User login
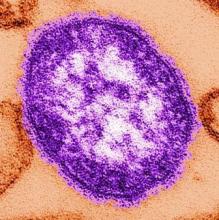
Maternal protection against measles steadily declines prior to vaccination
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
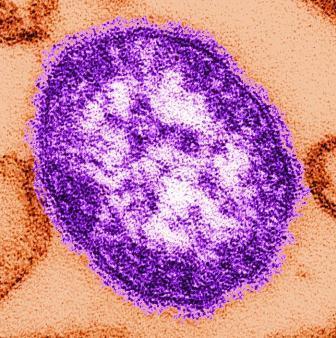
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
FROM VACCINE
Pneumococcal conjugate vaccines modestly reduce complex acute otitis media
Incidence rate ratios of children hospitalized with acute otitis media (hAOM) or more advanced stages, such as mastoidismus and acute mastoiditis (M+AM) declined by 10% and 20%, respectively, after introduction of pneumococcal conjugate vaccines (PCV) in the central region of Denmark, reported Bjarke B. Laursen of Aarhus University in Denmark, and associates.
The use of antibiotics for AOM prior to hospitalization increased markedly during the study period, and that may have impacted the modest reduction in hAOM and M+AM, the researchers said.
Incidence of Streptococcus pneumoniae cases decreased from 38% in the prevaccine era to 31% in the PCV-7 era and decreased even more to 16% in the PCV-13 era. The incidence of the second most frequently isolated bacteria, group A streptococcus (GAS), fell from 17% in the prevaccine era to 16% in the PCV-13 era, becoming equal to S. pneumoniae. The “no growth” results rose from 12% in the prevaccine era to 38% and 44% in the PCV-7 and PCV-13 eras, respectively (Int J Pediatr Otorhinolaryngol. 2017 Jul 4. doi: 10.1016/j.ijporl.2017.07.002) .
In the M+AM group, S. pneumoniae–positive cases fell to 10% in the PCV-13 era, compared with 44% in the prevaccine era and 41% in the PCV-7 era. A rise in GAS-positive cultures was seen in the M+AM group, from 15% in the prevaccine era to 30% in the PCV-13 era. The “no growth” group rose in incidence from 13% of cases in the prevaccine era to 26% in the PCV-7 era and 33% in the PCV-13 era.
“This microbiological shift is worrisome, because GAS may cause very serious infections due to its invasive nature,” Dr. Laursen and associates wrote. “An increase in GAS as described in this study has not been demonstrated elsewhere so far. In contrast to our findings, the most common species to ‘take over’ in the United States was Haemophilus influenzae.
“As [S. pneumoniae] and GAS are potentially invasive pathogens causing more severe clinical signs and symptoms, such cases are more likely to be admitted compared to cases caused by non-typable Haemophilus influenzae that gives rise to more subtle middle ear infections and clinical pictures,” the researchers noted.
Considering how many patients received antibiotics prior to admission in the hAOM group, there was a slight increase from 45% in the prevaccine era to 54% in the PCV-13 era, but a “more pronounced increase was found in the M+AM group, from 27% in the prevaccine era to 46% in the PCV-13 era,” they said.
The investigators called for continued surveillance of the microbiology associated with complex AOM.
No study funding or investigator disclosure information was provided.
Incidence rate ratios of children hospitalized with acute otitis media (hAOM) or more advanced stages, such as mastoidismus and acute mastoiditis (M+AM) declined by 10% and 20%, respectively, after introduction of pneumococcal conjugate vaccines (PCV) in the central region of Denmark, reported Bjarke B. Laursen of Aarhus University in Denmark, and associates.
The use of antibiotics for AOM prior to hospitalization increased markedly during the study period, and that may have impacted the modest reduction in hAOM and M+AM, the researchers said.
Incidence of Streptococcus pneumoniae cases decreased from 38% in the prevaccine era to 31% in the PCV-7 era and decreased even more to 16% in the PCV-13 era. The incidence of the second most frequently isolated bacteria, group A streptococcus (GAS), fell from 17% in the prevaccine era to 16% in the PCV-13 era, becoming equal to S. pneumoniae. The “no growth” results rose from 12% in the prevaccine era to 38% and 44% in the PCV-7 and PCV-13 eras, respectively (Int J Pediatr Otorhinolaryngol. 2017 Jul 4. doi: 10.1016/j.ijporl.2017.07.002) .
In the M+AM group, S. pneumoniae–positive cases fell to 10% in the PCV-13 era, compared with 44% in the prevaccine era and 41% in the PCV-7 era. A rise in GAS-positive cultures was seen in the M+AM group, from 15% in the prevaccine era to 30% in the PCV-13 era. The “no growth” group rose in incidence from 13% of cases in the prevaccine era to 26% in the PCV-7 era and 33% in the PCV-13 era.
“This microbiological shift is worrisome, because GAS may cause very serious infections due to its invasive nature,” Dr. Laursen and associates wrote. “An increase in GAS as described in this study has not been demonstrated elsewhere so far. In contrast to our findings, the most common species to ‘take over’ in the United States was Haemophilus influenzae.
“As [S. pneumoniae] and GAS are potentially invasive pathogens causing more severe clinical signs and symptoms, such cases are more likely to be admitted compared to cases caused by non-typable Haemophilus influenzae that gives rise to more subtle middle ear infections and clinical pictures,” the researchers noted.
Considering how many patients received antibiotics prior to admission in the hAOM group, there was a slight increase from 45% in the prevaccine era to 54% in the PCV-13 era, but a “more pronounced increase was found in the M+AM group, from 27% in the prevaccine era to 46% in the PCV-13 era,” they said.
The investigators called for continued surveillance of the microbiology associated with complex AOM.
No study funding or investigator disclosure information was provided.
Incidence rate ratios of children hospitalized with acute otitis media (hAOM) or more advanced stages, such as mastoidismus and acute mastoiditis (M+AM) declined by 10% and 20%, respectively, after introduction of pneumococcal conjugate vaccines (PCV) in the central region of Denmark, reported Bjarke B. Laursen of Aarhus University in Denmark, and associates.
The use of antibiotics for AOM prior to hospitalization increased markedly during the study period, and that may have impacted the modest reduction in hAOM and M+AM, the researchers said.
Incidence of Streptococcus pneumoniae cases decreased from 38% in the prevaccine era to 31% in the PCV-7 era and decreased even more to 16% in the PCV-13 era. The incidence of the second most frequently isolated bacteria, group A streptococcus (GAS), fell from 17% in the prevaccine era to 16% in the PCV-13 era, becoming equal to S. pneumoniae. The “no growth” results rose from 12% in the prevaccine era to 38% and 44% in the PCV-7 and PCV-13 eras, respectively (Int J Pediatr Otorhinolaryngol. 2017 Jul 4. doi: 10.1016/j.ijporl.2017.07.002) .
In the M+AM group, S. pneumoniae–positive cases fell to 10% in the PCV-13 era, compared with 44% in the prevaccine era and 41% in the PCV-7 era. A rise in GAS-positive cultures was seen in the M+AM group, from 15% in the prevaccine era to 30% in the PCV-13 era. The “no growth” group rose in incidence from 13% of cases in the prevaccine era to 26% in the PCV-7 era and 33% in the PCV-13 era.
“This microbiological shift is worrisome, because GAS may cause very serious infections due to its invasive nature,” Dr. Laursen and associates wrote. “An increase in GAS as described in this study has not been demonstrated elsewhere so far. In contrast to our findings, the most common species to ‘take over’ in the United States was Haemophilus influenzae.
“As [S. pneumoniae] and GAS are potentially invasive pathogens causing more severe clinical signs and symptoms, such cases are more likely to be admitted compared to cases caused by non-typable Haemophilus influenzae that gives rise to more subtle middle ear infections and clinical pictures,” the researchers noted.
Considering how many patients received antibiotics prior to admission in the hAOM group, there was a slight increase from 45% in the prevaccine era to 54% in the PCV-13 era, but a “more pronounced increase was found in the M+AM group, from 27% in the prevaccine era to 46% in the PCV-13 era,” they said.
The investigators called for continued surveillance of the microbiology associated with complex AOM.
No study funding or investigator disclosure information was provided.
FROM THE INTERNATIONAL JOURNAL OF PEDIATRIC OTORHINOLARYNGOLOGY
Key clinical point:
Major finding: Overall incidence in hAOM decreased numerically from 6.45/100,000 annually in the prevaccine era to 2.43/100,000 in the PCV-7 era, and to 5.88/100,000 annually in the PCV-13 era.
Data source: A retrospective study of 246 cases of children hospitalized with acute otitis media.
Disclosures: No study funding or investigator disclosure information was provided.
Prenatal methadone maintenance linked to poorer child neurodevelopment
SAN FRANCISCO – Infants born to mothers receiving methadone maintenance treatment show poorer-than-average neurodevelopment outcomes, a retrospective study found.
Delays or difficulties in motor abilities appeared first in these children, followed by evidence of cognitive problems in their second year of life, reported Cristina Borradori Tolsa, MD, of University Hospital, Geneva.
“Higher methadone doses during pregnancy can have a detrimental effect on neonatal characteristics and children’s psychomotor development,” Dr. Borradori Tolsa said at the Pediatric Academic Societies meeting. She noted the need for long-term follow-up of children prenatally exposed to methadone maintenance therapy to evaluate their cognitive abilities and school readiness at preschool ages.
Only 38% of the women had exclusively used methadone, while the other 62% had used a variety of substances, including cocaine, alcohol, benzodiazepine, marijuana, and antidepressants. The women had a low average socioeconomic status based on their level of education and the occupations of the children’s fathers.
The researchers drew children’s development data from their scores on the Bayley Scales of Infant Development, Second Edition (BSID-II), at 6 months and 18-24 months. The BSID-II has an average score of 100 and includes a mental development index for language and cognitive development, and a psychomotor development index to assess fine and gross motor skills.
At age 6 months, 75% of the 40 children assessed showed some level of motor skills delay, and 33% had a moderate to severe delay in psychomotor skills. A quarter had no delay at all (a score of at least 85). The average psychomotor score at 6 months was 76, and the average cognitive score was 88. Most of the children (60%) did, however, show mental development within the normal range at 6 months.
By the age of 18-24 months, half of the 36 children assessed showed no motor delays, and half showed no cognitive delays. One in five (20%) showed a moderate to severe psychomotor delay, and 14% showed a moderate to severe mental development delay. Mild delays in mental development occurred in 36% of the toddlers assessed, and 30% showed mild delays in psychomotor skills.
A dose-response effect was seen with mothers’ higher doses of methadone at birth and their children’s psychomotor scores at 6 months. No similar association existed for mental development, and the psychomotor association disappeared by 18-24 months. At this older age, however, 68% of children born to mothers taking a high dose of methadone showed cognitive delays, compared with 29% of children born to mothers on a low dose.
Although no differences were seen in newborns’ average gestational age (an average of 37.8 weeks overall) or birth weight between the high-dose and low-dose methadone groups, infants born to mothers with high doses were more likely to be small for gestational age (P = .01) and to need longer treatment duration for neonatal abstinence syndrome (NAS) (P = .03). Overall, 44% of the newborns were small for gestational age, 28% were born microcephalic, and all but three required pharmacologic treatment for NAS. NAS treatment lasted an average 54 days for the cohort, and the average hospital stay for the babies was 76 days.
The researchers did not report having any external funding or relevant financial disclosures.
SAN FRANCISCO – Infants born to mothers receiving methadone maintenance treatment show poorer-than-average neurodevelopment outcomes, a retrospective study found.
Delays or difficulties in motor abilities appeared first in these children, followed by evidence of cognitive problems in their second year of life, reported Cristina Borradori Tolsa, MD, of University Hospital, Geneva.
“Higher methadone doses during pregnancy can have a detrimental effect on neonatal characteristics and children’s psychomotor development,” Dr. Borradori Tolsa said at the Pediatric Academic Societies meeting. She noted the need for long-term follow-up of children prenatally exposed to methadone maintenance therapy to evaluate their cognitive abilities and school readiness at preschool ages.
Only 38% of the women had exclusively used methadone, while the other 62% had used a variety of substances, including cocaine, alcohol, benzodiazepine, marijuana, and antidepressants. The women had a low average socioeconomic status based on their level of education and the occupations of the children’s fathers.
The researchers drew children’s development data from their scores on the Bayley Scales of Infant Development, Second Edition (BSID-II), at 6 months and 18-24 months. The BSID-II has an average score of 100 and includes a mental development index for language and cognitive development, and a psychomotor development index to assess fine and gross motor skills.
At age 6 months, 75% of the 40 children assessed showed some level of motor skills delay, and 33% had a moderate to severe delay in psychomotor skills. A quarter had no delay at all (a score of at least 85). The average psychomotor score at 6 months was 76, and the average cognitive score was 88. Most of the children (60%) did, however, show mental development within the normal range at 6 months.
By the age of 18-24 months, half of the 36 children assessed showed no motor delays, and half showed no cognitive delays. One in five (20%) showed a moderate to severe psychomotor delay, and 14% showed a moderate to severe mental development delay. Mild delays in mental development occurred in 36% of the toddlers assessed, and 30% showed mild delays in psychomotor skills.
A dose-response effect was seen with mothers’ higher doses of methadone at birth and their children’s psychomotor scores at 6 months. No similar association existed for mental development, and the psychomotor association disappeared by 18-24 months. At this older age, however, 68% of children born to mothers taking a high dose of methadone showed cognitive delays, compared with 29% of children born to mothers on a low dose.
Although no differences were seen in newborns’ average gestational age (an average of 37.8 weeks overall) or birth weight between the high-dose and low-dose methadone groups, infants born to mothers with high doses were more likely to be small for gestational age (P = .01) and to need longer treatment duration for neonatal abstinence syndrome (NAS) (P = .03). Overall, 44% of the newborns were small for gestational age, 28% were born microcephalic, and all but three required pharmacologic treatment for NAS. NAS treatment lasted an average 54 days for the cohort, and the average hospital stay for the babies was 76 days.
The researchers did not report having any external funding or relevant financial disclosures.
SAN FRANCISCO – Infants born to mothers receiving methadone maintenance treatment show poorer-than-average neurodevelopment outcomes, a retrospective study found.
Delays or difficulties in motor abilities appeared first in these children, followed by evidence of cognitive problems in their second year of life, reported Cristina Borradori Tolsa, MD, of University Hospital, Geneva.
“Higher methadone doses during pregnancy can have a detrimental effect on neonatal characteristics and children’s psychomotor development,” Dr. Borradori Tolsa said at the Pediatric Academic Societies meeting. She noted the need for long-term follow-up of children prenatally exposed to methadone maintenance therapy to evaluate their cognitive abilities and school readiness at preschool ages.
Only 38% of the women had exclusively used methadone, while the other 62% had used a variety of substances, including cocaine, alcohol, benzodiazepine, marijuana, and antidepressants. The women had a low average socioeconomic status based on their level of education and the occupations of the children’s fathers.
The researchers drew children’s development data from their scores on the Bayley Scales of Infant Development, Second Edition (BSID-II), at 6 months and 18-24 months. The BSID-II has an average score of 100 and includes a mental development index for language and cognitive development, and a psychomotor development index to assess fine and gross motor skills.
At age 6 months, 75% of the 40 children assessed showed some level of motor skills delay, and 33% had a moderate to severe delay in psychomotor skills. A quarter had no delay at all (a score of at least 85). The average psychomotor score at 6 months was 76, and the average cognitive score was 88. Most of the children (60%) did, however, show mental development within the normal range at 6 months.
By the age of 18-24 months, half of the 36 children assessed showed no motor delays, and half showed no cognitive delays. One in five (20%) showed a moderate to severe psychomotor delay, and 14% showed a moderate to severe mental development delay. Mild delays in mental development occurred in 36% of the toddlers assessed, and 30% showed mild delays in psychomotor skills.
A dose-response effect was seen with mothers’ higher doses of methadone at birth and their children’s psychomotor scores at 6 months. No similar association existed for mental development, and the psychomotor association disappeared by 18-24 months. At this older age, however, 68% of children born to mothers taking a high dose of methadone showed cognitive delays, compared with 29% of children born to mothers on a low dose.
Although no differences were seen in newborns’ average gestational age (an average of 37.8 weeks overall) or birth weight between the high-dose and low-dose methadone groups, infants born to mothers with high doses were more likely to be small for gestational age (P = .01) and to need longer treatment duration for neonatal abstinence syndrome (NAS) (P = .03). Overall, 44% of the newborns were small for gestational age, 28% were born microcephalic, and all but three required pharmacologic treatment for NAS. NAS treatment lasted an average 54 days for the cohort, and the average hospital stay for the babies was 76 days.
The researchers did not report having any external funding or relevant financial disclosures.
AT PAS 17
Key clinical point:
Major finding: Three-fourths of methadone-exposed infants showed psychomotor delays at 6 months, and 50% showed cognitive delays and/or psychomotor delays at 18-24 months.
Data source: A retrospective analysis of neurodevelopment scores of children born to 61 mothers in Geneva who received methadone maintenance therapy during pregnancy.
Disclosures: The researchers did not report having any external funding or relevant financial disclosures.
FDA has the resources to answer questions about medicines and pregnancy
There are about 6 million pregnancies in the United States each year, and it’s estimated that 50% of pregnant women take at least one medicine. Physicians play an important role in helping their pregnant patients make informed health choices, especially when it comes to the safe use of medications.
- Emphasize that patients should always talk to their health care provider before taking any medicines, herbs, or vitamins. The website provides tips on how to start the conversation with patients about what medicines, herbs, or vitamins to avoid when pregnant.
- Encourage patients to check the drug label and other information that comes with their medicine to learn about possible risks for women who are pregnant or breastfeeding.
- Assist pregnant patients with changing medications as needed.
- Advise pregnant patients if they need to take more or less of their medicines.
- Advise patients about medicines that can and cannot be used when they start breastfeeding.
- Encourage patients to talk about any problems they have with their medicine.
- Report any serious problems your pregnant patients have had after taking a medicine to the FDA. It falls to physicians to report to the FDA any cases of serious side effects, problems with product quality, and product-use errors or with any of the following products: human drugs, medical devices, blood products and other biologics (except vaccines), and/or medical foods.
- Encourage patients to enroll in a Pregnancy Exposure Registry, if applicable at the FDA website, which collects information on pregnancy outcomes in women who already are taking medications. Observational studies of the patients that physicians help enroll in a pregnancy exposure registry can improve drug safety information for medicines used during pregnancy and can be used to update drug labeling. The observational studies included with the registries can also help physicians make medicine recommendations for use during pregnancy. The list includes contact information for each registry. Physicians can check online to see if there is a registry for their patients’ medicine.
The FDA website also provides information about the Pregnancy and Lactation Labeling Final Rule, which requires changes to the content and format for information presented in prescription drug labeling. The changes are implemented to help health care providers assess risk versus benefit and in subsequent counseling of pregnant women and nursing mothers.
The FDA offers free medicine safety and pregnancy resources for pregnant women, including downloadable infographics; a Medicines Record Keeper brochure in English, Spanish
Pregnancy is an exciting time for women, but they may have questions and concerns about how medicines they take will affect their babies. Our pregnancy website can help make a woman’s pregnancy happier and healthier.
Dr. Yao is the director of the division of pediatrics and maternal health, Office of Drug Evaluation IV, Center for Drug Evaluation and Research at the FDA, in Silver Spring, Md.
There are about 6 million pregnancies in the United States each year, and it’s estimated that 50% of pregnant women take at least one medicine. Physicians play an important role in helping their pregnant patients make informed health choices, especially when it comes to the safe use of medications.
- Emphasize that patients should always talk to their health care provider before taking any medicines, herbs, or vitamins. The website provides tips on how to start the conversation with patients about what medicines, herbs, or vitamins to avoid when pregnant.
- Encourage patients to check the drug label and other information that comes with their medicine to learn about possible risks for women who are pregnant or breastfeeding.
- Assist pregnant patients with changing medications as needed.
- Advise pregnant patients if they need to take more or less of their medicines.
- Advise patients about medicines that can and cannot be used when they start breastfeeding.
- Encourage patients to talk about any problems they have with their medicine.
- Report any serious problems your pregnant patients have had after taking a medicine to the FDA. It falls to physicians to report to the FDA any cases of serious side effects, problems with product quality, and product-use errors or with any of the following products: human drugs, medical devices, blood products and other biologics (except vaccines), and/or medical foods.
- Encourage patients to enroll in a Pregnancy Exposure Registry, if applicable at the FDA website, which collects information on pregnancy outcomes in women who already are taking medications. Observational studies of the patients that physicians help enroll in a pregnancy exposure registry can improve drug safety information for medicines used during pregnancy and can be used to update drug labeling. The observational studies included with the registries can also help physicians make medicine recommendations for use during pregnancy. The list includes contact information for each registry. Physicians can check online to see if there is a registry for their patients’ medicine.
The FDA website also provides information about the Pregnancy and Lactation Labeling Final Rule, which requires changes to the content and format for information presented in prescription drug labeling. The changes are implemented to help health care providers assess risk versus benefit and in subsequent counseling of pregnant women and nursing mothers.
The FDA offers free medicine safety and pregnancy resources for pregnant women, including downloadable infographics; a Medicines Record Keeper brochure in English, Spanish
Pregnancy is an exciting time for women, but they may have questions and concerns about how medicines they take will affect their babies. Our pregnancy website can help make a woman’s pregnancy happier and healthier.
Dr. Yao is the director of the division of pediatrics and maternal health, Office of Drug Evaluation IV, Center for Drug Evaluation and Research at the FDA, in Silver Spring, Md.
There are about 6 million pregnancies in the United States each year, and it’s estimated that 50% of pregnant women take at least one medicine. Physicians play an important role in helping their pregnant patients make informed health choices, especially when it comes to the safe use of medications.
- Emphasize that patients should always talk to their health care provider before taking any medicines, herbs, or vitamins. The website provides tips on how to start the conversation with patients about what medicines, herbs, or vitamins to avoid when pregnant.
- Encourage patients to check the drug label and other information that comes with their medicine to learn about possible risks for women who are pregnant or breastfeeding.
- Assist pregnant patients with changing medications as needed.
- Advise pregnant patients if they need to take more or less of their medicines.
- Advise patients about medicines that can and cannot be used when they start breastfeeding.
- Encourage patients to talk about any problems they have with their medicine.
- Report any serious problems your pregnant patients have had after taking a medicine to the FDA. It falls to physicians to report to the FDA any cases of serious side effects, problems with product quality, and product-use errors or with any of the following products: human drugs, medical devices, blood products and other biologics (except vaccines), and/or medical foods.
- Encourage patients to enroll in a Pregnancy Exposure Registry, if applicable at the FDA website, which collects information on pregnancy outcomes in women who already are taking medications. Observational studies of the patients that physicians help enroll in a pregnancy exposure registry can improve drug safety information for medicines used during pregnancy and can be used to update drug labeling. The observational studies included with the registries can also help physicians make medicine recommendations for use during pregnancy. The list includes contact information for each registry. Physicians can check online to see if there is a registry for their patients’ medicine.
The FDA website also provides information about the Pregnancy and Lactation Labeling Final Rule, which requires changes to the content and format for information presented in prescription drug labeling. The changes are implemented to help health care providers assess risk versus benefit and in subsequent counseling of pregnant women and nursing mothers.
The FDA offers free medicine safety and pregnancy resources for pregnant women, including downloadable infographics; a Medicines Record Keeper brochure in English, Spanish
Pregnancy is an exciting time for women, but they may have questions and concerns about how medicines they take will affect their babies. Our pregnancy website can help make a woman’s pregnancy happier and healthier.
Dr. Yao is the director of the division of pediatrics and maternal health, Office of Drug Evaluation IV, Center for Drug Evaluation and Research at the FDA, in Silver Spring, Md.
Start ART in first 3 months in infants with perinatal HIV
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
AT ESPID 2017
Key clinical point:
Major finding: With each 1-month delay in starting antiretroviral therapy, the likelihood of attaining viral suppression by age 12 months drops by 16%.
Data source: This observational study included 420 infants with perinatally acquired HIV infection who began antiretroviral therapy prior to age 6 months.
Disclosures: Dr. Palma reported having no relevant financial disclosures.
Privacy and maternal records
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Fifty-year retrospective by Dr. William G. Wilkoff
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
When the first issue of Pediatric News was published 50 years ago, I was starting the second half of my first year in medical school. Over the ensuing 50 years, I have lived through and witnessed some dramatic changes in pediatrics. Here are just a few of the transitions that I’ve observed and Pediatric News has covered:
The birth of interventional neonatology
When I was an intern at Duke University Medical Center in Durham, N.C., a paper appeared in the New England Journal of Medicine describing the use of a simple continuous positive pressure apparatus for the treatment of respiratory distress syndrome entitled, “Treatment of idiopathic respiratory-distress syndrome with continuous positive airway pressure,” (1971 Jun 17;284[24]:1333-40). After seeing the paper, George Brumley, MD, the head of nursery, immediately had the hospital engineers build us our own setup, and we became part of what could arguably be called the revolution that turned neonatology into an interventional specialty.
From meningitis to mental health
Although it came gradually, one of the most significant changes over the last 50 years has been the shift in the mix of pathology presenting to the general pediatrician. In the 1970s and 1980s, the threat of invasive bacterial disease, usually from Haemophilus influenzae, was always hanging over us. It was not unusual for a single community pediatrician to see four or five cases of meningitis in a year. The introduction of effective vaccines and more potent antibiotics lessened the threat of serious bacterial infection, and in its place came a flood of mental health complaints, including anxiety (25% prevalence among 13- to 18-year-olds, depression (13% prevalence among 12- to 17-year-olds) and attention-deficit/hyperactivity disorder (ADHD) (9% prevalence among 13- to 18-year-olds). The result is the impression that, at times, being a general pediatrician today feels like being a more than part-time psychiatrist/psychologist.
Mental retardation and autism
In the 1970s and 1980s, the diagnosis of autism was usually reserved for children with serious communication difficulties. Many physicians and the lay public expected that a child who was diagnosed with autism would have no speech at all. The prevalence of the condition in the last quarter of the century was felt to be about 1 in 2,000.
The more common diagnosis during that period was mental retardation. However, as the result of insensitive stereotyping, “mental retardation” has become an offensive term and has vanished from the pediatric lexicon.
Autism, however, has flourished, and a recent estimate cited by the CDC pegs its prevalence at 1 in 68. Based on my observations, I expect that much, if not most, of this increase is the result of expanded diagnostic criteria and relabeling.
Chicken scratches to mouse clicks
In keeping with a long tradition in medicine, my office notes when I began in practice were unreadable by anyone except a very few my long-term coworkers. My scribbles were brief and often included sketches of wounds and body parts. Their primary purpose was to remind me what had transpired at that office visit and to record the biometrics. Unfortunately, as the cloud of malpractice crept over the landscape, with it came the nonsensical mantra, “if it wasn’t documented, it didn’t happen.”
With the introduction of computers, medical records became inflated and often inaccurate, documents to be used primarily for data collection and risk management. The physician now is tasked with being the data entry clerk who must keep her eyes on the computer screen at the expense of a meaningful interaction with the patient. Sadly, the physician-unfriendliness of electronic medical records has driven many older and experienced pediatricians into premature retirement, robbing general pediatrics of their accumulated wisdom.
A part-time job
In 1975, there were 22,730 practicing pediatricians, of whom 23% were women. In 2011, there were 80,992 pediatricians, of whom 56.6% were women. The percentage of women practicing pediatrics continues to climb, with the most recent figure being 58%. From the patient perspective, this shift in gender dominance has been well received.
At the same time, there has been a trend toward more pediatricians of both genders pursuing part-time employment. The model of the physician being the owner/operator of a medical practice that was flourishing when I began in practice has been replaced by one in which the physician is an employee of a much larger entity, which is pressured from all sides to cut costs. To make matters worse, the Medical Home model that currently is in vogue is proving to be a more expensive vehicle for delivering health care. The patient now is asked to view his physician as the director of a team and may see him or her only infrequently, at the expense of the therapeutic benefits of familiarity.
When I was in medical school, the tuition was around $2,500/year, and I graduated with a debt of about $3,000 – with an interest rate so low that I was in no rush to pay it off. Now a student entering medical school can expect to pay around $60,000/year – an amount that has far outstripped inflation.
These realities combine to create a potentially unsustainable economic climate for pediatricians. I have had a wonderful 50 years being a pediatrician. But I can’t promise the same level of enjoyment to the next generation of pediatricians, unless someone can figure how to cut the expense of medical school and/or make part-time employment fit into a health care delivery system that must contain costs to survive.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.” Email him at [email protected].
All isn’t well with HIV-exposed uninfected infants
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
MADRID – Children who were HIV-exposed antenatally but not infected are at double the risk of hospitalization for infectious diseases during their first year of life, compared with HIV-unexposed controls, according to what’s believed to be the first prospective study examining the issue in a Western industrialized country.
That’s one key take-away message from the study conducted in Brussels. Another key finding was that the sharply increased risk of hospitalization for infection during infancy was erased if HIV-infected mothers started antiretroviral therapy prior to, rather than during, pregnancy, Catherine Adler, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
She presented a prospective study of 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds. All of the HIV-positive mothers were on antiretroviral therapy, which they started either prior to or during pregnancy.
The two groups of women gave birth to 132 HEU and 123 HIV-unexposed babies, all born after 35 weeks’ gestation. The babies didn’t differ in terms of gender, prematurity rate, mode of delivery, or the use of antibiotics at delivery. However, 17% of the HEU babies had a birth weight below 2,500 g, compared with just 3% of the HIV-unexposed controls. Also, as a matter of policy, none of the HEU babies were breastfed, while 95% of the controls were, Dr. Adler explained.
The primary outcome in the study was the rate of hospitalization for infection during the first 12 months of life. The rate was 21% in the HEU babies, significantly greater than the 11% rate in HIV-unexposed babies. In a multivariate analysis adjusted for preterm birth, low birth weight, literacy, and maternal age, HEU status was associated with twofold increased risk of hospitalization for infection in infancy.
“The increased susceptibility of HEU infants to infectious disease is not restricted to children born in developing countries,” she declared.
The disparity in hospitalization rates was driven by hospitalization for viral infections, which occurred at a rate of 20% in the HEU group, versus 9% in controls. Particularly notable were the 10 hospitalizations for respiratory syncytial virus infection in the HEU patients, compared with just 1 in the controls.
Dr. Adler and her coinvestigators will continue following the children out to about 3 years of age. After age 12 months, the two groups no longer differed significantly in their risk of hospitalization for infection.
“The first year is a vulnerable period. Our data highlight the importance of a close follow-up of these infants,” she said.
The biggest risk factor for hospitalization for infectious illness in the HEU group was initiation of antiretroviral therapy during pregnancy. The hospitalization rate in HEU infants whose mothers began therapy prior to pregnancy was the same as in HIV-unexposed infants. The inference is that it’s not in utero exposure to antiretroviral drugs that is responsible for the increased risk of hospitalization during infancy.
“This observation supports the notion that it’s the activity of the maternal HIV infection – the exposure to a strongly proinflammatory state in the mother – that contributes to the risk of severe infection in HEU infants, probably by causing changes in innate immunity cells,” according to Dr. Adler.
Even though the increased risk of hospitalization for infectious illnesses in HEU children falls off after age 12 months, she continued, her group is following them out to about age 3 years because “we have the impression that they are at risk for neurodevelopmental problems, including language delay.”
Other researchers in the audience confirmed this risk, reporting that, as they follow HEU children through adolescence, they see an increased rate of attention deficits and associated comorbidities.
Dr. Adler called the administration of antiretroviral therapy to pregnant HIV-infected women in order to prevent maternal-to-child transmission of the disease “one of the major successes of the 21st century.”
“The number of new HIV infections among children has collapsed, leading to an increasing number of HIV-exposed but uninfected children. One million of them are born each year,” she said.
Dr. Adler reported having no financial conflicts of interest regarding her study.
*The article was updated 6/15/17.
AT ESPID 2017
Key clinical point:
Major finding: The rate of hospitalization for a serious infectious illness during the first 12 months of life was 21% in HIV-exposed uninfected children, significantly greater than the 11% rate in HIV-unexposed babies.
Data source: This prospective observational study included 125 HIV-positive and 119 HIV-negative pregnant Belgian women of comparable ethnic and sociodemographic backgrounds and their offspring, followed to date through the infants’ first birthday.
Disclosures: Dr. Adler reported having no financial conflicts of interest.
OSA in pregnancy linked to congenital anomalies
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
BOSTON – Newborns exposed to obstructive sleep apnea (OSA) in utero are at a higher risk of being diagnosed with congenital anomalies, according to a new study presented at the annual meeting of the Associated Professional Sleep Societies.
The researchers’ analysis covered data from more than 1.4 million births during 2010-2014. Circulatory, musculoskeletal, and central nervous systems were among the types of anomalies they saw in the 17.3% of babies born to mothers who had OSA during pregnancy. These babies were also more likely to require intensive care at birth, compared with those born to mothers who had not been diagnosed with OSA.
Additionally, the investigators found that the 0.1% of women who had a diagnosis of OSA were 2.76 times more likely to have babies that required some kind of resuscitative effort at birth. Specifically, 0.5% of the newborns of the mothers with OSA required resuscitation, compared with 0.1% of the other group’s babies. The newborns of women with OSA were also 2.25 times more likely to have a longer hospital stay.
Mothers with OSA were older and more likely to be non-Hispanic black and have a diagnosis of obesity, tobacco use, and drug use but not alcohol use.
“We can’t say for sure that sleep apnea is causing these outcomes,” said abstract presenter and principal investigator Ghada Bourjeily, MD, of Brown University and Miriam Hospital, both in Providence, R.I., in an interview.
“We know that women who have sleep apnea also often have other morbidities, so we don’t know what might have contributed to the congenital outcomes,” said Dr. Bourjeily. “We also don’t know if treating sleep apnea can reverse or prevent birth complications or even maternal complications, like preeclampsia or gestational diabetes.”
Ongoing studies are looking at maternal continuous positive airway pressure therapy use and neonatal outcomes, but “they are nothing to write home about yet,” she said.
“This is an underdiagnosed condition and it’s probably undercoded too, but we know from another study that the prevalence of OSA in the first trimester in an all-comers population that was screened for the condition is 4%,” said Dr. Bourjeily. “If another 3% of [the study participants] actually had OSA, then all of these findings are potentially underestimated.”
The majority of OSA in pregnant women that has been identified in prospective studies is mild and not necessarily something that most physicians would treat, she noted. “In our study, the ones who were diagnosed were those who probably went to their doctors and complained of sleepiness or loud snoring.”
The researchers also determined that the newborns of mothers with sleep apnea were more likely to be admitted to an intensive care unit (25.3% vs. 8.1%) or a special care nursery (34.9% vs. 13.6%).
A diagnosis of OSA was established when a diagnosis code for OSA was present on the delivery discharge record. Maternal and infant outcomes were collected for ICD-9 and procedural codes.
Dr. Bourjeily received research equipment support from Respironics.
AT SLEEP 2017
Key clinical point: This large cohort study is the first study to show an increased risk of congenital anomalies and resuscitation at birth in newborns born to mothers with diagnosed obstructive sleep apnea (OSA).
Major finding: Of babies born to a mother with OSA, 17.3% had a congenital anomaly, compared with 10.6% of those born to mothers without OSA (P less than .001). This difference remained significant after adjusting for potential confounders.
Data source: A national cohort study including more than 1.4 million linked maternal and newborn records with a delivery hospitalization during 2010-2014.
Disclosures: Dr. Bourjeily received research equipment support from Respironics.
Telemedicine visits after NICU discharge improved care, processes
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
SAN FRANCISCO – Using telemedicine for a follow-up appointment 1 week after discharge of medically complex infants reduced extra visits or calls to a clinic or emergency department, a recent study found.
The telemedicine visits also helped providers identify ways to improve the neonatal ICU (NICU) discharge process while assessing infants’ home care and answering parents’ questions.
The researchers assessed whether telemedicine visits could ease the transition from neonatal intensive care to home care, respond adequately to caregivers’ needs during that transition, reduce emergency department visits and readmissions, and detect and address any potential problems. The visits also provided an opportunity for feedback on caregivers’ experiences during discharge.
The 92 patients all were medically complex infants who went home with respiratory or feeding equipment, surgical sites and/or complex medication administration. For example, 28 infants had been sent home with a nasogastric tube, 13 had a gastrostomy tube, and 13 had an apnea monitor. Overall, participants had been discharged with an average 2.3 medications and 4.8 scheduled subspecialty follow-up appointments.
The most common conditions among the participants were gastrointestinal disease, neurologic disease, and congenital diaphragmatic hernia or lung lesions. Other conditions included omphalocele, genetic disorders, tracheoesophageal fistula or esophageal atresia and chronic lung disease, or another respiratory disease, Dr. Brant reported at the Pediatric Academic Societies meeting.
Families could enroll in the study only if they had a smart device (such as a tablet) and wireless Internet access at home. One week after the infant’s discharge from the NICU, the caregivers received one telemedicine visit with a team that included neonatologists, neonatal fellows, nurse practitioners, and a telemedicine coordinator or support staffer. During the visit, the providers observed the infant and the home environment, and evaluated care practices, including tube feedings, respiratory support, management of surgical wound sites, and administration of medications.
The providers also reviewed how to use the medical equipment, gathered follow-up information about the child’s health, and answered caregivers’ questions. The providers did not bill for telemedicine visits since it was part of a pilot study, but the participants did need to reside in Pennsylvania or New Jersey to meet provider licensing regulations.
Among the 93 telemedicine visits, half (50%) prevented the family from calling or visiting a provider, and 12% of them led to an earlier follow-up appointment for the child. During the video observations, providers addressed 14 issues related to the child’s sleep environment, respiratory status, surgical sites, or dermatological issues. Among 78 total concerns identified in the visits, 35% related to the surgical site, 33% related to feeding, 19% related to respiratory concerns, and 13% related to medication administration.
The provider team also asked families during the visit about their experiences during discharge. A quarter of the families (26%) said they needed more parental education during discharge. In addition, 14% mentioned problems with scheduling follow-up appointments, and 12% had problems related to case management and insurance. Other issues raised by parents related to home equipment, early intervention, home feeding or medications, and diagnostic logistics.
In subsequent satisfaction surveys filled out by caregivers about the telemedicine visit itself, the median rating was 94.5 on a scale of 0 (not at all satisfied) to 100 (extremely satisfied). The overall intervention was 92% successful in its completion. The only follow-up telemedicine visits that did not occur resulted from malfunctioning wireless connection or a mobile app problem. On a scale of 1 to 100 (best), caregivers rated the video quality as an average 78, the Internet reliability as 79, and the ease of using the camera as 91. One of the biggest benefits of the intervention, Dr. Brant pointed out, is that using telemedicine bypasses some of the geographic and time-related obstacles that can occur with follow-ups.
Dr. Brant had no relevant financial disclosures and did not report using any external funding.
FROM PAS 17
Key clinical point:
Major finding: Telemedicine visits prevented 50% of participants from calling or visiting a provider and led 12% of families to bring infants in sooner than originally scheduled.
Data source: The findings are based on a pilot project at the Children’s Hospital of Philadelphia involving 93 medically complex infants discharged from the NICU with medical equipment, surgical sites, and/or complex medication administration.
Disclosures: Dr. Brant had no relevant financial disclosures and did not report external funding.