. Harding IH et al. Hum Gene Ther. 2020;31(23-24):1226-36. doi: 10.1089/hum.2020.264
A new chapter for research on treating Huntington’s disease
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
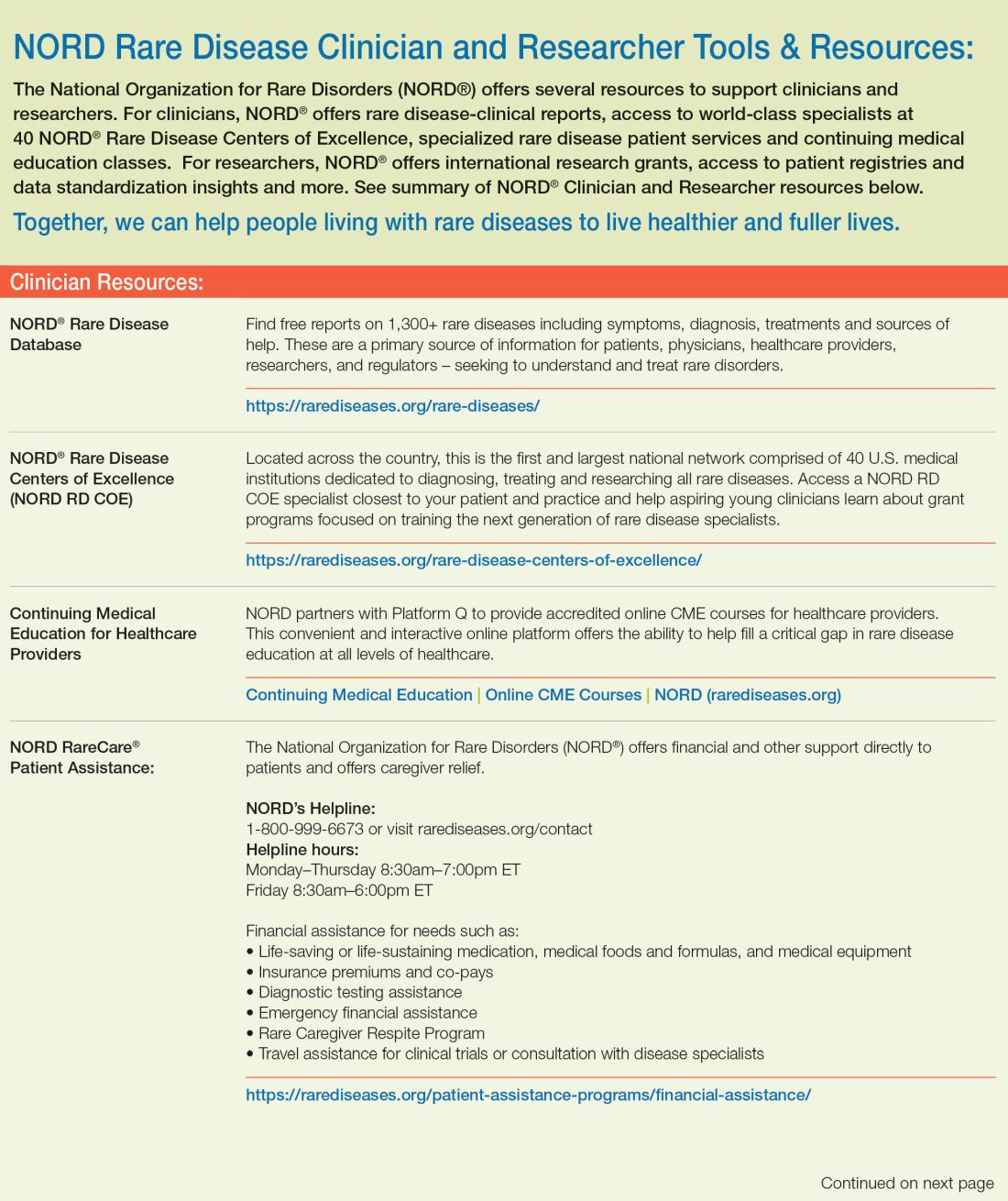
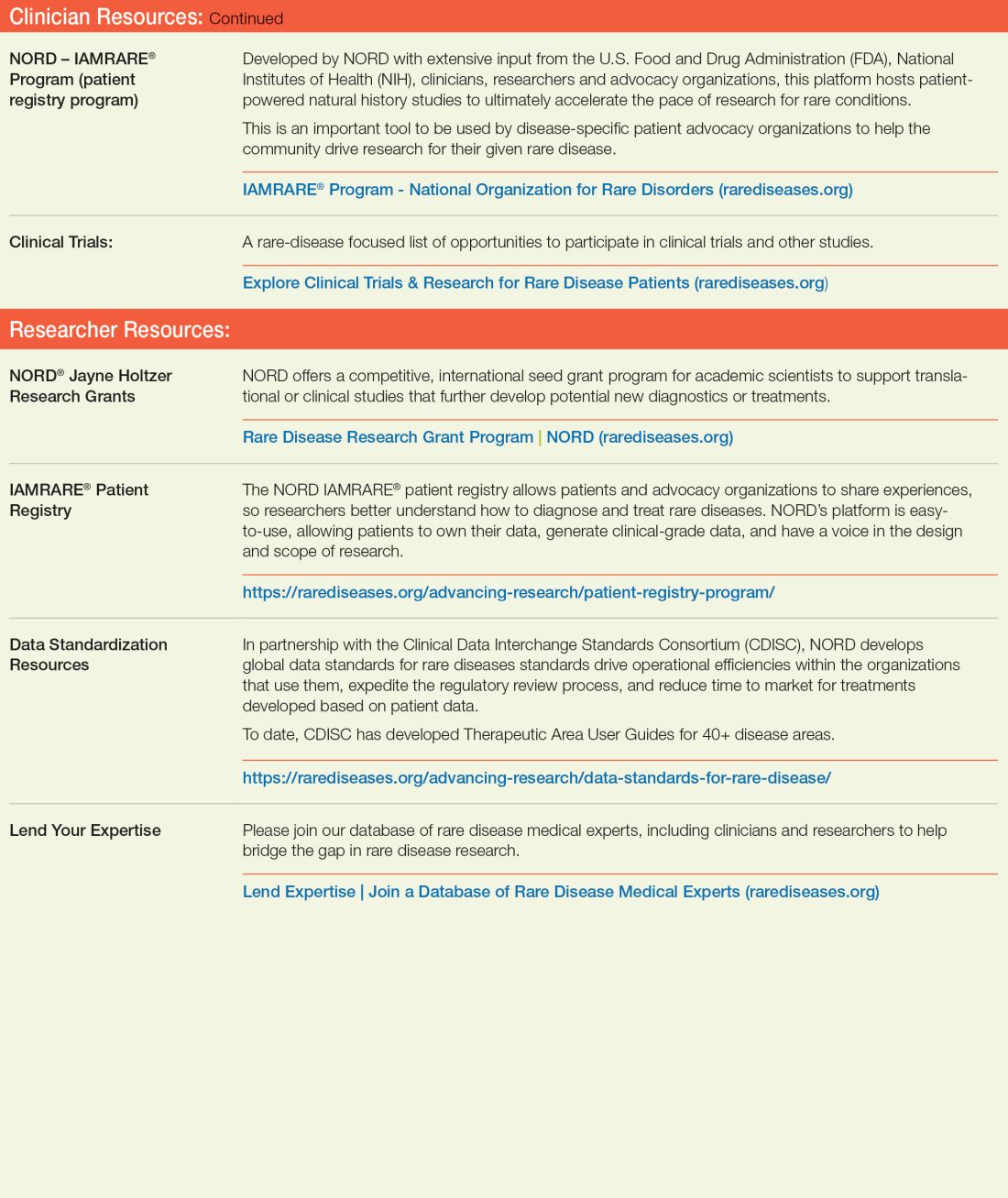
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
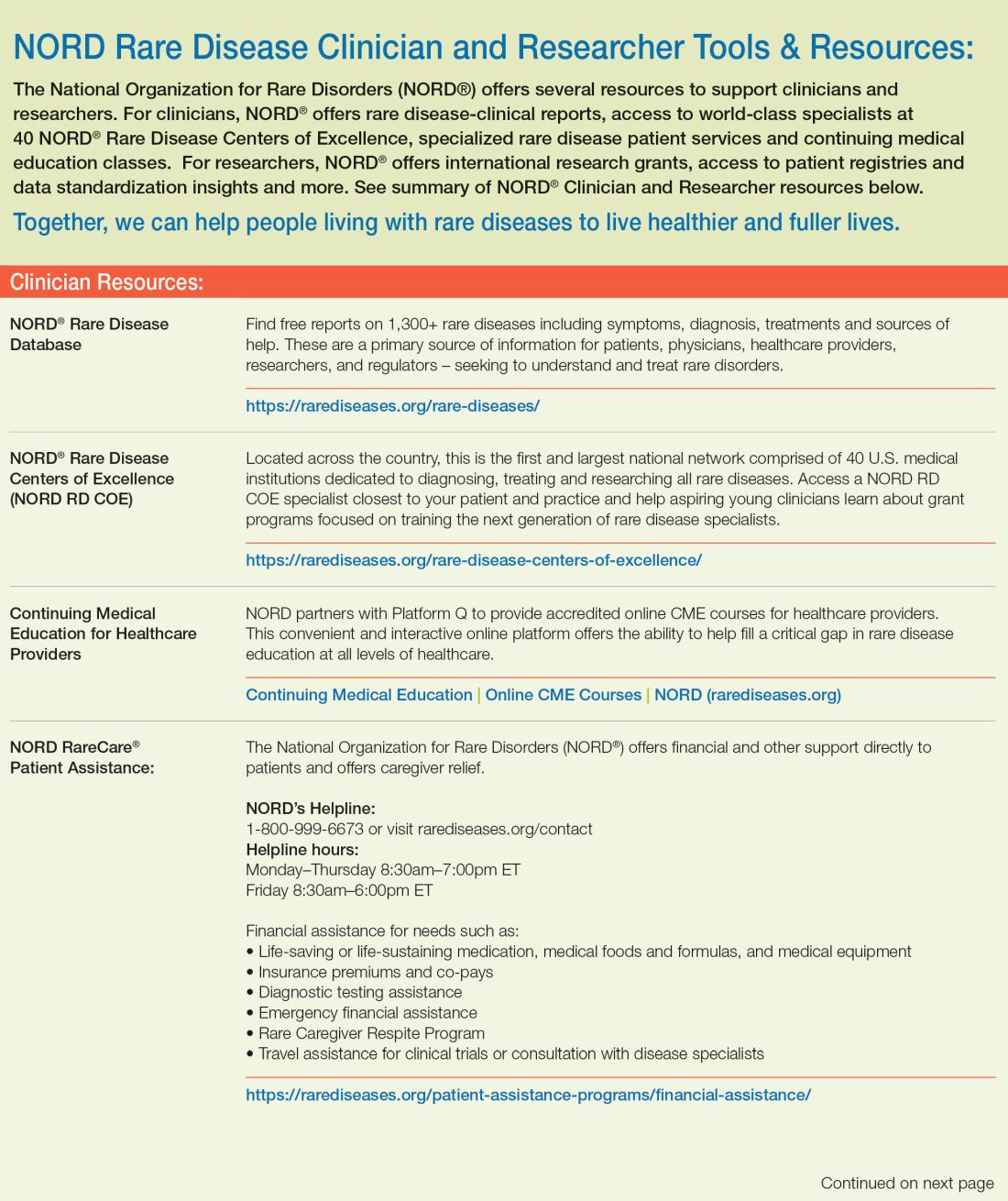
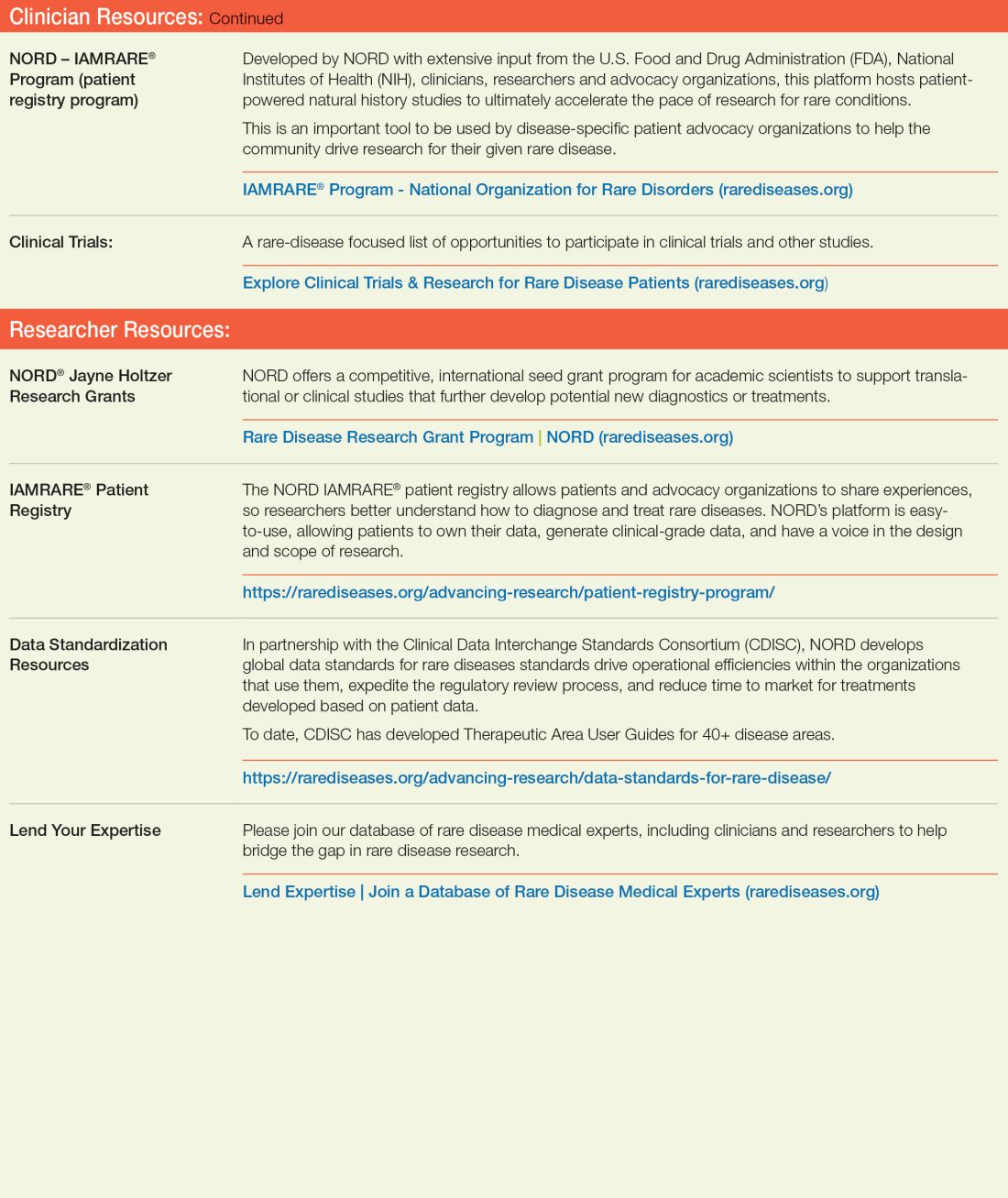
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
In 1976, Abbey S. Meyers, a mother from Connecticut, finally got a diagnosis for her son. He had been displaying “very bizarre symptoms,” Ms. Meyers said in an interview with IndoUSRare,1 but, eventually, at 8 years of age, he was given a diagnosis of Tourette syndrome.
“They tried some medicine to try to get him to sit still, but the drugs didn’t work – or if they did, they put him to sleep,” she recounted. “The teachers would be angry that he fell asleep in the classroom.”
Ms. Meyers consulted the late Arthur K. Shapiro, MD, at what was then named the Mount Sinai School of Medicine in New York. Dr. Shapiro was conducting a small clinical trial of pimozide, a drug under investigation for schizophrenia, for its utility in children with Tourette syndrome.
“The drug worked like magic,” Ms. Meyers reported. Her son’s symptoms were substantially reduced, without sedation. He was followed by Dr. Shapiro every 3 months, at which point he would receive a 90-day refill.
However, when her son turned 10 years of age, Dr. Shapiro was no longer able to provide refills: The Food and Drug Administration (FDA) had turned down the drug manufacturer’s application for approval of pimozide for a schizophrenia indication. The company opted not to pursue further development of the drug because it was not deemed profitable.2
Pimozide became unavailable in the United States. The fact that the drug was so promising for Tourette syndrome did not warrant further investment because Tourette syndrome affected a relatively small number of people.
“I was just devastated,” Ms. Meyers reported.
Springing into advocacy
Ms. Meyers, who was working with the Tourette Syndrome Association at the time (now the Tourette Association of America), contacted people from other rare disease organizations, including the National Huntington’s Disease Association (today the Huntington’s Disease Society of America) and the Paget Foundation (today part of the Bone Health and Osteoporosis Foundation). Those organizations were experiencing similar problems with drug companies that wouldn’t engage in research and development of drugs for patients who had a rare disorder.
“We realized we had to work together to get something done to solve this problem,” Ms. Meyers said.
The sense of urgency over this roadblock increased when another patient who was taking pimozide tried to get a supply of the drug from Canada and was blocked from doing so by customs officials at the airport because the drug was not FDA approved. Working with that patient’s mother, Ms. Meyers contacted U.S. Representative Henry A. Waxman (D-Calif.), who was chair of the Subcommittee on Health and the Environment of the House Energy & Commerce Committee.
Ms. Meyers thought that Congress needed Rep. Waxman’s support if it was going to get involved with this problem. “So, we got Henry Waxman and his staff familiar with the orphan drug problem.”
ODA: Breakthrough legislation
The impetus for the Orphan Drug Act (ODA) started in 1979 with an FDA task force report calling for measures to address what was labeled the “orphan drug problem.”3
In 1982, Rep. Waxman convened a hearing and invited several pharmaceutical companies to attend. They declined the invitation. Ms. Meyers testified at the hearing, which was covered by the Los Angeles Times, giving the issue notoriety.
The issue was also addressed in the popular television series Quincy, M.E. Episodes depicted challenges facing a patient with Tourette syndrome and a patient with myoclonus. Series star Jack Klugman testified before Congress about the need for legislation regarding the development of drugs targeting the treatment of rare diseases.4
Rep. Waxman became the bill’s primary House sponsor. The ODA was approved by the House of Representatives on Dec. 14, 1982.
The combined efforts of the advocacy coalition ultimately culminated in the original ODA being signed into law by President Ronald Reagan on Jan. 4, 1983. The ODA incentivized pharmaceutical companies to allot more resources toward research on and development and distribution of therapeutics for people with a rare disease who had, until that point, been “orphaned,” so to speak, by the medical and scientific community.5
What is it to be a ‘rare disorder’ or an ‘orphan drug’?
The ODA defines a rare disorder as either a condition that affects fewer than 200,000 people or a condition that affects more than 200,000 people but for which there is no reasonable expectation that a pharmaceutical company will recoup the cost of developing a drug by selling it.5
In an interview Peter L. Saltonstall, president and CEO of the National Organization for Rare Disorders, commended Ms. Meyers on her tireless work: “She went from being a mom to a powerful advocate who got thousands of people in D.C. moving Congress to a point where they felt passing the law was necessary. In fact, she was there when the bill was signed into law.”
The FDA can grant orphan drug approval for several categories of products. These include new molecular entities, already-approved drugs for which an additional indication has been designated, and new formulations of existing or established drugs.5
Orphan-drug designation includes tax credits for the developer-manufacturer, a waiver of the usual approval fees that the company must pay to the FDA, and 7 years’ market exclusivity, during which time the FDA cannot award approval of similar treatments for the same indication.
“This [designation] ensures that the company that developed the drug can retain the opportunity for profit,” explained Mr. Saltonstall. “Companies thought: ‘We can afford to do this now. And if we market it the right way and have exclusivity, we can recover some of our profits.’”
Before the ODA, 30 drugs had been approved by the FDA for orphan conditions. By the end of 2022, more than 880 drugs were FDA approved to treat hundreds of rare disorders.
“This just shows the motivation and how the process works,” Mr. Saltonstall said. In fact, almost 50% of novel drugs approved in 2022 by the FDA were an orphan product or had an orphan indication.
In addition to the impact on drug development in the United States, enactment of the ODA had a broader ripple effect, inspiring similar changes internationally in Europe, Australia, Singapore, Japan, and other regions.5
NORD is born
The creation of NORD was initiated by the same group of advocates who lobbied tirelessly for passage of the ODA – including Ms. Meyers, who served as president of the organization for many years. Heidi Ross, MPH, NORD’s vice president of policy and regulatory affairs, called these advocates “trailblazers.”
NORD was founded in May 1983. The organization included, at that time, 40-50 disease-specific organizations. Today, NORD membership comprises more than 330 patient advocacy groups.
“The goal was to be a voice for those organizations and help get them mobilized, help them get their 501(c)3 [status], help them develop their relationship with the FDA, and similar tasks,” Mr. Saltonstall said. “We continue this important work today as the patient groups play a central role in driving care, research, and policies for their given disease. Also, there’s strength in numbers. We call upon these groups and members to help advocate in Washington for policies that impact the greater rare disease community.”
The ODA launched 4 decades of innovation and change, with NORD strengthening the rare disorder community, which encompasses more than 30 million Americans.
“The organization exists to support people living with rare disorders and tries to improve their quality of life,” according to Katie Kowalski, MPH, NORD’s associate director of education.
Education. The role of Ms. Kowalski’s department is to “educate patients and caregivers, the general public, health care professionals, and students preparing for health care careers about rare conditions,” Ms. Kowalski said. The education department maintains NORD’s Rare Disease Database,6 which contains more than 1,300 reports about rare conditions. Plus, NORD’s Rare Disease Library archives videos about specific diseases and other topics of interest to the rare disease community, including genetic testing and gene therapy.Continuing medical education programs are available for health care providers.
Events. NORD hosts:
An annual Rare Diseases and Orphan Products Breakthrough Summit for various rare disease stakeholders, including global rare disease medical experts, policy makers, regulatory agencies, industry leaders, and patient community members.
An annual patient and family conference; the 2024 edition is scheduled for June 7-8, 2024, in Los Angeles.
Membership support. NORD’s membership department supports any advocacy organization that represents a rare
disorder. “Some [organizations] are more evolved and sophisticated and can do their own educational programming,” Ms. Kowalski said. “Others are fledgling, nascent organizations that may not have the staff or money for salaries. We try to support them, teach them how to budget and raise funds and form a board of directors.”
Advocacy. NORD has a policy department that works at state and federal levels to advocate for policies affecting patients with a rare disease. Mr. Saltonstall shared that NORD was responsible for setting up and helping put together the rare disease office at the National Institutes of Health and the FDA, and continues to foster a close relationship with those offices.8,9 “In fact,” he said, “nothing happens in Washington regarding rare diseases without our being consulted or at the table.”
Focus on the patient. Mr. Saltonstall assumed his role at NORD in 2008. “By then, many fundamental things had been mastered, and we were ready to take things to the next level,” he said. “There were opportunities to leverage the ODA to help patient organizations.”
“We’re one of the only nonprofit advocacy organizations I know of without industry on the board or as members,” Mr. Saltonstall said. “The organization is completely patient focused. Everything we do comes back to committees with patients who make the decisions and management who helps implement those decisions. This makes us unique. The fact that we’re independent makes Congress trust us to be the true voice of patients.”
Spotlight: Patient care and research
Edward Neilan, MD, PhD, recently joined NORD as chief medical and scientific officer. As a pediatrician, medical geneticist, and molecular biologist, Dr. Neilan became acquainted with NORD as far back as medical school and his residency, when he used a book called the NORD Guide to Rare Disorders to help him explain certain diseases to patients and families.10 “I had a favorable view of NORD because of how useful the book was,” he said.
Dr. Neilan had also received research funding from NORD, almost 20 years ago – a pilot grant for Cockayne syndrome, an extremely rare multisystem genetic disorder characterized by premature aging. “At any given time, there are only about 100 or so identified patients with this condition.”11
Pilot grants are awarded after NORD announces a request for proposals and the proposals received are scored by rare disease medical experts, Dr. Neilan explained. “Because this grant helped me research the condition and get my academic career moving, I always had a warm spot for NORD.”
Excellence in care. Dr. Neilan assumed his position at NORD to become involved with the NORD Rare Disease Centers of Excellence program, which he describes as encouraging “collaboration with, and between, dozens of leading medical centers around the country.”
Dr. Neilan is the first physician to work full time at NORD. “Taking the step of designating and directing collaboration amongst centers of excellence around the country seemed to require having a full-time physician on board,” he said, “so I decided to jump in.”
Ms. Kowalski elaborated: “NORD’s Rare Disease Centers of Excellence includes 11 different working groups to address the big problems that need to be solved in rare diseases: working collaboratively. [This] is sometimes rare in academic medicine, but necessary, especially when there aren’t many patients with a given condition.”
Since Dr. Neilan’s arrival, NORD has designated 40 institutions across the country as a NORD Rare Disease Centers of Excellence.12
Natural history research
NORD’s research department awards seed grants to academic investigators who are researching rare disorders and has built an online patient registry platform that helps other, disease-specific patient advocacy organizations conduct natural history studies.
Dr. Neilan said that the registry program was motivated by input from the FDA indicating that companies were sometimes trying to develop drugs to treat a rare disease before fully understanding the natural history of that disease.
“There was a perceived lack of enough natural history data,” Dr. Neilan explained, “so how could the effectiveness of the drug be measured? What would be a meaningful improvement?” NORD assists in making these rare disease foundations more “research ready” so that enough will be known about the disease for drug development “to have a greater chance of success.”
“There’s a lot of promise on the horizon with gene therapy, and the new platforms may accelerate the production of these therapies,” Ms. Kowalski said.
Registries are customized to each disease and foundation by experts, patients, and families involved with that particular disease and foundation. For example: An ongoing study on the NORD platform is a study of metachromatic leukodystrophy (MLD), an autosomal-recessive lysosomal disorder that results in a buildup of sulfatides, a major lipid group in serum, which lead to destruction of the myelin sheath and progressive demyelination of the nervous system.13
“[MLD] is a tragic disorder that can first present in late infancy and may progress rapidly over 6 months or so to the point that children lose much of their neurological functioning,” Dr. Neilan said.
The FDA funded NORD to run the HOME study,14,15 in which families can participate without visiting a research site in person. This was particularly valuable during the COVID-19 pandemic, when many studies were “forced to shift gears and see how much data could be collected if patients were afraid to come to the hospital or not allowed to go to a hospital for nonemergency visits,” Dr. Neilan said.
The HOME study was designed before the onset of the COVID-19 pandemic to reduce the burden on patients of participating in research. The trial became a trend-setter in the shift to what are known as decentralized trials, in which research can be conducted through video, using a tablet that NORD mails to the family.
“This is obviously much more convenient for families who no longer have to travel long distances to the few sites in the country – which are often hundreds or even thousands of miles away – that are studying the condition,” Dr. Neilan said. The decentralized trial model is being used with other conditions, as well.
“There are infantile, juvenile, and adult-onset forms of MLD, and the limited therapeutic options may involve bone-marrow transplant, which may be at least partially effective, as donor-derived bone marrow–derived cells can provide enzymes to protect the brain,” said Dr. Neilan. Gene therapy for MLD has also been developed and is approved in Europe, but not in the United States. “MLD is typical of conditions that often start early in childhood and are progressive, so that, sometimes, by the time the parent realizes that there’s a problem, too much damage has been done to the brain for much repair to take place. Prevention of further damage is easier than reversing an ongoing disease process, so early treatment is important.” That’s why the number of movements to expand newborn screening for various conditions, to identify them before symptoms develop, is increasing.
“That’s another area where NORD has historically been active – in encouraging newborn screening,” Dr. Neilan said.
Evolution of the ODA
Since 1983, “a number of amendments ... made the original [ODA] stronger or refined it in various ways,” said Mr. Saltonstall. NORD continues to “very carefully watch any attempts to change it, alter it, move it, take pieces away from it, or – some people say – to make it ‘better.’ To us, it’s a very important law.”
Orphan Drug Credit (ODC). Ms. Ross elaborated: “In recent years, Congress has considered significant changes to the Orphan Drug Credit, which is one of several critical incentives established by the ODA.” When established in 1983, the ODC provided sponsors of a drug with a 50% tax credit for qualified clinical testing expenses associated with developing an orphan drug.
“Unfortunately, despite fierce opposition from NORD and our army of membership organizations and grassroots advocates,” Ms. Ross said, “the Tax Cuts and Jobs Act of 2017 reduced the ODC from 50% to 25%. Given the significant amount of time it takes to conduct research and development into rare diseases, we still don’t have a good sense as to the impact of the ODC being reduced to 25%.”
However, efforts to further limit the availability of the ODC during debate around the Build Back Better framework in 2021 were ultimately defeated. That defeat was, in part, a result of NORD’s rare disease community’s advocacy,16 when no changes to the ODC were included in the Inflation Reduction Act.
Patient Assistance Program. In 1987, NORD’s multifaceted patient assistance program (serving today under the umbrella name RareCare17) was founded to help patients obtain lifesaving or life-sustaining medication that they could not otherwise afford, Ms. Ross said. This was based on an unmet need for patients living and struggling with a rare disease who didn’t have access to the care and treatment they needed. “There was no other foundation equipped to do this at the time. NORD came forward to develop the first program of its kind.”
The program provides medication, financial assistance with insurance premiums and copays, diagnostic testing assistance, and travel assistance for clinical trials or consultation with disease specialists. According to Ms. Ross, “today, NORD’s patient assistance program provides, on average, $30 million to $40 million in patient assistance annually to eligible patients and families.”
Pharmaceutical companies do contribute to the patient assistance program. “However, they’re in the dark as to how the money is allocated,” said Mr. Saltonstall. “For example, a given company might donate money for patients with a particular disease but won’t know if patients who have that disease will necessarily receive funds to use toward that company’s drug. The patient might receive assistance to take a drug made by a different company – a competitor.”
There are approximately 14 foundations around the country that have worked within the constraints of the Department of Health & Human Services Office of Inspector General, which established rules about how foundations must operate. Under the broader umbrella of NORD, these foundations also help pay coinsurance costs or provide drugs at no cost to patients who meet financial criteria.
An enduring movement
Despite the successes brought about by the ODA, the search for new rare disorder treatments is far from over. We know of more than 7,000 rare diseases; scientists discover more every year. Fewer than 5% of rare disorders have an FDA-approved treatment.
Similar to advancements made in other diseases, progress in rare disease care and treatments will continue to require an all-in approach to solve what is a looming and massive public health challenge.
As NORD founder Abbey S. Meyers wrote in her 2016 book, Orphan Drugs: A Global Crusade: “It was all of us working together that built an impregnable movement demanding a solution. In the end, with the help of government and a touch of Hollywood, the forces opposing us could not win.”
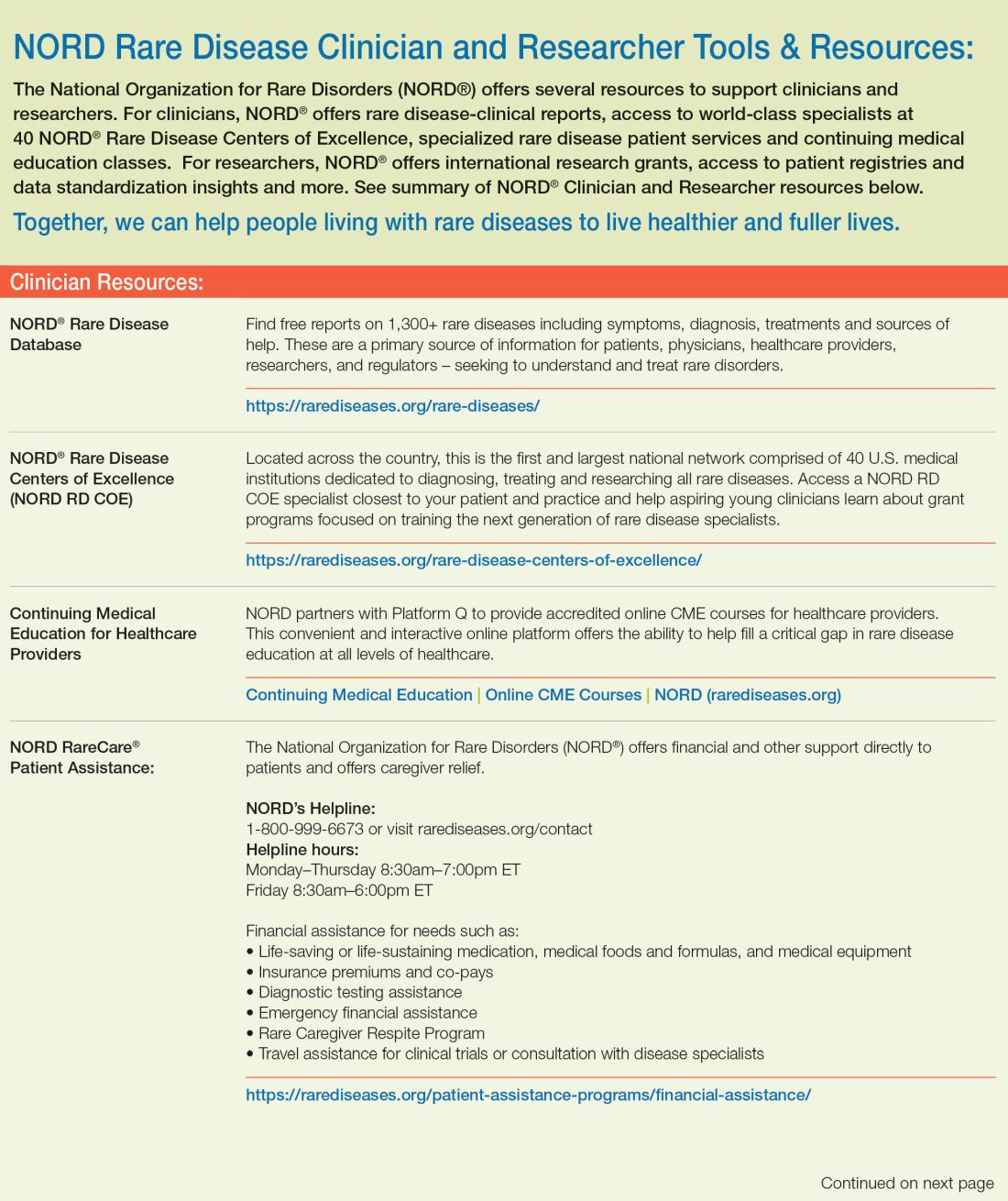
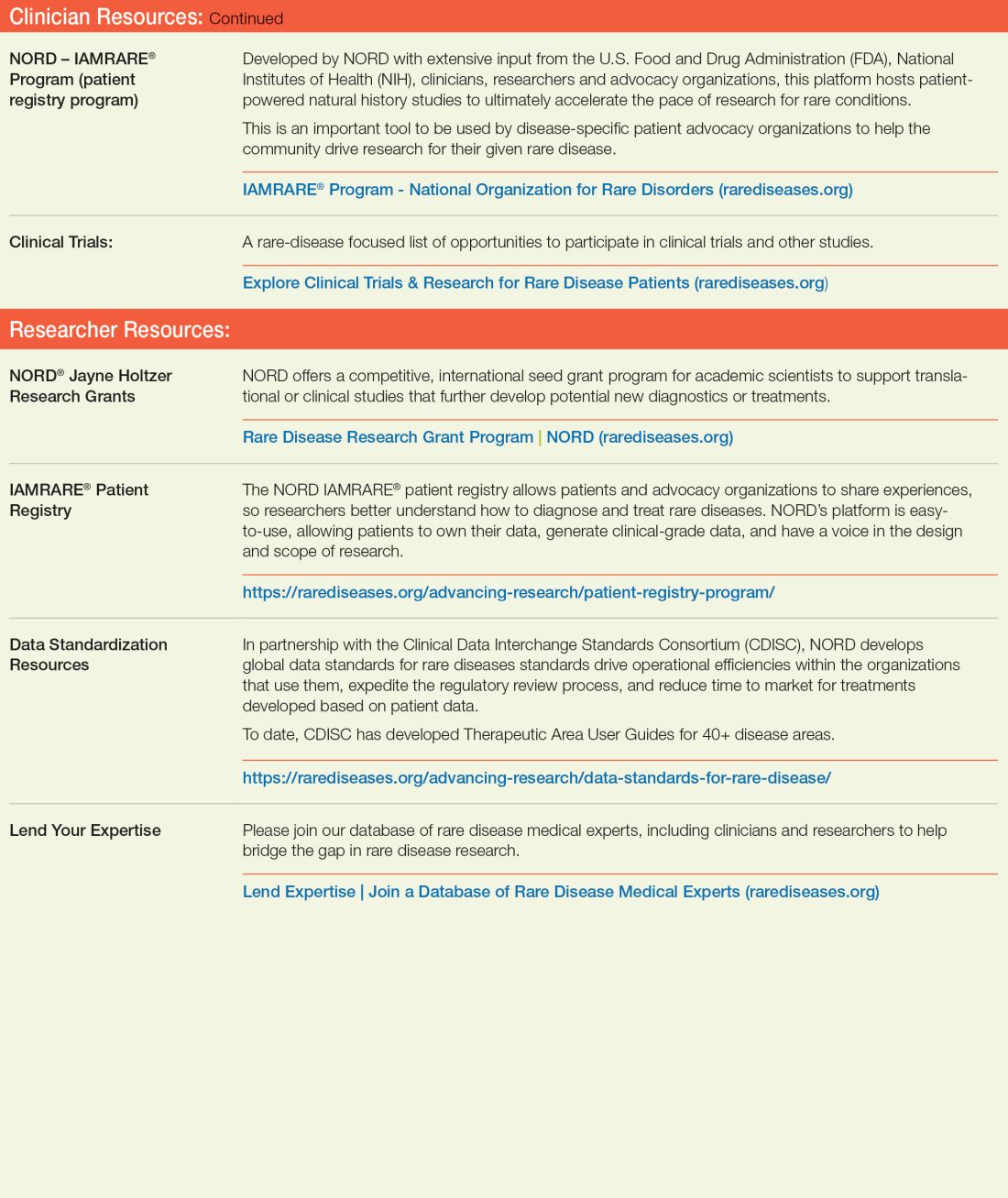
References
1. Rare Disease Day 2023 at IndoUSrare – Fireside Chat with Dr. Abbey S. Meyers. 2023 Mar 3. Indo US Organization for Rare Diseases. https://www.youtube.com/watch?v=fGTWUcQJPlU.
2. Mikami K. Soc Hist Med. 2019;32(3):609-30. doi: 10.1093/shm/hkx098.
3. National Organization for Rare Disorders. The Orphan Drug Act Turns 40: NORD Celebrates Its Impact on Rare Diseases. 2023 Jan 4. https://rarediseases.org/the-orphan-drug-act-turns-40-nord-celebrates-its-impact-on-rare-diseases. 4. Swann J. The story behind the Orphan Drug Act. US Food and Drug Administration. 2018 Feb 23. https://www.fda.gov/industry/fdas-rare-disease-day/story-behind-orphan-drug-act.
5. Roberts A-D and Wadhwa R. Orphan drug approval laws, in StatPearls (Internet). StatPearls Publishing. 2023 Jun 5. www.ncbi.nlm.nih.gov/books/NBK572052/#.
6. National Organization for Rare Disorders. Rare disease database. https://rarediseases.org/rare-diseases/.
7. National Organization for Rare Disorders. Rare disease video library. 2023 Jan 19. https://rarediseases.org/video-library/.
8. National Center for Advancing Translational Sciences. Rare disease research and resources. 2023 May 16. Accessed Sep. 17., 2023. https://ncats.nih.gov/rare-diseases.
9. Food and Drug Administration. Rare diseases team. 2023 Aug 29. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/rare-diseases-team.
10. National Organization for Rare Disorders. “NORD Guide to Rare Disorders,” 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2002.
11. National Organization for Rare Disorders. Cockayne syndrome. 2022 Jun 7. https://rarediseases.org/rare-diseases/cockayne-syndrome/.
12. National Organization for Rare Disorders. NORD Rare Disease Centers of Excellence. 2023 Jun 28. https://rarediseases.org/rare-disease-centers-of-excellence/.
13. National Organization for Rare Disorders. Metachromatic leukodystrophy. 2022 Mar 22. https://rarediseases.org/rare-diseases/metachromatic-leukodystrophy/#complete-report.
14. National Organization for Rare Disorders. The Natural History of Metachromatic Leukodystrophy Study. 2023 Feb 23. https://rarediseases.org/mld-home-study/.
15. The Natural History of Metachromatic Leukodystrophy Study (HOME Study). 2023 Jun 13. https://clinicaltrials.gov/study/NCT04628364?.
16. National Organization for Rare Disorders, Saltonstall PL. Letter to US Congress House Committee on Ways and Means. 2021 Sep 13. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
17. National Organization for Rare Disorders. RareCare®: NORD’s patient assistance programs. 2022 Nov 1. https://rarediseases.org/wp-content/uploads/2022/04/NORD_ODTC-Letter_FINAL.pdf.
2023 Rare Neurological Disease Special Report
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.
INTRODUCTIONS
Editor’s note
By Glenn S. Williams
2023 is indeed a noteworthy year. As you will read in this issue, it marks the 40th anniversary of the landmark Orphan Drug Act (ODA) and the formation of the National Organization for Rare Disorders. 2023 also marks the 30th anniversary of Neurology Reviews, the parent publication of the Rare Neurological Disease Special Report.
A note from NORD
By Edward Neilan, MD, PhD
The coalition of rare disease advocates who sparked rare disease advocacy and convinced lawmakers to pass the ODA in 1983 established NORD that same year to provide an ongoing, unified voice for the needs of the rare disease community.
Rare disease roundup
A look back at some of the 2023 rare disease headlines from Neurology Reviews.
CLINICAL REVIEWS
The Orphan Drug Act and NORD at their 40th anniversary: Dramatic achievements and ongoing innovation
By Batya Swift Yasgur, MA, MSW
The movement whose face is ODA and NORD continues to build its legacy. Next? Progress in rare disease care will require an all-in approach to solving a looming and massive public health challenge.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
By Frieda Wiley, PharmD
Newly approved and investigational therapies, and enhanced diagnostics, are sparking optimism about treating MD – especially Duchenne and facioscapulohumeral types.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
By Ted Bosworth
Optimism is high about improving the survival and care of ALS patients. Neurologists who don’t specialize in ALS can add to the positivity by endorsing a role in speedier diagnostic pathways.
A new chapter for research on treating Huntington’s disease
By Jennie Smith
Setbacks in trials of protein-lowering therapies – mostly over their safety – mask a story of rapid advances and a more recently discovered treatment pathway that also offers promise for other diseases.
The dawning age of therapy for Friedreich ataxia
By Neil Osterweil
The first therapy to target the underlying pathology of Friedreich ataxia was approved in 2023. Other drug and genetic therapies are in the pipeline.
Stiff person syndrome: When a rare disorder hits the headlines
By Kate Johnson
Awareness of this disorder is increasing, but clinicians are challenged to apply the proper workup to avoid wrong turns in identifying affected patients.
Advances in testing and therapeutics are improving the lives of patients with Fabry disease
By Lorraine L. Janeczko, MPH
Thanks to robust research efforts, treatment options are expanding and patients are getting their diagnosis earlier – often, when they are presymptomatic and treatment has greater potential for enhancing quality of life.
Guillain-Barré syndrome: Honing treatment strategies
By John Jesitus
Classic subtypes of Guillain-Barré syndrome are varying manifestations of a shared disease process, novel insights into the disease indicate. This understanding is yielding new treatment strategies.
Has prompt diagnosis of amyotrophic lateral sclerosis become urgent?
Amyotrophic lateral sclerosis (ALS) falls easily into the Food and Drug Administration definition of “rare disease.” With an estimated prevalence in the United States of fewer than 20,000 cases,1 ALS sits comfortably below the cutoff of 200,000 cases that serves to define a disease as “rare.”
After a recent steep climb, there are something on the order of 50 therapies, across more than 10 drug classes, in clinical trials for the treatment of ALS.2 This bounty represents exciting progress toward the development of targeted therapies for a characteristically fatal disease.
That headway is coupled with a sobering limitation, however: Relatively few ALS patients are being enrolled.
The knotty problem with therapeutic trials for ALS
“Trials are generally designed for patients with adequate functional reserve and predicted survival, to ensure that a signal of benefit can be seen,” said Nicholas John Maragakis, MD, director of the ALS Clinical Trials Unit at Johns Hopkins University, Baltimore. “Many of my patients are too severely affected at presentation.”
Dr. Maragakis hasn’t calculated the precise percentage of patients he is enrolling in one of the many available trials available at the Johns Hopkins center. He estimates that it is less than 20%, however.
That percentage is comparable to what is reported by Stephen Scelsa, MD, and Daniel J. Macgowan, MD, who share much of the ALS caseload in a dedicated, comprehensive ALS center at Mount Sinai Beth Israel, New York. Both are on the faculty at the Icahn School of Medicine at Mount Sinai.
“The considerable delay in the diagnosis of ALS remains a challenge,” Dr. Scelsa acknowledges. Like Dr. Maragakis, he reports that, by the time patients develop symptoms that make referral to a comprehensive ALS center like Mount Sinai Beth Israel appropriate, many no longer meet eligibility criteria for most experimental treatments.
Some therapeutic targets in clinical trials, such as neuroinflammation, offer potential benefit even in advancing disease, but it is prevention that is usually the goal of experimental ALS therapies. This approach is associated with far more promise than attempting to reverse existing neurologic damage, which might not be possible, according to both Dr. Scelsa and Dr. Macgowan.
“The clinical trials are typically looking for patients with less than 2 years since the onset of symptoms and at least 60% of predicted respiratory function,” Dr. Macgowan said.
Because of these or other similarly restrictive criteria, coupled with common delays before patients arrive at a center where trials are available, “the window for clinical research closes very quickly,” Dr. Macgowan added, and “the band of patients who are eligible is relatively narrow.”
At Hennepin Healthcare in Minneapolis, which, like Johns Hopkins and Mount Sinai, offers an advanced multidisciplinary approach to ALS care in a dedicated clinic, the problem of late referrals is no different. Samuel Maiser, MD, chair of neurology, does attempt to counter this delay by moving quickly.
“I almost always offer a therapeutic trial to a patient with early-stage ALS,” he said. He does so earlier, rather than later, and explains: “I do not want to delay that conversation, because any delay might reduce the chance for getting into a trial.”
The generalist can make a difference in therapeutic success
The proliferation of clinical trials has made early diagnosis of ALS urgent. However, the experts interviewed for this article agreed: Accelerating the time to diagnosis is more dependent on the general neurologist or primary care physician than on the ALS specialist. ALS is a diagnosis of exclusion, but there is now very little delay in reaching a probable diagnosis at a dedicated center.
Yet neurodegenerative complaints in early-stage ALS are often nonspecific and mild; confidence in making a potential diagnosis of ALS is limited among primary care clinicians and general neurologists, who almost always see these patients first. Usually, the problem is not failure to include ALS in the differential diagnosis but hesitation in being candid when there is still doubt.
General neurologists, in particular, Dr. Maragakis said, “are often highly suspicious of a diagnosis of ALS very early on but are concerned about using this term until the clinical signs are more compelling.”
This is understandable. There is reluctance to deliver bad news when confidence in the diagnosis is limited. But the experts agreed: Delayed diagnosis is not in the patient’s interest now that there is at least the potential for entering a trial supported by a scientific rationale for benefit.
“Waiting for 100% certainty – this could actually harm our patients,” Dr. Maiser said. The tendency to avoid delivering bad news, he said, “is human nature, and it is not easy to tell people that ALS is the potential cause, but it’s important for early treatment.”
Some evidence suggests that the incidence of ALS is increasing3 but this is not necessarily evident at the clinical level. “It is not my impression that the incidence of ALS is increasing,” Dr. Macgowan said, “so much as I think we are getting better at making the diagnosis.”
Where we stand: Pathophysiology, diagnosis, treatment
Pathophysiology. ALS is characterized by muscle denervation.4 In the great majority of cases, the disease represents a proteinopathy involving loss of the TDP-43 protein from nuclei. However, pathological heterogeneity means that other pathophysiological mechanisms – mediated by oxidative stress, mitochondrial dysfunction, and neurotoxicity related to excessive stimulation of postsynaptic glutamate receptors – can participate.2,5,6
Approximately 10% of patients have a known gene associated with ALS.7 The rest have what is considered sporadic ALS, although some experts estimate that heritability will eventually be confirmed in 50% or more of cases that have been given the “sporadic” label.8,9 More than 30 genes have been linked to ALS in genomewide association studies. Among patients whose disease carries a known familial link, four genes – SOD1, TARDBP, FUS, and C9orf72 – account for approximately 70% of cases.2
Diagnosis. Genetic testing in patients with suspected or confirmed ALS is the standard of care at most, if not all, comprehensive ALS treatment centers, according to the four experts interviewed by Neurology Reviews 2023 Rare Neurological Disease Special Report for this article. Such testing was routine for years because of its potential for helping researchers to understand subtypes of disease; today, testing has assumed even greater practical value with recent approval of the first ALS gene therapy: Tofersen (Qalsody, Biogen), licensed in 2023, is an antisense oligonucleotide therapy that targets SOD1 mRNA to reduce production of the SOD1 protein, a mediator of disease progression.
“Genetic testing has been useful for telling us something about the disease and its prognosis,” Dr. Maragakis said, “but an approved gene therapy means it can have a direct effect on treatment.”
ALS therapeutics. Other gene therapies are in development. Gene signatures are likely to provide even more opportunities for clinical trials in the future.
Following three loading doses of tofersen at 14-day intervals, the maintenance regimen, administered intrathecally by lumbar puncture, is every 28 days. In the phase 3 trial, tofersen reduced levels of SOD1 protein and neurofilament light chain, a biomarker of axonal injury.10 Tofersen is appropriate only in patients with SOD1-associated ALS; the drug’s favorable clinical impact, including a positive effect, if any, on survival has not been demonstrated. Extension studies are underway.
Tofersen joins three other FDA-approved ALS therapies:
• Riluzole, an oral drug available since 1995 that slows disease progression by blocking glutamate.
• Edaravone, an antioxidant approved in 2017, administered orally or intravenously.
• An orally administered combination of sodium phenylbutyrate and taurursodiol marketed as Relyvrio and formerly known as AMX0035, that was introduced in 2022.
“We offer riluzole, which is safe in combination with other therapies, to most patients,” said Dr. Scelsa, who noted that treatment trials often test experimental drugs on top of riluzole. He moves to edaravone or Relyvrio, which are far more expensive, selectively. Tofersen, which is also expensive, is reserved for patients with SOD1-associated disease; however, not all eligible patients opt for this therapy after reviewing its benefits and risks.
“There is not yet a guarantee that tofersen will improve outcomes, and it requires intrathecal injections for life,”
Dr. Maiser said. “Some patients, particularly my older patients, have said, ‘No thank you,’ based on the available data.”
Dr. Macgowan pointed out that lumbar puncture repeated indefinitely can be “challenging.” He, too, discusses all available treatment options with every patient, including riluzole, which he agreed is associated with a meaningful benefit, particularly when started early.
Because of the safety of riluzole, Dr. Maragakis takes early treatment a step further. For neurologists who have a high level of suspicion of ALS in a given patient, “my advice would be to treat aggressively from the get-go. Even if not 100% certain of the diagnosis, I would start them on riluzole while waiting for confirmation.” Like the other experts interviewed here, he acknowledged that referral to a busy comprehensive ALS center often takes time, making it reasonable to initiate treatment when suspicion is high.
On the front lines, “the neurologist can tell the patient that ALS is just one of several potential explanations for symptoms but there is concern,” said Dr. Maragakis, proposing a strategy to introduce the possibility of ALS and start treatment that might slow disease while waiting for confirmation of the diagnosis. “My biggest concern is that no one is making that call,” he said, trying to address at least one reason for the current delay in making referrals.
Comprehensive care at specialty centers
Whenever possible, ALS is a disease best managed at a center that offers comprehensive management, including multidisciplinary care. On this point, the four experts agreed.
“Tertiary-care centers for ALS serve a critical purpose,”
Dr. Maiser said. For a disease that affects nearly every aspect of life, the skills of a multidisciplinary support staff offer an “opportunity to stay in front of the disease” for as long as possible. Teamwork often leads to “outside-of-the-box thinking” for helping patients and families cope with the range of disabilities that undermine the patient’s quality of life.
Details of ALS management matter. At Mount Sinai and Hennepin Healthcare, and at Johns Hopkins, where demand recently led to the opening of a second ALS clinic, the ALS center is set up to address the full spectrum of needs. Staff members have multiple skills so that they can work together to make patients comfortable and prepare them for what is inevitably progression – even if the rate of that progression varies.
All these centers incorporate a rational, thorough discussion of end-of-life options in a palliative care approach that targets optimized quality of life. One goal is to prepare patients to consider and be prepared to make decisions when it is time for tracheostomy, percutaneous endoscopic gastrostomy, and other life support options that are not always well tolerated. The goal? Avoiding unnecessary anguish during end-stage disease when impaired respiratory function – the primary cause of ALS-related death – no longer sustains unassisted survival.
“I am concerned for the many ALS patients without access to this type of comprehensive care,” Dr. Macgowan said.
Like the other experts here, he emphasized that the demands of ALS care can be “overwhelming” outside a comprehensive care setting – for the patient, their family, and individual providers.
Looking ahead
There are many reasons to be optimistic about improving the survival and care of patients with ALS. Besides therapies in clinical trials, Dr. Scelsa explained, there is the potential role for monitoring neurofilament light changes, a biomarker of neurodegeneration, in patients who are at risk of ALS.
Dr. Maragakis offered an analogy to the gene therapy onasemnogene abeparvovec, which can prevent the associated neurodegeneration of spinal muscular atrophy if initiated before symptoms appear. He said that, in ALS, neurofilament light changes or other biomarkers might offer an opportunity to halt the progression of disease before it starts – if one or more therapies in development prove workable.
In the meantime, neurologists who do not specialize in ALS should be thinking about how they can participate in speedier diagnostic pathways.
“There are a number of therapies that look promising,” Dr. Maiser told Rare Neurological Disease Special Report. He singled out strategies to degrade TDP-43 or prevent it from forming. If these treatments are found effective, it’s expected that they would be of value in sporadic ALS, the most common form. Again, though, “the challenge is getting patients on this therapy at the earliest stages of disease.”
Dr. Maragakis discloses equity ownership/stock options with Braintrust Bio and Akava; he is a patent holder with Johns Hopkins [ALS] and has received grant/research/clinical trial support from Apellis Pharma, Biogen Idec, Cytokinetics, Helixmith, Calico, Sanofi, Department of Defense ALSRP, Maryland Stem Cell Research Fund, Massachusetts General Hospital, Medicinova, and NINDS. He serves as consultant or advisory board member for Amylyx; Cytokinetics, Roche, Healey Center, Nura Bio, Northeast ALS Consortium, Akava, Inflammx, and Secretome. Dr. Scelsa did not report any conflicts of interest. Dr. Macgowan and Dr. Maiser have no relevant conflicts of interest to disclose.
References
1. Mehta P et al. Prevalence of amyotrophic lateral sclerosis in the United States using established and novel methodologies, 2017. Amyotroph Lateral Scler Frontotemporal Degener. 2023;24(1-2):108-16. doi: 10.1080/21678421.2022.2059380.
2. Mead RJ et al. Amyotrophic lateral sclerosis: A neurodegenerative disorder poised for successful therapeutic translation. Nat Rev Drug Discov. 2023;22(3):185-212. doi: 10.1038/s41573-022-00612-2.
3. Longinetti E and Fang F. Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr Opin Neurol. 2019;32(5):771-6. doi: 10.1097/WCO.0000000000000730.
4. van den Bos MAJ et al. Pathophysiology and diagnosis of ALS: Insights from advances in neurophysiological techniques. Int J Mol Sci. 2019;20(11):2818. doi: 10.3390/ijms20112818.
5. Neumann M et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130-3. doi: 10.1126/science.1134108.
6. Ling S-C et al. Converging mechanisms in ALS and FTD: Disrupted RNA and protein homeostasis. Neuron. 2013;79(3):416-38. doi: 10.1016/j.neuron.2013.07.033.
7. Ranganathan R et al. Multifaceted genes in amyotrophic lateral sclerosis-frontotemporal dementia. Front Neurosci. 2020;14:684. doi: 10.3389/fnins.2020.00684.
8. Ryan M et al. Lifetime risk and heritability of amyotrophic lateral sclerosis. JAMA Neurol. 2019;76(11):1367-74. doi: 10.1001/jamaneurol.2019.2044.
9. van Rheenen W et al. Common and rare variant association analyses in amyotrophic lateral sclerosis identify 15 risk loci with distinct genetic architectures and neuron-specific biology. Nat Genet. 2021;53(12):1636-48. doi: 10.1038/s41588-021-00973-1.
10. Miller TM et al; VALOR and OLE Working Group. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N Engl J Med. 2022;387(12):1099-110. doi: 10.1056/NEJMoa2204705.
Amyotrophic lateral sclerosis (ALS) falls easily into the Food and Drug Administration definition of “rare disease.” With an estimated prevalence in the United States of fewer than 20,000 cases,1 ALS sits comfortably below the cutoff of 200,000 cases that serves to define a disease as “rare.”
After a recent steep climb, there are something on the order of 50 therapies, across more than 10 drug classes, in clinical trials for the treatment of ALS.2 This bounty represents exciting progress toward the development of targeted therapies for a characteristically fatal disease.
That headway is coupled with a sobering limitation, however: Relatively few ALS patients are being enrolled.
The knotty problem with therapeutic trials for ALS
“Trials are generally designed for patients with adequate functional reserve and predicted survival, to ensure that a signal of benefit can be seen,” said Nicholas John Maragakis, MD, director of the ALS Clinical Trials Unit at Johns Hopkins University, Baltimore. “Many of my patients are too severely affected at presentation.”
Dr. Maragakis hasn’t calculated the precise percentage of patients he is enrolling in one of the many available trials available at the Johns Hopkins center. He estimates that it is less than 20%, however.
That percentage is comparable to what is reported by Stephen Scelsa, MD, and Daniel J. Macgowan, MD, who share much of the ALS caseload in a dedicated, comprehensive ALS center at Mount Sinai Beth Israel, New York. Both are on the faculty at the Icahn School of Medicine at Mount Sinai.
“The considerable delay in the diagnosis of ALS remains a challenge,” Dr. Scelsa acknowledges. Like Dr. Maragakis, he reports that, by the time patients develop symptoms that make referral to a comprehensive ALS center like Mount Sinai Beth Israel appropriate, many no longer meet eligibility criteria for most experimental treatments.
Some therapeutic targets in clinical trials, such as neuroinflammation, offer potential benefit even in advancing disease, but it is prevention that is usually the goal of experimental ALS therapies. This approach is associated with far more promise than attempting to reverse existing neurologic damage, which might not be possible, according to both Dr. Scelsa and Dr. Macgowan.
“The clinical trials are typically looking for patients with less than 2 years since the onset of symptoms and at least 60% of predicted respiratory function,” Dr. Macgowan said.
Because of these or other similarly restrictive criteria, coupled with common delays before patients arrive at a center where trials are available, “the window for clinical research closes very quickly,” Dr. Macgowan added, and “the band of patients who are eligible is relatively narrow.”
At Hennepin Healthcare in Minneapolis, which, like Johns Hopkins and Mount Sinai, offers an advanced multidisciplinary approach to ALS care in a dedicated clinic, the problem of late referrals is no different. Samuel Maiser, MD, chair of neurology, does attempt to counter this delay by moving quickly.
“I almost always offer a therapeutic trial to a patient with early-stage ALS,” he said. He does so earlier, rather than later, and explains: “I do not want to delay that conversation, because any delay might reduce the chance for getting into a trial.”
The generalist can make a difference in therapeutic success
The proliferation of clinical trials has made early diagnosis of ALS urgent. However, the experts interviewed for this article agreed: Accelerating the time to diagnosis is more dependent on the general neurologist or primary care physician than on the ALS specialist. ALS is a diagnosis of exclusion, but there is now very little delay in reaching a probable diagnosis at a dedicated center.
Yet neurodegenerative complaints in early-stage ALS are often nonspecific and mild; confidence in making a potential diagnosis of ALS is limited among primary care clinicians and general neurologists, who almost always see these patients first. Usually, the problem is not failure to include ALS in the differential diagnosis but hesitation in being candid when there is still doubt.
General neurologists, in particular, Dr. Maragakis said, “are often highly suspicious of a diagnosis of ALS very early on but are concerned about using this term until the clinical signs are more compelling.”
This is understandable. There is reluctance to deliver bad news when confidence in the diagnosis is limited. But the experts agreed: Delayed diagnosis is not in the patient’s interest now that there is at least the potential for entering a trial supported by a scientific rationale for benefit.
“Waiting for 100% certainty – this could actually harm our patients,” Dr. Maiser said. The tendency to avoid delivering bad news, he said, “is human nature, and it is not easy to tell people that ALS is the potential cause, but it’s important for early treatment.”
Some evidence suggests that the incidence of ALS is increasing3 but this is not necessarily evident at the clinical level. “It is not my impression that the incidence of ALS is increasing,” Dr. Macgowan said, “so much as I think we are getting better at making the diagnosis.”
Where we stand: Pathophysiology, diagnosis, treatment
Pathophysiology. ALS is characterized by muscle denervation.4 In the great majority of cases, the disease represents a proteinopathy involving loss of the TDP-43 protein from nuclei. However, pathological heterogeneity means that other pathophysiological mechanisms – mediated by oxidative stress, mitochondrial dysfunction, and neurotoxicity related to excessive stimulation of postsynaptic glutamate receptors – can participate.2,5,6
Approximately 10% of patients have a known gene associated with ALS.7 The rest have what is considered sporadic ALS, although some experts estimate that heritability will eventually be confirmed in 50% or more of cases that have been given the “sporadic” label.8,9 More than 30 genes have been linked to ALS in genomewide association studies. Among patients whose disease carries a known familial link, four genes – SOD1, TARDBP, FUS, and C9orf72 – account for approximately 70% of cases.2
Diagnosis. Genetic testing in patients with suspected or confirmed ALS is the standard of care at most, if not all, comprehensive ALS treatment centers, according to the four experts interviewed by Neurology Reviews 2023 Rare Neurological Disease Special Report for this article. Such testing was routine for years because of its potential for helping researchers to understand subtypes of disease; today, testing has assumed even greater practical value with recent approval of the first ALS gene therapy: Tofersen (Qalsody, Biogen), licensed in 2023, is an antisense oligonucleotide therapy that targets SOD1 mRNA to reduce production of the SOD1 protein, a mediator of disease progression.
“Genetic testing has been useful for telling us something about the disease and its prognosis,” Dr. Maragakis said, “but an approved gene therapy means it can have a direct effect on treatment.”
ALS therapeutics. Other gene therapies are in development. Gene signatures are likely to provide even more opportunities for clinical trials in the future.
Following three loading doses of tofersen at 14-day intervals, the maintenance regimen, administered intrathecally by lumbar puncture, is every 28 days. In the phase 3 trial, tofersen reduced levels of SOD1 protein and neurofilament light chain, a biomarker of axonal injury.10 Tofersen is appropriate only in patients with SOD1-associated ALS; the drug’s favorable clinical impact, including a positive effect, if any, on survival has not been demonstrated. Extension studies are underway.
Tofersen joins three other FDA-approved ALS therapies:
• Riluzole, an oral drug available since 1995 that slows disease progression by blocking glutamate.
• Edaravone, an antioxidant approved in 2017, administered orally or intravenously.
• An orally administered combination of sodium phenylbutyrate and taurursodiol marketed as Relyvrio and formerly known as AMX0035, that was introduced in 2022.
“We offer riluzole, which is safe in combination with other therapies, to most patients,” said Dr. Scelsa, who noted that treatment trials often test experimental drugs on top of riluzole. He moves to edaravone or Relyvrio, which are far more expensive, selectively. Tofersen, which is also expensive, is reserved for patients with SOD1-associated disease; however, not all eligible patients opt for this therapy after reviewing its benefits and risks.
“There is not yet a guarantee that tofersen will improve outcomes, and it requires intrathecal injections for life,”
Dr. Maiser said. “Some patients, particularly my older patients, have said, ‘No thank you,’ based on the available data.”
Dr. Macgowan pointed out that lumbar puncture repeated indefinitely can be “challenging.” He, too, discusses all available treatment options with every patient, including riluzole, which he agreed is associated with a meaningful benefit, particularly when started early.
Because of the safety of riluzole, Dr. Maragakis takes early treatment a step further. For neurologists who have a high level of suspicion of ALS in a given patient, “my advice would be to treat aggressively from the get-go. Even if not 100% certain of the diagnosis, I would start them on riluzole while waiting for confirmation.” Like the other experts interviewed here, he acknowledged that referral to a busy comprehensive ALS center often takes time, making it reasonable to initiate treatment when suspicion is high.
On the front lines, “the neurologist can tell the patient that ALS is just one of several potential explanations for symptoms but there is concern,” said Dr. Maragakis, proposing a strategy to introduce the possibility of ALS and start treatment that might slow disease while waiting for confirmation of the diagnosis. “My biggest concern is that no one is making that call,” he said, trying to address at least one reason for the current delay in making referrals.
Comprehensive care at specialty centers
Whenever possible, ALS is a disease best managed at a center that offers comprehensive management, including multidisciplinary care. On this point, the four experts agreed.
“Tertiary-care centers for ALS serve a critical purpose,”
Dr. Maiser said. For a disease that affects nearly every aspect of life, the skills of a multidisciplinary support staff offer an “opportunity to stay in front of the disease” for as long as possible. Teamwork often leads to “outside-of-the-box thinking” for helping patients and families cope with the range of disabilities that undermine the patient’s quality of life.
Details of ALS management matter. At Mount Sinai and Hennepin Healthcare, and at Johns Hopkins, where demand recently led to the opening of a second ALS clinic, the ALS center is set up to address the full spectrum of needs. Staff members have multiple skills so that they can work together to make patients comfortable and prepare them for what is inevitably progression – even if the rate of that progression varies.
All these centers incorporate a rational, thorough discussion of end-of-life options in a palliative care approach that targets optimized quality of life. One goal is to prepare patients to consider and be prepared to make decisions when it is time for tracheostomy, percutaneous endoscopic gastrostomy, and other life support options that are not always well tolerated. The goal? Avoiding unnecessary anguish during end-stage disease when impaired respiratory function – the primary cause of ALS-related death – no longer sustains unassisted survival.
“I am concerned for the many ALS patients without access to this type of comprehensive care,” Dr. Macgowan said.
Like the other experts here, he emphasized that the demands of ALS care can be “overwhelming” outside a comprehensive care setting – for the patient, their family, and individual providers.
Looking ahead
There are many reasons to be optimistic about improving the survival and care of patients with ALS. Besides therapies in clinical trials, Dr. Scelsa explained, there is the potential role for monitoring neurofilament light changes, a biomarker of neurodegeneration, in patients who are at risk of ALS.
Dr. Maragakis offered an analogy to the gene therapy onasemnogene abeparvovec, which can prevent the associated neurodegeneration of spinal muscular atrophy if initiated before symptoms appear. He said that, in ALS, neurofilament light changes or other biomarkers might offer an opportunity to halt the progression of disease before it starts – if one or more therapies in development prove workable.
In the meantime, neurologists who do not specialize in ALS should be thinking about how they can participate in speedier diagnostic pathways.
“There are a number of therapies that look promising,” Dr. Maiser told Rare Neurological Disease Special Report. He singled out strategies to degrade TDP-43 or prevent it from forming. If these treatments are found effective, it’s expected that they would be of value in sporadic ALS, the most common form. Again, though, “the challenge is getting patients on this therapy at the earliest stages of disease.”
Dr. Maragakis discloses equity ownership/stock options with Braintrust Bio and Akava; he is a patent holder with Johns Hopkins [ALS] and has received grant/research/clinical trial support from Apellis Pharma, Biogen Idec, Cytokinetics, Helixmith, Calico, Sanofi, Department of Defense ALSRP, Maryland Stem Cell Research Fund, Massachusetts General Hospital, Medicinova, and NINDS. He serves as consultant or advisory board member for Amylyx; Cytokinetics, Roche, Healey Center, Nura Bio, Northeast ALS Consortium, Akava, Inflammx, and Secretome. Dr. Scelsa did not report any conflicts of interest. Dr. Macgowan and Dr. Maiser have no relevant conflicts of interest to disclose.
References
1. Mehta P et al. Prevalence of amyotrophic lateral sclerosis in the United States using established and novel methodologies, 2017. Amyotroph Lateral Scler Frontotemporal Degener. 2023;24(1-2):108-16. doi: 10.1080/21678421.2022.2059380.
2. Mead RJ et al. Amyotrophic lateral sclerosis: A neurodegenerative disorder poised for successful therapeutic translation. Nat Rev Drug Discov. 2023;22(3):185-212. doi: 10.1038/s41573-022-00612-2.
3. Longinetti E and Fang F. Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr Opin Neurol. 2019;32(5):771-6. doi: 10.1097/WCO.0000000000000730.
4. van den Bos MAJ et al. Pathophysiology and diagnosis of ALS: Insights from advances in neurophysiological techniques. Int J Mol Sci. 2019;20(11):2818. doi: 10.3390/ijms20112818.
5. Neumann M et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130-3. doi: 10.1126/science.1134108.
6. Ling S-C et al. Converging mechanisms in ALS and FTD: Disrupted RNA and protein homeostasis. Neuron. 2013;79(3):416-38. doi: 10.1016/j.neuron.2013.07.033.
7. Ranganathan R et al. Multifaceted genes in amyotrophic lateral sclerosis-frontotemporal dementia. Front Neurosci. 2020;14:684. doi: 10.3389/fnins.2020.00684.
8. Ryan M et al. Lifetime risk and heritability of amyotrophic lateral sclerosis. JAMA Neurol. 2019;76(11):1367-74. doi: 10.1001/jamaneurol.2019.2044.
9. van Rheenen W et al. Common and rare variant association analyses in amyotrophic lateral sclerosis identify 15 risk loci with distinct genetic architectures and neuron-specific biology. Nat Genet. 2021;53(12):1636-48. doi: 10.1038/s41588-021-00973-1.
10. Miller TM et al; VALOR and OLE Working Group. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N Engl J Med. 2022;387(12):1099-110. doi: 10.1056/NEJMoa2204705.
Amyotrophic lateral sclerosis (ALS) falls easily into the Food and Drug Administration definition of “rare disease.” With an estimated prevalence in the United States of fewer than 20,000 cases,1 ALS sits comfortably below the cutoff of 200,000 cases that serves to define a disease as “rare.”
After a recent steep climb, there are something on the order of 50 therapies, across more than 10 drug classes, in clinical trials for the treatment of ALS.2 This bounty represents exciting progress toward the development of targeted therapies for a characteristically fatal disease.
That headway is coupled with a sobering limitation, however: Relatively few ALS patients are being enrolled.
The knotty problem with therapeutic trials for ALS
“Trials are generally designed for patients with adequate functional reserve and predicted survival, to ensure that a signal of benefit can be seen,” said Nicholas John Maragakis, MD, director of the ALS Clinical Trials Unit at Johns Hopkins University, Baltimore. “Many of my patients are too severely affected at presentation.”
Dr. Maragakis hasn’t calculated the precise percentage of patients he is enrolling in one of the many available trials available at the Johns Hopkins center. He estimates that it is less than 20%, however.
That percentage is comparable to what is reported by Stephen Scelsa, MD, and Daniel J. Macgowan, MD, who share much of the ALS caseload in a dedicated, comprehensive ALS center at Mount Sinai Beth Israel, New York. Both are on the faculty at the Icahn School of Medicine at Mount Sinai.
“The considerable delay in the diagnosis of ALS remains a challenge,” Dr. Scelsa acknowledges. Like Dr. Maragakis, he reports that, by the time patients develop symptoms that make referral to a comprehensive ALS center like Mount Sinai Beth Israel appropriate, many no longer meet eligibility criteria for most experimental treatments.
Some therapeutic targets in clinical trials, such as neuroinflammation, offer potential benefit even in advancing disease, but it is prevention that is usually the goal of experimental ALS therapies. This approach is associated with far more promise than attempting to reverse existing neurologic damage, which might not be possible, according to both Dr. Scelsa and Dr. Macgowan.
“The clinical trials are typically looking for patients with less than 2 years since the onset of symptoms and at least 60% of predicted respiratory function,” Dr. Macgowan said.
Because of these or other similarly restrictive criteria, coupled with common delays before patients arrive at a center where trials are available, “the window for clinical research closes very quickly,” Dr. Macgowan added, and “the band of patients who are eligible is relatively narrow.”
At Hennepin Healthcare in Minneapolis, which, like Johns Hopkins and Mount Sinai, offers an advanced multidisciplinary approach to ALS care in a dedicated clinic, the problem of late referrals is no different. Samuel Maiser, MD, chair of neurology, does attempt to counter this delay by moving quickly.
“I almost always offer a therapeutic trial to a patient with early-stage ALS,” he said. He does so earlier, rather than later, and explains: “I do not want to delay that conversation, because any delay might reduce the chance for getting into a trial.”
The generalist can make a difference in therapeutic success
The proliferation of clinical trials has made early diagnosis of ALS urgent. However, the experts interviewed for this article agreed: Accelerating the time to diagnosis is more dependent on the general neurologist or primary care physician than on the ALS specialist. ALS is a diagnosis of exclusion, but there is now very little delay in reaching a probable diagnosis at a dedicated center.
Yet neurodegenerative complaints in early-stage ALS are often nonspecific and mild; confidence in making a potential diagnosis of ALS is limited among primary care clinicians and general neurologists, who almost always see these patients first. Usually, the problem is not failure to include ALS in the differential diagnosis but hesitation in being candid when there is still doubt.
General neurologists, in particular, Dr. Maragakis said, “are often highly suspicious of a diagnosis of ALS very early on but are concerned about using this term until the clinical signs are more compelling.”
This is understandable. There is reluctance to deliver bad news when confidence in the diagnosis is limited. But the experts agreed: Delayed diagnosis is not in the patient’s interest now that there is at least the potential for entering a trial supported by a scientific rationale for benefit.
“Waiting for 100% certainty – this could actually harm our patients,” Dr. Maiser said. The tendency to avoid delivering bad news, he said, “is human nature, and it is not easy to tell people that ALS is the potential cause, but it’s important for early treatment.”
Some evidence suggests that the incidence of ALS is increasing3 but this is not necessarily evident at the clinical level. “It is not my impression that the incidence of ALS is increasing,” Dr. Macgowan said, “so much as I think we are getting better at making the diagnosis.”
Where we stand: Pathophysiology, diagnosis, treatment
Pathophysiology. ALS is characterized by muscle denervation.4 In the great majority of cases, the disease represents a proteinopathy involving loss of the TDP-43 protein from nuclei. However, pathological heterogeneity means that other pathophysiological mechanisms – mediated by oxidative stress, mitochondrial dysfunction, and neurotoxicity related to excessive stimulation of postsynaptic glutamate receptors – can participate.2,5,6
Approximately 10% of patients have a known gene associated with ALS.7 The rest have what is considered sporadic ALS, although some experts estimate that heritability will eventually be confirmed in 50% or more of cases that have been given the “sporadic” label.8,9 More than 30 genes have been linked to ALS in genomewide association studies. Among patients whose disease carries a known familial link, four genes – SOD1, TARDBP, FUS, and C9orf72 – account for approximately 70% of cases.2
Diagnosis. Genetic testing in patients with suspected or confirmed ALS is the standard of care at most, if not all, comprehensive ALS treatment centers, according to the four experts interviewed by Neurology Reviews 2023 Rare Neurological Disease Special Report for this article. Such testing was routine for years because of its potential for helping researchers to understand subtypes of disease; today, testing has assumed even greater practical value with recent approval of the first ALS gene therapy: Tofersen (Qalsody, Biogen), licensed in 2023, is an antisense oligonucleotide therapy that targets SOD1 mRNA to reduce production of the SOD1 protein, a mediator of disease progression.
“Genetic testing has been useful for telling us something about the disease and its prognosis,” Dr. Maragakis said, “but an approved gene therapy means it can have a direct effect on treatment.”
ALS therapeutics. Other gene therapies are in development. Gene signatures are likely to provide even more opportunities for clinical trials in the future.
Following three loading doses of tofersen at 14-day intervals, the maintenance regimen, administered intrathecally by lumbar puncture, is every 28 days. In the phase 3 trial, tofersen reduced levels of SOD1 protein and neurofilament light chain, a biomarker of axonal injury.10 Tofersen is appropriate only in patients with SOD1-associated ALS; the drug’s favorable clinical impact, including a positive effect, if any, on survival has not been demonstrated. Extension studies are underway.
Tofersen joins three other FDA-approved ALS therapies:
• Riluzole, an oral drug available since 1995 that slows disease progression by blocking glutamate.
• Edaravone, an antioxidant approved in 2017, administered orally or intravenously.
• An orally administered combination of sodium phenylbutyrate and taurursodiol marketed as Relyvrio and formerly known as AMX0035, that was introduced in 2022.
“We offer riluzole, which is safe in combination with other therapies, to most patients,” said Dr. Scelsa, who noted that treatment trials often test experimental drugs on top of riluzole. He moves to edaravone or Relyvrio, which are far more expensive, selectively. Tofersen, which is also expensive, is reserved for patients with SOD1-associated disease; however, not all eligible patients opt for this therapy after reviewing its benefits and risks.
“There is not yet a guarantee that tofersen will improve outcomes, and it requires intrathecal injections for life,”
Dr. Maiser said. “Some patients, particularly my older patients, have said, ‘No thank you,’ based on the available data.”
Dr. Macgowan pointed out that lumbar puncture repeated indefinitely can be “challenging.” He, too, discusses all available treatment options with every patient, including riluzole, which he agreed is associated with a meaningful benefit, particularly when started early.
Because of the safety of riluzole, Dr. Maragakis takes early treatment a step further. For neurologists who have a high level of suspicion of ALS in a given patient, “my advice would be to treat aggressively from the get-go. Even if not 100% certain of the diagnosis, I would start them on riluzole while waiting for confirmation.” Like the other experts interviewed here, he acknowledged that referral to a busy comprehensive ALS center often takes time, making it reasonable to initiate treatment when suspicion is high.
On the front lines, “the neurologist can tell the patient that ALS is just one of several potential explanations for symptoms but there is concern,” said Dr. Maragakis, proposing a strategy to introduce the possibility of ALS and start treatment that might slow disease while waiting for confirmation of the diagnosis. “My biggest concern is that no one is making that call,” he said, trying to address at least one reason for the current delay in making referrals.
Comprehensive care at specialty centers
Whenever possible, ALS is a disease best managed at a center that offers comprehensive management, including multidisciplinary care. On this point, the four experts agreed.
“Tertiary-care centers for ALS serve a critical purpose,”
Dr. Maiser said. For a disease that affects nearly every aspect of life, the skills of a multidisciplinary support staff offer an “opportunity to stay in front of the disease” for as long as possible. Teamwork often leads to “outside-of-the-box thinking” for helping patients and families cope with the range of disabilities that undermine the patient’s quality of life.
Details of ALS management matter. At Mount Sinai and Hennepin Healthcare, and at Johns Hopkins, where demand recently led to the opening of a second ALS clinic, the ALS center is set up to address the full spectrum of needs. Staff members have multiple skills so that they can work together to make patients comfortable and prepare them for what is inevitably progression – even if the rate of that progression varies.
All these centers incorporate a rational, thorough discussion of end-of-life options in a palliative care approach that targets optimized quality of life. One goal is to prepare patients to consider and be prepared to make decisions when it is time for tracheostomy, percutaneous endoscopic gastrostomy, and other life support options that are not always well tolerated. The goal? Avoiding unnecessary anguish during end-stage disease when impaired respiratory function – the primary cause of ALS-related death – no longer sustains unassisted survival.
“I am concerned for the many ALS patients without access to this type of comprehensive care,” Dr. Macgowan said.
Like the other experts here, he emphasized that the demands of ALS care can be “overwhelming” outside a comprehensive care setting – for the patient, their family, and individual providers.
Looking ahead
There are many reasons to be optimistic about improving the survival and care of patients with ALS. Besides therapies in clinical trials, Dr. Scelsa explained, there is the potential role for monitoring neurofilament light changes, a biomarker of neurodegeneration, in patients who are at risk of ALS.
Dr. Maragakis offered an analogy to the gene therapy onasemnogene abeparvovec, which can prevent the associated neurodegeneration of spinal muscular atrophy if initiated before symptoms appear. He said that, in ALS, neurofilament light changes or other biomarkers might offer an opportunity to halt the progression of disease before it starts – if one or more therapies in development prove workable.
In the meantime, neurologists who do not specialize in ALS should be thinking about how they can participate in speedier diagnostic pathways.
“There are a number of therapies that look promising,” Dr. Maiser told Rare Neurological Disease Special Report. He singled out strategies to degrade TDP-43 or prevent it from forming. If these treatments are found effective, it’s expected that they would be of value in sporadic ALS, the most common form. Again, though, “the challenge is getting patients on this therapy at the earliest stages of disease.”
Dr. Maragakis discloses equity ownership/stock options with Braintrust Bio and Akava; he is a patent holder with Johns Hopkins [ALS] and has received grant/research/clinical trial support from Apellis Pharma, Biogen Idec, Cytokinetics, Helixmith, Calico, Sanofi, Department of Defense ALSRP, Maryland Stem Cell Research Fund, Massachusetts General Hospital, Medicinova, and NINDS. He serves as consultant or advisory board member for Amylyx; Cytokinetics, Roche, Healey Center, Nura Bio, Northeast ALS Consortium, Akava, Inflammx, and Secretome. Dr. Scelsa did not report any conflicts of interest. Dr. Macgowan and Dr. Maiser have no relevant conflicts of interest to disclose.
References
1. Mehta P et al. Prevalence of amyotrophic lateral sclerosis in the United States using established and novel methodologies, 2017. Amyotroph Lateral Scler Frontotemporal Degener. 2023;24(1-2):108-16. doi: 10.1080/21678421.2022.2059380.
2. Mead RJ et al. Amyotrophic lateral sclerosis: A neurodegenerative disorder poised for successful therapeutic translation. Nat Rev Drug Discov. 2023;22(3):185-212. doi: 10.1038/s41573-022-00612-2.
3. Longinetti E and Fang F. Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr Opin Neurol. 2019;32(5):771-6. doi: 10.1097/WCO.0000000000000730.
4. van den Bos MAJ et al. Pathophysiology and diagnosis of ALS: Insights from advances in neurophysiological techniques. Int J Mol Sci. 2019;20(11):2818. doi: 10.3390/ijms20112818.
5. Neumann M et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130-3. doi: 10.1126/science.1134108.
6. Ling S-C et al. Converging mechanisms in ALS and FTD: Disrupted RNA and protein homeostasis. Neuron. 2013;79(3):416-38. doi: 10.1016/j.neuron.2013.07.033.
7. Ranganathan R et al. Multifaceted genes in amyotrophic lateral sclerosis-frontotemporal dementia. Front Neurosci. 2020;14:684. doi: 10.3389/fnins.2020.00684.
8. Ryan M et al. Lifetime risk and heritability of amyotrophic lateral sclerosis. JAMA Neurol. 2019;76(11):1367-74. doi: 10.1001/jamaneurol.2019.2044.
9. van Rheenen W et al. Common and rare variant association analyses in amyotrophic lateral sclerosis identify 15 risk loci with distinct genetic architectures and neuron-specific biology. Nat Genet. 2021;53(12):1636-48. doi: 10.1038/s41588-021-00973-1.
10. Miller TM et al; VALOR and OLE Working Group. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N Engl J Med. 2022;387(12):1099-110. doi: 10.1056/NEJMoa2204705.
Emerging therapies in Duchenne and facioscapulohumeral muscular dystrophy
“There have been so many breakthroughs recently on the side of genetically targeted treatment [for muscular dystrophy] that supports muscle better,” said John F. Brandsema, MD, a child neurologist and section head at Children’s Hospital of Philadelphia, in an interview with Neurology Reviews 2023 Rare Neurological Disease Special Report. “We’re starting to see clinical response to some things that have been in trials – after decades of banging our heads on the wall trying new therapies, only to see them fail. I think it’s about reframing Duchenne muscular dystrophy [DMD] and facioscapulohumeral muscular dystrophy [FSHD] as treatable by target therapy because previously, they were treated with supportive care.”
DMD: Current and emerging therapies
DMD is caused by a mutation in the dystrophin gene on the X chromosome that inhibits production of dystrophin, a protein that shields muscles from injury during contraction. Dystrophin deficiency prevents muscle recovery, resulting in muscle-cell death and, ultimately, loss of function due to muscle degeneration.
FDA-approved exon-skipping therapies. Treatment modalities for what has historically been an incurable, lifespan-shortening disease involved supportive care that addresses symptoms, not the underlying cause. Consequently, many patients with DMD live only into their 20s and 30s. The tide began to turn in 2016, however, when the U.S. Food and Drug Administration granted accelerated approval for eteplirsen, an exon 51–skipping treatment that was the first RNA-based therapy for DMD to target the underlying cause. Additional exon-skipping therapies followed, including casimersen, which skips exon 45, and golodirsen and viltolarsen, which skip exon 53.
AOC 1044: Novel exon-skipping. In April 2023, the FDA granted orphan-drug designation to the experimental drug antibody oligonucleotide conjugate (AOC) 1044 that skips exon 44. A small interfering RNA (siRNA), AOC 1044 works in patients who have a mutation amenable to exon 44 skipping (a disease type known as DMD44) by delivering phosphorodiamidate morpholino to skeletal muscle and heart tissue that skips exon 44. The process allows for dystrophin production, thereby preventing degradation of muscle tissue.
The orphan drug status of AOC 1044 made it available to the population of patients enrolled in the EXPLORE44 Phase 1/2 trial. However, studies demonstrating effectiveness of the drug – with the hope of, ultimately, providing widespread access to AOC 1044 – are still underway. In one of those studies, investigators expect to enroll approximately 40 healthy volunteers and 24 DMD44 patients 7-27 years of age.3 The study will evaluate the effects of exon skipping and dystrophin protein levels in participants who have DMD44.
Delandistrogene moxeparvovec. Oct. 27, 2021, marked the inception of the phase 3 Multinational, Randomized, Double-Blind, Placebo-Controlled Systemic Gene Delivery Study to Evaluate the Safety and Efficacy of SRP-9001 in Subjects With Duchenne Muscular Dystrophy (EMBARK). The trial is evaluating the safety and efficacy of the gene-therapy agent delandistrogene moxeparvovec in ambulatory boys who were 4 to less than 8 years of age at randomization. The 126 boys enrolled in the trial met the criteria of (1) a diagnosis of DMD confirmed by documented clinical findings and previous genetic testing and (2) a pathogenic frameshift mutation stop codon located between exons 18 and 79 (inclusive), except for a mutation fully contained within exon 45.
Additional inclusion criteria were (1) the ability to cooperate with motor-assessment testing and (2) receiving a steady daily dose of oral corticosteroid for 12 weeks or longer prior to screening, and (3) the expectation of maintaining the study dosage throughout screening. Boys who had previously received gene therapy, investigational medication, or any treatment that could have amplified dystrophin expression within the time limit specified by the protocol were ineligible to participate. Boys were excluded from the study if they presented with any other illness, medical condition, or need for chronic drug treatment.
Exon-skipping therapies in trials. Various biotech and pharmaceutical companies have initiated clinical trials to explore the potential of additional exon-skipping therapies for the DMD population:
ENTR-601-44 is another exon 44–skipping therapy in the pipeline.
On Aug. 22, 2023, the FDA approved delandistrogene moxeparvovec-rokl, a recombinant gene therapy utilizing an adenovirus vector. The product is indicated for ambulatory patients with DMD 4-5 years of age who have a confirmed mutation of the dystrophin gene.
Dyne Therapeutics is actively recruiting participants to investigate Dyne 251, its exon 51–skipping therapy.
Trials are in the works by BioMarin Pharmaceutical for its next-generation peptide-conjugated phosphorodiamidate morpholino oligomers (PPMO) for skipping exon 51.
Despite the prospects of such therapy, therapeutic targeting of exon 44 addresses only patients with DMD44, who account for approximately 10% of the DMD population. Disease involving the most prevalent site of a dystrophin gene mutation, exon 51, affects 13% of the DMD population. This leaves the majority of patients with DMD without gene therapy. Yet Dr. Brandsema is optimistic nevertheless.
“We were just failing over and over again with DMD treatment, but there is some hope now,” Dr. Brandsema said. “Also, FSHD is right on the cusp of having new therapies approaching.”
FSHD: Emerging therapies
The third more common type of muscular dystrophy is not a life-threatening condition. FSHD affects approximately 4 of every 100,000 people.1 An autosomal-dominant condition, FSHD is ultimately caused by inappropriate expression of the DUX4 protein product – a consequence of a complex genetic activity involving DUX4, its chromosomal locus, and the number of repeats of a microsatellite called D4Z4.4 The disease usually starts in proximal regions of the face (that is, surrounding the eyes and mouth), before spreading to muscular groups of the limbs – most prominently, muscles of the scapulae and humeri. Symptoms usually appear in these places initially, but the condition can affect any part of the body. Fifty percent of FSHD patients experience loss of high-frequency hearing and present with retinovasculopathy. Like DMD, FSHD varies in severity, with some forms presenting at birth.
AOC 1020-CS1 is an example of a new FSHD treatment under investigation. The phase 1/2 FORTITUDE trial is a randomized, double-blind, placebo-controlled study exploring the safety, tolerability, pharmacokinetics, pharmacodynamics, and potential efficacy of single- and multiple-dose AOC 1020-CS1 therapy in FSHD.5 The trial began in April 2023; estimated completion date is September 2025.
As with many rare diseases, however, following patients and capturing data that fully narrate their story remains challenging in both DMD and FSHD. Although clinical trials undoubtedly offer hope of expanding treatment options and additional insights into disease-state management, the often insidious, complex nature of some rare diseases, such as DMD and FSHD, presents some limitations.
“Patients are hard to measure,” Dr. Brandsema explained, “because they’re so variable at baseline in history and progress in a different [slower] way than timelines are set up in our system to study drugs.”
Neonatal screening and early diagnosis: Imperative for improving outcomes
Neonatal screening helps with early detection and treatment. Prompt diagnosis does not necessarily prolong a DMD patient’s life, but it can enhance their quality of life.
DNA diagnostics. A critical component of the path to treatment is DNA diagnostics. According to Barry J. Byrne, MD, PhD, chief medical advisor of the Muscular Dystrophy Association, the Human Genome Project conducted by the National Institutes of Health helped make DNA tests affordable; such tests run about $800 today. However, given continuous advancements in sequencing, Dr. Byrne said that whole-exome sequencing for $100 is within reach.
In terms of accessibility, some nations – Canada is an example – include testing as part of national health care services. In the United States, coverage for testing varies by health insurance plan. In addition, some plans have favored rapid diagnostic testing, and the overall cost is often individualized to the patient.
Early diagnosis and supportive care. Early diagnosis can certainly help improve DMD patients’ quality of life; supportive care provides some benefit. Dr. Byrne stressed the importance of managing extraskeletal clinical manifestations in this patient population. A critical area is initiating cardiovascular treatment immediately following diagnosis, even if the patient does not exhibit cardiovascular symptoms.
“Cardiac manifestations are actually the cause of mortality in DMD, and most boys with DMD should begin cardiovascular treatment shortly after diagnosis,” Dr. Byrne told Neurology Reviews 2023 Rare Neurological Disease Special Report. “The message to neurologists is that these patients can benefit from early cardiovascular treatment because we can prevent the complications of DMD-related heart failure until much later in life.”
Historically, clinicians used echocardiography as the mainstay tool to assess cardiovascular function; however, more and more clinicians are turning to magnetic resonance imaging for such investigation. Dr. Byrne, a cardiologist, explained that magnetic resonance imaging identifies cardiovascular dysfunction at earlier stages than echocardiography can. In addition, although DMD patients frequently experience fatigue, Dr. Byrne cautions neurologists that fatigue is usually related to muscle weakness, not necessarily heart failure.
DMD therapies carry a hefty price
Right now, the projected price range of AOC 1044 is $3.2 million to $3.4 million. Akin to the case with onasemnogene abeparvovec-xioi (Zolgensma) for spinal muscular atrophy, the world’s first gene therapy and first seven-figure drug, the manufacturer of AOC 1044 based pricing on the anticipated cost of treating a DMD44 patient throughout the lifespan, according to Dr. Byrne.
Delandistrogene moxeparvovec might come with an even higher price tag. A cost-effectiveness analysis study priced the therapy at $5 million. In a presentation to investors, the manufacturer projected the price in the range of $5 million to $13 million.6,7
‘It takes a village’: Comprehensive care requires a multidisciplinary team
Dr. Brandsema and Dr. Byrne agree: Optimizing outcomes requires ongoing coordinated and collaborative efforts of an interdisciplinary team of health care providers for the duration of DMD and FSHD patients’ lifespan.
A neurologist by training, Dr. Brandsema recognizes the importance of interdisciplinary collaboration in caring for patients with DMD, given the multiorgan manifestations of the disease.
“We have some hope with DMD, and FSHD is right on the cusp of having new therapies approaching ... It is important to recognize that interdisciplinary follow-up and optimized standard of care are important after dosing.”
“I think many patients living with neurological disorders have multiple providers they rely on for care,” Dr. Byrne said, “but cardiovascular and pulmonary care are important because both are affected in the case of DMD – not so much in FSHD.”
Ultimately, advancements in therapy and care give patients living with these disorders, and their caregivers, a renewed sense of hope – hope that their life will be improved by breakthrough therapies that have been approved or will arrive soon.
Dr. Brandsema discloses he is a consultant for Alexion, Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech/Roche, Janssen, Marathon, Momenta, NS Pharma, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is a speaker for AveXis and Biogen, a medical advisory council member for Cure SMA, and a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Catabasis, CSL Behring, Cytokinetics, Fibrogen, Genentech/Roche, Ionis, Lilly, Janssen, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Dr. Byrne has no relevant financial disclosures.
References
1. Centers for Disease Control and Prevention. What is muscular dystrophy? Updated Nov. 21, 2022. Accessed Sept. 3, 2023. https://www.cdc.gov/ncbddd/musculardystrophy/facts.html.
2. FDA approves first gene therapy for treatment of certain patients with Duchenne muscular dystrophy. U.S. Food and Drug Administration. Press release. June 22, 2023. Accessed Sept. 3, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapy-treatment-certain-patients-duchenne-muscular-dystrophy.
3. Study of AOC 1044 in healthy adult volunteers and participants with Duchenne muscular dystrophy (DMD) mutations amenable to exon 44 skipping (EXPLORE44). ClinicalTrials.gov Identifier: NCT05670730. Updated April 4, 2023. Accessed Sep. 3, 2023. https://www.clinicaltrials.gov/study/NCT05670730?cond=DMD&intr=AOC%201044&rank=1.
4. Statland JM, Tawil R. Facioscapulohumeral muscular dystrophy. Continuum (Minneap. Minn). 2016;22(6, Muscle and Neuromuscular Junction Disorders):1916-31. doi: 10.1212/CON.0000000000000399.
5. Phase 1/2 study of AOC 1020 in adults with facioscapulohumeral muscular dystrophy (FSHD) (FORTITUDE). ClinicalTrials.gov Identifier: NCT05747924. Updated Aug. 9, 2023. Accessed Sept. 3, 2023. https://clinicaltrials.gov/study/NCT05747924?term=fORTITUDE&cond=Facioscapulohumeral%20Muscular%20Dystrophy&rank=1.
6. Klimchak AC, Sedita LE, Rodino-Klapac LR, et al. Assessing the value of delandistrogene moxeparvovec (SRP-9001) gene therapy in patients with Duchenne muscular dystrophy in the United States. J Mark Access Health Policy. 2023;11(1):2216518. doi: 10.1080/20016689.2023.2216518.
7. Ingram D. [Investor relations presentation.] Sarepta Therapeutics website. June 22, 2023. Accessed Sept. 3, 2023. https://investorrelations.sarepta.com/static-files/7216948c-f688-4024-922e-39761bc7a984.
“There have been so many breakthroughs recently on the side of genetically targeted treatment [for muscular dystrophy] that supports muscle better,” said John F. Brandsema, MD, a child neurologist and section head at Children’s Hospital of Philadelphia, in an interview with Neurology Reviews 2023 Rare Neurological Disease Special Report. “We’re starting to see clinical response to some things that have been in trials – after decades of banging our heads on the wall trying new therapies, only to see them fail. I think it’s about reframing Duchenne muscular dystrophy [DMD] and facioscapulohumeral muscular dystrophy [FSHD] as treatable by target therapy because previously, they were treated with supportive care.”
DMD: Current and emerging therapies
DMD is caused by a mutation in the dystrophin gene on the X chromosome that inhibits production of dystrophin, a protein that shields muscles from injury during contraction. Dystrophin deficiency prevents muscle recovery, resulting in muscle-cell death and, ultimately, loss of function due to muscle degeneration.
FDA-approved exon-skipping therapies. Treatment modalities for what has historically been an incurable, lifespan-shortening disease involved supportive care that addresses symptoms, not the underlying cause. Consequently, many patients with DMD live only into their 20s and 30s. The tide began to turn in 2016, however, when the U.S. Food and Drug Administration granted accelerated approval for eteplirsen, an exon 51–skipping treatment that was the first RNA-based therapy for DMD to target the underlying cause. Additional exon-skipping therapies followed, including casimersen, which skips exon 45, and golodirsen and viltolarsen, which skip exon 53.
AOC 1044: Novel exon-skipping. In April 2023, the FDA granted orphan-drug designation to the experimental drug antibody oligonucleotide conjugate (AOC) 1044 that skips exon 44. A small interfering RNA (siRNA), AOC 1044 works in patients who have a mutation amenable to exon 44 skipping (a disease type known as DMD44) by delivering phosphorodiamidate morpholino to skeletal muscle and heart tissue that skips exon 44. The process allows for dystrophin production, thereby preventing degradation of muscle tissue.
The orphan drug status of AOC 1044 made it available to the population of patients enrolled in the EXPLORE44 Phase 1/2 trial. However, studies demonstrating effectiveness of the drug – with the hope of, ultimately, providing widespread access to AOC 1044 – are still underway. In one of those studies, investigators expect to enroll approximately 40 healthy volunteers and 24 DMD44 patients 7-27 years of age.3 The study will evaluate the effects of exon skipping and dystrophin protein levels in participants who have DMD44.
Delandistrogene moxeparvovec. Oct. 27, 2021, marked the inception of the phase 3 Multinational, Randomized, Double-Blind, Placebo-Controlled Systemic Gene Delivery Study to Evaluate the Safety and Efficacy of SRP-9001 in Subjects With Duchenne Muscular Dystrophy (EMBARK). The trial is evaluating the safety and efficacy of the gene-therapy agent delandistrogene moxeparvovec in ambulatory boys who were 4 to less than 8 years of age at randomization. The 126 boys enrolled in the trial met the criteria of (1) a diagnosis of DMD confirmed by documented clinical findings and previous genetic testing and (2) a pathogenic frameshift mutation stop codon located between exons 18 and 79 (inclusive), except for a mutation fully contained within exon 45.
Additional inclusion criteria were (1) the ability to cooperate with motor-assessment testing and (2) receiving a steady daily dose of oral corticosteroid for 12 weeks or longer prior to screening, and (3) the expectation of maintaining the study dosage throughout screening. Boys who had previously received gene therapy, investigational medication, or any treatment that could have amplified dystrophin expression within the time limit specified by the protocol were ineligible to participate. Boys were excluded from the study if they presented with any other illness, medical condition, or need for chronic drug treatment.
Exon-skipping therapies in trials. Various biotech and pharmaceutical companies have initiated clinical trials to explore the potential of additional exon-skipping therapies for the DMD population:
ENTR-601-44 is another exon 44–skipping therapy in the pipeline.
On Aug. 22, 2023, the FDA approved delandistrogene moxeparvovec-rokl, a recombinant gene therapy utilizing an adenovirus vector. The product is indicated for ambulatory patients with DMD 4-5 years of age who have a confirmed mutation of the dystrophin gene.
Dyne Therapeutics is actively recruiting participants to investigate Dyne 251, its exon 51–skipping therapy.
Trials are in the works by BioMarin Pharmaceutical for its next-generation peptide-conjugated phosphorodiamidate morpholino oligomers (PPMO) for skipping exon 51.
Despite the prospects of such therapy, therapeutic targeting of exon 44 addresses only patients with DMD44, who account for approximately 10% of the DMD population. Disease involving the most prevalent site of a dystrophin gene mutation, exon 51, affects 13% of the DMD population. This leaves the majority of patients with DMD without gene therapy. Yet Dr. Brandsema is optimistic nevertheless.
“We were just failing over and over again with DMD treatment, but there is some hope now,” Dr. Brandsema said. “Also, FSHD is right on the cusp of having new therapies approaching.”
FSHD: Emerging therapies
The third more common type of muscular dystrophy is not a life-threatening condition. FSHD affects approximately 4 of every 100,000 people.1 An autosomal-dominant condition, FSHD is ultimately caused by inappropriate expression of the DUX4 protein product – a consequence of a complex genetic activity involving DUX4, its chromosomal locus, and the number of repeats of a microsatellite called D4Z4.4 The disease usually starts in proximal regions of the face (that is, surrounding the eyes and mouth), before spreading to muscular groups of the limbs – most prominently, muscles of the scapulae and humeri. Symptoms usually appear in these places initially, but the condition can affect any part of the body. Fifty percent of FSHD patients experience loss of high-frequency hearing and present with retinovasculopathy. Like DMD, FSHD varies in severity, with some forms presenting at birth.
AOC 1020-CS1 is an example of a new FSHD treatment under investigation. The phase 1/2 FORTITUDE trial is a randomized, double-blind, placebo-controlled study exploring the safety, tolerability, pharmacokinetics, pharmacodynamics, and potential efficacy of single- and multiple-dose AOC 1020-CS1 therapy in FSHD.5 The trial began in April 2023; estimated completion date is September 2025.
As with many rare diseases, however, following patients and capturing data that fully narrate their story remains challenging in both DMD and FSHD. Although clinical trials undoubtedly offer hope of expanding treatment options and additional insights into disease-state management, the often insidious, complex nature of some rare diseases, such as DMD and FSHD, presents some limitations.
“Patients are hard to measure,” Dr. Brandsema explained, “because they’re so variable at baseline in history and progress in a different [slower] way than timelines are set up in our system to study drugs.”
Neonatal screening and early diagnosis: Imperative for improving outcomes
Neonatal screening helps with early detection and treatment. Prompt diagnosis does not necessarily prolong a DMD patient’s life, but it can enhance their quality of life.
DNA diagnostics. A critical component of the path to treatment is DNA diagnostics. According to Barry J. Byrne, MD, PhD, chief medical advisor of the Muscular Dystrophy Association, the Human Genome Project conducted by the National Institutes of Health helped make DNA tests affordable; such tests run about $800 today. However, given continuous advancements in sequencing, Dr. Byrne said that whole-exome sequencing for $100 is within reach.
In terms of accessibility, some nations – Canada is an example – include testing as part of national health care services. In the United States, coverage for testing varies by health insurance plan. In addition, some plans have favored rapid diagnostic testing, and the overall cost is often individualized to the patient.
Early diagnosis and supportive care. Early diagnosis can certainly help improve DMD patients’ quality of life; supportive care provides some benefit. Dr. Byrne stressed the importance of managing extraskeletal clinical manifestations in this patient population. A critical area is initiating cardiovascular treatment immediately following diagnosis, even if the patient does not exhibit cardiovascular symptoms.
“Cardiac manifestations are actually the cause of mortality in DMD, and most boys with DMD should begin cardiovascular treatment shortly after diagnosis,” Dr. Byrne told Neurology Reviews 2023 Rare Neurological Disease Special Report. “The message to neurologists is that these patients can benefit from early cardiovascular treatment because we can prevent the complications of DMD-related heart failure until much later in life.”
Historically, clinicians used echocardiography as the mainstay tool to assess cardiovascular function; however, more and more clinicians are turning to magnetic resonance imaging for such investigation. Dr. Byrne, a cardiologist, explained that magnetic resonance imaging identifies cardiovascular dysfunction at earlier stages than echocardiography can. In addition, although DMD patients frequently experience fatigue, Dr. Byrne cautions neurologists that fatigue is usually related to muscle weakness, not necessarily heart failure.
DMD therapies carry a hefty price
Right now, the projected price range of AOC 1044 is $3.2 million to $3.4 million. Akin to the case with onasemnogene abeparvovec-xioi (Zolgensma) for spinal muscular atrophy, the world’s first gene therapy and first seven-figure drug, the manufacturer of AOC 1044 based pricing on the anticipated cost of treating a DMD44 patient throughout the lifespan, according to Dr. Byrne.
Delandistrogene moxeparvovec might come with an even higher price tag. A cost-effectiveness analysis study priced the therapy at $5 million. In a presentation to investors, the manufacturer projected the price in the range of $5 million to $13 million.6,7
‘It takes a village’: Comprehensive care requires a multidisciplinary team
Dr. Brandsema and Dr. Byrne agree: Optimizing outcomes requires ongoing coordinated and collaborative efforts of an interdisciplinary team of health care providers for the duration of DMD and FSHD patients’ lifespan.
A neurologist by training, Dr. Brandsema recognizes the importance of interdisciplinary collaboration in caring for patients with DMD, given the multiorgan manifestations of the disease.
“We have some hope with DMD, and FSHD is right on the cusp of having new therapies approaching ... It is important to recognize that interdisciplinary follow-up and optimized standard of care are important after dosing.”
“I think many patients living with neurological disorders have multiple providers they rely on for care,” Dr. Byrne said, “but cardiovascular and pulmonary care are important because both are affected in the case of DMD – not so much in FSHD.”
Ultimately, advancements in therapy and care give patients living with these disorders, and their caregivers, a renewed sense of hope – hope that their life will be improved by breakthrough therapies that have been approved or will arrive soon.
Dr. Brandsema discloses he is a consultant for Alexion, Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech/Roche, Janssen, Marathon, Momenta, NS Pharma, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is a speaker for AveXis and Biogen, a medical advisory council member for Cure SMA, and a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Catabasis, CSL Behring, Cytokinetics, Fibrogen, Genentech/Roche, Ionis, Lilly, Janssen, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Dr. Byrne has no relevant financial disclosures.
References
1. Centers for Disease Control and Prevention. What is muscular dystrophy? Updated Nov. 21, 2022. Accessed Sept. 3, 2023. https://www.cdc.gov/ncbddd/musculardystrophy/facts.html.
2. FDA approves first gene therapy for treatment of certain patients with Duchenne muscular dystrophy. U.S. Food and Drug Administration. Press release. June 22, 2023. Accessed Sept. 3, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapy-treatment-certain-patients-duchenne-muscular-dystrophy.
3. Study of AOC 1044 in healthy adult volunteers and participants with Duchenne muscular dystrophy (DMD) mutations amenable to exon 44 skipping (EXPLORE44). ClinicalTrials.gov Identifier: NCT05670730. Updated April 4, 2023. Accessed Sep. 3, 2023. https://www.clinicaltrials.gov/study/NCT05670730?cond=DMD&intr=AOC%201044&rank=1.
4. Statland JM, Tawil R. Facioscapulohumeral muscular dystrophy. Continuum (Minneap. Minn). 2016;22(6, Muscle and Neuromuscular Junction Disorders):1916-31. doi: 10.1212/CON.0000000000000399.
5. Phase 1/2 study of AOC 1020 in adults with facioscapulohumeral muscular dystrophy (FSHD) (FORTITUDE). ClinicalTrials.gov Identifier: NCT05747924. Updated Aug. 9, 2023. Accessed Sept. 3, 2023. https://clinicaltrials.gov/study/NCT05747924?term=fORTITUDE&cond=Facioscapulohumeral%20Muscular%20Dystrophy&rank=1.
6. Klimchak AC, Sedita LE, Rodino-Klapac LR, et al. Assessing the value of delandistrogene moxeparvovec (SRP-9001) gene therapy in patients with Duchenne muscular dystrophy in the United States. J Mark Access Health Policy. 2023;11(1):2216518. doi: 10.1080/20016689.2023.2216518.
7. Ingram D. [Investor relations presentation.] Sarepta Therapeutics website. June 22, 2023. Accessed Sept. 3, 2023. https://investorrelations.sarepta.com/static-files/7216948c-f688-4024-922e-39761bc7a984.
“There have been so many breakthroughs recently on the side of genetically targeted treatment [for muscular dystrophy] that supports muscle better,” said John F. Brandsema, MD, a child neurologist and section head at Children’s Hospital of Philadelphia, in an interview with Neurology Reviews 2023 Rare Neurological Disease Special Report. “We’re starting to see clinical response to some things that have been in trials – after decades of banging our heads on the wall trying new therapies, only to see them fail. I think it’s about reframing Duchenne muscular dystrophy [DMD] and facioscapulohumeral muscular dystrophy [FSHD] as treatable by target therapy because previously, they were treated with supportive care.”
DMD: Current and emerging therapies
DMD is caused by a mutation in the dystrophin gene on the X chromosome that inhibits production of dystrophin, a protein that shields muscles from injury during contraction. Dystrophin deficiency prevents muscle recovery, resulting in muscle-cell death and, ultimately, loss of function due to muscle degeneration.
FDA-approved exon-skipping therapies. Treatment modalities for what has historically been an incurable, lifespan-shortening disease involved supportive care that addresses symptoms, not the underlying cause. Consequently, many patients with DMD live only into their 20s and 30s. The tide began to turn in 2016, however, when the U.S. Food and Drug Administration granted accelerated approval for eteplirsen, an exon 51–skipping treatment that was the first RNA-based therapy for DMD to target the underlying cause. Additional exon-skipping therapies followed, including casimersen, which skips exon 45, and golodirsen and viltolarsen, which skip exon 53.
AOC 1044: Novel exon-skipping. In April 2023, the FDA granted orphan-drug designation to the experimental drug antibody oligonucleotide conjugate (AOC) 1044 that skips exon 44. A small interfering RNA (siRNA), AOC 1044 works in patients who have a mutation amenable to exon 44 skipping (a disease type known as DMD44) by delivering phosphorodiamidate morpholino to skeletal muscle and heart tissue that skips exon 44. The process allows for dystrophin production, thereby preventing degradation of muscle tissue.
The orphan drug status of AOC 1044 made it available to the population of patients enrolled in the EXPLORE44 Phase 1/2 trial. However, studies demonstrating effectiveness of the drug – with the hope of, ultimately, providing widespread access to AOC 1044 – are still underway. In one of those studies, investigators expect to enroll approximately 40 healthy volunteers and 24 DMD44 patients 7-27 years of age.3 The study will evaluate the effects of exon skipping and dystrophin protein levels in participants who have DMD44.
Delandistrogene moxeparvovec. Oct. 27, 2021, marked the inception of the phase 3 Multinational, Randomized, Double-Blind, Placebo-Controlled Systemic Gene Delivery Study to Evaluate the Safety and Efficacy of SRP-9001 in Subjects With Duchenne Muscular Dystrophy (EMBARK). The trial is evaluating the safety and efficacy of the gene-therapy agent delandistrogene moxeparvovec in ambulatory boys who were 4 to less than 8 years of age at randomization. The 126 boys enrolled in the trial met the criteria of (1) a diagnosis of DMD confirmed by documented clinical findings and previous genetic testing and (2) a pathogenic frameshift mutation stop codon located between exons 18 and 79 (inclusive), except for a mutation fully contained within exon 45.
Additional inclusion criteria were (1) the ability to cooperate with motor-assessment testing and (2) receiving a steady daily dose of oral corticosteroid for 12 weeks or longer prior to screening, and (3) the expectation of maintaining the study dosage throughout screening. Boys who had previously received gene therapy, investigational medication, or any treatment that could have amplified dystrophin expression within the time limit specified by the protocol were ineligible to participate. Boys were excluded from the study if they presented with any other illness, medical condition, or need for chronic drug treatment.
Exon-skipping therapies in trials. Various biotech and pharmaceutical companies have initiated clinical trials to explore the potential of additional exon-skipping therapies for the DMD population:
ENTR-601-44 is another exon 44–skipping therapy in the pipeline.
On Aug. 22, 2023, the FDA approved delandistrogene moxeparvovec-rokl, a recombinant gene therapy utilizing an adenovirus vector. The product is indicated for ambulatory patients with DMD 4-5 years of age who have a confirmed mutation of the dystrophin gene.
Dyne Therapeutics is actively recruiting participants to investigate Dyne 251, its exon 51–skipping therapy.
Trials are in the works by BioMarin Pharmaceutical for its next-generation peptide-conjugated phosphorodiamidate morpholino oligomers (PPMO) for skipping exon 51.
Despite the prospects of such therapy, therapeutic targeting of exon 44 addresses only patients with DMD44, who account for approximately 10% of the DMD population. Disease involving the most prevalent site of a dystrophin gene mutation, exon 51, affects 13% of the DMD population. This leaves the majority of patients with DMD without gene therapy. Yet Dr. Brandsema is optimistic nevertheless.
“We were just failing over and over again with DMD treatment, but there is some hope now,” Dr. Brandsema said. “Also, FSHD is right on the cusp of having new therapies approaching.”
FSHD: Emerging therapies
The third more common type of muscular dystrophy is not a life-threatening condition. FSHD affects approximately 4 of every 100,000 people.1 An autosomal-dominant condition, FSHD is ultimately caused by inappropriate expression of the DUX4 protein product – a consequence of a complex genetic activity involving DUX4, its chromosomal locus, and the number of repeats of a microsatellite called D4Z4.4 The disease usually starts in proximal regions of the face (that is, surrounding the eyes and mouth), before spreading to muscular groups of the limbs – most prominently, muscles of the scapulae and humeri. Symptoms usually appear in these places initially, but the condition can affect any part of the body. Fifty percent of FSHD patients experience loss of high-frequency hearing and present with retinovasculopathy. Like DMD, FSHD varies in severity, with some forms presenting at birth.
AOC 1020-CS1 is an example of a new FSHD treatment under investigation. The phase 1/2 FORTITUDE trial is a randomized, double-blind, placebo-controlled study exploring the safety, tolerability, pharmacokinetics, pharmacodynamics, and potential efficacy of single- and multiple-dose AOC 1020-CS1 therapy in FSHD.5 The trial began in April 2023; estimated completion date is September 2025.
As with many rare diseases, however, following patients and capturing data that fully narrate their story remains challenging in both DMD and FSHD. Although clinical trials undoubtedly offer hope of expanding treatment options and additional insights into disease-state management, the often insidious, complex nature of some rare diseases, such as DMD and FSHD, presents some limitations.
“Patients are hard to measure,” Dr. Brandsema explained, “because they’re so variable at baseline in history and progress in a different [slower] way than timelines are set up in our system to study drugs.”
Neonatal screening and early diagnosis: Imperative for improving outcomes
Neonatal screening helps with early detection and treatment. Prompt diagnosis does not necessarily prolong a DMD patient’s life, but it can enhance their quality of life.
DNA diagnostics. A critical component of the path to treatment is DNA diagnostics. According to Barry J. Byrne, MD, PhD, chief medical advisor of the Muscular Dystrophy Association, the Human Genome Project conducted by the National Institutes of Health helped make DNA tests affordable; such tests run about $800 today. However, given continuous advancements in sequencing, Dr. Byrne said that whole-exome sequencing for $100 is within reach.
In terms of accessibility, some nations – Canada is an example – include testing as part of national health care services. In the United States, coverage for testing varies by health insurance plan. In addition, some plans have favored rapid diagnostic testing, and the overall cost is often individualized to the patient.
Early diagnosis and supportive care. Early diagnosis can certainly help improve DMD patients’ quality of life; supportive care provides some benefit. Dr. Byrne stressed the importance of managing extraskeletal clinical manifestations in this patient population. A critical area is initiating cardiovascular treatment immediately following diagnosis, even if the patient does not exhibit cardiovascular symptoms.
“Cardiac manifestations are actually the cause of mortality in DMD, and most boys with DMD should begin cardiovascular treatment shortly after diagnosis,” Dr. Byrne told Neurology Reviews 2023 Rare Neurological Disease Special Report. “The message to neurologists is that these patients can benefit from early cardiovascular treatment because we can prevent the complications of DMD-related heart failure until much later in life.”
Historically, clinicians used echocardiography as the mainstay tool to assess cardiovascular function; however, more and more clinicians are turning to magnetic resonance imaging for such investigation. Dr. Byrne, a cardiologist, explained that magnetic resonance imaging identifies cardiovascular dysfunction at earlier stages than echocardiography can. In addition, although DMD patients frequently experience fatigue, Dr. Byrne cautions neurologists that fatigue is usually related to muscle weakness, not necessarily heart failure.
DMD therapies carry a hefty price
Right now, the projected price range of AOC 1044 is $3.2 million to $3.4 million. Akin to the case with onasemnogene abeparvovec-xioi (Zolgensma) for spinal muscular atrophy, the world’s first gene therapy and first seven-figure drug, the manufacturer of AOC 1044 based pricing on the anticipated cost of treating a DMD44 patient throughout the lifespan, according to Dr. Byrne.
Delandistrogene moxeparvovec might come with an even higher price tag. A cost-effectiveness analysis study priced the therapy at $5 million. In a presentation to investors, the manufacturer projected the price in the range of $5 million to $13 million.6,7
‘It takes a village’: Comprehensive care requires a multidisciplinary team
Dr. Brandsema and Dr. Byrne agree: Optimizing outcomes requires ongoing coordinated and collaborative efforts of an interdisciplinary team of health care providers for the duration of DMD and FSHD patients’ lifespan.
A neurologist by training, Dr. Brandsema recognizes the importance of interdisciplinary collaboration in caring for patients with DMD, given the multiorgan manifestations of the disease.
“We have some hope with DMD, and FSHD is right on the cusp of having new therapies approaching ... It is important to recognize that interdisciplinary follow-up and optimized standard of care are important after dosing.”
“I think many patients living with neurological disorders have multiple providers they rely on for care,” Dr. Byrne said, “but cardiovascular and pulmonary care are important because both are affected in the case of DMD – not so much in FSHD.”
Ultimately, advancements in therapy and care give patients living with these disorders, and their caregivers, a renewed sense of hope – hope that their life will be improved by breakthrough therapies that have been approved or will arrive soon.
Dr. Brandsema discloses he is a consultant for Alexion, Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech/Roche, Janssen, Marathon, Momenta, NS Pharma, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is a speaker for AveXis and Biogen, a medical advisory council member for Cure SMA, and a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Catabasis, CSL Behring, Cytokinetics, Fibrogen, Genentech/Roche, Ionis, Lilly, Janssen, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Dr. Byrne has no relevant financial disclosures.
References
1. Centers for Disease Control and Prevention. What is muscular dystrophy? Updated Nov. 21, 2022. Accessed Sept. 3, 2023. https://www.cdc.gov/ncbddd/musculardystrophy/facts.html.
2. FDA approves first gene therapy for treatment of certain patients with Duchenne muscular dystrophy. U.S. Food and Drug Administration. Press release. June 22, 2023. Accessed Sept. 3, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapy-treatment-certain-patients-duchenne-muscular-dystrophy.
3. Study of AOC 1044 in healthy adult volunteers and participants with Duchenne muscular dystrophy (DMD) mutations amenable to exon 44 skipping (EXPLORE44). ClinicalTrials.gov Identifier: NCT05670730. Updated April 4, 2023. Accessed Sep. 3, 2023. https://www.clinicaltrials.gov/study/NCT05670730?cond=DMD&intr=AOC%201044&rank=1.
4. Statland JM, Tawil R. Facioscapulohumeral muscular dystrophy. Continuum (Minneap. Minn). 2016;22(6, Muscle and Neuromuscular Junction Disorders):1916-31. doi: 10.1212/CON.0000000000000399.
5. Phase 1/2 study of AOC 1020 in adults with facioscapulohumeral muscular dystrophy (FSHD) (FORTITUDE). ClinicalTrials.gov Identifier: NCT05747924. Updated Aug. 9, 2023. Accessed Sept. 3, 2023. https://clinicaltrials.gov/study/NCT05747924?term=fORTITUDE&cond=Facioscapulohumeral%20Muscular%20Dystrophy&rank=1.
6. Klimchak AC, Sedita LE, Rodino-Klapac LR, et al. Assessing the value of delandistrogene moxeparvovec (SRP-9001) gene therapy in patients with Duchenne muscular dystrophy in the United States. J Mark Access Health Policy. 2023;11(1):2216518. doi: 10.1080/20016689.2023.2216518.
7. Ingram D. [Investor relations presentation.] Sarepta Therapeutics website. June 22, 2023. Accessed Sept. 3, 2023. https://investorrelations.sarepta.com/static-files/7216948c-f688-4024-922e-39761bc7a984.
3-D stereophotogrammetry helps detect progression of craniofacial morphea
TOPLINE:
over time.
METHODOLOGY:
- Existing tools that detect disease progression in patients with CM are limited.
- In a prospective cohort study, researchers evaluated the use of 3-D stereophotogrammetry, a noninvasive, radiation-free imaging modality, to detect disease progression in 27 consecutive patients with CM seen at Boston Children’s Hospital and Brigham and Women’s Hospital from April 1, 2019, to March 1, 2023.
- After clinical and 3-D stereophotogrammetry assessments were performed at 2- to 12-month intervals, the 3-D images were rated by an expert (a board-certified plastic craniofacial surgeon) and a nonexpert (a board-certified dermatologist) as demonstrating progression or no progression.
- Kappa coefficients were used to calculate inter-rater reliability.
TAKEAWAY:
- Most of the study participants (73%) were female, their median age was 14 years (range, 5-40 years), and each underwent 3-D stereophotogrammetry imaging at least two times spaced a median of 3 months apart.
- On the basis of clinical assessments during the 48-month study period, 10 patients (37%) experienced progression of their disease.
- 3-D stereophotogrammetry not only corroborated clinical impressions of disease progression with strong inter-rater reliability (kappa = 0.80; 95% confidence interval, 0.61-0.99), but it also detected occult progression of asymmetry not noted on clinical examination in three additional patients.
- In subgroup analyses, assessment of 3-D images demonstrated substantial to near-perfect inter-rater reliability in patients with Fitzpatrick skin types IV-VI.
IN PRACTICE:
“Further work is necessary to validate this measure in a larger cohort and to guide its incorporation into medical decision-making for patients with CM,” the researchers wrote.
SOURCE:
Katharina S. Shaw, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
The sample was small, and a criterion standard for assessing CM was lacking.
DISCLOSURES:
The researchers reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
over time.
METHODOLOGY:
- Existing tools that detect disease progression in patients with CM are limited.
- In a prospective cohort study, researchers evaluated the use of 3-D stereophotogrammetry, a noninvasive, radiation-free imaging modality, to detect disease progression in 27 consecutive patients with CM seen at Boston Children’s Hospital and Brigham and Women’s Hospital from April 1, 2019, to March 1, 2023.
- After clinical and 3-D stereophotogrammetry assessments were performed at 2- to 12-month intervals, the 3-D images were rated by an expert (a board-certified plastic craniofacial surgeon) and a nonexpert (a board-certified dermatologist) as demonstrating progression or no progression.
- Kappa coefficients were used to calculate inter-rater reliability.
TAKEAWAY:
- Most of the study participants (73%) were female, their median age was 14 years (range, 5-40 years), and each underwent 3-D stereophotogrammetry imaging at least two times spaced a median of 3 months apart.
- On the basis of clinical assessments during the 48-month study period, 10 patients (37%) experienced progression of their disease.
- 3-D stereophotogrammetry not only corroborated clinical impressions of disease progression with strong inter-rater reliability (kappa = 0.80; 95% confidence interval, 0.61-0.99), but it also detected occult progression of asymmetry not noted on clinical examination in three additional patients.
- In subgroup analyses, assessment of 3-D images demonstrated substantial to near-perfect inter-rater reliability in patients with Fitzpatrick skin types IV-VI.
IN PRACTICE:
“Further work is necessary to validate this measure in a larger cohort and to guide its incorporation into medical decision-making for patients with CM,” the researchers wrote.
SOURCE:
Katharina S. Shaw, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
The sample was small, and a criterion standard for assessing CM was lacking.
DISCLOSURES:
The researchers reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
over time.
METHODOLOGY:
- Existing tools that detect disease progression in patients with CM are limited.
- In a prospective cohort study, researchers evaluated the use of 3-D stereophotogrammetry, a noninvasive, radiation-free imaging modality, to detect disease progression in 27 consecutive patients with CM seen at Boston Children’s Hospital and Brigham and Women’s Hospital from April 1, 2019, to March 1, 2023.
- After clinical and 3-D stereophotogrammetry assessments were performed at 2- to 12-month intervals, the 3-D images were rated by an expert (a board-certified plastic craniofacial surgeon) and a nonexpert (a board-certified dermatologist) as demonstrating progression or no progression.
- Kappa coefficients were used to calculate inter-rater reliability.
TAKEAWAY:
- Most of the study participants (73%) were female, their median age was 14 years (range, 5-40 years), and each underwent 3-D stereophotogrammetry imaging at least two times spaced a median of 3 months apart.
- On the basis of clinical assessments during the 48-month study period, 10 patients (37%) experienced progression of their disease.
- 3-D stereophotogrammetry not only corroborated clinical impressions of disease progression with strong inter-rater reliability (kappa = 0.80; 95% confidence interval, 0.61-0.99), but it also detected occult progression of asymmetry not noted on clinical examination in three additional patients.
- In subgroup analyses, assessment of 3-D images demonstrated substantial to near-perfect inter-rater reliability in patients with Fitzpatrick skin types IV-VI.
IN PRACTICE:
“Further work is necessary to validate this measure in a larger cohort and to guide its incorporation into medical decision-making for patients with CM,” the researchers wrote.
SOURCE:
Katharina S. Shaw, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
The sample was small, and a criterion standard for assessing CM was lacking.
DISCLOSURES:
The researchers reported having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Anti-acid meds lower strength of systemic sclerosis drug
TOPLINE:
Anti-acid drugs used by patients with systemic sclerosis reduce the bioavailability of mycophenolate mofetil (MMF).
METHODOLOGY:
- Researchers conducted an open-label, pragmatic crossover study of 20 patients (all female) with systemic sclerosis at a single center who were on a stable MMF dose (1.5-2 g/day) for the last 3 months or more.
- Participants sequentially took MMF alone for 1 month, then with the H2 receptor blocker (HRB) ranitidine 300 mg/day in the second month, then with the proton pump inhibitor (PPI) esomeprazole 40 mg/day in the third month.
- Researchers measured the bioavailability of MMF in the patients during treatment with ranitidine or esomeprazole and the impact of the drugs on the total GI score of the UCLA Scleroderma Clinical Trial Consortium Gastrointestinal Tract 2.0 instrument.
- Patients were excluded if they were receiving co-prescription of cholestyramine, magnesium- or aluminum-containing antacids, and rifampicin; taking prednisolone-equivalent dose > 5 mg/day; taking MMF plus a PPI or an HRB at baseline; living with chronic kidney disease with a glomerular filtration rate < 30 mL/min; positive for HIV, HCV, or HBV; or living with end-stage lung disease or gastroduodenal ulcers.
TAKEAWAY:
- Mean estimated 12-hour area under curve levels of mycophenolic acid dropped by 32.7% (mean difference = 22.28 mcg h mL–1) when patients added esomeprazole, and they dipped by 21.97% (mean difference = 14.93 mcg h mL–1) when they added ranitidine vs. MMF alone.
- The pharmacokinetic parameter T-max did not differ significantly between MMF alone vs. MMF plus ranitidine but was significantly different with esomeprazole. C-max significantly declined with administration of ranitidine or esomeprazole vs. MMF alone.
- Total GI scores dipped when patients added esomeprazole or ranitidine.
IN PRACTICE:
In patients with significant gastroesophageal reflux disease symptoms who need to take MMF, management options may include monitoring MMF drug levels, switching to enteric-coated mycophenolate sodium, and spacing doses with anti-acid drugs.
SOURCE:
Glaxon Alex, MD, and colleagues from the Center for Arthritis and Rheumatism Excellence in Kochi, India, conducted the study, which was published online in Seminars in Arthritis & Rheumatism.
LIMITATIONS:
The sample size is small, and the optimum dose of MMF is unknown.
DISCLOSURES:
The study had no outside funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Anti-acid drugs used by patients with systemic sclerosis reduce the bioavailability of mycophenolate mofetil (MMF).
METHODOLOGY:
- Researchers conducted an open-label, pragmatic crossover study of 20 patients (all female) with systemic sclerosis at a single center who were on a stable MMF dose (1.5-2 g/day) for the last 3 months or more.
- Participants sequentially took MMF alone for 1 month, then with the H2 receptor blocker (HRB) ranitidine 300 mg/day in the second month, then with the proton pump inhibitor (PPI) esomeprazole 40 mg/day in the third month.
- Researchers measured the bioavailability of MMF in the patients during treatment with ranitidine or esomeprazole and the impact of the drugs on the total GI score of the UCLA Scleroderma Clinical Trial Consortium Gastrointestinal Tract 2.0 instrument.
- Patients were excluded if they were receiving co-prescription of cholestyramine, magnesium- or aluminum-containing antacids, and rifampicin; taking prednisolone-equivalent dose > 5 mg/day; taking MMF plus a PPI or an HRB at baseline; living with chronic kidney disease with a glomerular filtration rate < 30 mL/min; positive for HIV, HCV, or HBV; or living with end-stage lung disease or gastroduodenal ulcers.
TAKEAWAY:
- Mean estimated 12-hour area under curve levels of mycophenolic acid dropped by 32.7% (mean difference = 22.28 mcg h mL–1) when patients added esomeprazole, and they dipped by 21.97% (mean difference = 14.93 mcg h mL–1) when they added ranitidine vs. MMF alone.
- The pharmacokinetic parameter T-max did not differ significantly between MMF alone vs. MMF plus ranitidine but was significantly different with esomeprazole. C-max significantly declined with administration of ranitidine or esomeprazole vs. MMF alone.
- Total GI scores dipped when patients added esomeprazole or ranitidine.
IN PRACTICE:
In patients with significant gastroesophageal reflux disease symptoms who need to take MMF, management options may include monitoring MMF drug levels, switching to enteric-coated mycophenolate sodium, and spacing doses with anti-acid drugs.
SOURCE:
Glaxon Alex, MD, and colleagues from the Center for Arthritis and Rheumatism Excellence in Kochi, India, conducted the study, which was published online in Seminars in Arthritis & Rheumatism.
LIMITATIONS:
The sample size is small, and the optimum dose of MMF is unknown.
DISCLOSURES:
The study had no outside funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Anti-acid drugs used by patients with systemic sclerosis reduce the bioavailability of mycophenolate mofetil (MMF).
METHODOLOGY:
- Researchers conducted an open-label, pragmatic crossover study of 20 patients (all female) with systemic sclerosis at a single center who were on a stable MMF dose (1.5-2 g/day) for the last 3 months or more.
- Participants sequentially took MMF alone for 1 month, then with the H2 receptor blocker (HRB) ranitidine 300 mg/day in the second month, then with the proton pump inhibitor (PPI) esomeprazole 40 mg/day in the third month.
- Researchers measured the bioavailability of MMF in the patients during treatment with ranitidine or esomeprazole and the impact of the drugs on the total GI score of the UCLA Scleroderma Clinical Trial Consortium Gastrointestinal Tract 2.0 instrument.
- Patients were excluded if they were receiving co-prescription of cholestyramine, magnesium- or aluminum-containing antacids, and rifampicin; taking prednisolone-equivalent dose > 5 mg/day; taking MMF plus a PPI or an HRB at baseline; living with chronic kidney disease with a glomerular filtration rate < 30 mL/min; positive for HIV, HCV, or HBV; or living with end-stage lung disease or gastroduodenal ulcers.
TAKEAWAY:
- Mean estimated 12-hour area under curve levels of mycophenolic acid dropped by 32.7% (mean difference = 22.28 mcg h mL–1) when patients added esomeprazole, and they dipped by 21.97% (mean difference = 14.93 mcg h mL–1) when they added ranitidine vs. MMF alone.
- The pharmacokinetic parameter T-max did not differ significantly between MMF alone vs. MMF plus ranitidine but was significantly different with esomeprazole. C-max significantly declined with administration of ranitidine or esomeprazole vs. MMF alone.
- Total GI scores dipped when patients added esomeprazole or ranitidine.
IN PRACTICE:
In patients with significant gastroesophageal reflux disease symptoms who need to take MMF, management options may include monitoring MMF drug levels, switching to enteric-coated mycophenolate sodium, and spacing doses with anti-acid drugs.
SOURCE:
Glaxon Alex, MD, and colleagues from the Center for Arthritis and Rheumatism Excellence in Kochi, India, conducted the study, which was published online in Seminars in Arthritis & Rheumatism.
LIMITATIONS:
The sample size is small, and the optimum dose of MMF is unknown.
DISCLOSURES:
The study had no outside funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves first tocilizumab biosimilar
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.
The Food and Drug Administration has approved the biosimilar tocilizumab-bavi (Tofidence), Biogen, the drug’s manufacturer, announced on Sept. 29.
It is the first tocilizumab biosimilar approved by the FDA. The reference product, Actemra (Genentech), was first approved by the agency in 2010.
“The approval of Tofidence in the U.S. marks another positive step toward helping more people with chronic autoimmune conditions gain access to leading therapies,” Ian Henshaw, global head of biosimilars at Biogen, said in a statement. “With the increasing numbers of approved biosimilars, we expect increased savings and sustainability for health care systems and an increase in physician choice and patient access to biologics.”
Biogen’s pricing for tocilizumab-bavi will be available closer to the product’s launch date, which has yet to be determined, a company spokesman said. The U.S. average monthly cost of Actemra for rheumatoid arthritis, administered intravenously, is $2,134-$4,268 depending on dosage, according to a Genentech spokesperson.
Tocilizumab-bavi is an intravenous formulation (20 mg/mL) indicated for treatment of moderately to severely active RA, polyarticular juvenile idiopathic arthritis (PJIA), and systemic juvenile idiopathic arthritis (SJIA). The medication is administered every 4 weeks in RA and PJIA and every 8 weeks in SJIA as a single intravenous drip infusion over 1 hour.
The European Commission approved its first tocilizumab biosimilar, Tyenne (Fresenius Kabi), earlier in 2023 in both subcutaneous and intravenous formulations. Biogen did not comment on whether the company is working on a subcutaneous formulation for tocilizumab-bavi.
A version of this article appeared on Medscape.com.