User login
Basal Cell Carcinoma
THE COMPARISON
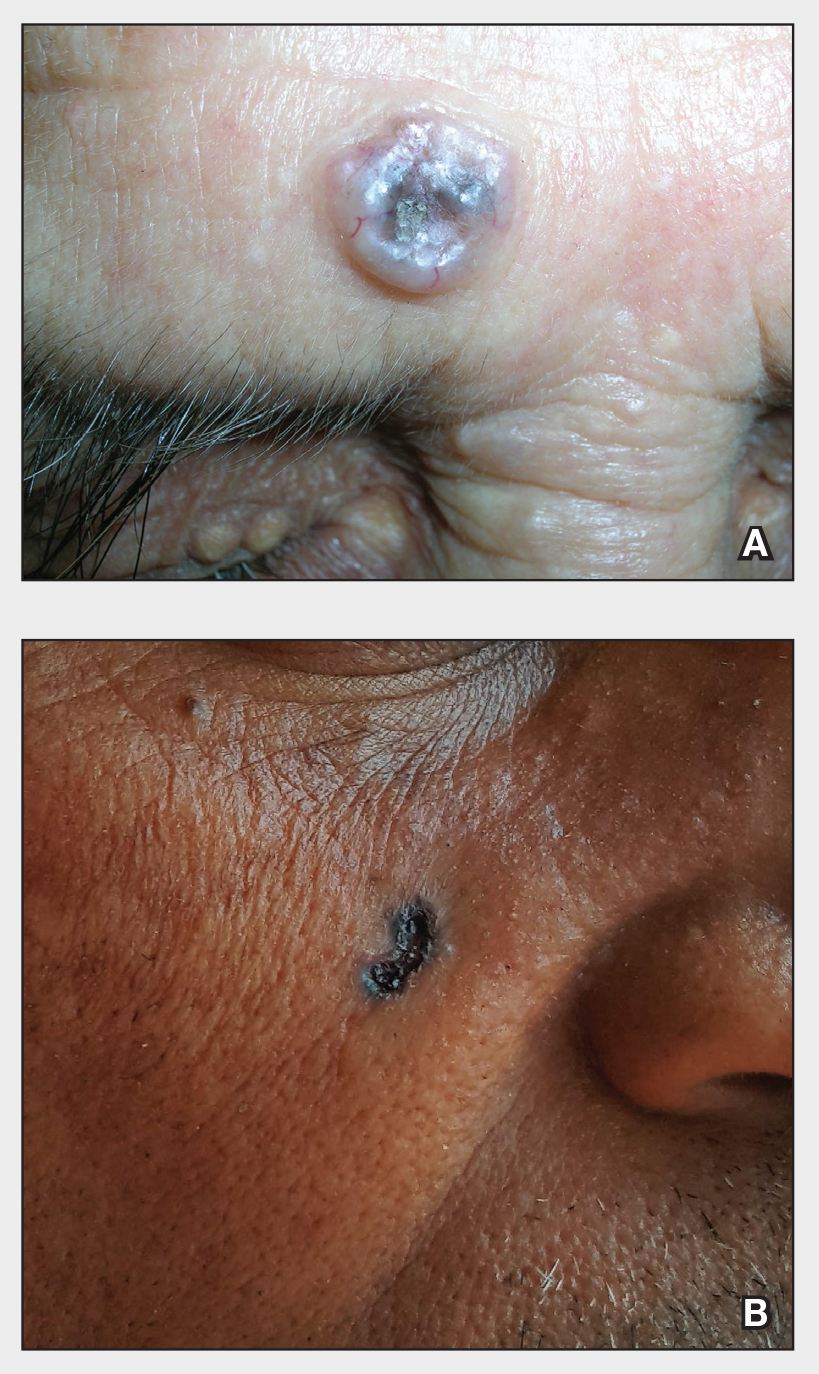
A Nodular basal cell carcinoma (BCC) with a pearly rolled border, central pigmentation, and telangiectasia on the forehead of an 80-year-old Hispanic woman (light skin tone).
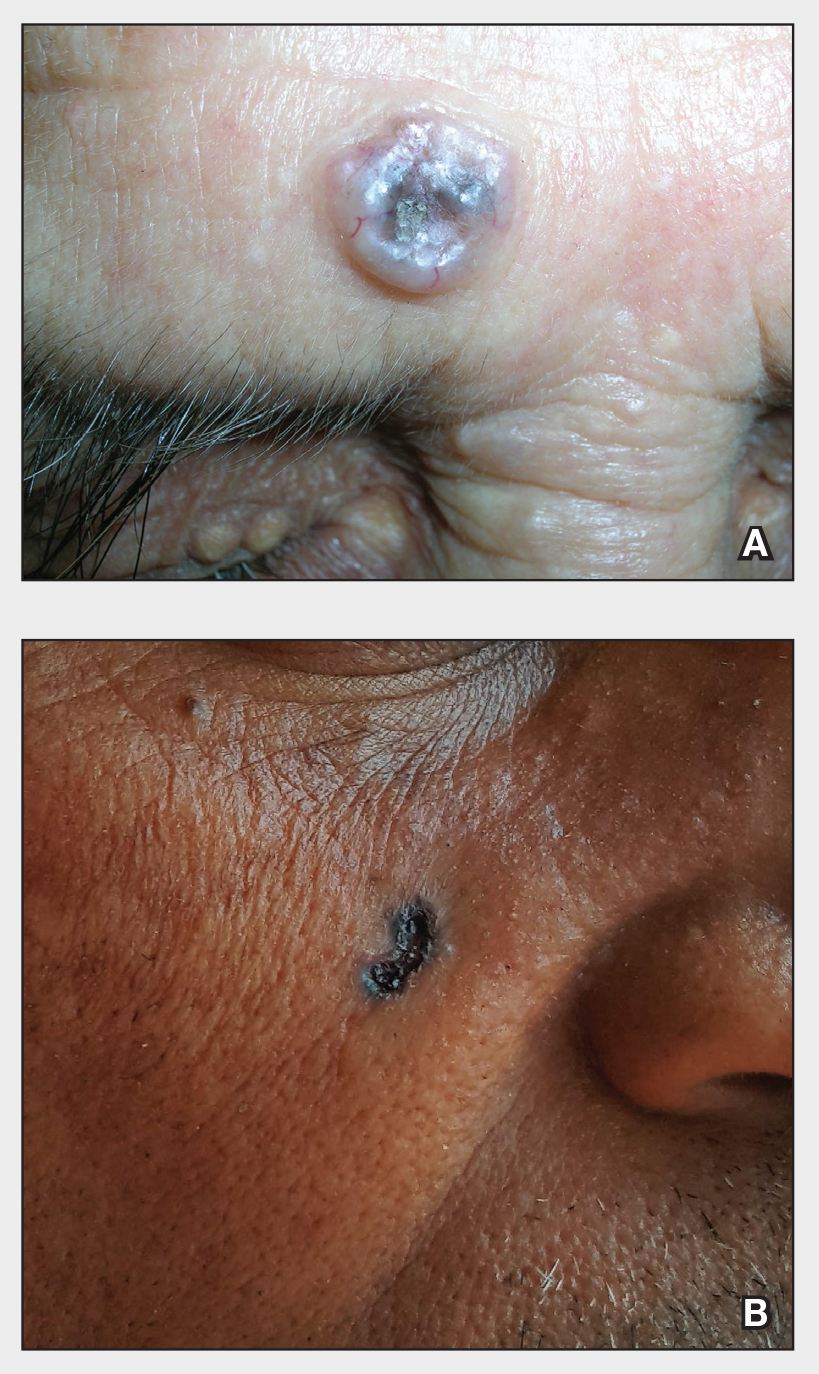
B Nodular BCC on the cheek of a 64-year-old Black man. The dark nonhealing ulcer had a subtle, pearly, rolled border and no visible telangiectasia.
Basal cell carcinoma is most prevalent in individuals with lighter skin tones and rarely affects those with darker skin tones. Unfortunately, the lower incidence and lack of surveillance frequently result in a delayed diagnosis and increased morbidity for the skin of color population.1
Epidemiology
Basal cell carcinoma is the most common skin cancer in White, Asian, and Hispanic individuals and the second most common in Black individuals. Squamous cell carcinoma is the most common skin cancer in Black individuals.2
Although BCCs are rare in individuals with darker skin tones, they most often develop in sun-exposed areas of the head and neck region.1 In one study in an academic urban medical center, BCCs were more likely to occur in lightly pigmented vs darkly pigmented Black individuals.3
Key clinical features in people with darker skin tones
The classic BCC manifestation of a pearly papule with rolled borders and telangiectasia may not be seen in the skin of color population, especially among those with darker skin tones.4 In patient A, a Hispanic woman, these features are present along with hyperpigmentation. More than 50% of BCCs are pigmented in patients with skin of color vs only 5% in White individuals.5-7 The incidence of a pigmented BCC is twice as frequent in Hispanic individuals (Figure, A) as in non-Hispanic White individuals.7 Any skin cancer can present with ulcerations, so while this is not specific to BCC, it is a reason to consider biopsy.
Worth noting
Pigmented BCC can mimic melanoma clinically and even when viewed with a dermatoscope, but such a suspicious lesion should prompt the clinician to perform a biopsy regardless of the type of suspected cancer. With experience and training, however, physicians can use dermoscopy to help make this distinction.
Note that skin of color is found in a heterogeneous population with a spectrum of skin tones and genetic/ ethnic variability. In my practice in San Antonio (R.P.U.), BCC is uncommon in Black patients and relatively common in Hispanic patients with lighter skin tones (Figure, A). There is speculation that a lower incidence of BCC in the skin of color population leads to a low index of suspicion, which contributes to delayed diagnoses with poorer outcomes. 1 There are no firm data to support this because the rare occurrence of BCC in darker skin tones makes this a challenge to study.
Health disparity highlight
In general, barriers to health care include poverty, lack of education, lack of health insurance, and systemic racism. One study on keratinocyte skin cancers including BCC and SCC found that these cancers were more costly to treat and required more health care resources, such as ambulatory visits and medication costs, in non-Hispanic Black and Hispanic White patients compared to non- Hispanic White patients.8
Final thoughts
Efforts are needed to achieve health equity through education of patients and health care providers about the appearance of BCC in skin of color with the goal of earlier diagnosis. Any nonhealing ulcer on the skin (Figure, B) should prompt consideration of skin cancer regardless of skin color.
- Ahluwalia J, Hadjicharalambous E, Mehregan D. Basal cell carcinoma in skin of color. J Drugs Dermatol. 2012;11:484-486.
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. doi:10.1007/s40257-021-00662-z
- Halder RM, Bang KM. Skin cancer in blacks in the United States. Dermatol Clin. 1988;6:397-405.
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Matsuoka LY, Schauer PK, Sordillo PP. Basal cell carcinoma in black patients. J Am Acad Dermatol. 1981;4:670-672. doi:10.1016/S0190-9622(81)70067-7
- Bigler C, Feldman J, Hall E, et al. Pigmented basal cell carcinoma in Hispanics. J Am Acad Dermatol. 1996;34:751-752. doi:10.1016/S0190-9622(96)90007-9
- Sierro TJ, Blumenthal LY, Hekmatjah J, et al. Differences in health care resource utilization and costs for keratinocyte carcinoma among racioethnic groups: a population-based study [published online July 9, 2021]. J Am Acad Dermatol. 2022;86:373-378. doi:10.1016/j.jaad.2021.07.005
THE COMPARISON
A Nodular basal cell carcinoma (BCC) with a pearly rolled border, central pigmentation, and telangiectasia on the forehead of an 80-year-old Hispanic woman (light skin tone).
B Nodular BCC on the cheek of a 64-year-old Black man. The dark nonhealing ulcer had a subtle, pearly, rolled border and no visible telangiectasia.
Basal cell carcinoma is most prevalent in individuals with lighter skin tones and rarely affects those with darker skin tones. Unfortunately, the lower incidence and lack of surveillance frequently result in a delayed diagnosis and increased morbidity for the skin of color population.1
Epidemiology
Basal cell carcinoma is the most common skin cancer in White, Asian, and Hispanic individuals and the second most common in Black individuals. Squamous cell carcinoma is the most common skin cancer in Black individuals.2
Although BCCs are rare in individuals with darker skin tones, they most often develop in sun-exposed areas of the head and neck region.1 In one study in an academic urban medical center, BCCs were more likely to occur in lightly pigmented vs darkly pigmented Black individuals.3
Key clinical features in people with darker skin tones
The classic BCC manifestation of a pearly papule with rolled borders and telangiectasia may not be seen in the skin of color population, especially among those with darker skin tones.4 In patient A, a Hispanic woman, these features are present along with hyperpigmentation. More than 50% of BCCs are pigmented in patients with skin of color vs only 5% in White individuals.5-7 The incidence of a pigmented BCC is twice as frequent in Hispanic individuals (Figure, A) as in non-Hispanic White individuals.7 Any skin cancer can present with ulcerations, so while this is not specific to BCC, it is a reason to consider biopsy.
Worth noting
Pigmented BCC can mimic melanoma clinically and even when viewed with a dermatoscope, but such a suspicious lesion should prompt the clinician to perform a biopsy regardless of the type of suspected cancer. With experience and training, however, physicians can use dermoscopy to help make this distinction.
Note that skin of color is found in a heterogeneous population with a spectrum of skin tones and genetic/ ethnic variability. In my practice in San Antonio (R.P.U.), BCC is uncommon in Black patients and relatively common in Hispanic patients with lighter skin tones (Figure, A). There is speculation that a lower incidence of BCC in the skin of color population leads to a low index of suspicion, which contributes to delayed diagnoses with poorer outcomes. 1 There are no firm data to support this because the rare occurrence of BCC in darker skin tones makes this a challenge to study.
Health disparity highlight
In general, barriers to health care include poverty, lack of education, lack of health insurance, and systemic racism. One study on keratinocyte skin cancers including BCC and SCC found that these cancers were more costly to treat and required more health care resources, such as ambulatory visits and medication costs, in non-Hispanic Black and Hispanic White patients compared to non- Hispanic White patients.8
Final thoughts
Efforts are needed to achieve health equity through education of patients and health care providers about the appearance of BCC in skin of color with the goal of earlier diagnosis. Any nonhealing ulcer on the skin (Figure, B) should prompt consideration of skin cancer regardless of skin color.
THE COMPARISON
A Nodular basal cell carcinoma (BCC) with a pearly rolled border, central pigmentation, and telangiectasia on the forehead of an 80-year-old Hispanic woman (light skin tone).
B Nodular BCC on the cheek of a 64-year-old Black man. The dark nonhealing ulcer had a subtle, pearly, rolled border and no visible telangiectasia.
Basal cell carcinoma is most prevalent in individuals with lighter skin tones and rarely affects those with darker skin tones. Unfortunately, the lower incidence and lack of surveillance frequently result in a delayed diagnosis and increased morbidity for the skin of color population.1
Epidemiology
Basal cell carcinoma is the most common skin cancer in White, Asian, and Hispanic individuals and the second most common in Black individuals. Squamous cell carcinoma is the most common skin cancer in Black individuals.2
Although BCCs are rare in individuals with darker skin tones, they most often develop in sun-exposed areas of the head and neck region.1 In one study in an academic urban medical center, BCCs were more likely to occur in lightly pigmented vs darkly pigmented Black individuals.3
Key clinical features in people with darker skin tones
The classic BCC manifestation of a pearly papule with rolled borders and telangiectasia may not be seen in the skin of color population, especially among those with darker skin tones.4 In patient A, a Hispanic woman, these features are present along with hyperpigmentation. More than 50% of BCCs are pigmented in patients with skin of color vs only 5% in White individuals.5-7 The incidence of a pigmented BCC is twice as frequent in Hispanic individuals (Figure, A) as in non-Hispanic White individuals.7 Any skin cancer can present with ulcerations, so while this is not specific to BCC, it is a reason to consider biopsy.
Worth noting
Pigmented BCC can mimic melanoma clinically and even when viewed with a dermatoscope, but such a suspicious lesion should prompt the clinician to perform a biopsy regardless of the type of suspected cancer. With experience and training, however, physicians can use dermoscopy to help make this distinction.
Note that skin of color is found in a heterogeneous population with a spectrum of skin tones and genetic/ ethnic variability. In my practice in San Antonio (R.P.U.), BCC is uncommon in Black patients and relatively common in Hispanic patients with lighter skin tones (Figure, A). There is speculation that a lower incidence of BCC in the skin of color population leads to a low index of suspicion, which contributes to delayed diagnoses with poorer outcomes. 1 There are no firm data to support this because the rare occurrence of BCC in darker skin tones makes this a challenge to study.
Health disparity highlight
In general, barriers to health care include poverty, lack of education, lack of health insurance, and systemic racism. One study on keratinocyte skin cancers including BCC and SCC found that these cancers were more costly to treat and required more health care resources, such as ambulatory visits and medication costs, in non-Hispanic Black and Hispanic White patients compared to non- Hispanic White patients.8
Final thoughts
Efforts are needed to achieve health equity through education of patients and health care providers about the appearance of BCC in skin of color with the goal of earlier diagnosis. Any nonhealing ulcer on the skin (Figure, B) should prompt consideration of skin cancer regardless of skin color.
- Ahluwalia J, Hadjicharalambous E, Mehregan D. Basal cell carcinoma in skin of color. J Drugs Dermatol. 2012;11:484-486.
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. doi:10.1007/s40257-021-00662-z
- Halder RM, Bang KM. Skin cancer in blacks in the United States. Dermatol Clin. 1988;6:397-405.
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Matsuoka LY, Schauer PK, Sordillo PP. Basal cell carcinoma in black patients. J Am Acad Dermatol. 1981;4:670-672. doi:10.1016/S0190-9622(81)70067-7
- Bigler C, Feldman J, Hall E, et al. Pigmented basal cell carcinoma in Hispanics. J Am Acad Dermatol. 1996;34:751-752. doi:10.1016/S0190-9622(96)90007-9
- Sierro TJ, Blumenthal LY, Hekmatjah J, et al. Differences in health care resource utilization and costs for keratinocyte carcinoma among racioethnic groups: a population-based study [published online July 9, 2021]. J Am Acad Dermatol. 2022;86:373-378. doi:10.1016/j.jaad.2021.07.005
- Ahluwalia J, Hadjicharalambous E, Mehregan D. Basal cell carcinoma in skin of color. J Drugs Dermatol. 2012;11:484-486.
- Zakhem GA, Pulavarty AN, Lester JC, et al. Skin cancer in people of color: a systematic review. Am J Clin Dermatol. 2022;23:137-151. doi:10.1007/s40257-021-00662-z
- Halder RM, Bang KM. Skin cancer in blacks in the United States. Dermatol Clin. 1988;6:397-405.
- Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37:519-526. doi:10.1016/j.det.2019.05.009
- Agbai ON, Buster K, Sanchez M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70:748-762. doi:10.1016/j.jaad.2013.11.038
- Matsuoka LY, Schauer PK, Sordillo PP. Basal cell carcinoma in black patients. J Am Acad Dermatol. 1981;4:670-672. doi:10.1016/S0190-9622(81)70067-7
- Bigler C, Feldman J, Hall E, et al. Pigmented basal cell carcinoma in Hispanics. J Am Acad Dermatol. 1996;34:751-752. doi:10.1016/S0190-9622(96)90007-9
- Sierro TJ, Blumenthal LY, Hekmatjah J, et al. Differences in health care resource utilization and costs for keratinocyte carcinoma among racioethnic groups: a population-based study [published online July 9, 2021]. J Am Acad Dermatol. 2022;86:373-378. doi:10.1016/j.jaad.2021.07.005
Assessing Treatment Delays for Vitiligo Patients: A Retrospective Chart Review
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
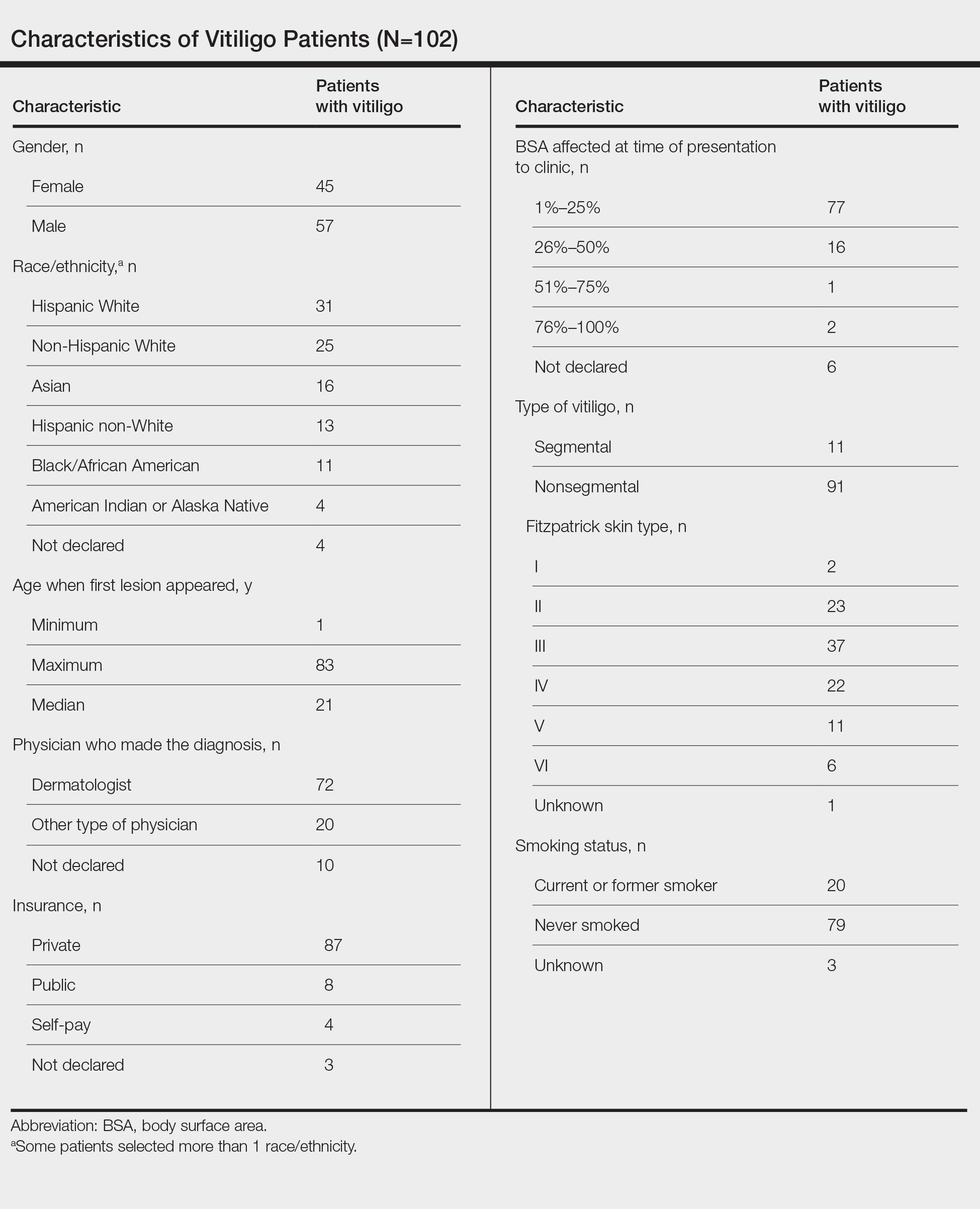
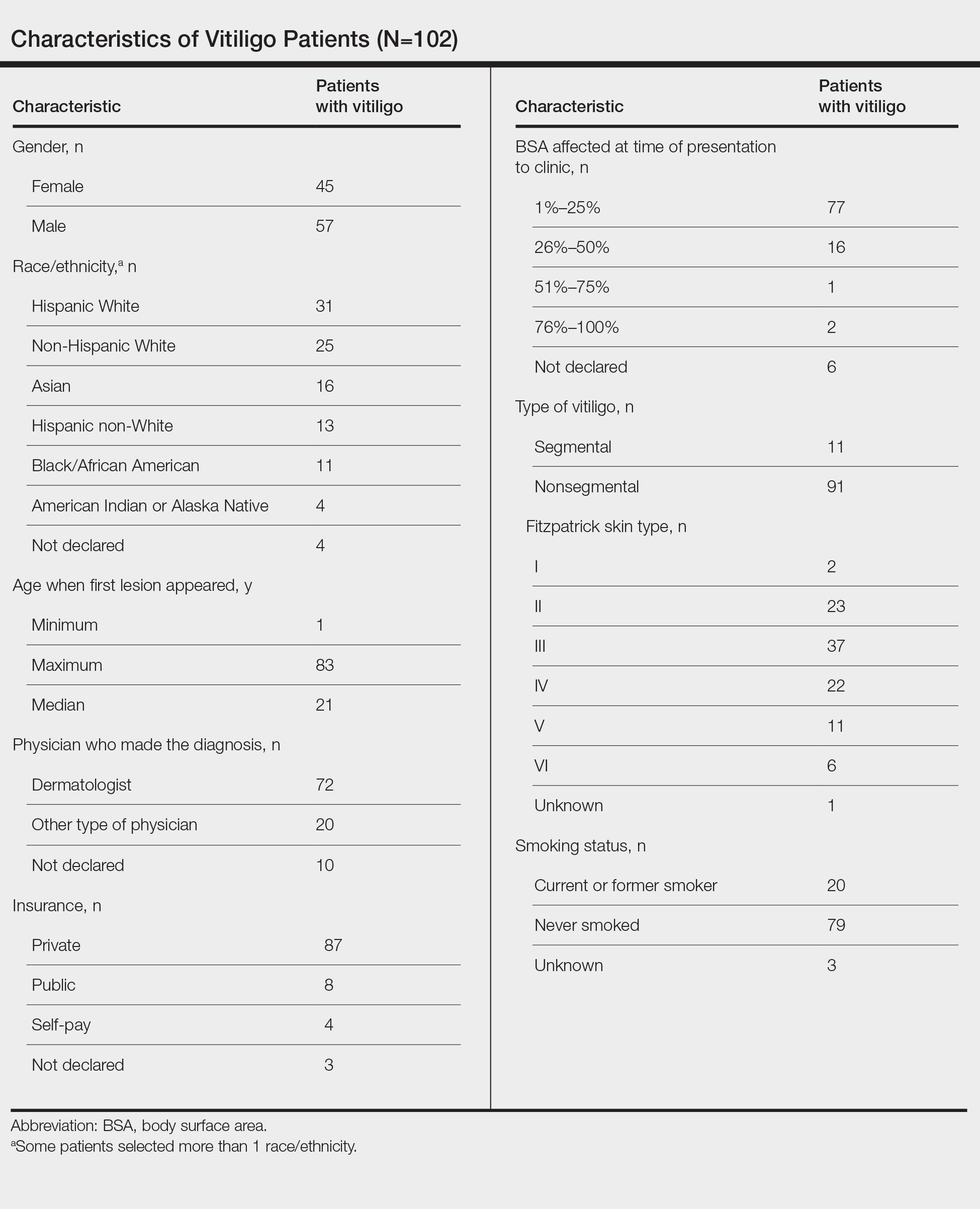
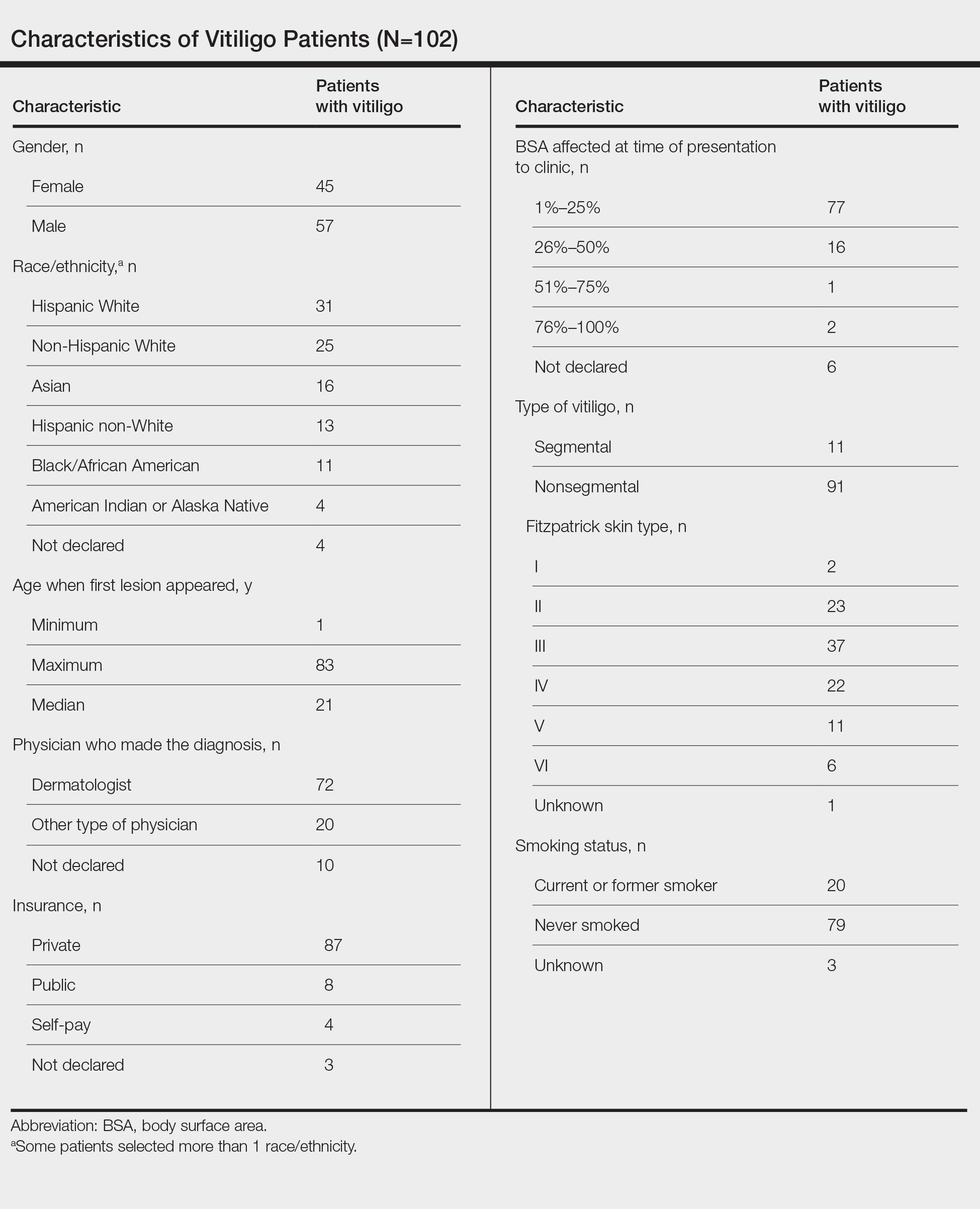
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
Similar to other dermatologic conditions, barriers to early care in patients with vitiligo can exacerbate health disparities.1 Delayed treatment of vitiligo is known to hamper successful disease stabilization and repigmentation, as therapies tend to work more effectively in early stages of the disease.2
To investigate the factors associated with treatment delays for patients with vitiligo, we conducted a retrospective chart review of 102 consecutive patients with vitiligo attending an academic outpatient clinic in Austin, Texas, over 36 months.
Methods
Our sample included 102 consecutive patients with vitiligo who attended an academic outpatient clinic in Austin, Texas, from January 2017 to January 2020. Demographic information, clinical characteristics of vitiligo, and treatment data were self-reported via a standardized questionnaire given to all patients with vitiligo and gathered from medical chart review. Patient characteristics are outlined in the Table. The delay to treatment was the time (in months) from the date the patient first noticed the lesion to the start date of first treatment. This retrospective chart review was reviewed by the University of Texas at Austin institutional review board and was determined to be exempt.
Statistical Analysis—The data were analyzed descriptively with a Wilcoxon rank sum test (type I error rate of .05).
Results
Of the 102 charts that were analyzed, 45 were females and 57 were males. More than half of the patients (54.9% [56/102]) were White. Sixteen were Asian, 13 were Hispanic non-White, 11 were Black/African American, and 4 were American Indian/Alaska Native. The median age of disease onset was 21 years, minimum age was 1 year, and maximum age was 83 years. The diagnosis of vitiligo was made by a dermatologist for 72 patients and by a physician of another specialty for 20 patients. Ten patients did not declare the specialty of the diagnosing physician.
Individuals older than 21 years when their disease started had a shorter delay to treatment than individuals who noticed their first lesion at an age younger than 21 years (median, 75 months vs 13 months; P<.01). Individuals diagnosed by a dermatologist had a shorter delay to treatment than individuals diagnosed by a physician of another specialty (median, 13 months vs 58 months; P<.05). White individuals had a shorter delay to treatment than individuals with skin of color (median, 13 months vs 31 months; P=.08), though this trend did not reach statistical significance. Individuals with 1% to 25% of body surface area (BSA) affected at time of presentation to clinic also had a shorter delay to treatment than those with a greater BSA affected (median, 13 months vs 74 months; P<.06), though this trend did not reach statistical significance. Type of vitiligo (P<.8), Fitzpatrick skin type (P<.6), and smoking status (P<.7) were not associated with differential delays.
Comment
Impact of Age on Vitiligo Treatment—Our data suggest that individuals who develop vitiligo at a younger age experience longer treatment delays compared to older individuals. Reasons for this are uncertain but could include access issues, medical decision-making agency, and younger patients not remembering being treated during their youth. Our data also could be influenced by some of the adult patients in our study first noticing their lesions many years ago when treatments for vitiligo were more limited. Nevertheless, detrimental effects on quality of life in children and adolescents with vitiligo suggest that motivating younger individuals with vitiligo to seek treatment or proactively making them aware of treatment opportunities may be beneficial.3
Diagnosis of Vitiligo by Nondermatologists—The increase in delay to treatment when a nondermatologist diagnoses vitiligo suggests that prompt initiation of treatment or referrals to dermatology by primary care providers may not routinely be occurring.4 Our data indicate the need to educate primary care providers on treatment opportunities for individuals with vitiligo and that early treatment generally is more effective.5
Impact of Race/Ethnicity on Vitiligo Treatment—Our data also show trends for longer treatment delays for individuals with skin of color. Although this did not reach statistical significance, we hope future studies will investigate this issue, especially because patients with skin of color experience more stigmatization and quality-of-life impacts by vitiligo than White patients.5
Impact of BSA on Vitiligo Treatment—Our data show that patients with a smaller BSA had a shorter delay to treatment than those with a greater BSA affected. This was a unique finding given it initially was hypothesized that patients with greater BSA would seek treatment earlier because of the associated increase in quality of life impact. This trend was not statistically significant, but further investigation would be helpful to analyze the reason behind treatment delays in patients with greater BSA affected.
Conclusion
The delay to treatment in our study population was correlated with the diagnosing physician’s specialty and patient age at disease onset, with trends also observed for race and BSA affected. These findings emphasize the need to investigate specific causes of barriers to early care to promote health equity among individuals with vitiligo.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
- Tripathi R, Archibald LK, Mazmudar RS, et al. Racial differences in time to treatment for melanoma. J Am Acad Dermatol. 2020;83:854-859.
- Boniface K, Seneschal J. Vitiligo as a skin memory disease: the need for early intervention with immunomodulating agents and a maintenance therapy to target resident memory T cells. Exp Dermatol. 2019;28:656-661.
- Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents with vitiligo. Pediatr Dermatol. 2014;31:309-318.
- Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the dermatology life quality index outcome over the past two decades. Int J Dermatol. 2016;55:608-614.
- Weibel L, Laguda B, Atherton D, et al. Misdiagnosis and delay in referral of children with localized scleroderma. Br J Dermatol. 2011;165:1308-1313.
Practice Points
- The medical community should be aware of factors associated with delay to treatment in patients with vitiligo, such as the diagnosing physician’s specialty and patient age at disease onset.
- Race and percentage of body surface area affected at time of presentation also demonstrate trends regarding treatment delays in patients with vitiligo.
Asian American teens have highest rate of suicidal ideation
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
AT APA 2022
Going Beyond Hydroquinone: Alternative Skin Lightening Agents
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
Disorders of hyperpigmentation—melasma, postinflammatory hyperpigmentation, lichen planus pigmentosus, erythema dyschromicum perstans, and pigmented contact dermatitis, among others—are common and challenging to treat. Although they can affect individuals of all skin types, they most commonly are seen in skin of color; in fact, dyspigmentation is one of the most common chief concerns for which individuals of color see a dermatologist.1,2
For many years, hydroquinone (HQ) was one of the main options available for use as a lightening agent. Although effective, it has the risk of causing irritant dermatitis, potentially leading to further dyspigmentation, in addition to the risk of ochronosis with long-term use. It remains an important and useful treatment for pigmentary disorders, but there are numerous other lightening agents that also can be considered in the treatment of disorders of hyperpigmentation.
Herein, we provide recommendations for traditional and newer non-HQ lightening agents that can be considered when treating disorders of hyperpigmentation.
Traditional Non-HQ Lightening Agents
Retinoids—Retinoids are topical vitamin A derivatives that have been used safely and effectively for decades in the treatment of pigmentary disorders. Retinoids have multiple mechanisms of action in improving pigmentation. In addition to impeding tyrosinase induction, they inhibit pigment transfer to keratinocytes and lead to accelerated pigment loss due to epidermal shedding.3 Over-the-counter formulations include retinol, retinaldehyde, and adapalene. Prescription formulations include tretinoin and tazarotene in different strengths and vehicle formulations.4
Glycolic Acid—Glycolic acid is derived from sugarcane and is considered an α-hydroxy acid that leads to rapid desquamation of pigmented keratinocytes.5 Glycolic acid can not only be used in chemical peels but also in topical creams. It is the most common α-hydroxy acid peel and is sometimes paired with HQ and other topical lightening agents for increased penetration. Glycolic acid peels are available in concentrations of 20% to 70% and can be used at various depths. When used incorrectly, it can cause redness, burning, and even skin discoloration; however, when used at the proper concentrations and depth according to Fitzpatrick skin type, there typically are no notable adverse effects, and clinical results are favorable.
Kojic Acid—Kojic acid is a natural metabolite derived from fungi and is widely used in Asian countries. It works by inhibiting the catecholase activity of tyrosinase6 and typically is available in concentrations of 1% to 4%. A study suggested that a concentration of 1% or less typically is safe to use for prolonged periods without adverse effects. Although not more effective than HQ as a monotherapy, kojic acid has been shown to haveimproved efficacy when used in combination with other lightening agents.7
Azelaic Acid—Azelaic acid works by inhibiting tyrosinase, mitochondrial oxidoreductase activation, and DNA synthesis. It preferentially targets heavily pigmented melanocytes and possesses anti-inflammatory and antibacterial properties.8 A 20% concentration of azelaic acid was compared to HQ 4% for the treatment of melasma, and results revealed that the liposomal form of azelaic acid was considerably more tolerable than HQ 4% and also more effective.9
Licorice Extracts—Licorice extracts have been safely used in several cosmeceutical skin lightening products.10 The main active compounds in licorice root are glabridin and liquiritin, which work to disperse melanin. These compounds often are used topically at concentrations of 10% to 40%. A study by Amer and Metwalli11 found that topical liquiritin produced a reduction of pigmentary intensity, with 80% of patients showing an excellent response, which was described as no difference between the previously pigmented area and the normal skin surrounding it.
Aloesin—Aloesin is a low-molecular-weight glycoprotein found in aloe vera plants. Its mechanism of action includes competitive inhibition of the dihydroxyphenylalanine oxidation site, resulting in the inhibition of tyrosinase.12 It often is combined with arbutin for an enhanced lightening effect.
Niacinamide—Niacinamide is a form of vitamin B3 that works by suppressing the transfer of melanosomes to keratinocytes.13 In addition to its skin lightening effects, it also is photoprotective and antimicrobial, and its tolerability and safety have led to its inclusion in many cosmeceutical and prescription products.14
Ascorbic Acid—Ascorbic acid affects the monopherase activity of tyrosinase, thus reducing the synthesis of melanin. It also serves as an antioxidant in the skin by preventing the production of free radicals that can induce melanogenesis.15 Although it tends to be well tolerated with a low adverse effect profile, its relative instability and varying permeability can present a challenge. It is less effective as a monotherapy, so it often is combined with other lightening ingredients for greater efficacy.
Corticosteroids—Topical corticosteroids are anti-inflammatory and impact melanogenesis, though the mechanism of action of the latter has not been fully elucidated.16,17 Low- to mid-potency topical steroids often are used in conjunction with skin lightening products to diminish irritation and decrease inflammation.18 However, prolonged use of corticosteroids can lead to cutaneous adverse effects such as striae, hypopigmentation, and acne, as well as systemic side effects if there is sufficient absorption over time.
Soybean Extracts—Soybean extracts contain serine protease inhibitors that reduce the transfer of melanosomes into keratinocytes by inhibiting the PAR-2 (protease-activated receptor 2) pathway.19,20
Ellagic Acid—Ellagic acid is found in common plants such as eucalyptus and strawberry as well as green tea.21 It works as an antioxidant and decreases melanogenesis through inhibition of tyrosinase activity.
Paper Mulberry—Paper mulberry extract comes from the roots of the Broussonetia papyrifera tree and functions by inhibiting tyrosinase activity. It is widely used in South Africa and Europe.22
Resveratrol—Resveratrol is an ingredient extracted from Morus alba L and functions as an antimelanogentic agent by directly inhibiting tyrosinase as well as transcriptional and posttranscriptional processing of tyrosinase.23 It also holds antiproliferative, anti-inflammatory, and antioxidant properties and has widely been used for antiaging and skin lightening purposes.24
Newer Non-HQ Lightening Agents
Silymarin—Silymarin (also known as milk thistle [Silybum marianum]), is a polyphenolic flavonoid that possesses anticarcinogenic, antioxidant, and anti-inflammatory properties. It prevents melanin production in a dose-dependent manner by inhibiting levodopa (L-dopa) oxidation activity of tyrosinase and also reduces the expression of tyrosinase protein.25 In combination with vitamins C and E and hexylresorcinol, silymarin has been found to reduce the effects of photodamage, brighten skin, improve evenness and lines, as well as improve global facial appearance.26
Malassezin—Malassezin is an indole produced by Malessezia furfur yeast and has recently been investigated for melanogenesis suppression. Grimes et al27 assessed the efficacy of topical malassezin in 7 patients with facial hyperpigmentation applied twice daily for 14 weeks. Punch biopsies were taken at weeks 0, 8, 14, and 22. Biopsies from weeks 8 and 14 demonstrated reduced epidermal melanin compared to baseline in all participants; however, at 22 weeks, biopsies showed no difference in melanin content compared to baseline, indicating a temporary process induced by the malassezin.27 More clinical studies are needed to investigate this further.
N-acetyl-glucosamine—N-acetyl-glucosamine is an aminosaccharide that inhibits the glycosylation of tyrosinase as well as its function in melanogenesis.28 It is synthesized and included in topical products for wound healing, rhytides, moisturization, and pigmentation disorders.
Topical Tranexamic Acid—Tranexamic acid traditionally has been used orally for the treatment of menorrhagia but also has been found to be beneficial as a therapy for hyperpigmentation and erythema. Tranexamic acid interferes with plasmin activity, thus indirectly inhibiting melanogenesis while also inhibiting angiogenesis by targeting vascular endothelial growth factor (VEGF) receptors.29 It also leads to an increase in the levels of β-endorphin and μ-opioid receptors as well as the expression of estrogen receptor β on the surface of mast cells.30 Its oral benefit led to the development of topical formulations, typically in 2% to 5% concentrations. It has proven particularly beneficial in the treatment of melasma due to its effects on improving pigmentation, erythema, and skin barrier function.31 Topical tranexamic acid has a relatively high safety profile, with minor side effects such as transient skin irritation and erythema being reported.32
Cysteamine—Cysteamine inhibits tyrosinase, peroxidase, and chelating copper ions necessary for melanogenesis. It has proven to be effective in treating melasma and chronic severe postinflammatory hyperpigmentation when used in a 5% cream formulation.33,34 Lima et al35 were the first to compare the effects of topical cysteamine to HQ in the treatment of facial melasma. They found that the mean reduction in modified Melasma Area and Severity Index score was 24% for cysteamine and 41% for HQ after 60 days. There were no severe adverse effects with either treatment group.35
Final Thoughts
Hydroquinone remains the gold standard for treatment of hyperpigmentation; however, its side-effect profile and risk of ochronosis with long-term use has ushered in various other safe and effective skin lightening agents that can be used as monotherapies or in combination with other lightening agents. Many of these products also can be used effectively with procedural treatments such as chemical peels, lasers, and microneedling for enhanced absorption and efficacy. As newer agents are developed, additional well-designed studies will be needed to determine their safety and efficacy in different skin types as well as their role in the treatment of pigmentary disorders.
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg. 2011;30:171-175. doi:10.1016/j.sder.2011.06.004
- Desai SR. Hyperpigmentation therapy: a review. J Clin Aesthet Dermatol. 2014;7:13-17.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Kligman AM, Grove GL, Hirose R, et al. Topical tretinoin for photoaged skin. J Am Acad Dermatol. 1986;15(4 pt 2):836-859. doi:10.1016/s0190-9622(86)70242-9
- Sharad J. Glycolic acid peel therapy—a current review. Clin Cosmet Investig Dermatol. 2013;6:281-288. doi:10.2147/CCID.S34029
- Nautiyal A, Wairkar S. Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res. 2021;34:1000-1014. doi:10.1111/pcmr.12986
- Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582-593. doi:10.1016/j.biopha.2018.12.006
- Schulte BC, Wu W, Rosen T. Azelaic acid: evidence-based update on mechanism of action and clinical application. J Drugs Dermatol. 2015;14:964-968.
- Akl EM. Liposomal azelaic acid 20% cream vs hydroquinone 4% cream as adjuvant to oral tranexamic acid in melasma: a comparative study [published online April 7, 2021]. J Dermatol Treat. doi:10.1080/09546634.2021.1905765
- Holloway VL. Ethnic cosmetic products. Dermatol Clin. 2003;21:743-749. doi:10.1016/s0733-8635(03)00089-5
- Amer M, Metwalli M. Topical liquiritin improves melasma. Int J Dermatol. 2000;39:299-301. doi:10.1046/j.1365-4362.2000.00943.x
- Jones K, Hughes J, Hong M, et al. Modulation of melanogenesis by aloesin: a competitive inhibitor of tyrosinase. Pigment Cell Res. 2002;15:335-340. doi:10.1034/j.1600-0749.2002.02014.x
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147:20-31. doi:10.1046/j.1365-2133.2002.04834.x
- Wohlrab J, Kreft D. Niacinamide—mechanisms of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311-315. doi:10.1159/000359974
- Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatol Surg. 2002;28:231-236. doi:10.1046/j.1524-4725.2002.01129.x
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378. doi:10.4103/0378-6323.178903
- Petit L, Piérard GE. Skin-lightening products revisited. Int J Cosmet Sci. 2003;25:169-181. doi:10.1046/j.1467-2494.2003.00182.x
- Kanwar AJ, Dhar S, Kaur S. Treatment of melasma with potent topical corticosteroids. Dermatol Basel Switz. 1994;188:170. doi:10.1159/000247129
- Paine C, Sharlow E, Liebel F, et al. An alternative approach to depigmentation by soybean extracts via inhibition of the PAR-2 pathway. J Invest Dermatol. 2001;116:587-595. doi:10.1046/j.1523-1747.2001.01291.x
- Seiberg M, Paine C, Sharlow E, et al. Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol. 2000;115:162-167. doi:10.1046/j.1523-1747.2000.00035.x
- Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci. 2000;22:291-303. doi:10.1046/j.1467-2494.2000.00023.x
- Rendon MI, Gaviria JI. Review of skin-lightening agents. Dermatol Surg. 2005;31(7 pt 2):886-889; discussion 889. doi:10.1111/j.1524-4725.2005.31736
- Na JI, Shin JW, Choi HR, et al. Resveratrol as a multifunctional topical hypopigmenting agent [published online February 22, 2019]. Int J Mol Sci. 2019;20:956. doi:10.3390/ijms20040956
- Ratz-Łyko A, Arct J. Resveratrol as an active ingredient for cosmetic and dermatological applications: a review. J Cosmet Laser Ther. 2019;21:84-90. doi:10.1080/14764172.2018.1469767
- Choo SJ, Ryoo IJ, Kim YH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol. 2009;61:663-667. doi:10.1211/jpp/61.05.0016
- Draelos ZD, Diaz I, Cohen A, et al. A novel skin brightening topical technology. J Cosmet Dermatol. 2020;19:3280-3285. doi:10.1111/jocd.13741
- Grimes P, Bhawan J, Howell M, et al. Histopathological changes induced by malassezin: a novel natural microbiome indole for treatment of facial hyperpigmentation. J Drugs Dermatol. 2022;21:141-145. doi:10.36849/jdd.6596
- Bissett DL. Glucosamine: an ingredient with skin and other benefits. J Cosmet Dermatol. 2006;5:309-315. doi:10.1111/j.1473-2165.2006.00277.x
- Zhu JW, Ni YJ, Tong XY, et al. Tranexamic acid inhibits angiogenesis and melanogenesis in vitro by targeting VEGF receptors. Int J Med Sci. 2020;17:903-911. doi:10.7150/ijms.44188
- Hiramoto K, Yamate Y, Sugiyama D, et al. Tranexamic acid inhibits the plasma and non-irradiated skin markers of photoaging induced by long-term UVA eye irradiation in female mice. Biomed Pharmacother. 2018;107:54-58. doi:10.1016/j.biopha.2018.07.146
- da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021;20:561-565. doi:10.1111/jocd.13545
- Kim HJ, Moon SH, Cho SH, et al. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776-781. doi:10.2340/00015555-2668
- Mathe N, Balogun M, Yoo J. A case report on the use of topical cysteamine 5% cream in the management of refractory postinflammatory hyperpigmentation (PIH) resistant to triple combination cream (hydroquinone, topical corticosteroids, and retinoids). J Cosmet Dermatol. 2021;20:204-206. doi:10.1111/jocd.13755
- Mansouri P, Farshi S, Hashemi Z, et al. Evaluation of the efficacy of cysteamine 5% cream in the treatment of epidermal melasma: a randomized double-blind placebo-controlled trial. Br J Dermatol. 2015;173:209-217. doi:10.1111/bjd.13424
- Lima PB, Dias JAF, Cassiano D, et al. A comparative study of topical 5% cysteamine versus 4% hydroquinone in the treatment of facial melasma in women. Int J Dermatol. 2020;59:1531-1536. doi:10.1111/ijd.15146
Non-White subjects are sparse in DMT trials for MS
NATIONAL HARBOR, MD. -- Over 25 years of clinical research, phase 3 trials of approved disease-modifying therapies (DMTs) for multiple sclerosis (MS) were overwhelmingly made up of White subjects, a new analysis finds, and many studies failed to report percentages of non-White subjects at all. Researchers also found that the websites of multiple major drug manufacturers don’t include any trial data about how medications may affect people of different races and ethnicities.
It’s clear that “non-White participants are significantly underreported and unrepresented,” said study corresponding author and Dell Medical School/The University of Texas at Austin neurologist Leorah Freeman, MD, PhD, in an interview.
The study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers and published in Neurology.
“The lack of diversity in MS research is something that has been sporadically discussed in the past. By conducting this systematic review of MS phase 3 trials, we wanted to put numbers on this issue and review the evidence systematically,” Dr. Freeman said. “By doing so, we hoped to raise awareness about the problem of underreporting and underrepresentation of non-White participants in trials so that we, as a community involved in MS research, can start having the difficult conversations needed for change to occur.”
25 years of clinical research
The researchers reviewed 44 phase 3 studies from 1995-2020 that represented 45 trials. “We wanted to capture data from the very first global trials being conducted for the approval of MS DMTs, and the first was published in 1995,” Dr. Freeman said. “We were interested in understanding the impact of trial globalization over a long period of time on diversity of enrollment.”
The studies include trials of mainstays of MS treatment such as interferon, glatiramer acetate, teriflunomide, dimethyl fumarate, diroximel fumarate, fingolimod, natalizumab, and others.
The researchers found that 17 (37.8%) of the trials did not report race or ethnicity, 14 (31.1%) reported race and ethnicity as proportion of White participants only, and 14 (31.1%) reported 2 or more races/ethnicities.
Of the 28 trials with racial breakdowns, the median percentage of White participants was 93.8% (range 78.5-99.6% across 28 studies), 1.9% for Black participants (range 0.1-8.1% across 14 studies), and 0.5% for Asian participants (range 0.1-14.5% across 11 studies).
The studies often failed to account for non-White subjects even though “Black people, in particular, have been shown to have a more severe disease course,” Dr. Freeman said.
A 2022 study of more than 2.6 million Southern California adults finds that prevalence of MS was similar among White and Black people at about 230 per 100,000. “Taken together with previous studies, these findings indicate that the burden of MS in the United States Black community has long been underrecognized,” the researchers wrote.
According to Dr. Freeman, it’s unclear why the studies were so dominated by White subjects. “Lack of awareness about the importance of this information likely explains why this information often goes unreported.”
She highlighted the TOWER (teriflunomide) and DEFINE and CONFIRM (dimethyl fumarate) studies as positive examples. “We noted the inclusion of trial sites in Asia and consequently a higher representation of Asian people with MS in those trials. We felt these studies were examples of how trial globalization can support better representation of underrepresented groups.”
And she noted that the ongoing CHIMES trial is examining the use of ocrelizumab in Black and Hispanic people with MS. “This study was designed in partnership with MS patients and advocacy groups to bridge gaps in clinical trial participation in these communities,” she said. “Innovative strategies were developed to increase participation of Black and Hispanic patients in this trial.”
What should happen next?
Going forward, Dr. Freeman said, “MS researchers, DMT manufacturers, sponsors, and publishers need to set better standards for racial and ethnic representation and reporting in trial publications.”
In an interview, epidemiologist Luisa N. Borrell, DDS, PhD, a professor who studies race and medicine at City University of New York, said the new study is valid and useful. She noted that it reflects the findings of a 2022 analysis of more than 20,500 clinical trials in the U.S. from 2000-2020: Only 43% reported racial/ethnic breakdowns, and the subjects were much more White than the population at large.
Possible reasons for the disparity include distrust among possible participants and lack of health literacy, she said, which are both “modifiable issues.”
Dr. Borrell added: “Clinical trials should aim to recruit populations affected by the outcome of interest. That would allow for the intervention to effectively treat those who need it the most. Moreover, the lack of diversity of trials brings issues of generalizability and transportability of the findings.”
No funding is reported. Dr. Freeman and some of the other study authors report various disclosures.
NATIONAL HARBOR, MD. -- Over 25 years of clinical research, phase 3 trials of approved disease-modifying therapies (DMTs) for multiple sclerosis (MS) were overwhelmingly made up of White subjects, a new analysis finds, and many studies failed to report percentages of non-White subjects at all. Researchers also found that the websites of multiple major drug manufacturers don’t include any trial data about how medications may affect people of different races and ethnicities.
It’s clear that “non-White participants are significantly underreported and unrepresented,” said study corresponding author and Dell Medical School/The University of Texas at Austin neurologist Leorah Freeman, MD, PhD, in an interview.
The study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers and published in Neurology.
“The lack of diversity in MS research is something that has been sporadically discussed in the past. By conducting this systematic review of MS phase 3 trials, we wanted to put numbers on this issue and review the evidence systematically,” Dr. Freeman said. “By doing so, we hoped to raise awareness about the problem of underreporting and underrepresentation of non-White participants in trials so that we, as a community involved in MS research, can start having the difficult conversations needed for change to occur.”
25 years of clinical research
The researchers reviewed 44 phase 3 studies from 1995-2020 that represented 45 trials. “We wanted to capture data from the very first global trials being conducted for the approval of MS DMTs, and the first was published in 1995,” Dr. Freeman said. “We were interested in understanding the impact of trial globalization over a long period of time on diversity of enrollment.”
The studies include trials of mainstays of MS treatment such as interferon, glatiramer acetate, teriflunomide, dimethyl fumarate, diroximel fumarate, fingolimod, natalizumab, and others.
The researchers found that 17 (37.8%) of the trials did not report race or ethnicity, 14 (31.1%) reported race and ethnicity as proportion of White participants only, and 14 (31.1%) reported 2 or more races/ethnicities.
Of the 28 trials with racial breakdowns, the median percentage of White participants was 93.8% (range 78.5-99.6% across 28 studies), 1.9% for Black participants (range 0.1-8.1% across 14 studies), and 0.5% for Asian participants (range 0.1-14.5% across 11 studies).
The studies often failed to account for non-White subjects even though “Black people, in particular, have been shown to have a more severe disease course,” Dr. Freeman said.
A 2022 study of more than 2.6 million Southern California adults finds that prevalence of MS was similar among White and Black people at about 230 per 100,000. “Taken together with previous studies, these findings indicate that the burden of MS in the United States Black community has long been underrecognized,” the researchers wrote.
According to Dr. Freeman, it’s unclear why the studies were so dominated by White subjects. “Lack of awareness about the importance of this information likely explains why this information often goes unreported.”
She highlighted the TOWER (teriflunomide) and DEFINE and CONFIRM (dimethyl fumarate) studies as positive examples. “We noted the inclusion of trial sites in Asia and consequently a higher representation of Asian people with MS in those trials. We felt these studies were examples of how trial globalization can support better representation of underrepresented groups.”
And she noted that the ongoing CHIMES trial is examining the use of ocrelizumab in Black and Hispanic people with MS. “This study was designed in partnership with MS patients and advocacy groups to bridge gaps in clinical trial participation in these communities,” she said. “Innovative strategies were developed to increase participation of Black and Hispanic patients in this trial.”
What should happen next?
Going forward, Dr. Freeman said, “MS researchers, DMT manufacturers, sponsors, and publishers need to set better standards for racial and ethnic representation and reporting in trial publications.”
In an interview, epidemiologist Luisa N. Borrell, DDS, PhD, a professor who studies race and medicine at City University of New York, said the new study is valid and useful. She noted that it reflects the findings of a 2022 analysis of more than 20,500 clinical trials in the U.S. from 2000-2020: Only 43% reported racial/ethnic breakdowns, and the subjects were much more White than the population at large.
Possible reasons for the disparity include distrust among possible participants and lack of health literacy, she said, which are both “modifiable issues.”
Dr. Borrell added: “Clinical trials should aim to recruit populations affected by the outcome of interest. That would allow for the intervention to effectively treat those who need it the most. Moreover, the lack of diversity of trials brings issues of generalizability and transportability of the findings.”
No funding is reported. Dr. Freeman and some of the other study authors report various disclosures.
NATIONAL HARBOR, MD. -- Over 25 years of clinical research, phase 3 trials of approved disease-modifying therapies (DMTs) for multiple sclerosis (MS) were overwhelmingly made up of White subjects, a new analysis finds, and many studies failed to report percentages of non-White subjects at all. Researchers also found that the websites of multiple major drug manufacturers don’t include any trial data about how medications may affect people of different races and ethnicities.
It’s clear that “non-White participants are significantly underreported and unrepresented,” said study corresponding author and Dell Medical School/The University of Texas at Austin neurologist Leorah Freeman, MD, PhD, in an interview.
The study was presented at the annual meeting of the Consortium of Multiple Sclerosis Centers and published in Neurology.
“The lack of diversity in MS research is something that has been sporadically discussed in the past. By conducting this systematic review of MS phase 3 trials, we wanted to put numbers on this issue and review the evidence systematically,” Dr. Freeman said. “By doing so, we hoped to raise awareness about the problem of underreporting and underrepresentation of non-White participants in trials so that we, as a community involved in MS research, can start having the difficult conversations needed for change to occur.”
25 years of clinical research
The researchers reviewed 44 phase 3 studies from 1995-2020 that represented 45 trials. “We wanted to capture data from the very first global trials being conducted for the approval of MS DMTs, and the first was published in 1995,” Dr. Freeman said. “We were interested in understanding the impact of trial globalization over a long period of time on diversity of enrollment.”
The studies include trials of mainstays of MS treatment such as interferon, glatiramer acetate, teriflunomide, dimethyl fumarate, diroximel fumarate, fingolimod, natalizumab, and others.
The researchers found that 17 (37.8%) of the trials did not report race or ethnicity, 14 (31.1%) reported race and ethnicity as proportion of White participants only, and 14 (31.1%) reported 2 or more races/ethnicities.
Of the 28 trials with racial breakdowns, the median percentage of White participants was 93.8% (range 78.5-99.6% across 28 studies), 1.9% for Black participants (range 0.1-8.1% across 14 studies), and 0.5% for Asian participants (range 0.1-14.5% across 11 studies).
The studies often failed to account for non-White subjects even though “Black people, in particular, have been shown to have a more severe disease course,” Dr. Freeman said.
A 2022 study of more than 2.6 million Southern California adults finds that prevalence of MS was similar among White and Black people at about 230 per 100,000. “Taken together with previous studies, these findings indicate that the burden of MS in the United States Black community has long been underrecognized,” the researchers wrote.
According to Dr. Freeman, it’s unclear why the studies were so dominated by White subjects. “Lack of awareness about the importance of this information likely explains why this information often goes unreported.”
She highlighted the TOWER (teriflunomide) and DEFINE and CONFIRM (dimethyl fumarate) studies as positive examples. “We noted the inclusion of trial sites in Asia and consequently a higher representation of Asian people with MS in those trials. We felt these studies were examples of how trial globalization can support better representation of underrepresented groups.”
And she noted that the ongoing CHIMES trial is examining the use of ocrelizumab in Black and Hispanic people with MS. “This study was designed in partnership with MS patients and advocacy groups to bridge gaps in clinical trial participation in these communities,” she said. “Innovative strategies were developed to increase participation of Black and Hispanic patients in this trial.”
What should happen next?
Going forward, Dr. Freeman said, “MS researchers, DMT manufacturers, sponsors, and publishers need to set better standards for racial and ethnic representation and reporting in trial publications.”
In an interview, epidemiologist Luisa N. Borrell, DDS, PhD, a professor who studies race and medicine at City University of New York, said the new study is valid and useful. She noted that it reflects the findings of a 2022 analysis of more than 20,500 clinical trials in the U.S. from 2000-2020: Only 43% reported racial/ethnic breakdowns, and the subjects were much more White than the population at large.
Possible reasons for the disparity include distrust among possible participants and lack of health literacy, she said, which are both “modifiable issues.”
Dr. Borrell added: “Clinical trials should aim to recruit populations affected by the outcome of interest. That would allow for the intervention to effectively treat those who need it the most. Moreover, the lack of diversity of trials brings issues of generalizability and transportability of the findings.”
No funding is reported. Dr. Freeman and some of the other study authors report various disclosures.
AT CMSC 2022
Antidiabetes drug costs keep patients away
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
AT ADA 2022
Telemedicine in cancer care: Not all patients can access
CHICAGO – for patients with cancer, but uptake of telemedicine was plagued by inequities, a retrospective study suggests.
Before March 2020, only a very small percentage of patients with cancer used telemedicine services.
By November 2021, nearly 16% of patients initiating cancer treatment were using this approach.
However, certain groups were less likely to use telemedicine, in particular, patients who were Black, uninsured, did not live in cities, and were less affluent, noted lead author Jenny S. Guadamuz, PhD, a quantitative scientist at Flatiron Health and a postdoctoral research associate at the University of Southern California, Los Angeles.
The results are concerning because they suggest that telemedicine expansion could widen cancer care disparities, Dr. Guadamuz said. Previous studies found racial disparities in care access and outcomes early on in the pandemic.
“These findings are critically important considering recent efforts to make coverage of telemedicine services permanent, instead of tied to the [Health and Human Services] public health emergency declaration,” she said. “There are also efforts to increase reimbursement rates for telemedicine services by Medicare, several Medicaid programs, and private insurers.”
This study was highlighted at a press briefing held in advance of the American Society of Clinical Oncology annual meeting, where it will be presented at a poster session (abstract 6511).
ASCO President Everett E. Vokes, MD, said telemedicine is “an important tool to communicate with patients” but that it is important to consider the “digital divide.”
He also emphasized the need “to expand and learn to use telehealth not in a crisis but as part of our regular care moving forward.” In July 2021, as telemedicine services were expanding, ASCO released practice recommendations specific to telehealth and oncology.
“Telemedicine can improve access to timely cancer care, but, as this study points out, telemedicine must be available equitably, so that every patient can access the care they need and deserve,” he said in a press statement.
Study details
For the study, Dr. Guadamuz and colleagues assessed telemedicine uptake by nearly 27,000 patients in a Flatiron electronic health record–derived deidentified database of patients who initiated treatment for any of 21 common cancers at about 280 community oncology clinics between March 2020 and November 2021.
They found that Black patients were significantly less likely than were White patients to use telemedicine (13.2% vs. 15.6%; odds ratio [OR], 0.82), as were patients without documented insurance, compared with those who were well insured (11.6% vs. 16.4%; OR, 0.68).
Those in rural and suburban areas were less likely than were those in urban areas to use telemedicine (9.7% and 13.0% vs. 17.7%; ORs, 0.50 and 0.69, respectively), and those in less affluent vs. more affluent areas were also less likely to use telemedicine (10.6% vs. 23.6%, OR, 0.39).
Dr. Guadamuz noted that the differences remained statistically significant after adjustment for clinical characteristics and that racial inequities were seen across cancer types and over time.
Future work should assess other potential characteristics associated with telemedicine inequities, evaluate whether health care delivered via telemedicine is of similar quality as in-person services, and determine the types of practice that are providing telemedicine more equitably to their patients, she concluded.
A version of this article first appeared on Medscape.com.
CHICAGO – for patients with cancer, but uptake of telemedicine was plagued by inequities, a retrospective study suggests.
Before March 2020, only a very small percentage of patients with cancer used telemedicine services.
By November 2021, nearly 16% of patients initiating cancer treatment were using this approach.
However, certain groups were less likely to use telemedicine, in particular, patients who were Black, uninsured, did not live in cities, and were less affluent, noted lead author Jenny S. Guadamuz, PhD, a quantitative scientist at Flatiron Health and a postdoctoral research associate at the University of Southern California, Los Angeles.
The results are concerning because they suggest that telemedicine expansion could widen cancer care disparities, Dr. Guadamuz said. Previous studies found racial disparities in care access and outcomes early on in the pandemic.
“These findings are critically important considering recent efforts to make coverage of telemedicine services permanent, instead of tied to the [Health and Human Services] public health emergency declaration,” she said. “There are also efforts to increase reimbursement rates for telemedicine services by Medicare, several Medicaid programs, and private insurers.”
This study was highlighted at a press briefing held in advance of the American Society of Clinical Oncology annual meeting, where it will be presented at a poster session (abstract 6511).
ASCO President Everett E. Vokes, MD, said telemedicine is “an important tool to communicate with patients” but that it is important to consider the “digital divide.”
He also emphasized the need “to expand and learn to use telehealth not in a crisis but as part of our regular care moving forward.” In July 2021, as telemedicine services were expanding, ASCO released practice recommendations specific to telehealth and oncology.
“Telemedicine can improve access to timely cancer care, but, as this study points out, telemedicine must be available equitably, so that every patient can access the care they need and deserve,” he said in a press statement.
Study details
For the study, Dr. Guadamuz and colleagues assessed telemedicine uptake by nearly 27,000 patients in a Flatiron electronic health record–derived deidentified database of patients who initiated treatment for any of 21 common cancers at about 280 community oncology clinics between March 2020 and November 2021.
They found that Black patients were significantly less likely than were White patients to use telemedicine (13.2% vs. 15.6%; odds ratio [OR], 0.82), as were patients without documented insurance, compared with those who were well insured (11.6% vs. 16.4%; OR, 0.68).
Those in rural and suburban areas were less likely than were those in urban areas to use telemedicine (9.7% and 13.0% vs. 17.7%; ORs, 0.50 and 0.69, respectively), and those in less affluent vs. more affluent areas were also less likely to use telemedicine (10.6% vs. 23.6%, OR, 0.39).
Dr. Guadamuz noted that the differences remained statistically significant after adjustment for clinical characteristics and that racial inequities were seen across cancer types and over time.
Future work should assess other potential characteristics associated with telemedicine inequities, evaluate whether health care delivered via telemedicine is of similar quality as in-person services, and determine the types of practice that are providing telemedicine more equitably to their patients, she concluded.
A version of this article first appeared on Medscape.com.
CHICAGO – for patients with cancer, but uptake of telemedicine was plagued by inequities, a retrospective study suggests.
Before March 2020, only a very small percentage of patients with cancer used telemedicine services.
By November 2021, nearly 16% of patients initiating cancer treatment were using this approach.
However, certain groups were less likely to use telemedicine, in particular, patients who were Black, uninsured, did not live in cities, and were less affluent, noted lead author Jenny S. Guadamuz, PhD, a quantitative scientist at Flatiron Health and a postdoctoral research associate at the University of Southern California, Los Angeles.
The results are concerning because they suggest that telemedicine expansion could widen cancer care disparities, Dr. Guadamuz said. Previous studies found racial disparities in care access and outcomes early on in the pandemic.
“These findings are critically important considering recent efforts to make coverage of telemedicine services permanent, instead of tied to the [Health and Human Services] public health emergency declaration,” she said. “There are also efforts to increase reimbursement rates for telemedicine services by Medicare, several Medicaid programs, and private insurers.”
This study was highlighted at a press briefing held in advance of the American Society of Clinical Oncology annual meeting, where it will be presented at a poster session (abstract 6511).
ASCO President Everett E. Vokes, MD, said telemedicine is “an important tool to communicate with patients” but that it is important to consider the “digital divide.”
He also emphasized the need “to expand and learn to use telehealth not in a crisis but as part of our regular care moving forward.” In July 2021, as telemedicine services were expanding, ASCO released practice recommendations specific to telehealth and oncology.
“Telemedicine can improve access to timely cancer care, but, as this study points out, telemedicine must be available equitably, so that every patient can access the care they need and deserve,” he said in a press statement.
Study details
For the study, Dr. Guadamuz and colleagues assessed telemedicine uptake by nearly 27,000 patients in a Flatiron electronic health record–derived deidentified database of patients who initiated treatment for any of 21 common cancers at about 280 community oncology clinics between March 2020 and November 2021.
They found that Black patients were significantly less likely than were White patients to use telemedicine (13.2% vs. 15.6%; odds ratio [OR], 0.82), as were patients without documented insurance, compared with those who were well insured (11.6% vs. 16.4%; OR, 0.68).
Those in rural and suburban areas were less likely than were those in urban areas to use telemedicine (9.7% and 13.0% vs. 17.7%; ORs, 0.50 and 0.69, respectively), and those in less affluent vs. more affluent areas were also less likely to use telemedicine (10.6% vs. 23.6%, OR, 0.39).
Dr. Guadamuz noted that the differences remained statistically significant after adjustment for clinical characteristics and that racial inequities were seen across cancer types and over time.
Future work should assess other potential characteristics associated with telemedicine inequities, evaluate whether health care delivered via telemedicine is of similar quality as in-person services, and determine the types of practice that are providing telemedicine more equitably to their patients, she concluded.
A version of this article first appeared on Medscape.com.
AT ASCO 2022
Increased social services spending ups cancer survival of Blacks
Five-year overall survival increased among non-Hispanic Black patients by 2.02% in conjunction with a 10% increase in spending. In addition, there was a decrease in racial disparities in survival between non-Hispanic Black patients and White patients for many types of cancers.
However, public welfare spending had no real impact on the overall 5-year survival for the entire cohort (0.25 % per 10% increase in spending; P = .78) or for non-Hispanic White patients (0.52% per 10% increase in spending, P = .58).
“We know from prior research that outcomes are worse for minorities,” said lead author Justin Michael Barnes, MD, from the department of radiation oncology at Washington University in St. Louis, Mo. “It’s thought that some of the differences are related to impaired access to health care for minorities, which is related to social determinants of health. This includes socioeconomic factors, educational attainment, place of residence, as well as environmental stressors.
“Our data show that greater state welfare expenditures were associated with greater 5-year survival among Black patients and decreased Black–White disparities,” said Dr. Barnes. “I think these data are thought provoking, but they certainly aren’t the end. I see these data as a proof-of-concept project.”
Dr. Barnes reported the findings at a press conference held in advance of the annual meeting of the American Society of Clinical Oncology, during which the study will be presented (Abstract 6509).
Improved 5-year survival in Black patients
For the study, Dr. Barnes and colleagues evaluated the association of 5-year overall survival and public welfare spending in 2,925,550 individuals aged 18 years and older who were diagnosed with cancer during the period 2007-2016. The cohort was drawn from the Surveillance, Epidemiology, and End Results Program. In addition, annual state spending data were obtained from the U.S. Census Bureau. The team examined survival outcomes by race and ethnicity as well as by cancer site. The investigators accounted for factors such as age, sex, metropolitan residence, state, county-level income and education, insurance status, cancer site, stage at diagnosis, and year of diagnosis.
Much of public welfare spending was related to Medicaid but also included programs that provide subsidy assistance for individuals, such as Supplemental Security Income.
As compared with White patients, the 5-year overall survival rate was 10.8% lower among non-Hispanic Black patients. But there was a 4.46% (P for interaction <.001) narrowing of the 5-year overall survival disparity in non-Hispanic Black patients in comparison with White patients per 10% increase in spending, or a 42% closure of the 10.8% disparity.
Regarding specific cancer types, increased public welfare spending was associated with a narrowing of the 5-year overall survival disparity between Black patients and non-Hispanic White patients for the following cancers: breast (a 6.15% survival increase for Black patients led to a 39% closing of the disparity), cervix (a 11.9% survival increase led to a 46% closing of the disparity), colorectum (a 4.42% survival increase led to a 48% closing of the disparity), head and neck (a 9.41% survival increase led to a 38% closing of the disparity), liver (a 7.02% survival increase led to a 49% closing of the disparity), ovary (an 8.95% survival increase led to a 41% closing of the disparity), bladder (an 8.18% survival increase led to a 44% closing of the disparity), and uterus (a 14.1% survival increase led to a 40% closing of the disparity).
“Some type of public welfare seems to be helping improve oncologic outcomes for some of our most socioeconomically at-risk patients, but we don’t know the specifics,” Dr. Barnes concluded. “Additional work is needed to identify the most influential public health expenditures. If we can do this, we can more rigorously evaluate state-level policies and their association with cancer outcomes.”
Public welfare improves outcomes
Weighing in on the data, Sarah P. Cate, MD, director, Special Surveillance and Breast Program, Mount Sinai Health System, New York, noted that racial disparities have been identified in many areas of health care and with respect to many diseases. “In the world of oncology, time to diagnosis and treatment significantly impacts overall survival,” she told this news organization. “Many studies are currently underway to investigate why certain ethnic groups have worse cancer outcomes.”
This study is important, she noted, in that it “highlights a discrete source of correcting these disparities in a large group of patients. Obviously there are multiple barriers to care, but increased public welfare spending in oncology should decrease some of these disparities.”
Julie R. Gralow, MD, ASCO’s chief medical officer and executive vice president, commented that it is known that state public welfare spending can mitigate structural racism and at least partially address social determinants of health, such as financial stability, education, place of residence, and insurance status. “This research found that states that increased their public health spending improved overall survival in Black patients with a variety of solid tumors and also resulted in a decrease in racial disparities in survival,” she said. “This important data provides clear support for the benefits of investment in public welfare spending at the state level, including Medicaid expansion.”
The study did not receive funding. Dr. Barnes and Dr. Cate have disclosed no relevant financial relationships. Dr. Gralow has relationships with Genentech, AstraZeneca Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
Five-year overall survival increased among non-Hispanic Black patients by 2.02% in conjunction with a 10% increase in spending. In addition, there was a decrease in racial disparities in survival between non-Hispanic Black patients and White patients for many types of cancers.
However, public welfare spending had no real impact on the overall 5-year survival for the entire cohort (0.25 % per 10% increase in spending; P = .78) or for non-Hispanic White patients (0.52% per 10% increase in spending, P = .58).
“We know from prior research that outcomes are worse for minorities,” said lead author Justin Michael Barnes, MD, from the department of radiation oncology at Washington University in St. Louis, Mo. “It’s thought that some of the differences are related to impaired access to health care for minorities, which is related to social determinants of health. This includes socioeconomic factors, educational attainment, place of residence, as well as environmental stressors.
“Our data show that greater state welfare expenditures were associated with greater 5-year survival among Black patients and decreased Black–White disparities,” said Dr. Barnes. “I think these data are thought provoking, but they certainly aren’t the end. I see these data as a proof-of-concept project.”
Dr. Barnes reported the findings at a press conference held in advance of the annual meeting of the American Society of Clinical Oncology, during which the study will be presented (Abstract 6509).
Improved 5-year survival in Black patients
For the study, Dr. Barnes and colleagues evaluated the association of 5-year overall survival and public welfare spending in 2,925,550 individuals aged 18 years and older who were diagnosed with cancer during the period 2007-2016. The cohort was drawn from the Surveillance, Epidemiology, and End Results Program. In addition, annual state spending data were obtained from the U.S. Census Bureau. The team examined survival outcomes by race and ethnicity as well as by cancer site. The investigators accounted for factors such as age, sex, metropolitan residence, state, county-level income and education, insurance status, cancer site, stage at diagnosis, and year of diagnosis.
Much of public welfare spending was related to Medicaid but also included programs that provide subsidy assistance for individuals, such as Supplemental Security Income.
As compared with White patients, the 5-year overall survival rate was 10.8% lower among non-Hispanic Black patients. But there was a 4.46% (P for interaction <.001) narrowing of the 5-year overall survival disparity in non-Hispanic Black patients in comparison with White patients per 10% increase in spending, or a 42% closure of the 10.8% disparity.
Regarding specific cancer types, increased public welfare spending was associated with a narrowing of the 5-year overall survival disparity between Black patients and non-Hispanic White patients for the following cancers: breast (a 6.15% survival increase for Black patients led to a 39% closing of the disparity), cervix (a 11.9% survival increase led to a 46% closing of the disparity), colorectum (a 4.42% survival increase led to a 48% closing of the disparity), head and neck (a 9.41% survival increase led to a 38% closing of the disparity), liver (a 7.02% survival increase led to a 49% closing of the disparity), ovary (an 8.95% survival increase led to a 41% closing of the disparity), bladder (an 8.18% survival increase led to a 44% closing of the disparity), and uterus (a 14.1% survival increase led to a 40% closing of the disparity).
“Some type of public welfare seems to be helping improve oncologic outcomes for some of our most socioeconomically at-risk patients, but we don’t know the specifics,” Dr. Barnes concluded. “Additional work is needed to identify the most influential public health expenditures. If we can do this, we can more rigorously evaluate state-level policies and their association with cancer outcomes.”
Public welfare improves outcomes
Weighing in on the data, Sarah P. Cate, MD, director, Special Surveillance and Breast Program, Mount Sinai Health System, New York, noted that racial disparities have been identified in many areas of health care and with respect to many diseases. “In the world of oncology, time to diagnosis and treatment significantly impacts overall survival,” she told this news organization. “Many studies are currently underway to investigate why certain ethnic groups have worse cancer outcomes.”
This study is important, she noted, in that it “highlights a discrete source of correcting these disparities in a large group of patients. Obviously there are multiple barriers to care, but increased public welfare spending in oncology should decrease some of these disparities.”
Julie R. Gralow, MD, ASCO’s chief medical officer and executive vice president, commented that it is known that state public welfare spending can mitigate structural racism and at least partially address social determinants of health, such as financial stability, education, place of residence, and insurance status. “This research found that states that increased their public health spending improved overall survival in Black patients with a variety of solid tumors and also resulted in a decrease in racial disparities in survival,” she said. “This important data provides clear support for the benefits of investment in public welfare spending at the state level, including Medicaid expansion.”
The study did not receive funding. Dr. Barnes and Dr. Cate have disclosed no relevant financial relationships. Dr. Gralow has relationships with Genentech, AstraZeneca Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
Five-year overall survival increased among non-Hispanic Black patients by 2.02% in conjunction with a 10% increase in spending. In addition, there was a decrease in racial disparities in survival between non-Hispanic Black patients and White patients for many types of cancers.
However, public welfare spending had no real impact on the overall 5-year survival for the entire cohort (0.25 % per 10% increase in spending; P = .78) or for non-Hispanic White patients (0.52% per 10% increase in spending, P = .58).
“We know from prior research that outcomes are worse for minorities,” said lead author Justin Michael Barnes, MD, from the department of radiation oncology at Washington University in St. Louis, Mo. “It’s thought that some of the differences are related to impaired access to health care for minorities, which is related to social determinants of health. This includes socioeconomic factors, educational attainment, place of residence, as well as environmental stressors.
“Our data show that greater state welfare expenditures were associated with greater 5-year survival among Black patients and decreased Black–White disparities,” said Dr. Barnes. “I think these data are thought provoking, but they certainly aren’t the end. I see these data as a proof-of-concept project.”
Dr. Barnes reported the findings at a press conference held in advance of the annual meeting of the American Society of Clinical Oncology, during which the study will be presented (Abstract 6509).
Improved 5-year survival in Black patients
For the study, Dr. Barnes and colleagues evaluated the association of 5-year overall survival and public welfare spending in 2,925,550 individuals aged 18 years and older who were diagnosed with cancer during the period 2007-2016. The cohort was drawn from the Surveillance, Epidemiology, and End Results Program. In addition, annual state spending data were obtained from the U.S. Census Bureau. The team examined survival outcomes by race and ethnicity as well as by cancer site. The investigators accounted for factors such as age, sex, metropolitan residence, state, county-level income and education, insurance status, cancer site, stage at diagnosis, and year of diagnosis.
Much of public welfare spending was related to Medicaid but also included programs that provide subsidy assistance for individuals, such as Supplemental Security Income.
As compared with White patients, the 5-year overall survival rate was 10.8% lower among non-Hispanic Black patients. But there was a 4.46% (P for interaction <.001) narrowing of the 5-year overall survival disparity in non-Hispanic Black patients in comparison with White patients per 10% increase in spending, or a 42% closure of the 10.8% disparity.
Regarding specific cancer types, increased public welfare spending was associated with a narrowing of the 5-year overall survival disparity between Black patients and non-Hispanic White patients for the following cancers: breast (a 6.15% survival increase for Black patients led to a 39% closing of the disparity), cervix (a 11.9% survival increase led to a 46% closing of the disparity), colorectum (a 4.42% survival increase led to a 48% closing of the disparity), head and neck (a 9.41% survival increase led to a 38% closing of the disparity), liver (a 7.02% survival increase led to a 49% closing of the disparity), ovary (an 8.95% survival increase led to a 41% closing of the disparity), bladder (an 8.18% survival increase led to a 44% closing of the disparity), and uterus (a 14.1% survival increase led to a 40% closing of the disparity).
“Some type of public welfare seems to be helping improve oncologic outcomes for some of our most socioeconomically at-risk patients, but we don’t know the specifics,” Dr. Barnes concluded. “Additional work is needed to identify the most influential public health expenditures. If we can do this, we can more rigorously evaluate state-level policies and their association with cancer outcomes.”
Public welfare improves outcomes
Weighing in on the data, Sarah P. Cate, MD, director, Special Surveillance and Breast Program, Mount Sinai Health System, New York, noted that racial disparities have been identified in many areas of health care and with respect to many diseases. “In the world of oncology, time to diagnosis and treatment significantly impacts overall survival,” she told this news organization. “Many studies are currently underway to investigate why certain ethnic groups have worse cancer outcomes.”
This study is important, she noted, in that it “highlights a discrete source of correcting these disparities in a large group of patients. Obviously there are multiple barriers to care, but increased public welfare spending in oncology should decrease some of these disparities.”
Julie R. Gralow, MD, ASCO’s chief medical officer and executive vice president, commented that it is known that state public welfare spending can mitigate structural racism and at least partially address social determinants of health, such as financial stability, education, place of residence, and insurance status. “This research found that states that increased their public health spending improved overall survival in Black patients with a variety of solid tumors and also resulted in a decrease in racial disparities in survival,” she said. “This important data provides clear support for the benefits of investment in public welfare spending at the state level, including Medicaid expansion.”
The study did not receive funding. Dr. Barnes and Dr. Cate have disclosed no relevant financial relationships. Dr. Gralow has relationships with Genentech, AstraZeneca Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
FROM ASCO 2022
White children more likely to get imaging in EDs: Study
Non-Hispanic White children were more likely to receive diagnostic imaging at children’s hospitals’ emergency departments across the United States than were Hispanic children and non-Hispanic Black children, according to a large study published in JAMA Network Open.
Researchers found that, the more the percentage of children from minority groups cared for by a hospital increased, the wider the imaging gap between those children and non-Hispanic White children.
The cross-sectional study, led by Margaret E. Samuels-Kalow, MD, MPhil, MSHP, with the department of emergency medicine, Massachusetts General Hospital and Harvard Medical School in Boston, included 38 children’s hospitals and more than 12 million ED visits.
“These findings emphasize the urgent need for interventions at the hospital level to improve equity in imaging in pediatric emergency medicine,” the authors write.
Patients included in the study were younger than 18 and visited an ED from January 2016 through December 2019. Data were pulled from the Pediatric Health Information System.
Of the more than 12 million visits in this study, 3.5 million (28.7%) involved at least one diagnostic imaging test.
Diagnostic imaging was performed in 1.5 million visits (34.2%) for non-Hispanic White children; 790,961 (24.6%) for non-Hispanic Black children; and 907,222 (26.1%) for Hispanic children (P < .001).
Non-Hispanic Black children were consistently less likely to get diagnostic imaging than non-Hispanic White counterparts at every hospital in the study, no matter the imaging modality: radiography, ultrasonography, computed tomography, or magnetic resonance imaging.
Hispanic patients were generally less likely to get imaging than non-Hispanic White patients, though results were less consistent for ultrasound and MRI.
In a sensitivity analysis, when looking at imaging from patients’ first visit across the study cohort, non-Hispanic Black children were significantly less likely to get imaging than non-Hispanic White children (adjusted odds ratio, 0.77; 95% confidence interval, 0.74-0.79).
“This remained significant even after adjustment for a priori specified confounders including hospital propensity to image,” the authors write.
Authors acknowledge that it is possible that some of the differences may be attributable to the patient mix regarding severity of cases or indications for imaging by hospital, but they note that all models were adjusted for diagnosis-related group and other potential confounders.
This study did not assess whether one group is being overtested. Researchers also note that higher rates of imaging do not necessarily indicate higher quality of care.
However, the authors note, previous research has suggested overtesting of non-Hispanic White patients for head CT and chest pain, as well as patterns of overtreatment of non-Hispanic White patients who have bronchiolitis or viral upper respiratory tract infections.
Medell Briggs-Malonson, MD, MPH, chief of health equity, diversity and inclusion for the University of California, Los Angeles, Hospital and Clinic System, who was not part of the study, said in an interview “this all rings true.”
“This is not the first study we have had in either the pediatric or adult populations that shows disparate levels of care as well as health outcomes. Now we are starting to be able to measure it,” she said.
This study is further evidence of medical racism, she says, and highlights that it’s not the hospital choice or the insurance type affecting the numbers, she said.
“When you control for those factors, it looks to be it’s only due to race and that’s because of the very deep levels of implicit bias as well as explicit bias that we still have in our health systems and even in our providers,” said Dr. Briggs-Malonson, who is also an associate professor of emergency medicine at UCLA. “It’s incredibly important to identify and immediately address.”
What can be done?
Changing these patterns starts with knowing the numbers, the authors write.
“Hospitals should measure their own differences in imaging rates and increase awareness of existing areas of differential treatment as a starting point for improvement,” Dr. Samuels-Kalow and coauthors say.
Dr. Briggs-Malonson added that guidelines are very clear about when children should get imaging. Adhering to evidence-based guidelines can help avoid variations in care from external factors.
“If children are not receiving the absolute best comprehensive evaluation in the emergency department that they deserve, we can miss many different illnesses, which can lead to worse outcomes,” she noted.
As for what might motivate lack of imaging, Dr. Briggs-Malonson pointed to longstanding trends of providers thinking complaints raised by minority patients may not be as severe as they report. Conversely, in caring for White patients there may be a feeling that more tests and imaging may be better out of more fear of missing something, she said.
At UCLA, she says, dashboards have been developed to track statistics on care by age, race, ethnicity, language, insurance type, etc., though not specifically in pediatric imaging, to assess and address any care inequities.
Summer L. Kaplan, MD, MS, director of emergency radiology at Children’s Hospital of Philadelphia, who also was not part of the study, said the finding of racial disparities in pediatric ED imaging provides evidence that gaps still exist in providing the best care to all children and families seeking emergency care.
“However, it is important to recognize that more imaging does not equal better care,” she said. “More imaging may be associated with unnecessary, low-value tests that may add radiation and other risks but do not improve care.”
She said higher rates of imaging may occur when patients present early in the course of a disease, when the differential diagnosis remains broad.
If families have delayed seeking care because of time constraints, transportation problems, cost of care, or mistrust of the health system, children may present later in the course of a disease and require less imaging for a diagnosis, she explained.
“This paper offers a valuable look at the inequities that exist in pediatric emergency imaging use, and further research will be essential to understand and address the causes of these differences,” Dr. Kaplan said.
A coauthor reported compensation as a member of a Medical Review Committee for Highmark. Other coauthors reported grants from the U.S. Agency for Healthcare Research and Quality outside the submitted work. Dr. Briggs-Malonson and Dr. Kaplan reported no relevant financial relationships.
Non-Hispanic White children were more likely to receive diagnostic imaging at children’s hospitals’ emergency departments across the United States than were Hispanic children and non-Hispanic Black children, according to a large study published in JAMA Network Open.
Researchers found that, the more the percentage of children from minority groups cared for by a hospital increased, the wider the imaging gap between those children and non-Hispanic White children.
The cross-sectional study, led by Margaret E. Samuels-Kalow, MD, MPhil, MSHP, with the department of emergency medicine, Massachusetts General Hospital and Harvard Medical School in Boston, included 38 children’s hospitals and more than 12 million ED visits.
“These findings emphasize the urgent need for interventions at the hospital level to improve equity in imaging in pediatric emergency medicine,” the authors write.
Patients included in the study were younger than 18 and visited an ED from January 2016 through December 2019. Data were pulled from the Pediatric Health Information System.
Of the more than 12 million visits in this study, 3.5 million (28.7%) involved at least one diagnostic imaging test.
Diagnostic imaging was performed in 1.5 million visits (34.2%) for non-Hispanic White children; 790,961 (24.6%) for non-Hispanic Black children; and 907,222 (26.1%) for Hispanic children (P < .001).
Non-Hispanic Black children were consistently less likely to get diagnostic imaging than non-Hispanic White counterparts at every hospital in the study, no matter the imaging modality: radiography, ultrasonography, computed tomography, or magnetic resonance imaging.
Hispanic patients were generally less likely to get imaging than non-Hispanic White patients, though results were less consistent for ultrasound and MRI.
In a sensitivity analysis, when looking at imaging from patients’ first visit across the study cohort, non-Hispanic Black children were significantly less likely to get imaging than non-Hispanic White children (adjusted odds ratio, 0.77; 95% confidence interval, 0.74-0.79).
“This remained significant even after adjustment for a priori specified confounders including hospital propensity to image,” the authors write.
Authors acknowledge that it is possible that some of the differences may be attributable to the patient mix regarding severity of cases or indications for imaging by hospital, but they note that all models were adjusted for diagnosis-related group and other potential confounders.
This study did not assess whether one group is being overtested. Researchers also note that higher rates of imaging do not necessarily indicate higher quality of care.
However, the authors note, previous research has suggested overtesting of non-Hispanic White patients for head CT and chest pain, as well as patterns of overtreatment of non-Hispanic White patients who have bronchiolitis or viral upper respiratory tract infections.
Medell Briggs-Malonson, MD, MPH, chief of health equity, diversity and inclusion for the University of California, Los Angeles, Hospital and Clinic System, who was not part of the study, said in an interview “this all rings true.”
“This is not the first study we have had in either the pediatric or adult populations that shows disparate levels of care as well as health outcomes. Now we are starting to be able to measure it,” she said.
This study is further evidence of medical racism, she says, and highlights that it’s not the hospital choice or the insurance type affecting the numbers, she said.
“When you control for those factors, it looks to be it’s only due to race and that’s because of the very deep levels of implicit bias as well as explicit bias that we still have in our health systems and even in our providers,” said Dr. Briggs-Malonson, who is also an associate professor of emergency medicine at UCLA. “It’s incredibly important to identify and immediately address.”
What can be done?
Changing these patterns starts with knowing the numbers, the authors write.
“Hospitals should measure their own differences in imaging rates and increase awareness of existing areas of differential treatment as a starting point for improvement,” Dr. Samuels-Kalow and coauthors say.
Dr. Briggs-Malonson added that guidelines are very clear about when children should get imaging. Adhering to evidence-based guidelines can help avoid variations in care from external factors.
“If children are not receiving the absolute best comprehensive evaluation in the emergency department that they deserve, we can miss many different illnesses, which can lead to worse outcomes,” she noted.
As for what might motivate lack of imaging, Dr. Briggs-Malonson pointed to longstanding trends of providers thinking complaints raised by minority patients may not be as severe as they report. Conversely, in caring for White patients there may be a feeling that more tests and imaging may be better out of more fear of missing something, she said.
At UCLA, she says, dashboards have been developed to track statistics on care by age, race, ethnicity, language, insurance type, etc., though not specifically in pediatric imaging, to assess and address any care inequities.
Summer L. Kaplan, MD, MS, director of emergency radiology at Children’s Hospital of Philadelphia, who also was not part of the study, said the finding of racial disparities in pediatric ED imaging provides evidence that gaps still exist in providing the best care to all children and families seeking emergency care.
“However, it is important to recognize that more imaging does not equal better care,” she said. “More imaging may be associated with unnecessary, low-value tests that may add radiation and other risks but do not improve care.”
She said higher rates of imaging may occur when patients present early in the course of a disease, when the differential diagnosis remains broad.
If families have delayed seeking care because of time constraints, transportation problems, cost of care, or mistrust of the health system, children may present later in the course of a disease and require less imaging for a diagnosis, she explained.
“This paper offers a valuable look at the inequities that exist in pediatric emergency imaging use, and further research will be essential to understand and address the causes of these differences,” Dr. Kaplan said.
A coauthor reported compensation as a member of a Medical Review Committee for Highmark. Other coauthors reported grants from the U.S. Agency for Healthcare Research and Quality outside the submitted work. Dr. Briggs-Malonson and Dr. Kaplan reported no relevant financial relationships.
Non-Hispanic White children were more likely to receive diagnostic imaging at children’s hospitals’ emergency departments across the United States than were Hispanic children and non-Hispanic Black children, according to a large study published in JAMA Network Open.
Researchers found that, the more the percentage of children from minority groups cared for by a hospital increased, the wider the imaging gap between those children and non-Hispanic White children.
The cross-sectional study, led by Margaret E. Samuels-Kalow, MD, MPhil, MSHP, with the department of emergency medicine, Massachusetts General Hospital and Harvard Medical School in Boston, included 38 children’s hospitals and more than 12 million ED visits.
“These findings emphasize the urgent need for interventions at the hospital level to improve equity in imaging in pediatric emergency medicine,” the authors write.
Patients included in the study were younger than 18 and visited an ED from January 2016 through December 2019. Data were pulled from the Pediatric Health Information System.
Of the more than 12 million visits in this study, 3.5 million (28.7%) involved at least one diagnostic imaging test.
Diagnostic imaging was performed in 1.5 million visits (34.2%) for non-Hispanic White children; 790,961 (24.6%) for non-Hispanic Black children; and 907,222 (26.1%) for Hispanic children (P < .001).
Non-Hispanic Black children were consistently less likely to get diagnostic imaging than non-Hispanic White counterparts at every hospital in the study, no matter the imaging modality: radiography, ultrasonography, computed tomography, or magnetic resonance imaging.
Hispanic patients were generally less likely to get imaging than non-Hispanic White patients, though results were less consistent for ultrasound and MRI.
In a sensitivity analysis, when looking at imaging from patients’ first visit across the study cohort, non-Hispanic Black children were significantly less likely to get imaging than non-Hispanic White children (adjusted odds ratio, 0.77; 95% confidence interval, 0.74-0.79).
“This remained significant even after adjustment for a priori specified confounders including hospital propensity to image,” the authors write.
Authors acknowledge that it is possible that some of the differences may be attributable to the patient mix regarding severity of cases or indications for imaging by hospital, but they note that all models were adjusted for diagnosis-related group and other potential confounders.
This study did not assess whether one group is being overtested. Researchers also note that higher rates of imaging do not necessarily indicate higher quality of care.
However, the authors note, previous research has suggested overtesting of non-Hispanic White patients for head CT and chest pain, as well as patterns of overtreatment of non-Hispanic White patients who have bronchiolitis or viral upper respiratory tract infections.
Medell Briggs-Malonson, MD, MPH, chief of health equity, diversity and inclusion for the University of California, Los Angeles, Hospital and Clinic System, who was not part of the study, said in an interview “this all rings true.”
“This is not the first study we have had in either the pediatric or adult populations that shows disparate levels of care as well as health outcomes. Now we are starting to be able to measure it,” she said.
This study is further evidence of medical racism, she says, and highlights that it’s not the hospital choice or the insurance type affecting the numbers, she said.
“When you control for those factors, it looks to be it’s only due to race and that’s because of the very deep levels of implicit bias as well as explicit bias that we still have in our health systems and even in our providers,” said Dr. Briggs-Malonson, who is also an associate professor of emergency medicine at UCLA. “It’s incredibly important to identify and immediately address.”
What can be done?
Changing these patterns starts with knowing the numbers, the authors write.
“Hospitals should measure their own differences in imaging rates and increase awareness of existing areas of differential treatment as a starting point for improvement,” Dr. Samuels-Kalow and coauthors say.
Dr. Briggs-Malonson added that guidelines are very clear about when children should get imaging. Adhering to evidence-based guidelines can help avoid variations in care from external factors.
“If children are not receiving the absolute best comprehensive evaluation in the emergency department that they deserve, we can miss many different illnesses, which can lead to worse outcomes,” she noted.
As for what might motivate lack of imaging, Dr. Briggs-Malonson pointed to longstanding trends of providers thinking complaints raised by minority patients may not be as severe as they report. Conversely, in caring for White patients there may be a feeling that more tests and imaging may be better out of more fear of missing something, she said.
At UCLA, she says, dashboards have been developed to track statistics on care by age, race, ethnicity, language, insurance type, etc., though not specifically in pediatric imaging, to assess and address any care inequities.
Summer L. Kaplan, MD, MS, director of emergency radiology at Children’s Hospital of Philadelphia, who also was not part of the study, said the finding of racial disparities in pediatric ED imaging provides evidence that gaps still exist in providing the best care to all children and families seeking emergency care.
“However, it is important to recognize that more imaging does not equal better care,” she said. “More imaging may be associated with unnecessary, low-value tests that may add radiation and other risks but do not improve care.”
She said higher rates of imaging may occur when patients present early in the course of a disease, when the differential diagnosis remains broad.
If families have delayed seeking care because of time constraints, transportation problems, cost of care, or mistrust of the health system, children may present later in the course of a disease and require less imaging for a diagnosis, she explained.
“This paper offers a valuable look at the inequities that exist in pediatric emergency imaging use, and further research will be essential to understand and address the causes of these differences,” Dr. Kaplan said.
A coauthor reported compensation as a member of a Medical Review Committee for Highmark. Other coauthors reported grants from the U.S. Agency for Healthcare Research and Quality outside the submitted work. Dr. Briggs-Malonson and Dr. Kaplan reported no relevant financial relationships.
FROM JAMA NETWORK OPEN
Caring for Muslim patients who fast during Ramadan
Ramadan is one of the obligatory pillars in Islam during which healthy Muslims are required to fast from dawn until sunset every day for 1 month. There are an estimated 3.45 million Muslims in the United States, and this population will continue to grow by 100,000 per year.1 With the increased growth of the Muslim population, it is important for clinicians to be aware of how patients of Muslim faith are affected during Ramadan. In this article, we explore the potential risks, as well as the benefits, the month of Ramadan brings to patients. We will also explain how being religiously aware is necessary to provide optimal care for these individuals.
For some patients, fasting may pose risks
Similar to other communities in the United States, individuals who are Muslim experience mood disorders, anxiety disorders, posttraumatic stress disorder, obsessive-compulsive disorder, schizophrenia, substance use disorders, and other psychiatric illnesses.2 During the month of Ramadan, Muslims are to abstain completely from eating and drinking from dawn until sunset. This includes medications as well as food and drink.
Due to these circumstances, patients will often change the timing, frequency, and dosing of their medications to allow them to fast. One study found 60% of Muslims made medication adjustments during Ramadan without seeking medical advice.3 It is possible that such alterations may be detrimental. During Ramadan, some Muslims wake up early in the morning to eat a pre-dawn meal, and often go back to sleep. This has been reported to cause a delay in sleep-wake times and to reduce rapid eye movement sleep.4 These circadian rhythm changes can be detrimental to patients with bipolar disorder. One study found higher rates of relapse to depression and mania in patients with bipolar disorder who were fasting during Ramadan.5 Circadian rhythm disturbances also may worsen depression.6 Another point of concern is patients with eating disorders. One small case series (N = 6) found that fasting during Ramadan exacerbated symptoms in patients with eating disorders.7
Another concern is that dehydration while fasting can lead to lithium toxicity. However, one study found lithium levels remained stable while fasting for 10 to 12 hours.5 Another showed that changing lithium dosing from twice a day to once a day allowed for easier administration without causing a subtherapeutic change in blood lithium levels.8
The practice also may have benefits for mental health
For many Muslims, Ramadan is the best time of the year, where they reconnect with their religion and experience the utmost spiritual growth. Studies have shown that the incidence of suicide is lowest during Ramadan compared to other months.9 A study of older men found that intermittent fasting and calorie restriction (not during Ramadan) resulted in decreases in tension, confusion, anger, and mood disturbance.10 Another study found that fasting during Ramadan had a positive impact on depression, anxiety, stress, and cognitive function.11
Clinical considerations
To provide the best care for Muslim patients during Ramadan, clinicians should take a holistic approach and take all factors into consideration. It is common for circadian rhythm disruptions to exacerbate mood disorders, so encourage patients to maintain healthy sleep hygiene to their best ability during this month. Another important consideration is medication timing and dosing.12 For patients prescribed a medication that typically is taken twice a day, determine if this dosing can be changed to once a day, or if both doses can be taken when it is permissible to eat (sunset to dawn). For medications that are absorbed with food, consider how these medications might be adjusted and maintained while a patient is fasting. Some medications may be sedating or activating, so the timing of administration may need to be adjusted to meet the patient’s needs. Lastly, keep in mind that certain medications can have withdrawal effects, and the likelihood of this occurring while a patient is fasting.
One vital point is that if a patient is at high risk of clinically decompensating due to fasting or medication adjustments or discontinuation, advise them to not fast. Muslims with physical or mental illnesses are excused from fasting. Bear in mind that because Ramadan is meant to be a month of heightened spirituality, many Muslims will prefer to fast.
1. Pew Research Center. Demographic portrait of Muslim Americans. Published July 26, 2017. Accessed January 15, 2019. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans
2. Basit A, Hamid M. Mental health issues of Muslim Americans. J IMA. 2010;42(3):106-110.
3. Aslam M, Assad A. Drug regimens and fasting during Ramadan: a survey in Kuwait. Public Health. 1986;100(1):49-53.
4. Qasrawi SO, Pandi-Perumal SR, BaHammam AS. The effect of intermittent fasting during Ramadan on sleep, sleepiness, cognitive function, and circadian rhythm. Sleep Breath. 2017;21(3):577-586.
5. Eddahby S, Kadri N, Moussaoui D. Fasting during Ramadan is associated with a higher recurrence rate in patients with bipolar disorder. World Psychiatry. 2014;13(1):97.
6. Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23(7):571-585.
7. Akgül S, Derman O, Kanbur NÖ. Fasting during Ramadan: a religious factor as a possible trigger or exacerbator for eating disorders in adolescents. Int J Eat Disord. 2014;47(8):905-910.
8. Kadri N, Mouchtaq N, Hakkou F, et al. Relapses in bipolar patients: changes in social rhythm? Int J Neuropsychopharmacol. 2000;3(1):45-49.
9. Taktak S, Kumral B, Unsal A, et al. Evidence for an association between suicide and religion: a 33-year retrospective autopsy analysis of suicide by hanging during the month of Ramadan in Istanbul. Aust J Forensic Sci. 2016;48(2):121-131.
10. Hussin NM, Shahar S, Teng NI, et al. Efficacy of fasting and calorie restriction (FCR) on mood and depression among ageing men. J Nutr Health Aging. 2013;17(8):674-680.
11. Amin A, Sai Sailesh K, Mishra S, et al. Effects of fasting during Ramadan month on depression, anxiety and stress and cognition. Int J Med Res Rev. 2016;4(5):771-774.
12. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.
Ramadan is one of the obligatory pillars in Islam during which healthy Muslims are required to fast from dawn until sunset every day for 1 month. There are an estimated 3.45 million Muslims in the United States, and this population will continue to grow by 100,000 per year.1 With the increased growth of the Muslim population, it is important for clinicians to be aware of how patients of Muslim faith are affected during Ramadan. In this article, we explore the potential risks, as well as the benefits, the month of Ramadan brings to patients. We will also explain how being religiously aware is necessary to provide optimal care for these individuals.
For some patients, fasting may pose risks
Similar to other communities in the United States, individuals who are Muslim experience mood disorders, anxiety disorders, posttraumatic stress disorder, obsessive-compulsive disorder, schizophrenia, substance use disorders, and other psychiatric illnesses.2 During the month of Ramadan, Muslims are to abstain completely from eating and drinking from dawn until sunset. This includes medications as well as food and drink.
Due to these circumstances, patients will often change the timing, frequency, and dosing of their medications to allow them to fast. One study found 60% of Muslims made medication adjustments during Ramadan without seeking medical advice.3 It is possible that such alterations may be detrimental. During Ramadan, some Muslims wake up early in the morning to eat a pre-dawn meal, and often go back to sleep. This has been reported to cause a delay in sleep-wake times and to reduce rapid eye movement sleep.4 These circadian rhythm changes can be detrimental to patients with bipolar disorder. One study found higher rates of relapse to depression and mania in patients with bipolar disorder who were fasting during Ramadan.5 Circadian rhythm disturbances also may worsen depression.6 Another point of concern is patients with eating disorders. One small case series (N = 6) found that fasting during Ramadan exacerbated symptoms in patients with eating disorders.7
Another concern is that dehydration while fasting can lead to lithium toxicity. However, one study found lithium levels remained stable while fasting for 10 to 12 hours.5 Another showed that changing lithium dosing from twice a day to once a day allowed for easier administration without causing a subtherapeutic change in blood lithium levels.8
The practice also may have benefits for mental health
For many Muslims, Ramadan is the best time of the year, where they reconnect with their religion and experience the utmost spiritual growth. Studies have shown that the incidence of suicide is lowest during Ramadan compared to other months.9 A study of older men found that intermittent fasting and calorie restriction (not during Ramadan) resulted in decreases in tension, confusion, anger, and mood disturbance.10 Another study found that fasting during Ramadan had a positive impact on depression, anxiety, stress, and cognitive function.11
Clinical considerations
To provide the best care for Muslim patients during Ramadan, clinicians should take a holistic approach and take all factors into consideration. It is common for circadian rhythm disruptions to exacerbate mood disorders, so encourage patients to maintain healthy sleep hygiene to their best ability during this month. Another important consideration is medication timing and dosing.12 For patients prescribed a medication that typically is taken twice a day, determine if this dosing can be changed to once a day, or if both doses can be taken when it is permissible to eat (sunset to dawn). For medications that are absorbed with food, consider how these medications might be adjusted and maintained while a patient is fasting. Some medications may be sedating or activating, so the timing of administration may need to be adjusted to meet the patient’s needs. Lastly, keep in mind that certain medications can have withdrawal effects, and the likelihood of this occurring while a patient is fasting.
One vital point is that if a patient is at high risk of clinically decompensating due to fasting or medication adjustments or discontinuation, advise them to not fast. Muslims with physical or mental illnesses are excused from fasting. Bear in mind that because Ramadan is meant to be a month of heightened spirituality, many Muslims will prefer to fast.
Ramadan is one of the obligatory pillars in Islam during which healthy Muslims are required to fast from dawn until sunset every day for 1 month. There are an estimated 3.45 million Muslims in the United States, and this population will continue to grow by 100,000 per year.1 With the increased growth of the Muslim population, it is important for clinicians to be aware of how patients of Muslim faith are affected during Ramadan. In this article, we explore the potential risks, as well as the benefits, the month of Ramadan brings to patients. We will also explain how being religiously aware is necessary to provide optimal care for these individuals.
For some patients, fasting may pose risks
Similar to other communities in the United States, individuals who are Muslim experience mood disorders, anxiety disorders, posttraumatic stress disorder, obsessive-compulsive disorder, schizophrenia, substance use disorders, and other psychiatric illnesses.2 During the month of Ramadan, Muslims are to abstain completely from eating and drinking from dawn until sunset. This includes medications as well as food and drink.
Due to these circumstances, patients will often change the timing, frequency, and dosing of their medications to allow them to fast. One study found 60% of Muslims made medication adjustments during Ramadan without seeking medical advice.3 It is possible that such alterations may be detrimental. During Ramadan, some Muslims wake up early in the morning to eat a pre-dawn meal, and often go back to sleep. This has been reported to cause a delay in sleep-wake times and to reduce rapid eye movement sleep.4 These circadian rhythm changes can be detrimental to patients with bipolar disorder. One study found higher rates of relapse to depression and mania in patients with bipolar disorder who were fasting during Ramadan.5 Circadian rhythm disturbances also may worsen depression.6 Another point of concern is patients with eating disorders. One small case series (N = 6) found that fasting during Ramadan exacerbated symptoms in patients with eating disorders.7
Another concern is that dehydration while fasting can lead to lithium toxicity. However, one study found lithium levels remained stable while fasting for 10 to 12 hours.5 Another showed that changing lithium dosing from twice a day to once a day allowed for easier administration without causing a subtherapeutic change in blood lithium levels.8
The practice also may have benefits for mental health
For many Muslims, Ramadan is the best time of the year, where they reconnect with their religion and experience the utmost spiritual growth. Studies have shown that the incidence of suicide is lowest during Ramadan compared to other months.9 A study of older men found that intermittent fasting and calorie restriction (not during Ramadan) resulted in decreases in tension, confusion, anger, and mood disturbance.10 Another study found that fasting during Ramadan had a positive impact on depression, anxiety, stress, and cognitive function.11
Clinical considerations
To provide the best care for Muslim patients during Ramadan, clinicians should take a holistic approach and take all factors into consideration. It is common for circadian rhythm disruptions to exacerbate mood disorders, so encourage patients to maintain healthy sleep hygiene to their best ability during this month. Another important consideration is medication timing and dosing.12 For patients prescribed a medication that typically is taken twice a day, determine if this dosing can be changed to once a day, or if both doses can be taken when it is permissible to eat (sunset to dawn). For medications that are absorbed with food, consider how these medications might be adjusted and maintained while a patient is fasting. Some medications may be sedating or activating, so the timing of administration may need to be adjusted to meet the patient’s needs. Lastly, keep in mind that certain medications can have withdrawal effects, and the likelihood of this occurring while a patient is fasting.
One vital point is that if a patient is at high risk of clinically decompensating due to fasting or medication adjustments or discontinuation, advise them to not fast. Muslims with physical or mental illnesses are excused from fasting. Bear in mind that because Ramadan is meant to be a month of heightened spirituality, many Muslims will prefer to fast.
1. Pew Research Center. Demographic portrait of Muslim Americans. Published July 26, 2017. Accessed January 15, 2019. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans
2. Basit A, Hamid M. Mental health issues of Muslim Americans. J IMA. 2010;42(3):106-110.
3. Aslam M, Assad A. Drug regimens and fasting during Ramadan: a survey in Kuwait. Public Health. 1986;100(1):49-53.
4. Qasrawi SO, Pandi-Perumal SR, BaHammam AS. The effect of intermittent fasting during Ramadan on sleep, sleepiness, cognitive function, and circadian rhythm. Sleep Breath. 2017;21(3):577-586.
5. Eddahby S, Kadri N, Moussaoui D. Fasting during Ramadan is associated with a higher recurrence rate in patients with bipolar disorder. World Psychiatry. 2014;13(1):97.
6. Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23(7):571-585.
7. Akgül S, Derman O, Kanbur NÖ. Fasting during Ramadan: a religious factor as a possible trigger or exacerbator for eating disorders in adolescents. Int J Eat Disord. 2014;47(8):905-910.
8. Kadri N, Mouchtaq N, Hakkou F, et al. Relapses in bipolar patients: changes in social rhythm? Int J Neuropsychopharmacol. 2000;3(1):45-49.
9. Taktak S, Kumral B, Unsal A, et al. Evidence for an association between suicide and religion: a 33-year retrospective autopsy analysis of suicide by hanging during the month of Ramadan in Istanbul. Aust J Forensic Sci. 2016;48(2):121-131.
10. Hussin NM, Shahar S, Teng NI, et al. Efficacy of fasting and calorie restriction (FCR) on mood and depression among ageing men. J Nutr Health Aging. 2013;17(8):674-680.
11. Amin A, Sai Sailesh K, Mishra S, et al. Effects of fasting during Ramadan month on depression, anxiety and stress and cognition. Int J Med Res Rev. 2016;4(5):771-774.
12. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.
1. Pew Research Center. Demographic portrait of Muslim Americans. Published July 26, 2017. Accessed January 15, 2019. https://www.pewforum.org/2017/07/26/demographic-portrait-of-muslim-americans
2. Basit A, Hamid M. Mental health issues of Muslim Americans. J IMA. 2010;42(3):106-110.
3. Aslam M, Assad A. Drug regimens and fasting during Ramadan: a survey in Kuwait. Public Health. 1986;100(1):49-53.
4. Qasrawi SO, Pandi-Perumal SR, BaHammam AS. The effect of intermittent fasting during Ramadan on sleep, sleepiness, cognitive function, and circadian rhythm. Sleep Breath. 2017;21(3):577-586.
5. Eddahby S, Kadri N, Moussaoui D. Fasting during Ramadan is associated with a higher recurrence rate in patients with bipolar disorder. World Psychiatry. 2014;13(1):97.
6. Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23(7):571-585.
7. Akgül S, Derman O, Kanbur NÖ. Fasting during Ramadan: a religious factor as a possible trigger or exacerbator for eating disorders in adolescents. Int J Eat Disord. 2014;47(8):905-910.
8. Kadri N, Mouchtaq N, Hakkou F, et al. Relapses in bipolar patients: changes in social rhythm? Int J Neuropsychopharmacol. 2000;3(1):45-49.
9. Taktak S, Kumral B, Unsal A, et al. Evidence for an association between suicide and religion: a 33-year retrospective autopsy analysis of suicide by hanging during the month of Ramadan in Istanbul. Aust J Forensic Sci. 2016;48(2):121-131.
10. Hussin NM, Shahar S, Teng NI, et al. Efficacy of fasting and calorie restriction (FCR) on mood and depression among ageing men. J Nutr Health Aging. 2013;17(8):674-680.
11. Amin A, Sai Sailesh K, Mishra S, et al. Effects of fasting during Ramadan month on depression, anxiety and stress and cognition. Int J Med Res Rev. 2016;4(5):771-774.
12. Furqan Z, Awaad R, Kurdyak P, et al. Considerations for clinicians treating Muslim patients with psychiatric disorders during Ramadan. Lancet Psychiatry. 2019;6(7):556-557.







