User login
For MD-IQ use only
Can a Risk Score Predict Kidney Injury After Cisplatin?
Cisplatin is a preferred treatment for a wide range of cancers, including breast, head and neck, lung, ovary, and more. However, its side effects — particularly nephrotoxicity — can be severe. Kidney injury on cisplatin is associated with higher mortality and can jeopardize a patient’s eligibility for other therapies.
Now, in a large study using data from six US cancer centers, researchers have developed a risk algorithm to predict acute kidney injury (AKI) after cisplatin administration.
A risk prediction calculator based on the algorithm is available online for patients and providers to determine an individual patient›s risk for kidney injury from cisplatin using readily available clinical data.
Other risk scores and risk prediction models have been developed to help clinicians assess in advance whether a patient might develop AKI after receiving cisplatin, so that more careful monitoring, dose adjustments, or an alternative treatment, if available, might be considered.
However, previous models were limited by factors such as small sample sizes, lack of external validation, older data, and liberal definitions of AKI, said Shruti Gupta, MD, MPH, director of onco-nephrology at Brigham and Women’s Hospital (BWH) and Dana-Farber Cancer Institute, and David E. Leaf, MD, MMSc, director of clinical and translational research in AKI, Division of Renal Medicine, BWH, Boston.
Dr. Gupta and Dr. Leaf believe their risk score for predicting severe AKI after intravenous (IV) cisplatin, published online in The BMJ, is “more accurate and generalizable than prior models for several reasons,” they told this news organization in a joint email.
“First, we externally validated our findings across cancer centers other than the one where it was developed,” they said. “Second, we focused on moderate to severe kidney injury, the most clinically relevant form of kidney damage, whereas prior models examined more mild forms of kidney injury. Third, we collected data on nearly 25,000 patients receiving their first dose of IV cisplatin, which is larger than all previous studies combined.”
‘Herculean Effort’
“We conceived of this study back in 2018, contacted collaborators at each participating cancer center, and had numerous meetings to try to gather granular data on patients treated with their first dose of intravenous (IV) cisplatin,” Dr. Gupta and Dr. Leaf explained. They also incorporated patient feedback from focus groups and surveys.
“This was truly a Herculean effort that involved physicians, programmers, research coordinators, and patients,” they said.
The multicenter study included 24,717 patients — 11,766 in the derivation cohort and 12,951 in the validation cohort. Overall, the median age was about 60 years, about 58% were men, and about 78% were White.
The primary outcome was cisplatin-induced AKI (CP-AKI), defined as a twofold or greater increase in serum creatinine or kidney replacement therapy within 14 days of a first dose of IV cisplatin.
Their simple risk score consisting of nine covariates — age, hypertension, type 2 diabetes, hemoglobin level, white blood cell count, platelet count, serum albumin level, serum magnesium level, and cisplatin dose — predicted a higher risk for CP-AKI in both cohorts.
Notably, adding serum creatinine to the model did not change the area under the curve, and therefore, serum creatinine, though also an independent risk factor for CP-AKI, was not included in the score.
Patients in the highest risk category had 24-fold higher odds of CP-AKI in the derivation cohort and close to 18-fold higher odds in the validation cohort than those in the lowest risk category.
The primary model had a C statistic of 0.75 (95% CI, 0.73-0.76) and showed better discrimination for CP-AKI than previously published models, for which the C statistics ranged from 0.60 to 0.68. The first author of a paper on an earlier model, Shveta Motwani, MD, MMSc, of BWH and Dana-Farber Cancer Institute in Boston, is also a coauthor of the new study.
Greater severity of CP-AKI was associated with shorter 90-day survival (adjusted hazard ratio, 4.63; 95% CI, 3.56-6.02) for stage III CP-AKI vs no CP-AKI.
‘Definitive Work’
Joel M. Topf, MD, a nephrologist with expertise in chronic kidney disease in Detroit, who wasn’t involved in the development of the risk score, called the study “a definitive work on an important concept in oncology and nephrology.”
“While this is not the first attempt to devise a risk score, it is by far the biggest,” he told this news organization. Furthermore, the authors “used a diverse population, recruiting patients with a variety of cancers (previous attempts had often used a homogenous diagnosis, putting into question how generalizable the results were) from six different cancer centers.”
In addition, he said, “The authors did not restrict patients with chronic kidney disease or other significant comorbidities and used the geographic diversity to produce a cohort that has an age, gender, racial, and ethnic distribution, which is more representative of the US than previous, single-center attempts to risk score patients.”
An earlier model used the Kidney Disease: Improving Global Outcomes (KDIGO) consensus definition of AKI of an increase in serum creatinine of 0.3 mg/dL, he noted. “While a sensitive definition of AKI, it captures mild, hemodynamic increases in creatinine of questionable significance,” he said.
By contrast, the new score uses KDIGO stage II and above to define AKI. “This is a better choice, as we do not want to dissuade patients and doctors from choosing chemotherapy due to a fear of insignificant kidney damage,” he said.
All that said, Dr. Topf noted that neither the current score nor the earlier model included serum creatinine. “This is curious to me and may represent the small number of patients with representative elevated creatinine in the derivation cohort (only 1.3% with an estimated glomerular filtration rate [eGFR] < 45).”
“Since the cohort is made up of people who received cis-platinum, the low prevalence of eGFRs < 45 may be due to physicians steering away from cis-platinum in this group,” he suggested. “It would be unfortunate if this risk score gave an unintentional ‘green light’ to these patients, exposing them to predictable harm.”
‘Certainly Useful’
Anushree Shirali, MD, an associate professor in the Section of Nephrology and consulting physician, Yale Onco-Nephrology, Yale School of Medicine, in New Haven, Connecticut, said that having a prediction score for which patients are more likely to develop AKI after a single dose of cisplatin would be helpful for oncologists, as well as nephrologists.
As a nephrologist, Dr. Shirali mostly sees patients who already have AKI, she told this news organization. But there are circumstances in which the tool could still be helpful.
“Let’s say someone has abnormal kidney function at baseline — ie, creatinine is higher than the normal range — and they were on dialysis 5 years ago for something else, and now, they have cancer and may be given cisplatin. They worry about their chances of getting AKI and needing dialysis again,” she said. “That’s just one scenario in which I might be asked to answer that question and the tool would certainly be useful.”
Other scenarios could include someone who has just one kidney because they donated a kidney for transplant years ago, and now, they have a malignancy and wonder what their actual risk is of getting kidney issues on cisplatin.
Oncologists could use the tool to determine whether a patient should be treated with cisplatin, or if they’re at high risk, whether an alternative that’s not nephrotoxic might be used. By contrast, “if somebody’s low risk and an oncologist thinks cisplatin is the best agent they have, then they might want to go ahead and use it,” Dr. Shirali said.
Future research could take into consideration that CP-AKI is dose dependent, she suggested, because a prediction score that included the number of cisplatin doses could be even more helpful to determine risk. And, even though the derivation and validation cohorts for the new tool are representative of the US population, additional research should also include more racial/ethnic diversity, she said.
Dr. Gupta and Dr. Leaf hope their tool “will be utilized immediately by patients and providers to help predict an individual’s risk of cisplatin-associated kidney damage. It is easy to use, available for free online, and incorporates readily available clinical variables.”
If a patient is at high risk, the clinical team can consider preventive measures such as administering more IV fluids before receiving cisplatin or monitoring kidney function more closely afterward, they suggested.
Dr. Gupta reported research support from the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases. She also reported research funding from BTG International, GE HealthCare, and AstraZeneca outside the submitted work. She is a member of GlaxoSmithKline’s Global Anemia Council, a consultant for Secretome and Proletariat Therapeutics, and founder and president emeritus of the American Society of Onconephrology (unpaid). Dr. Leaf is supported by NIH grants, reported research support from BioPorto, BTG International, and Metro International Biotech, and has served as a consultant. Dr. Topf reported an ownership stake in a few DaVita-run dialysis clinics. He also runs a vascular access center and has participated in advisory boards with Cara Therapeutics, Vifor, Astra Zeneca, Bayer, Renibus Therapeutics, Travere Therapeutics, and GlaxoSmithKline. He is president of NephJC, a nonprofit educational organization with no industry support. Dr. Shirali declared no competing interests.
A version of this article appeared on Medscape.com.
Cisplatin is a preferred treatment for a wide range of cancers, including breast, head and neck, lung, ovary, and more. However, its side effects — particularly nephrotoxicity — can be severe. Kidney injury on cisplatin is associated with higher mortality and can jeopardize a patient’s eligibility for other therapies.
Now, in a large study using data from six US cancer centers, researchers have developed a risk algorithm to predict acute kidney injury (AKI) after cisplatin administration.
A risk prediction calculator based on the algorithm is available online for patients and providers to determine an individual patient›s risk for kidney injury from cisplatin using readily available clinical data.
Other risk scores and risk prediction models have been developed to help clinicians assess in advance whether a patient might develop AKI after receiving cisplatin, so that more careful monitoring, dose adjustments, or an alternative treatment, if available, might be considered.
However, previous models were limited by factors such as small sample sizes, lack of external validation, older data, and liberal definitions of AKI, said Shruti Gupta, MD, MPH, director of onco-nephrology at Brigham and Women’s Hospital (BWH) and Dana-Farber Cancer Institute, and David E. Leaf, MD, MMSc, director of clinical and translational research in AKI, Division of Renal Medicine, BWH, Boston.
Dr. Gupta and Dr. Leaf believe their risk score for predicting severe AKI after intravenous (IV) cisplatin, published online in The BMJ, is “more accurate and generalizable than prior models for several reasons,” they told this news organization in a joint email.
“First, we externally validated our findings across cancer centers other than the one where it was developed,” they said. “Second, we focused on moderate to severe kidney injury, the most clinically relevant form of kidney damage, whereas prior models examined more mild forms of kidney injury. Third, we collected data on nearly 25,000 patients receiving their first dose of IV cisplatin, which is larger than all previous studies combined.”
‘Herculean Effort’
“We conceived of this study back in 2018, contacted collaborators at each participating cancer center, and had numerous meetings to try to gather granular data on patients treated with their first dose of intravenous (IV) cisplatin,” Dr. Gupta and Dr. Leaf explained. They also incorporated patient feedback from focus groups and surveys.
“This was truly a Herculean effort that involved physicians, programmers, research coordinators, and patients,” they said.
The multicenter study included 24,717 patients — 11,766 in the derivation cohort and 12,951 in the validation cohort. Overall, the median age was about 60 years, about 58% were men, and about 78% were White.
The primary outcome was cisplatin-induced AKI (CP-AKI), defined as a twofold or greater increase in serum creatinine or kidney replacement therapy within 14 days of a first dose of IV cisplatin.
Their simple risk score consisting of nine covariates — age, hypertension, type 2 diabetes, hemoglobin level, white blood cell count, platelet count, serum albumin level, serum magnesium level, and cisplatin dose — predicted a higher risk for CP-AKI in both cohorts.
Notably, adding serum creatinine to the model did not change the area under the curve, and therefore, serum creatinine, though also an independent risk factor for CP-AKI, was not included in the score.
Patients in the highest risk category had 24-fold higher odds of CP-AKI in the derivation cohort and close to 18-fold higher odds in the validation cohort than those in the lowest risk category.
The primary model had a C statistic of 0.75 (95% CI, 0.73-0.76) and showed better discrimination for CP-AKI than previously published models, for which the C statistics ranged from 0.60 to 0.68. The first author of a paper on an earlier model, Shveta Motwani, MD, MMSc, of BWH and Dana-Farber Cancer Institute in Boston, is also a coauthor of the new study.
Greater severity of CP-AKI was associated with shorter 90-day survival (adjusted hazard ratio, 4.63; 95% CI, 3.56-6.02) for stage III CP-AKI vs no CP-AKI.
‘Definitive Work’
Joel M. Topf, MD, a nephrologist with expertise in chronic kidney disease in Detroit, who wasn’t involved in the development of the risk score, called the study “a definitive work on an important concept in oncology and nephrology.”
“While this is not the first attempt to devise a risk score, it is by far the biggest,” he told this news organization. Furthermore, the authors “used a diverse population, recruiting patients with a variety of cancers (previous attempts had often used a homogenous diagnosis, putting into question how generalizable the results were) from six different cancer centers.”
In addition, he said, “The authors did not restrict patients with chronic kidney disease or other significant comorbidities and used the geographic diversity to produce a cohort that has an age, gender, racial, and ethnic distribution, which is more representative of the US than previous, single-center attempts to risk score patients.”
An earlier model used the Kidney Disease: Improving Global Outcomes (KDIGO) consensus definition of AKI of an increase in serum creatinine of 0.3 mg/dL, he noted. “While a sensitive definition of AKI, it captures mild, hemodynamic increases in creatinine of questionable significance,” he said.
By contrast, the new score uses KDIGO stage II and above to define AKI. “This is a better choice, as we do not want to dissuade patients and doctors from choosing chemotherapy due to a fear of insignificant kidney damage,” he said.
All that said, Dr. Topf noted that neither the current score nor the earlier model included serum creatinine. “This is curious to me and may represent the small number of patients with representative elevated creatinine in the derivation cohort (only 1.3% with an estimated glomerular filtration rate [eGFR] < 45).”
“Since the cohort is made up of people who received cis-platinum, the low prevalence of eGFRs < 45 may be due to physicians steering away from cis-platinum in this group,” he suggested. “It would be unfortunate if this risk score gave an unintentional ‘green light’ to these patients, exposing them to predictable harm.”
‘Certainly Useful’
Anushree Shirali, MD, an associate professor in the Section of Nephrology and consulting physician, Yale Onco-Nephrology, Yale School of Medicine, in New Haven, Connecticut, said that having a prediction score for which patients are more likely to develop AKI after a single dose of cisplatin would be helpful for oncologists, as well as nephrologists.
As a nephrologist, Dr. Shirali mostly sees patients who already have AKI, she told this news organization. But there are circumstances in which the tool could still be helpful.
“Let’s say someone has abnormal kidney function at baseline — ie, creatinine is higher than the normal range — and they were on dialysis 5 years ago for something else, and now, they have cancer and may be given cisplatin. They worry about their chances of getting AKI and needing dialysis again,” she said. “That’s just one scenario in which I might be asked to answer that question and the tool would certainly be useful.”
Other scenarios could include someone who has just one kidney because they donated a kidney for transplant years ago, and now, they have a malignancy and wonder what their actual risk is of getting kidney issues on cisplatin.
Oncologists could use the tool to determine whether a patient should be treated with cisplatin, or if they’re at high risk, whether an alternative that’s not nephrotoxic might be used. By contrast, “if somebody’s low risk and an oncologist thinks cisplatin is the best agent they have, then they might want to go ahead and use it,” Dr. Shirali said.
Future research could take into consideration that CP-AKI is dose dependent, she suggested, because a prediction score that included the number of cisplatin doses could be even more helpful to determine risk. And, even though the derivation and validation cohorts for the new tool are representative of the US population, additional research should also include more racial/ethnic diversity, she said.
Dr. Gupta and Dr. Leaf hope their tool “will be utilized immediately by patients and providers to help predict an individual’s risk of cisplatin-associated kidney damage. It is easy to use, available for free online, and incorporates readily available clinical variables.”
If a patient is at high risk, the clinical team can consider preventive measures such as administering more IV fluids before receiving cisplatin or monitoring kidney function more closely afterward, they suggested.
Dr. Gupta reported research support from the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases. She also reported research funding from BTG International, GE HealthCare, and AstraZeneca outside the submitted work. She is a member of GlaxoSmithKline’s Global Anemia Council, a consultant for Secretome and Proletariat Therapeutics, and founder and president emeritus of the American Society of Onconephrology (unpaid). Dr. Leaf is supported by NIH grants, reported research support from BioPorto, BTG International, and Metro International Biotech, and has served as a consultant. Dr. Topf reported an ownership stake in a few DaVita-run dialysis clinics. He also runs a vascular access center and has participated in advisory boards with Cara Therapeutics, Vifor, Astra Zeneca, Bayer, Renibus Therapeutics, Travere Therapeutics, and GlaxoSmithKline. He is president of NephJC, a nonprofit educational organization with no industry support. Dr. Shirali declared no competing interests.
A version of this article appeared on Medscape.com.
Cisplatin is a preferred treatment for a wide range of cancers, including breast, head and neck, lung, ovary, and more. However, its side effects — particularly nephrotoxicity — can be severe. Kidney injury on cisplatin is associated with higher mortality and can jeopardize a patient’s eligibility for other therapies.
Now, in a large study using data from six US cancer centers, researchers have developed a risk algorithm to predict acute kidney injury (AKI) after cisplatin administration.
A risk prediction calculator based on the algorithm is available online for patients and providers to determine an individual patient›s risk for kidney injury from cisplatin using readily available clinical data.
Other risk scores and risk prediction models have been developed to help clinicians assess in advance whether a patient might develop AKI after receiving cisplatin, so that more careful monitoring, dose adjustments, or an alternative treatment, if available, might be considered.
However, previous models were limited by factors such as small sample sizes, lack of external validation, older data, and liberal definitions of AKI, said Shruti Gupta, MD, MPH, director of onco-nephrology at Brigham and Women’s Hospital (BWH) and Dana-Farber Cancer Institute, and David E. Leaf, MD, MMSc, director of clinical and translational research in AKI, Division of Renal Medicine, BWH, Boston.
Dr. Gupta and Dr. Leaf believe their risk score for predicting severe AKI after intravenous (IV) cisplatin, published online in The BMJ, is “more accurate and generalizable than prior models for several reasons,” they told this news organization in a joint email.
“First, we externally validated our findings across cancer centers other than the one where it was developed,” they said. “Second, we focused on moderate to severe kidney injury, the most clinically relevant form of kidney damage, whereas prior models examined more mild forms of kidney injury. Third, we collected data on nearly 25,000 patients receiving their first dose of IV cisplatin, which is larger than all previous studies combined.”
‘Herculean Effort’
“We conceived of this study back in 2018, contacted collaborators at each participating cancer center, and had numerous meetings to try to gather granular data on patients treated with their first dose of intravenous (IV) cisplatin,” Dr. Gupta and Dr. Leaf explained. They also incorporated patient feedback from focus groups and surveys.
“This was truly a Herculean effort that involved physicians, programmers, research coordinators, and patients,” they said.
The multicenter study included 24,717 patients — 11,766 in the derivation cohort and 12,951 in the validation cohort. Overall, the median age was about 60 years, about 58% were men, and about 78% were White.
The primary outcome was cisplatin-induced AKI (CP-AKI), defined as a twofold or greater increase in serum creatinine or kidney replacement therapy within 14 days of a first dose of IV cisplatin.
Their simple risk score consisting of nine covariates — age, hypertension, type 2 diabetes, hemoglobin level, white blood cell count, platelet count, serum albumin level, serum magnesium level, and cisplatin dose — predicted a higher risk for CP-AKI in both cohorts.
Notably, adding serum creatinine to the model did not change the area under the curve, and therefore, serum creatinine, though also an independent risk factor for CP-AKI, was not included in the score.
Patients in the highest risk category had 24-fold higher odds of CP-AKI in the derivation cohort and close to 18-fold higher odds in the validation cohort than those in the lowest risk category.
The primary model had a C statistic of 0.75 (95% CI, 0.73-0.76) and showed better discrimination for CP-AKI than previously published models, for which the C statistics ranged from 0.60 to 0.68. The first author of a paper on an earlier model, Shveta Motwani, MD, MMSc, of BWH and Dana-Farber Cancer Institute in Boston, is also a coauthor of the new study.
Greater severity of CP-AKI was associated with shorter 90-day survival (adjusted hazard ratio, 4.63; 95% CI, 3.56-6.02) for stage III CP-AKI vs no CP-AKI.
‘Definitive Work’
Joel M. Topf, MD, a nephrologist with expertise in chronic kidney disease in Detroit, who wasn’t involved in the development of the risk score, called the study “a definitive work on an important concept in oncology and nephrology.”
“While this is not the first attempt to devise a risk score, it is by far the biggest,” he told this news organization. Furthermore, the authors “used a diverse population, recruiting patients with a variety of cancers (previous attempts had often used a homogenous diagnosis, putting into question how generalizable the results were) from six different cancer centers.”
In addition, he said, “The authors did not restrict patients with chronic kidney disease or other significant comorbidities and used the geographic diversity to produce a cohort that has an age, gender, racial, and ethnic distribution, which is more representative of the US than previous, single-center attempts to risk score patients.”
An earlier model used the Kidney Disease: Improving Global Outcomes (KDIGO) consensus definition of AKI of an increase in serum creatinine of 0.3 mg/dL, he noted. “While a sensitive definition of AKI, it captures mild, hemodynamic increases in creatinine of questionable significance,” he said.
By contrast, the new score uses KDIGO stage II and above to define AKI. “This is a better choice, as we do not want to dissuade patients and doctors from choosing chemotherapy due to a fear of insignificant kidney damage,” he said.
All that said, Dr. Topf noted that neither the current score nor the earlier model included serum creatinine. “This is curious to me and may represent the small number of patients with representative elevated creatinine in the derivation cohort (only 1.3% with an estimated glomerular filtration rate [eGFR] < 45).”
“Since the cohort is made up of people who received cis-platinum, the low prevalence of eGFRs < 45 may be due to physicians steering away from cis-platinum in this group,” he suggested. “It would be unfortunate if this risk score gave an unintentional ‘green light’ to these patients, exposing them to predictable harm.”
‘Certainly Useful’
Anushree Shirali, MD, an associate professor in the Section of Nephrology and consulting physician, Yale Onco-Nephrology, Yale School of Medicine, in New Haven, Connecticut, said that having a prediction score for which patients are more likely to develop AKI after a single dose of cisplatin would be helpful for oncologists, as well as nephrologists.
As a nephrologist, Dr. Shirali mostly sees patients who already have AKI, she told this news organization. But there are circumstances in which the tool could still be helpful.
“Let’s say someone has abnormal kidney function at baseline — ie, creatinine is higher than the normal range — and they were on dialysis 5 years ago for something else, and now, they have cancer and may be given cisplatin. They worry about their chances of getting AKI and needing dialysis again,” she said. “That’s just one scenario in which I might be asked to answer that question and the tool would certainly be useful.”
Other scenarios could include someone who has just one kidney because they donated a kidney for transplant years ago, and now, they have a malignancy and wonder what their actual risk is of getting kidney issues on cisplatin.
Oncologists could use the tool to determine whether a patient should be treated with cisplatin, or if they’re at high risk, whether an alternative that’s not nephrotoxic might be used. By contrast, “if somebody’s low risk and an oncologist thinks cisplatin is the best agent they have, then they might want to go ahead and use it,” Dr. Shirali said.
Future research could take into consideration that CP-AKI is dose dependent, she suggested, because a prediction score that included the number of cisplatin doses could be even more helpful to determine risk. And, even though the derivation and validation cohorts for the new tool are representative of the US population, additional research should also include more racial/ethnic diversity, she said.
Dr. Gupta and Dr. Leaf hope their tool “will be utilized immediately by patients and providers to help predict an individual’s risk of cisplatin-associated kidney damage. It is easy to use, available for free online, and incorporates readily available clinical variables.”
If a patient is at high risk, the clinical team can consider preventive measures such as administering more IV fluids before receiving cisplatin or monitoring kidney function more closely afterward, they suggested.
Dr. Gupta reported research support from the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases. She also reported research funding from BTG International, GE HealthCare, and AstraZeneca outside the submitted work. She is a member of GlaxoSmithKline’s Global Anemia Council, a consultant for Secretome and Proletariat Therapeutics, and founder and president emeritus of the American Society of Onconephrology (unpaid). Dr. Leaf is supported by NIH grants, reported research support from BioPorto, BTG International, and Metro International Biotech, and has served as a consultant. Dr. Topf reported an ownership stake in a few DaVita-run dialysis clinics. He also runs a vascular access center and has participated in advisory boards with Cara Therapeutics, Vifor, Astra Zeneca, Bayer, Renibus Therapeutics, Travere Therapeutics, and GlaxoSmithKline. He is president of NephJC, a nonprofit educational organization with no industry support. Dr. Shirali declared no competing interests.
A version of this article appeared on Medscape.com.
FROM THE BMJ
Growing Periumbilical Plaque: A Case of Perforating Calcific Elastosis
To the Editor:
Pseudoxanthoma elasticum (PXE) is a genetic perforating dermatosis characterized by fragmentation and calcification of elastic fibers that most commonly manifests on the skin, eyes, gastrointestinal tract, or cardiovascular system.1 Classic skin findings include multiple symmetric yellowish papules favoring the flexural surfaces of the body and neck as well as the periumbilical and inguinal regions.1,2 Many life-threatening complications from this disease can occur due to calcification of elastic fibers in other parts of the body, such as the internal elastic lamina of arteries, which can cause gastrointestinal tract bleeding and accelerated cardiovascular disease including valvular disease.2,3 If PXE is localized to the skin only without systemic involvement or a family history, a diagnosis of perforating calcific elastosis (PCE) can be made. We report a case of PCE in a patient with a growing umbilical lesion.
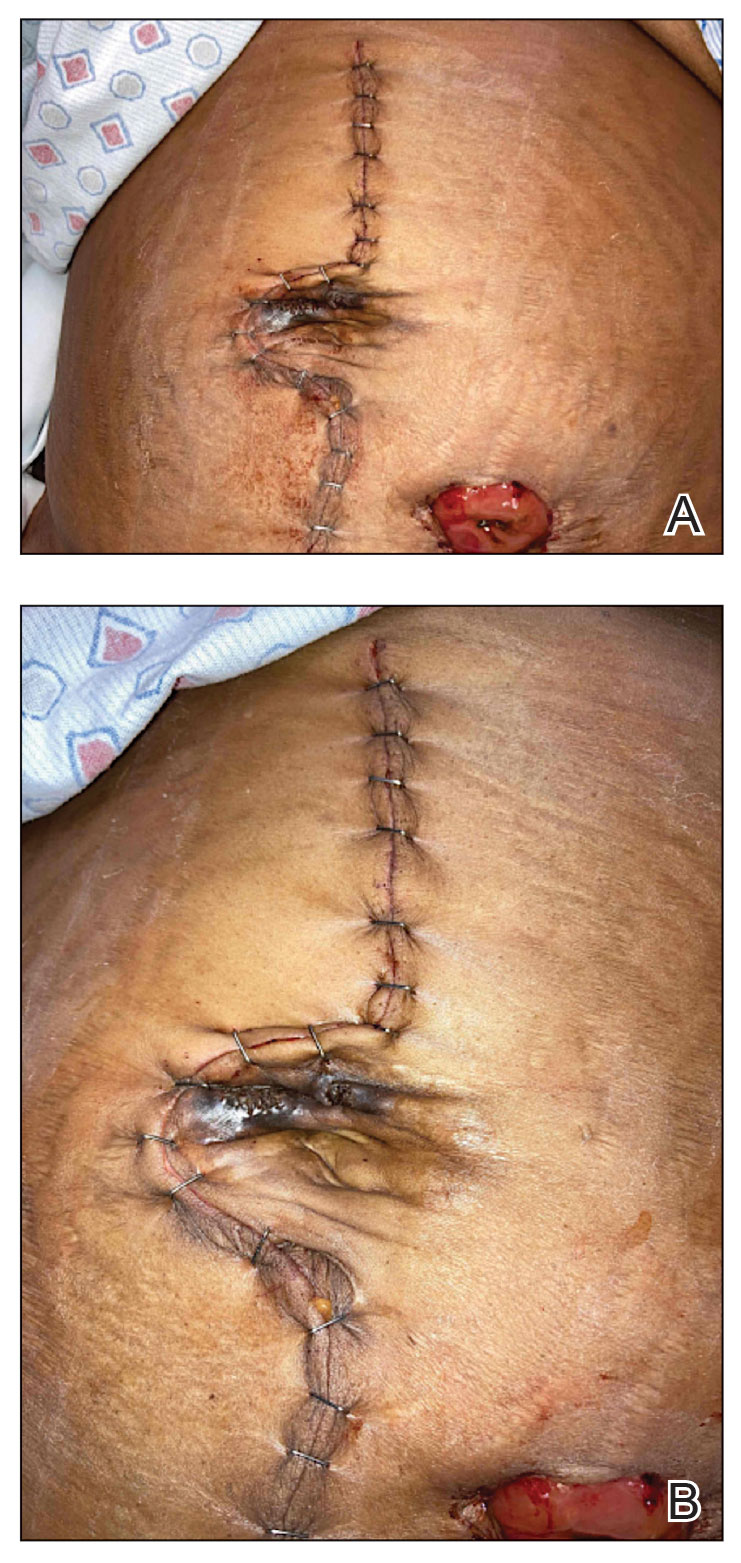
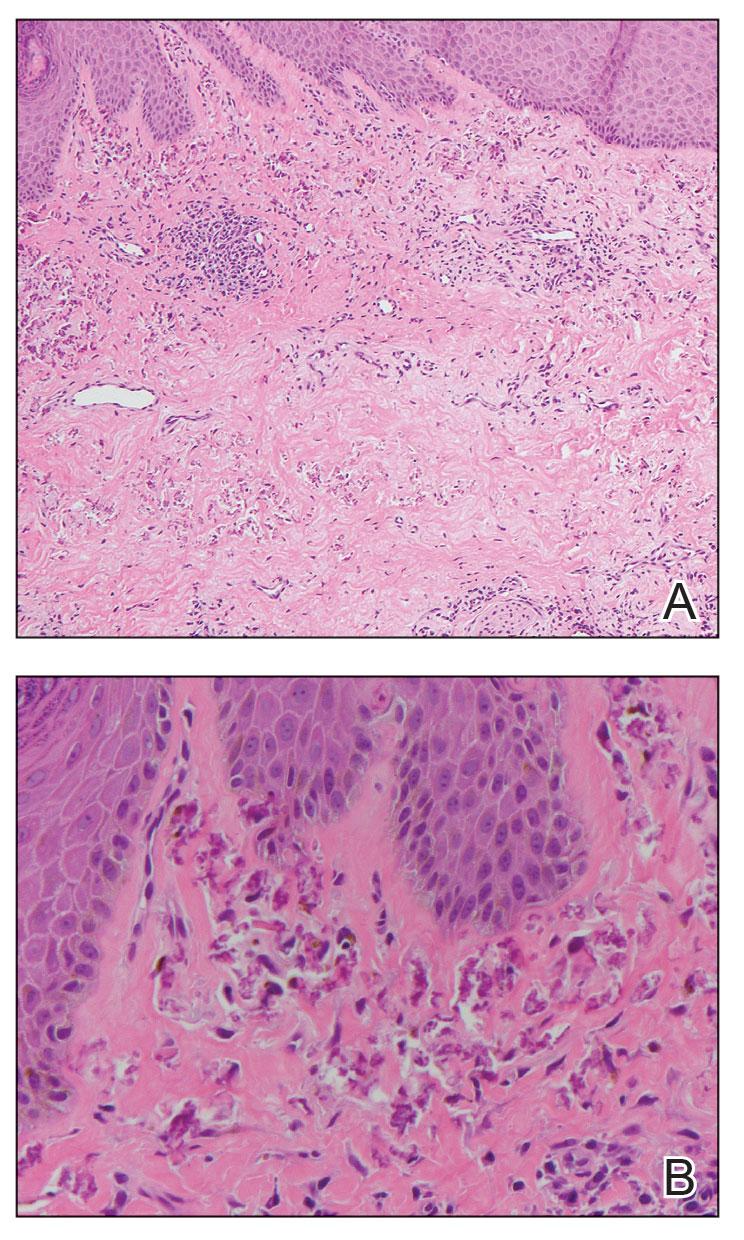
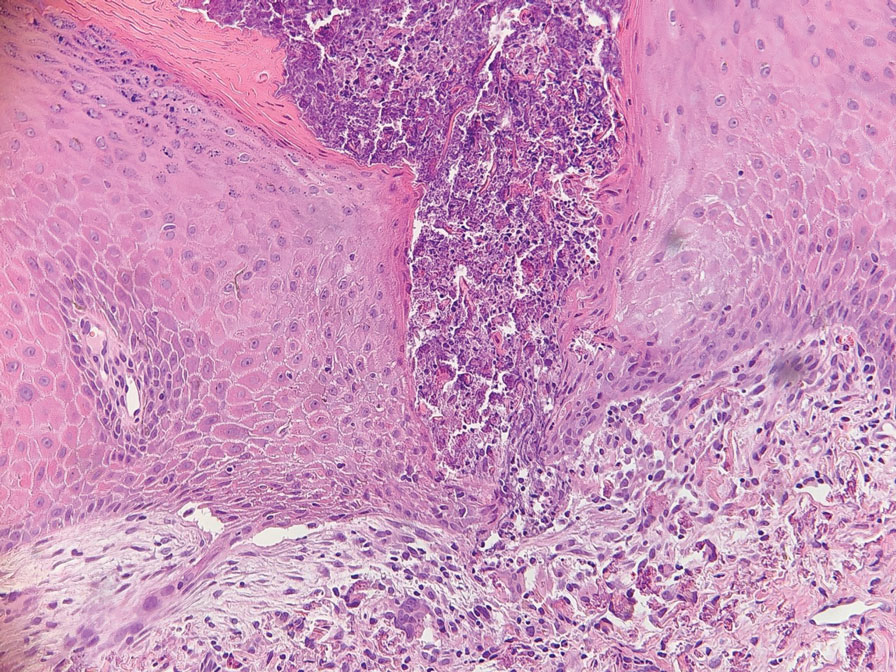
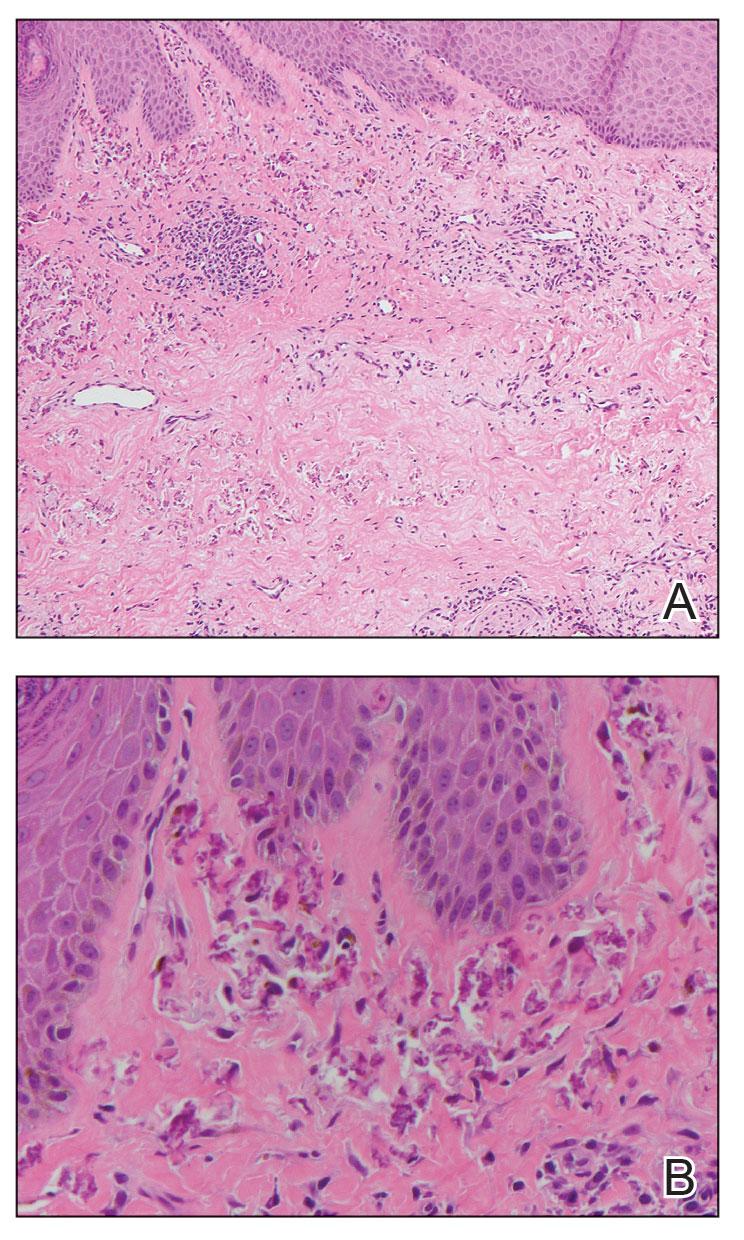
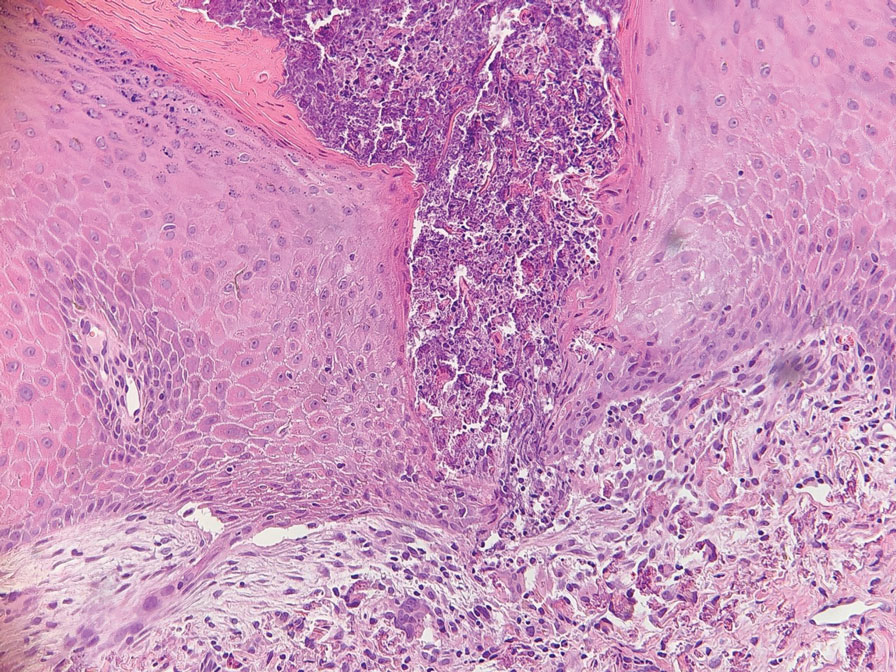
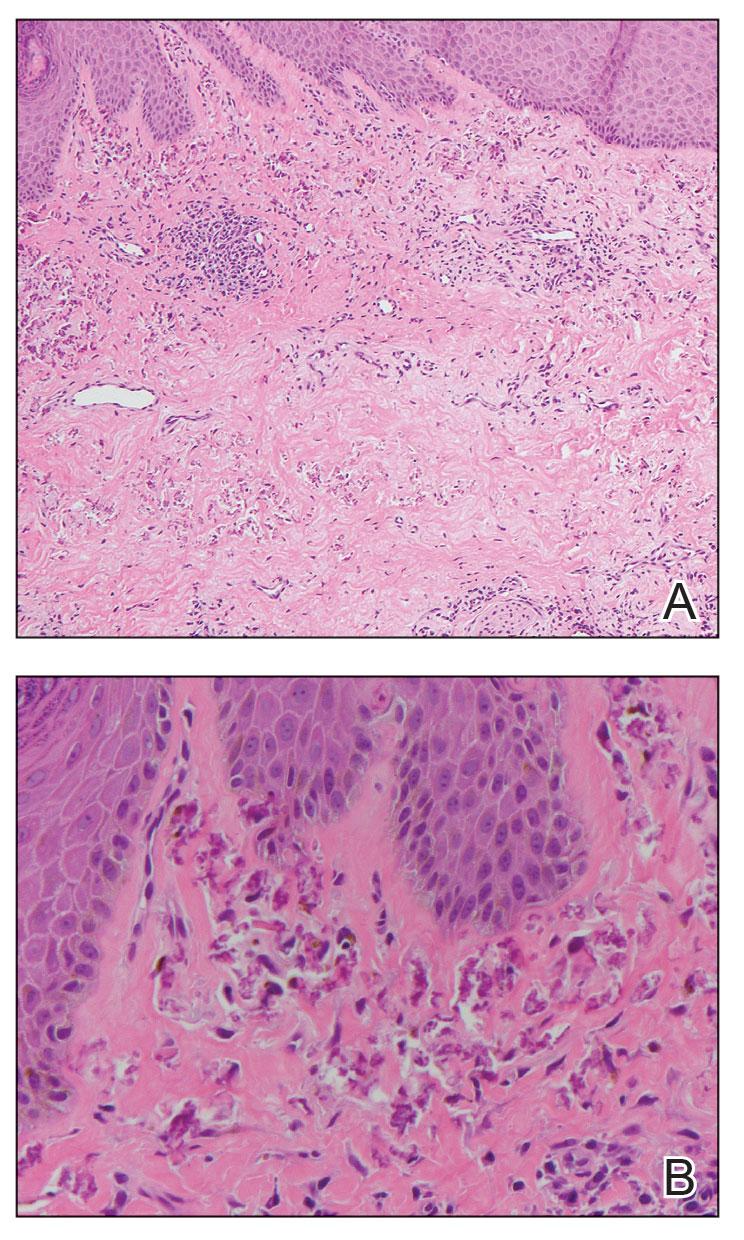
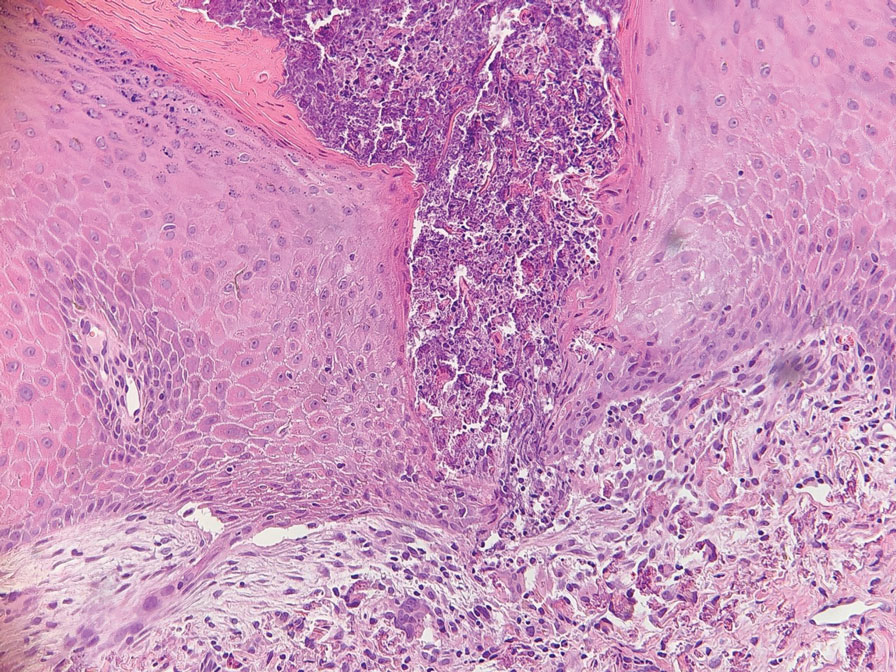
A 49-year-old multiparous (gravida 3, para 3) woman presented for evaluation of an evolving periumbilical lesion of 4 months’ duration. She denied pain, bleeding, or drainage from the area, as well as any systemic symptoms. The patient had a surgical history of a laparoscopic hysterectomy 7 years prior to the current presentation due to uterine fibroids, which resulted in a periumbilical scar. At the current presentation, physical examination revealed 2 hyperpigmented to violaceous periumbilical papules coalescing into a plaque with overlying hyperkeratosis and crusting (Figure 1). A punch biopsy was performed and histopathology showed diffuse dermal collections of degenerated eosinophilic distorted elastic fibers with calcification (Figure 2). Further sections showed a transepidermal channel in which the elastic fibers extruded from the dermis through the epidermis (Figure 3). The diagnosis of acquired PCE was made based on the clinical presentation, relevant medical history, and lack of underlying medical conditions or family history of PXE. No further workup was needed, and the patient reported no further progression and rather some improvement (decrease in size) of the lesion at 3-month follow-up.
Perforating calcific elastosis (also known as periumbilical perforating PXE) is a rare acquired condition that is seen predominantly in multiparous middle-aged women.4-6 This diagnosis consists of degenerated calcified elastic fibers that may perforate the skin of the abdominal or periumbilical region. It clinically manifests as multiple painless hyperkeratotic papules surrounding the periumbilical region.4-6
The etiology and pathogenesis of PCE have not been defined but have been attributed to recurrent stressing of elastic fibers due to repeat traumas,1 which is proposed to lead to degeneration of elastic fibers and calcification of damaged tissue.4-7 As a result, PCE most commonly manifests in multiparous, obese, middle-aged women and patients with multiple abdominal surgeries or ascites.1 It also has been reported in patients with renal failure due to deposition of abnormal calcium phosphate products onto elastic fibers.4 In our patient, the development of PCE was related to both multiparity and trauma from prior surgery.
The histopathologic findings of PCE and PXE are similar, warranting differentiation via thorough clinical examination as well as further investigation of the patient’s medical and family history. Both show degenerated, fragmented, curly elastic fibers with calcium deposition throughout the dermis and a transepidermal channel extruding these elastic fibers.7,8 The biopsies stain positive for elastic fibers and calcium deposition. Calcium staining can help to differentiate these entities from elastosis perforans serpiginosa, which lacks the presence of calcium staining.7
There are no definitive treatments for PCE. A single case report of a patient with PCE and renal failure showed regression with hemodialysis.9 In a study evaluating patients with inherited PXE, notable improvement was seen in skin lesions treated with bisphosphonates, possibly suggesting that regulating serum calcium may contribute to improvement of the disease.3 Most cases spontaneously resolve with atrophic plaques. Our patient required no additional treatment with no further progression and reported improvement of the lesion with spontaneous decrease in size.
- Jha AK, Zheeshan MD, Sinha BK, et al. Periumbilical perforating pseudoxanthoma elasticum: a rare case report. Dermatol Pract Concept. 2018;8:75-77. doi:10.5826/dpc.0802a02
- Ko JH, Shih YC, Huang YC, et al. Pseudoxanthoma elasticum. Lancet. 2013;381:565.
- Sherer DW, Singer G, Uribarri J, et al. Oral phosphate binders in the treatment of pseudoxanthoma elasticum. J Am Acad Dermatol. 2005;53:610-615.
- Lal NR, Bandyopadhyay D, Verma R, et al. Perforating calcific elastosis: revisiting a rare entity. Indian J Dermatol. 2018;63:186-188. doi:10.4103/ijd.IJD_111_17
- Kocatürk E, Kavala M, Zindanci I, et al. Periumbilical perforating pseudoxanthoma elasticum. Indian J Dermatol Venereol Leprol. 2009;75:329.
- Bressan AL, Vasconcelos BN, Silva RDS, et al. Periumbilical and periareolar perforating pseudoxanthoma elasticum. An Bras Dermatol. 2010;85:705-707. doi:10.1590/s0365-05962010000500018
- Hosen MJ, Lamoen A, De Paepe A, et al. Histopathology of pseudoxanthoma elasticum and related disorders: histological hallmarks and diagnostic clues. Scientifica (Cairo). 2012;2012:598262.
- Bathina M, Hedge SP, Shanavaz AA, et al. Pruritic periumbilical plaque as a presentation of rare perforating dermatosis. Indian Dermatol Online J. 2020;11:68-71. doi:10.4103/idoj.IDOJ_95_19
- Sapadin AN, Lebwohl MG, Teich SA, et al. Periumbilical pseudoxanthoma elasticum associated with chronic renal failure and angioid streaks—apparent regression with hemodialysis. J Am Acad Dermatol. 1998;39:338-344.
To the Editor:
Pseudoxanthoma elasticum (PXE) is a genetic perforating dermatosis characterized by fragmentation and calcification of elastic fibers that most commonly manifests on the skin, eyes, gastrointestinal tract, or cardiovascular system.1 Classic skin findings include multiple symmetric yellowish papules favoring the flexural surfaces of the body and neck as well as the periumbilical and inguinal regions.1,2 Many life-threatening complications from this disease can occur due to calcification of elastic fibers in other parts of the body, such as the internal elastic lamina of arteries, which can cause gastrointestinal tract bleeding and accelerated cardiovascular disease including valvular disease.2,3 If PXE is localized to the skin only without systemic involvement or a family history, a diagnosis of perforating calcific elastosis (PCE) can be made. We report a case of PCE in a patient with a growing umbilical lesion.
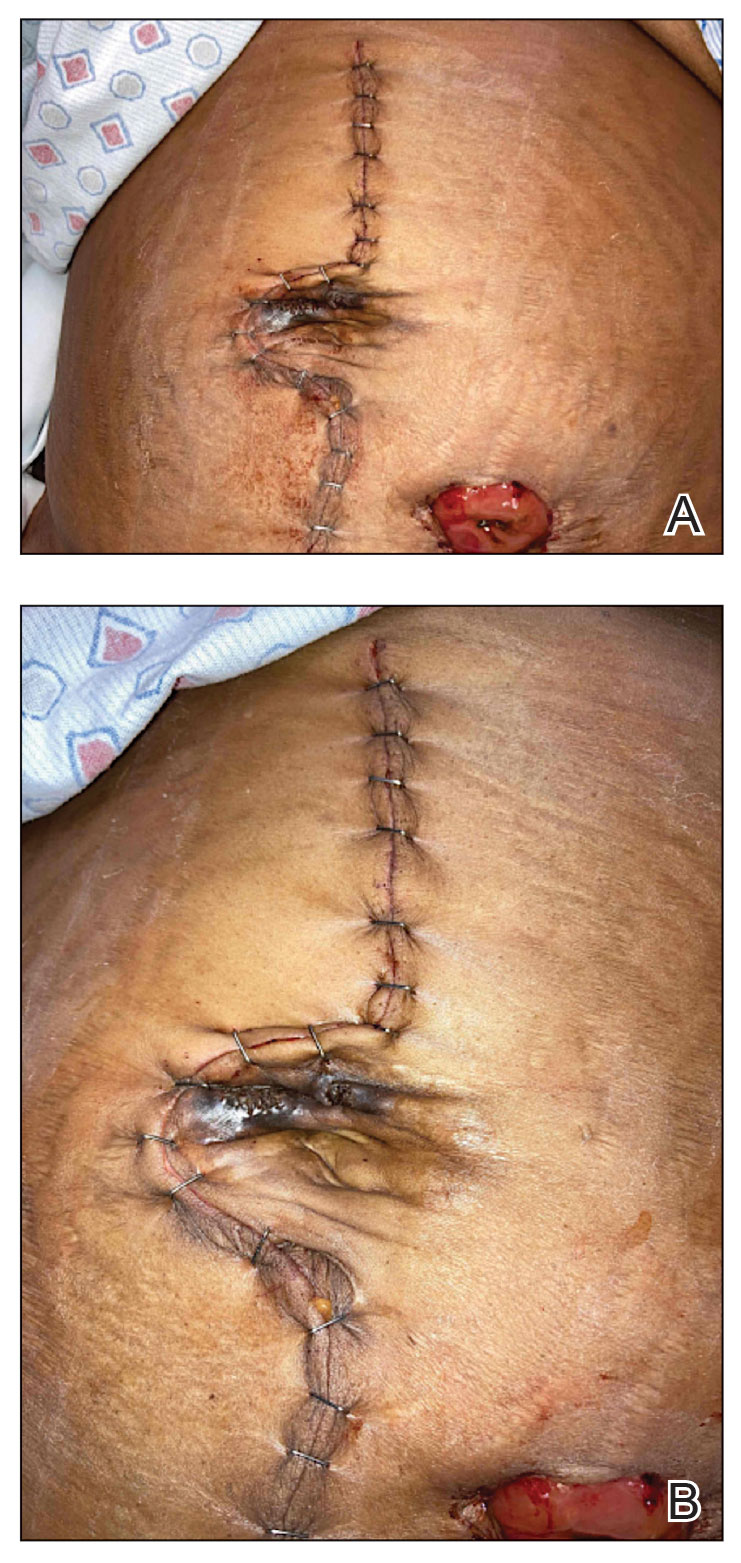
A 49-year-old multiparous (gravida 3, para 3) woman presented for evaluation of an evolving periumbilical lesion of 4 months’ duration. She denied pain, bleeding, or drainage from the area, as well as any systemic symptoms. The patient had a surgical history of a laparoscopic hysterectomy 7 years prior to the current presentation due to uterine fibroids, which resulted in a periumbilical scar. At the current presentation, physical examination revealed 2 hyperpigmented to violaceous periumbilical papules coalescing into a plaque with overlying hyperkeratosis and crusting (Figure 1). A punch biopsy was performed and histopathology showed diffuse dermal collections of degenerated eosinophilic distorted elastic fibers with calcification (Figure 2). Further sections showed a transepidermal channel in which the elastic fibers extruded from the dermis through the epidermis (Figure 3). The diagnosis of acquired PCE was made based on the clinical presentation, relevant medical history, and lack of underlying medical conditions or family history of PXE. No further workup was needed, and the patient reported no further progression and rather some improvement (decrease in size) of the lesion at 3-month follow-up.
Perforating calcific elastosis (also known as periumbilical perforating PXE) is a rare acquired condition that is seen predominantly in multiparous middle-aged women.4-6 This diagnosis consists of degenerated calcified elastic fibers that may perforate the skin of the abdominal or periumbilical region. It clinically manifests as multiple painless hyperkeratotic papules surrounding the periumbilical region.4-6
The etiology and pathogenesis of PCE have not been defined but have been attributed to recurrent stressing of elastic fibers due to repeat traumas,1 which is proposed to lead to degeneration of elastic fibers and calcification of damaged tissue.4-7 As a result, PCE most commonly manifests in multiparous, obese, middle-aged women and patients with multiple abdominal surgeries or ascites.1 It also has been reported in patients with renal failure due to deposition of abnormal calcium phosphate products onto elastic fibers.4 In our patient, the development of PCE was related to both multiparity and trauma from prior surgery.
The histopathologic findings of PCE and PXE are similar, warranting differentiation via thorough clinical examination as well as further investigation of the patient’s medical and family history. Both show degenerated, fragmented, curly elastic fibers with calcium deposition throughout the dermis and a transepidermal channel extruding these elastic fibers.7,8 The biopsies stain positive for elastic fibers and calcium deposition. Calcium staining can help to differentiate these entities from elastosis perforans serpiginosa, which lacks the presence of calcium staining.7
There are no definitive treatments for PCE. A single case report of a patient with PCE and renal failure showed regression with hemodialysis.9 In a study evaluating patients with inherited PXE, notable improvement was seen in skin lesions treated with bisphosphonates, possibly suggesting that regulating serum calcium may contribute to improvement of the disease.3 Most cases spontaneously resolve with atrophic plaques. Our patient required no additional treatment with no further progression and reported improvement of the lesion with spontaneous decrease in size.
To the Editor:
Pseudoxanthoma elasticum (PXE) is a genetic perforating dermatosis characterized by fragmentation and calcification of elastic fibers that most commonly manifests on the skin, eyes, gastrointestinal tract, or cardiovascular system.1 Classic skin findings include multiple symmetric yellowish papules favoring the flexural surfaces of the body and neck as well as the periumbilical and inguinal regions.1,2 Many life-threatening complications from this disease can occur due to calcification of elastic fibers in other parts of the body, such as the internal elastic lamina of arteries, which can cause gastrointestinal tract bleeding and accelerated cardiovascular disease including valvular disease.2,3 If PXE is localized to the skin only without systemic involvement or a family history, a diagnosis of perforating calcific elastosis (PCE) can be made. We report a case of PCE in a patient with a growing umbilical lesion.
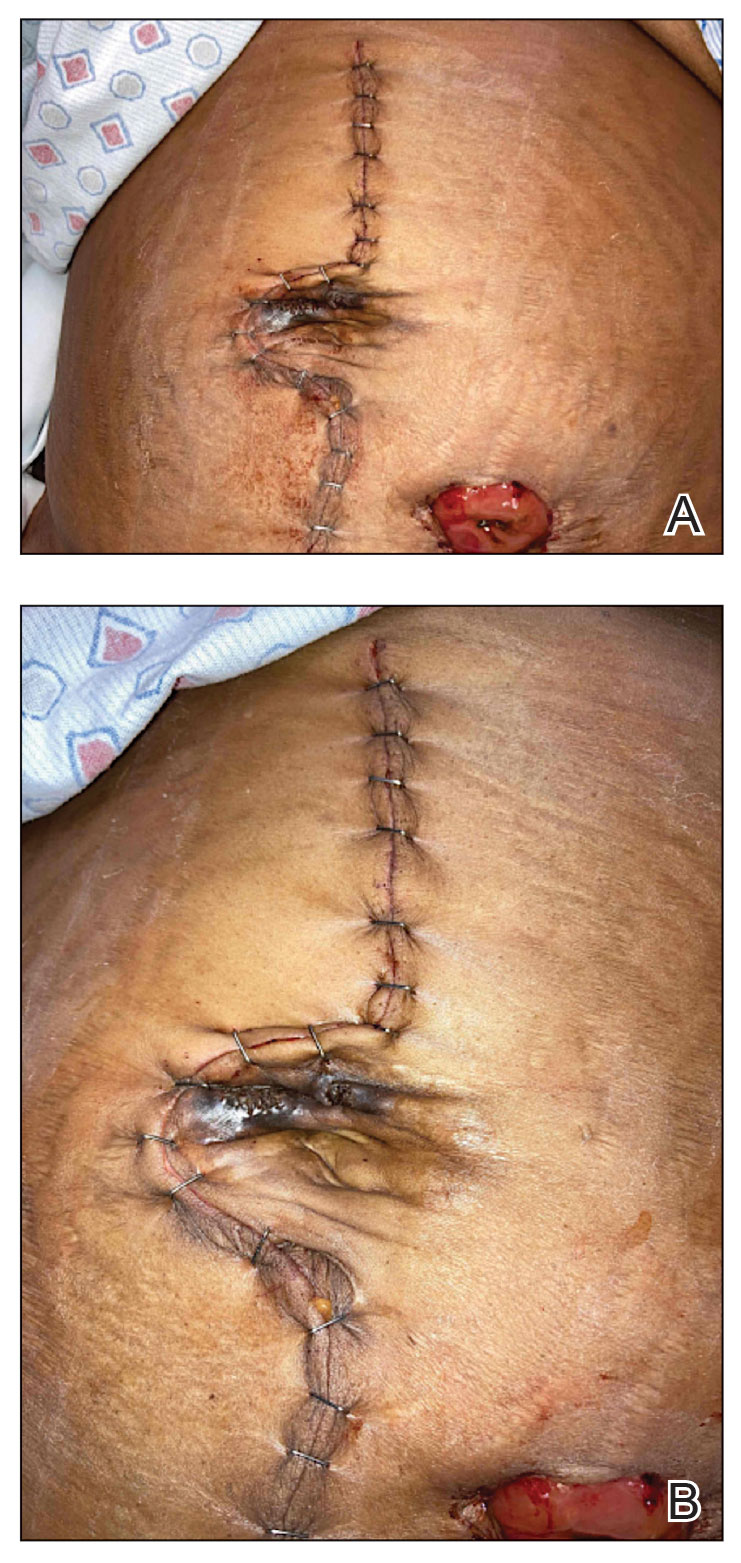
A 49-year-old multiparous (gravida 3, para 3) woman presented for evaluation of an evolving periumbilical lesion of 4 months’ duration. She denied pain, bleeding, or drainage from the area, as well as any systemic symptoms. The patient had a surgical history of a laparoscopic hysterectomy 7 years prior to the current presentation due to uterine fibroids, which resulted in a periumbilical scar. At the current presentation, physical examination revealed 2 hyperpigmented to violaceous periumbilical papules coalescing into a plaque with overlying hyperkeratosis and crusting (Figure 1). A punch biopsy was performed and histopathology showed diffuse dermal collections of degenerated eosinophilic distorted elastic fibers with calcification (Figure 2). Further sections showed a transepidermal channel in which the elastic fibers extruded from the dermis through the epidermis (Figure 3). The diagnosis of acquired PCE was made based on the clinical presentation, relevant medical history, and lack of underlying medical conditions or family history of PXE. No further workup was needed, and the patient reported no further progression and rather some improvement (decrease in size) of the lesion at 3-month follow-up.
Perforating calcific elastosis (also known as periumbilical perforating PXE) is a rare acquired condition that is seen predominantly in multiparous middle-aged women.4-6 This diagnosis consists of degenerated calcified elastic fibers that may perforate the skin of the abdominal or periumbilical region. It clinically manifests as multiple painless hyperkeratotic papules surrounding the periumbilical region.4-6
The etiology and pathogenesis of PCE have not been defined but have been attributed to recurrent stressing of elastic fibers due to repeat traumas,1 which is proposed to lead to degeneration of elastic fibers and calcification of damaged tissue.4-7 As a result, PCE most commonly manifests in multiparous, obese, middle-aged women and patients with multiple abdominal surgeries or ascites.1 It also has been reported in patients with renal failure due to deposition of abnormal calcium phosphate products onto elastic fibers.4 In our patient, the development of PCE was related to both multiparity and trauma from prior surgery.
The histopathologic findings of PCE and PXE are similar, warranting differentiation via thorough clinical examination as well as further investigation of the patient’s medical and family history. Both show degenerated, fragmented, curly elastic fibers with calcium deposition throughout the dermis and a transepidermal channel extruding these elastic fibers.7,8 The biopsies stain positive for elastic fibers and calcium deposition. Calcium staining can help to differentiate these entities from elastosis perforans serpiginosa, which lacks the presence of calcium staining.7
There are no definitive treatments for PCE. A single case report of a patient with PCE and renal failure showed regression with hemodialysis.9 In a study evaluating patients with inherited PXE, notable improvement was seen in skin lesions treated with bisphosphonates, possibly suggesting that regulating serum calcium may contribute to improvement of the disease.3 Most cases spontaneously resolve with atrophic plaques. Our patient required no additional treatment with no further progression and reported improvement of the lesion with spontaneous decrease in size.
- Jha AK, Zheeshan MD, Sinha BK, et al. Periumbilical perforating pseudoxanthoma elasticum: a rare case report. Dermatol Pract Concept. 2018;8:75-77. doi:10.5826/dpc.0802a02
- Ko JH, Shih YC, Huang YC, et al. Pseudoxanthoma elasticum. Lancet. 2013;381:565.
- Sherer DW, Singer G, Uribarri J, et al. Oral phosphate binders in the treatment of pseudoxanthoma elasticum. J Am Acad Dermatol. 2005;53:610-615.
- Lal NR, Bandyopadhyay D, Verma R, et al. Perforating calcific elastosis: revisiting a rare entity. Indian J Dermatol. 2018;63:186-188. doi:10.4103/ijd.IJD_111_17
- Kocatürk E, Kavala M, Zindanci I, et al. Periumbilical perforating pseudoxanthoma elasticum. Indian J Dermatol Venereol Leprol. 2009;75:329.
- Bressan AL, Vasconcelos BN, Silva RDS, et al. Periumbilical and periareolar perforating pseudoxanthoma elasticum. An Bras Dermatol. 2010;85:705-707. doi:10.1590/s0365-05962010000500018
- Hosen MJ, Lamoen A, De Paepe A, et al. Histopathology of pseudoxanthoma elasticum and related disorders: histological hallmarks and diagnostic clues. Scientifica (Cairo). 2012;2012:598262.
- Bathina M, Hedge SP, Shanavaz AA, et al. Pruritic periumbilical plaque as a presentation of rare perforating dermatosis. Indian Dermatol Online J. 2020;11:68-71. doi:10.4103/idoj.IDOJ_95_19
- Sapadin AN, Lebwohl MG, Teich SA, et al. Periumbilical pseudoxanthoma elasticum associated with chronic renal failure and angioid streaks—apparent regression with hemodialysis. J Am Acad Dermatol. 1998;39:338-344.
- Jha AK, Zheeshan MD, Sinha BK, et al. Periumbilical perforating pseudoxanthoma elasticum: a rare case report. Dermatol Pract Concept. 2018;8:75-77. doi:10.5826/dpc.0802a02
- Ko JH, Shih YC, Huang YC, et al. Pseudoxanthoma elasticum. Lancet. 2013;381:565.
- Sherer DW, Singer G, Uribarri J, et al. Oral phosphate binders in the treatment of pseudoxanthoma elasticum. J Am Acad Dermatol. 2005;53:610-615.
- Lal NR, Bandyopadhyay D, Verma R, et al. Perforating calcific elastosis: revisiting a rare entity. Indian J Dermatol. 2018;63:186-188. doi:10.4103/ijd.IJD_111_17
- Kocatürk E, Kavala M, Zindanci I, et al. Periumbilical perforating pseudoxanthoma elasticum. Indian J Dermatol Venereol Leprol. 2009;75:329.
- Bressan AL, Vasconcelos BN, Silva RDS, et al. Periumbilical and periareolar perforating pseudoxanthoma elasticum. An Bras Dermatol. 2010;85:705-707. doi:10.1590/s0365-05962010000500018
- Hosen MJ, Lamoen A, De Paepe A, et al. Histopathology of pseudoxanthoma elasticum and related disorders: histological hallmarks and diagnostic clues. Scientifica (Cairo). 2012;2012:598262.
- Bathina M, Hedge SP, Shanavaz AA, et al. Pruritic periumbilical plaque as a presentation of rare perforating dermatosis. Indian Dermatol Online J. 2020;11:68-71. doi:10.4103/idoj.IDOJ_95_19
- Sapadin AN, Lebwohl MG, Teich SA, et al. Periumbilical pseudoxanthoma elasticum associated with chronic renal failure and angioid streaks—apparent regression with hemodialysis. J Am Acad Dermatol. 1998;39:338-344.
PRACTICE POINTS
- Perforating calcific elastosis (PCE) is a rare, localized, acquired variant of the inherited connective tissue disorder pseudoxanthoma elasticum (PXE).
- Histopathologic findings are identical for PCE and PXE, warranting differentiation via thorough clinical examination as well as further investigation of the patient’s medical and family history.
- Although there are no definitive treatments, most cases of PCE resolve spontaneously.
- Dermatologists should be aware of the importance of clinically differentiating PCE from PXE to prevent extensive workup, which can lead to unnecessary testing and increased morbidity in patients.
Study Evaluates CVD, Mortality Risks In Patients With Prurigo Nodularis
TOPLINE:
, particularly among women and White patients.
METHODOLOGY:
- Studies have shown increased risks for cardiovascular diseases in patients with PN, but limited sample sizes have hindered further subgroup analysis. Given PN’s pronounced sex and ethnicity skew, it is important to examine underrepresented groups to accurately assess their cardiovascular risk.
- In this propensity-score matched analysis, researchers identified 64,801 patients (59.44% women) with PN using electronic health reports from the Global Collaborative Network of TriNetX and matched to individuals without PN.
- Researchers calculated risks for 15 cardiovascular endpoints and all-cause mortality within 10 years of diagnosis. Major adverse cardiovascular events (MACE) included acute cerebral and myocardial infarction (MI), heart failure, ventricular arrhythmia, and sudden cardiac death.
TAKEAWAY:
- Patients with PN showed a higher risk for death (hazard ratio [HR], 1.1243) and MACE (HR, 1.117) (P < .0001 for both).
- PN was also associated with a higher risk for heart failure (HR, 1.062), thrombotic venous disease (HR, 1.26), angina pectoris (HR, 1.096), and peripheral arterial diseases (HR, 1.082) (P < .0001 for all) and for acute MI (HR, 1.11; P = .0015) and valve disorders (HR, 1.08; P = .0018).
- White patients with PN had a significantly increased risk for MACE, death, heart failure, cardiac arrest, vascular diseases, and acute MI, but this was not observed in people of color.
- Women exhibited a higher risk for MACE, heart failure, peripheral artery disease, acute MI, conduction disease, and valve disorders, while men did not have an increased risk for major or acute cardiovascular events. Both men and women had a higher risk for death, chronic ischemic heart disease, and venous disease.
IN PRACTICE:
“Although no novel PN-specific treatment rationale can be derived from the presented data, the potential risk of subsequent cardiovascular disease should be considered in the care of patients with PN, which includes screening and optimal management of other additional cardiovascular risk factors,” the authors wrote.
LIMITATIONS:
Retrospective observational design introduced inherent biases. Misdiagnosis or false coding in electronic health records could affect the data accuracy and ethnicity-specific analyses.
SOURCE:
This work, led by Henning Olbrich, from the Department of Dermatology, University of Lübeck, Germany, was published online in eBioMedicine.
DISCLOSURES:
The study was supported by the University of Lübeck, the Deutsche Forschungsgemeinschaft, and the State of Schleswig-Holstein. One author declared financial ties outside this work, and one author is an employee of TriNetX.
A version of this article appeared on Medscape.com.
TOPLINE:
, particularly among women and White patients.
METHODOLOGY:
- Studies have shown increased risks for cardiovascular diseases in patients with PN, but limited sample sizes have hindered further subgroup analysis. Given PN’s pronounced sex and ethnicity skew, it is important to examine underrepresented groups to accurately assess their cardiovascular risk.
- In this propensity-score matched analysis, researchers identified 64,801 patients (59.44% women) with PN using electronic health reports from the Global Collaborative Network of TriNetX and matched to individuals without PN.
- Researchers calculated risks for 15 cardiovascular endpoints and all-cause mortality within 10 years of diagnosis. Major adverse cardiovascular events (MACE) included acute cerebral and myocardial infarction (MI), heart failure, ventricular arrhythmia, and sudden cardiac death.
TAKEAWAY:
- Patients with PN showed a higher risk for death (hazard ratio [HR], 1.1243) and MACE (HR, 1.117) (P < .0001 for both).
- PN was also associated with a higher risk for heart failure (HR, 1.062), thrombotic venous disease (HR, 1.26), angina pectoris (HR, 1.096), and peripheral arterial diseases (HR, 1.082) (P < .0001 for all) and for acute MI (HR, 1.11; P = .0015) and valve disorders (HR, 1.08; P = .0018).
- White patients with PN had a significantly increased risk for MACE, death, heart failure, cardiac arrest, vascular diseases, and acute MI, but this was not observed in people of color.
- Women exhibited a higher risk for MACE, heart failure, peripheral artery disease, acute MI, conduction disease, and valve disorders, while men did not have an increased risk for major or acute cardiovascular events. Both men and women had a higher risk for death, chronic ischemic heart disease, and venous disease.
IN PRACTICE:
“Although no novel PN-specific treatment rationale can be derived from the presented data, the potential risk of subsequent cardiovascular disease should be considered in the care of patients with PN, which includes screening and optimal management of other additional cardiovascular risk factors,” the authors wrote.
LIMITATIONS:
Retrospective observational design introduced inherent biases. Misdiagnosis or false coding in electronic health records could affect the data accuracy and ethnicity-specific analyses.
SOURCE:
This work, led by Henning Olbrich, from the Department of Dermatology, University of Lübeck, Germany, was published online in eBioMedicine.
DISCLOSURES:
The study was supported by the University of Lübeck, the Deutsche Forschungsgemeinschaft, and the State of Schleswig-Holstein. One author declared financial ties outside this work, and one author is an employee of TriNetX.
A version of this article appeared on Medscape.com.
TOPLINE:
, particularly among women and White patients.
METHODOLOGY:
- Studies have shown increased risks for cardiovascular diseases in patients with PN, but limited sample sizes have hindered further subgroup analysis. Given PN’s pronounced sex and ethnicity skew, it is important to examine underrepresented groups to accurately assess their cardiovascular risk.
- In this propensity-score matched analysis, researchers identified 64,801 patients (59.44% women) with PN using electronic health reports from the Global Collaborative Network of TriNetX and matched to individuals without PN.
- Researchers calculated risks for 15 cardiovascular endpoints and all-cause mortality within 10 years of diagnosis. Major adverse cardiovascular events (MACE) included acute cerebral and myocardial infarction (MI), heart failure, ventricular arrhythmia, and sudden cardiac death.
TAKEAWAY:
- Patients with PN showed a higher risk for death (hazard ratio [HR], 1.1243) and MACE (HR, 1.117) (P < .0001 for both).
- PN was also associated with a higher risk for heart failure (HR, 1.062), thrombotic venous disease (HR, 1.26), angina pectoris (HR, 1.096), and peripheral arterial diseases (HR, 1.082) (P < .0001 for all) and for acute MI (HR, 1.11; P = .0015) and valve disorders (HR, 1.08; P = .0018).
- White patients with PN had a significantly increased risk for MACE, death, heart failure, cardiac arrest, vascular diseases, and acute MI, but this was not observed in people of color.
- Women exhibited a higher risk for MACE, heart failure, peripheral artery disease, acute MI, conduction disease, and valve disorders, while men did not have an increased risk for major or acute cardiovascular events. Both men and women had a higher risk for death, chronic ischemic heart disease, and venous disease.
IN PRACTICE:
“Although no novel PN-specific treatment rationale can be derived from the presented data, the potential risk of subsequent cardiovascular disease should be considered in the care of patients with PN, which includes screening and optimal management of other additional cardiovascular risk factors,” the authors wrote.
LIMITATIONS:
Retrospective observational design introduced inherent biases. Misdiagnosis or false coding in electronic health records could affect the data accuracy and ethnicity-specific analyses.
SOURCE:
This work, led by Henning Olbrich, from the Department of Dermatology, University of Lübeck, Germany, was published online in eBioMedicine.
DISCLOSURES:
The study was supported by the University of Lübeck, the Deutsche Forschungsgemeinschaft, and the State of Schleswig-Holstein. One author declared financial ties outside this work, and one author is an employee of TriNetX.
A version of this article appeared on Medscape.com.
Do Patients Benefit from Cancer Trial Participation?
TOPLINE:
METHODOLOGY:
- The view that patients with cancer benefit from access to investigational drugs in the clinical trial setting is widely held but does necessarily align with trial findings, which often show limited evidence of a clinical benefit. First, most investigational treatments assessed in clinical trials fail to gain regulatory approval, and the minority that are approved tend to offer minimal clinical benefit, experts explained.
- To estimate the survival benefit and toxicities associated with receiving experimental treatments, researchers conducted a meta-analysis of 128 trials comprising 141 comparisons of an investigational drug and a control treatment, which included immunotherapies and targeted therapies.
- The analysis included 42 trials in non–small cell lung cancer (NSCLC), 37 in breast cancer, 15 in hepatobiliary cancer, 13 in pancreatic cancer, 12 in colorectal cancer, and 10 in prostate cancer, involving a total of 47,050 patients.
- The primary outcome was PFS and secondary outcomes were overall survival and grades 3-5 serious adverse events.
TAKEAWAY:
- Overall, the experimental treatment was associated with a 20% improvement in PFS (pooled hazard ratio [HR], 0.80), corresponding to a median 1.25-month PFS advantage. The PFS benefit was seen across all cancer types, except pancreatic cancer.
- Overall survival improved by 8% with experimental agents (HR, 0.92), corresponding to 1.18 additional months. A significant overall survival benefit was seen across NSCLC, breast cancer, and hepatobiliary cancer trials but not pancreatic, prostate, colorectal cancer trials.
- Patients in the experimental intervention group, however, experienced much higher risk for grade 3-5 serious adverse events (risk ratio [RR], 1.27), corresponding to 7.40% increase in absolute risk. The greater risk for serious adverse events was significant for all indications except prostate cancer (RR, 1.13; 95% CI, 0.91-1.40).
IN PRACTICE:
“We believe our findings are best interpreted as suggesting that access to experimental interventions that have not yet received full FDA approval is associated with a marginal but nonzero clinical benefit,” the authors wrote.
“Although our findings seem to reflect poorly on trials as a vehicle for extending survival for participants, they have reassuring implications for clinical investigators, policymakers, and institutional review boards,” the researchers said, explaining that this “scenario allows clinical trials to continue to pursue promising new treatments — supporting incremental advances that sum to large gains over extended periods of research — without disadvantaging patients in comparator groups.”
SOURCE:
Renata Iskander, MSc, of McGill University, Montreal, Quebec, Canada, led this work, which was published online on April 29, 2024, in Annals of Internal Medicine.
LIMITATIONS:
There was high heterogeneity across studies due to variations in drugs tested, comparators used, and populations involved. The use of comparators below standard care could have inflated survival benefits. Additionally, data collected from ClinicalTrials.gov might be biased due to some trials not being reported.
DISCLOSURES:
Canadian Institutes of Health Research supported this work. The authors received grants for this work from McGill University, Rossy Cancer Network, and National Science Foundation. One author received consulting fees outside this work. The other authors declared no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The view that patients with cancer benefit from access to investigational drugs in the clinical trial setting is widely held but does necessarily align with trial findings, which often show limited evidence of a clinical benefit. First, most investigational treatments assessed in clinical trials fail to gain regulatory approval, and the minority that are approved tend to offer minimal clinical benefit, experts explained.
- To estimate the survival benefit and toxicities associated with receiving experimental treatments, researchers conducted a meta-analysis of 128 trials comprising 141 comparisons of an investigational drug and a control treatment, which included immunotherapies and targeted therapies.
- The analysis included 42 trials in non–small cell lung cancer (NSCLC), 37 in breast cancer, 15 in hepatobiliary cancer, 13 in pancreatic cancer, 12 in colorectal cancer, and 10 in prostate cancer, involving a total of 47,050 patients.
- The primary outcome was PFS and secondary outcomes were overall survival and grades 3-5 serious adverse events.
TAKEAWAY:
- Overall, the experimental treatment was associated with a 20% improvement in PFS (pooled hazard ratio [HR], 0.80), corresponding to a median 1.25-month PFS advantage. The PFS benefit was seen across all cancer types, except pancreatic cancer.
- Overall survival improved by 8% with experimental agents (HR, 0.92), corresponding to 1.18 additional months. A significant overall survival benefit was seen across NSCLC, breast cancer, and hepatobiliary cancer trials but not pancreatic, prostate, colorectal cancer trials.
- Patients in the experimental intervention group, however, experienced much higher risk for grade 3-5 serious adverse events (risk ratio [RR], 1.27), corresponding to 7.40% increase in absolute risk. The greater risk for serious adverse events was significant for all indications except prostate cancer (RR, 1.13; 95% CI, 0.91-1.40).
IN PRACTICE:
“We believe our findings are best interpreted as suggesting that access to experimental interventions that have not yet received full FDA approval is associated with a marginal but nonzero clinical benefit,” the authors wrote.
“Although our findings seem to reflect poorly on trials as a vehicle for extending survival for participants, they have reassuring implications for clinical investigators, policymakers, and institutional review boards,” the researchers said, explaining that this “scenario allows clinical trials to continue to pursue promising new treatments — supporting incremental advances that sum to large gains over extended periods of research — without disadvantaging patients in comparator groups.”
SOURCE:
Renata Iskander, MSc, of McGill University, Montreal, Quebec, Canada, led this work, which was published online on April 29, 2024, in Annals of Internal Medicine.
LIMITATIONS:
There was high heterogeneity across studies due to variations in drugs tested, comparators used, and populations involved. The use of comparators below standard care could have inflated survival benefits. Additionally, data collected from ClinicalTrials.gov might be biased due to some trials not being reported.
DISCLOSURES:
Canadian Institutes of Health Research supported this work. The authors received grants for this work from McGill University, Rossy Cancer Network, and National Science Foundation. One author received consulting fees outside this work. The other authors declared no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The view that patients with cancer benefit from access to investigational drugs in the clinical trial setting is widely held but does necessarily align with trial findings, which often show limited evidence of a clinical benefit. First, most investigational treatments assessed in clinical trials fail to gain regulatory approval, and the minority that are approved tend to offer minimal clinical benefit, experts explained.
- To estimate the survival benefit and toxicities associated with receiving experimental treatments, researchers conducted a meta-analysis of 128 trials comprising 141 comparisons of an investigational drug and a control treatment, which included immunotherapies and targeted therapies.
- The analysis included 42 trials in non–small cell lung cancer (NSCLC), 37 in breast cancer, 15 in hepatobiliary cancer, 13 in pancreatic cancer, 12 in colorectal cancer, and 10 in prostate cancer, involving a total of 47,050 patients.
- The primary outcome was PFS and secondary outcomes were overall survival and grades 3-5 serious adverse events.
TAKEAWAY:
- Overall, the experimental treatment was associated with a 20% improvement in PFS (pooled hazard ratio [HR], 0.80), corresponding to a median 1.25-month PFS advantage. The PFS benefit was seen across all cancer types, except pancreatic cancer.
- Overall survival improved by 8% with experimental agents (HR, 0.92), corresponding to 1.18 additional months. A significant overall survival benefit was seen across NSCLC, breast cancer, and hepatobiliary cancer trials but not pancreatic, prostate, colorectal cancer trials.
- Patients in the experimental intervention group, however, experienced much higher risk for grade 3-5 serious adverse events (risk ratio [RR], 1.27), corresponding to 7.40% increase in absolute risk. The greater risk for serious adverse events was significant for all indications except prostate cancer (RR, 1.13; 95% CI, 0.91-1.40).
IN PRACTICE:
“We believe our findings are best interpreted as suggesting that access to experimental interventions that have not yet received full FDA approval is associated with a marginal but nonzero clinical benefit,” the authors wrote.
“Although our findings seem to reflect poorly on trials as a vehicle for extending survival for participants, they have reassuring implications for clinical investigators, policymakers, and institutional review boards,” the researchers said, explaining that this “scenario allows clinical trials to continue to pursue promising new treatments — supporting incremental advances that sum to large gains over extended periods of research — without disadvantaging patients in comparator groups.”
SOURCE:
Renata Iskander, MSc, of McGill University, Montreal, Quebec, Canada, led this work, which was published online on April 29, 2024, in Annals of Internal Medicine.
LIMITATIONS:
There was high heterogeneity across studies due to variations in drugs tested, comparators used, and populations involved. The use of comparators below standard care could have inflated survival benefits. Additionally, data collected from ClinicalTrials.gov might be biased due to some trials not being reported.
DISCLOSURES:
Canadian Institutes of Health Research supported this work. The authors received grants for this work from McGill University, Rossy Cancer Network, and National Science Foundation. One author received consulting fees outside this work. The other authors declared no competing interests.
A version of this article appeared on Medscape.com.
Do Health-Related Social Needs Raise Mortality Risk in Cancer Survivors?
Little is known about the specific association between health-related social needs (HRSNs) and mortality risk even though HRSNs, defined as challenges in affording food, housing, and other necessities of daily living, are potential challenges for cancer survivors, wrote Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and colleagues.
A 2020 study by Dr. Zheng and colleagues published in the Journal of the National Comprehensive Cancer Network (NCCN) showed that food insecurity and financial worries had a negative impact on cancer survivorship. In the new study, published in Cancer, the researchers identified cancer survivors using the 2013-2018 National Health Interview Survey (NHIS) and the NHIS Mortality File through December 31, 2019. The researchers examined mortality using the data from the Centers for Disease Control and Prevention’s National Death Index (NDI) through December 31, 2019, which links to the National Health Interview Survey Data used in the study.
Individuals’ HRSNs were categorized into three groups: severe, moderate, and minor/none. HRSNs included food insecurity and nonmedical financial concerns, such as housing costs (rent, mortgage). Medical financial hardship included material, psychological, and behavioral domains and was divided into three groups: 2-3 domains, 1 domain, or 0 domains.
What Are the Potential Financial Implications of this Research?
The high costs of cancer care often cause medical financial hardships for cancer survivors, and expenses also may cause psychological distress and nonmedical financial hardship as survivors try to make ends meet while facing medical bills, wrote Dr. Zheng and colleagues.
Policy makers are increasingly interested in adding HRSNs to insurance coverage; recent guidance from the Centers for Medicare & Medicaid Services (CMS) allows individual states to apply to provide nutrition and housing supports through state Medicaid programs, according to authors of a 2023 article published in JAMA Health Forum.
The new study adds to the understanding of how HRSNs impact people with cancer by examining the association with mortality risk, Yelak Biru, MSc, president and chief executive officer of the International Myeloma Foundation, said in an interview.
“This is a key area of study for addressing the disparities in treatments and outcomes that result in inequities,” said Mr. Biru, a patient advocate and multiple myeloma survivor who was not involved in the study.
What Does the New Study Show?
The new study characterized HRSNs in 5,855 adult cancer survivors aged 18-64 years and 5,918 aged 65-79 years. In the 18- to 64-year-old group, 25.5% reported moderate levels of HRSNs, and 18.3% reported severe HRSNs. In patients aged 65-79 years, 15.6% and 6.6% reported moderate HRSNs and severe HRSNs, respectively.
Severe HRSN was significantly associated with higher mortality risk in an adjusted analysis in patients aged 18-64 years (hazard ratio 2.00, P < .001).
Among adults aged 65-79 years, severe HRSN was not associated with higher mortality risk; however, in this older age group, those with 2-3 domains of medical financial hardship had significantly increased mortality risk compared with adults aged 65-79 years with zero domains of medical financial hardship (HR 1.58, P = .007).
Although the findings that HRSNs were associated with increased mortality risk, especially in the younger group, were not surprising, they serve as a call to action to address how HRSNs are contributing to cancer mortality, Mr. Biru said in an interview. “HRSNs, like food or housing insecurity, can lead to patients being unable to undergo the best treatment approach for their cancer,” he said.
What Are the Limitations and Research Gaps?
The study findings were limited by several factors including the use of self-reports to measure medical financial hardship, food insecurity, and nonmedical financial concerns in the NHIS, the researchers wrote in their discussion. More research with longer follow-up time beyond 1-5 years is needed, wrote Dr. Zheng and colleagues.
Studies also are needed to illustrate how patient navigation can help prevent patients from falling through the cracks with regard to social needs and financial hardships, Mr. Biru told this news organization.
Other areas for research include how addressing social needs affects health outcomes and whether programs designed to address social needs are effective, he said.
“Finally, qualitative research is needed to capture the lived experiences of cancer survivors facing these challenges. This knowledge can inform the development of more patient-centered interventions and policies that effectively address the social determinants of health and improve overall outcomes for all cancer survivors,” Mr. Biru said.
What Is the Takeaway Message for Clinicians?
HRSNs and financial hardship are significantly associated with increased risk of mortality in adult cancer survivors, Dr. Zheng and colleagues concluded. Looking ahead, comprehensive assessment of HRSNs and financial hardship may help clinicians connect patients with relevant services to mitigate the social and financial impacts of cancer, they wrote.
“The takeaway message for oncologists in practice is that addressing [HRSNs] and financial hardship is crucial for providing comprehensive and equitable cancer care,” Mr. Biru said during his interview.
“The impact of social determinants of health on cancer outcomes cannot be ignored, and oncologists play a vital role in identifying and addressing these needs,” he said. Sensitive, discussion-based screenings are needed to identify core needs such as food and transportation, but clinicians also can consider broader social factors and work with a team to connect patients to appropriate resources, he added.
“By recognizing the importance of HRSN screening and taking proactive steps to address these needs, oncologists can contribute to improving health outcomes, reducing healthcare disparities, and providing more equitable cancer care for their patients,” he said.
What Other Guidance Is Available?
“High-quality cancer care requires treating the whole person; measuring and addressing anything in their life that could result in poorer health outcomes is a key component of comprehensive care,” Mr. Biru emphasized.
In September 2023, the National Comprehensive Cancer Network (NCCN) convened a working group cochaired by Mr. Biru that developed recommendations for how oncology practices should routinely measure HRSNs (NCCN.org/social-needs).
“The working group proposed that every cancer patient be assessed for food, transportation access, and financial and housing security at least once a year, and be reassessed at every care transition point as well,” Mr. Biru said. Such screenings should include follow-up to connect patients with services to address any HRSNs they are experiencing, he added.
Lead author Dr. Zheng is employed by the American Cancer Society, which as a nonprofit receives funds from the public through fundraising and contributions, as well as some support from corporations and industry to support its mission programs and services. Mr. Biru had no financial conflicts to disclose.
Little is known about the specific association between health-related social needs (HRSNs) and mortality risk even though HRSNs, defined as challenges in affording food, housing, and other necessities of daily living, are potential challenges for cancer survivors, wrote Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and colleagues.
A 2020 study by Dr. Zheng and colleagues published in the Journal of the National Comprehensive Cancer Network (NCCN) showed that food insecurity and financial worries had a negative impact on cancer survivorship. In the new study, published in Cancer, the researchers identified cancer survivors using the 2013-2018 National Health Interview Survey (NHIS) and the NHIS Mortality File through December 31, 2019. The researchers examined mortality using the data from the Centers for Disease Control and Prevention’s National Death Index (NDI) through December 31, 2019, which links to the National Health Interview Survey Data used in the study.
Individuals’ HRSNs were categorized into three groups: severe, moderate, and minor/none. HRSNs included food insecurity and nonmedical financial concerns, such as housing costs (rent, mortgage). Medical financial hardship included material, psychological, and behavioral domains and was divided into three groups: 2-3 domains, 1 domain, or 0 domains.
What Are the Potential Financial Implications of this Research?
The high costs of cancer care often cause medical financial hardships for cancer survivors, and expenses also may cause psychological distress and nonmedical financial hardship as survivors try to make ends meet while facing medical bills, wrote Dr. Zheng and colleagues.
Policy makers are increasingly interested in adding HRSNs to insurance coverage; recent guidance from the Centers for Medicare & Medicaid Services (CMS) allows individual states to apply to provide nutrition and housing supports through state Medicaid programs, according to authors of a 2023 article published in JAMA Health Forum.
The new study adds to the understanding of how HRSNs impact people with cancer by examining the association with mortality risk, Yelak Biru, MSc, president and chief executive officer of the International Myeloma Foundation, said in an interview.
“This is a key area of study for addressing the disparities in treatments and outcomes that result in inequities,” said Mr. Biru, a patient advocate and multiple myeloma survivor who was not involved in the study.
What Does the New Study Show?
The new study characterized HRSNs in 5,855 adult cancer survivors aged 18-64 years and 5,918 aged 65-79 years. In the 18- to 64-year-old group, 25.5% reported moderate levels of HRSNs, and 18.3% reported severe HRSNs. In patients aged 65-79 years, 15.6% and 6.6% reported moderate HRSNs and severe HRSNs, respectively.
Severe HRSN was significantly associated with higher mortality risk in an adjusted analysis in patients aged 18-64 years (hazard ratio 2.00, P < .001).
Among adults aged 65-79 years, severe HRSN was not associated with higher mortality risk; however, in this older age group, those with 2-3 domains of medical financial hardship had significantly increased mortality risk compared with adults aged 65-79 years with zero domains of medical financial hardship (HR 1.58, P = .007).
Although the findings that HRSNs were associated with increased mortality risk, especially in the younger group, were not surprising, they serve as a call to action to address how HRSNs are contributing to cancer mortality, Mr. Biru said in an interview. “HRSNs, like food or housing insecurity, can lead to patients being unable to undergo the best treatment approach for their cancer,” he said.
What Are the Limitations and Research Gaps?
The study findings were limited by several factors including the use of self-reports to measure medical financial hardship, food insecurity, and nonmedical financial concerns in the NHIS, the researchers wrote in their discussion. More research with longer follow-up time beyond 1-5 years is needed, wrote Dr. Zheng and colleagues.
Studies also are needed to illustrate how patient navigation can help prevent patients from falling through the cracks with regard to social needs and financial hardships, Mr. Biru told this news organization.
Other areas for research include how addressing social needs affects health outcomes and whether programs designed to address social needs are effective, he said.
“Finally, qualitative research is needed to capture the lived experiences of cancer survivors facing these challenges. This knowledge can inform the development of more patient-centered interventions and policies that effectively address the social determinants of health and improve overall outcomes for all cancer survivors,” Mr. Biru said.
What Is the Takeaway Message for Clinicians?
HRSNs and financial hardship are significantly associated with increased risk of mortality in adult cancer survivors, Dr. Zheng and colleagues concluded. Looking ahead, comprehensive assessment of HRSNs and financial hardship may help clinicians connect patients with relevant services to mitigate the social and financial impacts of cancer, they wrote.
“The takeaway message for oncologists in practice is that addressing [HRSNs] and financial hardship is crucial for providing comprehensive and equitable cancer care,” Mr. Biru said during his interview.
“The impact of social determinants of health on cancer outcomes cannot be ignored, and oncologists play a vital role in identifying and addressing these needs,” he said. Sensitive, discussion-based screenings are needed to identify core needs such as food and transportation, but clinicians also can consider broader social factors and work with a team to connect patients to appropriate resources, he added.
“By recognizing the importance of HRSN screening and taking proactive steps to address these needs, oncologists can contribute to improving health outcomes, reducing healthcare disparities, and providing more equitable cancer care for their patients,” he said.
What Other Guidance Is Available?
“High-quality cancer care requires treating the whole person; measuring and addressing anything in their life that could result in poorer health outcomes is a key component of comprehensive care,” Mr. Biru emphasized.
In September 2023, the National Comprehensive Cancer Network (NCCN) convened a working group cochaired by Mr. Biru that developed recommendations for how oncology practices should routinely measure HRSNs (NCCN.org/social-needs).
“The working group proposed that every cancer patient be assessed for food, transportation access, and financial and housing security at least once a year, and be reassessed at every care transition point as well,” Mr. Biru said. Such screenings should include follow-up to connect patients with services to address any HRSNs they are experiencing, he added.
Lead author Dr. Zheng is employed by the American Cancer Society, which as a nonprofit receives funds from the public through fundraising and contributions, as well as some support from corporations and industry to support its mission programs and services. Mr. Biru had no financial conflicts to disclose.
Little is known about the specific association between health-related social needs (HRSNs) and mortality risk even though HRSNs, defined as challenges in affording food, housing, and other necessities of daily living, are potential challenges for cancer survivors, wrote Zhiyuan Zheng, PhD, of the American Cancer Society, Atlanta, and colleagues.
A 2020 study by Dr. Zheng and colleagues published in the Journal of the National Comprehensive Cancer Network (NCCN) showed that food insecurity and financial worries had a negative impact on cancer survivorship. In the new study, published in Cancer, the researchers identified cancer survivors using the 2013-2018 National Health Interview Survey (NHIS) and the NHIS Mortality File through December 31, 2019. The researchers examined mortality using the data from the Centers for Disease Control and Prevention’s National Death Index (NDI) through December 31, 2019, which links to the National Health Interview Survey Data used in the study.
Individuals’ HRSNs were categorized into three groups: severe, moderate, and minor/none. HRSNs included food insecurity and nonmedical financial concerns, such as housing costs (rent, mortgage). Medical financial hardship included material, psychological, and behavioral domains and was divided into three groups: 2-3 domains, 1 domain, or 0 domains.
What Are the Potential Financial Implications of this Research?
The high costs of cancer care often cause medical financial hardships for cancer survivors, and expenses also may cause psychological distress and nonmedical financial hardship as survivors try to make ends meet while facing medical bills, wrote Dr. Zheng and colleagues.
Policy makers are increasingly interested in adding HRSNs to insurance coverage; recent guidance from the Centers for Medicare & Medicaid Services (CMS) allows individual states to apply to provide nutrition and housing supports through state Medicaid programs, according to authors of a 2023 article published in JAMA Health Forum.
The new study adds to the understanding of how HRSNs impact people with cancer by examining the association with mortality risk, Yelak Biru, MSc, president and chief executive officer of the International Myeloma Foundation, said in an interview.
“This is a key area of study for addressing the disparities in treatments and outcomes that result in inequities,” said Mr. Biru, a patient advocate and multiple myeloma survivor who was not involved in the study.
What Does the New Study Show?
The new study characterized HRSNs in 5,855 adult cancer survivors aged 18-64 years and 5,918 aged 65-79 years. In the 18- to 64-year-old group, 25.5% reported moderate levels of HRSNs, and 18.3% reported severe HRSNs. In patients aged 65-79 years, 15.6% and 6.6% reported moderate HRSNs and severe HRSNs, respectively.
Severe HRSN was significantly associated with higher mortality risk in an adjusted analysis in patients aged 18-64 years (hazard ratio 2.00, P < .001).
Among adults aged 65-79 years, severe HRSN was not associated with higher mortality risk; however, in this older age group, those with 2-3 domains of medical financial hardship had significantly increased mortality risk compared with adults aged 65-79 years with zero domains of medical financial hardship (HR 1.58, P = .007).
Although the findings that HRSNs were associated with increased mortality risk, especially in the younger group, were not surprising, they serve as a call to action to address how HRSNs are contributing to cancer mortality, Mr. Biru said in an interview. “HRSNs, like food or housing insecurity, can lead to patients being unable to undergo the best treatment approach for their cancer,” he said.
What Are the Limitations and Research Gaps?
The study findings were limited by several factors including the use of self-reports to measure medical financial hardship, food insecurity, and nonmedical financial concerns in the NHIS, the researchers wrote in their discussion. More research with longer follow-up time beyond 1-5 years is needed, wrote Dr. Zheng and colleagues.
Studies also are needed to illustrate how patient navigation can help prevent patients from falling through the cracks with regard to social needs and financial hardships, Mr. Biru told this news organization.
Other areas for research include how addressing social needs affects health outcomes and whether programs designed to address social needs are effective, he said.
“Finally, qualitative research is needed to capture the lived experiences of cancer survivors facing these challenges. This knowledge can inform the development of more patient-centered interventions and policies that effectively address the social determinants of health and improve overall outcomes for all cancer survivors,” Mr. Biru said.
What Is the Takeaway Message for Clinicians?
HRSNs and financial hardship are significantly associated with increased risk of mortality in adult cancer survivors, Dr. Zheng and colleagues concluded. Looking ahead, comprehensive assessment of HRSNs and financial hardship may help clinicians connect patients with relevant services to mitigate the social and financial impacts of cancer, they wrote.
“The takeaway message for oncologists in practice is that addressing [HRSNs] and financial hardship is crucial for providing comprehensive and equitable cancer care,” Mr. Biru said during his interview.
“The impact of social determinants of health on cancer outcomes cannot be ignored, and oncologists play a vital role in identifying and addressing these needs,” he said. Sensitive, discussion-based screenings are needed to identify core needs such as food and transportation, but clinicians also can consider broader social factors and work with a team to connect patients to appropriate resources, he added.
“By recognizing the importance of HRSN screening and taking proactive steps to address these needs, oncologists can contribute to improving health outcomes, reducing healthcare disparities, and providing more equitable cancer care for their patients,” he said.
What Other Guidance Is Available?
“High-quality cancer care requires treating the whole person; measuring and addressing anything in their life that could result in poorer health outcomes is a key component of comprehensive care,” Mr. Biru emphasized.
In September 2023, the National Comprehensive Cancer Network (NCCN) convened a working group cochaired by Mr. Biru that developed recommendations for how oncology practices should routinely measure HRSNs (NCCN.org/social-needs).
“The working group proposed that every cancer patient be assessed for food, transportation access, and financial and housing security at least once a year, and be reassessed at every care transition point as well,” Mr. Biru said. Such screenings should include follow-up to connect patients with services to address any HRSNs they are experiencing, he added.
Lead author Dr. Zheng is employed by the American Cancer Society, which as a nonprofit receives funds from the public through fundraising and contributions, as well as some support from corporations and industry to support its mission programs and services. Mr. Biru had no financial conflicts to disclose.
FROM CANCER
Terminal Cancer: What Matters to Patients and Caregivers
New research found that patients and caregivers both tend to prioritize symptom control over life extension but often preferring a balance. Patients and caregivers, however, are less aligned on decisions about cost containment, with patients more likely to prioritize cost containment.
“Our research has revealed that patients and caregivers generally share similar end-of-life goals,” with a “notable exception” when it comes to costs, first author Semra Ozdemir, PhD, with the Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore, told this news organization.
However, when patients and caregivers have a better understanding of the patient’s prognosis, both may be more inclined to avoid costly life-extending treatments and prioritize symptom management.
In other words, the survey suggests that “knowing the prognosis helps patients and their families set realistic expectations for care and adequately prepare for end-of-life decisions,” said Dr. Ozdemir.
This study was published online in JAMA Network Open.
Patients with advanced cancer often face difficult decisions: Do they opt for treatments that may — or may not — extend life or do they focus more on symptom control?
Family caregivers, who also play an important role in this decision-making process, may have different care goals. Some research suggests that caregivers tend to prioritize treatments that could extend life, whereas patients prioritize symptom management, but it’s less clear how these priorities may change over time and how patients and caregivers may influence each other.
In the current study, the researchers examined goals of care among patients with stage IV solid tumors and caregivers during the last 2 years of life, focusing on life extension vs symptom management and cost containment, as well as how these goals changed over time.
The survey included 210 patient-caregiver pairs, recruited from outpatient clinics at two major cancer centers in Singapore. Patients had a mean age of 63 years, and about half were men. The caregivers had a mean age of 49 years, and almost two third (63%) were women.
Overall, 34% patients and 29% caregivers prioritized symptom management over life extension, whereas 24% patients and 19% caregivers prioritized life extension. Most patients and caregivers preferred balancing the two, with 34%-47% patients and 37%-69% caregivers supporting this approach.
When balancing cost and treatment decisions, however, patients were more likely to prioritize containing costs — 28% vs 17% for caregivers — over extending life — 26% of patients vs 35% of caregivers.
Cost containment tended to be more of a priority for older patients, those with a higher symptom burden, and those with less family caregiver support. For caregivers, cost containment was more of a priority for those who reported that caregiving had a big impact on their finances, those with worse self-esteem related to their caregiving abilities, as well as those caring for older patients.
To better align cost containment priorities between patients and caregivers, it’s essential for families to engage in open and thorough discussions about the allocation of resources, Dr. Ozdemir said.
Although “patients, families, and physicians often avoid discussions about prognosis,” such conversations are essential for setting realistic expectations for care and adequately preparing for end-of-life decisions, Dr. Ozdemir told this news organization.
“These conversations should aim to balance competing interests and create care plans that are mutually acceptable to both patients and caregivers,” she said, adding that “this approach will help in minimizing any potential conflicts and ensure that both parties feel respected and understood in their decision-making process.”
Managing Unrealistic Expectations
As patients approached the end of life, neither patients nor caregivers shifted their priorities from life extension to symptom management.
This finding raises concerns because it suggests that many patients hold unrealistic expectations regarding their care and “underscores the need for continuous dialogue and reassessment of care goals throughout the progression of illness,” Dr. Ozdemir said.
“This stability in preferences over time suggests that initial care decisions are deeply ingrained or that there may be a lack of ongoing communication about evolving care needs and possibilities as conditions change,” Ozdemir said.
Yet, it can be hard to define what unrealistic expectations mean, said Olivia Seecof, MD, who wasn’t involved in the study.
“I think people are hopeful that a devastating diagnosis won’t lead to the end of their life and that there will be a treatment or something that will change [their prognosis], and they’ll get better,” said Dr. Seecof, palliative care expert with the Supportive Oncology Program at NYU Langone Health’s Perlmutter Cancer Center in New York City.
Giving patients and caregivers a realistic understanding of the prognosis is important, but “there’s more to it than just telling the patient their diagnosis,” she said.
“We have to plan for end of life, what it can look like,” said Dr. Seecof, adding that “often we don’t do a very good job of talking about that early on in an illness course.”
Overall, though, Dr. Seecof stressed that no two patients or situations are the same, and it’s important to understand what’s important in each scenario. End-of-life care requires “an individual approach because every patient is different, even if they have the same diagnosis as someone else,” she said.
This work was supported by funding from the Singapore Millennium Foundation and the Lien Centre for Palliative Care. Dr. Ozdemir and Dr. Seecof had no relevant disclosures.
A version of this article appeared on Medscape.com.
New research found that patients and caregivers both tend to prioritize symptom control over life extension but often preferring a balance. Patients and caregivers, however, are less aligned on decisions about cost containment, with patients more likely to prioritize cost containment.
“Our research has revealed that patients and caregivers generally share similar end-of-life goals,” with a “notable exception” when it comes to costs, first author Semra Ozdemir, PhD, with the Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore, told this news organization.
However, when patients and caregivers have a better understanding of the patient’s prognosis, both may be more inclined to avoid costly life-extending treatments and prioritize symptom management.
In other words, the survey suggests that “knowing the prognosis helps patients and their families set realistic expectations for care and adequately prepare for end-of-life decisions,” said Dr. Ozdemir.
This study was published online in JAMA Network Open.
Patients with advanced cancer often face difficult decisions: Do they opt for treatments that may — or may not — extend life or do they focus more on symptom control?
Family caregivers, who also play an important role in this decision-making process, may have different care goals. Some research suggests that caregivers tend to prioritize treatments that could extend life, whereas patients prioritize symptom management, but it’s less clear how these priorities may change over time and how patients and caregivers may influence each other.
In the current study, the researchers examined goals of care among patients with stage IV solid tumors and caregivers during the last 2 years of life, focusing on life extension vs symptom management and cost containment, as well as how these goals changed over time.
The survey included 210 patient-caregiver pairs, recruited from outpatient clinics at two major cancer centers in Singapore. Patients had a mean age of 63 years, and about half were men. The caregivers had a mean age of 49 years, and almost two third (63%) were women.
Overall, 34% patients and 29% caregivers prioritized symptom management over life extension, whereas 24% patients and 19% caregivers prioritized life extension. Most patients and caregivers preferred balancing the two, with 34%-47% patients and 37%-69% caregivers supporting this approach.
When balancing cost and treatment decisions, however, patients were more likely to prioritize containing costs — 28% vs 17% for caregivers — over extending life — 26% of patients vs 35% of caregivers.
Cost containment tended to be more of a priority for older patients, those with a higher symptom burden, and those with less family caregiver support. For caregivers, cost containment was more of a priority for those who reported that caregiving had a big impact on their finances, those with worse self-esteem related to their caregiving abilities, as well as those caring for older patients.
To better align cost containment priorities between patients and caregivers, it’s essential for families to engage in open and thorough discussions about the allocation of resources, Dr. Ozdemir said.
Although “patients, families, and physicians often avoid discussions about prognosis,” such conversations are essential for setting realistic expectations for care and adequately preparing for end-of-life decisions, Dr. Ozdemir told this news organization.
“These conversations should aim to balance competing interests and create care plans that are mutually acceptable to both patients and caregivers,” she said, adding that “this approach will help in minimizing any potential conflicts and ensure that both parties feel respected and understood in their decision-making process.”
Managing Unrealistic Expectations
As patients approached the end of life, neither patients nor caregivers shifted their priorities from life extension to symptom management.
This finding raises concerns because it suggests that many patients hold unrealistic expectations regarding their care and “underscores the need for continuous dialogue and reassessment of care goals throughout the progression of illness,” Dr. Ozdemir said.
“This stability in preferences over time suggests that initial care decisions are deeply ingrained or that there may be a lack of ongoing communication about evolving care needs and possibilities as conditions change,” Ozdemir said.
Yet, it can be hard to define what unrealistic expectations mean, said Olivia Seecof, MD, who wasn’t involved in the study.
“I think people are hopeful that a devastating diagnosis won’t lead to the end of their life and that there will be a treatment or something that will change [their prognosis], and they’ll get better,” said Dr. Seecof, palliative care expert with the Supportive Oncology Program at NYU Langone Health’s Perlmutter Cancer Center in New York City.
Giving patients and caregivers a realistic understanding of the prognosis is important, but “there’s more to it than just telling the patient their diagnosis,” she said.
“We have to plan for end of life, what it can look like,” said Dr. Seecof, adding that “often we don’t do a very good job of talking about that early on in an illness course.”
Overall, though, Dr. Seecof stressed that no two patients or situations are the same, and it’s important to understand what’s important in each scenario. End-of-life care requires “an individual approach because every patient is different, even if they have the same diagnosis as someone else,” she said.
This work was supported by funding from the Singapore Millennium Foundation and the Lien Centre for Palliative Care. Dr. Ozdemir and Dr. Seecof had no relevant disclosures.
A version of this article appeared on Medscape.com.
New research found that patients and caregivers both tend to prioritize symptom control over life extension but often preferring a balance. Patients and caregivers, however, are less aligned on decisions about cost containment, with patients more likely to prioritize cost containment.
“Our research has revealed that patients and caregivers generally share similar end-of-life goals,” with a “notable exception” when it comes to costs, first author Semra Ozdemir, PhD, with the Lien Centre for Palliative Care, Duke-NUS Medical School, Singapore, told this news organization.
However, when patients and caregivers have a better understanding of the patient’s prognosis, both may be more inclined to avoid costly life-extending treatments and prioritize symptom management.
In other words, the survey suggests that “knowing the prognosis helps patients and their families set realistic expectations for care and adequately prepare for end-of-life decisions,” said Dr. Ozdemir.
This study was published online in JAMA Network Open.
Patients with advanced cancer often face difficult decisions: Do they opt for treatments that may — or may not — extend life or do they focus more on symptom control?
Family caregivers, who also play an important role in this decision-making process, may have different care goals. Some research suggests that caregivers tend to prioritize treatments that could extend life, whereas patients prioritize symptom management, but it’s less clear how these priorities may change over time and how patients and caregivers may influence each other.
In the current study, the researchers examined goals of care among patients with stage IV solid tumors and caregivers during the last 2 years of life, focusing on life extension vs symptom management and cost containment, as well as how these goals changed over time.
The survey included 210 patient-caregiver pairs, recruited from outpatient clinics at two major cancer centers in Singapore. Patients had a mean age of 63 years, and about half were men. The caregivers had a mean age of 49 years, and almost two third (63%) were women.
Overall, 34% patients and 29% caregivers prioritized symptom management over life extension, whereas 24% patients and 19% caregivers prioritized life extension. Most patients and caregivers preferred balancing the two, with 34%-47% patients and 37%-69% caregivers supporting this approach.
When balancing cost and treatment decisions, however, patients were more likely to prioritize containing costs — 28% vs 17% for caregivers — over extending life — 26% of patients vs 35% of caregivers.
Cost containment tended to be more of a priority for older patients, those with a higher symptom burden, and those with less family caregiver support. For caregivers, cost containment was more of a priority for those who reported that caregiving had a big impact on their finances, those with worse self-esteem related to their caregiving abilities, as well as those caring for older patients.
To better align cost containment priorities between patients and caregivers, it’s essential for families to engage in open and thorough discussions about the allocation of resources, Dr. Ozdemir said.
Although “patients, families, and physicians often avoid discussions about prognosis,” such conversations are essential for setting realistic expectations for care and adequately preparing for end-of-life decisions, Dr. Ozdemir told this news organization.
“These conversations should aim to balance competing interests and create care plans that are mutually acceptable to both patients and caregivers,” she said, adding that “this approach will help in minimizing any potential conflicts and ensure that both parties feel respected and understood in their decision-making process.”
Managing Unrealistic Expectations
As patients approached the end of life, neither patients nor caregivers shifted their priorities from life extension to symptom management.
This finding raises concerns because it suggests that many patients hold unrealistic expectations regarding their care and “underscores the need for continuous dialogue and reassessment of care goals throughout the progression of illness,” Dr. Ozdemir said.
“This stability in preferences over time suggests that initial care decisions are deeply ingrained or that there may be a lack of ongoing communication about evolving care needs and possibilities as conditions change,” Ozdemir said.
Yet, it can be hard to define what unrealistic expectations mean, said Olivia Seecof, MD, who wasn’t involved in the study.
“I think people are hopeful that a devastating diagnosis won’t lead to the end of their life and that there will be a treatment or something that will change [their prognosis], and they’ll get better,” said Dr. Seecof, palliative care expert with the Supportive Oncology Program at NYU Langone Health’s Perlmutter Cancer Center in New York City.
Giving patients and caregivers a realistic understanding of the prognosis is important, but “there’s more to it than just telling the patient their diagnosis,” she said.
“We have to plan for end of life, what it can look like,” said Dr. Seecof, adding that “often we don’t do a very good job of talking about that early on in an illness course.”
Overall, though, Dr. Seecof stressed that no two patients or situations are the same, and it’s important to understand what’s important in each scenario. End-of-life care requires “an individual approach because every patient is different, even if they have the same diagnosis as someone else,” she said.
This work was supported by funding from the Singapore Millennium Foundation and the Lien Centre for Palliative Care. Dr. Ozdemir and Dr. Seecof had no relevant disclosures.
A version of this article appeared on Medscape.com.
Persistent Flu-Like Symptoms in a Patient With Glaucoma and Osteoporosis
A 62-year-old man presented to the emergency department (ED) with 3 days of chills, myalgias, and nausea. The patient’s oral temperature at home ranged from 99.9 to 100.1 °F. He came to the ED after multiple phone discussions with primary care nursing over 3 days. His medical history included posttraumatic stress disorder, enlarged prostate, osteoporosis, gastroesophageal reflux, glaucoma, and left eye central retinal vein occlusion. Medications included fluoxetine 20 mg twice daily, omeprazole 20 mg twice daily, rosuvastatin 10 mg once daily, tamsulosin 0.4 mg nightly, and zolpidem 10 mg nightly. The patient’s glaucoma had been treated with a dexamethasone intraocular implant about 90 days earlier. The patient started on intravenous (IV) zoledronic acid for osteoporosis, with the first infusion 5 days prior to presentation.
In the ED, the patient’s temperature was 98.2 °F, blood pressure was 156/76 mm Hg, pulse was 94 bpm, respiratory rate was 16 breaths per minute, and 98% oxygen saturation on room air. He was in no acute distress, with an unremarkable physical examination reporting no abnormal respiratory sounds, no arrhythmia, normal gait, and no focal neurologic deficits. A comprehensive metabolic panel was unremarkable, creatine phosphokinase was 155 U/L (reference range, 30-240 U/L), and the complete blood count was notable only for an elevated white blood count of 15.3 × 109/L (reference range, 4.0-11.0 × 109/L), with 73.4% neutrophils, 16.2% lymphocytes, 9.1% monocytes, 0.5% eosinophils, and 0.4% basophils. The patient’s urinalysis was unremarkable.
What is your diagnosis?
How would you treat this patient?
Discussion
The ED physician considered viral infection and tested for both influenza and COVID-19. Laboratory results eliminated urinary tract infection and rhabdomyolysis as possible diagnoses. An acute phase reaction to zoledronic acid was determined to be the most likely cause. The patient was treated with IV saline in the ED, and acetaminophen both in the ED and at home.
Although initial nursing triage notes document consideration of acute phase reaction to zoledronic acid, the endocrinology service, which had recommended and arranged the zoledronic acid infusion, was not immediately notified of the reaction. It does not appear any treatment (eg, acetaminophen) was suggested, only that the patient was given advice this may resolve over 3 to 4 days. When he was seen 2 months later for an endocrinology follow-up appointment, he reported that all symptoms (chills, myalgias, and nausea) resolved gradually over 1 week. Since then, he has felt as well as he did before taking zoledronic acid. However, the patient was wary of further zoledronic acid, opting to defer deciding on a second dose until a future appointment.
Prior to starting zoledronic acid therapy, the patient was being treated for vitamin D deficiency. Four months prior to infusion, his 25-hydroxyvitamin D level was 12.0 ng/mL (reference range, 30 to 80 ng/mL). He then started taking cholecalciferol 100 mcg (4000 IU) daily. Eight days prior to infusion his 25-hydroxyvitamin D level was 29.5 ng/mL.
Federal health care practitioners, especially those working in the Veterans Health Administration (VHA), will commonly encounter patients similar to this case. Osteoporosisis is common in the United States with > 10 million diagnoses (including > 2 million men) and in VHA primary care populations.1,2 Zoledronic acid is a frequently prescribed treatment, appearing in guidelines for osteoporosis management.3-5
The acute phase reaction is a common adverse effect of both oral and IV bisphosphonates, although it’s substantially more common with IV bisphosphonates such as zoledronic acid. This reaction is characterized by flu-like symptoms of fever, myalgia, and arthralgia that occur within the first few days following bisphosphonate administration, and tends to be rated mild to moderate by patients.6 Clinical trial data from > 7000 women with postmenopausal osteoporosis found that 42% experienced ≥ 1 acute phase symptom following the first infusion (fever was most common, followed by musculoskeletal symptoms and gastrointestinal symptoms), compared with 12% for placebo. Incidence decreases with each subsequent infusion.7 Risk factors for reactions include low 25-hydroxyvitamin D levels,8,9 no prior bisphosphonate exposure,9 younger age (aged 64-67 years vs 78-89 years),7 lower body mass index,10 and higher lymphocyte levels at baseline.11 While most cases are mild and self-limited, severe consequences have been noted, such as precipitation of adrenal crisis.12,13 Additionally, more prolonged bone pain, sometimes quite severe, has been rarely reported with bisphosphonate use. However, it’s unclear whether this represents a separate adverse effect or a more severe acute phase reaction.6
The acute phase reaction is a transient inflammatory state marked by increases in proinflammatory cytokines such as C-reactive protein, interleukin-6, and tumor necrosis factor-α. Proposed mechanisms include: (1) inhibition of farnesyl pyrophosphate synthase, an enzyme of the mevalonate pathway, resulting inactivation of γϐ T cells and increased production of proinflammatory cytokines; (2) inhibition of the suppressor of cytokine signalling-3 in the macrophages, resulting in cessation of the suppression in cytokine signaling; or (3) negative regulation of γϐ T-cell expansion and interferon-c production by low serum 25-hydroxyvitamin D concentrations.11
Prevention
Can an acute phase reaction to zoledronic acid be prevented? Bourke and colleagues reported that baseline calcium and/or vitamin D intake do not appear to affect rates of acute phase reaction in data pooled from 2 trials of zoledronic acid in postmenopausal women.14 However, patients receiving zoledronic acid had 25-hydroxyvitamin D values > 20 ng/mL 86% of the time, and values > 30 ng/mL 36% of the time. Bourke and colleagues suggest that “coadministration of calcium and vitamin D with zoledronate may not be necessary for individuals not at risk of marked vitamin D deficiency.”14 However, they did not prospectively test this hypothesis.
In our patient, vitamin D deficiency had been identified and treated, nearly achieving 30 ng/mL. The 2020 guidelines for postmenopausal osteoporosis recommend maintaining serum 25-hydroxyvitamin D levels 30 to 50 ng/mL, advising to supplement with vitamin D3 as needed.5 The 2012 guidelines for osteoporosis in men from the Endocrine Society suggest that men with low vitamin D levels receive vitamin D supplements to raise the level > 30 ng/ml.4
Oral analgesics have been studied for the prevention of adverse effects related to zoledronic acid. Initiating 650 mg acetaminophen 45 minutes before zoledronic acid infusion and then every 6 hours over the next 3 days has been shown to significantly reduce symptoms.15 Acetaminophen or ibuprofen given every 6 hours for 3 days (starting 4 hours after zoledronic acid infusion) has been shown to reduce fever and other symptoms.16
Statins have been shown in vitro to prevent bisphosphonate-induced γϐ T cell activation.17 This has led to studies with various statins, although none have yet shown benefit in vivo. A double-blind, randomized, placebo-controlled trial of postmenopausal women for fluvastatin (single dose of 40 mg or 3 doses of 40 mg, each 24 hours apart) did not prevent acute phase reaction symptoms, nor did it prevent zoledronic acid-induced cytokine release.17 Rosuvastatin 10 mg daily starting 5 days before zoledronic acid treatment and taken for a total of 11 days did not show any difference in fever or pain.18 A protocol for pravastatin has been disseminated, but no study results have been published yet.19
Prophylactic dexamethasone has also been studied. A randomized double-blind, placebo-controlled trial of oral dexamethasone 4 mg at the time of first infusion of zoledronic acid found no significant difference in temperature change or symptom score over the following 3 days.20 Chen and colleagues compared the efficacy of acetaminophen alone vs acetaminophen plus dexamethasone over several days.21 Acetaminophen 500 mg was given on the day of infusion and 4 times daily for 3 to 7 days for both groups, while dexamethasone 4 mg was given for 3 to 7 days. The dexamethasone group reported substantially lower incidence of any acute phase reaction symptoms (34% vs 67%, P = .003). A more recent study by Murdoch and colleagues comparing dexamethasone (4 mg daily for 3 days with the first dose 90 minutes before zoledronic acid infusion) with placebo found that the dexamethasone group had a statistically significant lower mean temperature change and acute phase reaction symptom score.22
Adverse Effect Treatment
Treatment after development of acute phase reaction due to zoledronic acid infusion is generally limited to supportive care and/or nonsteroidal anti-inflammatory drugs (NSAIDs) acetaminophen or dexamethasone, largely based on extrapolation of the noted preventive trials and expert opinion.3,6 Experiencing an acute phase reaction may portend better fracture risk reduction from zoledronic acid, although there is a potential association between acute phase reaction and mortality risk.23,24
Our case was typical for acute phase reaction to zoledronic acid. The patient was already taking rosuvastatin 10 mg daily for hypercholesterolemia as prescribed by his primary care physician. Rosuvastatin was not shown to prevent symptoms, although it was not studied in patients on long-term statin therapy at the time of zoledronic acid infusion.18 The patient was also taking vitamin D3 supplementation and was nearly in the reference range.5 His ED treatment included IV fluids and acetaminophen. Pretreatment (prior to or at the time of zoledronic acid infusion) with acetaminophen or ibuprofen may have prevented his symptoms, or at least lessened them to the point that an ED visit would not have resulted. The endocrinologist who prescribed the zoledronic acid documented a detailed discussion of the adverse effects of zoledronic acid with the patient, and the initial nursing call documents consideration of acute phase reaction. It is unclear whether the persistence of symptoms or worsening of symptoms ultimately led to the ED visit. Because no treatment was offered, it is unknown whether earlier posttreatment with acetaminophen, ibuprofen, or dexamethasone might have prevented his ED visit.
Conclusions
Clinicians who treat patients with osteoporosis should be aware of several key points. First, acute phase reaction symptoms are common with bisphosphonates, especially zoledronic acid infusions. Second, the symptoms are nonspecific but should have a suggestive time course. Third, dexamethasone may be partially protective, but based on the various trials discussed, it likely needs to be given for multiple days (instead of a single dose on the day of infusion). Given that acetaminophen and NSAIDs also seem to be protective (when given for multiple days starting on the day of infusion), both have lower overall adverse effect profiles than dexamethasone, consideration may be given to using either of these prophylactically.6 Dexamethasone could then be prescribed if symptoms are severe or persistent despite the use of acetaminophen or NSAIDs.
1. Choksi P, Gay BL, Reyes-Gastelum D, Haymart MR, Papaleontiou M. Understanding osteoporosis screening practices in men: a nationwide physician survey. Endocr Pract. 2020;26(11):1237-1243. doi:10.4158/EP-2020-0123
2. Yu ZL, Fisher L, Hand J. Osteoporosis screening for male veterans in a resident based primary care clinic at Northport Veterans Affairs Medical Center. Am J Med Qual. 2023;38(5):272.doi:10.1097/JMQ.0000000000000134
3. Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. doi:10.1210/jc.2019-00221
4. Watts NB, Adler RA, Bilezikian JP, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802-1822. doi:10.1210/jc.2011-3045
5. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2020 update. Endocr Pract. 2020;26(suppl 1):1-46. doi:10.4158/GL-2020-0524SUPPL
6. Lim SY, Bolster MB. What can we do about musculoskeletal pain from bisphosphonates?. Cleve Clin J Med. 2018;85(9):675-678. doi:10.3949/ccjm.85a.18005
7. Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab. 2010;95(9):4380-4387. doi:10.1210/jc.2010-0597
8. Lu K, Shi Q, Gong YQ, Li C. Association between vitamin D and zoledronate-induced acute-phase response fever risk in osteoporotic patients. Front Endocrinol (Lausanne). 2022;13:991913. Published 2022 Oct 10. doi:10.3389/fendo.2022.991913
9. Popp AW, Senn R, Curkovic I, et al. Factors associated with acute-phase response of bisphosphonate-naïve or pretreated women with osteoporosis receiving an intravenous first dose of zoledronate or ibandronate. Osteoporos Int. 2017;28(6):1995-2002. doi:10.1007/s00198-017-3992-5
10. Zheng X, Ye J, Zhan Q, et al. Prediction of musculoskeletal pain after the first intravenous zoledronic acid injection in patients with primary osteoporosis: development and evaluation of a new nomogram. BMC Musculoskelet Disord. 2023;24(1):841. Published 2023 Oct 25. doi:10.1186/s12891-023-06965-y
11. Anastasilakis AD, Polyzos SA, Delaroudis S, et al. The role of cytokines and adipocytokines in zoledronate-induced acute phase reaction in postmenopausal women with low bone mass. Clin Endocrinol (Oxf). 2012;77(6):816-822. doi:10.1111/j.1365-2265.2012.04459.x
12. Smrecnik M, Kavcic Trsinar Z, Kocjan T. Adrenal crisis after first infusion of zoledronic acid: a case report. Osteoporos Int. 2018;29(7):1675-1678. doi:10.1007/s00198-018-4508-7
13. Kuo B, Koransky A, Vaz Wicks CL. Adrenal crisis as an adverse reaction to zoledronic acid in a patient with primary adrenal insufficiency: a case report and literature review. AACE Clin Case Rep. 2022;9(2):32-34. Published 2022 Dec 17. doi:10.1016/j.aace.2022.12.003
14. Bourke S, Bolland MJ, Grey A, et al. The impact of dietary calcium intake and vitamin D status on the effects of zoledronate. Osteoporos Int. 2013;24(1):349-354. doi:10.1007/s00198-012-2117-4
15. Silverman SL, Kriegman A, and Goncalves J, et al. Effect of acetaminophen and fluvastatin on post-dose symptoms following infusion of zoledronic acid. Osteoporos Int. 2011;22(8):2337-2345.
16. Wark JD, Bensen W, Recknor C, et al. Treatment with acetaminophen/paracetamol or ibuprofen alleviates post-dose symptoms related to intravenous infusion with zoledronic acid 5 mg. Osteoporos Int. 2012;23(2):503-512. doi:10.1007/s00198-011-1563-8
17. Thompson K, Keech F, McLernon DJ, et al. Fluvastatin does not prevent the acute-phase response to intravenous zoledronic acid in post-menopausal women. Bone. 2011;49(1):140-145. doi:10.1016/j.bone.2010.10.177
18. Makras P, Anastasilakis AD, Polyzos SA, Bisbinas I, Sakellariou GT, Papapoulos SE. No effect of rosuvastatin in the zoledronate-induced acute-phase response. Calcif Tissue Int. 2011;88(5):402-408. doi:10.1007/s00223-011-9468-2
19. Liu Q, Han G, Li R, et al. Reduction effect of oral pravastatin on the acute phase response to intravenous zoledronic acid: protocol for a real-world prospective, placebo-controlled trial. BMJ Open. 2022;12(7):e060703. Published 2022 Jul 13. doi:10.1136/bmjopen-2021-060703
20. Billington EO, Horne A, Gamble GD, Maslowski K, House M, Reid IR. Effect of single-dose dexamethasone on acute phase response following zoledronic acid: a randomized controlled trial. Osteoporos Int. 2017;28(6):1867-1874. doi:10.1007/s00198-017-3960-0
21. Chen FP, Fu TS, Lin YC, Lin YJ. Addition of dexamethasone to manage acute phase responses following initial zoledronic acid infusion. Osteoporos Int. 2021;32(4):663-670. doi:10.1007/s00198-020-05653-0
22. Murdoch R, Mellar A, Horne AM, et al. Effect of a three-day course of dexamethasone on acute phase response following treatment with zoledronate: a randomized controlled trial. J Bone Miner Res. 2023;38(5):631-638. doi:10.1002/jbmr.4802
23. Black DM, Reid IR, Napoli N, et al. The interaction of acute-phase reaction and efficacy for osteoporosis after zoledronic acid: HORIZON pivotal fracture trial. J Bone Miner Res. 2022;37(1):21-28. doi:10.1002/jbmr.4434
24. Lu K, Wu YM, Shi Q, Gong YQ, Zhang T, Li C. The impact of acute-phase reaction on mortality and re-fracture after zoledronic acid in hospitalized elderly osteoporotic fracture patients. Osteoporos Int. 2023;34(9):1613-1623. doi:10.1007/s00198-023-06803-w
A 62-year-old man presented to the emergency department (ED) with 3 days of chills, myalgias, and nausea. The patient’s oral temperature at home ranged from 99.9 to 100.1 °F. He came to the ED after multiple phone discussions with primary care nursing over 3 days. His medical history included posttraumatic stress disorder, enlarged prostate, osteoporosis, gastroesophageal reflux, glaucoma, and left eye central retinal vein occlusion. Medications included fluoxetine 20 mg twice daily, omeprazole 20 mg twice daily, rosuvastatin 10 mg once daily, tamsulosin 0.4 mg nightly, and zolpidem 10 mg nightly. The patient’s glaucoma had been treated with a dexamethasone intraocular implant about 90 days earlier. The patient started on intravenous (IV) zoledronic acid for osteoporosis, with the first infusion 5 days prior to presentation.
In the ED, the patient’s temperature was 98.2 °F, blood pressure was 156/76 mm Hg, pulse was 94 bpm, respiratory rate was 16 breaths per minute, and 98% oxygen saturation on room air. He was in no acute distress, with an unremarkable physical examination reporting no abnormal respiratory sounds, no arrhythmia, normal gait, and no focal neurologic deficits. A comprehensive metabolic panel was unremarkable, creatine phosphokinase was 155 U/L (reference range, 30-240 U/L), and the complete blood count was notable only for an elevated white blood count of 15.3 × 109/L (reference range, 4.0-11.0 × 109/L), with 73.4% neutrophils, 16.2% lymphocytes, 9.1% monocytes, 0.5% eosinophils, and 0.4% basophils. The patient’s urinalysis was unremarkable.
What is your diagnosis?
How would you treat this patient?
Discussion
The ED physician considered viral infection and tested for both influenza and COVID-19. Laboratory results eliminated urinary tract infection and rhabdomyolysis as possible diagnoses. An acute phase reaction to zoledronic acid was determined to be the most likely cause. The patient was treated with IV saline in the ED, and acetaminophen both in the ED and at home.
Although initial nursing triage notes document consideration of acute phase reaction to zoledronic acid, the endocrinology service, which had recommended and arranged the zoledronic acid infusion, was not immediately notified of the reaction. It does not appear any treatment (eg, acetaminophen) was suggested, only that the patient was given advice this may resolve over 3 to 4 days. When he was seen 2 months later for an endocrinology follow-up appointment, he reported that all symptoms (chills, myalgias, and nausea) resolved gradually over 1 week. Since then, he has felt as well as he did before taking zoledronic acid. However, the patient was wary of further zoledronic acid, opting to defer deciding on a second dose until a future appointment.
Prior to starting zoledronic acid therapy, the patient was being treated for vitamin D deficiency. Four months prior to infusion, his 25-hydroxyvitamin D level was 12.0 ng/mL (reference range, 30 to 80 ng/mL). He then started taking cholecalciferol 100 mcg (4000 IU) daily. Eight days prior to infusion his 25-hydroxyvitamin D level was 29.5 ng/mL.
Federal health care practitioners, especially those working in the Veterans Health Administration (VHA), will commonly encounter patients similar to this case. Osteoporosisis is common in the United States with > 10 million diagnoses (including > 2 million men) and in VHA primary care populations.1,2 Zoledronic acid is a frequently prescribed treatment, appearing in guidelines for osteoporosis management.3-5
The acute phase reaction is a common adverse effect of both oral and IV bisphosphonates, although it’s substantially more common with IV bisphosphonates such as zoledronic acid. This reaction is characterized by flu-like symptoms of fever, myalgia, and arthralgia that occur within the first few days following bisphosphonate administration, and tends to be rated mild to moderate by patients.6 Clinical trial data from > 7000 women with postmenopausal osteoporosis found that 42% experienced ≥ 1 acute phase symptom following the first infusion (fever was most common, followed by musculoskeletal symptoms and gastrointestinal symptoms), compared with 12% for placebo. Incidence decreases with each subsequent infusion.7 Risk factors for reactions include low 25-hydroxyvitamin D levels,8,9 no prior bisphosphonate exposure,9 younger age (aged 64-67 years vs 78-89 years),7 lower body mass index,10 and higher lymphocyte levels at baseline.11 While most cases are mild and self-limited, severe consequences have been noted, such as precipitation of adrenal crisis.12,13 Additionally, more prolonged bone pain, sometimes quite severe, has been rarely reported with bisphosphonate use. However, it’s unclear whether this represents a separate adverse effect or a more severe acute phase reaction.6
The acute phase reaction is a transient inflammatory state marked by increases in proinflammatory cytokines such as C-reactive protein, interleukin-6, and tumor necrosis factor-α. Proposed mechanisms include: (1) inhibition of farnesyl pyrophosphate synthase, an enzyme of the mevalonate pathway, resulting inactivation of γϐ T cells and increased production of proinflammatory cytokines; (2) inhibition of the suppressor of cytokine signalling-3 in the macrophages, resulting in cessation of the suppression in cytokine signaling; or (3) negative regulation of γϐ T-cell expansion and interferon-c production by low serum 25-hydroxyvitamin D concentrations.11
Prevention
Can an acute phase reaction to zoledronic acid be prevented? Bourke and colleagues reported that baseline calcium and/or vitamin D intake do not appear to affect rates of acute phase reaction in data pooled from 2 trials of zoledronic acid in postmenopausal women.14 However, patients receiving zoledronic acid had 25-hydroxyvitamin D values > 20 ng/mL 86% of the time, and values > 30 ng/mL 36% of the time. Bourke and colleagues suggest that “coadministration of calcium and vitamin D with zoledronate may not be necessary for individuals not at risk of marked vitamin D deficiency.”14 However, they did not prospectively test this hypothesis.
In our patient, vitamin D deficiency had been identified and treated, nearly achieving 30 ng/mL. The 2020 guidelines for postmenopausal osteoporosis recommend maintaining serum 25-hydroxyvitamin D levels 30 to 50 ng/mL, advising to supplement with vitamin D3 as needed.5 The 2012 guidelines for osteoporosis in men from the Endocrine Society suggest that men with low vitamin D levels receive vitamin D supplements to raise the level > 30 ng/ml.4
Oral analgesics have been studied for the prevention of adverse effects related to zoledronic acid. Initiating 650 mg acetaminophen 45 minutes before zoledronic acid infusion and then every 6 hours over the next 3 days has been shown to significantly reduce symptoms.15 Acetaminophen or ibuprofen given every 6 hours for 3 days (starting 4 hours after zoledronic acid infusion) has been shown to reduce fever and other symptoms.16
Statins have been shown in vitro to prevent bisphosphonate-induced γϐ T cell activation.17 This has led to studies with various statins, although none have yet shown benefit in vivo. A double-blind, randomized, placebo-controlled trial of postmenopausal women for fluvastatin (single dose of 40 mg or 3 doses of 40 mg, each 24 hours apart) did not prevent acute phase reaction symptoms, nor did it prevent zoledronic acid-induced cytokine release.17 Rosuvastatin 10 mg daily starting 5 days before zoledronic acid treatment and taken for a total of 11 days did not show any difference in fever or pain.18 A protocol for pravastatin has been disseminated, but no study results have been published yet.19
Prophylactic dexamethasone has also been studied. A randomized double-blind, placebo-controlled trial of oral dexamethasone 4 mg at the time of first infusion of zoledronic acid found no significant difference in temperature change or symptom score over the following 3 days.20 Chen and colleagues compared the efficacy of acetaminophen alone vs acetaminophen plus dexamethasone over several days.21 Acetaminophen 500 mg was given on the day of infusion and 4 times daily for 3 to 7 days for both groups, while dexamethasone 4 mg was given for 3 to 7 days. The dexamethasone group reported substantially lower incidence of any acute phase reaction symptoms (34% vs 67%, P = .003). A more recent study by Murdoch and colleagues comparing dexamethasone (4 mg daily for 3 days with the first dose 90 minutes before zoledronic acid infusion) with placebo found that the dexamethasone group had a statistically significant lower mean temperature change and acute phase reaction symptom score.22
Adverse Effect Treatment
Treatment after development of acute phase reaction due to zoledronic acid infusion is generally limited to supportive care and/or nonsteroidal anti-inflammatory drugs (NSAIDs) acetaminophen or dexamethasone, largely based on extrapolation of the noted preventive trials and expert opinion.3,6 Experiencing an acute phase reaction may portend better fracture risk reduction from zoledronic acid, although there is a potential association between acute phase reaction and mortality risk.23,24
Our case was typical for acute phase reaction to zoledronic acid. The patient was already taking rosuvastatin 10 mg daily for hypercholesterolemia as prescribed by his primary care physician. Rosuvastatin was not shown to prevent symptoms, although it was not studied in patients on long-term statin therapy at the time of zoledronic acid infusion.18 The patient was also taking vitamin D3 supplementation and was nearly in the reference range.5 His ED treatment included IV fluids and acetaminophen. Pretreatment (prior to or at the time of zoledronic acid infusion) with acetaminophen or ibuprofen may have prevented his symptoms, or at least lessened them to the point that an ED visit would not have resulted. The endocrinologist who prescribed the zoledronic acid documented a detailed discussion of the adverse effects of zoledronic acid with the patient, and the initial nursing call documents consideration of acute phase reaction. It is unclear whether the persistence of symptoms or worsening of symptoms ultimately led to the ED visit. Because no treatment was offered, it is unknown whether earlier posttreatment with acetaminophen, ibuprofen, or dexamethasone might have prevented his ED visit.
Conclusions
Clinicians who treat patients with osteoporosis should be aware of several key points. First, acute phase reaction symptoms are common with bisphosphonates, especially zoledronic acid infusions. Second, the symptoms are nonspecific but should have a suggestive time course. Third, dexamethasone may be partially protective, but based on the various trials discussed, it likely needs to be given for multiple days (instead of a single dose on the day of infusion). Given that acetaminophen and NSAIDs also seem to be protective (when given for multiple days starting on the day of infusion), both have lower overall adverse effect profiles than dexamethasone, consideration may be given to using either of these prophylactically.6 Dexamethasone could then be prescribed if symptoms are severe or persistent despite the use of acetaminophen or NSAIDs.
A 62-year-old man presented to the emergency department (ED) with 3 days of chills, myalgias, and nausea. The patient’s oral temperature at home ranged from 99.9 to 100.1 °F. He came to the ED after multiple phone discussions with primary care nursing over 3 days. His medical history included posttraumatic stress disorder, enlarged prostate, osteoporosis, gastroesophageal reflux, glaucoma, and left eye central retinal vein occlusion. Medications included fluoxetine 20 mg twice daily, omeprazole 20 mg twice daily, rosuvastatin 10 mg once daily, tamsulosin 0.4 mg nightly, and zolpidem 10 mg nightly. The patient’s glaucoma had been treated with a dexamethasone intraocular implant about 90 days earlier. The patient started on intravenous (IV) zoledronic acid for osteoporosis, with the first infusion 5 days prior to presentation.
In the ED, the patient’s temperature was 98.2 °F, blood pressure was 156/76 mm Hg, pulse was 94 bpm, respiratory rate was 16 breaths per minute, and 98% oxygen saturation on room air. He was in no acute distress, with an unremarkable physical examination reporting no abnormal respiratory sounds, no arrhythmia, normal gait, and no focal neurologic deficits. A comprehensive metabolic panel was unremarkable, creatine phosphokinase was 155 U/L (reference range, 30-240 U/L), and the complete blood count was notable only for an elevated white blood count of 15.3 × 109/L (reference range, 4.0-11.0 × 109/L), with 73.4% neutrophils, 16.2% lymphocytes, 9.1% monocytes, 0.5% eosinophils, and 0.4% basophils. The patient’s urinalysis was unremarkable.
What is your diagnosis?
How would you treat this patient?
Discussion
The ED physician considered viral infection and tested for both influenza and COVID-19. Laboratory results eliminated urinary tract infection and rhabdomyolysis as possible diagnoses. An acute phase reaction to zoledronic acid was determined to be the most likely cause. The patient was treated with IV saline in the ED, and acetaminophen both in the ED and at home.
Although initial nursing triage notes document consideration of acute phase reaction to zoledronic acid, the endocrinology service, which had recommended and arranged the zoledronic acid infusion, was not immediately notified of the reaction. It does not appear any treatment (eg, acetaminophen) was suggested, only that the patient was given advice this may resolve over 3 to 4 days. When he was seen 2 months later for an endocrinology follow-up appointment, he reported that all symptoms (chills, myalgias, and nausea) resolved gradually over 1 week. Since then, he has felt as well as he did before taking zoledronic acid. However, the patient was wary of further zoledronic acid, opting to defer deciding on a second dose until a future appointment.
Prior to starting zoledronic acid therapy, the patient was being treated for vitamin D deficiency. Four months prior to infusion, his 25-hydroxyvitamin D level was 12.0 ng/mL (reference range, 30 to 80 ng/mL). He then started taking cholecalciferol 100 mcg (4000 IU) daily. Eight days prior to infusion his 25-hydroxyvitamin D level was 29.5 ng/mL.
Federal health care practitioners, especially those working in the Veterans Health Administration (VHA), will commonly encounter patients similar to this case. Osteoporosisis is common in the United States with > 10 million diagnoses (including > 2 million men) and in VHA primary care populations.1,2 Zoledronic acid is a frequently prescribed treatment, appearing in guidelines for osteoporosis management.3-5
The acute phase reaction is a common adverse effect of both oral and IV bisphosphonates, although it’s substantially more common with IV bisphosphonates such as zoledronic acid. This reaction is characterized by flu-like symptoms of fever, myalgia, and arthralgia that occur within the first few days following bisphosphonate administration, and tends to be rated mild to moderate by patients.6 Clinical trial data from > 7000 women with postmenopausal osteoporosis found that 42% experienced ≥ 1 acute phase symptom following the first infusion (fever was most common, followed by musculoskeletal symptoms and gastrointestinal symptoms), compared with 12% for placebo. Incidence decreases with each subsequent infusion.7 Risk factors for reactions include low 25-hydroxyvitamin D levels,8,9 no prior bisphosphonate exposure,9 younger age (aged 64-67 years vs 78-89 years),7 lower body mass index,10 and higher lymphocyte levels at baseline.11 While most cases are mild and self-limited, severe consequences have been noted, such as precipitation of adrenal crisis.12,13 Additionally, more prolonged bone pain, sometimes quite severe, has been rarely reported with bisphosphonate use. However, it’s unclear whether this represents a separate adverse effect or a more severe acute phase reaction.6
The acute phase reaction is a transient inflammatory state marked by increases in proinflammatory cytokines such as C-reactive protein, interleukin-6, and tumor necrosis factor-α. Proposed mechanisms include: (1) inhibition of farnesyl pyrophosphate synthase, an enzyme of the mevalonate pathway, resulting inactivation of γϐ T cells and increased production of proinflammatory cytokines; (2) inhibition of the suppressor of cytokine signalling-3 in the macrophages, resulting in cessation of the suppression in cytokine signaling; or (3) negative regulation of γϐ T-cell expansion and interferon-c production by low serum 25-hydroxyvitamin D concentrations.11
Prevention
Can an acute phase reaction to zoledronic acid be prevented? Bourke and colleagues reported that baseline calcium and/or vitamin D intake do not appear to affect rates of acute phase reaction in data pooled from 2 trials of zoledronic acid in postmenopausal women.14 However, patients receiving zoledronic acid had 25-hydroxyvitamin D values > 20 ng/mL 86% of the time, and values > 30 ng/mL 36% of the time. Bourke and colleagues suggest that “coadministration of calcium and vitamin D with zoledronate may not be necessary for individuals not at risk of marked vitamin D deficiency.”14 However, they did not prospectively test this hypothesis.
In our patient, vitamin D deficiency had been identified and treated, nearly achieving 30 ng/mL. The 2020 guidelines for postmenopausal osteoporosis recommend maintaining serum 25-hydroxyvitamin D levels 30 to 50 ng/mL, advising to supplement with vitamin D3 as needed.5 The 2012 guidelines for osteoporosis in men from the Endocrine Society suggest that men with low vitamin D levels receive vitamin D supplements to raise the level > 30 ng/ml.4
Oral analgesics have been studied for the prevention of adverse effects related to zoledronic acid. Initiating 650 mg acetaminophen 45 minutes before zoledronic acid infusion and then every 6 hours over the next 3 days has been shown to significantly reduce symptoms.15 Acetaminophen or ibuprofen given every 6 hours for 3 days (starting 4 hours after zoledronic acid infusion) has been shown to reduce fever and other symptoms.16
Statins have been shown in vitro to prevent bisphosphonate-induced γϐ T cell activation.17 This has led to studies with various statins, although none have yet shown benefit in vivo. A double-blind, randomized, placebo-controlled trial of postmenopausal women for fluvastatin (single dose of 40 mg or 3 doses of 40 mg, each 24 hours apart) did not prevent acute phase reaction symptoms, nor did it prevent zoledronic acid-induced cytokine release.17 Rosuvastatin 10 mg daily starting 5 days before zoledronic acid treatment and taken for a total of 11 days did not show any difference in fever or pain.18 A protocol for pravastatin has been disseminated, but no study results have been published yet.19
Prophylactic dexamethasone has also been studied. A randomized double-blind, placebo-controlled trial of oral dexamethasone 4 mg at the time of first infusion of zoledronic acid found no significant difference in temperature change or symptom score over the following 3 days.20 Chen and colleagues compared the efficacy of acetaminophen alone vs acetaminophen plus dexamethasone over several days.21 Acetaminophen 500 mg was given on the day of infusion and 4 times daily for 3 to 7 days for both groups, while dexamethasone 4 mg was given for 3 to 7 days. The dexamethasone group reported substantially lower incidence of any acute phase reaction symptoms (34% vs 67%, P = .003). A more recent study by Murdoch and colleagues comparing dexamethasone (4 mg daily for 3 days with the first dose 90 minutes before zoledronic acid infusion) with placebo found that the dexamethasone group had a statistically significant lower mean temperature change and acute phase reaction symptom score.22
Adverse Effect Treatment
Treatment after development of acute phase reaction due to zoledronic acid infusion is generally limited to supportive care and/or nonsteroidal anti-inflammatory drugs (NSAIDs) acetaminophen or dexamethasone, largely based on extrapolation of the noted preventive trials and expert opinion.3,6 Experiencing an acute phase reaction may portend better fracture risk reduction from zoledronic acid, although there is a potential association between acute phase reaction and mortality risk.23,24
Our case was typical for acute phase reaction to zoledronic acid. The patient was already taking rosuvastatin 10 mg daily for hypercholesterolemia as prescribed by his primary care physician. Rosuvastatin was not shown to prevent symptoms, although it was not studied in patients on long-term statin therapy at the time of zoledronic acid infusion.18 The patient was also taking vitamin D3 supplementation and was nearly in the reference range.5 His ED treatment included IV fluids and acetaminophen. Pretreatment (prior to or at the time of zoledronic acid infusion) with acetaminophen or ibuprofen may have prevented his symptoms, or at least lessened them to the point that an ED visit would not have resulted. The endocrinologist who prescribed the zoledronic acid documented a detailed discussion of the adverse effects of zoledronic acid with the patient, and the initial nursing call documents consideration of acute phase reaction. It is unclear whether the persistence of symptoms or worsening of symptoms ultimately led to the ED visit. Because no treatment was offered, it is unknown whether earlier posttreatment with acetaminophen, ibuprofen, or dexamethasone might have prevented his ED visit.
Conclusions
Clinicians who treat patients with osteoporosis should be aware of several key points. First, acute phase reaction symptoms are common with bisphosphonates, especially zoledronic acid infusions. Second, the symptoms are nonspecific but should have a suggestive time course. Third, dexamethasone may be partially protective, but based on the various trials discussed, it likely needs to be given for multiple days (instead of a single dose on the day of infusion). Given that acetaminophen and NSAIDs also seem to be protective (when given for multiple days starting on the day of infusion), both have lower overall adverse effect profiles than dexamethasone, consideration may be given to using either of these prophylactically.6 Dexamethasone could then be prescribed if symptoms are severe or persistent despite the use of acetaminophen or NSAIDs.
1. Choksi P, Gay BL, Reyes-Gastelum D, Haymart MR, Papaleontiou M. Understanding osteoporosis screening practices in men: a nationwide physician survey. Endocr Pract. 2020;26(11):1237-1243. doi:10.4158/EP-2020-0123
2. Yu ZL, Fisher L, Hand J. Osteoporosis screening for male veterans in a resident based primary care clinic at Northport Veterans Affairs Medical Center. Am J Med Qual. 2023;38(5):272.doi:10.1097/JMQ.0000000000000134
3. Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. doi:10.1210/jc.2019-00221
4. Watts NB, Adler RA, Bilezikian JP, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802-1822. doi:10.1210/jc.2011-3045
5. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2020 update. Endocr Pract. 2020;26(suppl 1):1-46. doi:10.4158/GL-2020-0524SUPPL
6. Lim SY, Bolster MB. What can we do about musculoskeletal pain from bisphosphonates?. Cleve Clin J Med. 2018;85(9):675-678. doi:10.3949/ccjm.85a.18005
7. Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab. 2010;95(9):4380-4387. doi:10.1210/jc.2010-0597
8. Lu K, Shi Q, Gong YQ, Li C. Association between vitamin D and zoledronate-induced acute-phase response fever risk in osteoporotic patients. Front Endocrinol (Lausanne). 2022;13:991913. Published 2022 Oct 10. doi:10.3389/fendo.2022.991913
9. Popp AW, Senn R, Curkovic I, et al. Factors associated with acute-phase response of bisphosphonate-naïve or pretreated women with osteoporosis receiving an intravenous first dose of zoledronate or ibandronate. Osteoporos Int. 2017;28(6):1995-2002. doi:10.1007/s00198-017-3992-5
10. Zheng X, Ye J, Zhan Q, et al. Prediction of musculoskeletal pain after the first intravenous zoledronic acid injection in patients with primary osteoporosis: development and evaluation of a new nomogram. BMC Musculoskelet Disord. 2023;24(1):841. Published 2023 Oct 25. doi:10.1186/s12891-023-06965-y
11. Anastasilakis AD, Polyzos SA, Delaroudis S, et al. The role of cytokines and adipocytokines in zoledronate-induced acute phase reaction in postmenopausal women with low bone mass. Clin Endocrinol (Oxf). 2012;77(6):816-822. doi:10.1111/j.1365-2265.2012.04459.x
12. Smrecnik M, Kavcic Trsinar Z, Kocjan T. Adrenal crisis after first infusion of zoledronic acid: a case report. Osteoporos Int. 2018;29(7):1675-1678. doi:10.1007/s00198-018-4508-7
13. Kuo B, Koransky A, Vaz Wicks CL. Adrenal crisis as an adverse reaction to zoledronic acid in a patient with primary adrenal insufficiency: a case report and literature review. AACE Clin Case Rep. 2022;9(2):32-34. Published 2022 Dec 17. doi:10.1016/j.aace.2022.12.003
14. Bourke S, Bolland MJ, Grey A, et al. The impact of dietary calcium intake and vitamin D status on the effects of zoledronate. Osteoporos Int. 2013;24(1):349-354. doi:10.1007/s00198-012-2117-4
15. Silverman SL, Kriegman A, and Goncalves J, et al. Effect of acetaminophen and fluvastatin on post-dose symptoms following infusion of zoledronic acid. Osteoporos Int. 2011;22(8):2337-2345.
16. Wark JD, Bensen W, Recknor C, et al. Treatment with acetaminophen/paracetamol or ibuprofen alleviates post-dose symptoms related to intravenous infusion with zoledronic acid 5 mg. Osteoporos Int. 2012;23(2):503-512. doi:10.1007/s00198-011-1563-8
17. Thompson K, Keech F, McLernon DJ, et al. Fluvastatin does not prevent the acute-phase response to intravenous zoledronic acid in post-menopausal women. Bone. 2011;49(1):140-145. doi:10.1016/j.bone.2010.10.177
18. Makras P, Anastasilakis AD, Polyzos SA, Bisbinas I, Sakellariou GT, Papapoulos SE. No effect of rosuvastatin in the zoledronate-induced acute-phase response. Calcif Tissue Int. 2011;88(5):402-408. doi:10.1007/s00223-011-9468-2
19. Liu Q, Han G, Li R, et al. Reduction effect of oral pravastatin on the acute phase response to intravenous zoledronic acid: protocol for a real-world prospective, placebo-controlled trial. BMJ Open. 2022;12(7):e060703. Published 2022 Jul 13. doi:10.1136/bmjopen-2021-060703
20. Billington EO, Horne A, Gamble GD, Maslowski K, House M, Reid IR. Effect of single-dose dexamethasone on acute phase response following zoledronic acid: a randomized controlled trial. Osteoporos Int. 2017;28(6):1867-1874. doi:10.1007/s00198-017-3960-0
21. Chen FP, Fu TS, Lin YC, Lin YJ. Addition of dexamethasone to manage acute phase responses following initial zoledronic acid infusion. Osteoporos Int. 2021;32(4):663-670. doi:10.1007/s00198-020-05653-0
22. Murdoch R, Mellar A, Horne AM, et al. Effect of a three-day course of dexamethasone on acute phase response following treatment with zoledronate: a randomized controlled trial. J Bone Miner Res. 2023;38(5):631-638. doi:10.1002/jbmr.4802
23. Black DM, Reid IR, Napoli N, et al. The interaction of acute-phase reaction and efficacy for osteoporosis after zoledronic acid: HORIZON pivotal fracture trial. J Bone Miner Res. 2022;37(1):21-28. doi:10.1002/jbmr.4434
24. Lu K, Wu YM, Shi Q, Gong YQ, Zhang T, Li C. The impact of acute-phase reaction on mortality and re-fracture after zoledronic acid in hospitalized elderly osteoporotic fracture patients. Osteoporos Int. 2023;34(9):1613-1623. doi:10.1007/s00198-023-06803-w
1. Choksi P, Gay BL, Reyes-Gastelum D, Haymart MR, Papaleontiou M. Understanding osteoporosis screening practices in men: a nationwide physician survey. Endocr Pract. 2020;26(11):1237-1243. doi:10.4158/EP-2020-0123
2. Yu ZL, Fisher L, Hand J. Osteoporosis screening for male veterans in a resident based primary care clinic at Northport Veterans Affairs Medical Center. Am J Med Qual. 2023;38(5):272.doi:10.1097/JMQ.0000000000000134
3. Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. doi:10.1210/jc.2019-00221
4. Watts NB, Adler RA, Bilezikian JP, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802-1822. doi:10.1210/jc.2011-3045
5. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2020 update. Endocr Pract. 2020;26(suppl 1):1-46. doi:10.4158/GL-2020-0524SUPPL
6. Lim SY, Bolster MB. What can we do about musculoskeletal pain from bisphosphonates?. Cleve Clin J Med. 2018;85(9):675-678. doi:10.3949/ccjm.85a.18005
7. Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab. 2010;95(9):4380-4387. doi:10.1210/jc.2010-0597
8. Lu K, Shi Q, Gong YQ, Li C. Association between vitamin D and zoledronate-induced acute-phase response fever risk in osteoporotic patients. Front Endocrinol (Lausanne). 2022;13:991913. Published 2022 Oct 10. doi:10.3389/fendo.2022.991913
9. Popp AW, Senn R, Curkovic I, et al. Factors associated with acute-phase response of bisphosphonate-naïve or pretreated women with osteoporosis receiving an intravenous first dose of zoledronate or ibandronate. Osteoporos Int. 2017;28(6):1995-2002. doi:10.1007/s00198-017-3992-5
10. Zheng X, Ye J, Zhan Q, et al. Prediction of musculoskeletal pain after the first intravenous zoledronic acid injection in patients with primary osteoporosis: development and evaluation of a new nomogram. BMC Musculoskelet Disord. 2023;24(1):841. Published 2023 Oct 25. doi:10.1186/s12891-023-06965-y
11. Anastasilakis AD, Polyzos SA, Delaroudis S, et al. The role of cytokines and adipocytokines in zoledronate-induced acute phase reaction in postmenopausal women with low bone mass. Clin Endocrinol (Oxf). 2012;77(6):816-822. doi:10.1111/j.1365-2265.2012.04459.x
12. Smrecnik M, Kavcic Trsinar Z, Kocjan T. Adrenal crisis after first infusion of zoledronic acid: a case report. Osteoporos Int. 2018;29(7):1675-1678. doi:10.1007/s00198-018-4508-7
13. Kuo B, Koransky A, Vaz Wicks CL. Adrenal crisis as an adverse reaction to zoledronic acid in a patient with primary adrenal insufficiency: a case report and literature review. AACE Clin Case Rep. 2022;9(2):32-34. Published 2022 Dec 17. doi:10.1016/j.aace.2022.12.003
14. Bourke S, Bolland MJ, Grey A, et al. The impact of dietary calcium intake and vitamin D status on the effects of zoledronate. Osteoporos Int. 2013;24(1):349-354. doi:10.1007/s00198-012-2117-4
15. Silverman SL, Kriegman A, and Goncalves J, et al. Effect of acetaminophen and fluvastatin on post-dose symptoms following infusion of zoledronic acid. Osteoporos Int. 2011;22(8):2337-2345.
16. Wark JD, Bensen W, Recknor C, et al. Treatment with acetaminophen/paracetamol or ibuprofen alleviates post-dose symptoms related to intravenous infusion with zoledronic acid 5 mg. Osteoporos Int. 2012;23(2):503-512. doi:10.1007/s00198-011-1563-8
17. Thompson K, Keech F, McLernon DJ, et al. Fluvastatin does not prevent the acute-phase response to intravenous zoledronic acid in post-menopausal women. Bone. 2011;49(1):140-145. doi:10.1016/j.bone.2010.10.177
18. Makras P, Anastasilakis AD, Polyzos SA, Bisbinas I, Sakellariou GT, Papapoulos SE. No effect of rosuvastatin in the zoledronate-induced acute-phase response. Calcif Tissue Int. 2011;88(5):402-408. doi:10.1007/s00223-011-9468-2
19. Liu Q, Han G, Li R, et al. Reduction effect of oral pravastatin on the acute phase response to intravenous zoledronic acid: protocol for a real-world prospective, placebo-controlled trial. BMJ Open. 2022;12(7):e060703. Published 2022 Jul 13. doi:10.1136/bmjopen-2021-060703
20. Billington EO, Horne A, Gamble GD, Maslowski K, House M, Reid IR. Effect of single-dose dexamethasone on acute phase response following zoledronic acid: a randomized controlled trial. Osteoporos Int. 2017;28(6):1867-1874. doi:10.1007/s00198-017-3960-0
21. Chen FP, Fu TS, Lin YC, Lin YJ. Addition of dexamethasone to manage acute phase responses following initial zoledronic acid infusion. Osteoporos Int. 2021;32(4):663-670. doi:10.1007/s00198-020-05653-0
22. Murdoch R, Mellar A, Horne AM, et al. Effect of a three-day course of dexamethasone on acute phase response following treatment with zoledronate: a randomized controlled trial. J Bone Miner Res. 2023;38(5):631-638. doi:10.1002/jbmr.4802
23. Black DM, Reid IR, Napoli N, et al. The interaction of acute-phase reaction and efficacy for osteoporosis after zoledronic acid: HORIZON pivotal fracture trial. J Bone Miner Res. 2022;37(1):21-28. doi:10.1002/jbmr.4434
24. Lu K, Wu YM, Shi Q, Gong YQ, Zhang T, Li C. The impact of acute-phase reaction on mortality and re-fracture after zoledronic acid in hospitalized elderly osteoporotic fracture patients. Osteoporos Int. 2023;34(9):1613-1623. doi:10.1007/s00198-023-06803-w
Robotic Pet Therapy in the Intensive Care Unit
Critical illness is commonly associated with interrelated conditions including pain, agitation, delirium, immobility, and sleep disruption (PADIS). Managing PADIS is often complex and includes pharmacologic and nonpharmacologic interventions.1 Incorporating multifaceted practices to enhance PADIS management has been shown to improve several intensive care unit (ICU)-related outcomes.2
Many pharmacologic PADIS treatments are ineffective or associated with adverse effects. For example, antipsychotics used for treating ICU-related delirium have not shown improved outcomes.3,4 Commonly used medications for agitation, such as benzodiazepines, increase delirium risk.5,6 Because of these limitations, several nonpharmacologic interventions for PADIS have been evaluated.
Pet therapy has been implemented in some ICU settings, but is not widely adopted.7 Also referred to as animal-assisted activities, animal-assisted therapy, or animal-assisted interventions, pet therapy typically involves interaction between a patient and a live animal (most commonly a dog) under the direction of an animal handler, with the intention of providing therapeutic benefit. Interactions frequently include meet and greet activities such as petting, but also could include walking or other activities. Pet therapy has been reported to reduce pain, agitation, and stress among ICU patients.8 Introducing a pet therapy program with live animals in the ICU could be challenging because of factors such as identifying trained, accredited animals and handlers, and managing infection control and other risks.9 As an alternative to live pets, robotic pet therapy has been shown to be beneficial—mostly outside the ICU—in settings such as long-term care.10,11 Although uncommon, robotic pets have been used in the ICU and hospital settings for therapeutic purposes.12 Robotic pets reduce many concerns associated with live animals while mimicking the behaviors of live animals and potentially offering many of the same benefits.
OBSERVATIONS
The North Florida/South Georgia Veterans Health System (NF/SGVHS) implemented a novel robotic pet therapy program for patients requiring ICU care to improve the treatment of PADIS. Funding was provided through a Veterans Health Administration Innovation Grant procured by a clinical pharmacy specialist as the program’s champion. Goals of the robotic pet therapy program include reductions in: distressing symptoms associated with PADIS, use of psychoactive drugs and physical restraints, and ICU length of stay. The ICU team developed standard operating procedures and an order menu, which were integrated into the ICU prescriber ordering menu. Patients were selected for pet therapy based on PADIS scores and potential for positive response to pet therapy as assessed by the ICU team.Patients in medical and surgical ICU settings were eligible for the program. The robotic pets used in the program were Joy for All Companion Pets (Ageless Innovation LLC). Robotic cats and dogs were available and pets were “adopted’ by each patient (Figure). As an infection control measure, pets were not reissued or shared amongpatients and pets could be cleaned with a disinfectant solution. Nurses were primarily responsible for monitoring and documenting responses to robotic pet therapy.
It was necessary to secure buy-in from several services to successfully implement the program. The critical care clinical pharmacy specialists were responsible for ordering, storing, and dispensing the robotic pets. The NF/SGVHS innovation specialist helped secure funding, procure the robotic pet, and promote the program. The standard operating procedures for the program were developed by a multidisciplinary team with input from critical care nurses, intensivists, pharmacists, patient safety, and infection control (Table 1). Success of the program also required buy-in from ICU team members.
Program Impact
A retrospective cohort study was conducted to assess for improvements in PADIS symptoms and medication use post-intervention. Patients were included if they received robotic pet therapy in the ICU from July 10, 2019, to February 1, 2021. Individuals aged < 18 years or > 89 years, were pregnant, or were not receiving ICU-level care were excluded. Outcomes assessed included improvement in pain scores, agitation scores, sleep quality, resolution of delirium, and use of pain or psychoactive medications during patients’ ICU stay.
Thirty patients were included in the study (Table 2). After receiving a robotic pet, 9 (30%) patients recorded decreased pain scores, 15 (50%) recorded decreased agitation scores, 8 (27%) had resolution of delirium, and 2 (7%) described improvement in sleep. Pain medication use decreased in 12 (40%) patients and psychoactive medication use was reduced in 7 (23%) patients.
Limitations
The robotic pet therapy program has shown promising results; however, some aspects merit discussion. Evaluation of this program is limited by factors such as the observational study design, single-center patient sample, and lack of comparator group. Although no known adverse effects of robotic pet therapy were seen, it is possible that some patients may not have a favorable response. Challenges of implementing a robotic pet therapy program include cost and additional operational activities (storage, ordering, dispensing) necessary to maintain the program. Additional research is needed to evaluate the impact of robotic pet therapy on other outcomes including cost, ICU length of stay, and patient satisfaction.
CONCLUSIONS
Robotic pet therapy can be successfully implemented in the ICU and appears to provide a simple, safe, beneficial, nonpharmacologic intervention for PADIS. This study showed that many patients had favorable response to robotic pet therapy, indicating that it may be a viable alternative to traditional pet therapy. Other health systems could benefit from implementing programs similar to the robotic pet therapy program at NF/SGVHS.
Acknowledgments
The author would like to acknowledge Simran Panesar, PharmD, and Theresa Faison, PharmD, for their contributions to this project.
1. Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825-e873. doi:10.1097/CCM.0000000000003299
2. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU Liberation Collaborative in over 15,000 adults. Crit Care Med. 2019;47:3-14. doi:10.1097/CCM.0000000000003482
3. Andersen-Ranberg NC, Poulsen LM, Perner A, et al; AID-ICU Trial Group. Haloperidol for the treatment of delirium in ICU patients. N Engl J Med. 2022;387:2425-2435. doi:10.1056/NEJMoa2211868
4. Girard TD, Exline MC, Carson SS, et al; MIND-USA Investigators. Haloperidol and ziprasidone for treatment of delirium in critical illness. N Engl J Med. 2018;379:2506-2516. doi:10.1056/NEJMoa1808217
5. Riker RR, Shehabi Y, Bokesch PM, et al; SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489-499. doi:10.1001/jama.2009.56
6. Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21-26. doi:10.1097/00000542-200601000-00005
7. Society of Critical Care Medicine. ICU liberation bundle. Accessed February 27, 2024. https://www.sccm.org/ICULiberation/Home/ABCDEF-Bundles
8. Lovell T, Ranse K. Animal-assisted activities in the intensive care unit: a scoping review. Intensive Crit Care Nurs. 2022;73:103304. doi:10.1016/j.iccn.2022.103304
9. Hosey MM, Jaskulski J, Wegener ST, Chlan LL, Needham DM. Animal-assisted intervention in the ICU: a tool for humanization. Crit Care. 2018;22:22. doi:10.1186/s13054-018-1946-8
10. Jøranson N, Pedersen I, Rokstad AM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2015;16:867-873. doi:10.1016/j.jamda.2015.05.002
11. Robinson H, Macdonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667. doi:10.1016/j.jamda.2013.02.007
12. Schulman-Marcus J, Mookherjee S, Rice L, Lyubarova R. New approaches for the treatment of delirium: a case for robotic pets. Am J Med. 2019;132:781-782. doi:10.1016/j.amjmed.2018.12.039
Critical illness is commonly associated with interrelated conditions including pain, agitation, delirium, immobility, and sleep disruption (PADIS). Managing PADIS is often complex and includes pharmacologic and nonpharmacologic interventions.1 Incorporating multifaceted practices to enhance PADIS management has been shown to improve several intensive care unit (ICU)-related outcomes.2
Many pharmacologic PADIS treatments are ineffective or associated with adverse effects. For example, antipsychotics used for treating ICU-related delirium have not shown improved outcomes.3,4 Commonly used medications for agitation, such as benzodiazepines, increase delirium risk.5,6 Because of these limitations, several nonpharmacologic interventions for PADIS have been evaluated.
Pet therapy has been implemented in some ICU settings, but is not widely adopted.7 Also referred to as animal-assisted activities, animal-assisted therapy, or animal-assisted interventions, pet therapy typically involves interaction between a patient and a live animal (most commonly a dog) under the direction of an animal handler, with the intention of providing therapeutic benefit. Interactions frequently include meet and greet activities such as petting, but also could include walking or other activities. Pet therapy has been reported to reduce pain, agitation, and stress among ICU patients.8 Introducing a pet therapy program with live animals in the ICU could be challenging because of factors such as identifying trained, accredited animals and handlers, and managing infection control and other risks.9 As an alternative to live pets, robotic pet therapy has been shown to be beneficial—mostly outside the ICU—in settings such as long-term care.10,11 Although uncommon, robotic pets have been used in the ICU and hospital settings for therapeutic purposes.12 Robotic pets reduce many concerns associated with live animals while mimicking the behaviors of live animals and potentially offering many of the same benefits.
OBSERVATIONS
The North Florida/South Georgia Veterans Health System (NF/SGVHS) implemented a novel robotic pet therapy program for patients requiring ICU care to improve the treatment of PADIS. Funding was provided through a Veterans Health Administration Innovation Grant procured by a clinical pharmacy specialist as the program’s champion. Goals of the robotic pet therapy program include reductions in: distressing symptoms associated with PADIS, use of psychoactive drugs and physical restraints, and ICU length of stay. The ICU team developed standard operating procedures and an order menu, which were integrated into the ICU prescriber ordering menu. Patients were selected for pet therapy based on PADIS scores and potential for positive response to pet therapy as assessed by the ICU team.Patients in medical and surgical ICU settings were eligible for the program. The robotic pets used in the program were Joy for All Companion Pets (Ageless Innovation LLC). Robotic cats and dogs were available and pets were “adopted’ by each patient (Figure). As an infection control measure, pets were not reissued or shared amongpatients and pets could be cleaned with a disinfectant solution. Nurses were primarily responsible for monitoring and documenting responses to robotic pet therapy.
It was necessary to secure buy-in from several services to successfully implement the program. The critical care clinical pharmacy specialists were responsible for ordering, storing, and dispensing the robotic pets. The NF/SGVHS innovation specialist helped secure funding, procure the robotic pet, and promote the program. The standard operating procedures for the program were developed by a multidisciplinary team with input from critical care nurses, intensivists, pharmacists, patient safety, and infection control (Table 1). Success of the program also required buy-in from ICU team members.
Program Impact
A retrospective cohort study was conducted to assess for improvements in PADIS symptoms and medication use post-intervention. Patients were included if they received robotic pet therapy in the ICU from July 10, 2019, to February 1, 2021. Individuals aged < 18 years or > 89 years, were pregnant, or were not receiving ICU-level care were excluded. Outcomes assessed included improvement in pain scores, agitation scores, sleep quality, resolution of delirium, and use of pain or psychoactive medications during patients’ ICU stay.
Thirty patients were included in the study (Table 2). After receiving a robotic pet, 9 (30%) patients recorded decreased pain scores, 15 (50%) recorded decreased agitation scores, 8 (27%) had resolution of delirium, and 2 (7%) described improvement in sleep. Pain medication use decreased in 12 (40%) patients and psychoactive medication use was reduced in 7 (23%) patients.
Limitations
The robotic pet therapy program has shown promising results; however, some aspects merit discussion. Evaluation of this program is limited by factors such as the observational study design, single-center patient sample, and lack of comparator group. Although no known adverse effects of robotic pet therapy were seen, it is possible that some patients may not have a favorable response. Challenges of implementing a robotic pet therapy program include cost and additional operational activities (storage, ordering, dispensing) necessary to maintain the program. Additional research is needed to evaluate the impact of robotic pet therapy on other outcomes including cost, ICU length of stay, and patient satisfaction.
CONCLUSIONS
Robotic pet therapy can be successfully implemented in the ICU and appears to provide a simple, safe, beneficial, nonpharmacologic intervention for PADIS. This study showed that many patients had favorable response to robotic pet therapy, indicating that it may be a viable alternative to traditional pet therapy. Other health systems could benefit from implementing programs similar to the robotic pet therapy program at NF/SGVHS.
Acknowledgments
The author would like to acknowledge Simran Panesar, PharmD, and Theresa Faison, PharmD, for their contributions to this project.
Critical illness is commonly associated with interrelated conditions including pain, agitation, delirium, immobility, and sleep disruption (PADIS). Managing PADIS is often complex and includes pharmacologic and nonpharmacologic interventions.1 Incorporating multifaceted practices to enhance PADIS management has been shown to improve several intensive care unit (ICU)-related outcomes.2
Many pharmacologic PADIS treatments are ineffective or associated with adverse effects. For example, antipsychotics used for treating ICU-related delirium have not shown improved outcomes.3,4 Commonly used medications for agitation, such as benzodiazepines, increase delirium risk.5,6 Because of these limitations, several nonpharmacologic interventions for PADIS have been evaluated.
Pet therapy has been implemented in some ICU settings, but is not widely adopted.7 Also referred to as animal-assisted activities, animal-assisted therapy, or animal-assisted interventions, pet therapy typically involves interaction between a patient and a live animal (most commonly a dog) under the direction of an animal handler, with the intention of providing therapeutic benefit. Interactions frequently include meet and greet activities such as petting, but also could include walking or other activities. Pet therapy has been reported to reduce pain, agitation, and stress among ICU patients.8 Introducing a pet therapy program with live animals in the ICU could be challenging because of factors such as identifying trained, accredited animals and handlers, and managing infection control and other risks.9 As an alternative to live pets, robotic pet therapy has been shown to be beneficial—mostly outside the ICU—in settings such as long-term care.10,11 Although uncommon, robotic pets have been used in the ICU and hospital settings for therapeutic purposes.12 Robotic pets reduce many concerns associated with live animals while mimicking the behaviors of live animals and potentially offering many of the same benefits.
OBSERVATIONS
The North Florida/South Georgia Veterans Health System (NF/SGVHS) implemented a novel robotic pet therapy program for patients requiring ICU care to improve the treatment of PADIS. Funding was provided through a Veterans Health Administration Innovation Grant procured by a clinical pharmacy specialist as the program’s champion. Goals of the robotic pet therapy program include reductions in: distressing symptoms associated with PADIS, use of psychoactive drugs and physical restraints, and ICU length of stay. The ICU team developed standard operating procedures and an order menu, which were integrated into the ICU prescriber ordering menu. Patients were selected for pet therapy based on PADIS scores and potential for positive response to pet therapy as assessed by the ICU team.Patients in medical and surgical ICU settings were eligible for the program. The robotic pets used in the program were Joy for All Companion Pets (Ageless Innovation LLC). Robotic cats and dogs were available and pets were “adopted’ by each patient (Figure). As an infection control measure, pets were not reissued or shared amongpatients and pets could be cleaned with a disinfectant solution. Nurses were primarily responsible for monitoring and documenting responses to robotic pet therapy.
It was necessary to secure buy-in from several services to successfully implement the program. The critical care clinical pharmacy specialists were responsible for ordering, storing, and dispensing the robotic pets. The NF/SGVHS innovation specialist helped secure funding, procure the robotic pet, and promote the program. The standard operating procedures for the program were developed by a multidisciplinary team with input from critical care nurses, intensivists, pharmacists, patient safety, and infection control (Table 1). Success of the program also required buy-in from ICU team members.
Program Impact
A retrospective cohort study was conducted to assess for improvements in PADIS symptoms and medication use post-intervention. Patients were included if they received robotic pet therapy in the ICU from July 10, 2019, to February 1, 2021. Individuals aged < 18 years or > 89 years, were pregnant, or were not receiving ICU-level care were excluded. Outcomes assessed included improvement in pain scores, agitation scores, sleep quality, resolution of delirium, and use of pain or psychoactive medications during patients’ ICU stay.
Thirty patients were included in the study (Table 2). After receiving a robotic pet, 9 (30%) patients recorded decreased pain scores, 15 (50%) recorded decreased agitation scores, 8 (27%) had resolution of delirium, and 2 (7%) described improvement in sleep. Pain medication use decreased in 12 (40%) patients and psychoactive medication use was reduced in 7 (23%) patients.
Limitations
The robotic pet therapy program has shown promising results; however, some aspects merit discussion. Evaluation of this program is limited by factors such as the observational study design, single-center patient sample, and lack of comparator group. Although no known adverse effects of robotic pet therapy were seen, it is possible that some patients may not have a favorable response. Challenges of implementing a robotic pet therapy program include cost and additional operational activities (storage, ordering, dispensing) necessary to maintain the program. Additional research is needed to evaluate the impact of robotic pet therapy on other outcomes including cost, ICU length of stay, and patient satisfaction.
CONCLUSIONS
Robotic pet therapy can be successfully implemented in the ICU and appears to provide a simple, safe, beneficial, nonpharmacologic intervention for PADIS. This study showed that many patients had favorable response to robotic pet therapy, indicating that it may be a viable alternative to traditional pet therapy. Other health systems could benefit from implementing programs similar to the robotic pet therapy program at NF/SGVHS.
Acknowledgments
The author would like to acknowledge Simran Panesar, PharmD, and Theresa Faison, PharmD, for their contributions to this project.
1. Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825-e873. doi:10.1097/CCM.0000000000003299
2. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU Liberation Collaborative in over 15,000 adults. Crit Care Med. 2019;47:3-14. doi:10.1097/CCM.0000000000003482
3. Andersen-Ranberg NC, Poulsen LM, Perner A, et al; AID-ICU Trial Group. Haloperidol for the treatment of delirium in ICU patients. N Engl J Med. 2022;387:2425-2435. doi:10.1056/NEJMoa2211868
4. Girard TD, Exline MC, Carson SS, et al; MIND-USA Investigators. Haloperidol and ziprasidone for treatment of delirium in critical illness. N Engl J Med. 2018;379:2506-2516. doi:10.1056/NEJMoa1808217
5. Riker RR, Shehabi Y, Bokesch PM, et al; SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489-499. doi:10.1001/jama.2009.56
6. Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21-26. doi:10.1097/00000542-200601000-00005
7. Society of Critical Care Medicine. ICU liberation bundle. Accessed February 27, 2024. https://www.sccm.org/ICULiberation/Home/ABCDEF-Bundles
8. Lovell T, Ranse K. Animal-assisted activities in the intensive care unit: a scoping review. Intensive Crit Care Nurs. 2022;73:103304. doi:10.1016/j.iccn.2022.103304
9. Hosey MM, Jaskulski J, Wegener ST, Chlan LL, Needham DM. Animal-assisted intervention in the ICU: a tool for humanization. Crit Care. 2018;22:22. doi:10.1186/s13054-018-1946-8
10. Jøranson N, Pedersen I, Rokstad AM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2015;16:867-873. doi:10.1016/j.jamda.2015.05.002
11. Robinson H, Macdonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667. doi:10.1016/j.jamda.2013.02.007
12. Schulman-Marcus J, Mookherjee S, Rice L, Lyubarova R. New approaches for the treatment of delirium: a case for robotic pets. Am J Med. 2019;132:781-782. doi:10.1016/j.amjmed.2018.12.039
1. Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825-e873. doi:10.1097/CCM.0000000000003299
2. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU Liberation Collaborative in over 15,000 adults. Crit Care Med. 2019;47:3-14. doi:10.1097/CCM.0000000000003482
3. Andersen-Ranberg NC, Poulsen LM, Perner A, et al; AID-ICU Trial Group. Haloperidol for the treatment of delirium in ICU patients. N Engl J Med. 2022;387:2425-2435. doi:10.1056/NEJMoa2211868
4. Girard TD, Exline MC, Carson SS, et al; MIND-USA Investigators. Haloperidol and ziprasidone for treatment of delirium in critical illness. N Engl J Med. 2018;379:2506-2516. doi:10.1056/NEJMoa1808217
5. Riker RR, Shehabi Y, Bokesch PM, et al; SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489-499. doi:10.1001/jama.2009.56
6. Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21-26. doi:10.1097/00000542-200601000-00005
7. Society of Critical Care Medicine. ICU liberation bundle. Accessed February 27, 2024. https://www.sccm.org/ICULiberation/Home/ABCDEF-Bundles
8. Lovell T, Ranse K. Animal-assisted activities in the intensive care unit: a scoping review. Intensive Crit Care Nurs. 2022;73:103304. doi:10.1016/j.iccn.2022.103304
9. Hosey MM, Jaskulski J, Wegener ST, Chlan LL, Needham DM. Animal-assisted intervention in the ICU: a tool for humanization. Crit Care. 2018;22:22. doi:10.1186/s13054-018-1946-8
10. Jøranson N, Pedersen I, Rokstad AM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2015;16:867-873. doi:10.1016/j.jamda.2015.05.002
11. Robinson H, Macdonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667. doi:10.1016/j.jamda.2013.02.007
12. Schulman-Marcus J, Mookherjee S, Rice L, Lyubarova R. New approaches for the treatment of delirium: a case for robotic pets. Am J Med. 2019;132:781-782. doi:10.1016/j.amjmed.2018.12.039
Remembering the Dead in Unity and Peace
Soldiers’ graves are the greatest preachers of peace.
Albert Schweitzer 1
From the window of my room in the house where I grew up, I could see the American flag flying over Fort Sam Houston National Cemetery. I would ride my bicycle around the paths that divided the grassy sections of graves to the blocks where my father and grandfather were buried. I would stand before the gravesites in a state combining prayer, processing, and remembrance. Carved into my grandfather’s headstone were the 2 world wars he fought in and on my father’s, the 3 conflicts in which he served. I would walk up to their headstones and trace the emblems of belief: the engraved Star of David that marked my grandfather’s grave and the simple cross for my father.
My visits and writing about them may strike some readers as morbid. However, for me, the experience and memories are calming and peaceful, like the cemetery. There was something incredibly comforting about the uniformity of the headstones standing out for miles, mirroring the ranks of soldiers in the wars they commemorated. Yet, as with the men and women who fought each conflict, every grave told a succinct Hemingway-like story of their military career etched in stone. I know now that discrimination in the military segregated even the burial of service members.2 It appeared to my younger self that at least compared to civilian cemeteries with their massive monuments to the wealthy and powerful, there was an egalitarian effect: my master sergeant grandfather’s plot was indistinguishable from that of my colonel father.
Memorial Day and military cemeteries have a shared history. While Veterans Day honors all who have worn the uniform, living and dead, Memorial Day, as its name suggests, remembers those who have died in a broadly conceived line of duty. To emphasize the more solemn character of the holiday, the original name, Decoration Day, was changed to emphasize the reverence of remembrance.3 The first widespread observance of Memorial Day was to commemorate those who perished in the Civil War, which remains the conflict with the highest number of casualties in American history. The first national commemoration occurred at Arlington National Cemetery when 5000 volunteers decorated 20,000 Union and Confederate graves in an act of solidarity and reconciliation. The practice struck a chord in a country beleaguered by war and division.2
National cemeteries also emerged from the grief and gratitude that marked the Civil War. President Abraham Lincoln, who gave us the famous US Department of Veterans Affairs (VA) mission motto, also inaugurated national cemeteries. At the beginning of the Civil War, only Union soldiers who sacrificed their lives to end slavery were entitled to burial. Reflective of the rift that divided the country, Confederate soldiers contended that such divisiveness should not continue unto death and were granted the right to be buried beside those they fought against, united in death and memory.4
Today, the country is more divided than ever: more than a few observers of American culture, including the new popular film Civil War, believe we are on the brink of another civil war.5 While we take their warning seriously, there are still signs of unity amongst the people, like those who followed the war between the states. Recently, in that same national cemetery where I first contemplated these themes, justice, delayed too long, was not entirely denied. A ceremony was held to dedicate 17 headstones to honor the memories of Black World War I Army soldiers who were court-martialed and hanged in the wake of the Houston riots of 1917. As a sign of their dishonor, their headstones listed only their dates and names—nothing of their military service. At the urging of their descendants, the US Army reopened the files and found the verdict to have been racially motivated. They set aside their convictions, gave them honorable discharges for their service in life, and replaced their gravesites with ones that enshrined that respect in death.6
Some reading this column may, like me, have had the profound privilege of participating in a burial at a national cemetery. We recall the stirring mix of pride and loss when the honor guard hands the perfectly folded flag to the bereaved family member and bids farewell to their comrade with a salute. Yet, not all families have this privilege. One of the saddest experiences I recall is when I was in a leadership position at a VA facility and unable to help impoverished families who were denied VA burial benefits or payments to transport their deceased veteran closer to home. That sorrow often turned to thankful relief when a veterans service organization or other community group offered to pay the funerary expenses. Fortunately, like eligibility for VA health care, the criteria for burial benefits have steadily expanded to encompass spouses, adult children, and others who served.7
In a similar display of altruism this Memorial Day, veterans service organizations, Boy Scouts, and volunteers will place a flag on every grave to show that some memories are stronger than death. If you have never seen it, I encourage you to visit a VA or a national cemetery this holiday or, even better, volunteer to place flags. Either way, spend a few moments thankfully remembering that we can all engage in those uniquely American Memorial Day pastimes of barbecues and baseball games because so many served and died to protect our way of life. The epigraph at the beginning of this column is attributed to Albert Schweitzer, the physician-theologian of reverence for life. The news today is full of war and rumors of war.8 Let us all hope that the message is heard around the world so there is no need to build more national cemeteries to remember our veterans.
1. Cohen R. On Omaha Beach today, where’s the comradeship? The New York Times. June 5, 2024. Accessed April 26, 2024. https://www.nytimes.com/2004/06/05/world/on-omaha-beach-today-where-s-the-comradeship.html
2. Stillwell B. ‘How decoration day’ became memorial day. Military.com. Published May 12, 2020. Accessed April 26, 2024. https://www.military.com/holidays/memorial-day/how-decoration-day-became-memorial-day.html
3. The history of Memorial Day. PBS. Accessed April 26, 2024. https://www.pbs.org/national-memorial-day-concert/memorial-day/history/
4. US Department of Veterans Affairs, National Cemetery Administration. Facts: NCA history and development. Updated October 18, 2023. Accessed April 26, 2024. https://www.cem.va.gov/facts/NCA_History_and_Development_1.asp
5. Lerer L. How the movie ‘civil war’ echoes real political anxieties. The New York Times. April 21, 2024. Accessed April 26, 2024. https://www.nytimes.com/2024/04/21/us/politics/civil-war-movie-politics.html
6. VA’s national cemetery administration dedicates new headstones to honor black soldiers, correcting 1917 injustice. News release. US Department of Veterans Affairs. Published February 22, 2024. Accessed April 26, 2024. https://news.va.gov/press-room/va-headstones-black-soldiers-1917-injustice/
7. US Department of Veterans Affairs, National Cemetery Administration. Burial benefits. Updated September 27, 2023. Accessed April 26, 2024. https://www.cem.va.gov/burial_benefits/
8. Racker M. Why so many politicians are talking about world war III. Time. November 20, 2023. Accessed April 29, 2024. https://time.com/6336897/israel-war-gaza-world-war-iii/
Soldiers’ graves are the greatest preachers of peace.
Albert Schweitzer 1
From the window of my room in the house where I grew up, I could see the American flag flying over Fort Sam Houston National Cemetery. I would ride my bicycle around the paths that divided the grassy sections of graves to the blocks where my father and grandfather were buried. I would stand before the gravesites in a state combining prayer, processing, and remembrance. Carved into my grandfather’s headstone were the 2 world wars he fought in and on my father’s, the 3 conflicts in which he served. I would walk up to their headstones and trace the emblems of belief: the engraved Star of David that marked my grandfather’s grave and the simple cross for my father.
My visits and writing about them may strike some readers as morbid. However, for me, the experience and memories are calming and peaceful, like the cemetery. There was something incredibly comforting about the uniformity of the headstones standing out for miles, mirroring the ranks of soldiers in the wars they commemorated. Yet, as with the men and women who fought each conflict, every grave told a succinct Hemingway-like story of their military career etched in stone. I know now that discrimination in the military segregated even the burial of service members.2 It appeared to my younger self that at least compared to civilian cemeteries with their massive monuments to the wealthy and powerful, there was an egalitarian effect: my master sergeant grandfather’s plot was indistinguishable from that of my colonel father.
Memorial Day and military cemeteries have a shared history. While Veterans Day honors all who have worn the uniform, living and dead, Memorial Day, as its name suggests, remembers those who have died in a broadly conceived line of duty. To emphasize the more solemn character of the holiday, the original name, Decoration Day, was changed to emphasize the reverence of remembrance.3 The first widespread observance of Memorial Day was to commemorate those who perished in the Civil War, which remains the conflict with the highest number of casualties in American history. The first national commemoration occurred at Arlington National Cemetery when 5000 volunteers decorated 20,000 Union and Confederate graves in an act of solidarity and reconciliation. The practice struck a chord in a country beleaguered by war and division.2
National cemeteries also emerged from the grief and gratitude that marked the Civil War. President Abraham Lincoln, who gave us the famous US Department of Veterans Affairs (VA) mission motto, also inaugurated national cemeteries. At the beginning of the Civil War, only Union soldiers who sacrificed their lives to end slavery were entitled to burial. Reflective of the rift that divided the country, Confederate soldiers contended that such divisiveness should not continue unto death and were granted the right to be buried beside those they fought against, united in death and memory.4
Today, the country is more divided than ever: more than a few observers of American culture, including the new popular film Civil War, believe we are on the brink of another civil war.5 While we take their warning seriously, there are still signs of unity amongst the people, like those who followed the war between the states. Recently, in that same national cemetery where I first contemplated these themes, justice, delayed too long, was not entirely denied. A ceremony was held to dedicate 17 headstones to honor the memories of Black World War I Army soldiers who were court-martialed and hanged in the wake of the Houston riots of 1917. As a sign of their dishonor, their headstones listed only their dates and names—nothing of their military service. At the urging of their descendants, the US Army reopened the files and found the verdict to have been racially motivated. They set aside their convictions, gave them honorable discharges for their service in life, and replaced their gravesites with ones that enshrined that respect in death.6
Some reading this column may, like me, have had the profound privilege of participating in a burial at a national cemetery. We recall the stirring mix of pride and loss when the honor guard hands the perfectly folded flag to the bereaved family member and bids farewell to their comrade with a salute. Yet, not all families have this privilege. One of the saddest experiences I recall is when I was in a leadership position at a VA facility and unable to help impoverished families who were denied VA burial benefits or payments to transport their deceased veteran closer to home. That sorrow often turned to thankful relief when a veterans service organization or other community group offered to pay the funerary expenses. Fortunately, like eligibility for VA health care, the criteria for burial benefits have steadily expanded to encompass spouses, adult children, and others who served.7
In a similar display of altruism this Memorial Day, veterans service organizations, Boy Scouts, and volunteers will place a flag on every grave to show that some memories are stronger than death. If you have never seen it, I encourage you to visit a VA or a national cemetery this holiday or, even better, volunteer to place flags. Either way, spend a few moments thankfully remembering that we can all engage in those uniquely American Memorial Day pastimes of barbecues and baseball games because so many served and died to protect our way of life. The epigraph at the beginning of this column is attributed to Albert Schweitzer, the physician-theologian of reverence for life. The news today is full of war and rumors of war.8 Let us all hope that the message is heard around the world so there is no need to build more national cemeteries to remember our veterans.
Soldiers’ graves are the greatest preachers of peace.
Albert Schweitzer 1
From the window of my room in the house where I grew up, I could see the American flag flying over Fort Sam Houston National Cemetery. I would ride my bicycle around the paths that divided the grassy sections of graves to the blocks where my father and grandfather were buried. I would stand before the gravesites in a state combining prayer, processing, and remembrance. Carved into my grandfather’s headstone were the 2 world wars he fought in and on my father’s, the 3 conflicts in which he served. I would walk up to their headstones and trace the emblems of belief: the engraved Star of David that marked my grandfather’s grave and the simple cross for my father.
My visits and writing about them may strike some readers as morbid. However, for me, the experience and memories are calming and peaceful, like the cemetery. There was something incredibly comforting about the uniformity of the headstones standing out for miles, mirroring the ranks of soldiers in the wars they commemorated. Yet, as with the men and women who fought each conflict, every grave told a succinct Hemingway-like story of their military career etched in stone. I know now that discrimination in the military segregated even the burial of service members.2 It appeared to my younger self that at least compared to civilian cemeteries with their massive monuments to the wealthy and powerful, there was an egalitarian effect: my master sergeant grandfather’s plot was indistinguishable from that of my colonel father.
Memorial Day and military cemeteries have a shared history. While Veterans Day honors all who have worn the uniform, living and dead, Memorial Day, as its name suggests, remembers those who have died in a broadly conceived line of duty. To emphasize the more solemn character of the holiday, the original name, Decoration Day, was changed to emphasize the reverence of remembrance.3 The first widespread observance of Memorial Day was to commemorate those who perished in the Civil War, which remains the conflict with the highest number of casualties in American history. The first national commemoration occurred at Arlington National Cemetery when 5000 volunteers decorated 20,000 Union and Confederate graves in an act of solidarity and reconciliation. The practice struck a chord in a country beleaguered by war and division.2
National cemeteries also emerged from the grief and gratitude that marked the Civil War. President Abraham Lincoln, who gave us the famous US Department of Veterans Affairs (VA) mission motto, also inaugurated national cemeteries. At the beginning of the Civil War, only Union soldiers who sacrificed their lives to end slavery were entitled to burial. Reflective of the rift that divided the country, Confederate soldiers contended that such divisiveness should not continue unto death and were granted the right to be buried beside those they fought against, united in death and memory.4
Today, the country is more divided than ever: more than a few observers of American culture, including the new popular film Civil War, believe we are on the brink of another civil war.5 While we take their warning seriously, there are still signs of unity amongst the people, like those who followed the war between the states. Recently, in that same national cemetery where I first contemplated these themes, justice, delayed too long, was not entirely denied. A ceremony was held to dedicate 17 headstones to honor the memories of Black World War I Army soldiers who were court-martialed and hanged in the wake of the Houston riots of 1917. As a sign of their dishonor, their headstones listed only their dates and names—nothing of their military service. At the urging of their descendants, the US Army reopened the files and found the verdict to have been racially motivated. They set aside their convictions, gave them honorable discharges for their service in life, and replaced their gravesites with ones that enshrined that respect in death.6
Some reading this column may, like me, have had the profound privilege of participating in a burial at a national cemetery. We recall the stirring mix of pride and loss when the honor guard hands the perfectly folded flag to the bereaved family member and bids farewell to their comrade with a salute. Yet, not all families have this privilege. One of the saddest experiences I recall is when I was in a leadership position at a VA facility and unable to help impoverished families who were denied VA burial benefits or payments to transport their deceased veteran closer to home. That sorrow often turned to thankful relief when a veterans service organization or other community group offered to pay the funerary expenses. Fortunately, like eligibility for VA health care, the criteria for burial benefits have steadily expanded to encompass spouses, adult children, and others who served.7
In a similar display of altruism this Memorial Day, veterans service organizations, Boy Scouts, and volunteers will place a flag on every grave to show that some memories are stronger than death. If you have never seen it, I encourage you to visit a VA or a national cemetery this holiday or, even better, volunteer to place flags. Either way, spend a few moments thankfully remembering that we can all engage in those uniquely American Memorial Day pastimes of barbecues and baseball games because so many served and died to protect our way of life. The epigraph at the beginning of this column is attributed to Albert Schweitzer, the physician-theologian of reverence for life. The news today is full of war and rumors of war.8 Let us all hope that the message is heard around the world so there is no need to build more national cemeteries to remember our veterans.
1. Cohen R. On Omaha Beach today, where’s the comradeship? The New York Times. June 5, 2024. Accessed April 26, 2024. https://www.nytimes.com/2004/06/05/world/on-omaha-beach-today-where-s-the-comradeship.html
2. Stillwell B. ‘How decoration day’ became memorial day. Military.com. Published May 12, 2020. Accessed April 26, 2024. https://www.military.com/holidays/memorial-day/how-decoration-day-became-memorial-day.html
3. The history of Memorial Day. PBS. Accessed April 26, 2024. https://www.pbs.org/national-memorial-day-concert/memorial-day/history/
4. US Department of Veterans Affairs, National Cemetery Administration. Facts: NCA history and development. Updated October 18, 2023. Accessed April 26, 2024. https://www.cem.va.gov/facts/NCA_History_and_Development_1.asp
5. Lerer L. How the movie ‘civil war’ echoes real political anxieties. The New York Times. April 21, 2024. Accessed April 26, 2024. https://www.nytimes.com/2024/04/21/us/politics/civil-war-movie-politics.html
6. VA’s national cemetery administration dedicates new headstones to honor black soldiers, correcting 1917 injustice. News release. US Department of Veterans Affairs. Published February 22, 2024. Accessed April 26, 2024. https://news.va.gov/press-room/va-headstones-black-soldiers-1917-injustice/
7. US Department of Veterans Affairs, National Cemetery Administration. Burial benefits. Updated September 27, 2023. Accessed April 26, 2024. https://www.cem.va.gov/burial_benefits/
8. Racker M. Why so many politicians are talking about world war III. Time. November 20, 2023. Accessed April 29, 2024. https://time.com/6336897/israel-war-gaza-world-war-iii/
1. Cohen R. On Omaha Beach today, where’s the comradeship? The New York Times. June 5, 2024. Accessed April 26, 2024. https://www.nytimes.com/2004/06/05/world/on-omaha-beach-today-where-s-the-comradeship.html
2. Stillwell B. ‘How decoration day’ became memorial day. Military.com. Published May 12, 2020. Accessed April 26, 2024. https://www.military.com/holidays/memorial-day/how-decoration-day-became-memorial-day.html
3. The history of Memorial Day. PBS. Accessed April 26, 2024. https://www.pbs.org/national-memorial-day-concert/memorial-day/history/
4. US Department of Veterans Affairs, National Cemetery Administration. Facts: NCA history and development. Updated October 18, 2023. Accessed April 26, 2024. https://www.cem.va.gov/facts/NCA_History_and_Development_1.asp
5. Lerer L. How the movie ‘civil war’ echoes real political anxieties. The New York Times. April 21, 2024. Accessed April 26, 2024. https://www.nytimes.com/2024/04/21/us/politics/civil-war-movie-politics.html
6. VA’s national cemetery administration dedicates new headstones to honor black soldiers, correcting 1917 injustice. News release. US Department of Veterans Affairs. Published February 22, 2024. Accessed April 26, 2024. https://news.va.gov/press-room/va-headstones-black-soldiers-1917-injustice/
7. US Department of Veterans Affairs, National Cemetery Administration. Burial benefits. Updated September 27, 2023. Accessed April 26, 2024. https://www.cem.va.gov/burial_benefits/
8. Racker M. Why so many politicians are talking about world war III. Time. November 20, 2023. Accessed April 29, 2024. https://time.com/6336897/israel-war-gaza-world-war-iii/
A Structured Approach for the Management of Orodynia (Burning Mouth Syndrome)
Practice Gap
Orodynia (OD)—together with glossodynia colloquially termed “burning mouth syndrome”—is a chronic disorder characterized by a burning sensation within the oral cavity without objective clinical signs. It is most common in perimenopausal and postmenopausal women.1,2
Orodynia is a diagnosis of exclusion and is considered after 4 to 6 months of normal imaging and laboratory test results.1,2 Its pathophysiology is poorly understood, as it can be intermittent or continuous, manifest with a variety of symptoms, and affect various entities of the oral cavity.3,4 The most common structure affected is the tongue, and symptoms may include xerostomia, dysgeusia, and discomfort.1,2 Orodynia is a frustrating condition, as many patients do not respond to treatment and experience symptoms for years.1-4
The current approach to management of OD typically involves a combination of psychosocial strategies and pharmacologic agents. The psychosocial component consists of coping mechanisms (eg, stress management techniques and behavioral therapies) aimed at alleviating the psychological impact of the condition. Pharmacologic agents such as antidepressants, anticonvulsants, and topical medications often are prescribed to address neuropathic pain and dry mouth symptoms.1,2 Additionally, oral rinses, saliva substitutes, and dietary supplements may be recommended to counteract the discomfort associated with xerostomia.1,2 However, there is no stepwise protocol, leaving these treatments to be trialed in a disorganized manner.2
The Tools
In our unique approach to managing OD, physicians may employ a variety of tools, including autoantibody profiles, noninvasive salivary gland analysis, saliva analysis, patch testing for allergens, and—if deemed necessary—a minor salivary gland biopsy. The use of specific prescription medications is included in the later stages of our approach.
The Technique
First, exclude inflammatory conditions such as geographic tongue, oral lichen planus, autoimmune bullous disorders, and other treatable conditions such as dyspepsia and Sjögren syndrome using the tools described above. Noninvasive modalities should be exhausted first, and dermatologists/clinicians should exercise clinical judgement to determine whether all options should be trialed, including more invasive/costly ones.
If symptoms persist, clinicians may want to obtain a culture for oral candida. If results are positive, candida may be treated quickly with oral fluconazole. If that treatment fails and fissuring is present, advise the patient on treating the tongue; we recommend lightly brushing the tongue once daily with a hydrogen peroxide 3% solution, followed by rinsing. Next, the patient can allow an active probiotic yogurt to sit on the tongue for at least 1 minute to repopulate it with healthy oral bacteria.
If symptoms persist, prescribe gabapentin 100 to 300 mg to be taken at bedtime. Cevimeline 30 mg 3 times daily can be added to treat symptoms of xerostomia. As a last resort, a low daily dose of trifluoperazine 1 to 2 mg may alleviate the dysesthesia of OD. Because this medication is an antipsychotic, there is an increased risk for adverse effects such as tardive dyskinesia; however, given that we recommend using at most one-twentieth of the dose recommended for psychiatric illnesses such as schizophrenia, the risk appears to be minimal.5
We have found this protocol to be more structured, and in our practice, it has led to better outcomes than previously described therapeutic interventions.
Practice Implications
As a chronic condition, OD can be frustrating for patients, as many of them have attempted multiple treatments without success. It also may be challenging for dermatologists who are unfamiliar with its management. This approach to OD provides simple step-by-step diagnostic and therapeutic plans for a condition with an often-uncertain etiology and stubborn response to initial treatments. By following this protocol, dermatologists can be confident in their ability to help patients find relief from OD.
- Klein B, Thoppay JR, De Rossi SS, et al. Burning mouth syndrome. Dermatol Clin. 2020;38:477-483. doi:10.1016/j.det.2020.05.008
- Bender SD. Burning mouth syndrome. Dent Clin North Am. 2018;62:585-596. doi:10.1016/j.cden.2018.05.006
- Javali MA. Burning mouth syndrome: an enigmatic disorder. Kathmandu Univ Med J. 2013;11:175-178. doi:10.3126/kumj.v11i2.12498
- Sardella A, Lodi G, Demarosi F, et al. Burning mouth syndrome: a retrospective study investigating spontaneous remission and response to treatments. Oral Dis. 2006;12:152-155. doi:10.1111/j.1601-0825.2005.01174
- Macdonald R, Watts TP. Trifluoperazine dihydrochloride (stelazine) in paranoid schizophrenia. Br Med J. 1959;1:549-550. doi:10.1136/bmj.1.5121.549
Practice Gap
Orodynia (OD)—together with glossodynia colloquially termed “burning mouth syndrome”—is a chronic disorder characterized by a burning sensation within the oral cavity without objective clinical signs. It is most common in perimenopausal and postmenopausal women.1,2
Orodynia is a diagnosis of exclusion and is considered after 4 to 6 months of normal imaging and laboratory test results.1,2 Its pathophysiology is poorly understood, as it can be intermittent or continuous, manifest with a variety of symptoms, and affect various entities of the oral cavity.3,4 The most common structure affected is the tongue, and symptoms may include xerostomia, dysgeusia, and discomfort.1,2 Orodynia is a frustrating condition, as many patients do not respond to treatment and experience symptoms for years.1-4
The current approach to management of OD typically involves a combination of psychosocial strategies and pharmacologic agents. The psychosocial component consists of coping mechanisms (eg, stress management techniques and behavioral therapies) aimed at alleviating the psychological impact of the condition. Pharmacologic agents such as antidepressants, anticonvulsants, and topical medications often are prescribed to address neuropathic pain and dry mouth symptoms.1,2 Additionally, oral rinses, saliva substitutes, and dietary supplements may be recommended to counteract the discomfort associated with xerostomia.1,2 However, there is no stepwise protocol, leaving these treatments to be trialed in a disorganized manner.2
The Tools
In our unique approach to managing OD, physicians may employ a variety of tools, including autoantibody profiles, noninvasive salivary gland analysis, saliva analysis, patch testing for allergens, and—if deemed necessary—a minor salivary gland biopsy. The use of specific prescription medications is included in the later stages of our approach.
The Technique
First, exclude inflammatory conditions such as geographic tongue, oral lichen planus, autoimmune bullous disorders, and other treatable conditions such as dyspepsia and Sjögren syndrome using the tools described above. Noninvasive modalities should be exhausted first, and dermatologists/clinicians should exercise clinical judgement to determine whether all options should be trialed, including more invasive/costly ones.
If symptoms persist, clinicians may want to obtain a culture for oral candida. If results are positive, candida may be treated quickly with oral fluconazole. If that treatment fails and fissuring is present, advise the patient on treating the tongue; we recommend lightly brushing the tongue once daily with a hydrogen peroxide 3% solution, followed by rinsing. Next, the patient can allow an active probiotic yogurt to sit on the tongue for at least 1 minute to repopulate it with healthy oral bacteria.
If symptoms persist, prescribe gabapentin 100 to 300 mg to be taken at bedtime. Cevimeline 30 mg 3 times daily can be added to treat symptoms of xerostomia. As a last resort, a low daily dose of trifluoperazine 1 to 2 mg may alleviate the dysesthesia of OD. Because this medication is an antipsychotic, there is an increased risk for adverse effects such as tardive dyskinesia; however, given that we recommend using at most one-twentieth of the dose recommended for psychiatric illnesses such as schizophrenia, the risk appears to be minimal.5
We have found this protocol to be more structured, and in our practice, it has led to better outcomes than previously described therapeutic interventions.
Practice Implications
As a chronic condition, OD can be frustrating for patients, as many of them have attempted multiple treatments without success. It also may be challenging for dermatologists who are unfamiliar with its management. This approach to OD provides simple step-by-step diagnostic and therapeutic plans for a condition with an often-uncertain etiology and stubborn response to initial treatments. By following this protocol, dermatologists can be confident in their ability to help patients find relief from OD.
Practice Gap
Orodynia (OD)—together with glossodynia colloquially termed “burning mouth syndrome”—is a chronic disorder characterized by a burning sensation within the oral cavity without objective clinical signs. It is most common in perimenopausal and postmenopausal women.1,2
Orodynia is a diagnosis of exclusion and is considered after 4 to 6 months of normal imaging and laboratory test results.1,2 Its pathophysiology is poorly understood, as it can be intermittent or continuous, manifest with a variety of symptoms, and affect various entities of the oral cavity.3,4 The most common structure affected is the tongue, and symptoms may include xerostomia, dysgeusia, and discomfort.1,2 Orodynia is a frustrating condition, as many patients do not respond to treatment and experience symptoms for years.1-4
The current approach to management of OD typically involves a combination of psychosocial strategies and pharmacologic agents. The psychosocial component consists of coping mechanisms (eg, stress management techniques and behavioral therapies) aimed at alleviating the psychological impact of the condition. Pharmacologic agents such as antidepressants, anticonvulsants, and topical medications often are prescribed to address neuropathic pain and dry mouth symptoms.1,2 Additionally, oral rinses, saliva substitutes, and dietary supplements may be recommended to counteract the discomfort associated with xerostomia.1,2 However, there is no stepwise protocol, leaving these treatments to be trialed in a disorganized manner.2
The Tools
In our unique approach to managing OD, physicians may employ a variety of tools, including autoantibody profiles, noninvasive salivary gland analysis, saliva analysis, patch testing for allergens, and—if deemed necessary—a minor salivary gland biopsy. The use of specific prescription medications is included in the later stages of our approach.
The Technique
First, exclude inflammatory conditions such as geographic tongue, oral lichen planus, autoimmune bullous disorders, and other treatable conditions such as dyspepsia and Sjögren syndrome using the tools described above. Noninvasive modalities should be exhausted first, and dermatologists/clinicians should exercise clinical judgement to determine whether all options should be trialed, including more invasive/costly ones.
If symptoms persist, clinicians may want to obtain a culture for oral candida. If results are positive, candida may be treated quickly with oral fluconazole. If that treatment fails and fissuring is present, advise the patient on treating the tongue; we recommend lightly brushing the tongue once daily with a hydrogen peroxide 3% solution, followed by rinsing. Next, the patient can allow an active probiotic yogurt to sit on the tongue for at least 1 minute to repopulate it with healthy oral bacteria.
If symptoms persist, prescribe gabapentin 100 to 300 mg to be taken at bedtime. Cevimeline 30 mg 3 times daily can be added to treat symptoms of xerostomia. As a last resort, a low daily dose of trifluoperazine 1 to 2 mg may alleviate the dysesthesia of OD. Because this medication is an antipsychotic, there is an increased risk for adverse effects such as tardive dyskinesia; however, given that we recommend using at most one-twentieth of the dose recommended for psychiatric illnesses such as schizophrenia, the risk appears to be minimal.5
We have found this protocol to be more structured, and in our practice, it has led to better outcomes than previously described therapeutic interventions.
Practice Implications
As a chronic condition, OD can be frustrating for patients, as many of them have attempted multiple treatments without success. It also may be challenging for dermatologists who are unfamiliar with its management. This approach to OD provides simple step-by-step diagnostic and therapeutic plans for a condition with an often-uncertain etiology and stubborn response to initial treatments. By following this protocol, dermatologists can be confident in their ability to help patients find relief from OD.
- Klein B, Thoppay JR, De Rossi SS, et al. Burning mouth syndrome. Dermatol Clin. 2020;38:477-483. doi:10.1016/j.det.2020.05.008
- Bender SD. Burning mouth syndrome. Dent Clin North Am. 2018;62:585-596. doi:10.1016/j.cden.2018.05.006
- Javali MA. Burning mouth syndrome: an enigmatic disorder. Kathmandu Univ Med J. 2013;11:175-178. doi:10.3126/kumj.v11i2.12498
- Sardella A, Lodi G, Demarosi F, et al. Burning mouth syndrome: a retrospective study investigating spontaneous remission and response to treatments. Oral Dis. 2006;12:152-155. doi:10.1111/j.1601-0825.2005.01174
- Macdonald R, Watts TP. Trifluoperazine dihydrochloride (stelazine) in paranoid schizophrenia. Br Med J. 1959;1:549-550. doi:10.1136/bmj.1.5121.549
- Klein B, Thoppay JR, De Rossi SS, et al. Burning mouth syndrome. Dermatol Clin. 2020;38:477-483. doi:10.1016/j.det.2020.05.008
- Bender SD. Burning mouth syndrome. Dent Clin North Am. 2018;62:585-596. doi:10.1016/j.cden.2018.05.006
- Javali MA. Burning mouth syndrome: an enigmatic disorder. Kathmandu Univ Med J. 2013;11:175-178. doi:10.3126/kumj.v11i2.12498
- Sardella A, Lodi G, Demarosi F, et al. Burning mouth syndrome: a retrospective study investigating spontaneous remission and response to treatments. Oral Dis. 2006;12:152-155. doi:10.1111/j.1601-0825.2005.01174
- Macdonald R, Watts TP. Trifluoperazine dihydrochloride (stelazine) in paranoid schizophrenia. Br Med J. 1959;1:549-550. doi:10.1136/bmj.1.5121.549