User login
Children and COVID: New cases up slightly, vaccinations continue to slow
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.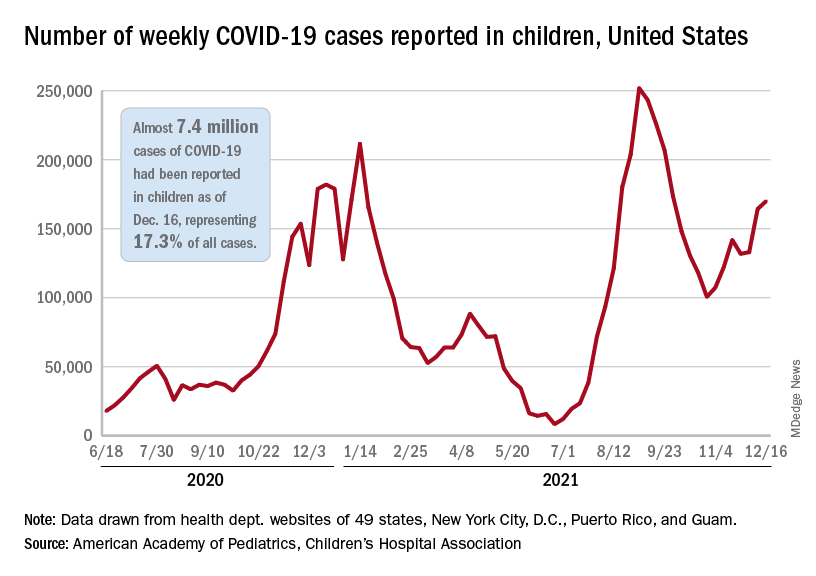
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.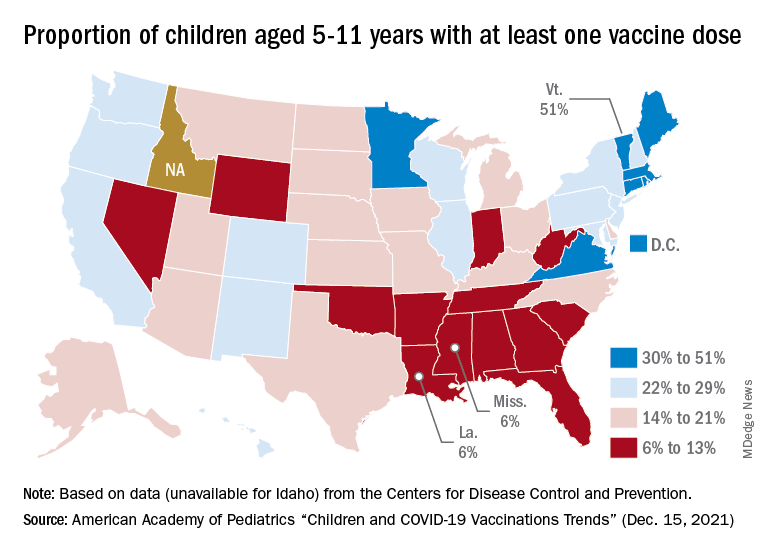
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.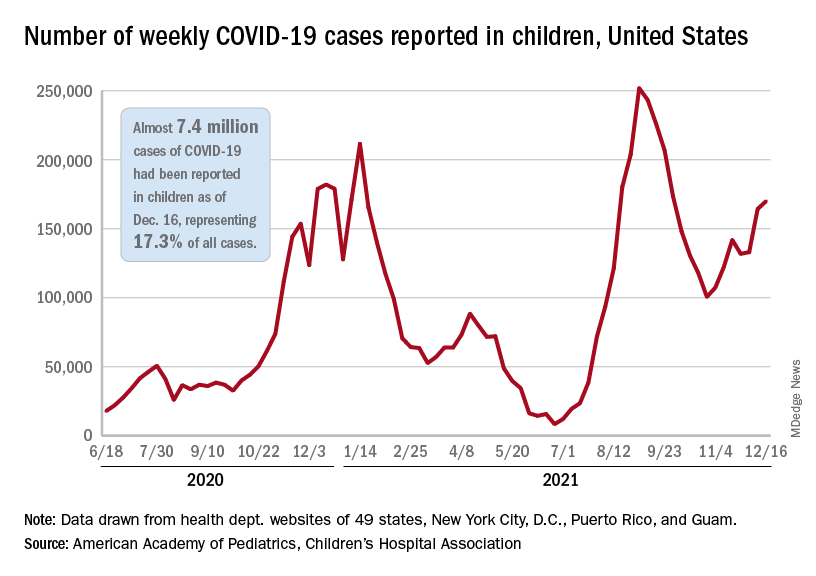
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.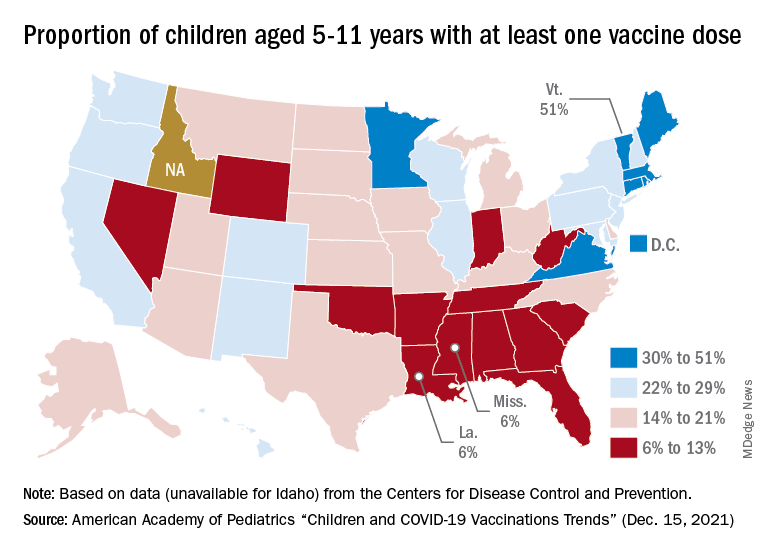
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.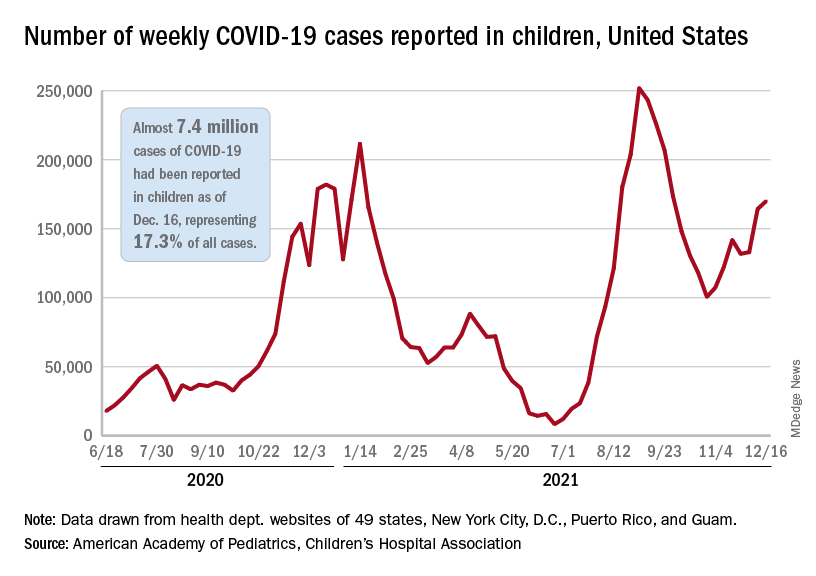
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
RSV resurgence likely in wake of COVID-19
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
The impact of respiratory syncytial virus (RSV)will likely be greater in 2021 and 2022 in the United States than in previous years as a result of the ongoing COVID-19 pandemic, based on data from a simulation-modeling study involving approximately 19 million individuals.
Although RSV usually follows consistent patterns of timing and duration, the disease all but disappeared starting in March 2020 after the introduction of measures to mitigate the spread of COVID-19, Zhe Zheng, MBBS, of Yale University, New Haven, Conn., and colleagues wrote.
However, lifting of mitigation measures has resulted in emergence of RSV in various parts of the world in early 2021, and trends may be similar in the United States, but data are needed to plan for prophylaxis and hospital use, they noted.
In a study published in JAMA Network Open, the researchers developed a simulation model for epidemics of RSV based on historical data. They acquired inpatient records from New York during 2005-2014 and from California during 2003-2011. The primary clinical outcome was the estimated monthly hospitalizations for RSV.
The simulated study population was 19.45 million individuals. After evaluating several scenarios including continued low transmission associated with social distancing and other mitigation measures, the researchers focused on the likely scenario that introduction of RSV from other regions would likely spark RSV epidemics in the United States.
They determined that spring and summer 2021 would show an increase in hospitalizations for RSV. Overall, higher rates of virus introduction from other regions were associated with more intense spring and summer RSV epidemics, with the trade-off of smaller winter epidemics. In the model, the expected RSV epidemic in spring and summer 2021 in New York was small, with a peak incidence of 419 hospitalizations per 100,000 people in April; by contrast, for states with less seasonal variability, such as Florida, the model predicted a larger summer epidemic.
In the model, the mean age of hospitalization for children younger than 5 years for January 2022 was expected to be 1.17 years, compared with 0.84 years in January 2019, the researchers noted.
Across all age groups, the greatest relative increase in the incidence of RSV infection was predicted for children aged 1-4 years (ranging from 82% to 86%), as were lower respiratory infections (87%-101%) and hospitalization (99%-119%), compared with prepandemic levels.
Hospitalizations for children aged 1 year were predicted to double compared with prepandemic seasons; 707 per 100,000 children per year for 2021 and 2022 versus 355 per 100,000 children per year in a typical prepandemic season. However, the largest incidence of lower respiratory infections (30,075 per 100,000) was predicted for infants aged 3-5 months, and the largest incidence of hospitalizations (3,116 per 100,000) was predicted for infants younger than 3 months.
“Without virus importation, the risk of RSV infections across all age groups in the winter of 2021 and 2022 would be greater, as more susceptible individuals were spared from infections in the absence of summer epidemics,” the researchers noted.
The older mean hospitalization age seen in the model was similar to the reported median patient age in Australia both before the pandemic and during the reemergent RSV epidemic.
“This makes intuitive sense, since many children born in 2020 were spared from RSV infection due to the low virus activity; these children will be older when they get infected for the first time during the reemergent epidemics,” the researchers wrote. “Consequently, stakeholders should consider modifying prophylaxis guidelines to include high-risk infants less than 2 years of age for the 2021-2022 season.”
The study findings were limited by several factors including the lack of data on level of virus introduction or on the impact of lack of boosting on infants with only transplacentally acquired RSV antibodies, the researchers noted. Other limitations include the use of historical data and the lack of data on values outside those included in the model, as well as the inability to control for other factors that could influence RSV, such as vaccines or long-lasting antibodies.
However, the results suggest that the rate of imported infections is associated with RSV hospitalizations, and the model effectively captured the RSV epidemics in the United States in spring and summer 2021.
Models can guide clinical preparations
“Health care simulation modeling is a growing field, with very exciting implications,” Lenore Jarvis, MD, of George Washington University, Washington, said in an interview. The field has the potential ability to influence health care in a data-driven way, including, but not limited to, staffing and other hospital operations, as well as patient care decision-making. “In short, accurate modeling and predictions can help us to make informed health care decisions that can lead to increased quality of care, potential cost savings, and even to help save lives,” she said.
Although the details of transmission modeling were not mentioned in the study, the authors evaluated the performances of several models and scenarios. “Scenario 4, for example, was focused on in particular because it best captured the observed dynamics [for RSV] that emerged during the spring and summer of 2021,” Dr. Jarvis said.
“Pediatricians can speak to these trends firsthand. A decrease in expected RSV infections and hospitalizations in 2020, followed by an unprecedented and early increase in RSV infections and severity in 2021, and the factors that the authors account for make sense, such as reintroduction of RSV from other regions and low immunity in the population,” she said. “It also makes sense that, in these transmission modeling scenarios, the expected mean age of hospitalization because of RSV increased with a temporary (hopefully) increase in RSV hospitalizations in the 2021 season, and potentially the 2022 RSV season.”
As for additional research, Dr. Jarvis said she would like to see follow-up data on the RSV transmission modeling. “For example, with scenario 4, does this scenario continue to perform well in other time periods, such as the winter? If the modeling continues to be accurate during other periods of evaluation and reevaluation, this modeling could be very useful in helping pediatric clinics and hospitals to prepare for RSV care and hospital capacity management.”
The study was supported by grants to various researchers from the National Institute of Allergy and Infectious Diseases/National Institutes of Health, the National Center for Advancing Translational Science at the National Institutes of Health, and NIH Roadmap for Medical Research. Lead author Ms. Zheng had no financial conflicts to disclose. Her study coauthors disclosed relationships with companies including AbbVie, Merck, Pfizer, GlaxoSmithKline, MedImmune, and Janssen. Dr. Jarvis had no financial conflicts to disclose and serves on the Pediatric News editorial advisory board.
FROM JAMA NETWORK OPEN
FDA approves cabotegravir LA; New HIV PrEP option fills an important gap
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
SILVER SPRING, MD – .
The priority review approval was based on phase 2b-3 clinical trial data submitted to the agency this past August, after the study was stopped early due to encouraging efficacy results of the first pre-planned interim end-point analysis.
“Although TDF-FTC PrEP could be almost astoundingly effective in preventing HIV acquisition across populations and risk exposures, the adherence to the daily protocols was really challenging and difficult to attain initially and to maintain for some of our most vulnerable populations,” Raphael Landovitz, MD, MDC, lead study investigator and co-director of The Center for HIV Identification, Prevention, and Treatment Services at UCLA, Los Angeles, told this news organization.
Dr. Landovitz noted that population level benefits observed with PrEP were limited to people who were highly engaged in health care and well resourced, but the same benefits were not observed in the most vulnerable, highest-risk populations.
“The idea was, is there anything that we can do to improve ... choices for different options, some of which – like long-acting agents – would remove the obligation to adhere to daily prescribing or a post-coital and be more discreet,” he said.
Data demonstrated superiority versus TDF-FTC
Details of the prospective, phase 2b-3 randomized, double-blind, double-dummy, active-controlled trial among 4,566 cisgender MSM (men who have sex with men) and transgender women highlighted the superiority of CAB 600 mg intramuscularly versus placebo or active TDF-FTC (300 mg/200 mg), with CAB-LA reducing HIV infection risk by 66%. These results were published August 11 in the New England Journal of Medicine and previously reported by this news organization.
Investigators identified HIV infections in 57 participants (including 52 who acquired HIV infections after enrollment). The hazard ratio for incident HIV infection versus TDG-FTC was 0.34, P < .001. Notably, effects were consistent across prespecified subgroups and populations.
Additionally, integrase strand-transfer inhibitor (INSTI) resistance mutations were detected in 1 of 4 of baseline HIV infection cases among CAB participants, while 2 of 39 incident infections in TDF-FTC participants occurred despite drug concentrations indicating good PrEP adherence.
Adverse events, breakthrough infections, and other important considerations
Because the trial was halted early, long-term safety data were lacking, thereby prompting investigators to launch an ongoing, open-label extension. In the initial trial, injection site reactions were reported in 81.4% (1,724) of CAB participants, most beginning a median of 1 day (IQR 0-2 days) post-injection, mild to moderate in severity (60.8% pain, 23.7% tenderness), and lasting a median of 3 days (IQR 2-6 days). In comparison, injection site reactions were reported in 31.3% of TDF-FTC participants (who, incidentally, received at least one placebo injection).
Severe adverse events (grade 3 or higher) were similar between CAB and TDF-FTC groups, They consisted mostly of an increase in creatine kinase level (14.2% with CAB vs. 13.5% with TDF-FTC) and a decrease in creatinine clearance (7.0% with CAB vs. 8.3% with TDF-FTC).
Although weight gain was higher among CAB participants (1.23 kg/year vs. 0.37 kg/year, TDF-FTC participants), most of the differences were observed during the first 40 weeks and were driven by weight loss in the TDF-FDC group. Weight changes were similar (~1 kg/year) thereafter.
Importantly, study participants assigned CAB underwent an oral-tablet, 5-week lead-in phase, which might have contributed to eventual treatment failure.
In a companion piece published Nov. 1 in the Journal of Infectious Diseases, investigators noted that adherence to the oral lead-in was poor in roughly one-third of participants with incident, breakthrough infections. They wrote that the barriers to adherence with daily oral PrEP regimens coupled with the favorable CAB-LA safety profile suggested that “the oral phase before CAB-LA initiation might not be necessary or desirable.”
The question remains as to whether or not strategies entailing viral load or other RNA screening tests at follow-up clinic visits might be warranted.
“It’s one of the biggest sort of ‘what’s next’ questions that’s come out of this study,” Dr. Landovitz said. “We’re now testing the strategy of using viral load or RNA screening at every visit to see if, in fact, we can catch these breakthrough infections earlier and potentially avoid resistance,” he added.
Until more data are available, Dr. Landovitz said that “the guidance for the clinician would be that until you have resistance testing back on someone who breaks through cabotegravir PrEP to use a protease inhibitor-based treatment regimen, at least initially.”
Institutional changes to ensure delivery of injections, tracking, and follow-up to ensure optimal use of long-acting PrEP agents are likely to challenge already overburdened health care systems and may require additional strategies for implementation (for example, pharmacy or at-home administration). Despite these factors, CAB-LA approval is welcome news to clinicians and patients alike.
“We’re constantly searching for new drugs to expand our repertoire of what we can provide patients,” Lina Rosengren-Hovee, MD, MPH, assistant professor of medicine and infectious disease specialist at UNC Health, Chapel Hill, N.C., said in an interview. Dr. Rosengren-Hovee was not involved in the study.
“For folks under 30, the sexual and gender minority, Black, and Latino, they are the ones with the highest need for PrEP, that are in a position that places them at higher risk for HIV. Being able to offer an injectable option is ... a game changer,” she said.
Dr. Rosengren-Hovee reports no relevant financial relationships. Dr. Landovitz has consulting relationships with Gilead, Janssen, Roche, and Cepheus.
A version of this article first appeared on Medscape.com.
Axilla swelling after COVID booster puts focus on mammogram timing
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
This inflammation is caused by the enlargement of lymph nodes and can show up as an abnormal finding on mammograms and other types of chest scans, causing concern and even the need for additional imaging and follow up, wrote Constance D. Lehman, MD, PhD, and colleagues in an article published in Journal of the American College of Radiology.
Lymph node swelling is a normal immune system reaction to vaccination, and “COVID-19 vaccinations in the arm are a well-documented cause of inflammatory unilateral axillary adenopathy,” noted Dr. Lehman, in an interview. The side effect will occur on the side of the body where the patient received a vaccine, and it is not always noticeable to the woman experiencing it, she said.
“We’re finding that the patients’ bodies are responding to the booster in many ways that are similar to the initial COVID vaccines, with lymph node swelling, muscle aches and pains, headaches, and so on,” said Dr. Lehman, who is chief of breast imaging at the Massachusetts General Hospital, Boston. There have been no real differences in reactions between the Moderna and Pfizer vaccines, she added.
Because axillary lymph node swelling can obscure mammogram results, staff of at least a few imaging centers, including Penn State Breast Center in Hershey, Pa., and Providence Women’s Imaging Center in Torrance, Calif., told this news organization that they are asking women to delay mammogram imaging either 6 weeks or 4-6 weeks after getting a COVID-19 booster.
Experts’ suggestions on mammograms, boosters timing
Other experts, including Jessica Leung, MD, acknowledged that vaccine-related reactive adenopathy is seen after the booster dose and provided recommendations for the timing of getting mammograms and the booster with this in mind.
“I would recommend getting the screening mammogram first, which can be followed immediately by vaccination, even on the same day,” said Jessica Leung, MD, a professor of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, Tex.
“If this is not possible from the scheduling perspective, then the patient should consult her health care provider regarding whether it is okay to wait a bit after receiving the vaccine before getting her screening mammogram.”
The answer to that question will likely depend on the time interval since the prior mammogram and the patient’s personal risk factors for developing breast cancer. Dr. Leung noted. “This is all predicated on the assumption that the patient is asymptomatic. If she has any symptoms, for example a palpable breast lump, then she should seek medical attention regardless of timing of vaccination.”
The same holds true for boosters, she said.
She emphasized that careful consideration should be given before delaying the mammogram. “The medical community has a great deal more knowledge at this time than in the early days of COVID-19 vaccination, so we are often able to identify reactive adenopathy related to vaccination. If patients were to delay the mammogram, any reactive adenopathy may persist, on average, for 4-6 weeks.”
Debra Patt, MD, PhD, MBA, executive vice president at Texas Oncology, professor at the University of Texas at Austin, provided a specific example of when a patient should not delay the diagnostic imaging, which is “in the event that there is an abnormal mass in the breast that requires evaluation.”
Providers are now prepared to address these issues, she added.
Dr. Lehman’s nuanced recommendations
“It’s easy to get both a mammogram and booster, and just a matter of timing them – so that the reaction doesn’t interfere with the mammography results,” Dr. Lehman said.
But she emphasized that women should not be choosing between their mammograms or a booster. “We are now saying the same thing that we did with the initial vaccine,” said Dr. Lehman. “We don’t want patients delaying their mammograms, and we don’t want them delaying their boosters – both are critical to staying healthy.”
In her center, a model was developed to navigate vaccine-associated adenopathy. While this approach was developed for the primary vaccine series, the same applies for the booster, which is essentially a third dose of the same vaccine, explained Dr. Lehman.
When patients present for mammography, ultrasound, or MRI, the technologist will document their COVID-19 vaccination status (first or second dose or booster), the date it was given, and the location. Adding vaccination documentation to intake forms helps to support appropriate management of patients who undergo imaging after COVID-19 vaccination. Six weeks is used as the cutoff point for defining “recent” vaccination.
For patients who are getting a screening mammography or MRI, and who have no symptoms beyond unilateral axillary adenopathy on the same side of the body where they received the COVID-19 vaccination (given in the arm) within a 6-week period, the following is included in the screening mammography or screening MRI report: “In the specific setting of a patient with documented recent (within the past 6 weeks) COVID-19 vaccination in the ipsilateral arm, axillary adenopathy is a benign imaging finding. No further imaging is indicated at this time. If there is clinical concern that persists more than 6 weeks after the patient received the final vaccine dose, axillary ultrasound is recommended.”
The experts interviewed reported no conflicts of interest.
AAP updates guidance on HIV testing and prophylaxis in youth
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
Pediatricians should take a more proactive role in protecting children and adolescents from HIV infections, according to updated guidance from the American Academy of Pediatrics. The comprehensive new recommendations stress winning the trust and confidence of pediatric patients and reaffirm support for testing and treating adolescents without parental consent where state laws allow.
While the number of HIV-infected people in the United States remains high, most sexually active youth do not believe they are at risk and have never been tested, noted authors Katherine K. Hsu, MD, MPH, of the Massachusetts Department of Public Health and Boston University Medical Center, and Natella Yurievna Rakhmanina, MD, PhD, of Children’s National Hospital and George Washington University, both in Washington.
That is a knowledge gap that pediatricians are well situated to fill. “Pediatricians can play a key role in preventing and controlling HIV infection by promoting risk-reduction counseling and offering routine HIV testing and prophylaxis to adolescent and young adult (youth) patients,” they wrote on Dec. 20, 2021, in their study published in Pediatrics.
Key components of youth encounters, they stressed, is creating safe environments for obtaining an accurate sexual and reproductive health assessment and providing nonstigmatizing risk counseling.
According to Dr. Rakhmanina, major barriers to addressing preventive HIV counseling have included pediatricians’ lack of time, cultural differences, adolescents’ inaccurate responses, discomfort discussing sexual issues, and adolescents’ fear of parent or caregiver notification. Other concerns have been lack of adequate payment and insufficient training in how to talk to adolescents about sexual and reproductive issues.
According to the Centers for Disease Control and Prevention, at year end in 2018 an estimated 1,173,900 people age 13 or older were living with HIV infection in the United States, of whom 47,800 (4%) were adolescents and young adults 13-24 years of age.
These estimates include diagnosed and undiagnosed individuals. Between 2014 and 2018, new diagnoses of HIV infection accounted for 21% (7,817 of 37,515) of all new HIV diagnoses in the United States.
The new AAP clinical report updates policy statements from 2001 and again 2011 that encouraged HIV testing of all sexually active youth.
It reflects changes in epidemiology, advances in diagnostic testing with improved immunoassays, and updated recommendations for HIV testing and postexposure prophylaxis (PEP), as well as new guidance for pre-exposure prophylaxis (PrEP).
A 2017 study found that the 2011 HIV testing guidelines was associated with only a slight increase in HIV screening and a shift toward testing younger people and away from testing on the basis of risk.
Against this backdrop of persistent HIV infection and to-date modest uptake of earlier guidance, the 2021 statement made 14 main recommendations to pediatricians. Among these:
- Foster open discussion of gender and sexual orientation and behavior, as well as reproductive health issues.
- Recognize the clinical presentation of the acute retroviral syndrome, which can present as syndromes resembling infectious mononucleosis and influenza.
- Consider including virologic testing in the diagnostic workup of sexually active youth.
- Consider routine HIV screening for all youth 15 years or older at least once and rescreening high-risk youth. Those at higher risk should be rescreened at least annually, and potentially as frequently as every 3-6 months.
- Youth at substantial risk should be routinely offered PrEP, while PEP with antiretroviral drugs is indicated after unsafe exposures such as unsafe sexual activity, unsafe needle use, or sexual violence. Survivors of sexual violence should have baseline HIV testing and sexually transmitted infection (STI) screening and treatment. They should also be offered mental health and other supportive counseling.
- Test youth who request HIV screening at any time even in the absence of reported risk factors. Although parent or guardian involvement is preferable, in most legal settings the adolescent’s consent should suffice for testing and treatment.
- For youth with a positive HIV test, facilitate and confirm prompt linkage to age-appropriate HIV specialty care.
Will the current report’s recommendations be met with greater uptake than previous iterations? Yes, according to Maria E. Trent, MD, MPH, chief of the division of adolescent/young adult medicine at Johns Hopkins University, Baltimore, but a fundamental first step will be the establishment of honesty and confidentiality. “Pediatricians are essential stakeholders in HIV prevention and intervention efforts in the United States. Recent data, however, suggest that pediatricians often struggle to create the essential alone time with adolescents and young adults to conduct critical sexual health conversations that allow for adequate STI/HIV risk screening,” said Dr. Trent, who was not involved in the report. “Consistently creating that space will be the first task for ensuring adherence to these recommendations.”
Strategies to optimize risk screening for clinical decision support, such as confidential online previsit questionnaires that link to the electronic medical record, may facilitate discussions during the visit while maintaining clinician efficiency, she added.
Furthermore, while one-time general HIV screening during adolescence will be an easy goal, “integrating annual testing, biomedical intervention for PrEP/PEP, and ongoing follow-up and testing for those on biomedical intervention may present practical but not insurmountable challenges,” Dr. Trent said.
When pediatricians recognize that care is suboptimal in practice, ensuring that pediatricians have established linkages to adolescent-friendly services for free or low-cost HIV testing, PrEP/PEP, and HIV management will prevent gaps in care, Dr. Trent continued. “The most exciting development in health care is that telemedicine can now be used to work with young people, giving the practicing pediatrician more opportunities and flexibility to deliver and triage care.”
Will any of the guidelines such as an adolescent’s right to independent consent be considered unacceptable by parents? “While this part of the recommendations is not new, the thought that their adolescent can initiate and receive confidential care for HIV prevention or intervention without their knowledge or consent may initially be challenging to process,” Dr. Trent said. “Ultimately, what I’ve observed in practice is that parents are relieved and often proud of their young person for taking the initiative to engage in self-care to maintain their health and relieved to be involved as a critical support person.”
She added that pediatricians need to make their practice policies clear and have information available for parents on state laws related to confidential care. “They also need to carefully use the electronic health record to avoid errors in disclosures to proxies without patient consent.”
Dr. Rakhmanina agreed there will likely be greater adherence to this round of recommendations. “The culture of addressing sexual and reproductive health issues among adolescents in the U.S. is changing among pediatric providers, and we start seeing more champions of PrEP and HIV testing in our communities,” she said.
This study received no external funding. The authors had no financial relationships or potential conflicts of interest to disclose. Dr. Trent disclosed no competing interests relevant to her comments.
FROM PEDIATRICS
Blastomycosislike Pyoderma: Verrucous Hyperpigmented Plaques on the Pretibial Shins
To the Editor:
Blastomycosislike pyoderma (BLP), also commonly referred to as pyoderma vegetans, is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 It is characterized by a collection of neutrophilic abscesses with pseudoepitheliomatous hyperplasia that coalesce into crusted plaques.
A 15-year-old adolescent girl with a history of type 1 diabetes mellitus was admitted for diabetic ketoacidosis. The patient presented with bilateral pretibial lesions of 6 years’ duration that developed after swimming in a pool following reported trauma to the site. These pruritic plaques had grown slowly and were occasionally tender. Of note, with episodes of hyperglycemia, the lesions developed purulent drainage.
Upon admission to the hospital and subsequent dermatology consultation, physical examination revealed the right pretibial shin had a 15×5-cm, gray-brown, hyperpigmented, verrucous, tender plaque with purulent drainage and overlying crust (Figure 1). The left pretibial shin had a similar smaller lesion (Figure 2). Laboratory test results were notable for a white blood cell count of 41.84 cells/µL (reference range, 3.8–10.5 cells/µL), blood glucose level of 586 mg/dL (reference range, 70–99 mg/dL), and hemoglobin A1c of 11.7% (reference range, 4.0%–5.6%). A biopsy specimen from the right pretibial shin was stained with hematoxylin and eosin for dermatopathologic evaluation as well as sent for tissue culture. Tissue and wound cultures grew Staphylococcus aureus and group B Streptococcus with no fungal or acid-fast bacilli growth.


Blood cultures were negative for bacteria. Results of radiographic imaging were negative for osteomyelitis. Biopsy specimens from the right pretibial plaque showed a markedly inflamed, ruptured follicular unit with a dense dermal lympho-neutrophilic infiltrate and overlying pseudoepitheliomatous hyperplasia (Figure 3). Periodic acid–Schiff, Gomori methenamine-silver, acid-fast bacilli, and Giemsa stains were negative for organisms. No granules consistent with a Splendore-Hoeppli phenomenon were observed. These observations were consistent with a diagnosis of BLP.
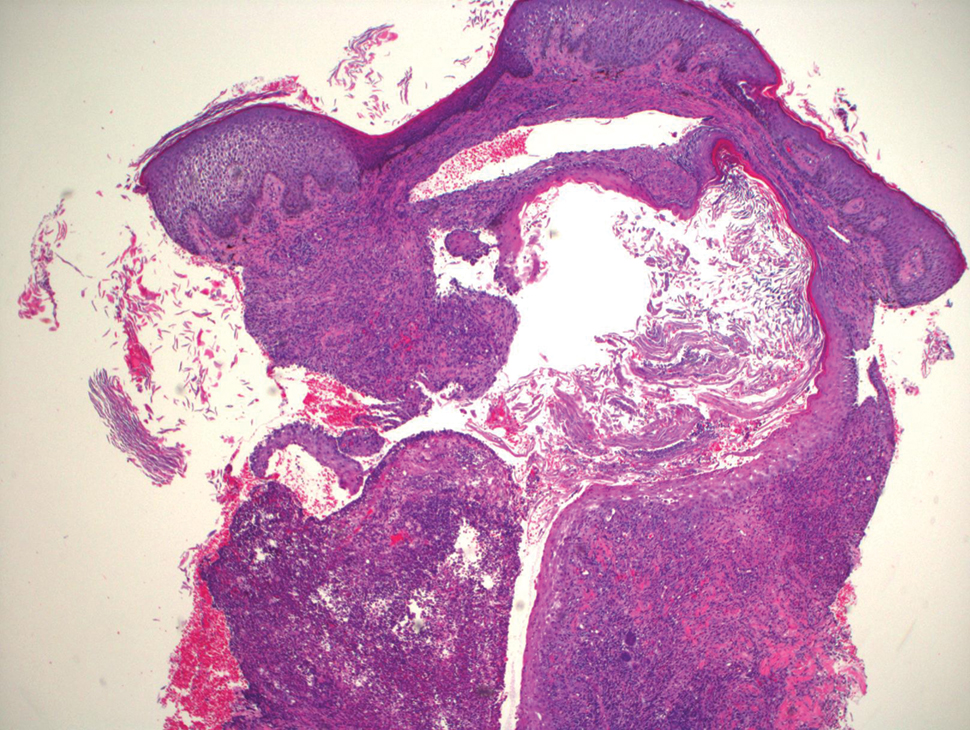
Blastomycosislike pyoderma is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 Pediatric cases also are uncommon. Blastomycosislike pyoderma most commonly is caused by infection with S aureus or group A streptococci, but several other organisms have been implicated.2 Clinically, BLP is similar to cutaneous botryomycosis, as both are caused by similar organisms.3 However, while BLP is limited to the skin, botryomycosis may involve visceral organs.
Blastomycosislike pyoderma typically presents as verrucous, hyperkeratotic, purulent plaques with raised borders. It most commonly occurs on the face, scalp, axillae, trunk, and distal extremities. Predisposing factors include immunosuppressed states such as poor nutrition, HIV, malignancy, alcoholism, and diabetes mellitus.3,4 Hyperglycemia is thought to suppress helper T cell (TH1)–dependent immunity, which may explain why our patient’s lesions worsened with hyperglycemic episodes.5Histopathology revealed pseudoepitheliomatous hyperplasia with neutrophilic abscesses.1 The distinguishing feature between botryomycosis and BLP is the development of grains known as the Splendore-Hoeppli phenomenon in botryomycosis.6 The grains are eosinophilic and contain the causative infectious agent. The presence of these grains is consistent with botryomycosis but is not pathognomonic, as it also can be found in several bacterial, fungal, and parasitic infections.3,6
The differential diagnosis of BLP includes atypical mycobacterial infection, pyoderma gangrenosum, fungal infection, and tuberculosis verrucosa cutis.7
Although BLP is caused by bacteria, response to systemic antibiotics is variable. Other treatment modalities include dapsone, systemic and intralesional corticosteroids, retinoids, debridement, CO2 laser, and excision.6,8 Lesions typically start out localized, but it is not uncommon for them to spread to distal or vulnerable tissue, such as sites of trauma or inflammation. Our patient was started on oral trimethoprim-sulfamethoxazole and showed improvement, but she worsened with subsequent hyperglycemic episodes when antibiotics were discontinued.
1. Adis¸en E, Tezel F, Gürer MA. Pyoderma vegetans: a case for discussion. Acta Derm Venereol. 2009;89:186-188.
2. Scuderi S, O’Brien B, Robertson I, et al. Heterogeneity of blastomycosis-like pyoderma: a selection of cases from the last 35 years. Australas J Dermatol. 2017;58:139-141.
3. Marschalko, M. Pyoderma vegetans: report on a case and review of data on pyoderma vegetans and cutaneous botryomycosis. Acta Dermatovenerol Alp Pannonica Adriat. 1995;4:55-59.
4. Cerullo L, Zussman J, Young L. An unusual presentation of blastomycosislike pyoderma (pyoderma vegetans) and a review of the literature. Cutis. 2009;84:201-204.
5. Tanaka Y. Immunosuppressive mechanisms in diabetes mellitus [in Japanese]. Nihon Rinsho. 2008;66:2233-2237.
6. Hussein MR. Mucocutaneous Splendore-Hoeppli phenomenon. J Cutan Pathol. 2008;35:979-988.
7. Lee YS, Jung SW, Sim HS, et al. Blastomycosis-like pyoderma with good response to acitretin. Ann Dermatol. 2011;23:365-368.
8. Kobraei KB, Wesson SK. Blastomycosis-like pyoderma: response to systemic retinoid therapy. Int J Dermatol. 2010;49:1336-1338.
To the Editor:
Blastomycosislike pyoderma (BLP), also commonly referred to as pyoderma vegetans, is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 It is characterized by a collection of neutrophilic abscesses with pseudoepitheliomatous hyperplasia that coalesce into crusted plaques.
A 15-year-old adolescent girl with a history of type 1 diabetes mellitus was admitted for diabetic ketoacidosis. The patient presented with bilateral pretibial lesions of 6 years’ duration that developed after swimming in a pool following reported trauma to the site. These pruritic plaques had grown slowly and were occasionally tender. Of note, with episodes of hyperglycemia, the lesions developed purulent drainage.
Upon admission to the hospital and subsequent dermatology consultation, physical examination revealed the right pretibial shin had a 15×5-cm, gray-brown, hyperpigmented, verrucous, tender plaque with purulent drainage and overlying crust (Figure 1). The left pretibial shin had a similar smaller lesion (Figure 2). Laboratory test results were notable for a white blood cell count of 41.84 cells/µL (reference range, 3.8–10.5 cells/µL), blood glucose level of 586 mg/dL (reference range, 70–99 mg/dL), and hemoglobin A1c of 11.7% (reference range, 4.0%–5.6%). A biopsy specimen from the right pretibial shin was stained with hematoxylin and eosin for dermatopathologic evaluation as well as sent for tissue culture. Tissue and wound cultures grew Staphylococcus aureus and group B Streptococcus with no fungal or acid-fast bacilli growth.


Blood cultures were negative for bacteria. Results of radiographic imaging were negative for osteomyelitis. Biopsy specimens from the right pretibial plaque showed a markedly inflamed, ruptured follicular unit with a dense dermal lympho-neutrophilic infiltrate and overlying pseudoepitheliomatous hyperplasia (Figure 3). Periodic acid–Schiff, Gomori methenamine-silver, acid-fast bacilli, and Giemsa stains were negative for organisms. No granules consistent with a Splendore-Hoeppli phenomenon were observed. These observations were consistent with a diagnosis of BLP.
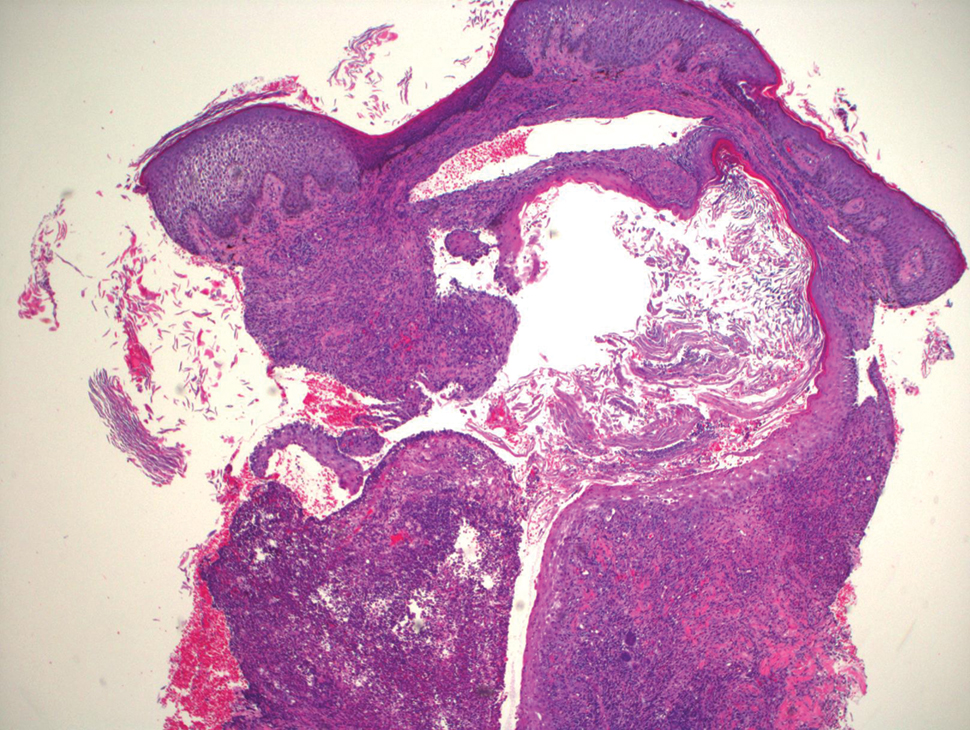
Blastomycosislike pyoderma is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 Pediatric cases also are uncommon. Blastomycosislike pyoderma most commonly is caused by infection with S aureus or group A streptococci, but several other organisms have been implicated.2 Clinically, BLP is similar to cutaneous botryomycosis, as both are caused by similar organisms.3 However, while BLP is limited to the skin, botryomycosis may involve visceral organs.
Blastomycosislike pyoderma typically presents as verrucous, hyperkeratotic, purulent plaques with raised borders. It most commonly occurs on the face, scalp, axillae, trunk, and distal extremities. Predisposing factors include immunosuppressed states such as poor nutrition, HIV, malignancy, alcoholism, and diabetes mellitus.3,4 Hyperglycemia is thought to suppress helper T cell (TH1)–dependent immunity, which may explain why our patient’s lesions worsened with hyperglycemic episodes.5Histopathology revealed pseudoepitheliomatous hyperplasia with neutrophilic abscesses.1 The distinguishing feature between botryomycosis and BLP is the development of grains known as the Splendore-Hoeppli phenomenon in botryomycosis.6 The grains are eosinophilic and contain the causative infectious agent. The presence of these grains is consistent with botryomycosis but is not pathognomonic, as it also can be found in several bacterial, fungal, and parasitic infections.3,6
The differential diagnosis of BLP includes atypical mycobacterial infection, pyoderma gangrenosum, fungal infection, and tuberculosis verrucosa cutis.7
Although BLP is caused by bacteria, response to systemic antibiotics is variable. Other treatment modalities include dapsone, systemic and intralesional corticosteroids, retinoids, debridement, CO2 laser, and excision.6,8 Lesions typically start out localized, but it is not uncommon for them to spread to distal or vulnerable tissue, such as sites of trauma or inflammation. Our patient was started on oral trimethoprim-sulfamethoxazole and showed improvement, but she worsened with subsequent hyperglycemic episodes when antibiotics were discontinued.
To the Editor:
Blastomycosislike pyoderma (BLP), also commonly referred to as pyoderma vegetans, is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 It is characterized by a collection of neutrophilic abscesses with pseudoepitheliomatous hyperplasia that coalesce into crusted plaques.
A 15-year-old adolescent girl with a history of type 1 diabetes mellitus was admitted for diabetic ketoacidosis. The patient presented with bilateral pretibial lesions of 6 years’ duration that developed after swimming in a pool following reported trauma to the site. These pruritic plaques had grown slowly and were occasionally tender. Of note, with episodes of hyperglycemia, the lesions developed purulent drainage.
Upon admission to the hospital and subsequent dermatology consultation, physical examination revealed the right pretibial shin had a 15×5-cm, gray-brown, hyperpigmented, verrucous, tender plaque with purulent drainage and overlying crust (Figure 1). The left pretibial shin had a similar smaller lesion (Figure 2). Laboratory test results were notable for a white blood cell count of 41.84 cells/µL (reference range, 3.8–10.5 cells/µL), blood glucose level of 586 mg/dL (reference range, 70–99 mg/dL), and hemoglobin A1c of 11.7% (reference range, 4.0%–5.6%). A biopsy specimen from the right pretibial shin was stained with hematoxylin and eosin for dermatopathologic evaluation as well as sent for tissue culture. Tissue and wound cultures grew Staphylococcus aureus and group B Streptococcus with no fungal or acid-fast bacilli growth.


Blood cultures were negative for bacteria. Results of radiographic imaging were negative for osteomyelitis. Biopsy specimens from the right pretibial plaque showed a markedly inflamed, ruptured follicular unit with a dense dermal lympho-neutrophilic infiltrate and overlying pseudoepitheliomatous hyperplasia (Figure 3). Periodic acid–Schiff, Gomori methenamine-silver, acid-fast bacilli, and Giemsa stains were negative for organisms. No granules consistent with a Splendore-Hoeppli phenomenon were observed. These observations were consistent with a diagnosis of BLP.
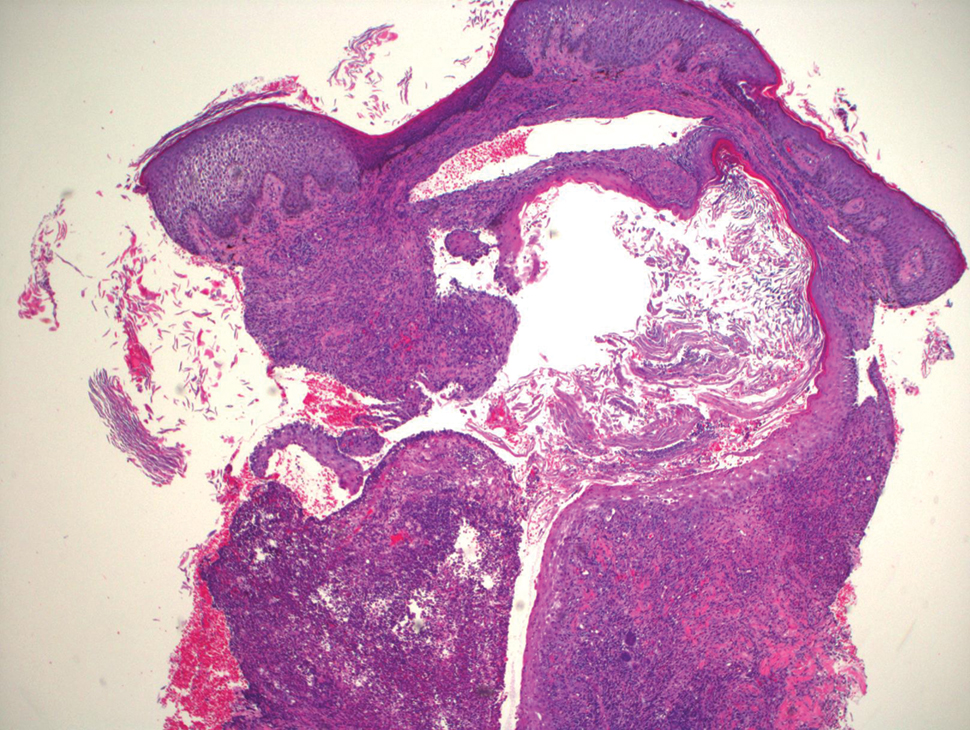
Blastomycosislike pyoderma is a rare cutaneous bacterial infection that often mimics other fungal, inflammatory, or neoplastic disorders.1 Pediatric cases also are uncommon. Blastomycosislike pyoderma most commonly is caused by infection with S aureus or group A streptococci, but several other organisms have been implicated.2 Clinically, BLP is similar to cutaneous botryomycosis, as both are caused by similar organisms.3 However, while BLP is limited to the skin, botryomycosis may involve visceral organs.
Blastomycosislike pyoderma typically presents as verrucous, hyperkeratotic, purulent plaques with raised borders. It most commonly occurs on the face, scalp, axillae, trunk, and distal extremities. Predisposing factors include immunosuppressed states such as poor nutrition, HIV, malignancy, alcoholism, and diabetes mellitus.3,4 Hyperglycemia is thought to suppress helper T cell (TH1)–dependent immunity, which may explain why our patient’s lesions worsened with hyperglycemic episodes.5Histopathology revealed pseudoepitheliomatous hyperplasia with neutrophilic abscesses.1 The distinguishing feature between botryomycosis and BLP is the development of grains known as the Splendore-Hoeppli phenomenon in botryomycosis.6 The grains are eosinophilic and contain the causative infectious agent. The presence of these grains is consistent with botryomycosis but is not pathognomonic, as it also can be found in several bacterial, fungal, and parasitic infections.3,6
The differential diagnosis of BLP includes atypical mycobacterial infection, pyoderma gangrenosum, fungal infection, and tuberculosis verrucosa cutis.7
Although BLP is caused by bacteria, response to systemic antibiotics is variable. Other treatment modalities include dapsone, systemic and intralesional corticosteroids, retinoids, debridement, CO2 laser, and excision.6,8 Lesions typically start out localized, but it is not uncommon for them to spread to distal or vulnerable tissue, such as sites of trauma or inflammation. Our patient was started on oral trimethoprim-sulfamethoxazole and showed improvement, but she worsened with subsequent hyperglycemic episodes when antibiotics were discontinued.
1. Adis¸en E, Tezel F, Gürer MA. Pyoderma vegetans: a case for discussion. Acta Derm Venereol. 2009;89:186-188.
2. Scuderi S, O’Brien B, Robertson I, et al. Heterogeneity of blastomycosis-like pyoderma: a selection of cases from the last 35 years. Australas J Dermatol. 2017;58:139-141.
3. Marschalko, M. Pyoderma vegetans: report on a case and review of data on pyoderma vegetans and cutaneous botryomycosis. Acta Dermatovenerol Alp Pannonica Adriat. 1995;4:55-59.
4. Cerullo L, Zussman J, Young L. An unusual presentation of blastomycosislike pyoderma (pyoderma vegetans) and a review of the literature. Cutis. 2009;84:201-204.
5. Tanaka Y. Immunosuppressive mechanisms in diabetes mellitus [in Japanese]. Nihon Rinsho. 2008;66:2233-2237.
6. Hussein MR. Mucocutaneous Splendore-Hoeppli phenomenon. J Cutan Pathol. 2008;35:979-988.
7. Lee YS, Jung SW, Sim HS, et al. Blastomycosis-like pyoderma with good response to acitretin. Ann Dermatol. 2011;23:365-368.
8. Kobraei KB, Wesson SK. Blastomycosis-like pyoderma: response to systemic retinoid therapy. Int J Dermatol. 2010;49:1336-1338.
1. Adis¸en E, Tezel F, Gürer MA. Pyoderma vegetans: a case for discussion. Acta Derm Venereol. 2009;89:186-188.
2. Scuderi S, O’Brien B, Robertson I, et al. Heterogeneity of blastomycosis-like pyoderma: a selection of cases from the last 35 years. Australas J Dermatol. 2017;58:139-141.
3. Marschalko, M. Pyoderma vegetans: report on a case and review of data on pyoderma vegetans and cutaneous botryomycosis. Acta Dermatovenerol Alp Pannonica Adriat. 1995;4:55-59.
4. Cerullo L, Zussman J, Young L. An unusual presentation of blastomycosislike pyoderma (pyoderma vegetans) and a review of the literature. Cutis. 2009;84:201-204.
5. Tanaka Y. Immunosuppressive mechanisms in diabetes mellitus [in Japanese]. Nihon Rinsho. 2008;66:2233-2237.
6. Hussein MR. Mucocutaneous Splendore-Hoeppli phenomenon. J Cutan Pathol. 2008;35:979-988.
7. Lee YS, Jung SW, Sim HS, et al. Blastomycosis-like pyoderma with good response to acitretin. Ann Dermatol. 2011;23:365-368.
8. Kobraei KB, Wesson SK. Blastomycosis-like pyoderma: response to systemic retinoid therapy. Int J Dermatol. 2010;49:1336-1338.
Practice Points
- Blastomycosislike pyoderma is a rare condition secondary to bacterial infection, but as the name suggests, it also can resemble cutaneous blastomycosis.
- Blastomycosislike pyoderma most commonly occurs in immunocompromised patients.
- The most common histologic findings include suppurative and neutrophilic inflammation with pseudoepitheliomatous hyperplasia.
COVID cases spike as questions remain about Omicron’s threat
The best way to stay protected is by getting vaccinated and boosted, they said.
“For the unvaccinated, you’re looking at a winter of severe illness and death – for yourselves, families, and the hospitals who may soon overwhelm,” White House COVID-19 Response Coordinator Jeff Zients said at a news briefing Dec. 17. “We need the American people to do their part.”
The Omicron variant has been detected in at least 39 states and 75 countries, according to CDC director Rochelle Walensky, MD.
The strain is more transmissible than the already highly infectious Delta variant, and although there was early evidence that it caused more mild disease, she said that is likely because many of those infected have been vaccinated and boosted.
“Although Delta continues to circulate widely in the United States, Omicron is increasing rapidly and we expect it to become the dominant strain in the United States, as it has in other countries, in the coming weeks,” Dr. Walensky said.
The United States is averaging close to 1,300 deaths from COVID-19 each day. New cases, deaths, and hospitalizations are higher now than in the previous winter – before vaccines were so widely available. The New York Times reported on Dec. 17 that new infections in Connecticut and Maine have grown 150% in the past 2 weeks, and Ohio and Indiana are seeing hospitalization rates nearing the worst of 2020-2021’s winter surge.
Dueling reports released recently gave cause for relief and concern about Omicron.
A study from South Africa released on Dec. 14 shows lower hospitalizations during the first 3 weeks of the Omicron wave than during earlier waves from other variants. That’s the good news.
The concerning news is out of the United Kingdom, where Imperial College London reported Dec. 17 that the risk of reinfection with COVID-19 from Omicron is more than 5 times as high and that cases of Omicron-based COVID-19 are doubling every 2 days.
What’s more, the study “finds no evidence of Omicron having lower severity than Delta, judged by either the proportion of people testing positive who report symptoms, or by the proportion of cases seeking hospital care after infection. However, hospitalization data remains very limited at this time,” the researchers said.
“We have no evidence that the virus itself is more mild,” Eric Topol, MD, executive vice president of Scripps Research and editor-in-chief of Medscape, told PBS NewsHour. “Until we have that, we have to assume that people who don’t have any protection are highly vulnerable to getting very ill.”
The White House COVID-19 team continues to urge parents and guardians to get their children vaccinated, especially in anticipation of a post-holiday spike. Dr. Walensky said the CDC’s vaccine advisory board met on Dec. 16 to continue the safety discussion about COVID-19 vaccinations in children.
So far, 20 million children under 17 and 5 million under 11 have received their shots.
“Looking specifically at vaccine safety data from over 50,000 children 5-11 years old, we found no evidence of serious safety concerns,” Dr. Walensky said.
Top infectious disease expert Anthony S. Fauci, MD, highlighted the importance of getting vaccinated and boosted to avoid serious disease from Delta and Omicron.
“We’re in a situation where we are now facing a very important Delta surge and we are looking over our shoulder at an oncoming Omicron surge,” he said. “The optimum protection is fully vaccinated plus a boost.”
A version of this article first appeared on WebMD.com.
The best way to stay protected is by getting vaccinated and boosted, they said.
“For the unvaccinated, you’re looking at a winter of severe illness and death – for yourselves, families, and the hospitals who may soon overwhelm,” White House COVID-19 Response Coordinator Jeff Zients said at a news briefing Dec. 17. “We need the American people to do their part.”
The Omicron variant has been detected in at least 39 states and 75 countries, according to CDC director Rochelle Walensky, MD.
The strain is more transmissible than the already highly infectious Delta variant, and although there was early evidence that it caused more mild disease, she said that is likely because many of those infected have been vaccinated and boosted.
“Although Delta continues to circulate widely in the United States, Omicron is increasing rapidly and we expect it to become the dominant strain in the United States, as it has in other countries, in the coming weeks,” Dr. Walensky said.
The United States is averaging close to 1,300 deaths from COVID-19 each day. New cases, deaths, and hospitalizations are higher now than in the previous winter – before vaccines were so widely available. The New York Times reported on Dec. 17 that new infections in Connecticut and Maine have grown 150% in the past 2 weeks, and Ohio and Indiana are seeing hospitalization rates nearing the worst of 2020-2021’s winter surge.
Dueling reports released recently gave cause for relief and concern about Omicron.
A study from South Africa released on Dec. 14 shows lower hospitalizations during the first 3 weeks of the Omicron wave than during earlier waves from other variants. That’s the good news.
The concerning news is out of the United Kingdom, where Imperial College London reported Dec. 17 that the risk of reinfection with COVID-19 from Omicron is more than 5 times as high and that cases of Omicron-based COVID-19 are doubling every 2 days.
What’s more, the study “finds no evidence of Omicron having lower severity than Delta, judged by either the proportion of people testing positive who report symptoms, or by the proportion of cases seeking hospital care after infection. However, hospitalization data remains very limited at this time,” the researchers said.
“We have no evidence that the virus itself is more mild,” Eric Topol, MD, executive vice president of Scripps Research and editor-in-chief of Medscape, told PBS NewsHour. “Until we have that, we have to assume that people who don’t have any protection are highly vulnerable to getting very ill.”
The White House COVID-19 team continues to urge parents and guardians to get their children vaccinated, especially in anticipation of a post-holiday spike. Dr. Walensky said the CDC’s vaccine advisory board met on Dec. 16 to continue the safety discussion about COVID-19 vaccinations in children.
So far, 20 million children under 17 and 5 million under 11 have received their shots.
“Looking specifically at vaccine safety data from over 50,000 children 5-11 years old, we found no evidence of serious safety concerns,” Dr. Walensky said.
Top infectious disease expert Anthony S. Fauci, MD, highlighted the importance of getting vaccinated and boosted to avoid serious disease from Delta and Omicron.
“We’re in a situation where we are now facing a very important Delta surge and we are looking over our shoulder at an oncoming Omicron surge,” he said. “The optimum protection is fully vaccinated plus a boost.”
A version of this article first appeared on WebMD.com.
The best way to stay protected is by getting vaccinated and boosted, they said.
“For the unvaccinated, you’re looking at a winter of severe illness and death – for yourselves, families, and the hospitals who may soon overwhelm,” White House COVID-19 Response Coordinator Jeff Zients said at a news briefing Dec. 17. “We need the American people to do their part.”
The Omicron variant has been detected in at least 39 states and 75 countries, according to CDC director Rochelle Walensky, MD.
The strain is more transmissible than the already highly infectious Delta variant, and although there was early evidence that it caused more mild disease, she said that is likely because many of those infected have been vaccinated and boosted.
“Although Delta continues to circulate widely in the United States, Omicron is increasing rapidly and we expect it to become the dominant strain in the United States, as it has in other countries, in the coming weeks,” Dr. Walensky said.
The United States is averaging close to 1,300 deaths from COVID-19 each day. New cases, deaths, and hospitalizations are higher now than in the previous winter – before vaccines were so widely available. The New York Times reported on Dec. 17 that new infections in Connecticut and Maine have grown 150% in the past 2 weeks, and Ohio and Indiana are seeing hospitalization rates nearing the worst of 2020-2021’s winter surge.
Dueling reports released recently gave cause for relief and concern about Omicron.
A study from South Africa released on Dec. 14 shows lower hospitalizations during the first 3 weeks of the Omicron wave than during earlier waves from other variants. That’s the good news.
The concerning news is out of the United Kingdom, where Imperial College London reported Dec. 17 that the risk of reinfection with COVID-19 from Omicron is more than 5 times as high and that cases of Omicron-based COVID-19 are doubling every 2 days.
What’s more, the study “finds no evidence of Omicron having lower severity than Delta, judged by either the proportion of people testing positive who report symptoms, or by the proportion of cases seeking hospital care after infection. However, hospitalization data remains very limited at this time,” the researchers said.
“We have no evidence that the virus itself is more mild,” Eric Topol, MD, executive vice president of Scripps Research and editor-in-chief of Medscape, told PBS NewsHour. “Until we have that, we have to assume that people who don’t have any protection are highly vulnerable to getting very ill.”
The White House COVID-19 team continues to urge parents and guardians to get their children vaccinated, especially in anticipation of a post-holiday spike. Dr. Walensky said the CDC’s vaccine advisory board met on Dec. 16 to continue the safety discussion about COVID-19 vaccinations in children.
So far, 20 million children under 17 and 5 million under 11 have received their shots.
“Looking specifically at vaccine safety data from over 50,000 children 5-11 years old, we found no evidence of serious safety concerns,” Dr. Walensky said.
Top infectious disease expert Anthony S. Fauci, MD, highlighted the importance of getting vaccinated and boosted to avoid serious disease from Delta and Omicron.
“We’re in a situation where we are now facing a very important Delta surge and we are looking over our shoulder at an oncoming Omicron surge,” he said. “The optimum protection is fully vaccinated plus a boost.”
A version of this article first appeared on WebMD.com.
HIV: FDA stops all islatravir oral and implant trials
, the investigational drug’s developer, Merck, announced in a press release.
Investigational new drug applications were halted for the oral and implant formulations of islatravir, a nucleoside reverse transcriptase translocation inhibitor, for pre-exposure prophylaxis (PrEP); the injectable formulation of islatravir for treatment and prophylaxis; and the oral doravirine/islatravir (DOR/ISL) once-daily treatment, the company announced.
The FDA’s hold followed observations that total lymphocyte and T-cell counts had dropped in some participants receiving islatravir in clinical studies.
The trials have dealt a major setback to Merck’s HIV program momentum: Thirteen trials are now on hold (six on partial hold and seven on full hold). Seven of the trials were in phase 3. But primarily the news is disappointing for patients looking for options with the confounding disease.
Tristan Barber, MD, an HIV consultant with Royal Free London National Health Service Foundation Trust, told this news organization that “the hold on these studies is a blow for those hoping for longer-acting therapies for HIV treatment and prevention. Islatravir and [investigational drug] MK-8507 were being explored in oral and other formulations and potentially would offer a non-integrase, two-drug option, increasing options for people with HIV. Whilst we don’t know the clinical significance of these CD4 drops, [Merck] made the correct decision in pausing these studies until the data is clearer.”
Merck announced in November that it had stopped dosing in the phase 2 IMAGINE-DR clinical trial of islatravir in combination with MK-8507. MK-8507 and islatravir, alone and combined, are investigational and not approved for use.
In that trial as well, decreases were observed in total lymphocyte and T-cell counts in study participants randomly assigned to receive the combination. A review by the external Data Monitoring Committee determined that the drop was related to treatment with the combination.
“We are grateful to the participants and the study investigators for their ongoing contributions to this research,” Joan Butterton, MD, vice president of infectious diseases in Global Clinical Development at Merck Research Laboratories, said in a statement. “Merck continues to investigate the potential of islatravir and nucleoside reverse transcriptase translocation inhibitors and remains committed to helping to address unmet needs in HIV treatment and prevention.”
In light of the hold, no new studies using islatravir may be initiated. People currently receiving islatravir as part of the studies for PrEP, as well as injectable islatravir for treatment and prophylaxis, will no longer receive the study drug, and T-cell and lymphocyte counts will be monitored for recovery.
Those participating in the PrEP studies will be offered approved, once-daily, oral PrEP and those in studies of DOR/ISL who already started treatment will continue to receive study medication under a partial clinical hold.
A full list of the trials that have been placed on full or partial clinical holds can be found in the press release.
In an interview with this news organization, Monica Gandhi, MD, MPH, director of University of California, San Francisco’s Gladstone Center for AIDS Research, described the news of the islatravir trial holds as “very disappointing.”
“There were high hopes for this drug,” she said, adding that the hope was it would be paired with Gilead’s lenacapavir (another long-acting agent) for treatment and be able to give a once-weekly option for HIV treatment.
Lenacapavir is Gilead’s potential first-in-class, long-acting HIV-1 capsid inhibitor in development for treatment and prevention of HIV.
“Moreover,” she said, “additional hope was that, because of [islatravir’s] long half-life, it could be used as a monthly medication for pre-exposure prophylaxis.”
Gilead and Merck have decided to stop all dosing of participants in the phase 2 clinical trial evaluating an oral, weekly combination treatment of islatravir and lenacapavir in people living with HIV who are virologically suppressed on antiretroviral therapy, according to Merck’s press release.
Participants in that trial will stop taking the study drug and restart their previous antiretroviral regimen. According to the press release, both companies are considering whether a different dosing of islatravir combined with lenacapavir may become a once-weekly oral therapy option for people living with HIV.
Neither Merck nor Gilead representatives responded to request for comment by publication time.
Dr. Barber reported conference support, speaker fees, and advisory board honoraria from Gilead, Janssen, Merck, Roche, Thera, and ViiV and research/educational grants from Gilead, Roche, and ViiV. Dr. Gandhi has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, the investigational drug’s developer, Merck, announced in a press release.
Investigational new drug applications were halted for the oral and implant formulations of islatravir, a nucleoside reverse transcriptase translocation inhibitor, for pre-exposure prophylaxis (PrEP); the injectable formulation of islatravir for treatment and prophylaxis; and the oral doravirine/islatravir (DOR/ISL) once-daily treatment, the company announced.
The FDA’s hold followed observations that total lymphocyte and T-cell counts had dropped in some participants receiving islatravir in clinical studies.
The trials have dealt a major setback to Merck’s HIV program momentum: Thirteen trials are now on hold (six on partial hold and seven on full hold). Seven of the trials were in phase 3. But primarily the news is disappointing for patients looking for options with the confounding disease.
Tristan Barber, MD, an HIV consultant with Royal Free London National Health Service Foundation Trust, told this news organization that “the hold on these studies is a blow for those hoping for longer-acting therapies for HIV treatment and prevention. Islatravir and [investigational drug] MK-8507 were being explored in oral and other formulations and potentially would offer a non-integrase, two-drug option, increasing options for people with HIV. Whilst we don’t know the clinical significance of these CD4 drops, [Merck] made the correct decision in pausing these studies until the data is clearer.”
Merck announced in November that it had stopped dosing in the phase 2 IMAGINE-DR clinical trial of islatravir in combination with MK-8507. MK-8507 and islatravir, alone and combined, are investigational and not approved for use.
In that trial as well, decreases were observed in total lymphocyte and T-cell counts in study participants randomly assigned to receive the combination. A review by the external Data Monitoring Committee determined that the drop was related to treatment with the combination.
“We are grateful to the participants and the study investigators for their ongoing contributions to this research,” Joan Butterton, MD, vice president of infectious diseases in Global Clinical Development at Merck Research Laboratories, said in a statement. “Merck continues to investigate the potential of islatravir and nucleoside reverse transcriptase translocation inhibitors and remains committed to helping to address unmet needs in HIV treatment and prevention.”
In light of the hold, no new studies using islatravir may be initiated. People currently receiving islatravir as part of the studies for PrEP, as well as injectable islatravir for treatment and prophylaxis, will no longer receive the study drug, and T-cell and lymphocyte counts will be monitored for recovery.
Those participating in the PrEP studies will be offered approved, once-daily, oral PrEP and those in studies of DOR/ISL who already started treatment will continue to receive study medication under a partial clinical hold.
A full list of the trials that have been placed on full or partial clinical holds can be found in the press release.
In an interview with this news organization, Monica Gandhi, MD, MPH, director of University of California, San Francisco’s Gladstone Center for AIDS Research, described the news of the islatravir trial holds as “very disappointing.”
“There were high hopes for this drug,” she said, adding that the hope was it would be paired with Gilead’s lenacapavir (another long-acting agent) for treatment and be able to give a once-weekly option for HIV treatment.
Lenacapavir is Gilead’s potential first-in-class, long-acting HIV-1 capsid inhibitor in development for treatment and prevention of HIV.
“Moreover,” she said, “additional hope was that, because of [islatravir’s] long half-life, it could be used as a monthly medication for pre-exposure prophylaxis.”
Gilead and Merck have decided to stop all dosing of participants in the phase 2 clinical trial evaluating an oral, weekly combination treatment of islatravir and lenacapavir in people living with HIV who are virologically suppressed on antiretroviral therapy, according to Merck’s press release.
Participants in that trial will stop taking the study drug and restart their previous antiretroviral regimen. According to the press release, both companies are considering whether a different dosing of islatravir combined with lenacapavir may become a once-weekly oral therapy option for people living with HIV.
Neither Merck nor Gilead representatives responded to request for comment by publication time.
Dr. Barber reported conference support, speaker fees, and advisory board honoraria from Gilead, Janssen, Merck, Roche, Thera, and ViiV and research/educational grants from Gilead, Roche, and ViiV. Dr. Gandhi has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, the investigational drug’s developer, Merck, announced in a press release.
Investigational new drug applications were halted for the oral and implant formulations of islatravir, a nucleoside reverse transcriptase translocation inhibitor, for pre-exposure prophylaxis (PrEP); the injectable formulation of islatravir for treatment and prophylaxis; and the oral doravirine/islatravir (DOR/ISL) once-daily treatment, the company announced.
The FDA’s hold followed observations that total lymphocyte and T-cell counts had dropped in some participants receiving islatravir in clinical studies.
The trials have dealt a major setback to Merck’s HIV program momentum: Thirteen trials are now on hold (six on partial hold and seven on full hold). Seven of the trials were in phase 3. But primarily the news is disappointing for patients looking for options with the confounding disease.
Tristan Barber, MD, an HIV consultant with Royal Free London National Health Service Foundation Trust, told this news organization that “the hold on these studies is a blow for those hoping for longer-acting therapies for HIV treatment and prevention. Islatravir and [investigational drug] MK-8507 were being explored in oral and other formulations and potentially would offer a non-integrase, two-drug option, increasing options for people with HIV. Whilst we don’t know the clinical significance of these CD4 drops, [Merck] made the correct decision in pausing these studies until the data is clearer.”
Merck announced in November that it had stopped dosing in the phase 2 IMAGINE-DR clinical trial of islatravir in combination with MK-8507. MK-8507 and islatravir, alone and combined, are investigational and not approved for use.
In that trial as well, decreases were observed in total lymphocyte and T-cell counts in study participants randomly assigned to receive the combination. A review by the external Data Monitoring Committee determined that the drop was related to treatment with the combination.
“We are grateful to the participants and the study investigators for their ongoing contributions to this research,” Joan Butterton, MD, vice president of infectious diseases in Global Clinical Development at Merck Research Laboratories, said in a statement. “Merck continues to investigate the potential of islatravir and nucleoside reverse transcriptase translocation inhibitors and remains committed to helping to address unmet needs in HIV treatment and prevention.”
In light of the hold, no new studies using islatravir may be initiated. People currently receiving islatravir as part of the studies for PrEP, as well as injectable islatravir for treatment and prophylaxis, will no longer receive the study drug, and T-cell and lymphocyte counts will be monitored for recovery.
Those participating in the PrEP studies will be offered approved, once-daily, oral PrEP and those in studies of DOR/ISL who already started treatment will continue to receive study medication under a partial clinical hold.
A full list of the trials that have been placed on full or partial clinical holds can be found in the press release.
In an interview with this news organization, Monica Gandhi, MD, MPH, director of University of California, San Francisco’s Gladstone Center for AIDS Research, described the news of the islatravir trial holds as “very disappointing.”
“There were high hopes for this drug,” she said, adding that the hope was it would be paired with Gilead’s lenacapavir (another long-acting agent) for treatment and be able to give a once-weekly option for HIV treatment.
Lenacapavir is Gilead’s potential first-in-class, long-acting HIV-1 capsid inhibitor in development for treatment and prevention of HIV.
“Moreover,” she said, “additional hope was that, because of [islatravir’s] long half-life, it could be used as a monthly medication for pre-exposure prophylaxis.”
Gilead and Merck have decided to stop all dosing of participants in the phase 2 clinical trial evaluating an oral, weekly combination treatment of islatravir and lenacapavir in people living with HIV who are virologically suppressed on antiretroviral therapy, according to Merck’s press release.
Participants in that trial will stop taking the study drug and restart their previous antiretroviral regimen. According to the press release, both companies are considering whether a different dosing of islatravir combined with lenacapavir may become a once-weekly oral therapy option for people living with HIV.
Neither Merck nor Gilead representatives responded to request for comment by publication time.
Dr. Barber reported conference support, speaker fees, and advisory board honoraria from Gilead, Janssen, Merck, Roche, Thera, and ViiV and research/educational grants from Gilead, Roche, and ViiV. Dr. Gandhi has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New hepatitis B vaccination recommendations praised amid low awareness
An updated recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) calling for universal hepatitis B vaccination of all adults aged 59 and younger has boosted the call to improve clinicians’ awareness of the increasing infection and low vaccination rates – and raise the issue with patients.
“This new recommendation from [the] ACIP will be instrumental [in] raising adult hepatitis B vaccination rates in the U.S. to levels that will allow us to finally eliminate hepatitis B in this country,” said Rita K. Kuwahara, MD, a primary care internal medicine physician and health policy fellow at Georgetown University, in Washington, D.C., in addressing the issue at the U.S. Conference on HIV/AIDS (USCHA) this month.
“We have the tools to prevent hepatitis B, and since we have such safe and highly effective vaccines to protect against community [spread], we should not have a single new infection in our nation,” she asserted.
The unanimously approved updated ACIP recommendation was issued in November and still requires adoption by the CDC director. The ACIP specifically recommends that adults aged 19 to 59 and those 60 years and older with risk factors for infection “should” receive the hepatitis B vaccine, and it further stipulates that those 60 years and older without known risk factors for hepatitis B “may” receive the vaccine.
The recommendation was previously only for adults at risk for hepatitis B infection due to a variety of factors, including sexual exposure, percutaneous or mucosal exposure to blood, hepatitis C infection, chronic liver disease, end-stage renal disease, and HIV infection.
“The number of risk factors was long, and for a busy primary care provider to have to go through a lengthy risk-based protocol like that, it may not happen,” Dr. Kuwahara told this news organization.
“Now we have a really helpful new recommendation that is simply age based, and clinicians can just tell patients that if they were born before this certain period, a hepatitis B vaccination is recommended.”
The change comes amid a troubling trajectory of hepatitis B, with up to 2.4 million individuals currently having chronic hepatitis B in the U.S. and infection rates soaring by 100% to more than 400% in states with high opioid use, such as West Virginia, Kentucky, Tennessee, and Maine, Dr. Kuwahara said.
Notably, hepatitis B is the leading cause of liver disease, and one in four individuals with unmanaged chronic hepatitis B goes on to develop liver failure and/or cirrhosis or liver cancer, which has a 5-year survival rate of only 18%.
Despite the rising infection rates, only 25%-30% of adults in the U.S. are reported to be currently vaccinated for hepatitis B, even though safe and highly effective vaccines are available, notably including a new two-dose vaccine (Heplisav-B) that can be provided over just a month (vs. other hepatitis B vaccines requiring 3 doses over 6 months).
Clinician awareness of low vaccination rates lacking
Dr. Kuwahara noted that awareness among clinicians of the issues surrounding hepatitis B appears low, with one small survey that she and her colleagues conducted of 30 primary care physicians showing that not one of the respondents was aware of the low vaccination rate.
Dr. Kuwahara says a key reason for the low awareness to discuss the hepatitis B vaccination with adults is the common impression that the responsibility for the vaccination lies in the hands of pediatricians.
But that’s only half correct – universal vaccination for hepatitis B in all infants and children is indeed currently the policy in the U.S. – but that was not implemented in all states until the mid-to-late ‘90s, meaning the millions of adults over the age of about 25 to 30, born before that period, are likely not fully vaccinated against hepatitis B.
“When I was in medical school, there wasn’t a lot of discussion of how low the hepatitis B vaccination rate was because everyone knew there was universal childhood vaccination, and I think there was an assumption that it had been going on for a long time,” Dr. Kuwahara said. “So I think it’s clearly a misconception, and it’s really important to improve clinician awareness around the issue.”
Opioid use a key factor in rising infection rates
Importantly, a large proportion of opioid users are among the population of patients born before the mid-’90s – and those adults have a particularly high risk of transmission, with data indicating that 36% of new hepatitis B infections are the result of the opioid epidemic, Dr. Kuwahara noted.
“In the opioid epidemic, we have seen some of the greatest increases in acute hepatitis B presenting in adults aged 30 to 49 years old, as most adults in this age range would not have been vaccinated as children in the U.S.,” she said.
Approximately two-thirds of individuals with chronic hepatitis B are reportedly not even aware of their infection status due to ineffective prevention and vaccination programs, adding to the spread of infection, Dr. Kuwahara said.
Meanwhile, COVID-19 has only exacerbated the problem, with record-high instances of overdoses and overdose-related deaths during the pandemic, she explained.
However, the pandemic, and specifically the sweeping innovations that have been implemented in desperate efforts to bring COVID-19 vaccines to the public, could in fact represent a critical opportunity for hepatitis B prevention, Dr. Kuwahara said.
“Significant resources and federal funding have already been invested to develop a robust infrastructure for multi-dose COVID-19 vaccine administration during the pandemic, which has resulted in millions of people across the U.S. receiving the COVID-19 vaccine in easily accessible settings within their communities,” she said.
“It is essential that we expand the infrastructure development ... so that we may use this infrastructure to administer other vaccines such as the hepatitis B vaccine to adults throughout the nation and prevent additional outbreaks.”
Implementation of vaccine recommendations key
Dr. Kuwahara outlined key measures that will be important in implementing the hepatitis B vaccine recommendations:
- Awareness of the hepatitis B vaccination recommendations at the primary care level: “The first step in implementing universal [guidelines] will be to ensure that health care providers, particularly in primary care, are aware of the new ACIP guidelines so that they can speak with their patients about this and appropriately order hepatitis B testing and vaccination,” she said.
- Availability of vaccines: In addition to making sure primary care clinics are well stocked with hepatitis B vaccines, the vaccines should also be available in pharmacies and other convenient nonclinical settings through community outreach, similar to COVID-19 vaccines.
- Follow-up: Systems should be established to remind patients to receive follow-up doses.
- Public funding for vaccines: Policy changes will need to occur to allocate appropriate Section 317 funding to provide hepatitis B vaccines to adults without health insurance coverage, Dr. Kuwahara said, underscoring concerns about health equity in vaccination.
- Track vaccinations: Communication should be established between places administering vaccines and primary care providers to make sure that vaccination status can be documented in a reliable setting.
Dr. Kuwahara also noted that a federal immunization information system will be essential to track vaccines across a lifespan, providing one integrated vaccine record that can be accessed even when patients travel or move to different states.
Commenting on the issue, Frank Hood, manager of hepatitis advocacy for The AIDS Institute in Washington, D.C., added that, in addition to simplifying the process, the new age-based recommendation removes the issue of perceived judgement from the advice.
“The previous recommendations were more risk based, and patients may tend to say ‘oh, I don’t have any of those behaviors,’ and there can be some stigma,” he said. “But having something that says everyone in these age groups should be or may be vaccinated just makes it much easier and covers a greater number of individuals.”
Mr. Hood further underscored the need for continued diligence in improving measures to prevent and eradicate HBV as well as other infectious diseases.
“It is imperative that the systems being built now to respond to future infectious disease outbreaks are done so in a way to equitably support the efforts and end goal of eliminating current infectious disease epidemics like viral hepatitis and HIV,” he emphasized.“Elimination can’t be achieved if we leave people behind.”
Dr. Kuwahara and Mr. Hood had no disclosures to report.
A version of this article first appeared on Medscape.com.
An updated recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) calling for universal hepatitis B vaccination of all adults aged 59 and younger has boosted the call to improve clinicians’ awareness of the increasing infection and low vaccination rates – and raise the issue with patients.
“This new recommendation from [the] ACIP will be instrumental [in] raising adult hepatitis B vaccination rates in the U.S. to levels that will allow us to finally eliminate hepatitis B in this country,” said Rita K. Kuwahara, MD, a primary care internal medicine physician and health policy fellow at Georgetown University, in Washington, D.C., in addressing the issue at the U.S. Conference on HIV/AIDS (USCHA) this month.
“We have the tools to prevent hepatitis B, and since we have such safe and highly effective vaccines to protect against community [spread], we should not have a single new infection in our nation,” she asserted.
The unanimously approved updated ACIP recommendation was issued in November and still requires adoption by the CDC director. The ACIP specifically recommends that adults aged 19 to 59 and those 60 years and older with risk factors for infection “should” receive the hepatitis B vaccine, and it further stipulates that those 60 years and older without known risk factors for hepatitis B “may” receive the vaccine.
The recommendation was previously only for adults at risk for hepatitis B infection due to a variety of factors, including sexual exposure, percutaneous or mucosal exposure to blood, hepatitis C infection, chronic liver disease, end-stage renal disease, and HIV infection.
“The number of risk factors was long, and for a busy primary care provider to have to go through a lengthy risk-based protocol like that, it may not happen,” Dr. Kuwahara told this news organization.
“Now we have a really helpful new recommendation that is simply age based, and clinicians can just tell patients that if they were born before this certain period, a hepatitis B vaccination is recommended.”
The change comes amid a troubling trajectory of hepatitis B, with up to 2.4 million individuals currently having chronic hepatitis B in the U.S. and infection rates soaring by 100% to more than 400% in states with high opioid use, such as West Virginia, Kentucky, Tennessee, and Maine, Dr. Kuwahara said.
Notably, hepatitis B is the leading cause of liver disease, and one in four individuals with unmanaged chronic hepatitis B goes on to develop liver failure and/or cirrhosis or liver cancer, which has a 5-year survival rate of only 18%.
Despite the rising infection rates, only 25%-30% of adults in the U.S. are reported to be currently vaccinated for hepatitis B, even though safe and highly effective vaccines are available, notably including a new two-dose vaccine (Heplisav-B) that can be provided over just a month (vs. other hepatitis B vaccines requiring 3 doses over 6 months).
Clinician awareness of low vaccination rates lacking
Dr. Kuwahara noted that awareness among clinicians of the issues surrounding hepatitis B appears low, with one small survey that she and her colleagues conducted of 30 primary care physicians showing that not one of the respondents was aware of the low vaccination rate.
Dr. Kuwahara says a key reason for the low awareness to discuss the hepatitis B vaccination with adults is the common impression that the responsibility for the vaccination lies in the hands of pediatricians.
But that’s only half correct – universal vaccination for hepatitis B in all infants and children is indeed currently the policy in the U.S. – but that was not implemented in all states until the mid-to-late ‘90s, meaning the millions of adults over the age of about 25 to 30, born before that period, are likely not fully vaccinated against hepatitis B.
“When I was in medical school, there wasn’t a lot of discussion of how low the hepatitis B vaccination rate was because everyone knew there was universal childhood vaccination, and I think there was an assumption that it had been going on for a long time,” Dr. Kuwahara said. “So I think it’s clearly a misconception, and it’s really important to improve clinician awareness around the issue.”
Opioid use a key factor in rising infection rates
Importantly, a large proportion of opioid users are among the population of patients born before the mid-’90s – and those adults have a particularly high risk of transmission, with data indicating that 36% of new hepatitis B infections are the result of the opioid epidemic, Dr. Kuwahara noted.
“In the opioid epidemic, we have seen some of the greatest increases in acute hepatitis B presenting in adults aged 30 to 49 years old, as most adults in this age range would not have been vaccinated as children in the U.S.,” she said.
Approximately two-thirds of individuals with chronic hepatitis B are reportedly not even aware of their infection status due to ineffective prevention and vaccination programs, adding to the spread of infection, Dr. Kuwahara said.
Meanwhile, COVID-19 has only exacerbated the problem, with record-high instances of overdoses and overdose-related deaths during the pandemic, she explained.
However, the pandemic, and specifically the sweeping innovations that have been implemented in desperate efforts to bring COVID-19 vaccines to the public, could in fact represent a critical opportunity for hepatitis B prevention, Dr. Kuwahara said.
“Significant resources and federal funding have already been invested to develop a robust infrastructure for multi-dose COVID-19 vaccine administration during the pandemic, which has resulted in millions of people across the U.S. receiving the COVID-19 vaccine in easily accessible settings within their communities,” she said.
“It is essential that we expand the infrastructure development ... so that we may use this infrastructure to administer other vaccines such as the hepatitis B vaccine to adults throughout the nation and prevent additional outbreaks.”
Implementation of vaccine recommendations key
Dr. Kuwahara outlined key measures that will be important in implementing the hepatitis B vaccine recommendations:
- Awareness of the hepatitis B vaccination recommendations at the primary care level: “The first step in implementing universal [guidelines] will be to ensure that health care providers, particularly in primary care, are aware of the new ACIP guidelines so that they can speak with their patients about this and appropriately order hepatitis B testing and vaccination,” she said.
- Availability of vaccines: In addition to making sure primary care clinics are well stocked with hepatitis B vaccines, the vaccines should also be available in pharmacies and other convenient nonclinical settings through community outreach, similar to COVID-19 vaccines.
- Follow-up: Systems should be established to remind patients to receive follow-up doses.
- Public funding for vaccines: Policy changes will need to occur to allocate appropriate Section 317 funding to provide hepatitis B vaccines to adults without health insurance coverage, Dr. Kuwahara said, underscoring concerns about health equity in vaccination.
- Track vaccinations: Communication should be established between places administering vaccines and primary care providers to make sure that vaccination status can be documented in a reliable setting.
Dr. Kuwahara also noted that a federal immunization information system will be essential to track vaccines across a lifespan, providing one integrated vaccine record that can be accessed even when patients travel or move to different states.
Commenting on the issue, Frank Hood, manager of hepatitis advocacy for The AIDS Institute in Washington, D.C., added that, in addition to simplifying the process, the new age-based recommendation removes the issue of perceived judgement from the advice.
“The previous recommendations were more risk based, and patients may tend to say ‘oh, I don’t have any of those behaviors,’ and there can be some stigma,” he said. “But having something that says everyone in these age groups should be or may be vaccinated just makes it much easier and covers a greater number of individuals.”
Mr. Hood further underscored the need for continued diligence in improving measures to prevent and eradicate HBV as well as other infectious diseases.
“It is imperative that the systems being built now to respond to future infectious disease outbreaks are done so in a way to equitably support the efforts and end goal of eliminating current infectious disease epidemics like viral hepatitis and HIV,” he emphasized.“Elimination can’t be achieved if we leave people behind.”
Dr. Kuwahara and Mr. Hood had no disclosures to report.
A version of this article first appeared on Medscape.com.
An updated recommendation from the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) calling for universal hepatitis B vaccination of all adults aged 59 and younger has boosted the call to improve clinicians’ awareness of the increasing infection and low vaccination rates – and raise the issue with patients.
“This new recommendation from [the] ACIP will be instrumental [in] raising adult hepatitis B vaccination rates in the U.S. to levels that will allow us to finally eliminate hepatitis B in this country,” said Rita K. Kuwahara, MD, a primary care internal medicine physician and health policy fellow at Georgetown University, in Washington, D.C., in addressing the issue at the U.S. Conference on HIV/AIDS (USCHA) this month.
“We have the tools to prevent hepatitis B, and since we have such safe and highly effective vaccines to protect against community [spread], we should not have a single new infection in our nation,” she asserted.
The unanimously approved updated ACIP recommendation was issued in November and still requires adoption by the CDC director. The ACIP specifically recommends that adults aged 19 to 59 and those 60 years and older with risk factors for infection “should” receive the hepatitis B vaccine, and it further stipulates that those 60 years and older without known risk factors for hepatitis B “may” receive the vaccine.
The recommendation was previously only for adults at risk for hepatitis B infection due to a variety of factors, including sexual exposure, percutaneous or mucosal exposure to blood, hepatitis C infection, chronic liver disease, end-stage renal disease, and HIV infection.
“The number of risk factors was long, and for a busy primary care provider to have to go through a lengthy risk-based protocol like that, it may not happen,” Dr. Kuwahara told this news organization.
“Now we have a really helpful new recommendation that is simply age based, and clinicians can just tell patients that if they were born before this certain period, a hepatitis B vaccination is recommended.”
The change comes amid a troubling trajectory of hepatitis B, with up to 2.4 million individuals currently having chronic hepatitis B in the U.S. and infection rates soaring by 100% to more than 400% in states with high opioid use, such as West Virginia, Kentucky, Tennessee, and Maine, Dr. Kuwahara said.
Notably, hepatitis B is the leading cause of liver disease, and one in four individuals with unmanaged chronic hepatitis B goes on to develop liver failure and/or cirrhosis or liver cancer, which has a 5-year survival rate of only 18%.
Despite the rising infection rates, only 25%-30% of adults in the U.S. are reported to be currently vaccinated for hepatitis B, even though safe and highly effective vaccines are available, notably including a new two-dose vaccine (Heplisav-B) that can be provided over just a month (vs. other hepatitis B vaccines requiring 3 doses over 6 months).
Clinician awareness of low vaccination rates lacking
Dr. Kuwahara noted that awareness among clinicians of the issues surrounding hepatitis B appears low, with one small survey that she and her colleagues conducted of 30 primary care physicians showing that not one of the respondents was aware of the low vaccination rate.
Dr. Kuwahara says a key reason for the low awareness to discuss the hepatitis B vaccination with adults is the common impression that the responsibility for the vaccination lies in the hands of pediatricians.
But that’s only half correct – universal vaccination for hepatitis B in all infants and children is indeed currently the policy in the U.S. – but that was not implemented in all states until the mid-to-late ‘90s, meaning the millions of adults over the age of about 25 to 30, born before that period, are likely not fully vaccinated against hepatitis B.
“When I was in medical school, there wasn’t a lot of discussion of how low the hepatitis B vaccination rate was because everyone knew there was universal childhood vaccination, and I think there was an assumption that it had been going on for a long time,” Dr. Kuwahara said. “So I think it’s clearly a misconception, and it’s really important to improve clinician awareness around the issue.”
Opioid use a key factor in rising infection rates
Importantly, a large proportion of opioid users are among the population of patients born before the mid-’90s – and those adults have a particularly high risk of transmission, with data indicating that 36% of new hepatitis B infections are the result of the opioid epidemic, Dr. Kuwahara noted.
“In the opioid epidemic, we have seen some of the greatest increases in acute hepatitis B presenting in adults aged 30 to 49 years old, as most adults in this age range would not have been vaccinated as children in the U.S.,” she said.
Approximately two-thirds of individuals with chronic hepatitis B are reportedly not even aware of their infection status due to ineffective prevention and vaccination programs, adding to the spread of infection, Dr. Kuwahara said.
Meanwhile, COVID-19 has only exacerbated the problem, with record-high instances of overdoses and overdose-related deaths during the pandemic, she explained.
However, the pandemic, and specifically the sweeping innovations that have been implemented in desperate efforts to bring COVID-19 vaccines to the public, could in fact represent a critical opportunity for hepatitis B prevention, Dr. Kuwahara said.
“Significant resources and federal funding have already been invested to develop a robust infrastructure for multi-dose COVID-19 vaccine administration during the pandemic, which has resulted in millions of people across the U.S. receiving the COVID-19 vaccine in easily accessible settings within their communities,” she said.
“It is essential that we expand the infrastructure development ... so that we may use this infrastructure to administer other vaccines such as the hepatitis B vaccine to adults throughout the nation and prevent additional outbreaks.”
Implementation of vaccine recommendations key
Dr. Kuwahara outlined key measures that will be important in implementing the hepatitis B vaccine recommendations:
- Awareness of the hepatitis B vaccination recommendations at the primary care level: “The first step in implementing universal [guidelines] will be to ensure that health care providers, particularly in primary care, are aware of the new ACIP guidelines so that they can speak with their patients about this and appropriately order hepatitis B testing and vaccination,” she said.
- Availability of vaccines: In addition to making sure primary care clinics are well stocked with hepatitis B vaccines, the vaccines should also be available in pharmacies and other convenient nonclinical settings through community outreach, similar to COVID-19 vaccines.
- Follow-up: Systems should be established to remind patients to receive follow-up doses.
- Public funding for vaccines: Policy changes will need to occur to allocate appropriate Section 317 funding to provide hepatitis B vaccines to adults without health insurance coverage, Dr. Kuwahara said, underscoring concerns about health equity in vaccination.
- Track vaccinations: Communication should be established between places administering vaccines and primary care providers to make sure that vaccination status can be documented in a reliable setting.
Dr. Kuwahara also noted that a federal immunization information system will be essential to track vaccines across a lifespan, providing one integrated vaccine record that can be accessed even when patients travel or move to different states.
Commenting on the issue, Frank Hood, manager of hepatitis advocacy for The AIDS Institute in Washington, D.C., added that, in addition to simplifying the process, the new age-based recommendation removes the issue of perceived judgement from the advice.
“The previous recommendations were more risk based, and patients may tend to say ‘oh, I don’t have any of those behaviors,’ and there can be some stigma,” he said. “But having something that says everyone in these age groups should be or may be vaccinated just makes it much easier and covers a greater number of individuals.”
Mr. Hood further underscored the need for continued diligence in improving measures to prevent and eradicate HBV as well as other infectious diseases.
“It is imperative that the systems being built now to respond to future infectious disease outbreaks are done so in a way to equitably support the efforts and end goal of eliminating current infectious disease epidemics like viral hepatitis and HIV,” he emphasized.“Elimination can’t be achieved if we leave people behind.”
Dr. Kuwahara and Mr. Hood had no disclosures to report.
A version of this article first appeared on Medscape.com.
COVID-19 interrupted global poliovirus surveillance and immunization
Most (86%) of these outbreaks were caused by cVDPV2 (circulating VDPV type 2 poliovirus, which originated with the vaccine), and most occurred in Africa, according to a new study of vaccine-derived poliovirus outbreaks between Jan. 2020 and June 2021 published in the CDC’s Morbidity and Mortality Weekly Report.
The Global Polio Eradication Initiative (GPEI) was launched in 1988 and used live attenuated oral poliovirus vaccine (OPV). Since then, cases of wild poliovirus have declined more than 99.99%.
The cVDPV2 likely originated among children born in areas with poor vaccine coverage. Jay Wenger, MD, director, Polio, at the Bill and Melinda Gates Foundation, told this news organization that “the inactivated vaccines that we give in most developed countries now are good in that they provide humoral immunity, the antibodies in the bloodstream. They don’t necessarily provide mucosal immunity. They don’t make the kid’s gut immune to getting reinfected or actually immune to reproducing the virus if they get it in their gut. So we could still have a situation where everybody was vaccinated with IPV [inactivated poliovirus], but the virus could still be transmitting around because kids’ guts would still be producing the virus and there will still be transmission in your population, probably without much or any paralysis because of the IPV. As soon as that virus hit a population that was not vaccinated, they would get paralyzed.”
Dr. Wenger added, “The ideal vaccine would be an oral vaccine that didn’t mutate back and couldn’t cause these VDPVs.” Scientists developed such a vaccine, approved by the World Health Organization last year under an Emergency Use Authorization. This nOPV2 (novel oral poliovirus type 2) vaccine has been given since March 2021 in areas with the VDPD2 outbreaks. The nOPV2 should allow them to “basically stamp out the outbreaks.”
The world had almost eradicated the disease, with the last cases of polio from wild virus occurring in Nigeria, Afghanistan, and Pakistan as of 2014. Africa was declared free of wild polio in 2020 after it had been eradicated from Nigeria, which accounted for more than half of the world’s cases only a decade earlier. Now cVDPV outbreaks affect 28 African countries, plus Iran, Yemen, Afghanistan, Pakistan, Tajikistan, Malaysia, the Philippines, and Indonesia. And there was also one case in China. Globally, there were 1,335 cases of cVDPV causing paralysis during the reporting period.
The COVID-19 pandemic has had a significant impact on polio, accounting for much of this year’s increase in cases. Dr. Wenger said, “We couldn’t do any campaigns. We pretty much stopped doing outbreak response campaigns in the middle of the year because of COVID.”
The CDC report notes that many of the supplementary immunizations in response to cVDPV2 outbreaks were of “poor quality,” and prolonged delays enabled geographically expanding cVDPV2 transmission.
Steve Wassilak, MD, chief coauthor of the CDC study, told this news organization that, because of COVID, “what we’ve been lacking is a rapid response for the most part. Some of that is due to laboratory delays and shipment because of COVID’s effect on international travel.” He noted, however, that there has been good recovery in surveillance and immunization activities despite COVID. And, he added, eradication “can be done, and many outbreaks have closed even during the [COVID] outbreak.”
Dr. Wassilak said that in Nigeria, “the face of the campaign became national.” In Pakistan, much of the work is done by national and international partners.
Dr. Wenger said that in Nigeria and other challenging areas, “the approach was essentially to make direct contact with the traditional leaders and the religious leaders and the local actors in each of these populations. So, it’s really getting down to the grassroots level.” Infectious disease officials send teams to speak with individuals in the “local, traditional leader system.”
“Just talking to them actually got us a long way and giving them the information that they need. In most cases, I mean, people want to do things to help their kids,” said Dr. Wenger.
For now, the initial plan, per the CDC, is to “initiate prompt and high coverage outbreak responses with available type 2 OPV to interrupt transmission” until a better supply of nOPV2 is available, then switch to IPVs.
Dr. Wenger and Dr. Wassilak report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most (86%) of these outbreaks were caused by cVDPV2 (circulating VDPV type 2 poliovirus, which originated with the vaccine), and most occurred in Africa, according to a new study of vaccine-derived poliovirus outbreaks between Jan. 2020 and June 2021 published in the CDC’s Morbidity and Mortality Weekly Report.
The Global Polio Eradication Initiative (GPEI) was launched in 1988 and used live attenuated oral poliovirus vaccine (OPV). Since then, cases of wild poliovirus have declined more than 99.99%.
The cVDPV2 likely originated among children born in areas with poor vaccine coverage. Jay Wenger, MD, director, Polio, at the Bill and Melinda Gates Foundation, told this news organization that “the inactivated vaccines that we give in most developed countries now are good in that they provide humoral immunity, the antibodies in the bloodstream. They don’t necessarily provide mucosal immunity. They don’t make the kid’s gut immune to getting reinfected or actually immune to reproducing the virus if they get it in their gut. So we could still have a situation where everybody was vaccinated with IPV [inactivated poliovirus], but the virus could still be transmitting around because kids’ guts would still be producing the virus and there will still be transmission in your population, probably without much or any paralysis because of the IPV. As soon as that virus hit a population that was not vaccinated, they would get paralyzed.”
Dr. Wenger added, “The ideal vaccine would be an oral vaccine that didn’t mutate back and couldn’t cause these VDPVs.” Scientists developed such a vaccine, approved by the World Health Organization last year under an Emergency Use Authorization. This nOPV2 (novel oral poliovirus type 2) vaccine has been given since March 2021 in areas with the VDPD2 outbreaks. The nOPV2 should allow them to “basically stamp out the outbreaks.”
The world had almost eradicated the disease, with the last cases of polio from wild virus occurring in Nigeria, Afghanistan, and Pakistan as of 2014. Africa was declared free of wild polio in 2020 after it had been eradicated from Nigeria, which accounted for more than half of the world’s cases only a decade earlier. Now cVDPV outbreaks affect 28 African countries, plus Iran, Yemen, Afghanistan, Pakistan, Tajikistan, Malaysia, the Philippines, and Indonesia. And there was also one case in China. Globally, there were 1,335 cases of cVDPV causing paralysis during the reporting period.
The COVID-19 pandemic has had a significant impact on polio, accounting for much of this year’s increase in cases. Dr. Wenger said, “We couldn’t do any campaigns. We pretty much stopped doing outbreak response campaigns in the middle of the year because of COVID.”
The CDC report notes that many of the supplementary immunizations in response to cVDPV2 outbreaks were of “poor quality,” and prolonged delays enabled geographically expanding cVDPV2 transmission.
Steve Wassilak, MD, chief coauthor of the CDC study, told this news organization that, because of COVID, “what we’ve been lacking is a rapid response for the most part. Some of that is due to laboratory delays and shipment because of COVID’s effect on international travel.” He noted, however, that there has been good recovery in surveillance and immunization activities despite COVID. And, he added, eradication “can be done, and many outbreaks have closed even during the [COVID] outbreak.”
Dr. Wassilak said that in Nigeria, “the face of the campaign became national.” In Pakistan, much of the work is done by national and international partners.
Dr. Wenger said that in Nigeria and other challenging areas, “the approach was essentially to make direct contact with the traditional leaders and the religious leaders and the local actors in each of these populations. So, it’s really getting down to the grassroots level.” Infectious disease officials send teams to speak with individuals in the “local, traditional leader system.”
“Just talking to them actually got us a long way and giving them the information that they need. In most cases, I mean, people want to do things to help their kids,” said Dr. Wenger.
For now, the initial plan, per the CDC, is to “initiate prompt and high coverage outbreak responses with available type 2 OPV to interrupt transmission” until a better supply of nOPV2 is available, then switch to IPVs.
Dr. Wenger and Dr. Wassilak report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most (86%) of these outbreaks were caused by cVDPV2 (circulating VDPV type 2 poliovirus, which originated with the vaccine), and most occurred in Africa, according to a new study of vaccine-derived poliovirus outbreaks between Jan. 2020 and June 2021 published in the CDC’s Morbidity and Mortality Weekly Report.
The Global Polio Eradication Initiative (GPEI) was launched in 1988 and used live attenuated oral poliovirus vaccine (OPV). Since then, cases of wild poliovirus have declined more than 99.99%.
The cVDPV2 likely originated among children born in areas with poor vaccine coverage. Jay Wenger, MD, director, Polio, at the Bill and Melinda Gates Foundation, told this news organization that “the inactivated vaccines that we give in most developed countries now are good in that they provide humoral immunity, the antibodies in the bloodstream. They don’t necessarily provide mucosal immunity. They don’t make the kid’s gut immune to getting reinfected or actually immune to reproducing the virus if they get it in their gut. So we could still have a situation where everybody was vaccinated with IPV [inactivated poliovirus], but the virus could still be transmitting around because kids’ guts would still be producing the virus and there will still be transmission in your population, probably without much or any paralysis because of the IPV. As soon as that virus hit a population that was not vaccinated, they would get paralyzed.”
Dr. Wenger added, “The ideal vaccine would be an oral vaccine that didn’t mutate back and couldn’t cause these VDPVs.” Scientists developed such a vaccine, approved by the World Health Organization last year under an Emergency Use Authorization. This nOPV2 (novel oral poliovirus type 2) vaccine has been given since March 2021 in areas with the VDPD2 outbreaks. The nOPV2 should allow them to “basically stamp out the outbreaks.”
The world had almost eradicated the disease, with the last cases of polio from wild virus occurring in Nigeria, Afghanistan, and Pakistan as of 2014. Africa was declared free of wild polio in 2020 after it had been eradicated from Nigeria, which accounted for more than half of the world’s cases only a decade earlier. Now cVDPV outbreaks affect 28 African countries, plus Iran, Yemen, Afghanistan, Pakistan, Tajikistan, Malaysia, the Philippines, and Indonesia. And there was also one case in China. Globally, there were 1,335 cases of cVDPV causing paralysis during the reporting period.
The COVID-19 pandemic has had a significant impact on polio, accounting for much of this year’s increase in cases. Dr. Wenger said, “We couldn’t do any campaigns. We pretty much stopped doing outbreak response campaigns in the middle of the year because of COVID.”
The CDC report notes that many of the supplementary immunizations in response to cVDPV2 outbreaks were of “poor quality,” and prolonged delays enabled geographically expanding cVDPV2 transmission.
Steve Wassilak, MD, chief coauthor of the CDC study, told this news organization that, because of COVID, “what we’ve been lacking is a rapid response for the most part. Some of that is due to laboratory delays and shipment because of COVID’s effect on international travel.” He noted, however, that there has been good recovery in surveillance and immunization activities despite COVID. And, he added, eradication “can be done, and many outbreaks have closed even during the [COVID] outbreak.”
Dr. Wassilak said that in Nigeria, “the face of the campaign became national.” In Pakistan, much of the work is done by national and international partners.
Dr. Wenger said that in Nigeria and other challenging areas, “the approach was essentially to make direct contact with the traditional leaders and the religious leaders and the local actors in each of these populations. So, it’s really getting down to the grassroots level.” Infectious disease officials send teams to speak with individuals in the “local, traditional leader system.”
“Just talking to them actually got us a long way and giving them the information that they need. In most cases, I mean, people want to do things to help their kids,” said Dr. Wenger.
For now, the initial plan, per the CDC, is to “initiate prompt and high coverage outbreak responses with available type 2 OPV to interrupt transmission” until a better supply of nOPV2 is available, then switch to IPVs.
Dr. Wenger and Dr. Wassilak report no relevant financial relationships.
A version of this article first appeared on Medscape.com.