User login
Storytelling tool can assist elderly in the ICU
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
REPORTING FROM CLINICAL CONGRESS 2019
Short-course DAA therapy may prevent hepatitis transmission in transplant patients
BOSTON – A short course of results of a recent study show.
The regimen, given right before transplantation and for 7 days afterward, reduced the cost of direct-acting antiviral (DAA) therapy and allowed patients to complete hepatitis C virus (HCV) therapy before hospital discharge, according to authors of the study, which was presented at the annual meeting of the American Association for the Study of Liver Diseases.
If confirmed in subsequent studies, this regimen could become the standard of care for donor-positive, recipient-negative transplantation, said lead study author Jordan J. Feld, MD, R. Phelan Chair in translational liver disease research at the University of Toronto and research director at the Toronto Centre for Liver Disease.
“Transplant recipients are understandably nervous about accepting organs from people with HCV infection,” said Dr. Feld in a press release. “This very short therapy allows them to leave hospital free of HCV, which is a huge benefit. Not only is it cheaper and likely safer, but the patients really prefer not having to worry about HCV with all of the other challenges after a transplant.”
Results of this study come at a time when the proportion of overdose death organ donors is on the rise, from just 1% in 2000 to 15% in 2016, according to Dr. Feld. Overdose deaths account for the largest percentage of HCV-infected donors, most of whom are young and often otherwise healthy, he added.
Recipients of HCV-infected organs can be cured after transplant as a number of studies have previously shown. However, preventing transmission would be better than cure, Dr. Feld said, in part because of issues with drug-drug interactions, potential for relapse, and issues with procuring the drugs after transplant.
Accordingly, Dr. Feld and colleagues sought to evaluate “preemptive” treatment with DAA therapy combined with ezetimibe, which they said has been shown to inhibit HCV entry blockers. The recipients, who were listed for heart, lung, kidney, or kidney-pancreas transplant, were given glecaprevir/pibrentasvir plus ezetimibe starting 6-12 hours prior to transplantation, and then daily for 7 days.
The median age was 36 years for the 16 donors reported, and 61 years for the 25 recipients. Most recipients (12 patients) had a lung transplant, while 8 had a heart transplant, 4 had a kidney transplant, and 1 had a kidney-pancreas transplant.
There were no virologic failures, according to the investigators, with sustained virologic response (SVR) after 6 weeks in 7 patients, and SVR after 12 weeks in the remaining 18. Three recipients did have detectable HCV RNA, though all cleared and had SVR at 6 weeks in one case, and SVR at 12 weeks in the other two, according to the investigators’ report.
Of 22 serious adverse events noted in the study, 1 was considered treatment related, according to the report, and there were 2 deaths among lung transplant patients, caused by sepsis in 1 case to sepsis and subarachnoid hemorrhage in another.
It’s not clear whether ezetimibe is needed in this short-duration regimen, but in any case, it is well tolerated and inexpensive, and so there is “minimal downside” to include it, Dr. Feld and coinvestigators wrote in their report.
Dr. Feld reported disclosures related to Abbvie, Abbott, Enanta Pharmaceuticals, Gilead, Janssen, Merck, and Roche.
SOURCE: Feld JJ et al. The Liver Meeting 2019, Abstract 38.
BOSTON – A short course of results of a recent study show.
The regimen, given right before transplantation and for 7 days afterward, reduced the cost of direct-acting antiviral (DAA) therapy and allowed patients to complete hepatitis C virus (HCV) therapy before hospital discharge, according to authors of the study, which was presented at the annual meeting of the American Association for the Study of Liver Diseases.
If confirmed in subsequent studies, this regimen could become the standard of care for donor-positive, recipient-negative transplantation, said lead study author Jordan J. Feld, MD, R. Phelan Chair in translational liver disease research at the University of Toronto and research director at the Toronto Centre for Liver Disease.
“Transplant recipients are understandably nervous about accepting organs from people with HCV infection,” said Dr. Feld in a press release. “This very short therapy allows them to leave hospital free of HCV, which is a huge benefit. Not only is it cheaper and likely safer, but the patients really prefer not having to worry about HCV with all of the other challenges after a transplant.”
Results of this study come at a time when the proportion of overdose death organ donors is on the rise, from just 1% in 2000 to 15% in 2016, according to Dr. Feld. Overdose deaths account for the largest percentage of HCV-infected donors, most of whom are young and often otherwise healthy, he added.
Recipients of HCV-infected organs can be cured after transplant as a number of studies have previously shown. However, preventing transmission would be better than cure, Dr. Feld said, in part because of issues with drug-drug interactions, potential for relapse, and issues with procuring the drugs after transplant.
Accordingly, Dr. Feld and colleagues sought to evaluate “preemptive” treatment with DAA therapy combined with ezetimibe, which they said has been shown to inhibit HCV entry blockers. The recipients, who were listed for heart, lung, kidney, or kidney-pancreas transplant, were given glecaprevir/pibrentasvir plus ezetimibe starting 6-12 hours prior to transplantation, and then daily for 7 days.
The median age was 36 years for the 16 donors reported, and 61 years for the 25 recipients. Most recipients (12 patients) had a lung transplant, while 8 had a heart transplant, 4 had a kidney transplant, and 1 had a kidney-pancreas transplant.
There were no virologic failures, according to the investigators, with sustained virologic response (SVR) after 6 weeks in 7 patients, and SVR after 12 weeks in the remaining 18. Three recipients did have detectable HCV RNA, though all cleared and had SVR at 6 weeks in one case, and SVR at 12 weeks in the other two, according to the investigators’ report.
Of 22 serious adverse events noted in the study, 1 was considered treatment related, according to the report, and there were 2 deaths among lung transplant patients, caused by sepsis in 1 case to sepsis and subarachnoid hemorrhage in another.
It’s not clear whether ezetimibe is needed in this short-duration regimen, but in any case, it is well tolerated and inexpensive, and so there is “minimal downside” to include it, Dr. Feld and coinvestigators wrote in their report.
Dr. Feld reported disclosures related to Abbvie, Abbott, Enanta Pharmaceuticals, Gilead, Janssen, Merck, and Roche.
SOURCE: Feld JJ et al. The Liver Meeting 2019, Abstract 38.
BOSTON – A short course of results of a recent study show.
The regimen, given right before transplantation and for 7 days afterward, reduced the cost of direct-acting antiviral (DAA) therapy and allowed patients to complete hepatitis C virus (HCV) therapy before hospital discharge, according to authors of the study, which was presented at the annual meeting of the American Association for the Study of Liver Diseases.
If confirmed in subsequent studies, this regimen could become the standard of care for donor-positive, recipient-negative transplantation, said lead study author Jordan J. Feld, MD, R. Phelan Chair in translational liver disease research at the University of Toronto and research director at the Toronto Centre for Liver Disease.
“Transplant recipients are understandably nervous about accepting organs from people with HCV infection,” said Dr. Feld in a press release. “This very short therapy allows them to leave hospital free of HCV, which is a huge benefit. Not only is it cheaper and likely safer, but the patients really prefer not having to worry about HCV with all of the other challenges after a transplant.”
Results of this study come at a time when the proportion of overdose death organ donors is on the rise, from just 1% in 2000 to 15% in 2016, according to Dr. Feld. Overdose deaths account for the largest percentage of HCV-infected donors, most of whom are young and often otherwise healthy, he added.
Recipients of HCV-infected organs can be cured after transplant as a number of studies have previously shown. However, preventing transmission would be better than cure, Dr. Feld said, in part because of issues with drug-drug interactions, potential for relapse, and issues with procuring the drugs after transplant.
Accordingly, Dr. Feld and colleagues sought to evaluate “preemptive” treatment with DAA therapy combined with ezetimibe, which they said has been shown to inhibit HCV entry blockers. The recipients, who were listed for heart, lung, kidney, or kidney-pancreas transplant, were given glecaprevir/pibrentasvir plus ezetimibe starting 6-12 hours prior to transplantation, and then daily for 7 days.
The median age was 36 years for the 16 donors reported, and 61 years for the 25 recipients. Most recipients (12 patients) had a lung transplant, while 8 had a heart transplant, 4 had a kidney transplant, and 1 had a kidney-pancreas transplant.
There were no virologic failures, according to the investigators, with sustained virologic response (SVR) after 6 weeks in 7 patients, and SVR after 12 weeks in the remaining 18. Three recipients did have detectable HCV RNA, though all cleared and had SVR at 6 weeks in one case, and SVR at 12 weeks in the other two, according to the investigators’ report.
Of 22 serious adverse events noted in the study, 1 was considered treatment related, according to the report, and there were 2 deaths among lung transplant patients, caused by sepsis in 1 case to sepsis and subarachnoid hemorrhage in another.
It’s not clear whether ezetimibe is needed in this short-duration regimen, but in any case, it is well tolerated and inexpensive, and so there is “minimal downside” to include it, Dr. Feld and coinvestigators wrote in their report.
Dr. Feld reported disclosures related to Abbvie, Abbott, Enanta Pharmaceuticals, Gilead, Janssen, Merck, and Roche.
SOURCE: Feld JJ et al. The Liver Meeting 2019, Abstract 38.
REPORTING FROM THE LIVER MEETING 2019
Strategy critical to surviving drug shortages
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
NATIONAL HARBOR, MD. –
“Statistically speaking, there is no proof that patients are worse off from drug shortages,” Matt Grissinger, RPh, director of error-reporting programs at the Institute for Safe Medication Practices, told the audience at the annual conference of the Academy of Managed Care Pharmacy. The data and anecdotes he presented suggest the contrary.
As Mr. Grissinger pointed out, drug shortages can create a sequela of events that stress health care workers seeking to find the next-best available and most appropriate therapy for their patients. In the process, numerous medication-related errors can occur, resulting in patient harm, including adverse drug events and even death.
One potential problems is erroneous or inappropriate drug substitution stemming from mis- or uncalculated doses because of factors such as incorrect labeling and lack of knowledge regarding acceptable therapeutic interchanges. Other potential errors include non–therapeutically equivalent drug substitutions, resulting in supraoptimal therapy or overdoses, and unfamiliarity with drug labeling from outsourced facilities.
As a result, patients may experience worse outcomes as a consequence of the drug shortage: Worsening of the disease, disease prolongation, side effects stemming from alternative drug selections, untreated pain, psychological effects, severe electrolyte imbalances, severe acid/base imbalances, and death.
While a paper trail can help piece together clues regarding how a medication error occurred, documentation or lack thereof can also introduce errors when drug shortages occur.
Any changes to a drug order or prescription that deviate from the prescriber’s original request require prescriber approval but can still create opportunities for error. While documenting these changes and updating labeling is essential, appropriate documentation does not always occur and raises the question of who is responsible for making such changes.
Drug shortages also challenge a clinician’s professional judgment. Mr. Grissinger cited an example in which a nurse used half of a 0.5-mg single-use vial of promethazine for a patient requiring a 0.25 mg dose. The nurse wrote on the label that the remainder should be saved. While the vial was manufactured for one-time use, whether to discard the unused contents in a situation of drug shortages required the nurse to make a judgment call. In this case, the nurse chose to save the balance of the drug – a choice Mr. Grissinger stated he might have made had he been in a similar situation.
Additionally, drug shortages can create a climate in which more ethical questions arise – especially with regard to disease states such as cancer.
“If you only have 10 vials of vincristine, who gets it?” Mr. Grissinger asked the audience.
To help answer these difficult life-or-death questions, hospital settings need to engage the ethics committees and social workers.
While education plays a vital role in bringing attention to and addressing errors stemming from drug shortages, Mr. Grissinger cautioned the audience not to rely on education as the solution.
“Education is a poor strategy for addressing drug shortages,” he said. While education can draw awareness to drug shortages and subsequent medication-related errors, Mr. Grissinger recommends that organizations implement strategies to help ameliorate the havoc created by drug shortages.
Drug shortage assessment checklists can help organizations evaluate the impact of shortages by verifying inventory, and proactively searching for alternatives. From there, they can enact strategies such as assigning priority to patients who have the greatest need, altering packaging and concentrations, and finding suitable therapeutic substitutions.
REPORTING FROM AMCP NEXUS 2019
VA Boston Healthcare System First Friday Faculty Development Presentation Series
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
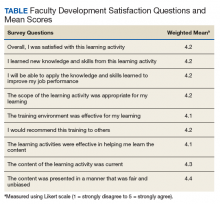
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
The US Department of Veterans Affairs (VA) trains a large number of learners from across multiple health care professions— more than 122,000 in 2017.1 The VA has affiliation agreements with almost all American medical schools (97%), and annually about one-third of all medical residents in the US train at VA academic medical centers (AMCs).1,2 The VA also trains learners in more than 40 health care professions from >1,800 training programs.1,3 This large commitment to training aides the recruitment of these learners as VA clinicians. In fact, a high percentage of current VA clinicians previously trained at the VA. For example, 60% of VA physicians and about 70% of both VA optometrists and psychologists trained at the VA.1
Given the large scope of training experiences and the impact on future employment, it is critical that VA educators provide a highquality learning experience for trainees. To do this, VA educators need both initial and ongoing education and support to grow and develop as teachers and as supervisors.4 Few educators currently report receiving this type of training, which includes effectively providing feedback to trainees, assessing trainee learning, and teaching on interprofessional teams.5
Numerous benefits to the AMC may be realized when a structured approach to faculty development is implemented. Systematic literature reviews of such approaches found that faculty members were satisfied with programming and that the content of programing was useful and relevant to their teaching.6,7 Faculty reported increased positive attitudes toward faculty development and toward teaching, increased knowledge of educational principles, greater establishment of faculty networks, and positive changes in teaching behavior (as identified by faculty and students).6,7 Further, participating in faculty development programming increased teaching effectiveness.6-8 Faculty development programs also provided direct and indirect financial benefits to the AMC and may lead to increased patient safety, increased patient satisfaction with care, and higher quality of care.9,10 Faculty development programming can be delivered via an online system that is as effective as face-to-face trainings and is more cost-efficient than are face-to-face trainings, particularly for educators at rural sites.11
Methods
The VA Boston Healthcare System (VABHS) is a large AMC with more than 350 academic affiliations, 500 faculty members, and 3200 trainees from a wide range of health care professions. Despite this robust presence of trainees, like many other AMCs, in 2014 VABHS lacked a structured approach to faculty development programming.12,13
To realize the potential benefits of this programming, VABHS developed a framework to conceptualize multiple components of faculty development programming. The framework focused on faculty development activities in 5 areas: teaching, research, awards, interprofessional, networking (TRAIN).14 The TRAIN framework allowed VABHS to develop specific faculty development programs in a strategic and organized manner.
In this article, we describe the VABHS First Friday Faculty Development Presentation series, a faculty development program that was created to improve teaching and supervising skill. The presentation series began in 2014. Faculty members at all 3 VABHS campuses participated in the presentations either in-person or via videoconference. Over time, faculty members at other New England VA AMCs began to express interest in participating, and audio and videoconferences were used to allow participation from those sites.
The program soon developed a national audience. In January 2017, this program provided the opportunity for faculty members to earn continuing education (CE) credits for participation. This allowed faculty members a unique opportunity to earn CE for presentations specifically geared toward improving skills as an educator, which is not widely available—particularly at rural and remote VA sites.
Presentations were 1 hour and held on the first Friday of the month at 12 pm Eastern Standard time. Topics for the presentations were identified through formal and informal needs assessments of faculty and through faculty development needs identified in the literature. Presentation topics consistent with the components of the TRAIN framework were selected. The cost to develop the program was largely related to time spent by presentation organizers to arrange speakers, advertise the presentations, develop a protocol for the use of the technology, and apply for accreditation for participants to receive CE credits.
Presenters were educators from a range of health care professions, including physicians, psychologists, nurses, and other professions from VABHS and neighboring Boston-area AMCs. Topics included providing feedback to learners, using active learning strategies, teaching clinical thinking, reducing burnout among educators, managing work-life balance, and developing interprofessional learning curricula. Presentations are archived online.
Results
From January 2017 to June 2018, 869 CE credits were earned by faculty members at VA AMCs nationwide for participating in this faculty development program, including 359 credits for nurses (41.3%), 164 credits for pharmacists (18.9%), 128 credits for physicians (14.7%), 67 credits for social workers (7.7%), and 54 credits for psychologists (6.2%). Other CE credits were earned by dieticians (14), dentists (13), speech pathologists (3), and occupational therapists (2), and other health care professionals (65).
Participants completed satisfaction surveys, responding to 9 questions using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) (Table). Data collection practices were reviewed by the VABHS Internal Review Board, which determined that the data did not meet the definition of human subject research and did not require further review.
Participants were asked 2 additional questions to further assess the programming. Seven hundred forty-eight participants responded to the question “How much did you learn as a result of this CE program?” using Likert-scale responses (1 = very little to 5 = great deal): 56.6% responded with a 4, (fair amount), and 21.5% responded with a 5 (great deal). Participants also were asked whether the content of this CE program was useful for their practice or other professional development (1 = not useful to 5 = extremely useful). Seven hundred forty-nine participants responded with a 4 (useful), and 25.4% of participants responded with a 5 (extremely useful).
Discussion
Overall, participants reported that the presentations were effective in teaching content, they acquired new knowledge, and they can apply this knowledge in future teaching. Participants reported satisfaction with the training activities and that the content was presented in a fair and unbiased manner. Further, they reported the training environment was effective, and they would recommend the training to others.
Conclusion
VABHS will continue to identify mechanisms to further disseminate and enhance this programming, particularly in rural areas, where there is a shortage of faculty development programming.2 We will continue to assess the impact of these presentations on many factors, including patient safety and veteran satisfaction with their health care. We will also seek to understand how many total participants attend each presentation, as we currently have data only from participants who completed the satisfaction survey.
We invite faculty members from all VA AMCs and training sites to attend future presentations. Information about upcoming presentations is disseminated across multiple VA listservs; you can also e-mail the authors to receive notification of future presentations.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.
1. US Department of Veterans Affairs, Office of Academic Affiliations. 2017 statistics: health professions trainees. https://www.va.gov/OAA/docs/OAA_Statistics.pdf. Accessed September 6, 2019.
2. Chang BK, Brannen JL. The Veterans Access, Choice, and Accountability Act of 2014: examining graduate medical education enhancement in the Department of Veterans Affairs. Acad Med. 2015;90(9):1196-1198.
3. Lee J, Sanders K, Cox M. Honoring those who have served: how can health professionals provide optimal care for members of the military, veterans, and their families? Acad Med. 2014;89(9):1198-1200.
4. Houston TK, Ferenchick GS, Clark JM, et al. Faculty development needs. J Gen Intern Med. 2004;19(4):375-379.
5. Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency based medical education. Acad Med. 2011;86(4):460-467.
6. Steinert Y, Mann K, Centeno A, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526.
7. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769-786.
8. Lee SM, Lee MC, Reed DA, et al. Success of a faculty development program for teachers at the Mayo Clinic. J Grad Med Educ. 2014;6(4):704-708.
9. Topor DR, Roberts DH. Faculty development programming at academic medical centers: identifying financial benefits and value. Med Sci Educ. 2016;26(3):417-419.
10. Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
11. Maloney S, Haas R, Keating JL, et al. Breakeven, cost benefit, cost effectiveness, and willingness to pay for web-based versus face-to-face education delivery for health professionals. J Med Internet Res. 2012;14(2):e47.
12. Clark JM, Houston TK, Kolodner K, Branch WT, Levine RB, Kern DE. Teaching the teachers: national survey of faculty development in departments of medicine of U.S. teaching hospitals. J Gen Intern Med. 2004;19(3):205-214.
13. Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: helping faculty become better teachers and agents of educational change. Acad Med. 2006;81(11):941-944.
14. Topor DR, Budson AE. A framework for faculty development programming at VA and non-VA Academic Medical.
Previously healthy patients hospitalized for sepsis show increased mortality
WASHINGTON – Although severe, community-acquired sepsis in previously healthy U.S. adults is relatively uncommon, it occurs often enough to strike about 40,000 people annually, and when previously healthy people are hospitalized for severe sepsis, their rate of in-hospital mortality was double the rate in people with one or more comorbidities who have severe, community-acquired sepsis, based on a review of almost 7 million Americans hospitalized for sepsis.
The findings “underscore the importance of improving public awareness of sepsis and emphasizing early sepsis recognition and treatment in all patients,” including those without comorbidities, Chanu Rhee, MD, said at an annual scientific meeting on infectious diseases. He hypothesized that the increased sepsis mortality among previously healthy patients may have stemmed from factors such as delayed sepsis recognition resulting in hospitalization at a more advanced stage and less aggressive management.
In addition, “the findings provide context for high-profile reports about sepsis death in previously healthy people,” said Dr. Rhee, an infectious diseases and critical care physician at Brigham and Women’s Hospital in Boston. Dr. Rhee and associates found that, among patients hospitalized with what the researchers defined as “community-acquired” sepsis, 3% were judged previously healthy by having no identified major or minor comorbidity or pregnancy at the time of hospitalization, a percentage that – while small – still translates into roughly 40,000 such cases annually in the United States. That helps explain why every so often a headline appears about a famous person who died suddenly and unexpectedly from sepsis, he noted.
The study used data collected on hospitalized U.S. patients in the Cerner Health Facts, HCA Healthcare, and Institute for Health Metrics and Evaluation databases, which included about 6.7 million people total including 337,983 identified as having community-acquired sepsis, defined as patients who met the criteria for adult sepsis advanced by the Centers for Disease Control and Prevention within 2 days of their hospital admission. The researchers looked further into the hospital records of these patients and divided them into patients with one or more major comorbidities (96% of the cohort), patients who were pregnant or had a “minor” comorbidity such as a lipid disorder, benign neoplasm, or obesity (1% of the study group), or those with no chronic comorbidity (3%; the subgroup the researchers deemed previously healthy).
In a multivariate analysis that adjusted for patients’ age, sex, race, infection site, and illness severity at the time of hospital admission the researchers found that the rate of in-hospital death among the previously healthy patients was exactly twice the rate of those who had at least one major chronic comorbidity, Dr. Rhee reported. Differences in the treatment received by the previously-healthy patients or in their medical status compared with patients with a major comorbidity suggested that the previously health patients were sicker. They had a higher rate of mechanical ventilation, 30%, compared with about 18% for those with a comorbidity; a higher rate of acute kidney injury, about 43% in those previously healthy and 28% in those with a comorbidity; and a higher percentage had an elevated lactate level, about 41% among the previously healthy patients and about 22% among those with a comorbidity.
SOURCE: Alrawashdeh M et al. Open Forum Infect Dis. 2019 Oct 23;6. Abstract 891.
WASHINGTON – Although severe, community-acquired sepsis in previously healthy U.S. adults is relatively uncommon, it occurs often enough to strike about 40,000 people annually, and when previously healthy people are hospitalized for severe sepsis, their rate of in-hospital mortality was double the rate in people with one or more comorbidities who have severe, community-acquired sepsis, based on a review of almost 7 million Americans hospitalized for sepsis.
The findings “underscore the importance of improving public awareness of sepsis and emphasizing early sepsis recognition and treatment in all patients,” including those without comorbidities, Chanu Rhee, MD, said at an annual scientific meeting on infectious diseases. He hypothesized that the increased sepsis mortality among previously healthy patients may have stemmed from factors such as delayed sepsis recognition resulting in hospitalization at a more advanced stage and less aggressive management.
In addition, “the findings provide context for high-profile reports about sepsis death in previously healthy people,” said Dr. Rhee, an infectious diseases and critical care physician at Brigham and Women’s Hospital in Boston. Dr. Rhee and associates found that, among patients hospitalized with what the researchers defined as “community-acquired” sepsis, 3% were judged previously healthy by having no identified major or minor comorbidity or pregnancy at the time of hospitalization, a percentage that – while small – still translates into roughly 40,000 such cases annually in the United States. That helps explain why every so often a headline appears about a famous person who died suddenly and unexpectedly from sepsis, he noted.
The study used data collected on hospitalized U.S. patients in the Cerner Health Facts, HCA Healthcare, and Institute for Health Metrics and Evaluation databases, which included about 6.7 million people total including 337,983 identified as having community-acquired sepsis, defined as patients who met the criteria for adult sepsis advanced by the Centers for Disease Control and Prevention within 2 days of their hospital admission. The researchers looked further into the hospital records of these patients and divided them into patients with one or more major comorbidities (96% of the cohort), patients who were pregnant or had a “minor” comorbidity such as a lipid disorder, benign neoplasm, or obesity (1% of the study group), or those with no chronic comorbidity (3%; the subgroup the researchers deemed previously healthy).
In a multivariate analysis that adjusted for patients’ age, sex, race, infection site, and illness severity at the time of hospital admission the researchers found that the rate of in-hospital death among the previously healthy patients was exactly twice the rate of those who had at least one major chronic comorbidity, Dr. Rhee reported. Differences in the treatment received by the previously-healthy patients or in their medical status compared with patients with a major comorbidity suggested that the previously health patients were sicker. They had a higher rate of mechanical ventilation, 30%, compared with about 18% for those with a comorbidity; a higher rate of acute kidney injury, about 43% in those previously healthy and 28% in those with a comorbidity; and a higher percentage had an elevated lactate level, about 41% among the previously healthy patients and about 22% among those with a comorbidity.
SOURCE: Alrawashdeh M et al. Open Forum Infect Dis. 2019 Oct 23;6. Abstract 891.
WASHINGTON – Although severe, community-acquired sepsis in previously healthy U.S. adults is relatively uncommon, it occurs often enough to strike about 40,000 people annually, and when previously healthy people are hospitalized for severe sepsis, their rate of in-hospital mortality was double the rate in people with one or more comorbidities who have severe, community-acquired sepsis, based on a review of almost 7 million Americans hospitalized for sepsis.
The findings “underscore the importance of improving public awareness of sepsis and emphasizing early sepsis recognition and treatment in all patients,” including those without comorbidities, Chanu Rhee, MD, said at an annual scientific meeting on infectious diseases. He hypothesized that the increased sepsis mortality among previously healthy patients may have stemmed from factors such as delayed sepsis recognition resulting in hospitalization at a more advanced stage and less aggressive management.
In addition, “the findings provide context for high-profile reports about sepsis death in previously healthy people,” said Dr. Rhee, an infectious diseases and critical care physician at Brigham and Women’s Hospital in Boston. Dr. Rhee and associates found that, among patients hospitalized with what the researchers defined as “community-acquired” sepsis, 3% were judged previously healthy by having no identified major or minor comorbidity or pregnancy at the time of hospitalization, a percentage that – while small – still translates into roughly 40,000 such cases annually in the United States. That helps explain why every so often a headline appears about a famous person who died suddenly and unexpectedly from sepsis, he noted.
The study used data collected on hospitalized U.S. patients in the Cerner Health Facts, HCA Healthcare, and Institute for Health Metrics and Evaluation databases, which included about 6.7 million people total including 337,983 identified as having community-acquired sepsis, defined as patients who met the criteria for adult sepsis advanced by the Centers for Disease Control and Prevention within 2 days of their hospital admission. The researchers looked further into the hospital records of these patients and divided them into patients with one or more major comorbidities (96% of the cohort), patients who were pregnant or had a “minor” comorbidity such as a lipid disorder, benign neoplasm, or obesity (1% of the study group), or those with no chronic comorbidity (3%; the subgroup the researchers deemed previously healthy).
In a multivariate analysis that adjusted for patients’ age, sex, race, infection site, and illness severity at the time of hospital admission the researchers found that the rate of in-hospital death among the previously healthy patients was exactly twice the rate of those who had at least one major chronic comorbidity, Dr. Rhee reported. Differences in the treatment received by the previously-healthy patients or in their medical status compared with patients with a major comorbidity suggested that the previously health patients were sicker. They had a higher rate of mechanical ventilation, 30%, compared with about 18% for those with a comorbidity; a higher rate of acute kidney injury, about 43% in those previously healthy and 28% in those with a comorbidity; and a higher percentage had an elevated lactate level, about 41% among the previously healthy patients and about 22% among those with a comorbidity.
SOURCE: Alrawashdeh M et al. Open Forum Infect Dis. 2019 Oct 23;6. Abstract 891.
REPORTING FROM ID WEEK 2019
Using Voogle to Search Within Patient Records in the VA Corporate Data Warehouse
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
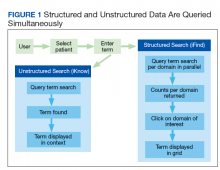
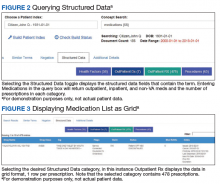
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
Letters: Reframing Clinician Distress: Moral Injury Not Burnout
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie ([email protected])
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie ([email protected])
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta ([email protected])
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie ([email protected])
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
Atraumatic splenic rupture in acute myeloid leukemia
A 50-year-old man with acute myeloid leukemia (AML) with a complex karyotype was admitted to the hospital with several days of dull, left-sided abdominal pain. His most recent bone marrow biopsy showed 30% blasts, and immunophenotyping was suggestive of persistent AML (CD13+, CD34+, CD117+, CD33+, CD7+, MPO–). He was on treatment with venetoclax and cytarabine after induction therapy had failed.
On admission, his heart rate was 101 beats per minute and his blood pressure was 122/85 mm Hg. Abdominal examination revealed mild distention, hepatomegaly, and previously known massive splenomegaly, with the splenic tip extending to the umbilicus, and mild tenderness.
Results of laboratory testing revealed persistent pancytopenia:
- Hemoglobin level 6.8 g/dL (reference range 13.0–17.0)
- Total white blood cell count 0.8 × 109/L (4.5–11.0)
- Platelet count 8 × 109/L (150–400).
The next day, he developed severe, acute-onset left-sided abdominal pain. A check of vital signs showed worsening sinus tachycardia at 132 beats per minute and a drop in blood pressure to 90/56 mm Hg. He had worsening diffuse abdominal tenderness with sluggish bowel sounds. His hemoglobin concentration was 6.4 g/dL and platelet count 12 × 109/L.
He received supportive transfusions of blood products. Surgical exploration was deemed risky, given his overall condition and severe thrombocytopenia. Splenic angiography showed no evidence of pseudoaneurysm or focal contrast extravasation. He underwent empiric embolization of the midsplenic artery, after which his hemodynamic status stabilized. He died 4 weeks later of acute respiratory failure from pneumonia.
SPLENIC RUPTURE IN AML
Atraumatic splenic rupture is rare but potentially life-threatening, especially if the diagnosis is delayed. Conditions that can cause splenomegaly and predispose to rupture include infection (infectious mononucleosis, malaria), malignant hematologic disorders (leukemia, lymphoma), other neoplasms, and amyloidosis.1
The literature includes a few reports of splenic rupture in patients with AML.2–4 The proposed mechanisms include bleeding from infarction sites or tumor foci, dysregulated hemostasis, and leukostasis.
The classic presentation of splenic rupture is acute-onset left-sided abdominal pain associated with hypotension and decreasing hemoglobin levels. CT of the abdomen is confirmatory, and resuscitation with crystalloids and blood products is a vital initial step in management. Choice of treatment depends on the patient’s surgical risk and hemodynamic status; options include conservative medical management, splenic artery embolization, and exploratory laparotomy.
In patients with AML and splenomegaly presenting with acute abdominal pain, clinicians need to be aware of this potential hematologic emergency.
- Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg 2009; 96(10):1114–1121. doi:10.1002/bjs.6737
- Gardner JA, Bao L, Ornstein DL. Spontaneous splenic rupture in acute myeloid leukemia with mixed-lineage leukemia gene rearrangement. Med Rep Case Stud 2016; 1:119. doi:10.4172/2572-5130.1000119
- Zeidan AM, Mitchell M, Khatri R, et al. Spontaneous splenic rupture during induction chemotherapy for acute myeloid leukemia. Leuk Lymphoma 2014; 55(1):209–212. doi:10.3109/10428194.2013.796060
- Fahmi Y, Elabbasi T, Khaiz D, et al. Splenic spontaneous rupture associated with acute myeloïd leukemia: report of a case and literature review. Surgery Curr Res 2014; 4:170. doi:10.4172/2161-1076.1000170
A 50-year-old man with acute myeloid leukemia (AML) with a complex karyotype was admitted to the hospital with several days of dull, left-sided abdominal pain. His most recent bone marrow biopsy showed 30% blasts, and immunophenotyping was suggestive of persistent AML (CD13+, CD34+, CD117+, CD33+, CD7+, MPO–). He was on treatment with venetoclax and cytarabine after induction therapy had failed.
On admission, his heart rate was 101 beats per minute and his blood pressure was 122/85 mm Hg. Abdominal examination revealed mild distention, hepatomegaly, and previously known massive splenomegaly, with the splenic tip extending to the umbilicus, and mild tenderness.
Results of laboratory testing revealed persistent pancytopenia:
- Hemoglobin level 6.8 g/dL (reference range 13.0–17.0)
- Total white blood cell count 0.8 × 109/L (4.5–11.0)
- Platelet count 8 × 109/L (150–400).
The next day, he developed severe, acute-onset left-sided abdominal pain. A check of vital signs showed worsening sinus tachycardia at 132 beats per minute and a drop in blood pressure to 90/56 mm Hg. He had worsening diffuse abdominal tenderness with sluggish bowel sounds. His hemoglobin concentration was 6.4 g/dL and platelet count 12 × 109/L.
He received supportive transfusions of blood products. Surgical exploration was deemed risky, given his overall condition and severe thrombocytopenia. Splenic angiography showed no evidence of pseudoaneurysm or focal contrast extravasation. He underwent empiric embolization of the midsplenic artery, after which his hemodynamic status stabilized. He died 4 weeks later of acute respiratory failure from pneumonia.
SPLENIC RUPTURE IN AML
Atraumatic splenic rupture is rare but potentially life-threatening, especially if the diagnosis is delayed. Conditions that can cause splenomegaly and predispose to rupture include infection (infectious mononucleosis, malaria), malignant hematologic disorders (leukemia, lymphoma), other neoplasms, and amyloidosis.1
The literature includes a few reports of splenic rupture in patients with AML.2–4 The proposed mechanisms include bleeding from infarction sites or tumor foci, dysregulated hemostasis, and leukostasis.
The classic presentation of splenic rupture is acute-onset left-sided abdominal pain associated with hypotension and decreasing hemoglobin levels. CT of the abdomen is confirmatory, and resuscitation with crystalloids and blood products is a vital initial step in management. Choice of treatment depends on the patient’s surgical risk and hemodynamic status; options include conservative medical management, splenic artery embolization, and exploratory laparotomy.
In patients with AML and splenomegaly presenting with acute abdominal pain, clinicians need to be aware of this potential hematologic emergency.
A 50-year-old man with acute myeloid leukemia (AML) with a complex karyotype was admitted to the hospital with several days of dull, left-sided abdominal pain. His most recent bone marrow biopsy showed 30% blasts, and immunophenotyping was suggestive of persistent AML (CD13+, CD34+, CD117+, CD33+, CD7+, MPO–). He was on treatment with venetoclax and cytarabine after induction therapy had failed.
On admission, his heart rate was 101 beats per minute and his blood pressure was 122/85 mm Hg. Abdominal examination revealed mild distention, hepatomegaly, and previously known massive splenomegaly, with the splenic tip extending to the umbilicus, and mild tenderness.
Results of laboratory testing revealed persistent pancytopenia:
- Hemoglobin level 6.8 g/dL (reference range 13.0–17.0)
- Total white blood cell count 0.8 × 109/L (4.5–11.0)
- Platelet count 8 × 109/L (150–400).
The next day, he developed severe, acute-onset left-sided abdominal pain. A check of vital signs showed worsening sinus tachycardia at 132 beats per minute and a drop in blood pressure to 90/56 mm Hg. He had worsening diffuse abdominal tenderness with sluggish bowel sounds. His hemoglobin concentration was 6.4 g/dL and platelet count 12 × 109/L.
He received supportive transfusions of blood products. Surgical exploration was deemed risky, given his overall condition and severe thrombocytopenia. Splenic angiography showed no evidence of pseudoaneurysm or focal contrast extravasation. He underwent empiric embolization of the midsplenic artery, after which his hemodynamic status stabilized. He died 4 weeks later of acute respiratory failure from pneumonia.
SPLENIC RUPTURE IN AML
Atraumatic splenic rupture is rare but potentially life-threatening, especially if the diagnosis is delayed. Conditions that can cause splenomegaly and predispose to rupture include infection (infectious mononucleosis, malaria), malignant hematologic disorders (leukemia, lymphoma), other neoplasms, and amyloidosis.1
The literature includes a few reports of splenic rupture in patients with AML.2–4 The proposed mechanisms include bleeding from infarction sites or tumor foci, dysregulated hemostasis, and leukostasis.
The classic presentation of splenic rupture is acute-onset left-sided abdominal pain associated with hypotension and decreasing hemoglobin levels. CT of the abdomen is confirmatory, and resuscitation with crystalloids and blood products is a vital initial step in management. Choice of treatment depends on the patient’s surgical risk and hemodynamic status; options include conservative medical management, splenic artery embolization, and exploratory laparotomy.
In patients with AML and splenomegaly presenting with acute abdominal pain, clinicians need to be aware of this potential hematologic emergency.
- Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg 2009; 96(10):1114–1121. doi:10.1002/bjs.6737
- Gardner JA, Bao L, Ornstein DL. Spontaneous splenic rupture in acute myeloid leukemia with mixed-lineage leukemia gene rearrangement. Med Rep Case Stud 2016; 1:119. doi:10.4172/2572-5130.1000119
- Zeidan AM, Mitchell M, Khatri R, et al. Spontaneous splenic rupture during induction chemotherapy for acute myeloid leukemia. Leuk Lymphoma 2014; 55(1):209–212. doi:10.3109/10428194.2013.796060
- Fahmi Y, Elabbasi T, Khaiz D, et al. Splenic spontaneous rupture associated with acute myeloïd leukemia: report of a case and literature review. Surgery Curr Res 2014; 4:170. doi:10.4172/2161-1076.1000170
- Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg 2009; 96(10):1114–1121. doi:10.1002/bjs.6737
- Gardner JA, Bao L, Ornstein DL. Spontaneous splenic rupture in acute myeloid leukemia with mixed-lineage leukemia gene rearrangement. Med Rep Case Stud 2016; 1:119. doi:10.4172/2572-5130.1000119
- Zeidan AM, Mitchell M, Khatri R, et al. Spontaneous splenic rupture during induction chemotherapy for acute myeloid leukemia. Leuk Lymphoma 2014; 55(1):209–212. doi:10.3109/10428194.2013.796060
- Fahmi Y, Elabbasi T, Khaiz D, et al. Splenic spontaneous rupture associated with acute myeloïd leukemia: report of a case and literature review. Surgery Curr Res 2014; 4:170. doi:10.4172/2161-1076.1000170
Severe hypercalcemia in a 54-year-old woman
A morbidly obese 54-year-old woman presented to the emergency department after experiencing generalized abdominal pain for 3 days. She rated the pain as 5 on a scale of 10 and described it as dull, cramping, waxing and waning, not radiating, and not relieved with changes of position—in fact, not alleviated by anything she had tried. Her pain was associated with nausea and 1 episode of vomiting. She also experienced constipation before the onset of pain.
She denied recent trauma, recent travel, diarrhea, fevers, weakness, shortness of breath, chest pain, other muscle pains, or recent changes in diet. She also denied having this pain in the past. She said she had unintentionally lost some weight but was not certain how much. She denied tobacco, alcohol, or illicit drug use. She had no history of surgery.
Her medical history included hypertension, anemia, and uterine fibroids. Her current medications included losartan, hydrochlorothiazide, and albuterol. She had no family history of significant disease.
INITIAL EVALUATION AND MANAGEMENT
On admission, her temperature was 97.8°F (36.6°C), heart rate 100 beats per minute, blood pressure 136/64 mm Hg, respiratory rate 18 breaths per minute, oxygen saturation 97% on room air, weight 130.6 kg, and body mass index 35 kg/m2.
She was alert and oriented to person, place, and time. She was in mild discomfort but no distress. Her lungs were clear to auscultation, with no wheezing or crackles. Heart rate and rhythm were regular, with no extra heart sounds or murmurs. Bowel sounds were normal in all 4 quadrants, with tenderness to palpation of the epigastric area, but with no guarding or rebound tenderness.
Laboratory test results
Notable results of blood testing at presentation were as follows:
- Hemoglobin 8.2 g/dL (reference range 12.3–15.3)
- Hematocrit 26% (41–50)
- Mean corpuscular volume 107 fL (80–100)
- Blood urea nitrogen 33 mg/dL (8–21); 6 months earlier it was 16
- Serum creatinine 3.6 mg/dL (0.58–0.96); 6 months earlier, it was 0.75
- Albumin 3.3 g/dL (3.5–5)
- Calcium 18.4 mg/dL (8.4–10.2); 6 months earlier, it was 9.6
- Corrected calcium 19 mg/dL.
Findings on imaging, electrocardiography
Chest radiography showed no acute cardiopulmonary abnormalities. Abdominal computed tomography without contrast showed no abnormalities within the pancreas and no evidence of inflammation or obstruction. Electrocardiography showed sinus tachycardia.
DIFFERENTIAL DIAGNOSIS
1. Which is the most likely cause of this patient’s symptoms?
- Primary hyperparathyroidism
- Malignancy
- Her drug therapy
- Familial hypercalcemic hypocalciuria
In total, her laboratory results were consistent with macrocytic anemia, severe hypercalcemia, and acute kidney injury, and she had generalized symptoms.
Primary hyperparathyroidism
A main cause of hypercalcemia is primary hyperparathyroidism, and this needs to be ruled out. Benign adenomas are the most common cause of primary hyperparathyroidism, and a risk factor for benign adenoma is exposure to therapeutic levels of radiation.3
In hyperparathyroidism, there is an increased secretion of parathyroid hormone (PTH), which has multiple effects including increased reabsorption of calcium from the urine, increased excretion of phosphate, and increased expression of 1,25-hydroxyvitamin D hydroxylase to activate vitamin D. PTH also stimulates osteoclasts to increase their expression of receptor activator of nuclear factor kappa B ligand (RANKL), which has a downstream effect on osteoclast precursors to cause bone reabsorption.3
Inherited primary hyperparathyroidism tends to present at a younger age, with multiple overactive parathyroid glands.3 Given our patient’s age, inherited primary hyparathyroidism is thus less likely.
Malignancy
The probability that malignancy is causing the hypercalcemia increases with calcium levels greater than 13 mg/dL. Epidemiologically, in hospitalized patients with hypercalcemia, the source tends to be malignancy.4 Typically, patients who develop hypercalcemia from malignancy have a worse prognosis.5
Solid tumors and leukemias can cause hypercalcemia. The mechanisms include humoral factors secreted by the malignancy, local osteolysis due to tumor invasion of bone, and excessive absorption of calcium due to excess vitamin D produced by malignancies.5 The cancers that most frequently cause an increase in calcium resorption are lung cancer, renal cancer, breast cancer, and multiple myeloma.1
Solid tumors with no bone metastasis and non-Hodgkin lymphoma that release PTH-related protein (PTHrP) cause humoral hypercalcemia in malignancy. The patient is typically in an advanced stage of disease. PTHrP increases serum calcium levels by decreasing the kidney’s ability to excrete calcium and by increasing bone turnover. It has no effect on intestinal absorption because of its inability to stimulate activated vitamin D3. Thus, the increase in systemic calcium comes directly from breakdown of bone and inability to excrete the excess.
PTHrP has a unique role in breast cancer: it is released locally in areas where cancer cells have metastasized to bone, but it does not cause a systemic effect. Bone resorption occurs in areas of metastasis and results from an increase in expression of RANKL and RANK in osteoclasts in response to the effects of PTHrP, leading to an increase in the production of osteoclastic cells.1
Tamoxifen, an endocrine therapy often used in breast cancer, also causes a release of bone-reabsorbing factors from tumor cells, which can partially contribute to hypercalcemia.5
Myeloma cells secrete RANKL, which stimulates osteoclastic activity, and they also release interleukin 6 (IL-6) and activating macrophage inflammatory protein alpha. Serum testing usually shows low or normal intact PTH, PTHrP, and 1,25-dihydroxyvitamin D.1
Patients with multiple myeloma have a worse prognosis if they have a high red blood cell distribution width, a condition shown to correlate with malnutrition, leading to deficiencies in vitamin B12 and to poor response to treatment.6 Up to 14% of patients with multiple myeloma have vitamin B12 deficiency.7
Our patient’s recent weight loss and severe hypercalcemia raise suspicion of malignancy. Further, her obesity makes proper routine breast examination difficult and thus increases the chance of undiagnosed breast cancer.8 Her decrease in renal function and her anemia complicated by hypercalcemia also raise suspicion of multiple myeloma.
Hypercalcemia due to drug therapy
Thiazide diuretics, lithium, teriparatide, and vitamin A in excessive amounts can raise the serum calcium concentration.5 Our patient was taking a thiazide for hypertension, but her extremely high calcium level places drug-induced hypercalcemia as the sole cause lower on the differential list.
Familial hypercalcemic hypocalciuria
Familial hypercalcemic hypocalciuria is a rare autosomal-dominant cause of hypercalcemia in which the ability of the body (and especially the kidneys) to sense levels of calcium is impaired, leading to a decrease in excretion of calcium in the urine.3 Very high calcium levels are rare in hypercalcemic hypocalciuria.3 In our patient with a corrected calcium concentration of nearly 19 mg/dL, familial hypercalcemic hypocalciuria is very unlikely to be the cause of the hypercalcemia.
WHAT ARE THE NEXT STEPS IN THE WORKUP?
As hypercalcemia has been confirmed, the intact PTH level should be checked to determine whether the patient’s condition is PTH-mediated. If the PTH level is in the upper range of normal or is minimally elevated, primary hyperparathyroidism is likely. Elevated PTH confirms primary hyperparathyroidism. A low-normal or low intact PTH confirms a non-PTH-mediated process, and once this is confirmed, PTHrP levels should be checked. An elevated PTHrP suggests humoral hypercalcemia of malignancy. Serum protein electrophoresis, urine protein electrophoresis, and a serum light chain assay should be performed to rule out multiple myeloma.
Vitamin D toxicity is associated with high concentrations of 1,25-dihydroxyvitamin D and 25-hydroxyvitamin D metabolites. These levels should be checked in this patient.
Other disorders that cause hypercalcemia are vitamin A toxicity and hyperthyroidism, so vitamin A and thyroid-stimulating hormone levels should also be checked.5
CASE CONTINUED
After further questioning, the patient said that she had had lower back pain about 1 to 2 weeks before coming to the emergency room; her primary care doctor had said the pain was likely from muscle strain. The pain had almost resolved but was still present.
The results of further laboratory testing were as follows:
- Serum PTH 11 pg/mL (15–65)
- PTHrP 3.4 pmol/L (< 2.0)
- Protein electrophoresis showed a monoclonal (M) spike of 0.2 g/dL (0)
- Activated vitamin D < 5 ng/mL (19.9–79.3)
- Vitamin A 7.2 mg/dL (33.1–100)
- Vitamin B12 194 pg/mL (239–931)
- Thyroid-stimulating hormone 1.21 mIU/ L (0.47–4.68
- Free thyroxine 1.27 ng/dL (0.78–2.19)
- Iron 103 µg/dL (37–170)
- Total iron-binding capacity 335 µg/dL (265–497)
- Transferrin 248 mg/dL (206–381)
- Ferritin 66 ng/mL (11.1–264)
- Urine protein (random) 100 mg/dL (0–20)
- Urine microalbumin (random) 5.9 mg/dL (0–1.6)
- Urine creatinine clearance 88.5 mL/min (88–128)
- Urine albumin-creatinine ratio 66.66 mg/g (< 30).
Imaging reports
A nuclear bone scan showed increased bone uptake in the hip and both shoulders, consistent with arthritis, and increased activity in 2 of the lower left ribs, associated with rib fractures secondary to lytic lesions. A skeletal survey at a later date showed multiple well-circumscribed “punched-out” lytic lesions in both forearms and both femurs.
2. What should be the next step in this patient’s management?
- Intravenous (IV) fluids
- Calcitonin
- Bisphosphonate treatment
- Denosumab
- Hemodialysis
Initial treatment of severe hypercalcemia includes the following:
Start IV isotonic fluids at a rate of 150 mL/h (if the patient is making urine) to maintain urine output at more than 100 mL/h. Closely monitor urine output.
Give calcitonin 4 IU/kg in combination with IV fluids to reduce calcium levels within the first 12 to 48 hours of treatment.
Give a bisphosphonate, eg, zoledronic acid 4 mg over 15 minutes, or pamidronate 60 to 90 mg over 2 hours. Zoledronic acid is preferred in malignancy-induced hypercalcemia because it is more potent. Doses should be adjusted in patients with renal failure.
Give denosumab if hypercalcemia is refractory to bisphosphonates, or when bisphosphonates cannot be used in renal failure.9
Hemodialysis is performed in patients who have significant neurologic symptoms irrespective of acute renal insufficiency.
Our patient was started on 0.9% sodium chloride at a rate of 150 mL/h for severe hypercalcemia. Zoledronic acid 4 mg IV was given once. These measures lowered her calcium level and lessened her acute kidney injury.
ADDITIONAL FINDINGS
Urine testing was positive for Bence Jones protein. Immune electrophoresis, performed because of suspicion of multiple myeloma, showed an elevated level of kappa light chains at 806.7 mg/dL (0.33–1.94) and normal lambda light chains at 0.62 mg/dL (0.57–2.63). The immunoglobulin G level was low at 496 mg/dL (610–1,660). In patients with severe hypercalcemia, these results point to a diagnosis of malignancy. Bone marrow aspiration study showed greater than 10% plasma cells, confirming multiple myeloma.
MULTIPLE MYELOMA
The diagnosis of multiple myeloma is based in part on the presence of 10% or more of clonal bone marrow plasma cells10 and of specific end-organ damage (anemia, hypercalcemia, renal insufficiency, or bone lesions).9
Bone marrow clonality can be shown by the ratio of kappa to lambda light chains as detected with immunohistochemistry, immunofluorescence, or flow cytometry.11 The normal ratio is 0.26 to 1.65 for a patient with normal kidney function. In this patient, however, the ratio was 1,301.08 (806.67 kappa to 0.62 lambda), which was extremely out of range. The patient’s bone marrow biopsy results revealed the presence of 15% clonal bone marrow plasma cells.
Multiple myeloma causes osteolytic lesions through increased activation of osteoclast activating factor that stimulates the growth of osteoclast precursors. At the same time, it inhibits osteoblast formation via multiple pathways, including the action of sclerostin.11 Our patient had lytic lesions in 2 left lower ribs and in both forearms and femurs.
Hypercalcemia in multiple myeloma is attributed to 2 main factors: bone breakdown and macrophage overactivation. Multiple myeloma cells increase the release of macrophage inflammatory protein 1-alpha and tumor necrosis factor, which are inflammatory proteins that cause an increase in macrophages, which cause an increase in calcitriol.11 As noted, our patient’s calcium level at presentation was 18.4 mg/dL uncorrected and 18.96 mg/dL corrected.
Cast nephropathy can occur in the distal tubules from the increased free light chains circulating and combining with Tamm-Horsfall protein, which in turn causes obstruction and local inflammation,12 leading to a rise in creatinine levels and resulting in acute kidney injury,12 as in our patient.
TREATMENT CONSIDERATIONS IN MULTIPLE MYELOMA
Our patient was referred to an oncologist for management.
In the management of multiple myeloma, the patient’s quality of life needs to be considered. With the development of new agents to combat the damages of the osteolytic effects, there is hope for improving quality of life.13,14 New agents under study include anabolic agents such as antisclerostin and anti-Dickkopf-1, which promote osteoblastogenesis, leading to bone formation, with the possibility of repairing existing damage.15
TAKE-HOME POINTS
- If hypercalcemia is mild to moderate, consider primary hyperparathyroidism.
- Identify patients with severe symptoms of hypercalcemia such as volume depletion, acute kidney injury, arrhythmia, or seizures.
- Confirm severe cases of hypercalcemia and treat severe cases effectively.
- Severe hypercalcemia may need further investigation into a potential underlying malignancy.
- Sternlicht H, Glezerman IG. Hypercalcemia of malignancy and new treatment options. Ther Clin Risk Manag 2015; 11:1779–1788. doi:10.2147/TCRM.S83681
- Ahmed R, Hashiba K. Reliability of QT intervals as indicators of clinical hypercalcemia. Clin Cardiol 1988; 11(6):395–400. doi:10.1002/clc.4960110607
- Bilezikian JP, Cusano NE, Khan AA, Liu JM, Marcocci C, Bandeira F. Primary hyperparathyroidism. Nat Rev Dis Primers 2016; 2:16033. doi:10.1038/nrdp.2016.33
- Kuchay MS, Kaur P, Mishra SK, Mithal A. The changing profile of hypercalcemia in a tertiary care setting in North India: an 18-month retrospective study. Clin Cases Miner Bone Metab 2017; 14(2):131–135. doi:10.11138/ccmbm/2017.14.1.131
- Rosner MH, Dalkin AC. Onco-nephrology: the pathophysiology and treatment of malignancy-associated hypercalcemia. Clin J Am Soc Nephrol 2012; 7(10):1722–1729. doi:10.2215/CJN.02470312
- Ai L, Mu S, Hu Y. Prognostic role of RDW in hematological malignancies: a systematic review and meta-analysis. Cancer Cell Int 2018; 18:61. doi:10.1186/s12935-018-0558-3
- Baz R, Alemany C, Green R, Hussein MA. Prevalence of vitamin B12 deficiency in patients with plasma cell dyscrasias: a retrospective review. Cancer 2004; 101(4):790–795. doi:10.1002/cncr.20441
- Elmore JG, Carney PA, Abraham LA, et al. The association between obesity and screening mammography accuracy. Arch Intern Med 2004; 164(10):1140–1147. doi:10.1001/archinte.164.10.1140
- Gerecke C, Fuhrmann S, Strifler S, Schmidt-Hieber M, Einsele H, Knop S. The diagnosis and treatment of multiple myeloma. Dtsch Arztebl Int 2016; 113(27–28):470–476. doi:10.3238/arztebl.2016.0470
- Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol 2016; 91(7):719–734. doi:10.1002/ajh.24402
- Silbermann R, Roodman GD. Myeloma bone disease: pathophysiology and management. J Bone Oncol 2013; 2(2):59–69. doi:10.1016/j.jbo.2013.04.001
- Doshi M, Lahoti A, Danesh FR, Batuman V, Sanders PW; American Society of Nephrology Onco-Nephrology Forum. Paraprotein-related kidney disease: kidney injury from paraproteins—what determines the site of injury? Clin J Am Soc Nephrol 2016; 11(12):2288–2294. doi:10.2215/CJN.02560316
- Reece D. Update on the initial therapy of multiple myeloma. Am Soc Clin Oncol Educ Book 2013. doi:10.1200/EdBook_AM.2013.33.e307
- Nishida H. Bone-targeted agents in multiple myeloma. Hematol Rep 2018; 10(1):7401. doi:10.4081/hr.2018.7401
- Ring ES, Lawson MA, Snowden JA, Jolley I, Chantry AD. New agents in the treatment of myeloma bone disease. Calcif Tissue Int 2018; 102(2):196–209. doi:10.1007/s00223-017-0351-7
A morbidly obese 54-year-old woman presented to the emergency department after experiencing generalized abdominal pain for 3 days. She rated the pain as 5 on a scale of 10 and described it as dull, cramping, waxing and waning, not radiating, and not relieved with changes of position—in fact, not alleviated by anything she had tried. Her pain was associated with nausea and 1 episode of vomiting. She also experienced constipation before the onset of pain.
She denied recent trauma, recent travel, diarrhea, fevers, weakness, shortness of breath, chest pain, other muscle pains, or recent changes in diet. She also denied having this pain in the past. She said she had unintentionally lost some weight but was not certain how much. She denied tobacco, alcohol, or illicit drug use. She had no history of surgery.
Her medical history included hypertension, anemia, and uterine fibroids. Her current medications included losartan, hydrochlorothiazide, and albuterol. She had no family history of significant disease.
INITIAL EVALUATION AND MANAGEMENT
On admission, her temperature was 97.8°F (36.6°C), heart rate 100 beats per minute, blood pressure 136/64 mm Hg, respiratory rate 18 breaths per minute, oxygen saturation 97% on room air, weight 130.6 kg, and body mass index 35 kg/m2.
She was alert and oriented to person, place, and time. She was in mild discomfort but no distress. Her lungs were clear to auscultation, with no wheezing or crackles. Heart rate and rhythm were regular, with no extra heart sounds or murmurs. Bowel sounds were normal in all 4 quadrants, with tenderness to palpation of the epigastric area, but with no guarding or rebound tenderness.
Laboratory test results
Notable results of blood testing at presentation were as follows:
- Hemoglobin 8.2 g/dL (reference range 12.3–15.3)
- Hematocrit 26% (41–50)
- Mean corpuscular volume 107 fL (80–100)
- Blood urea nitrogen 33 mg/dL (8–21); 6 months earlier it was 16
- Serum creatinine 3.6 mg/dL (0.58–0.96); 6 months earlier, it was 0.75
- Albumin 3.3 g/dL (3.5–5)
- Calcium 18.4 mg/dL (8.4–10.2); 6 months earlier, it was 9.6
- Corrected calcium 19 mg/dL.
Findings on imaging, electrocardiography
Chest radiography showed no acute cardiopulmonary abnormalities. Abdominal computed tomography without contrast showed no abnormalities within the pancreas and no evidence of inflammation or obstruction. Electrocardiography showed sinus tachycardia.
DIFFERENTIAL DIAGNOSIS
1. Which is the most likely cause of this patient’s symptoms?
- Primary hyperparathyroidism
- Malignancy
- Her drug therapy
- Familial hypercalcemic hypocalciuria
In total, her laboratory results were consistent with macrocytic anemia, severe hypercalcemia, and acute kidney injury, and she had generalized symptoms.
Primary hyperparathyroidism
A main cause of hypercalcemia is primary hyperparathyroidism, and this needs to be ruled out. Benign adenomas are the most common cause of primary hyperparathyroidism, and a risk factor for benign adenoma is exposure to therapeutic levels of radiation.3
In hyperparathyroidism, there is an increased secretion of parathyroid hormone (PTH), which has multiple effects including increased reabsorption of calcium from the urine, increased excretion of phosphate, and increased expression of 1,25-hydroxyvitamin D hydroxylase to activate vitamin D. PTH also stimulates osteoclasts to increase their expression of receptor activator of nuclear factor kappa B ligand (RANKL), which has a downstream effect on osteoclast precursors to cause bone reabsorption.3
Inherited primary hyperparathyroidism tends to present at a younger age, with multiple overactive parathyroid glands.3 Given our patient’s age, inherited primary hyparathyroidism is thus less likely.
Malignancy
The probability that malignancy is causing the hypercalcemia increases with calcium levels greater than 13 mg/dL. Epidemiologically, in hospitalized patients with hypercalcemia, the source tends to be malignancy.4 Typically, patients who develop hypercalcemia from malignancy have a worse prognosis.5
Solid tumors and leukemias can cause hypercalcemia. The mechanisms include humoral factors secreted by the malignancy, local osteolysis due to tumor invasion of bone, and excessive absorption of calcium due to excess vitamin D produced by malignancies.5 The cancers that most frequently cause an increase in calcium resorption are lung cancer, renal cancer, breast cancer, and multiple myeloma.1
Solid tumors with no bone metastasis and non-Hodgkin lymphoma that release PTH-related protein (PTHrP) cause humoral hypercalcemia in malignancy. The patient is typically in an advanced stage of disease. PTHrP increases serum calcium levels by decreasing the kidney’s ability to excrete calcium and by increasing bone turnover. It has no effect on intestinal absorption because of its inability to stimulate activated vitamin D3. Thus, the increase in systemic calcium comes directly from breakdown of bone and inability to excrete the excess.
PTHrP has a unique role in breast cancer: it is released locally in areas where cancer cells have metastasized to bone, but it does not cause a systemic effect. Bone resorption occurs in areas of metastasis and results from an increase in expression of RANKL and RANK in osteoclasts in response to the effects of PTHrP, leading to an increase in the production of osteoclastic cells.1
Tamoxifen, an endocrine therapy often used in breast cancer, also causes a release of bone-reabsorbing factors from tumor cells, which can partially contribute to hypercalcemia.5
Myeloma cells secrete RANKL, which stimulates osteoclastic activity, and they also release interleukin 6 (IL-6) and activating macrophage inflammatory protein alpha. Serum testing usually shows low or normal intact PTH, PTHrP, and 1,25-dihydroxyvitamin D.1
Patients with multiple myeloma have a worse prognosis if they have a high red blood cell distribution width, a condition shown to correlate with malnutrition, leading to deficiencies in vitamin B12 and to poor response to treatment.6 Up to 14% of patients with multiple myeloma have vitamin B12 deficiency.7
Our patient’s recent weight loss and severe hypercalcemia raise suspicion of malignancy. Further, her obesity makes proper routine breast examination difficult and thus increases the chance of undiagnosed breast cancer.8 Her decrease in renal function and her anemia complicated by hypercalcemia also raise suspicion of multiple myeloma.
Hypercalcemia due to drug therapy
Thiazide diuretics, lithium, teriparatide, and vitamin A in excessive amounts can raise the serum calcium concentration.5 Our patient was taking a thiazide for hypertension, but her extremely high calcium level places drug-induced hypercalcemia as the sole cause lower on the differential list.
Familial hypercalcemic hypocalciuria
Familial hypercalcemic hypocalciuria is a rare autosomal-dominant cause of hypercalcemia in which the ability of the body (and especially the kidneys) to sense levels of calcium is impaired, leading to a decrease in excretion of calcium in the urine.3 Very high calcium levels are rare in hypercalcemic hypocalciuria.3 In our patient with a corrected calcium concentration of nearly 19 mg/dL, familial hypercalcemic hypocalciuria is very unlikely to be the cause of the hypercalcemia.
WHAT ARE THE NEXT STEPS IN THE WORKUP?
As hypercalcemia has been confirmed, the intact PTH level should be checked to determine whether the patient’s condition is PTH-mediated. If the PTH level is in the upper range of normal or is minimally elevated, primary hyperparathyroidism is likely. Elevated PTH confirms primary hyperparathyroidism. A low-normal or low intact PTH confirms a non-PTH-mediated process, and once this is confirmed, PTHrP levels should be checked. An elevated PTHrP suggests humoral hypercalcemia of malignancy. Serum protein electrophoresis, urine protein electrophoresis, and a serum light chain assay should be performed to rule out multiple myeloma.
Vitamin D toxicity is associated with high concentrations of 1,25-dihydroxyvitamin D and 25-hydroxyvitamin D metabolites. These levels should be checked in this patient.
Other disorders that cause hypercalcemia are vitamin A toxicity and hyperthyroidism, so vitamin A and thyroid-stimulating hormone levels should also be checked.5
CASE CONTINUED
After further questioning, the patient said that she had had lower back pain about 1 to 2 weeks before coming to the emergency room; her primary care doctor had said the pain was likely from muscle strain. The pain had almost resolved but was still present.
The results of further laboratory testing were as follows:
- Serum PTH 11 pg/mL (15–65)
- PTHrP 3.4 pmol/L (< 2.0)
- Protein electrophoresis showed a monoclonal (M) spike of 0.2 g/dL (0)
- Activated vitamin D < 5 ng/mL (19.9–79.3)
- Vitamin A 7.2 mg/dL (33.1–100)
- Vitamin B12 194 pg/mL (239–931)
- Thyroid-stimulating hormone 1.21 mIU/ L (0.47–4.68
- Free thyroxine 1.27 ng/dL (0.78–2.19)
- Iron 103 µg/dL (37–170)
- Total iron-binding capacity 335 µg/dL (265–497)
- Transferrin 248 mg/dL (206–381)
- Ferritin 66 ng/mL (11.1–264)
- Urine protein (random) 100 mg/dL (0–20)
- Urine microalbumin (random) 5.9 mg/dL (0–1.6)
- Urine creatinine clearance 88.5 mL/min (88–128)
- Urine albumin-creatinine ratio 66.66 mg/g (< 30).
Imaging reports
A nuclear bone scan showed increased bone uptake in the hip and both shoulders, consistent with arthritis, and increased activity in 2 of the lower left ribs, associated with rib fractures secondary to lytic lesions. A skeletal survey at a later date showed multiple well-circumscribed “punched-out” lytic lesions in both forearms and both femurs.
2. What should be the next step in this patient’s management?
- Intravenous (IV) fluids
- Calcitonin
- Bisphosphonate treatment
- Denosumab
- Hemodialysis
Initial treatment of severe hypercalcemia includes the following:
Start IV isotonic fluids at a rate of 150 mL/h (if the patient is making urine) to maintain urine output at more than 100 mL/h. Closely monitor urine output.
Give calcitonin 4 IU/kg in combination with IV fluids to reduce calcium levels within the first 12 to 48 hours of treatment.
Give a bisphosphonate, eg, zoledronic acid 4 mg over 15 minutes, or pamidronate 60 to 90 mg over 2 hours. Zoledronic acid is preferred in malignancy-induced hypercalcemia because it is more potent. Doses should be adjusted in patients with renal failure.
Give denosumab if hypercalcemia is refractory to bisphosphonates, or when bisphosphonates cannot be used in renal failure.9
Hemodialysis is performed in patients who have significant neurologic symptoms irrespective of acute renal insufficiency.
Our patient was started on 0.9% sodium chloride at a rate of 150 mL/h for severe hypercalcemia. Zoledronic acid 4 mg IV was given once. These measures lowered her calcium level and lessened her acute kidney injury.
ADDITIONAL FINDINGS
Urine testing was positive for Bence Jones protein. Immune electrophoresis, performed because of suspicion of multiple myeloma, showed an elevated level of kappa light chains at 806.7 mg/dL (0.33–1.94) and normal lambda light chains at 0.62 mg/dL (0.57–2.63). The immunoglobulin G level was low at 496 mg/dL (610–1,660). In patients with severe hypercalcemia, these results point to a diagnosis of malignancy. Bone marrow aspiration study showed greater than 10% plasma cells, confirming multiple myeloma.
MULTIPLE MYELOMA
The diagnosis of multiple myeloma is based in part on the presence of 10% or more of clonal bone marrow plasma cells10 and of specific end-organ damage (anemia, hypercalcemia, renal insufficiency, or bone lesions).9
Bone marrow clonality can be shown by the ratio of kappa to lambda light chains as detected with immunohistochemistry, immunofluorescence, or flow cytometry.11 The normal ratio is 0.26 to 1.65 for a patient with normal kidney function. In this patient, however, the ratio was 1,301.08 (806.67 kappa to 0.62 lambda), which was extremely out of range. The patient’s bone marrow biopsy results revealed the presence of 15% clonal bone marrow plasma cells.
Multiple myeloma causes osteolytic lesions through increased activation of osteoclast activating factor that stimulates the growth of osteoclast precursors. At the same time, it inhibits osteoblast formation via multiple pathways, including the action of sclerostin.11 Our patient had lytic lesions in 2 left lower ribs and in both forearms and femurs.
Hypercalcemia in multiple myeloma is attributed to 2 main factors: bone breakdown and macrophage overactivation. Multiple myeloma cells increase the release of macrophage inflammatory protein 1-alpha and tumor necrosis factor, which are inflammatory proteins that cause an increase in macrophages, which cause an increase in calcitriol.11 As noted, our patient’s calcium level at presentation was 18.4 mg/dL uncorrected and 18.96 mg/dL corrected.
Cast nephropathy can occur in the distal tubules from the increased free light chains circulating and combining with Tamm-Horsfall protein, which in turn causes obstruction and local inflammation,12 leading to a rise in creatinine levels and resulting in acute kidney injury,12 as in our patient.
TREATMENT CONSIDERATIONS IN MULTIPLE MYELOMA
Our patient was referred to an oncologist for management.
In the management of multiple myeloma, the patient’s quality of life needs to be considered. With the development of new agents to combat the damages of the osteolytic effects, there is hope for improving quality of life.13,14 New agents under study include anabolic agents such as antisclerostin and anti-Dickkopf-1, which promote osteoblastogenesis, leading to bone formation, with the possibility of repairing existing damage.15
TAKE-HOME POINTS
- If hypercalcemia is mild to moderate, consider primary hyperparathyroidism.
- Identify patients with severe symptoms of hypercalcemia such as volume depletion, acute kidney injury, arrhythmia, or seizures.
- Confirm severe cases of hypercalcemia and treat severe cases effectively.
- Severe hypercalcemia may need further investigation into a potential underlying malignancy.
A morbidly obese 54-year-old woman presented to the emergency department after experiencing generalized abdominal pain for 3 days. She rated the pain as 5 on a scale of 10 and described it as dull, cramping, waxing and waning, not radiating, and not relieved with changes of position—in fact, not alleviated by anything she had tried. Her pain was associated with nausea and 1 episode of vomiting. She also experienced constipation before the onset of pain.
She denied recent trauma, recent travel, diarrhea, fevers, weakness, shortness of breath, chest pain, other muscle pains, or recent changes in diet. She also denied having this pain in the past. She said she had unintentionally lost some weight but was not certain how much. She denied tobacco, alcohol, or illicit drug use. She had no history of surgery.
Her medical history included hypertension, anemia, and uterine fibroids. Her current medications included losartan, hydrochlorothiazide, and albuterol. She had no family history of significant disease.
INITIAL EVALUATION AND MANAGEMENT
On admission, her temperature was 97.8°F (36.6°C), heart rate 100 beats per minute, blood pressure 136/64 mm Hg, respiratory rate 18 breaths per minute, oxygen saturation 97% on room air, weight 130.6 kg, and body mass index 35 kg/m2.
She was alert and oriented to person, place, and time. She was in mild discomfort but no distress. Her lungs were clear to auscultation, with no wheezing or crackles. Heart rate and rhythm were regular, with no extra heart sounds or murmurs. Bowel sounds were normal in all 4 quadrants, with tenderness to palpation of the epigastric area, but with no guarding or rebound tenderness.
Laboratory test results
Notable results of blood testing at presentation were as follows:
- Hemoglobin 8.2 g/dL (reference range 12.3–15.3)
- Hematocrit 26% (41–50)
- Mean corpuscular volume 107 fL (80–100)
- Blood urea nitrogen 33 mg/dL (8–21); 6 months earlier it was 16
- Serum creatinine 3.6 mg/dL (0.58–0.96); 6 months earlier, it was 0.75
- Albumin 3.3 g/dL (3.5–5)
- Calcium 18.4 mg/dL (8.4–10.2); 6 months earlier, it was 9.6
- Corrected calcium 19 mg/dL.
Findings on imaging, electrocardiography
Chest radiography showed no acute cardiopulmonary abnormalities. Abdominal computed tomography without contrast showed no abnormalities within the pancreas and no evidence of inflammation or obstruction. Electrocardiography showed sinus tachycardia.
DIFFERENTIAL DIAGNOSIS
1. Which is the most likely cause of this patient’s symptoms?
- Primary hyperparathyroidism
- Malignancy
- Her drug therapy
- Familial hypercalcemic hypocalciuria
In total, her laboratory results were consistent with macrocytic anemia, severe hypercalcemia, and acute kidney injury, and she had generalized symptoms.
Primary hyperparathyroidism
A main cause of hypercalcemia is primary hyperparathyroidism, and this needs to be ruled out. Benign adenomas are the most common cause of primary hyperparathyroidism, and a risk factor for benign adenoma is exposure to therapeutic levels of radiation.3
In hyperparathyroidism, there is an increased secretion of parathyroid hormone (PTH), which has multiple effects including increased reabsorption of calcium from the urine, increased excretion of phosphate, and increased expression of 1,25-hydroxyvitamin D hydroxylase to activate vitamin D. PTH also stimulates osteoclasts to increase their expression of receptor activator of nuclear factor kappa B ligand (RANKL), which has a downstream effect on osteoclast precursors to cause bone reabsorption.3
Inherited primary hyperparathyroidism tends to present at a younger age, with multiple overactive parathyroid glands.3 Given our patient’s age, inherited primary hyparathyroidism is thus less likely.
Malignancy
The probability that malignancy is causing the hypercalcemia increases with calcium levels greater than 13 mg/dL. Epidemiologically, in hospitalized patients with hypercalcemia, the source tends to be malignancy.4 Typically, patients who develop hypercalcemia from malignancy have a worse prognosis.5
Solid tumors and leukemias can cause hypercalcemia. The mechanisms include humoral factors secreted by the malignancy, local osteolysis due to tumor invasion of bone, and excessive absorption of calcium due to excess vitamin D produced by malignancies.5 The cancers that most frequently cause an increase in calcium resorption are lung cancer, renal cancer, breast cancer, and multiple myeloma.1
Solid tumors with no bone metastasis and non-Hodgkin lymphoma that release PTH-related protein (PTHrP) cause humoral hypercalcemia in malignancy. The patient is typically in an advanced stage of disease. PTHrP increases serum calcium levels by decreasing the kidney’s ability to excrete calcium and by increasing bone turnover. It has no effect on intestinal absorption because of its inability to stimulate activated vitamin D3. Thus, the increase in systemic calcium comes directly from breakdown of bone and inability to excrete the excess.
PTHrP has a unique role in breast cancer: it is released locally in areas where cancer cells have metastasized to bone, but it does not cause a systemic effect. Bone resorption occurs in areas of metastasis and results from an increase in expression of RANKL and RANK in osteoclasts in response to the effects of PTHrP, leading to an increase in the production of osteoclastic cells.1
Tamoxifen, an endocrine therapy often used in breast cancer, also causes a release of bone-reabsorbing factors from tumor cells, which can partially contribute to hypercalcemia.5
Myeloma cells secrete RANKL, which stimulates osteoclastic activity, and they also release interleukin 6 (IL-6) and activating macrophage inflammatory protein alpha. Serum testing usually shows low or normal intact PTH, PTHrP, and 1,25-dihydroxyvitamin D.1
Patients with multiple myeloma have a worse prognosis if they have a high red blood cell distribution width, a condition shown to correlate with malnutrition, leading to deficiencies in vitamin B12 and to poor response to treatment.6 Up to 14% of patients with multiple myeloma have vitamin B12 deficiency.7
Our patient’s recent weight loss and severe hypercalcemia raise suspicion of malignancy. Further, her obesity makes proper routine breast examination difficult and thus increases the chance of undiagnosed breast cancer.8 Her decrease in renal function and her anemia complicated by hypercalcemia also raise suspicion of multiple myeloma.
Hypercalcemia due to drug therapy
Thiazide diuretics, lithium, teriparatide, and vitamin A in excessive amounts can raise the serum calcium concentration.5 Our patient was taking a thiazide for hypertension, but her extremely high calcium level places drug-induced hypercalcemia as the sole cause lower on the differential list.
Familial hypercalcemic hypocalciuria
Familial hypercalcemic hypocalciuria is a rare autosomal-dominant cause of hypercalcemia in which the ability of the body (and especially the kidneys) to sense levels of calcium is impaired, leading to a decrease in excretion of calcium in the urine.3 Very high calcium levels are rare in hypercalcemic hypocalciuria.3 In our patient with a corrected calcium concentration of nearly 19 mg/dL, familial hypercalcemic hypocalciuria is very unlikely to be the cause of the hypercalcemia.
WHAT ARE THE NEXT STEPS IN THE WORKUP?
As hypercalcemia has been confirmed, the intact PTH level should be checked to determine whether the patient’s condition is PTH-mediated. If the PTH level is in the upper range of normal or is minimally elevated, primary hyperparathyroidism is likely. Elevated PTH confirms primary hyperparathyroidism. A low-normal or low intact PTH confirms a non-PTH-mediated process, and once this is confirmed, PTHrP levels should be checked. An elevated PTHrP suggests humoral hypercalcemia of malignancy. Serum protein electrophoresis, urine protein electrophoresis, and a serum light chain assay should be performed to rule out multiple myeloma.
Vitamin D toxicity is associated with high concentrations of 1,25-dihydroxyvitamin D and 25-hydroxyvitamin D metabolites. These levels should be checked in this patient.
Other disorders that cause hypercalcemia are vitamin A toxicity and hyperthyroidism, so vitamin A and thyroid-stimulating hormone levels should also be checked.5
CASE CONTINUED
After further questioning, the patient said that she had had lower back pain about 1 to 2 weeks before coming to the emergency room; her primary care doctor had said the pain was likely from muscle strain. The pain had almost resolved but was still present.
The results of further laboratory testing were as follows:
- Serum PTH 11 pg/mL (15–65)
- PTHrP 3.4 pmol/L (< 2.0)
- Protein electrophoresis showed a monoclonal (M) spike of 0.2 g/dL (0)
- Activated vitamin D < 5 ng/mL (19.9–79.3)
- Vitamin A 7.2 mg/dL (33.1–100)
- Vitamin B12 194 pg/mL (239–931)
- Thyroid-stimulating hormone 1.21 mIU/ L (0.47–4.68
- Free thyroxine 1.27 ng/dL (0.78–2.19)
- Iron 103 µg/dL (37–170)
- Total iron-binding capacity 335 µg/dL (265–497)
- Transferrin 248 mg/dL (206–381)
- Ferritin 66 ng/mL (11.1–264)
- Urine protein (random) 100 mg/dL (0–20)
- Urine microalbumin (random) 5.9 mg/dL (0–1.6)
- Urine creatinine clearance 88.5 mL/min (88–128)
- Urine albumin-creatinine ratio 66.66 mg/g (< 30).
Imaging reports
A nuclear bone scan showed increased bone uptake in the hip and both shoulders, consistent with arthritis, and increased activity in 2 of the lower left ribs, associated with rib fractures secondary to lytic lesions. A skeletal survey at a later date showed multiple well-circumscribed “punched-out” lytic lesions in both forearms and both femurs.
2. What should be the next step in this patient’s management?
- Intravenous (IV) fluids
- Calcitonin
- Bisphosphonate treatment
- Denosumab
- Hemodialysis
Initial treatment of severe hypercalcemia includes the following:
Start IV isotonic fluids at a rate of 150 mL/h (if the patient is making urine) to maintain urine output at more than 100 mL/h. Closely monitor urine output.
Give calcitonin 4 IU/kg in combination with IV fluids to reduce calcium levels within the first 12 to 48 hours of treatment.
Give a bisphosphonate, eg, zoledronic acid 4 mg over 15 minutes, or pamidronate 60 to 90 mg over 2 hours. Zoledronic acid is preferred in malignancy-induced hypercalcemia because it is more potent. Doses should be adjusted in patients with renal failure.
Give denosumab if hypercalcemia is refractory to bisphosphonates, or when bisphosphonates cannot be used in renal failure.9
Hemodialysis is performed in patients who have significant neurologic symptoms irrespective of acute renal insufficiency.
Our patient was started on 0.9% sodium chloride at a rate of 150 mL/h for severe hypercalcemia. Zoledronic acid 4 mg IV was given once. These measures lowered her calcium level and lessened her acute kidney injury.
ADDITIONAL FINDINGS
Urine testing was positive for Bence Jones protein. Immune electrophoresis, performed because of suspicion of multiple myeloma, showed an elevated level of kappa light chains at 806.7 mg/dL (0.33–1.94) and normal lambda light chains at 0.62 mg/dL (0.57–2.63). The immunoglobulin G level was low at 496 mg/dL (610–1,660). In patients with severe hypercalcemia, these results point to a diagnosis of malignancy. Bone marrow aspiration study showed greater than 10% plasma cells, confirming multiple myeloma.
MULTIPLE MYELOMA
The diagnosis of multiple myeloma is based in part on the presence of 10% or more of clonal bone marrow plasma cells10 and of specific end-organ damage (anemia, hypercalcemia, renal insufficiency, or bone lesions).9
Bone marrow clonality can be shown by the ratio of kappa to lambda light chains as detected with immunohistochemistry, immunofluorescence, or flow cytometry.11 The normal ratio is 0.26 to 1.65 for a patient with normal kidney function. In this patient, however, the ratio was 1,301.08 (806.67 kappa to 0.62 lambda), which was extremely out of range. The patient’s bone marrow biopsy results revealed the presence of 15% clonal bone marrow plasma cells.
Multiple myeloma causes osteolytic lesions through increased activation of osteoclast activating factor that stimulates the growth of osteoclast precursors. At the same time, it inhibits osteoblast formation via multiple pathways, including the action of sclerostin.11 Our patient had lytic lesions in 2 left lower ribs and in both forearms and femurs.
Hypercalcemia in multiple myeloma is attributed to 2 main factors: bone breakdown and macrophage overactivation. Multiple myeloma cells increase the release of macrophage inflammatory protein 1-alpha and tumor necrosis factor, which are inflammatory proteins that cause an increase in macrophages, which cause an increase in calcitriol.11 As noted, our patient’s calcium level at presentation was 18.4 mg/dL uncorrected and 18.96 mg/dL corrected.
Cast nephropathy can occur in the distal tubules from the increased free light chains circulating and combining with Tamm-Horsfall protein, which in turn causes obstruction and local inflammation,12 leading to a rise in creatinine levels and resulting in acute kidney injury,12 as in our patient.
TREATMENT CONSIDERATIONS IN MULTIPLE MYELOMA
Our patient was referred to an oncologist for management.
In the management of multiple myeloma, the patient’s quality of life needs to be considered. With the development of new agents to combat the damages of the osteolytic effects, there is hope for improving quality of life.13,14 New agents under study include anabolic agents such as antisclerostin and anti-Dickkopf-1, which promote osteoblastogenesis, leading to bone formation, with the possibility of repairing existing damage.15
TAKE-HOME POINTS
- If hypercalcemia is mild to moderate, consider primary hyperparathyroidism.
- Identify patients with severe symptoms of hypercalcemia such as volume depletion, acute kidney injury, arrhythmia, or seizures.
- Confirm severe cases of hypercalcemia and treat severe cases effectively.
- Severe hypercalcemia may need further investigation into a potential underlying malignancy.
- Sternlicht H, Glezerman IG. Hypercalcemia of malignancy and new treatment options. Ther Clin Risk Manag 2015; 11:1779–1788. doi:10.2147/TCRM.S83681
- Ahmed R, Hashiba K. Reliability of QT intervals as indicators of clinical hypercalcemia. Clin Cardiol 1988; 11(6):395–400. doi:10.1002/clc.4960110607
- Bilezikian JP, Cusano NE, Khan AA, Liu JM, Marcocci C, Bandeira F. Primary hyperparathyroidism. Nat Rev Dis Primers 2016; 2:16033. doi:10.1038/nrdp.2016.33
- Kuchay MS, Kaur P, Mishra SK, Mithal A. The changing profile of hypercalcemia in a tertiary care setting in North India: an 18-month retrospective study. Clin Cases Miner Bone Metab 2017; 14(2):131–135. doi:10.11138/ccmbm/2017.14.1.131
- Rosner MH, Dalkin AC. Onco-nephrology: the pathophysiology and treatment of malignancy-associated hypercalcemia. Clin J Am Soc Nephrol 2012; 7(10):1722–1729. doi:10.2215/CJN.02470312
- Ai L, Mu S, Hu Y. Prognostic role of RDW in hematological malignancies: a systematic review and meta-analysis. Cancer Cell Int 2018; 18:61. doi:10.1186/s12935-018-0558-3
- Baz R, Alemany C, Green R, Hussein MA. Prevalence of vitamin B12 deficiency in patients with plasma cell dyscrasias: a retrospective review. Cancer 2004; 101(4):790–795. doi:10.1002/cncr.20441
- Elmore JG, Carney PA, Abraham LA, et al. The association between obesity and screening mammography accuracy. Arch Intern Med 2004; 164(10):1140–1147. doi:10.1001/archinte.164.10.1140
- Gerecke C, Fuhrmann S, Strifler S, Schmidt-Hieber M, Einsele H, Knop S. The diagnosis and treatment of multiple myeloma. Dtsch Arztebl Int 2016; 113(27–28):470–476. doi:10.3238/arztebl.2016.0470
- Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol 2016; 91(7):719–734. doi:10.1002/ajh.24402
- Silbermann R, Roodman GD. Myeloma bone disease: pathophysiology and management. J Bone Oncol 2013; 2(2):59–69. doi:10.1016/j.jbo.2013.04.001
- Doshi M, Lahoti A, Danesh FR, Batuman V, Sanders PW; American Society of Nephrology Onco-Nephrology Forum. Paraprotein-related kidney disease: kidney injury from paraproteins—what determines the site of injury? Clin J Am Soc Nephrol 2016; 11(12):2288–2294. doi:10.2215/CJN.02560316
- Reece D. Update on the initial therapy of multiple myeloma. Am Soc Clin Oncol Educ Book 2013. doi:10.1200/EdBook_AM.2013.33.e307
- Nishida H. Bone-targeted agents in multiple myeloma. Hematol Rep 2018; 10(1):7401. doi:10.4081/hr.2018.7401
- Ring ES, Lawson MA, Snowden JA, Jolley I, Chantry AD. New agents in the treatment of myeloma bone disease. Calcif Tissue Int 2018; 102(2):196–209. doi:10.1007/s00223-017-0351-7
- Sternlicht H, Glezerman IG. Hypercalcemia of malignancy and new treatment options. Ther Clin Risk Manag 2015; 11:1779–1788. doi:10.2147/TCRM.S83681
- Ahmed R, Hashiba K. Reliability of QT intervals as indicators of clinical hypercalcemia. Clin Cardiol 1988; 11(6):395–400. doi:10.1002/clc.4960110607
- Bilezikian JP, Cusano NE, Khan AA, Liu JM, Marcocci C, Bandeira F. Primary hyperparathyroidism. Nat Rev Dis Primers 2016; 2:16033. doi:10.1038/nrdp.2016.33
- Kuchay MS, Kaur P, Mishra SK, Mithal A. The changing profile of hypercalcemia in a tertiary care setting in North India: an 18-month retrospective study. Clin Cases Miner Bone Metab 2017; 14(2):131–135. doi:10.11138/ccmbm/2017.14.1.131
- Rosner MH, Dalkin AC. Onco-nephrology: the pathophysiology and treatment of malignancy-associated hypercalcemia. Clin J Am Soc Nephrol 2012; 7(10):1722–1729. doi:10.2215/CJN.02470312
- Ai L, Mu S, Hu Y. Prognostic role of RDW in hematological malignancies: a systematic review and meta-analysis. Cancer Cell Int 2018; 18:61. doi:10.1186/s12935-018-0558-3
- Baz R, Alemany C, Green R, Hussein MA. Prevalence of vitamin B12 deficiency in patients with plasma cell dyscrasias: a retrospective review. Cancer 2004; 101(4):790–795. doi:10.1002/cncr.20441
- Elmore JG, Carney PA, Abraham LA, et al. The association between obesity and screening mammography accuracy. Arch Intern Med 2004; 164(10):1140–1147. doi:10.1001/archinte.164.10.1140
- Gerecke C, Fuhrmann S, Strifler S, Schmidt-Hieber M, Einsele H, Knop S. The diagnosis and treatment of multiple myeloma. Dtsch Arztebl Int 2016; 113(27–28):470–476. doi:10.3238/arztebl.2016.0470
- Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol 2016; 91(7):719–734. doi:10.1002/ajh.24402
- Silbermann R, Roodman GD. Myeloma bone disease: pathophysiology and management. J Bone Oncol 2013; 2(2):59–69. doi:10.1016/j.jbo.2013.04.001
- Doshi M, Lahoti A, Danesh FR, Batuman V, Sanders PW; American Society of Nephrology Onco-Nephrology Forum. Paraprotein-related kidney disease: kidney injury from paraproteins—what determines the site of injury? Clin J Am Soc Nephrol 2016; 11(12):2288–2294. doi:10.2215/CJN.02560316
- Reece D. Update on the initial therapy of multiple myeloma. Am Soc Clin Oncol Educ Book 2013. doi:10.1200/EdBook_AM.2013.33.e307
- Nishida H. Bone-targeted agents in multiple myeloma. Hematol Rep 2018; 10(1):7401. doi:10.4081/hr.2018.7401
- Ring ES, Lawson MA, Snowden JA, Jolley I, Chantry AD. New agents in the treatment of myeloma bone disease. Calcif Tissue Int 2018; 102(2):196–209. doi:10.1007/s00223-017-0351-7
Low-dose steroids for acute exacerbations of COPD in a non-ICU setting: Worth consideration
Despite guidelines recommending low-dose oral glucocorticoids over high-dose intravenous (IV) glucocorticoids for inpatient management of acute exacerbations of chronic obstructive pulmonary disease (COPD), we have observed that most patients still receive high-dose IV therapy before being transitioned to low-dose oral therapy at discharge. Clinical inertia undoubtedly plays a significant role in the slow adoption of new recommendations, but in this era of evidence-based practice, the unfortunate lack of data supporting low over high steroid doses for acute exacerbations of COPD also contributes to hesitancy of physicians.
A SIGNIFICANT AND GROWING BURDEN
COPD is one of the most common pulmonary conditions managed by hospitalists today, and by the year 2030, it is predicted to become the third leading cause of death worldwide.1
COPD is also a significant economic burden, costing $50 billion to manage in the United States, most of that from the cost of lengthy hospital stays.2 COPD patients have 1 to 2 exacerbations per year.3 Bacterial and viral infections are responsible for most exacerbations, and 15% to 20% are from air pollution and other environmental causes of airway inflammation.3
CHALLENGES TO CHANGING PRACTICE
Glucocorticoids are the gold standard for treatment of acute exacerbations of COPD. It is well-documented that compared with placebo, glucocorticoids reduce mortality risk, length of hospital stay, and exacerbation recurrence after 1 month.4 And while high-dose IV steroid therapy has been the standard approach, oral administration has been found to be noninferior to IV administration with regard to treatment and length of hospital stay.5
While adverse effects are more common at higher doses, the optimal dose and duration of systemic glucocorticoid therapy for acute exacerbations of COPD are still largely at the discretion of the physician. The 2019 report of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends low doses (40 mg) for no more than 5 to 7 days for exacerbations, based on reports that showed no worse outcomes with low-dose oral than with high-dose IV therapy.6,7 (In the 2010 study by Lindenauer et al,7 92% of nearly 80,000 patients received high-dose IV steroids, reflecting standard practice at that time.) However, the GOLD guidelines do not address mortality rates, length of stay, or readmission rates for either approach, as they are devised to direct treatment in patients with stable mild to advanced COPD, not exacerbations.
THE EVIDENCE FOR LOW-DOSE STEROIDS
Mortality rates
Aksoy et al8 established that, compared with placebo, low-dose steroids improved mortality rates in a subset of patients with acute exacerbations, specifically those with eosinophilic exacerbations. This study followed the 2013 Reduction in the Use of Corticosteroids in Exacerbated COPD (REDUCE) trial, which showed mortality rates were not lower with 14 days of low-dose prednisone treatment than with 5 days.9
Length of hospital stay
With regard to length of hospital stay, in 2011 Wang et al10 found no statistically significant difference between high- and low-dose steroid treatment.However, the REDUCE trial found that low-dose steroids shortened the median length of stay by 1 day compared with placebo.9
Hospital readmission rates
The REDUCE trial found no statistically significant difference in readmission rates when comparing 5 days of low-dose treatment vs 14 days.9 However, Aksoy et al8 found that readmission rates were significantly lower with low-dose treatment than with placebo.No study has yet examined readmission rates with high-dose vs low-dose steroid treatment.
What does the evidence tell us?
Low-dose oral glucocorticoid treatment shows definitive benefits in terms of lower mortality rates, shorter hospital length of stay, and lower readmission rates vs placebo in the treatment of acute exacerbations of COPD. Furthermore, a 14-day course is no better than 5 days in terms of mortality rates. And low-dose glucocorticoid treatment shows reduced mortality rates in addition to similar hospital length of stay when compared to high-dose glucocorticoid treatment.
Together, these findings lend credibility to the current GOLD recommendations. However, we have observed that in sharp contrast to the leading clinical guidelines, most patients hospitalized for acute exacerbations of COPD are still treated initially with high-dose IV corticosteroids. Why?
Obstacles that perpetuate the use of high-dose over low-dose treatment include lack of knowledge of glucocorticoid pharmacokinetics among clinicians, use of outdated order sets, and the reflex notion that more of a drug is more efficacious in its desired effect. In addition, administrative obstacles include using high-dose IV steroids to justify an inpatient stay or continued hospitalization.
COUNTERING THE OBSTACLES: THE HOSPITALIST’S ROLE
To counter these obstacles, we propose standardization of inpatient treatment of acute exacerbations of COPD to include initial low-dose steroid treatment in accordance with the most recent GOLD guidelines.6 This would benefit the patient by reducing undesirable effects of high-dose steroids, and at the same time reduce the economic burden of managing COPD exacerbations. Considering the large number of hospitalizations for COPD exacerbation each year, hospitalists can play a large role in this effort by routinely incorporating the low-dose steroid recommendation into their clinical practice.
- World Health Organization. Chronic respiratory diseases: burden of COPD. www.who.int/respiratory/copd/burden/en. Accessed October 16, 2019.
- Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013; 5:235–245. doi:10.2147/CEOR.S34321
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med 2008; 359(22):2355–2365. doi:10.1056/NEJMra0800353
- Walters JA, Tan DJ, White CJ, Gibson PG, Wood-Baker R, Walters EH. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; (9):CD001288. doi:10.1002/14651858.CD001288.pub4
- de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind study. Chest 2007; 132(6):1741–1747. doi:10.1378/chest.07-0208
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2019 report. www.goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed October 16, 2019.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA 2010; 303(23):2359–2367. doi:10.1001/jama.2010.796
- Aksoy E, Güngör S, Agca MÇ, et al. A revised treatment approach for hospitalized patients with eosinophilic and neutrophilic exacerbations of chronic obstructive pulmonary disease. Turk Thorac J 2018; 19(4):193–200. doi:10.5152/TurkThoracJ.2018.18004
- Leuppi JD, Schuetz P, Bingisser R, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA 2013; 309(21):2223–2231. doi:10.1001/jama.2013.5023
- Wang PH, Cheng SL, Wang HC, et al. Systemic steroids in acute exacerbation of COPD—from guidelines to bedside. Int J Clin Pharmacol Ther 2011; 49(11):705–708. doi:10.5414/cp201588
Despite guidelines recommending low-dose oral glucocorticoids over high-dose intravenous (IV) glucocorticoids for inpatient management of acute exacerbations of chronic obstructive pulmonary disease (COPD), we have observed that most patients still receive high-dose IV therapy before being transitioned to low-dose oral therapy at discharge. Clinical inertia undoubtedly plays a significant role in the slow adoption of new recommendations, but in this era of evidence-based practice, the unfortunate lack of data supporting low over high steroid doses for acute exacerbations of COPD also contributes to hesitancy of physicians.
A SIGNIFICANT AND GROWING BURDEN
COPD is one of the most common pulmonary conditions managed by hospitalists today, and by the year 2030, it is predicted to become the third leading cause of death worldwide.1
COPD is also a significant economic burden, costing $50 billion to manage in the United States, most of that from the cost of lengthy hospital stays.2 COPD patients have 1 to 2 exacerbations per year.3 Bacterial and viral infections are responsible for most exacerbations, and 15% to 20% are from air pollution and other environmental causes of airway inflammation.3
CHALLENGES TO CHANGING PRACTICE
Glucocorticoids are the gold standard for treatment of acute exacerbations of COPD. It is well-documented that compared with placebo, glucocorticoids reduce mortality risk, length of hospital stay, and exacerbation recurrence after 1 month.4 And while high-dose IV steroid therapy has been the standard approach, oral administration has been found to be noninferior to IV administration with regard to treatment and length of hospital stay.5
While adverse effects are more common at higher doses, the optimal dose and duration of systemic glucocorticoid therapy for acute exacerbations of COPD are still largely at the discretion of the physician. The 2019 report of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends low doses (40 mg) for no more than 5 to 7 days for exacerbations, based on reports that showed no worse outcomes with low-dose oral than with high-dose IV therapy.6,7 (In the 2010 study by Lindenauer et al,7 92% of nearly 80,000 patients received high-dose IV steroids, reflecting standard practice at that time.) However, the GOLD guidelines do not address mortality rates, length of stay, or readmission rates for either approach, as they are devised to direct treatment in patients with stable mild to advanced COPD, not exacerbations.
THE EVIDENCE FOR LOW-DOSE STEROIDS
Mortality rates
Aksoy et al8 established that, compared with placebo, low-dose steroids improved mortality rates in a subset of patients with acute exacerbations, specifically those with eosinophilic exacerbations. This study followed the 2013 Reduction in the Use of Corticosteroids in Exacerbated COPD (REDUCE) trial, which showed mortality rates were not lower with 14 days of low-dose prednisone treatment than with 5 days.9
Length of hospital stay
With regard to length of hospital stay, in 2011 Wang et al10 found no statistically significant difference between high- and low-dose steroid treatment.However, the REDUCE trial found that low-dose steroids shortened the median length of stay by 1 day compared with placebo.9
Hospital readmission rates
The REDUCE trial found no statistically significant difference in readmission rates when comparing 5 days of low-dose treatment vs 14 days.9 However, Aksoy et al8 found that readmission rates were significantly lower with low-dose treatment than with placebo.No study has yet examined readmission rates with high-dose vs low-dose steroid treatment.
What does the evidence tell us?
Low-dose oral glucocorticoid treatment shows definitive benefits in terms of lower mortality rates, shorter hospital length of stay, and lower readmission rates vs placebo in the treatment of acute exacerbations of COPD. Furthermore, a 14-day course is no better than 5 days in terms of mortality rates. And low-dose glucocorticoid treatment shows reduced mortality rates in addition to similar hospital length of stay when compared to high-dose glucocorticoid treatment.
Together, these findings lend credibility to the current GOLD recommendations. However, we have observed that in sharp contrast to the leading clinical guidelines, most patients hospitalized for acute exacerbations of COPD are still treated initially with high-dose IV corticosteroids. Why?
Obstacles that perpetuate the use of high-dose over low-dose treatment include lack of knowledge of glucocorticoid pharmacokinetics among clinicians, use of outdated order sets, and the reflex notion that more of a drug is more efficacious in its desired effect. In addition, administrative obstacles include using high-dose IV steroids to justify an inpatient stay or continued hospitalization.
COUNTERING THE OBSTACLES: THE HOSPITALIST’S ROLE
To counter these obstacles, we propose standardization of inpatient treatment of acute exacerbations of COPD to include initial low-dose steroid treatment in accordance with the most recent GOLD guidelines.6 This would benefit the patient by reducing undesirable effects of high-dose steroids, and at the same time reduce the economic burden of managing COPD exacerbations. Considering the large number of hospitalizations for COPD exacerbation each year, hospitalists can play a large role in this effort by routinely incorporating the low-dose steroid recommendation into their clinical practice.
Despite guidelines recommending low-dose oral glucocorticoids over high-dose intravenous (IV) glucocorticoids for inpatient management of acute exacerbations of chronic obstructive pulmonary disease (COPD), we have observed that most patients still receive high-dose IV therapy before being transitioned to low-dose oral therapy at discharge. Clinical inertia undoubtedly plays a significant role in the slow adoption of new recommendations, but in this era of evidence-based practice, the unfortunate lack of data supporting low over high steroid doses for acute exacerbations of COPD also contributes to hesitancy of physicians.
A SIGNIFICANT AND GROWING BURDEN
COPD is one of the most common pulmonary conditions managed by hospitalists today, and by the year 2030, it is predicted to become the third leading cause of death worldwide.1
COPD is also a significant economic burden, costing $50 billion to manage in the United States, most of that from the cost of lengthy hospital stays.2 COPD patients have 1 to 2 exacerbations per year.3 Bacterial and viral infections are responsible for most exacerbations, and 15% to 20% are from air pollution and other environmental causes of airway inflammation.3
CHALLENGES TO CHANGING PRACTICE
Glucocorticoids are the gold standard for treatment of acute exacerbations of COPD. It is well-documented that compared with placebo, glucocorticoids reduce mortality risk, length of hospital stay, and exacerbation recurrence after 1 month.4 And while high-dose IV steroid therapy has been the standard approach, oral administration has been found to be noninferior to IV administration with regard to treatment and length of hospital stay.5
While adverse effects are more common at higher doses, the optimal dose and duration of systemic glucocorticoid therapy for acute exacerbations of COPD are still largely at the discretion of the physician. The 2019 report of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends low doses (40 mg) for no more than 5 to 7 days for exacerbations, based on reports that showed no worse outcomes with low-dose oral than with high-dose IV therapy.6,7 (In the 2010 study by Lindenauer et al,7 92% of nearly 80,000 patients received high-dose IV steroids, reflecting standard practice at that time.) However, the GOLD guidelines do not address mortality rates, length of stay, or readmission rates for either approach, as they are devised to direct treatment in patients with stable mild to advanced COPD, not exacerbations.
THE EVIDENCE FOR LOW-DOSE STEROIDS
Mortality rates
Aksoy et al8 established that, compared with placebo, low-dose steroids improved mortality rates in a subset of patients with acute exacerbations, specifically those with eosinophilic exacerbations. This study followed the 2013 Reduction in the Use of Corticosteroids in Exacerbated COPD (REDUCE) trial, which showed mortality rates were not lower with 14 days of low-dose prednisone treatment than with 5 days.9
Length of hospital stay
With regard to length of hospital stay, in 2011 Wang et al10 found no statistically significant difference between high- and low-dose steroid treatment.However, the REDUCE trial found that low-dose steroids shortened the median length of stay by 1 day compared with placebo.9
Hospital readmission rates
The REDUCE trial found no statistically significant difference in readmission rates when comparing 5 days of low-dose treatment vs 14 days.9 However, Aksoy et al8 found that readmission rates were significantly lower with low-dose treatment than with placebo.No study has yet examined readmission rates with high-dose vs low-dose steroid treatment.
What does the evidence tell us?
Low-dose oral glucocorticoid treatment shows definitive benefits in terms of lower mortality rates, shorter hospital length of stay, and lower readmission rates vs placebo in the treatment of acute exacerbations of COPD. Furthermore, a 14-day course is no better than 5 days in terms of mortality rates. And low-dose glucocorticoid treatment shows reduced mortality rates in addition to similar hospital length of stay when compared to high-dose glucocorticoid treatment.
Together, these findings lend credibility to the current GOLD recommendations. However, we have observed that in sharp contrast to the leading clinical guidelines, most patients hospitalized for acute exacerbations of COPD are still treated initially with high-dose IV corticosteroids. Why?
Obstacles that perpetuate the use of high-dose over low-dose treatment include lack of knowledge of glucocorticoid pharmacokinetics among clinicians, use of outdated order sets, and the reflex notion that more of a drug is more efficacious in its desired effect. In addition, administrative obstacles include using high-dose IV steroids to justify an inpatient stay or continued hospitalization.
COUNTERING THE OBSTACLES: THE HOSPITALIST’S ROLE
To counter these obstacles, we propose standardization of inpatient treatment of acute exacerbations of COPD to include initial low-dose steroid treatment in accordance with the most recent GOLD guidelines.6 This would benefit the patient by reducing undesirable effects of high-dose steroids, and at the same time reduce the economic burden of managing COPD exacerbations. Considering the large number of hospitalizations for COPD exacerbation each year, hospitalists can play a large role in this effort by routinely incorporating the low-dose steroid recommendation into their clinical practice.
- World Health Organization. Chronic respiratory diseases: burden of COPD. www.who.int/respiratory/copd/burden/en. Accessed October 16, 2019.
- Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013; 5:235–245. doi:10.2147/CEOR.S34321
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med 2008; 359(22):2355–2365. doi:10.1056/NEJMra0800353
- Walters JA, Tan DJ, White CJ, Gibson PG, Wood-Baker R, Walters EH. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; (9):CD001288. doi:10.1002/14651858.CD001288.pub4
- de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind study. Chest 2007; 132(6):1741–1747. doi:10.1378/chest.07-0208
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2019 report. www.goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed October 16, 2019.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA 2010; 303(23):2359–2367. doi:10.1001/jama.2010.796
- Aksoy E, Güngör S, Agca MÇ, et al. A revised treatment approach for hospitalized patients with eosinophilic and neutrophilic exacerbations of chronic obstructive pulmonary disease. Turk Thorac J 2018; 19(4):193–200. doi:10.5152/TurkThoracJ.2018.18004
- Leuppi JD, Schuetz P, Bingisser R, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA 2013; 309(21):2223–2231. doi:10.1001/jama.2013.5023
- Wang PH, Cheng SL, Wang HC, et al. Systemic steroids in acute exacerbation of COPD—from guidelines to bedside. Int J Clin Pharmacol Ther 2011; 49(11):705–708. doi:10.5414/cp201588
- World Health Organization. Chronic respiratory diseases: burden of COPD. www.who.int/respiratory/copd/burden/en. Accessed October 16, 2019.
- Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013; 5:235–245. doi:10.2147/CEOR.S34321
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med 2008; 359(22):2355–2365. doi:10.1056/NEJMra0800353
- Walters JA, Tan DJ, White CJ, Gibson PG, Wood-Baker R, Walters EH. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; (9):CD001288. doi:10.1002/14651858.CD001288.pub4
- de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind study. Chest 2007; 132(6):1741–1747. doi:10.1378/chest.07-0208
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2019 report. www.goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Accessed October 16, 2019.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA 2010; 303(23):2359–2367. doi:10.1001/jama.2010.796
- Aksoy E, Güngör S, Agca MÇ, et al. A revised treatment approach for hospitalized patients with eosinophilic and neutrophilic exacerbations of chronic obstructive pulmonary disease. Turk Thorac J 2018; 19(4):193–200. doi:10.5152/TurkThoracJ.2018.18004
- Leuppi JD, Schuetz P, Bingisser R, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA 2013; 309(21):2223–2231. doi:10.1001/jama.2013.5023
- Wang PH, Cheng SL, Wang HC, et al. Systemic steroids in acute exacerbation of COPD—from guidelines to bedside. Int J Clin Pharmacol Ther 2011; 49(11):705–708. doi:10.5414/cp201588