User login
A Tale of Two Babies and the ‘Family Tragedy’ of Congenital Syphilis
Delivered at 34 weeks’ gestation, Baby “Alex” had an enlarged liver and spleen on his initial newborn exam, poor tone, and a diffuse, peeling rash. Baby “Aaliyah” was born at term and appeared healthy. By 1 month of age, she was gaining weight poorly and developed copious nasal drainage and a salmon-colored rash on the soles of her feet.
The connection? Both babies were ultimately diagnosed with congenital syphilis. Infections in both babies could have been prevented if their mothers had been tested for syphilis and treated during pregnancy. Alex’s mom had no prenatal care. Aaliyah’s mom had tested negative for syphilis during her first trimester but had not been re-tested, despite sharing with her health care provider that she had a new sexual partner.
Alex and Aaliyah are representative of what Centers for Disease Control and Prevention (CDC) Chief Medical Officer Debra Houry, MD, MPH, calls a “family tragedy.” Cases of congenital syphilis are rising rapidly in the United States, reaching a 30-year high in 2021.1 Cases increased by 755% between 2012 and 2021, from 335 in 2012 to 2,865 in 2021. In 2022, cases rose again: 3,761 cases of congenital syphilis were reported, including 231 stillbirths and 51 infant deaths. Infants with congenital syphilis are at risk for lifelong complications, including deafness, blindness, and intellectual disability.
Most of these cases were preventable. Congenital syphilis is rare when pregnant people complete adequate treatment at least 30 days before delivery. In 2022, lack of testing or timely testing contributed to 36.8% of congenital syphilis cases. Nearly 40% of birth parents of infected babies received inadequate treatment during pregnancy, and 11.2% received no treatment or treatment was not documented.
, suggesting ongoing barriers to care related to social determinants of health. In 2021, the highest rates of congenital syphilis were among babies born to individuals who were non-Hispanic American Indian or Alaska Native (384 cases per 100,000 live births), non-Hispanic Native Hawaiian or other Pacific Islander (192 cases per 100,000 live births), and non-Hispanic Black or African American (169 cases per 100,000 live births). Six states had rates of congenital syphilis that exceeded 160 cases per 100,000 population, including Arizona, New Mexico, Louisiana, Mississippi, Texas, and Oklahoma. That is more than twice the national rate of 77.9 cases/100,000.
Reducing the Risk
To reduce rates of congenital syphilis in all people, barriers to testing must be eliminated. The CDC recommends that all pregnant people be tested early in pregnancy, with repeat testing at 28 weeks and at delivery for those at increased risk for infection based on individual risk factors or residence in a high-prevalence community. Rapid syphilis testing and treatment during pregnancy is recommended in settings such as emergency departments, syringe service programs, prisons/jails, and maternal and child health programs to minimize missed opportunities for care.
While pediatric clinicians rarely care for pregnant patients, they also have an essential role to play in reducing the adverse health outcomes associated with congenital syphilis. No infant should be discharged from the newborn nursery without confirming that the birth parent was tested for syphilis at least once and was treated appropriately if positive. Appropriate treatment during pregnancy is a single dose of benzathine penicillin G for primary, secondary, or early latent syphilis. Late-latent syphilis or syphilis of unknown duration is treated with three doses of benzathine penicillin G spaced 7-9 days apart. If the doses are given further than 9 days apart, treatment is considered inadequate, and the series of doses must be restarted. Benzathine penicillin G remains in short supply in the United States, but is the only drug recommended to treat syphilis during pregnancy.
Collaboration between obstetrical and newborn care providers is essential. Those who care for newborns need easy access to birthing parents’ syphilis treatment results. As more health care facilities implement routine syphilis testing at delivery, rapid syphilis testing must be available to avoid prolonging newborn hospital stays.
Pediatricians need to maintain an index of suspicion for congenital syphilis, regardless of maternal history, because symptomatic congenital syphilis can mimic a variety of infectious and noninfectious conditions. Most infected infants look normal at birth. While the majority of cases of congenital syphilis are identified in the newborn period, a 2021 paper published in Pediatrics described 84 infants born between 2014 and 2018 who were diagnosed beyond a month of age.2 These represented 2.2% of all infants born with congenital syphilis. Common symptoms included rash, snuffles, and hepatomegaly. Sixty-nine percent of infants who had long bone radiographs obtained had findings consistent with congenital syphilis. Typical imaging findings include periostitis and demineralization of the metaphysis and diaphysis of long bones, although fractures can also occur. Case reports describe infants who presented with fractures and were initially evaluated for nonaccidental trauma.3
Another critical approach is to treat syphilis in people of childbearing age before pregnancy occurs. The CDC recommends syphilis testing for sexually active females 18-44 years of age and living in communities with high rates of syphilis. County-specific specific rates of syphilis rates are available at https://www.cdc.gov/nchhstp/atlas/syphilis/. Point-of-care tests are now available for syphilis and may facilitate timely treatment.
Additional resources describing syphilis testing and treatment are available from the CDC and the American Academy of Pediatrics.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead. Email her at [email protected]. (Also [email protected].)
References
1. McDonald R et al. Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. MMWR Morb Mortal Wkly Rep. 2023 Nov 17;72(46):1269-74. doi: 10.15585/mmwr.mm7246e1.
2. Kimball A et al. Congenital Syphilis Diagnosed Beyond the Neonatal Period in the United States: 2014-2018. Pediatrics. 2021 Sep;148(3):e2020049080. doi: 10.1542/peds.2020-049080.
3. Jacobs K et al. Congenital Syphilis Misdiagnosed as Suspected Nonaccidental Trauma. Pediatrics. 2019 Oct;144(4):e20191564. doi: 10.1542/peds.2019-1564.
Delivered at 34 weeks’ gestation, Baby “Alex” had an enlarged liver and spleen on his initial newborn exam, poor tone, and a diffuse, peeling rash. Baby “Aaliyah” was born at term and appeared healthy. By 1 month of age, she was gaining weight poorly and developed copious nasal drainage and a salmon-colored rash on the soles of her feet.
The connection? Both babies were ultimately diagnosed with congenital syphilis. Infections in both babies could have been prevented if their mothers had been tested for syphilis and treated during pregnancy. Alex’s mom had no prenatal care. Aaliyah’s mom had tested negative for syphilis during her first trimester but had not been re-tested, despite sharing with her health care provider that she had a new sexual partner.
Alex and Aaliyah are representative of what Centers for Disease Control and Prevention (CDC) Chief Medical Officer Debra Houry, MD, MPH, calls a “family tragedy.” Cases of congenital syphilis are rising rapidly in the United States, reaching a 30-year high in 2021.1 Cases increased by 755% between 2012 and 2021, from 335 in 2012 to 2,865 in 2021. In 2022, cases rose again: 3,761 cases of congenital syphilis were reported, including 231 stillbirths and 51 infant deaths. Infants with congenital syphilis are at risk for lifelong complications, including deafness, blindness, and intellectual disability.
Most of these cases were preventable. Congenital syphilis is rare when pregnant people complete adequate treatment at least 30 days before delivery. In 2022, lack of testing or timely testing contributed to 36.8% of congenital syphilis cases. Nearly 40% of birth parents of infected babies received inadequate treatment during pregnancy, and 11.2% received no treatment or treatment was not documented.
, suggesting ongoing barriers to care related to social determinants of health. In 2021, the highest rates of congenital syphilis were among babies born to individuals who were non-Hispanic American Indian or Alaska Native (384 cases per 100,000 live births), non-Hispanic Native Hawaiian or other Pacific Islander (192 cases per 100,000 live births), and non-Hispanic Black or African American (169 cases per 100,000 live births). Six states had rates of congenital syphilis that exceeded 160 cases per 100,000 population, including Arizona, New Mexico, Louisiana, Mississippi, Texas, and Oklahoma. That is more than twice the national rate of 77.9 cases/100,000.
Reducing the Risk
To reduce rates of congenital syphilis in all people, barriers to testing must be eliminated. The CDC recommends that all pregnant people be tested early in pregnancy, with repeat testing at 28 weeks and at delivery for those at increased risk for infection based on individual risk factors or residence in a high-prevalence community. Rapid syphilis testing and treatment during pregnancy is recommended in settings such as emergency departments, syringe service programs, prisons/jails, and maternal and child health programs to minimize missed opportunities for care.
While pediatric clinicians rarely care for pregnant patients, they also have an essential role to play in reducing the adverse health outcomes associated with congenital syphilis. No infant should be discharged from the newborn nursery without confirming that the birth parent was tested for syphilis at least once and was treated appropriately if positive. Appropriate treatment during pregnancy is a single dose of benzathine penicillin G for primary, secondary, or early latent syphilis. Late-latent syphilis or syphilis of unknown duration is treated with three doses of benzathine penicillin G spaced 7-9 days apart. If the doses are given further than 9 days apart, treatment is considered inadequate, and the series of doses must be restarted. Benzathine penicillin G remains in short supply in the United States, but is the only drug recommended to treat syphilis during pregnancy.
Collaboration between obstetrical and newborn care providers is essential. Those who care for newborns need easy access to birthing parents’ syphilis treatment results. As more health care facilities implement routine syphilis testing at delivery, rapid syphilis testing must be available to avoid prolonging newborn hospital stays.
Pediatricians need to maintain an index of suspicion for congenital syphilis, regardless of maternal history, because symptomatic congenital syphilis can mimic a variety of infectious and noninfectious conditions. Most infected infants look normal at birth. While the majority of cases of congenital syphilis are identified in the newborn period, a 2021 paper published in Pediatrics described 84 infants born between 2014 and 2018 who were diagnosed beyond a month of age.2 These represented 2.2% of all infants born with congenital syphilis. Common symptoms included rash, snuffles, and hepatomegaly. Sixty-nine percent of infants who had long bone radiographs obtained had findings consistent with congenital syphilis. Typical imaging findings include periostitis and demineralization of the metaphysis and diaphysis of long bones, although fractures can also occur. Case reports describe infants who presented with fractures and were initially evaluated for nonaccidental trauma.3
Another critical approach is to treat syphilis in people of childbearing age before pregnancy occurs. The CDC recommends syphilis testing for sexually active females 18-44 years of age and living in communities with high rates of syphilis. County-specific specific rates of syphilis rates are available at https://www.cdc.gov/nchhstp/atlas/syphilis/. Point-of-care tests are now available for syphilis and may facilitate timely treatment.
Additional resources describing syphilis testing and treatment are available from the CDC and the American Academy of Pediatrics.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead. Email her at [email protected]. (Also [email protected].)
References
1. McDonald R et al. Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. MMWR Morb Mortal Wkly Rep. 2023 Nov 17;72(46):1269-74. doi: 10.15585/mmwr.mm7246e1.
2. Kimball A et al. Congenital Syphilis Diagnosed Beyond the Neonatal Period in the United States: 2014-2018. Pediatrics. 2021 Sep;148(3):e2020049080. doi: 10.1542/peds.2020-049080.
3. Jacobs K et al. Congenital Syphilis Misdiagnosed as Suspected Nonaccidental Trauma. Pediatrics. 2019 Oct;144(4):e20191564. doi: 10.1542/peds.2019-1564.
Delivered at 34 weeks’ gestation, Baby “Alex” had an enlarged liver and spleen on his initial newborn exam, poor tone, and a diffuse, peeling rash. Baby “Aaliyah” was born at term and appeared healthy. By 1 month of age, she was gaining weight poorly and developed copious nasal drainage and a salmon-colored rash on the soles of her feet.
The connection? Both babies were ultimately diagnosed with congenital syphilis. Infections in both babies could have been prevented if their mothers had been tested for syphilis and treated during pregnancy. Alex’s mom had no prenatal care. Aaliyah’s mom had tested negative for syphilis during her first trimester but had not been re-tested, despite sharing with her health care provider that she had a new sexual partner.
Alex and Aaliyah are representative of what Centers for Disease Control and Prevention (CDC) Chief Medical Officer Debra Houry, MD, MPH, calls a “family tragedy.” Cases of congenital syphilis are rising rapidly in the United States, reaching a 30-year high in 2021.1 Cases increased by 755% between 2012 and 2021, from 335 in 2012 to 2,865 in 2021. In 2022, cases rose again: 3,761 cases of congenital syphilis were reported, including 231 stillbirths and 51 infant deaths. Infants with congenital syphilis are at risk for lifelong complications, including deafness, blindness, and intellectual disability.
Most of these cases were preventable. Congenital syphilis is rare when pregnant people complete adequate treatment at least 30 days before delivery. In 2022, lack of testing or timely testing contributed to 36.8% of congenital syphilis cases. Nearly 40% of birth parents of infected babies received inadequate treatment during pregnancy, and 11.2% received no treatment or treatment was not documented.
, suggesting ongoing barriers to care related to social determinants of health. In 2021, the highest rates of congenital syphilis were among babies born to individuals who were non-Hispanic American Indian or Alaska Native (384 cases per 100,000 live births), non-Hispanic Native Hawaiian or other Pacific Islander (192 cases per 100,000 live births), and non-Hispanic Black or African American (169 cases per 100,000 live births). Six states had rates of congenital syphilis that exceeded 160 cases per 100,000 population, including Arizona, New Mexico, Louisiana, Mississippi, Texas, and Oklahoma. That is more than twice the national rate of 77.9 cases/100,000.
Reducing the Risk
To reduce rates of congenital syphilis in all people, barriers to testing must be eliminated. The CDC recommends that all pregnant people be tested early in pregnancy, with repeat testing at 28 weeks and at delivery for those at increased risk for infection based on individual risk factors or residence in a high-prevalence community. Rapid syphilis testing and treatment during pregnancy is recommended in settings such as emergency departments, syringe service programs, prisons/jails, and maternal and child health programs to minimize missed opportunities for care.
While pediatric clinicians rarely care for pregnant patients, they also have an essential role to play in reducing the adverse health outcomes associated with congenital syphilis. No infant should be discharged from the newborn nursery without confirming that the birth parent was tested for syphilis at least once and was treated appropriately if positive. Appropriate treatment during pregnancy is a single dose of benzathine penicillin G for primary, secondary, or early latent syphilis. Late-latent syphilis or syphilis of unknown duration is treated with three doses of benzathine penicillin G spaced 7-9 days apart. If the doses are given further than 9 days apart, treatment is considered inadequate, and the series of doses must be restarted. Benzathine penicillin G remains in short supply in the United States, but is the only drug recommended to treat syphilis during pregnancy.
Collaboration between obstetrical and newborn care providers is essential. Those who care for newborns need easy access to birthing parents’ syphilis treatment results. As more health care facilities implement routine syphilis testing at delivery, rapid syphilis testing must be available to avoid prolonging newborn hospital stays.
Pediatricians need to maintain an index of suspicion for congenital syphilis, regardless of maternal history, because symptomatic congenital syphilis can mimic a variety of infectious and noninfectious conditions. Most infected infants look normal at birth. While the majority of cases of congenital syphilis are identified in the newborn period, a 2021 paper published in Pediatrics described 84 infants born between 2014 and 2018 who were diagnosed beyond a month of age.2 These represented 2.2% of all infants born with congenital syphilis. Common symptoms included rash, snuffles, and hepatomegaly. Sixty-nine percent of infants who had long bone radiographs obtained had findings consistent with congenital syphilis. Typical imaging findings include periostitis and demineralization of the metaphysis and diaphysis of long bones, although fractures can also occur. Case reports describe infants who presented with fractures and were initially evaluated for nonaccidental trauma.3
Another critical approach is to treat syphilis in people of childbearing age before pregnancy occurs. The CDC recommends syphilis testing for sexually active females 18-44 years of age and living in communities with high rates of syphilis. County-specific specific rates of syphilis rates are available at https://www.cdc.gov/nchhstp/atlas/syphilis/. Point-of-care tests are now available for syphilis and may facilitate timely treatment.
Additional resources describing syphilis testing and treatment are available from the CDC and the American Academy of Pediatrics.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022-2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead. Email her at [email protected]. (Also [email protected].)
References
1. McDonald R et al. Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022. MMWR Morb Mortal Wkly Rep. 2023 Nov 17;72(46):1269-74. doi: 10.15585/mmwr.mm7246e1.
2. Kimball A et al. Congenital Syphilis Diagnosed Beyond the Neonatal Period in the United States: 2014-2018. Pediatrics. 2021 Sep;148(3):e2020049080. doi: 10.1542/peds.2020-049080.
3. Jacobs K et al. Congenital Syphilis Misdiagnosed as Suspected Nonaccidental Trauma. Pediatrics. 2019 Oct;144(4):e20191564. doi: 10.1542/peds.2019-1564.
FDA Gives Nod to Berdazimer Gel for Molluscum Contagiosum
On January 5, the Food and Drug Administration (FDA) approved berdazimer gel 10.3% for the treatment of molluscum contagiosum (MC) in adults and children aged 1 year or older.
Approval of berdazimer, a topical nitric oxide–releasing agent, was based largely on a 12-week pivotal phase 3 trial known as B-SIMPLE4, in which 891 patients with a mean age of 6.6 years (range, 0.9-47.5 years) were randomly assigned to treatment with berdazimer gel 10.3% or a vehicle gel applied in a thin layer to all lesions once daily. At 12 weeks, 32.4% of patients in the berdazimer group achieved complete clearance of MC lesions compared with 19.7% of those in the vehicle group (P < .001).
Only 4.1% of patients on berdazimer and 0.7% of those on the vehicle experienced adverse events that led to discontinuation of treatment. The most common adverse events in both groups were application-site pain and erythema, and most of these were mild or moderate.
According to a press release announcing the approval from Ligand Pharmaceuticals, which acquired berdazimer topical gel from Novan in September 2023, the development makes berdazimer topical gel 10.3% the first and only topical prescription medication that can be applied by patients, parents, or caregivers at home; outside of a physician›s office; or outside of other medical settings to treat MC. Nitric oxide has been shown to have antiviral effects, although the mechanism of action of berdazimer for treating molluscum “is unknown,” the company said in the release.
The drug will be marketed under the name Zelsuvmi and is expected to be available in the second half of 2024.
On July 21, 2023, topical cantharidin became the first approved treatment of MC for adults and pediatric patients aged 2 years or older, with the FDA approval of a drug-device combination (Ycanth) that contains a formulation of cantharidin solution 0.7% and is administered by healthcare professionals.
A version of this article appeared on Medscape.com.
On January 5, the Food and Drug Administration (FDA) approved berdazimer gel 10.3% for the treatment of molluscum contagiosum (MC) in adults and children aged 1 year or older.
Approval of berdazimer, a topical nitric oxide–releasing agent, was based largely on a 12-week pivotal phase 3 trial known as B-SIMPLE4, in which 891 patients with a mean age of 6.6 years (range, 0.9-47.5 years) were randomly assigned to treatment with berdazimer gel 10.3% or a vehicle gel applied in a thin layer to all lesions once daily. At 12 weeks, 32.4% of patients in the berdazimer group achieved complete clearance of MC lesions compared with 19.7% of those in the vehicle group (P < .001).
Only 4.1% of patients on berdazimer and 0.7% of those on the vehicle experienced adverse events that led to discontinuation of treatment. The most common adverse events in both groups were application-site pain and erythema, and most of these were mild or moderate.
According to a press release announcing the approval from Ligand Pharmaceuticals, which acquired berdazimer topical gel from Novan in September 2023, the development makes berdazimer topical gel 10.3% the first and only topical prescription medication that can be applied by patients, parents, or caregivers at home; outside of a physician›s office; or outside of other medical settings to treat MC. Nitric oxide has been shown to have antiviral effects, although the mechanism of action of berdazimer for treating molluscum “is unknown,” the company said in the release.
The drug will be marketed under the name Zelsuvmi and is expected to be available in the second half of 2024.
On July 21, 2023, topical cantharidin became the first approved treatment of MC for adults and pediatric patients aged 2 years or older, with the FDA approval of a drug-device combination (Ycanth) that contains a formulation of cantharidin solution 0.7% and is administered by healthcare professionals.
A version of this article appeared on Medscape.com.
On January 5, the Food and Drug Administration (FDA) approved berdazimer gel 10.3% for the treatment of molluscum contagiosum (MC) in adults and children aged 1 year or older.
Approval of berdazimer, a topical nitric oxide–releasing agent, was based largely on a 12-week pivotal phase 3 trial known as B-SIMPLE4, in which 891 patients with a mean age of 6.6 years (range, 0.9-47.5 years) were randomly assigned to treatment with berdazimer gel 10.3% or a vehicle gel applied in a thin layer to all lesions once daily. At 12 weeks, 32.4% of patients in the berdazimer group achieved complete clearance of MC lesions compared with 19.7% of those in the vehicle group (P < .001).
Only 4.1% of patients on berdazimer and 0.7% of those on the vehicle experienced adverse events that led to discontinuation of treatment. The most common adverse events in both groups were application-site pain and erythema, and most of these were mild or moderate.
According to a press release announcing the approval from Ligand Pharmaceuticals, which acquired berdazimer topical gel from Novan in September 2023, the development makes berdazimer topical gel 10.3% the first and only topical prescription medication that can be applied by patients, parents, or caregivers at home; outside of a physician›s office; or outside of other medical settings to treat MC. Nitric oxide has been shown to have antiviral effects, although the mechanism of action of berdazimer for treating molluscum “is unknown,” the company said in the release.
The drug will be marketed under the name Zelsuvmi and is expected to be available in the second half of 2024.
On July 21, 2023, topical cantharidin became the first approved treatment of MC for adults and pediatric patients aged 2 years or older, with the FDA approval of a drug-device combination (Ycanth) that contains a formulation of cantharidin solution 0.7% and is administered by healthcare professionals.
A version of this article appeared on Medscape.com.
Study: Early Tecovirimat Stops Mpox Progression in HIV Patients
A new analysis supports using the smallpox antiviral tecovirimat (TPOXX/ST-246) in HIV patients showing the first symptoms of the human smallpox disease mpox (monkeypox), caused by the variola virus.
In a small prospective matched cohort analysis, people with HIV (PWH) and mpox disease who received tecovirimat within 7 days of symptom onset were 13 times less likely to experience progression, compared with PWH not prescribed tecovirimat within that window. In a matched cohort of 112 PWH, mpox disease progression occurred in 5.4% in an early tecovirimat group and in 26.8% in a late- or no-tecovirimat group, for a paired odds ratio of 13.00 (95% CI, 1.71-99.40; P = .002).
“Results of the present study suggest that tecovirimat treatment should be started early at the time of suspected mpox diagnosis in all PWH, especially in those with nonsuppressed HIV viremia or mucosal site involvement,” wrote a team led by Bruce Aldred, MD, of the Division of Infectious Diseases in the Department of Medicine at Emory University School of Medicine in Atlanta, in JAMA Internal Medicine. Early symptoms of mpox include skin rash and mucosal lesions, along with viral symptoms such as fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
As of March 1 of last year, the United States reported more than 30,000 cases, while cases numbered more than 86,000 worldwide.
Despite a lack of effectiveness data in humans, tecovirimat was widely prescribed to PWH with mpox during the 2022 epidemic, which disproportionately affected PWH, particularly those with low CD4+ T-cell counts or severe mpox clinical manifestations who needed urgent therapy. Developed to treat smallpox, tecovirimat has antiviral activity against other orthopoxviruses, and has reduced mpox-related morbidity and mortality in animals.
Based on the animal data, approval was granted by the US Food and Drug Administration (FDA) for human mpox treatment. Dr. Aldred and colleagues undertook this cohort analysis in the absence of human data and with the postoutbreak decline in cases impeding recruitment to a full-scale clinical trial.
Study design
The preponderantly Black cohort included 112 PWH diagnosed with mpox at four Atlanta hospitals from June 1 to October 7, 2022. Patients were grouped in an early cohort receiving tecovirimat within 7 days of symptom onset or a no or late cohort (no tecovirimat or treatment more than 7 days after symptom onset. Multivariate logistic regression models identified factors associated with progression, defined as development of at least one severe CDC mpox criterion after symptom day 7.
The cohorts were then matched 1:1 using propensity scores based on the identified factors, and mpox disease progression was compared.
Of 112 PWH, 56 receive early tecovirimat and 56 received no or late treatment. In the early group, the median (interquartile range [IQR]) age was 35 (30-42) years; 54 individuals (96.4%) were cisgender men, 46 (82.1%) were Black, and 10 (17.9%) were, variously, White, American Indian, Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, or of unknown race.
In the late- or no-tecovirimat group, the median (IQR) age was 36 (32-43) years; 54 (96.4%) were cisgender men, 49 (87.5%) were Black, and 7 (12.5%) were individuals of other or unknown race. Mpox disease progression occurred in 3 PWH in the early-tecovirimat group and 15 PWH (26.8%) in the late- or no-tecovirimat group.
Dr. Aldred and colleagues acknowledged that more research is needed to confirm the findings and cited several study limitations. These included the small sample size, the preponderance of Black participants, and the possibility that unmatched confounding variables could have led to the observation of fewer cases of severe disease in the early-tecovirimat cohort.
This study was supported by a grant from the Emory Center for AIDS Research. Coauthors reported grants from various institutes at the National Institutes of Health as well as from multiple pharmaceutical companies.
A new analysis supports using the smallpox antiviral tecovirimat (TPOXX/ST-246) in HIV patients showing the first symptoms of the human smallpox disease mpox (monkeypox), caused by the variola virus.
In a small prospective matched cohort analysis, people with HIV (PWH) and mpox disease who received tecovirimat within 7 days of symptom onset were 13 times less likely to experience progression, compared with PWH not prescribed tecovirimat within that window. In a matched cohort of 112 PWH, mpox disease progression occurred in 5.4% in an early tecovirimat group and in 26.8% in a late- or no-tecovirimat group, for a paired odds ratio of 13.00 (95% CI, 1.71-99.40; P = .002).
“Results of the present study suggest that tecovirimat treatment should be started early at the time of suspected mpox diagnosis in all PWH, especially in those with nonsuppressed HIV viremia or mucosal site involvement,” wrote a team led by Bruce Aldred, MD, of the Division of Infectious Diseases in the Department of Medicine at Emory University School of Medicine in Atlanta, in JAMA Internal Medicine. Early symptoms of mpox include skin rash and mucosal lesions, along with viral symptoms such as fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
As of March 1 of last year, the United States reported more than 30,000 cases, while cases numbered more than 86,000 worldwide.
Despite a lack of effectiveness data in humans, tecovirimat was widely prescribed to PWH with mpox during the 2022 epidemic, which disproportionately affected PWH, particularly those with low CD4+ T-cell counts or severe mpox clinical manifestations who needed urgent therapy. Developed to treat smallpox, tecovirimat has antiviral activity against other orthopoxviruses, and has reduced mpox-related morbidity and mortality in animals.
Based on the animal data, approval was granted by the US Food and Drug Administration (FDA) for human mpox treatment. Dr. Aldred and colleagues undertook this cohort analysis in the absence of human data and with the postoutbreak decline in cases impeding recruitment to a full-scale clinical trial.
Study design
The preponderantly Black cohort included 112 PWH diagnosed with mpox at four Atlanta hospitals from June 1 to October 7, 2022. Patients were grouped in an early cohort receiving tecovirimat within 7 days of symptom onset or a no or late cohort (no tecovirimat or treatment more than 7 days after symptom onset. Multivariate logistic regression models identified factors associated with progression, defined as development of at least one severe CDC mpox criterion after symptom day 7.
The cohorts were then matched 1:1 using propensity scores based on the identified factors, and mpox disease progression was compared.
Of 112 PWH, 56 receive early tecovirimat and 56 received no or late treatment. In the early group, the median (interquartile range [IQR]) age was 35 (30-42) years; 54 individuals (96.4%) were cisgender men, 46 (82.1%) were Black, and 10 (17.9%) were, variously, White, American Indian, Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, or of unknown race.
In the late- or no-tecovirimat group, the median (IQR) age was 36 (32-43) years; 54 (96.4%) were cisgender men, 49 (87.5%) were Black, and 7 (12.5%) were individuals of other or unknown race. Mpox disease progression occurred in 3 PWH in the early-tecovirimat group and 15 PWH (26.8%) in the late- or no-tecovirimat group.
Dr. Aldred and colleagues acknowledged that more research is needed to confirm the findings and cited several study limitations. These included the small sample size, the preponderance of Black participants, and the possibility that unmatched confounding variables could have led to the observation of fewer cases of severe disease in the early-tecovirimat cohort.
This study was supported by a grant from the Emory Center for AIDS Research. Coauthors reported grants from various institutes at the National Institutes of Health as well as from multiple pharmaceutical companies.
A new analysis supports using the smallpox antiviral tecovirimat (TPOXX/ST-246) in HIV patients showing the first symptoms of the human smallpox disease mpox (monkeypox), caused by the variola virus.
In a small prospective matched cohort analysis, people with HIV (PWH) and mpox disease who received tecovirimat within 7 days of symptom onset were 13 times less likely to experience progression, compared with PWH not prescribed tecovirimat within that window. In a matched cohort of 112 PWH, mpox disease progression occurred in 5.4% in an early tecovirimat group and in 26.8% in a late- or no-tecovirimat group, for a paired odds ratio of 13.00 (95% CI, 1.71-99.40; P = .002).
“Results of the present study suggest that tecovirimat treatment should be started early at the time of suspected mpox diagnosis in all PWH, especially in those with nonsuppressed HIV viremia or mucosal site involvement,” wrote a team led by Bruce Aldred, MD, of the Division of Infectious Diseases in the Department of Medicine at Emory University School of Medicine in Atlanta, in JAMA Internal Medicine. Early symptoms of mpox include skin rash and mucosal lesions, along with viral symptoms such as fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
As of March 1 of last year, the United States reported more than 30,000 cases, while cases numbered more than 86,000 worldwide.
Despite a lack of effectiveness data in humans, tecovirimat was widely prescribed to PWH with mpox during the 2022 epidemic, which disproportionately affected PWH, particularly those with low CD4+ T-cell counts or severe mpox clinical manifestations who needed urgent therapy. Developed to treat smallpox, tecovirimat has antiviral activity against other orthopoxviruses, and has reduced mpox-related morbidity and mortality in animals.
Based on the animal data, approval was granted by the US Food and Drug Administration (FDA) for human mpox treatment. Dr. Aldred and colleagues undertook this cohort analysis in the absence of human data and with the postoutbreak decline in cases impeding recruitment to a full-scale clinical trial.
Study design
The preponderantly Black cohort included 112 PWH diagnosed with mpox at four Atlanta hospitals from June 1 to October 7, 2022. Patients were grouped in an early cohort receiving tecovirimat within 7 days of symptom onset or a no or late cohort (no tecovirimat or treatment more than 7 days after symptom onset. Multivariate logistic regression models identified factors associated with progression, defined as development of at least one severe CDC mpox criterion after symptom day 7.
The cohorts were then matched 1:1 using propensity scores based on the identified factors, and mpox disease progression was compared.
Of 112 PWH, 56 receive early tecovirimat and 56 received no or late treatment. In the early group, the median (interquartile range [IQR]) age was 35 (30-42) years; 54 individuals (96.4%) were cisgender men, 46 (82.1%) were Black, and 10 (17.9%) were, variously, White, American Indian, Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, or of unknown race.
In the late- or no-tecovirimat group, the median (IQR) age was 36 (32-43) years; 54 (96.4%) were cisgender men, 49 (87.5%) were Black, and 7 (12.5%) were individuals of other or unknown race. Mpox disease progression occurred in 3 PWH in the early-tecovirimat group and 15 PWH (26.8%) in the late- or no-tecovirimat group.
Dr. Aldred and colleagues acknowledged that more research is needed to confirm the findings and cited several study limitations. These included the small sample size, the preponderance of Black participants, and the possibility that unmatched confounding variables could have led to the observation of fewer cases of severe disease in the early-tecovirimat cohort.
This study was supported by a grant from the Emory Center for AIDS Research. Coauthors reported grants from various institutes at the National Institutes of Health as well as from multiple pharmaceutical companies.
FROM JAMA INTERNAL MEDICINE
Asymptomatic Violaceous Plaques on the Face and Back
The Diagnosis: Cutaneous Sarcoidosis
A biopsy of a plaque on the back confirmed cutaneous sarcoidosis (CS). A chest radiograph demonstrated hilar nodes, and a referral was placed for comanagement with a pulmonologist. Histopathology was critical in making the diagnosis, with well-circumscribed noncaseating granulomas present in the dermis. The granulomas in CS often are described as naked, as there are minimal lymphocytes present and plasma cells normally are absent.1 Because the lungs are the most common site of involvement, a chest radiograph is necessary to examine for systemic sarcoidosis. Laboratory workup is used to evaluate for lymphopenia, hypercalcemia, elevated blood sedimentation rate, and elevated angiotensin- converting enzyme levels, which are common in systemic sarcoidosis.1
Sarcoidosis is a multisystemic granulomatous disorder with an unknown etiology. It is believed to develop in genetically predisposed individuals as a reaction to unidentified antigens in the environment.1 Helper T cells (TH1) respond to these environmental antigens in those who are susceptible, which leads to the disease process, but paradoxically, even with the elevation of cellular immune activity at the sites of the granulomatous inflammation, the peripheral immune response in these patients is suppressed as shown by lymphopenia.2
Cutaneous sarcoidosis is found in approximately one-third of patients with systemic sarcoidosis but can occur without systemic involvement.1,2 Sarcoidosis is reported worldwide and affects patients of all races and ethnicities, ages, and sexes but does have a higher prevalence among Black individuals in the United States, patients younger than 40 years (peak incidence, 20–29 years of age), and females.2 In 80% of patients, CS occurs before systemic sarcoidosis develops, or they may develop simultaneously.1
Cutaneous sarcoidosis has a wide range of clinical presentations that are classified as specific and nonspecific. Specific lesions in CS contain noncaseating granulomas while nonspecific lesions in CS appear as reactive processes.2 The most common specific presentation of CS includes papules that are brown in pigmentation in lighter skin tones and red to violaceous in darker skin tones (Figure). The most common nonspecific skin manifestation is erythema nodosum, which represents a hypersensitivity reaction. Cutaneous sarcoidosis can appear as hypopigmented or hyperpigmented patches or plaques.1

Treatments for CS vary based on the individual.1 For milder and more localized cases, topical or intralesional steroids may be used. If systemic sarcoidosis is suspected or if there is diffuse involvement of the skin, systemic steroids, antimalarials (eg, hydroxychloroquine), low-dose methotrexate, minocycline, allopurinol, azathioprine, isotretinoin, tumor necrosis factor α inhibitors, or psoralen plus long-wave UVA radiation may be used. If systemic sarcoidosis is present, referral to a pulmonologist is recommended for co-management.1
Cutaneous sarcoidosis is known as the “great imitator,” and there are multiple diseases to consider in the differential that are distinguished by the physical findings.1 In our case of a middle-aged Black woman with indurated plaques, a few diagnoses to consider were psoriasis, discoid lupus erythematosus (DLE), mycosis fungoides (MF), and tinea infection.
Psoriasis is a common disease, and 90% of patients have chronic plaquelike disease with well-demarcated erythematous plaques that have a silver-gray scale and a positive Auspitz sign (also known as pinpoint bleeding).3 Plaques often are distributed on the trunk, limb extensors, and scalp, along with nail changes. Some patients also have joint pain, indicating psoriatic arthritis. The etiology of psoriasis is unknown, but it develops due to unrestrained keratinocyte proliferation and defective differentiation, which leads to histopathology showing regular acanthosis and papillary dermal ectasia with rouleaux. Mild cases typically are treated with topical steroids or vitamin D, while more severe cases are treated with methotrexate, cyclosporine, retinoids, or biologics.3
Discoid lupus erythematosus occurs 4 times more often in Black patients than in White patients. Clinically, DLE begins as well-defined, erythematous, scaly patches that expand with hyperpigmentation at the periphery and leave an atrophic, scarred, hypopigmented center.4 It typically is localized to the head and neck, but in cases where it disseminates elsewhere on the body, the risk for systemic lupus erythematosus increases from 1.2% to 28%.5 Histopathology of DLE shows vacuolar degeneration of the basal cell layer in the epidermis along with patchy lymphocytic infiltrate in the dermis. Treatments range from topical steroids for mild cases to antimalarial agents, retinoids, anti-inflammatory drugs, and calcineurin inhibitors for more severe cases.4
Although there are multiple types of cutaneous T-cell lymphoma, the most common is MF, which traditionally is nonaggressive. The typical patient with MF is older than 60 years and presents with indolent, ongoing, flat to minimally indurated patches or plaques that have cigarette paper scale. As MF progresses, some plaques grow into tumors and can become more aggressive. Histologically, MF changes based on its clinical stage, with the initial phase showing epidermotropic atypical lymphocytes and later phases showing less epitheliotropic, larger, atypical lymphocytes. The treatment algorithm varies depending on cutaneous T-cell lymphoma staging.6
Tinea infections are caused by dermatophytes. In prepubertal children, they predominantly appear as tinea corporis (on the body) or tinea capitis (on the scalp), but in adults they appear as tinea cruris (on the groin), tinea pedis (on the feet), or tinea unguium (on the nails).7 Tinea infections classically are known to appear as an annular patch with an active erythematous scaling border and central clearing. The patches can be pruritic. Potassium hydroxide preparation of a skin scraping is a quick test to use in the office; if the results are inconclusive, a culture may be required. Treatment depends on the location of the infection but typically involves either topical or oral antifungal agents.7
- Tchernev G, Cardoso JC, Chokoeva AA, et al. The “mystery” of cutaneous sarcoidosis: facts and controversies. Int J Immunopathol Pharmacol. 2014;27:321-330. doi:10.1177/039463201402700302
- Ali MM, Atwan AA, Gonzalez ML. Cutaneous sarcoidosis: updates in the pathogenesis. J Eur Acad Dermatol Venereol. 2010;24:747-755. doi:10.1111/j.1468-3083.2009.03517.x
- Rendon A, Schäkel K. Psoriasis pathogenesis and treatment [published online March 23, 2019]. Int J Mol Sci. 2019;20:1475. doi:10.3390/ijms20061475
- McDaniel B, Sukumaran S, Koritala T, et al. Discoid lupus erythematosus. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK493145/
- Bhat MR, Hulmani M, Dandakeri S, et al. Disseminated discoid lupus erythematosus leading to squamous cell carcinoma. Indian J Dermatol. 2012;57:158-161. doi:10.4103/0019-5154.94298
- Pulitzer M. Cutaneous T-cell Lymphoma. Clin Lab Med. 2017; 37:527-546. doi:10.1016/j.cll.2017.06.006
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90:702-710.
The Diagnosis: Cutaneous Sarcoidosis
A biopsy of a plaque on the back confirmed cutaneous sarcoidosis (CS). A chest radiograph demonstrated hilar nodes, and a referral was placed for comanagement with a pulmonologist. Histopathology was critical in making the diagnosis, with well-circumscribed noncaseating granulomas present in the dermis. The granulomas in CS often are described as naked, as there are minimal lymphocytes present and plasma cells normally are absent.1 Because the lungs are the most common site of involvement, a chest radiograph is necessary to examine for systemic sarcoidosis. Laboratory workup is used to evaluate for lymphopenia, hypercalcemia, elevated blood sedimentation rate, and elevated angiotensin- converting enzyme levels, which are common in systemic sarcoidosis.1
Sarcoidosis is a multisystemic granulomatous disorder with an unknown etiology. It is believed to develop in genetically predisposed individuals as a reaction to unidentified antigens in the environment.1 Helper T cells (TH1) respond to these environmental antigens in those who are susceptible, which leads to the disease process, but paradoxically, even with the elevation of cellular immune activity at the sites of the granulomatous inflammation, the peripheral immune response in these patients is suppressed as shown by lymphopenia.2
Cutaneous sarcoidosis is found in approximately one-third of patients with systemic sarcoidosis but can occur without systemic involvement.1,2 Sarcoidosis is reported worldwide and affects patients of all races and ethnicities, ages, and sexes but does have a higher prevalence among Black individuals in the United States, patients younger than 40 years (peak incidence, 20–29 years of age), and females.2 In 80% of patients, CS occurs before systemic sarcoidosis develops, or they may develop simultaneously.1
Cutaneous sarcoidosis has a wide range of clinical presentations that are classified as specific and nonspecific. Specific lesions in CS contain noncaseating granulomas while nonspecific lesions in CS appear as reactive processes.2 The most common specific presentation of CS includes papules that are brown in pigmentation in lighter skin tones and red to violaceous in darker skin tones (Figure). The most common nonspecific skin manifestation is erythema nodosum, which represents a hypersensitivity reaction. Cutaneous sarcoidosis can appear as hypopigmented or hyperpigmented patches or plaques.1

Treatments for CS vary based on the individual.1 For milder and more localized cases, topical or intralesional steroids may be used. If systemic sarcoidosis is suspected or if there is diffuse involvement of the skin, systemic steroids, antimalarials (eg, hydroxychloroquine), low-dose methotrexate, minocycline, allopurinol, azathioprine, isotretinoin, tumor necrosis factor α inhibitors, or psoralen plus long-wave UVA radiation may be used. If systemic sarcoidosis is present, referral to a pulmonologist is recommended for co-management.1
Cutaneous sarcoidosis is known as the “great imitator,” and there are multiple diseases to consider in the differential that are distinguished by the physical findings.1 In our case of a middle-aged Black woman with indurated plaques, a few diagnoses to consider were psoriasis, discoid lupus erythematosus (DLE), mycosis fungoides (MF), and tinea infection.
Psoriasis is a common disease, and 90% of patients have chronic plaquelike disease with well-demarcated erythematous plaques that have a silver-gray scale and a positive Auspitz sign (also known as pinpoint bleeding).3 Plaques often are distributed on the trunk, limb extensors, and scalp, along with nail changes. Some patients also have joint pain, indicating psoriatic arthritis. The etiology of psoriasis is unknown, but it develops due to unrestrained keratinocyte proliferation and defective differentiation, which leads to histopathology showing regular acanthosis and papillary dermal ectasia with rouleaux. Mild cases typically are treated with topical steroids or vitamin D, while more severe cases are treated with methotrexate, cyclosporine, retinoids, or biologics.3
Discoid lupus erythematosus occurs 4 times more often in Black patients than in White patients. Clinically, DLE begins as well-defined, erythematous, scaly patches that expand with hyperpigmentation at the periphery and leave an atrophic, scarred, hypopigmented center.4 It typically is localized to the head and neck, but in cases where it disseminates elsewhere on the body, the risk for systemic lupus erythematosus increases from 1.2% to 28%.5 Histopathology of DLE shows vacuolar degeneration of the basal cell layer in the epidermis along with patchy lymphocytic infiltrate in the dermis. Treatments range from topical steroids for mild cases to antimalarial agents, retinoids, anti-inflammatory drugs, and calcineurin inhibitors for more severe cases.4
Although there are multiple types of cutaneous T-cell lymphoma, the most common is MF, which traditionally is nonaggressive. The typical patient with MF is older than 60 years and presents with indolent, ongoing, flat to minimally indurated patches or plaques that have cigarette paper scale. As MF progresses, some plaques grow into tumors and can become more aggressive. Histologically, MF changes based on its clinical stage, with the initial phase showing epidermotropic atypical lymphocytes and later phases showing less epitheliotropic, larger, atypical lymphocytes. The treatment algorithm varies depending on cutaneous T-cell lymphoma staging.6
Tinea infections are caused by dermatophytes. In prepubertal children, they predominantly appear as tinea corporis (on the body) or tinea capitis (on the scalp), but in adults they appear as tinea cruris (on the groin), tinea pedis (on the feet), or tinea unguium (on the nails).7 Tinea infections classically are known to appear as an annular patch with an active erythematous scaling border and central clearing. The patches can be pruritic. Potassium hydroxide preparation of a skin scraping is a quick test to use in the office; if the results are inconclusive, a culture may be required. Treatment depends on the location of the infection but typically involves either topical or oral antifungal agents.7
The Diagnosis: Cutaneous Sarcoidosis
A biopsy of a plaque on the back confirmed cutaneous sarcoidosis (CS). A chest radiograph demonstrated hilar nodes, and a referral was placed for comanagement with a pulmonologist. Histopathology was critical in making the diagnosis, with well-circumscribed noncaseating granulomas present in the dermis. The granulomas in CS often are described as naked, as there are minimal lymphocytes present and plasma cells normally are absent.1 Because the lungs are the most common site of involvement, a chest radiograph is necessary to examine for systemic sarcoidosis. Laboratory workup is used to evaluate for lymphopenia, hypercalcemia, elevated blood sedimentation rate, and elevated angiotensin- converting enzyme levels, which are common in systemic sarcoidosis.1
Sarcoidosis is a multisystemic granulomatous disorder with an unknown etiology. It is believed to develop in genetically predisposed individuals as a reaction to unidentified antigens in the environment.1 Helper T cells (TH1) respond to these environmental antigens in those who are susceptible, which leads to the disease process, but paradoxically, even with the elevation of cellular immune activity at the sites of the granulomatous inflammation, the peripheral immune response in these patients is suppressed as shown by lymphopenia.2
Cutaneous sarcoidosis is found in approximately one-third of patients with systemic sarcoidosis but can occur without systemic involvement.1,2 Sarcoidosis is reported worldwide and affects patients of all races and ethnicities, ages, and sexes but does have a higher prevalence among Black individuals in the United States, patients younger than 40 years (peak incidence, 20–29 years of age), and females.2 In 80% of patients, CS occurs before systemic sarcoidosis develops, or they may develop simultaneously.1
Cutaneous sarcoidosis has a wide range of clinical presentations that are classified as specific and nonspecific. Specific lesions in CS contain noncaseating granulomas while nonspecific lesions in CS appear as reactive processes.2 The most common specific presentation of CS includes papules that are brown in pigmentation in lighter skin tones and red to violaceous in darker skin tones (Figure). The most common nonspecific skin manifestation is erythema nodosum, which represents a hypersensitivity reaction. Cutaneous sarcoidosis can appear as hypopigmented or hyperpigmented patches or plaques.1

Treatments for CS vary based on the individual.1 For milder and more localized cases, topical or intralesional steroids may be used. If systemic sarcoidosis is suspected or if there is diffuse involvement of the skin, systemic steroids, antimalarials (eg, hydroxychloroquine), low-dose methotrexate, minocycline, allopurinol, azathioprine, isotretinoin, tumor necrosis factor α inhibitors, or psoralen plus long-wave UVA radiation may be used. If systemic sarcoidosis is present, referral to a pulmonologist is recommended for co-management.1
Cutaneous sarcoidosis is known as the “great imitator,” and there are multiple diseases to consider in the differential that are distinguished by the physical findings.1 In our case of a middle-aged Black woman with indurated plaques, a few diagnoses to consider were psoriasis, discoid lupus erythematosus (DLE), mycosis fungoides (MF), and tinea infection.
Psoriasis is a common disease, and 90% of patients have chronic plaquelike disease with well-demarcated erythematous plaques that have a silver-gray scale and a positive Auspitz sign (also known as pinpoint bleeding).3 Plaques often are distributed on the trunk, limb extensors, and scalp, along with nail changes. Some patients also have joint pain, indicating psoriatic arthritis. The etiology of psoriasis is unknown, but it develops due to unrestrained keratinocyte proliferation and defective differentiation, which leads to histopathology showing regular acanthosis and papillary dermal ectasia with rouleaux. Mild cases typically are treated with topical steroids or vitamin D, while more severe cases are treated with methotrexate, cyclosporine, retinoids, or biologics.3
Discoid lupus erythematosus occurs 4 times more often in Black patients than in White patients. Clinically, DLE begins as well-defined, erythematous, scaly patches that expand with hyperpigmentation at the periphery and leave an atrophic, scarred, hypopigmented center.4 It typically is localized to the head and neck, but in cases where it disseminates elsewhere on the body, the risk for systemic lupus erythematosus increases from 1.2% to 28%.5 Histopathology of DLE shows vacuolar degeneration of the basal cell layer in the epidermis along with patchy lymphocytic infiltrate in the dermis. Treatments range from topical steroids for mild cases to antimalarial agents, retinoids, anti-inflammatory drugs, and calcineurin inhibitors for more severe cases.4
Although there are multiple types of cutaneous T-cell lymphoma, the most common is MF, which traditionally is nonaggressive. The typical patient with MF is older than 60 years and presents with indolent, ongoing, flat to minimally indurated patches or plaques that have cigarette paper scale. As MF progresses, some plaques grow into tumors and can become more aggressive. Histologically, MF changes based on its clinical stage, with the initial phase showing epidermotropic atypical lymphocytes and later phases showing less epitheliotropic, larger, atypical lymphocytes. The treatment algorithm varies depending on cutaneous T-cell lymphoma staging.6
Tinea infections are caused by dermatophytes. In prepubertal children, they predominantly appear as tinea corporis (on the body) or tinea capitis (on the scalp), but in adults they appear as tinea cruris (on the groin), tinea pedis (on the feet), or tinea unguium (on the nails).7 Tinea infections classically are known to appear as an annular patch with an active erythematous scaling border and central clearing. The patches can be pruritic. Potassium hydroxide preparation of a skin scraping is a quick test to use in the office; if the results are inconclusive, a culture may be required. Treatment depends on the location of the infection but typically involves either topical or oral antifungal agents.7
- Tchernev G, Cardoso JC, Chokoeva AA, et al. The “mystery” of cutaneous sarcoidosis: facts and controversies. Int J Immunopathol Pharmacol. 2014;27:321-330. doi:10.1177/039463201402700302
- Ali MM, Atwan AA, Gonzalez ML. Cutaneous sarcoidosis: updates in the pathogenesis. J Eur Acad Dermatol Venereol. 2010;24:747-755. doi:10.1111/j.1468-3083.2009.03517.x
- Rendon A, Schäkel K. Psoriasis pathogenesis and treatment [published online March 23, 2019]. Int J Mol Sci. 2019;20:1475. doi:10.3390/ijms20061475
- McDaniel B, Sukumaran S, Koritala T, et al. Discoid lupus erythematosus. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK493145/
- Bhat MR, Hulmani M, Dandakeri S, et al. Disseminated discoid lupus erythematosus leading to squamous cell carcinoma. Indian J Dermatol. 2012;57:158-161. doi:10.4103/0019-5154.94298
- Pulitzer M. Cutaneous T-cell Lymphoma. Clin Lab Med. 2017; 37:527-546. doi:10.1016/j.cll.2017.06.006
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90:702-710.
- Tchernev G, Cardoso JC, Chokoeva AA, et al. The “mystery” of cutaneous sarcoidosis: facts and controversies. Int J Immunopathol Pharmacol. 2014;27:321-330. doi:10.1177/039463201402700302
- Ali MM, Atwan AA, Gonzalez ML. Cutaneous sarcoidosis: updates in the pathogenesis. J Eur Acad Dermatol Venereol. 2010;24:747-755. doi:10.1111/j.1468-3083.2009.03517.x
- Rendon A, Schäkel K. Psoriasis pathogenesis and treatment [published online March 23, 2019]. Int J Mol Sci. 2019;20:1475. doi:10.3390/ijms20061475
- McDaniel B, Sukumaran S, Koritala T, et al. Discoid lupus erythematosus. StatPearls [Internet]. StatPearls Publishing; 2023. Accessed December 11, 2023. https://www.ncbi.nlm.nih.gov/books/NBK493145/
- Bhat MR, Hulmani M, Dandakeri S, et al. Disseminated discoid lupus erythematosus leading to squamous cell carcinoma. Indian J Dermatol. 2012;57:158-161. doi:10.4103/0019-5154.94298
- Pulitzer M. Cutaneous T-cell Lymphoma. Clin Lab Med. 2017; 37:527-546. doi:10.1016/j.cll.2017.06.006
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90:702-710.
A 35-year-old Black woman presented to dermatology as a new patient for evaluation of an asymptomatic rash that had enlarged and spread to involve both the face and back over the last 4 months. She had not tried any treatments. She had no notable medical history and was uncertain of her family history. Physical examination showed indurated, flesh-colored to violaceous plaques around the alar-facial groove (top), nasal tip, chin, and back (bottom). The mucosae and nails were not involved.

Long COVID Has Caused Thousands of US Deaths: New CDC Data
While COVID has now claimed more than 1 million lives in the United States alone, these aren’t the only fatalities caused at least in part by the virus. A small but growing number of Americans are surviving acute infections only to succumb months later to the lingering health problems caused by long COVID.
Much of the attention on long COVID has centered on the sometimes debilitating symptoms that strike people with the condition, with no formal diagnostic tests or standard treatments available, and the effect it has on quality of life. But new figures from the US Centers for Disease Control and Prevention (CDC) show that long COVID can also be deadly.
More than 5000 Americans have died from long COVID since the start of the pandemic, according to new estimates from the CDC.
This total, based on death certificate data collected by the CDC, includes a preliminary tally of 1491 long COVID deaths in 2023 in addition to 3544 fatalities previously reported from January 2020 through June 2022.
Guidance issued in 2023 on how to formally report long COVID as a cause of death on death certificates should help get a more accurate count of these fatalities going forward, said Robert Anderson, PhD, chief mortality statistician for the CDC, Atlanta, Georgia.
“We hope that the guidance will help cause of death certifiers be more aware of the impact of long COVID and more likely to report long COVID as a cause of death when appropriate,” Dr. Anderson said. “That said, we do not expect that this guidance will have a dramatic impact on the trend.”
There’s no standard definition or diagnostic test for long COVID. It’s typically diagnosed when people have symptoms at least 3 months after an acute infection that weren’t present before they got sick. As of the end of last year, about 7% of American adults had experienced long COVID at some point, the CDC estimated in September 2023.
The new death tally indicates long COVID remains a significant public health threat and is likely to grow in the years ahead, even though the pandemic may no longer be considered a global health crisis, experts said.
For example, the death certificate figures indicate:
COVID-19 was the third leading cause of American deaths in 2020 and 2021, and the fourth leading cause of death in the United States in 2023.
Nearly 1% of the more than one million deaths related to COVID-19 since the start of the pandemic have been attributed to long COVID, according to data released by the CDC.
The proportion of COVID-related deaths from long COVID peaked in June 2021 at 1.2% and again in April 2022 at 3.8%, according to the CDC. Both of these peaks coincided with periods of declining fatalities from acute infections.
“I do expect that deaths associated with long COVID will make up an increasingly larger proportion of total deaths associated with COVID-19,” said Mark Czeisler, PhD, a researcher at Harvard Medical School, Boston, Massachusetts, who has studied long COVID fatalities.
Months and even years after an acute infection, long COVID can contribute to serious and potentially life-threatening conditions that impact nearly every major system in the body, according to the CDC guidelines for identifying the condition on death certificates.
This means long COVID may often be listed as an underlying cause of death when people with this condition die of issues related to their heart, lungs, brain or kidneys, the CDC guidelines noted.
The risk for long COVID fatalities remains elevated for at least 6 months for people with milder acute infections and for at least 2 years in severe cases that require hospitalization, some previous research suggested.
As happens with other acute infections, certain people are more at risk for fatal case of long COVID. Age, race, and ethnicity have all been cited as risk factors by researchers who have been tracking the condition since the start of the pandemic.
Half of long COVID fatalities from July 2021 to June 2022 occurred in people aged 65 years and older, and another 23% were recorded among people aged 50-64 years old, according a report from CDC.
Long COVID death rates also varied by race and ethnicity, from a high of 14.1 cases per million among America Indian and Alaskan natives to a low of 1.5 cases per million among Asian people, the CDC found. Death rates per million were 6.7 for White individuals, 6.4 for Black people, and 4.7 for Hispanic people.
The disproportionate share of Black and Hispanic people who developed and died from severe acute infections may have left fewer survivors to develop long COVID, limiting long COVID fatalities among these groups, the CDC report concluded.
It’s also possible that long COVID fatalities were undercounted in these populations because they faced challenges accessing healthcare or seeing providers who could recognize the hallmark symptoms of long COVID.
It’s also difficult to distinguish between how many deaths related to the virus ultimately occur as a result of long COVID rather than acute infections. That’s because it may depend on a variety of factors, including how consistently medical examiners follow the CDC guidelines, said Ziyad Al-Aly, MD, chief of research at the Veterans Affairs, St. Louis Health Care System and a senior clinical epidemiologist at Washington University in St. Louis.
“Long COVID remains massively underdiagnosed, and death in people with long COVID is misattributed to other things,” Dr. Al-Aly said.
An accurate test for long COVID could help lead to a more accurate count of these fatalities, Dr. Czeisler said. Some preliminary research suggests that it might one day be possible to diagnose long COVID with a blood test.
“The timeline for such a test and the extent to which it would be widely applied is uncertain,” Dr. Czeisler noted, “though that would certainly be a gamechanger.”
A version of this article appeared on Medscape.com.
While COVID has now claimed more than 1 million lives in the United States alone, these aren’t the only fatalities caused at least in part by the virus. A small but growing number of Americans are surviving acute infections only to succumb months later to the lingering health problems caused by long COVID.
Much of the attention on long COVID has centered on the sometimes debilitating symptoms that strike people with the condition, with no formal diagnostic tests or standard treatments available, and the effect it has on quality of life. But new figures from the US Centers for Disease Control and Prevention (CDC) show that long COVID can also be deadly.
More than 5000 Americans have died from long COVID since the start of the pandemic, according to new estimates from the CDC.
This total, based on death certificate data collected by the CDC, includes a preliminary tally of 1491 long COVID deaths in 2023 in addition to 3544 fatalities previously reported from January 2020 through June 2022.
Guidance issued in 2023 on how to formally report long COVID as a cause of death on death certificates should help get a more accurate count of these fatalities going forward, said Robert Anderson, PhD, chief mortality statistician for the CDC, Atlanta, Georgia.
“We hope that the guidance will help cause of death certifiers be more aware of the impact of long COVID and more likely to report long COVID as a cause of death when appropriate,” Dr. Anderson said. “That said, we do not expect that this guidance will have a dramatic impact on the trend.”
There’s no standard definition or diagnostic test for long COVID. It’s typically diagnosed when people have symptoms at least 3 months after an acute infection that weren’t present before they got sick. As of the end of last year, about 7% of American adults had experienced long COVID at some point, the CDC estimated in September 2023.
The new death tally indicates long COVID remains a significant public health threat and is likely to grow in the years ahead, even though the pandemic may no longer be considered a global health crisis, experts said.
For example, the death certificate figures indicate:
COVID-19 was the third leading cause of American deaths in 2020 and 2021, and the fourth leading cause of death in the United States in 2023.
Nearly 1% of the more than one million deaths related to COVID-19 since the start of the pandemic have been attributed to long COVID, according to data released by the CDC.
The proportion of COVID-related deaths from long COVID peaked in June 2021 at 1.2% and again in April 2022 at 3.8%, according to the CDC. Both of these peaks coincided with periods of declining fatalities from acute infections.
“I do expect that deaths associated with long COVID will make up an increasingly larger proportion of total deaths associated with COVID-19,” said Mark Czeisler, PhD, a researcher at Harvard Medical School, Boston, Massachusetts, who has studied long COVID fatalities.
Months and even years after an acute infection, long COVID can contribute to serious and potentially life-threatening conditions that impact nearly every major system in the body, according to the CDC guidelines for identifying the condition on death certificates.
This means long COVID may often be listed as an underlying cause of death when people with this condition die of issues related to their heart, lungs, brain or kidneys, the CDC guidelines noted.
The risk for long COVID fatalities remains elevated for at least 6 months for people with milder acute infections and for at least 2 years in severe cases that require hospitalization, some previous research suggested.
As happens with other acute infections, certain people are more at risk for fatal case of long COVID. Age, race, and ethnicity have all been cited as risk factors by researchers who have been tracking the condition since the start of the pandemic.
Half of long COVID fatalities from July 2021 to June 2022 occurred in people aged 65 years and older, and another 23% were recorded among people aged 50-64 years old, according a report from CDC.
Long COVID death rates also varied by race and ethnicity, from a high of 14.1 cases per million among America Indian and Alaskan natives to a low of 1.5 cases per million among Asian people, the CDC found. Death rates per million were 6.7 for White individuals, 6.4 for Black people, and 4.7 for Hispanic people.
The disproportionate share of Black and Hispanic people who developed and died from severe acute infections may have left fewer survivors to develop long COVID, limiting long COVID fatalities among these groups, the CDC report concluded.
It’s also possible that long COVID fatalities were undercounted in these populations because they faced challenges accessing healthcare or seeing providers who could recognize the hallmark symptoms of long COVID.
It’s also difficult to distinguish between how many deaths related to the virus ultimately occur as a result of long COVID rather than acute infections. That’s because it may depend on a variety of factors, including how consistently medical examiners follow the CDC guidelines, said Ziyad Al-Aly, MD, chief of research at the Veterans Affairs, St. Louis Health Care System and a senior clinical epidemiologist at Washington University in St. Louis.
“Long COVID remains massively underdiagnosed, and death in people with long COVID is misattributed to other things,” Dr. Al-Aly said.
An accurate test for long COVID could help lead to a more accurate count of these fatalities, Dr. Czeisler said. Some preliminary research suggests that it might one day be possible to diagnose long COVID with a blood test.
“The timeline for such a test and the extent to which it would be widely applied is uncertain,” Dr. Czeisler noted, “though that would certainly be a gamechanger.”
A version of this article appeared on Medscape.com.
While COVID has now claimed more than 1 million lives in the United States alone, these aren’t the only fatalities caused at least in part by the virus. A small but growing number of Americans are surviving acute infections only to succumb months later to the lingering health problems caused by long COVID.
Much of the attention on long COVID has centered on the sometimes debilitating symptoms that strike people with the condition, with no formal diagnostic tests or standard treatments available, and the effect it has on quality of life. But new figures from the US Centers for Disease Control and Prevention (CDC) show that long COVID can also be deadly.
More than 5000 Americans have died from long COVID since the start of the pandemic, according to new estimates from the CDC.
This total, based on death certificate data collected by the CDC, includes a preliminary tally of 1491 long COVID deaths in 2023 in addition to 3544 fatalities previously reported from January 2020 through June 2022.
Guidance issued in 2023 on how to formally report long COVID as a cause of death on death certificates should help get a more accurate count of these fatalities going forward, said Robert Anderson, PhD, chief mortality statistician for the CDC, Atlanta, Georgia.
“We hope that the guidance will help cause of death certifiers be more aware of the impact of long COVID and more likely to report long COVID as a cause of death when appropriate,” Dr. Anderson said. “That said, we do not expect that this guidance will have a dramatic impact on the trend.”
There’s no standard definition or diagnostic test for long COVID. It’s typically diagnosed when people have symptoms at least 3 months after an acute infection that weren’t present before they got sick. As of the end of last year, about 7% of American adults had experienced long COVID at some point, the CDC estimated in September 2023.
The new death tally indicates long COVID remains a significant public health threat and is likely to grow in the years ahead, even though the pandemic may no longer be considered a global health crisis, experts said.
For example, the death certificate figures indicate:
COVID-19 was the third leading cause of American deaths in 2020 and 2021, and the fourth leading cause of death in the United States in 2023.
Nearly 1% of the more than one million deaths related to COVID-19 since the start of the pandemic have been attributed to long COVID, according to data released by the CDC.
The proportion of COVID-related deaths from long COVID peaked in June 2021 at 1.2% and again in April 2022 at 3.8%, according to the CDC. Both of these peaks coincided with periods of declining fatalities from acute infections.
“I do expect that deaths associated with long COVID will make up an increasingly larger proportion of total deaths associated with COVID-19,” said Mark Czeisler, PhD, a researcher at Harvard Medical School, Boston, Massachusetts, who has studied long COVID fatalities.
Months and even years after an acute infection, long COVID can contribute to serious and potentially life-threatening conditions that impact nearly every major system in the body, according to the CDC guidelines for identifying the condition on death certificates.
This means long COVID may often be listed as an underlying cause of death when people with this condition die of issues related to their heart, lungs, brain or kidneys, the CDC guidelines noted.
The risk for long COVID fatalities remains elevated for at least 6 months for people with milder acute infections and for at least 2 years in severe cases that require hospitalization, some previous research suggested.
As happens with other acute infections, certain people are more at risk for fatal case of long COVID. Age, race, and ethnicity have all been cited as risk factors by researchers who have been tracking the condition since the start of the pandemic.
Half of long COVID fatalities from July 2021 to June 2022 occurred in people aged 65 years and older, and another 23% were recorded among people aged 50-64 years old, according a report from CDC.
Long COVID death rates also varied by race and ethnicity, from a high of 14.1 cases per million among America Indian and Alaskan natives to a low of 1.5 cases per million among Asian people, the CDC found. Death rates per million were 6.7 for White individuals, 6.4 for Black people, and 4.7 for Hispanic people.
The disproportionate share of Black and Hispanic people who developed and died from severe acute infections may have left fewer survivors to develop long COVID, limiting long COVID fatalities among these groups, the CDC report concluded.
It’s also possible that long COVID fatalities were undercounted in these populations because they faced challenges accessing healthcare or seeing providers who could recognize the hallmark symptoms of long COVID.
It’s also difficult to distinguish between how many deaths related to the virus ultimately occur as a result of long COVID rather than acute infections. That’s because it may depend on a variety of factors, including how consistently medical examiners follow the CDC guidelines, said Ziyad Al-Aly, MD, chief of research at the Veterans Affairs, St. Louis Health Care System and a senior clinical epidemiologist at Washington University in St. Louis.
“Long COVID remains massively underdiagnosed, and death in people with long COVID is misattributed to other things,” Dr. Al-Aly said.
An accurate test for long COVID could help lead to a more accurate count of these fatalities, Dr. Czeisler said. Some preliminary research suggests that it might one day be possible to diagnose long COVID with a blood test.
“The timeline for such a test and the extent to which it would be widely applied is uncertain,” Dr. Czeisler noted, “though that would certainly be a gamechanger.”
A version of this article appeared on Medscape.com.
Short Course of Amoxicillin Shows Effectiveness for Febrile UTIs
Use of oral amoxicillin-clavulanic acid for 5 days was noninferior to a 10-day course of treatment among children with noncomplicated febrile urinary tract infections (UTIs), according to new research.
Well-appearing children with febrile UTIs are generally treated with a 10-day course of oral antibiotics, but the effectiveness of a 5-day course has not been evaluated, wrote Giovanni Montini, MD, of the University of Milan, Milan, Italy, and colleagues.
Robert W. Frenck Jr, MD, a director of the Center for Vaccine Research at Cincinnati Children’s Hospital Medical Center, Ohio, said he was not surprised that the shorter course was sufficient to treat these cases. The antibiotic concentration in the urine often significantly exceeds the levels in the blood, he said.
Dr. Frenck, who was not involved in the study, said that he saw no real barriers to the use of a shorter course of therapy in clinical practice.
“I think both parents and the medical team would be happy to be able to use a shorter course of therapy,” he said.
In the study published in Pediatrics , researchers randomized 142 children aged 3 months to 5 years with uncomplicated febrile UTIs to 50 mg/kg/d of amoxicillin-clavulanate for either the short or standard period. The study took place at eight pediatric emergency departments in Italy between May 2020 and September 2022. All patients received prescriptions for 5 days of antibiotics, and those randomized to the standard course received a second prescription after randomization.
The primary endpoint was recurrence of the UTI within 30 days of completion of therapy. Secondary endpoints included clinical recovery at the end of treatment, adverse events related to the therapy, and signs of antibiotic resistance.
The UTI recurrence rate within 30 days of treatment completion was 2.8% in the short-course group and 14.3% in the standard group. A post hoc analysis excluding patients with vesicoureteral reflux and non–Escherichia coli UTIs further confirmed the noninferiority of short-course treatment.
“It is a bit surprising that the short-course group had fewer relapses within 30 days of discontinuing antibiotics,” Dr. Frenck said. “However, the differences may be due to small sample sizes and do not appear to be statistically significant differences in recurrence rates.”
Resolution of symptoms was similar between the short-course and standard groups (97.2% and 92.9%, respectively), and indications of antibiotic resistance were similar between the groups. No adverse events were reported in the standard group, and one case of diarrhea occurred in the short-course group.
The findings were limited by the study’s unblinded randomization, so parents were aware of the trial and were potentially sensitized to look for signs of infection. Researchers also relied on parent reports of adverse drug effects rather than through a standardized questionnaire, the researchers noted.
Dr. Frenck said a potential benefit to shortening treatment is that adherence usually increases.
“But you only want to decrease the length of a course of medicine if you can do so without compromising the effectiveness of the treatment,” Dr. Frenck said.
Dr. Frenck also noted a recent study, which demonstrated that 5 days of antibiotics had equivalent efficacy as 10 days for uncomplicated pneumonia.
“The current paper further demonstrates that shorter courses of antibiotics may be possible for other mild forms of infections.”
Looking ahead, researchers could evaluate the use of short-course antibiotics for other common infections such as otitis media, he noted.
The study was supported by the Ministry of Health, Rome, Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy. The researchers report no financial conflicts. Dr. Frenck disclosed conducting clinical trials for Pfizer, Moderna, AstraZeneca, Merck, and GSK; none of those trials were for antibiotics or urinary tract infections.
A version of this article appeared on Medscape.com.
Use of oral amoxicillin-clavulanic acid for 5 days was noninferior to a 10-day course of treatment among children with noncomplicated febrile urinary tract infections (UTIs), according to new research.
Well-appearing children with febrile UTIs are generally treated with a 10-day course of oral antibiotics, but the effectiveness of a 5-day course has not been evaluated, wrote Giovanni Montini, MD, of the University of Milan, Milan, Italy, and colleagues.
Robert W. Frenck Jr, MD, a director of the Center for Vaccine Research at Cincinnati Children’s Hospital Medical Center, Ohio, said he was not surprised that the shorter course was sufficient to treat these cases. The antibiotic concentration in the urine often significantly exceeds the levels in the blood, he said.
Dr. Frenck, who was not involved in the study, said that he saw no real barriers to the use of a shorter course of therapy in clinical practice.
“I think both parents and the medical team would be happy to be able to use a shorter course of therapy,” he said.
In the study published in Pediatrics , researchers randomized 142 children aged 3 months to 5 years with uncomplicated febrile UTIs to 50 mg/kg/d of amoxicillin-clavulanate for either the short or standard period. The study took place at eight pediatric emergency departments in Italy between May 2020 and September 2022. All patients received prescriptions for 5 days of antibiotics, and those randomized to the standard course received a second prescription after randomization.
The primary endpoint was recurrence of the UTI within 30 days of completion of therapy. Secondary endpoints included clinical recovery at the end of treatment, adverse events related to the therapy, and signs of antibiotic resistance.
The UTI recurrence rate within 30 days of treatment completion was 2.8% in the short-course group and 14.3% in the standard group. A post hoc analysis excluding patients with vesicoureteral reflux and non–Escherichia coli UTIs further confirmed the noninferiority of short-course treatment.
“It is a bit surprising that the short-course group had fewer relapses within 30 days of discontinuing antibiotics,” Dr. Frenck said. “However, the differences may be due to small sample sizes and do not appear to be statistically significant differences in recurrence rates.”
Resolution of symptoms was similar between the short-course and standard groups (97.2% and 92.9%, respectively), and indications of antibiotic resistance were similar between the groups. No adverse events were reported in the standard group, and one case of diarrhea occurred in the short-course group.
The findings were limited by the study’s unblinded randomization, so parents were aware of the trial and were potentially sensitized to look for signs of infection. Researchers also relied on parent reports of adverse drug effects rather than through a standardized questionnaire, the researchers noted.
Dr. Frenck said a potential benefit to shortening treatment is that adherence usually increases.
“But you only want to decrease the length of a course of medicine if you can do so without compromising the effectiveness of the treatment,” Dr. Frenck said.
Dr. Frenck also noted a recent study, which demonstrated that 5 days of antibiotics had equivalent efficacy as 10 days for uncomplicated pneumonia.
“The current paper further demonstrates that shorter courses of antibiotics may be possible for other mild forms of infections.”
Looking ahead, researchers could evaluate the use of short-course antibiotics for other common infections such as otitis media, he noted.
The study was supported by the Ministry of Health, Rome, Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy. The researchers report no financial conflicts. Dr. Frenck disclosed conducting clinical trials for Pfizer, Moderna, AstraZeneca, Merck, and GSK; none of those trials were for antibiotics or urinary tract infections.
A version of this article appeared on Medscape.com.
Use of oral amoxicillin-clavulanic acid for 5 days was noninferior to a 10-day course of treatment among children with noncomplicated febrile urinary tract infections (UTIs), according to new research.
Well-appearing children with febrile UTIs are generally treated with a 10-day course of oral antibiotics, but the effectiveness of a 5-day course has not been evaluated, wrote Giovanni Montini, MD, of the University of Milan, Milan, Italy, and colleagues.
Robert W. Frenck Jr, MD, a director of the Center for Vaccine Research at Cincinnati Children’s Hospital Medical Center, Ohio, said he was not surprised that the shorter course was sufficient to treat these cases. The antibiotic concentration in the urine often significantly exceeds the levels in the blood, he said.
Dr. Frenck, who was not involved in the study, said that he saw no real barriers to the use of a shorter course of therapy in clinical practice.
“I think both parents and the medical team would be happy to be able to use a shorter course of therapy,” he said.
In the study published in Pediatrics , researchers randomized 142 children aged 3 months to 5 years with uncomplicated febrile UTIs to 50 mg/kg/d of amoxicillin-clavulanate for either the short or standard period. The study took place at eight pediatric emergency departments in Italy between May 2020 and September 2022. All patients received prescriptions for 5 days of antibiotics, and those randomized to the standard course received a second prescription after randomization.
The primary endpoint was recurrence of the UTI within 30 days of completion of therapy. Secondary endpoints included clinical recovery at the end of treatment, adverse events related to the therapy, and signs of antibiotic resistance.
The UTI recurrence rate within 30 days of treatment completion was 2.8% in the short-course group and 14.3% in the standard group. A post hoc analysis excluding patients with vesicoureteral reflux and non–Escherichia coli UTIs further confirmed the noninferiority of short-course treatment.
“It is a bit surprising that the short-course group had fewer relapses within 30 days of discontinuing antibiotics,” Dr. Frenck said. “However, the differences may be due to small sample sizes and do not appear to be statistically significant differences in recurrence rates.”
Resolution of symptoms was similar between the short-course and standard groups (97.2% and 92.9%, respectively), and indications of antibiotic resistance were similar between the groups. No adverse events were reported in the standard group, and one case of diarrhea occurred in the short-course group.
The findings were limited by the study’s unblinded randomization, so parents were aware of the trial and were potentially sensitized to look for signs of infection. Researchers also relied on parent reports of adverse drug effects rather than through a standardized questionnaire, the researchers noted.
Dr. Frenck said a potential benefit to shortening treatment is that adherence usually increases.
“But you only want to decrease the length of a course of medicine if you can do so without compromising the effectiveness of the treatment,” Dr. Frenck said.
Dr. Frenck also noted a recent study, which demonstrated that 5 days of antibiotics had equivalent efficacy as 10 days for uncomplicated pneumonia.
“The current paper further demonstrates that shorter courses of antibiotics may be possible for other mild forms of infections.”
Looking ahead, researchers could evaluate the use of short-course antibiotics for other common infections such as otitis media, he noted.
The study was supported by the Ministry of Health, Rome, Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy. The researchers report no financial conflicts. Dr. Frenck disclosed conducting clinical trials for Pfizer, Moderna, AstraZeneca, Merck, and GSK; none of those trials were for antibiotics or urinary tract infections.
A version of this article appeared on Medscape.com.
FROM PEDIATRICS
Hospital Adverse Events Rise After Private Equity Acquisition
Hospital-acquired adverse events or conditions including falls and infections increased by approximately 25% after hospitals’ acquisition by private equity compared with control hospitals, on the basis of a study of Medicare claims for more than 4,500,000 hospitalizations.
“Prior research on private equity in health care showed that acquisition is associated with higher charges, prices, and spending; however, the implications for quality of care and patient outcomes remained less understood,” corresponding author Zirui Song, MD, of Harvard Medical School, Boston, said in an interview. “This was particularly true for measures of clinical quality that were less susceptible to changes in patient mix or coding behavior, such as hospital-acquired adverse events.”
In the study, published in JAMA, the researchers compared data from 100% Medicare Part A claims for 662,095 hospitalizations at 51 hospitals acquired by private equities and 4,160,720 hospitalizations at 259 control hospitals. The hospitalizations occurred between 2009 and 2019. The researchers also used a difference-in-differences design to evaluate hospitalizations from 3 years before to 3 years after acquisition, controlling for patient and hospital attributes.
Hospital-acquired adverse events as defined by the US Centers for Medicare & Medicaid Services included falls, infections, stage III or IV pressure ulcers, foreign objects retained after surgery, air embolism, and blood incompatibility.
Overall, Medicare patients in private equity hospitals experienced a 25.4% increase in hospital-acquired conditions compared with those in control hospitals through a period of up to 3 years after acquisition, with a difference of 4.6 additional hospital-acquired conditions per 10,000 hospitalizations (P = .004). Central line-associated bloodstream infections accounted for 37.7% of the increase (P = .04), despite a 16.2% decrease in placement of central lines, and falls accounted for 27.3% (P = .02).
Notably, the incidence of surgical site infections increased from 10.8 per 10,000 hospitalizations before acquisition to 21.6 per 10,000 hospitalizations after acquisition, despite a reduction of 8.1% in surgical volume. By contrast, surgical site infections decreased at control hospitals over the study period.
In-hospital mortality decreased slightly at private equity hospitals compared with the control hospitals, but there was no differential change in mortality by 30 days after hospital discharge. The slight difference might be caused by the trend in slightly younger Medicare beneficiaries treated at private equity hospitals; these patients were less likely to be eligible for both Medicaid and Medicare and were more likely to be transferred to other hospitals, the researchers noted.
The findings were limited by several factors including the lack of generalizability to all private equity-acquired hospitals and to non-Medicare patients, the researchers noted. Other limitations include the use of the International Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) codes that might have failed to capture all hospital-acquired conditions and the inability to account for all confounding factors.
However, the results suggest that private equity acquisition was associated with increased hospital-acquired adverse events and highlight concerns about the impact of private equity ownership on healthcare delivery, the researchers concluded.
In a related story published in July 2023, this news organization described a report showing an association between private equity ownership of medical practices and increased consumer prices for multiple medical specialties.
“Medicare patients admitted to private equity-owned hospitals experienced, on average, an 25% increase in hospital-acquired adverse events after the hospital was bought compared to similar patients at hospitals not acquired by private equity firms. We were surprised by the extent of this change relative to the comparison (non-private equity) hospitals, including the sizable increase in central line-associated bloodstream infections and the doubling of surgical site infections at private equity hospitals — both of which went down at the comparison hospitals during the same period,” Dr. Song said in an interview.
“A key implication is that patients, providers, and policymakers might be more attuned to the potential clinical impact of private equity ownership in the delivery system. Given that a plausible explanation for these findings is reductions in clinician staffing, clinical organizations and policymakers might also be more aware of cost-cutting strategies after acquisition,” Dr. Song said. “Prior research has shown that hospitals, nursing homes, and physician practices experience staffing cuts after private equity acquisition, which is a common way to reduce operating costs and boost the profitability of acquired entities,” he noted.
“More research is needed to understand the impact of private equity acquisitions across health care settings and the potential effects of policy levers that aim to protect patients and societal resources,” said Dr. Song, who coauthored an article outlining a policy framework for addressing private equity in healthcare, published in JAMA in April 2023. “Potential regulatory remedies include minimum staffing ratios, antitrust enforcement, mitigating the financial risk of such acquisitions, increasing the transparency of these acquisitions, and protecting patients and society from the higher prices of care attributed to this model of provider ownership,” he said.
Patients Pay the Price of Private Equity Acquisition
“The exponential growth in private equity ownership in hospital and physician practices in the past few decades has left a majority of health care providers disillusioned with cost-cutting practices resulting in staffing reductions and ratios that sacrifice patient care as part of their approach to running clinical operations ‘lean,’ ” Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, NY, said in an interview.
“While private equity companies argue that such practices are essential to meet their bottom line and increase operating margins, it doesn’t translate into ideal care for patients; lean practices in staffing which focus on profits at the expense of patient safety and quality of care.
“When you look at patient outcomes, it is the patients who ultimately pay the price — not the shareholders,” Dr. Glatter said. “This translates to higher risks of hospital-acquired complications including falls and blood-borne infections, including surgical site infections, as noted by the authors of the current study when private equity took over operations in hospitals.
Dr. Glatter said he was not surprised by the findings. “In my world, patient care and safety come first. Period,” he said. “Would you want your family’s health and well-being sacrificed in the name of company profits? I think it’s a rhetorical question, but one that every health care provider who works in a hospital or practice run by private equity must consider.”
Despite a decline in utilization at private equity hospitals as noted in the current study, hospital-acquired infections and adverse outcomes still increased, illustrating a decline in quality of care, said Dr. Glatter. “While these disparities were not evident when looking at 30-day outcomes, they demonstrate how operational changes impact patient outcomes in the near term. Having younger and healthier patients, and fewer Medicare and Medicaid patients combined with more hospital transfers to non–private equity run hospitals, resulted in lower in-hospital mortality in the near term, which was not apparent at 30 days post discharge,” he said.
“The explosion of hospital mergers and consolidation in the past several decades has led to skyrocketing health care costs at the expense of patient satisfaction, but also health care providers’ autonomy to manage and maintain quality care for their patients,” Dr. Glatter said.
“It’s important to understand that private equity’s interests are primarily aligned with their shareholder’s interests, as opposed to patients’ outcomes and interests,” Dr. Glatter told this news organization. “Within 5-7 years, the goal is to increase operating margins and profits and then sell a practice or hospital, which is ultimately part of a ‘health care portfolio,’ ” he said.
Additional research is needed to examine whether other hospital-acquired conditions including pressure sores, catheter-associated UTIs, methicillin-resistant Staphylococcus aureus infections, Clostridium difficile infections, and nosocomial pneumonia have increased in hospitals following private equity acquisition, given the overall national decline in these events, he said.
“At the same time, it is vital to also look at management and readmission rates for patients with strokes, heart attacks, and congestive heart failure in hospitals that are run by private equity,” Dr. Glatter noted. “These are important benchmarks of care monitored by CMS that reflect the quality of care that payers ultimately factor into reimbursement.”
Examining the metrics associated with these diagnoses will help in understanding whether private equity-managed facilities are leading to adverse outcomes and mortality, increased length of stay, hospital readmissions, and increased nosocomial infections, apart from other aspects of patient experience, Dr. Glatter added.
The study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and Arnold Ventures. The researchers had no financial conflicts to disclose. Dr. Glatter had no financial conflicts to disclose and serves on the Medscape Emergency Medicine Editorial Board.
A version of this article appeared on Medscape.com.
Hospital-acquired adverse events or conditions including falls and infections increased by approximately 25% after hospitals’ acquisition by private equity compared with control hospitals, on the basis of a study of Medicare claims for more than 4,500,000 hospitalizations.
“Prior research on private equity in health care showed that acquisition is associated with higher charges, prices, and spending; however, the implications for quality of care and patient outcomes remained less understood,” corresponding author Zirui Song, MD, of Harvard Medical School, Boston, said in an interview. “This was particularly true for measures of clinical quality that were less susceptible to changes in patient mix or coding behavior, such as hospital-acquired adverse events.”
In the study, published in JAMA, the researchers compared data from 100% Medicare Part A claims for 662,095 hospitalizations at 51 hospitals acquired by private equities and 4,160,720 hospitalizations at 259 control hospitals. The hospitalizations occurred between 2009 and 2019. The researchers also used a difference-in-differences design to evaluate hospitalizations from 3 years before to 3 years after acquisition, controlling for patient and hospital attributes.
Hospital-acquired adverse events as defined by the US Centers for Medicare & Medicaid Services included falls, infections, stage III or IV pressure ulcers, foreign objects retained after surgery, air embolism, and blood incompatibility.
Overall, Medicare patients in private equity hospitals experienced a 25.4% increase in hospital-acquired conditions compared with those in control hospitals through a period of up to 3 years after acquisition, with a difference of 4.6 additional hospital-acquired conditions per 10,000 hospitalizations (P = .004). Central line-associated bloodstream infections accounted for 37.7% of the increase (P = .04), despite a 16.2% decrease in placement of central lines, and falls accounted for 27.3% (P = .02).
Notably, the incidence of surgical site infections increased from 10.8 per 10,000 hospitalizations before acquisition to 21.6 per 10,000 hospitalizations after acquisition, despite a reduction of 8.1% in surgical volume. By contrast, surgical site infections decreased at control hospitals over the study period.
In-hospital mortality decreased slightly at private equity hospitals compared with the control hospitals, but there was no differential change in mortality by 30 days after hospital discharge. The slight difference might be caused by the trend in slightly younger Medicare beneficiaries treated at private equity hospitals; these patients were less likely to be eligible for both Medicaid and Medicare and were more likely to be transferred to other hospitals, the researchers noted.
The findings were limited by several factors including the lack of generalizability to all private equity-acquired hospitals and to non-Medicare patients, the researchers noted. Other limitations include the use of the International Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) codes that might have failed to capture all hospital-acquired conditions and the inability to account for all confounding factors.
However, the results suggest that private equity acquisition was associated with increased hospital-acquired adverse events and highlight concerns about the impact of private equity ownership on healthcare delivery, the researchers concluded.
In a related story published in July 2023, this news organization described a report showing an association between private equity ownership of medical practices and increased consumer prices for multiple medical specialties.
“Medicare patients admitted to private equity-owned hospitals experienced, on average, an 25% increase in hospital-acquired adverse events after the hospital was bought compared to similar patients at hospitals not acquired by private equity firms. We were surprised by the extent of this change relative to the comparison (non-private equity) hospitals, including the sizable increase in central line-associated bloodstream infections and the doubling of surgical site infections at private equity hospitals — both of which went down at the comparison hospitals during the same period,” Dr. Song said in an interview.
“A key implication is that patients, providers, and policymakers might be more attuned to the potential clinical impact of private equity ownership in the delivery system. Given that a plausible explanation for these findings is reductions in clinician staffing, clinical organizations and policymakers might also be more aware of cost-cutting strategies after acquisition,” Dr. Song said. “Prior research has shown that hospitals, nursing homes, and physician practices experience staffing cuts after private equity acquisition, which is a common way to reduce operating costs and boost the profitability of acquired entities,” he noted.
“More research is needed to understand the impact of private equity acquisitions across health care settings and the potential effects of policy levers that aim to protect patients and societal resources,” said Dr. Song, who coauthored an article outlining a policy framework for addressing private equity in healthcare, published in JAMA in April 2023. “Potential regulatory remedies include minimum staffing ratios, antitrust enforcement, mitigating the financial risk of such acquisitions, increasing the transparency of these acquisitions, and protecting patients and society from the higher prices of care attributed to this model of provider ownership,” he said.
Patients Pay the Price of Private Equity Acquisition
“The exponential growth in private equity ownership in hospital and physician practices in the past few decades has left a majority of health care providers disillusioned with cost-cutting practices resulting in staffing reductions and ratios that sacrifice patient care as part of their approach to running clinical operations ‘lean,’ ” Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, NY, said in an interview.
“While private equity companies argue that such practices are essential to meet their bottom line and increase operating margins, it doesn’t translate into ideal care for patients; lean practices in staffing which focus on profits at the expense of patient safety and quality of care.
“When you look at patient outcomes, it is the patients who ultimately pay the price — not the shareholders,” Dr. Glatter said. “This translates to higher risks of hospital-acquired complications including falls and blood-borne infections, including surgical site infections, as noted by the authors of the current study when private equity took over operations in hospitals.
Dr. Glatter said he was not surprised by the findings. “In my world, patient care and safety come first. Period,” he said. “Would you want your family’s health and well-being sacrificed in the name of company profits? I think it’s a rhetorical question, but one that every health care provider who works in a hospital or practice run by private equity must consider.”
Despite a decline in utilization at private equity hospitals as noted in the current study, hospital-acquired infections and adverse outcomes still increased, illustrating a decline in quality of care, said Dr. Glatter. “While these disparities were not evident when looking at 30-day outcomes, they demonstrate how operational changes impact patient outcomes in the near term. Having younger and healthier patients, and fewer Medicare and Medicaid patients combined with more hospital transfers to non–private equity run hospitals, resulted in lower in-hospital mortality in the near term, which was not apparent at 30 days post discharge,” he said.
“The explosion of hospital mergers and consolidation in the past several decades has led to skyrocketing health care costs at the expense of patient satisfaction, but also health care providers’ autonomy to manage and maintain quality care for their patients,” Dr. Glatter said.
“It’s important to understand that private equity’s interests are primarily aligned with their shareholder’s interests, as opposed to patients’ outcomes and interests,” Dr. Glatter told this news organization. “Within 5-7 years, the goal is to increase operating margins and profits and then sell a practice or hospital, which is ultimately part of a ‘health care portfolio,’ ” he said.
Additional research is needed to examine whether other hospital-acquired conditions including pressure sores, catheter-associated UTIs, methicillin-resistant Staphylococcus aureus infections, Clostridium difficile infections, and nosocomial pneumonia have increased in hospitals following private equity acquisition, given the overall national decline in these events, he said.
“At the same time, it is vital to also look at management and readmission rates for patients with strokes, heart attacks, and congestive heart failure in hospitals that are run by private equity,” Dr. Glatter noted. “These are important benchmarks of care monitored by CMS that reflect the quality of care that payers ultimately factor into reimbursement.”
Examining the metrics associated with these diagnoses will help in understanding whether private equity-managed facilities are leading to adverse outcomes and mortality, increased length of stay, hospital readmissions, and increased nosocomial infections, apart from other aspects of patient experience, Dr. Glatter added.
The study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and Arnold Ventures. The researchers had no financial conflicts to disclose. Dr. Glatter had no financial conflicts to disclose and serves on the Medscape Emergency Medicine Editorial Board.
A version of this article appeared on Medscape.com.
Hospital-acquired adverse events or conditions including falls and infections increased by approximately 25% after hospitals’ acquisition by private equity compared with control hospitals, on the basis of a study of Medicare claims for more than 4,500,000 hospitalizations.
“Prior research on private equity in health care showed that acquisition is associated with higher charges, prices, and spending; however, the implications for quality of care and patient outcomes remained less understood,” corresponding author Zirui Song, MD, of Harvard Medical School, Boston, said in an interview. “This was particularly true for measures of clinical quality that were less susceptible to changes in patient mix or coding behavior, such as hospital-acquired adverse events.”
In the study, published in JAMA, the researchers compared data from 100% Medicare Part A claims for 662,095 hospitalizations at 51 hospitals acquired by private equities and 4,160,720 hospitalizations at 259 control hospitals. The hospitalizations occurred between 2009 and 2019. The researchers also used a difference-in-differences design to evaluate hospitalizations from 3 years before to 3 years after acquisition, controlling for patient and hospital attributes.
Hospital-acquired adverse events as defined by the US Centers for Medicare & Medicaid Services included falls, infections, stage III or IV pressure ulcers, foreign objects retained after surgery, air embolism, and blood incompatibility.
Overall, Medicare patients in private equity hospitals experienced a 25.4% increase in hospital-acquired conditions compared with those in control hospitals through a period of up to 3 years after acquisition, with a difference of 4.6 additional hospital-acquired conditions per 10,000 hospitalizations (P = .004). Central line-associated bloodstream infections accounted for 37.7% of the increase (P = .04), despite a 16.2% decrease in placement of central lines, and falls accounted for 27.3% (P = .02).
Notably, the incidence of surgical site infections increased from 10.8 per 10,000 hospitalizations before acquisition to 21.6 per 10,000 hospitalizations after acquisition, despite a reduction of 8.1% in surgical volume. By contrast, surgical site infections decreased at control hospitals over the study period.
In-hospital mortality decreased slightly at private equity hospitals compared with the control hospitals, but there was no differential change in mortality by 30 days after hospital discharge. The slight difference might be caused by the trend in slightly younger Medicare beneficiaries treated at private equity hospitals; these patients were less likely to be eligible for both Medicaid and Medicare and were more likely to be transferred to other hospitals, the researchers noted.
The findings were limited by several factors including the lack of generalizability to all private equity-acquired hospitals and to non-Medicare patients, the researchers noted. Other limitations include the use of the International Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) codes that might have failed to capture all hospital-acquired conditions and the inability to account for all confounding factors.
However, the results suggest that private equity acquisition was associated with increased hospital-acquired adverse events and highlight concerns about the impact of private equity ownership on healthcare delivery, the researchers concluded.
In a related story published in July 2023, this news organization described a report showing an association between private equity ownership of medical practices and increased consumer prices for multiple medical specialties.
“Medicare patients admitted to private equity-owned hospitals experienced, on average, an 25% increase in hospital-acquired adverse events after the hospital was bought compared to similar patients at hospitals not acquired by private equity firms. We were surprised by the extent of this change relative to the comparison (non-private equity) hospitals, including the sizable increase in central line-associated bloodstream infections and the doubling of surgical site infections at private equity hospitals — both of which went down at the comparison hospitals during the same period,” Dr. Song said in an interview.
“A key implication is that patients, providers, and policymakers might be more attuned to the potential clinical impact of private equity ownership in the delivery system. Given that a plausible explanation for these findings is reductions in clinician staffing, clinical organizations and policymakers might also be more aware of cost-cutting strategies after acquisition,” Dr. Song said. “Prior research has shown that hospitals, nursing homes, and physician practices experience staffing cuts after private equity acquisition, which is a common way to reduce operating costs and boost the profitability of acquired entities,” he noted.
“More research is needed to understand the impact of private equity acquisitions across health care settings and the potential effects of policy levers that aim to protect patients and societal resources,” said Dr. Song, who coauthored an article outlining a policy framework for addressing private equity in healthcare, published in JAMA in April 2023. “Potential regulatory remedies include minimum staffing ratios, antitrust enforcement, mitigating the financial risk of such acquisitions, increasing the transparency of these acquisitions, and protecting patients and society from the higher prices of care attributed to this model of provider ownership,” he said.
Patients Pay the Price of Private Equity Acquisition
“The exponential growth in private equity ownership in hospital and physician practices in the past few decades has left a majority of health care providers disillusioned with cost-cutting practices resulting in staffing reductions and ratios that sacrifice patient care as part of their approach to running clinical operations ‘lean,’ ” Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, NY, said in an interview.
“While private equity companies argue that such practices are essential to meet their bottom line and increase operating margins, it doesn’t translate into ideal care for patients; lean practices in staffing which focus on profits at the expense of patient safety and quality of care.
“When you look at patient outcomes, it is the patients who ultimately pay the price — not the shareholders,” Dr. Glatter said. “This translates to higher risks of hospital-acquired complications including falls and blood-borne infections, including surgical site infections, as noted by the authors of the current study when private equity took over operations in hospitals.
Dr. Glatter said he was not surprised by the findings. “In my world, patient care and safety come first. Period,” he said. “Would you want your family’s health and well-being sacrificed in the name of company profits? I think it’s a rhetorical question, but one that every health care provider who works in a hospital or practice run by private equity must consider.”
Despite a decline in utilization at private equity hospitals as noted in the current study, hospital-acquired infections and adverse outcomes still increased, illustrating a decline in quality of care, said Dr. Glatter. “While these disparities were not evident when looking at 30-day outcomes, they demonstrate how operational changes impact patient outcomes in the near term. Having younger and healthier patients, and fewer Medicare and Medicaid patients combined with more hospital transfers to non–private equity run hospitals, resulted in lower in-hospital mortality in the near term, which was not apparent at 30 days post discharge,” he said.
“The explosion of hospital mergers and consolidation in the past several decades has led to skyrocketing health care costs at the expense of patient satisfaction, but also health care providers’ autonomy to manage and maintain quality care for their patients,” Dr. Glatter said.
“It’s important to understand that private equity’s interests are primarily aligned with their shareholder’s interests, as opposed to patients’ outcomes and interests,” Dr. Glatter told this news organization. “Within 5-7 years, the goal is to increase operating margins and profits and then sell a practice or hospital, which is ultimately part of a ‘health care portfolio,’ ” he said.
Additional research is needed to examine whether other hospital-acquired conditions including pressure sores, catheter-associated UTIs, methicillin-resistant Staphylococcus aureus infections, Clostridium difficile infections, and nosocomial pneumonia have increased in hospitals following private equity acquisition, given the overall national decline in these events, he said.
“At the same time, it is vital to also look at management and readmission rates for patients with strokes, heart attacks, and congestive heart failure in hospitals that are run by private equity,” Dr. Glatter noted. “These are important benchmarks of care monitored by CMS that reflect the quality of care that payers ultimately factor into reimbursement.”
Examining the metrics associated with these diagnoses will help in understanding whether private equity-managed facilities are leading to adverse outcomes and mortality, increased length of stay, hospital readmissions, and increased nosocomial infections, apart from other aspects of patient experience, Dr. Glatter added.
The study was supported by the National Heart, Lung, and Blood Institute, the National Institute on Aging, and Arnold Ventures. The researchers had no financial conflicts to disclose. Dr. Glatter had no financial conflicts to disclose and serves on the Medscape Emergency Medicine Editorial Board.
A version of this article appeared on Medscape.com.
Migratory Nodules in a Traveler
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
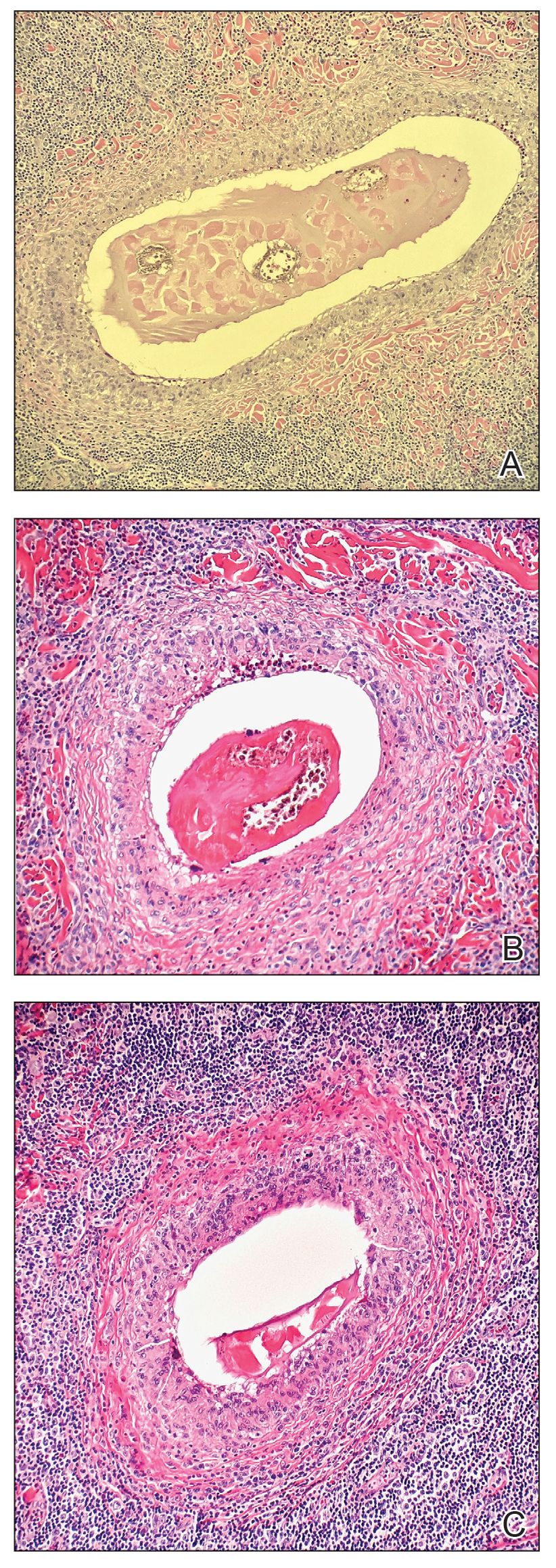
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
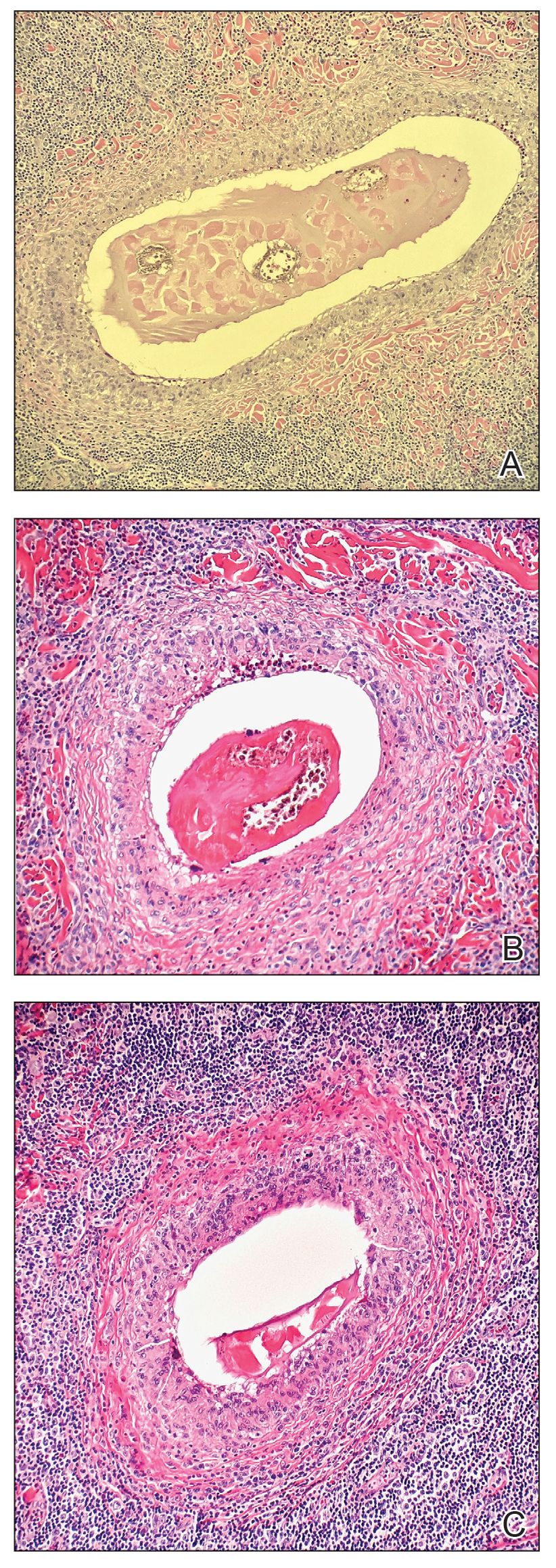
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
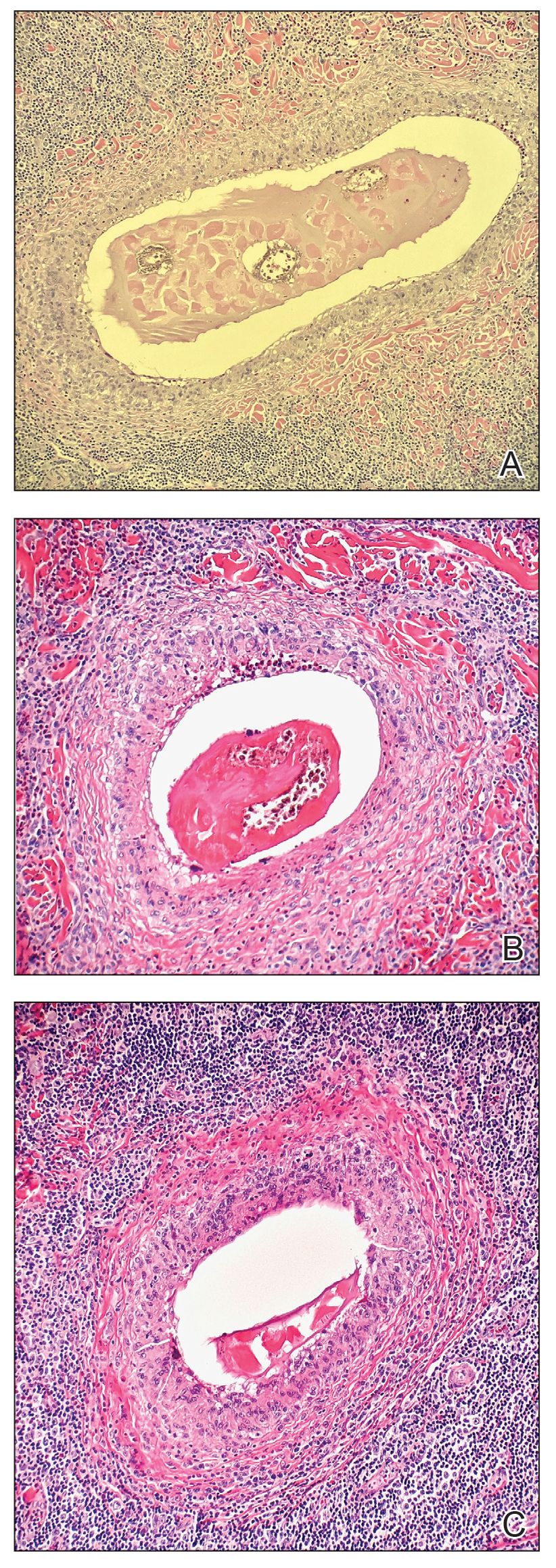
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
A 41-year-old man presented to a dermatology clinic in the United States with a migratory subcutaneous nodule overlying the left upper chest that initially developed 12 months prior and continued to migrate along the trunk and proximal aspect of the arms. The patient had spent the last 3 years residing in Peru. He never observed more than 1 nodule at a time and denied associated fever, headache, visual changes, chest pain, cough, abdominal pain, and diarrhea. Laboratory studies including a blood eosinophil count and serum Strongyloides immunoglobulins were within reference range. An excisional biopsy was performed.

New Insights, New Standards: How 2023 Changed Care for Internists
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
ME/CFS and Long COVID: Research Aims to Identify Treatable, Druggable Pathways
BETHESDA, MD — New research into the mechanisms underlying myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID is aimed at identifying potential approaches to treatment of the two overlapping illnesses.
According to a new data brief from the National Center for Health Statistics, in 2021-2022, 1.3% of US adults had ME/CFS, a complex, multisystem illness characterized by activity-limiting fatigue, worsening of symptoms after exertion, unrefreshing sleep, and other symptoms.
A 2-day conference, Advancing ME/CFS Research: Identifying Targets for Potential Intervention and Learning from Long COVID, was held in December 12-13 on the main campus of the US National Institutes of Health (NIH) and was livestreamed. The last such meeting, also featuring results from NIH-funded research, was held in April 2019.
“Things have changed since 2019 ... The idea of this meeting is to try and identify pathways that will be treatable and druggable and really make an impact for patients based on the things that we’ve learned over the last number of years and including, fortunately or unfortunately, the huge number of people who are suffering from long COVID, where the symptoms overlap so much with those who have been suffering for a long time with ME/CFS,” said Conference Chair Joe Breen, PhD, of the National Institute of Allergy and Infectious Diseases.
As in 2019, the meeting was preceded by a day of research presentations from young investigators, some of whom also presented their findings at the main meeting. New this year were four “lived experience” speakers who described their physical, emotional, and financial struggles with ME/CFS or long COVID. Two of them presented virtually because they were too ill to travel.
Social worker and patient advocate Terri Wilder of Minneapolis, Minnesota, reported some feedback she received on social media after she asked people with ME/CFS about their priorities for the research and clinical communities.
Among the top responses were the need to recognize and study the phenomenon of “post-exertional malaise” and to stop recommending exercise for people with these illnesses, to accelerate research to find effective treatments, and to put an end to stigma around the condition. “People don’t believe us when we tell them we’re sick, people make fun of us, misperceptions persist,” Wilder said.
One person commented, “[Clinicians] shouldn’t be afraid to try off-label meds with us if needed. There may be some secondary effects, but they are better options than us taking our own lives because we can’t stand the suffering.”
Research areas covered at the conference included immunology, virology, metabolism, gene regulation, and neurology of both ME/CFS and long COVID, as well as the latest findings regarding the overlap between the two conditions.
Oxidative Stress in Both ME/CFS and Long COVID: A Role for Metformin?
Mark M. Davis, PhD, professor and director of the Institute for Immunity, Transplantation, and Infection at Stanford University, Palo Alto, California, summarized published data suggesting that oxidative stress is a shared characteristic of both ME/CFS and long COVID. Most cellular reactive oxygen species (ROS) are produced in the cell’s mitochondria, and T-cell activation is ROS-dependent.
Women in particular with ME/CFS show high ROS levels with consistent T-cell hyperproliferation, “which can be suppressed with specific drugs such as metformin. This raises the prospect of optimizing drug treatment and drug discovery with a simple in vitro assay of the effects on a patient’s lymphocytes,” Dr. Davis said. He also cited a study suggesting that metformin may help prevent long COVID.
Asked to comment on that, longtime ME/CFS researcher Anthony L. Komaroff, MD, of Harvard University, Cambridge, Massachusetts, cautioned that although metformin is used safely by millions of people with type 2 diabetes worldwide, it’s possible that some people with ME/CFS may be more likely to experience its known adverse effects such as lactic acidosis.
To repurpose metformin or any other already-marketed drugs for ME/CFS and/or long COVID, Dr. Komaroff said, “We should entertain treatment trials.” However, as he and many others lamented at the conference, funding for off-patent drugs often isn’t forthcoming.
Addressing the Microbiome, Innate Immunity
W. Ian Lipkin, MD, of Columbia University, New York, NY, was one of two speakers who discussed the role of disruptions in the microbiome and innate immunity in ME/CFS. He presented data suggesting that “dysregulation of the gut microbiome in ME/CFS may interfere with butyrate production, resulting in inflammation and porosity to bacteria and bacterial products that trigger innate immunity.”
Dr. Lipkin highlighted a “really intriguing” paper in which exogenous administration of interleukin 37 (IL-37), a naturally occurring inhibitor of inflammation, reversed the decrease in exercise performance observed during inflammation-induced fatigue and increased exercise performance, both in mice.
“Although we do not fully understand the pathophysiology of ME/CFS, it is not premature to consider randomized clinical trials of pro- and pre-biotics that address dysbiosis as well as drugs that modify innate immune responses such as poly (I:C) and IL-37,” Dr. Lipkin said.
Alleviating Endoplasmic Reticulum (ER) Stress: A Strategy to Increase Energy?
Paul M. Hwang, MD, PhD, from the Cardiovascular Branch of the National Heart, Lung, and Blood Institute, Bethesda, Maryland, described work that he and his colleagues recently published around a case of a 38-year-old woman with Li-Fraumeni syndrome, a genetic early-onset cancer, who also had extensive fatigue, exercise intolerance, and post-exertional malaise that began after she contracted mononucleosis as a teenager.
Testing revealed that her cells had increased expression of Wiskott-Aldrich Syndrome Protein Family Member 3 (WASF3), a “top candidate” gene found to be associated with ME/CFS in a bioinformatics study published more than a decade ago. Moreover, immunoblotting of deidentified skeletal muscle biopsy samples obtained from patients with postinfectious ME/CFS also revealed significantly increased WASF3 levels.
Hwang and colleagues showed in mice that ER stress–induced WASF3 protein localizes to mitochondria and disrupts respiratory supercomplex assembly, leading to decreased oxygen consumption and exercise endurance.
However, use of the investigational protein phosphatase 1 inhibitor salubrinal in the female patient’s cells inhibited the ER stress, which in turn decreased WASF3 expression and improved mitochondrial supercomplex formation and respiration, “suggesting a treatment strategy in ME/CFS,” Dr. Hwang said.
Neurovascular Dysregulation During Exercise: A Role for Pyridostigmine?
David M. Systrom, MD, a pulmonary and critical care medicine specialist at the Brigham and Women’s Hospital, Boston, Massachusetts, gave an update of his work investigating neurovascular dysregulation during exercise in both ME/CFS and long COVID using invasive cardiopulmonary testing.
In a 2021 publication, Dr. Systrom and his colleagues identified the mechanism of “preload failure,” or lower filling pressures of blood in the heart chambers because of insufficient vein constriction and reduced return of blood to the right side of the heart in people with ME/CFS, compared with healthy controls.
Subsequently, in a randomized trial of 45 patients with ME/CFS, Systrom and his colleagues published in November 2022, use of the cholinesterase inhibitor pyridostigmine, currently approved for treating myasthenia gravis and related conditions, improved peak Vo2 by increasing cardiac output and filling pressures.
Now, Dr. Systrom’s team is conducting a randomized trial comparing 60 mg pyridostigmine with or without low-dose naltrexone (LDN) vs placebo in 160 patients with ME/CFS for 3 months. Metabolomic, transcriptomic, proteomic, and other assessments will be conducted on urine and blood samples. Participants will also wear devices that measure steps, sleep, heart rate, and other metrics.
Komaroff cautioned that pyridostigmine, too, has potential adverse effects. “I’m not sure pyridostigmine is ready for prime time ... It’s a drug developed for a very different purpose ... Now will it hold up in a larger trial, and will there be any side effects that turn up in larger studies? It’s not unreasonable to study.”
Brain Inflammation: Measuring and Treating It
Hannah F. Bues, clinical research coordinator at Massachusetts General Hospital, Boston, presented data now in preprint (ie, not yet peer-reviewed) in which researchers used [11C]PBR28 PET neuroimaging, a marker of neuroinflammation, to compare 12 individuals with long COVID vs 43 healthy controls. They found significantly increased neuroinflammation in several different brain regions in the long COVID group compared with controls.
Samples of peripheral blood plasma also showed significant correlations between neuroinflammation and circulating analytes related to vascular dysfunction. This work is ongoing in both long COVID and pre-COVID ME/CFS populations, Bues said.
Jarred Younger, PhD, of the Neuroinflammation, Pain, and Fatigue Laboratory at the University of Alabama, Birmingham, also gave an update of his ongoing work demonstrating significant brain inflammation seen in neuroimaging of people with ME/CFS compared with healthy controls.
Dr. Younger has been investigating the use of LDN for pain in fibromyalgia. Anecdotally, there have been reports of fatigue reduction with LDN in ME/CFS.
Dr. Younger conducted a post hoc analysis of his previous trial of LDN for 12 weeks in 30 patients with fibromyalgia. Of those, 16 met older CFS criteria. There was a significant reduction in their fatigue severity, with P <.0001 from baseline and P < .009 compared with placebo. The P values were high because the data included daily symptom reports. The average fatigue reduction was 25%.
“It wasn’t a study designed for ME/CFS, but I think it’s compelling evidence and enough with the other types of data we have to say we need to do a proper clinical trial of low-dose naltrexone in ME/CFS now,” Dr. Younger said.
‘We Need to Do Something’ About the Underfunding
Another NIH-funded ME/CFS researcher, Maureen Hanson, PhD, of Cornell University, Ithaca, NY, noted that the NIH currently funds ME/CFS research at about $13 million compared with $1.15 billion for the Researching COVID to Enhance Recovery Initiative granted to NIH by Congress for “post-acute sequelae of SARS-CoV-2 (PASC)” in 2021 “because of the urgency of studying this. Most of us here are well aware of the underfunding of ME/CFS relative to the burden of illness,” she said.
Current 2024 funding for AIDS research is $3294 million. “There are 1.2 million individuals living with HIV in the United States, and there are over 3 million who are barely living with ME/CFS in the United States. We need to do something about this ... It’s certainly possible that future funding for PASC is now going to disappear,” Dr. Hanson cautioned.
Wilder, the patient advocate, reminded the audience that “There is a cohort of people with ME who got sick in the 1980s and 1990s in the prime of their life ... They have dreamed of a day when there would be a major announcement that a treatment has been discovered to take away the suffering of this disease ... They keep waiting and waiting, year after year, missing more and more of their lives with each passing day ... We’re all depending on you.”
Dr. Systrom has received funding from the Solve ME/CFS Initiative, Department of Defense, and Open Medicine Foundation. Dr. Younger’s work is funded by the NIH, Department of Defense, SolveME, the American Fibromyalgia Association, and ME Research UK. Dr. Lipkin and Dr. Hanson receive NIH funding. Dr. Komaroff has no disclosures.
A version of this article appeared on Medscape.com.
BETHESDA, MD — New research into the mechanisms underlying myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID is aimed at identifying potential approaches to treatment of the two overlapping illnesses.
According to a new data brief from the National Center for Health Statistics, in 2021-2022, 1.3% of US adults had ME/CFS, a complex, multisystem illness characterized by activity-limiting fatigue, worsening of symptoms after exertion, unrefreshing sleep, and other symptoms.
A 2-day conference, Advancing ME/CFS Research: Identifying Targets for Potential Intervention and Learning from Long COVID, was held in December 12-13 on the main campus of the US National Institutes of Health (NIH) and was livestreamed. The last such meeting, also featuring results from NIH-funded research, was held in April 2019.
“Things have changed since 2019 ... The idea of this meeting is to try and identify pathways that will be treatable and druggable and really make an impact for patients based on the things that we’ve learned over the last number of years and including, fortunately or unfortunately, the huge number of people who are suffering from long COVID, where the symptoms overlap so much with those who have been suffering for a long time with ME/CFS,” said Conference Chair Joe Breen, PhD, of the National Institute of Allergy and Infectious Diseases.
As in 2019, the meeting was preceded by a day of research presentations from young investigators, some of whom also presented their findings at the main meeting. New this year were four “lived experience” speakers who described their physical, emotional, and financial struggles with ME/CFS or long COVID. Two of them presented virtually because they were too ill to travel.
Social worker and patient advocate Terri Wilder of Minneapolis, Minnesota, reported some feedback she received on social media after she asked people with ME/CFS about their priorities for the research and clinical communities.
Among the top responses were the need to recognize and study the phenomenon of “post-exertional malaise” and to stop recommending exercise for people with these illnesses, to accelerate research to find effective treatments, and to put an end to stigma around the condition. “People don’t believe us when we tell them we’re sick, people make fun of us, misperceptions persist,” Wilder said.
One person commented, “[Clinicians] shouldn’t be afraid to try off-label meds with us if needed. There may be some secondary effects, but they are better options than us taking our own lives because we can’t stand the suffering.”
Research areas covered at the conference included immunology, virology, metabolism, gene regulation, and neurology of both ME/CFS and long COVID, as well as the latest findings regarding the overlap between the two conditions.
Oxidative Stress in Both ME/CFS and Long COVID: A Role for Metformin?
Mark M. Davis, PhD, professor and director of the Institute for Immunity, Transplantation, and Infection at Stanford University, Palo Alto, California, summarized published data suggesting that oxidative stress is a shared characteristic of both ME/CFS and long COVID. Most cellular reactive oxygen species (ROS) are produced in the cell’s mitochondria, and T-cell activation is ROS-dependent.
Women in particular with ME/CFS show high ROS levels with consistent T-cell hyperproliferation, “which can be suppressed with specific drugs such as metformin. This raises the prospect of optimizing drug treatment and drug discovery with a simple in vitro assay of the effects on a patient’s lymphocytes,” Dr. Davis said. He also cited a study suggesting that metformin may help prevent long COVID.
Asked to comment on that, longtime ME/CFS researcher Anthony L. Komaroff, MD, of Harvard University, Cambridge, Massachusetts, cautioned that although metformin is used safely by millions of people with type 2 diabetes worldwide, it’s possible that some people with ME/CFS may be more likely to experience its known adverse effects such as lactic acidosis.
To repurpose metformin or any other already-marketed drugs for ME/CFS and/or long COVID, Dr. Komaroff said, “We should entertain treatment trials.” However, as he and many others lamented at the conference, funding for off-patent drugs often isn’t forthcoming.
Addressing the Microbiome, Innate Immunity
W. Ian Lipkin, MD, of Columbia University, New York, NY, was one of two speakers who discussed the role of disruptions in the microbiome and innate immunity in ME/CFS. He presented data suggesting that “dysregulation of the gut microbiome in ME/CFS may interfere with butyrate production, resulting in inflammation and porosity to bacteria and bacterial products that trigger innate immunity.”
Dr. Lipkin highlighted a “really intriguing” paper in which exogenous administration of interleukin 37 (IL-37), a naturally occurring inhibitor of inflammation, reversed the decrease in exercise performance observed during inflammation-induced fatigue and increased exercise performance, both in mice.
“Although we do not fully understand the pathophysiology of ME/CFS, it is not premature to consider randomized clinical trials of pro- and pre-biotics that address dysbiosis as well as drugs that modify innate immune responses such as poly (I:C) and IL-37,” Dr. Lipkin said.
Alleviating Endoplasmic Reticulum (ER) Stress: A Strategy to Increase Energy?
Paul M. Hwang, MD, PhD, from the Cardiovascular Branch of the National Heart, Lung, and Blood Institute, Bethesda, Maryland, described work that he and his colleagues recently published around a case of a 38-year-old woman with Li-Fraumeni syndrome, a genetic early-onset cancer, who also had extensive fatigue, exercise intolerance, and post-exertional malaise that began after she contracted mononucleosis as a teenager.
Testing revealed that her cells had increased expression of Wiskott-Aldrich Syndrome Protein Family Member 3 (WASF3), a “top candidate” gene found to be associated with ME/CFS in a bioinformatics study published more than a decade ago. Moreover, immunoblotting of deidentified skeletal muscle biopsy samples obtained from patients with postinfectious ME/CFS also revealed significantly increased WASF3 levels.
Hwang and colleagues showed in mice that ER stress–induced WASF3 protein localizes to mitochondria and disrupts respiratory supercomplex assembly, leading to decreased oxygen consumption and exercise endurance.
However, use of the investigational protein phosphatase 1 inhibitor salubrinal in the female patient’s cells inhibited the ER stress, which in turn decreased WASF3 expression and improved mitochondrial supercomplex formation and respiration, “suggesting a treatment strategy in ME/CFS,” Dr. Hwang said.
Neurovascular Dysregulation During Exercise: A Role for Pyridostigmine?
David M. Systrom, MD, a pulmonary and critical care medicine specialist at the Brigham and Women’s Hospital, Boston, Massachusetts, gave an update of his work investigating neurovascular dysregulation during exercise in both ME/CFS and long COVID using invasive cardiopulmonary testing.
In a 2021 publication, Dr. Systrom and his colleagues identified the mechanism of “preload failure,” or lower filling pressures of blood in the heart chambers because of insufficient vein constriction and reduced return of blood to the right side of the heart in people with ME/CFS, compared with healthy controls.
Subsequently, in a randomized trial of 45 patients with ME/CFS, Systrom and his colleagues published in November 2022, use of the cholinesterase inhibitor pyridostigmine, currently approved for treating myasthenia gravis and related conditions, improved peak Vo2 by increasing cardiac output and filling pressures.
Now, Dr. Systrom’s team is conducting a randomized trial comparing 60 mg pyridostigmine with or without low-dose naltrexone (LDN) vs placebo in 160 patients with ME/CFS for 3 months. Metabolomic, transcriptomic, proteomic, and other assessments will be conducted on urine and blood samples. Participants will also wear devices that measure steps, sleep, heart rate, and other metrics.
Komaroff cautioned that pyridostigmine, too, has potential adverse effects. “I’m not sure pyridostigmine is ready for prime time ... It’s a drug developed for a very different purpose ... Now will it hold up in a larger trial, and will there be any side effects that turn up in larger studies? It’s not unreasonable to study.”
Brain Inflammation: Measuring and Treating It
Hannah F. Bues, clinical research coordinator at Massachusetts General Hospital, Boston, presented data now in preprint (ie, not yet peer-reviewed) in which researchers used [11C]PBR28 PET neuroimaging, a marker of neuroinflammation, to compare 12 individuals with long COVID vs 43 healthy controls. They found significantly increased neuroinflammation in several different brain regions in the long COVID group compared with controls.
Samples of peripheral blood plasma also showed significant correlations between neuroinflammation and circulating analytes related to vascular dysfunction. This work is ongoing in both long COVID and pre-COVID ME/CFS populations, Bues said.
Jarred Younger, PhD, of the Neuroinflammation, Pain, and Fatigue Laboratory at the University of Alabama, Birmingham, also gave an update of his ongoing work demonstrating significant brain inflammation seen in neuroimaging of people with ME/CFS compared with healthy controls.
Dr. Younger has been investigating the use of LDN for pain in fibromyalgia. Anecdotally, there have been reports of fatigue reduction with LDN in ME/CFS.
Dr. Younger conducted a post hoc analysis of his previous trial of LDN for 12 weeks in 30 patients with fibromyalgia. Of those, 16 met older CFS criteria. There was a significant reduction in their fatigue severity, with P <.0001 from baseline and P < .009 compared with placebo. The P values were high because the data included daily symptom reports. The average fatigue reduction was 25%.
“It wasn’t a study designed for ME/CFS, but I think it’s compelling evidence and enough with the other types of data we have to say we need to do a proper clinical trial of low-dose naltrexone in ME/CFS now,” Dr. Younger said.
‘We Need to Do Something’ About the Underfunding
Another NIH-funded ME/CFS researcher, Maureen Hanson, PhD, of Cornell University, Ithaca, NY, noted that the NIH currently funds ME/CFS research at about $13 million compared with $1.15 billion for the Researching COVID to Enhance Recovery Initiative granted to NIH by Congress for “post-acute sequelae of SARS-CoV-2 (PASC)” in 2021 “because of the urgency of studying this. Most of us here are well aware of the underfunding of ME/CFS relative to the burden of illness,” she said.
Current 2024 funding for AIDS research is $3294 million. “There are 1.2 million individuals living with HIV in the United States, and there are over 3 million who are barely living with ME/CFS in the United States. We need to do something about this ... It’s certainly possible that future funding for PASC is now going to disappear,” Dr. Hanson cautioned.
Wilder, the patient advocate, reminded the audience that “There is a cohort of people with ME who got sick in the 1980s and 1990s in the prime of their life ... They have dreamed of a day when there would be a major announcement that a treatment has been discovered to take away the suffering of this disease ... They keep waiting and waiting, year after year, missing more and more of their lives with each passing day ... We’re all depending on you.”
Dr. Systrom has received funding from the Solve ME/CFS Initiative, Department of Defense, and Open Medicine Foundation. Dr. Younger’s work is funded by the NIH, Department of Defense, SolveME, the American Fibromyalgia Association, and ME Research UK. Dr. Lipkin and Dr. Hanson receive NIH funding. Dr. Komaroff has no disclosures.
A version of this article appeared on Medscape.com.
BETHESDA, MD — New research into the mechanisms underlying myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long COVID is aimed at identifying potential approaches to treatment of the two overlapping illnesses.
According to a new data brief from the National Center for Health Statistics, in 2021-2022, 1.3% of US adults had ME/CFS, a complex, multisystem illness characterized by activity-limiting fatigue, worsening of symptoms after exertion, unrefreshing sleep, and other symptoms.
A 2-day conference, Advancing ME/CFS Research: Identifying Targets for Potential Intervention and Learning from Long COVID, was held in December 12-13 on the main campus of the US National Institutes of Health (NIH) and was livestreamed. The last such meeting, also featuring results from NIH-funded research, was held in April 2019.
“Things have changed since 2019 ... The idea of this meeting is to try and identify pathways that will be treatable and druggable and really make an impact for patients based on the things that we’ve learned over the last number of years and including, fortunately or unfortunately, the huge number of people who are suffering from long COVID, where the symptoms overlap so much with those who have been suffering for a long time with ME/CFS,” said Conference Chair Joe Breen, PhD, of the National Institute of Allergy and Infectious Diseases.
As in 2019, the meeting was preceded by a day of research presentations from young investigators, some of whom also presented their findings at the main meeting. New this year were four “lived experience” speakers who described their physical, emotional, and financial struggles with ME/CFS or long COVID. Two of them presented virtually because they were too ill to travel.
Social worker and patient advocate Terri Wilder of Minneapolis, Minnesota, reported some feedback she received on social media after she asked people with ME/CFS about their priorities for the research and clinical communities.
Among the top responses were the need to recognize and study the phenomenon of “post-exertional malaise” and to stop recommending exercise for people with these illnesses, to accelerate research to find effective treatments, and to put an end to stigma around the condition. “People don’t believe us when we tell them we’re sick, people make fun of us, misperceptions persist,” Wilder said.
One person commented, “[Clinicians] shouldn’t be afraid to try off-label meds with us if needed. There may be some secondary effects, but they are better options than us taking our own lives because we can’t stand the suffering.”
Research areas covered at the conference included immunology, virology, metabolism, gene regulation, and neurology of both ME/CFS and long COVID, as well as the latest findings regarding the overlap between the two conditions.
Oxidative Stress in Both ME/CFS and Long COVID: A Role for Metformin?
Mark M. Davis, PhD, professor and director of the Institute for Immunity, Transplantation, and Infection at Stanford University, Palo Alto, California, summarized published data suggesting that oxidative stress is a shared characteristic of both ME/CFS and long COVID. Most cellular reactive oxygen species (ROS) are produced in the cell’s mitochondria, and T-cell activation is ROS-dependent.
Women in particular with ME/CFS show high ROS levels with consistent T-cell hyperproliferation, “which can be suppressed with specific drugs such as metformin. This raises the prospect of optimizing drug treatment and drug discovery with a simple in vitro assay of the effects on a patient’s lymphocytes,” Dr. Davis said. He also cited a study suggesting that metformin may help prevent long COVID.
Asked to comment on that, longtime ME/CFS researcher Anthony L. Komaroff, MD, of Harvard University, Cambridge, Massachusetts, cautioned that although metformin is used safely by millions of people with type 2 diabetes worldwide, it’s possible that some people with ME/CFS may be more likely to experience its known adverse effects such as lactic acidosis.
To repurpose metformin or any other already-marketed drugs for ME/CFS and/or long COVID, Dr. Komaroff said, “We should entertain treatment trials.” However, as he and many others lamented at the conference, funding for off-patent drugs often isn’t forthcoming.
Addressing the Microbiome, Innate Immunity
W. Ian Lipkin, MD, of Columbia University, New York, NY, was one of two speakers who discussed the role of disruptions in the microbiome and innate immunity in ME/CFS. He presented data suggesting that “dysregulation of the gut microbiome in ME/CFS may interfere with butyrate production, resulting in inflammation and porosity to bacteria and bacterial products that trigger innate immunity.”
Dr. Lipkin highlighted a “really intriguing” paper in which exogenous administration of interleukin 37 (IL-37), a naturally occurring inhibitor of inflammation, reversed the decrease in exercise performance observed during inflammation-induced fatigue and increased exercise performance, both in mice.
“Although we do not fully understand the pathophysiology of ME/CFS, it is not premature to consider randomized clinical trials of pro- and pre-biotics that address dysbiosis as well as drugs that modify innate immune responses such as poly (I:C) and IL-37,” Dr. Lipkin said.
Alleviating Endoplasmic Reticulum (ER) Stress: A Strategy to Increase Energy?
Paul M. Hwang, MD, PhD, from the Cardiovascular Branch of the National Heart, Lung, and Blood Institute, Bethesda, Maryland, described work that he and his colleagues recently published around a case of a 38-year-old woman with Li-Fraumeni syndrome, a genetic early-onset cancer, who also had extensive fatigue, exercise intolerance, and post-exertional malaise that began after she contracted mononucleosis as a teenager.
Testing revealed that her cells had increased expression of Wiskott-Aldrich Syndrome Protein Family Member 3 (WASF3), a “top candidate” gene found to be associated with ME/CFS in a bioinformatics study published more than a decade ago. Moreover, immunoblotting of deidentified skeletal muscle biopsy samples obtained from patients with postinfectious ME/CFS also revealed significantly increased WASF3 levels.
Hwang and colleagues showed in mice that ER stress–induced WASF3 protein localizes to mitochondria and disrupts respiratory supercomplex assembly, leading to decreased oxygen consumption and exercise endurance.
However, use of the investigational protein phosphatase 1 inhibitor salubrinal in the female patient’s cells inhibited the ER stress, which in turn decreased WASF3 expression and improved mitochondrial supercomplex formation and respiration, “suggesting a treatment strategy in ME/CFS,” Dr. Hwang said.
Neurovascular Dysregulation During Exercise: A Role for Pyridostigmine?
David M. Systrom, MD, a pulmonary and critical care medicine specialist at the Brigham and Women’s Hospital, Boston, Massachusetts, gave an update of his work investigating neurovascular dysregulation during exercise in both ME/CFS and long COVID using invasive cardiopulmonary testing.
In a 2021 publication, Dr. Systrom and his colleagues identified the mechanism of “preload failure,” or lower filling pressures of blood in the heart chambers because of insufficient vein constriction and reduced return of blood to the right side of the heart in people with ME/CFS, compared with healthy controls.
Subsequently, in a randomized trial of 45 patients with ME/CFS, Systrom and his colleagues published in November 2022, use of the cholinesterase inhibitor pyridostigmine, currently approved for treating myasthenia gravis and related conditions, improved peak Vo2 by increasing cardiac output and filling pressures.
Now, Dr. Systrom’s team is conducting a randomized trial comparing 60 mg pyridostigmine with or without low-dose naltrexone (LDN) vs placebo in 160 patients with ME/CFS for 3 months. Metabolomic, transcriptomic, proteomic, and other assessments will be conducted on urine and blood samples. Participants will also wear devices that measure steps, sleep, heart rate, and other metrics.
Komaroff cautioned that pyridostigmine, too, has potential adverse effects. “I’m not sure pyridostigmine is ready for prime time ... It’s a drug developed for a very different purpose ... Now will it hold up in a larger trial, and will there be any side effects that turn up in larger studies? It’s not unreasonable to study.”
Brain Inflammation: Measuring and Treating It
Hannah F. Bues, clinical research coordinator at Massachusetts General Hospital, Boston, presented data now in preprint (ie, not yet peer-reviewed) in which researchers used [11C]PBR28 PET neuroimaging, a marker of neuroinflammation, to compare 12 individuals with long COVID vs 43 healthy controls. They found significantly increased neuroinflammation in several different brain regions in the long COVID group compared with controls.
Samples of peripheral blood plasma also showed significant correlations between neuroinflammation and circulating analytes related to vascular dysfunction. This work is ongoing in both long COVID and pre-COVID ME/CFS populations, Bues said.
Jarred Younger, PhD, of the Neuroinflammation, Pain, and Fatigue Laboratory at the University of Alabama, Birmingham, also gave an update of his ongoing work demonstrating significant brain inflammation seen in neuroimaging of people with ME/CFS compared with healthy controls.
Dr. Younger has been investigating the use of LDN for pain in fibromyalgia. Anecdotally, there have been reports of fatigue reduction with LDN in ME/CFS.
Dr. Younger conducted a post hoc analysis of his previous trial of LDN for 12 weeks in 30 patients with fibromyalgia. Of those, 16 met older CFS criteria. There was a significant reduction in their fatigue severity, with P <.0001 from baseline and P < .009 compared with placebo. The P values were high because the data included daily symptom reports. The average fatigue reduction was 25%.
“It wasn’t a study designed for ME/CFS, but I think it’s compelling evidence and enough with the other types of data we have to say we need to do a proper clinical trial of low-dose naltrexone in ME/CFS now,” Dr. Younger said.
‘We Need to Do Something’ About the Underfunding
Another NIH-funded ME/CFS researcher, Maureen Hanson, PhD, of Cornell University, Ithaca, NY, noted that the NIH currently funds ME/CFS research at about $13 million compared with $1.15 billion for the Researching COVID to Enhance Recovery Initiative granted to NIH by Congress for “post-acute sequelae of SARS-CoV-2 (PASC)” in 2021 “because of the urgency of studying this. Most of us here are well aware of the underfunding of ME/CFS relative to the burden of illness,” she said.
Current 2024 funding for AIDS research is $3294 million. “There are 1.2 million individuals living with HIV in the United States, and there are over 3 million who are barely living with ME/CFS in the United States. We need to do something about this ... It’s certainly possible that future funding for PASC is now going to disappear,” Dr. Hanson cautioned.
Wilder, the patient advocate, reminded the audience that “There is a cohort of people with ME who got sick in the 1980s and 1990s in the prime of their life ... They have dreamed of a day when there would be a major announcement that a treatment has been discovered to take away the suffering of this disease ... They keep waiting and waiting, year after year, missing more and more of their lives with each passing day ... We’re all depending on you.”
Dr. Systrom has received funding from the Solve ME/CFS Initiative, Department of Defense, and Open Medicine Foundation. Dr. Younger’s work is funded by the NIH, Department of Defense, SolveME, the American Fibromyalgia Association, and ME Research UK. Dr. Lipkin and Dr. Hanson receive NIH funding. Dr. Komaroff has no disclosures.
A version of this article appeared on Medscape.com.
FROM AN NIH RESEARCH CONFERENCE



