User login
Reports increasingly suggest anosmia/hyposmia can signal early COVID-19 infection
Unexplained anosmia, hyposmia, and dysgeusia should be added to the list of possible COVID-19 symptoms for screening purposes, and individuals with such symptoms should consider self-isolation, the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) has proposed.
However, a World Health Organization expert said during a March 23 daily briefing on the novel coronavirus pandemic that the jury is still out on that.
The AAO-HNS proposal is based on “rapidly accumulating” anecdotal evidence that such symptoms – in the absence of other symptoms suggestive of COVID-19 – have sometimes preceded a COVID-19 diagnosis.
“ ... anosmia, hyposmia, and dysgeusia in the absence of other respiratory disease such as allergic rhinitis, acute rhinosinusitis, or chronic rhinosinusitis should alert physicians to the possibility of COVID-19 infection and warrant serious consideration for self-isolation and testing of these individuals,” the AAO-HNS said in a statement on the proposal.
ENT UK, an organization representing Ear, Nose, and Throat surgery and its related specialties in the UK, also is emphasizing the potential importance of these symptoms. In a March 21 letter, ENT UK experts cited “good evidence from South Korea, China and Italy that significant numbers of patients with proven COVID-19 infection have developed anosmia/hyposmia.”
Claire Hopkins, BMBCh, president of the British Rhinological Society and a professor of Rhinology at King’s College London, along with ENT UK president Nirmal Kumar, also noted in the letter that two of every three cases in Germany, and 30% of patients testing positive in South Korea, had anosmia as their first symptom.
“While there is a chance the apparent increase in incidence could merely reflect the attention COVID-19 has attracted in the media, and that such cases may be caused by typical rhinovirus and coronavirus strains, it could potentially be used as a screening tool to help identify otherwise asymptomatic patients, who could then be better instructed on self-isolation,” they wrote.
Maria Van Kerkhove, MD, technical lead of the WHO Medical Emergencies Program, acknowledged the anecdotal evidence during the WHO briefing.
“Yes, we’ve seen quite a few reports ... but this is something that we need to look into to really capture if this is one of the early signs and symptoms of COVID-19,” she said, noting that WHO is working with more than a dozen countries that are systematically collecting data using molecular and serological testing to “capture more robustly” the early signs and symptoms, and is “reaching out to a number of countries and looking at the cases that have already been reported to see if [anosmia] is a common feature.”
“We don’t have the answer to that,” she said, adding that, in addition to the major symptoms – including dry cough, fever, and shortness of breath – that are well known at this point, “there are likely to be many signs and symptoms that people have.”
“A loss of smell or a loss of taste is something that we’re looking into, and we’re looking forward to the results of these early investigations ... so that we have a more evidence-based approach and we can add that to the list.”
Unexplained anosmia, hyposmia, and dysgeusia should be added to the list of possible COVID-19 symptoms for screening purposes, and individuals with such symptoms should consider self-isolation, the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) has proposed.
However, a World Health Organization expert said during a March 23 daily briefing on the novel coronavirus pandemic that the jury is still out on that.
The AAO-HNS proposal is based on “rapidly accumulating” anecdotal evidence that such symptoms – in the absence of other symptoms suggestive of COVID-19 – have sometimes preceded a COVID-19 diagnosis.
“ ... anosmia, hyposmia, and dysgeusia in the absence of other respiratory disease such as allergic rhinitis, acute rhinosinusitis, or chronic rhinosinusitis should alert physicians to the possibility of COVID-19 infection and warrant serious consideration for self-isolation and testing of these individuals,” the AAO-HNS said in a statement on the proposal.
ENT UK, an organization representing Ear, Nose, and Throat surgery and its related specialties in the UK, also is emphasizing the potential importance of these symptoms. In a March 21 letter, ENT UK experts cited “good evidence from South Korea, China and Italy that significant numbers of patients with proven COVID-19 infection have developed anosmia/hyposmia.”
Claire Hopkins, BMBCh, president of the British Rhinological Society and a professor of Rhinology at King’s College London, along with ENT UK president Nirmal Kumar, also noted in the letter that two of every three cases in Germany, and 30% of patients testing positive in South Korea, had anosmia as their first symptom.
“While there is a chance the apparent increase in incidence could merely reflect the attention COVID-19 has attracted in the media, and that such cases may be caused by typical rhinovirus and coronavirus strains, it could potentially be used as a screening tool to help identify otherwise asymptomatic patients, who could then be better instructed on self-isolation,” they wrote.
Maria Van Kerkhove, MD, technical lead of the WHO Medical Emergencies Program, acknowledged the anecdotal evidence during the WHO briefing.
“Yes, we’ve seen quite a few reports ... but this is something that we need to look into to really capture if this is one of the early signs and symptoms of COVID-19,” she said, noting that WHO is working with more than a dozen countries that are systematically collecting data using molecular and serological testing to “capture more robustly” the early signs and symptoms, and is “reaching out to a number of countries and looking at the cases that have already been reported to see if [anosmia] is a common feature.”
“We don’t have the answer to that,” she said, adding that, in addition to the major symptoms – including dry cough, fever, and shortness of breath – that are well known at this point, “there are likely to be many signs and symptoms that people have.”
“A loss of smell or a loss of taste is something that we’re looking into, and we’re looking forward to the results of these early investigations ... so that we have a more evidence-based approach and we can add that to the list.”
Unexplained anosmia, hyposmia, and dysgeusia should be added to the list of possible COVID-19 symptoms for screening purposes, and individuals with such symptoms should consider self-isolation, the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) has proposed.
However, a World Health Organization expert said during a March 23 daily briefing on the novel coronavirus pandemic that the jury is still out on that.
The AAO-HNS proposal is based on “rapidly accumulating” anecdotal evidence that such symptoms – in the absence of other symptoms suggestive of COVID-19 – have sometimes preceded a COVID-19 diagnosis.
“ ... anosmia, hyposmia, and dysgeusia in the absence of other respiratory disease such as allergic rhinitis, acute rhinosinusitis, or chronic rhinosinusitis should alert physicians to the possibility of COVID-19 infection and warrant serious consideration for self-isolation and testing of these individuals,” the AAO-HNS said in a statement on the proposal.
ENT UK, an organization representing Ear, Nose, and Throat surgery and its related specialties in the UK, also is emphasizing the potential importance of these symptoms. In a March 21 letter, ENT UK experts cited “good evidence from South Korea, China and Italy that significant numbers of patients with proven COVID-19 infection have developed anosmia/hyposmia.”
Claire Hopkins, BMBCh, president of the British Rhinological Society and a professor of Rhinology at King’s College London, along with ENT UK president Nirmal Kumar, also noted in the letter that two of every three cases in Germany, and 30% of patients testing positive in South Korea, had anosmia as their first symptom.
“While there is a chance the apparent increase in incidence could merely reflect the attention COVID-19 has attracted in the media, and that such cases may be caused by typical rhinovirus and coronavirus strains, it could potentially be used as a screening tool to help identify otherwise asymptomatic patients, who could then be better instructed on self-isolation,” they wrote.
Maria Van Kerkhove, MD, technical lead of the WHO Medical Emergencies Program, acknowledged the anecdotal evidence during the WHO briefing.
“Yes, we’ve seen quite a few reports ... but this is something that we need to look into to really capture if this is one of the early signs and symptoms of COVID-19,” she said, noting that WHO is working with more than a dozen countries that are systematically collecting data using molecular and serological testing to “capture more robustly” the early signs and symptoms, and is “reaching out to a number of countries and looking at the cases that have already been reported to see if [anosmia] is a common feature.”
“We don’t have the answer to that,” she said, adding that, in addition to the major symptoms – including dry cough, fever, and shortness of breath – that are well known at this point, “there are likely to be many signs and symptoms that people have.”
“A loss of smell or a loss of taste is something that we’re looking into, and we’re looking forward to the results of these early investigations ... so that we have a more evidence-based approach and we can add that to the list.”
High rate of asymptomatic COVID-19 seen in cruise ship passengers
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
The high rate of asymptomatic COVID-19 infections aboard the cruise ship Diamond Princess “could partially explain the high attack rate among” the passengers and crew, according to the Centers for Disease Control and Prevention.

Testing of the 3,711 passengers and crew aboard the ship – the source of the largest outbreak outside of China during the initial stages of the pandemic – revealed that 19.2% were positive for COVID-19, Leah F. Moriarty, MPH, and associates reported in the Morbidity and Mortality Weekly Report.
At the time of testing, 46.5% (331) of the 712 infected individuals were asymptomatic, and “statistical models of the Diamond Princess outbreak suggest that 17.9% of infected persons never developed symptoms,” wrote Ms. Moriarty of the CDC COVID-19 response team, and associates.
RNA from the SARS-CoV-2 virus was found on surfaces in cabins up to 17 days after they had been vacated by passengers but before the cabins had been disinfected, the investigators noted.
The Diamond Princess departed from Yokohama, Japan, on Jan. 20, 2020, and returned on Feb. 3 after making six stops in three countries. The ship was quarantined upon its return because a symptomatic passenger who had departed Jan. 25 in Hong Kong tested positive for SARS-CoV-2, Ms. Moriarty and associates explained.
Of the 381 people from the ship who were symptomatic and tested positive, 37 (9.7%) needed intensive care and 9 (1.3%) died. There were 428 Americans on the ship, of whom 107 (25.0%) tested positive and 11 remained hospitalized in Japan as of March 13, they said.
“Many other cruise ships have since been implicated in SARS-CoV-2 transmission,” the investigators said, including the Grand Princess, which sailed out of San Francisco with 3,571 people on Feb. 21 and returned to Oakland on March 8.
That ship had been the site of virus transmission during its previous voyage from Feb. 11 to Feb. 21, from which more than 20 cases have been identified. During the latter trip, 21 of 45 passengers and crew tested positive before the ship docked. During the subsequent land-based quarantine, there have been 78 positive tests among the 469 people tested as of March 21, a rate of 16.6%, the research team reported.
“Public health responses to cruise ship outbreaks require extensive resources,” they wrote. “These responses required the coordination of stakeholders across multiple sectors, including U.S. government departments and agencies, foreign ministries of health, foreign embassies, state and local public health departments, hospitals, laboratories, and cruise ship companies.”
SOURCE: Moriarty LF et al. MMWR. 2020 Mar 23;69[early release]:1-6.
FROM MMWR
CDC coronavirus testing decision likely to haunt nation for months to come
As the novel coronavirus snaked its way across the globe, the Centers for Disease Control and Prevention in early February distributed 200 test kits it had produced to more than 100 public health labs run by states and counties nationwide.
Each kit contained material to test a mere 300-400 patients. And labs, whether serving the population of New York or tiny towns in rural America, apparently received the same kits.
The kits were distributed roughly equally to locales in all 50 states. That decision presaged weeks of chaos, in which the availability of COVID-19 tests seemed oddly out of sync with where testing was needed.
A woman in South Dakota with mild symptoms and no fever readily got the test and the results. Meanwhile, political leaders and public officials in places like New York, Boston, Seattle, and the San Francisco Bay area – all in the throes of serious outbreaks – couldn’t get enough tests to screen ill patients or, thereby, the information they needed to protect the general public and stem the outbreak of the virus, whose symptoms mimic those of common respiratory illnesses.
Rapid testing is crucial in the early stages of an outbreak. It allows health workers and families to identify and focus on treating those infected and isolate them.
Yet health officials in New York and such states as New York, Washington, Pennsylvania, and Georgia confirmed that they each initially got one test kit, calling into question whether they would have even stood a chance to contain the outbreaks that would emerge. They would soon discover that the tests they did receive were flawed, lacking critical components, and delivering faulty results.
During those early weeks, the virus took off, infecting thousands of people and leading to nationwide social distancing and sheltering in place. Public health officials are just beginning to grapple with the fallout from that early bungling of testing, which is likely to haunt the country in the months to come.
Too little too late
The first shipment to Washington state arrived more than 2 weeks after officials there announced the first U.S. case of coronavirus, and at a moment when deadly outbreaks of the disease were already festering in places like the Life Care Center in Kirkland. Within weeks, three dozen people infected with COVID-19 would die at the nursing home in the suburbs of Seattle.
The spread of COVID-19 would not take long to overwhelm the state, which as of March 20, 2020, had more than 1,300 cases.
The Trump administration in recent days has attempted to speed testing for the virus after early missteps hampered the government’s response to contain the contagion, and officials have had to respond to a barrage of criticism from public health experts, state officials, and members of Congress.
Federal health officials have eased the process for university and commercial labs to perform their own tests, and they are ramping up their capacity. As of March 16, public and private labs in the United States had the ability to test more than 36,000 people a day, according to estimates compiled by the American Enterprise Institute, a conservative-leaning think tank in Washington, a figure expected to rapidly escalate in coming weeks. That figure, however, can vary considerably by state and does not indicate how many tests are actually given to patients.
“We are now beginning to see that they have spread out in a prioritized way. We asked them to prioritize the regions that were mostly affected,” Deborah Birx, the coronavirus response coordinator for the White House Coronavirus Task Force, said March 18 of private labs’ testing, without elaboration.
The scaling up of testing is set to take place after weeks of faltering and hundreds, if not thousands, of undiagnosed people spreading the virus. For example, New York’s state health department received a faulty CDC test kit on Feb. 8 for 800 patient specimens, an amount that’s consistent with other states, according to a spokesperson. It later began testing patients with a test that state officials developed based on the CDC protocol and has significantly increased testing – as of March 20, more than 7,200 people had tested positive statewide.
In New York City, the first batch was obtained on Feb. 7.
“The other state and local public health laboratories got test kits as they became available,” said Eric Blank, chief program officer of the Association of Public Health Laboratories.
Places in the middle of the country with no outbreaks had the luxury of time to plan. For example, Missouri officials have had about 800 tests to work with, leading to only 395 performed so far in the region by public health labs – 26 of which were positive. When private lab tests are accounted for, as of March 20 there were 47 confirmed cases.
Health care providers and public health staff in the state, however, benefited from the fact that there is less international travel to the region, according to infectious disease expert Steven Lawrence, MD, of Washington University, St. Louis.
“This is very similar to 1918 with the influenza pandemic – St. Louis had more time to prepare and was able to put measures in place to flatten the curve than, say, Philadelphia,” Dr. Lawrence said. “Seattle didn’t have an opportunity to prepare as much in advance.”
While commercial labs are coming online, strict restrictions are limiting testing capabilities, Dr. Lawrence said.
“The state has had their hands tied,” he added.
Waiting And wondering
Because of a widespread lag in testing, it is still a mystery for thousands of people to know whether they’ve come into contact with an infected person until well after it happens. As of March 20, the pandemic had killed more than 11,000 globally. More than 16,000 Americans were confirmed infected and at least 216 have died.
“CDC will distribute tests based on where they can do the most good. But without hospital-based testing and commercial testing, it will not be possible to meet the need,” said Tom Frieden, who led the CDC during President Obama’s administration and is a former commissioner of the New York City Health Department.
In California, public school teacher Claire Dugan, whose state was among the hardest hit in the initial wave of U.S. coronavirus cases, was told she didn’t qualify for testing because she had not traveled abroad to any country with an outbreak of the virus or been in contact with an infected person. Ms. Dugan, who lives in the San Francisco Bay area and is already medically fragile after a stray bullet nearly killed her while driving 4 years ago, sought a test from her doctor after registering a temperature of 100.7° F earlier this month.
“There are a lot of layers as to why this is so messed up,” said Ms. Dugan, who relies on a feeding tube and said she sought a test not only to protect herself but her students. “It’s community spreading right now, so it’s kind of silly we’re still insisting on [the early criteria for testing]. How would I know?”
Since the CDC’s initial distribution, states have been reordering more tests through the office’s International Reagent Resource – a long-standing tool that public health labs have relied on. They have also revised testing protocols to use only one sample per person, which boosts the number of people screened.
Yet problems still abound with tests or other materials needed to be able to detect the virus. California Gov. Gavin Newsom (D) said on March 12 that county public health labs can’t use all of the 8,000 test kits the state has because they are missing key components.
In Pennsylvania, state officials weren’t able to begin testing until March 2 because of problems with the CDC’s initial kit, according to Nate Wardle, a spokesperson at its department of health. New York received two newly manufactured CDC test kits on Feb. 29 and also began performing tests March 2, according to its health department.
“We are still limited on extraction kits,” Mandy Cohen, the Health & Human Services secretary in North Carolina, said in an interview in mid-March. Officials earlier this month could test only 300 patients because of shortages in the extraction materials needed to register whether the novel coronavirus is present.
In North Dakota, Loralyn Hegland wrote her physician’s practice an email on March 10 with the subject line “dry cough,” wondering if she should come in for testing after learning that was one symptom of COVID-19. The recommendation she got echoes those of countless others across the United States, saying her risk of being exposed was very low because she hadn’t traveled outside the United States and had not come into contact with a person who had been “definitely” diagnosed with the virus.
Ms. Hegland, who lives in Fargo, didn’t have a fever but decided to shelter herself, anyway, out of caution.
Would she push to get a test?
“What’s the point?” she said. “You can’t know what you don’t know. It’s just that simple. How else do you explain it to people when you’re not testing?”
KHN Midwest correspondent Lauren Weber in St. Louis contributed to this article.
Kaiser Health News is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
As the novel coronavirus snaked its way across the globe, the Centers for Disease Control and Prevention in early February distributed 200 test kits it had produced to more than 100 public health labs run by states and counties nationwide.
Each kit contained material to test a mere 300-400 patients. And labs, whether serving the population of New York or tiny towns in rural America, apparently received the same kits.
The kits were distributed roughly equally to locales in all 50 states. That decision presaged weeks of chaos, in which the availability of COVID-19 tests seemed oddly out of sync with where testing was needed.
A woman in South Dakota with mild symptoms and no fever readily got the test and the results. Meanwhile, political leaders and public officials in places like New York, Boston, Seattle, and the San Francisco Bay area – all in the throes of serious outbreaks – couldn’t get enough tests to screen ill patients or, thereby, the information they needed to protect the general public and stem the outbreak of the virus, whose symptoms mimic those of common respiratory illnesses.
Rapid testing is crucial in the early stages of an outbreak. It allows health workers and families to identify and focus on treating those infected and isolate them.
Yet health officials in New York and such states as New York, Washington, Pennsylvania, and Georgia confirmed that they each initially got one test kit, calling into question whether they would have even stood a chance to contain the outbreaks that would emerge. They would soon discover that the tests they did receive were flawed, lacking critical components, and delivering faulty results.
During those early weeks, the virus took off, infecting thousands of people and leading to nationwide social distancing and sheltering in place. Public health officials are just beginning to grapple with the fallout from that early bungling of testing, which is likely to haunt the country in the months to come.
Too little too late
The first shipment to Washington state arrived more than 2 weeks after officials there announced the first U.S. case of coronavirus, and at a moment when deadly outbreaks of the disease were already festering in places like the Life Care Center in Kirkland. Within weeks, three dozen people infected with COVID-19 would die at the nursing home in the suburbs of Seattle.
The spread of COVID-19 would not take long to overwhelm the state, which as of March 20, 2020, had more than 1,300 cases.
The Trump administration in recent days has attempted to speed testing for the virus after early missteps hampered the government’s response to contain the contagion, and officials have had to respond to a barrage of criticism from public health experts, state officials, and members of Congress.
Federal health officials have eased the process for university and commercial labs to perform their own tests, and they are ramping up their capacity. As of March 16, public and private labs in the United States had the ability to test more than 36,000 people a day, according to estimates compiled by the American Enterprise Institute, a conservative-leaning think tank in Washington, a figure expected to rapidly escalate in coming weeks. That figure, however, can vary considerably by state and does not indicate how many tests are actually given to patients.
“We are now beginning to see that they have spread out in a prioritized way. We asked them to prioritize the regions that were mostly affected,” Deborah Birx, the coronavirus response coordinator for the White House Coronavirus Task Force, said March 18 of private labs’ testing, without elaboration.
The scaling up of testing is set to take place after weeks of faltering and hundreds, if not thousands, of undiagnosed people spreading the virus. For example, New York’s state health department received a faulty CDC test kit on Feb. 8 for 800 patient specimens, an amount that’s consistent with other states, according to a spokesperson. It later began testing patients with a test that state officials developed based on the CDC protocol and has significantly increased testing – as of March 20, more than 7,200 people had tested positive statewide.
In New York City, the first batch was obtained on Feb. 7.
“The other state and local public health laboratories got test kits as they became available,” said Eric Blank, chief program officer of the Association of Public Health Laboratories.
Places in the middle of the country with no outbreaks had the luxury of time to plan. For example, Missouri officials have had about 800 tests to work with, leading to only 395 performed so far in the region by public health labs – 26 of which were positive. When private lab tests are accounted for, as of March 20 there were 47 confirmed cases.
Health care providers and public health staff in the state, however, benefited from the fact that there is less international travel to the region, according to infectious disease expert Steven Lawrence, MD, of Washington University, St. Louis.
“This is very similar to 1918 with the influenza pandemic – St. Louis had more time to prepare and was able to put measures in place to flatten the curve than, say, Philadelphia,” Dr. Lawrence said. “Seattle didn’t have an opportunity to prepare as much in advance.”
While commercial labs are coming online, strict restrictions are limiting testing capabilities, Dr. Lawrence said.
“The state has had their hands tied,” he added.
Waiting And wondering
Because of a widespread lag in testing, it is still a mystery for thousands of people to know whether they’ve come into contact with an infected person until well after it happens. As of March 20, the pandemic had killed more than 11,000 globally. More than 16,000 Americans were confirmed infected and at least 216 have died.
“CDC will distribute tests based on where they can do the most good. But without hospital-based testing and commercial testing, it will not be possible to meet the need,” said Tom Frieden, who led the CDC during President Obama’s administration and is a former commissioner of the New York City Health Department.
In California, public school teacher Claire Dugan, whose state was among the hardest hit in the initial wave of U.S. coronavirus cases, was told she didn’t qualify for testing because she had not traveled abroad to any country with an outbreak of the virus or been in contact with an infected person. Ms. Dugan, who lives in the San Francisco Bay area and is already medically fragile after a stray bullet nearly killed her while driving 4 years ago, sought a test from her doctor after registering a temperature of 100.7° F earlier this month.
“There are a lot of layers as to why this is so messed up,” said Ms. Dugan, who relies on a feeding tube and said she sought a test not only to protect herself but her students. “It’s community spreading right now, so it’s kind of silly we’re still insisting on [the early criteria for testing]. How would I know?”
Since the CDC’s initial distribution, states have been reordering more tests through the office’s International Reagent Resource – a long-standing tool that public health labs have relied on. They have also revised testing protocols to use only one sample per person, which boosts the number of people screened.
Yet problems still abound with tests or other materials needed to be able to detect the virus. California Gov. Gavin Newsom (D) said on March 12 that county public health labs can’t use all of the 8,000 test kits the state has because they are missing key components.
In Pennsylvania, state officials weren’t able to begin testing until March 2 because of problems with the CDC’s initial kit, according to Nate Wardle, a spokesperson at its department of health. New York received two newly manufactured CDC test kits on Feb. 29 and also began performing tests March 2, according to its health department.
“We are still limited on extraction kits,” Mandy Cohen, the Health & Human Services secretary in North Carolina, said in an interview in mid-March. Officials earlier this month could test only 300 patients because of shortages in the extraction materials needed to register whether the novel coronavirus is present.
In North Dakota, Loralyn Hegland wrote her physician’s practice an email on March 10 with the subject line “dry cough,” wondering if she should come in for testing after learning that was one symptom of COVID-19. The recommendation she got echoes those of countless others across the United States, saying her risk of being exposed was very low because she hadn’t traveled outside the United States and had not come into contact with a person who had been “definitely” diagnosed with the virus.
Ms. Hegland, who lives in Fargo, didn’t have a fever but decided to shelter herself, anyway, out of caution.
Would she push to get a test?
“What’s the point?” she said. “You can’t know what you don’t know. It’s just that simple. How else do you explain it to people when you’re not testing?”
KHN Midwest correspondent Lauren Weber in St. Louis contributed to this article.
Kaiser Health News is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
As the novel coronavirus snaked its way across the globe, the Centers for Disease Control and Prevention in early February distributed 200 test kits it had produced to more than 100 public health labs run by states and counties nationwide.
Each kit contained material to test a mere 300-400 patients. And labs, whether serving the population of New York or tiny towns in rural America, apparently received the same kits.
The kits were distributed roughly equally to locales in all 50 states. That decision presaged weeks of chaos, in which the availability of COVID-19 tests seemed oddly out of sync with where testing was needed.
A woman in South Dakota with mild symptoms and no fever readily got the test and the results. Meanwhile, political leaders and public officials in places like New York, Boston, Seattle, and the San Francisco Bay area – all in the throes of serious outbreaks – couldn’t get enough tests to screen ill patients or, thereby, the information they needed to protect the general public and stem the outbreak of the virus, whose symptoms mimic those of common respiratory illnesses.
Rapid testing is crucial in the early stages of an outbreak. It allows health workers and families to identify and focus on treating those infected and isolate them.
Yet health officials in New York and such states as New York, Washington, Pennsylvania, and Georgia confirmed that they each initially got one test kit, calling into question whether they would have even stood a chance to contain the outbreaks that would emerge. They would soon discover that the tests they did receive were flawed, lacking critical components, and delivering faulty results.
During those early weeks, the virus took off, infecting thousands of people and leading to nationwide social distancing and sheltering in place. Public health officials are just beginning to grapple with the fallout from that early bungling of testing, which is likely to haunt the country in the months to come.
Too little too late
The first shipment to Washington state arrived more than 2 weeks after officials there announced the first U.S. case of coronavirus, and at a moment when deadly outbreaks of the disease were already festering in places like the Life Care Center in Kirkland. Within weeks, three dozen people infected with COVID-19 would die at the nursing home in the suburbs of Seattle.
The spread of COVID-19 would not take long to overwhelm the state, which as of March 20, 2020, had more than 1,300 cases.
The Trump administration in recent days has attempted to speed testing for the virus after early missteps hampered the government’s response to contain the contagion, and officials have had to respond to a barrage of criticism from public health experts, state officials, and members of Congress.
Federal health officials have eased the process for university and commercial labs to perform their own tests, and they are ramping up their capacity. As of March 16, public and private labs in the United States had the ability to test more than 36,000 people a day, according to estimates compiled by the American Enterprise Institute, a conservative-leaning think tank in Washington, a figure expected to rapidly escalate in coming weeks. That figure, however, can vary considerably by state and does not indicate how many tests are actually given to patients.
“We are now beginning to see that they have spread out in a prioritized way. We asked them to prioritize the regions that were mostly affected,” Deborah Birx, the coronavirus response coordinator for the White House Coronavirus Task Force, said March 18 of private labs’ testing, without elaboration.
The scaling up of testing is set to take place after weeks of faltering and hundreds, if not thousands, of undiagnosed people spreading the virus. For example, New York’s state health department received a faulty CDC test kit on Feb. 8 for 800 patient specimens, an amount that’s consistent with other states, according to a spokesperson. It later began testing patients with a test that state officials developed based on the CDC protocol and has significantly increased testing – as of March 20, more than 7,200 people had tested positive statewide.
In New York City, the first batch was obtained on Feb. 7.
“The other state and local public health laboratories got test kits as they became available,” said Eric Blank, chief program officer of the Association of Public Health Laboratories.
Places in the middle of the country with no outbreaks had the luxury of time to plan. For example, Missouri officials have had about 800 tests to work with, leading to only 395 performed so far in the region by public health labs – 26 of which were positive. When private lab tests are accounted for, as of March 20 there were 47 confirmed cases.
Health care providers and public health staff in the state, however, benefited from the fact that there is less international travel to the region, according to infectious disease expert Steven Lawrence, MD, of Washington University, St. Louis.
“This is very similar to 1918 with the influenza pandemic – St. Louis had more time to prepare and was able to put measures in place to flatten the curve than, say, Philadelphia,” Dr. Lawrence said. “Seattle didn’t have an opportunity to prepare as much in advance.”
While commercial labs are coming online, strict restrictions are limiting testing capabilities, Dr. Lawrence said.
“The state has had their hands tied,” he added.
Waiting And wondering
Because of a widespread lag in testing, it is still a mystery for thousands of people to know whether they’ve come into contact with an infected person until well after it happens. As of March 20, the pandemic had killed more than 11,000 globally. More than 16,000 Americans were confirmed infected and at least 216 have died.
“CDC will distribute tests based on where they can do the most good. But without hospital-based testing and commercial testing, it will not be possible to meet the need,” said Tom Frieden, who led the CDC during President Obama’s administration and is a former commissioner of the New York City Health Department.
In California, public school teacher Claire Dugan, whose state was among the hardest hit in the initial wave of U.S. coronavirus cases, was told she didn’t qualify for testing because she had not traveled abroad to any country with an outbreak of the virus or been in contact with an infected person. Ms. Dugan, who lives in the San Francisco Bay area and is already medically fragile after a stray bullet nearly killed her while driving 4 years ago, sought a test from her doctor after registering a temperature of 100.7° F earlier this month.
“There are a lot of layers as to why this is so messed up,” said Ms. Dugan, who relies on a feeding tube and said she sought a test not only to protect herself but her students. “It’s community spreading right now, so it’s kind of silly we’re still insisting on [the early criteria for testing]. How would I know?”
Since the CDC’s initial distribution, states have been reordering more tests through the office’s International Reagent Resource – a long-standing tool that public health labs have relied on. They have also revised testing protocols to use only one sample per person, which boosts the number of people screened.
Yet problems still abound with tests or other materials needed to be able to detect the virus. California Gov. Gavin Newsom (D) said on March 12 that county public health labs can’t use all of the 8,000 test kits the state has because they are missing key components.
In Pennsylvania, state officials weren’t able to begin testing until March 2 because of problems with the CDC’s initial kit, according to Nate Wardle, a spokesperson at its department of health. New York received two newly manufactured CDC test kits on Feb. 29 and also began performing tests March 2, according to its health department.
“We are still limited on extraction kits,” Mandy Cohen, the Health & Human Services secretary in North Carolina, said in an interview in mid-March. Officials earlier this month could test only 300 patients because of shortages in the extraction materials needed to register whether the novel coronavirus is present.
In North Dakota, Loralyn Hegland wrote her physician’s practice an email on March 10 with the subject line “dry cough,” wondering if she should come in for testing after learning that was one symptom of COVID-19. The recommendation she got echoes those of countless others across the United States, saying her risk of being exposed was very low because she hadn’t traveled outside the United States and had not come into contact with a person who had been “definitely” diagnosed with the virus.
Ms. Hegland, who lives in Fargo, didn’t have a fever but decided to shelter herself, anyway, out of caution.
Would she push to get a test?
“What’s the point?” she said. “You can’t know what you don’t know. It’s just that simple. How else do you explain it to people when you’re not testing?”
KHN Midwest correspondent Lauren Weber in St. Louis contributed to this article.
Kaiser Health News is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
AMA offers resources for front-line physicians
.
The literature include news, advocacy, and other information to help front-line physicians provide care to patients and keep themselves safe “in a rapidly changing environment,” the organization said in a statement.
“The AMA continues to forcefully advocate for [personal protective equipment] and critical policy and regulatory changes needed to address our public health and health system needs. Because so many of the challenges of the pandemic are felt at a practice level, we are also providing new tools and information to help physicians respond,” AMA President Patrice A. Harris, MD, said in the statement.
The COVID-19 physician and practice resources released by the AMA include:
- A Physicians Guide to COVID-19 .
- An AMA COVID-19 online resource center and a COVID-19 FAQ.
- A Quick Guide to Telemedicine in Practice.
- Ethical guidance for physicians .
- Evidence-based resources from the The JAMA Network COVID-19 Resource Center.
- CME for physicians through the JAMA Network’s JN Learning website.
.
The literature include news, advocacy, and other information to help front-line physicians provide care to patients and keep themselves safe “in a rapidly changing environment,” the organization said in a statement.
“The AMA continues to forcefully advocate for [personal protective equipment] and critical policy and regulatory changes needed to address our public health and health system needs. Because so many of the challenges of the pandemic are felt at a practice level, we are also providing new tools and information to help physicians respond,” AMA President Patrice A. Harris, MD, said in the statement.
The COVID-19 physician and practice resources released by the AMA include:
- A Physicians Guide to COVID-19 .
- An AMA COVID-19 online resource center and a COVID-19 FAQ.
- A Quick Guide to Telemedicine in Practice.
- Ethical guidance for physicians .
- Evidence-based resources from the The JAMA Network COVID-19 Resource Center.
- CME for physicians through the JAMA Network’s JN Learning website.
.
The literature include news, advocacy, and other information to help front-line physicians provide care to patients and keep themselves safe “in a rapidly changing environment,” the organization said in a statement.
“The AMA continues to forcefully advocate for [personal protective equipment] and critical policy and regulatory changes needed to address our public health and health system needs. Because so many of the challenges of the pandemic are felt at a practice level, we are also providing new tools and information to help physicians respond,” AMA President Patrice A. Harris, MD, said in the statement.
The COVID-19 physician and practice resources released by the AMA include:
- A Physicians Guide to COVID-19 .
- An AMA COVID-19 online resource center and a COVID-19 FAQ.
- A Quick Guide to Telemedicine in Practice.
- Ethical guidance for physicians .
- Evidence-based resources from the The JAMA Network COVID-19 Resource Center.
- CME for physicians through the JAMA Network’s JN Learning website.
How texting unites Seattle’s critical care departments
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
Psoriasis Therapy During the COVID-19 Pandemic: Should Patients Continue Biologics?



Webinar confronts unique issues for the bleeding disorders community facing COVID-19
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
Should patients with COVID-19 avoid ibuprofen or RAAS antagonists?
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
Researchers have hypothesized that treatments that increase angiotensin-converting enzyme 2 (ACE2) may also increase the risk of novel coronavirus disease (COVID-19). This speculation and other concerns have led some officials and organizations to question whether ibuprofen or other drugs such as renin angiotensin aldosterone system (RAAS) antagonists should be avoided as treatments in patients with COVID-19. Health agencies and professional organizations have said they are not recommending against these medications.
The Food and Drug Administration on March 19 advised patients that it was “not aware of scientific evidence connecting” nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen “with worsening COVID-19 symptoms.”
“The agency is investigating this issue further and will communicate publicly when more information is available,” the FDA said. “However, all prescription NSAID labels warn that ‘the pharmacological activity of NSAIDs in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.’ ” The FDA also noted that other over-the-counter and prescription medications are available for pain relief and fever reduction, and patients who “are concerned about taking NSAIDs and rely on these medications to treat chronic diseases” should talk to a health care provider.
A World Health Organization spokesperson said during a press conference on March 17 that the organization was looking into concerns about ibuprofen use in patients with COVID-19 and suggested that in the meantime patients take acetaminophen for fever instead. On March 18, the WHO said that it was not recommending against the use of ibuprofen.
“At present, based on currently available information, WHO does not recommend against the use of ibuprofen,” the organization said. “We are also consulting with physicians treating COVID-19 patients and are not aware of reports of any negative effects of ibuprofen, beyond the usual known side effects that limit its use in certain populations. WHO is not aware of published clinical or population-based data on this topic.”
A spokesperson for the National Institute of Allergy and Infectious Diseases said on March 18, “More research is needed to evaluate reports that ibruprofen and other over-the-counter anti-inflammatory drugs may affect the course of COVID-19. Currently, there is no conclusive evidence that ibuprofen and other over-the-counter anti-inflammatory drugs increase the risk of serious complications or of acquiring the virus that causes COVID-19. There is also no conclusive evidence that taking over-the-counter anti-inflammatory drugs is harmful for other respiratory infections.”
The European Medicines Agency (EMA) on March 18 said, “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID‑19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic.”
In correspondence published March 11 in the Lancet Respiratory Medicine, Lei Fang, MD, of the department of biomedicine at University Hospital Basel (Switzerland), and colleagues suggested that patients with hypertension and diabetes mellitus may be at increased risk of COVID-19 because these comorbidities “are often treated with angiotensin converting enzyme (ACE) inhibitors.” In addition, “ACE2 polymorphisms that have been linked to diabetes mellitus, cerebral stroke, and hypertension” also may play a role, the researchers said (Lancet Respir Med. 2020 Mar 11. https://doi.org/10.1016/S2213-2600(20)30116-8).
“ACE2 is substantially increased in patients with type 1 or type 2 diabetes, who are treated with ACE inhibitors and angiotensin II type-I receptor blockers (ARBs). Hypertension is also treated with ACE inhibitors and ARBs, which results in an upregulation of ACE2. ACE2 can also be increased by thiazolidinediones and ibuprofen.”
A March 16 statement from the Heart Failure Society of America (HSFC), American College of Cardiology (ACC), and American Heart Association (AHA) addressed concerns about using RAAS antagonists in COVID-19.
“Patients with underlying cardiovascular diseases appear to have an increased risk for adverse outcomes with [COVID-19],” the organizations said. “Although the clinical manifestations of COVID-19 are dominated by respiratory symptoms, some patients also may have severe cardiovascular damage. [ACE2] receptors have been shown to be the entry point into human cells for SARS-CoV-2, the virus that causes COVID-19. In a few experimental studies with animal models, both [ACE] inhibitors and angiotensin receptor blockers (ARBs) have been shown to upregulate ACE2 expression in the heart. Though these have not been shown in human studies, or in the setting of COVID-19, such potential upregulation of ACE2 by ACE inhibitors or ARBs has resulted in a speculation of potential increased risk for COVID-19 infection in patients with background treatment of these medications.”
ACE2, ACE, angiotensin II, and other RAAS system interactions “are quite complex, and at times, paradoxical,” the statement says. “In experimental studies, both ACE inhibitors and ARBs have been shown to reduce severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.
“Currently there are no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists in COVID-19 or among COVID-19 patients with a history of cardiovascular disease treated with such agents. The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic heart disease. In the event patients with cardiovascular disease are diagnosed with COVID-19, individualized treatment decisions should be made according to each patient’s hemodynamic status and clinical presentation. Therefore, be advised not to add or remove any RAAS-related treatments, beyond actions based on standard clinical practice.
“These theoretical concerns and findings of cardiovascular involvement with COVID-19 deserve much more detailed research, and quickly. As further research and developments related to this issue evolve, we will update these recommendations as needed.”
Dr. Fang and colleagues had no competing interests.
SOURCE: Fang L et al. Lancet Respir Med. 2020 Mar 11. doi: 10.1016/S2213-2600(20)30116-8.
Managing the COVID-19 isolation floor at UCSF Medical Center
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Flu now riding on COVID-19’s coattails
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
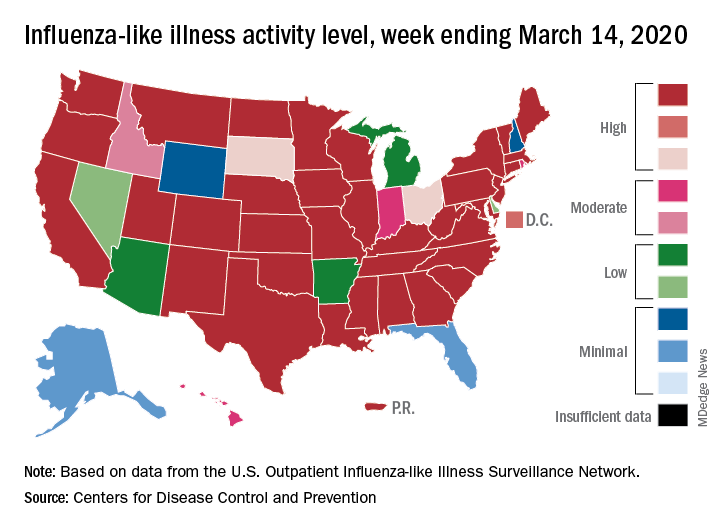
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
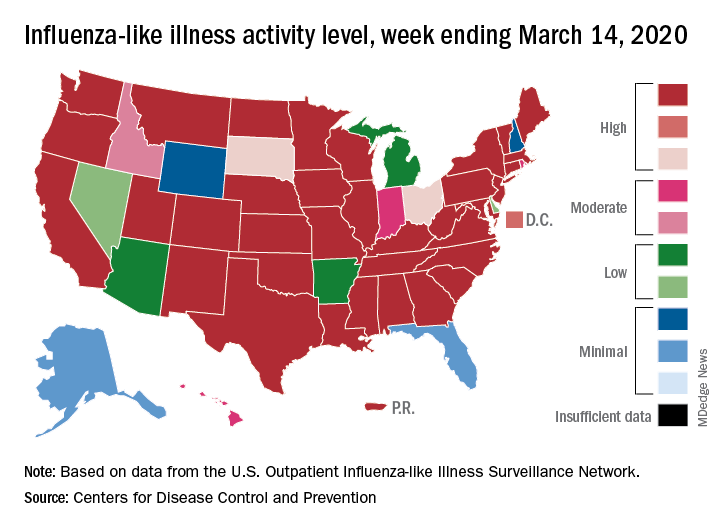
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
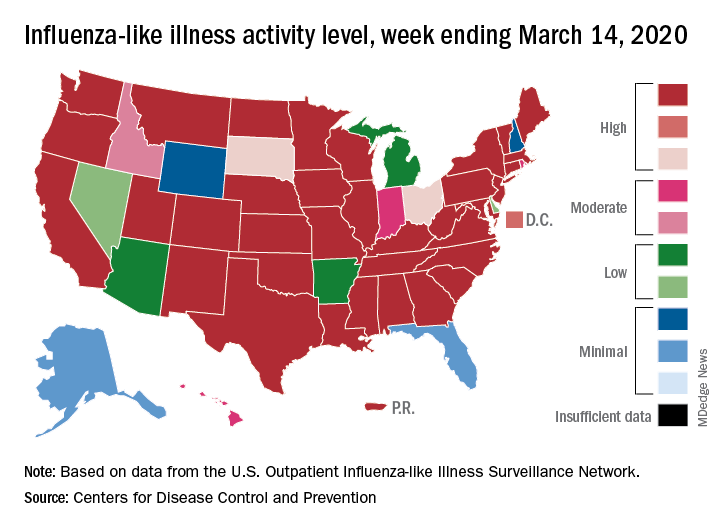
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.

