User login
For MD-IQ use only
Derms in survey say climate change is impacting their patients
in which the majority of participants said their patients are already being impacted.
Almost 80% of the 148 participants who responded to an electronic survey reported this belief.
The survey was designed and distributed to the membership of various dermatological organizations by Misha Rosenbach, MD, and coauthors. The results were published in the British Journal of Dermatology.
Asked also about specific types of climate-driven phenomena with a current – or future – impact on their patients, 80.1% reported that they believed that increased exposure to ultraviolet radiation (UVR) is impactful, or will be. Changes in temporal or geographic patterns of vector-borne illnesses were affirmed by 78.7%, and an increase in social displacement caused by extreme weather or other events was affirmed by 67.1% as having an impact on their patients currently or in the future.
Other phenomena affirmed by respondents as already having an impact or impacting patients in the future were an increased incidence of heat exposure or heat-related illness (58.2%); an increase in rates of inflammatory skin disease flares (43.2%); increased incidence of waterborne infections (42.5%); and increased rates of allergic contact dermatitis (29.5%).
The survey was sent to the membership of the American Society of Dermatologic Surgery, the Society for Pediatric Dermatology, the Society for Investigative Dermatology, and the American Academy of Dermatology’s Climate Change Expert Resource Group (ERG), among other organizations.
The study design and membership overlap made it impossible to calculate a response rate, the authors said, but they estimated it to be about 10%.
Almost all respondents were from the United States, and most (86.3%) practiced in an academic setting. The findings are similar to those of an online survey of members of the International Society of Dermatology (ISD), published in 2020, which found that 89% of 158 respondents believed climate change will impact the incidence of skin diseases in their area.
“Physicians, including dermatologists, are starting to understand the impact of the climate crisis on both their patients and themselves ... both through lived experiences and [issues raised] more in the scientific literature and in meetings,” Dr. Rosenbach, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said in an interview.
A majority of participants in the U.S. survey agreed they have a responsibility to bring awareness of the health effects of climate change to patients (77.2%) and to policymakers (88.6%). (In the ISD survey, 88% said they believed that dermatologists should play an advocacy role in climate change-related issues).
Only a minority of respondents in the U.S. survey said that they would feel comfortable discussing climate change with their patients (37.2%). Almost one-third of the respondents said they would like to be better informed about climate change before doing so. And 81.8% said they would like to read more about the dermatological effects of climate change in scientific journals.
“There continues to be unfilled interest in education and advocacy regarding climate change, suggesting a ‘practice gap’ even among dermatologists,” Dr. Rosenbach and his colleagues wrote, noting opportunities for professional organizations and journals to provide more resources and “actionable items” regarding climate change.
Some dermatologists have been taking action, in the meantime, to reduce the carbon footprint of their practices and institutions. Reductions in facility energy consumption, and reductions in medical waste/optimization of recycling, were each reported by more than one-third of survey respondents.
And almost half indicated that their practice or institution had increased capacity for telemedicine or telecommuting in response to climate change. Only 8% said their practice or institution had divested from fossil fuel stocks and/or bonds.
“There are a lot of sustainability-in-medicine solutions that are actually cost-neutral or cost-saving for practices,” said Dr. Rosenbach, who is a founder and co-chair of the AAD’s ERG on Climate Change and Environmental Issues.
Research in dermatology is starting to quantify the environmental impact of some of these changes. In a research letter also published in the British Journal of Dermatology, researchers from Cardiff University and the department of dermatology at University Hospital of Wales, described how they determined that reusable surgical packs used for skin surgery are more sustainable than single-use packs because of their reduced cost and reduced greenhouse gas emissions.
Such single-site reports are “early feeders” into what will become a stream of larger studies quantifying the impact of measures taken in dermatology, Dr. Rosenbach said.
Across medicine, there is evidence that health care professionals are now seeing climate change as a threat to their patients. In a multinational survey published last year in The Lancet Planetary Health, 77% of 3,977 participants said that climate change will cause a moderate or great deal of harm for their patients.
Climate change will be discussed at the AAD’s annual meeting in late March in a session devoted to the topic, and as part of a broader session on controversies in dermatology.
Dr. Rosenbach and two of the five authors of the dermatology research letter are members of the AAD’s ERG on climate change, but in the publication they noted that they were not writing on behalf of the AAD. None of the authors reported any disclosures, and there was no funding source for the survey.
in which the majority of participants said their patients are already being impacted.
Almost 80% of the 148 participants who responded to an electronic survey reported this belief.
The survey was designed and distributed to the membership of various dermatological organizations by Misha Rosenbach, MD, and coauthors. The results were published in the British Journal of Dermatology.
Asked also about specific types of climate-driven phenomena with a current – or future – impact on their patients, 80.1% reported that they believed that increased exposure to ultraviolet radiation (UVR) is impactful, or will be. Changes in temporal or geographic patterns of vector-borne illnesses were affirmed by 78.7%, and an increase in social displacement caused by extreme weather or other events was affirmed by 67.1% as having an impact on their patients currently or in the future.
Other phenomena affirmed by respondents as already having an impact or impacting patients in the future were an increased incidence of heat exposure or heat-related illness (58.2%); an increase in rates of inflammatory skin disease flares (43.2%); increased incidence of waterborne infections (42.5%); and increased rates of allergic contact dermatitis (29.5%).
The survey was sent to the membership of the American Society of Dermatologic Surgery, the Society for Pediatric Dermatology, the Society for Investigative Dermatology, and the American Academy of Dermatology’s Climate Change Expert Resource Group (ERG), among other organizations.
The study design and membership overlap made it impossible to calculate a response rate, the authors said, but they estimated it to be about 10%.
Almost all respondents were from the United States, and most (86.3%) practiced in an academic setting. The findings are similar to those of an online survey of members of the International Society of Dermatology (ISD), published in 2020, which found that 89% of 158 respondents believed climate change will impact the incidence of skin diseases in their area.
“Physicians, including dermatologists, are starting to understand the impact of the climate crisis on both their patients and themselves ... both through lived experiences and [issues raised] more in the scientific literature and in meetings,” Dr. Rosenbach, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said in an interview.
A majority of participants in the U.S. survey agreed they have a responsibility to bring awareness of the health effects of climate change to patients (77.2%) and to policymakers (88.6%). (In the ISD survey, 88% said they believed that dermatologists should play an advocacy role in climate change-related issues).
Only a minority of respondents in the U.S. survey said that they would feel comfortable discussing climate change with their patients (37.2%). Almost one-third of the respondents said they would like to be better informed about climate change before doing so. And 81.8% said they would like to read more about the dermatological effects of climate change in scientific journals.
“There continues to be unfilled interest in education and advocacy regarding climate change, suggesting a ‘practice gap’ even among dermatologists,” Dr. Rosenbach and his colleagues wrote, noting opportunities for professional organizations and journals to provide more resources and “actionable items” regarding climate change.
Some dermatologists have been taking action, in the meantime, to reduce the carbon footprint of their practices and institutions. Reductions in facility energy consumption, and reductions in medical waste/optimization of recycling, were each reported by more than one-third of survey respondents.
And almost half indicated that their practice or institution had increased capacity for telemedicine or telecommuting in response to climate change. Only 8% said their practice or institution had divested from fossil fuel stocks and/or bonds.
“There are a lot of sustainability-in-medicine solutions that are actually cost-neutral or cost-saving for practices,” said Dr. Rosenbach, who is a founder and co-chair of the AAD’s ERG on Climate Change and Environmental Issues.
Research in dermatology is starting to quantify the environmental impact of some of these changes. In a research letter also published in the British Journal of Dermatology, researchers from Cardiff University and the department of dermatology at University Hospital of Wales, described how they determined that reusable surgical packs used for skin surgery are more sustainable than single-use packs because of their reduced cost and reduced greenhouse gas emissions.
Such single-site reports are “early feeders” into what will become a stream of larger studies quantifying the impact of measures taken in dermatology, Dr. Rosenbach said.
Across medicine, there is evidence that health care professionals are now seeing climate change as a threat to their patients. In a multinational survey published last year in The Lancet Planetary Health, 77% of 3,977 participants said that climate change will cause a moderate or great deal of harm for their patients.
Climate change will be discussed at the AAD’s annual meeting in late March in a session devoted to the topic, and as part of a broader session on controversies in dermatology.
Dr. Rosenbach and two of the five authors of the dermatology research letter are members of the AAD’s ERG on climate change, but in the publication they noted that they were not writing on behalf of the AAD. None of the authors reported any disclosures, and there was no funding source for the survey.
in which the majority of participants said their patients are already being impacted.
Almost 80% of the 148 participants who responded to an electronic survey reported this belief.
The survey was designed and distributed to the membership of various dermatological organizations by Misha Rosenbach, MD, and coauthors. The results were published in the British Journal of Dermatology.
Asked also about specific types of climate-driven phenomena with a current – or future – impact on their patients, 80.1% reported that they believed that increased exposure to ultraviolet radiation (UVR) is impactful, or will be. Changes in temporal or geographic patterns of vector-borne illnesses were affirmed by 78.7%, and an increase in social displacement caused by extreme weather or other events was affirmed by 67.1% as having an impact on their patients currently or in the future.
Other phenomena affirmed by respondents as already having an impact or impacting patients in the future were an increased incidence of heat exposure or heat-related illness (58.2%); an increase in rates of inflammatory skin disease flares (43.2%); increased incidence of waterborne infections (42.5%); and increased rates of allergic contact dermatitis (29.5%).
The survey was sent to the membership of the American Society of Dermatologic Surgery, the Society for Pediatric Dermatology, the Society for Investigative Dermatology, and the American Academy of Dermatology’s Climate Change Expert Resource Group (ERG), among other organizations.
The study design and membership overlap made it impossible to calculate a response rate, the authors said, but they estimated it to be about 10%.
Almost all respondents were from the United States, and most (86.3%) practiced in an academic setting. The findings are similar to those of an online survey of members of the International Society of Dermatology (ISD), published in 2020, which found that 89% of 158 respondents believed climate change will impact the incidence of skin diseases in their area.
“Physicians, including dermatologists, are starting to understand the impact of the climate crisis on both their patients and themselves ... both through lived experiences and [issues raised] more in the scientific literature and in meetings,” Dr. Rosenbach, associate professor of dermatology at the University of Pennsylvania, Philadelphia, said in an interview.
A majority of participants in the U.S. survey agreed they have a responsibility to bring awareness of the health effects of climate change to patients (77.2%) and to policymakers (88.6%). (In the ISD survey, 88% said they believed that dermatologists should play an advocacy role in climate change-related issues).
Only a minority of respondents in the U.S. survey said that they would feel comfortable discussing climate change with their patients (37.2%). Almost one-third of the respondents said they would like to be better informed about climate change before doing so. And 81.8% said they would like to read more about the dermatological effects of climate change in scientific journals.
“There continues to be unfilled interest in education and advocacy regarding climate change, suggesting a ‘practice gap’ even among dermatologists,” Dr. Rosenbach and his colleagues wrote, noting opportunities for professional organizations and journals to provide more resources and “actionable items” regarding climate change.
Some dermatologists have been taking action, in the meantime, to reduce the carbon footprint of their practices and institutions. Reductions in facility energy consumption, and reductions in medical waste/optimization of recycling, were each reported by more than one-third of survey respondents.
And almost half indicated that their practice or institution had increased capacity for telemedicine or telecommuting in response to climate change. Only 8% said their practice or institution had divested from fossil fuel stocks and/or bonds.
“There are a lot of sustainability-in-medicine solutions that are actually cost-neutral or cost-saving for practices,” said Dr. Rosenbach, who is a founder and co-chair of the AAD’s ERG on Climate Change and Environmental Issues.
Research in dermatology is starting to quantify the environmental impact of some of these changes. In a research letter also published in the British Journal of Dermatology, researchers from Cardiff University and the department of dermatology at University Hospital of Wales, described how they determined that reusable surgical packs used for skin surgery are more sustainable than single-use packs because of their reduced cost and reduced greenhouse gas emissions.
Such single-site reports are “early feeders” into what will become a stream of larger studies quantifying the impact of measures taken in dermatology, Dr. Rosenbach said.
Across medicine, there is evidence that health care professionals are now seeing climate change as a threat to their patients. In a multinational survey published last year in The Lancet Planetary Health, 77% of 3,977 participants said that climate change will cause a moderate or great deal of harm for their patients.
Climate change will be discussed at the AAD’s annual meeting in late March in a session devoted to the topic, and as part of a broader session on controversies in dermatology.
Dr. Rosenbach and two of the five authors of the dermatology research letter are members of the AAD’s ERG on climate change, but in the publication they noted that they were not writing on behalf of the AAD. None of the authors reported any disclosures, and there was no funding source for the survey.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Clinical data affirm dupilumab for chronic nasal polyps
In a specialty clinic, dupilumab (Dupixent) injections significantly improved symptoms for patients with chronic rhinosinusitis with nasal polyps, based on provisional data from more than 100 adults.
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a significant burden among working-age adults. Symptom control remains a challenge for many of these patients, and the cost in lost productivity and health care consumption can be substantial, write Rik J.L. van der Lans, MD, of the University of Amsterdam, and colleagues.
Dupilumab, a biologic that targets components of the type 2 inflammatory pathway, represents a new option that has shown effectiveness in clinical trials for regulatory approval, they said.
A new observational study tests dupilumab in patients who met criteria for biological treatment proposed in a recent major systematic review. The findings were published in the journal Allergy.
In the study, the researchers identified 131 adults older than 18 years (mean age 51.7) with CRSwNP treated at a single tertiary care center. Participants received 300 mg of dupilumab subcutaneous injection every 2 weeks for at least 12 weeks.
The primary outcomes were scores on several measures, including the SinoNasal Outcome Test-22 (SNOT-22, scale of 0-110), the bilateral Nasal Polyp Score (NPS, scale of 0-8), and the Sniffin’ Sticks-12 identification test (SSIT-12, scale of 0-6 anosmia, 7-10 hyposmia, 11-12 normosmia).
The mean scores on all three outcomes improved significantly from baseline to both 24 weeks and 48 weeks. Scores on the SNOT-22 improved from 52.4 at baseline to 18.5 and 16.8 at weeks 24 and 48, respectively. NPS improved from 5.4 at baseline to 1.6 and 1.0, respectively. SSIT-12 scores improved from 3.6 at baseline to 7.3 and 8.3, respectively.
At baseline, 95.8% of the patients had uncontrolled chronic rhinosinusitis, but at 24 and 48 weeks, respectively, 24.3% and 6.2% were uncontrolled.
Approximately half of the patients experienced treatment-emergent adverse events, but these were “mild and decreased in occurrence and intensity throughout treatment,” the researchers say.
For patients with a strong response, the researchers also tested an extension of the interval between doses to 4 weeks and 6 weeks, in a provisional indication of continued established control at these timepoints.
The study findings were limited by several factors, including the potential for selection bias, and data from only the first patient cohort, the researchers noted. However, the results were strengthened by the real-life context, standardized indications, and long-term follow up for almost a year, they said.
More research is needed on nonacademic patient cohorts, but the current data confirm the effectiveness of dupilumab as an add-on for difficult-to-treat CRSwNP, they concluded. The findings also validate the European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS2020) inclusion criteria for biologic treatment, they said.
The new study is important because of the need for verification of results from randomized controlled trials using real-world data, Dr. Van der Lans told this news organization.
“For example, differences in treatment efficacy might result from differing indication criteria, and the inclusion/exclusion criteria in the RCTs might have excluded patients one would encounter in daily practice,” he said. “With our prospective observational cohort, we are seeking to verify efficacy, monitor pharmacovigilance, and evaluate and advance the indication criteria and positioning of biologicals registered for CRSwNP, such as dupilumab.”
These cross-sectional results suggest dupilumab is more effective in preventing possibly harmful escape treatments, such as oral corticosteroids and/or surgery, than reported by the registration trials.
“Additionally, it appears possible to maintain established CRS-control during response-dependent, stepwise, interdose interval prolongation of up to 6 weeks, which is officially an off-label dosing interval,” he said. “This would greatly benefit patients’ treatment burden and direct costs,” he said. However, both findings require corroboration by anticipated longitudinal results in 2022, he noted.
The key message for clinicians in practice: “Biologicals like dupilumab are a potent and promising treatment for severe CRSwNP when conventional medical and surgical therapy fails,” he emphasized.
Looking ahead, important research objectives include head-on comparison studies of the diverse biological agents, establishing biomarkers to guide preferential therapy, and evaluating the economics of biologics compared with conventional therapy, Dr. Van der Lans added. Such research is vital not only for improving patient-centered care but to sustain the use of biologicals in a health-economic perspective.
One of the greatest criticisms of biologic therapy for CRSwNP is cost, particularly in a setting of ever-increasing health care costs. A recent review noted the average cost per year is greater than $30,000.
Real-life study verifies effectiveness
“As the authors pointed out, this is a real-life, prospective observational cohort with a decently large size, evaluating the therapeutic efficacy of add-on dupilumab,” said Seong H. Cho, MD, of the University of South Florida, Tampa, in an interview.
“Dupilumab is the first FDA-approved biologic to treat severe chronic rhinosinusitis with nasal polyps based on two phase 3 clinical trials,” said Dr. Cho, who was not involved with the study. “It has been more than 2 years since dupilumab was approved for severe CRSwNP by the FDA and EMA. This real-life, prospective, observational study with a decent size verified the efficacy of dupilumab as an add-on treatment when used with a proper indication such as EPOS2020 indication criteria.
“I am not surprised by the efficacy of dupilumab on severe CRSwNP, based on my clinical experience. My clinical observation is similar to the results of this study. This study verifies that dupilumab is highly efficacious in treating refractory and severe CRSwNP in a real-life setting by improving all subjective and objective clinical outcomes such as SNOT-22, NPS, and smell test score,” he said. The study also confirms that a stepwise, interdose interval prolongation from every 2-4 weeks for CRSwNP patients with good response should be a consideration for clinical practice, he added.
The cost-effectiveness of dupilumab is the main barrier to more consistent use, Dr. Cho said. “There is no evidence that dupilumab can change the course of the disease, and we don’t know how long patients need to be on this drug. Therefore, nasal polyps need to be refractory and severe enough to use dupilumab and other biologics,” he explained.
Consequently, proper indication criteria, such as the EPOS2020 indication criteria for biologics, should be established before initiating dupilumab, Dr. Cho noted.
“Generally, endoscopic sinus surgery would be preferred in sinus-surgery naive CRSwNP patients, unless surgery is contraindicated or refused by patients because of cost-effectiveness rather than the superior efficacy,” he said. “If surgery fails, then dupilumab can be considered. In addition, proper evaluation of nasal polyp severity would be important.”
“One should establish an objective NPS by endoscopic exam before initiation of dupilumab. This baseline score would be an important marker to assess the efficacy of dupilumab in the course of treatment.”
Monitoring of the NPS together with the patient’s symptom improvement would be essential to implementing a stepwise, interdose interval prolongation to reduce the cost, he emphasized.
“The most crucial additional research is establishing suitable biomarkers for the response of dupilumab and other biologics,” said Dr. Cho. “Overall, the performance of dupilumab seems to be good. But there are patients unresponsive to dupilumab, even more to other recently FDA-approved biologics for CRSwNP.”
Blood eosinophils and exhaled nitric oxide can be a good biomarker for type 2 asthma, Dr. Cho added. “Still, there is no evidence that these biomarkers are decent for CRSwNP, even though CRSwNP is mostly considered as type 2 disease. Therefore, it would be essential to find promising biomarkers for severe CRSwNP.”
Dr. Van der Lans disclosed serving as a consultant for GlaxoSmithKline, and several coauthors disclosed relationships with companies including Sanofi and Novartis. The patient registry from which the study population was drawn is cofunded by Sanofi and Novartis. Dr. Cho has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a specialty clinic, dupilumab (Dupixent) injections significantly improved symptoms for patients with chronic rhinosinusitis with nasal polyps, based on provisional data from more than 100 adults.
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a significant burden among working-age adults. Symptom control remains a challenge for many of these patients, and the cost in lost productivity and health care consumption can be substantial, write Rik J.L. van der Lans, MD, of the University of Amsterdam, and colleagues.
Dupilumab, a biologic that targets components of the type 2 inflammatory pathway, represents a new option that has shown effectiveness in clinical trials for regulatory approval, they said.
A new observational study tests dupilumab in patients who met criteria for biological treatment proposed in a recent major systematic review. The findings were published in the journal Allergy.
In the study, the researchers identified 131 adults older than 18 years (mean age 51.7) with CRSwNP treated at a single tertiary care center. Participants received 300 mg of dupilumab subcutaneous injection every 2 weeks for at least 12 weeks.
The primary outcomes were scores on several measures, including the SinoNasal Outcome Test-22 (SNOT-22, scale of 0-110), the bilateral Nasal Polyp Score (NPS, scale of 0-8), and the Sniffin’ Sticks-12 identification test (SSIT-12, scale of 0-6 anosmia, 7-10 hyposmia, 11-12 normosmia).
The mean scores on all three outcomes improved significantly from baseline to both 24 weeks and 48 weeks. Scores on the SNOT-22 improved from 52.4 at baseline to 18.5 and 16.8 at weeks 24 and 48, respectively. NPS improved from 5.4 at baseline to 1.6 and 1.0, respectively. SSIT-12 scores improved from 3.6 at baseline to 7.3 and 8.3, respectively.
At baseline, 95.8% of the patients had uncontrolled chronic rhinosinusitis, but at 24 and 48 weeks, respectively, 24.3% and 6.2% were uncontrolled.
Approximately half of the patients experienced treatment-emergent adverse events, but these were “mild and decreased in occurrence and intensity throughout treatment,” the researchers say.
For patients with a strong response, the researchers also tested an extension of the interval between doses to 4 weeks and 6 weeks, in a provisional indication of continued established control at these timepoints.
The study findings were limited by several factors, including the potential for selection bias, and data from only the first patient cohort, the researchers noted. However, the results were strengthened by the real-life context, standardized indications, and long-term follow up for almost a year, they said.
More research is needed on nonacademic patient cohorts, but the current data confirm the effectiveness of dupilumab as an add-on for difficult-to-treat CRSwNP, they concluded. The findings also validate the European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS2020) inclusion criteria for biologic treatment, they said.
The new study is important because of the need for verification of results from randomized controlled trials using real-world data, Dr. Van der Lans told this news organization.
“For example, differences in treatment efficacy might result from differing indication criteria, and the inclusion/exclusion criteria in the RCTs might have excluded patients one would encounter in daily practice,” he said. “With our prospective observational cohort, we are seeking to verify efficacy, monitor pharmacovigilance, and evaluate and advance the indication criteria and positioning of biologicals registered for CRSwNP, such as dupilumab.”
These cross-sectional results suggest dupilumab is more effective in preventing possibly harmful escape treatments, such as oral corticosteroids and/or surgery, than reported by the registration trials.
“Additionally, it appears possible to maintain established CRS-control during response-dependent, stepwise, interdose interval prolongation of up to 6 weeks, which is officially an off-label dosing interval,” he said. “This would greatly benefit patients’ treatment burden and direct costs,” he said. However, both findings require corroboration by anticipated longitudinal results in 2022, he noted.
The key message for clinicians in practice: “Biologicals like dupilumab are a potent and promising treatment for severe CRSwNP when conventional medical and surgical therapy fails,” he emphasized.
Looking ahead, important research objectives include head-on comparison studies of the diverse biological agents, establishing biomarkers to guide preferential therapy, and evaluating the economics of biologics compared with conventional therapy, Dr. Van der Lans added. Such research is vital not only for improving patient-centered care but to sustain the use of biologicals in a health-economic perspective.
One of the greatest criticisms of biologic therapy for CRSwNP is cost, particularly in a setting of ever-increasing health care costs. A recent review noted the average cost per year is greater than $30,000.
Real-life study verifies effectiveness
“As the authors pointed out, this is a real-life, prospective observational cohort with a decently large size, evaluating the therapeutic efficacy of add-on dupilumab,” said Seong H. Cho, MD, of the University of South Florida, Tampa, in an interview.
“Dupilumab is the first FDA-approved biologic to treat severe chronic rhinosinusitis with nasal polyps based on two phase 3 clinical trials,” said Dr. Cho, who was not involved with the study. “It has been more than 2 years since dupilumab was approved for severe CRSwNP by the FDA and EMA. This real-life, prospective, observational study with a decent size verified the efficacy of dupilumab as an add-on treatment when used with a proper indication such as EPOS2020 indication criteria.
“I am not surprised by the efficacy of dupilumab on severe CRSwNP, based on my clinical experience. My clinical observation is similar to the results of this study. This study verifies that dupilumab is highly efficacious in treating refractory and severe CRSwNP in a real-life setting by improving all subjective and objective clinical outcomes such as SNOT-22, NPS, and smell test score,” he said. The study also confirms that a stepwise, interdose interval prolongation from every 2-4 weeks for CRSwNP patients with good response should be a consideration for clinical practice, he added.
The cost-effectiveness of dupilumab is the main barrier to more consistent use, Dr. Cho said. “There is no evidence that dupilumab can change the course of the disease, and we don’t know how long patients need to be on this drug. Therefore, nasal polyps need to be refractory and severe enough to use dupilumab and other biologics,” he explained.
Consequently, proper indication criteria, such as the EPOS2020 indication criteria for biologics, should be established before initiating dupilumab, Dr. Cho noted.
“Generally, endoscopic sinus surgery would be preferred in sinus-surgery naive CRSwNP patients, unless surgery is contraindicated or refused by patients because of cost-effectiveness rather than the superior efficacy,” he said. “If surgery fails, then dupilumab can be considered. In addition, proper evaluation of nasal polyp severity would be important.”
“One should establish an objective NPS by endoscopic exam before initiation of dupilumab. This baseline score would be an important marker to assess the efficacy of dupilumab in the course of treatment.”
Monitoring of the NPS together with the patient’s symptom improvement would be essential to implementing a stepwise, interdose interval prolongation to reduce the cost, he emphasized.
“The most crucial additional research is establishing suitable biomarkers for the response of dupilumab and other biologics,” said Dr. Cho. “Overall, the performance of dupilumab seems to be good. But there are patients unresponsive to dupilumab, even more to other recently FDA-approved biologics for CRSwNP.”
Blood eosinophils and exhaled nitric oxide can be a good biomarker for type 2 asthma, Dr. Cho added. “Still, there is no evidence that these biomarkers are decent for CRSwNP, even though CRSwNP is mostly considered as type 2 disease. Therefore, it would be essential to find promising biomarkers for severe CRSwNP.”
Dr. Van der Lans disclosed serving as a consultant for GlaxoSmithKline, and several coauthors disclosed relationships with companies including Sanofi and Novartis. The patient registry from which the study population was drawn is cofunded by Sanofi and Novartis. Dr. Cho has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a specialty clinic, dupilumab (Dupixent) injections significantly improved symptoms for patients with chronic rhinosinusitis with nasal polyps, based on provisional data from more than 100 adults.
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a significant burden among working-age adults. Symptom control remains a challenge for many of these patients, and the cost in lost productivity and health care consumption can be substantial, write Rik J.L. van der Lans, MD, of the University of Amsterdam, and colleagues.
Dupilumab, a biologic that targets components of the type 2 inflammatory pathway, represents a new option that has shown effectiveness in clinical trials for regulatory approval, they said.
A new observational study tests dupilumab in patients who met criteria for biological treatment proposed in a recent major systematic review. The findings were published in the journal Allergy.
In the study, the researchers identified 131 adults older than 18 years (mean age 51.7) with CRSwNP treated at a single tertiary care center. Participants received 300 mg of dupilumab subcutaneous injection every 2 weeks for at least 12 weeks.
The primary outcomes were scores on several measures, including the SinoNasal Outcome Test-22 (SNOT-22, scale of 0-110), the bilateral Nasal Polyp Score (NPS, scale of 0-8), and the Sniffin’ Sticks-12 identification test (SSIT-12, scale of 0-6 anosmia, 7-10 hyposmia, 11-12 normosmia).
The mean scores on all three outcomes improved significantly from baseline to both 24 weeks and 48 weeks. Scores on the SNOT-22 improved from 52.4 at baseline to 18.5 and 16.8 at weeks 24 and 48, respectively. NPS improved from 5.4 at baseline to 1.6 and 1.0, respectively. SSIT-12 scores improved from 3.6 at baseline to 7.3 and 8.3, respectively.
At baseline, 95.8% of the patients had uncontrolled chronic rhinosinusitis, but at 24 and 48 weeks, respectively, 24.3% and 6.2% were uncontrolled.
Approximately half of the patients experienced treatment-emergent adverse events, but these were “mild and decreased in occurrence and intensity throughout treatment,” the researchers say.
For patients with a strong response, the researchers also tested an extension of the interval between doses to 4 weeks and 6 weeks, in a provisional indication of continued established control at these timepoints.
The study findings were limited by several factors, including the potential for selection bias, and data from only the first patient cohort, the researchers noted. However, the results were strengthened by the real-life context, standardized indications, and long-term follow up for almost a year, they said.
More research is needed on nonacademic patient cohorts, but the current data confirm the effectiveness of dupilumab as an add-on for difficult-to-treat CRSwNP, they concluded. The findings also validate the European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS2020) inclusion criteria for biologic treatment, they said.
The new study is important because of the need for verification of results from randomized controlled trials using real-world data, Dr. Van der Lans told this news organization.
“For example, differences in treatment efficacy might result from differing indication criteria, and the inclusion/exclusion criteria in the RCTs might have excluded patients one would encounter in daily practice,” he said. “With our prospective observational cohort, we are seeking to verify efficacy, monitor pharmacovigilance, and evaluate and advance the indication criteria and positioning of biologicals registered for CRSwNP, such as dupilumab.”
These cross-sectional results suggest dupilumab is more effective in preventing possibly harmful escape treatments, such as oral corticosteroids and/or surgery, than reported by the registration trials.
“Additionally, it appears possible to maintain established CRS-control during response-dependent, stepwise, interdose interval prolongation of up to 6 weeks, which is officially an off-label dosing interval,” he said. “This would greatly benefit patients’ treatment burden and direct costs,” he said. However, both findings require corroboration by anticipated longitudinal results in 2022, he noted.
The key message for clinicians in practice: “Biologicals like dupilumab are a potent and promising treatment for severe CRSwNP when conventional medical and surgical therapy fails,” he emphasized.
Looking ahead, important research objectives include head-on comparison studies of the diverse biological agents, establishing biomarkers to guide preferential therapy, and evaluating the economics of biologics compared with conventional therapy, Dr. Van der Lans added. Such research is vital not only for improving patient-centered care but to sustain the use of biologicals in a health-economic perspective.
One of the greatest criticisms of biologic therapy for CRSwNP is cost, particularly in a setting of ever-increasing health care costs. A recent review noted the average cost per year is greater than $30,000.
Real-life study verifies effectiveness
“As the authors pointed out, this is a real-life, prospective observational cohort with a decently large size, evaluating the therapeutic efficacy of add-on dupilumab,” said Seong H. Cho, MD, of the University of South Florida, Tampa, in an interview.
“Dupilumab is the first FDA-approved biologic to treat severe chronic rhinosinusitis with nasal polyps based on two phase 3 clinical trials,” said Dr. Cho, who was not involved with the study. “It has been more than 2 years since dupilumab was approved for severe CRSwNP by the FDA and EMA. This real-life, prospective, observational study with a decent size verified the efficacy of dupilumab as an add-on treatment when used with a proper indication such as EPOS2020 indication criteria.
“I am not surprised by the efficacy of dupilumab on severe CRSwNP, based on my clinical experience. My clinical observation is similar to the results of this study. This study verifies that dupilumab is highly efficacious in treating refractory and severe CRSwNP in a real-life setting by improving all subjective and objective clinical outcomes such as SNOT-22, NPS, and smell test score,” he said. The study also confirms that a stepwise, interdose interval prolongation from every 2-4 weeks for CRSwNP patients with good response should be a consideration for clinical practice, he added.
The cost-effectiveness of dupilumab is the main barrier to more consistent use, Dr. Cho said. “There is no evidence that dupilumab can change the course of the disease, and we don’t know how long patients need to be on this drug. Therefore, nasal polyps need to be refractory and severe enough to use dupilumab and other biologics,” he explained.
Consequently, proper indication criteria, such as the EPOS2020 indication criteria for biologics, should be established before initiating dupilumab, Dr. Cho noted.
“Generally, endoscopic sinus surgery would be preferred in sinus-surgery naive CRSwNP patients, unless surgery is contraindicated or refused by patients because of cost-effectiveness rather than the superior efficacy,” he said. “If surgery fails, then dupilumab can be considered. In addition, proper evaluation of nasal polyp severity would be important.”
“One should establish an objective NPS by endoscopic exam before initiation of dupilumab. This baseline score would be an important marker to assess the efficacy of dupilumab in the course of treatment.”
Monitoring of the NPS together with the patient’s symptom improvement would be essential to implementing a stepwise, interdose interval prolongation to reduce the cost, he emphasized.
“The most crucial additional research is establishing suitable biomarkers for the response of dupilumab and other biologics,” said Dr. Cho. “Overall, the performance of dupilumab seems to be good. But there are patients unresponsive to dupilumab, even more to other recently FDA-approved biologics for CRSwNP.”
Blood eosinophils and exhaled nitric oxide can be a good biomarker for type 2 asthma, Dr. Cho added. “Still, there is no evidence that these biomarkers are decent for CRSwNP, even though CRSwNP is mostly considered as type 2 disease. Therefore, it would be essential to find promising biomarkers for severe CRSwNP.”
Dr. Van der Lans disclosed serving as a consultant for GlaxoSmithKline, and several coauthors disclosed relationships with companies including Sanofi and Novartis. The patient registry from which the study population was drawn is cofunded by Sanofi and Novartis. Dr. Cho has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALLERGY
Sepsis common cause of ICU admissions in patients with MS
Sepsis is an alarmingly common cause behind ICU admissions in patients with multiple sclerosis (MS), a retrospective, population-based cohort study indicates.
Furthermore, it contributes to a disproportionately high percentage of the short-term mortality risk among patients with MS admitted to the ICU, findings also show. Short-term mortality risk was defined in the study as a combination of in-hospital death or discharge to hospice.
“We found that the risk of short-term mortality in critically ill patients with MS is four times higher among those with sepsis ... so sepsis appears to be comparatively more lethal among patients with MS than in the general population,” Lavi Oud, MD, professor of medicine, Texas Tech University HSC at the Permian Basin, Odessa, said in an email.
“[Although] the specific mechanisms underlying the markedly higher risk of sepsis among patients with MS compared to the general population remain to be fully elucidated ... it’s thought that the risk may stem from the dysfunction of the immune system in these patients related to MS itself and to the potentially adverse effect of the immunomodulating therapy we use in these patients,” he added.
The study was published online Jan. 11 in the Journal of Critical Care.
Sepsis rates
The Texas Inpatient Public Use Data File was used to identify adults with a diagnosis of MS admitted to the hospital between 2010 and 2017. Among the 19,837 patients with MS admitted to the ICU during the study interval, almost one-third (31.5%) had sepsis, investigators report. “The rate of sepsis among ICU admissions increased with age, ranging from 20.8% among those aged 18-44 to 39.4% among those aged 65 years or older,” investigators note.
The most common site of infection among MS patients admitted to the ICU were urinary in nature (65.2%), followed by respiratory (36.1%). A smaller proportion of infections (7.6%) involved the skin and soft tissues, researchers note. A full one-quarter of patients developed septic shock in response to their infection while the length of stay among patients with sepsis (mean of 10.9 days) was substantially longer than it was for those without sepsis (mean of 5.6 days), they observe.
At a mean total hospital cost of $121,797 for each ICU patient with sepsis, the cost of caring for each patient was nearly twofold higher than the mean total cost of taking care of ICU patients without sepsis (mean total cost, $65,179). On adjusted analysis, sepsis was associated with a 42.7% (95% confidence interval, 38.9-46.5; P < .0001) longer length of hospital stay and a 26.2% (95% CI, 23.1-29.1; P < .0001) higher total hospital cost compared with patients without sepsis, the authors point out.
Indeed, ICU admissions with sepsis accounted for 47.3% of all hospital days and for 46.1% of the aggregate hospital charges among all MS patients admitted to the ICU.
“The adjusted probability of short-term mortality was 13.4% (95% CI, 13.0-13.7) among ICU admissions with sepsis and 3.3% (95% CI, 3.2-3.4) among ICU admissions without sepsis,” the authors report.
This translated into a 44% higher risk of short-term mortality at an adjusted odds ratio of 1.44 (95% CI, 1.23-1.69; P < .0001) for those with sepsis, compared with those without, they add. Among all ICU admissions, sepsis was reported in over two-thirds of documented short-term mortality events. The risk of short-term mortality was also almost threefold higher among patients with sepsis who were age 65 years and older compared with patients aged 18-44.
As Dr. Oud noted, there is no specific test for sepsis, and it can initially present in an atypical manner, especially in older, frailer, chronically ill patients as well as in patients with immune dysfunction. “Thus, considering sepsis as a possible cause of new deterioration in a patient’s condition is essential, along with the timely start of sepsis-related care,” Dr. Oud observed.
A limitation of the study was that the dataset did not include information on the type of MS a patient had, the duration of their illness, the treatment received, the level of disease activity, or the level of disability.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis is an alarmingly common cause behind ICU admissions in patients with multiple sclerosis (MS), a retrospective, population-based cohort study indicates.
Furthermore, it contributes to a disproportionately high percentage of the short-term mortality risk among patients with MS admitted to the ICU, findings also show. Short-term mortality risk was defined in the study as a combination of in-hospital death or discharge to hospice.
“We found that the risk of short-term mortality in critically ill patients with MS is four times higher among those with sepsis ... so sepsis appears to be comparatively more lethal among patients with MS than in the general population,” Lavi Oud, MD, professor of medicine, Texas Tech University HSC at the Permian Basin, Odessa, said in an email.
“[Although] the specific mechanisms underlying the markedly higher risk of sepsis among patients with MS compared to the general population remain to be fully elucidated ... it’s thought that the risk may stem from the dysfunction of the immune system in these patients related to MS itself and to the potentially adverse effect of the immunomodulating therapy we use in these patients,” he added.
The study was published online Jan. 11 in the Journal of Critical Care.
Sepsis rates
The Texas Inpatient Public Use Data File was used to identify adults with a diagnosis of MS admitted to the hospital between 2010 and 2017. Among the 19,837 patients with MS admitted to the ICU during the study interval, almost one-third (31.5%) had sepsis, investigators report. “The rate of sepsis among ICU admissions increased with age, ranging from 20.8% among those aged 18-44 to 39.4% among those aged 65 years or older,” investigators note.
The most common site of infection among MS patients admitted to the ICU were urinary in nature (65.2%), followed by respiratory (36.1%). A smaller proportion of infections (7.6%) involved the skin and soft tissues, researchers note. A full one-quarter of patients developed septic shock in response to their infection while the length of stay among patients with sepsis (mean of 10.9 days) was substantially longer than it was for those without sepsis (mean of 5.6 days), they observe.
At a mean total hospital cost of $121,797 for each ICU patient with sepsis, the cost of caring for each patient was nearly twofold higher than the mean total cost of taking care of ICU patients without sepsis (mean total cost, $65,179). On adjusted analysis, sepsis was associated with a 42.7% (95% confidence interval, 38.9-46.5; P < .0001) longer length of hospital stay and a 26.2% (95% CI, 23.1-29.1; P < .0001) higher total hospital cost compared with patients without sepsis, the authors point out.
Indeed, ICU admissions with sepsis accounted for 47.3% of all hospital days and for 46.1% of the aggregate hospital charges among all MS patients admitted to the ICU.
“The adjusted probability of short-term mortality was 13.4% (95% CI, 13.0-13.7) among ICU admissions with sepsis and 3.3% (95% CI, 3.2-3.4) among ICU admissions without sepsis,” the authors report.
This translated into a 44% higher risk of short-term mortality at an adjusted odds ratio of 1.44 (95% CI, 1.23-1.69; P < .0001) for those with sepsis, compared with those without, they add. Among all ICU admissions, sepsis was reported in over two-thirds of documented short-term mortality events. The risk of short-term mortality was also almost threefold higher among patients with sepsis who were age 65 years and older compared with patients aged 18-44.
As Dr. Oud noted, there is no specific test for sepsis, and it can initially present in an atypical manner, especially in older, frailer, chronically ill patients as well as in patients with immune dysfunction. “Thus, considering sepsis as a possible cause of new deterioration in a patient’s condition is essential, along with the timely start of sepsis-related care,” Dr. Oud observed.
A limitation of the study was that the dataset did not include information on the type of MS a patient had, the duration of their illness, the treatment received, the level of disease activity, or the level of disability.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis is an alarmingly common cause behind ICU admissions in patients with multiple sclerosis (MS), a retrospective, population-based cohort study indicates.
Furthermore, it contributes to a disproportionately high percentage of the short-term mortality risk among patients with MS admitted to the ICU, findings also show. Short-term mortality risk was defined in the study as a combination of in-hospital death or discharge to hospice.
“We found that the risk of short-term mortality in critically ill patients with MS is four times higher among those with sepsis ... so sepsis appears to be comparatively more lethal among patients with MS than in the general population,” Lavi Oud, MD, professor of medicine, Texas Tech University HSC at the Permian Basin, Odessa, said in an email.
“[Although] the specific mechanisms underlying the markedly higher risk of sepsis among patients with MS compared to the general population remain to be fully elucidated ... it’s thought that the risk may stem from the dysfunction of the immune system in these patients related to MS itself and to the potentially adverse effect of the immunomodulating therapy we use in these patients,” he added.
The study was published online Jan. 11 in the Journal of Critical Care.
Sepsis rates
The Texas Inpatient Public Use Data File was used to identify adults with a diagnosis of MS admitted to the hospital between 2010 and 2017. Among the 19,837 patients with MS admitted to the ICU during the study interval, almost one-third (31.5%) had sepsis, investigators report. “The rate of sepsis among ICU admissions increased with age, ranging from 20.8% among those aged 18-44 to 39.4% among those aged 65 years or older,” investigators note.
The most common site of infection among MS patients admitted to the ICU were urinary in nature (65.2%), followed by respiratory (36.1%). A smaller proportion of infections (7.6%) involved the skin and soft tissues, researchers note. A full one-quarter of patients developed septic shock in response to their infection while the length of stay among patients with sepsis (mean of 10.9 days) was substantially longer than it was for those without sepsis (mean of 5.6 days), they observe.
At a mean total hospital cost of $121,797 for each ICU patient with sepsis, the cost of caring for each patient was nearly twofold higher than the mean total cost of taking care of ICU patients without sepsis (mean total cost, $65,179). On adjusted analysis, sepsis was associated with a 42.7% (95% confidence interval, 38.9-46.5; P < .0001) longer length of hospital stay and a 26.2% (95% CI, 23.1-29.1; P < .0001) higher total hospital cost compared with patients without sepsis, the authors point out.
Indeed, ICU admissions with sepsis accounted for 47.3% of all hospital days and for 46.1% of the aggregate hospital charges among all MS patients admitted to the ICU.
“The adjusted probability of short-term mortality was 13.4% (95% CI, 13.0-13.7) among ICU admissions with sepsis and 3.3% (95% CI, 3.2-3.4) among ICU admissions without sepsis,” the authors report.
This translated into a 44% higher risk of short-term mortality at an adjusted odds ratio of 1.44 (95% CI, 1.23-1.69; P < .0001) for those with sepsis, compared with those without, they add. Among all ICU admissions, sepsis was reported in over two-thirds of documented short-term mortality events. The risk of short-term mortality was also almost threefold higher among patients with sepsis who were age 65 years and older compared with patients aged 18-44.
As Dr. Oud noted, there is no specific test for sepsis, and it can initially present in an atypical manner, especially in older, frailer, chronically ill patients as well as in patients with immune dysfunction. “Thus, considering sepsis as a possible cause of new deterioration in a patient’s condition is essential, along with the timely start of sepsis-related care,” Dr. Oud observed.
A limitation of the study was that the dataset did not include information on the type of MS a patient had, the duration of their illness, the treatment received, the level of disease activity, or the level of disability.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CRITICAL CARE
Sarcoidosis Presenting as Telangiectatic Macules
To the Editor:
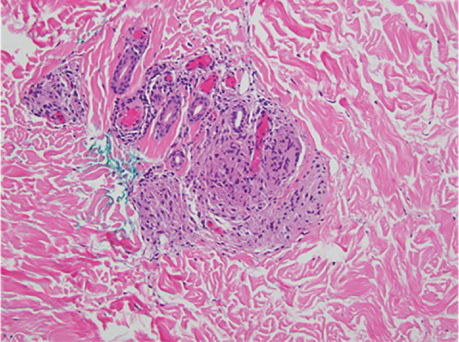
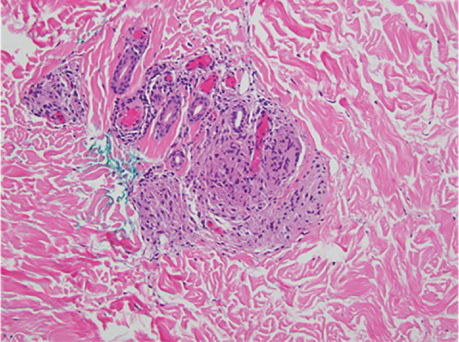
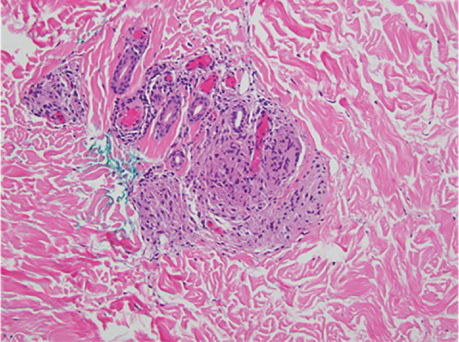
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
To the Editor:
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
To the Editor:
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
Practice Points
- Cutaneous manifestations of sarcoidosis can encompass numerous morphologies. A high degree of suspicion should be maintained for any uncertain dermatologic presentation.
- Although papular eruptions are the most common cutaneous findings in sarcoidosis, this case report illustrates a less common vascular-appearing presentation.
- A systemic workup is indicated in any presentation of sarcoidosis.
Medicaid expansion benefits some colorectal patients, others not so lucky
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
FROM THE GI CANCERS SYMPOSIUM 2022
Male alopecia agents ranked by efficacy in meta-analysis
While up to 90% of men experience AGA in their lifetime, only three therapies are currently approved for treatment of the condition by the Food and Drug Administration – topical minoxidil, oral finasteride 1 mg, and low-level light therapy.
However, with common use of off-label oral minoxidil, as well as oral dutasteride and higher doses of oral finasteride, the latter two being 5-alpha reductase inhibitors, Aditya K. Gupta, MD, PhD, of Mediprobe Research, in London, Ont., and colleagues sought to compare the data on the three agents. Their results were published in JAMA Dermatology.
They note that, while there have been recent comparisons between oral and topical minoxidil, “to our knowledge no study has determined the comparative effectiveness of these 2 [formulations] with that of local and systemic dutasteride and finasteride.”
For the meta-analysis, the authors identified 23 studies meeting their criteria, involving patients with mean ages ranging from 22.8 to 41.8 years.
For the primary endpoint of the greatest increases in total hair count at 24 weeks, the analysis showed the 0.5-mg/day dose of dutasteride topped the list, with significantly greater efficacy, compared with 1 mg/day of finasteride (mean difference, 7.1 hairs per cm2).
The 0.5-mg/d dutasteride dose also showed higher efficacy than oral minoxidil at 0.25 mg/day (mean difference, 23.7 hairs per cm2) and 5 mg/day (mean difference, 15.0 hairs per cm2) and topical minoxidil at 2% (mean difference, 8.5 hairs per cm2).
For the secondary endpoint of the greatest increase in terminal hair count at 24 weeks, the 5-mg/day dose of minoxidil had significantly greater efficacy compared with the 0.25-mg/day dose of the drug, as well as with minoxidil’s 2% and 5% topical formulations.
The minoxidil 5-mg/day dose was also significantly more effective than 1 mg/day of finasteride for terminal hair count at 24 weeks.
In longer-term outcomes at 48 weeks, the greatest increase in total hair count at 48 weeks was observed with 5 mg/day of finasteride, which was significantly more effective, compared with 2% topical minoxidil.
And the greatest increase in terminal hair count at 48 weeks was observed with 1 mg/day of oral finasteride, which was significantly more effective than 2% as well as 5% topical minoxidil.
Based on the results, the authors ranked the agents in a decreasing order of efficacy: 0.5 mg/day of oral dutasteride, 5 mg/day of oral finasteride, 5 mg/day of oral minoxidil, 1 mg/day of oral finasteride, 5% topical minoxidil, 2% topical minoxidil, and 0.25 mg/day of oral minoxidil.
Commenting on the analysis in an accompanying editorial, Kathie P. Huang, MD, of the department of dermatology, Brigham and Women’s Hospital, Boston, and Maryanne M. Senna, MD, of the department of dermatology, Massachusetts General Hospital, Boston, said the results, in general, are consistent with their experiences, noting that 2% minoxidil is typically not used in men.
They noted that, “although topical minoxidil ranked higher than the very-low-dose 0.25 mg oral minoxidil, our personal experience is that oral minoxidil at doses of 1.25 mg to 5 mg are far superior to topical minoxidil for treating AGA.”
Adverse event considerations important
Importantly, however, strong consideration needs to be given to adverse-event profiles, as well as patient comorbidities in selecting agents, the editorial authors asserted.
With 1 mg finasteride, for instance, potential adverse events include decreased libido, erectile dysfunction, decreased ejaculatory volume, reduction in sperm count, testicular pain, depression, and gynecomastia, they noted.
And while finasteride appears to be associated with a decreased risk of prostate cancer, those receiving the drug who do develop prostate cancer may be diagnosed with higher-grade prostate cancer; however, that “might be related to tissue sampling artifact,” the editorial authors said.
Less has been published on dutasteride’s adverse-event profile, and that, in itself, is a concern.
Overall, “as more direct-to-consumer companies treating male AGA emerge, it is especially important that the potential risks of these medications be made clear to patients,” they added.
Further commenting on the analysis to this news organization, Antonella Tosti, MD, the Fredric Brandt Endowed Professor of Dermatology and Cutaneous Surgery at the University of Miami, said the study offers some important insights – and caveats.
“I think this is a very interesting study, but you have to consider what works for your patients,” she said.
Dr. Tosti noted that the 5-mg dose of minoxidil is a concern in terms of side effects. “That dose is pretty high and could feasibly cause some hypertrichosis, which can be a concern to men as well as women.”
She agrees that the lack of data on side effects with dutasteride is also a concern, especially in light of some of the known side effects with other agents.
“That’s why I don’t use it very much in younger patients – because I’m afraid it could potentially affect their fertility,” Dr. Tosti said.
In general, Dr. Tosti said she finds a combination of agents provides the best results, as many clinicians use.
“I find dutasteride (0.5 mg/day) plus oral minoxidil (1-2.5 mg/day) plus topical 5% minoxidil is the best combination,” she said.
The authors and Dr. Tosti disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While up to 90% of men experience AGA in their lifetime, only three therapies are currently approved for treatment of the condition by the Food and Drug Administration – topical minoxidil, oral finasteride 1 mg, and low-level light therapy.
However, with common use of off-label oral minoxidil, as well as oral dutasteride and higher doses of oral finasteride, the latter two being 5-alpha reductase inhibitors, Aditya K. Gupta, MD, PhD, of Mediprobe Research, in London, Ont., and colleagues sought to compare the data on the three agents. Their results were published in JAMA Dermatology.
They note that, while there have been recent comparisons between oral and topical minoxidil, “to our knowledge no study has determined the comparative effectiveness of these 2 [formulations] with that of local and systemic dutasteride and finasteride.”
For the meta-analysis, the authors identified 23 studies meeting their criteria, involving patients with mean ages ranging from 22.8 to 41.8 years.
For the primary endpoint of the greatest increases in total hair count at 24 weeks, the analysis showed the 0.5-mg/day dose of dutasteride topped the list, with significantly greater efficacy, compared with 1 mg/day of finasteride (mean difference, 7.1 hairs per cm2).
The 0.5-mg/d dutasteride dose also showed higher efficacy than oral minoxidil at 0.25 mg/day (mean difference, 23.7 hairs per cm2) and 5 mg/day (mean difference, 15.0 hairs per cm2) and topical minoxidil at 2% (mean difference, 8.5 hairs per cm2).
For the secondary endpoint of the greatest increase in terminal hair count at 24 weeks, the 5-mg/day dose of minoxidil had significantly greater efficacy compared with the 0.25-mg/day dose of the drug, as well as with minoxidil’s 2% and 5% topical formulations.
The minoxidil 5-mg/day dose was also significantly more effective than 1 mg/day of finasteride for terminal hair count at 24 weeks.
In longer-term outcomes at 48 weeks, the greatest increase in total hair count at 48 weeks was observed with 5 mg/day of finasteride, which was significantly more effective, compared with 2% topical minoxidil.
And the greatest increase in terminal hair count at 48 weeks was observed with 1 mg/day of oral finasteride, which was significantly more effective than 2% as well as 5% topical minoxidil.
Based on the results, the authors ranked the agents in a decreasing order of efficacy: 0.5 mg/day of oral dutasteride, 5 mg/day of oral finasteride, 5 mg/day of oral minoxidil, 1 mg/day of oral finasteride, 5% topical minoxidil, 2% topical minoxidil, and 0.25 mg/day of oral minoxidil.
Commenting on the analysis in an accompanying editorial, Kathie P. Huang, MD, of the department of dermatology, Brigham and Women’s Hospital, Boston, and Maryanne M. Senna, MD, of the department of dermatology, Massachusetts General Hospital, Boston, said the results, in general, are consistent with their experiences, noting that 2% minoxidil is typically not used in men.
They noted that, “although topical minoxidil ranked higher than the very-low-dose 0.25 mg oral minoxidil, our personal experience is that oral minoxidil at doses of 1.25 mg to 5 mg are far superior to topical minoxidil for treating AGA.”
Adverse event considerations important
Importantly, however, strong consideration needs to be given to adverse-event profiles, as well as patient comorbidities in selecting agents, the editorial authors asserted.
With 1 mg finasteride, for instance, potential adverse events include decreased libido, erectile dysfunction, decreased ejaculatory volume, reduction in sperm count, testicular pain, depression, and gynecomastia, they noted.
And while finasteride appears to be associated with a decreased risk of prostate cancer, those receiving the drug who do develop prostate cancer may be diagnosed with higher-grade prostate cancer; however, that “might be related to tissue sampling artifact,” the editorial authors said.
Less has been published on dutasteride’s adverse-event profile, and that, in itself, is a concern.
Overall, “as more direct-to-consumer companies treating male AGA emerge, it is especially important that the potential risks of these medications be made clear to patients,” they added.
Further commenting on the analysis to this news organization, Antonella Tosti, MD, the Fredric Brandt Endowed Professor of Dermatology and Cutaneous Surgery at the University of Miami, said the study offers some important insights – and caveats.
“I think this is a very interesting study, but you have to consider what works for your patients,” she said.
Dr. Tosti noted that the 5-mg dose of minoxidil is a concern in terms of side effects. “That dose is pretty high and could feasibly cause some hypertrichosis, which can be a concern to men as well as women.”
She agrees that the lack of data on side effects with dutasteride is also a concern, especially in light of some of the known side effects with other agents.
“That’s why I don’t use it very much in younger patients – because I’m afraid it could potentially affect their fertility,” Dr. Tosti said.
In general, Dr. Tosti said she finds a combination of agents provides the best results, as many clinicians use.
“I find dutasteride (0.5 mg/day) plus oral minoxidil (1-2.5 mg/day) plus topical 5% minoxidil is the best combination,” she said.
The authors and Dr. Tosti disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While up to 90% of men experience AGA in their lifetime, only three therapies are currently approved for treatment of the condition by the Food and Drug Administration – topical minoxidil, oral finasteride 1 mg, and low-level light therapy.
However, with common use of off-label oral minoxidil, as well as oral dutasteride and higher doses of oral finasteride, the latter two being 5-alpha reductase inhibitors, Aditya K. Gupta, MD, PhD, of Mediprobe Research, in London, Ont., and colleagues sought to compare the data on the three agents. Their results were published in JAMA Dermatology.
They note that, while there have been recent comparisons between oral and topical minoxidil, “to our knowledge no study has determined the comparative effectiveness of these 2 [formulations] with that of local and systemic dutasteride and finasteride.”
For the meta-analysis, the authors identified 23 studies meeting their criteria, involving patients with mean ages ranging from 22.8 to 41.8 years.
For the primary endpoint of the greatest increases in total hair count at 24 weeks, the analysis showed the 0.5-mg/day dose of dutasteride topped the list, with significantly greater efficacy, compared with 1 mg/day of finasteride (mean difference, 7.1 hairs per cm2).
The 0.5-mg/d dutasteride dose also showed higher efficacy than oral minoxidil at 0.25 mg/day (mean difference, 23.7 hairs per cm2) and 5 mg/day (mean difference, 15.0 hairs per cm2) and topical minoxidil at 2% (mean difference, 8.5 hairs per cm2).
For the secondary endpoint of the greatest increase in terminal hair count at 24 weeks, the 5-mg/day dose of minoxidil had significantly greater efficacy compared with the 0.25-mg/day dose of the drug, as well as with minoxidil’s 2% and 5% topical formulations.
The minoxidil 5-mg/day dose was also significantly more effective than 1 mg/day of finasteride for terminal hair count at 24 weeks.
In longer-term outcomes at 48 weeks, the greatest increase in total hair count at 48 weeks was observed with 5 mg/day of finasteride, which was significantly more effective, compared with 2% topical minoxidil.
And the greatest increase in terminal hair count at 48 weeks was observed with 1 mg/day of oral finasteride, which was significantly more effective than 2% as well as 5% topical minoxidil.
Based on the results, the authors ranked the agents in a decreasing order of efficacy: 0.5 mg/day of oral dutasteride, 5 mg/day of oral finasteride, 5 mg/day of oral minoxidil, 1 mg/day of oral finasteride, 5% topical minoxidil, 2% topical minoxidil, and 0.25 mg/day of oral minoxidil.
Commenting on the analysis in an accompanying editorial, Kathie P. Huang, MD, of the department of dermatology, Brigham and Women’s Hospital, Boston, and Maryanne M. Senna, MD, of the department of dermatology, Massachusetts General Hospital, Boston, said the results, in general, are consistent with their experiences, noting that 2% minoxidil is typically not used in men.
They noted that, “although topical minoxidil ranked higher than the very-low-dose 0.25 mg oral minoxidil, our personal experience is that oral minoxidil at doses of 1.25 mg to 5 mg are far superior to topical minoxidil for treating AGA.”
Adverse event considerations important
Importantly, however, strong consideration needs to be given to adverse-event profiles, as well as patient comorbidities in selecting agents, the editorial authors asserted.
With 1 mg finasteride, for instance, potential adverse events include decreased libido, erectile dysfunction, decreased ejaculatory volume, reduction in sperm count, testicular pain, depression, and gynecomastia, they noted.
And while finasteride appears to be associated with a decreased risk of prostate cancer, those receiving the drug who do develop prostate cancer may be diagnosed with higher-grade prostate cancer; however, that “might be related to tissue sampling artifact,” the editorial authors said.
Less has been published on dutasteride’s adverse-event profile, and that, in itself, is a concern.
Overall, “as more direct-to-consumer companies treating male AGA emerge, it is especially important that the potential risks of these medications be made clear to patients,” they added.
Further commenting on the analysis to this news organization, Antonella Tosti, MD, the Fredric Brandt Endowed Professor of Dermatology and Cutaneous Surgery at the University of Miami, said the study offers some important insights – and caveats.
“I think this is a very interesting study, but you have to consider what works for your patients,” she said.
Dr. Tosti noted that the 5-mg dose of minoxidil is a concern in terms of side effects. “That dose is pretty high and could feasibly cause some hypertrichosis, which can be a concern to men as well as women.”
She agrees that the lack of data on side effects with dutasteride is also a concern, especially in light of some of the known side effects with other agents.
“That’s why I don’t use it very much in younger patients – because I’m afraid it could potentially affect their fertility,” Dr. Tosti said.
In general, Dr. Tosti said she finds a combination of agents provides the best results, as many clinicians use.
“I find dutasteride (0.5 mg/day) plus oral minoxidil (1-2.5 mg/day) plus topical 5% minoxidil is the best combination,” she said.
The authors and Dr. Tosti disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
President Biden’s ‘Cancer Moonshot’ to be relaunched
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
The “Cancer Moonshot” is about to be relaunched.
In a White House briefing, President Joe Biden announced that he is “reigniting” the initiative he spearheaded when he was vice president during the Obama administration.
During the livestreamed event, the president discussed his plans to bring a “fierce sense of urgency” to the fight against cancer and better support patients with cancer and their families.
He emphasized that cancer is one of the truly bipartisan issues. There is strong support from both “sides of the aisle,” he said, and he sees it as an issue that can bring the country together.
“We can do this. I promise you, we can do this. For all those we lost, for all those we miss. We can end cancer as we know it,” he said. “This is a presidential White House priority.”
The aim is to reduce the death rate from cancer by at least 50% over the next 25 years.
There is also a proposal to create the Advanced Research Projects Agency for Health, which would focus on driving cutting-edge innovation in health research.
Part of the plan is to assemble a “cancer cabinet” that includes 18 federal departments, agencies, and offices, including leaders from the departments of Health & Human Services, Veterans Affairs, Defense, Energy, and Agriculture.
At present, there are few details about the new program or how it will be funded.
Presumably more will be revealed at the Cancer Moonshot Summit being planned, as well as on a planned new website where people can track its progress.
President priority
Cancer Moonshot began back in 2016, when during his last State of the Union Address, former President Barack Obama announced the ambitious initiative. A few days later, Obama asked Congress for $1 billion to send cancer to the moon, and he put Biden, then vice president, in charge of “mission control” in the remaining months of the administration.
The new initiative will be headed by Danielle Carnival, PhD, who serves in the White House Office of Science and Technology Policy and has been appointed as White House Cancer Moonshot coordinator.
At the briefing, Mr. Biden and Vice President Kamala Harris spoke about losing family members to cancer. The president spoke about his eldest son, Beau, who died from brain cancer when he was 46 years old, while Ms. Harris spoke about her mother, Shyamala Gopalan, a breast cancer researcher who died of colon cancer in 2009.
Accolades but a bit of caution
The president’s speech was applauded by many cancer groups, both professional organizations and patient advocacy groups.
Karen E. Knudsen, PhD, chief executive officer of the American Cancer Society and its advocacy affiliate, the American Cancer Society Cancer Action Network, commended Mr. Biden for reigniting Cancer Moonshot.
“In 2022 alone, there will be an estimated 1.9 million people diagnosed with cancer and more than 600,000 people in the U.S. will die. Marshaling the resources of the federal government will be critical in our ability to reduce death and suffering from this disease,” she said.
The American Society for Radiation Oncology issued a press release, saying: “On behalf of radiation oncologists who treat people with cancer every day, we support the Biden-Harris administration’s move to drastically reduce the number of cancer deaths in the United States and improve the lives of people diagnosed with this disease.
“We believe the administration’s commitment to expand cancer prevention efforts and to increase equitable access to screenings and treatments will help mitigate some of the negative impact of the COVID-19 pandemic,” the society added.
At the American Association for Cancer Research, Chief Executive Officer Margaret Foti, MD, PhD, said she was thrilled to hear the announcement after the devastating interruptions in cancer research and patient care over the past 2 years.
“The reignited Cancer Moonshot will provide an important framework to help improve cancer prevention strategies, increase cancer screenings and early detection, reduce cancer disparities, and propel new lifesaving cures for patients with cancer,” she said.
However, increased funding from Congress will be needed for these goals to be achieved, she emphasized.
A version of this article first appeared on Medscape.com.
CDC releases updated draft guidance on opioid prescribing
The Centers for Disease Controls and Prevention has released a draft update of its current Clinical Practice Guidelines for Prescribing Opioids for pain management and is asking for public comment before moving forward.
The last guidance on this topic was released in 2016 and, among other things, noted that clinicians should be cautious when considering increasing dosage of opioids to 50 or more morphine milligram equivalents (MME)/day and should avoid increasing to a dose of 90 or more MME/day. It also noted that 3 days or less “will often be sufficient” regarding the quantity of lowest effective dose of immediate-release opioids to be prescribed for acute pain – and that more than 7 days “will rarely be needed.”
In the new report from the CDC’s National Center for Injury Prevention and Control (NCIPC), those dose limits have been replaced with the suggestion that clinicians use their best judgement – albeit still urging conservative use and even the possibility of nonopioid treatments.
The updated recommendations are now open for public comment via the Federal Register’s website through April 11.
“This comment period provides another critical opportunity for diverse audiences to offer their perspective on the draft clinical practice guideline,” Christopher M. Jones, PharmD, DrPH, acting director for the NCIPC, said in a release.
“We want to hear many voices from the public, including people living with pain and health care providers who help their patients manage pain,” Dr. Jones added.
Outpatient recommendations
The CDC noted that the updated guidance provides “evidence-based recommendations” for treatment of adults with acute, subacute, or chronic pain. It does not include guidance for managing pain related to sickle cell disease, cancer, or palliative care.
It is aimed at primary care clinicians and others who manage pain in an outpatient setting, including in dental and postsurgical practices and for those discharging patients from emergency departments. It does not apply to inpatient care.
The draft guidance includes 12 recommendations focused on four key areas:
- Helping clinicians determine whether or not to initiate opioid treatment for pain
- Opioid selection and dosage
- Duration of use and follow-up
- Assessing risk and addressing potential harms from use
The overall aim “is to ensure people have access to safe, accessible, and effective pain management that improves their function and quality of life while illuminating and reducing risks associated with prescription opioids and ultimately reducing the consequences of prescription opioid misuse and overdose,” the CDC notes.
In addition, the guidance itself “is intended to be a clinical tool to improve communication between providers and patients and empower them to make informed, patient-centered decisions,” the agency said in a press release.
It added that the new recommendations “are not intended to be applied as inflexible standards of care.” Rather, it is intended as a guide to support health care providers in their clinical decisionmaking as they provide individualized patient care.
Patients, caregivers, and providers are invited to submit comments over the next 60 days through the Federal Register docket.
“It is vitally important to CDC that we receive, process, and understand public feedback during the guideline update process,” the agency noted.
“The ultimate goal of this clinical practice guideline is to help people set and achieve personal goals to reduce their pain and improve their function and quality of life. Getting feedback from the public is essential to achieving this goal,” Dr. Jones said.
A version of this article first appeared on Medscape.com.
The Centers for Disease Controls and Prevention has released a draft update of its current Clinical Practice Guidelines for Prescribing Opioids for pain management and is asking for public comment before moving forward.
The last guidance on this topic was released in 2016 and, among other things, noted that clinicians should be cautious when considering increasing dosage of opioids to 50 or more morphine milligram equivalents (MME)/day and should avoid increasing to a dose of 90 or more MME/day. It also noted that 3 days or less “will often be sufficient” regarding the quantity of lowest effective dose of immediate-release opioids to be prescribed for acute pain – and that more than 7 days “will rarely be needed.”
In the new report from the CDC’s National Center for Injury Prevention and Control (NCIPC), those dose limits have been replaced with the suggestion that clinicians use their best judgement – albeit still urging conservative use and even the possibility of nonopioid treatments.
The updated recommendations are now open for public comment via the Federal Register’s website through April 11.
“This comment period provides another critical opportunity for diverse audiences to offer their perspective on the draft clinical practice guideline,” Christopher M. Jones, PharmD, DrPH, acting director for the NCIPC, said in a release.
“We want to hear many voices from the public, including people living with pain and health care providers who help their patients manage pain,” Dr. Jones added.
Outpatient recommendations
The CDC noted that the updated guidance provides “evidence-based recommendations” for treatment of adults with acute, subacute, or chronic pain. It does not include guidance for managing pain related to sickle cell disease, cancer, or palliative care.
It is aimed at primary care clinicians and others who manage pain in an outpatient setting, including in dental and postsurgical practices and for those discharging patients from emergency departments. It does not apply to inpatient care.
The draft guidance includes 12 recommendations focused on four key areas:
- Helping clinicians determine whether or not to initiate opioid treatment for pain
- Opioid selection and dosage
- Duration of use and follow-up
- Assessing risk and addressing potential harms from use
The overall aim “is to ensure people have access to safe, accessible, and effective pain management that improves their function and quality of life while illuminating and reducing risks associated with prescription opioids and ultimately reducing the consequences of prescription opioid misuse and overdose,” the CDC notes.
In addition, the guidance itself “is intended to be a clinical tool to improve communication between providers and patients and empower them to make informed, patient-centered decisions,” the agency said in a press release.
It added that the new recommendations “are not intended to be applied as inflexible standards of care.” Rather, it is intended as a guide to support health care providers in their clinical decisionmaking as they provide individualized patient care.
Patients, caregivers, and providers are invited to submit comments over the next 60 days through the Federal Register docket.
“It is vitally important to CDC that we receive, process, and understand public feedback during the guideline update process,” the agency noted.
“The ultimate goal of this clinical practice guideline is to help people set and achieve personal goals to reduce their pain and improve their function and quality of life. Getting feedback from the public is essential to achieving this goal,” Dr. Jones said.
A version of this article first appeared on Medscape.com.
The Centers for Disease Controls and Prevention has released a draft update of its current Clinical Practice Guidelines for Prescribing Opioids for pain management and is asking for public comment before moving forward.
The last guidance on this topic was released in 2016 and, among other things, noted that clinicians should be cautious when considering increasing dosage of opioids to 50 or more morphine milligram equivalents (MME)/day and should avoid increasing to a dose of 90 or more MME/day. It also noted that 3 days or less “will often be sufficient” regarding the quantity of lowest effective dose of immediate-release opioids to be prescribed for acute pain – and that more than 7 days “will rarely be needed.”
In the new report from the CDC’s National Center for Injury Prevention and Control (NCIPC), those dose limits have been replaced with the suggestion that clinicians use their best judgement – albeit still urging conservative use and even the possibility of nonopioid treatments.
The updated recommendations are now open for public comment via the Federal Register’s website through April 11.
“This comment period provides another critical opportunity for diverse audiences to offer their perspective on the draft clinical practice guideline,” Christopher M. Jones, PharmD, DrPH, acting director for the NCIPC, said in a release.
“We want to hear many voices from the public, including people living with pain and health care providers who help their patients manage pain,” Dr. Jones added.
Outpatient recommendations
The CDC noted that the updated guidance provides “evidence-based recommendations” for treatment of adults with acute, subacute, or chronic pain. It does not include guidance for managing pain related to sickle cell disease, cancer, or palliative care.
It is aimed at primary care clinicians and others who manage pain in an outpatient setting, including in dental and postsurgical practices and for those discharging patients from emergency departments. It does not apply to inpatient care.
The draft guidance includes 12 recommendations focused on four key areas:
- Helping clinicians determine whether or not to initiate opioid treatment for pain
- Opioid selection and dosage
- Duration of use and follow-up
- Assessing risk and addressing potential harms from use
The overall aim “is to ensure people have access to safe, accessible, and effective pain management that improves their function and quality of life while illuminating and reducing risks associated with prescription opioids and ultimately reducing the consequences of prescription opioid misuse and overdose,” the CDC notes.
In addition, the guidance itself “is intended to be a clinical tool to improve communication between providers and patients and empower them to make informed, patient-centered decisions,” the agency said in a press release.
It added that the new recommendations “are not intended to be applied as inflexible standards of care.” Rather, it is intended as a guide to support health care providers in their clinical decisionmaking as they provide individualized patient care.
Patients, caregivers, and providers are invited to submit comments over the next 60 days through the Federal Register docket.
“It is vitally important to CDC that we receive, process, and understand public feedback during the guideline update process,” the agency noted.
“The ultimate goal of this clinical practice guideline is to help people set and achieve personal goals to reduce their pain and improve their function and quality of life. Getting feedback from the public is essential to achieving this goal,” Dr. Jones said.
A version of this article first appeared on Medscape.com.
Docs react: NyQuil chicken and endless eye mucus
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
If you’ve got 3 seconds, then you’ve got time to work out
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?