User login
‘Down to my last diaper’: The anxiety of parenting in poverty
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Major increase seen in cosmeceutical alternatives to topical hydroquinone
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
FROM SOC 2021
Identify patient and hospital factors to reduce maternal mortality
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
FROM ADVANCING NIH RESEARCH ON THE HEALTH OF WOMEN
Transgender use of dermatologic procedures has strong gender tilt
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.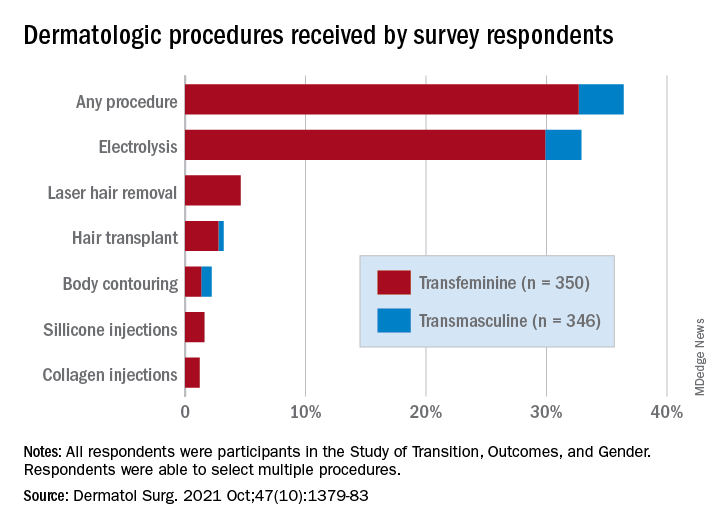
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.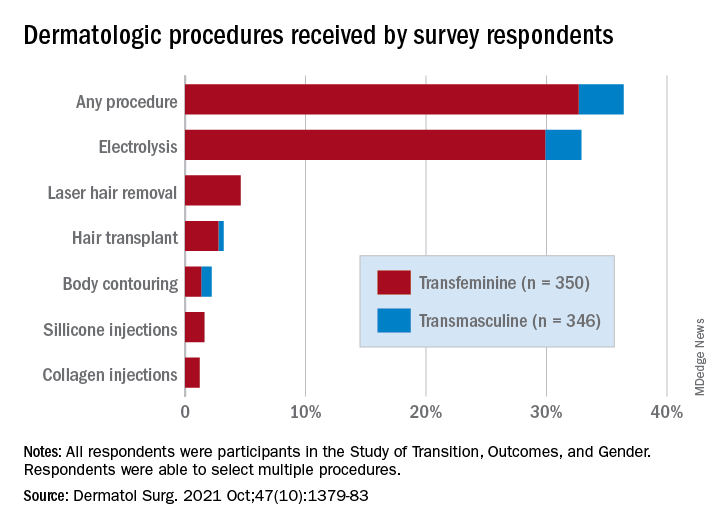
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.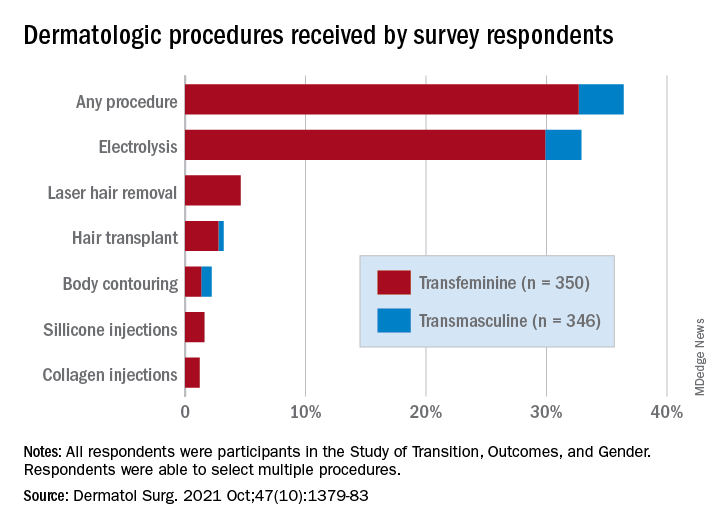
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
FROM DERMATOLOGIC SURGERY
Social determinants of health may drive CVD risk in Black Americans
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).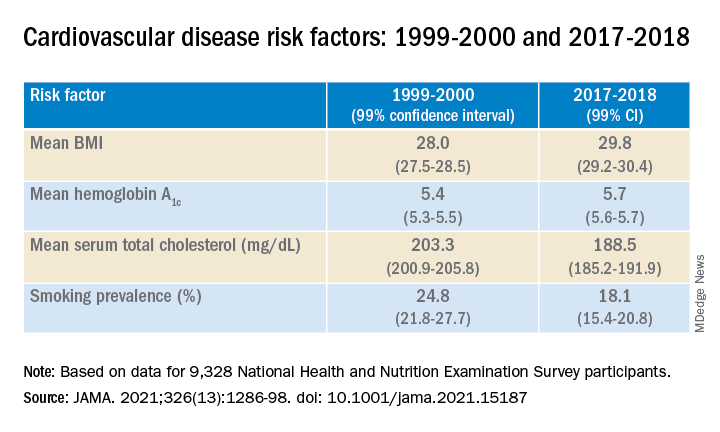
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).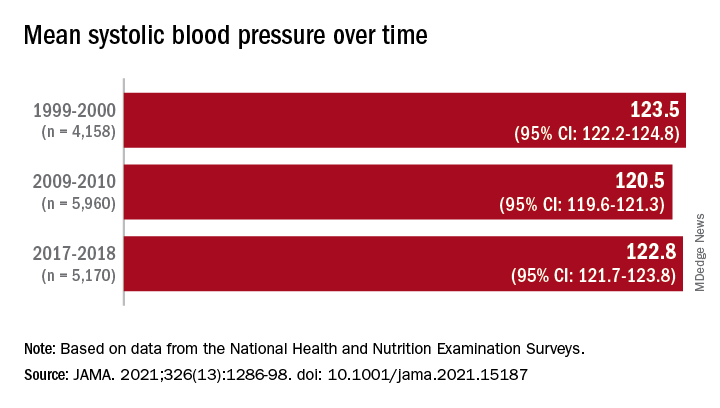
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).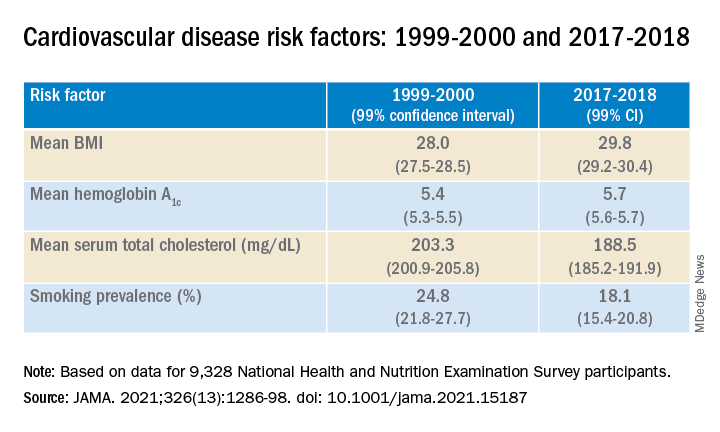
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).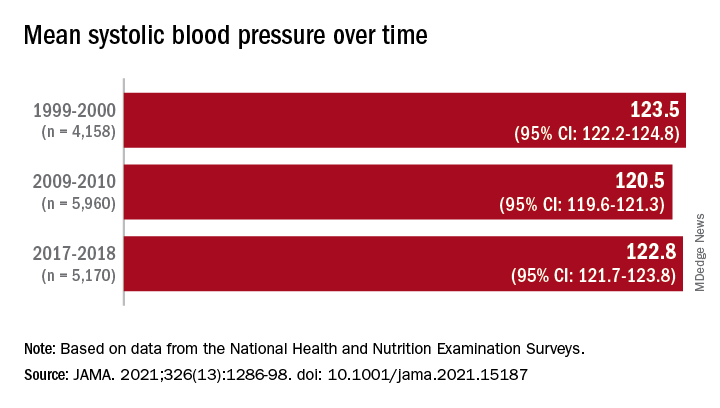
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).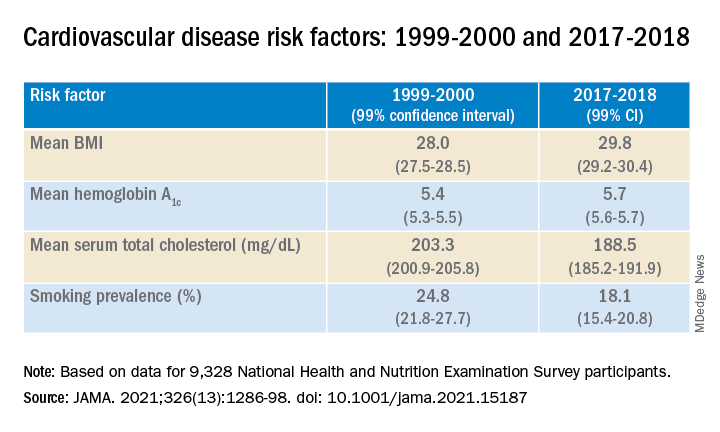
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).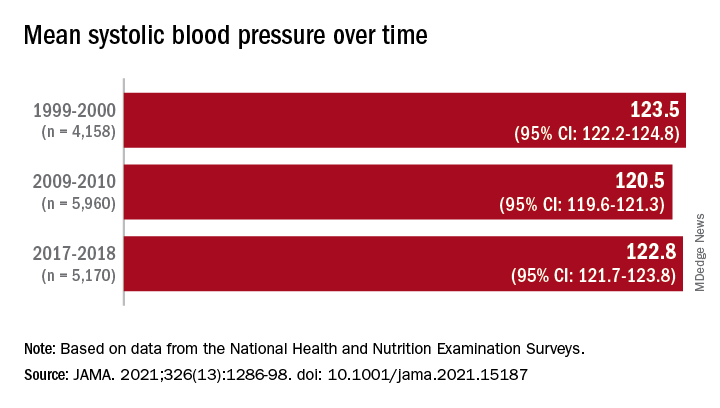
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Comorbidities larger factor than race in COVID ICU deaths?
Racial/ethnic disparities in COVID-19 mortality rates may be related more to comorbidities than to demographics, suggest authors of a new study.
Researchers compared the length of stay in intensive care units in two suburban hospitals for patients with severe SARS-CoV-2 infections. Their study shows that although the incidence of comorbidities and rates of use of mechanical ventilation and death were higher among Black patients than among patients of other races, length of stay in the ICU was generally similar for patients of all races. The study was conducted by Tripti Kumar, DO, from Lankenau Medical Center, Wynnewood, Pennsylvania, and colleagues.
“Racial disparities are observed in the United States concerning COVID-19, and studies have discovered that minority populations are at ongoing risk for health inequity,” Dr. Kumar said in a narrated e-poster presented during the American College of Chest Physicians (CHEST) 2021 Annual Meeting.
“Primary prevention initiatives should take precedence in mitigating the effect that comorbidities have on these vulnerable populations to help reduce necessity for mechanical ventilation, hospital length of stay, and overall mortality,” she said.
Higher death rates for Black patients
At the time the study was conducted, the COVID-19 death rate in the United States had topped 500,000 (as of this writing, it stands at 726,000). Of those who died, 22.4% were Black, 18.1% were Hispanic, and 3.6% were of Asian descent. The numbers of COVID-19 diagnoses and deaths were significantly higher in U.S. counties where the proportions of Black residents were higher, the authors note.
To see whether differences in COVID-19 outcomes were reflected in ICU length of stay, the researchers conducted a retrospective chart review of data on 162 patients admitted to ICUs at Paoli Hospital and Lankenau Medical Center, both in the suburban Philadelphia town of Wynnewood.
All patients were diagnosed with COVID-19 from March through June 2020.
In all, 60% of the study population were Black, 35% were White, 3% were Asian, and 2% were Hispanic. Women composed 46% of the sample.
The average length of ICU stay, which was the primary endpoint, was similar among Black patients (15.4 days), White patients (15.5 days), and Asians (16 days). The shortest average hospital stay was among Hispanic patients, at 11.3 days.
The investigators determined that among all races, the prevalence of type 2 diabetes, obesity, hypertension, and smoking was highest among Black patients.
Overall, nearly 85% of patients required mechanical ventilation. Among the patients who required it, 86% were Black, 84% were White, 66% were Hispanic, and 75% were Asian.
Overall mortality was 62%. It was higher among Black patients, at 60%, than among White patients, at 33%. The investigators did not report mortality rates for Hispanic or Asian patients.
Missing data
Demondes Haynes, MD, FCCP, professor of medicine in the Division of Pulmonary and Critical Care and associate dean for admissions at the University of Mississippi Medical Center and School of Medicine, Jackson, who was not involved in the study, told this news organization that there are some gaps in the study that make it difficult to draw strong conclusions about the findings.
“For sure, comorbidities contribute a great deal to mortality, but is there something else going on? I think this poster is incomplete in that it cannot answer that question,” he said in an interview.
He noted that the use of retrospective rather than prospective data makes it hard to account for potential confounders.
“I agree that these findings show the potential contribution of comorbidities, but to me, this is a little incomplete to make that a definitive statement,” he said.
“I can’t argue with their recommendation for primary prevention – we definitely want to do primary prevention to decrease comorbidities. Would it decrease overall mortality? It might, it sure might, for just COVID-19 I’d say no, we need more information.”
No funding source for the study was reported. Dr. Kumar and colleagues and Dr. Haynes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial/ethnic disparities in COVID-19 mortality rates may be related more to comorbidities than to demographics, suggest authors of a new study.
Researchers compared the length of stay in intensive care units in two suburban hospitals for patients with severe SARS-CoV-2 infections. Their study shows that although the incidence of comorbidities and rates of use of mechanical ventilation and death were higher among Black patients than among patients of other races, length of stay in the ICU was generally similar for patients of all races. The study was conducted by Tripti Kumar, DO, from Lankenau Medical Center, Wynnewood, Pennsylvania, and colleagues.
“Racial disparities are observed in the United States concerning COVID-19, and studies have discovered that minority populations are at ongoing risk for health inequity,” Dr. Kumar said in a narrated e-poster presented during the American College of Chest Physicians (CHEST) 2021 Annual Meeting.
“Primary prevention initiatives should take precedence in mitigating the effect that comorbidities have on these vulnerable populations to help reduce necessity for mechanical ventilation, hospital length of stay, and overall mortality,” she said.
Higher death rates for Black patients
At the time the study was conducted, the COVID-19 death rate in the United States had topped 500,000 (as of this writing, it stands at 726,000). Of those who died, 22.4% were Black, 18.1% were Hispanic, and 3.6% were of Asian descent. The numbers of COVID-19 diagnoses and deaths were significantly higher in U.S. counties where the proportions of Black residents were higher, the authors note.
To see whether differences in COVID-19 outcomes were reflected in ICU length of stay, the researchers conducted a retrospective chart review of data on 162 patients admitted to ICUs at Paoli Hospital and Lankenau Medical Center, both in the suburban Philadelphia town of Wynnewood.
All patients were diagnosed with COVID-19 from March through June 2020.
In all, 60% of the study population were Black, 35% were White, 3% were Asian, and 2% were Hispanic. Women composed 46% of the sample.
The average length of ICU stay, which was the primary endpoint, was similar among Black patients (15.4 days), White patients (15.5 days), and Asians (16 days). The shortest average hospital stay was among Hispanic patients, at 11.3 days.
The investigators determined that among all races, the prevalence of type 2 diabetes, obesity, hypertension, and smoking was highest among Black patients.
Overall, nearly 85% of patients required mechanical ventilation. Among the patients who required it, 86% were Black, 84% were White, 66% were Hispanic, and 75% were Asian.
Overall mortality was 62%. It was higher among Black patients, at 60%, than among White patients, at 33%. The investigators did not report mortality rates for Hispanic or Asian patients.
Missing data
Demondes Haynes, MD, FCCP, professor of medicine in the Division of Pulmonary and Critical Care and associate dean for admissions at the University of Mississippi Medical Center and School of Medicine, Jackson, who was not involved in the study, told this news organization that there are some gaps in the study that make it difficult to draw strong conclusions about the findings.
“For sure, comorbidities contribute a great deal to mortality, but is there something else going on? I think this poster is incomplete in that it cannot answer that question,” he said in an interview.
He noted that the use of retrospective rather than prospective data makes it hard to account for potential confounders.
“I agree that these findings show the potential contribution of comorbidities, but to me, this is a little incomplete to make that a definitive statement,” he said.
“I can’t argue with their recommendation for primary prevention – we definitely want to do primary prevention to decrease comorbidities. Would it decrease overall mortality? It might, it sure might, for just COVID-19 I’d say no, we need more information.”
No funding source for the study was reported. Dr. Kumar and colleagues and Dr. Haynes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial/ethnic disparities in COVID-19 mortality rates may be related more to comorbidities than to demographics, suggest authors of a new study.
Researchers compared the length of stay in intensive care units in two suburban hospitals for patients with severe SARS-CoV-2 infections. Their study shows that although the incidence of comorbidities and rates of use of mechanical ventilation and death were higher among Black patients than among patients of other races, length of stay in the ICU was generally similar for patients of all races. The study was conducted by Tripti Kumar, DO, from Lankenau Medical Center, Wynnewood, Pennsylvania, and colleagues.
“Racial disparities are observed in the United States concerning COVID-19, and studies have discovered that minority populations are at ongoing risk for health inequity,” Dr. Kumar said in a narrated e-poster presented during the American College of Chest Physicians (CHEST) 2021 Annual Meeting.
“Primary prevention initiatives should take precedence in mitigating the effect that comorbidities have on these vulnerable populations to help reduce necessity for mechanical ventilation, hospital length of stay, and overall mortality,” she said.
Higher death rates for Black patients
At the time the study was conducted, the COVID-19 death rate in the United States had topped 500,000 (as of this writing, it stands at 726,000). Of those who died, 22.4% were Black, 18.1% were Hispanic, and 3.6% were of Asian descent. The numbers of COVID-19 diagnoses and deaths were significantly higher in U.S. counties where the proportions of Black residents were higher, the authors note.
To see whether differences in COVID-19 outcomes were reflected in ICU length of stay, the researchers conducted a retrospective chart review of data on 162 patients admitted to ICUs at Paoli Hospital and Lankenau Medical Center, both in the suburban Philadelphia town of Wynnewood.
All patients were diagnosed with COVID-19 from March through June 2020.
In all, 60% of the study population were Black, 35% were White, 3% were Asian, and 2% were Hispanic. Women composed 46% of the sample.
The average length of ICU stay, which was the primary endpoint, was similar among Black patients (15.4 days), White patients (15.5 days), and Asians (16 days). The shortest average hospital stay was among Hispanic patients, at 11.3 days.
The investigators determined that among all races, the prevalence of type 2 diabetes, obesity, hypertension, and smoking was highest among Black patients.
Overall, nearly 85% of patients required mechanical ventilation. Among the patients who required it, 86% were Black, 84% were White, 66% were Hispanic, and 75% were Asian.
Overall mortality was 62%. It was higher among Black patients, at 60%, than among White patients, at 33%. The investigators did not report mortality rates for Hispanic or Asian patients.
Missing data
Demondes Haynes, MD, FCCP, professor of medicine in the Division of Pulmonary and Critical Care and associate dean for admissions at the University of Mississippi Medical Center and School of Medicine, Jackson, who was not involved in the study, told this news organization that there are some gaps in the study that make it difficult to draw strong conclusions about the findings.
“For sure, comorbidities contribute a great deal to mortality, but is there something else going on? I think this poster is incomplete in that it cannot answer that question,” he said in an interview.
He noted that the use of retrospective rather than prospective data makes it hard to account for potential confounders.
“I agree that these findings show the potential contribution of comorbidities, but to me, this is a little incomplete to make that a definitive statement,” he said.
“I can’t argue with their recommendation for primary prevention – we definitely want to do primary prevention to decrease comorbidities. Would it decrease overall mortality? It might, it sure might, for just COVID-19 I’d say no, we need more information.”
No funding source for the study was reported. Dr. Kumar and colleagues and Dr. Haynes reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Racial disparities found in treatment of tubal pregnancies
Black and Latina women are more likely to have an open surgery compared with a minimally invasive procedure to treat ectopic pregnancy, according to research presented at the American Society for Reproductive Medicine’s 2021 meeting.
The researchers found that Black and Latina women had 50% lesser odds of undergoing laparoscopic surgery, a minimally invasive procedure, compared to their White peers.
“We see these disparities in minority populations, [especially in] women with regard to so many other aspects of [gynecologic] surgery,” study author Alexandra Huttler, MD, said in an interview. “The fact that these disparities exist [in the treatment of tubal pregnancies] was unfortunately not surprising to us.”
Dr. Huttler and her team analyzed data from the American College of Surgeons’ National Surgical Quality Improvement Program, which followed more than 9,000 patients who had undergone surgical management of a tubal ectopic pregnancy between 2010 and 2019. Of the group, 85% underwent laparoscopic surgery while 14% had open surgery, which requires a longer recovery time.
The proportion of cases performed laparoscopically increased from 81% in 2010 to 91% in 2019. However, a disproportionate number of Black and Latina women underwent open surgery to treat ectopic pregnancies during this time. Because they are more invasive, open surgeries are associated with longer operative times, hospital stays, and increased complications, Dr. Huttler said. They are typically associated with more pain and patients are more likely to be admitted to the hospital for postoperative care.
On the other hand, minimally invasive surgeries are associated with decreased operative time, “less recovery and less pain,” Dr. Huttler explained.
The researchers also looked at trends of the related surgical procedure salpingectomy, which is surgical removal of one or both fallopian tubes versus salpingostomy, a surgical unblocking of the tube. Of the group, 91% underwent salpingectomy and 9% underwent salpingostomy.
Researchers found that Black and Latina women had 78% and 54% greater odds, respectively, of receiving a salpingectomy. However, the clinical significance of these findings are unclear because there are “many factors” that are patient and case specific, Dr. Huttler said.
The study is important and adds to a litany of studies that have shown that women of color do not receive optimal care, said Ruben Alvero, MD, who was not involved in the study.
“Women of color in general have seen compromises in their care at many levels in the system,” Dr. Alvero, professor of obstetrics and gynecology at Stanford (Calif.) University, said in an interview. “We really have to do a massive overhaul of how we treat women of color so they get the same level of treatment that all other populations receive.”
While the factors contributing to these health disparities can be complicated, Dr. Alvero said that one reason for this multivariate discrepancy could be that Black and Latina women tend to seek care at, or only have access to, underresourced hospitals.
Dr. Huttler said she hopes her findings prompt further discussion of these disparities.
“There really are disparities at all levels of care here and figuring out what the root of this is certainly requires further research,” Dr. Huttler said.
The experts interviewed disclosed no conflicts on interests.
Black and Latina women are more likely to have an open surgery compared with a minimally invasive procedure to treat ectopic pregnancy, according to research presented at the American Society for Reproductive Medicine’s 2021 meeting.
The researchers found that Black and Latina women had 50% lesser odds of undergoing laparoscopic surgery, a minimally invasive procedure, compared to their White peers.
“We see these disparities in minority populations, [especially in] women with regard to so many other aspects of [gynecologic] surgery,” study author Alexandra Huttler, MD, said in an interview. “The fact that these disparities exist [in the treatment of tubal pregnancies] was unfortunately not surprising to us.”
Dr. Huttler and her team analyzed data from the American College of Surgeons’ National Surgical Quality Improvement Program, which followed more than 9,000 patients who had undergone surgical management of a tubal ectopic pregnancy between 2010 and 2019. Of the group, 85% underwent laparoscopic surgery while 14% had open surgery, which requires a longer recovery time.
The proportion of cases performed laparoscopically increased from 81% in 2010 to 91% in 2019. However, a disproportionate number of Black and Latina women underwent open surgery to treat ectopic pregnancies during this time. Because they are more invasive, open surgeries are associated with longer operative times, hospital stays, and increased complications, Dr. Huttler said. They are typically associated with more pain and patients are more likely to be admitted to the hospital for postoperative care.
On the other hand, minimally invasive surgeries are associated with decreased operative time, “less recovery and less pain,” Dr. Huttler explained.
The researchers also looked at trends of the related surgical procedure salpingectomy, which is surgical removal of one or both fallopian tubes versus salpingostomy, a surgical unblocking of the tube. Of the group, 91% underwent salpingectomy and 9% underwent salpingostomy.
Researchers found that Black and Latina women had 78% and 54% greater odds, respectively, of receiving a salpingectomy. However, the clinical significance of these findings are unclear because there are “many factors” that are patient and case specific, Dr. Huttler said.
The study is important and adds to a litany of studies that have shown that women of color do not receive optimal care, said Ruben Alvero, MD, who was not involved in the study.
“Women of color in general have seen compromises in their care at many levels in the system,” Dr. Alvero, professor of obstetrics and gynecology at Stanford (Calif.) University, said in an interview. “We really have to do a massive overhaul of how we treat women of color so they get the same level of treatment that all other populations receive.”
While the factors contributing to these health disparities can be complicated, Dr. Alvero said that one reason for this multivariate discrepancy could be that Black and Latina women tend to seek care at, or only have access to, underresourced hospitals.
Dr. Huttler said she hopes her findings prompt further discussion of these disparities.
“There really are disparities at all levels of care here and figuring out what the root of this is certainly requires further research,” Dr. Huttler said.
The experts interviewed disclosed no conflicts on interests.
Black and Latina women are more likely to have an open surgery compared with a minimally invasive procedure to treat ectopic pregnancy, according to research presented at the American Society for Reproductive Medicine’s 2021 meeting.
The researchers found that Black and Latina women had 50% lesser odds of undergoing laparoscopic surgery, a minimally invasive procedure, compared to their White peers.
“We see these disparities in minority populations, [especially in] women with regard to so many other aspects of [gynecologic] surgery,” study author Alexandra Huttler, MD, said in an interview. “The fact that these disparities exist [in the treatment of tubal pregnancies] was unfortunately not surprising to us.”
Dr. Huttler and her team analyzed data from the American College of Surgeons’ National Surgical Quality Improvement Program, which followed more than 9,000 patients who had undergone surgical management of a tubal ectopic pregnancy between 2010 and 2019. Of the group, 85% underwent laparoscopic surgery while 14% had open surgery, which requires a longer recovery time.
The proportion of cases performed laparoscopically increased from 81% in 2010 to 91% in 2019. However, a disproportionate number of Black and Latina women underwent open surgery to treat ectopic pregnancies during this time. Because they are more invasive, open surgeries are associated with longer operative times, hospital stays, and increased complications, Dr. Huttler said. They are typically associated with more pain and patients are more likely to be admitted to the hospital for postoperative care.
On the other hand, minimally invasive surgeries are associated with decreased operative time, “less recovery and less pain,” Dr. Huttler explained.
The researchers also looked at trends of the related surgical procedure salpingectomy, which is surgical removal of one or both fallopian tubes versus salpingostomy, a surgical unblocking of the tube. Of the group, 91% underwent salpingectomy and 9% underwent salpingostomy.
Researchers found that Black and Latina women had 78% and 54% greater odds, respectively, of receiving a salpingectomy. However, the clinical significance of these findings are unclear because there are “many factors” that are patient and case specific, Dr. Huttler said.
The study is important and adds to a litany of studies that have shown that women of color do not receive optimal care, said Ruben Alvero, MD, who was not involved in the study.
“Women of color in general have seen compromises in their care at many levels in the system,” Dr. Alvero, professor of obstetrics and gynecology at Stanford (Calif.) University, said in an interview. “We really have to do a massive overhaul of how we treat women of color so they get the same level of treatment that all other populations receive.”
While the factors contributing to these health disparities can be complicated, Dr. Alvero said that one reason for this multivariate discrepancy could be that Black and Latina women tend to seek care at, or only have access to, underresourced hospitals.
Dr. Huttler said she hopes her findings prompt further discussion of these disparities.
“There really are disparities at all levels of care here and figuring out what the root of this is certainly requires further research,” Dr. Huttler said.
The experts interviewed disclosed no conflicts on interests.
FROM ASRM 2021
Survey spotlights double-edged sword for minority cardiologists
Survey results paint a stark picture of discrimination among racial minorities in the cardiology workforce but also a strong sense of belonging.
Among respondents to the 2015 American College of Cardiology (ACC) Professional Life Survey, which is the most recent survey, over half (52.3%) of underrepresented racial and ethnic minorities (URMs) and 45.5% of Asian or Pacific Islanders reported experiencing discrimination compared with 36.4% of Whites (both P < .01).
Nevertheless, 91.2% of URMs reported being satisfied with their career, as did 90% of Asians or Pacific Islanders and 89.1% of Whites.
Satisfaction with financial compensation also did not differ between groups, and most cardiologists believed their opportunities for advancement were similar to those of their peers.
One possible explanation is that the respondents may simply be people who’ve had better experiences, lead author Kevin L. Thomas, MD, Duke Clinical Research Institute, Durham, N.C., and colleagues told this news organization. A second hypothesis looks more to sheer determination, or grit.
“Perhaps along the sometimes circuitous pathway to being a cardiologist – which is a lot of training, a lot of standardized testing, a lot of applications – that maybe you sub-select a group of individuals who are simply more resilient based on their life experiences and things that they’ve overcome to get where they are,” he said.
Interestingly, rates of burnout were lower among URMs (22.4%) and Asians/Pacific Islanders (20.1%) than Whites (30.3%; P = .02 and P < .01, respectively). The finding is unexpected but in line with a recent report of more than 4,400 U.S. physicians finding lower odds of burnout among Asian, Hispanic/Latinx, and Black physicians.
The new study, published October 18 in the Journal of the American College of Cardiology, however, affirms that women of all racial and ethnic groups face significant headwinds in the White, male-dominated cardiology workforce.
Just 13.9% of White men reported experiencing discrimination, compared with 44.6% of URM men and 36.2% of Asians/Pacific Islander men. In comparison, 69.2% of White women reported discrimination, as did 62.7% of URM women and 57% of Asian/Pacific Islander women (both P <.01).
“When you look specifically at White men versus White women, there is a large discrepancy there, and it just shows us, I think, for a lot of different groups, we still have a long way to go in terms of trying to achieve equity and to try to be inclusive in the workplace,” Dr. Thomas said.
Men were more likely to experience race- and religion-based discrimination in the workplace, whereas nearly all women reported sex discrimination, with parenting an important second. Approximately 85% of cardiologists reported being satisfied with their family lives, although unpublished data suggest URMs were less likely to be married and to have fewer children, Dr. Thomas said.
During job negotiations, URM cardiologists were less likely to prioritize salary, benefits, and work hours for their first job (13.6%, 10.9% 19.3%) than White cardiologists (20.6%, 23.3%, 31.3%; P < .02 for all).
In subsequent negotiations, URMs placed more emphasis on salary, benefits, and work hours than Whites, whereas both URMs and Asians/Pacific Islanders placed a greater importance on travel benefits, diversity, mentoring, workspace, time to promotion, academic rank, and roles with community, institutional, or national recognition, which the authors say, “might indicate a greater need to overcome systemic barriers.”
Three-fourths of all cardiologist respondents had a mentor during training, which can take many shapes, Dr. Thomas noted. “Within my own section as an electrophysiologist, which is a very subspecialized category, we have four Black electrophysiologists, and I think it was because many of us mentored each other as we came along, and it inspired us.”
URMs are more likely to experience the so-called “minority tax” of being tapped for added responsibilities in the name of inclusivity efforts, he said, and called on individuals from the dominant culture to mentor or sponsor cardiologists from other racial groups and to carve out leadership pathways for women and minorities so they “can use their gifts to benefit the profession at large,” leading clinical trials or steering committees and serving in high-profile roles.
Although the events of 2020 sharpened attention on the issue of diversity in America, Dr. Thomas and colleagues say that more work needs to be done defining the problem and that professional organizations and health systems also should systematically collect sex, racial, and ethnic identifies of members using classifications similar to the 2020 U.S. Census.
The study was based on 2,245 respondents to the 2015 Professional Life Survey, which was not specifically designed to assess racial/ethnic diversity topics and had a response rate of 21%, which limited representatives of each group.
In all, 197 were from URMs (80 Blacks, 113 Hispanics, 4 Native Americans), 564 were Asians/Pacific Islanders, 1,447 were Whites, and 37 listed multiracial/other. More than half (58%) were men, and most were adult cardiologists (83% to 85%), followed by pediatric cardiology (6% to 10%) and cardiovascular surgery (1% to 2%).
“Further research is needed to understand these findings and their significance, because ongoing efforts within ACC and other organizations to increase diversity will fail unless this is successfully addressed,” the authors conclude.
To that end, Dr. Thomas said they are looking to develop a new survey that taps other groups like the Association of Black Cardiologists and members of the LGBTQ community.
“I’m really excited about the opportunity to develop a survey that specifically has the objective of trying to understand the experiences of systematically disadvantaged, historically marginalized groups to see if we can see the same information, but maybe through a clear lens, and then be able to develop strategies to mitigate some of the challenges that we see” he said. “So we can increase the numbers and also have a workforce that is reflective of the populations that we take care of and the nation as a whole.”
The study was funded by the American College of Cardiology. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Survey results paint a stark picture of discrimination among racial minorities in the cardiology workforce but also a strong sense of belonging.
Among respondents to the 2015 American College of Cardiology (ACC) Professional Life Survey, which is the most recent survey, over half (52.3%) of underrepresented racial and ethnic minorities (URMs) and 45.5% of Asian or Pacific Islanders reported experiencing discrimination compared with 36.4% of Whites (both P < .01).
Nevertheless, 91.2% of URMs reported being satisfied with their career, as did 90% of Asians or Pacific Islanders and 89.1% of Whites.
Satisfaction with financial compensation also did not differ between groups, and most cardiologists believed their opportunities for advancement were similar to those of their peers.
One possible explanation is that the respondents may simply be people who’ve had better experiences, lead author Kevin L. Thomas, MD, Duke Clinical Research Institute, Durham, N.C., and colleagues told this news organization. A second hypothesis looks more to sheer determination, or grit.
“Perhaps along the sometimes circuitous pathway to being a cardiologist – which is a lot of training, a lot of standardized testing, a lot of applications – that maybe you sub-select a group of individuals who are simply more resilient based on their life experiences and things that they’ve overcome to get where they are,” he said.
Interestingly, rates of burnout were lower among URMs (22.4%) and Asians/Pacific Islanders (20.1%) than Whites (30.3%; P = .02 and P < .01, respectively). The finding is unexpected but in line with a recent report of more than 4,400 U.S. physicians finding lower odds of burnout among Asian, Hispanic/Latinx, and Black physicians.
The new study, published October 18 in the Journal of the American College of Cardiology, however, affirms that women of all racial and ethnic groups face significant headwinds in the White, male-dominated cardiology workforce.
Just 13.9% of White men reported experiencing discrimination, compared with 44.6% of URM men and 36.2% of Asians/Pacific Islander men. In comparison, 69.2% of White women reported discrimination, as did 62.7% of URM women and 57% of Asian/Pacific Islander women (both P <.01).
“When you look specifically at White men versus White women, there is a large discrepancy there, and it just shows us, I think, for a lot of different groups, we still have a long way to go in terms of trying to achieve equity and to try to be inclusive in the workplace,” Dr. Thomas said.
Men were more likely to experience race- and religion-based discrimination in the workplace, whereas nearly all women reported sex discrimination, with parenting an important second. Approximately 85% of cardiologists reported being satisfied with their family lives, although unpublished data suggest URMs were less likely to be married and to have fewer children, Dr. Thomas said.
During job negotiations, URM cardiologists were less likely to prioritize salary, benefits, and work hours for their first job (13.6%, 10.9% 19.3%) than White cardiologists (20.6%, 23.3%, 31.3%; P < .02 for all).
In subsequent negotiations, URMs placed more emphasis on salary, benefits, and work hours than Whites, whereas both URMs and Asians/Pacific Islanders placed a greater importance on travel benefits, diversity, mentoring, workspace, time to promotion, academic rank, and roles with community, institutional, or national recognition, which the authors say, “might indicate a greater need to overcome systemic barriers.”
Three-fourths of all cardiologist respondents had a mentor during training, which can take many shapes, Dr. Thomas noted. “Within my own section as an electrophysiologist, which is a very subspecialized category, we have four Black electrophysiologists, and I think it was because many of us mentored each other as we came along, and it inspired us.”
URMs are more likely to experience the so-called “minority tax” of being tapped for added responsibilities in the name of inclusivity efforts, he said, and called on individuals from the dominant culture to mentor or sponsor cardiologists from other racial groups and to carve out leadership pathways for women and minorities so they “can use their gifts to benefit the profession at large,” leading clinical trials or steering committees and serving in high-profile roles.
Although the events of 2020 sharpened attention on the issue of diversity in America, Dr. Thomas and colleagues say that more work needs to be done defining the problem and that professional organizations and health systems also should systematically collect sex, racial, and ethnic identifies of members using classifications similar to the 2020 U.S. Census.
The study was based on 2,245 respondents to the 2015 Professional Life Survey, which was not specifically designed to assess racial/ethnic diversity topics and had a response rate of 21%, which limited representatives of each group.
In all, 197 were from URMs (80 Blacks, 113 Hispanics, 4 Native Americans), 564 were Asians/Pacific Islanders, 1,447 were Whites, and 37 listed multiracial/other. More than half (58%) were men, and most were adult cardiologists (83% to 85%), followed by pediatric cardiology (6% to 10%) and cardiovascular surgery (1% to 2%).
“Further research is needed to understand these findings and their significance, because ongoing efforts within ACC and other organizations to increase diversity will fail unless this is successfully addressed,” the authors conclude.
To that end, Dr. Thomas said they are looking to develop a new survey that taps other groups like the Association of Black Cardiologists and members of the LGBTQ community.
“I’m really excited about the opportunity to develop a survey that specifically has the objective of trying to understand the experiences of systematically disadvantaged, historically marginalized groups to see if we can see the same information, but maybe through a clear lens, and then be able to develop strategies to mitigate some of the challenges that we see” he said. “So we can increase the numbers and also have a workforce that is reflective of the populations that we take care of and the nation as a whole.”
The study was funded by the American College of Cardiology. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Survey results paint a stark picture of discrimination among racial minorities in the cardiology workforce but also a strong sense of belonging.
Among respondents to the 2015 American College of Cardiology (ACC) Professional Life Survey, which is the most recent survey, over half (52.3%) of underrepresented racial and ethnic minorities (URMs) and 45.5% of Asian or Pacific Islanders reported experiencing discrimination compared with 36.4% of Whites (both P < .01).
Nevertheless, 91.2% of URMs reported being satisfied with their career, as did 90% of Asians or Pacific Islanders and 89.1% of Whites.
Satisfaction with financial compensation also did not differ between groups, and most cardiologists believed their opportunities for advancement were similar to those of their peers.
One possible explanation is that the respondents may simply be people who’ve had better experiences, lead author Kevin L. Thomas, MD, Duke Clinical Research Institute, Durham, N.C., and colleagues told this news organization. A second hypothesis looks more to sheer determination, or grit.
“Perhaps along the sometimes circuitous pathway to being a cardiologist – which is a lot of training, a lot of standardized testing, a lot of applications – that maybe you sub-select a group of individuals who are simply more resilient based on their life experiences and things that they’ve overcome to get where they are,” he said.
Interestingly, rates of burnout were lower among URMs (22.4%) and Asians/Pacific Islanders (20.1%) than Whites (30.3%; P = .02 and P < .01, respectively). The finding is unexpected but in line with a recent report of more than 4,400 U.S. physicians finding lower odds of burnout among Asian, Hispanic/Latinx, and Black physicians.
The new study, published October 18 in the Journal of the American College of Cardiology, however, affirms that women of all racial and ethnic groups face significant headwinds in the White, male-dominated cardiology workforce.
Just 13.9% of White men reported experiencing discrimination, compared with 44.6% of URM men and 36.2% of Asians/Pacific Islander men. In comparison, 69.2% of White women reported discrimination, as did 62.7% of URM women and 57% of Asian/Pacific Islander women (both P <.01).
“When you look specifically at White men versus White women, there is a large discrepancy there, and it just shows us, I think, for a lot of different groups, we still have a long way to go in terms of trying to achieve equity and to try to be inclusive in the workplace,” Dr. Thomas said.
Men were more likely to experience race- and religion-based discrimination in the workplace, whereas nearly all women reported sex discrimination, with parenting an important second. Approximately 85% of cardiologists reported being satisfied with their family lives, although unpublished data suggest URMs were less likely to be married and to have fewer children, Dr. Thomas said.
During job negotiations, URM cardiologists were less likely to prioritize salary, benefits, and work hours for their first job (13.6%, 10.9% 19.3%) than White cardiologists (20.6%, 23.3%, 31.3%; P < .02 for all).
In subsequent negotiations, URMs placed more emphasis on salary, benefits, and work hours than Whites, whereas both URMs and Asians/Pacific Islanders placed a greater importance on travel benefits, diversity, mentoring, workspace, time to promotion, academic rank, and roles with community, institutional, or national recognition, which the authors say, “might indicate a greater need to overcome systemic barriers.”
Three-fourths of all cardiologist respondents had a mentor during training, which can take many shapes, Dr. Thomas noted. “Within my own section as an electrophysiologist, which is a very subspecialized category, we have four Black electrophysiologists, and I think it was because many of us mentored each other as we came along, and it inspired us.”
URMs are more likely to experience the so-called “minority tax” of being tapped for added responsibilities in the name of inclusivity efforts, he said, and called on individuals from the dominant culture to mentor or sponsor cardiologists from other racial groups and to carve out leadership pathways for women and minorities so they “can use their gifts to benefit the profession at large,” leading clinical trials or steering committees and serving in high-profile roles.
Although the events of 2020 sharpened attention on the issue of diversity in America, Dr. Thomas and colleagues say that more work needs to be done defining the problem and that professional organizations and health systems also should systematically collect sex, racial, and ethnic identifies of members using classifications similar to the 2020 U.S. Census.
The study was based on 2,245 respondents to the 2015 Professional Life Survey, which was not specifically designed to assess racial/ethnic diversity topics and had a response rate of 21%, which limited representatives of each group.
In all, 197 were from URMs (80 Blacks, 113 Hispanics, 4 Native Americans), 564 were Asians/Pacific Islanders, 1,447 were Whites, and 37 listed multiracial/other. More than half (58%) were men, and most were adult cardiologists (83% to 85%), followed by pediatric cardiology (6% to 10%) and cardiovascular surgery (1% to 2%).
“Further research is needed to understand these findings and their significance, because ongoing efforts within ACC and other organizations to increase diversity will fail unless this is successfully addressed,” the authors conclude.
To that end, Dr. Thomas said they are looking to develop a new survey that taps other groups like the Association of Black Cardiologists and members of the LGBTQ community.
“I’m really excited about the opportunity to develop a survey that specifically has the objective of trying to understand the experiences of systematically disadvantaged, historically marginalized groups to see if we can see the same information, but maybe through a clear lens, and then be able to develop strategies to mitigate some of the challenges that we see” he said. “So we can increase the numbers and also have a workforce that is reflective of the populations that we take care of and the nation as a whole.”
The study was funded by the American College of Cardiology. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How the Navajo’s cultural values are driving COVID vaccinations
COVID-19 has killed Native Americans at twice the rate of White Americans, underscoring the health inequities and deep-rooted distrust tribal nations have of federal government entities.
And yet, Native Americans have the highest vaccination rates of any major racial or ethnic group in the United States. Like many other tribal nations, the Navajo had to embrace Western science to reclaim its social customs and ceremonies. “We’re a very social culture, so having to isolate really impacted our mental health,” said Mary Hasbah Roessel, MD, DLFAPA, a Navajo psychiatrist who is affiliated with Santa Fe Indian Hospital in New Mexico.
The Navajo nation occupies the largest Native American reservation in the United States, spanning New Mexico, Arizona, and Utah. As of mid-October, the nation had reported more than 34,000 COVID-19 cases and 1,400 deaths in its jurisdiction.
In an interview with this news organization, Dr. Roessel described the partnerships that mobilized a nation of more than 250,000 individuals to get vaccinated.
Question: Why has the death rate been so high in the Navajo nation?
Answer: A lot of health disparities before the pandemic were blatantly revealed during COVID. Only 40% of people on the reservation had running water. Having to stay home and isolate led to food insecurity. Further insecurity issues affected our ability to stay healthy, such as having good sanitation. There’s a lot of poverty, a high unemployment rate. Some people had to go to work off reservation and were potentially bringing the virus home. A lot of generations live in the same household. Elders were vulnerable to getting the infection, and there was little ability to isolate if someone wasn’t having symptoms. Hospitals nearby didn’t have ICUs.
Therefore, the rate of cases skyrocketed early on. We were disproportionately affected. The Navajo nation per capita had the highest rate of cases in any state.
Q: What changes took place within the Navajo nation to get people vaccinated? What role did the federal Indian Health Service have in promoting this?
A: There had to be a shift in acceptance of the vaccinations.
With the IHS, we went into a disaster response mode with all-hands-on deck meetings. We had to figure out how we could access mass vaccination clinics. Partnering with the Navajo Department of Health, we did that right away with hospitals and small clinics across the Navajo nation. Casinos owned by tribal entities that closed during COVID reopened and were used as vaccination clinics.
Vaccinations were sent to us fairly quickly. I ended up getting vaccinated in December 2020, when it was first rolled out.
Native and Navajo individuals have been reluctant to rely on government services. Because IHS came through with the vaccines, COVID reduced that stigma to access its services. Even the Navajo Department of Health partnered with the Indian Health Service to provide culturally relevant campaigns that explain why the vaccine is valuable.
I think because people were so impacted, they saw something valuable with the vaccine. Given the education and access, people were ready to get vaccinated. They realized if a whole household got vaccinated, they could see early on that they could be social again.
Q: What cultural factors have been contributing to this positive development?
A: In our Navajo culture, we’ve dealt with monsters before. We talk about that in terms of how we teach our young people to be strong and resilient. We talked about this virus as being another monster we had to tackle and control. The teaching was along those lines. We’ve dealt with this before, and we can handle it. We’re resilient. Our culture is very strong in that way. So how do we do it? We have to partner; we have to embrace Western medicine to return back to the ceremonies we want to have again and be social again. We focus on positive things, so if we see something as potentially positive, such as the vaccine, we see that and know that’s something to help us come into our life again.
Q: I would expect that protecting elders in the tribe would be a big incentive in taking the vaccine.
A: Yes, we didn’t want to lose our language and culture, and we wanted to protect our elders. Having a way to do that was very important as well. They were among the first to get vaccinated.
Q: What is the current vaccination rate in the Navajo nation?
A: I think it’s in the upper 80th percentile. It’s very high.
Q: What have been the biggest takeaways so far, and what are your hopes for the future?
A: Even though the Navajo Nation has been impacted and devastated with the loss of elders and knowledge keepers, we still have our culture and ceremonies intact to the point that we know we can be resilient get through this difficult time.
Through collaborations with the federal and state governments and the clinics, we see that things are different now. Going forward, my hope is these partnerships will continue, that we’ll build those relationships and not be so siloed in our care. When the New Mexico Department of Health rolled out its first vaccination clinic, for example, we jumped on and saw how they did it. We were then able to do our own, collaborating with the state.
We also saw how important our culture was, how it helped our Navajo people through these difficult times.
Dr. Roessel, a distinguished fellow of the American Psychiatric Association, has special expertise in cultural psychiatry. Her childhood was spent growing up in the Navajo nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating Indigenous knowledge and principles.
References
American Public Media Research Lab. “The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.” 2021 Mar 5.
Centers for Disease Control and Prevention. “Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States.” Data as of 2021 Oct 14.
Navajo Nation. Indian Health Service. U.S. Department of Health & Human Services.
The Navajo Nation’s Office of the President and Vice President. “11 New Cases, 32,735 Recoveries, and Six Recent Deaths Related to COVID-19.” 2021 Oct 13.
Navajo Nation Government web page.
COVID-19 has killed Native Americans at twice the rate of White Americans, underscoring the health inequities and deep-rooted distrust tribal nations have of federal government entities.
And yet, Native Americans have the highest vaccination rates of any major racial or ethnic group in the United States. Like many other tribal nations, the Navajo had to embrace Western science to reclaim its social customs and ceremonies. “We’re a very social culture, so having to isolate really impacted our mental health,” said Mary Hasbah Roessel, MD, DLFAPA, a Navajo psychiatrist who is affiliated with Santa Fe Indian Hospital in New Mexico.
The Navajo nation occupies the largest Native American reservation in the United States, spanning New Mexico, Arizona, and Utah. As of mid-October, the nation had reported more than 34,000 COVID-19 cases and 1,400 deaths in its jurisdiction.
In an interview with this news organization, Dr. Roessel described the partnerships that mobilized a nation of more than 250,000 individuals to get vaccinated.
Question: Why has the death rate been so high in the Navajo nation?
Answer: A lot of health disparities before the pandemic were blatantly revealed during COVID. Only 40% of people on the reservation had running water. Having to stay home and isolate led to food insecurity. Further insecurity issues affected our ability to stay healthy, such as having good sanitation. There’s a lot of poverty, a high unemployment rate. Some people had to go to work off reservation and were potentially bringing the virus home. A lot of generations live in the same household. Elders were vulnerable to getting the infection, and there was little ability to isolate if someone wasn’t having symptoms. Hospitals nearby didn’t have ICUs.
Therefore, the rate of cases skyrocketed early on. We were disproportionately affected. The Navajo nation per capita had the highest rate of cases in any state.
Q: What changes took place within the Navajo nation to get people vaccinated? What role did the federal Indian Health Service have in promoting this?
A: There had to be a shift in acceptance of the vaccinations.
With the IHS, we went into a disaster response mode with all-hands-on deck meetings. We had to figure out how we could access mass vaccination clinics. Partnering with the Navajo Department of Health, we did that right away with hospitals and small clinics across the Navajo nation. Casinos owned by tribal entities that closed during COVID reopened and were used as vaccination clinics.
Vaccinations were sent to us fairly quickly. I ended up getting vaccinated in December 2020, when it was first rolled out.
Native and Navajo individuals have been reluctant to rely on government services. Because IHS came through with the vaccines, COVID reduced that stigma to access its services. Even the Navajo Department of Health partnered with the Indian Health Service to provide culturally relevant campaigns that explain why the vaccine is valuable.
I think because people were so impacted, they saw something valuable with the vaccine. Given the education and access, people were ready to get vaccinated. They realized if a whole household got vaccinated, they could see early on that they could be social again.
Q: What cultural factors have been contributing to this positive development?
A: In our Navajo culture, we’ve dealt with monsters before. We talk about that in terms of how we teach our young people to be strong and resilient. We talked about this virus as being another monster we had to tackle and control. The teaching was along those lines. We’ve dealt with this before, and we can handle it. We’re resilient. Our culture is very strong in that way. So how do we do it? We have to partner; we have to embrace Western medicine to return back to the ceremonies we want to have again and be social again. We focus on positive things, so if we see something as potentially positive, such as the vaccine, we see that and know that’s something to help us come into our life again.
Q: I would expect that protecting elders in the tribe would be a big incentive in taking the vaccine.
A: Yes, we didn’t want to lose our language and culture, and we wanted to protect our elders. Having a way to do that was very important as well. They were among the first to get vaccinated.
Q: What is the current vaccination rate in the Navajo nation?
A: I think it’s in the upper 80th percentile. It’s very high.
Q: What have been the biggest takeaways so far, and what are your hopes for the future?
A: Even though the Navajo Nation has been impacted and devastated with the loss of elders and knowledge keepers, we still have our culture and ceremonies intact to the point that we know we can be resilient get through this difficult time.
Through collaborations with the federal and state governments and the clinics, we see that things are different now. Going forward, my hope is these partnerships will continue, that we’ll build those relationships and not be so siloed in our care. When the New Mexico Department of Health rolled out its first vaccination clinic, for example, we jumped on and saw how they did it. We were then able to do our own, collaborating with the state.
We also saw how important our culture was, how it helped our Navajo people through these difficult times.
Dr. Roessel, a distinguished fellow of the American Psychiatric Association, has special expertise in cultural psychiatry. Her childhood was spent growing up in the Navajo nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating Indigenous knowledge and principles.
References
American Public Media Research Lab. “The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.” 2021 Mar 5.
Centers for Disease Control and Prevention. “Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States.” Data as of 2021 Oct 14.
Navajo Nation. Indian Health Service. U.S. Department of Health & Human Services.
The Navajo Nation’s Office of the President and Vice President. “11 New Cases, 32,735 Recoveries, and Six Recent Deaths Related to COVID-19.” 2021 Oct 13.
Navajo Nation Government web page.
COVID-19 has killed Native Americans at twice the rate of White Americans, underscoring the health inequities and deep-rooted distrust tribal nations have of federal government entities.
And yet, Native Americans have the highest vaccination rates of any major racial or ethnic group in the United States. Like many other tribal nations, the Navajo had to embrace Western science to reclaim its social customs and ceremonies. “We’re a very social culture, so having to isolate really impacted our mental health,” said Mary Hasbah Roessel, MD, DLFAPA, a Navajo psychiatrist who is affiliated with Santa Fe Indian Hospital in New Mexico.
The Navajo nation occupies the largest Native American reservation in the United States, spanning New Mexico, Arizona, and Utah. As of mid-October, the nation had reported more than 34,000 COVID-19 cases and 1,400 deaths in its jurisdiction.
In an interview with this news organization, Dr. Roessel described the partnerships that mobilized a nation of more than 250,000 individuals to get vaccinated.
Question: Why has the death rate been so high in the Navajo nation?
Answer: A lot of health disparities before the pandemic were blatantly revealed during COVID. Only 40% of people on the reservation had running water. Having to stay home and isolate led to food insecurity. Further insecurity issues affected our ability to stay healthy, such as having good sanitation. There’s a lot of poverty, a high unemployment rate. Some people had to go to work off reservation and were potentially bringing the virus home. A lot of generations live in the same household. Elders were vulnerable to getting the infection, and there was little ability to isolate if someone wasn’t having symptoms. Hospitals nearby didn’t have ICUs.
Therefore, the rate of cases skyrocketed early on. We were disproportionately affected. The Navajo nation per capita had the highest rate of cases in any state.
Q: What changes took place within the Navajo nation to get people vaccinated? What role did the federal Indian Health Service have in promoting this?
A: There had to be a shift in acceptance of the vaccinations.
With the IHS, we went into a disaster response mode with all-hands-on deck meetings. We had to figure out how we could access mass vaccination clinics. Partnering with the Navajo Department of Health, we did that right away with hospitals and small clinics across the Navajo nation. Casinos owned by tribal entities that closed during COVID reopened and were used as vaccination clinics.
Vaccinations were sent to us fairly quickly. I ended up getting vaccinated in December 2020, when it was first rolled out.
Native and Navajo individuals have been reluctant to rely on government services. Because IHS came through with the vaccines, COVID reduced that stigma to access its services. Even the Navajo Department of Health partnered with the Indian Health Service to provide culturally relevant campaigns that explain why the vaccine is valuable.
I think because people were so impacted, they saw something valuable with the vaccine. Given the education and access, people were ready to get vaccinated. They realized if a whole household got vaccinated, they could see early on that they could be social again.
Q: What cultural factors have been contributing to this positive development?
A: In our Navajo culture, we’ve dealt with monsters before. We talk about that in terms of how we teach our young people to be strong and resilient. We talked about this virus as being another monster we had to tackle and control. The teaching was along those lines. We’ve dealt with this before, and we can handle it. We’re resilient. Our culture is very strong in that way. So how do we do it? We have to partner; we have to embrace Western medicine to return back to the ceremonies we want to have again and be social again. We focus on positive things, so if we see something as potentially positive, such as the vaccine, we see that and know that’s something to help us come into our life again.
Q: I would expect that protecting elders in the tribe would be a big incentive in taking the vaccine.
A: Yes, we didn’t want to lose our language and culture, and we wanted to protect our elders. Having a way to do that was very important as well. They were among the first to get vaccinated.
Q: What is the current vaccination rate in the Navajo nation?
A: I think it’s in the upper 80th percentile. It’s very high.
Q: What have been the biggest takeaways so far, and what are your hopes for the future?
A: Even though the Navajo Nation has been impacted and devastated with the loss of elders and knowledge keepers, we still have our culture and ceremonies intact to the point that we know we can be resilient get through this difficult time.
Through collaborations with the federal and state governments and the clinics, we see that things are different now. Going forward, my hope is these partnerships will continue, that we’ll build those relationships and not be so siloed in our care. When the New Mexico Department of Health rolled out its first vaccination clinic, for example, we jumped on and saw how they did it. We were then able to do our own, collaborating with the state.
We also saw how important our culture was, how it helped our Navajo people through these difficult times.
Dr. Roessel, a distinguished fellow of the American Psychiatric Association, has special expertise in cultural psychiatry. Her childhood was spent growing up in the Navajo nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating Indigenous knowledge and principles.
References
American Public Media Research Lab. “The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.” 2021 Mar 5.
Centers for Disease Control and Prevention. “Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States.” Data as of 2021 Oct 14.
Navajo Nation. Indian Health Service. U.S. Department of Health & Human Services.
The Navajo Nation’s Office of the President and Vice President. “11 New Cases, 32,735 Recoveries, and Six Recent Deaths Related to COVID-19.” 2021 Oct 13.
Navajo Nation Government web page.
Call them by their names in your office
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.







