User login
RSV causes 1 in 50 deaths in children under age 5: European study
But RSV – formally known as respiratory syncytial virus – is also a problem in high-income nations. In those countries, 1 in 56 otherwise healthy babies are hospitalized with RSV during their first year of life, said the study, which was published in the Lancet Respiratory Medicine.
Researchers looked at the health records of 9,154 infants born between July 1, 2017, and July 31, 2020, who were treated at health centers across Europe. Previous studies have concentrated on babies with preexisting conditions, but this one looked at otherwise healthy children, researchers said.
“This is the lowest-risk baby who is being hospitalized for this, so really, numbers are really much higher than I think some people would have guessed,” said study coauthor Louis Bont, MD, a professor of pediatric infectious diseases at Wilhelmina Children’s Hospital at University Medical Center Utrecht in the Netherlands, according to CNN. He is also chairman of the ReSViNET foundation, which aims to reduce RSV infection globally.
The study said more than 97% of deaths from RSV occur in low-income and middle-income countries. The study concluded that “maternal vaccination and passive [immunization] could have a profound impact on the RSV burden.”
In developed nations, children who get RSV usually survive because they have access to ventilators and other health care equipment. Still, just being treated for RSV can have long-range negative effects on a child’s health, Kristina Deeter, MD, chair of pediatrics at the University of Nevada, Reno, told CNN.
“Whether that is just traumatic psychosocial, emotional issues after hospitalization or even having more vulnerable lungs – you can develop asthma later on, for instance, if you’ve had a really severe infection at a young age – it can damage your lungs permanently,” she said of the study. “It’s still an important virus in our world and something that we really focus on.”
The Lancet study was published days after the CDC warned public health officials that respiratory viruses, including RSV, are surging among children across the country.
A version of this article first appeared on WebMD.com.
But RSV – formally known as respiratory syncytial virus – is also a problem in high-income nations. In those countries, 1 in 56 otherwise healthy babies are hospitalized with RSV during their first year of life, said the study, which was published in the Lancet Respiratory Medicine.
Researchers looked at the health records of 9,154 infants born between July 1, 2017, and July 31, 2020, who were treated at health centers across Europe. Previous studies have concentrated on babies with preexisting conditions, but this one looked at otherwise healthy children, researchers said.
“This is the lowest-risk baby who is being hospitalized for this, so really, numbers are really much higher than I think some people would have guessed,” said study coauthor Louis Bont, MD, a professor of pediatric infectious diseases at Wilhelmina Children’s Hospital at University Medical Center Utrecht in the Netherlands, according to CNN. He is also chairman of the ReSViNET foundation, which aims to reduce RSV infection globally.
The study said more than 97% of deaths from RSV occur in low-income and middle-income countries. The study concluded that “maternal vaccination and passive [immunization] could have a profound impact on the RSV burden.”
In developed nations, children who get RSV usually survive because they have access to ventilators and other health care equipment. Still, just being treated for RSV can have long-range negative effects on a child’s health, Kristina Deeter, MD, chair of pediatrics at the University of Nevada, Reno, told CNN.
“Whether that is just traumatic psychosocial, emotional issues after hospitalization or even having more vulnerable lungs – you can develop asthma later on, for instance, if you’ve had a really severe infection at a young age – it can damage your lungs permanently,” she said of the study. “It’s still an important virus in our world and something that we really focus on.”
The Lancet study was published days after the CDC warned public health officials that respiratory viruses, including RSV, are surging among children across the country.
A version of this article first appeared on WebMD.com.
But RSV – formally known as respiratory syncytial virus – is also a problem in high-income nations. In those countries, 1 in 56 otherwise healthy babies are hospitalized with RSV during their first year of life, said the study, which was published in the Lancet Respiratory Medicine.
Researchers looked at the health records of 9,154 infants born between July 1, 2017, and July 31, 2020, who were treated at health centers across Europe. Previous studies have concentrated on babies with preexisting conditions, but this one looked at otherwise healthy children, researchers said.
“This is the lowest-risk baby who is being hospitalized for this, so really, numbers are really much higher than I think some people would have guessed,” said study coauthor Louis Bont, MD, a professor of pediatric infectious diseases at Wilhelmina Children’s Hospital at University Medical Center Utrecht in the Netherlands, according to CNN. He is also chairman of the ReSViNET foundation, which aims to reduce RSV infection globally.
The study said more than 97% of deaths from RSV occur in low-income and middle-income countries. The study concluded that “maternal vaccination and passive [immunization] could have a profound impact on the RSV burden.”
In developed nations, children who get RSV usually survive because they have access to ventilators and other health care equipment. Still, just being treated for RSV can have long-range negative effects on a child’s health, Kristina Deeter, MD, chair of pediatrics at the University of Nevada, Reno, told CNN.
“Whether that is just traumatic psychosocial, emotional issues after hospitalization or even having more vulnerable lungs – you can develop asthma later on, for instance, if you’ve had a really severe infection at a young age – it can damage your lungs permanently,” she said of the study. “It’s still an important virus in our world and something that we really focus on.”
The Lancet study was published days after the CDC warned public health officials that respiratory viruses, including RSV, are surging among children across the country.
A version of this article first appeared on WebMD.com.
FROM LANCET RESPIRATORY MEDICINE
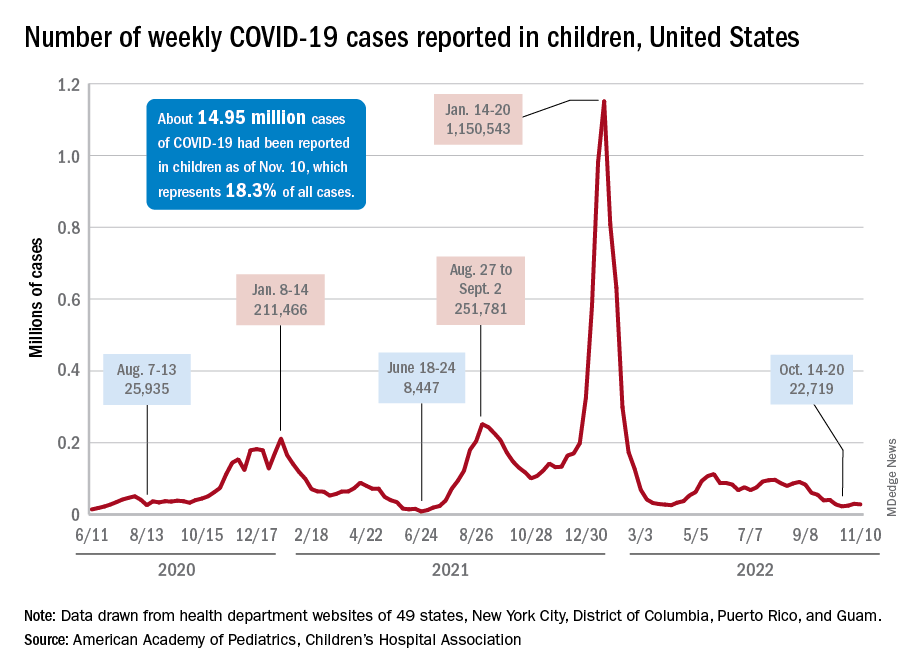
Children and COVID: Weekly cases continue to hold fairly steady
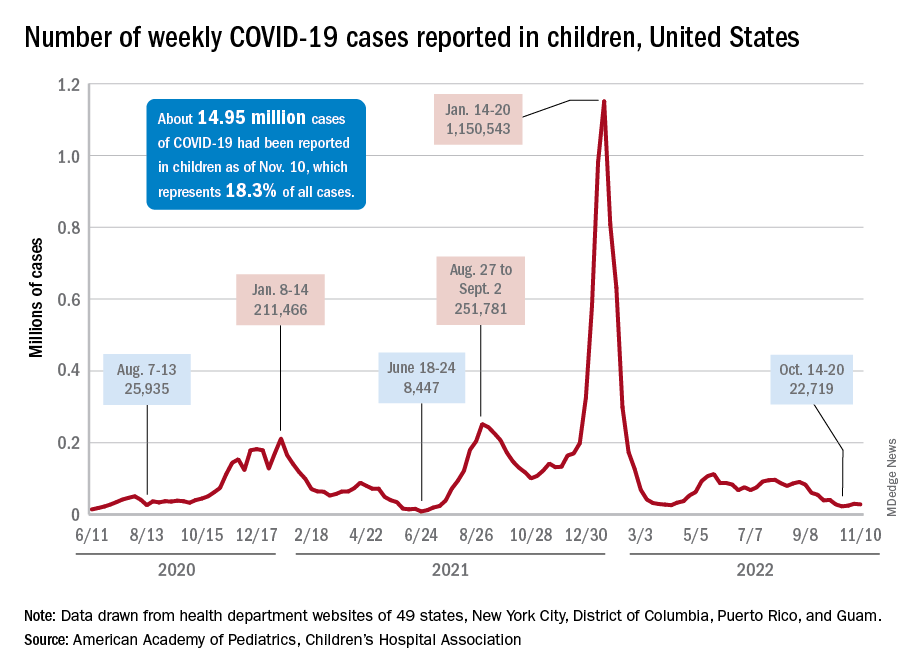
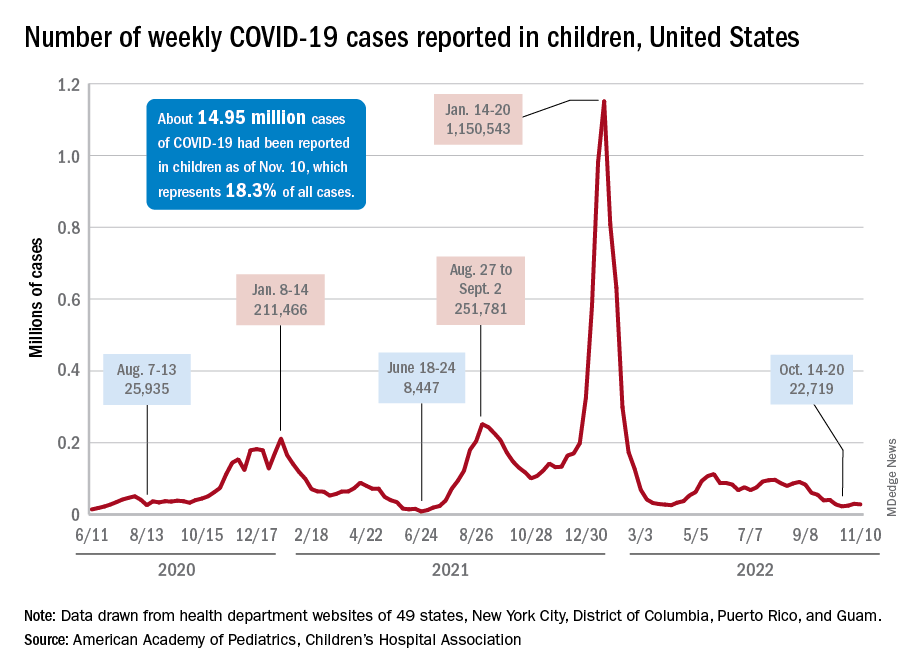
The incidence of new COVID-19 cases in children seems to have stabilized as the national count remained under 30,000 for the fifth consecutive week, but hospitalization data may indicate some possible turbulence.
Just over 28,000 pediatric cases were reported during the week of Nov. 4-10, a drop of 5.4% from the previous week, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report involving data from state and territorial health departments, several of which are no longer updating their websites.
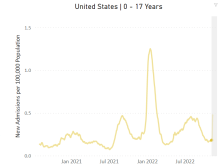
The stability in weekly cases, however, comes in contrast to a very recent and considerable increase in new hospital admissions of children aged 0-17 years with confirmed COVID-19. That rate, which was 0.18 hospitalizations per 100,000 population on Nov. 7 and 0.19 per 100,000 on Nov. 8 and 9, jumped all the way to 0.34 on Nov. 10 and 0.48 on Nov. 11, according to data from the Centers for Disease Control and Prevention. That is the highest rate since the closing days of the Omicron surge in February.
The rate for Nov. 12, the most recent one available, was down slightly to 0.47 admissions per 100,000. There doesn’t seem to be any evidence in the CDC’s data of a similar sudden increase in new hospitalizations among any other age group, and no age group, including children, shows any sign of a recent increase in emergency department visits with diagnosed COVID. (The CDC has not yet responded to our inquiry about this development.)
The two most recent 7-day averages for new admissions in children aged 0-17 show a small increase, but they cover the periods of Oct. 15 to Oct. 31, when there were 126 admissions per day, and Nov. 1 to Nov. 7, when the average went up to 133 per day, the CDC said on its COVID Data Tracker.
The CDC does not publish a weekly count of new COVID cases, but its latest data on the rate of incident cases seem to agree with the AAP/CHA figures: A gradual decline in all age groups, including children, since the beginning of September.
Vaccinations, on the other hand, bucked their recent trend and increased in the last week. About 43,000 children under age 5 years received their initial dose of COVID vaccine during Nov. 3-9, compared with 30,000 and 33,000 the 2 previous weeks, while 5- to 11-year-olds hit their highest weekly mark (31,000) since late August and 12- to 17-year-olds had their biggest week (27,000) since mid-August, the AAP reported based on CDC data.
The incidence of new COVID-19 cases in children seems to have stabilized as the national count remained under 30,000 for the fifth consecutive week, but hospitalization data may indicate some possible turbulence.
Just over 28,000 pediatric cases were reported during the week of Nov. 4-10, a drop of 5.4% from the previous week, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report involving data from state and territorial health departments, several of which are no longer updating their websites.
The stability in weekly cases, however, comes in contrast to a very recent and considerable increase in new hospital admissions of children aged 0-17 years with confirmed COVID-19. That rate, which was 0.18 hospitalizations per 100,000 population on Nov. 7 and 0.19 per 100,000 on Nov. 8 and 9, jumped all the way to 0.34 on Nov. 10 and 0.48 on Nov. 11, according to data from the Centers for Disease Control and Prevention. That is the highest rate since the closing days of the Omicron surge in February.
The rate for Nov. 12, the most recent one available, was down slightly to 0.47 admissions per 100,000. There doesn’t seem to be any evidence in the CDC’s data of a similar sudden increase in new hospitalizations among any other age group, and no age group, including children, shows any sign of a recent increase in emergency department visits with diagnosed COVID. (The CDC has not yet responded to our inquiry about this development.)
The two most recent 7-day averages for new admissions in children aged 0-17 show a small increase, but they cover the periods of Oct. 15 to Oct. 31, when there were 126 admissions per day, and Nov. 1 to Nov. 7, when the average went up to 133 per day, the CDC said on its COVID Data Tracker.
The CDC does not publish a weekly count of new COVID cases, but its latest data on the rate of incident cases seem to agree with the AAP/CHA figures: A gradual decline in all age groups, including children, since the beginning of September.
Vaccinations, on the other hand, bucked their recent trend and increased in the last week. About 43,000 children under age 5 years received their initial dose of COVID vaccine during Nov. 3-9, compared with 30,000 and 33,000 the 2 previous weeks, while 5- to 11-year-olds hit their highest weekly mark (31,000) since late August and 12- to 17-year-olds had their biggest week (27,000) since mid-August, the AAP reported based on CDC data.
The incidence of new COVID-19 cases in children seems to have stabilized as the national count remained under 30,000 for the fifth consecutive week, but hospitalization data may indicate some possible turbulence.
Just over 28,000 pediatric cases were reported during the week of Nov. 4-10, a drop of 5.4% from the previous week, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report involving data from state and territorial health departments, several of which are no longer updating their websites.
The stability in weekly cases, however, comes in contrast to a very recent and considerable increase in new hospital admissions of children aged 0-17 years with confirmed COVID-19. That rate, which was 0.18 hospitalizations per 100,000 population on Nov. 7 and 0.19 per 100,000 on Nov. 8 and 9, jumped all the way to 0.34 on Nov. 10 and 0.48 on Nov. 11, according to data from the Centers for Disease Control and Prevention. That is the highest rate since the closing days of the Omicron surge in February.
The rate for Nov. 12, the most recent one available, was down slightly to 0.47 admissions per 100,000. There doesn’t seem to be any evidence in the CDC’s data of a similar sudden increase in new hospitalizations among any other age group, and no age group, including children, shows any sign of a recent increase in emergency department visits with diagnosed COVID. (The CDC has not yet responded to our inquiry about this development.)
The two most recent 7-day averages for new admissions in children aged 0-17 show a small increase, but they cover the periods of Oct. 15 to Oct. 31, when there were 126 admissions per day, and Nov. 1 to Nov. 7, when the average went up to 133 per day, the CDC said on its COVID Data Tracker.
The CDC does not publish a weekly count of new COVID cases, but its latest data on the rate of incident cases seem to agree with the AAP/CHA figures: A gradual decline in all age groups, including children, since the beginning of September.
Vaccinations, on the other hand, bucked their recent trend and increased in the last week. About 43,000 children under age 5 years received their initial dose of COVID vaccine during Nov. 3-9, compared with 30,000 and 33,000 the 2 previous weeks, while 5- to 11-year-olds hit their highest weekly mark (31,000) since late August and 12- to 17-year-olds had their biggest week (27,000) since mid-August, the AAP reported based on CDC data.
Meditation for children
Meditation has become a popular practice in the United States over the last decade. It is not limited to adults, but can be learned and practiced by children and teenagers also. Variants are being used in many schools as parts of a social and emotional learning curriculum, and different kinds of mindfulness practices are common parts of psychological treatments. In this month’s column, we will review the evidence that supports the efficacy of a meditation practice to treat the mental health problems that are common in children and adolescents, and review how it might be a useful adjunct to the screening, education, and treatments that you offer your young patients.
There are many different types of meditation practices, but the unifying feature is known as mindfulness. Most broadly, mindfulness refers to a state of nonjudgmental awareness of one’s thoughts, feelings, or sensations. A mindfulness meditation practice involves physical stillness and focused attention, typically on the physical sensations of one’s breath. When thoughts, feelings, or physical sensations intrude on the stillness, one learns to cultivate a nonjudgmental awareness of those experiences without disrupting the state of quiet concentration. It could be said that meditation is easy to learn and difficult to master, and that is why it should be practiced regularly. Part of its growing popularity has undoubtedly been served by the ease with which people can access a variety of guided meditations (through apps, YouTube, and beyond) that make it relatively easy to access a variety of methods to learn how to practice mindfulness meditation.
The benefits of meditation in adults are well-established, including lower blood pressure, lower rates of heart disease, lower markers of inflammation, better sleep, and self-described levels of well-being. Meditation appears to be especially effective at mitigating the cardiovascular, metabolic, autoimmune, and inflammatory consequences of high-stress or unhealthy lifestyles in adults. Children and adolescents typically do not suffer from these diseases, but there is growing evidence that mindfulness practices can improve self-reported stress management skills, well-being, and sleep in young people; skills that can protect their physical and mental health. In addition, there is some evidence that mindfulness can be effective as a treatment for the common psychiatric illnesses of youth.
Anxiety
There is robust evidence for the efficacy of mindfulness-based interventions (including a regular mindfulness meditation practice) in the treatment of anxiety disorders in youth. Multiple studies and meta-analyses have demonstrated significant and sustained improvement in anxiety symptoms in these young patients. This makes sense when one considers that most psychotherapy treatments for anxiety include the cultivation of self-awareness and the ability to recognize the feelings of anxiety. This is critical as youth with anxiety disorders often mistake these feelings for facts. The treatment then shifts toward practice tolerating these feelings to help children develop an appreciation that they can face and manage anxiety and that it does not need to be avoided. Part of tolerating these feelings includes building skills to facilitate calm and physical relaxation in the face of these anxious feelings.
This is the core of exposure-based psychotherapies. Mindfulness practices echo the cultivation of self-awareness with focus and physical calm. Studies have shown that mindfulness-based interventions have significant and lasting effects on the symptoms of anxiety disorders in youth, including those youth with comorbid ADHD and learning disabilities. It is important to be aware that, for youth who have experienced trauma, mindfulness meditation can trigger a flood of re-experiencing phenomena, and it is important that those youth also are receiving treatment for PTSD.
Depression
There is evidence that some of the symptoms that occur as part of depression in adolescents improve with mindfulness-based interventions. In particular, symptoms of anger, irritability, disruptive behaviors, suicidality, and even impulsive self-injury improve with mindfulness-based interventions. Dialectical behavioral therapy (DBT) and acceptance and commitment therapy (ACT) have the nonjudgmental self-awareness of mindfulness built in as a component of the therapy. But mindfulness practices without explicit cognitive and behavioral components of psychotherapy for depression are not effective as stand-alone treatment of major depressive disorder in youth.
Multiple meta-analyses have demonstrated that stimulant treatment is more effective than behavioral or environmental interventions in the treatment of ADHD in children and adolescents, and combined treatments have not shown substantial additional improvement over medications alone in randomized controlled studies. But there is a lot of interest in finding effective treatments beyond medications that will help children with ADHD build important cognitive and behavioral skills that may lag developmentally.
Now there is an emerging body of evidence indicating that mindfulness skills in children with ADHD are quite effective for improving their sustained attention, social skills, behavioral control, and even hyperactivity. Additionally, methods to teach mindfulness skills to children who struggle with stillness and focused attention have been developed for these studies (“mindful martial arts”). Again, this intervention has not yet shown the same level of efficacy as medication treatments for ADHD symptoms, but it has demonstrated promise in early trials. Interestingly, it has also shown promise as a component of parenting interventions for youth with ADHD.
You do not need to wait for decisive evidence from randomized controlled trials to recommend mindfulness training for your patients with anxiety, ADHD, or even depression. Indeed, this practice alone may be adequate as a treatment for mild to moderate anxiety disorders. But you can also recommend it as an empowering and effective adjunctive treatment for almost every psychiatric illness and subclinical syndrome, and one that is affordable and easy for families to access. It would be valuable for you to recommend that your patients and their parents both try a mindfulness practice alongside your recommendations about healthy sleep, exercise, and nutrition. There are free apps such as Smiling Mind, Sound Mind, and Thrive Global that families can try together. Some children may need to move physically to be able to practice mindfulness, so yoga or walking meditations can be a better practice for them. When parents can try mindfulness practice alongside their children, it will facilitate their child’s efforts to develop these skills, and the improved sleep, focus, and stress management skills in parents can make a significant difference in the health and well-being of the whole family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Meditation has become a popular practice in the United States over the last decade. It is not limited to adults, but can be learned and practiced by children and teenagers also. Variants are being used in many schools as parts of a social and emotional learning curriculum, and different kinds of mindfulness practices are common parts of psychological treatments. In this month’s column, we will review the evidence that supports the efficacy of a meditation practice to treat the mental health problems that are common in children and adolescents, and review how it might be a useful adjunct to the screening, education, and treatments that you offer your young patients.
There are many different types of meditation practices, but the unifying feature is known as mindfulness. Most broadly, mindfulness refers to a state of nonjudgmental awareness of one’s thoughts, feelings, or sensations. A mindfulness meditation practice involves physical stillness and focused attention, typically on the physical sensations of one’s breath. When thoughts, feelings, or physical sensations intrude on the stillness, one learns to cultivate a nonjudgmental awareness of those experiences without disrupting the state of quiet concentration. It could be said that meditation is easy to learn and difficult to master, and that is why it should be practiced regularly. Part of its growing popularity has undoubtedly been served by the ease with which people can access a variety of guided meditations (through apps, YouTube, and beyond) that make it relatively easy to access a variety of methods to learn how to practice mindfulness meditation.
The benefits of meditation in adults are well-established, including lower blood pressure, lower rates of heart disease, lower markers of inflammation, better sleep, and self-described levels of well-being. Meditation appears to be especially effective at mitigating the cardiovascular, metabolic, autoimmune, and inflammatory consequences of high-stress or unhealthy lifestyles in adults. Children and adolescents typically do not suffer from these diseases, but there is growing evidence that mindfulness practices can improve self-reported stress management skills, well-being, and sleep in young people; skills that can protect their physical and mental health. In addition, there is some evidence that mindfulness can be effective as a treatment for the common psychiatric illnesses of youth.
Anxiety
There is robust evidence for the efficacy of mindfulness-based interventions (including a regular mindfulness meditation practice) in the treatment of anxiety disorders in youth. Multiple studies and meta-analyses have demonstrated significant and sustained improvement in anxiety symptoms in these young patients. This makes sense when one considers that most psychotherapy treatments for anxiety include the cultivation of self-awareness and the ability to recognize the feelings of anxiety. This is critical as youth with anxiety disorders often mistake these feelings for facts. The treatment then shifts toward practice tolerating these feelings to help children develop an appreciation that they can face and manage anxiety and that it does not need to be avoided. Part of tolerating these feelings includes building skills to facilitate calm and physical relaxation in the face of these anxious feelings.
This is the core of exposure-based psychotherapies. Mindfulness practices echo the cultivation of self-awareness with focus and physical calm. Studies have shown that mindfulness-based interventions have significant and lasting effects on the symptoms of anxiety disorders in youth, including those youth with comorbid ADHD and learning disabilities. It is important to be aware that, for youth who have experienced trauma, mindfulness meditation can trigger a flood of re-experiencing phenomena, and it is important that those youth also are receiving treatment for PTSD.
Depression
There is evidence that some of the symptoms that occur as part of depression in adolescents improve with mindfulness-based interventions. In particular, symptoms of anger, irritability, disruptive behaviors, suicidality, and even impulsive self-injury improve with mindfulness-based interventions. Dialectical behavioral therapy (DBT) and acceptance and commitment therapy (ACT) have the nonjudgmental self-awareness of mindfulness built in as a component of the therapy. But mindfulness practices without explicit cognitive and behavioral components of psychotherapy for depression are not effective as stand-alone treatment of major depressive disorder in youth.
Multiple meta-analyses have demonstrated that stimulant treatment is more effective than behavioral or environmental interventions in the treatment of ADHD in children and adolescents, and combined treatments have not shown substantial additional improvement over medications alone in randomized controlled studies. But there is a lot of interest in finding effective treatments beyond medications that will help children with ADHD build important cognitive and behavioral skills that may lag developmentally.
Now there is an emerging body of evidence indicating that mindfulness skills in children with ADHD are quite effective for improving their sustained attention, social skills, behavioral control, and even hyperactivity. Additionally, methods to teach mindfulness skills to children who struggle with stillness and focused attention have been developed for these studies (“mindful martial arts”). Again, this intervention has not yet shown the same level of efficacy as medication treatments for ADHD symptoms, but it has demonstrated promise in early trials. Interestingly, it has also shown promise as a component of parenting interventions for youth with ADHD.
You do not need to wait for decisive evidence from randomized controlled trials to recommend mindfulness training for your patients with anxiety, ADHD, or even depression. Indeed, this practice alone may be adequate as a treatment for mild to moderate anxiety disorders. But you can also recommend it as an empowering and effective adjunctive treatment for almost every psychiatric illness and subclinical syndrome, and one that is affordable and easy for families to access. It would be valuable for you to recommend that your patients and their parents both try a mindfulness practice alongside your recommendations about healthy sleep, exercise, and nutrition. There are free apps such as Smiling Mind, Sound Mind, and Thrive Global that families can try together. Some children may need to move physically to be able to practice mindfulness, so yoga or walking meditations can be a better practice for them. When parents can try mindfulness practice alongside their children, it will facilitate their child’s efforts to develop these skills, and the improved sleep, focus, and stress management skills in parents can make a significant difference in the health and well-being of the whole family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Meditation has become a popular practice in the United States over the last decade. It is not limited to adults, but can be learned and practiced by children and teenagers also. Variants are being used in many schools as parts of a social and emotional learning curriculum, and different kinds of mindfulness practices are common parts of psychological treatments. In this month’s column, we will review the evidence that supports the efficacy of a meditation practice to treat the mental health problems that are common in children and adolescents, and review how it might be a useful adjunct to the screening, education, and treatments that you offer your young patients.
There are many different types of meditation practices, but the unifying feature is known as mindfulness. Most broadly, mindfulness refers to a state of nonjudgmental awareness of one’s thoughts, feelings, or sensations. A mindfulness meditation practice involves physical stillness and focused attention, typically on the physical sensations of one’s breath. When thoughts, feelings, or physical sensations intrude on the stillness, one learns to cultivate a nonjudgmental awareness of those experiences without disrupting the state of quiet concentration. It could be said that meditation is easy to learn and difficult to master, and that is why it should be practiced regularly. Part of its growing popularity has undoubtedly been served by the ease with which people can access a variety of guided meditations (through apps, YouTube, and beyond) that make it relatively easy to access a variety of methods to learn how to practice mindfulness meditation.
The benefits of meditation in adults are well-established, including lower blood pressure, lower rates of heart disease, lower markers of inflammation, better sleep, and self-described levels of well-being. Meditation appears to be especially effective at mitigating the cardiovascular, metabolic, autoimmune, and inflammatory consequences of high-stress or unhealthy lifestyles in adults. Children and adolescents typically do not suffer from these diseases, but there is growing evidence that mindfulness practices can improve self-reported stress management skills, well-being, and sleep in young people; skills that can protect their physical and mental health. In addition, there is some evidence that mindfulness can be effective as a treatment for the common psychiatric illnesses of youth.
Anxiety
There is robust evidence for the efficacy of mindfulness-based interventions (including a regular mindfulness meditation practice) in the treatment of anxiety disorders in youth. Multiple studies and meta-analyses have demonstrated significant and sustained improvement in anxiety symptoms in these young patients. This makes sense when one considers that most psychotherapy treatments for anxiety include the cultivation of self-awareness and the ability to recognize the feelings of anxiety. This is critical as youth with anxiety disorders often mistake these feelings for facts. The treatment then shifts toward practice tolerating these feelings to help children develop an appreciation that they can face and manage anxiety and that it does not need to be avoided. Part of tolerating these feelings includes building skills to facilitate calm and physical relaxation in the face of these anxious feelings.
This is the core of exposure-based psychotherapies. Mindfulness practices echo the cultivation of self-awareness with focus and physical calm. Studies have shown that mindfulness-based interventions have significant and lasting effects on the symptoms of anxiety disorders in youth, including those youth with comorbid ADHD and learning disabilities. It is important to be aware that, for youth who have experienced trauma, mindfulness meditation can trigger a flood of re-experiencing phenomena, and it is important that those youth also are receiving treatment for PTSD.
Depression
There is evidence that some of the symptoms that occur as part of depression in adolescents improve with mindfulness-based interventions. In particular, symptoms of anger, irritability, disruptive behaviors, suicidality, and even impulsive self-injury improve with mindfulness-based interventions. Dialectical behavioral therapy (DBT) and acceptance and commitment therapy (ACT) have the nonjudgmental self-awareness of mindfulness built in as a component of the therapy. But mindfulness practices without explicit cognitive and behavioral components of psychotherapy for depression are not effective as stand-alone treatment of major depressive disorder in youth.
Multiple meta-analyses have demonstrated that stimulant treatment is more effective than behavioral or environmental interventions in the treatment of ADHD in children and adolescents, and combined treatments have not shown substantial additional improvement over medications alone in randomized controlled studies. But there is a lot of interest in finding effective treatments beyond medications that will help children with ADHD build important cognitive and behavioral skills that may lag developmentally.
Now there is an emerging body of evidence indicating that mindfulness skills in children with ADHD are quite effective for improving their sustained attention, social skills, behavioral control, and even hyperactivity. Additionally, methods to teach mindfulness skills to children who struggle with stillness and focused attention have been developed for these studies (“mindful martial arts”). Again, this intervention has not yet shown the same level of efficacy as medication treatments for ADHD symptoms, but it has demonstrated promise in early trials. Interestingly, it has also shown promise as a component of parenting interventions for youth with ADHD.
You do not need to wait for decisive evidence from randomized controlled trials to recommend mindfulness training for your patients with anxiety, ADHD, or even depression. Indeed, this practice alone may be adequate as a treatment for mild to moderate anxiety disorders. But you can also recommend it as an empowering and effective adjunctive treatment for almost every psychiatric illness and subclinical syndrome, and one that is affordable and easy for families to access. It would be valuable for you to recommend that your patients and their parents both try a mindfulness practice alongside your recommendations about healthy sleep, exercise, and nutrition. There are free apps such as Smiling Mind, Sound Mind, and Thrive Global that families can try together. Some children may need to move physically to be able to practice mindfulness, so yoga or walking meditations can be a better practice for them. When parents can try mindfulness practice alongside their children, it will facilitate their child’s efforts to develop these skills, and the improved sleep, focus, and stress management skills in parents can make a significant difference in the health and well-being of the whole family.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Combination therapy may boost remission in JIA
Benefit endures at 3 years
PHILADELPHIA – Aggressive therapy using conventional synthetic disease-modifying antirheumatic drugs (DMARDs) in combination with biologic agents early, soon after a child is diagnosed with polyarticular juvenile idiopathic arthritis (pJIA), enabled more patients to achieve clinical remission and longer times in inactive disease than more conventional therapeutic approaches, 3-year results of prospective, observational study demonstrated.
The results of The Childhood Arthritis and Rheumatology Research Alliance STOP-JIA study, which Yukiko Kimura, MD, presented at the annual meeting of the American College of Rheumatology, showed early combination therapy had benefits, compared with other treatment strategies that were more evident at 3 years than at 1 year of study.
“The STOP-JIA study showed that, after 3 years, patients who started a biologic early on in combination with methotrexate spent more time in inactive disease and achieved clinical remission more often when compared to those started on traditional step-up therapy,” Dr. Kimura, chief of pediatric rheumatology at Hackensack (N.J.) Meridian Health and professor of pediatrics at the Hackensack Meridian School of Medicine, said at a press conference. “This study shows that the treatment of poly-JIA patients receive initially very early on in their disease matters even 3 years after that treatment was started.”
The study compared three CARRA consensus treatment plans (CTP) for untreated pediatric pJIA patients: step-up (SU) – starting conventional synthetic DMARD therapy and adding a biologic if needed after 3 or more months; early-combination (EC) therapy – starting synthetic and biologic DMARDs together; and biologic first (BF) therapy – starting biologic DMARD monotherapy.
Dr. Kimura explained the rationale for the study. “Since biologic treatments were introduced more than 20 years ago, the prognosis for JIA significantly improved. These very effective medicines often work wonders, quickly reducing pain and inflammation in joint disease activity,” she said in the press conference. “What is not known, however, is when is the best time to start these very effective treatments.”
The most common approach is to start with a synthetic DMARD, typically methotrexate, and wait before starting a biologic, Dr. Kimura said.
“But even though methotrexate can work very well by itself, it does not work for every patient, and we don’t know whether waiting months for it to work and then starting a biologic might potentially lessen their effectiveness,” Dr. Kimura added. “We don’t know if there’s a window of opportunity that’s lost while waiting to see whether methotrexate will work.”
The study originally enrolled 400 patients, 297 of whom completed the 3-year visit – 190 in SU, 76 in EC and 31 in BF. At 12 months, the study found no statistically significant difference in clinically inactive disease (CID) between the groups, Dr. Kimura said.
Even at the 3-year visit, the percentage of patients in CID off glucocorticoids and clinical Juvenile Arthritis Disease Activity Score based on 10 joints inactive disease (cJADAS 10 ID) did not differ among the three groups, Dr. Kimura said in presenting the results. “But,” she added, “greater proportions of early-combination CTP group were able to achieve clinical remissions and spend more time with inactive disease in both CID and cJADAS 10.”
A closer look at the outcomes showed some separation between early-combination therapy and the other two treatment plans. The incidence of clinical remission (at any time point over 36 months) was 67.1% in the EC group vs. 49.1% and 47.3%, respectively, in the BF and SU groups, Dr. Kimura said. “The difference between the early-combination and step-up groups was highly significant [P = .007],” she added.
EC also had an edge in the percentage of time patients spent in CID (over 36 months): 39.2% versus 32% and 27.4%, respectively, in the BF and SU groups (P = .006 for EV vs. SU), as well as cJADAS 10 ID (50.6% in EC group vs. 42.8% and 37.5%, respectively in the BF and SU groups; P = .005 for EC vs. SU).
Dr. Kimura said that the STOP JIA trial will continue with longer-term analysis and ongoing monitoring of study patients through the CARRA registry. “These longer-term analyses and readouts will be important because even though the results at 12 months didn’t seem as definitive, it seems the longer we go, the more impact we see of the treatments that were started early on in this disease.”
The findings from this study are “significantly important,” Nina T. Washington, MD, MPH, a pediatric rheumatologist at the University of New Mexico Hospital, Albuquerque, and the Mary Bridge Children’s Hospital in Tacoma, Wash., said in an interview. “At least for the past decade we’ve really been advocating towards earlier and aggressive therapy, and that’s what this study shows: the sooner you can treat this disease, the sooner you can attack those joints that are inflamed, the better outcome you give the patient.”
The study also confirms that pediatric rheumatologists are not overtreating patients with pJIA, she added.
“In a sense we’re actually treating and preventing and if you have a child that has arthritis, it’s okay to treat that child,” Dr. Washington said. “For me that’s the most reassuring thing: that I’m not necessarily going overboard. If I have a child with polyarticular JIA and they have multiple inflamed joints and I have the evidence as they’re sitting in front of me, and I treat them. I’m going to give them the best outcome.”
The Patient Centered Outcomes Research Institute provided study funding. Dr. Kimura is chair of the CARRA JIA disease research committee and cochair of the CARRA Registry and Research Oversight Committee. She disclosed a financial relationship with Genentech. Dr. Washington has no relevant relationships to disclose.
Benefit endures at 3 years
Benefit endures at 3 years
PHILADELPHIA – Aggressive therapy using conventional synthetic disease-modifying antirheumatic drugs (DMARDs) in combination with biologic agents early, soon after a child is diagnosed with polyarticular juvenile idiopathic arthritis (pJIA), enabled more patients to achieve clinical remission and longer times in inactive disease than more conventional therapeutic approaches, 3-year results of prospective, observational study demonstrated.
The results of The Childhood Arthritis and Rheumatology Research Alliance STOP-JIA study, which Yukiko Kimura, MD, presented at the annual meeting of the American College of Rheumatology, showed early combination therapy had benefits, compared with other treatment strategies that were more evident at 3 years than at 1 year of study.
“The STOP-JIA study showed that, after 3 years, patients who started a biologic early on in combination with methotrexate spent more time in inactive disease and achieved clinical remission more often when compared to those started on traditional step-up therapy,” Dr. Kimura, chief of pediatric rheumatology at Hackensack (N.J.) Meridian Health and professor of pediatrics at the Hackensack Meridian School of Medicine, said at a press conference. “This study shows that the treatment of poly-JIA patients receive initially very early on in their disease matters even 3 years after that treatment was started.”
The study compared three CARRA consensus treatment plans (CTP) for untreated pediatric pJIA patients: step-up (SU) – starting conventional synthetic DMARD therapy and adding a biologic if needed after 3 or more months; early-combination (EC) therapy – starting synthetic and biologic DMARDs together; and biologic first (BF) therapy – starting biologic DMARD monotherapy.
Dr. Kimura explained the rationale for the study. “Since biologic treatments were introduced more than 20 years ago, the prognosis for JIA significantly improved. These very effective medicines often work wonders, quickly reducing pain and inflammation in joint disease activity,” she said in the press conference. “What is not known, however, is when is the best time to start these very effective treatments.”
The most common approach is to start with a synthetic DMARD, typically methotrexate, and wait before starting a biologic, Dr. Kimura said.
“But even though methotrexate can work very well by itself, it does not work for every patient, and we don’t know whether waiting months for it to work and then starting a biologic might potentially lessen their effectiveness,” Dr. Kimura added. “We don’t know if there’s a window of opportunity that’s lost while waiting to see whether methotrexate will work.”
The study originally enrolled 400 patients, 297 of whom completed the 3-year visit – 190 in SU, 76 in EC and 31 in BF. At 12 months, the study found no statistically significant difference in clinically inactive disease (CID) between the groups, Dr. Kimura said.
Even at the 3-year visit, the percentage of patients in CID off glucocorticoids and clinical Juvenile Arthritis Disease Activity Score based on 10 joints inactive disease (cJADAS 10 ID) did not differ among the three groups, Dr. Kimura said in presenting the results. “But,” she added, “greater proportions of early-combination CTP group were able to achieve clinical remissions and spend more time with inactive disease in both CID and cJADAS 10.”
A closer look at the outcomes showed some separation between early-combination therapy and the other two treatment plans. The incidence of clinical remission (at any time point over 36 months) was 67.1% in the EC group vs. 49.1% and 47.3%, respectively, in the BF and SU groups, Dr. Kimura said. “The difference between the early-combination and step-up groups was highly significant [P = .007],” she added.
EC also had an edge in the percentage of time patients spent in CID (over 36 months): 39.2% versus 32% and 27.4%, respectively, in the BF and SU groups (P = .006 for EV vs. SU), as well as cJADAS 10 ID (50.6% in EC group vs. 42.8% and 37.5%, respectively in the BF and SU groups; P = .005 for EC vs. SU).
Dr. Kimura said that the STOP JIA trial will continue with longer-term analysis and ongoing monitoring of study patients through the CARRA registry. “These longer-term analyses and readouts will be important because even though the results at 12 months didn’t seem as definitive, it seems the longer we go, the more impact we see of the treatments that were started early on in this disease.”
The findings from this study are “significantly important,” Nina T. Washington, MD, MPH, a pediatric rheumatologist at the University of New Mexico Hospital, Albuquerque, and the Mary Bridge Children’s Hospital in Tacoma, Wash., said in an interview. “At least for the past decade we’ve really been advocating towards earlier and aggressive therapy, and that’s what this study shows: the sooner you can treat this disease, the sooner you can attack those joints that are inflamed, the better outcome you give the patient.”
The study also confirms that pediatric rheumatologists are not overtreating patients with pJIA, she added.
“In a sense we’re actually treating and preventing and if you have a child that has arthritis, it’s okay to treat that child,” Dr. Washington said. “For me that’s the most reassuring thing: that I’m not necessarily going overboard. If I have a child with polyarticular JIA and they have multiple inflamed joints and I have the evidence as they’re sitting in front of me, and I treat them. I’m going to give them the best outcome.”
The Patient Centered Outcomes Research Institute provided study funding. Dr. Kimura is chair of the CARRA JIA disease research committee and cochair of the CARRA Registry and Research Oversight Committee. She disclosed a financial relationship with Genentech. Dr. Washington has no relevant relationships to disclose.
PHILADELPHIA – Aggressive therapy using conventional synthetic disease-modifying antirheumatic drugs (DMARDs) in combination with biologic agents early, soon after a child is diagnosed with polyarticular juvenile idiopathic arthritis (pJIA), enabled more patients to achieve clinical remission and longer times in inactive disease than more conventional therapeutic approaches, 3-year results of prospective, observational study demonstrated.
The results of The Childhood Arthritis and Rheumatology Research Alliance STOP-JIA study, which Yukiko Kimura, MD, presented at the annual meeting of the American College of Rheumatology, showed early combination therapy had benefits, compared with other treatment strategies that were more evident at 3 years than at 1 year of study.
“The STOP-JIA study showed that, after 3 years, patients who started a biologic early on in combination with methotrexate spent more time in inactive disease and achieved clinical remission more often when compared to those started on traditional step-up therapy,” Dr. Kimura, chief of pediatric rheumatology at Hackensack (N.J.) Meridian Health and professor of pediatrics at the Hackensack Meridian School of Medicine, said at a press conference. “This study shows that the treatment of poly-JIA patients receive initially very early on in their disease matters even 3 years after that treatment was started.”
The study compared three CARRA consensus treatment plans (CTP) for untreated pediatric pJIA patients: step-up (SU) – starting conventional synthetic DMARD therapy and adding a biologic if needed after 3 or more months; early-combination (EC) therapy – starting synthetic and biologic DMARDs together; and biologic first (BF) therapy – starting biologic DMARD monotherapy.
Dr. Kimura explained the rationale for the study. “Since biologic treatments were introduced more than 20 years ago, the prognosis for JIA significantly improved. These very effective medicines often work wonders, quickly reducing pain and inflammation in joint disease activity,” she said in the press conference. “What is not known, however, is when is the best time to start these very effective treatments.”
The most common approach is to start with a synthetic DMARD, typically methotrexate, and wait before starting a biologic, Dr. Kimura said.
“But even though methotrexate can work very well by itself, it does not work for every patient, and we don’t know whether waiting months for it to work and then starting a biologic might potentially lessen their effectiveness,” Dr. Kimura added. “We don’t know if there’s a window of opportunity that’s lost while waiting to see whether methotrexate will work.”
The study originally enrolled 400 patients, 297 of whom completed the 3-year visit – 190 in SU, 76 in EC and 31 in BF. At 12 months, the study found no statistically significant difference in clinically inactive disease (CID) between the groups, Dr. Kimura said.
Even at the 3-year visit, the percentage of patients in CID off glucocorticoids and clinical Juvenile Arthritis Disease Activity Score based on 10 joints inactive disease (cJADAS 10 ID) did not differ among the three groups, Dr. Kimura said in presenting the results. “But,” she added, “greater proportions of early-combination CTP group were able to achieve clinical remissions and spend more time with inactive disease in both CID and cJADAS 10.”
A closer look at the outcomes showed some separation between early-combination therapy and the other two treatment plans. The incidence of clinical remission (at any time point over 36 months) was 67.1% in the EC group vs. 49.1% and 47.3%, respectively, in the BF and SU groups, Dr. Kimura said. “The difference between the early-combination and step-up groups was highly significant [P = .007],” she added.
EC also had an edge in the percentage of time patients spent in CID (over 36 months): 39.2% versus 32% and 27.4%, respectively, in the BF and SU groups (P = .006 for EV vs. SU), as well as cJADAS 10 ID (50.6% in EC group vs. 42.8% and 37.5%, respectively in the BF and SU groups; P = .005 for EC vs. SU).
Dr. Kimura said that the STOP JIA trial will continue with longer-term analysis and ongoing monitoring of study patients through the CARRA registry. “These longer-term analyses and readouts will be important because even though the results at 12 months didn’t seem as definitive, it seems the longer we go, the more impact we see of the treatments that were started early on in this disease.”
The findings from this study are “significantly important,” Nina T. Washington, MD, MPH, a pediatric rheumatologist at the University of New Mexico Hospital, Albuquerque, and the Mary Bridge Children’s Hospital in Tacoma, Wash., said in an interview. “At least for the past decade we’ve really been advocating towards earlier and aggressive therapy, and that’s what this study shows: the sooner you can treat this disease, the sooner you can attack those joints that are inflamed, the better outcome you give the patient.”
The study also confirms that pediatric rheumatologists are not overtreating patients with pJIA, she added.
“In a sense we’re actually treating and preventing and if you have a child that has arthritis, it’s okay to treat that child,” Dr. Washington said. “For me that’s the most reassuring thing: that I’m not necessarily going overboard. If I have a child with polyarticular JIA and they have multiple inflamed joints and I have the evidence as they’re sitting in front of me, and I treat them. I’m going to give them the best outcome.”
The Patient Centered Outcomes Research Institute provided study funding. Dr. Kimura is chair of the CARRA JIA disease research committee and cochair of the CARRA Registry and Research Oversight Committee. She disclosed a financial relationship with Genentech. Dr. Washington has no relevant relationships to disclose.
AT ACR 2022
Love them or hate them, masks in schools work
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Infant anaphylaxis: Study characterizes symptoms, treatment
LOUISVILLE, KY. – , research findings indicate.
Given that early administration of epinephrine can be potentially lifesaving for infants with anaphylaxis, the study highlighted the real-world successes in increased uptake of treatment in this vulnerable patient population.
Most infants in the study who presented to the ED and received epinephrine were able to be discharged home after just a few hours, with only 1 out of 10 requiring hospitalization.
The study also reported that most symptoms were in the skin/mucosal, gastrointestinal, respiratory, and cardiovascular (CV) systems, providing improved characterization of anaphylaxis symptoms in the infant population.
Nearly “all episodes were triggered by food – especially egg, peanut, milk, and cashew,” commented Colleen Shannon, MD, a pediatrician at Children’s Hospital of Philadelphia, who presented the research findings at the annual meeting of the American College of Allergy, Asthma, and Immunology.
Dr. Shannon noted that despite previous research demonstrating age-based differences in the presentation of anaphylaxis, the symptomatology of anaphylaxis in infants has not been robustly characterized. Better characterization of anaphylaxis in infants with allergies may help ensure earlier and more accurate diagnosis and management, she said.
For the study, the researchers performed a retrospective chart review of 169 patients between 0 and 24 months of age (mean age, 1.0 years) who presented to the emergency department of a pediatric tertiary referral center between 2019 and 2022.
All patients in the study met diagnostic criteria for anaphylaxis. The investigators used the medical records of patients to evaluate for demographics, as well as presenting symptoms and treatment.
More than half (56.2%) of infants in the study were 12 months of age or younger, and 64.5% were male.
Nearly all (96.5%) anaphylaxis episodes presenting to the ED were triggered by food. The most common foods triggering these episodes were egg (26.6%), peanut (25.4%), milk (13.6%), and cashew (10.1%).
Most symptoms involved the skin/mucosal (97.6%) and GI (74.6%) systems, followed by respiratory (56.8%) and CV (34.3%) systems. Isolated tachycardia was recorded in 84.5% of patients with CV-related symptoms.
Epinephrine was administered to 86.4% of infants who presented to the ED with anaphylaxis. Nearly a third (30.1%) of these infants received epinephrine before arriving to the ED, and 9.5% required more than 1 dose.
The researchers also found that 10.1% of patients required hospital admission, but none had symptoms severe enough to require intensive care.
Jennifer Hoffmann, MD, an emergency medicine physician at the Lurie Children’s Hospital of Chicago, told this news organization that while characterizing anaphylaxis symptoms is relevant for clinicians, it also remains vitally important “to teach parents of infants how to recognize the signs of anaphylaxis, particularly as they begin to introduce new foods,” to ensure timely treatment.
She added that since most infants in the study improved after a single dose of epinephrine, most infants presenting to the ED with anaphylaxis can therefore be safely discharged home after only a brief period of observation. “That is, age alone should not be a reason for admission,” explained Dr. Hoffmann, who wasn’t involved in the research study.
The study was independently supported. Dr. Shannon and Dr. Hoffmann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LOUISVILLE, KY. – , research findings indicate.
Given that early administration of epinephrine can be potentially lifesaving for infants with anaphylaxis, the study highlighted the real-world successes in increased uptake of treatment in this vulnerable patient population.
Most infants in the study who presented to the ED and received epinephrine were able to be discharged home after just a few hours, with only 1 out of 10 requiring hospitalization.
The study also reported that most symptoms were in the skin/mucosal, gastrointestinal, respiratory, and cardiovascular (CV) systems, providing improved characterization of anaphylaxis symptoms in the infant population.
Nearly “all episodes were triggered by food – especially egg, peanut, milk, and cashew,” commented Colleen Shannon, MD, a pediatrician at Children’s Hospital of Philadelphia, who presented the research findings at the annual meeting of the American College of Allergy, Asthma, and Immunology.
Dr. Shannon noted that despite previous research demonstrating age-based differences in the presentation of anaphylaxis, the symptomatology of anaphylaxis in infants has not been robustly characterized. Better characterization of anaphylaxis in infants with allergies may help ensure earlier and more accurate diagnosis and management, she said.
For the study, the researchers performed a retrospective chart review of 169 patients between 0 and 24 months of age (mean age, 1.0 years) who presented to the emergency department of a pediatric tertiary referral center between 2019 and 2022.
All patients in the study met diagnostic criteria for anaphylaxis. The investigators used the medical records of patients to evaluate for demographics, as well as presenting symptoms and treatment.
More than half (56.2%) of infants in the study were 12 months of age or younger, and 64.5% were male.
Nearly all (96.5%) anaphylaxis episodes presenting to the ED were triggered by food. The most common foods triggering these episodes were egg (26.6%), peanut (25.4%), milk (13.6%), and cashew (10.1%).
Most symptoms involved the skin/mucosal (97.6%) and GI (74.6%) systems, followed by respiratory (56.8%) and CV (34.3%) systems. Isolated tachycardia was recorded in 84.5% of patients with CV-related symptoms.
Epinephrine was administered to 86.4% of infants who presented to the ED with anaphylaxis. Nearly a third (30.1%) of these infants received epinephrine before arriving to the ED, and 9.5% required more than 1 dose.
The researchers also found that 10.1% of patients required hospital admission, but none had symptoms severe enough to require intensive care.
Jennifer Hoffmann, MD, an emergency medicine physician at the Lurie Children’s Hospital of Chicago, told this news organization that while characterizing anaphylaxis symptoms is relevant for clinicians, it also remains vitally important “to teach parents of infants how to recognize the signs of anaphylaxis, particularly as they begin to introduce new foods,” to ensure timely treatment.
She added that since most infants in the study improved after a single dose of epinephrine, most infants presenting to the ED with anaphylaxis can therefore be safely discharged home after only a brief period of observation. “That is, age alone should not be a reason for admission,” explained Dr. Hoffmann, who wasn’t involved in the research study.
The study was independently supported. Dr. Shannon and Dr. Hoffmann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LOUISVILLE, KY. – , research findings indicate.
Given that early administration of epinephrine can be potentially lifesaving for infants with anaphylaxis, the study highlighted the real-world successes in increased uptake of treatment in this vulnerable patient population.
Most infants in the study who presented to the ED and received epinephrine were able to be discharged home after just a few hours, with only 1 out of 10 requiring hospitalization.
The study also reported that most symptoms were in the skin/mucosal, gastrointestinal, respiratory, and cardiovascular (CV) systems, providing improved characterization of anaphylaxis symptoms in the infant population.
Nearly “all episodes were triggered by food – especially egg, peanut, milk, and cashew,” commented Colleen Shannon, MD, a pediatrician at Children’s Hospital of Philadelphia, who presented the research findings at the annual meeting of the American College of Allergy, Asthma, and Immunology.
Dr. Shannon noted that despite previous research demonstrating age-based differences in the presentation of anaphylaxis, the symptomatology of anaphylaxis in infants has not been robustly characterized. Better characterization of anaphylaxis in infants with allergies may help ensure earlier and more accurate diagnosis and management, she said.
For the study, the researchers performed a retrospective chart review of 169 patients between 0 and 24 months of age (mean age, 1.0 years) who presented to the emergency department of a pediatric tertiary referral center between 2019 and 2022.
All patients in the study met diagnostic criteria for anaphylaxis. The investigators used the medical records of patients to evaluate for demographics, as well as presenting symptoms and treatment.
More than half (56.2%) of infants in the study were 12 months of age or younger, and 64.5% were male.
Nearly all (96.5%) anaphylaxis episodes presenting to the ED were triggered by food. The most common foods triggering these episodes were egg (26.6%), peanut (25.4%), milk (13.6%), and cashew (10.1%).
Most symptoms involved the skin/mucosal (97.6%) and GI (74.6%) systems, followed by respiratory (56.8%) and CV (34.3%) systems. Isolated tachycardia was recorded in 84.5% of patients with CV-related symptoms.
Epinephrine was administered to 86.4% of infants who presented to the ED with anaphylaxis. Nearly a third (30.1%) of these infants received epinephrine before arriving to the ED, and 9.5% required more than 1 dose.
The researchers also found that 10.1% of patients required hospital admission, but none had symptoms severe enough to require intensive care.
Jennifer Hoffmann, MD, an emergency medicine physician at the Lurie Children’s Hospital of Chicago, told this news organization that while characterizing anaphylaxis symptoms is relevant for clinicians, it also remains vitally important “to teach parents of infants how to recognize the signs of anaphylaxis, particularly as they begin to introduce new foods,” to ensure timely treatment.
She added that since most infants in the study improved after a single dose of epinephrine, most infants presenting to the ED with anaphylaxis can therefore be safely discharged home after only a brief period of observation. “That is, age alone should not be a reason for admission,” explained Dr. Hoffmann, who wasn’t involved in the research study.
The study was independently supported. Dr. Shannon and Dr. Hoffmann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACAAI
ED visits for kids with suicidal thoughts increasing: Study
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
FROM PEDIATRICS
Watching violent TV in preschool linked with emotional, behavioral issues at age 12
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
FROM THE JOURNAL OF DEVELOPMENTAL & BEHAVIORAL PEDIATRICS
Clinical signs differ between children and adults with vasculitis
Researchers have found a link between age of diagnosis and various clinical characteristics and outcomes in patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV).
The findings, presented at the annual meeting of the American College of Rheumatology, may have implications for research and treatment, especially in children.
AAV is a group of conditions characterized by the development of autoantibodies to the neutrophil proteins proteinase 3 (PR3-ANCA) or myeloperoxidase (MPO-ANCA).
The rare autoimmune condition can cause systemic inflammation and damage, sometimes permanent, to small- and medium-sized arteries. Clinical presentations vary and can include several organs, including skin, stomach, intestines, lung, and kidney, as well as airways in ear, nose, and throat.
Data limited on child vs. adult characteristics
AAV can be diagnosed in any decade of life, but clinical characteristics and outcomes often differ between children and adults, and data are limited. Studies often exclude children.
Lead author Jessica Bloom, MD, MSCS, a pediatric rheumatologist and assistant professor of pediatrics at Children’s Hospital Colorado, Aurora, and colleagues performed an analysis of patients with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) who were enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021.
Patients with eosinophilic GPA (EGPA) were analyzed separately. Children and young adults with EGPA were combined because of the small sample size (n = 87).
The groups were sorted by the age they were diagnosed: under 18 years old, 18-40, 40-65, and older than 65.
More than 1,000 patients included
Dr. Bloom’s team analyzed data from 1,020 patients: 61 diagnosed as children, 240 as young adults, 560 as middle-aged adults, and 159 diagnosed as older adults. At all ages, about nine out of 10 patients were White.
They found 852 (84%) had GPA and 165 (16%) had MPA. The analysis also showed 893 (92%) of patients with ANCA results were ANCA positive: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA, and 9 (1%) with both.
Differences between age groups included:
- Children experienced more subglottic stenosis and alveolar hemorrhage than adults with the condition.
- About half of patients diagnosed in childhood received both cyclophosphamide and rituximab. That rate decreased with increasing age of diagnosis to as low as 14% for those diagnosed in older adulthood.
- More females than males in all age groups were diagnosed with AAV, but the difference was most pronounced when diagnosed in childhood, and female predominance declined as age increased.
- Older adults experienced more neurologic disease and less musculoskeletal and sinus involvement.
Additionally, for those diagnosed after age 65, after adjusting for disease length and whether they were taking cyclophosphamide and/or rituximab, the Vasculitis Damage Index (VDI) and ANCA Vasculitis Index of Damage (AVID) scores were higher than for those diagnosed in childhood.
“However, these differences are no longer significant when medication toxicity and comorbidity-related items are excluded. Thus, differences in the VDI and AVID scores are driven by non–disease-specific damage,” Dr. Bloom said.
Bringing children into the clinical discussion
Dr. Bloom said in an interview that
For example, the findings that children have more subglottic stenosis and alveolar hemorrhage than adults “may warrant more aggressive therapy,” she said. Children also have different growth and psychosocial risk factors during their disease course and may live longer with the disease than those in older age groups.
“Our study helps to point out these differences and bring children into the discussion,” Dr. Bloom said. “It also recognizes that damage scores used in studies and care may not adequately assess disease across the lifespan, as they are largely influenced by items not specific to the disease but rather medication toxicity and comorbidities, such as osteoporosis, cataracts, and malignancy.”
Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at Hospital for Special Surgery, New York, said in an interview that the work highlights interesting information about the fact that disease features are skewed differently in children – “in particular the higher likelihood of upper airway [subglottic] disease, and potentially severe lower airway disease [alveolar hemorrhage].”
However, from a practical standpoint, Dr. Spiera said, “I am not sure that this will change our clinical approach to different patients, but the differences in disease features and even the sex differences in terms of who are afflicted with GPA [more often children and more likely to be female] may offer insights into disease pathogenesis.”
Dr. Bloom received funding from the Vasculitis Clinical Research Consortium and Vasculitis Foundation to conduct this work as a VCRC-VF fellow. Several coauthors reported various conflicts of interest with pharmaceutical companies. Dr. Spiera declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have found a link between age of diagnosis and various clinical characteristics and outcomes in patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV).
The findings, presented at the annual meeting of the American College of Rheumatology, may have implications for research and treatment, especially in children.
AAV is a group of conditions characterized by the development of autoantibodies to the neutrophil proteins proteinase 3 (PR3-ANCA) or myeloperoxidase (MPO-ANCA).
The rare autoimmune condition can cause systemic inflammation and damage, sometimes permanent, to small- and medium-sized arteries. Clinical presentations vary and can include several organs, including skin, stomach, intestines, lung, and kidney, as well as airways in ear, nose, and throat.
Data limited on child vs. adult characteristics
AAV can be diagnosed in any decade of life, but clinical characteristics and outcomes often differ between children and adults, and data are limited. Studies often exclude children.
Lead author Jessica Bloom, MD, MSCS, a pediatric rheumatologist and assistant professor of pediatrics at Children’s Hospital Colorado, Aurora, and colleagues performed an analysis of patients with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) who were enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021.
Patients with eosinophilic GPA (EGPA) were analyzed separately. Children and young adults with EGPA were combined because of the small sample size (n = 87).
The groups were sorted by the age they were diagnosed: under 18 years old, 18-40, 40-65, and older than 65.
More than 1,000 patients included
Dr. Bloom’s team analyzed data from 1,020 patients: 61 diagnosed as children, 240 as young adults, 560 as middle-aged adults, and 159 diagnosed as older adults. At all ages, about nine out of 10 patients were White.
They found 852 (84%) had GPA and 165 (16%) had MPA. The analysis also showed 893 (92%) of patients with ANCA results were ANCA positive: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA, and 9 (1%) with both.
Differences between age groups included:
- Children experienced more subglottic stenosis and alveolar hemorrhage than adults with the condition.
- About half of patients diagnosed in childhood received both cyclophosphamide and rituximab. That rate decreased with increasing age of diagnosis to as low as 14% for those diagnosed in older adulthood.
- More females than males in all age groups were diagnosed with AAV, but the difference was most pronounced when diagnosed in childhood, and female predominance declined as age increased.
- Older adults experienced more neurologic disease and less musculoskeletal and sinus involvement.
Additionally, for those diagnosed after age 65, after adjusting for disease length and whether they were taking cyclophosphamide and/or rituximab, the Vasculitis Damage Index (VDI) and ANCA Vasculitis Index of Damage (AVID) scores were higher than for those diagnosed in childhood.
“However, these differences are no longer significant when medication toxicity and comorbidity-related items are excluded. Thus, differences in the VDI and AVID scores are driven by non–disease-specific damage,” Dr. Bloom said.
Bringing children into the clinical discussion
Dr. Bloom said in an interview that
For example, the findings that children have more subglottic stenosis and alveolar hemorrhage than adults “may warrant more aggressive therapy,” she said. Children also have different growth and psychosocial risk factors during their disease course and may live longer with the disease than those in older age groups.
“Our study helps to point out these differences and bring children into the discussion,” Dr. Bloom said. “It also recognizes that damage scores used in studies and care may not adequately assess disease across the lifespan, as they are largely influenced by items not specific to the disease but rather medication toxicity and comorbidities, such as osteoporosis, cataracts, and malignancy.”
Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at Hospital for Special Surgery, New York, said in an interview that the work highlights interesting information about the fact that disease features are skewed differently in children – “in particular the higher likelihood of upper airway [subglottic] disease, and potentially severe lower airway disease [alveolar hemorrhage].”
However, from a practical standpoint, Dr. Spiera said, “I am not sure that this will change our clinical approach to different patients, but the differences in disease features and even the sex differences in terms of who are afflicted with GPA [more often children and more likely to be female] may offer insights into disease pathogenesis.”
Dr. Bloom received funding from the Vasculitis Clinical Research Consortium and Vasculitis Foundation to conduct this work as a VCRC-VF fellow. Several coauthors reported various conflicts of interest with pharmaceutical companies. Dr. Spiera declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have found a link between age of diagnosis and various clinical characteristics and outcomes in patients with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV).
The findings, presented at the annual meeting of the American College of Rheumatology, may have implications for research and treatment, especially in children.
AAV is a group of conditions characterized by the development of autoantibodies to the neutrophil proteins proteinase 3 (PR3-ANCA) or myeloperoxidase (MPO-ANCA).
The rare autoimmune condition can cause systemic inflammation and damage, sometimes permanent, to small- and medium-sized arteries. Clinical presentations vary and can include several organs, including skin, stomach, intestines, lung, and kidney, as well as airways in ear, nose, and throat.
Data limited on child vs. adult characteristics
AAV can be diagnosed in any decade of life, but clinical characteristics and outcomes often differ between children and adults, and data are limited. Studies often exclude children.
Lead author Jessica Bloom, MD, MSCS, a pediatric rheumatologist and assistant professor of pediatrics at Children’s Hospital Colorado, Aurora, and colleagues performed an analysis of patients with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA) who were enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021.
Patients with eosinophilic GPA (EGPA) were analyzed separately. Children and young adults with EGPA were combined because of the small sample size (n = 87).
The groups were sorted by the age they were diagnosed: under 18 years old, 18-40, 40-65, and older than 65.
More than 1,000 patients included
Dr. Bloom’s team analyzed data from 1,020 patients: 61 diagnosed as children, 240 as young adults, 560 as middle-aged adults, and 159 diagnosed as older adults. At all ages, about nine out of 10 patients were White.
They found 852 (84%) had GPA and 165 (16%) had MPA. The analysis also showed 893 (92%) of patients with ANCA results were ANCA positive: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA, and 9 (1%) with both.
Differences between age groups included:
- Children experienced more subglottic stenosis and alveolar hemorrhage than adults with the condition.
- About half of patients diagnosed in childhood received both cyclophosphamide and rituximab. That rate decreased with increasing age of diagnosis to as low as 14% for those diagnosed in older adulthood.
- More females than males in all age groups were diagnosed with AAV, but the difference was most pronounced when diagnosed in childhood, and female predominance declined as age increased.
- Older adults experienced more neurologic disease and less musculoskeletal and sinus involvement.
Additionally, for those diagnosed after age 65, after adjusting for disease length and whether they were taking cyclophosphamide and/or rituximab, the Vasculitis Damage Index (VDI) and ANCA Vasculitis Index of Damage (AVID) scores were higher than for those diagnosed in childhood.
“However, these differences are no longer significant when medication toxicity and comorbidity-related items are excluded. Thus, differences in the VDI and AVID scores are driven by non–disease-specific damage,” Dr. Bloom said.
Bringing children into the clinical discussion
Dr. Bloom said in an interview that
For example, the findings that children have more subglottic stenosis and alveolar hemorrhage than adults “may warrant more aggressive therapy,” she said. Children also have different growth and psychosocial risk factors during their disease course and may live longer with the disease than those in older age groups.
“Our study helps to point out these differences and bring children into the discussion,” Dr. Bloom said. “It also recognizes that damage scores used in studies and care may not adequately assess disease across the lifespan, as they are largely influenced by items not specific to the disease but rather medication toxicity and comorbidities, such as osteoporosis, cataracts, and malignancy.”
Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at Hospital for Special Surgery, New York, said in an interview that the work highlights interesting information about the fact that disease features are skewed differently in children – “in particular the higher likelihood of upper airway [subglottic] disease, and potentially severe lower airway disease [alveolar hemorrhage].”
However, from a practical standpoint, Dr. Spiera said, “I am not sure that this will change our clinical approach to different patients, but the differences in disease features and even the sex differences in terms of who are afflicted with GPA [more often children and more likely to be female] may offer insights into disease pathogenesis.”
Dr. Bloom received funding from the Vasculitis Clinical Research Consortium and Vasculitis Foundation to conduct this work as a VCRC-VF fellow. Several coauthors reported various conflicts of interest with pharmaceutical companies. Dr. Spiera declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACR 2022
Serum dupilumab levels do not predict clinical response
The finding that serum levels, according to a study published in JAMA Dermatology.
The study results mean that researchers should continue exploring potential AD drugs with novel mechanisms to help patients who fail type 2 inflammatory inhibition, experts told this news organization. The search for accurate augurs of clinical performance also must continue.
Addressing inadequate response
Quantifying nonresponse and incomplete response levels with dupilumab is difficult, said Jonathan I. Silverberg, MD, PhD, MPH, offering perspective on the study. “True nonresponse is probably less than 20%, but many other patients are inadequate responders even if they are having partial response.” Dr. Silverberg, professor of dermatology and director of clinical research, at George Washington University, Washington, was not an investigator.
Robert Sidbury, MD, MPH, added, “When a patient doesn’t respond to a medication that you expect they should, we always ask ourselves why.” Dermatologists have long assumed that, as with biologics for psoriasis, low blood levels were to blame for dupilumab nonresponse, said Dr. Sidbury, who is division chief of dermatology at Seattle Children’s Hospital and was not involved with the study. “This study showed that there was no correlation between response and blood levels.”
In the study, Lotte S. Spekhorst, MD, of National Expertise Center for Atopic Dermatitis, department of dermatology and allergology, University Medical Center Utrecht (the Netherlands) and coinvestigators prospectively followed 295 consecutive adult patients with moderate AD who were treated with dupilumab for 1 year. All patients received the same loading (600 mg) and biweekly (300 mg) doses.
The median dupilumab level at 16 weeks was 86.6 mcg/mL, which is higher than serum levels observed with other monoclonal antibodies used for other indications, such as psoriasis and inflammatory bowel disease, the authors noted. More importantly, researchers found no significant relationship between median week 16 dupilumab levels and 1-year clinical responses measured either discretely (Eczema Area and Severity Index [EASI] < 50, 50, 75, or 90; P = .18) or as quartiles (P = .06).
“It may be that response is dependent on target availability of the IL-4R-alpha, with an interpatient variability producing heterogeneity in response,” the authors wrote. But because serum dupilumab levels were relatively high, they said, all patients’ IL-4R-alpha “was likely fully saturated” at 16 weeks.
“This would explain why serum dupilumab levels were not related to effectiveness,” they noted, “although we cannot rule out differential effects in the tissue associated with heterogeneity in serum dupilumab levels.”
The study helps explain why some patients do not fully respond to dupilumab, said Eric L. Simpson, MD, professor of dermatology, Oregon Health & Science University, Portland, who was not involved with the study.
“One hypothesis would be that drug serum levels differ due to metabolism or absorption reasons,” Dr. Simpson said in an interview. Results also suggest that heterogeneity in disease biology, such as other uninhibited cytokine pathways, might explain differences in clinical results. “Thus, more therapeutics that target different inflammatory pathways are needed to capture responses in patients not adequately responding to type 2 inflammatory blockade,” he said.
Assessing AEs
As with response levels, serum dupilumab levels at week 16 did not predict AEs including dupilumab-associated ocular surface disease (DAOSD), which impacted 46.4% of 216 patients who reported AEs. These findings also contradict what happens with biologics in other diseases such as psoriasis and inflammatory bowel disease, said Dr. Sidbury, wherein serum drug levels may predict both clinical response and side-effect risks.
A previous study showed that lowering dupilumab levels led to improvement in DAOSD. Authors of the current study therefore surmised that DAOSD development might be more associated with interpatient variability in IL-4R-alpha expression than with serum drug levels. “More research is necessary to confirm the hypothesis of interpatient variability of the IL-4Ra and the pharmacokinetics of dupilumab,” they concluded.
For now, said Dr. Sidbury, the study helps clinicians look beyond serum drug levels when patients respond inadequately to dupilumab. Moreover, added Dr. Silverberg, study results mean that physicians must find other ways to predict dupilumab response levels. “We need better predictors of clinical response – theranostic markers that we could test the patient to and understand how well they’re going to do,” he said.
Be it dupilumab or any other medication, he said, physicians lack even confirmatory biomarkers to reflect when a drug is working well. “Right now, we go with clinical assessments. But if it’s not drug levels, we have to figure out why some patients do markedly better than others.”
It was not unreasonable, Dr. Silverberg said, for the investigators to seek a biomarker in blood rather than tissue. “But in this disease, we believe that the more important place to look for biomarkers and drug levels would be in the skin itself. So we are still left with the issue” that drug levels in tissue might reflect response when serum levels do not.
The study was supported by grants from AbbVie, Eli Lilly, Leo Pharma, Pfizer, and Sanofi. Study patients participated in the BioDay Registry, which is sponsored by Sanofi, Regeneron, AbbVie, Eli Lilly, LEO Pharma, and Pfizer; the sponsors had no role in the study design and conduct. Dr. Spekhorst discloses receiving speaking fees from Abbvie outside the work; disclosures of other authors included receiving advisory, speaking consulting, and/or investigator fees from Sanofi Genzyme during the study. Several authors had no disclosures.
Dr. Simpson has been an investigator and consultant for Regeneron and Sanofi, makers of dupilumab. Dr. Silverberg has been an investigator, consultant, and speaker for Regeneron and Sanofi. Dr. Sidbury has been a clinical investigator for all dupilumab pediatric trials. (His institution has a contract with Regeneron and Sanofi, but he receives no money from the arrangement.)
The finding that serum levels, according to a study published in JAMA Dermatology.
The study results mean that researchers should continue exploring potential AD drugs with novel mechanisms to help patients who fail type 2 inflammatory inhibition, experts told this news organization. The search for accurate augurs of clinical performance also must continue.
Addressing inadequate response
Quantifying nonresponse and incomplete response levels with dupilumab is difficult, said Jonathan I. Silverberg, MD, PhD, MPH, offering perspective on the study. “True nonresponse is probably less than 20%, but many other patients are inadequate responders even if they are having partial response.” Dr. Silverberg, professor of dermatology and director of clinical research, at George Washington University, Washington, was not an investigator.
Robert Sidbury, MD, MPH, added, “When a patient doesn’t respond to a medication that you expect they should, we always ask ourselves why.” Dermatologists have long assumed that, as with biologics for psoriasis, low blood levels were to blame for dupilumab nonresponse, said Dr. Sidbury, who is division chief of dermatology at Seattle Children’s Hospital and was not involved with the study. “This study showed that there was no correlation between response and blood levels.”
In the study, Lotte S. Spekhorst, MD, of National Expertise Center for Atopic Dermatitis, department of dermatology and allergology, University Medical Center Utrecht (the Netherlands) and coinvestigators prospectively followed 295 consecutive adult patients with moderate AD who were treated with dupilumab for 1 year. All patients received the same loading (600 mg) and biweekly (300 mg) doses.
The median dupilumab level at 16 weeks was 86.6 mcg/mL, which is higher than serum levels observed with other monoclonal antibodies used for other indications, such as psoriasis and inflammatory bowel disease, the authors noted. More importantly, researchers found no significant relationship between median week 16 dupilumab levels and 1-year clinical responses measured either discretely (Eczema Area and Severity Index [EASI] < 50, 50, 75, or 90; P = .18) or as quartiles (P = .06).
“It may be that response is dependent on target availability of the IL-4R-alpha, with an interpatient variability producing heterogeneity in response,” the authors wrote. But because serum dupilumab levels were relatively high, they said, all patients’ IL-4R-alpha “was likely fully saturated” at 16 weeks.
“This would explain why serum dupilumab levels were not related to effectiveness,” they noted, “although we cannot rule out differential effects in the tissue associated with heterogeneity in serum dupilumab levels.”
The study helps explain why some patients do not fully respond to dupilumab, said Eric L. Simpson, MD, professor of dermatology, Oregon Health & Science University, Portland, who was not involved with the study.
“One hypothesis would be that drug serum levels differ due to metabolism or absorption reasons,” Dr. Simpson said in an interview. Results also suggest that heterogeneity in disease biology, such as other uninhibited cytokine pathways, might explain differences in clinical results. “Thus, more therapeutics that target different inflammatory pathways are needed to capture responses in patients not adequately responding to type 2 inflammatory blockade,” he said.
Assessing AEs
As with response levels, serum dupilumab levels at week 16 did not predict AEs including dupilumab-associated ocular surface disease (DAOSD), which impacted 46.4% of 216 patients who reported AEs. These findings also contradict what happens with biologics in other diseases such as psoriasis and inflammatory bowel disease, said Dr. Sidbury, wherein serum drug levels may predict both clinical response and side-effect risks.
A previous study showed that lowering dupilumab levels led to improvement in DAOSD. Authors of the current study therefore surmised that DAOSD development might be more associated with interpatient variability in IL-4R-alpha expression than with serum drug levels. “More research is necessary to confirm the hypothesis of interpatient variability of the IL-4Ra and the pharmacokinetics of dupilumab,” they concluded.
For now, said Dr. Sidbury, the study helps clinicians look beyond serum drug levels when patients respond inadequately to dupilumab. Moreover, added Dr. Silverberg, study results mean that physicians must find other ways to predict dupilumab response levels. “We need better predictors of clinical response – theranostic markers that we could test the patient to and understand how well they’re going to do,” he said.
Be it dupilumab or any other medication, he said, physicians lack even confirmatory biomarkers to reflect when a drug is working well. “Right now, we go with clinical assessments. But if it’s not drug levels, we have to figure out why some patients do markedly better than others.”
It was not unreasonable, Dr. Silverberg said, for the investigators to seek a biomarker in blood rather than tissue. “But in this disease, we believe that the more important place to look for biomarkers and drug levels would be in the skin itself. So we are still left with the issue” that drug levels in tissue might reflect response when serum levels do not.
The study was supported by grants from AbbVie, Eli Lilly, Leo Pharma, Pfizer, and Sanofi. Study patients participated in the BioDay Registry, which is sponsored by Sanofi, Regeneron, AbbVie, Eli Lilly, LEO Pharma, and Pfizer; the sponsors had no role in the study design and conduct. Dr. Spekhorst discloses receiving speaking fees from Abbvie outside the work; disclosures of other authors included receiving advisory, speaking consulting, and/or investigator fees from Sanofi Genzyme during the study. Several authors had no disclosures.
Dr. Simpson has been an investigator and consultant for Regeneron and Sanofi, makers of dupilumab. Dr. Silverberg has been an investigator, consultant, and speaker for Regeneron and Sanofi. Dr. Sidbury has been a clinical investigator for all dupilumab pediatric trials. (His institution has a contract with Regeneron and Sanofi, but he receives no money from the arrangement.)
The finding that serum levels, according to a study published in JAMA Dermatology.
The study results mean that researchers should continue exploring potential AD drugs with novel mechanisms to help patients who fail type 2 inflammatory inhibition, experts told this news organization. The search for accurate augurs of clinical performance also must continue.
Addressing inadequate response
Quantifying nonresponse and incomplete response levels with dupilumab is difficult, said Jonathan I. Silverberg, MD, PhD, MPH, offering perspective on the study. “True nonresponse is probably less than 20%, but many other patients are inadequate responders even if they are having partial response.” Dr. Silverberg, professor of dermatology and director of clinical research, at George Washington University, Washington, was not an investigator.
Robert Sidbury, MD, MPH, added, “When a patient doesn’t respond to a medication that you expect they should, we always ask ourselves why.” Dermatologists have long assumed that, as with biologics for psoriasis, low blood levels were to blame for dupilumab nonresponse, said Dr. Sidbury, who is division chief of dermatology at Seattle Children’s Hospital and was not involved with the study. “This study showed that there was no correlation between response and blood levels.”
In the study, Lotte S. Spekhorst, MD, of National Expertise Center for Atopic Dermatitis, department of dermatology and allergology, University Medical Center Utrecht (the Netherlands) and coinvestigators prospectively followed 295 consecutive adult patients with moderate AD who were treated with dupilumab for 1 year. All patients received the same loading (600 mg) and biweekly (300 mg) doses.
The median dupilumab level at 16 weeks was 86.6 mcg/mL, which is higher than serum levels observed with other monoclonal antibodies used for other indications, such as psoriasis and inflammatory bowel disease, the authors noted. More importantly, researchers found no significant relationship between median week 16 dupilumab levels and 1-year clinical responses measured either discretely (Eczema Area and Severity Index [EASI] < 50, 50, 75, or 90; P = .18) or as quartiles (P = .06).
“It may be that response is dependent on target availability of the IL-4R-alpha, with an interpatient variability producing heterogeneity in response,” the authors wrote. But because serum dupilumab levels were relatively high, they said, all patients’ IL-4R-alpha “was likely fully saturated” at 16 weeks.
“This would explain why serum dupilumab levels were not related to effectiveness,” they noted, “although we cannot rule out differential effects in the tissue associated with heterogeneity in serum dupilumab levels.”
The study helps explain why some patients do not fully respond to dupilumab, said Eric L. Simpson, MD, professor of dermatology, Oregon Health & Science University, Portland, who was not involved with the study.
“One hypothesis would be that drug serum levels differ due to metabolism or absorption reasons,” Dr. Simpson said in an interview. Results also suggest that heterogeneity in disease biology, such as other uninhibited cytokine pathways, might explain differences in clinical results. “Thus, more therapeutics that target different inflammatory pathways are needed to capture responses in patients not adequately responding to type 2 inflammatory blockade,” he said.
Assessing AEs
As with response levels, serum dupilumab levels at week 16 did not predict AEs including dupilumab-associated ocular surface disease (DAOSD), which impacted 46.4% of 216 patients who reported AEs. These findings also contradict what happens with biologics in other diseases such as psoriasis and inflammatory bowel disease, said Dr. Sidbury, wherein serum drug levels may predict both clinical response and side-effect risks.
A previous study showed that lowering dupilumab levels led to improvement in DAOSD. Authors of the current study therefore surmised that DAOSD development might be more associated with interpatient variability in IL-4R-alpha expression than with serum drug levels. “More research is necessary to confirm the hypothesis of interpatient variability of the IL-4Ra and the pharmacokinetics of dupilumab,” they concluded.
For now, said Dr. Sidbury, the study helps clinicians look beyond serum drug levels when patients respond inadequately to dupilumab. Moreover, added Dr. Silverberg, study results mean that physicians must find other ways to predict dupilumab response levels. “We need better predictors of clinical response – theranostic markers that we could test the patient to and understand how well they’re going to do,” he said.
Be it dupilumab or any other medication, he said, physicians lack even confirmatory biomarkers to reflect when a drug is working well. “Right now, we go with clinical assessments. But if it’s not drug levels, we have to figure out why some patients do markedly better than others.”
It was not unreasonable, Dr. Silverberg said, for the investigators to seek a biomarker in blood rather than tissue. “But in this disease, we believe that the more important place to look for biomarkers and drug levels would be in the skin itself. So we are still left with the issue” that drug levels in tissue might reflect response when serum levels do not.
The study was supported by grants from AbbVie, Eli Lilly, Leo Pharma, Pfizer, and Sanofi. Study patients participated in the BioDay Registry, which is sponsored by Sanofi, Regeneron, AbbVie, Eli Lilly, LEO Pharma, and Pfizer; the sponsors had no role in the study design and conduct. Dr. Spekhorst discloses receiving speaking fees from Abbvie outside the work; disclosures of other authors included receiving advisory, speaking consulting, and/or investigator fees from Sanofi Genzyme during the study. Several authors had no disclosures.
Dr. Simpson has been an investigator and consultant for Regeneron and Sanofi, makers of dupilumab. Dr. Silverberg has been an investigator, consultant, and speaker for Regeneron and Sanofi. Dr. Sidbury has been a clinical investigator for all dupilumab pediatric trials. (His institution has a contract with Regeneron and Sanofi, but he receives no money from the arrangement.)
FROM JAMA DERMATOLOGY