User login
Diagnosis by dog: Canines detect COVID in schoolchildren with no symptoms
Scent-detecting dogs have long been used to sniff out medical conditions ranging from low blood sugar and cancer to malaria, impending seizures, and migraines – not to mention explosives and narcotics.
Recently, the sensitivity of the canine nose has been tested as a strategy for screening for SARS-CoV-2 infection in schoolchildren showing no outward symptoms of the virus. A pilot study led by Carol A. Glaser, DVM, MD, of the California Department of Public Health in Richmond, found that trained dogs had an accuracy of more than 95% for detecting the odor of volatile organic compounds, or VOCs, produced by COVID-infected individuals.
The authors believe that odor-based diagnosis with dogs could eventually provide a rapid, inexpensive, and noninvasive way to screen large groups for COVID-19 without the need for antigen testing.
“This is a new program with research ongoing, so it would be premature to consider it from a consumer’s perspective,” Dr. Glaser said in an interview. “However, the data look promising and we are hopeful we can continue to pilot various programs in various settings to see where, and if, dogs can be used for biomedical detection.”
In the lab and in the field
In a study published online in JAMA Pediatrics, Dr. Glaser’s group found that after 2 months’ training on COVID-19 scent samples in the laboratory, the dogs detected the presence of the virus more than 95% of the time. Antigen tests were used as a comparative reference.
In medical terms, the dogs achieved a greater than 95% accuracy on two important measures of effectiveness: sensitivity – a test’s ability to correctly detect the positive presence of disease – and specificity – the ability of a test to accurately rule out the presence of disease and identify as negative an uninfected person.
Next, the researchers piloted field tests in 50 visits at 27 schools from April 1 to May 25, 2022, to compare dogs’ detection ability with that of standard laboratory antigen testing. Participants in the completely voluntary screening numbered 1,558 and ranged in age from 9 to 17 years. Of these, 56% were girls and 89% were students. Almost 70% were screened at least twice.
Overall, the field test compared 3,897 paired antigen-vs.-dog screenings. The dogs accurately signaled the presence of 85 infections and ruled out 3,411 infections, for an overall accuracy of 90%. In 383 cases, however, they inaccurately signaled the presence of infection (false positives) and missed 18 actual infections (false negatives). That translated to a sensitivity in the field of 83%, considerably lower than that of their lab performance.
Direct screening of individuals with dogs outside of the lab involved circumstantial factors that likely contributed to decreased sensitivity and specificity, the authors acknowledged. These included such distractions as noise and the presence of excitable young children as well environmental conditions such as wind and other odors. What about dog phobia and dog hair allergy? “Dog screening takes only a few seconds per student and the dogs do not generally touch the participant as they run a line and sniff at ankles,” Dr. Glaser explained.
As for allergies, the rapid, ankle-level screening occurred in outdoor settings. “The chance of allergies is very low. This would be similar to someone who is out walking on the sidewalk and walks by a dog,” Dr. Glaser said.
Last year, a British trial of almost 4,000 adults tested six dogs trained to detect differences in VOCs between COVID-infected and uninfected individuals. Given samples from both groups, the dogs were able to distinguish between infected and uninfected samples with a sensitivity for detecting the virus ranging from 82% to 94% and a specificity for ruling it out of 76% to 92%. And they were able to smell the VOCs even when the viral load was low. The study also tested organic sensors, which proved even more accurate than the canines.
According to lead author James G. Logan, PhD, a disease control expert at the London School of Hygiene & Tropical Medicine in London, “Odour-based diagnostics using dogs and/or sensors may prove a rapid and effective tool for screening large numbers of people. Mathematical modelling suggests that dog screening plus a confirmatory PCR test could detect up to 89% of SARS-CoV-2 infections, averting up to 2.2 times as much transmission compared to isolation of symptomatic individuals only.”
Funding was provided by the Centers for Disease Control and Prevention Foundation (CDCF) to Early Alert Canines for the purchase and care of the dogs and the support of the handlers and trainers. The CDCF had no other role in the study. Coauthor Carol A. Edwards of Early Alert Canines reported receiving grants from the CDCF.
Scent-detecting dogs have long been used to sniff out medical conditions ranging from low blood sugar and cancer to malaria, impending seizures, and migraines – not to mention explosives and narcotics.
Recently, the sensitivity of the canine nose has been tested as a strategy for screening for SARS-CoV-2 infection in schoolchildren showing no outward symptoms of the virus. A pilot study led by Carol A. Glaser, DVM, MD, of the California Department of Public Health in Richmond, found that trained dogs had an accuracy of more than 95% for detecting the odor of volatile organic compounds, or VOCs, produced by COVID-infected individuals.
The authors believe that odor-based diagnosis with dogs could eventually provide a rapid, inexpensive, and noninvasive way to screen large groups for COVID-19 without the need for antigen testing.
“This is a new program with research ongoing, so it would be premature to consider it from a consumer’s perspective,” Dr. Glaser said in an interview. “However, the data look promising and we are hopeful we can continue to pilot various programs in various settings to see where, and if, dogs can be used for biomedical detection.”
In the lab and in the field
In a study published online in JAMA Pediatrics, Dr. Glaser’s group found that after 2 months’ training on COVID-19 scent samples in the laboratory, the dogs detected the presence of the virus more than 95% of the time. Antigen tests were used as a comparative reference.
In medical terms, the dogs achieved a greater than 95% accuracy on two important measures of effectiveness: sensitivity – a test’s ability to correctly detect the positive presence of disease – and specificity – the ability of a test to accurately rule out the presence of disease and identify as negative an uninfected person.
Next, the researchers piloted field tests in 50 visits at 27 schools from April 1 to May 25, 2022, to compare dogs’ detection ability with that of standard laboratory antigen testing. Participants in the completely voluntary screening numbered 1,558 and ranged in age from 9 to 17 years. Of these, 56% were girls and 89% were students. Almost 70% were screened at least twice.
Overall, the field test compared 3,897 paired antigen-vs.-dog screenings. The dogs accurately signaled the presence of 85 infections and ruled out 3,411 infections, for an overall accuracy of 90%. In 383 cases, however, they inaccurately signaled the presence of infection (false positives) and missed 18 actual infections (false negatives). That translated to a sensitivity in the field of 83%, considerably lower than that of their lab performance.
Direct screening of individuals with dogs outside of the lab involved circumstantial factors that likely contributed to decreased sensitivity and specificity, the authors acknowledged. These included such distractions as noise and the presence of excitable young children as well environmental conditions such as wind and other odors. What about dog phobia and dog hair allergy? “Dog screening takes only a few seconds per student and the dogs do not generally touch the participant as they run a line and sniff at ankles,” Dr. Glaser explained.
As for allergies, the rapid, ankle-level screening occurred in outdoor settings. “The chance of allergies is very low. This would be similar to someone who is out walking on the sidewalk and walks by a dog,” Dr. Glaser said.
Last year, a British trial of almost 4,000 adults tested six dogs trained to detect differences in VOCs between COVID-infected and uninfected individuals. Given samples from both groups, the dogs were able to distinguish between infected and uninfected samples with a sensitivity for detecting the virus ranging from 82% to 94% and a specificity for ruling it out of 76% to 92%. And they were able to smell the VOCs even when the viral load was low. The study also tested organic sensors, which proved even more accurate than the canines.
According to lead author James G. Logan, PhD, a disease control expert at the London School of Hygiene & Tropical Medicine in London, “Odour-based diagnostics using dogs and/or sensors may prove a rapid and effective tool for screening large numbers of people. Mathematical modelling suggests that dog screening plus a confirmatory PCR test could detect up to 89% of SARS-CoV-2 infections, averting up to 2.2 times as much transmission compared to isolation of symptomatic individuals only.”
Funding was provided by the Centers for Disease Control and Prevention Foundation (CDCF) to Early Alert Canines for the purchase and care of the dogs and the support of the handlers and trainers. The CDCF had no other role in the study. Coauthor Carol A. Edwards of Early Alert Canines reported receiving grants from the CDCF.
Scent-detecting dogs have long been used to sniff out medical conditions ranging from low blood sugar and cancer to malaria, impending seizures, and migraines – not to mention explosives and narcotics.
Recently, the sensitivity of the canine nose has been tested as a strategy for screening for SARS-CoV-2 infection in schoolchildren showing no outward symptoms of the virus. A pilot study led by Carol A. Glaser, DVM, MD, of the California Department of Public Health in Richmond, found that trained dogs had an accuracy of more than 95% for detecting the odor of volatile organic compounds, or VOCs, produced by COVID-infected individuals.
The authors believe that odor-based diagnosis with dogs could eventually provide a rapid, inexpensive, and noninvasive way to screen large groups for COVID-19 without the need for antigen testing.
“This is a new program with research ongoing, so it would be premature to consider it from a consumer’s perspective,” Dr. Glaser said in an interview. “However, the data look promising and we are hopeful we can continue to pilot various programs in various settings to see where, and if, dogs can be used for biomedical detection.”
In the lab and in the field
In a study published online in JAMA Pediatrics, Dr. Glaser’s group found that after 2 months’ training on COVID-19 scent samples in the laboratory, the dogs detected the presence of the virus more than 95% of the time. Antigen tests were used as a comparative reference.
In medical terms, the dogs achieved a greater than 95% accuracy on two important measures of effectiveness: sensitivity – a test’s ability to correctly detect the positive presence of disease – and specificity – the ability of a test to accurately rule out the presence of disease and identify as negative an uninfected person.
Next, the researchers piloted field tests in 50 visits at 27 schools from April 1 to May 25, 2022, to compare dogs’ detection ability with that of standard laboratory antigen testing. Participants in the completely voluntary screening numbered 1,558 and ranged in age from 9 to 17 years. Of these, 56% were girls and 89% were students. Almost 70% were screened at least twice.
Overall, the field test compared 3,897 paired antigen-vs.-dog screenings. The dogs accurately signaled the presence of 85 infections and ruled out 3,411 infections, for an overall accuracy of 90%. In 383 cases, however, they inaccurately signaled the presence of infection (false positives) and missed 18 actual infections (false negatives). That translated to a sensitivity in the field of 83%, considerably lower than that of their lab performance.
Direct screening of individuals with dogs outside of the lab involved circumstantial factors that likely contributed to decreased sensitivity and specificity, the authors acknowledged. These included such distractions as noise and the presence of excitable young children as well environmental conditions such as wind and other odors. What about dog phobia and dog hair allergy? “Dog screening takes only a few seconds per student and the dogs do not generally touch the participant as they run a line and sniff at ankles,” Dr. Glaser explained.
As for allergies, the rapid, ankle-level screening occurred in outdoor settings. “The chance of allergies is very low. This would be similar to someone who is out walking on the sidewalk and walks by a dog,” Dr. Glaser said.
Last year, a British trial of almost 4,000 adults tested six dogs trained to detect differences in VOCs between COVID-infected and uninfected individuals. Given samples from both groups, the dogs were able to distinguish between infected and uninfected samples with a sensitivity for detecting the virus ranging from 82% to 94% and a specificity for ruling it out of 76% to 92%. And they were able to smell the VOCs even when the viral load was low. The study also tested organic sensors, which proved even more accurate than the canines.
According to lead author James G. Logan, PhD, a disease control expert at the London School of Hygiene & Tropical Medicine in London, “Odour-based diagnostics using dogs and/or sensors may prove a rapid and effective tool for screening large numbers of people. Mathematical modelling suggests that dog screening plus a confirmatory PCR test could detect up to 89% of SARS-CoV-2 infections, averting up to 2.2 times as much transmission compared to isolation of symptomatic individuals only.”
Funding was provided by the Centers for Disease Control and Prevention Foundation (CDCF) to Early Alert Canines for the purchase and care of the dogs and the support of the handlers and trainers. The CDCF had no other role in the study. Coauthor Carol A. Edwards of Early Alert Canines reported receiving grants from the CDCF.
FROM JAMA PEDIATRICS
Child’s health improves by applying new obesity guidelines
At age 15 years, Maya was referred by her primary care provider to our pediatric obesity center. She weighed 151 kg and had a body mass index (BMI) over 48 kg/m2. One year earlier, she had been diagnosed with hypertension and prediabetes.
A review of her growth charts showed that she had been in the 95th percentile at age 8 years. Her weight had steadily risen, with an exponential increase of 55 lb between 2020 and 2022, during the COVID-19 pandemic. Her primary care provider monitored her from age 8 to 12 years, providing nutrition and physical activity counseling.
In February, the American Academy of Pediatrics released new clinical practice guidelines for managing childhood obesity. A better understanding of the pathophysiology has challenged the old-worn concept of lack of will power and personal responsibility as the cause of obesity, which has been the basis for weight-related bias and stigma. The updated guidelines have also been influenced by lifestyle intervention studies, the US Food and Drug Administration approval of new anti-obesity medications, and the 2013 designation of obesity as a disease by the American Medical Association.
We used these updated guidelines in our approach to treating Maya.
Starting with the assessment
In the new AAP guidelines, assessing the genetic, environmental, and social-determinant risks for obesity form the basis for evaluation and intervention. Following this approach, we conducted a complete medical evaluation of Maya, including a review of her symptoms and her family history along with a physical examination to assess for comorbidities and other cause of obesity (for example, genetic, hypothyroidism).
We also collected information regarding her diet and behaviors (for example, drinking sweet beverages, fruit and vegetable intake, parent feeding style, portion sizes, emotional eating, hyperphagia), physical activity behaviors (for example, physical education, organized sports), screen time, social drivers of health (for example, food insecurity, neighborhood, school environment), family and household factors (for example, family composition, support, number of caregivers, parenting style) and mental and physical health (autism, attention-deficit/hyperactivity disorder, history of being bullied, developmental and physical disabilities). Because Maya had a BMI of 48, she met the criterion for severe obesity, which is having a BMI at least 120% of the 95th percentile.
The guidelines use BMI as a criterion for screening for obesity because it is inexpensive and easy to obtain in the clinic setting. The Centers for Disease Control and Prevention growth chart uses BMI as well. Recently, there has been controversy about solely using BMI to define obesity, which is a point that the guidelines address by emphasizing evaluation of the whole child along with BMI to make a diagnosis of obesity.
The child’s age and the severity of their obesity drive the evaluation for comorbidities and treatment. In children aged 10 years or older, pediatricians and other primary care providers should evaluate for lipid abnormalities, abnormal glucose metabolism, and abnormal liver function in children and adolescents with obesity (BMI ≥ 95th percentile).
Maya presented with snoring, early-morning headaches, daytime sleepiness, and abdominal pain. A sleep study revealed an apnea-hypopnea index of 15, indicating obstructive sleep apnea, and she was placed on a continuous positive airway pressure machine.
Her laboratory studies showed elevated triglycerides of 169 mg/dL and abnormal ALT (123 IU/L). Potential causes of elevated liver function test results (such as abnormal ceruloplasmin levels or infectious or autoimmune hepatitis) were excluded, and a liver ultrasound with elastography indicated steatohepatitis. Maya was referred to gastroenterology for nonalcoholic fatty liver disease.
Maya experienced depressive symptoms, including difficulty with peer relationships and declining academic performance. Her Patient Health Questionnaire–9 score was 21, with a moderate impact on her daily functioning. Prior attempts at counseling had been sporadic and not helpful. She was diagnosed with intermittent moderate clinical depression, started on a selective serotonin reuptake inhibitor, and resumed counseling with a new therapist.
Considering treatment options
Based on shared decision-making, our team began a more intensive lifestyle behavior treatment as recommended in the updated guidelines. Maya chose to decrease sugar-sweetened beverages as her initial nutrition goal, a change that can lead to a reduction of liver function test results and triglycerides, even in the absence of weight loss.
As emphasized in the guidelines, we stressed the importance of managing obesity and comorbidities concurrently to the family. In addition to lifestyle behavior intervention, once her mental health stabilized, Maya and her mother opted for bariatric surgery. Sleeve gastrectomy was elected because she met the criteria.
If the child already has obesity, the guidelines discourage watchful waiting (that is, the expectation that the child will grow into their weight) as Maya’s primary care provider had done when she was younger. The staged treatment approach where progressively more intensive interventions are adopted (a hallmark of the 2007 guidelines) is no longer recommended. Rather, the primary care provider should offer treatment options guided by age, severity of obesity, and comorbidities.
Maya completed a bariatric preoperative program, extensive mental health evaluation, and tolerated the sleeve gastrectomy well with no complications. At her 6-month postoperative visit, she had lost 99 lb (45 kg) since the surgery, with an 18% decline in BMI. She is taking daily multivitamins as well as calcium and vitamin D. She continues to incorporate healthy eating into her life, with a focus on adequate protein intake and is exercising three to four times per week in the apartment complex gym. She reports better physical and mental health, her school performance has improved, and she still receives regular counseling.
Maya’s story outlines the benefits of early and intensive intervention as recommended by the new AAP guidelines. The shift from some of the earlier recommendations is partly driven by the persistence of childhood obesity into adulthood, especially for older children with serious psychosocial and physical comorbidities. Hopefully by implementing the new guidelines, the physician can provide empathetic, bias-free, and effective care that recognizes the needs and environment of the whole child.
Dr. Salhah is a pediatric endocrinology fellow at Nationwide Children’s Hospital, Columbus, Ohio. Dr. Eneli is director of the Center for Healthy Weight and Nutrition at Nationwide Children’s Hospital. Dr. Salhah reported no conflicts of interest. Dr. Eneli reported receiving research grants and income from the National Institutes of Health, the AAP, and the National Academy of Medicine.
A version of this article first appeared on Medscape.com.
At age 15 years, Maya was referred by her primary care provider to our pediatric obesity center. She weighed 151 kg and had a body mass index (BMI) over 48 kg/m2. One year earlier, she had been diagnosed with hypertension and prediabetes.
A review of her growth charts showed that she had been in the 95th percentile at age 8 years. Her weight had steadily risen, with an exponential increase of 55 lb between 2020 and 2022, during the COVID-19 pandemic. Her primary care provider monitored her from age 8 to 12 years, providing nutrition and physical activity counseling.
In February, the American Academy of Pediatrics released new clinical practice guidelines for managing childhood obesity. A better understanding of the pathophysiology has challenged the old-worn concept of lack of will power and personal responsibility as the cause of obesity, which has been the basis for weight-related bias and stigma. The updated guidelines have also been influenced by lifestyle intervention studies, the US Food and Drug Administration approval of new anti-obesity medications, and the 2013 designation of obesity as a disease by the American Medical Association.
We used these updated guidelines in our approach to treating Maya.
Starting with the assessment
In the new AAP guidelines, assessing the genetic, environmental, and social-determinant risks for obesity form the basis for evaluation and intervention. Following this approach, we conducted a complete medical evaluation of Maya, including a review of her symptoms and her family history along with a physical examination to assess for comorbidities and other cause of obesity (for example, genetic, hypothyroidism).
We also collected information regarding her diet and behaviors (for example, drinking sweet beverages, fruit and vegetable intake, parent feeding style, portion sizes, emotional eating, hyperphagia), physical activity behaviors (for example, physical education, organized sports), screen time, social drivers of health (for example, food insecurity, neighborhood, school environment), family and household factors (for example, family composition, support, number of caregivers, parenting style) and mental and physical health (autism, attention-deficit/hyperactivity disorder, history of being bullied, developmental and physical disabilities). Because Maya had a BMI of 48, she met the criterion for severe obesity, which is having a BMI at least 120% of the 95th percentile.
The guidelines use BMI as a criterion for screening for obesity because it is inexpensive and easy to obtain in the clinic setting. The Centers for Disease Control and Prevention growth chart uses BMI as well. Recently, there has been controversy about solely using BMI to define obesity, which is a point that the guidelines address by emphasizing evaluation of the whole child along with BMI to make a diagnosis of obesity.
The child’s age and the severity of their obesity drive the evaluation for comorbidities and treatment. In children aged 10 years or older, pediatricians and other primary care providers should evaluate for lipid abnormalities, abnormal glucose metabolism, and abnormal liver function in children and adolescents with obesity (BMI ≥ 95th percentile).
Maya presented with snoring, early-morning headaches, daytime sleepiness, and abdominal pain. A sleep study revealed an apnea-hypopnea index of 15, indicating obstructive sleep apnea, and she was placed on a continuous positive airway pressure machine.
Her laboratory studies showed elevated triglycerides of 169 mg/dL and abnormal ALT (123 IU/L). Potential causes of elevated liver function test results (such as abnormal ceruloplasmin levels or infectious or autoimmune hepatitis) were excluded, and a liver ultrasound with elastography indicated steatohepatitis. Maya was referred to gastroenterology for nonalcoholic fatty liver disease.
Maya experienced depressive symptoms, including difficulty with peer relationships and declining academic performance. Her Patient Health Questionnaire–9 score was 21, with a moderate impact on her daily functioning. Prior attempts at counseling had been sporadic and not helpful. She was diagnosed with intermittent moderate clinical depression, started on a selective serotonin reuptake inhibitor, and resumed counseling with a new therapist.
Considering treatment options
Based on shared decision-making, our team began a more intensive lifestyle behavior treatment as recommended in the updated guidelines. Maya chose to decrease sugar-sweetened beverages as her initial nutrition goal, a change that can lead to a reduction of liver function test results and triglycerides, even in the absence of weight loss.
As emphasized in the guidelines, we stressed the importance of managing obesity and comorbidities concurrently to the family. In addition to lifestyle behavior intervention, once her mental health stabilized, Maya and her mother opted for bariatric surgery. Sleeve gastrectomy was elected because she met the criteria.
If the child already has obesity, the guidelines discourage watchful waiting (that is, the expectation that the child will grow into their weight) as Maya’s primary care provider had done when she was younger. The staged treatment approach where progressively more intensive interventions are adopted (a hallmark of the 2007 guidelines) is no longer recommended. Rather, the primary care provider should offer treatment options guided by age, severity of obesity, and comorbidities.
Maya completed a bariatric preoperative program, extensive mental health evaluation, and tolerated the sleeve gastrectomy well with no complications. At her 6-month postoperative visit, she had lost 99 lb (45 kg) since the surgery, with an 18% decline in BMI. She is taking daily multivitamins as well as calcium and vitamin D. She continues to incorporate healthy eating into her life, with a focus on adequate protein intake and is exercising three to four times per week in the apartment complex gym. She reports better physical and mental health, her school performance has improved, and she still receives regular counseling.
Maya’s story outlines the benefits of early and intensive intervention as recommended by the new AAP guidelines. The shift from some of the earlier recommendations is partly driven by the persistence of childhood obesity into adulthood, especially for older children with serious psychosocial and physical comorbidities. Hopefully by implementing the new guidelines, the physician can provide empathetic, bias-free, and effective care that recognizes the needs and environment of the whole child.
Dr. Salhah is a pediatric endocrinology fellow at Nationwide Children’s Hospital, Columbus, Ohio. Dr. Eneli is director of the Center for Healthy Weight and Nutrition at Nationwide Children’s Hospital. Dr. Salhah reported no conflicts of interest. Dr. Eneli reported receiving research grants and income from the National Institutes of Health, the AAP, and the National Academy of Medicine.
A version of this article first appeared on Medscape.com.
At age 15 years, Maya was referred by her primary care provider to our pediatric obesity center. She weighed 151 kg and had a body mass index (BMI) over 48 kg/m2. One year earlier, she had been diagnosed with hypertension and prediabetes.
A review of her growth charts showed that she had been in the 95th percentile at age 8 years. Her weight had steadily risen, with an exponential increase of 55 lb between 2020 and 2022, during the COVID-19 pandemic. Her primary care provider monitored her from age 8 to 12 years, providing nutrition and physical activity counseling.
In February, the American Academy of Pediatrics released new clinical practice guidelines for managing childhood obesity. A better understanding of the pathophysiology has challenged the old-worn concept of lack of will power and personal responsibility as the cause of obesity, which has been the basis for weight-related bias and stigma. The updated guidelines have also been influenced by lifestyle intervention studies, the US Food and Drug Administration approval of new anti-obesity medications, and the 2013 designation of obesity as a disease by the American Medical Association.
We used these updated guidelines in our approach to treating Maya.
Starting with the assessment
In the new AAP guidelines, assessing the genetic, environmental, and social-determinant risks for obesity form the basis for evaluation and intervention. Following this approach, we conducted a complete medical evaluation of Maya, including a review of her symptoms and her family history along with a physical examination to assess for comorbidities and other cause of obesity (for example, genetic, hypothyroidism).
We also collected information regarding her diet and behaviors (for example, drinking sweet beverages, fruit and vegetable intake, parent feeding style, portion sizes, emotional eating, hyperphagia), physical activity behaviors (for example, physical education, organized sports), screen time, social drivers of health (for example, food insecurity, neighborhood, school environment), family and household factors (for example, family composition, support, number of caregivers, parenting style) and mental and physical health (autism, attention-deficit/hyperactivity disorder, history of being bullied, developmental and physical disabilities). Because Maya had a BMI of 48, she met the criterion for severe obesity, which is having a BMI at least 120% of the 95th percentile.
The guidelines use BMI as a criterion for screening for obesity because it is inexpensive and easy to obtain in the clinic setting. The Centers for Disease Control and Prevention growth chart uses BMI as well. Recently, there has been controversy about solely using BMI to define obesity, which is a point that the guidelines address by emphasizing evaluation of the whole child along with BMI to make a diagnosis of obesity.
The child’s age and the severity of their obesity drive the evaluation for comorbidities and treatment. In children aged 10 years or older, pediatricians and other primary care providers should evaluate for lipid abnormalities, abnormal glucose metabolism, and abnormal liver function in children and adolescents with obesity (BMI ≥ 95th percentile).
Maya presented with snoring, early-morning headaches, daytime sleepiness, and abdominal pain. A sleep study revealed an apnea-hypopnea index of 15, indicating obstructive sleep apnea, and she was placed on a continuous positive airway pressure machine.
Her laboratory studies showed elevated triglycerides of 169 mg/dL and abnormal ALT (123 IU/L). Potential causes of elevated liver function test results (such as abnormal ceruloplasmin levels or infectious or autoimmune hepatitis) were excluded, and a liver ultrasound with elastography indicated steatohepatitis. Maya was referred to gastroenterology for nonalcoholic fatty liver disease.
Maya experienced depressive symptoms, including difficulty with peer relationships and declining academic performance. Her Patient Health Questionnaire–9 score was 21, with a moderate impact on her daily functioning. Prior attempts at counseling had been sporadic and not helpful. She was diagnosed with intermittent moderate clinical depression, started on a selective serotonin reuptake inhibitor, and resumed counseling with a new therapist.
Considering treatment options
Based on shared decision-making, our team began a more intensive lifestyle behavior treatment as recommended in the updated guidelines. Maya chose to decrease sugar-sweetened beverages as her initial nutrition goal, a change that can lead to a reduction of liver function test results and triglycerides, even in the absence of weight loss.
As emphasized in the guidelines, we stressed the importance of managing obesity and comorbidities concurrently to the family. In addition to lifestyle behavior intervention, once her mental health stabilized, Maya and her mother opted for bariatric surgery. Sleeve gastrectomy was elected because she met the criteria.
If the child already has obesity, the guidelines discourage watchful waiting (that is, the expectation that the child will grow into their weight) as Maya’s primary care provider had done when she was younger. The staged treatment approach where progressively more intensive interventions are adopted (a hallmark of the 2007 guidelines) is no longer recommended. Rather, the primary care provider should offer treatment options guided by age, severity of obesity, and comorbidities.
Maya completed a bariatric preoperative program, extensive mental health evaluation, and tolerated the sleeve gastrectomy well with no complications. At her 6-month postoperative visit, she had lost 99 lb (45 kg) since the surgery, with an 18% decline in BMI. She is taking daily multivitamins as well as calcium and vitamin D. She continues to incorporate healthy eating into her life, with a focus on adequate protein intake and is exercising three to four times per week in the apartment complex gym. She reports better physical and mental health, her school performance has improved, and she still receives regular counseling.
Maya’s story outlines the benefits of early and intensive intervention as recommended by the new AAP guidelines. The shift from some of the earlier recommendations is partly driven by the persistence of childhood obesity into adulthood, especially for older children with serious psychosocial and physical comorbidities. Hopefully by implementing the new guidelines, the physician can provide empathetic, bias-free, and effective care that recognizes the needs and environment of the whole child.
Dr. Salhah is a pediatric endocrinology fellow at Nationwide Children’s Hospital, Columbus, Ohio. Dr. Eneli is director of the Center for Healthy Weight and Nutrition at Nationwide Children’s Hospital. Dr. Salhah reported no conflicts of interest. Dr. Eneli reported receiving research grants and income from the National Institutes of Health, the AAP, and the National Academy of Medicine.
A version of this article first appeared on Medscape.com.
Study focuses on adolescent data in upadacitinib AD trials
(AD), an analysis of three clinical trials reports.
Upadacitinib (Rinvoq) was approved by the Food and Drug Administration for treating adults and pediatric patients 12 years of age and older with refractory, moderate to severe AD, in January 2022. This study analyzed the adolescent data in three double-blind, placebo-controlled phase 3 randomized clinical trials, which included adults and 552 adolescents between 12 and 17 years of age with moderate to severe AD in more than 20 countries in Europe, North and South America, the Middle East, Oceania, and the Asia-Pacific region from July 2018 through December 2020.
In the studies, “treatment of moderate to severe AD in adolescents with upadacitinib was effective and generally well tolerated, with an overall efficacy and safety profile similar to that observed in adults, and patient-reported outcomes indicated an overall better health-related quality of life compared with placebo,” lead study author Amy S. Paller, MD, chair of the department of dermatology and professor of dermatology and pediatrics, at Northwestern University, Chicago, and her colleagues write in JAMA Dermatology.
Adolescents in the three studies – Measure Up 1, Measure Up 2, and AD Up – received once-daily oral upadacitinib 15 mg, 30 mg, or placebo. All participants in AD Up used topical corticosteroids.
At 16 weeks, in Measure Up 1, Measure Up 2, and AD Up, respectively, a greater proportion of adolescents improved by at least 75% in the Eczema Area and Severity Index (EASI 75) with upadacitinib 15 mg (73%, 69%, 63%); and with upadacitinib 30 mg (78%, 73%, 84%), compared with placebo (12%, 13%, 30%), (P < .001 for all comparisons vs. placebo).
Upadacitinib was generally well tolerated among the adolescents, with mild or moderate acne being the most common adverse event, reported in 10%-13% of those on 15 mg and 15%-16% of those on 30 mg vs. 2%-3% of those on placebo.
Asked to comment on the study, Peck Ong, MD, a pediatric allergist and immunologist at Children’s Hospital Los Angeles, said that he was not surprised by the drug’s effectiveness because JAK inhibitors are potent immunosuppressants. Strengths of the studies include the many pediatric participants, its international reach, and its use of standardized and validated measures, said Dr. Ong, who was not involved in the study.
“The effect of JAK inhibitors is more specific than traditional immunosuppressants such as cyclosporine and methotrexate but not as specific as biologics; therefore, long-term safety data are needed,” he advised. “16 weeks is a very short time to study a chronic disease like atopic dermatitis. We need safety data longer than 1 year.”
Given the disease’s potential impact on self-esteem, sleep, and other important areas of life, Sean Reynolds, MBBCH, a pediatric dermatologist at Children’s Mercy Kansas City (Mo.), welcomed the data on the newer pharmacologic agents.
“FDA-approved systemic treatment options for adolescents with AD are currently limited, which necessitates studies such as this that explore additional treatment options,” said Dr. Reynolds, who also was not involved in the study, told this news organization.
He added that oral upadacitinib may especially help patients who have not found relief with other topical or systemic treatments or who are needle phobic. While the overall efficacy and relatively mild side effects for most patients taking upadacitinib in the trials are encouraging, “the long-term efficacy and side effects in this population require further study, especially considering the limited systemic AD treatment options available in this age group,” he added.
“Given the reported use of other JAK inhibitors to treat myriad inflammatory skin conditions beyond atopic dermatitis, the potential use of upadacitinib and other JAK inhibitors to treat these skin diseases in children and adolescents represents an exciting area for future study in the field of pediatric dermatology,” Dr. Reynolds noted.
The study was funded by AbbVie, the developer and manufacturer of upadacitinib. Dr. Paller and almost all other authors reported relevant financial relationships with AbbVie and other pharmaceutical companies. Dr. Ong reported serving on an AbbVie advisory board, and Dr. Reynolds reported no conflict of interest with the study.
(AD), an analysis of three clinical trials reports.
Upadacitinib (Rinvoq) was approved by the Food and Drug Administration for treating adults and pediatric patients 12 years of age and older with refractory, moderate to severe AD, in January 2022. This study analyzed the adolescent data in three double-blind, placebo-controlled phase 3 randomized clinical trials, which included adults and 552 adolescents between 12 and 17 years of age with moderate to severe AD in more than 20 countries in Europe, North and South America, the Middle East, Oceania, and the Asia-Pacific region from July 2018 through December 2020.
In the studies, “treatment of moderate to severe AD in adolescents with upadacitinib was effective and generally well tolerated, with an overall efficacy and safety profile similar to that observed in adults, and patient-reported outcomes indicated an overall better health-related quality of life compared with placebo,” lead study author Amy S. Paller, MD, chair of the department of dermatology and professor of dermatology and pediatrics, at Northwestern University, Chicago, and her colleagues write in JAMA Dermatology.
Adolescents in the three studies – Measure Up 1, Measure Up 2, and AD Up – received once-daily oral upadacitinib 15 mg, 30 mg, or placebo. All participants in AD Up used topical corticosteroids.
At 16 weeks, in Measure Up 1, Measure Up 2, and AD Up, respectively, a greater proportion of adolescents improved by at least 75% in the Eczema Area and Severity Index (EASI 75) with upadacitinib 15 mg (73%, 69%, 63%); and with upadacitinib 30 mg (78%, 73%, 84%), compared with placebo (12%, 13%, 30%), (P < .001 for all comparisons vs. placebo).
Upadacitinib was generally well tolerated among the adolescents, with mild or moderate acne being the most common adverse event, reported in 10%-13% of those on 15 mg and 15%-16% of those on 30 mg vs. 2%-3% of those on placebo.
Asked to comment on the study, Peck Ong, MD, a pediatric allergist and immunologist at Children’s Hospital Los Angeles, said that he was not surprised by the drug’s effectiveness because JAK inhibitors are potent immunosuppressants. Strengths of the studies include the many pediatric participants, its international reach, and its use of standardized and validated measures, said Dr. Ong, who was not involved in the study.
“The effect of JAK inhibitors is more specific than traditional immunosuppressants such as cyclosporine and methotrexate but not as specific as biologics; therefore, long-term safety data are needed,” he advised. “16 weeks is a very short time to study a chronic disease like atopic dermatitis. We need safety data longer than 1 year.”
Given the disease’s potential impact on self-esteem, sleep, and other important areas of life, Sean Reynolds, MBBCH, a pediatric dermatologist at Children’s Mercy Kansas City (Mo.), welcomed the data on the newer pharmacologic agents.
“FDA-approved systemic treatment options for adolescents with AD are currently limited, which necessitates studies such as this that explore additional treatment options,” said Dr. Reynolds, who also was not involved in the study, told this news organization.
He added that oral upadacitinib may especially help patients who have not found relief with other topical or systemic treatments or who are needle phobic. While the overall efficacy and relatively mild side effects for most patients taking upadacitinib in the trials are encouraging, “the long-term efficacy and side effects in this population require further study, especially considering the limited systemic AD treatment options available in this age group,” he added.
“Given the reported use of other JAK inhibitors to treat myriad inflammatory skin conditions beyond atopic dermatitis, the potential use of upadacitinib and other JAK inhibitors to treat these skin diseases in children and adolescents represents an exciting area for future study in the field of pediatric dermatology,” Dr. Reynolds noted.
The study was funded by AbbVie, the developer and manufacturer of upadacitinib. Dr. Paller and almost all other authors reported relevant financial relationships with AbbVie and other pharmaceutical companies. Dr. Ong reported serving on an AbbVie advisory board, and Dr. Reynolds reported no conflict of interest with the study.
(AD), an analysis of three clinical trials reports.
Upadacitinib (Rinvoq) was approved by the Food and Drug Administration for treating adults and pediatric patients 12 years of age and older with refractory, moderate to severe AD, in January 2022. This study analyzed the adolescent data in three double-blind, placebo-controlled phase 3 randomized clinical trials, which included adults and 552 adolescents between 12 and 17 years of age with moderate to severe AD in more than 20 countries in Europe, North and South America, the Middle East, Oceania, and the Asia-Pacific region from July 2018 through December 2020.
In the studies, “treatment of moderate to severe AD in adolescents with upadacitinib was effective and generally well tolerated, with an overall efficacy and safety profile similar to that observed in adults, and patient-reported outcomes indicated an overall better health-related quality of life compared with placebo,” lead study author Amy S. Paller, MD, chair of the department of dermatology and professor of dermatology and pediatrics, at Northwestern University, Chicago, and her colleagues write in JAMA Dermatology.
Adolescents in the three studies – Measure Up 1, Measure Up 2, and AD Up – received once-daily oral upadacitinib 15 mg, 30 mg, or placebo. All participants in AD Up used topical corticosteroids.
At 16 weeks, in Measure Up 1, Measure Up 2, and AD Up, respectively, a greater proportion of adolescents improved by at least 75% in the Eczema Area and Severity Index (EASI 75) with upadacitinib 15 mg (73%, 69%, 63%); and with upadacitinib 30 mg (78%, 73%, 84%), compared with placebo (12%, 13%, 30%), (P < .001 for all comparisons vs. placebo).
Upadacitinib was generally well tolerated among the adolescents, with mild or moderate acne being the most common adverse event, reported in 10%-13% of those on 15 mg and 15%-16% of those on 30 mg vs. 2%-3% of those on placebo.
Asked to comment on the study, Peck Ong, MD, a pediatric allergist and immunologist at Children’s Hospital Los Angeles, said that he was not surprised by the drug’s effectiveness because JAK inhibitors are potent immunosuppressants. Strengths of the studies include the many pediatric participants, its international reach, and its use of standardized and validated measures, said Dr. Ong, who was not involved in the study.
“The effect of JAK inhibitors is more specific than traditional immunosuppressants such as cyclosporine and methotrexate but not as specific as biologics; therefore, long-term safety data are needed,” he advised. “16 weeks is a very short time to study a chronic disease like atopic dermatitis. We need safety data longer than 1 year.”
Given the disease’s potential impact on self-esteem, sleep, and other important areas of life, Sean Reynolds, MBBCH, a pediatric dermatologist at Children’s Mercy Kansas City (Mo.), welcomed the data on the newer pharmacologic agents.
“FDA-approved systemic treatment options for adolescents with AD are currently limited, which necessitates studies such as this that explore additional treatment options,” said Dr. Reynolds, who also was not involved in the study, told this news organization.
He added that oral upadacitinib may especially help patients who have not found relief with other topical or systemic treatments or who are needle phobic. While the overall efficacy and relatively mild side effects for most patients taking upadacitinib in the trials are encouraging, “the long-term efficacy and side effects in this population require further study, especially considering the limited systemic AD treatment options available in this age group,” he added.
“Given the reported use of other JAK inhibitors to treat myriad inflammatory skin conditions beyond atopic dermatitis, the potential use of upadacitinib and other JAK inhibitors to treat these skin diseases in children and adolescents represents an exciting area for future study in the field of pediatric dermatology,” Dr. Reynolds noted.
The study was funded by AbbVie, the developer and manufacturer of upadacitinib. Dr. Paller and almost all other authors reported relevant financial relationships with AbbVie and other pharmaceutical companies. Dr. Ong reported serving on an AbbVie advisory board, and Dr. Reynolds reported no conflict of interest with the study.
FROM JAMA DERMATOLOGY
How safe is the blackout rage gallon drinking trend?
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
This discussion was recorded on April 6, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining us today is Dr. Lewis Nelson, professor and chair of emergency medicine at Rutgers New Jersey Medical School and a certified medical toxicologist.
Today, we will be discussing an important and disturbing Gen Z trend circulating on social media, known as blackout rage gallon, or BORG.
Welcome, Lewis.
Lewis S. Nelson, MD: Thanks for having me.
Dr. Glatter: Thanks so much for joining us. This trend that’s been circulating on social media is really disturbing. It has elements that focus on binge drinking: Talking about taking a jug; emptying half of it out; and putting one fifth of vodka and some electrolytes, caffeine, or other things too is just incredibly disturbing. Teens and parents are looking at this. I’ll let you jump into the discussion.
Dr. Nelson: You’re totally right, it is disturbing. Binge drinking is a huge problem in this country in general. It’s a particular problem with young people – teenagers and young adults. I don’t think people appreciate the dangers associated with binge drinking, such as the amount of alcohol they consume and some of the unintended consequences of doing that.
To frame things quickly, we think there are probably around six people a day in the United States who die of alcohol poisoning. Alcohol poisoning basically is binge drinking to such an extent that you die of the alcohol itself. You’re not dying of a car crash or doing something that injures you. You’re dying of the alcohol. You’re drinking so much that your breathing slows, it stops, you have heart rhythm disturbances, and so on. It totals about 2,200 people a year in the United States.
Dr. Glatter: That’s alarming. For this trend, their argument is that half of the gallon is water. Therefore, I’m fine. I can drink it over 8-12 hours and it’s not an issue. How would you respond to that?
Dr. Nelson: Well, alcohol is alcohol. It’s all about how much you take in over what time period. I guess, in concept, it could be safer if you do it right. That’s not the way it’s been, so to speak, marketed on the various social media platforms. It’s meant to be a way to protect yourself from having your drink spiked or eating or ingesting contaminants from other people’s mouths when you share glasses or dip cups into communal pots like jungle juice or something.
Clearly, if you’re going to drink a large amount of alcohol over a short or long period of time, you do run the risk of having significant consequences, including bad decision-making if you’re just a little drunk all the way down to that of the complications you described about alcohol poisoning.
Dr. Glatter: There has been a comment made that this could be a form of harm reduction. The point of harm reduction is that we run trials, we validate it, and we test it. This, certainly in my mind, is no form of true harm reduction. I think you would agree.
Dr. Nelson: Many things that are marketed as harm reduction aren’t. There could be some aspects of this that could be considered harm reduction. You may believe – and there’s no reason not to – that protecting your drink is a good idea. If you’re at a bar and you leave your glass open and somebody put something in it, you can be drugged. Drug-facilitated sexual assault, for example, is a big issue. That means you have to leave your glass unattended. If you tend to your glass, it’s probably fine. One of the ways of harm reduction they mention is that by having a cap and having this bottle with you at all times, that can’t happen.
Now, in fairness, by far the drug most commonly associated with sexual assault is alcohol. It’s not gamma-hydroxybutyrate or ketamine. It’s not the other things that people are concerned about. Those happen, but those are small problems in the big picture. It’s drinking too much.
A form of harm reduction that you can comment on perhaps is that you make this drink concoction yourself, so you know what is in there. You can take that bottle, pour out half the water, and fill up the other half with water and nobody’s going to know. More likely, the way they say you should do it is you take your gallon jug, you pour it out, and you fill it up with one fifth of vodka.
One fifth of vodka is the same amount of volume as a bottle of wine. At 750 mL, that’s a huge amount of alcohol. If you measure the number of shots in that bottle, it’s about 17 shots. Even if you drink that over 6 hours, that’s still several shots an hour. That’s a large amount of alcohol. You might do two or three shots once and then not drink for a few hours. To sit and drink two or three shots an hour for 6 hours, that’s just an exceptional amount of alcohol.
They flavorize it and add caffeine, which only adds to the risk. It doesn’t make it in any way safer. With the volume, 1 gal of water or equivalent over a short period of time in and of itself could be a problem. There’s a large amount of mismessaging here. Whether something’s harm reduction, it could flip around to be easily construed or understood as being harmful.
Not to mention, the idea that when you make something safer, one of the unintended consequences of harm reduction is what we call risk compensation. This is best probably described as what’s called the Peltzman effect. The way that we think about airbags and seatbelts is that they’re going to reduce car crash deaths; and they do, but people drive faster and more recklessly because they know they’re safe.
This is a well-described problem in epidemiology: You expect a certain amount of harm reduction through some implemented process, but you don’t meet that because people take increased risks.
Dr. Glatter: Right. The idea of not developing a hangover is common among many teens and 20-somethings, thinking that because there’s hydration there, because half of it is water, it’s just not going to happen. There’s your “harm reduction,” but your judgment’s impaired. It’s day drinking at its best, all day long. Then someone has the idea to get behind the wheel. These are the disastrous consequences that we all fear.
Dr. Nelson: There is a great example, perhaps of an unintended consequence of harm reduction. By putting caffeine in it, depending on how much caffeine you put in, some of these mixtures can have up to 1,000 mg of caffeine. Remember, a cup of coffee is about 1-200 mg, so you’re talking about several cups of coffee. The idea is that you will not be able to sense, as you normally do, how drunk you are. You’re not going to be a sleepy drunk, you’re going to be an awake drunk.
The idea that you’re going to have to drive so you’re going to drink a strong cup of black coffee before you go driving, you’re not going to drive any better. I can assure you that. You’re going to be more awake, perhaps, and not fall asleep at the wheel, but you’re still going to have psychomotor impairment. Your judgment is going to be impaired. There’s nothing good that comes with adding caffeine except that you’re going to be awake.
From a hangover perspective, there are many things that we’ve guessed at or suggested as either prevention or cures for hangovers. I don’t doubt that you’re going to have some volume depletion if you drink a large amount of alcohol. Alcohol’s a diuretic, so you’re going to lose more volume than you bring in.
Hydrating is probably always a good idea, but there is hydrating and then there’s overhydrating. We don’t need volumes like that. If you drink a cup or two of water, you’re probably fine. You don’t need to drink half a gallon of water. That can lead to problems like delusional hyponatremia, and so forth. There’s not any clear benefit to doing it.
If you want to prevent a hangover, one of the ways you might do it is by using vodka. There are nice data that show that clear alcohols typically, particularly vodka, don’t have many of the congeners that make the specific forms of alcohol what they are. Bourbon smells and tastes like bourbon because of these little molecules, these alkalis and ketones and amino acids and things that make it taste and smell the way it does. That’s true for all the other alcohols.
Vodka has the least amount of that. Even wine and beer have those in them, but vodka is basically alcohol mixed with water. It’s probably the least hangover-prone of all the alcohols; but still, if you drink a lot of vodka, you’re going to have a hangover. It’s just a dose-response curve to how much alcohol you drink, to how drunk you get, and to how much of a hangover you’re going to have.
Dr. Glatter: The hangover is really what it’s about because people want to be functional the next day. There are many companies out there that market hangover remedies, but people are using this as the hangover remedy in a way that’s socially accepted. That’s a good point you make.
The question is how do we get the message out to parents and teens? What’s the best way you feel to really sound the alarm here?
Dr. Nelson: These are challenging issues. We face this all the time with all the sorts of social media in particular. Most parents are not as savvy on social media as their kids are. You have to know what your children are doing. You should know what they’re listening to and watching. You do have to pay attention to the media directed at parents that will inform you a little bit about what your kids are doing. You have to talk with your kids and make sure they understand what it is that they’re doing.
We do this with our kids for some things. Hopefully, we talk about drinking, smoking, sex, and other things with our children (like driving if they get to that stage) and make sure they understand what the risks are and how to mitigate those risks. Being an attentive parent is part of it.
Sometimes you need outside messengers to do it. We’d like to believe that these social media companies are able to police themselves – at least they pay lip service to the fact they do. They have warnings that they’ll take things down that aren’t socially appropriate. Whether they do or not, I don’t know, because you keep seeing things about BORG on these media sites. If they are doing it, they’re not doing it efficiently or quickly enough.
Dr. Glatter: There has to be some censorship. These are young persons who are impressionable, who have developing brains, who are looking at this, thinking that if it’s out there on social media, such as TikTok or Instagram, then it’s okay to do so. That message has to be driven home.
Dr. Nelson: That’s a great point, and it’s tough. We know there’s been debate over the liability of social media or what they post, and whether or not they should be held liable like a more conventional media company or not. That’s politics and philosophy, and we’re probably not going to solve it here.
All these things wind up going viral and there’s probably got to be some filter on things that go viral. Maybe they need to have a bit more attentiveness to that when those things start happening. Now, clearly not every one of these is viral. When you think about some of the challenges we’ve seen in the past, such as the Tide Pod challenge and cinnamon challenge, some of these things could be quickly figured out to be dangerous.
I remember that the ice bucket challenge for amyotrophic lateral sclerosis was pretty benign. You pour a bucket of water over your head, and people aren’t really getting hurt. That’s fun and good, and let people go out and do that. That could pass through the filter. When you start to see people drinking excessive amounts of alcohol, it doesn’t take an emergency physician to know that’s not a good thing. Any parent should know that if my kid drinks half a bottle or a bottle of vodka over a short period of time, that just can’t be okay.
Dr. Glatter: It’s a public health issue. That’s what we need to elevate it to because ultimately that’s what it impacts: welfare and safety.
Speaking of buckets, there’s a new bucket challenge, wherein unsuspecting people have a bucket put on their head, can’t breathe, and then pass out. There’s been a number of these reported and actually filmed on social media. Here’s another example of dangerous types of behavior that essentially are a form of assault. Unsuspecting people suffer injuries from young children and teens trying to play pranks.
Again, had there not been this medium, we wouldn’t necessarily see the extent of the injuries. I guess going forward, the next step would be to send a message to colleges that there should be some form of warning if this trend is seen, at least from a public health standpoint.
Dr. Nelson: Education is a necessary thing to do, but it’s almost never the real solution to a problem. We can educate people as best we can that they need to do things right. At some point, we’re going to need to regulate it or manage it somehow.
Whether it’s through a carrot or a stick approach, or whether you want to give people kudos for doing the right thing or punish them for doing something wrong, that’s a tough decision to make and one that is going to be made by a parent or guardian, a school official, or law enforcement. Somehow, we have to figure out how to make this happen.
There’s not going to be a single size that fits all for this. At some level, we have to do something to educate and regulate. The balance between those two things is going to be political and philosophical in nature.
Dr. Glatter: Right, and the element of peer pressure and conformity in this is really part of the element. If we try to remove that aspect of it, then often these trends would go away. That aspect of conformity and peer pressure is instrumental in fueling these trends. Maybe we can make a full gallon of water be the trend without any alcohol in there.
Dr. Nelson: We say water is only water, but as a medical toxicologist, I can tell you that one of the foundations in medical toxicology is that everything is toxic. It’s just the dose that determines the toxicity. Oxygen is toxic, water is toxic. Everything’s toxic if you take enough of it.
We know that whether it’s psychogenic or intentional, polydipsia by drinking excessive amounts of water, especially without electrolytes, is one of the reasons they say you should add electrolytes. That’s all relative as well, because depending on the electrolyte and how much you put in and things like that, that could also become dangerous. Drinking excessive amounts of water like they’re suggesting, which sounds like a good thing to prevent hangover and so on, can in and of itself be a problem too.
Dr. Glatter: Right, and we know that there’s no magic bullet for a hangover. Obviously, abstinence is the only thing that truly works.
Dr. Nelson: Or moderation.
Dr. Glatter: Until research proves further.
Thank you so much. You’ve made some really important points. Thank you for talking about the BORG phenomenon, how it relates to society in general, and what we can do to try to change people’s perception of alcohol and the bigger picture of binge drinking. I really appreciate it.
Dr. Nelson: Thanks, Rob, for having me. It’s an important topic and hopefully we can get a handle on this. I appreciate your time.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y. Dr. Nelson is professor and chair of the department of emergency medicine and chief of the division of medical toxicology at Rutgers New Jersey Medical School, Newark. He is a member of the board of directors of the American Board of Emergency Medicine, the Accreditation Council for Continuing Medical Education, and Association of Academic Chairs in Emergency Medicine and is past-president of the American College of Medical Toxicology. Dr. Glatter and Dr. Nelson disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Steep rise in cannabis-related suicide attempts
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
A baby stops breathing at a grocery store – An ICU nurse steps in
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
My son needed a physical for his football team, and we couldn’t get an appointment. So, we went to the urgent care next to the H Mart in Cary, N.C. While I was waiting, I thought, let me go get a coffee or an iced tea at the H Mart. They have this French bakery in there.
I went in and ordered my drink, and I was waiting in line. I saw this woman pass me running with a baby. Another woman – I found out later it was her sister – was running after her, and she said: “Call 911!”
“I don’t have my phone,” I said. I left my phone with my son; he was using it.
I said: “Are you okay?” And she just handed me the baby. The baby was gray, and there was blood in her nose and mouth. The woman said: “She’s my baby. She’s 1 week old.”
I was trying to think very quickly. I didn’t see any bubbles in the blood around the baby’s nose or mouth to tell me if she was breathing. She was just limp. The mom was still screaming, but I couldn’t even hear her anymore. It was like I was having an out-of-body experience. All I could hear were my thoughts: “I need to put this baby down to start CPR. Someone was calling 911. I should go in the front of the store to save time, so EMS doesn’t have to look for me when they come.”
I started moving and trying to clean the blood from the baby’s face with her blanket. At the front of the store, I saw a display of rice bags. I put the baby on top of one of the bags. “Okay, where do I check for a pulse on a baby?” I took care of adults, never pediatric patients, never babies. She was so tiny. I put my hand on her chest and felt nothing. No heartbeat. She still wasn’t breathing.
People were around me, but I couldn’t see or hear anybody. All I was thinking was: “What can I do for this patient right now?” I started CPR with two fingers. Nothing was happening. It wasn’t that long, but it felt like forever for me. I couldn’t do mouth-to-mouth because there was so much blood on her face. I still don’t know what caused the bleeding.
It was COVID time, so I had my mask on. I was, like: “You know what? Screw this. She’s a 1-week-old baby. Her lungs are tiny. Maybe I don’t have to do mouth-to-mouth. I can just blow in her mouth.” I took off my mask and opened her mouth. I took a deep breath and blew a little bit of air in her mouth. I continued CPR for maybe 5 or 10 seconds.
And then she gasped! She opened her eyes, but they were rolled up. I was still doing CPR, and maybe 2 second after that, I could feel under my hand a very rapid heart rate. I took my hand away and lifted her up.
Just then the EMS got there. I gave them the baby and said: “I did CPR. I don’t know how long it lasted.” The EMS person looked at me, said: “Thank you for what you did. Now we need you to help us with mom.” I said, “okay.”
I turned around, and the mom was still screaming and crying. I asked one of the ladies that worked there, “Can you get me water?” She brought it, and I gave some to the mom, and she started talking to EMS.
People were asking me: “What happened? What happened?” It’s funny, I guess the nurse in me didn’t want to give out information. And I didn’t want to ask for information. I was thinking about privacy. I said, “I don’t know,” and walked away.
The mom’s sister came and hugged me and said thank you. I was still in this out-of-body zone, and I just wanted to get the hell out of there. So, I left. I went to my car and when I got in it, I started shaking and sweating and crying.
I had been so calm in the moment, not thinking about if the baby was going to survive or not. I didn’t know how long she was without oxygen, if she would have some anoxic brain injury or stroke. I’m a mom, too. I would have been just as terrified as that mom. I just hoped there was a chance that she could take her baby home.
I went back to the urgent care, and my son was, like, “are you okay?” I said: “You will not believe this. I just did CPR on a baby.” He said: “Oh. Okay.” I don’t think he even knew what that meant.
I’ve been an ICU nurse since 2008. I’ve been in very critical moments with patients, life or death situations. I help save people all the time at the hospital. Most of the time, you know what you’re getting. You can prepare. You have everything you need, and everyone knows what to do. You know what the worst will look like. You know the outcome.
But this was something else. You read about things like this. You hear about them. But you never think it’ll happen to you – until it happens.
I couldn’t stop thinking about the baby. So, 2 days later, I posted on Next Door to see if somebody would read it and say, “hey, the baby survived.” I was amazed at how many people responded, but no one knew the family.
The local news got hold of me and asked me to do a story. I told them, “the only way I can do a story is if the baby survived. I’m not going to do a story about a dead baby, and the mom has to live through it again.”
The reporter called me later on that day and said she had talked to the police. They said the family was visiting from out of state. The baby went to the hospital and was discharged home 2 days later. I said, “okay, then I can talk.”
When the news story came out, I started getting texts from people at work the same night. So many people were reaching out. Even people from out of state. But I never heard from the family. No one knew how to reach them.
Since I was very young, I wanted to work in a hospital, to help people. It really brings me joy, seeing somebody go home, knowing, yes, we did this. It’s a great feeling. I love this job. I wouldn’t trade it for anything.
I just wish I had asked the mom’s name. Because I always think about that baby. I always wonder, what did she become? I hope somebody reads this who might know that little girl. It would be so nice to meet her one day.
Ms. Diallo is an ICU nurse and now works as nurse care coordinator at the University of North Carolina’s Children’s Neurology Clinic in Chapel Hill.
A version of this article first appeared on Medscape.com.
PARP/ATR inhibitor combo shows hints of promise in children with tumors
The small phase 1 trial also identified some molecular signatures in responders that may inform future clinical trials.
The results, presented at the annual meeting of the American Association of Cancer Research, came from a single arm of the European Proof-of-Concept Therapeutic Stratification Trial of Molecular Anomalies in Relapsed or Refractory Tumors (ESMART) trial. This trial matches pediatric, adolescent, and young adult cancer patients with treatment regimens based on the molecular profile of their tumors.
In over 220 children to date, the trial has investigated 15 different treatment regimens, most of which are combination therapies.
In adults, PARP) inhibitors have been shown to be effective in tumors with deficiencies in homologous repair, which is a DNA repair mechanism, with notable successes in patients carrying the BRCA1 and BRCA2 mutations. But BRCA1 and BRCA2 mutations are rare in pediatric cancer, and there is a belief that there may be primary resistance to PARP inhibitors in pediatric tumors, according to Susanne Gatz, MD, PhD, who presented the research at the meeting.
Previous research identified alterations in pediatric tumors that are candidates for patient selection. “These tumors have alterations which could potentially cause this resistance effect [against PARP inhibitors] and [also cause] sensitivity to ataxia telangiectasia–mutated Rad3-related inhibitors. This is how this arm [of the ESMART trial] was born,” said Dr. Gatz.
The phase 1 portion of the study included 18 pediatric and young adult patients with relapsed or treatment-refractory tumors. There were eight sarcomas, five central nervous system tumors, four neuroblastomas, and one carcinoma. Each had mutations thought to lead to HR deficiency or replication stress. The study included three dose levels of twice-daily oral olaparib that was given continuously, and ceralasertib, which was given day 1-14 of each 28-day cycle.
Patients underwent a median of 3.5 cycles of treatment. There were dose-limiting adverse events of thrombocytopenia and neutropenia in five patients, two of which occurred at the dose that was recommended for phase 2.
There were some positive clinical signs, including one partial response in a pineoblastoma patient who received treatment for 11 cycles. A neuroblastoma patient had stable disease until cycle 9 of treatment, and then converted to a partial response and is currently in cycle 12. Two other patients remain in treatment at cycle 8 and one is in treatment at cycle 15. None of the patients who experienced clinical benefit had BRCA mutations.
An important goal of the study was to understand molecular signature that might predict response to the drug combination. Although no firm conclusions could be drawn, there were some interesting patterns. In particular, five of the six worst responders had TP53 mutations. “It is striking ... so we need to learn what TP53 in this setting means if it’s mutated, and if it could be a resistance factor,” said Dr. Gatz, an associate clinical professor in pediatric oncology at the Institute of Cancer and Genomic Sciences of the University of Birmingham, during her talk.
Although the study is too small and included too many tumor types to identify tumor-based patterns of response, it did provide some hints as to biomarkers that could inform future studies, according to Julia Glade Bender, MD, who served as a discussant following the presentation and is a pediatric oncologist at Memorial Sloan Kettering Cancer Center, New York.
“The pediatric frequency of the common DNA damage repair biomarkers that have been [identified in] the adult literature – that is to say, BRCA1 and 2 and [ataxia-telangiectasia mutation] – are exceedingly rare in pediatrics,” said Dr. Bender during the session while serving as a discussant. She highlighted the following findings: Loss of the 11q region on chromosome 11 is common among the patients and that region contains three genes involved in the DNA damage response, along with a gene involved in homologous recombination, telomere maintenance, and double strand break repair.
She added that 11q deletion is also found in up to 40% of neuroblastomas, and is associated with poor prognosis, and the patients have multiple segmental chromosomal abnormalities. “That begs the question [of] whether chromosomal instability is another biomarker for pediatric cancer,” said Dr. Bender.
“The research highlights the complexity of pediatric cancers, whose distinct biology could make them more vulnerable to ATR [kinase], [checkpoint kinase 1], and WEE1 pathway inhibition with a PARP inhibitor used to induce replication stress and be the sensitizer. The biomarker profiles are going to be complex, context-dependent, and likely to reflect a constellation of findings that would be signatures or algorithms, rather than single gene alterations. The post hoc iterative analysis of responders and nonresponders is going to be absolutely critical to understanding those biomarkers and the role of DNA damage response inhibitors in pediatrics. Given the rarity of these diagnoses, and then the molecular subclasses, I think collaboration across ages and geography is absolutely critical, and I really congratulate the ESMART consortium for doing just that in Europe,” said Dr. Bender.
The study is limited by its small sample size and the fact that it was not randomized.
The study received funding from French Institut National de Cancer, Imagine for Margo, Fondation ARC, AstraZeneca France, AstraZeneca Global R&D, AstraZeneca UK, Cancer Research UK, Fondation Gustave Roussy, and Little Princess Trust/Children’s Cancer and Leukaemia Group. Dr. Gatz has no relevant financial disclosures. Dr. Bender has done paid consulting for Jazz Pharmaceuticals and has done unpaid work for Bristol-Myers Squibb, Eisai, Springworks Therapeutics, Merck Sharp & Dohme, and Pfizer. She has received research support from Eli Lilly, Loxo-oncology, Eisai, Cellectar, Bayer, Amgen, and Jazz Pharmaceuticals.
From American Association for Cancer Research (AACR) Annual Meeting 2023: Abstract CT019. Presented Tuesday, April 18.
The small phase 1 trial also identified some molecular signatures in responders that may inform future clinical trials.
The results, presented at the annual meeting of the American Association of Cancer Research, came from a single arm of the European Proof-of-Concept Therapeutic Stratification Trial of Molecular Anomalies in Relapsed or Refractory Tumors (ESMART) trial. This trial matches pediatric, adolescent, and young adult cancer patients with treatment regimens based on the molecular profile of their tumors.
In over 220 children to date, the trial has investigated 15 different treatment regimens, most of which are combination therapies.
In adults, PARP) inhibitors have been shown to be effective in tumors with deficiencies in homologous repair, which is a DNA repair mechanism, with notable successes in patients carrying the BRCA1 and BRCA2 mutations. But BRCA1 and BRCA2 mutations are rare in pediatric cancer, and there is a belief that there may be primary resistance to PARP inhibitors in pediatric tumors, according to Susanne Gatz, MD, PhD, who presented the research at the meeting.
Previous research identified alterations in pediatric tumors that are candidates for patient selection. “These tumors have alterations which could potentially cause this resistance effect [against PARP inhibitors] and [also cause] sensitivity to ataxia telangiectasia–mutated Rad3-related inhibitors. This is how this arm [of the ESMART trial] was born,” said Dr. Gatz.
The phase 1 portion of the study included 18 pediatric and young adult patients with relapsed or treatment-refractory tumors. There were eight sarcomas, five central nervous system tumors, four neuroblastomas, and one carcinoma. Each had mutations thought to lead to HR deficiency or replication stress. The study included three dose levels of twice-daily oral olaparib that was given continuously, and ceralasertib, which was given day 1-14 of each 28-day cycle.
Patients underwent a median of 3.5 cycles of treatment. There were dose-limiting adverse events of thrombocytopenia and neutropenia in five patients, two of which occurred at the dose that was recommended for phase 2.
There were some positive clinical signs, including one partial response in a pineoblastoma patient who received treatment for 11 cycles. A neuroblastoma patient had stable disease until cycle 9 of treatment, and then converted to a partial response and is currently in cycle 12. Two other patients remain in treatment at cycle 8 and one is in treatment at cycle 15. None of the patients who experienced clinical benefit had BRCA mutations.
An important goal of the study was to understand molecular signature that might predict response to the drug combination. Although no firm conclusions could be drawn, there were some interesting patterns. In particular, five of the six worst responders had TP53 mutations. “It is striking ... so we need to learn what TP53 in this setting means if it’s mutated, and if it could be a resistance factor,” said Dr. Gatz, an associate clinical professor in pediatric oncology at the Institute of Cancer and Genomic Sciences of the University of Birmingham, during her talk.
Although the study is too small and included too many tumor types to identify tumor-based patterns of response, it did provide some hints as to biomarkers that could inform future studies, according to Julia Glade Bender, MD, who served as a discussant following the presentation and is a pediatric oncologist at Memorial Sloan Kettering Cancer Center, New York.
“The pediatric frequency of the common DNA damage repair biomarkers that have been [identified in] the adult literature – that is to say, BRCA1 and 2 and [ataxia-telangiectasia mutation] – are exceedingly rare in pediatrics,” said Dr. Bender during the session while serving as a discussant. She highlighted the following findings: Loss of the 11q region on chromosome 11 is common among the patients and that region contains three genes involved in the DNA damage response, along with a gene involved in homologous recombination, telomere maintenance, and double strand break repair.
She added that 11q deletion is also found in up to 40% of neuroblastomas, and is associated with poor prognosis, and the patients have multiple segmental chromosomal abnormalities. “That begs the question [of] whether chromosomal instability is another biomarker for pediatric cancer,” said Dr. Bender.
“The research highlights the complexity of pediatric cancers, whose distinct biology could make them more vulnerable to ATR [kinase], [checkpoint kinase 1], and WEE1 pathway inhibition with a PARP inhibitor used to induce replication stress and be the sensitizer. The biomarker profiles are going to be complex, context-dependent, and likely to reflect a constellation of findings that would be signatures or algorithms, rather than single gene alterations. The post hoc iterative analysis of responders and nonresponders is going to be absolutely critical to understanding those biomarkers and the role of DNA damage response inhibitors in pediatrics. Given the rarity of these diagnoses, and then the molecular subclasses, I think collaboration across ages and geography is absolutely critical, and I really congratulate the ESMART consortium for doing just that in Europe,” said Dr. Bender.
The study is limited by its small sample size and the fact that it was not randomized.
The study received funding from French Institut National de Cancer, Imagine for Margo, Fondation ARC, AstraZeneca France, AstraZeneca Global R&D, AstraZeneca UK, Cancer Research UK, Fondation Gustave Roussy, and Little Princess Trust/Children’s Cancer and Leukaemia Group. Dr. Gatz has no relevant financial disclosures. Dr. Bender has done paid consulting for Jazz Pharmaceuticals and has done unpaid work for Bristol-Myers Squibb, Eisai, Springworks Therapeutics, Merck Sharp & Dohme, and Pfizer. She has received research support from Eli Lilly, Loxo-oncology, Eisai, Cellectar, Bayer, Amgen, and Jazz Pharmaceuticals.
From American Association for Cancer Research (AACR) Annual Meeting 2023: Abstract CT019. Presented Tuesday, April 18.
The small phase 1 trial also identified some molecular signatures in responders that may inform future clinical trials.
The results, presented at the annual meeting of the American Association of Cancer Research, came from a single arm of the European Proof-of-Concept Therapeutic Stratification Trial of Molecular Anomalies in Relapsed or Refractory Tumors (ESMART) trial. This trial matches pediatric, adolescent, and young adult cancer patients with treatment regimens based on the molecular profile of their tumors.
In over 220 children to date, the trial has investigated 15 different treatment regimens, most of which are combination therapies.
In adults, PARP) inhibitors have been shown to be effective in tumors with deficiencies in homologous repair, which is a DNA repair mechanism, with notable successes in patients carrying the BRCA1 and BRCA2 mutations. But BRCA1 and BRCA2 mutations are rare in pediatric cancer, and there is a belief that there may be primary resistance to PARP inhibitors in pediatric tumors, according to Susanne Gatz, MD, PhD, who presented the research at the meeting.
Previous research identified alterations in pediatric tumors that are candidates for patient selection. “These tumors have alterations which could potentially cause this resistance effect [against PARP inhibitors] and [also cause] sensitivity to ataxia telangiectasia–mutated Rad3-related inhibitors. This is how this arm [of the ESMART trial] was born,” said Dr. Gatz.
The phase 1 portion of the study included 18 pediatric and young adult patients with relapsed or treatment-refractory tumors. There were eight sarcomas, five central nervous system tumors, four neuroblastomas, and one carcinoma. Each had mutations thought to lead to HR deficiency or replication stress. The study included three dose levels of twice-daily oral olaparib that was given continuously, and ceralasertib, which was given day 1-14 of each 28-day cycle.
Patients underwent a median of 3.5 cycles of treatment. There were dose-limiting adverse events of thrombocytopenia and neutropenia in five patients, two of which occurred at the dose that was recommended for phase 2.
There were some positive clinical signs, including one partial response in a pineoblastoma patient who received treatment for 11 cycles. A neuroblastoma patient had stable disease until cycle 9 of treatment, and then converted to a partial response and is currently in cycle 12. Two other patients remain in treatment at cycle 8 and one is in treatment at cycle 15. None of the patients who experienced clinical benefit had BRCA mutations.
An important goal of the study was to understand molecular signature that might predict response to the drug combination. Although no firm conclusions could be drawn, there were some interesting patterns. In particular, five of the six worst responders had TP53 mutations. “It is striking ... so we need to learn what TP53 in this setting means if it’s mutated, and if it could be a resistance factor,” said Dr. Gatz, an associate clinical professor in pediatric oncology at the Institute of Cancer and Genomic Sciences of the University of Birmingham, during her talk.
Although the study is too small and included too many tumor types to identify tumor-based patterns of response, it did provide some hints as to biomarkers that could inform future studies, according to Julia Glade Bender, MD, who served as a discussant following the presentation and is a pediatric oncologist at Memorial Sloan Kettering Cancer Center, New York.
“The pediatric frequency of the common DNA damage repair biomarkers that have been [identified in] the adult literature – that is to say, BRCA1 and 2 and [ataxia-telangiectasia mutation] – are exceedingly rare in pediatrics,” said Dr. Bender during the session while serving as a discussant. She highlighted the following findings: Loss of the 11q region on chromosome 11 is common among the patients and that region contains three genes involved in the DNA damage response, along with a gene involved in homologous recombination, telomere maintenance, and double strand break repair.
She added that 11q deletion is also found in up to 40% of neuroblastomas, and is associated with poor prognosis, and the patients have multiple segmental chromosomal abnormalities. “That begs the question [of] whether chromosomal instability is another biomarker for pediatric cancer,” said Dr. Bender.
“The research highlights the complexity of pediatric cancers, whose distinct biology could make them more vulnerable to ATR [kinase], [checkpoint kinase 1], and WEE1 pathway inhibition with a PARP inhibitor used to induce replication stress and be the sensitizer. The biomarker profiles are going to be complex, context-dependent, and likely to reflect a constellation of findings that would be signatures or algorithms, rather than single gene alterations. The post hoc iterative analysis of responders and nonresponders is going to be absolutely critical to understanding those biomarkers and the role of DNA damage response inhibitors in pediatrics. Given the rarity of these diagnoses, and then the molecular subclasses, I think collaboration across ages and geography is absolutely critical, and I really congratulate the ESMART consortium for doing just that in Europe,” said Dr. Bender.
The study is limited by its small sample size and the fact that it was not randomized.
The study received funding from French Institut National de Cancer, Imagine for Margo, Fondation ARC, AstraZeneca France, AstraZeneca Global R&D, AstraZeneca UK, Cancer Research UK, Fondation Gustave Roussy, and Little Princess Trust/Children’s Cancer and Leukaemia Group. Dr. Gatz has no relevant financial disclosures. Dr. Bender has done paid consulting for Jazz Pharmaceuticals and has done unpaid work for Bristol-Myers Squibb, Eisai, Springworks Therapeutics, Merck Sharp & Dohme, and Pfizer. She has received research support from Eli Lilly, Loxo-oncology, Eisai, Cellectar, Bayer, Amgen, and Jazz Pharmaceuticals.
From American Association for Cancer Research (AACR) Annual Meeting 2023: Abstract CT019. Presented Tuesday, April 18.
FROM AACR 2023
Rabies: How to respond to parents’ questions
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
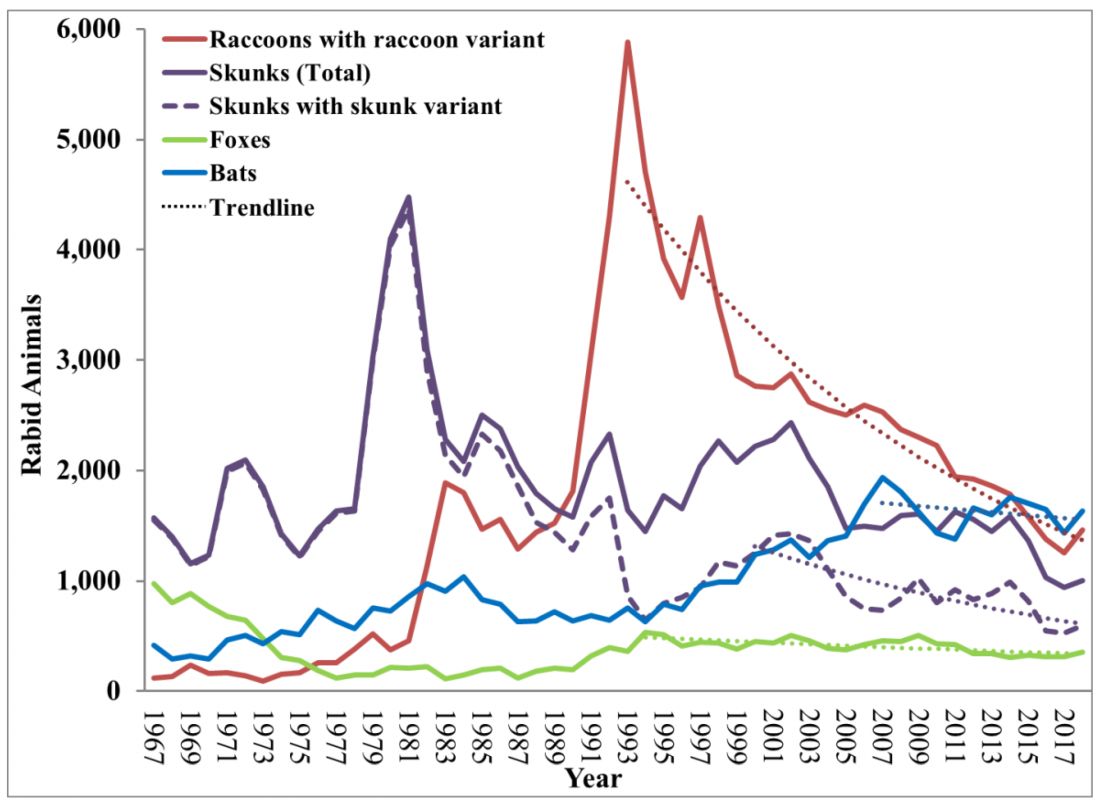
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
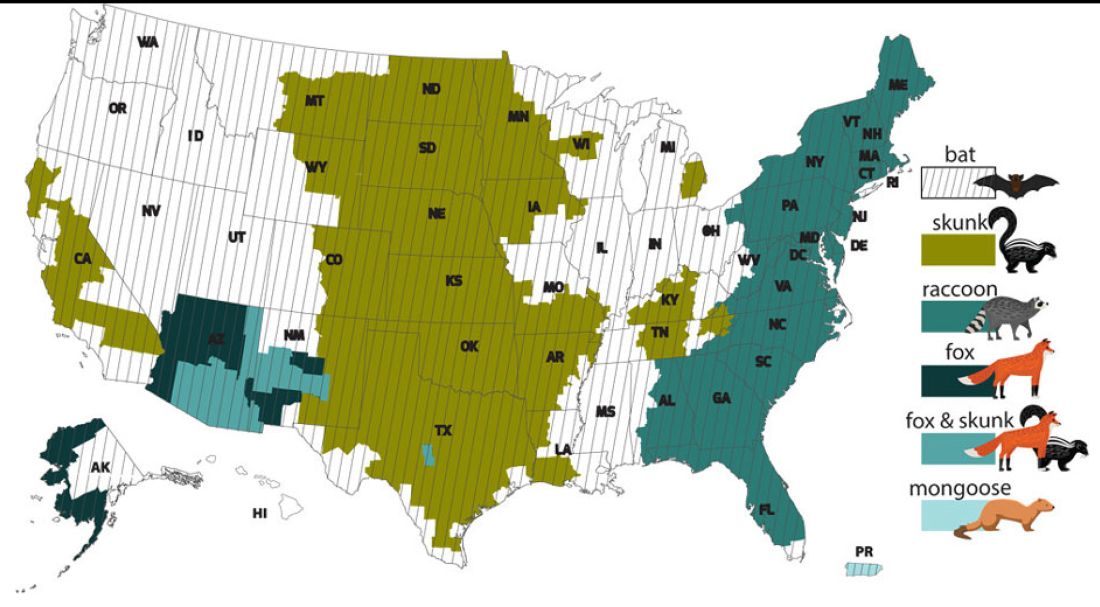
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
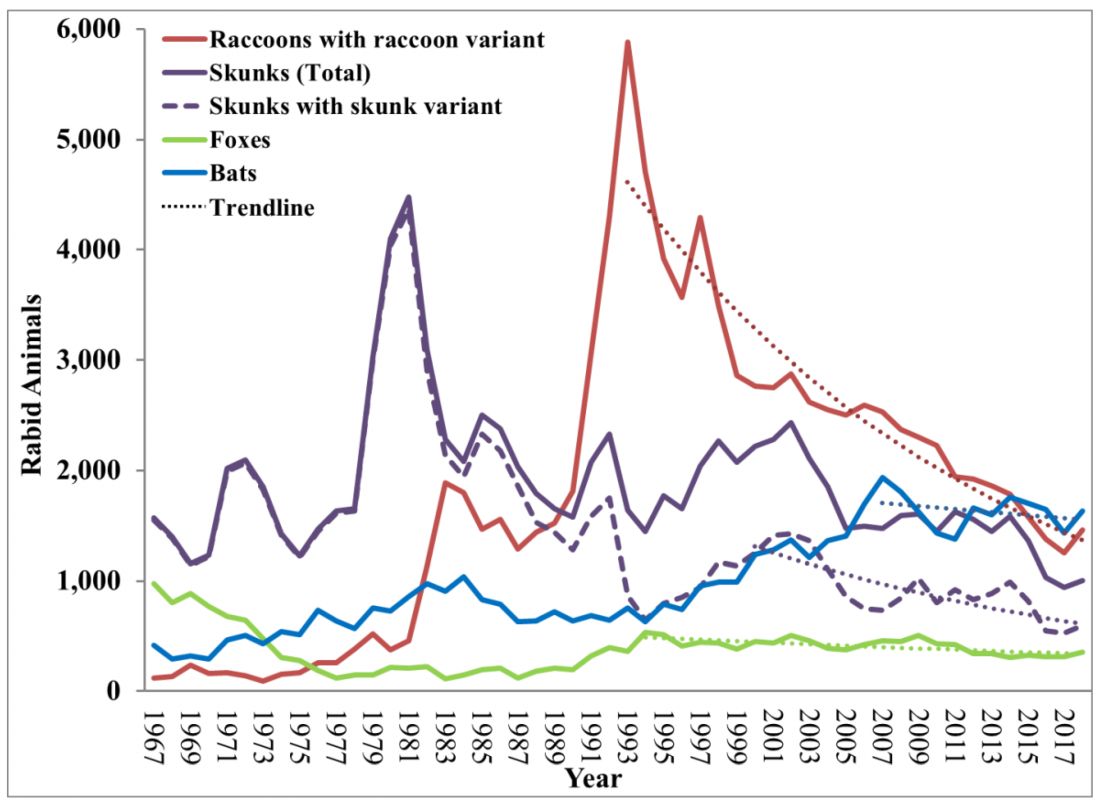
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
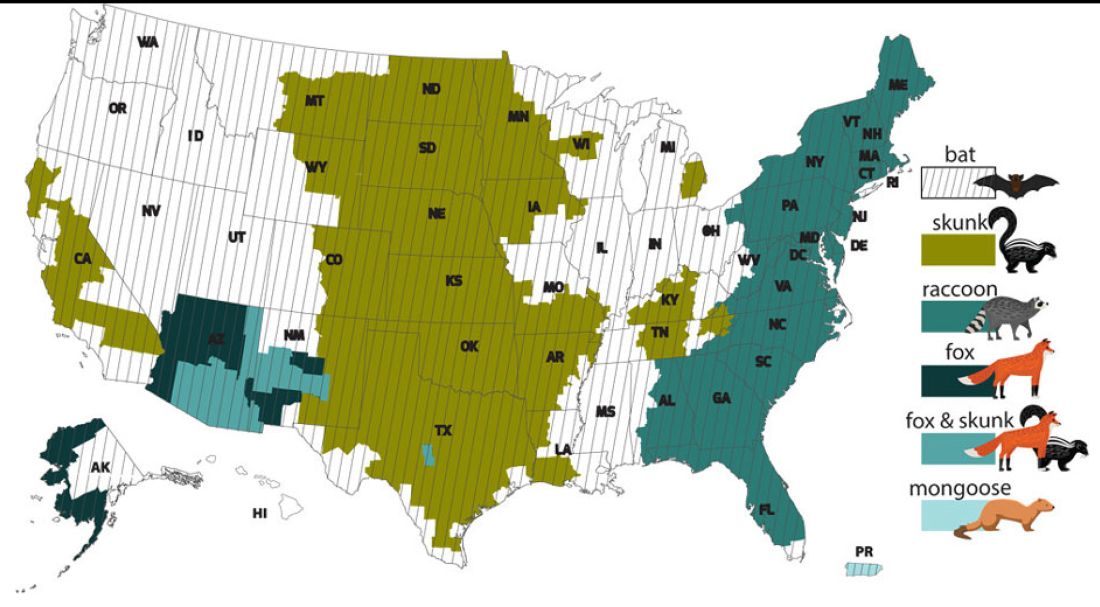
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
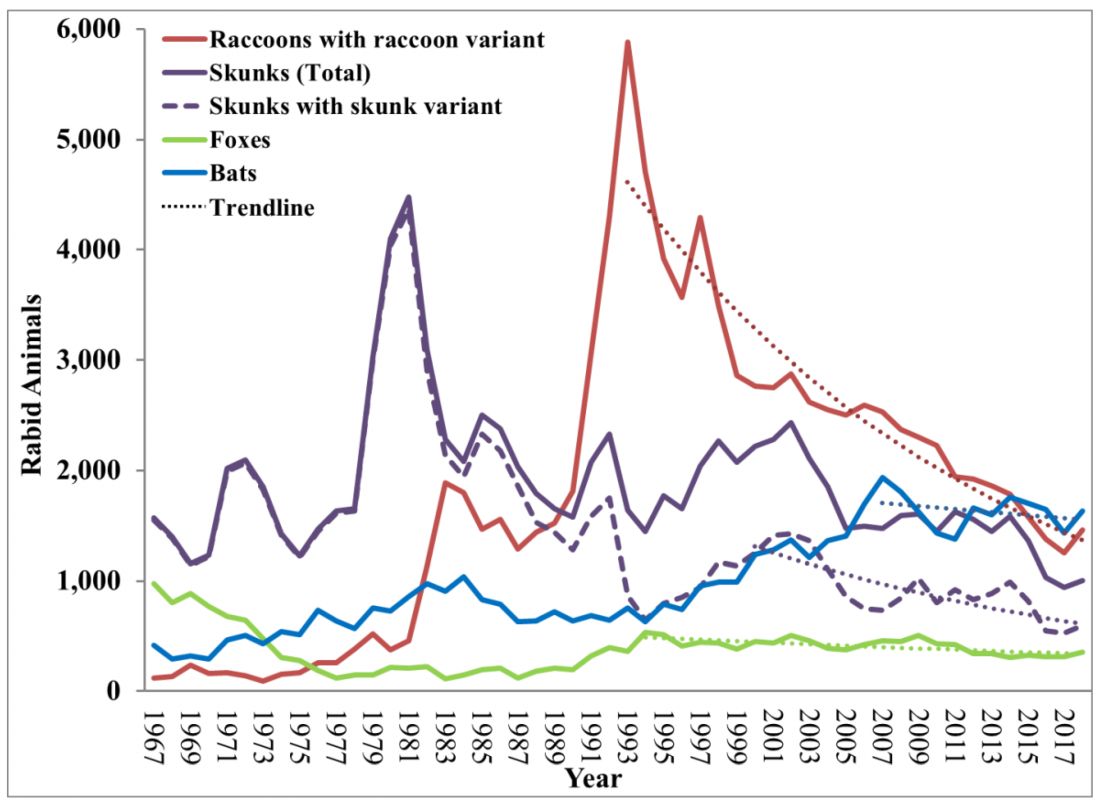
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
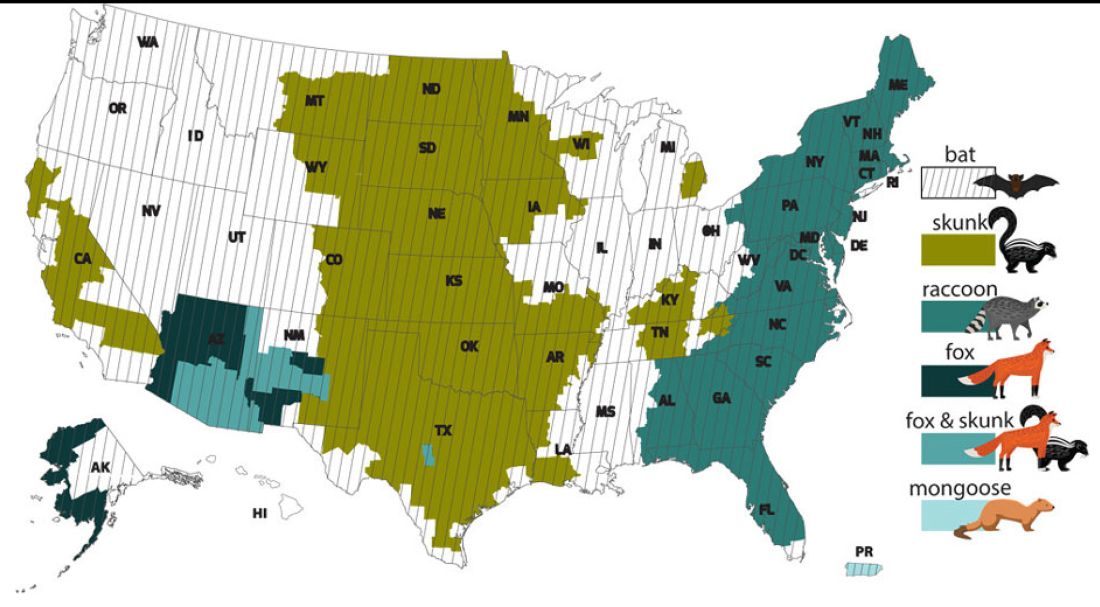
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
Most adults, more than one in three children take dietary supplements: Report
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
The new figures continue a 15-year trend of small, steady increases in how many people in the United States use the products that can deliver essential nutrients, but their usage includes a risk of getting more nutrients than recommended. In 2007, 48% of adults took supplements, and that figure has reached nearly 59% in this latest count.
The new report looked at whether people took a multivitamin, as well as other more specific supplements. Among children and adolescents aged 19 and under, 23.5% took a multivitamin, while 31.5% of adults reported taking one. The most common specialized supplement that people took was vitamin D.
The report, released by the CDC’s National Center for Health Statistics, compiled survey data from 2017 through 2020 in which 15,548 people reported their household’s usage of dietary supplements. Dietary supplements include vitamins, minerals, herbs, or other botanicals that are taken by mouth in pill, capsule, tablet, or liquid form. The researchers said the vitamin and supplement market is large and growing, totaling $55.7 billion in sales in 2020.
More than one-third of adults (36%) reported taking more than one supplement, and one in four people aged 60 and older said they took four or more.
The data showed demographic trends in who uses dietary supplements. Women and girls were more likely to take supplements than men and boys, although there were similar usage levels for both genders among 1- to 2-year-olds. People with higher education or income levels were more likely to use supplements. Asian people and White people were more likely to take supplements, compared with Hispanic people and Black people.
The authors wrote that monitoring trends in supplement use is important because the products “contribute substantially to nutrient intake as well as increase the risk of excessive intake of certain micronutrients.”
A version of this article originally appeared on WebMD.com.
Scattered Red-Brown, Centrally Violaceous, Blanching Papules on an Infant
The Diagnosis: Neonatal-Onset Multisystem Inflammatory Disorder (NOMID)
The punch biopsy demonstrated a predominantly deep but somewhat superficial, periadnexal, neutrophilic and eosinophilic infiltrate (Figure). The eruption resolved 3 days later with supportive treatment, including appropriate wound care. Genetic analysis revealed an autosomal-dominant NLR family pyrin domain containing 3 gene, NLRP3, de novo variant associated with neonatal-onset multisystem inflammatory disorder (NOMID). Additional workup to characterize our patient’s inflammatory profile revealed elevated IL-18, CD3, CD4, S100A12, and S100A8/A9 levels. On day 48 of life, she was started on anakinra, an IL-1 inhibitor, at a dose of 1 mg/kg subcutaneously, which eventually was titrated to 10 mg/kg at hospital discharge. Hearing screenings were within normal limits.
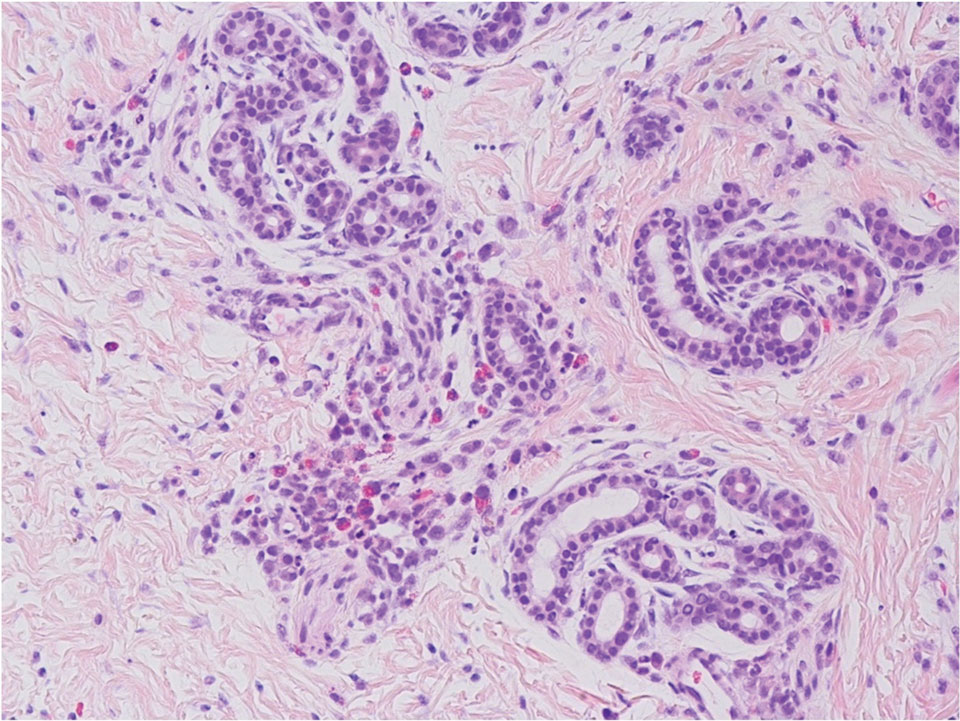
Cryopyrin-associated periodic syndromes (CAPS) consist of 3 rare, IL-1–associated, autoinflammatory disorders, including familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and NOMID (also known as chronic infantile neurologic cutaneous and articular syndrome). These conditions result from a sporadic or autosomal-dominant gain-of-function mutations in a single gene, NLRP3, on chromosome 1q44. NLRP3 encodes for cryopyrin, an important component of an IL-1 and IL-18 activating inflammasome.1 The most severe manifestation of CAPS is NOMID, which typically presents at birth as a migratory urticarial eruption, growth failure, myalgia, fever, and abnormal facial features, including frontal bossing, saddle-shaped nose, and protruding eyes.2 The illness also can manifest with hepatosplenomegaly, lymphadenopathy, uveitis, sensorineural hearing loss, cerebral atrophy, and other neurologic manifestations.3 A diagnosis of chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome was less likely given that our patient remained afebrile and did not show signs of lipodystrophy and persistent violaceous eyelid swelling. Both FCAS and MWS are less severe forms of CAPS when compared to NOMID. Familial cold autoinflammatory syndrome was less likely given the absence of the typical periodic fever pattern associated with the condition and severity of our patient’s symptoms. Muckle-Wells syndrome typically presents in adolescence with symptoms of FCAS, painful urticarial plaques, and progressive sensorinueral hearing loss. Tumor necrosis factor receptor–associated periodic fever (TRAPS) usually is associated with episodic fevers, abdominal pain, periorbital edema, migratory erythema, and arthralgia.1,3,4
Diagnostic criteria for CAPS include elevated inflammatory markers and serum amyloid, plus at least 2 of the typical CAPS symptoms: urticarial rash, cold-triggered episodes, sensorineural hearing loss, musculoskeletal symptoms, chronic aseptic meningitis, and skeletal abnormalities.4 The sensitivity and specificity of these diagnostic criteria are 84% and 91%, respectively. Additional findings that can be seen but are not part of the diagnostic criteria include intermittent fever, transient joint swelling, bony overgrowths, uveitis, optic disc edema, impaired growth, and hepatosplenomegaly.5 Laboratory findings may reveal leukocytosis, eosinophilia, anemia, and/or thrombocytopenia.3,5
Genetic testing, skin biopsies, ophthalmic examinations, neuroimaging, joint radiography, cerebrospinal fluid tests, and hearing examinations can be performed for confirmation of diagnosis and evaluation of systemic complications.4 A skin biopsy may reveal a neutrophilic infiltrate. Ophthalmic examination can demonstrate uveitis and optic disk edema. Neuroimaging may reveal cerebral atrophy or ventricular dilation. Lastly, joint radiography can be used to evaluate for the presence of premature long bone ossification or osseous overgrowth.4
In summary, NOMID is a multisystemic disorder with cutaneous manifestations. Early recognition of this entity is important given the severe sequelae and available efficacious therapy. Dermatologists should be aware of these manifestations, as dermatologic consultation and a skin biopsy may aid in diagnosis.
- Lachmann HJ. Periodic fever syndromes. Best Pract Res Clin Rheumatol. 2017;31:596-609. doi:10.1016/j.berh.2017.12.001
- Hull KM, Shoham N, Jin Chae J, et al. The expanding spectrum of systemic autoinflammatory disorders and their rheumatic manifestations. Curr Opin Rheumatol. 2003;15:61-69. doi:10.1097/00002281-200301000-00011
- Ahmadi N, Brewer CC, Zalewski C, et al. Cryopyrin-associated periodic syndromes: otolaryngologic and audiologic manifestations. Otolaryngol Head Neck Surg. 2011;145:295-302. doi:10.1177/0194599811402296
- Kuemmerle-Deschner JB, Ozen S, Tyrrell PN, et al. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS). Ann Rheum Dis. 2017;76:942-947. doi:10.1136/annrheumdis-2016-209686
- Aksentijevich I, Nowak M, Mallah M, et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrinassociated autoinflammatory diseases. Arthritis Rheum. 2002; 46:3340-3348. doi:10.1002/art.10688
The Diagnosis: Neonatal-Onset Multisystem Inflammatory Disorder (NOMID)
The punch biopsy demonstrated a predominantly deep but somewhat superficial, periadnexal, neutrophilic and eosinophilic infiltrate (Figure). The eruption resolved 3 days later with supportive treatment, including appropriate wound care. Genetic analysis revealed an autosomal-dominant NLR family pyrin domain containing 3 gene, NLRP3, de novo variant associated with neonatal-onset multisystem inflammatory disorder (NOMID). Additional workup to characterize our patient’s inflammatory profile revealed elevated IL-18, CD3, CD4, S100A12, and S100A8/A9 levels. On day 48 of life, she was started on anakinra, an IL-1 inhibitor, at a dose of 1 mg/kg subcutaneously, which eventually was titrated to 10 mg/kg at hospital discharge. Hearing screenings were within normal limits.
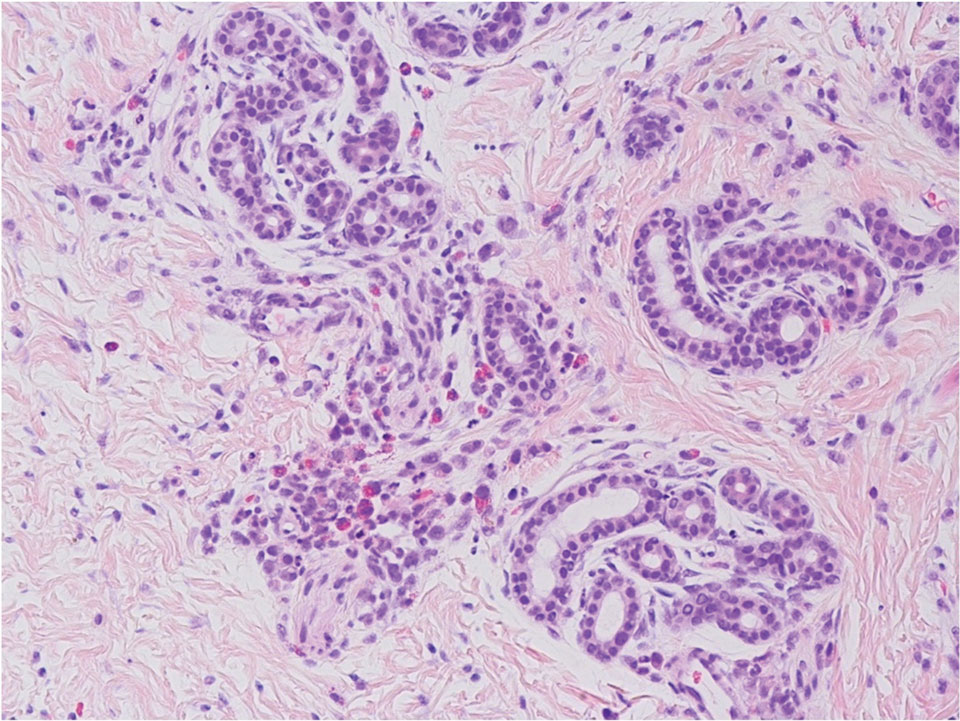
Cryopyrin-associated periodic syndromes (CAPS) consist of 3 rare, IL-1–associated, autoinflammatory disorders, including familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and NOMID (also known as chronic infantile neurologic cutaneous and articular syndrome). These conditions result from a sporadic or autosomal-dominant gain-of-function mutations in a single gene, NLRP3, on chromosome 1q44. NLRP3 encodes for cryopyrin, an important component of an IL-1 and IL-18 activating inflammasome.1 The most severe manifestation of CAPS is NOMID, which typically presents at birth as a migratory urticarial eruption, growth failure, myalgia, fever, and abnormal facial features, including frontal bossing, saddle-shaped nose, and protruding eyes.2 The illness also can manifest with hepatosplenomegaly, lymphadenopathy, uveitis, sensorineural hearing loss, cerebral atrophy, and other neurologic manifestations.3 A diagnosis of chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome was less likely given that our patient remained afebrile and did not show signs of lipodystrophy and persistent violaceous eyelid swelling. Both FCAS and MWS are less severe forms of CAPS when compared to NOMID. Familial cold autoinflammatory syndrome was less likely given the absence of the typical periodic fever pattern associated with the condition and severity of our patient’s symptoms. Muckle-Wells syndrome typically presents in adolescence with symptoms of FCAS, painful urticarial plaques, and progressive sensorinueral hearing loss. Tumor necrosis factor receptor–associated periodic fever (TRAPS) usually is associated with episodic fevers, abdominal pain, periorbital edema, migratory erythema, and arthralgia.1,3,4
Diagnostic criteria for CAPS include elevated inflammatory markers and serum amyloid, plus at least 2 of the typical CAPS symptoms: urticarial rash, cold-triggered episodes, sensorineural hearing loss, musculoskeletal symptoms, chronic aseptic meningitis, and skeletal abnormalities.4 The sensitivity and specificity of these diagnostic criteria are 84% and 91%, respectively. Additional findings that can be seen but are not part of the diagnostic criteria include intermittent fever, transient joint swelling, bony overgrowths, uveitis, optic disc edema, impaired growth, and hepatosplenomegaly.5 Laboratory findings may reveal leukocytosis, eosinophilia, anemia, and/or thrombocytopenia.3,5
Genetic testing, skin biopsies, ophthalmic examinations, neuroimaging, joint radiography, cerebrospinal fluid tests, and hearing examinations can be performed for confirmation of diagnosis and evaluation of systemic complications.4 A skin biopsy may reveal a neutrophilic infiltrate. Ophthalmic examination can demonstrate uveitis and optic disk edema. Neuroimaging may reveal cerebral atrophy or ventricular dilation. Lastly, joint radiography can be used to evaluate for the presence of premature long bone ossification or osseous overgrowth.4
In summary, NOMID is a multisystemic disorder with cutaneous manifestations. Early recognition of this entity is important given the severe sequelae and available efficacious therapy. Dermatologists should be aware of these manifestations, as dermatologic consultation and a skin biopsy may aid in diagnosis.
The Diagnosis: Neonatal-Onset Multisystem Inflammatory Disorder (NOMID)
The punch biopsy demonstrated a predominantly deep but somewhat superficial, periadnexal, neutrophilic and eosinophilic infiltrate (Figure). The eruption resolved 3 days later with supportive treatment, including appropriate wound care. Genetic analysis revealed an autosomal-dominant NLR family pyrin domain containing 3 gene, NLRP3, de novo variant associated with neonatal-onset multisystem inflammatory disorder (NOMID). Additional workup to characterize our patient’s inflammatory profile revealed elevated IL-18, CD3, CD4, S100A12, and S100A8/A9 levels. On day 48 of life, she was started on anakinra, an IL-1 inhibitor, at a dose of 1 mg/kg subcutaneously, which eventually was titrated to 10 mg/kg at hospital discharge. Hearing screenings were within normal limits.
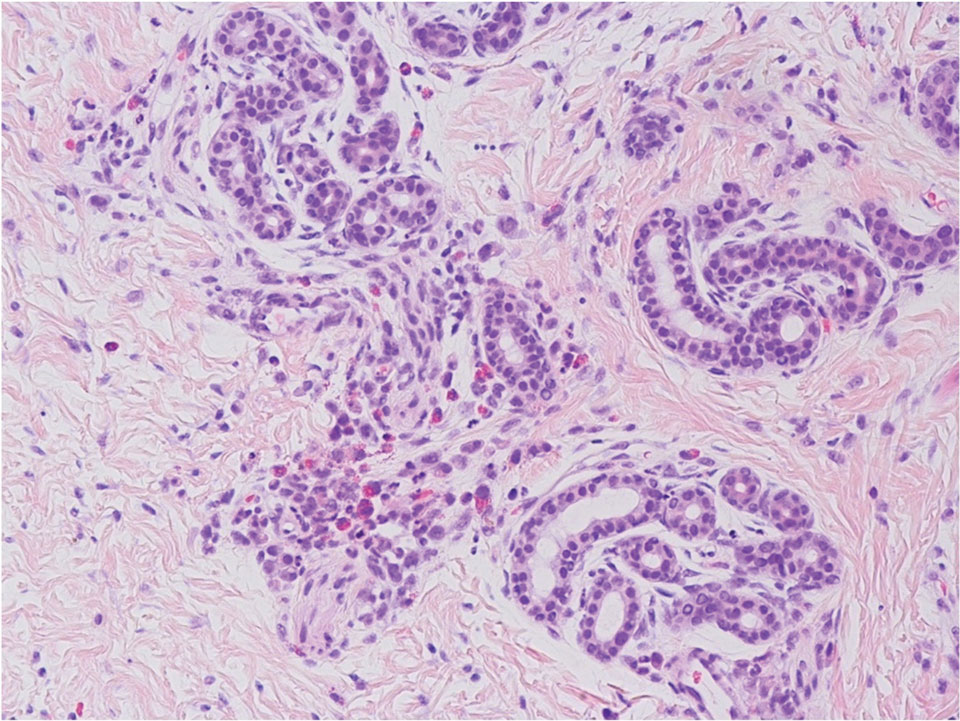
Cryopyrin-associated periodic syndromes (CAPS) consist of 3 rare, IL-1–associated, autoinflammatory disorders, including familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and NOMID (also known as chronic infantile neurologic cutaneous and articular syndrome). These conditions result from a sporadic or autosomal-dominant gain-of-function mutations in a single gene, NLRP3, on chromosome 1q44. NLRP3 encodes for cryopyrin, an important component of an IL-1 and IL-18 activating inflammasome.1 The most severe manifestation of CAPS is NOMID, which typically presents at birth as a migratory urticarial eruption, growth failure, myalgia, fever, and abnormal facial features, including frontal bossing, saddle-shaped nose, and protruding eyes.2 The illness also can manifest with hepatosplenomegaly, lymphadenopathy, uveitis, sensorineural hearing loss, cerebral atrophy, and other neurologic manifestations.3 A diagnosis of chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome was less likely given that our patient remained afebrile and did not show signs of lipodystrophy and persistent violaceous eyelid swelling. Both FCAS and MWS are less severe forms of CAPS when compared to NOMID. Familial cold autoinflammatory syndrome was less likely given the absence of the typical periodic fever pattern associated with the condition and severity of our patient’s symptoms. Muckle-Wells syndrome typically presents in adolescence with symptoms of FCAS, painful urticarial plaques, and progressive sensorinueral hearing loss. Tumor necrosis factor receptor–associated periodic fever (TRAPS) usually is associated with episodic fevers, abdominal pain, periorbital edema, migratory erythema, and arthralgia.1,3,4
Diagnostic criteria for CAPS include elevated inflammatory markers and serum amyloid, plus at least 2 of the typical CAPS symptoms: urticarial rash, cold-triggered episodes, sensorineural hearing loss, musculoskeletal symptoms, chronic aseptic meningitis, and skeletal abnormalities.4 The sensitivity and specificity of these diagnostic criteria are 84% and 91%, respectively. Additional findings that can be seen but are not part of the diagnostic criteria include intermittent fever, transient joint swelling, bony overgrowths, uveitis, optic disc edema, impaired growth, and hepatosplenomegaly.5 Laboratory findings may reveal leukocytosis, eosinophilia, anemia, and/or thrombocytopenia.3,5
Genetic testing, skin biopsies, ophthalmic examinations, neuroimaging, joint radiography, cerebrospinal fluid tests, and hearing examinations can be performed for confirmation of diagnosis and evaluation of systemic complications.4 A skin biopsy may reveal a neutrophilic infiltrate. Ophthalmic examination can demonstrate uveitis and optic disk edema. Neuroimaging may reveal cerebral atrophy or ventricular dilation. Lastly, joint radiography can be used to evaluate for the presence of premature long bone ossification or osseous overgrowth.4
In summary, NOMID is a multisystemic disorder with cutaneous manifestations. Early recognition of this entity is important given the severe sequelae and available efficacious therapy. Dermatologists should be aware of these manifestations, as dermatologic consultation and a skin biopsy may aid in diagnosis.
- Lachmann HJ. Periodic fever syndromes. Best Pract Res Clin Rheumatol. 2017;31:596-609. doi:10.1016/j.berh.2017.12.001
- Hull KM, Shoham N, Jin Chae J, et al. The expanding spectrum of systemic autoinflammatory disorders and their rheumatic manifestations. Curr Opin Rheumatol. 2003;15:61-69. doi:10.1097/00002281-200301000-00011
- Ahmadi N, Brewer CC, Zalewski C, et al. Cryopyrin-associated periodic syndromes: otolaryngologic and audiologic manifestations. Otolaryngol Head Neck Surg. 2011;145:295-302. doi:10.1177/0194599811402296
- Kuemmerle-Deschner JB, Ozen S, Tyrrell PN, et al. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS). Ann Rheum Dis. 2017;76:942-947. doi:10.1136/annrheumdis-2016-209686
- Aksentijevich I, Nowak M, Mallah M, et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrinassociated autoinflammatory diseases. Arthritis Rheum. 2002; 46:3340-3348. doi:10.1002/art.10688
- Lachmann HJ. Periodic fever syndromes. Best Pract Res Clin Rheumatol. 2017;31:596-609. doi:10.1016/j.berh.2017.12.001
- Hull KM, Shoham N, Jin Chae J, et al. The expanding spectrum of systemic autoinflammatory disorders and their rheumatic manifestations. Curr Opin Rheumatol. 2003;15:61-69. doi:10.1097/00002281-200301000-00011
- Ahmadi N, Brewer CC, Zalewski C, et al. Cryopyrin-associated periodic syndromes: otolaryngologic and audiologic manifestations. Otolaryngol Head Neck Surg. 2011;145:295-302. doi:10.1177/0194599811402296
- Kuemmerle-Deschner JB, Ozen S, Tyrrell PN, et al. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS). Ann Rheum Dis. 2017;76:942-947. doi:10.1136/annrheumdis-2016-209686
- Aksentijevich I, Nowak M, Mallah M, et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrinassociated autoinflammatory diseases. Arthritis Rheum. 2002; 46:3340-3348. doi:10.1002/art.10688
A 2-week-old infant girl was transferred to a specialty pediatric hospital where dermatology was consulted for evaluation of a diffuse eruption triggered by cold that was similar to an eruption present at birth. She was born at 31 weeks and 2 days’ gestation at an outside hospital via caesarean delivery. Early delivery was prompted by superimposed pre-eclampsia with severe hypertension after administration of antenatal steroids. At birth, the infant was cyanotic and apneic and had a documented skin eruption, according to the medical record. She had thrombocytopenia, elevated C-reactive protein, and an elevated temperature without fever. Extensive septic workup, including blood, urine, and cerebrospinal fluid cultures; herpes simplex virus and cytomegalovirus screening; and Toxoplasma polymerase chain reaction were negative. Magnetic resonance imaging of the brain revealed no evidence of intracranial congenital infection. Ampicillinsulbactam was initiated for presumed culture-negative sepsis. On day 2 of hospitalization, she developed conjunctival icterus, hepatomegaly, and jaundice. Direct hyperbilirubinemia; anemia; and elevated triglycerides, ferritin, and ammonia all were present. Coagulation studies were normal. Subsequent workup, including abdominal ultrasonography and hepatobiliary iminodiacetic acid scan, was concerning for biliary atresia. Despite appropriate treatment, her condition did not improve and she was transferred. Repeat abdominal ultrasonography on day 24 of life confirmed hepatomegaly but did not demonstrate other findings of biliary atresia. At the current presentation, physical examination revealed many scattered, redbrown and centrally violaceous, blanching papules measuring a few millimeters involving the trunk, arms, buttocks, and legs. A punch biopsy was obtained.




