User login
Survivors of childhood cancers at increased risk for autoimmune diseases
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
FROM ANNALS OF RHEUMATIC DISEASES
Key clinical point: Survivors of childhood cancers, especially leukemia, Hodgkin lymphoma, and renal tumors, had a significantly increased risk of autoimmune disease.
Major finding: Compared with matched controls, survivors had a 1.4-fold increased risk for hospital contact concerning an autoimmune disease.
Data source: The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before age 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008.
Disclosures: Dr. Holmqvist and coauthors reported having no disclosures.
FDA finds long-term clopidogrel does not increase death or cancer risks
Long-term use of the blood-thinning agent clopidogrel did not alter the risk of death in people with heart disease or at risk of developing heart disease, nor did the drug appear to affect cancer risk, according to a statement from the U.S. Food and Drug Administration.
The FDA’s meta-analysis looked at results from 12 trials enrolling a total of 56,799 patients to evaluate the effect of long-term clopidogrel use on all-cause mortality. The incidence of all-cause mortality was 6.7% for the long-term clopidogrel plus aspirin arm and 6.6% for the comparator, resulting in a Mantel Haenszel Risk Difference (MH RD) of 0.04% (95% confidence interval, –0.35%-0.44%).
“The results indicate that long-term (12 months or longer) dual-antiplatelet therapy with clopidogrel and aspirin do not appear to change the overall risk of death, compared with short-term (6 months or less) clopidogrel and aspirin, or aspirin alone,” the agency said in its statement.
The FDA also conducted a meta-analysis looking at nine of these trials (n = 45,374) that had enrolled patients with coronary artery disease or patients at risk of CAD. This also suggested no difference in the risk of all-cause mortality (MH RD –0.07%; 95% CI, –0.43%- 0.29%).
The meta-analysis included results from the Dual-Antiplatelet Therapy Trial (DAPT), whose results included a worrisome safety signal for extended use of clopidogrel (N Engl J Med 2014; 371:2155-66). Patients in the DAPT underwent percutaneous coronary intervention and placement of a drug-eluting stent, after which they received 1 year of clopidogrel or prasugrel plus aspirin. About 1,000 patients were then randomized to 18 additional months of one of the dual-antiplatelet therapies or to aspirin plus placebo. Extended (30-month) use of clopidogrel plus aspirin was associated with a significantly increased risk of death (2.2% for 30 months vs. 1.5% for 12 months), whereas no increased risk was seen for prasugrel plus aspirin. A higher risk of death was mainly due to noncardiovascular causes, including cancer and trauma.
The DAPT did not show an increased risk of cancer-related adverse events related to treatment duration. However, the FDA performed two meta-analyses of other trials, with about 40,000 patients included in each analysis, to determine whether a signal could be found for either cancer-related adverse events or cancer-related death. Neither revealed an increased risk related to long-term clopidogrel use.
Long-term use of the blood-thinning agent clopidogrel did not alter the risk of death in people with heart disease or at risk of developing heart disease, nor did the drug appear to affect cancer risk, according to a statement from the U.S. Food and Drug Administration.
The FDA’s meta-analysis looked at results from 12 trials enrolling a total of 56,799 patients to evaluate the effect of long-term clopidogrel use on all-cause mortality. The incidence of all-cause mortality was 6.7% for the long-term clopidogrel plus aspirin arm and 6.6% for the comparator, resulting in a Mantel Haenszel Risk Difference (MH RD) of 0.04% (95% confidence interval, –0.35%-0.44%).
“The results indicate that long-term (12 months or longer) dual-antiplatelet therapy with clopidogrel and aspirin do not appear to change the overall risk of death, compared with short-term (6 months or less) clopidogrel and aspirin, or aspirin alone,” the agency said in its statement.
The FDA also conducted a meta-analysis looking at nine of these trials (n = 45,374) that had enrolled patients with coronary artery disease or patients at risk of CAD. This also suggested no difference in the risk of all-cause mortality (MH RD –0.07%; 95% CI, –0.43%- 0.29%).
The meta-analysis included results from the Dual-Antiplatelet Therapy Trial (DAPT), whose results included a worrisome safety signal for extended use of clopidogrel (N Engl J Med 2014; 371:2155-66). Patients in the DAPT underwent percutaneous coronary intervention and placement of a drug-eluting stent, after which they received 1 year of clopidogrel or prasugrel plus aspirin. About 1,000 patients were then randomized to 18 additional months of one of the dual-antiplatelet therapies or to aspirin plus placebo. Extended (30-month) use of clopidogrel plus aspirin was associated with a significantly increased risk of death (2.2% for 30 months vs. 1.5% for 12 months), whereas no increased risk was seen for prasugrel plus aspirin. A higher risk of death was mainly due to noncardiovascular causes, including cancer and trauma.
The DAPT did not show an increased risk of cancer-related adverse events related to treatment duration. However, the FDA performed two meta-analyses of other trials, with about 40,000 patients included in each analysis, to determine whether a signal could be found for either cancer-related adverse events or cancer-related death. Neither revealed an increased risk related to long-term clopidogrel use.
Long-term use of the blood-thinning agent clopidogrel did not alter the risk of death in people with heart disease or at risk of developing heart disease, nor did the drug appear to affect cancer risk, according to a statement from the U.S. Food and Drug Administration.
The FDA’s meta-analysis looked at results from 12 trials enrolling a total of 56,799 patients to evaluate the effect of long-term clopidogrel use on all-cause mortality. The incidence of all-cause mortality was 6.7% for the long-term clopidogrel plus aspirin arm and 6.6% for the comparator, resulting in a Mantel Haenszel Risk Difference (MH RD) of 0.04% (95% confidence interval, –0.35%-0.44%).
“The results indicate that long-term (12 months or longer) dual-antiplatelet therapy with clopidogrel and aspirin do not appear to change the overall risk of death, compared with short-term (6 months or less) clopidogrel and aspirin, or aspirin alone,” the agency said in its statement.
The FDA also conducted a meta-analysis looking at nine of these trials (n = 45,374) that had enrolled patients with coronary artery disease or patients at risk of CAD. This also suggested no difference in the risk of all-cause mortality (MH RD –0.07%; 95% CI, –0.43%- 0.29%).
The meta-analysis included results from the Dual-Antiplatelet Therapy Trial (DAPT), whose results included a worrisome safety signal for extended use of clopidogrel (N Engl J Med 2014; 371:2155-66). Patients in the DAPT underwent percutaneous coronary intervention and placement of a drug-eluting stent, after which they received 1 year of clopidogrel or prasugrel plus aspirin. About 1,000 patients were then randomized to 18 additional months of one of the dual-antiplatelet therapies or to aspirin plus placebo. Extended (30-month) use of clopidogrel plus aspirin was associated with a significantly increased risk of death (2.2% for 30 months vs. 1.5% for 12 months), whereas no increased risk was seen for prasugrel plus aspirin. A higher risk of death was mainly due to noncardiovascular causes, including cancer and trauma.
The DAPT did not show an increased risk of cancer-related adverse events related to treatment duration. However, the FDA performed two meta-analyses of other trials, with about 40,000 patients included in each analysis, to determine whether a signal could be found for either cancer-related adverse events or cancer-related death. Neither revealed an increased risk related to long-term clopidogrel use.
Dexamethasone reduces radiation therapy–induced pain flare
SAN ANTONIO – Dexamethasone given before radiotherapy for bone metastases reduced the risk for subsequent pain flare by 8.9% when compared with placebo in a double blind, randomized phase III trial.
Of the 148 patients treated with the steroid, 26.4% experienced a pain flare up to 10 days after an 8-Gy dose of radiation was given versus 35.3% of the 150 patients who had received placebo (P = .05) in an intent-to-treat analysis. The first 8-mg oral dose of dexamethasone was given at least 1 hour before the single shot of palliative radiotherapy and continued for 4 days.
“Bone metastases are very prevalent in advanced cancer,” Dr. Edward Chow of Sunnybrook Health Sciences Center in Toronto said at the annual meeting of the American Society for Radiation Oncology.
“Palliative radiotherapy is effective in the treatment of painful bone metastases but acute pain flare can occur,” he said. Previous research from three Canadian centers had shown that up to 40% of patients can experience an acute and temporary worsening of pain during, or for up to 10 days after, palliative radiotherapy.
As the impact of these pain flares can be severe, often interfering with patients’ daily activities and ability to function normally, as well as causing additional anxiety about the success of treatment, Dr. Chow and associates aimed to see if the anti-inflammatory action of dexamethasone might stop them from happening. Two prior pilot studies had suggested that it might, but a randomized controlled trial was needed.
The phase III trial (results also published in the Lancet Oncology to coincide with presentation at the meeting) was conducted between May 2011 and Dec 2014 at 23 Canadian centers. Just under 300 patients with a median age of 69 years who were due to undergo palliative radiation therapy were enrolled into the trial, of whom 28% had lung cancer, 25% had prostate cancer, and 22% had breast cancer. The remainder (25%) had other cancers, but these excluded hematologic malignancies since corticosteroids can be used as anticancer therapy in these patients.
Patients recorded their level of pain in a diary using a scale of 0, meaning no pain, to 10, meaning the worst possible pain, before radiation and then for 10 days after treatment. The primary endpoint was the per-patient incidence of pain flare, defined as either a two-point increase in the pain score without a reduction in analgesic use or a 25% or greater reduction in analgesic use without a reduction in the pain score.
Dr. Chow reported that pain flares occurring in the first 5 days of follow-up were significantly less common in the dexamethasone- than placebo-treated patients, at 19.5% and 30.7%, with an absolute difference of 11.1% (P = .03), but that there was no significant difference from days 6-10. Similar results were seen in a sensitivity analysis.
A secondary endpoint was the proportion of patients achieving an overall response to radiation therapy, which showed no difference between the groups. “Whether a patient developed a pain flare or not was not predictive of radiation response in either arm,” Dr. Chow reported.
Adverse effects were mostly grade 1 or 2 and there was no statistical difference between the two groups, he added. Three patients treated with dexamethasone experienced hyperglycemic events identified by biochemistry rather than clinical presentation, none of which required hospitalization. There were a similar number of deaths, 11 in the dexamethasone arm and 15 in the placebo arm, none of which were related to treatment.
Several validated measures were used to assess patient quality of life, including the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life QLQ-C15-PAL questionnaire, the EORTC QLQ-BM22 bone metastases module, and the Dexamethasone Symptom Questionnaire (DSQ). Results showed patients treated with dexamethasone had significant improvements in nausea, function interference, and appetite by day 10 and improved physical domains and sleep by day 42. There was also an indication of better DSQ depression scores at day 42 with the steroid treatment.
“Given how easy and inexpensive this treatment is we believe that it should become standard of care for patients getting palliative radiotherapy for painful bone metastases as it seems to improve both pain associated with radiation treatment and also quality of life,” said coinvestigator Dr. Alysa Fairchild of the Cross Cancer Institute in Edmonton in an interview.
“We believe that our study results are robust, and this is a fairly large sample size across many Canadian centers so we believe these results are practice changing,” she added. “Ideally it would be nice to be able to predict which of the patients treated with [radiation therapy] are going to experience a pain flare, but at present we are not able to do that, so we do believe that dexamethasone should be given to everybody undergoing this type of [radiation] treatment.”
In an editorial accompanying the published findings, however, Dr. Barry Laird and Dr. Marnie Fallon of the University of Edinburgh in Scotland, comment: “Although the findings are encouraging, caution is advised before dexamethasone is used routinely to prevent pain flares after radiotherapy.”
While they commend the research team for performing the trial in this advanced cancer patient population, they note that the small reduction in pain flares seen may not be sufficient to warrant routine treatment with dexamethasone. They point out that the number needed to treat (NNT) was high, at 9-11, and that other analgesics, such as strong opioids had lower NNT (3-4) and so could perhaps be used instead. Steroids can also have adverse effects on muscle mass and glycemic control, they observed.
Dr. Chow, Dr. Fairchild, and a third investigator reported having no disclosures. The study was funded by a grant from the Canadian Cancer Society Research Institute.
SAN ANTONIO – Dexamethasone given before radiotherapy for bone metastases reduced the risk for subsequent pain flare by 8.9% when compared with placebo in a double blind, randomized phase III trial.
Of the 148 patients treated with the steroid, 26.4% experienced a pain flare up to 10 days after an 8-Gy dose of radiation was given versus 35.3% of the 150 patients who had received placebo (P = .05) in an intent-to-treat analysis. The first 8-mg oral dose of dexamethasone was given at least 1 hour before the single shot of palliative radiotherapy and continued for 4 days.
“Bone metastases are very prevalent in advanced cancer,” Dr. Edward Chow of Sunnybrook Health Sciences Center in Toronto said at the annual meeting of the American Society for Radiation Oncology.
“Palliative radiotherapy is effective in the treatment of painful bone metastases but acute pain flare can occur,” he said. Previous research from three Canadian centers had shown that up to 40% of patients can experience an acute and temporary worsening of pain during, or for up to 10 days after, palliative radiotherapy.
As the impact of these pain flares can be severe, often interfering with patients’ daily activities and ability to function normally, as well as causing additional anxiety about the success of treatment, Dr. Chow and associates aimed to see if the anti-inflammatory action of dexamethasone might stop them from happening. Two prior pilot studies had suggested that it might, but a randomized controlled trial was needed.
The phase III trial (results also published in the Lancet Oncology to coincide with presentation at the meeting) was conducted between May 2011 and Dec 2014 at 23 Canadian centers. Just under 300 patients with a median age of 69 years who were due to undergo palliative radiation therapy were enrolled into the trial, of whom 28% had lung cancer, 25% had prostate cancer, and 22% had breast cancer. The remainder (25%) had other cancers, but these excluded hematologic malignancies since corticosteroids can be used as anticancer therapy in these patients.
Patients recorded their level of pain in a diary using a scale of 0, meaning no pain, to 10, meaning the worst possible pain, before radiation and then for 10 days after treatment. The primary endpoint was the per-patient incidence of pain flare, defined as either a two-point increase in the pain score without a reduction in analgesic use or a 25% or greater reduction in analgesic use without a reduction in the pain score.
Dr. Chow reported that pain flares occurring in the first 5 days of follow-up were significantly less common in the dexamethasone- than placebo-treated patients, at 19.5% and 30.7%, with an absolute difference of 11.1% (P = .03), but that there was no significant difference from days 6-10. Similar results were seen in a sensitivity analysis.
A secondary endpoint was the proportion of patients achieving an overall response to radiation therapy, which showed no difference between the groups. “Whether a patient developed a pain flare or not was not predictive of radiation response in either arm,” Dr. Chow reported.
Adverse effects were mostly grade 1 or 2 and there was no statistical difference between the two groups, he added. Three patients treated with dexamethasone experienced hyperglycemic events identified by biochemistry rather than clinical presentation, none of which required hospitalization. There were a similar number of deaths, 11 in the dexamethasone arm and 15 in the placebo arm, none of which were related to treatment.
Several validated measures were used to assess patient quality of life, including the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life QLQ-C15-PAL questionnaire, the EORTC QLQ-BM22 bone metastases module, and the Dexamethasone Symptom Questionnaire (DSQ). Results showed patients treated with dexamethasone had significant improvements in nausea, function interference, and appetite by day 10 and improved physical domains and sleep by day 42. There was also an indication of better DSQ depression scores at day 42 with the steroid treatment.
“Given how easy and inexpensive this treatment is we believe that it should become standard of care for patients getting palliative radiotherapy for painful bone metastases as it seems to improve both pain associated with radiation treatment and also quality of life,” said coinvestigator Dr. Alysa Fairchild of the Cross Cancer Institute in Edmonton in an interview.
“We believe that our study results are robust, and this is a fairly large sample size across many Canadian centers so we believe these results are practice changing,” she added. “Ideally it would be nice to be able to predict which of the patients treated with [radiation therapy] are going to experience a pain flare, but at present we are not able to do that, so we do believe that dexamethasone should be given to everybody undergoing this type of [radiation] treatment.”
In an editorial accompanying the published findings, however, Dr. Barry Laird and Dr. Marnie Fallon of the University of Edinburgh in Scotland, comment: “Although the findings are encouraging, caution is advised before dexamethasone is used routinely to prevent pain flares after radiotherapy.”
While they commend the research team for performing the trial in this advanced cancer patient population, they note that the small reduction in pain flares seen may not be sufficient to warrant routine treatment with dexamethasone. They point out that the number needed to treat (NNT) was high, at 9-11, and that other analgesics, such as strong opioids had lower NNT (3-4) and so could perhaps be used instead. Steroids can also have adverse effects on muscle mass and glycemic control, they observed.
Dr. Chow, Dr. Fairchild, and a third investigator reported having no disclosures. The study was funded by a grant from the Canadian Cancer Society Research Institute.
SAN ANTONIO – Dexamethasone given before radiotherapy for bone metastases reduced the risk for subsequent pain flare by 8.9% when compared with placebo in a double blind, randomized phase III trial.
Of the 148 patients treated with the steroid, 26.4% experienced a pain flare up to 10 days after an 8-Gy dose of radiation was given versus 35.3% of the 150 patients who had received placebo (P = .05) in an intent-to-treat analysis. The first 8-mg oral dose of dexamethasone was given at least 1 hour before the single shot of palliative radiotherapy and continued for 4 days.
“Bone metastases are very prevalent in advanced cancer,” Dr. Edward Chow of Sunnybrook Health Sciences Center in Toronto said at the annual meeting of the American Society for Radiation Oncology.
“Palliative radiotherapy is effective in the treatment of painful bone metastases but acute pain flare can occur,” he said. Previous research from three Canadian centers had shown that up to 40% of patients can experience an acute and temporary worsening of pain during, or for up to 10 days after, palliative radiotherapy.
As the impact of these pain flares can be severe, often interfering with patients’ daily activities and ability to function normally, as well as causing additional anxiety about the success of treatment, Dr. Chow and associates aimed to see if the anti-inflammatory action of dexamethasone might stop them from happening. Two prior pilot studies had suggested that it might, but a randomized controlled trial was needed.
The phase III trial (results also published in the Lancet Oncology to coincide with presentation at the meeting) was conducted between May 2011 and Dec 2014 at 23 Canadian centers. Just under 300 patients with a median age of 69 years who were due to undergo palliative radiation therapy were enrolled into the trial, of whom 28% had lung cancer, 25% had prostate cancer, and 22% had breast cancer. The remainder (25%) had other cancers, but these excluded hematologic malignancies since corticosteroids can be used as anticancer therapy in these patients.
Patients recorded their level of pain in a diary using a scale of 0, meaning no pain, to 10, meaning the worst possible pain, before radiation and then for 10 days after treatment. The primary endpoint was the per-patient incidence of pain flare, defined as either a two-point increase in the pain score without a reduction in analgesic use or a 25% or greater reduction in analgesic use without a reduction in the pain score.
Dr. Chow reported that pain flares occurring in the first 5 days of follow-up were significantly less common in the dexamethasone- than placebo-treated patients, at 19.5% and 30.7%, with an absolute difference of 11.1% (P = .03), but that there was no significant difference from days 6-10. Similar results were seen in a sensitivity analysis.
A secondary endpoint was the proportion of patients achieving an overall response to radiation therapy, which showed no difference between the groups. “Whether a patient developed a pain flare or not was not predictive of radiation response in either arm,” Dr. Chow reported.
Adverse effects were mostly grade 1 or 2 and there was no statistical difference between the two groups, he added. Three patients treated with dexamethasone experienced hyperglycemic events identified by biochemistry rather than clinical presentation, none of which required hospitalization. There were a similar number of deaths, 11 in the dexamethasone arm and 15 in the placebo arm, none of which were related to treatment.
Several validated measures were used to assess patient quality of life, including the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life QLQ-C15-PAL questionnaire, the EORTC QLQ-BM22 bone metastases module, and the Dexamethasone Symptom Questionnaire (DSQ). Results showed patients treated with dexamethasone had significant improvements in nausea, function interference, and appetite by day 10 and improved physical domains and sleep by day 42. There was also an indication of better DSQ depression scores at day 42 with the steroid treatment.
“Given how easy and inexpensive this treatment is we believe that it should become standard of care for patients getting palliative radiotherapy for painful bone metastases as it seems to improve both pain associated with radiation treatment and also quality of life,” said coinvestigator Dr. Alysa Fairchild of the Cross Cancer Institute in Edmonton in an interview.
“We believe that our study results are robust, and this is a fairly large sample size across many Canadian centers so we believe these results are practice changing,” she added. “Ideally it would be nice to be able to predict which of the patients treated with [radiation therapy] are going to experience a pain flare, but at present we are not able to do that, so we do believe that dexamethasone should be given to everybody undergoing this type of [radiation] treatment.”
In an editorial accompanying the published findings, however, Dr. Barry Laird and Dr. Marnie Fallon of the University of Edinburgh in Scotland, comment: “Although the findings are encouraging, caution is advised before dexamethasone is used routinely to prevent pain flares after radiotherapy.”
While they commend the research team for performing the trial in this advanced cancer patient population, they note that the small reduction in pain flares seen may not be sufficient to warrant routine treatment with dexamethasone. They point out that the number needed to treat (NNT) was high, at 9-11, and that other analgesics, such as strong opioids had lower NNT (3-4) and so could perhaps be used instead. Steroids can also have adverse effects on muscle mass and glycemic control, they observed.
Dr. Chow, Dr. Fairchild, and a third investigator reported having no disclosures. The study was funded by a grant from the Canadian Cancer Society Research Institute.
AT THE ASTRO ANNUAL MEETING
Key clinical point:Pain flares associated with radiotherapy for bone metastases could be managed by giving dexamethasone.
Major finding: Fewer patients given dexamethasone experienced pain flares 10 days after receiving palliative radiotherapy (35% vs. 26% for placebo, P = .05)
Data source: Double-blind, placebo-controlled, randomized phase III trial of 298 cancer patients treated at 23 Canadian centers between May 2011 and Dec 2014.
Disclosures: Dr. Chow, Dr. Fairchild, and a third investigator reported having no disclosures. The study was funded by a grant from the Canadian Cancer Society Research Institute.
NCCN unveils 'Evidence Blocks' to facilitate treatment discussions
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
SAN FRANCISCO – The National Comprehensive Cancer Network (NCCN) has introduced an easy-to-use visual tool called Evidence Blocks to help physicians and patients compare various treatment options and individualize the selection among them.
“This information can serve as a starting point for shared decision making between the patient and health care team based on individual patients’ value systems,” chief executive officer Dr. Robert W. Carlson said at the NCCN Annual Congress: Hematologic Malignancies, where the tool was unveiled in a session and related press conference.
The first two NCCN guidelines to incorporate the Evidence Blocks – those for multiple myeloma and chronic myelogenous leukemia – were released at the same time. The organization hopes to incorporate them into all of its guidelines by early 2017, he said.
Development of the Evidence Blocks
The NCCN developed the Evidence Blocks to address requests from various stakeholders, according to Dr. Carlson. Guideline users wanted to know more about the rationale behind recommended therapies, asked for inclusion of information on costs, and sought an aid that would allow patients to make decisions based on their individual values.
“The patient perception of value is what should be most important to us,” he commented. “But even among patients, the concept of value differs greatly from patient to patient,” based on factors such as age, comorbidities, treatment goals, and health insurance coverage.
Each Evidence Block graphically displays five measures of information on a recommended therapy: efficacy, safety, quality of the evidence supporting the recommendation, consistency of the evidence supporting the recommendation, and affordability. Each column in the block represents one measure.
Blue shading indicates panelists’ average numeric score for the therapy on that measure rounded to the nearest integer, ranging from 1 (least favorable) to 5 (most favorable). Therefore, the more shading a therapy has, the more favorable its score.
The Evidence Blocks are added to the guidelines and aligned vertically on pages. “This display of the information graphically allows for very efficient scanning of multiple options for therapy. Comparisons across several regimens can be done very quickly and intuitively,” Dr. Carlson noted.
“We believe that the presentation of this type of information allows the health care provider and patient to make their own judgments of the value of specific interventions,” he added.
The affordability measure has generated the most discussion among panelists and stakeholders, according to Dr. Carlson. For this measure, panelists estimated the total cost of care for a therapy, including the costs of drugs, administration, required supportive care, toxicity monitoring, and care associated with management of toxicity. Scores range from very expensive to very inexpensive.
“We don’t use a dollar amount. Rather, it’s sort of what’s the total cost to society, if you will, of the medical intervention part of this,” he explained. “It’s important to understand that these estimates are not necessarily what a patient would pay because many patients have insurance programs that cover all of this cost.… However, we felt it was important to give patients as well as providers an estimate of what the overall magnitude of expense is because there are patients who have huge deductibles, there’s the doughnut hole within Medicare, and there are patients who have no insurance.”
The Evidence Blocks may help address a “conspiracy of silence” between physicians and patients when it comes to discussing treatment costs, whereby neither party wants to bring up this thorny issue, according to Dr. Carlson. “The Evidence Blocks demystify the discussion of cost because the affordability issue is there in front of you. So it gives people permission to talk about cost and affordability.”
It should be relatively easy to teach patients to use the Evidence Blocks. “I think you’ll find your patients will actually be interested in this and that they will not have as much difficulty interpreting this as you think they will, because the patient advocacy groups and the patient advocates that we have spoken with about this, they get this almost instantly,” he said.
Oncologist perspective
There is a critical need for tools such as the Evidence Blocks in making treatment decisions today, according to Dr. George Somlo, professor in the department of medical oncology and therapeutics research at the City of Hope Comprehensive Cancer Center in Duarte, Calif., and also a member of the NCCN multiple myeloma and breast cancer guideline panels.
Treatment options for multiple myeloma, as for many cancers, have exploded in the past few decades, he noted. “How do you go from making sense of having two drugs with a very poor outcome predicted to having literally dozens of agents approved and used in combination, and in essence being at the verge of curing patients with multiple myeloma?”
Dr. Somlo agreed that inclusion of costs in the Evidence Blocks would likely be beneficial as a conversation starter, recalling, “I’ve had patients who did not fill their prescription for a potentially curative medication because they were worried about the $2,500 or $3,500 copay.”
Patient-physician discussion will be important when it comes to using information from the new tool, he said. For example, in the NCCN guideline for multiple myeloma, some of the first-line regimens have identical Evidence Blocks; thus, consideration of factors such as comorbidities will become important.
“This kind of evidence-based scoring system can guide that kind of discussion with the patient and can tailor the individual therapeutic regimens,” he concluded.
Patient perspective
Breast cancer survivor Marta Nichols, who is vice president of investor relations at GoDaddy and a member of the California Breast Cancer Research Council based in San Francisco, welcomed the Evidence Blocks as a tool that will allow patients to make more informed decisions according to what matters most to them.
Only 33 years old at diagnosis, she and her husband had just begun to think about starting a family. “So my primary concern coming into my physician’s office was my fertility and what impact the treatment would have on my fertility. Certainly most physicians are concerned with efficacy – they want to see you survive. My concern was not just surviving, but also thriving and being able to give birth to children down the line,” she explained.
Patients today are overwhelmed not only by their cancer diagnosis, but also by the many treatment options and the new emphasis on shared decision making, Ms. Nichols noted. And that’s where the Evidence Blocks can make a difference.
“When I was diagnosed, it would have been hugely helpful for me to have information laid out in this very clear and systematic way… It would have given us the ability to make a much more informed decision,” she commented.
Multiple myeloma survivor Donald B. Orosco, who is president and chief financial officer of Orosco & Associates and owner of Monterey (Calif.) Speed and Sport, agreed, noting that his priorities when given the diagnosis more than two decades ago at age 47 differed somewhat.
“I adopted the feeling early on that I probably wasn’t going to see a cure for the disease in my lifetime, but I could accept that,” he elaborated. “I just said ‘Really, I’m interested in quality-of-life issues. I’d like to see my kids go into high school or possibly college.’ So I adopted [an approach of] trying to find something for me that would keep me alive and give me a relatively comfortable quality of life, that would allow me to continue to race cars or do whatever I had to do.”
Dr. Carlson, Dr. Somlo, Ms. Nichols, and Mr. Orosco disclosed no relevant conflicts of interest.
AT NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Prolonged zoledronic acid-induced hypocalcemia in hypercalcemia of malignancy
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Cancer-related pain management in clinical oncology
Uncontrolled pain is one of the most feared and debilitating symptoms among cancer patients, and many suffer unnecessarily from suboptimal pain control. Cancer-related pain is often multidimensional and can affect all aspects of a patient’s life. Hence, achieving adequate pain relief among cancer patients involves a proper assessment of psychosocial, spiritual, and physical pain issues, matched with an individualized treatment plan involving pharmacologic, nonpharmacologic, and procedural therapies when appropriate. Providing effective pain relief can help ease the overall burden of disease among oncology patients while helping them tolerate cancer-directed therapies and achieve the most optimal quality of life throughout all phases of the disease continuum. In this review, the authors will discuss the syndromes, assessment of, and treatment for cancer-related pain in the outpatient setting.
Click on the PDF icon at the top of this introduction to read the full article.
Uncontrolled pain is one of the most feared and debilitating symptoms among cancer patients, and many suffer unnecessarily from suboptimal pain control. Cancer-related pain is often multidimensional and can affect all aspects of a patient’s life. Hence, achieving adequate pain relief among cancer patients involves a proper assessment of psychosocial, spiritual, and physical pain issues, matched with an individualized treatment plan involving pharmacologic, nonpharmacologic, and procedural therapies when appropriate. Providing effective pain relief can help ease the overall burden of disease among oncology patients while helping them tolerate cancer-directed therapies and achieve the most optimal quality of life throughout all phases of the disease continuum. In this review, the authors will discuss the syndromes, assessment of, and treatment for cancer-related pain in the outpatient setting.
Click on the PDF icon at the top of this introduction to read the full article.
Uncontrolled pain is one of the most feared and debilitating symptoms among cancer patients, and many suffer unnecessarily from suboptimal pain control. Cancer-related pain is often multidimensional and can affect all aspects of a patient’s life. Hence, achieving adequate pain relief among cancer patients involves a proper assessment of psychosocial, spiritual, and physical pain issues, matched with an individualized treatment plan involving pharmacologic, nonpharmacologic, and procedural therapies when appropriate. Providing effective pain relief can help ease the overall burden of disease among oncology patients while helping them tolerate cancer-directed therapies and achieve the most optimal quality of life throughout all phases of the disease continuum. In this review, the authors will discuss the syndromes, assessment of, and treatment for cancer-related pain in the outpatient setting.
Click on the PDF icon at the top of this introduction to read the full article.
How to fix clinical trial accrual
Editor Jame Abraham argues that once there is appropriate clinical trial infrastructure, there is only one person who can increase the clinical trial accrual: the treating oncologist.
Click on the PDF icon at the top of this introduction to read the full article.
Editor Jame Abraham argues that once there is appropriate clinical trial infrastructure, there is only one person who can increase the clinical trial accrual: the treating oncologist.
Click on the PDF icon at the top of this introduction to read the full article.
Editor Jame Abraham argues that once there is appropriate clinical trial infrastructure, there is only one person who can increase the clinical trial accrual: the treating oncologist.
Click on the PDF icon at the top of this introduction to read the full article.
Decline in antibiotic effectiveness could harm surgical, chemotherapy patients
An increase of surgical site infections (SSIs) stemming from pathogens resistant to antibiotic prophylaxis could result in thousands of infection-related deaths in surgical and chemotherapy patients, according to a new study published in the Lancet Infectious Diseases.
A total of 31 published meta-analyses of randomized or quasi–randomized controlled trials were included in the study by Dr. Ramanan Laxminarayan of the Center for Disease Dynamics, Economics & Policy in Washington, and his associates. The researchers surveyed the 10 most common surgeries in which antibiotic prophylaxis provides the greatest benefit. The infection rate in surgical patients receiving prophylaxis was 4.2%, and was 11.1% in patients who did not receive prophylaxis. Relative risk reduction for infection was least in cancer chemotherapy at 35% and greatest in pacemaker implantation at 86%.
Between 38.7% and 50.9% of SSIs and 26.8% of infections after chemotherapy are caused by antibiotic-resistant pathogens. A decrease in prophylaxis effectiveness of 10% would cause 40,000 additional infections and 2,100 additional deaths, while a decrease in effectiveness of 70% would cause 280,000 additional infections and 15,000 additional deaths.
The authors say more data are needed to establish how antibiotic prophylaxis recommendations should be modified in the context of increasing rates of resistance.
In a related comment, Dr. Joshua Wolf from St. Jude Children’s Research Hospital, Memphis, said, “To improve stewardship outcomes, we need more research that focuses on understanding impediments to appropriate antibiotic prescribing, strategies that target these impediments, resources to implement the strategies, and leadership that understands the urgency and complexity of the task. In view of the lack of progress so far, mandatory implementation of these steps could be necessary to achieve notable change.”
Find the full study in the Lancet Infectious Diseases (doi: 10.1016/S1473-3099[15]00270-4).
An increase of surgical site infections (SSIs) stemming from pathogens resistant to antibiotic prophylaxis could result in thousands of infection-related deaths in surgical and chemotherapy patients, according to a new study published in the Lancet Infectious Diseases.
A total of 31 published meta-analyses of randomized or quasi–randomized controlled trials were included in the study by Dr. Ramanan Laxminarayan of the Center for Disease Dynamics, Economics & Policy in Washington, and his associates. The researchers surveyed the 10 most common surgeries in which antibiotic prophylaxis provides the greatest benefit. The infection rate in surgical patients receiving prophylaxis was 4.2%, and was 11.1% in patients who did not receive prophylaxis. Relative risk reduction for infection was least in cancer chemotherapy at 35% and greatest in pacemaker implantation at 86%.
Between 38.7% and 50.9% of SSIs and 26.8% of infections after chemotherapy are caused by antibiotic-resistant pathogens. A decrease in prophylaxis effectiveness of 10% would cause 40,000 additional infections and 2,100 additional deaths, while a decrease in effectiveness of 70% would cause 280,000 additional infections and 15,000 additional deaths.
The authors say more data are needed to establish how antibiotic prophylaxis recommendations should be modified in the context of increasing rates of resistance.
In a related comment, Dr. Joshua Wolf from St. Jude Children’s Research Hospital, Memphis, said, “To improve stewardship outcomes, we need more research that focuses on understanding impediments to appropriate antibiotic prescribing, strategies that target these impediments, resources to implement the strategies, and leadership that understands the urgency and complexity of the task. In view of the lack of progress so far, mandatory implementation of these steps could be necessary to achieve notable change.”
Find the full study in the Lancet Infectious Diseases (doi: 10.1016/S1473-3099[15]00270-4).
An increase of surgical site infections (SSIs) stemming from pathogens resistant to antibiotic prophylaxis could result in thousands of infection-related deaths in surgical and chemotherapy patients, according to a new study published in the Lancet Infectious Diseases.
A total of 31 published meta-analyses of randomized or quasi–randomized controlled trials were included in the study by Dr. Ramanan Laxminarayan of the Center for Disease Dynamics, Economics & Policy in Washington, and his associates. The researchers surveyed the 10 most common surgeries in which antibiotic prophylaxis provides the greatest benefit. The infection rate in surgical patients receiving prophylaxis was 4.2%, and was 11.1% in patients who did not receive prophylaxis. Relative risk reduction for infection was least in cancer chemotherapy at 35% and greatest in pacemaker implantation at 86%.
Between 38.7% and 50.9% of SSIs and 26.8% of infections after chemotherapy are caused by antibiotic-resistant pathogens. A decrease in prophylaxis effectiveness of 10% would cause 40,000 additional infections and 2,100 additional deaths, while a decrease in effectiveness of 70% would cause 280,000 additional infections and 15,000 additional deaths.
The authors say more data are needed to establish how antibiotic prophylaxis recommendations should be modified in the context of increasing rates of resistance.
In a related comment, Dr. Joshua Wolf from St. Jude Children’s Research Hospital, Memphis, said, “To improve stewardship outcomes, we need more research that focuses on understanding impediments to appropriate antibiotic prescribing, strategies that target these impediments, resources to implement the strategies, and leadership that understands the urgency and complexity of the task. In view of the lack of progress so far, mandatory implementation of these steps could be necessary to achieve notable change.”
Find the full study in the Lancet Infectious Diseases (doi: 10.1016/S1473-3099[15]00270-4).
Big declines seen in aspergillosis mortality
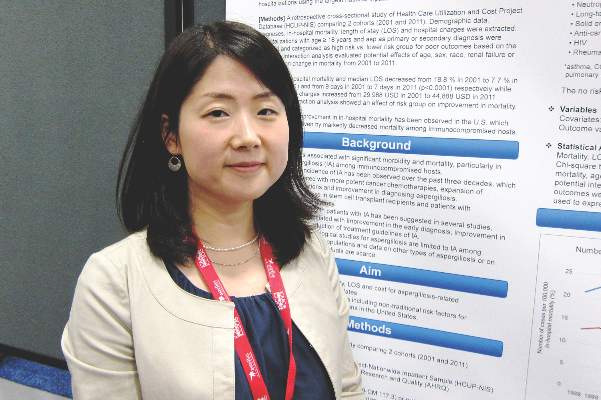
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
SAN DIEGO – In-hospital mortality in patients with aspergillosis plummeted nationally, according to data from 2001-2011, with the biggest improvement seen in immunocompromised patients traditionally considered at high mortality risk, Dr. Masako Mizusawa reported at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
The decline in in-hospital mortality wasn’t linear. Rather, it followed a stepwise pattern, and those steps occurred in association with three major advances during the study years: Food and Drug Administration approval of voriconazole in 2002, the FDA’s 2003 approval of the galactomannan serologic assay allowing for speedier diagnosis of aspergillosis, and the 2008 Infectious Diseases Society of America clinical practice guidelines on the treatment of aspergillosis (Clin Infect Dis. 2008 Feb 1;46[3]:327-60).
“This was an observational study and we can’t actually say that these events are causative. But just looking at the time relationship, it certainly looks plausible,” Dr. Mizusawa said.
In addition, the median hospital length of stay decreased from 9 to 7 days in patients with this potentially life-threatening infection, noted Dr. Mizusawa of Tufts Medical Center, Boston.
She presented what she believes is the largest U.S. longitudinal study of hospital care for aspergillosis. The retrospective study used nationally representative data from the Agency for Healthcare Research and Quality’s Healthcare Utilization and Cost Project–Nationwide Inpatient Sample.
Dr. Mizusawa and coinvestigators defined aspergillosis patients as being at high mortality risk if they had established risk factors indicative of immunocompromise, including hematologic malignancy, neutropenia, recent stem cell or solid organ transplantation, HIV, or rheumatologic disease. Patients at lower mortality risk included those with asthma, COPD, diabetes, malnutrition, pulmonary tuberculosis, or non-TB mycobacterial infection.
The proportion of patients who were high risk climbed over the years, from 41% among the 892 patients with aspergillosis-related hospitalization in the 2001 sample to 50% among 1,420 patients in 2011. Yet in-hospital mortality in high-risk patients fell from 26.4% in 2001 to 9.1% in 2011. Meanwhile, the mortality rate in lower-risk patients improved from 14.6% to 6.6%. The overall in-hospital mortality rate went from 18.8% to 7.7%.
Of note, the proportion of aspergillosis patients with renal failure jumped from 9.8% in 2001 to 21.5% in 2011, even though the treatments for aspergillosis are relatively non-nephrotoxic, with the exception of amphotericin B. The outlook for these patients has improved greatly: In-hospital mortality for aspergillosis patients in renal failure went from 40.2% in 2001 to 16.1% in 2011.
While in-hospital mortality and length of stay were decreasing during the study years, total hospital charges for patients with aspergillosis were going up: from a median of $29,998 in 2001 to $44,888 in 2001 dollars a decade later. This cost-of-care increase was confined to patients at lower baseline risk or with no risk factors. Somewhat surprisingly, the high-risk group didn’t have a significant increase in hospital charges over the 10-year period.
“Maybe we’re just doing a better job of treating them, so they may not necessarily have to use a lot of resources,” Dr. Mizusawa offered as explanation.
She reported having no financial conflicts regarding this unfunded study.
AT ICAAC 2015
Key clinical point: In-hospital mortality has more than halved for patients with aspergillosis-related hospitalization during a recent 10-year period.
Major finding: In-hospital mortality among patients with an aspergillosis-related hospitalization fell nationally from 18.8% in 2001 to 7.7% in 2011, with the biggest drop occurring in those at high risk.
Data source: A retrospective study of nationally representative data from the Healthcare Utilization and Cost Project–Nationwide Inpatient Sample for 2001-2011.
Disclosures: The presenter reported having no financial conflicts regarding this unfunded study.
Noninvasive ventilation no better than oxygen alone in immunocompromised ICU patients
Early noninvasive ventilation, compared with oxygen therapy alone, did not reduce 28-day all-cause mortality in critically ill immunocompromised patients with acute respiratory failure, based on a randomized, parallel-group study of 374 patients conducted in 28 ICUs in France and Belgium.
Overall, 46 of 191 patients (24%) in the noninvasive ventilation group died, compared with 50 of 183 (27%) in the oxygen-alone group. A similar number of patients from each group required intubation – 38% in the noninvasive ventilation group and 45% in the oxygen group – with similar time to intubation. Nearly 85% of the patients were receiving treatment for hematologic malignancies or solid tumors, researchers reported in a study published online Oct. 7 in JAMA.
No significant differences between groups were observed in requirement for intubation, ICU or hospital length of stay, or duration of invasive mechanical ventilation. The study found no evidence that noninvasive ventilation influenced mortality estimates or was beneficial to any subgroup based on hypoxemia severity or underlying condition.
The study was limited, however, by a lower than expected mortality rate with oxygen alone, and as a result was not powered to detect significant between-group differences. Based on earlier studies, the researchers assumed a 35% mortality rate in the oxygen-alone group, but the actual rate was 27% (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12402).
“Therefore, there remains uncertainty regarding our null finding, which may nonetheless fail to exclude a clinically important effect,” wrote Dr. Virginie Lemiale of Saint-Louis University Hospital, Paris, and colleagues.
Furthermore, high-flow nasal oxygen was used in about 40% of all patients, which may have decreased requirements for intubation as well as mortality rates. High-flow nasal oxygen was used more often in the oxygen group (44%) than in the noninvasive ventilation group (31%) (P = .01).
Dr. Lemiale and coauthors reported having no disclosures.
In contrast to reports from 10 years ago, the current study by Lemiale et al. failed to demonstrate a mortality benefit for noninvasive ventilation, compared with oxygen alone. However, the results should be interpreted in the context of recent advances in ICU care. Targeted chemotherapy, prophylactic use of antibiotics, and improved supportive care have contributed to overall mortality declines in the immunocompromised critically ill population. Dr. Lemiale and colleagues anticipated a higher baseline mortality rate (35% vs. 27% observed). The lower mortality rate limited the study’s power to detect a mortality difference between groups.
Second, patients in this trial may have had a lower acuity of illness, evidenced by less tachypnea, compared with that seen in earlier studies.
Third, the oxygen-alone group received more high-flow oxygen via nasal cannula than the noninvasive ventilation group, which may have diluted the benefits of noninvasive ventilation.
As efforts continue to reduce requirements for invasive mechanical ventilation, further examination of strategies for noninvasive ventilation, such as high-flow oxygen, compared with noninvasive ventilation, are warranted.
Dr. Bhakti Patel is a clinical instructor of medicine in the section of pulmonary and critical care, department of medicine, University of Chicago. Dr. John Kress is professor of medicine and director of the Medical Intensive Care Unit at University of Chicago Medicine. These remarks were part of an editorial accompanying the report (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12401). Dr. Patel and Dr. Kress reported having no disclosures.
In contrast to reports from 10 years ago, the current study by Lemiale et al. failed to demonstrate a mortality benefit for noninvasive ventilation, compared with oxygen alone. However, the results should be interpreted in the context of recent advances in ICU care. Targeted chemotherapy, prophylactic use of antibiotics, and improved supportive care have contributed to overall mortality declines in the immunocompromised critically ill population. Dr. Lemiale and colleagues anticipated a higher baseline mortality rate (35% vs. 27% observed). The lower mortality rate limited the study’s power to detect a mortality difference between groups.
Second, patients in this trial may have had a lower acuity of illness, evidenced by less tachypnea, compared with that seen in earlier studies.
Third, the oxygen-alone group received more high-flow oxygen via nasal cannula than the noninvasive ventilation group, which may have diluted the benefits of noninvasive ventilation.
As efforts continue to reduce requirements for invasive mechanical ventilation, further examination of strategies for noninvasive ventilation, such as high-flow oxygen, compared with noninvasive ventilation, are warranted.
Dr. Bhakti Patel is a clinical instructor of medicine in the section of pulmonary and critical care, department of medicine, University of Chicago. Dr. John Kress is professor of medicine and director of the Medical Intensive Care Unit at University of Chicago Medicine. These remarks were part of an editorial accompanying the report (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12401). Dr. Patel and Dr. Kress reported having no disclosures.
In contrast to reports from 10 years ago, the current study by Lemiale et al. failed to demonstrate a mortality benefit for noninvasive ventilation, compared with oxygen alone. However, the results should be interpreted in the context of recent advances in ICU care. Targeted chemotherapy, prophylactic use of antibiotics, and improved supportive care have contributed to overall mortality declines in the immunocompromised critically ill population. Dr. Lemiale and colleagues anticipated a higher baseline mortality rate (35% vs. 27% observed). The lower mortality rate limited the study’s power to detect a mortality difference between groups.
Second, patients in this trial may have had a lower acuity of illness, evidenced by less tachypnea, compared with that seen in earlier studies.
Third, the oxygen-alone group received more high-flow oxygen via nasal cannula than the noninvasive ventilation group, which may have diluted the benefits of noninvasive ventilation.
As efforts continue to reduce requirements for invasive mechanical ventilation, further examination of strategies for noninvasive ventilation, such as high-flow oxygen, compared with noninvasive ventilation, are warranted.
Dr. Bhakti Patel is a clinical instructor of medicine in the section of pulmonary and critical care, department of medicine, University of Chicago. Dr. John Kress is professor of medicine and director of the Medical Intensive Care Unit at University of Chicago Medicine. These remarks were part of an editorial accompanying the report (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12401). Dr. Patel and Dr. Kress reported having no disclosures.
Early noninvasive ventilation, compared with oxygen therapy alone, did not reduce 28-day all-cause mortality in critically ill immunocompromised patients with acute respiratory failure, based on a randomized, parallel-group study of 374 patients conducted in 28 ICUs in France and Belgium.
Overall, 46 of 191 patients (24%) in the noninvasive ventilation group died, compared with 50 of 183 (27%) in the oxygen-alone group. A similar number of patients from each group required intubation – 38% in the noninvasive ventilation group and 45% in the oxygen group – with similar time to intubation. Nearly 85% of the patients were receiving treatment for hematologic malignancies or solid tumors, researchers reported in a study published online Oct. 7 in JAMA.
No significant differences between groups were observed in requirement for intubation, ICU or hospital length of stay, or duration of invasive mechanical ventilation. The study found no evidence that noninvasive ventilation influenced mortality estimates or was beneficial to any subgroup based on hypoxemia severity or underlying condition.
The study was limited, however, by a lower than expected mortality rate with oxygen alone, and as a result was not powered to detect significant between-group differences. Based on earlier studies, the researchers assumed a 35% mortality rate in the oxygen-alone group, but the actual rate was 27% (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12402).
“Therefore, there remains uncertainty regarding our null finding, which may nonetheless fail to exclude a clinically important effect,” wrote Dr. Virginie Lemiale of Saint-Louis University Hospital, Paris, and colleagues.
Furthermore, high-flow nasal oxygen was used in about 40% of all patients, which may have decreased requirements for intubation as well as mortality rates. High-flow nasal oxygen was used more often in the oxygen group (44%) than in the noninvasive ventilation group (31%) (P = .01).
Dr. Lemiale and coauthors reported having no disclosures.
Early noninvasive ventilation, compared with oxygen therapy alone, did not reduce 28-day all-cause mortality in critically ill immunocompromised patients with acute respiratory failure, based on a randomized, parallel-group study of 374 patients conducted in 28 ICUs in France and Belgium.
Overall, 46 of 191 patients (24%) in the noninvasive ventilation group died, compared with 50 of 183 (27%) in the oxygen-alone group. A similar number of patients from each group required intubation – 38% in the noninvasive ventilation group and 45% in the oxygen group – with similar time to intubation. Nearly 85% of the patients were receiving treatment for hematologic malignancies or solid tumors, researchers reported in a study published online Oct. 7 in JAMA.
No significant differences between groups were observed in requirement for intubation, ICU or hospital length of stay, or duration of invasive mechanical ventilation. The study found no evidence that noninvasive ventilation influenced mortality estimates or was beneficial to any subgroup based on hypoxemia severity or underlying condition.
The study was limited, however, by a lower than expected mortality rate with oxygen alone, and as a result was not powered to detect significant between-group differences. Based on earlier studies, the researchers assumed a 35% mortality rate in the oxygen-alone group, but the actual rate was 27% (JAMA. 2015 Oct 7. doi: 10.1001/jama.2015.12402).
“Therefore, there remains uncertainty regarding our null finding, which may nonetheless fail to exclude a clinically important effect,” wrote Dr. Virginie Lemiale of Saint-Louis University Hospital, Paris, and colleagues.
Furthermore, high-flow nasal oxygen was used in about 40% of all patients, which may have decreased requirements for intubation as well as mortality rates. High-flow nasal oxygen was used more often in the oxygen group (44%) than in the noninvasive ventilation group (31%) (P = .01).
Dr. Lemiale and coauthors reported having no disclosures.
Key clinical point: Noninvasive ventilation, compared with oxygen therapy alone, did not reduce 28-day mortality among immunocompromised patients with acute respiratory failure.
Major finding: After 28 days, 46 of 191 patients (24%) in the noninvasive ventilation group had died, compared with 50 of 183 (27%) in the oxygen-alone group.
Data source: The randomized, parallel-group study was conducted in 28 ICUs in France and Belgium and included 374 immunocompromised patients with acute respiratory failure.
Disclosures: Dr. Lemiale and coauthors reported having no disclosures.