User login
For MD-IQ use only
Preemptive CMV monitoring beats prophylaxis post liver transplant
Preemptive monitoring and treatment of cytomegalovirus infections in CMV-seronegative liver transplant recipients who receive organs from CMV-positive donors appears to be better at preventing infections than a viral prophylaxis strategy, according to infectious disease and organ transplant specialists.
In a study published in JAMA that may have gotten scant notice because of its publication during the early days of the COVID-19 pandemic, investigators at the University of Pittsburgh and other transplant centers reported results of a randomized clinical trial comparing the two CMV management strategies, and found that the incidence of CMV disease was significantly lower for patients who were started on valganciclovir when asymptomatic CMV viremia was detected, compared with patients on antiviral prophylaxis with valganciclovir.
The study “is a significant game changer for the field of transplantation,” commented Michael G. Ison, MD, professor of infectious diseases and organ transplantation at Northwestern University, Chicago.
Dr. Ison discussed the study and its implications during a session on potentially practice-changing clinical trials presented virtually during IDWeek 2020, an annual scientific meeting on infectious diseases.
In the trial, Nina Singh, MD, and colleagues randomly assigned 100 CMV-seronegative liver transplant recipients to receive preemptive therapy, in which patients underwent weekly testing for 100 days with a highly sensitive real-time plasma polymerase chain reaction assay for CMV. If viremia at any level was detected, the patients received oral valganciclovir 900 mg twice daily until two consecutive tests performed 1 week apart came back negative.
The remaining 105 patients were randomly assigned to 100 days of oral prophylaxis with 900 mg valganciclovir twice daily, started within 10 days of transplant.
CMV disease incidence lower
The incidence of CMV disease within 12 months of transplants, the primary outcome, was 9% in the preemptive therapy group, compared with 19% in the prophylaxis group (P = .04)
The difference between the groups was largely accounted for by a reduction in disease onset beyond 100 days in the preemptive therapy group (6% vs. 17%, respectively, P = .01)
There were no significant differences in secondary endpoints of rejection, opportunistic infections, graft loss because of retransplantation, neutropenia, or receipt of one or more doses of granulocyte colony–stimulating factor for the management of neutropenia.
At 1-year follow-up, the incidence of all-cause mortality was 15% in the preemptive therapy group, and 19% in the prophylaxis group; the difference was not statistically significant.
“While most transplant centers utilize universal prophylaxis, I think that this study really suggests that preemptive monitoring, if it can be safely accomplished at your center, may be of the greatest benefit to your patients,” Dr. Ison said.
He noted that Singh et al. also looked in an exploratory analysis at CMV-specific immunity and observed that patients assigned to preemptive therapy “clearly had better CMV-specific immunity, whether CD4 or CD8 cells, and had higher lymphocyte numbers than those patients that had received universal prophylaxis.”
In a comment, Sarah Doernberg, MD, from the division of infectious diseases at the University of California, San Francisco, agreed that “exploratory analysis of CMV-specific immune responses suggested increased CMV-specific immunity in those in the preemptive group, a finding that warrants further study. The feasibility of adopting reliable preemptive monitoring must be considered as individual centers ponder adopting this approach.”
Dr. Doernberg moderated the session where Dr. Ison discussed the data, but was not involved in the research.
The study by Singh et al. was supported by the National Institutes of Health. Dr. Singh reported research grants from NIH. Dr. Ison disclosed research support and paid consultation for several companies. Dr. Doernberg disclosed consulting for Basilea and Genentech.
Preemptive monitoring and treatment of cytomegalovirus infections in CMV-seronegative liver transplant recipients who receive organs from CMV-positive donors appears to be better at preventing infections than a viral prophylaxis strategy, according to infectious disease and organ transplant specialists.
In a study published in JAMA that may have gotten scant notice because of its publication during the early days of the COVID-19 pandemic, investigators at the University of Pittsburgh and other transplant centers reported results of a randomized clinical trial comparing the two CMV management strategies, and found that the incidence of CMV disease was significantly lower for patients who were started on valganciclovir when asymptomatic CMV viremia was detected, compared with patients on antiviral prophylaxis with valganciclovir.
The study “is a significant game changer for the field of transplantation,” commented Michael G. Ison, MD, professor of infectious diseases and organ transplantation at Northwestern University, Chicago.
Dr. Ison discussed the study and its implications during a session on potentially practice-changing clinical trials presented virtually during IDWeek 2020, an annual scientific meeting on infectious diseases.
In the trial, Nina Singh, MD, and colleagues randomly assigned 100 CMV-seronegative liver transplant recipients to receive preemptive therapy, in which patients underwent weekly testing for 100 days with a highly sensitive real-time plasma polymerase chain reaction assay for CMV. If viremia at any level was detected, the patients received oral valganciclovir 900 mg twice daily until two consecutive tests performed 1 week apart came back negative.
The remaining 105 patients were randomly assigned to 100 days of oral prophylaxis with 900 mg valganciclovir twice daily, started within 10 days of transplant.
CMV disease incidence lower
The incidence of CMV disease within 12 months of transplants, the primary outcome, was 9% in the preemptive therapy group, compared with 19% in the prophylaxis group (P = .04)
The difference between the groups was largely accounted for by a reduction in disease onset beyond 100 days in the preemptive therapy group (6% vs. 17%, respectively, P = .01)
There were no significant differences in secondary endpoints of rejection, opportunistic infections, graft loss because of retransplantation, neutropenia, or receipt of one or more doses of granulocyte colony–stimulating factor for the management of neutropenia.
At 1-year follow-up, the incidence of all-cause mortality was 15% in the preemptive therapy group, and 19% in the prophylaxis group; the difference was not statistically significant.
“While most transplant centers utilize universal prophylaxis, I think that this study really suggests that preemptive monitoring, if it can be safely accomplished at your center, may be of the greatest benefit to your patients,” Dr. Ison said.
He noted that Singh et al. also looked in an exploratory analysis at CMV-specific immunity and observed that patients assigned to preemptive therapy “clearly had better CMV-specific immunity, whether CD4 or CD8 cells, and had higher lymphocyte numbers than those patients that had received universal prophylaxis.”
In a comment, Sarah Doernberg, MD, from the division of infectious diseases at the University of California, San Francisco, agreed that “exploratory analysis of CMV-specific immune responses suggested increased CMV-specific immunity in those in the preemptive group, a finding that warrants further study. The feasibility of adopting reliable preemptive monitoring must be considered as individual centers ponder adopting this approach.”
Dr. Doernberg moderated the session where Dr. Ison discussed the data, but was not involved in the research.
The study by Singh et al. was supported by the National Institutes of Health. Dr. Singh reported research grants from NIH. Dr. Ison disclosed research support and paid consultation for several companies. Dr. Doernberg disclosed consulting for Basilea and Genentech.
Preemptive monitoring and treatment of cytomegalovirus infections in CMV-seronegative liver transplant recipients who receive organs from CMV-positive donors appears to be better at preventing infections than a viral prophylaxis strategy, according to infectious disease and organ transplant specialists.
In a study published in JAMA that may have gotten scant notice because of its publication during the early days of the COVID-19 pandemic, investigators at the University of Pittsburgh and other transplant centers reported results of a randomized clinical trial comparing the two CMV management strategies, and found that the incidence of CMV disease was significantly lower for patients who were started on valganciclovir when asymptomatic CMV viremia was detected, compared with patients on antiviral prophylaxis with valganciclovir.
The study “is a significant game changer for the field of transplantation,” commented Michael G. Ison, MD, professor of infectious diseases and organ transplantation at Northwestern University, Chicago.
Dr. Ison discussed the study and its implications during a session on potentially practice-changing clinical trials presented virtually during IDWeek 2020, an annual scientific meeting on infectious diseases.
In the trial, Nina Singh, MD, and colleagues randomly assigned 100 CMV-seronegative liver transplant recipients to receive preemptive therapy, in which patients underwent weekly testing for 100 days with a highly sensitive real-time plasma polymerase chain reaction assay for CMV. If viremia at any level was detected, the patients received oral valganciclovir 900 mg twice daily until two consecutive tests performed 1 week apart came back negative.
The remaining 105 patients were randomly assigned to 100 days of oral prophylaxis with 900 mg valganciclovir twice daily, started within 10 days of transplant.
CMV disease incidence lower
The incidence of CMV disease within 12 months of transplants, the primary outcome, was 9% in the preemptive therapy group, compared with 19% in the prophylaxis group (P = .04)
The difference between the groups was largely accounted for by a reduction in disease onset beyond 100 days in the preemptive therapy group (6% vs. 17%, respectively, P = .01)
There were no significant differences in secondary endpoints of rejection, opportunistic infections, graft loss because of retransplantation, neutropenia, or receipt of one or more doses of granulocyte colony–stimulating factor for the management of neutropenia.
At 1-year follow-up, the incidence of all-cause mortality was 15% in the preemptive therapy group, and 19% in the prophylaxis group; the difference was not statistically significant.
“While most transplant centers utilize universal prophylaxis, I think that this study really suggests that preemptive monitoring, if it can be safely accomplished at your center, may be of the greatest benefit to your patients,” Dr. Ison said.
He noted that Singh et al. also looked in an exploratory analysis at CMV-specific immunity and observed that patients assigned to preemptive therapy “clearly had better CMV-specific immunity, whether CD4 or CD8 cells, and had higher lymphocyte numbers than those patients that had received universal prophylaxis.”
In a comment, Sarah Doernberg, MD, from the division of infectious diseases at the University of California, San Francisco, agreed that “exploratory analysis of CMV-specific immune responses suggested increased CMV-specific immunity in those in the preemptive group, a finding that warrants further study. The feasibility of adopting reliable preemptive monitoring must be considered as individual centers ponder adopting this approach.”
Dr. Doernberg moderated the session where Dr. Ison discussed the data, but was not involved in the research.
The study by Singh et al. was supported by the National Institutes of Health. Dr. Singh reported research grants from NIH. Dr. Ison disclosed research support and paid consultation for several companies. Dr. Doernberg disclosed consulting for Basilea and Genentech.
FROM IDWEEK 2020
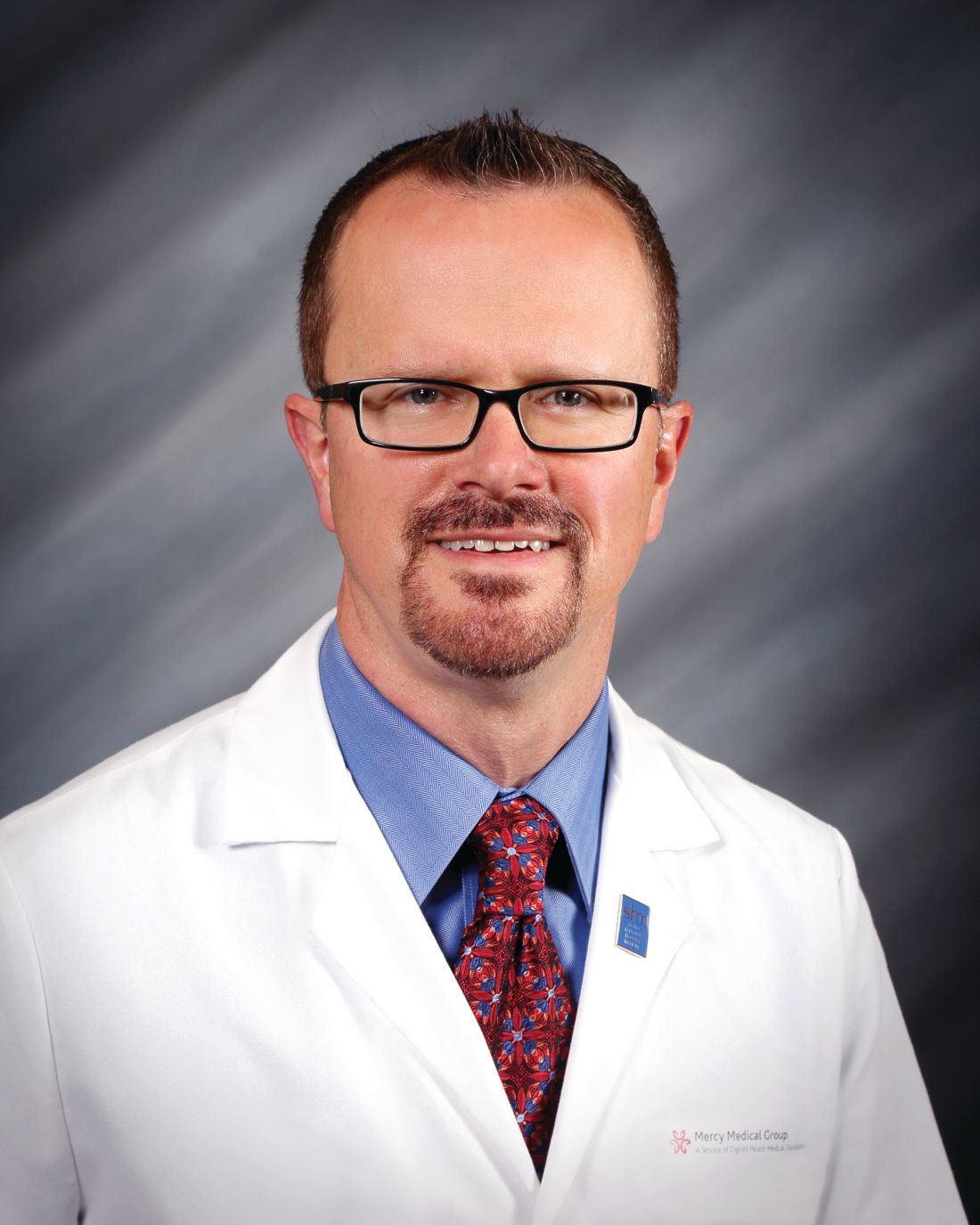
Health sector has spent $464 million on lobbying in 2020
, according to the Center for Responsive Politics.
PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
, according to the Center for Responsive Politics.
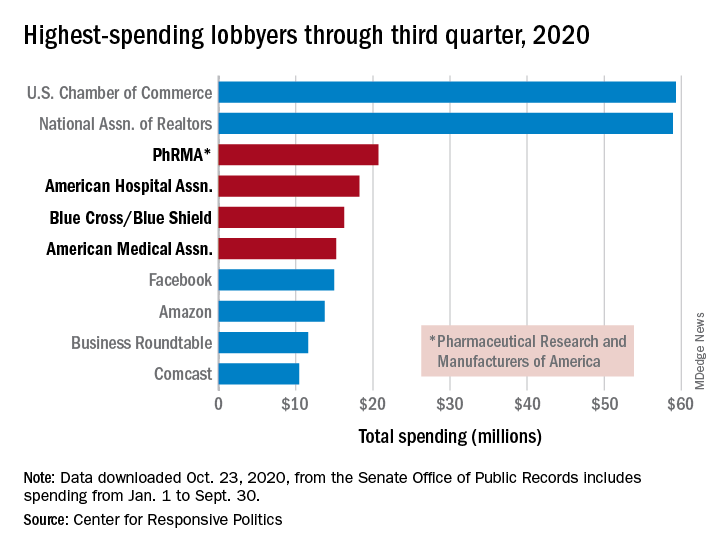
PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
, according to the Center for Responsive Politics.
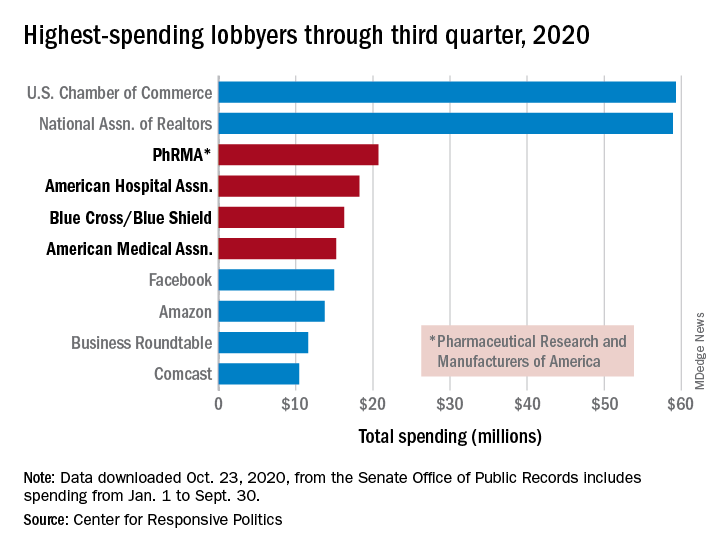
PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
Physician burnout costly to organizations and U.S. health system
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Web-based interviews, financial planning in a pandemic, and more
Dear colleagues,
I’m excited to introduce the November issue of The New Gastroenterologist – the last edition of 2020 features a fantastic line-up of articles! As the year comes to a close, we reflect on what has certainly been an interesting year, defined by a set of unique challenges we have faced as a nation and as a specialty.
The fellowship recruitment season is one that has looked starkly different as interviews have converted to a virtual format. Dr. Wissam Khan, Dr. Nada Al Masalmeh, Dr. Stephanie Judd, and Dr. Diane Levine (Wayne State University) compile a helpful list of tips and tricks on proper interview etiquette in the new era of web-based interviews.
Financial planning in the face of a pandemic is a formidable task – Jonathan Tudor (Fidelity Investments) offers valuable advice for gastroenterologists on how to remain secure in your finances even in uncertain circumstances.
This quarter’s “In Focus” feature, written by Dr. Yutaka Tomizawa (University of Washington), is a comprehensive piece elucidating the role of gastroenterologists in the management of gastric cancer. The article reviews the individual risk factors that exist for gastric cancer and provides guidance on how to stratify patients accordingly, which is critical in the ethnically diverse population of the United States.
Keeping a procedure log during fellowship can seem daunting and cumbersome, but it is important. Dr. Houman Rezaizadeh (University of Connecticut) shares his program’s experience with the AGA Procedure Log, a convenient online tracking tool, which can provide accurate and secure documentation of endoscopic procedures performed throughout fellowship.
Dr. Nazia Hasan (North Bay Health Care) and Dr. Allison Schulman (University of Michigan) broach an incredibly important topic: the paucity of women in interventional endoscopy. Dr. Hasan and Dr. Shulman candidly discuss the barriers women face in pursuing this subspecialty and offer practical solutions on how to approach these challenges – a piece that will surely resonate with many young gastroenterologists.
We wrap up our first year of TNG’s ethics series with two cases discussing the utilization of cannabis therapy in inflammatory bowel disease (IBD). Dr. Jami Kinnucan (University of Michigan) and Dr. Arun Swaminath (Lenox Hill Hospital) systematically review existing data on the efficacy of cannabis use in IBD, the risks associated with therapy, and legal implications for both physicians and patients.
Also in this issue is a high-yield clinical review on the endoscopic drainage of pancreatic fluid collections by Dr. Robert Moran and Dr. Joseph Elmunzer (Medical University of South Carolina). Dr. Manol Jovani (Johns Hopkins) teaches us about confounding – a critical concept to keep in mind when evaluating any manuscript. Lastly, our DHPA Private Practice Perspectives article, written by Dr. Mehul Lalani (US Digestive), reviews how quality measures and initiatives are tracked and implemented in private practice.
If you have interest in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Ryan Farrell ([email protected]), managing editor of TNG.
Stay well,
Vijaya L. Rao, MD
Editor in Chief
Assistant Professor of Medicine, University of Chicago, Section of Gastroenterology, Hepatology & Nutrition
Dear colleagues,
I’m excited to introduce the November issue of The New Gastroenterologist – the last edition of 2020 features a fantastic line-up of articles! As the year comes to a close, we reflect on what has certainly been an interesting year, defined by a set of unique challenges we have faced as a nation and as a specialty.
The fellowship recruitment season is one that has looked starkly different as interviews have converted to a virtual format. Dr. Wissam Khan, Dr. Nada Al Masalmeh, Dr. Stephanie Judd, and Dr. Diane Levine (Wayne State University) compile a helpful list of tips and tricks on proper interview etiquette in the new era of web-based interviews.
Financial planning in the face of a pandemic is a formidable task – Jonathan Tudor (Fidelity Investments) offers valuable advice for gastroenterologists on how to remain secure in your finances even in uncertain circumstances.
This quarter’s “In Focus” feature, written by Dr. Yutaka Tomizawa (University of Washington), is a comprehensive piece elucidating the role of gastroenterologists in the management of gastric cancer. The article reviews the individual risk factors that exist for gastric cancer and provides guidance on how to stratify patients accordingly, which is critical in the ethnically diverse population of the United States.
Keeping a procedure log during fellowship can seem daunting and cumbersome, but it is important. Dr. Houman Rezaizadeh (University of Connecticut) shares his program’s experience with the AGA Procedure Log, a convenient online tracking tool, which can provide accurate and secure documentation of endoscopic procedures performed throughout fellowship.
Dr. Nazia Hasan (North Bay Health Care) and Dr. Allison Schulman (University of Michigan) broach an incredibly important topic: the paucity of women in interventional endoscopy. Dr. Hasan and Dr. Shulman candidly discuss the barriers women face in pursuing this subspecialty and offer practical solutions on how to approach these challenges – a piece that will surely resonate with many young gastroenterologists.
We wrap up our first year of TNG’s ethics series with two cases discussing the utilization of cannabis therapy in inflammatory bowel disease (IBD). Dr. Jami Kinnucan (University of Michigan) and Dr. Arun Swaminath (Lenox Hill Hospital) systematically review existing data on the efficacy of cannabis use in IBD, the risks associated with therapy, and legal implications for both physicians and patients.
Also in this issue is a high-yield clinical review on the endoscopic drainage of pancreatic fluid collections by Dr. Robert Moran and Dr. Joseph Elmunzer (Medical University of South Carolina). Dr. Manol Jovani (Johns Hopkins) teaches us about confounding – a critical concept to keep in mind when evaluating any manuscript. Lastly, our DHPA Private Practice Perspectives article, written by Dr. Mehul Lalani (US Digestive), reviews how quality measures and initiatives are tracked and implemented in private practice.
If you have interest in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Ryan Farrell ([email protected]), managing editor of TNG.
Stay well,
Vijaya L. Rao, MD
Editor in Chief
Assistant Professor of Medicine, University of Chicago, Section of Gastroenterology, Hepatology & Nutrition
Dear colleagues,
I’m excited to introduce the November issue of The New Gastroenterologist – the last edition of 2020 features a fantastic line-up of articles! As the year comes to a close, we reflect on what has certainly been an interesting year, defined by a set of unique challenges we have faced as a nation and as a specialty.
The fellowship recruitment season is one that has looked starkly different as interviews have converted to a virtual format. Dr. Wissam Khan, Dr. Nada Al Masalmeh, Dr. Stephanie Judd, and Dr. Diane Levine (Wayne State University) compile a helpful list of tips and tricks on proper interview etiquette in the new era of web-based interviews.
Financial planning in the face of a pandemic is a formidable task – Jonathan Tudor (Fidelity Investments) offers valuable advice for gastroenterologists on how to remain secure in your finances even in uncertain circumstances.
This quarter’s “In Focus” feature, written by Dr. Yutaka Tomizawa (University of Washington), is a comprehensive piece elucidating the role of gastroenterologists in the management of gastric cancer. The article reviews the individual risk factors that exist for gastric cancer and provides guidance on how to stratify patients accordingly, which is critical in the ethnically diverse population of the United States.
Keeping a procedure log during fellowship can seem daunting and cumbersome, but it is important. Dr. Houman Rezaizadeh (University of Connecticut) shares his program’s experience with the AGA Procedure Log, a convenient online tracking tool, which can provide accurate and secure documentation of endoscopic procedures performed throughout fellowship.
Dr. Nazia Hasan (North Bay Health Care) and Dr. Allison Schulman (University of Michigan) broach an incredibly important topic: the paucity of women in interventional endoscopy. Dr. Hasan and Dr. Shulman candidly discuss the barriers women face in pursuing this subspecialty and offer practical solutions on how to approach these challenges – a piece that will surely resonate with many young gastroenterologists.
We wrap up our first year of TNG’s ethics series with two cases discussing the utilization of cannabis therapy in inflammatory bowel disease (IBD). Dr. Jami Kinnucan (University of Michigan) and Dr. Arun Swaminath (Lenox Hill Hospital) systematically review existing data on the efficacy of cannabis use in IBD, the risks associated with therapy, and legal implications for both physicians and patients.
Also in this issue is a high-yield clinical review on the endoscopic drainage of pancreatic fluid collections by Dr. Robert Moran and Dr. Joseph Elmunzer (Medical University of South Carolina). Dr. Manol Jovani (Johns Hopkins) teaches us about confounding – a critical concept to keep in mind when evaluating any manuscript. Lastly, our DHPA Private Practice Perspectives article, written by Dr. Mehul Lalani (US Digestive), reviews how quality measures and initiatives are tracked and implemented in private practice.
If you have interest in contributing or have ideas for future TNG topics, please contact me ([email protected]), or Ryan Farrell ([email protected]), managing editor of TNG.
Stay well,
Vijaya L. Rao, MD
Editor in Chief
Assistant Professor of Medicine, University of Chicago, Section of Gastroenterology, Hepatology & Nutrition
Disruption of postpandemic world will precipitate innovation
When this editorial is published, we will know the results of the national election (hopefully) and whether there will be a smooth transition of power. We should know whether the Affordable Care Act will remain intact, and we will have indications about the impact of a COVID/flu combination. Health care will never be the same.
According to a recent Medscape survey, 62% of U.S. physicians saw a reduction of monthly income (12% saw a reduction of over 70%) in the first 6 months of this year. Almost a third of the physician workforce is contemplating retirement earlier than anticipated. As worrisome, according to a JAMA article (Aug 4, 2020;324:510-3) the United States saw a 35% increase in excess deaths because of non-COVID etiologies, an indication of health care deferral and avoidance. We all are scrambling to catch up and accommodate an enormous demand.
We are witnessing a “K” shaped recovery for both individuals and GI practices. If your health care is covered by Medicare, you own a mortgage-free home and your wealth is based on a balanced equity/bond portfolio, then all of your assets increased in value compared to last year’s peak valuations. For the other 90% of Americans, the recovery is modest, neutral, or more often nonexistent. Gastroenterologists who work in academic centers or large health systems did not lose income this year and were protected by billion-dollar credit lines and cash-on-hand accounts from robust days available to these entities. Independent practices (critically dependent on monthly cash flow) were decimated, furthering the trend towards consolidation, retirement, and acquisitions. With the new CMS E/M valuations we will see further reduction in procedural reimbursement.
However, disruption always precipitates innovation. Challenges are great but opportunities are clearly evident for those willing to risk.
John I. Allen, MD, MBA, AGAF
Editor in Chief
When this editorial is published, we will know the results of the national election (hopefully) and whether there will be a smooth transition of power. We should know whether the Affordable Care Act will remain intact, and we will have indications about the impact of a COVID/flu combination. Health care will never be the same.
According to a recent Medscape survey, 62% of U.S. physicians saw a reduction of monthly income (12% saw a reduction of over 70%) in the first 6 months of this year. Almost a third of the physician workforce is contemplating retirement earlier than anticipated. As worrisome, according to a JAMA article (Aug 4, 2020;324:510-3) the United States saw a 35% increase in excess deaths because of non-COVID etiologies, an indication of health care deferral and avoidance. We all are scrambling to catch up and accommodate an enormous demand.
We are witnessing a “K” shaped recovery for both individuals and GI practices. If your health care is covered by Medicare, you own a mortgage-free home and your wealth is based on a balanced equity/bond portfolio, then all of your assets increased in value compared to last year’s peak valuations. For the other 90% of Americans, the recovery is modest, neutral, or more often nonexistent. Gastroenterologists who work in academic centers or large health systems did not lose income this year and were protected by billion-dollar credit lines and cash-on-hand accounts from robust days available to these entities. Independent practices (critically dependent on monthly cash flow) were decimated, furthering the trend towards consolidation, retirement, and acquisitions. With the new CMS E/M valuations we will see further reduction in procedural reimbursement.
However, disruption always precipitates innovation. Challenges are great but opportunities are clearly evident for those willing to risk.
John I. Allen, MD, MBA, AGAF
Editor in Chief
When this editorial is published, we will know the results of the national election (hopefully) and whether there will be a smooth transition of power. We should know whether the Affordable Care Act will remain intact, and we will have indications about the impact of a COVID/flu combination. Health care will never be the same.
According to a recent Medscape survey, 62% of U.S. physicians saw a reduction of monthly income (12% saw a reduction of over 70%) in the first 6 months of this year. Almost a third of the physician workforce is contemplating retirement earlier than anticipated. As worrisome, according to a JAMA article (Aug 4, 2020;324:510-3) the United States saw a 35% increase in excess deaths because of non-COVID etiologies, an indication of health care deferral and avoidance. We all are scrambling to catch up and accommodate an enormous demand.
We are witnessing a “K” shaped recovery for both individuals and GI practices. If your health care is covered by Medicare, you own a mortgage-free home and your wealth is based on a balanced equity/bond portfolio, then all of your assets increased in value compared to last year’s peak valuations. For the other 90% of Americans, the recovery is modest, neutral, or more often nonexistent. Gastroenterologists who work in academic centers or large health systems did not lose income this year and were protected by billion-dollar credit lines and cash-on-hand accounts from robust days available to these entities. Independent practices (critically dependent on monthly cash flow) were decimated, furthering the trend towards consolidation, retirement, and acquisitions. With the new CMS E/M valuations we will see further reduction in procedural reimbursement.
However, disruption always precipitates innovation. Challenges are great but opportunities are clearly evident for those willing to risk.
John I. Allen, MD, MBA, AGAF
Editor in Chief
OTC topical ivermectin lotion earns FDA approval for head lice
in patients aged 6 months and older.
Ivermectin was approved as a prescription treatment for head lice in February 2012, according to an FDA press release, and is now approved as an over-the-counter treatment through an “Rx-to-OTC” switch process. The approval was granted to Arbor Pharmaceuticals.
The expanded approval for ivermectin increases access to effective care for head lice, which is estimated to affect between 6 million and 12 million children each year in the United States, according to the Centers for Disease Control and Prevention.
“The Rx-to-OTC switch process aims to promote public health by increasing consumer access to drugs that would otherwise only be available by prescription,” Theresa Michele, MD, acting director of the Office of Nonprescription Drugs in the FDA’s Center for Drug Evaluation and Research, said in the press release.
The FDA also noted in the press release that “Sklice, and its active ingredient ivermectin, have not been shown to be safe or effective for the treatment or prevention of COVID-19 and they are not FDA-approved for this use.”
The drug is approved only for treating head lice, and should be used on the scalp and dry hair, according to the labeling. In the wake of the approval, ivermectin will no longer be available as a prescription drug, according to the FDA, and patients currently using prescription versions should contact their health care providers.
An Rx-to-OTC switch is contingent on the manufacturer’s data showing that the drug is safe and effective when used as directed. In addition, “the manufacturer must show that consumers can understand how to use the drug safely and effectively without the supervision of a health care professional,” according to the FDA.
in patients aged 6 months and older.
Ivermectin was approved as a prescription treatment for head lice in February 2012, according to an FDA press release, and is now approved as an over-the-counter treatment through an “Rx-to-OTC” switch process. The approval was granted to Arbor Pharmaceuticals.
The expanded approval for ivermectin increases access to effective care for head lice, which is estimated to affect between 6 million and 12 million children each year in the United States, according to the Centers for Disease Control and Prevention.
“The Rx-to-OTC switch process aims to promote public health by increasing consumer access to drugs that would otherwise only be available by prescription,” Theresa Michele, MD, acting director of the Office of Nonprescription Drugs in the FDA’s Center for Drug Evaluation and Research, said in the press release.
The FDA also noted in the press release that “Sklice, and its active ingredient ivermectin, have not been shown to be safe or effective for the treatment or prevention of COVID-19 and they are not FDA-approved for this use.”
The drug is approved only for treating head lice, and should be used on the scalp and dry hair, according to the labeling. In the wake of the approval, ivermectin will no longer be available as a prescription drug, according to the FDA, and patients currently using prescription versions should contact their health care providers.
An Rx-to-OTC switch is contingent on the manufacturer’s data showing that the drug is safe and effective when used as directed. In addition, “the manufacturer must show that consumers can understand how to use the drug safely and effectively without the supervision of a health care professional,” according to the FDA.
in patients aged 6 months and older.
Ivermectin was approved as a prescription treatment for head lice in February 2012, according to an FDA press release, and is now approved as an over-the-counter treatment through an “Rx-to-OTC” switch process. The approval was granted to Arbor Pharmaceuticals.
The expanded approval for ivermectin increases access to effective care for head lice, which is estimated to affect between 6 million and 12 million children each year in the United States, according to the Centers for Disease Control and Prevention.
“The Rx-to-OTC switch process aims to promote public health by increasing consumer access to drugs that would otherwise only be available by prescription,” Theresa Michele, MD, acting director of the Office of Nonprescription Drugs in the FDA’s Center for Drug Evaluation and Research, said in the press release.
The FDA also noted in the press release that “Sklice, and its active ingredient ivermectin, have not been shown to be safe or effective for the treatment or prevention of COVID-19 and they are not FDA-approved for this use.”
The drug is approved only for treating head lice, and should be used on the scalp and dry hair, according to the labeling. In the wake of the approval, ivermectin will no longer be available as a prescription drug, according to the FDA, and patients currently using prescription versions should contact their health care providers.
An Rx-to-OTC switch is contingent on the manufacturer’s data showing that the drug is safe and effective when used as directed. In addition, “the manufacturer must show that consumers can understand how to use the drug safely and effectively without the supervision of a health care professional,” according to the FDA.
October 2020 - What's the diagnosis?
Answer: Celiac hepatitis
Endoscopic biopsy of this severely scalloped duodenal mucosa demonstrated characteristic findings of gluten-sensitive enteropathy, or celiac disease. Celiac disease involvement of the liver is a common extraintestinal manifestation of this immune-mediated disorder, termed celiac hepatitis. Celiac hepatitis affects 40% of adults with celiac disease.1 The pathogenesis is poorly understood, but posited to be related to autoimmunity or toxin-mediated liver injury in the setting of gluten exposure, gut permeability, chronic inflammation, and host susceptibility, among other mechanisms.1-3
Clinical manifestations of celiac hepatitis range from unexplained enzyme elevations in the absence of known liver disease to autoimmune hepatitis to hepatic steatosis, and even cirrhosis.1 The initial presentation can also be elevated liver enzymes in the setting of known celiac disease, without known hepatic disease. Histology of the liver is similarly variable, from a mild or a chronic hepatitis to steatohepatitis and even fibrosis.2 Elevated transaminases less than five times the upper limit of normal when found at celiac diagnosis suggest celiac hepatitis, and do not require further workup.1 For these individuals, response to a gluten-free diet should be monitored and liver chemistries should be repeated at 6–12 months. Persistently elevated aminotransferases should prompt further workup.1 Generally, enzyme elevation and even the histologic appearance of the liver improve after implementation of a gluten-free diet, although not all.2 In celiac hepatitis associated with autoimmune liver disease, immunosuppression may be required in addition to abstaining from gluten.3 Our patient was found to have a tissue transglutaminase level > 100 U/mL (normal, < 4 U/mL). He began a gluten-free diet guided by a nutritionist 4 weeks ago, with rapid improvement in abdominal symptoms, and will be followed to ensure normalization of liver enzymes, which can take up to 1 year.
References
1. Rubio-Tapia A, Murray JA. Liver involvement in celiac disease. Minerva Med. 2008;99:595-604.
2. Majumdar K, Sakhuja P, Puri AS, et al. Coeliac disease and the liver: spectrum of liver histology, serology and treatment response at a tertiary referral centre. J Clin Pathol. 2018;71:412-9.
3. Marciano F, Savoia M, Vajro P. Celiac disease-related hepatic injury: insights into associated conditions and underlying pathomechanisms. Dig Liver Dis. 2016;48:112-9.
Answer: Celiac hepatitis
Endoscopic biopsy of this severely scalloped duodenal mucosa demonstrated characteristic findings of gluten-sensitive enteropathy, or celiac disease. Celiac disease involvement of the liver is a common extraintestinal manifestation of this immune-mediated disorder, termed celiac hepatitis. Celiac hepatitis affects 40% of adults with celiac disease.1 The pathogenesis is poorly understood, but posited to be related to autoimmunity or toxin-mediated liver injury in the setting of gluten exposure, gut permeability, chronic inflammation, and host susceptibility, among other mechanisms.1-3
Clinical manifestations of celiac hepatitis range from unexplained enzyme elevations in the absence of known liver disease to autoimmune hepatitis to hepatic steatosis, and even cirrhosis.1 The initial presentation can also be elevated liver enzymes in the setting of known celiac disease, without known hepatic disease. Histology of the liver is similarly variable, from a mild or a chronic hepatitis to steatohepatitis and even fibrosis.2 Elevated transaminases less than five times the upper limit of normal when found at celiac diagnosis suggest celiac hepatitis, and do not require further workup.1 For these individuals, response to a gluten-free diet should be monitored and liver chemistries should be repeated at 6–12 months. Persistently elevated aminotransferases should prompt further workup.1 Generally, enzyme elevation and even the histologic appearance of the liver improve after implementation of a gluten-free diet, although not all.2 In celiac hepatitis associated with autoimmune liver disease, immunosuppression may be required in addition to abstaining from gluten.3 Our patient was found to have a tissue transglutaminase level > 100 U/mL (normal, < 4 U/mL). He began a gluten-free diet guided by a nutritionist 4 weeks ago, with rapid improvement in abdominal symptoms, and will be followed to ensure normalization of liver enzymes, which can take up to 1 year.
References
1. Rubio-Tapia A, Murray JA. Liver involvement in celiac disease. Minerva Med. 2008;99:595-604.
2. Majumdar K, Sakhuja P, Puri AS, et al. Coeliac disease and the liver: spectrum of liver histology, serology and treatment response at a tertiary referral centre. J Clin Pathol. 2018;71:412-9.
3. Marciano F, Savoia M, Vajro P. Celiac disease-related hepatic injury: insights into associated conditions and underlying pathomechanisms. Dig Liver Dis. 2016;48:112-9.
Answer: Celiac hepatitis
Endoscopic biopsy of this severely scalloped duodenal mucosa demonstrated characteristic findings of gluten-sensitive enteropathy, or celiac disease. Celiac disease involvement of the liver is a common extraintestinal manifestation of this immune-mediated disorder, termed celiac hepatitis. Celiac hepatitis affects 40% of adults with celiac disease.1 The pathogenesis is poorly understood, but posited to be related to autoimmunity or toxin-mediated liver injury in the setting of gluten exposure, gut permeability, chronic inflammation, and host susceptibility, among other mechanisms.1-3
Clinical manifestations of celiac hepatitis range from unexplained enzyme elevations in the absence of known liver disease to autoimmune hepatitis to hepatic steatosis, and even cirrhosis.1 The initial presentation can also be elevated liver enzymes in the setting of known celiac disease, without known hepatic disease. Histology of the liver is similarly variable, from a mild or a chronic hepatitis to steatohepatitis and even fibrosis.2 Elevated transaminases less than five times the upper limit of normal when found at celiac diagnosis suggest celiac hepatitis, and do not require further workup.1 For these individuals, response to a gluten-free diet should be monitored and liver chemistries should be repeated at 6–12 months. Persistently elevated aminotransferases should prompt further workup.1 Generally, enzyme elevation and even the histologic appearance of the liver improve after implementation of a gluten-free diet, although not all.2 In celiac hepatitis associated with autoimmune liver disease, immunosuppression may be required in addition to abstaining from gluten.3 Our patient was found to have a tissue transglutaminase level > 100 U/mL (normal, < 4 U/mL). He began a gluten-free diet guided by a nutritionist 4 weeks ago, with rapid improvement in abdominal symptoms, and will be followed to ensure normalization of liver enzymes, which can take up to 1 year.
References
1. Rubio-Tapia A, Murray JA. Liver involvement in celiac disease. Minerva Med. 2008;99:595-604.
2. Majumdar K, Sakhuja P, Puri AS, et al. Coeliac disease and the liver: spectrum of liver histology, serology and treatment response at a tertiary referral centre. J Clin Pathol. 2018;71:412-9.
3. Marciano F, Savoia M, Vajro P. Celiac disease-related hepatic injury: insights into associated conditions and underlying pathomechanisms. Dig Liver Dis. 2016;48:112-9.
Question: A 24-year-old white man with depression and anxiety disorder is referred for an isolated alanine aminotransferase elevation found by his primary medical doctor on routine blood work. He denies a family history of liver disease, although he does report a family history of lupus. He denies risk factors for viral hepatitis. He drinks about three alcoholic beverages per week. His family is originally from Germany and Ireland. He denies use of over-the-counter medications or supplements beyond a rare use of ibuprofen. His only medication is daily escitalopram. On further questioning he also reports abdominal pain. The abdominal pain is described as dull, constant, right upper quadrant pain near his rib cage. The pain occasionally becomes worse if he eats fast foods. He also notes a 3-month history of bloating and alternating bowel habits between diarrhea and constipation.
Physical examination is notable for unremarkable vital signs and a normal body mass index. He has no stigmata of chronic liver disease or hepatomegaly. He has normal bowel sounds without any tenderness to palpation. An in-office FibroScan is normal with a value of 3 kPa. Aspartate aminotransferase is 33 U/L (normal, 10-40 U/L). Viral serologies are notable for nonreactive hepatitis B surface antigen, surface antibody, and core antibody. Hepatitis C virus RNA is undetectable. Ferritin, iron, and creatine kinase are normal. Thyroid-stimulating hormone, antimitochondrial antibody, and antinuclear antibody are negative. Ceruloplasmin is normal and alpha-1 antitrypsin showed MZ phenotype. An abdominal ultrasound scan shows a normal size liver, normal echotexture, and sludge in the gallbladder, without any intrahepatic or extrahepatic bile duct dilation. The extrahepatic bile duct diameter is 0.3 cm.
Antismooth muscle and quantitative immunoglobulin tests were ordered. An endoscopy is performed for abdominal pain, and duodenal endoscopic and histologic images are provided.
Novel drug slows progression of diabetic kidney disease
For patients with diabetic kidney disease, finerenone, an agent from a new class of selective, nonsteroidal mineralocorticoid receptor antagonists, led to significant reductions in combined adverse renal outcomes and in combined adverse cardiovascular outcomes in the pivotal FIDELIO-DKD trial.
And the safety results showed a good level of tolerability. The rate of hyperkalemia was higher with finerenone than with placebo, but the rate of drug discontinuations for elevated potassium was lower than that seen with spironolactone, a steroidal mineralocorticoid receptor antagonist (MRA).
“An ideal drug would cause no hyperkalemia, but the absolute risk we saw is a fraction of what we see with spironolactone in this vulnerable patient population,” said Rajiv Agarwal, MD, from Indiana in Indianapolis, during a press briefing.
After a median follow-up of 2.6 years, finerenone was associated with a 3.4% absolute reduction in the rate of combined adverse renal events, the study’s primary end point, which comprised kidney failure, renal death, and a drop in estimated glomerular filtration rate (eGFR) of at least 40% from baseline. This produced a significant relative risk reduction of 18%, with a number needed to treat of 32 to prevent one of these events, Dr. Agarwal reported at Kidney Week 2020. Findings from the FIDELIO-DKD trial were published simultaneously in the New England Journal of Medicine.
Finerenone was also associated with an absolute 2.4% reduction in the rate of combined adverse cardiovascular events, the study’s “key secondary end point,” which included cardiovascular death, nonfatal MI, nonfatal stroke, and hospitalization for heart failure. This translated into a significant relative risk reduction of 14% and a number needed to treat of 42 to prevent one of these events.
FIDELIO-DKD assessed 5,734 patients with type 2 diabetes and chronic kidney disease from more than 1,000 sites in 48 countries, including the United States, from 2015 to 2018. In the study cohort, average age was slightly more than 65 years, average baseline systolic blood pressure was 138 mm Hg, average duration of diabetes was nearly 17 years, average baseline glycated hemoglobin (A1c) was 7.7%, and fewer than 5% of patients were Black, 25% were Asian, and about 63% were White.
A suggestion of less severe hyperkalemia
Finerenone was well tolerated by the participants, and the findings suggest that it caused less clinically meaningful hyperkalemia than spironolactone, the most established and widely used MRA.
Like all MRA drugs, finerenone led to an increase in serum potassium in all patient subgroups – in this case 0.2 mmol/L – unlike placebo, said Dr. Agarwal.
The overall incidence of hyperkalemia was 16% in the 2,827 evaluable patients in the finerenone group and 8% in the 2,831 evaluable patients in the placebo group. Fewer than 10% of patients in the trial received a potassium-binding agent.
The rate of hyperkalemia leading to treatment discontinuation was higher in the finerenone group than in the placebo group (2.3% vs. 0.9%).
That 2.3% rate is 10 times lower than the 23.0% rate of hyperkalemia-related treatment discontinuation in patients who received spironolactone and no potassium-binding agent, said Dr. Agarwal, citing a previous study he was involved with.
He hypothesized that finerenone might cause less clinically meaningful hyperkalemia because it creates no active metabolites that linger in the body, whereas spironolactone produces active metabolites with a half life of about 1 week.
“The risk for hyperkalemia is clearly increased with finerenone compared with placebo, and in the absence of head-to-head studies, it’s hard to know how it compares with spironolactone or eplerenone [Inspra],” the other agents in the MRA class, said Mikhail N. Kosiborod, MD, from the University of Missouri–Kansas City.
“The rates of hyperkalemia observed in FIDELIO-DKD were overall comparable to what we would expect from eplerenone. But the rate of serious hyperkalemia was quite low with finerenone, which is reassuring,” Dr. Kosiborod said in an interview.
And the adverse-effect profile showed that finerenone “is as safe as you could expect from an MRA,” said Janani Rangaswami, MD, from the Einstein Medical Center in Philadelphia.
The rate of hyperkalemia should be interpreted in the context of the high risk the enrolled patients faced, given that they all had moderate to severe diabetic kidney disease with albuminuria and, in some cases, eGFR rates as low as 25 mL/min per 1.73m2, she explained. In addition, all patients were on maximally tolerated treatment with either an angiotensin-converting–enzyme inhibitor or an angiotensin receptor blocker to inhibit the renin angiotensin system (RAS).
“Considering this background, it’s a very acceptable adverse-event profile,” Dr. Rangaswami said in an interview.
Renal drugs that could work together
More than 99% of patients in FIDELIO-DKD were on an RAS inhibitor, but fewer than 5% were on a sodium glucose cotransporter 2 (SGLT2) inhibitor at baseline, and fewer than 10% started on this drug class during the course of the study.
Despite that, both Dr. Kosiborod and Dr. Rangaswami are enthusiastic about the prospect of using the three drugs in combination to maximize renal and cardiovascular benefits in FIDELIO-DKD–type patients. Recent results from the CREDENCE study of canagliflozin (Invokana) and from the DAPA-CKD study of dapagluflozin (Farxiga) have established SGLT2 inhibitors – at least those two – as key agents for patients with chronic kidney disease.
Dual treatment with an RAS inhibitor and an SGLT2 inhibitor is “clearly established” for patients with diabetic kidney disease, said Dr. Agarwal.
“After CREDENCE, DAPA-CKD, and now FIDELIO-DKD, we need to seriously consider triple therapy as the future of treatment for diabetic kidney disease to prevent both cardiovascular and kidney complications,” said Dr. Kosiborod. The approach will mimic the multidrug therapy that’s now standard for patients with heart failure with reduced ejection fraction (HFrEF). But he cautioned that this triple combination needs further testing.
“Triple therapy will be the standard of care” for patients with diabetic kidney disease, Dr. Rangaswami agreed, but she cautioned that she would not currently expand the target population for finerenone to patients without type 2 diabetes or to patients without the level of albuminuria required for entry into FIDELIO-DKD: at least 30 mg/g of creatinine per day. And patients with HFrEF were excluded from FIDELIO-DKD, so that limitation on finerenone use should remain for the time being, she added.
Dr. Rangaswami said she is optimistic about the potential efficacy of finerenone added to an SGLT2 inhibitor because of the likelihood that the two drug classes work in different but complementary ways. SGLT2 inhibitors seem to exert their renal protective effects largely through hemodynamic effects, whereas it is likely that finerenone exerts its effects largely as an anti-inflammatory and antifibrotic agent, she speculated. The FIDELIO-DKD results appear to rule out any major effect of finerenone on blood pressure lowering because average systolic pressure fell by only about 2 mm Hg in the treatment group.
“The benefits of finerenone for cardiorenal outcomes are substantial and clinically meaningful,” Dr. Kosiborod said. “We cannot assume that other MRAs, such as spironolactone, provide similar benefits,” he cautioned, but the results are “very good news for patients with type 2 diabetes and chronic kidney disease. We now have another effective intervention with a different mechanism of action.”
FIDELIO-DKD was sponsored by Bayer, the company developing finerenone (BAY 94-8862). Dr. Agarwal has been a consultant to and has received honoraria from Bayer and from several other companies. Dr. Kosiborod has been a consultant to Bayer and to AstraZeneca, Boehringer Ingelheim, Jansse, Merck, and Vifor and has received research funding from AstraZeneca and Boehringer Ingelheim. Dr. Rangaswami has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
For patients with diabetic kidney disease, finerenone, an agent from a new class of selective, nonsteroidal mineralocorticoid receptor antagonists, led to significant reductions in combined adverse renal outcomes and in combined adverse cardiovascular outcomes in the pivotal FIDELIO-DKD trial.
And the safety results showed a good level of tolerability. The rate of hyperkalemia was higher with finerenone than with placebo, but the rate of drug discontinuations for elevated potassium was lower than that seen with spironolactone, a steroidal mineralocorticoid receptor antagonist (MRA).
“An ideal drug would cause no hyperkalemia, but the absolute risk we saw is a fraction of what we see with spironolactone in this vulnerable patient population,” said Rajiv Agarwal, MD, from Indiana in Indianapolis, during a press briefing.
After a median follow-up of 2.6 years, finerenone was associated with a 3.4% absolute reduction in the rate of combined adverse renal events, the study’s primary end point, which comprised kidney failure, renal death, and a drop in estimated glomerular filtration rate (eGFR) of at least 40% from baseline. This produced a significant relative risk reduction of 18%, with a number needed to treat of 32 to prevent one of these events, Dr. Agarwal reported at Kidney Week 2020. Findings from the FIDELIO-DKD trial were published simultaneously in the New England Journal of Medicine.
Finerenone was also associated with an absolute 2.4% reduction in the rate of combined adverse cardiovascular events, the study’s “key secondary end point,” which included cardiovascular death, nonfatal MI, nonfatal stroke, and hospitalization for heart failure. This translated into a significant relative risk reduction of 14% and a number needed to treat of 42 to prevent one of these events.
FIDELIO-DKD assessed 5,734 patients with type 2 diabetes and chronic kidney disease from more than 1,000 sites in 48 countries, including the United States, from 2015 to 2018. In the study cohort, average age was slightly more than 65 years, average baseline systolic blood pressure was 138 mm Hg, average duration of diabetes was nearly 17 years, average baseline glycated hemoglobin (A1c) was 7.7%, and fewer than 5% of patients were Black, 25% were Asian, and about 63% were White.
A suggestion of less severe hyperkalemia
Finerenone was well tolerated by the participants, and the findings suggest that it caused less clinically meaningful hyperkalemia than spironolactone, the most established and widely used MRA.
Like all MRA drugs, finerenone led to an increase in serum potassium in all patient subgroups – in this case 0.2 mmol/L – unlike placebo, said Dr. Agarwal.
The overall incidence of hyperkalemia was 16% in the 2,827 evaluable patients in the finerenone group and 8% in the 2,831 evaluable patients in the placebo group. Fewer than 10% of patients in the trial received a potassium-binding agent.
The rate of hyperkalemia leading to treatment discontinuation was higher in the finerenone group than in the placebo group (2.3% vs. 0.9%).
That 2.3% rate is 10 times lower than the 23.0% rate of hyperkalemia-related treatment discontinuation in patients who received spironolactone and no potassium-binding agent, said Dr. Agarwal, citing a previous study he was involved with.
He hypothesized that finerenone might cause less clinically meaningful hyperkalemia because it creates no active metabolites that linger in the body, whereas spironolactone produces active metabolites with a half life of about 1 week.
“The risk for hyperkalemia is clearly increased with finerenone compared with placebo, and in the absence of head-to-head studies, it’s hard to know how it compares with spironolactone or eplerenone [Inspra],” the other agents in the MRA class, said Mikhail N. Kosiborod, MD, from the University of Missouri–Kansas City.
“The rates of hyperkalemia observed in FIDELIO-DKD were overall comparable to what we would expect from eplerenone. But the rate of serious hyperkalemia was quite low with finerenone, which is reassuring,” Dr. Kosiborod said in an interview.
And the adverse-effect profile showed that finerenone “is as safe as you could expect from an MRA,” said Janani Rangaswami, MD, from the Einstein Medical Center in Philadelphia.
The rate of hyperkalemia should be interpreted in the context of the high risk the enrolled patients faced, given that they all had moderate to severe diabetic kidney disease with albuminuria and, in some cases, eGFR rates as low as 25 mL/min per 1.73m2, she explained. In addition, all patients were on maximally tolerated treatment with either an angiotensin-converting–enzyme inhibitor or an angiotensin receptor blocker to inhibit the renin angiotensin system (RAS).
“Considering this background, it’s a very acceptable adverse-event profile,” Dr. Rangaswami said in an interview.
Renal drugs that could work together
More than 99% of patients in FIDELIO-DKD were on an RAS inhibitor, but fewer than 5% were on a sodium glucose cotransporter 2 (SGLT2) inhibitor at baseline, and fewer than 10% started on this drug class during the course of the study.
Despite that, both Dr. Kosiborod and Dr. Rangaswami are enthusiastic about the prospect of using the three drugs in combination to maximize renal and cardiovascular benefits in FIDELIO-DKD–type patients. Recent results from the CREDENCE study of canagliflozin (Invokana) and from the DAPA-CKD study of dapagluflozin (Farxiga) have established SGLT2 inhibitors – at least those two – as key agents for patients with chronic kidney disease.
Dual treatment with an RAS inhibitor and an SGLT2 inhibitor is “clearly established” for patients with diabetic kidney disease, said Dr. Agarwal.
“After CREDENCE, DAPA-CKD, and now FIDELIO-DKD, we need to seriously consider triple therapy as the future of treatment for diabetic kidney disease to prevent both cardiovascular and kidney complications,” said Dr. Kosiborod. The approach will mimic the multidrug therapy that’s now standard for patients with heart failure with reduced ejection fraction (HFrEF). But he cautioned that this triple combination needs further testing.
“Triple therapy will be the standard of care” for patients with diabetic kidney disease, Dr. Rangaswami agreed, but she cautioned that she would not currently expand the target population for finerenone to patients without type 2 diabetes or to patients without the level of albuminuria required for entry into FIDELIO-DKD: at least 30 mg/g of creatinine per day. And patients with HFrEF were excluded from FIDELIO-DKD, so that limitation on finerenone use should remain for the time being, she added.
Dr. Rangaswami said she is optimistic about the potential efficacy of finerenone added to an SGLT2 inhibitor because of the likelihood that the two drug classes work in different but complementary ways. SGLT2 inhibitors seem to exert their renal protective effects largely through hemodynamic effects, whereas it is likely that finerenone exerts its effects largely as an anti-inflammatory and antifibrotic agent, she speculated. The FIDELIO-DKD results appear to rule out any major effect of finerenone on blood pressure lowering because average systolic pressure fell by only about 2 mm Hg in the treatment group.
“The benefits of finerenone for cardiorenal outcomes are substantial and clinically meaningful,” Dr. Kosiborod said. “We cannot assume that other MRAs, such as spironolactone, provide similar benefits,” he cautioned, but the results are “very good news for patients with type 2 diabetes and chronic kidney disease. We now have another effective intervention with a different mechanism of action.”
FIDELIO-DKD was sponsored by Bayer, the company developing finerenone (BAY 94-8862). Dr. Agarwal has been a consultant to and has received honoraria from Bayer and from several other companies. Dr. Kosiborod has been a consultant to Bayer and to AstraZeneca, Boehringer Ingelheim, Jansse, Merck, and Vifor and has received research funding from AstraZeneca and Boehringer Ingelheim. Dr. Rangaswami has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
For patients with diabetic kidney disease, finerenone, an agent from a new class of selective, nonsteroidal mineralocorticoid receptor antagonists, led to significant reductions in combined adverse renal outcomes and in combined adverse cardiovascular outcomes in the pivotal FIDELIO-DKD trial.
And the safety results showed a good level of tolerability. The rate of hyperkalemia was higher with finerenone than with placebo, but the rate of drug discontinuations for elevated potassium was lower than that seen with spironolactone, a steroidal mineralocorticoid receptor antagonist (MRA).
“An ideal drug would cause no hyperkalemia, but the absolute risk we saw is a fraction of what we see with spironolactone in this vulnerable patient population,” said Rajiv Agarwal, MD, from Indiana in Indianapolis, during a press briefing.
After a median follow-up of 2.6 years, finerenone was associated with a 3.4% absolute reduction in the rate of combined adverse renal events, the study’s primary end point, which comprised kidney failure, renal death, and a drop in estimated glomerular filtration rate (eGFR) of at least 40% from baseline. This produced a significant relative risk reduction of 18%, with a number needed to treat of 32 to prevent one of these events, Dr. Agarwal reported at Kidney Week 2020. Findings from the FIDELIO-DKD trial were published simultaneously in the New England Journal of Medicine.
Finerenone was also associated with an absolute 2.4% reduction in the rate of combined adverse cardiovascular events, the study’s “key secondary end point,” which included cardiovascular death, nonfatal MI, nonfatal stroke, and hospitalization for heart failure. This translated into a significant relative risk reduction of 14% and a number needed to treat of 42 to prevent one of these events.
FIDELIO-DKD assessed 5,734 patients with type 2 diabetes and chronic kidney disease from more than 1,000 sites in 48 countries, including the United States, from 2015 to 2018. In the study cohort, average age was slightly more than 65 years, average baseline systolic blood pressure was 138 mm Hg, average duration of diabetes was nearly 17 years, average baseline glycated hemoglobin (A1c) was 7.7%, and fewer than 5% of patients were Black, 25% were Asian, and about 63% were White.
A suggestion of less severe hyperkalemia
Finerenone was well tolerated by the participants, and the findings suggest that it caused less clinically meaningful hyperkalemia than spironolactone, the most established and widely used MRA.
Like all MRA drugs, finerenone led to an increase in serum potassium in all patient subgroups – in this case 0.2 mmol/L – unlike placebo, said Dr. Agarwal.
The overall incidence of hyperkalemia was 16% in the 2,827 evaluable patients in the finerenone group and 8% in the 2,831 evaluable patients in the placebo group. Fewer than 10% of patients in the trial received a potassium-binding agent.
The rate of hyperkalemia leading to treatment discontinuation was higher in the finerenone group than in the placebo group (2.3% vs. 0.9%).
That 2.3% rate is 10 times lower than the 23.0% rate of hyperkalemia-related treatment discontinuation in patients who received spironolactone and no potassium-binding agent, said Dr. Agarwal, citing a previous study he was involved with.
He hypothesized that finerenone might cause less clinically meaningful hyperkalemia because it creates no active metabolites that linger in the body, whereas spironolactone produces active metabolites with a half life of about 1 week.
“The risk for hyperkalemia is clearly increased with finerenone compared with placebo, and in the absence of head-to-head studies, it’s hard to know how it compares with spironolactone or eplerenone [Inspra],” the other agents in the MRA class, said Mikhail N. Kosiborod, MD, from the University of Missouri–Kansas City.
“The rates of hyperkalemia observed in FIDELIO-DKD were overall comparable to what we would expect from eplerenone. But the rate of serious hyperkalemia was quite low with finerenone, which is reassuring,” Dr. Kosiborod said in an interview.
And the adverse-effect profile showed that finerenone “is as safe as you could expect from an MRA,” said Janani Rangaswami, MD, from the Einstein Medical Center in Philadelphia.
The rate of hyperkalemia should be interpreted in the context of the high risk the enrolled patients faced, given that they all had moderate to severe diabetic kidney disease with albuminuria and, in some cases, eGFR rates as low as 25 mL/min per 1.73m2, she explained. In addition, all patients were on maximally tolerated treatment with either an angiotensin-converting–enzyme inhibitor or an angiotensin receptor blocker to inhibit the renin angiotensin system (RAS).
“Considering this background, it’s a very acceptable adverse-event profile,” Dr. Rangaswami said in an interview.
Renal drugs that could work together
More than 99% of patients in FIDELIO-DKD were on an RAS inhibitor, but fewer than 5% were on a sodium glucose cotransporter 2 (SGLT2) inhibitor at baseline, and fewer than 10% started on this drug class during the course of the study.
Despite that, both Dr. Kosiborod and Dr. Rangaswami are enthusiastic about the prospect of using the three drugs in combination to maximize renal and cardiovascular benefits in FIDELIO-DKD–type patients. Recent results from the CREDENCE study of canagliflozin (Invokana) and from the DAPA-CKD study of dapagluflozin (Farxiga) have established SGLT2 inhibitors – at least those two – as key agents for patients with chronic kidney disease.
Dual treatment with an RAS inhibitor and an SGLT2 inhibitor is “clearly established” for patients with diabetic kidney disease, said Dr. Agarwal.
“After CREDENCE, DAPA-CKD, and now FIDELIO-DKD, we need to seriously consider triple therapy as the future of treatment for diabetic kidney disease to prevent both cardiovascular and kidney complications,” said Dr. Kosiborod. The approach will mimic the multidrug therapy that’s now standard for patients with heart failure with reduced ejection fraction (HFrEF). But he cautioned that this triple combination needs further testing.
“Triple therapy will be the standard of care” for patients with diabetic kidney disease, Dr. Rangaswami agreed, but she cautioned that she would not currently expand the target population for finerenone to patients without type 2 diabetes or to patients without the level of albuminuria required for entry into FIDELIO-DKD: at least 30 mg/g of creatinine per day. And patients with HFrEF were excluded from FIDELIO-DKD, so that limitation on finerenone use should remain for the time being, she added.
Dr. Rangaswami said she is optimistic about the potential efficacy of finerenone added to an SGLT2 inhibitor because of the likelihood that the two drug classes work in different but complementary ways. SGLT2 inhibitors seem to exert their renal protective effects largely through hemodynamic effects, whereas it is likely that finerenone exerts its effects largely as an anti-inflammatory and antifibrotic agent, she speculated. The FIDELIO-DKD results appear to rule out any major effect of finerenone on blood pressure lowering because average systolic pressure fell by only about 2 mm Hg in the treatment group.
“The benefits of finerenone for cardiorenal outcomes are substantial and clinically meaningful,” Dr. Kosiborod said. “We cannot assume that other MRAs, such as spironolactone, provide similar benefits,” he cautioned, but the results are “very good news for patients with type 2 diabetes and chronic kidney disease. We now have another effective intervention with a different mechanism of action.”
FIDELIO-DKD was sponsored by Bayer, the company developing finerenone (BAY 94-8862). Dr. Agarwal has been a consultant to and has received honoraria from Bayer and from several other companies. Dr. Kosiborod has been a consultant to Bayer and to AstraZeneca, Boehringer Ingelheim, Jansse, Merck, and Vifor and has received research funding from AstraZeneca and Boehringer Ingelheim. Dr. Rangaswami has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM KIDNEY WEEK
The authority/accountability balance
Evaluating your career trajectory
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
Evaluating your career trajectory
Evaluating your career trajectory
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
Brain imaging reveals a neural basis for partisan politics
The differences between politically left- and right-leaning individuals may have neural underpinnings, results from a new brain imaging study suggest.
Investigators found that despite watching the same videos related to immigration policy, neural responses differed between liberals and conservatives.
“This divergence was strongest when the videos used language that highlighted threat, morality, and emotions, suggesting that certain words are more likely to drive polarized response,” lead researcher Yuan Chang Leong, PhD, a postdoctoral scholar in cognitive neuroscience at the University of California, Berkeley, told Medscape Medical News.
“The results suggest a neural basis for partisan biases in interpreting political messages, the effects these biases have on attitude change, and the type of language most likely to drive biased interpretations,” Leong added.
The study was published online Oct. 20 in Proceedings of the National Academy of Sciences.
Hardwired to disagree?
The researchers combined fMRI with semantic content analysis to investigate neural mechanisms that underlie the biased processing of political content.
They scanned 38 middle-aged men and women with liberal- or conservative-leaning immigration attitudes while the participants watched short news clips, campaign ads, and public speeches related to various immigration policies.
These policies included those that led to the United States–Mexico border wall, Deferred Action for Childhood Arrivals (DACA) protections for undocumented immigrants, the ban on refugees from majority-Muslim countries coming to the United States, and the cutting of federal funding to sanctuary cities.
After each video, participants rated on a scale of 1 to 5 how much they agreed with the general message of the video, the credibility of the information presented, and the extent to which the video made them likely to change their position and to support the policy in question.
The study revealed evidence of “neural polarization” – activity in the brain that diverges between people who hold liberal vs. conservative political views, the researchers reported.
Neural polarization was observed in the dorsomedial prefrontal cortex (DMPFC), a brain region associated with the interpretation of narrative content.
Neural polarization in this region intensified during moments in the videos that included risk-related and moral-emotional language, highlighting content features most likely to drive divergent interpretations between conservatives and liberals, they noted.
For a given individual, the closer that brain activity resembled that of the “average conservative” or “average liberal,” the more likely the person was to adopt that group’s position after watching the videos.
“We know that partisans respond differently to the same information. So in that sense, it’s not surprising to find that their brains respond differently as well,” Leong told Medscape Medical News.
“What we weren’t sure about was where in the brain we would find these differences, how neural differences were related to attitude change, and what type of content would be most likely to be associated with these differences,” he said.
Importantly, said Leong, these differences do not imply that people are hardwired to disagree. Rather, individual experiences and the media that is consumed likely contribute to neural polarization.
“ – for example, by framing messages to appeal to the core values of the respective voter,” he said.
Brain stimulation to alter political perception?
Reached for comment, Shaheen Lakhan, MD, PhD, neurologist in Newton, Mass., and executive director, Global Neuroscience Initiative Foundation, said the research “puts us one step closer to identifying how our brains interpret political information.”
The study, Lakhan noted, implicates a specific brain structure, the DMPFC, which is the “lens” in which information that gets into our brain is “viewed and acted on.”
“I trust that there will be plenty more work using a similar fMRI approach to tease out scenarios outside of immigration policy, as used in this study. Down the line, brain signatures through fMRI may be able to tell an individual’s political bent, and perhaps technologies like transcranial magnetic stimulation may be able to modulate our perceptions of political content, Shaheen said.
The research was supported by a grant from the Army Research Office. Leong and Lakhan have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The differences between politically left- and right-leaning individuals may have neural underpinnings, results from a new brain imaging study suggest.
Investigators found that despite watching the same videos related to immigration policy, neural responses differed between liberals and conservatives.
“This divergence was strongest when the videos used language that highlighted threat, morality, and emotions, suggesting that certain words are more likely to drive polarized response,” lead researcher Yuan Chang Leong, PhD, a postdoctoral scholar in cognitive neuroscience at the University of California, Berkeley, told Medscape Medical News.
“The results suggest a neural basis for partisan biases in interpreting political messages, the effects these biases have on attitude change, and the type of language most likely to drive biased interpretations,” Leong added.
The study was published online Oct. 20 in Proceedings of the National Academy of Sciences.
Hardwired to disagree?
The researchers combined fMRI with semantic content analysis to investigate neural mechanisms that underlie the biased processing of political content.
They scanned 38 middle-aged men and women with liberal- or conservative-leaning immigration attitudes while the participants watched short news clips, campaign ads, and public speeches related to various immigration policies.
These policies included those that led to the United States–Mexico border wall, Deferred Action for Childhood Arrivals (DACA) protections for undocumented immigrants, the ban on refugees from majority-Muslim countries coming to the United States, and the cutting of federal funding to sanctuary cities.
After each video, participants rated on a scale of 1 to 5 how much they agreed with the general message of the video, the credibility of the information presented, and the extent to which the video made them likely to change their position and to support the policy in question.
The study revealed evidence of “neural polarization” – activity in the brain that diverges between people who hold liberal vs. conservative political views, the researchers reported.
Neural polarization was observed in the dorsomedial prefrontal cortex (DMPFC), a brain region associated with the interpretation of narrative content.
Neural polarization in this region intensified during moments in the videos that included risk-related and moral-emotional language, highlighting content features most likely to drive divergent interpretations between conservatives and liberals, they noted.
For a given individual, the closer that brain activity resembled that of the “average conservative” or “average liberal,” the more likely the person was to adopt that group’s position after watching the videos.
“We know that partisans respond differently to the same information. So in that sense, it’s not surprising to find that their brains respond differently as well,” Leong told Medscape Medical News.
“What we weren’t sure about was where in the brain we would find these differences, how neural differences were related to attitude change, and what type of content would be most likely to be associated with these differences,” he said.
Importantly, said Leong, these differences do not imply that people are hardwired to disagree. Rather, individual experiences and the media that is consumed likely contribute to neural polarization.
“ – for example, by framing messages to appeal to the core values of the respective voter,” he said.
Brain stimulation to alter political perception?
Reached for comment, Shaheen Lakhan, MD, PhD, neurologist in Newton, Mass., and executive director, Global Neuroscience Initiative Foundation, said the research “puts us one step closer to identifying how our brains interpret political information.”
The study, Lakhan noted, implicates a specific brain structure, the DMPFC, which is the “lens” in which information that gets into our brain is “viewed and acted on.”
“I trust that there will be plenty more work using a similar fMRI approach to tease out scenarios outside of immigration policy, as used in this study. Down the line, brain signatures through fMRI may be able to tell an individual’s political bent, and perhaps technologies like transcranial magnetic stimulation may be able to modulate our perceptions of political content, Shaheen said.
The research was supported by a grant from the Army Research Office. Leong and Lakhan have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The differences between politically left- and right-leaning individuals may have neural underpinnings, results from a new brain imaging study suggest.
Investigators found that despite watching the same videos related to immigration policy, neural responses differed between liberals and conservatives.
“This divergence was strongest when the videos used language that highlighted threat, morality, and emotions, suggesting that certain words are more likely to drive polarized response,” lead researcher Yuan Chang Leong, PhD, a postdoctoral scholar in cognitive neuroscience at the University of California, Berkeley, told Medscape Medical News.
“The results suggest a neural basis for partisan biases in interpreting political messages, the effects these biases have on attitude change, and the type of language most likely to drive biased interpretations,” Leong added.
The study was published online Oct. 20 in Proceedings of the National Academy of Sciences.
Hardwired to disagree?
The researchers combined fMRI with semantic content analysis to investigate neural mechanisms that underlie the biased processing of political content.
They scanned 38 middle-aged men and women with liberal- or conservative-leaning immigration attitudes while the participants watched short news clips, campaign ads, and public speeches related to various immigration policies.
These policies included those that led to the United States–Mexico border wall, Deferred Action for Childhood Arrivals (DACA) protections for undocumented immigrants, the ban on refugees from majority-Muslim countries coming to the United States, and the cutting of federal funding to sanctuary cities.
After each video, participants rated on a scale of 1 to 5 how much they agreed with the general message of the video, the credibility of the information presented, and the extent to which the video made them likely to change their position and to support the policy in question.
The study revealed evidence of “neural polarization” – activity in the brain that diverges between people who hold liberal vs. conservative political views, the researchers reported.
Neural polarization was observed in the dorsomedial prefrontal cortex (DMPFC), a brain region associated with the interpretation of narrative content.
Neural polarization in this region intensified during moments in the videos that included risk-related and moral-emotional language, highlighting content features most likely to drive divergent interpretations between conservatives and liberals, they noted.
For a given individual, the closer that brain activity resembled that of the “average conservative” or “average liberal,” the more likely the person was to adopt that group’s position after watching the videos.
“We know that partisans respond differently to the same information. So in that sense, it’s not surprising to find that their brains respond differently as well,” Leong told Medscape Medical News.
“What we weren’t sure about was where in the brain we would find these differences, how neural differences were related to attitude change, and what type of content would be most likely to be associated with these differences,” he said.
Importantly, said Leong, these differences do not imply that people are hardwired to disagree. Rather, individual experiences and the media that is consumed likely contribute to neural polarization.
“ – for example, by framing messages to appeal to the core values of the respective voter,” he said.
Brain stimulation to alter political perception?
Reached for comment, Shaheen Lakhan, MD, PhD, neurologist in Newton, Mass., and executive director, Global Neuroscience Initiative Foundation, said the research “puts us one step closer to identifying how our brains interpret political information.”
The study, Lakhan noted, implicates a specific brain structure, the DMPFC, which is the “lens” in which information that gets into our brain is “viewed and acted on.”
“I trust that there will be plenty more work using a similar fMRI approach to tease out scenarios outside of immigration policy, as used in this study. Down the line, brain signatures through fMRI may be able to tell an individual’s political bent, and perhaps technologies like transcranial magnetic stimulation may be able to modulate our perceptions of political content, Shaheen said.
The research was supported by a grant from the Army Research Office. Leong and Lakhan have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.