User login
Using Computed Tomography to Assess Proximal Humerus Fractures
Transcranial ultrasound method outdoes echocardiography for finding PFO
SAN DIEGO – Transcranial Doppler saline studies were superior to transesophageal echocardiography in diagnosing a hole in the heart, according to a prospective study of patients who had a cryptogenic stroke.
Researchers analyzed data from 340 patients with cryptogenic stroke suspected of paradoxical embolism who had had their right-left shunt confirmed with transcranial Doppler saline study (TCDSS). Transesophageal echocardiography (TEE) failed to show a shunt such as patent foramen ovale (PFO) in 15% of the cases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. J. David Spence, Robarts Research Institute
"I was surprised by the number," said Dr. J. David Spence, senior researcher of the study, who presented the findings at the International Stroke Conference, sponsored by the American Heart Association. "I had realized that some of the patients with shunts were missed by TEE, ... but I was surprised by how often that happened."
Nearly a quarter of the population has a PFO, and 4.0%-5.5% of strokes are due to paradoxical embolism through a right-left shunt. But patching the shunts isn’t the simple answer, because the procedure is not without complications, and so far, the studies haven’t been able to make a strong case for the procedure.
TCDSS is an ultrasound method in which 1 mL of tiny bubbles is injected into the vein and if detected in the brain, could give clues to a right-left shunt. The method is safer, the equipment is cheaper, and the training is faster than for TEE, Dr. Spence said.
He added that one reason that TCDSS may be more sensitive than TEE is that sedation for TEE may prevent an adequate Valsalva maneuver. He also showed in a video that detecting the bubbles in TCDSS is rather straightforward.
Given the findings of his study, Dr. Spence said that there’s a need to identify which PFO patients are more likely to have paradoxical embolism and are more likely to respond to patching.
One solution is paying attention to the clinical clues of paradoxical embolism (J. Neurol. Sci. 2008;275:121-7). And Dr. Spence’s recent findings may add another tool to help with this prediction.
Aside from the superiority of TCDSS to TEE in identifying PFO, Dr. Spence and his colleagues found that TCDSS was also better for risk stratification of PFOs. The analysis found that 25% of the shunts that were missed on TEE were high-grade shunts (Spencer grade 3 or higher). Patients with a shunt grade of 3 or higher were significantly more likely to have a stroke or transient ischemic attack in the 4-year follow-up period (P = .028), said Dr. Spence, director of the Stroke Prevention & Atherosclerosis Research Centre at the University of Western Ontario, London. This was not predicted by the presence of shunt on TEE, nor was it predicted by mobile atrial septum or septal aneurysm. TEE missed nearly 46% of grade 1 shunts, 32% of grade 2, 13% of grade 3, 7% of grade 4, and almost 5% of grade 5.
"This doesn’t mean that everyone should go pack up their TEE machines, because we still need it for diagnosis of other cardioembolism," said Dr. Spence. "But these techniques can be complementary."
He added that it’s too soon to use these findings as grounds for change in clinical practice, and there’s a need for further studies such as randomized trials.
The majority (62%) of the study’s 340 patients were female. The patients had a mean age of 53 years and underwent follow-up for a median of 420 days. All the patients, who visited the center between 2000 and 2013, had cryptogenic stroke and were suspected of having paradoxical embolism. A total of 280 cases had TEE data available.
Dr. Spence said he had no disclosures relevant to the study.
On Twitter @naseemsmiller
SAN DIEGO – Transcranial Doppler saline studies were superior to transesophageal echocardiography in diagnosing a hole in the heart, according to a prospective study of patients who had a cryptogenic stroke.
Researchers analyzed data from 340 patients with cryptogenic stroke suspected of paradoxical embolism who had had their right-left shunt confirmed with transcranial Doppler saline study (TCDSS). Transesophageal echocardiography (TEE) failed to show a shunt such as patent foramen ovale (PFO) in 15% of the cases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. J. David Spence, Robarts Research Institute
"I was surprised by the number," said Dr. J. David Spence, senior researcher of the study, who presented the findings at the International Stroke Conference, sponsored by the American Heart Association. "I had realized that some of the patients with shunts were missed by TEE, ... but I was surprised by how often that happened."
Nearly a quarter of the population has a PFO, and 4.0%-5.5% of strokes are due to paradoxical embolism through a right-left shunt. But patching the shunts isn’t the simple answer, because the procedure is not without complications, and so far, the studies haven’t been able to make a strong case for the procedure.
TCDSS is an ultrasound method in which 1 mL of tiny bubbles is injected into the vein and if detected in the brain, could give clues to a right-left shunt. The method is safer, the equipment is cheaper, and the training is faster than for TEE, Dr. Spence said.
He added that one reason that TCDSS may be more sensitive than TEE is that sedation for TEE may prevent an adequate Valsalva maneuver. He also showed in a video that detecting the bubbles in TCDSS is rather straightforward.
Given the findings of his study, Dr. Spence said that there’s a need to identify which PFO patients are more likely to have paradoxical embolism and are more likely to respond to patching.
One solution is paying attention to the clinical clues of paradoxical embolism (J. Neurol. Sci. 2008;275:121-7). And Dr. Spence’s recent findings may add another tool to help with this prediction.
Aside from the superiority of TCDSS to TEE in identifying PFO, Dr. Spence and his colleagues found that TCDSS was also better for risk stratification of PFOs. The analysis found that 25% of the shunts that were missed on TEE were high-grade shunts (Spencer grade 3 or higher). Patients with a shunt grade of 3 or higher were significantly more likely to have a stroke or transient ischemic attack in the 4-year follow-up period (P = .028), said Dr. Spence, director of the Stroke Prevention & Atherosclerosis Research Centre at the University of Western Ontario, London. This was not predicted by the presence of shunt on TEE, nor was it predicted by mobile atrial septum or septal aneurysm. TEE missed nearly 46% of grade 1 shunts, 32% of grade 2, 13% of grade 3, 7% of grade 4, and almost 5% of grade 5.
"This doesn’t mean that everyone should go pack up their TEE machines, because we still need it for diagnosis of other cardioembolism," said Dr. Spence. "But these techniques can be complementary."
He added that it’s too soon to use these findings as grounds for change in clinical practice, and there’s a need for further studies such as randomized trials.
The majority (62%) of the study’s 340 patients were female. The patients had a mean age of 53 years and underwent follow-up for a median of 420 days. All the patients, who visited the center between 2000 and 2013, had cryptogenic stroke and were suspected of having paradoxical embolism. A total of 280 cases had TEE data available.
Dr. Spence said he had no disclosures relevant to the study.
On Twitter @naseemsmiller
SAN DIEGO – Transcranial Doppler saline studies were superior to transesophageal echocardiography in diagnosing a hole in the heart, according to a prospective study of patients who had a cryptogenic stroke.
Researchers analyzed data from 340 patients with cryptogenic stroke suspected of paradoxical embolism who had had their right-left shunt confirmed with transcranial Doppler saline study (TCDSS). Transesophageal echocardiography (TEE) failed to show a shunt such as patent foramen ovale (PFO) in 15% of the cases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. J. David Spence, Robarts Research Institute
"I was surprised by the number," said Dr. J. David Spence, senior researcher of the study, who presented the findings at the International Stroke Conference, sponsored by the American Heart Association. "I had realized that some of the patients with shunts were missed by TEE, ... but I was surprised by how often that happened."
Nearly a quarter of the population has a PFO, and 4.0%-5.5% of strokes are due to paradoxical embolism through a right-left shunt. But patching the shunts isn’t the simple answer, because the procedure is not without complications, and so far, the studies haven’t been able to make a strong case for the procedure.
TCDSS is an ultrasound method in which 1 mL of tiny bubbles is injected into the vein and if detected in the brain, could give clues to a right-left shunt. The method is safer, the equipment is cheaper, and the training is faster than for TEE, Dr. Spence said.
He added that one reason that TCDSS may be more sensitive than TEE is that sedation for TEE may prevent an adequate Valsalva maneuver. He also showed in a video that detecting the bubbles in TCDSS is rather straightforward.
Given the findings of his study, Dr. Spence said that there’s a need to identify which PFO patients are more likely to have paradoxical embolism and are more likely to respond to patching.
One solution is paying attention to the clinical clues of paradoxical embolism (J. Neurol. Sci. 2008;275:121-7). And Dr. Spence’s recent findings may add another tool to help with this prediction.
Aside from the superiority of TCDSS to TEE in identifying PFO, Dr. Spence and his colleagues found that TCDSS was also better for risk stratification of PFOs. The analysis found that 25% of the shunts that were missed on TEE were high-grade shunts (Spencer grade 3 or higher). Patients with a shunt grade of 3 or higher were significantly more likely to have a stroke or transient ischemic attack in the 4-year follow-up period (P = .028), said Dr. Spence, director of the Stroke Prevention & Atherosclerosis Research Centre at the University of Western Ontario, London. This was not predicted by the presence of shunt on TEE, nor was it predicted by mobile atrial septum or septal aneurysm. TEE missed nearly 46% of grade 1 shunts, 32% of grade 2, 13% of grade 3, 7% of grade 4, and almost 5% of grade 5.
"This doesn’t mean that everyone should go pack up their TEE machines, because we still need it for diagnosis of other cardioembolism," said Dr. Spence. "But these techniques can be complementary."
He added that it’s too soon to use these findings as grounds for change in clinical practice, and there’s a need for further studies such as randomized trials.
The majority (62%) of the study’s 340 patients were female. The patients had a mean age of 53 years and underwent follow-up for a median of 420 days. All the patients, who visited the center between 2000 and 2013, had cryptogenic stroke and were suspected of having paradoxical embolism. A total of 280 cases had TEE data available.
Dr. Spence said he had no disclosures relevant to the study.
On Twitter @naseemsmiller
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Echocardiography (TEE) failed to show right-to-left shunts, such as patent foramen ovale, which were identified by TCDSS, in 15% of the cases.
Data source: Prospective study of 340 patients who had a cryptogenic stroke.
Disclosures: Dr. Spence had no disclosures relevant to the study.
Compared With Magnetic Resonance Imaging, Radiographs Underestimate the Magnitude of Negative Ulnar Variance
Emergency Imaging: Wrist injury in a woman with multiple sclerosis
Case
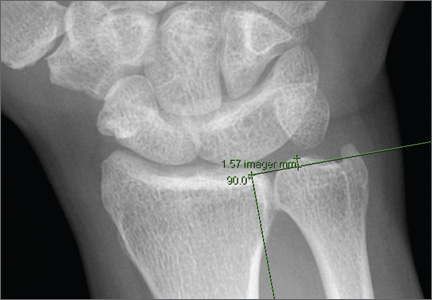
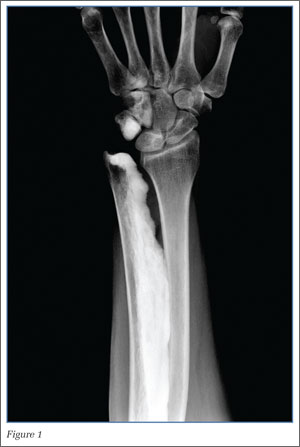
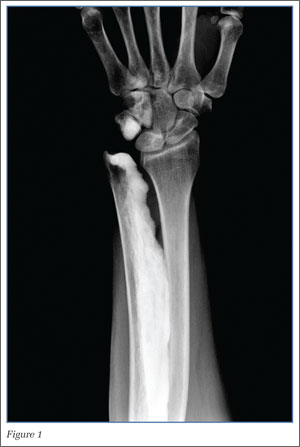
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512
Case
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
Case
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512
Sizzle magnets: a worrisome buzz in the emergency department
NAPLES, FLA. – They sizzle, they buzz, they vibrate. And they’re sending some children to the emergency department.
"One of the newest things we’re seeing a fair amount of are magnets, those sizzle magnets," reported Karen Macauley, DHA, R.N., trauma program director, All Children’s Hospital, St. Petersburg, Fla., and secretary of the Society of Trauma Nurses.
So-called "sizzle" magnets make a sound when they connect and are being sold as novelty toys, jewelry, and even for purported health benefits. One website specializing in gifts for the visually impaired notes that the magnetic field of these hematite magnets is "so strong," they’ll stay put if placed on the front and back of hands or ear lobes.
That strong magnetic force, however, can create havoc if children ingest magnets of any kind, Dr. Macauley said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"If the magnets stay in a string, they’re probably okay; but if they swallow one and wait a little while and swallow another, you can start to imagine what happens as it starts to pass through," she said. "One magnet stays, another comes in another part of the bowel, and they sizzle together. Now all of a sudden you have magnets that aren’t moving and cause a lot of necrosis. They’re actually very dangerous, and we don’t think too much about how dangerous they can be."
Between 2009 and 2011, an estimated 1,700 emergency department visits occurred because of magnet ingestion, with more than 70% of those cases involving children between age 4 and 12 years, according to researchers at the U.S. Public Interest Research Group, which highlighted magnets in its most recent annual toy safety survey.
Dr. Macauley also cautioned that button-size batteries, now in everything from remote controls to Grandma’s singing greeting card and hearing aid, are also a concern because they can cause burns or erode through tissue if ingested or put into body orifices.
"These batteries are everywhere, and kids do crazy stuff with them," she said.
The National Capital Poison Center, which operates a 24-hour National Battery Ingestion Hotline (202-625-3333)* for swallowed battery cases, estimates 3,500 Americans of all ages swallow miniature disc or button batteries each year.
The problem has been recognized for some time, but what few parents or providers realize is how quickly burns can occur, Dr. Macauley said.
She described a case involving a 6-year-old girl who picked up a small battery off the playground and amazed her friends by making it disappear in her ear. The child complained of severe pain overnight and presented to the emergency department in the morning, where surgery to remove the battery revealed third-degree burns to the ear canal and 65% perforation of the eardrum.
"It seemed like it should have been nothing; it was in there maybe 12 hours, but she had very severe injuries to her ear," Dr. Macauley said. "She’s been in the operating room probably a total of six different times trying to get that repaired, has a fair amount of hearing loss that stays, and ended up at a specialist hospital, out of network, to get a graft put in that ear."
Greeting card makers such as Hallmark have taken steps to secure button batteries, such as enclosing them underneath metal caps or in modules in which the cap is secured with screws. And the card makers warn consumers to properly dispose of old batteries after they’ve been replaced.
Dr. Macauley reported having no financial disclosures.
Correction, 3/5/2014: An earlier version of this article misstated the phone number for the Battery Ingestion hotline.
NAPLES, FLA. – They sizzle, they buzz, they vibrate. And they’re sending some children to the emergency department.
"One of the newest things we’re seeing a fair amount of are magnets, those sizzle magnets," reported Karen Macauley, DHA, R.N., trauma program director, All Children’s Hospital, St. Petersburg, Fla., and secretary of the Society of Trauma Nurses.
So-called "sizzle" magnets make a sound when they connect and are being sold as novelty toys, jewelry, and even for purported health benefits. One website specializing in gifts for the visually impaired notes that the magnetic field of these hematite magnets is "so strong," they’ll stay put if placed on the front and back of hands or ear lobes.
That strong magnetic force, however, can create havoc if children ingest magnets of any kind, Dr. Macauley said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"If the magnets stay in a string, they’re probably okay; but if they swallow one and wait a little while and swallow another, you can start to imagine what happens as it starts to pass through," she said. "One magnet stays, another comes in another part of the bowel, and they sizzle together. Now all of a sudden you have magnets that aren’t moving and cause a lot of necrosis. They’re actually very dangerous, and we don’t think too much about how dangerous they can be."
Between 2009 and 2011, an estimated 1,700 emergency department visits occurred because of magnet ingestion, with more than 70% of those cases involving children between age 4 and 12 years, according to researchers at the U.S. Public Interest Research Group, which highlighted magnets in its most recent annual toy safety survey.
Dr. Macauley also cautioned that button-size batteries, now in everything from remote controls to Grandma’s singing greeting card and hearing aid, are also a concern because they can cause burns or erode through tissue if ingested or put into body orifices.
"These batteries are everywhere, and kids do crazy stuff with them," she said.
The National Capital Poison Center, which operates a 24-hour National Battery Ingestion Hotline (202-625-3333)* for swallowed battery cases, estimates 3,500 Americans of all ages swallow miniature disc or button batteries each year.
The problem has been recognized for some time, but what few parents or providers realize is how quickly burns can occur, Dr. Macauley said.
She described a case involving a 6-year-old girl who picked up a small battery off the playground and amazed her friends by making it disappear in her ear. The child complained of severe pain overnight and presented to the emergency department in the morning, where surgery to remove the battery revealed third-degree burns to the ear canal and 65% perforation of the eardrum.
"It seemed like it should have been nothing; it was in there maybe 12 hours, but she had very severe injuries to her ear," Dr. Macauley said. "She’s been in the operating room probably a total of six different times trying to get that repaired, has a fair amount of hearing loss that stays, and ended up at a specialist hospital, out of network, to get a graft put in that ear."
Greeting card makers such as Hallmark have taken steps to secure button batteries, such as enclosing them underneath metal caps or in modules in which the cap is secured with screws. And the card makers warn consumers to properly dispose of old batteries after they’ve been replaced.
Dr. Macauley reported having no financial disclosures.
Correction, 3/5/2014: An earlier version of this article misstated the phone number for the Battery Ingestion hotline.
NAPLES, FLA. – They sizzle, they buzz, they vibrate. And they’re sending some children to the emergency department.
"One of the newest things we’re seeing a fair amount of are magnets, those sizzle magnets," reported Karen Macauley, DHA, R.N., trauma program director, All Children’s Hospital, St. Petersburg, Fla., and secretary of the Society of Trauma Nurses.
So-called "sizzle" magnets make a sound when they connect and are being sold as novelty toys, jewelry, and even for purported health benefits. One website specializing in gifts for the visually impaired notes that the magnetic field of these hematite magnets is "so strong," they’ll stay put if placed on the front and back of hands or ear lobes.
That strong magnetic force, however, can create havoc if children ingest magnets of any kind, Dr. Macauley said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
"If the magnets stay in a string, they’re probably okay; but if they swallow one and wait a little while and swallow another, you can start to imagine what happens as it starts to pass through," she said. "One magnet stays, another comes in another part of the bowel, and they sizzle together. Now all of a sudden you have magnets that aren’t moving and cause a lot of necrosis. They’re actually very dangerous, and we don’t think too much about how dangerous they can be."
Between 2009 and 2011, an estimated 1,700 emergency department visits occurred because of magnet ingestion, with more than 70% of those cases involving children between age 4 and 12 years, according to researchers at the U.S. Public Interest Research Group, which highlighted magnets in its most recent annual toy safety survey.
Dr. Macauley also cautioned that button-size batteries, now in everything from remote controls to Grandma’s singing greeting card and hearing aid, are also a concern because they can cause burns or erode through tissue if ingested or put into body orifices.
"These batteries are everywhere, and kids do crazy stuff with them," she said.
The National Capital Poison Center, which operates a 24-hour National Battery Ingestion Hotline (202-625-3333)* for swallowed battery cases, estimates 3,500 Americans of all ages swallow miniature disc or button batteries each year.
The problem has been recognized for some time, but what few parents or providers realize is how quickly burns can occur, Dr. Macauley said.
She described a case involving a 6-year-old girl who picked up a small battery off the playground and amazed her friends by making it disappear in her ear. The child complained of severe pain overnight and presented to the emergency department in the morning, where surgery to remove the battery revealed third-degree burns to the ear canal and 65% perforation of the eardrum.
"It seemed like it should have been nothing; it was in there maybe 12 hours, but she had very severe injuries to her ear," Dr. Macauley said. "She’s been in the operating room probably a total of six different times trying to get that repaired, has a fair amount of hearing loss that stays, and ended up at a specialist hospital, out of network, to get a graft put in that ear."
Greeting card makers such as Hallmark have taken steps to secure button batteries, such as enclosing them underneath metal caps or in modules in which the cap is secured with screws. And the card makers warn consumers to properly dispose of old batteries after they’ve been replaced.
Dr. Macauley reported having no financial disclosures.
Correction, 3/5/2014: An earlier version of this article misstated the phone number for the Battery Ingestion hotline.
AT EAST 2014
Myocardial fibrosis assessment fine-tunes ICD selection
SNOWMASS, COLO. – Detection of myocardial midwall fibrosis via cardiovascular magnetic resonance in patients with nonischemic dilated cardiomyopathy provides prognostic information independent of left ventricular ejection fraction.
"Low LVEF and fibrosis uniquely identify the need for an ICD [implantable cardioverter-defibrillator]. This is new information that helps refine our understanding of whom it is that’s uniquely at risk. We’ve always had these troublesome questions in patients with nonischemic heart failure," Dr. Clyde W. Yancy observed at the Annual Cardiovascular Conference at Snowmass.
He highlighted what he called "very provocative data" in a recent study led by Dr. Sanjay K. Prasad of Royal Brompton Hospital in London. The investigators evaluated 472 consecutive patients with nonischemic dilated cardiomyopathy using late gadolinium cardiovascular magnetic resonance (CMR). Thirty percent of them were found to have midwall fibrosis. Their all-cause mortality rate during a median 5.3 years of prospective follow-up was 26.8%, compared with 10.6% in the 330 patients without fibrosis. An arrhythmic composite event comprising sudden cardiac death (SCD), aborted SCD, or sustained ventricular tachycardia occurred in 29.6% of the group with fibrosis vs. 7% of patients without fibrosis.
In a multivariate analysis adjusted for LVEF and other prognostic factors, the presence of midwall fibrosis was independently associated with a 2.43-fold increased risk of all-cause mortality, a 3.2-fold greater risk of cardiovascular mortality or heart transplantation, a 4.6-fold increase in SCD or aborted SCD, and a 1.6-fold increased likelihood of a composite of heart failure hospitalization, mortality from heart failure, or cardiac transplantation (JAMA 2013;309:896-908).
Dr. Yancy, who chaired the writing committee for the 2013 ACC/AHA Guideline for the Management of Heart Failure, noted that the guidelines grant a strong Class I/Level of Evidence B recommendation for implantation of an ICD for primary prevention in nonischemic dilated cardiomyopathy patients who are in New York Heart Association functional class II or III and have an LVEF of 35% or less. But there is a pressing need for refined implantation criteria. Basing the ICD decision on only these criteria results in a low rate of appropriate shocks, a high frequency of inappropriate shocks, and exclusion from device therapy of a group of patients with a high relative risk of SCD.
The British study provides reason for optimism in this regard. Using a greater than 15% estimated SCD risk based upon LVEF plus midwall fibrosis as a proposed indication for ICD implantation, the investigators found that an additional 12 patients in their cohort would receive an ICD and 43 others would now avoid ICD implantation, noted Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
He reported having no financial conflicts.
SNOWMASS, COLO. – Detection of myocardial midwall fibrosis via cardiovascular magnetic resonance in patients with nonischemic dilated cardiomyopathy provides prognostic information independent of left ventricular ejection fraction.
"Low LVEF and fibrosis uniquely identify the need for an ICD [implantable cardioverter-defibrillator]. This is new information that helps refine our understanding of whom it is that’s uniquely at risk. We’ve always had these troublesome questions in patients with nonischemic heart failure," Dr. Clyde W. Yancy observed at the Annual Cardiovascular Conference at Snowmass.
He highlighted what he called "very provocative data" in a recent study led by Dr. Sanjay K. Prasad of Royal Brompton Hospital in London. The investigators evaluated 472 consecutive patients with nonischemic dilated cardiomyopathy using late gadolinium cardiovascular magnetic resonance (CMR). Thirty percent of them were found to have midwall fibrosis. Their all-cause mortality rate during a median 5.3 years of prospective follow-up was 26.8%, compared with 10.6% in the 330 patients without fibrosis. An arrhythmic composite event comprising sudden cardiac death (SCD), aborted SCD, or sustained ventricular tachycardia occurred in 29.6% of the group with fibrosis vs. 7% of patients without fibrosis.
In a multivariate analysis adjusted for LVEF and other prognostic factors, the presence of midwall fibrosis was independently associated with a 2.43-fold increased risk of all-cause mortality, a 3.2-fold greater risk of cardiovascular mortality or heart transplantation, a 4.6-fold increase in SCD or aborted SCD, and a 1.6-fold increased likelihood of a composite of heart failure hospitalization, mortality from heart failure, or cardiac transplantation (JAMA 2013;309:896-908).
Dr. Yancy, who chaired the writing committee for the 2013 ACC/AHA Guideline for the Management of Heart Failure, noted that the guidelines grant a strong Class I/Level of Evidence B recommendation for implantation of an ICD for primary prevention in nonischemic dilated cardiomyopathy patients who are in New York Heart Association functional class II or III and have an LVEF of 35% or less. But there is a pressing need for refined implantation criteria. Basing the ICD decision on only these criteria results in a low rate of appropriate shocks, a high frequency of inappropriate shocks, and exclusion from device therapy of a group of patients with a high relative risk of SCD.
The British study provides reason for optimism in this regard. Using a greater than 15% estimated SCD risk based upon LVEF plus midwall fibrosis as a proposed indication for ICD implantation, the investigators found that an additional 12 patients in their cohort would receive an ICD and 43 others would now avoid ICD implantation, noted Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
He reported having no financial conflicts.
SNOWMASS, COLO. – Detection of myocardial midwall fibrosis via cardiovascular magnetic resonance in patients with nonischemic dilated cardiomyopathy provides prognostic information independent of left ventricular ejection fraction.
"Low LVEF and fibrosis uniquely identify the need for an ICD [implantable cardioverter-defibrillator]. This is new information that helps refine our understanding of whom it is that’s uniquely at risk. We’ve always had these troublesome questions in patients with nonischemic heart failure," Dr. Clyde W. Yancy observed at the Annual Cardiovascular Conference at Snowmass.
He highlighted what he called "very provocative data" in a recent study led by Dr. Sanjay K. Prasad of Royal Brompton Hospital in London. The investigators evaluated 472 consecutive patients with nonischemic dilated cardiomyopathy using late gadolinium cardiovascular magnetic resonance (CMR). Thirty percent of them were found to have midwall fibrosis. Their all-cause mortality rate during a median 5.3 years of prospective follow-up was 26.8%, compared with 10.6% in the 330 patients without fibrosis. An arrhythmic composite event comprising sudden cardiac death (SCD), aborted SCD, or sustained ventricular tachycardia occurred in 29.6% of the group with fibrosis vs. 7% of patients without fibrosis.
In a multivariate analysis adjusted for LVEF and other prognostic factors, the presence of midwall fibrosis was independently associated with a 2.43-fold increased risk of all-cause mortality, a 3.2-fold greater risk of cardiovascular mortality or heart transplantation, a 4.6-fold increase in SCD or aborted SCD, and a 1.6-fold increased likelihood of a composite of heart failure hospitalization, mortality from heart failure, or cardiac transplantation (JAMA 2013;309:896-908).
Dr. Yancy, who chaired the writing committee for the 2013 ACC/AHA Guideline for the Management of Heart Failure, noted that the guidelines grant a strong Class I/Level of Evidence B recommendation for implantation of an ICD for primary prevention in nonischemic dilated cardiomyopathy patients who are in New York Heart Association functional class II or III and have an LVEF of 35% or less. But there is a pressing need for refined implantation criteria. Basing the ICD decision on only these criteria results in a low rate of appropriate shocks, a high frequency of inappropriate shocks, and exclusion from device therapy of a group of patients with a high relative risk of SCD.
The British study provides reason for optimism in this regard. Using a greater than 15% estimated SCD risk based upon LVEF plus midwall fibrosis as a proposed indication for ICD implantation, the investigators found that an additional 12 patients in their cohort would receive an ICD and 43 others would now avoid ICD implantation, noted Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Imaging no-nos top list of avoidable tests in emergency medicine
But it’s how the emergency medicine list’s creators developed it that may prove most valuable in future efforts to reduce unnecessary tests throughout medicine.
Several specialty societies have developed Top-5 lists of avoidable tests or procedures to comply with the American Board of Internal Medicine’s Choosing Wisely campaign. The lists are "a new idea to engage clinicians in resource stewardship and to address rising health care costs," said Dr. Jeremiah D. Schuur of the department of emergency medicine, Brigham and Women’s Hospital, Boston, and his associates (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed/2013.12688]).
To create the emergency medicine list, Dr. Jeremiah D. Schuur and his associates took the traditional Choosing Wisely approach, then added a consensus-based twist.
They convened a technical expert panel that included the chiefs of the two academic hospital emergency departments (EDs) and four community hospital EDs in their health care system, which covers more than 320,000 ED visits annually in eastern Massachusetts. The panel also included an emergency physician with expertise in affordability, another with expertise in diagnostic imaging, and a third with expertise in hospital admissions and transfers, as well as a chief resident in emergency medicine.
The panel devised a preliminary list of 64 "low-value clinical decisions that were under the control of emergency clinicians and were thought to have a potential for cost savings."
Then came the twist: A total of 283 frontline emergency clinicians from the health system’s six emergency departments then were invited to complete a Web-based survey tool measuring their opinions of the potential benefit or harm to patients if clinicians discontinued the top 17 potentially avoidable items on the list.
The panel reviewed results from the 174 clinicians who completed the survey, and it then distilled them into a list of the Top-5 unnecessary tests and procedures:
• Do not order CT of the cervical spine for trauma patients who do not meet the National Emergency X-ray Utilization Study (NEXUS) low-risk criteria or the Canadian C-Spine Rule.
• Do not order CT to diagnose pulmonary embolism without first risk stratifying for pulmonary embolism (pretest probability and D-dimer tests if low probability).
• Do not order MRI of the lumbar spine for patients with low-back pain without high-risk features.
• Do not order CT of the head for patients with mild traumatic head injury who do not meet New Orleans Criteria or Canadian CT Head Rule.
• Do not order coagulation studies for patients without hemorrhage or suspected coagulopathy (for example, with anticoagulation therapy or clinical coagulopathy).
Every item on this list "received similar ratings by different groups of ED clinicians, including physicians and midlevel practitioners, clinicians in academic and community-hospital EDs, and practitioners with experience ranging from less than 3 years to more than 10 years," the authors explained. That suggests that emergency health care clinicians in other locations, as well as members of other specialty societies, also can achieve such consensus, Dr. Schuur and his associates noted.
Emergency medicine "is under immense pressure" to improve the value of services, they added.
"Some emergency physicians may be hesitant to embrace stewardship efforts, such as Choosing Wisely, for fear of losing autonomy and the medicolegal risk," the investigators noted. "However, if emergency physicians, who best understand the clinical evidence and unique needs of our patients, do not define measures of overuse for our specialty, others will."
The American College of Emergency Physicians has wrestled with the question of complying with the ABIM’s Choosing Wisely campaign and developing a Top-5 list, beginning with "a passionate floor debate" at the 2012 national ACEP Council meeting and including a dramatic reversal of the initial decision not to join the effort, said Dr. Deborah Grady, Dr. Rita F. Redberg, and Dr. William K. Mallon.
At least 50 specialty societies have now developed their Top-5 lists – but most haven’t disclosed their methods, and some clearly developed their lists without much input from frontline practitioners and without clear criteria. So, emergency medicine’s contribution to the Choosing Wisely campaign "is as much about the methodology ... as it is about the final recommendations," they noted.
"We hope the article by [Dr. Schuur and his colleagues] will stimulate other professional societies to adopt clear, transparent methods for developing and revising Top-5 lists with substantial input from practicing clinicians," the three physicians said.
Dr. Grady and Dr. Redberg are in the department of medicine at the University of California, San Francisco; Dr. Grady is also at the San Francisco Veterans Affairs Medical Center. Dr. Mallon is in the department of clinical emergency medicine at the University of Southern California, Los Angeles. They reported no potential conflicts of interest. These remarks were taken from their editorial accompanying Dr. Schuur’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2013.8272]).
The American College of Emergency Physicians has wrestled with the question of complying with the ABIM’s Choosing Wisely campaign and developing a Top-5 list, beginning with "a passionate floor debate" at the 2012 national ACEP Council meeting and including a dramatic reversal of the initial decision not to join the effort, said Dr. Deborah Grady, Dr. Rita F. Redberg, and Dr. William K. Mallon.
At least 50 specialty societies have now developed their Top-5 lists – but most haven’t disclosed their methods, and some clearly developed their lists without much input from frontline practitioners and without clear criteria. So, emergency medicine’s contribution to the Choosing Wisely campaign "is as much about the methodology ... as it is about the final recommendations," they noted.
"We hope the article by [Dr. Schuur and his colleagues] will stimulate other professional societies to adopt clear, transparent methods for developing and revising Top-5 lists with substantial input from practicing clinicians," the three physicians said.
Dr. Grady and Dr. Redberg are in the department of medicine at the University of California, San Francisco; Dr. Grady is also at the San Francisco Veterans Affairs Medical Center. Dr. Mallon is in the department of clinical emergency medicine at the University of Southern California, Los Angeles. They reported no potential conflicts of interest. These remarks were taken from their editorial accompanying Dr. Schuur’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2013.8272]).
The American College of Emergency Physicians has wrestled with the question of complying with the ABIM’s Choosing Wisely campaign and developing a Top-5 list, beginning with "a passionate floor debate" at the 2012 national ACEP Council meeting and including a dramatic reversal of the initial decision not to join the effort, said Dr. Deborah Grady, Dr. Rita F. Redberg, and Dr. William K. Mallon.
At least 50 specialty societies have now developed their Top-5 lists – but most haven’t disclosed their methods, and some clearly developed their lists without much input from frontline practitioners and without clear criteria. So, emergency medicine’s contribution to the Choosing Wisely campaign "is as much about the methodology ... as it is about the final recommendations," they noted.
"We hope the article by [Dr. Schuur and his colleagues] will stimulate other professional societies to adopt clear, transparent methods for developing and revising Top-5 lists with substantial input from practicing clinicians," the three physicians said.
Dr. Grady and Dr. Redberg are in the department of medicine at the University of California, San Francisco; Dr. Grady is also at the San Francisco Veterans Affairs Medical Center. Dr. Mallon is in the department of clinical emergency medicine at the University of Southern California, Los Angeles. They reported no potential conflicts of interest. These remarks were taken from their editorial accompanying Dr. Schuur’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2013.8272]).
But it’s how the emergency medicine list’s creators developed it that may prove most valuable in future efforts to reduce unnecessary tests throughout medicine.
Several specialty societies have developed Top-5 lists of avoidable tests or procedures to comply with the American Board of Internal Medicine’s Choosing Wisely campaign. The lists are "a new idea to engage clinicians in resource stewardship and to address rising health care costs," said Dr. Jeremiah D. Schuur of the department of emergency medicine, Brigham and Women’s Hospital, Boston, and his associates (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed/2013.12688]).
To create the emergency medicine list, Dr. Jeremiah D. Schuur and his associates took the traditional Choosing Wisely approach, then added a consensus-based twist.
They convened a technical expert panel that included the chiefs of the two academic hospital emergency departments (EDs) and four community hospital EDs in their health care system, which covers more than 320,000 ED visits annually in eastern Massachusetts. The panel also included an emergency physician with expertise in affordability, another with expertise in diagnostic imaging, and a third with expertise in hospital admissions and transfers, as well as a chief resident in emergency medicine.
The panel devised a preliminary list of 64 "low-value clinical decisions that were under the control of emergency clinicians and were thought to have a potential for cost savings."
Then came the twist: A total of 283 frontline emergency clinicians from the health system’s six emergency departments then were invited to complete a Web-based survey tool measuring their opinions of the potential benefit or harm to patients if clinicians discontinued the top 17 potentially avoidable items on the list.
The panel reviewed results from the 174 clinicians who completed the survey, and it then distilled them into a list of the Top-5 unnecessary tests and procedures:
• Do not order CT of the cervical spine for trauma patients who do not meet the National Emergency X-ray Utilization Study (NEXUS) low-risk criteria or the Canadian C-Spine Rule.
• Do not order CT to diagnose pulmonary embolism without first risk stratifying for pulmonary embolism (pretest probability and D-dimer tests if low probability).
• Do not order MRI of the lumbar spine for patients with low-back pain without high-risk features.
• Do not order CT of the head for patients with mild traumatic head injury who do not meet New Orleans Criteria or Canadian CT Head Rule.
• Do not order coagulation studies for patients without hemorrhage or suspected coagulopathy (for example, with anticoagulation therapy or clinical coagulopathy).
Every item on this list "received similar ratings by different groups of ED clinicians, including physicians and midlevel practitioners, clinicians in academic and community-hospital EDs, and practitioners with experience ranging from less than 3 years to more than 10 years," the authors explained. That suggests that emergency health care clinicians in other locations, as well as members of other specialty societies, also can achieve such consensus, Dr. Schuur and his associates noted.
Emergency medicine "is under immense pressure" to improve the value of services, they added.
"Some emergency physicians may be hesitant to embrace stewardship efforts, such as Choosing Wisely, for fear of losing autonomy and the medicolegal risk," the investigators noted. "However, if emergency physicians, who best understand the clinical evidence and unique needs of our patients, do not define measures of overuse for our specialty, others will."
But it’s how the emergency medicine list’s creators developed it that may prove most valuable in future efforts to reduce unnecessary tests throughout medicine.
Several specialty societies have developed Top-5 lists of avoidable tests or procedures to comply with the American Board of Internal Medicine’s Choosing Wisely campaign. The lists are "a new idea to engage clinicians in resource stewardship and to address rising health care costs," said Dr. Jeremiah D. Schuur of the department of emergency medicine, Brigham and Women’s Hospital, Boston, and his associates (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed/2013.12688]).
To create the emergency medicine list, Dr. Jeremiah D. Schuur and his associates took the traditional Choosing Wisely approach, then added a consensus-based twist.
They convened a technical expert panel that included the chiefs of the two academic hospital emergency departments (EDs) and four community hospital EDs in their health care system, which covers more than 320,000 ED visits annually in eastern Massachusetts. The panel also included an emergency physician with expertise in affordability, another with expertise in diagnostic imaging, and a third with expertise in hospital admissions and transfers, as well as a chief resident in emergency medicine.
The panel devised a preliminary list of 64 "low-value clinical decisions that were under the control of emergency clinicians and were thought to have a potential for cost savings."
Then came the twist: A total of 283 frontline emergency clinicians from the health system’s six emergency departments then were invited to complete a Web-based survey tool measuring their opinions of the potential benefit or harm to patients if clinicians discontinued the top 17 potentially avoidable items on the list.
The panel reviewed results from the 174 clinicians who completed the survey, and it then distilled them into a list of the Top-5 unnecessary tests and procedures:
• Do not order CT of the cervical spine for trauma patients who do not meet the National Emergency X-ray Utilization Study (NEXUS) low-risk criteria or the Canadian C-Spine Rule.
• Do not order CT to diagnose pulmonary embolism without first risk stratifying for pulmonary embolism (pretest probability and D-dimer tests if low probability).
• Do not order MRI of the lumbar spine for patients with low-back pain without high-risk features.
• Do not order CT of the head for patients with mild traumatic head injury who do not meet New Orleans Criteria or Canadian CT Head Rule.
• Do not order coagulation studies for patients without hemorrhage or suspected coagulopathy (for example, with anticoagulation therapy or clinical coagulopathy).
Every item on this list "received similar ratings by different groups of ED clinicians, including physicians and midlevel practitioners, clinicians in academic and community-hospital EDs, and practitioners with experience ranging from less than 3 years to more than 10 years," the authors explained. That suggests that emergency health care clinicians in other locations, as well as members of other specialty societies, also can achieve such consensus, Dr. Schuur and his associates noted.
Emergency medicine "is under immense pressure" to improve the value of services, they added.
"Some emergency physicians may be hesitant to embrace stewardship efforts, such as Choosing Wisely, for fear of losing autonomy and the medicolegal risk," the investigators noted. "However, if emergency physicians, who best understand the clinical evidence and unique needs of our patients, do not define measures of overuse for our specialty, others will."
FROM JAMA INTERNAL MEDICINE
ACC highlights noninvasive cardiovascular imaging issues
Noninvasive cardiovascular imaging in U.S. medical practice today raises two policy challenges, according to a statement released on Feb. 17 by the American College of Cardiology and 13 collaborating medical groups: fostering a volume of imaging that balances patient needs with responsible use of societal resources, and continued improvement in the quality of care based on noninvasive cardiovascular imaging.
"The purpose of this document is to provide a brief exposition of the issues involved [in usage volume of noninvasive cardiovascular imaging] and the possible ways in which the medical care system can balance responsible use of imaging with patient safety concerns while maintaining or even enhancing quality of care," wrote the 20-member panel in a health policy statement (J. Am. Coll. Cardiol. 2014;63:698-721). "Policy makers must take into account the complex interplay between medical care quality (of which proper use of diagnostic testing is an integral part), patient health outcomes, and medical costs," said the statement’s panel, which included representatives from the American Society of Nuclear Cardiology, the American Society of Echocardiography, the Radiological Society of North America, and six other imaging groups.
"The current situation in noninvasive cardiovascular imaging is pretty much unsatisfactory from everyone’s point of view," said Dr. Daniel B. Mark, a cardiologist and professor of medicine at Duke University in Durham, N.C., who chaired the statement-writing committee."However, it is encouraging that we now have much more knowledge and several new informatics tools that can be used to help us apply that knowledge. We have many of the ingredients needed to create a more responsible, cost-conscious approach to imaging that still preserves – at its core – patient-physician decision making," said Dr. Mark in a written statement.
Over the past 20 years, U.S. health care payers implemented three main strategies to control expenditures for diagnostic imaging, the statement said: requiring prior authorization from a radiology benefits manager; requiring prior notification before performing selected, advanced diagnostic imaging methods like MRI and PET; and reduced payments for imaging. The statement characterized all three as "blunt instruments,’ and added these can lead to "limited patient access to necessary services and greater administrative inefficiencies."
One approach that would likely improve imaging-use policy is an "iterative process" that uses high-quality data to guide development of policy interventions with the potential to reduce imaging overuse, underuse, and misuse. Another approach the panel endorsed is integration of appropriate-use software into the process of care. "Development of computerized appropriate-use tools would be efficient and also greatly enhance transparency," the panel said. "Validated patient-specific point-of-care/referral appropriateness tools and other decision-support tools are examples of innovations that could support a higher-quality, more accountable use of cardiovascular imaging."
Recent data show that growth of advanced cardiovascular imaging has substantially slowed since 2006, likely because of a combination of professional society and payer initiatives. "Many clinicians and patients fear that imaging policy decisions will continue to be driven primarily, if not exclusively, by cost considerations without adequate consideration of clinical benefit and value," said the statement.
"The complexity of our current health care system and the competing macro-forces that push it in myriad different directions can make responsible imaging use seem impossibly daunting. What we need is a convergence of will from all key stakeholders to make it happen. This statement is hopefully a step in that direction," Dr. Mark said.
Dr. Mark said that he had no disclosures.
On Twitter @mitchelzoler
Noninvasive cardiovascular imaging in U.S. medical practice today raises two policy challenges, according to a statement released on Feb. 17 by the American College of Cardiology and 13 collaborating medical groups: fostering a volume of imaging that balances patient needs with responsible use of societal resources, and continued improvement in the quality of care based on noninvasive cardiovascular imaging.
"The purpose of this document is to provide a brief exposition of the issues involved [in usage volume of noninvasive cardiovascular imaging] and the possible ways in which the medical care system can balance responsible use of imaging with patient safety concerns while maintaining or even enhancing quality of care," wrote the 20-member panel in a health policy statement (J. Am. Coll. Cardiol. 2014;63:698-721). "Policy makers must take into account the complex interplay between medical care quality (of which proper use of diagnostic testing is an integral part), patient health outcomes, and medical costs," said the statement’s panel, which included representatives from the American Society of Nuclear Cardiology, the American Society of Echocardiography, the Radiological Society of North America, and six other imaging groups.
"The current situation in noninvasive cardiovascular imaging is pretty much unsatisfactory from everyone’s point of view," said Dr. Daniel B. Mark, a cardiologist and professor of medicine at Duke University in Durham, N.C., who chaired the statement-writing committee."However, it is encouraging that we now have much more knowledge and several new informatics tools that can be used to help us apply that knowledge. We have many of the ingredients needed to create a more responsible, cost-conscious approach to imaging that still preserves – at its core – patient-physician decision making," said Dr. Mark in a written statement.
Over the past 20 years, U.S. health care payers implemented three main strategies to control expenditures for diagnostic imaging, the statement said: requiring prior authorization from a radiology benefits manager; requiring prior notification before performing selected, advanced diagnostic imaging methods like MRI and PET; and reduced payments for imaging. The statement characterized all three as "blunt instruments,’ and added these can lead to "limited patient access to necessary services and greater administrative inefficiencies."
One approach that would likely improve imaging-use policy is an "iterative process" that uses high-quality data to guide development of policy interventions with the potential to reduce imaging overuse, underuse, and misuse. Another approach the panel endorsed is integration of appropriate-use software into the process of care. "Development of computerized appropriate-use tools would be efficient and also greatly enhance transparency," the panel said. "Validated patient-specific point-of-care/referral appropriateness tools and other decision-support tools are examples of innovations that could support a higher-quality, more accountable use of cardiovascular imaging."
Recent data show that growth of advanced cardiovascular imaging has substantially slowed since 2006, likely because of a combination of professional society and payer initiatives. "Many clinicians and patients fear that imaging policy decisions will continue to be driven primarily, if not exclusively, by cost considerations without adequate consideration of clinical benefit and value," said the statement.
"The complexity of our current health care system and the competing macro-forces that push it in myriad different directions can make responsible imaging use seem impossibly daunting. What we need is a convergence of will from all key stakeholders to make it happen. This statement is hopefully a step in that direction," Dr. Mark said.
Dr. Mark said that he had no disclosures.
On Twitter @mitchelzoler
Noninvasive cardiovascular imaging in U.S. medical practice today raises two policy challenges, according to a statement released on Feb. 17 by the American College of Cardiology and 13 collaborating medical groups: fostering a volume of imaging that balances patient needs with responsible use of societal resources, and continued improvement in the quality of care based on noninvasive cardiovascular imaging.
"The purpose of this document is to provide a brief exposition of the issues involved [in usage volume of noninvasive cardiovascular imaging] and the possible ways in which the medical care system can balance responsible use of imaging with patient safety concerns while maintaining or even enhancing quality of care," wrote the 20-member panel in a health policy statement (J. Am. Coll. Cardiol. 2014;63:698-721). "Policy makers must take into account the complex interplay between medical care quality (of which proper use of diagnostic testing is an integral part), patient health outcomes, and medical costs," said the statement’s panel, which included representatives from the American Society of Nuclear Cardiology, the American Society of Echocardiography, the Radiological Society of North America, and six other imaging groups.
"The current situation in noninvasive cardiovascular imaging is pretty much unsatisfactory from everyone’s point of view," said Dr. Daniel B. Mark, a cardiologist and professor of medicine at Duke University in Durham, N.C., who chaired the statement-writing committee."However, it is encouraging that we now have much more knowledge and several new informatics tools that can be used to help us apply that knowledge. We have many of the ingredients needed to create a more responsible, cost-conscious approach to imaging that still preserves – at its core – patient-physician decision making," said Dr. Mark in a written statement.
Over the past 20 years, U.S. health care payers implemented three main strategies to control expenditures for diagnostic imaging, the statement said: requiring prior authorization from a radiology benefits manager; requiring prior notification before performing selected, advanced diagnostic imaging methods like MRI and PET; and reduced payments for imaging. The statement characterized all three as "blunt instruments,’ and added these can lead to "limited patient access to necessary services and greater administrative inefficiencies."
One approach that would likely improve imaging-use policy is an "iterative process" that uses high-quality data to guide development of policy interventions with the potential to reduce imaging overuse, underuse, and misuse. Another approach the panel endorsed is integration of appropriate-use software into the process of care. "Development of computerized appropriate-use tools would be efficient and also greatly enhance transparency," the panel said. "Validated patient-specific point-of-care/referral appropriateness tools and other decision-support tools are examples of innovations that could support a higher-quality, more accountable use of cardiovascular imaging."
Recent data show that growth of advanced cardiovascular imaging has substantially slowed since 2006, likely because of a combination of professional society and payer initiatives. "Many clinicians and patients fear that imaging policy decisions will continue to be driven primarily, if not exclusively, by cost considerations without adequate consideration of clinical benefit and value," said the statement.
"The complexity of our current health care system and the competing macro-forces that push it in myriad different directions can make responsible imaging use seem impossibly daunting. What we need is a convergence of will from all key stakeholders to make it happen. This statement is hopefully a step in that direction," Dr. Mark said.
Dr. Mark said that he had no disclosures.
On Twitter @mitchelzoler
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Complicated Acromioclavicular Joint Cyst With Massive Rotator Cuff Tear
Challenges in Sports Medicine and Orthopedics
Dr Patterson, editor of “Challenges in Sports Medicine and Orthopedics,” is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
|
|
A 5-year-old boy presented to the ED after sustaining an injury to his left leg during play with a friend. He was unable to bear weight on the left foot and had a visible deformity to his lower extremity. The left foot was neurovascularly intact. Radiographs were completed (Figures 1 and 2).
What is your interpretation of the following radiographs?
Answer
|
|
The radiographs revealed a 20˚ anteriorly (apex posterior) angulated fracture through the metaphysis of the distal tibia and fibula. Angulated distal tibia fractures in adults are usually fixed with surgery; however, in children, displaced or angulated fractures to long bones such as the tibia stimulate a significant amount of growth. In treating pediatric patients, there is a greater amount of acceptable angulation the closer a fracture is to the end of bone.1
The patient in this case was placed in a long leg cast, and the fractures were reduced with three-point fixation technique. He remained in the cast for 5 weeks; thereafter, a below-the-knee orthopedic walking boot was placed for 3 weeks. The radiographs in Figures 3 and 4, taken 8 weeks after initiation of treatment, show a healed distal tibia and fibula fracture with an acceptable 7˚ of anterior angulation.
Dr Patterson, editor of “Challenges in Sports Medicine and Orthopedics,” is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
|
|
A 5-year-old boy presented to the ED after sustaining an injury to his left leg during play with a friend. He was unable to bear weight on the left foot and had a visible deformity to his lower extremity. The left foot was neurovascularly intact. Radiographs were completed (Figures 1 and 2).
What is your interpretation of the following radiographs?
Answer
|
|
The radiographs revealed a 20˚ anteriorly (apex posterior) angulated fracture through the metaphysis of the distal tibia and fibula. Angulated distal tibia fractures in adults are usually fixed with surgery; however, in children, displaced or angulated fractures to long bones such as the tibia stimulate a significant amount of growth. In treating pediatric patients, there is a greater amount of acceptable angulation the closer a fracture is to the end of bone.1
The patient in this case was placed in a long leg cast, and the fractures were reduced with three-point fixation technique. He remained in the cast for 5 weeks; thereafter, a below-the-knee orthopedic walking boot was placed for 3 weeks. The radiographs in Figures 3 and 4, taken 8 weeks after initiation of treatment, show a healed distal tibia and fibula fracture with an acceptable 7˚ of anterior angulation.
Dr Patterson, editor of “Challenges in Sports Medicine and Orthopedics,” is a sports medicine physician at Florida Sports Injury in Clermont, Florida. Dr Patterson is board certified in family medicine and spinal cord injury medicine, and is a member of the faculty of sports and exercise medicine of the Royal College of Surgeons in Ireland.
|
|
A 5-year-old boy presented to the ED after sustaining an injury to his left leg during play with a friend. He was unable to bear weight on the left foot and had a visible deformity to his lower extremity. The left foot was neurovascularly intact. Radiographs were completed (Figures 1 and 2).
What is your interpretation of the following radiographs?
Answer
|
|
The radiographs revealed a 20˚ anteriorly (apex posterior) angulated fracture through the metaphysis of the distal tibia and fibula. Angulated distal tibia fractures in adults are usually fixed with surgery; however, in children, displaced or angulated fractures to long bones such as the tibia stimulate a significant amount of growth. In treating pediatric patients, there is a greater amount of acceptable angulation the closer a fracture is to the end of bone.1
The patient in this case was placed in a long leg cast, and the fractures were reduced with three-point fixation technique. He remained in the cast for 5 weeks; thereafter, a below-the-knee orthopedic walking boot was placed for 3 weeks. The radiographs in Figures 3 and 4, taken 8 weeks after initiation of treatment, show a healed distal tibia and fibula fracture with an acceptable 7˚ of anterior angulation.