User login
Pediatricians see drop in income during the pandemic
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”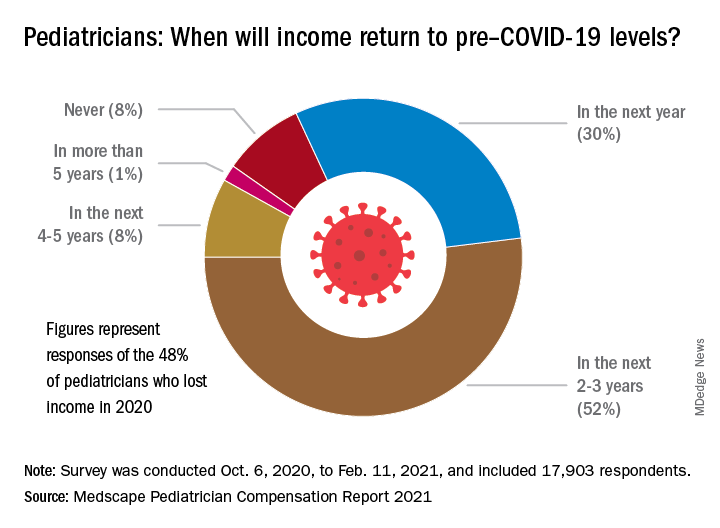
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”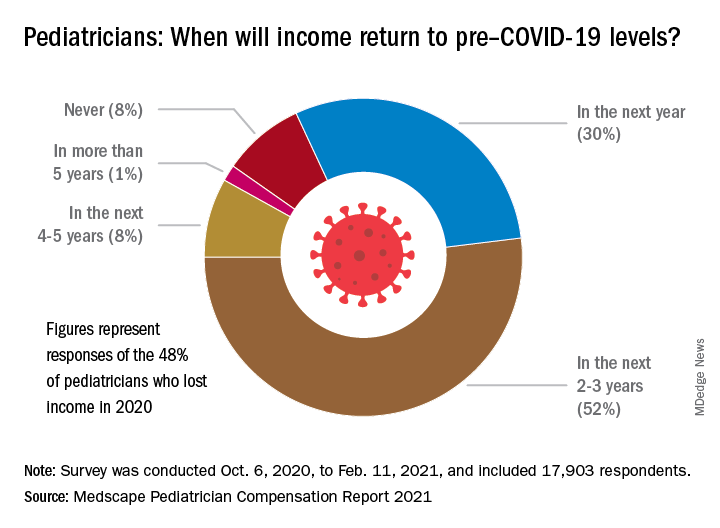
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
The average income for pediatricians declined slightly from 2019 to 2020, according to the Medscape Pediatrician Compensation Report 2021.

The report, which was conducted between October 2020 and February 2021, found that the average pediatrician income was down $11,000 – from $232,000 in 2019 to $221,000 in 2020, with 48% of pediatricians reporting at least some decline in compensation.
The specialty also earned the least amount of money in 2020, compared with all of the other specialties, which isn’t surprising since pediatricians have been among the lowest-paid physician specialties since 2013. The highest-earning specialty was plastic surgery with an average income of $526,000 annually.
Most pediatricians who saw a drop in income cited pandemic-related issues such as job loss, fewer hours, and fewer patients.
Jesse Hackell, MD, vice president and chief operating officer of Ponoma Pediatrics in New York, said in an interview the reduced wages pediatricians saw in 2020 didn’t surprise him because many pediatric offices saw a huge drop in visits that were not urgent.
“[The report] shows that procedural specialties tended to do a lot better than the nonprocedural specialties,” Dr. Hackell said. “That’s because, during the shutdown, if you broke your leg, you still needed the orthopedist. And even though the hospitals weren’t doing elective surgeries, they were certainly doing the emergency stuff.”
Meanwhile, in pediatrician offices, where Dr. Hackell said office visits dropped 70%-80% at the beginning of the pandemic, “parents weren’t going to bring a healthy kid out for routine visits and they weren’t going to bring a kid out for minor illnesses and expose them to possibly communicable diseases in the office.”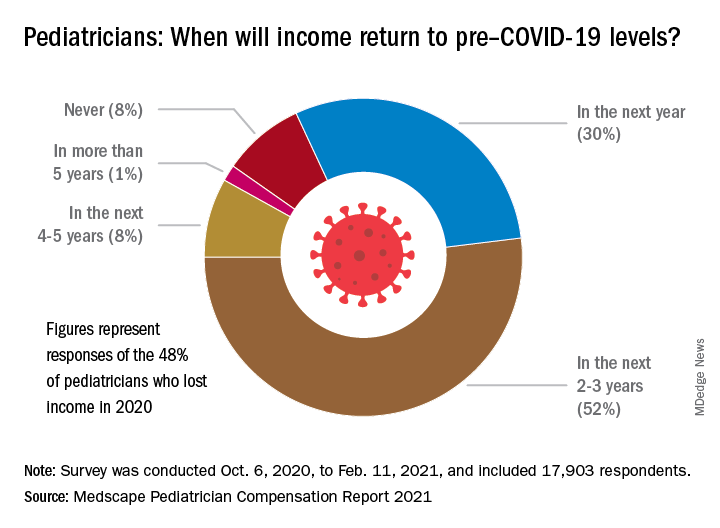
About 52% of pediatricians who lost income because of the pandemic believe their income levels will return to normal in 2-3 years. Meanwhile 30% of pediatricians expect their income to return to normal within a year, and 8% believe it will take 4 years for them to bounce back.
Physician work hours generally declined for some time during the pandemic, according to the report. However, most pediatricians are working about the same number of hours as they did before the pandemic, which is 47 hours per week.
Despite working the same number of hours per week that they did prepandemic, they are seeing fewer patients. They are currently seeing on average 64 patients per week, compared with the 78 patients they used to see weekly before the pandemic.
Dr. Hackell said that might be because pediatric offices are trying to make up the loss of revenue during the beginning of the pandemic, from the reduced number of well visits and immunizations, in the second half of the year with outreach.
“Since about June 2020, we’ve been making concerted efforts to remind parents that preventing other infectious diseases is critically important,” Dr. Hackell explained. “And so actually, for the second half of the year, many of us saw more well visits and immunization volume than in 2019 as we sought to make up the gap. It wasn’t that we were seeing more overall, but we’re trying to make up the gap that happened from March, April, May, [and] June.”
Most pediatricians find their work rewarding. One-third say the most rewarding part of their job is gratitude from and relationships with their patients. Meanwhile, 31% of pediatricians said knowing they are making the world a better place was a rewarding part of their job. Only 8% of them said making money was a rewarding part of their job.
Dr. Hackell said he did not go into pediatrics to make money, it was because he found it stimulating and has “no complaints.”
“I’ve been a pediatrician for 40 years and I wouldn’t do anything else,” Dr. Hackell said. “I don’t know that there’s anything that I would find as rewarding as the relationships that I’ve had over 40 years with my patients. You know, getting invited to weddings of kids who I saw when they were newborns is pretty impressive. It’s the gratification of having ongoing relationships with families.”
Furthermore, the report revealed that 77% of pediatricians said they would pick medicine again if they had a choice, and 82% said they would choose the same specialty.
The experts disclosed no relevant financial interests.
*This story was updated on 5/18/2021.
Patients with CLL have significantly reduced response to COVID-19 vaccine
Patients with chronic lymphocytic leukemia (CLL) have increased risk for severe COVID-19 disease as well as mortality.
Such patients are likely to have compromised immune systems, making them respond poorly to vaccines, as has been seen in studies involving pneumococcal, hepatitis B, and influenza A and B vaccination.
In order to determine if vaccination against COVID-19 disease will be effective among these patients, researchers performed a study to determine the efficacy of a single COVID-19 vaccine in patients with CLL. They found that the response rate of patients with CLL to vaccination was significantly lower than that of healthy controls, according to the study published in Blood Advances.
Study details
The study (NCT04746092) assessed the humoral immune responses to BNT162b2 mRNA COVID-19 (Pfizer) vaccination in adult patients with CLL and compared responses with those obtained in age-matched healthy controls. Patients received two vaccine doses, 21 days apart, and antibody titers were measured 2-3 weeks after administration of the second dose, according to Yair Herishanu, MD, of the Tel-Aviv Sourasky Medical Center, Tel Aviv University, and colleagues.
Troubling results
The researchers found an antibody-mediated response to the BNT162b2 mRNA COVID-19 vaccine in only 66 of 167 (39.5%) of all patients with CLL. The response rate of 52 of these responding patients with CLL to the vaccine was significantly lower than that occurring in 52 age- and sex-matched healthy controls (52% vs. 100%, respectively; adjusted odds ratio, 0.010; 95% confidence interval, 0.001-0.162; P < .001).
Among the patients with CLL, the response rate was highest in those who obtained clinical remission after treatment (79.2%), followed by 55.2% in treatment-naive patients, and it was only 16% in patients under treatment at the time of vaccination.
In patients treated with either BTK inhibitors or venetoclax with and without anti-CD20 antibody, response rates were low (16.0% and 13.6%, respectively). In particular, none of the patients exposed to anti-CD20 antibodies less than 12 months prior to vaccination responded, according to the researchers.
Multivariate analysis showed that the independent predictors of a vaccine response were age (65 years or younger; odds ratio, 3.17; P = .025), sex (women; OR, 3.66; P = .006), lack of active therapy (including treatment naive and previously treated patients; OR 6.59; P < .001), IgG levels 550 mg/dL or greater (OR, 3.70; P = .037), and IgM levels 40mg/dL or greater (OR, 2.92; P = .017).
Within a median follow-up period of 75 days since the first vaccine dose, none of the CLL patients developed COVID-19 infection, the researchers reported.
“Vaccinated patients with CLL should continue to adhere to masking, social distancing, and vaccination of their close contacts should be strongly recommended. Serological tests after the second injection of the COVID-19 vaccine can provide valuable information to the individual patient and perhaps, may be integrated in future clinical decisions,” the researchers concluded.
The study was sponsored by the Tel-Aviv Sourasky Medical Center. The authors reported that they had no conflicts of interest.
Patients with chronic lymphocytic leukemia (CLL) have increased risk for severe COVID-19 disease as well as mortality.
Such patients are likely to have compromised immune systems, making them respond poorly to vaccines, as has been seen in studies involving pneumococcal, hepatitis B, and influenza A and B vaccination.
In order to determine if vaccination against COVID-19 disease will be effective among these patients, researchers performed a study to determine the efficacy of a single COVID-19 vaccine in patients with CLL. They found that the response rate of patients with CLL to vaccination was significantly lower than that of healthy controls, according to the study published in Blood Advances.
Study details
The study (NCT04746092) assessed the humoral immune responses to BNT162b2 mRNA COVID-19 (Pfizer) vaccination in adult patients with CLL and compared responses with those obtained in age-matched healthy controls. Patients received two vaccine doses, 21 days apart, and antibody titers were measured 2-3 weeks after administration of the second dose, according to Yair Herishanu, MD, of the Tel-Aviv Sourasky Medical Center, Tel Aviv University, and colleagues.
Troubling results
The researchers found an antibody-mediated response to the BNT162b2 mRNA COVID-19 vaccine in only 66 of 167 (39.5%) of all patients with CLL. The response rate of 52 of these responding patients with CLL to the vaccine was significantly lower than that occurring in 52 age- and sex-matched healthy controls (52% vs. 100%, respectively; adjusted odds ratio, 0.010; 95% confidence interval, 0.001-0.162; P < .001).
Among the patients with CLL, the response rate was highest in those who obtained clinical remission after treatment (79.2%), followed by 55.2% in treatment-naive patients, and it was only 16% in patients under treatment at the time of vaccination.
In patients treated with either BTK inhibitors or venetoclax with and without anti-CD20 antibody, response rates were low (16.0% and 13.6%, respectively). In particular, none of the patients exposed to anti-CD20 antibodies less than 12 months prior to vaccination responded, according to the researchers.
Multivariate analysis showed that the independent predictors of a vaccine response were age (65 years or younger; odds ratio, 3.17; P = .025), sex (women; OR, 3.66; P = .006), lack of active therapy (including treatment naive and previously treated patients; OR 6.59; P < .001), IgG levels 550 mg/dL or greater (OR, 3.70; P = .037), and IgM levels 40mg/dL or greater (OR, 2.92; P = .017).
Within a median follow-up period of 75 days since the first vaccine dose, none of the CLL patients developed COVID-19 infection, the researchers reported.
“Vaccinated patients with CLL should continue to adhere to masking, social distancing, and vaccination of their close contacts should be strongly recommended. Serological tests after the second injection of the COVID-19 vaccine can provide valuable information to the individual patient and perhaps, may be integrated in future clinical decisions,” the researchers concluded.
The study was sponsored by the Tel-Aviv Sourasky Medical Center. The authors reported that they had no conflicts of interest.
Patients with chronic lymphocytic leukemia (CLL) have increased risk for severe COVID-19 disease as well as mortality.
Such patients are likely to have compromised immune systems, making them respond poorly to vaccines, as has been seen in studies involving pneumococcal, hepatitis B, and influenza A and B vaccination.
In order to determine if vaccination against COVID-19 disease will be effective among these patients, researchers performed a study to determine the efficacy of a single COVID-19 vaccine in patients with CLL. They found that the response rate of patients with CLL to vaccination was significantly lower than that of healthy controls, according to the study published in Blood Advances.
Study details
The study (NCT04746092) assessed the humoral immune responses to BNT162b2 mRNA COVID-19 (Pfizer) vaccination in adult patients with CLL and compared responses with those obtained in age-matched healthy controls. Patients received two vaccine doses, 21 days apart, and antibody titers were measured 2-3 weeks after administration of the second dose, according to Yair Herishanu, MD, of the Tel-Aviv Sourasky Medical Center, Tel Aviv University, and colleagues.
Troubling results
The researchers found an antibody-mediated response to the BNT162b2 mRNA COVID-19 vaccine in only 66 of 167 (39.5%) of all patients with CLL. The response rate of 52 of these responding patients with CLL to the vaccine was significantly lower than that occurring in 52 age- and sex-matched healthy controls (52% vs. 100%, respectively; adjusted odds ratio, 0.010; 95% confidence interval, 0.001-0.162; P < .001).
Among the patients with CLL, the response rate was highest in those who obtained clinical remission after treatment (79.2%), followed by 55.2% in treatment-naive patients, and it was only 16% in patients under treatment at the time of vaccination.
In patients treated with either BTK inhibitors or venetoclax with and without anti-CD20 antibody, response rates were low (16.0% and 13.6%, respectively). In particular, none of the patients exposed to anti-CD20 antibodies less than 12 months prior to vaccination responded, according to the researchers.
Multivariate analysis showed that the independent predictors of a vaccine response were age (65 years or younger; odds ratio, 3.17; P = .025), sex (women; OR, 3.66; P = .006), lack of active therapy (including treatment naive and previously treated patients; OR 6.59; P < .001), IgG levels 550 mg/dL or greater (OR, 3.70; P = .037), and IgM levels 40mg/dL or greater (OR, 2.92; P = .017).
Within a median follow-up period of 75 days since the first vaccine dose, none of the CLL patients developed COVID-19 infection, the researchers reported.
“Vaccinated patients with CLL should continue to adhere to masking, social distancing, and vaccination of their close contacts should be strongly recommended. Serological tests after the second injection of the COVID-19 vaccine can provide valuable information to the individual patient and perhaps, may be integrated in future clinical decisions,” the researchers concluded.
The study was sponsored by the Tel-Aviv Sourasky Medical Center. The authors reported that they had no conflicts of interest.
FROM BLOOD ADVANCES
How to improve our response to COVID’s mental tolls
We have no way of precisely knowing how many lives might have been saved, and how much grief and loneliness spared and economic ruin contained during COVID-19 if we had risen to its myriad challenges in a timely fashion. However, I feel we can safely say that the United States deserves to be graded with an “F” for its management of the pandemic.
To render this grade, we need only to read the countless verified reports of how critically needed public health measures were not taken soon enough, or sufficiently, to substantially mitigate human and societal suffering.
This began with the failure to protect doctors, nurses, and technicians, who did not have the personal protective equipment needed to prevent infection and spare risk to their loved ones. It soon extended to the country’s failure to adequately protect all its citizens and residents. COVID-19 then rained its grievous consequences disproportionately upon people of color, those living in poverty, and those with housing and food insecurity – those already greatly foreclosed from opportunities to exit from their circumstances.
We all have heard, “Fool me once, shame on you; fool me twice, shame on me.”
Bear witness, colleagues and friends: It will be our shared shame if we too continue to fail in our response to COVID-19. But failure need not happen because protecting ourselves and our country is a solvable problem; complex and demanding for sure, but solvable.
To battle trauma, we must first define it
The sine qua non of a disaster is its psychic and social trauma. I asked Maureen Sayres Van Niel, MD, chair of the American Psychiatric Association’s Minority and Underrepresented Caucus and a former steering committee member of the U.S. Preventive Services Task Force, to define trauma. She said, “It is [the product of] a catastrophic, unexpected event over which we have little control, with grave consequences to the lives and psychological functioning of those individuals and groups affected.”
The COVID-19 pandemic is a massively amplified traumatic event because of the virulence and contagious properties of the virus and its variants; the absence of end date on the horizon; its effect as a proverbial ax that disproportionately falls on the majority of the populace experiencing racial and social inequities; and the ironic yet necessary imperative to distance ourselves from those we care about and who care about us.
Four interdependent factors drive the magnitude of the traumatic impact of a disaster: the degree of exposure to the life-threatening event; the duration and threat of recurrence; an individual’s preexisting (natural and human-made) trauma and mental and addictive disorders; and the adequacy of family and fundamental resources such as housing, food, safety, and access to health care (the social dimensions of health and mental health). These factors underline the “who,” “what,” “where,” and “how” of what should have been (and continue to be) an effective public health response to the COVID-19 pandemic.
Yet existing categories that we have used to predict risk for trauma no longer hold. The gravity, prevalence, and persistence of COVID-19’s horrors erase any differences among victims, witnesses, and bystanders. Dr Sayres Van Niel asserts that we have a “collective, national trauma.” In April, the Kaiser Family Foundation’s Vaccine Monitor reported that 24% of U.S. adults had a close friend or family member who died of COVID-19. That’s 82 million Americans! Our country has eclipsed individual victimization and trauma because we are all in its maw.
Vital lessons from the past
In a previous column, I described my role as New York City’s mental health commissioner after 9/11 and the many lessons we learned during that multiyear process. Our work served as a template for other disasters to follow, such as Hurricane Sandy. Its value to COVID-19 is equally apparent.
We learned that those most at risk of developing symptomatic, functionally impairing mental illness had prior traumatic experiences (for example, from childhood abuse or neglect, violence, war, and forced displacement from their native land) and/or a preexisting mental or substance use disorder.
Once these individuals and communities were identified, we could prioritize their treatment and care. Doing so required mobilizing both inner and external (social) resources, which can be used before disaster strikes or in its wake.
For individuals, adaptive resources include developing any of a number of mind-body activities (for example, meditation, mindfulness, slow breathing, and yoga); sufficient but not necessarily excessive levels of exercise (as has been said, if exercise were a pill, it would be the most potent of medicines); nourishing diets; sleep, nature’s restorative state; and perhaps most important, attachment and human connection to people who care about you and whom you care about and trust.
This does not necessarily mean holding or following an institutional religion or belonging to house of worship (though, of course, that melds and augments faith with community). For a great many, myself included, there is spirituality, the belief in a greater power, which need not be a God yet instills a sense of the vastness, universality, and continuity of life.
For communities, adaptive resources include safe homes and neighborhoods; diminishing housing and food insecurity; education, including pre-K; employment, with a livable wage; ridding human interactions of the endless, so-called microaggressions (which are not micro at all, because they accrue) of race, ethnic, class, and age discrimination and injustice; and ready access to quality and affordable health care, now more than ever for the rising tide of mental and substance use disorders that COVID-19 has unleashed.
Every gain we make to ablate racism, social injustice, discrimination, and widely and deeply spread resource and opportunity inequities means more cohesion among the members of our collective tribe. Greater cohesion, a love for thy neighbor, and equity (in action, not polemics) will fuel the resilience we will need to withstand more of COVID-19’s ongoing trauma; that of other, inescapable disasters and losses; and the wear and tear of everyday life. The rewards of equity are priceless and include the dignity that derives from fairness and justice – given and received.
An unprecedented disaster requires a bold response
My, what a list. But to me, the encompassing nature of what’s needed means that we can make differences anywhere, everywhere, and in countless and continuous ways.
The measure of any society is in how it cares for those who are foreclosed, through no fault of their own, from what we all want: a life safe from violence, secure in housing and food, with loving relationships and the pride that comes of making contributions, each in our own, wonderfully unique way.
Where will we all be in a year, 2, or 3 from now? Prepared, or not? Emotionally inoculated, or not? Better equipped, or not? As divided, or more cohesive?
Well, I imagine that depends on each and every one of us.
Lloyd I. Sederer, MD, is a psychiatrist, public health doctor, and writer. He is an adjunct professor at the Columbia University School of Public Health, director of Columbia Psychiatry Media, chief medical officer of Bongo Media, and chair of the advisory board of Get Help. He has been chief medical officer of McLean Hospital, a Harvard teaching hospital; mental health commissioner of New York City (in the Bloomberg administration); and chief medical officer of the New York State Office of Mental Health, the nation’s largest state mental health agency.
A version of this article first appeared on Medscape.com.
We have no way of precisely knowing how many lives might have been saved, and how much grief and loneliness spared and economic ruin contained during COVID-19 if we had risen to its myriad challenges in a timely fashion. However, I feel we can safely say that the United States deserves to be graded with an “F” for its management of the pandemic.
To render this grade, we need only to read the countless verified reports of how critically needed public health measures were not taken soon enough, or sufficiently, to substantially mitigate human and societal suffering.
This began with the failure to protect doctors, nurses, and technicians, who did not have the personal protective equipment needed to prevent infection and spare risk to their loved ones. It soon extended to the country’s failure to adequately protect all its citizens and residents. COVID-19 then rained its grievous consequences disproportionately upon people of color, those living in poverty, and those with housing and food insecurity – those already greatly foreclosed from opportunities to exit from their circumstances.
We all have heard, “Fool me once, shame on you; fool me twice, shame on me.”
Bear witness, colleagues and friends: It will be our shared shame if we too continue to fail in our response to COVID-19. But failure need not happen because protecting ourselves and our country is a solvable problem; complex and demanding for sure, but solvable.
To battle trauma, we must first define it
The sine qua non of a disaster is its psychic and social trauma. I asked Maureen Sayres Van Niel, MD, chair of the American Psychiatric Association’s Minority and Underrepresented Caucus and a former steering committee member of the U.S. Preventive Services Task Force, to define trauma. She said, “It is [the product of] a catastrophic, unexpected event over which we have little control, with grave consequences to the lives and psychological functioning of those individuals and groups affected.”
The COVID-19 pandemic is a massively amplified traumatic event because of the virulence and contagious properties of the virus and its variants; the absence of end date on the horizon; its effect as a proverbial ax that disproportionately falls on the majority of the populace experiencing racial and social inequities; and the ironic yet necessary imperative to distance ourselves from those we care about and who care about us.
Four interdependent factors drive the magnitude of the traumatic impact of a disaster: the degree of exposure to the life-threatening event; the duration and threat of recurrence; an individual’s preexisting (natural and human-made) trauma and mental and addictive disorders; and the adequacy of family and fundamental resources such as housing, food, safety, and access to health care (the social dimensions of health and mental health). These factors underline the “who,” “what,” “where,” and “how” of what should have been (and continue to be) an effective public health response to the COVID-19 pandemic.
Yet existing categories that we have used to predict risk for trauma no longer hold. The gravity, prevalence, and persistence of COVID-19’s horrors erase any differences among victims, witnesses, and bystanders. Dr Sayres Van Niel asserts that we have a “collective, national trauma.” In April, the Kaiser Family Foundation’s Vaccine Monitor reported that 24% of U.S. adults had a close friend or family member who died of COVID-19. That’s 82 million Americans! Our country has eclipsed individual victimization and trauma because we are all in its maw.
Vital lessons from the past
In a previous column, I described my role as New York City’s mental health commissioner after 9/11 and the many lessons we learned during that multiyear process. Our work served as a template for other disasters to follow, such as Hurricane Sandy. Its value to COVID-19 is equally apparent.
We learned that those most at risk of developing symptomatic, functionally impairing mental illness had prior traumatic experiences (for example, from childhood abuse or neglect, violence, war, and forced displacement from their native land) and/or a preexisting mental or substance use disorder.
Once these individuals and communities were identified, we could prioritize their treatment and care. Doing so required mobilizing both inner and external (social) resources, which can be used before disaster strikes or in its wake.
For individuals, adaptive resources include developing any of a number of mind-body activities (for example, meditation, mindfulness, slow breathing, and yoga); sufficient but not necessarily excessive levels of exercise (as has been said, if exercise were a pill, it would be the most potent of medicines); nourishing diets; sleep, nature’s restorative state; and perhaps most important, attachment and human connection to people who care about you and whom you care about and trust.
This does not necessarily mean holding or following an institutional religion or belonging to house of worship (though, of course, that melds and augments faith with community). For a great many, myself included, there is spirituality, the belief in a greater power, which need not be a God yet instills a sense of the vastness, universality, and continuity of life.
For communities, adaptive resources include safe homes and neighborhoods; diminishing housing and food insecurity; education, including pre-K; employment, with a livable wage; ridding human interactions of the endless, so-called microaggressions (which are not micro at all, because they accrue) of race, ethnic, class, and age discrimination and injustice; and ready access to quality and affordable health care, now more than ever for the rising tide of mental and substance use disorders that COVID-19 has unleashed.
Every gain we make to ablate racism, social injustice, discrimination, and widely and deeply spread resource and opportunity inequities means more cohesion among the members of our collective tribe. Greater cohesion, a love for thy neighbor, and equity (in action, not polemics) will fuel the resilience we will need to withstand more of COVID-19’s ongoing trauma; that of other, inescapable disasters and losses; and the wear and tear of everyday life. The rewards of equity are priceless and include the dignity that derives from fairness and justice – given and received.
An unprecedented disaster requires a bold response
My, what a list. But to me, the encompassing nature of what’s needed means that we can make differences anywhere, everywhere, and in countless and continuous ways.
The measure of any society is in how it cares for those who are foreclosed, through no fault of their own, from what we all want: a life safe from violence, secure in housing and food, with loving relationships and the pride that comes of making contributions, each in our own, wonderfully unique way.
Where will we all be in a year, 2, or 3 from now? Prepared, or not? Emotionally inoculated, or not? Better equipped, or not? As divided, or more cohesive?
Well, I imagine that depends on each and every one of us.
Lloyd I. Sederer, MD, is a psychiatrist, public health doctor, and writer. He is an adjunct professor at the Columbia University School of Public Health, director of Columbia Psychiatry Media, chief medical officer of Bongo Media, and chair of the advisory board of Get Help. He has been chief medical officer of McLean Hospital, a Harvard teaching hospital; mental health commissioner of New York City (in the Bloomberg administration); and chief medical officer of the New York State Office of Mental Health, the nation’s largest state mental health agency.
A version of this article first appeared on Medscape.com.
We have no way of precisely knowing how many lives might have been saved, and how much grief and loneliness spared and economic ruin contained during COVID-19 if we had risen to its myriad challenges in a timely fashion. However, I feel we can safely say that the United States deserves to be graded with an “F” for its management of the pandemic.
To render this grade, we need only to read the countless verified reports of how critically needed public health measures were not taken soon enough, or sufficiently, to substantially mitigate human and societal suffering.
This began with the failure to protect doctors, nurses, and technicians, who did not have the personal protective equipment needed to prevent infection and spare risk to their loved ones. It soon extended to the country’s failure to adequately protect all its citizens and residents. COVID-19 then rained its grievous consequences disproportionately upon people of color, those living in poverty, and those with housing and food insecurity – those already greatly foreclosed from opportunities to exit from their circumstances.
We all have heard, “Fool me once, shame on you; fool me twice, shame on me.”
Bear witness, colleagues and friends: It will be our shared shame if we too continue to fail in our response to COVID-19. But failure need not happen because protecting ourselves and our country is a solvable problem; complex and demanding for sure, but solvable.
To battle trauma, we must first define it
The sine qua non of a disaster is its psychic and social trauma. I asked Maureen Sayres Van Niel, MD, chair of the American Psychiatric Association’s Minority and Underrepresented Caucus and a former steering committee member of the U.S. Preventive Services Task Force, to define trauma. She said, “It is [the product of] a catastrophic, unexpected event over which we have little control, with grave consequences to the lives and psychological functioning of those individuals and groups affected.”
The COVID-19 pandemic is a massively amplified traumatic event because of the virulence and contagious properties of the virus and its variants; the absence of end date on the horizon; its effect as a proverbial ax that disproportionately falls on the majority of the populace experiencing racial and social inequities; and the ironic yet necessary imperative to distance ourselves from those we care about and who care about us.
Four interdependent factors drive the magnitude of the traumatic impact of a disaster: the degree of exposure to the life-threatening event; the duration and threat of recurrence; an individual’s preexisting (natural and human-made) trauma and mental and addictive disorders; and the adequacy of family and fundamental resources such as housing, food, safety, and access to health care (the social dimensions of health and mental health). These factors underline the “who,” “what,” “where,” and “how” of what should have been (and continue to be) an effective public health response to the COVID-19 pandemic.
Yet existing categories that we have used to predict risk for trauma no longer hold. The gravity, prevalence, and persistence of COVID-19’s horrors erase any differences among victims, witnesses, and bystanders. Dr Sayres Van Niel asserts that we have a “collective, national trauma.” In April, the Kaiser Family Foundation’s Vaccine Monitor reported that 24% of U.S. adults had a close friend or family member who died of COVID-19. That’s 82 million Americans! Our country has eclipsed individual victimization and trauma because we are all in its maw.
Vital lessons from the past
In a previous column, I described my role as New York City’s mental health commissioner after 9/11 and the many lessons we learned during that multiyear process. Our work served as a template for other disasters to follow, such as Hurricane Sandy. Its value to COVID-19 is equally apparent.
We learned that those most at risk of developing symptomatic, functionally impairing mental illness had prior traumatic experiences (for example, from childhood abuse or neglect, violence, war, and forced displacement from their native land) and/or a preexisting mental or substance use disorder.
Once these individuals and communities were identified, we could prioritize their treatment and care. Doing so required mobilizing both inner and external (social) resources, which can be used before disaster strikes or in its wake.
For individuals, adaptive resources include developing any of a number of mind-body activities (for example, meditation, mindfulness, slow breathing, and yoga); sufficient but not necessarily excessive levels of exercise (as has been said, if exercise were a pill, it would be the most potent of medicines); nourishing diets; sleep, nature’s restorative state; and perhaps most important, attachment and human connection to people who care about you and whom you care about and trust.
This does not necessarily mean holding or following an institutional religion or belonging to house of worship (though, of course, that melds and augments faith with community). For a great many, myself included, there is spirituality, the belief in a greater power, which need not be a God yet instills a sense of the vastness, universality, and continuity of life.
For communities, adaptive resources include safe homes and neighborhoods; diminishing housing and food insecurity; education, including pre-K; employment, with a livable wage; ridding human interactions of the endless, so-called microaggressions (which are not micro at all, because they accrue) of race, ethnic, class, and age discrimination and injustice; and ready access to quality and affordable health care, now more than ever for the rising tide of mental and substance use disorders that COVID-19 has unleashed.
Every gain we make to ablate racism, social injustice, discrimination, and widely and deeply spread resource and opportunity inequities means more cohesion among the members of our collective tribe. Greater cohesion, a love for thy neighbor, and equity (in action, not polemics) will fuel the resilience we will need to withstand more of COVID-19’s ongoing trauma; that of other, inescapable disasters and losses; and the wear and tear of everyday life. The rewards of equity are priceless and include the dignity that derives from fairness and justice – given and received.
An unprecedented disaster requires a bold response
My, what a list. But to me, the encompassing nature of what’s needed means that we can make differences anywhere, everywhere, and in countless and continuous ways.
The measure of any society is in how it cares for those who are foreclosed, through no fault of their own, from what we all want: a life safe from violence, secure in housing and food, with loving relationships and the pride that comes of making contributions, each in our own, wonderfully unique way.
Where will we all be in a year, 2, or 3 from now? Prepared, or not? Emotionally inoculated, or not? Better equipped, or not? As divided, or more cohesive?
Well, I imagine that depends on each and every one of us.
Lloyd I. Sederer, MD, is a psychiatrist, public health doctor, and writer. He is an adjunct professor at the Columbia University School of Public Health, director of Columbia Psychiatry Media, chief medical officer of Bongo Media, and chair of the advisory board of Get Help. He has been chief medical officer of McLean Hospital, a Harvard teaching hospital; mental health commissioner of New York City (in the Bloomberg administration); and chief medical officer of the New York State Office of Mental Health, the nation’s largest state mental health agency.
A version of this article first appeared on Medscape.com.
Among asymptomatic, 2% may harbor 90% of community’s viral load: Study
About 2% of asymptomatic college students carried 90% of COVID-19 viral load levels on a Colorado campus last year, new research reveals. Furthermore, the viral loads in these students were as elevated as those seen in hospitalized patients.
“College campuses were one of the few places where people without any symptoms or suspicions of exposure were being screened for the virus. This allowed us to make some powerful comparisons between symptomatic vs healthy carriers of the virus,” senior study author Sara Sawyer, PhD, professor of virology at the University of Colorado, Boulder, said in an interview.
“It turns out, walking around a college campus can be as dangerous as walking through a COVID ward in the hospital, in that you will experience these viral ‘super carriers’ equally in both settings,” she said.
“This is an important study in advancing our understanding of how SARS-CoV-2 is distributed in the population,” Thomas Giordano, MD, MPH, professor and section chief of infectious diseases at Baylor College of Medicine, Houston, said in an interview.
The study “adds to the evidence that viral load is not too tightly correlated with symptoms.” In fact, Dr. Giordano added, “this study suggests viral load is not at all correlated with symptoms.”
Viral load may not be correlated with transmissibility either, said Raphael Viscidi, MD, when asked to comment. “This is not a transmissibility study. They did not show that viral load is the factor related to transmission.”
“It’s true that 2% of the population they studied carried 90% of the virus, but it does not establish any biological importance to that 2%,” added Dr. Viscidi, professor of pediatrics and oncology at Johns Hopkins University, Baltimore,.
The 2% could just be the upper tail end of a normal bell-shaped distribution curve, Dr. Viscidi said, or there could be something biologically unique about that group. But the study does not make that distinction, he said.
The study was published online May 10, 2021, in PNAS, the official journal of the National Academy of Sciences.
A similar picture in hospitalized patients
Out of more than 72,500 saliva samples taken during COVID-19 screening at the University of Colorado Boulder between Aug. 27 and Dec. 11, 2020, 1,405 were positive for SARS-CoV-2.
The investigators also compared viral loads from students with those of hospitalized patients based on published data. They found the distribution of viral loads between these groups “indistinguishable.”
“Strikingly, these datasets demonstrate dramatic differences in viral levels between individuals, with a very small minority of the infected individuals harboring the vast majority of the infectious virions,” the researchers wrote. The comparison “really represents two extremes: One group is mostly hospitalized, while the other group represents a mostly young and healthy (but infected) college population.”
“It would be interesting to adjust public health recommendations based on a person’s viral load,” Dr. Giordano said. “One could speculate that a person with a very high viral load could be isolated longer or more thoroughly, while someone with a very low viral load could be minimally isolated.
“This is speculation, and more data are needed to test this concept,” he added. Also, quantitative viral load testing would need to be standardized before it could be used to guide such decision-making
Preceding the COVID-19 vaccine era
It should be noted that the research was conducted in fall 2020, before access to COVID-19 immunization.
“The study was performed prior to vaccine availability in a cohort of young people. It adds further data to support prior observations that the majority of infections are spread by a much smaller group of individuals,” David Hirschwerk, MD, said in an interview.
“Now that vaccines are available, I think it is very likely that a repeat study of this type would show diminished transmission from vaccinated people who were infected yet asymptomatic,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in New Hyde Park, N.Y., who was not affiliated with the research.
Mechanism still a mystery
“This finding has been in the literature in piecemeal fashion since the beginning of the pandemic,” Dr. Sawyer said. “I just think we were the first to realize the bigger implications of these plots of viral load that we have all been seeing over and over again.”
How a minority of people walk around asymptomatic with a majority of virus remains unanswered. Are there special people who can harbor these extremely high viral loads? Or do many infected individuals experience a short period of time when they carry such elevated levels?
The highest observed viral load in the current study was more than 6 trillion virions per mL. “It is remarkable to consider that this individual was on campus and reported no symptoms at our testing site,” the researchers wrote.
In contrast, the lowest viral load detected was 8 virions per mL.
Although more research is needed, the investigators noted that “a strong implication is that these individuals who are viral ‘super carriers’ may also be ‘superspreaders.’ ”
Some of the study authors have financial ties to companies that offer commercial SARS-CoV-2 testing, including Darwin Biosciences, TUMI Genomics, Faze Medicines, and Arpeggio Biosciences.
A version of this article first appeared on Medscape.com.
About 2% of asymptomatic college students carried 90% of COVID-19 viral load levels on a Colorado campus last year, new research reveals. Furthermore, the viral loads in these students were as elevated as those seen in hospitalized patients.
“College campuses were one of the few places where people without any symptoms or suspicions of exposure were being screened for the virus. This allowed us to make some powerful comparisons between symptomatic vs healthy carriers of the virus,” senior study author Sara Sawyer, PhD, professor of virology at the University of Colorado, Boulder, said in an interview.
“It turns out, walking around a college campus can be as dangerous as walking through a COVID ward in the hospital, in that you will experience these viral ‘super carriers’ equally in both settings,” she said.
“This is an important study in advancing our understanding of how SARS-CoV-2 is distributed in the population,” Thomas Giordano, MD, MPH, professor and section chief of infectious diseases at Baylor College of Medicine, Houston, said in an interview.
The study “adds to the evidence that viral load is not too tightly correlated with symptoms.” In fact, Dr. Giordano added, “this study suggests viral load is not at all correlated with symptoms.”
Viral load may not be correlated with transmissibility either, said Raphael Viscidi, MD, when asked to comment. “This is not a transmissibility study. They did not show that viral load is the factor related to transmission.”
“It’s true that 2% of the population they studied carried 90% of the virus, but it does not establish any biological importance to that 2%,” added Dr. Viscidi, professor of pediatrics and oncology at Johns Hopkins University, Baltimore,.
The 2% could just be the upper tail end of a normal bell-shaped distribution curve, Dr. Viscidi said, or there could be something biologically unique about that group. But the study does not make that distinction, he said.
The study was published online May 10, 2021, in PNAS, the official journal of the National Academy of Sciences.
A similar picture in hospitalized patients
Out of more than 72,500 saliva samples taken during COVID-19 screening at the University of Colorado Boulder between Aug. 27 and Dec. 11, 2020, 1,405 were positive for SARS-CoV-2.
The investigators also compared viral loads from students with those of hospitalized patients based on published data. They found the distribution of viral loads between these groups “indistinguishable.”
“Strikingly, these datasets demonstrate dramatic differences in viral levels between individuals, with a very small minority of the infected individuals harboring the vast majority of the infectious virions,” the researchers wrote. The comparison “really represents two extremes: One group is mostly hospitalized, while the other group represents a mostly young and healthy (but infected) college population.”
“It would be interesting to adjust public health recommendations based on a person’s viral load,” Dr. Giordano said. “One could speculate that a person with a very high viral load could be isolated longer or more thoroughly, while someone with a very low viral load could be minimally isolated.
“This is speculation, and more data are needed to test this concept,” he added. Also, quantitative viral load testing would need to be standardized before it could be used to guide such decision-making
Preceding the COVID-19 vaccine era
It should be noted that the research was conducted in fall 2020, before access to COVID-19 immunization.
“The study was performed prior to vaccine availability in a cohort of young people. It adds further data to support prior observations that the majority of infections are spread by a much smaller group of individuals,” David Hirschwerk, MD, said in an interview.
“Now that vaccines are available, I think it is very likely that a repeat study of this type would show diminished transmission from vaccinated people who were infected yet asymptomatic,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in New Hyde Park, N.Y., who was not affiliated with the research.
Mechanism still a mystery
“This finding has been in the literature in piecemeal fashion since the beginning of the pandemic,” Dr. Sawyer said. “I just think we were the first to realize the bigger implications of these plots of viral load that we have all been seeing over and over again.”
How a minority of people walk around asymptomatic with a majority of virus remains unanswered. Are there special people who can harbor these extremely high viral loads? Or do many infected individuals experience a short period of time when they carry such elevated levels?
The highest observed viral load in the current study was more than 6 trillion virions per mL. “It is remarkable to consider that this individual was on campus and reported no symptoms at our testing site,” the researchers wrote.
In contrast, the lowest viral load detected was 8 virions per mL.
Although more research is needed, the investigators noted that “a strong implication is that these individuals who are viral ‘super carriers’ may also be ‘superspreaders.’ ”
Some of the study authors have financial ties to companies that offer commercial SARS-CoV-2 testing, including Darwin Biosciences, TUMI Genomics, Faze Medicines, and Arpeggio Biosciences.
A version of this article first appeared on Medscape.com.
About 2% of asymptomatic college students carried 90% of COVID-19 viral load levels on a Colorado campus last year, new research reveals. Furthermore, the viral loads in these students were as elevated as those seen in hospitalized patients.
“College campuses were one of the few places where people without any symptoms or suspicions of exposure were being screened for the virus. This allowed us to make some powerful comparisons between symptomatic vs healthy carriers of the virus,” senior study author Sara Sawyer, PhD, professor of virology at the University of Colorado, Boulder, said in an interview.
“It turns out, walking around a college campus can be as dangerous as walking through a COVID ward in the hospital, in that you will experience these viral ‘super carriers’ equally in both settings,” she said.
“This is an important study in advancing our understanding of how SARS-CoV-2 is distributed in the population,” Thomas Giordano, MD, MPH, professor and section chief of infectious diseases at Baylor College of Medicine, Houston, said in an interview.
The study “adds to the evidence that viral load is not too tightly correlated with symptoms.” In fact, Dr. Giordano added, “this study suggests viral load is not at all correlated with symptoms.”
Viral load may not be correlated with transmissibility either, said Raphael Viscidi, MD, when asked to comment. “This is not a transmissibility study. They did not show that viral load is the factor related to transmission.”
“It’s true that 2% of the population they studied carried 90% of the virus, but it does not establish any biological importance to that 2%,” added Dr. Viscidi, professor of pediatrics and oncology at Johns Hopkins University, Baltimore,.
The 2% could just be the upper tail end of a normal bell-shaped distribution curve, Dr. Viscidi said, or there could be something biologically unique about that group. But the study does not make that distinction, he said.
The study was published online May 10, 2021, in PNAS, the official journal of the National Academy of Sciences.
A similar picture in hospitalized patients
Out of more than 72,500 saliva samples taken during COVID-19 screening at the University of Colorado Boulder between Aug. 27 and Dec. 11, 2020, 1,405 were positive for SARS-CoV-2.
The investigators also compared viral loads from students with those of hospitalized patients based on published data. They found the distribution of viral loads between these groups “indistinguishable.”
“Strikingly, these datasets demonstrate dramatic differences in viral levels between individuals, with a very small minority of the infected individuals harboring the vast majority of the infectious virions,” the researchers wrote. The comparison “really represents two extremes: One group is mostly hospitalized, while the other group represents a mostly young and healthy (but infected) college population.”
“It would be interesting to adjust public health recommendations based on a person’s viral load,” Dr. Giordano said. “One could speculate that a person with a very high viral load could be isolated longer or more thoroughly, while someone with a very low viral load could be minimally isolated.
“This is speculation, and more data are needed to test this concept,” he added. Also, quantitative viral load testing would need to be standardized before it could be used to guide such decision-making
Preceding the COVID-19 vaccine era
It should be noted that the research was conducted in fall 2020, before access to COVID-19 immunization.
“The study was performed prior to vaccine availability in a cohort of young people. It adds further data to support prior observations that the majority of infections are spread by a much smaller group of individuals,” David Hirschwerk, MD, said in an interview.
“Now that vaccines are available, I think it is very likely that a repeat study of this type would show diminished transmission from vaccinated people who were infected yet asymptomatic,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in New Hyde Park, N.Y., who was not affiliated with the research.
Mechanism still a mystery
“This finding has been in the literature in piecemeal fashion since the beginning of the pandemic,” Dr. Sawyer said. “I just think we were the first to realize the bigger implications of these plots of viral load that we have all been seeing over and over again.”
How a minority of people walk around asymptomatic with a majority of virus remains unanswered. Are there special people who can harbor these extremely high viral loads? Or do many infected individuals experience a short period of time when they carry such elevated levels?
The highest observed viral load in the current study was more than 6 trillion virions per mL. “It is remarkable to consider that this individual was on campus and reported no symptoms at our testing site,” the researchers wrote.
In contrast, the lowest viral load detected was 8 virions per mL.
Although more research is needed, the investigators noted that “a strong implication is that these individuals who are viral ‘super carriers’ may also be ‘superspreaders.’ ”
Some of the study authors have financial ties to companies that offer commercial SARS-CoV-2 testing, including Darwin Biosciences, TUMI Genomics, Faze Medicines, and Arpeggio Biosciences.
A version of this article first appeared on Medscape.com.
Who is my neighbor? The ethics of sharing medical resources in the world
India is in a crisis as the burden of COVID-19 has collapsed parts of the health care system. There are not enough beds, not enough oxygen, and not enough crematoria to handle the pandemic. India is also a major supplier of vaccines for itself and many other countries. That production capacity has also been affected by the local events, further worsening the response to the pandemic over the next few months.
This collapse is the specter that, in April 2020, placed a hospital ship next to Manhattan and rows of beds in its convention center. Fortunately, the lockdown in March 2020 sufficiently flattened the curve. The city avoided utilizing that disaster capacity, though many New Yorkers died out of sight in nursing homes. When the third and largest wave of cases in the United States peaked in January 2021, hospitals throughout California reached capacity but avoided bursting. In April 2021, localized outbreaks in Michigan, Arizona, and Ontario again tested the maximum capacity for providing modern medical treatments. Great Britain used a second lockdown in October 2020 and a third in January 2021 to control the pandemic, with Prime Minister Boris Johnson emphasizing that it was these social interventions, and not vaccines, which provided the mitigating effects. Other European Union nations adopted similar strategies. Prudent choices by government guided by science, combined with the cooperation of the public, have been and still are crucial to mollify the pandemic.
There is hope that soon vaccines will return daily life to a new normal. In the United States, the Centers for Disease Control and Prevention has loosened restrictions on social gathering. An increase in daily new cases of COVID-19 in April 2021 has turned into just a blip before continuing to recede. Perhaps that is the first sign of vaccination working at the level of public health. However, the May 2021 lockdown in highly vaccinated Seychelles is a warning that the danger remains. A single match can start a huge forest fire. The first 150 million cases of COVID-19 worldwide have, through natural rates of mutation, produced several variants that might partially evade current vaccines. The danger of newer variants persists with the next 150 million cases as the pandemic continues to rage in many nations which are just one airplane ride away. All human inhabitants of this blue-covered third rock from the sun are interconnected.
The benefits of scientific advancement have been extolled for centuries. This includes both individual discoveries as well as a mindset that favors rationalism over fatalism. On the whole, the benefits of scientific progress outweigh the negatives. Negative environmental impacts include pollution and climate change. Economic impacts include raising the mean economic standard of living but with greater inequity. Historically, governmental and social institutions have attempted to mitigate these negative consequences. Those efforts have attempted to provide guidance and a moral compass to direct the progress of scientific advancement, particularly in fields like gene therapy. Those efforts have called upon developed nations to share the bounties of progress with other nations.
Modern medicine has provided the fruit of these scientific advancements to a limited fraction of the world’s population during the 20th century. The improvements in life expectancy and infant mortality have come primarily from civil engineers getting running water into cities and sewage out. A smaller portion of the benefits are from public health measures that reduced tuberculosis, smallpox, polio, and measles. Agriculture became more reliable, productive, and nutritious. In the 21st century, medical care (control of hypertension, diabetes, and clotting) aimed at reducing heart disease and strokes have added another 2-3 years to the life expectancy in the United States, with much of that benefit erased by the epidemics of obesity and opioid abuse.
Modern medical technology has created treatments that cost $10,000 a month to add a few extra months of life to geriatric patients with terminal cancer. Meanwhile, in more mundane care, efforts like Choosing Wisely seek to save money wasted on low-value, useless, and even harmful tests and therapies. There is no single person or agency managing this chaotic process of inventing expensive new technologies while inadequately addressing the widespread shortages of mental health care, disparities in education, and other social determinants of health. The pandemic has highlighted these preexisting weaknesses in the social fabric.
The cries from India have been accompanied by voices of anger from India and other nations accusing the United States of hoarding vaccines and the raw materials needed to produce them. This has been called vaccine apartheid. The United States is not alone in its political decision to prioritize domestic interests over international ones; India’s recent government is similarly nationalistic. Scientists warn that no one is safe locally as long as the pandemic rages in other countries. The Biden administration, in a delayed response to the crisis in India, finally announced plans to share some unused vaccines (of a brand not yet Food and Drug Administration approved) as well as some vaccine raw materials whose export was forbidden by a regulation under the Defense Production Act. Reading below the headlines, the promised response won’t be implemented for weeks or months. We must do better.
The logistics of sharing the benefits of advanced science are complicated. The ethics are not. Who is my neighbor? If you didn’t learn the answer to that in Sunday school, there isn’t much more I can say.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures, Email him at [email protected]
India is in a crisis as the burden of COVID-19 has collapsed parts of the health care system. There are not enough beds, not enough oxygen, and not enough crematoria to handle the pandemic. India is also a major supplier of vaccines for itself and many other countries. That production capacity has also been affected by the local events, further worsening the response to the pandemic over the next few months.
This collapse is the specter that, in April 2020, placed a hospital ship next to Manhattan and rows of beds in its convention center. Fortunately, the lockdown in March 2020 sufficiently flattened the curve. The city avoided utilizing that disaster capacity, though many New Yorkers died out of sight in nursing homes. When the third and largest wave of cases in the United States peaked in January 2021, hospitals throughout California reached capacity but avoided bursting. In April 2021, localized outbreaks in Michigan, Arizona, and Ontario again tested the maximum capacity for providing modern medical treatments. Great Britain used a second lockdown in October 2020 and a third in January 2021 to control the pandemic, with Prime Minister Boris Johnson emphasizing that it was these social interventions, and not vaccines, which provided the mitigating effects. Other European Union nations adopted similar strategies. Prudent choices by government guided by science, combined with the cooperation of the public, have been and still are crucial to mollify the pandemic.
There is hope that soon vaccines will return daily life to a new normal. In the United States, the Centers for Disease Control and Prevention has loosened restrictions on social gathering. An increase in daily new cases of COVID-19 in April 2021 has turned into just a blip before continuing to recede. Perhaps that is the first sign of vaccination working at the level of public health. However, the May 2021 lockdown in highly vaccinated Seychelles is a warning that the danger remains. A single match can start a huge forest fire. The first 150 million cases of COVID-19 worldwide have, through natural rates of mutation, produced several variants that might partially evade current vaccines. The danger of newer variants persists with the next 150 million cases as the pandemic continues to rage in many nations which are just one airplane ride away. All human inhabitants of this blue-covered third rock from the sun are interconnected.
The benefits of scientific advancement have been extolled for centuries. This includes both individual discoveries as well as a mindset that favors rationalism over fatalism. On the whole, the benefits of scientific progress outweigh the negatives. Negative environmental impacts include pollution and climate change. Economic impacts include raising the mean economic standard of living but with greater inequity. Historically, governmental and social institutions have attempted to mitigate these negative consequences. Those efforts have attempted to provide guidance and a moral compass to direct the progress of scientific advancement, particularly in fields like gene therapy. Those efforts have called upon developed nations to share the bounties of progress with other nations.
Modern medicine has provided the fruit of these scientific advancements to a limited fraction of the world’s population during the 20th century. The improvements in life expectancy and infant mortality have come primarily from civil engineers getting running water into cities and sewage out. A smaller portion of the benefits are from public health measures that reduced tuberculosis, smallpox, polio, and measles. Agriculture became more reliable, productive, and nutritious. In the 21st century, medical care (control of hypertension, diabetes, and clotting) aimed at reducing heart disease and strokes have added another 2-3 years to the life expectancy in the United States, with much of that benefit erased by the epidemics of obesity and opioid abuse.
Modern medical technology has created treatments that cost $10,000 a month to add a few extra months of life to geriatric patients with terminal cancer. Meanwhile, in more mundane care, efforts like Choosing Wisely seek to save money wasted on low-value, useless, and even harmful tests and therapies. There is no single person or agency managing this chaotic process of inventing expensive new technologies while inadequately addressing the widespread shortages of mental health care, disparities in education, and other social determinants of health. The pandemic has highlighted these preexisting weaknesses in the social fabric.
The cries from India have been accompanied by voices of anger from India and other nations accusing the United States of hoarding vaccines and the raw materials needed to produce them. This has been called vaccine apartheid. The United States is not alone in its political decision to prioritize domestic interests over international ones; India’s recent government is similarly nationalistic. Scientists warn that no one is safe locally as long as the pandemic rages in other countries. The Biden administration, in a delayed response to the crisis in India, finally announced plans to share some unused vaccines (of a brand not yet Food and Drug Administration approved) as well as some vaccine raw materials whose export was forbidden by a regulation under the Defense Production Act. Reading below the headlines, the promised response won’t be implemented for weeks or months. We must do better.
The logistics of sharing the benefits of advanced science are complicated. The ethics are not. Who is my neighbor? If you didn’t learn the answer to that in Sunday school, there isn’t much more I can say.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures, Email him at [email protected]
India is in a crisis as the burden of COVID-19 has collapsed parts of the health care system. There are not enough beds, not enough oxygen, and not enough crematoria to handle the pandemic. India is also a major supplier of vaccines for itself and many other countries. That production capacity has also been affected by the local events, further worsening the response to the pandemic over the next few months.
This collapse is the specter that, in April 2020, placed a hospital ship next to Manhattan and rows of beds in its convention center. Fortunately, the lockdown in March 2020 sufficiently flattened the curve. The city avoided utilizing that disaster capacity, though many New Yorkers died out of sight in nursing homes. When the third and largest wave of cases in the United States peaked in January 2021, hospitals throughout California reached capacity but avoided bursting. In April 2021, localized outbreaks in Michigan, Arizona, and Ontario again tested the maximum capacity for providing modern medical treatments. Great Britain used a second lockdown in October 2020 and a third in January 2021 to control the pandemic, with Prime Minister Boris Johnson emphasizing that it was these social interventions, and not vaccines, which provided the mitigating effects. Other European Union nations adopted similar strategies. Prudent choices by government guided by science, combined with the cooperation of the public, have been and still are crucial to mollify the pandemic.
There is hope that soon vaccines will return daily life to a new normal. In the United States, the Centers for Disease Control and Prevention has loosened restrictions on social gathering. An increase in daily new cases of COVID-19 in April 2021 has turned into just a blip before continuing to recede. Perhaps that is the first sign of vaccination working at the level of public health. However, the May 2021 lockdown in highly vaccinated Seychelles is a warning that the danger remains. A single match can start a huge forest fire. The first 150 million cases of COVID-19 worldwide have, through natural rates of mutation, produced several variants that might partially evade current vaccines. The danger of newer variants persists with the next 150 million cases as the pandemic continues to rage in many nations which are just one airplane ride away. All human inhabitants of this blue-covered third rock from the sun are interconnected.
The benefits of scientific advancement have been extolled for centuries. This includes both individual discoveries as well as a mindset that favors rationalism over fatalism. On the whole, the benefits of scientific progress outweigh the negatives. Negative environmental impacts include pollution and climate change. Economic impacts include raising the mean economic standard of living but with greater inequity. Historically, governmental and social institutions have attempted to mitigate these negative consequences. Those efforts have attempted to provide guidance and a moral compass to direct the progress of scientific advancement, particularly in fields like gene therapy. Those efforts have called upon developed nations to share the bounties of progress with other nations.
Modern medicine has provided the fruit of these scientific advancements to a limited fraction of the world’s population during the 20th century. The improvements in life expectancy and infant mortality have come primarily from civil engineers getting running water into cities and sewage out. A smaller portion of the benefits are from public health measures that reduced tuberculosis, smallpox, polio, and measles. Agriculture became more reliable, productive, and nutritious. In the 21st century, medical care (control of hypertension, diabetes, and clotting) aimed at reducing heart disease and strokes have added another 2-3 years to the life expectancy in the United States, with much of that benefit erased by the epidemics of obesity and opioid abuse.
Modern medical technology has created treatments that cost $10,000 a month to add a few extra months of life to geriatric patients with terminal cancer. Meanwhile, in more mundane care, efforts like Choosing Wisely seek to save money wasted on low-value, useless, and even harmful tests and therapies. There is no single person or agency managing this chaotic process of inventing expensive new technologies while inadequately addressing the widespread shortages of mental health care, disparities in education, and other social determinants of health. The pandemic has highlighted these preexisting weaknesses in the social fabric.
The cries from India have been accompanied by voices of anger from India and other nations accusing the United States of hoarding vaccines and the raw materials needed to produce them. This has been called vaccine apartheid. The United States is not alone in its political decision to prioritize domestic interests over international ones; India’s recent government is similarly nationalistic. Scientists warn that no one is safe locally as long as the pandemic rages in other countries. The Biden administration, in a delayed response to the crisis in India, finally announced plans to share some unused vaccines (of a brand not yet Food and Drug Administration approved) as well as some vaccine raw materials whose export was forbidden by a regulation under the Defense Production Act. Reading below the headlines, the promised response won’t be implemented for weeks or months. We must do better.
The logistics of sharing the benefits of advanced science are complicated. The ethics are not. Who is my neighbor? If you didn’t learn the answer to that in Sunday school, there isn’t much more I can say.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. He has no financial disclosures, Email him at [email protected]
COVID-19 in children and adolescents: Disease burden and severity
My first thought on this column was maybe Pediatric News has written sufficiently about SARS-CoV-2 infection, and it is time to move on. However, the agenda for the May 12th Advisory Committee on Immunization Practice includes a review of the Pfizer-BioNTech COVID-19 vaccine safety and immunogenicity data for the 12- to 15-year-old age cohort that suggests the potential for vaccine availability and roll out for early adolescents in the near future and the need for up-to-date knowledge about the incidence, severity, and long-term outcome of COVID-19 in the pediatric population.
Updating and summarizing the pediatric experience for the pediatric community on what children and adolescents have experienced because of SARS-CoV-2 infection is critical to address the myriad of questions that will come from colleagues, parents, and adolescents themselves. A great resource, published weekly, is the joint report from the American Academy of Pediatrics and the Children’s Hospital Association.1 As of April 29, 2021, 3,782,724 total child COVID-19 cases have been reported from 49 states, New York City (NYC), the District of Columbia, Guam, and Puerto Rico. Children represent approximately 14% of cases in the United States and not surprisingly are an increasing proportion of total cases as vaccine impact reduces cases among older age groups. Nearly 5% of the pediatric population has already been infected with SARS-CoV-2. Fortunately, compared with adults, hospitalization, severe disease, and mortality remain far lower both in number and proportion than in the adult population. Cumulative hospitalizations from 24 states and NYC total 15,456 (0.8%) among those infected, with 303 deaths reported (from 43 states, NYC, Guam, and Puerto Rico). Case fatality rate approximates 0.01% in the most recent summary of state reports. One of the limitations of this report is that each state decides how to report the age distribution of COVID-19 cases resulting in variation in age range; another is the data are limited to those details individual states chose to make publicly available.
Although children do not commonly develop severe disease, and the case fatality is low, there are still insights to be learned from understanding risk features for severe disease. Preston et al. reviewed discharge data from 869 medical facilities to describe patients 18 years or younger who had an inpatient or emergency department encounter with a primary or secondary COVID-19 discharge diagnosis from March 1 through October 31, 2020.2 They reported that approximately 2,430 (11.7%) children were hospitalized and 746, nearly 31% of those hospitalized, had severe COVID disease. Those at greatest risk for severe disease were children with comorbid conditions and those less than 12 years, compared with the 12- to 18-year age group. They did not identify race as a risk for severe disease in this study. Moreira et al. described risk factors for morbidity and death from COVID in children less than 18 years of age3 using CDC COVID-NET, the Centers for Disease Control and Prevention COVID-19–associated hospitalization surveillance network. They reported a hospitalization rate of 4.7% among 27,045 cases. They identified three risk factors for hospitalization – age, race/ethnicity, and comorbid conditions. Thirty-nine children (0.19%) died; children who were black, non-Hispanic, and those with an underlying medical condition had a significantly increased risk of death. Thirty-three (85%) children who died had a comorbidity, and 27 (69%) were African American or Hispanic/Latino. The U.S. experience in children is also consistent with reports from the United Kingdom, Italy, Spain, Germany, France, and South Korea.4 Deaths from COVID-19 were uncommon but relatively more frequent in older children, compared with younger age groups among children less than 18 years of age in these countries.
Acute COVID-19 and multisystem inflammatory syndrome in children (MIS-C) do not predominantly target the neurologic systems; however, neurologic complications have been reported, some of which appear to result in long-lasting disability. LaRovere et al. identified 354 (22%) of 1,695 patients less than 21 years of age with acute COVID or MIS-C who had neurologic signs or symptoms during their illness. Among those with neurologic involvement, most children had prior neurologic deficits, mild symptoms, that resolved by the time of discharge. Forty-three (12%) were considered life threatening and included severe encephalopathy, stroke, central nervous system infection/demyelination, Guillain-Barre syndrome or variant, or acute cerebral edema. Several children, including some who were previously healthy prior to COVID, had persistent neurologic deficits at discharge. In addition to neurologic morbidity, long COVID – a syndrome of persistent symptoms following acute COVID that lasts for more than 12 weeks without alternative diagnosis – has also been described in children. Buonsenso et al. assessed 129 children diagnosed with COVID-19 between March and November 2020 in Rome, Italy.5 Persisting symptoms after 120 days were reported by more than 50%. Symptoms like fatigue, muscle and joint pain, headache, insomnia, respiratory problems, and palpitations were most common. Clearly, further follow-up of the long-term outcomes is necessary to understand the full spectrum of morbidity resulting from COVID-19 disease in children and its natural history.
The current picture of COVID infection in children younger than 18 reinforces that children are part of the pandemic. Although deaths in children have now exceeded 300 cases, severe disease remains uncommon in both the United States and western Europe. Risk factors for severe disease include comorbid illness and race/ethnicity with a disproportionate number of severe cases in children with underlying comorbidity and in African American and Hispanic/Latino children. Ongoing surveillance is critical as changes are likely to be observed over time as viral evolution affects disease burden and characteristics.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University schools of medicine and public health and senior attending physician in pediatric infectious diseases, Boston Medical Center. Email him at [email protected].
References
1. Children and COVID-19: State-Level Data Report. Services AAP.org.
2. Preston LE et al. JAMA Network Open. 2021;4(4):e215298. doi:10.1001/jamanetworkopen.2021.5298
3. Moreira A et al. Eur J Pediatr. 2021;180:1659-63.
4. SS Bhopal et al. Lancet 2021. doi: 10.1016/ S2352-4642(21)00066-3.
5. Buonsenso D et al. medRxiv preprint. doi: 10.1101/2021.01.23.21250375.
My first thought on this column was maybe Pediatric News has written sufficiently about SARS-CoV-2 infection, and it is time to move on. However, the agenda for the May 12th Advisory Committee on Immunization Practice includes a review of the Pfizer-BioNTech COVID-19 vaccine safety and immunogenicity data for the 12- to 15-year-old age cohort that suggests the potential for vaccine availability and roll out for early adolescents in the near future and the need for up-to-date knowledge about the incidence, severity, and long-term outcome of COVID-19 in the pediatric population.
Updating and summarizing the pediatric experience for the pediatric community on what children and adolescents have experienced because of SARS-CoV-2 infection is critical to address the myriad of questions that will come from colleagues, parents, and adolescents themselves. A great resource, published weekly, is the joint report from the American Academy of Pediatrics and the Children’s Hospital Association.1 As of April 29, 2021, 3,782,724 total child COVID-19 cases have been reported from 49 states, New York City (NYC), the District of Columbia, Guam, and Puerto Rico. Children represent approximately 14% of cases in the United States and not surprisingly are an increasing proportion of total cases as vaccine impact reduces cases among older age groups. Nearly 5% of the pediatric population has already been infected with SARS-CoV-2. Fortunately, compared with adults, hospitalization, severe disease, and mortality remain far lower both in number and proportion than in the adult population. Cumulative hospitalizations from 24 states and NYC total 15,456 (0.8%) among those infected, with 303 deaths reported (from 43 states, NYC, Guam, and Puerto Rico). Case fatality rate approximates 0.01% in the most recent summary of state reports. One of the limitations of this report is that each state decides how to report the age distribution of COVID-19 cases resulting in variation in age range; another is the data are limited to those details individual states chose to make publicly available.
Although children do not commonly develop severe disease, and the case fatality is low, there are still insights to be learned from understanding risk features for severe disease. Preston et al. reviewed discharge data from 869 medical facilities to describe patients 18 years or younger who had an inpatient or emergency department encounter with a primary or secondary COVID-19 discharge diagnosis from March 1 through October 31, 2020.2 They reported that approximately 2,430 (11.7%) children were hospitalized and 746, nearly 31% of those hospitalized, had severe COVID disease. Those at greatest risk for severe disease were children with comorbid conditions and those less than 12 years, compared with the 12- to 18-year age group. They did not identify race as a risk for severe disease in this study. Moreira et al. described risk factors for morbidity and death from COVID in children less than 18 years of age3 using CDC COVID-NET, the Centers for Disease Control and Prevention COVID-19–associated hospitalization surveillance network. They reported a hospitalization rate of 4.7% among 27,045 cases. They identified three risk factors for hospitalization – age, race/ethnicity, and comorbid conditions. Thirty-nine children (0.19%) died; children who were black, non-Hispanic, and those with an underlying medical condition had a significantly increased risk of death. Thirty-three (85%) children who died had a comorbidity, and 27 (69%) were African American or Hispanic/Latino. The U.S. experience in children is also consistent with reports from the United Kingdom, Italy, Spain, Germany, France, and South Korea.4 Deaths from COVID-19 were uncommon but relatively more frequent in older children, compared with younger age groups among children less than 18 years of age in these countries.
Acute COVID-19 and multisystem inflammatory syndrome in children (MIS-C) do not predominantly target the neurologic systems; however, neurologic complications have been reported, some of which appear to result in long-lasting disability. LaRovere et al. identified 354 (22%) of 1,695 patients less than 21 years of age with acute COVID or MIS-C who had neurologic signs or symptoms during their illness. Among those with neurologic involvement, most children had prior neurologic deficits, mild symptoms, that resolved by the time of discharge. Forty-three (12%) were considered life threatening and included severe encephalopathy, stroke, central nervous system infection/demyelination, Guillain-Barre syndrome or variant, or acute cerebral edema. Several children, including some who were previously healthy prior to COVID, had persistent neurologic deficits at discharge. In addition to neurologic morbidity, long COVID – a syndrome of persistent symptoms following acute COVID that lasts for more than 12 weeks without alternative diagnosis – has also been described in children. Buonsenso et al. assessed 129 children diagnosed with COVID-19 between March and November 2020 in Rome, Italy.5 Persisting symptoms after 120 days were reported by more than 50%. Symptoms like fatigue, muscle and joint pain, headache, insomnia, respiratory problems, and palpitations were most common. Clearly, further follow-up of the long-term outcomes is necessary to understand the full spectrum of morbidity resulting from COVID-19 disease in children and its natural history.
The current picture of COVID infection in children younger than 18 reinforces that children are part of the pandemic. Although deaths in children have now exceeded 300 cases, severe disease remains uncommon in both the United States and western Europe. Risk factors for severe disease include comorbid illness and race/ethnicity with a disproportionate number of severe cases in children with underlying comorbidity and in African American and Hispanic/Latino children. Ongoing surveillance is critical as changes are likely to be observed over time as viral evolution affects disease burden and characteristics.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University schools of medicine and public health and senior attending physician in pediatric infectious diseases, Boston Medical Center. Email him at [email protected].
References
1. Children and COVID-19: State-Level Data Report. Services AAP.org.
2. Preston LE et al. JAMA Network Open. 2021;4(4):e215298. doi:10.1001/jamanetworkopen.2021.5298
3. Moreira A et al. Eur J Pediatr. 2021;180:1659-63.
4. SS Bhopal et al. Lancet 2021. doi: 10.1016/ S2352-4642(21)00066-3.
5. Buonsenso D et al. medRxiv preprint. doi: 10.1101/2021.01.23.21250375.
My first thought on this column was maybe Pediatric News has written sufficiently about SARS-CoV-2 infection, and it is time to move on. However, the agenda for the May 12th Advisory Committee on Immunization Practice includes a review of the Pfizer-BioNTech COVID-19 vaccine safety and immunogenicity data for the 12- to 15-year-old age cohort that suggests the potential for vaccine availability and roll out for early adolescents in the near future and the need for up-to-date knowledge about the incidence, severity, and long-term outcome of COVID-19 in the pediatric population.
Updating and summarizing the pediatric experience for the pediatric community on what children and adolescents have experienced because of SARS-CoV-2 infection is critical to address the myriad of questions that will come from colleagues, parents, and adolescents themselves. A great resource, published weekly, is the joint report from the American Academy of Pediatrics and the Children’s Hospital Association.1 As of April 29, 2021, 3,782,724 total child COVID-19 cases have been reported from 49 states, New York City (NYC), the District of Columbia, Guam, and Puerto Rico. Children represent approximately 14% of cases in the United States and not surprisingly are an increasing proportion of total cases as vaccine impact reduces cases among older age groups. Nearly 5% of the pediatric population has already been infected with SARS-CoV-2. Fortunately, compared with adults, hospitalization, severe disease, and mortality remain far lower both in number and proportion than in the adult population. Cumulative hospitalizations from 24 states and NYC total 15,456 (0.8%) among those infected, with 303 deaths reported (from 43 states, NYC, Guam, and Puerto Rico). Case fatality rate approximates 0.01% in the most recent summary of state reports. One of the limitations of this report is that each state decides how to report the age distribution of COVID-19 cases resulting in variation in age range; another is the data are limited to those details individual states chose to make publicly available.
Although children do not commonly develop severe disease, and the case fatality is low, there are still insights to be learned from understanding risk features for severe disease. Preston et al. reviewed discharge data from 869 medical facilities to describe patients 18 years or younger who had an inpatient or emergency department encounter with a primary or secondary COVID-19 discharge diagnosis from March 1 through October 31, 2020.2 They reported that approximately 2,430 (11.7%) children were hospitalized and 746, nearly 31% of those hospitalized, had severe COVID disease. Those at greatest risk for severe disease were children with comorbid conditions and those less than 12 years, compared with the 12- to 18-year age group. They did not identify race as a risk for severe disease in this study. Moreira et al. described risk factors for morbidity and death from COVID in children less than 18 years of age3 using CDC COVID-NET, the Centers for Disease Control and Prevention COVID-19–associated hospitalization surveillance network. They reported a hospitalization rate of 4.7% among 27,045 cases. They identified three risk factors for hospitalization – age, race/ethnicity, and comorbid conditions. Thirty-nine children (0.19%) died; children who were black, non-Hispanic, and those with an underlying medical condition had a significantly increased risk of death. Thirty-three (85%) children who died had a comorbidity, and 27 (69%) were African American or Hispanic/Latino. The U.S. experience in children is also consistent with reports from the United Kingdom, Italy, Spain, Germany, France, and South Korea.4 Deaths from COVID-19 were uncommon but relatively more frequent in older children, compared with younger age groups among children less than 18 years of age in these countries.
Acute COVID-19 and multisystem inflammatory syndrome in children (MIS-C) do not predominantly target the neurologic systems; however, neurologic complications have been reported, some of which appear to result in long-lasting disability. LaRovere et al. identified 354 (22%) of 1,695 patients less than 21 years of age with acute COVID or MIS-C who had neurologic signs or symptoms during their illness. Among those with neurologic involvement, most children had prior neurologic deficits, mild symptoms, that resolved by the time of discharge. Forty-three (12%) were considered life threatening and included severe encephalopathy, stroke, central nervous system infection/demyelination, Guillain-Barre syndrome or variant, or acute cerebral edema. Several children, including some who were previously healthy prior to COVID, had persistent neurologic deficits at discharge. In addition to neurologic morbidity, long COVID – a syndrome of persistent symptoms following acute COVID that lasts for more than 12 weeks without alternative diagnosis – has also been described in children. Buonsenso et al. assessed 129 children diagnosed with COVID-19 between March and November 2020 in Rome, Italy.5 Persisting symptoms after 120 days were reported by more than 50%. Symptoms like fatigue, muscle and joint pain, headache, insomnia, respiratory problems, and palpitations were most common. Clearly, further follow-up of the long-term outcomes is necessary to understand the full spectrum of morbidity resulting from COVID-19 disease in children and its natural history.
The current picture of COVID infection in children younger than 18 reinforces that children are part of the pandemic. Although deaths in children have now exceeded 300 cases, severe disease remains uncommon in both the United States and western Europe. Risk factors for severe disease include comorbid illness and race/ethnicity with a disproportionate number of severe cases in children with underlying comorbidity and in African American and Hispanic/Latino children. Ongoing surveillance is critical as changes are likely to be observed over time as viral evolution affects disease burden and characteristics.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University schools of medicine and public health and senior attending physician in pediatric infectious diseases, Boston Medical Center. Email him at [email protected].
References
1. Children and COVID-19: State-Level Data Report. Services AAP.org.
2. Preston LE et al. JAMA Network Open. 2021;4(4):e215298. doi:10.1001/jamanetworkopen.2021.5298
3. Moreira A et al. Eur J Pediatr. 2021;180:1659-63.
4. SS Bhopal et al. Lancet 2021. doi: 10.1016/ S2352-4642(21)00066-3.
5. Buonsenso D et al. medRxiv preprint. doi: 10.1101/2021.01.23.21250375.
CDC: Vaccinated? You don’t need a mask indoors
the CDC announced on May 13.
“Anyone who is fully vaccinated can participate in indoor and outdoor activities, large or small, without wearing a mask or physically distancing,” CDC director Rochelle Walensky, MD, said at a press briefing. “We have all longed for this moment when we can get back to some sense of normalcy.
“This is an exciting and powerful moment,” she added, “It could only happen because of the work from so many who made sure we had the rapid administration of three safe and effective vaccines.”
Dr. Walensky cited three large studies on the effectiveness of COVID-19 vaccines against the original virus and its variants. One study from Israel found the vaccine to be 97% effective against symptomatic infection.
Those who are symptomatic should still wear masks, Dr. Walensky said, and those who are immunocompromised should talk to their doctors for further guidance. The CDC still advises travelers to wear masks while on airplanes or trains.
The COVID-19 death rates are now the lowest they have been since April 2020.
A version of this article first appeared on Medscape.com.
the CDC announced on May 13.
“Anyone who is fully vaccinated can participate in indoor and outdoor activities, large or small, without wearing a mask or physically distancing,” CDC director Rochelle Walensky, MD, said at a press briefing. “We have all longed for this moment when we can get back to some sense of normalcy.
“This is an exciting and powerful moment,” she added, “It could only happen because of the work from so many who made sure we had the rapid administration of three safe and effective vaccines.”
Dr. Walensky cited three large studies on the effectiveness of COVID-19 vaccines against the original virus and its variants. One study from Israel found the vaccine to be 97% effective against symptomatic infection.
Those who are symptomatic should still wear masks, Dr. Walensky said, and those who are immunocompromised should talk to their doctors for further guidance. The CDC still advises travelers to wear masks while on airplanes or trains.
The COVID-19 death rates are now the lowest they have been since April 2020.
A version of this article first appeared on Medscape.com.
the CDC announced on May 13.
“Anyone who is fully vaccinated can participate in indoor and outdoor activities, large or small, without wearing a mask or physically distancing,” CDC director Rochelle Walensky, MD, said at a press briefing. “We have all longed for this moment when we can get back to some sense of normalcy.
“This is an exciting and powerful moment,” she added, “It could only happen because of the work from so many who made sure we had the rapid administration of three safe and effective vaccines.”
Dr. Walensky cited three large studies on the effectiveness of COVID-19 vaccines against the original virus and its variants. One study from Israel found the vaccine to be 97% effective against symptomatic infection.
Those who are symptomatic should still wear masks, Dr. Walensky said, and those who are immunocompromised should talk to their doctors for further guidance. The CDC still advises travelers to wear masks while on airplanes or trains.
The COVID-19 death rates are now the lowest they have been since April 2020.
A version of this article first appeared on Medscape.com.
Trends in hospital medicine program operations during COVID-19
Staffing was a challenge for most groups
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.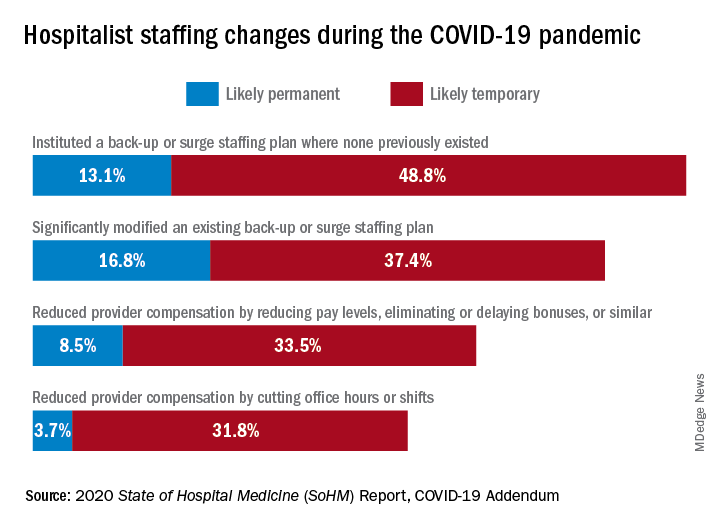
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
Staffing was a challenge for most groups
Staffing was a challenge for most groups
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.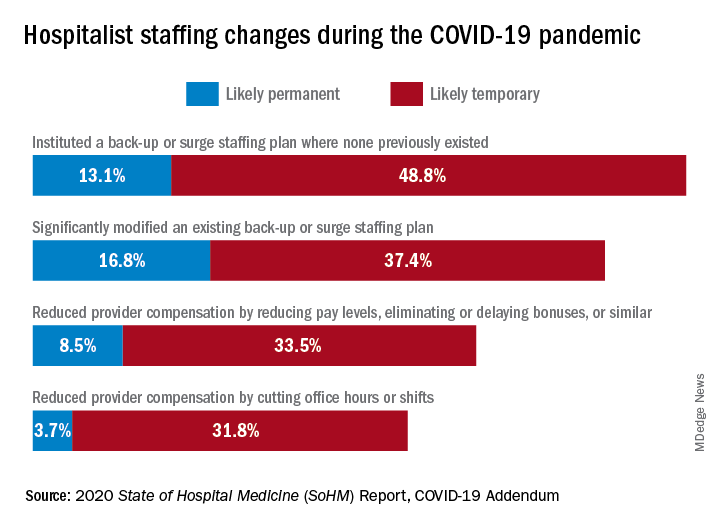
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.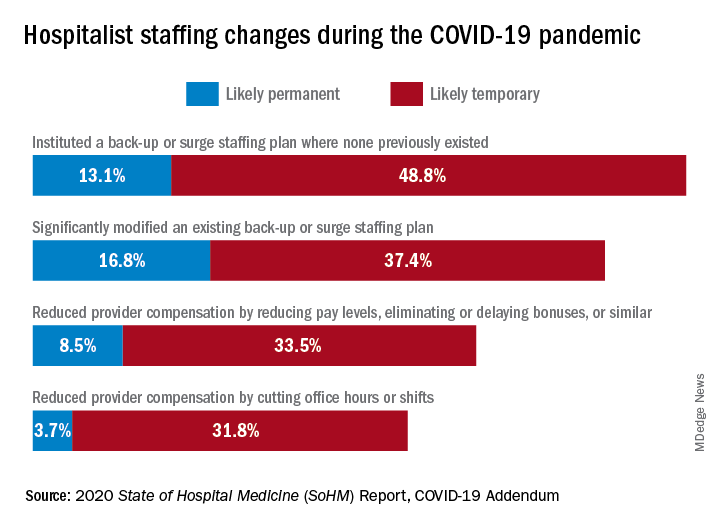
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
Canned diabetes prevention and a haunted COVID castle
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
Lower blood sugar with sardines
If you’ve ever turned your nose up at someone eating sardines straight from the can, you could be the one missing out on a good way to boost your own health.
New research from Open University of Catalonia (Spain) has found that eating two cans of whole sardines a week can help prevent people from developing type 2 diabetes (T2D). Now you might be thinking: That’s a lot of fish, can’t I just take a supplement pill? Actually, no.
“Nutrients can play an essential role in the prevention and treatment of many different pathologies, but their effect is usually caused by the synergy that exists between them and the food that they are contained in,” study coauthor Diana Rizzolo, PhD, said in a written statement. See, we told you.
In a study of 152 patients with prediabetes, each participant was put on a specific diet to reduce their chances of developing T2D. Among the patients who were not given sardines each week, the proportion considered to be at the highest risk fell from 27% to 22% after 1 year, but for those who did get the sardines, the size of the high-risk group shrank from 37% to just 8%.
Suggesting sardines during checkups could make eating them more widely accepted, Dr. Rizzolo and associates said. Sardines are cheap, easy to find, and also have the benefits of other oily fish, like boosting insulin resistance and increasing good cholesterol.
So why not have a can with a couple of saltine crackers for lunch? Your blood sugar will thank you. Just please avoid indulging on a plane or in your office, where workers are slowly returning – no need to give them another excuse to avoid their cubicle.
Come for the torture, stay for the vaccine
Bran Castle. Home of Dracula and Vlad the Impaler (at least in pop culture’s eyes). A moody Gothic structure atop a hill. You can practically hear the ancient screams of thousands of tortured souls as you wander the grounds and its cursed halls. Naturally, it’s a major tourist destination.
Unfortunately for Romania, the pandemic has rather put a damper on tourism. The restrictions have done their damage, but here’s a quick LOTME theory: Perhaps people don’t want to be reminded of medieval tortures when we’ve got plenty of modern-day ones right now.
The management of Bran Castle has developed a new gimmick to drum up attendance – come to Bran Castle and get your COVID vaccine. Anyone can come and get jabbed with the Pfizer vaccine on all weekends in May, and when they do, they gain free admittance to the castle and the exhibit within, home to 52 medieval torture instruments. “The idea … was to show how people got jabbed 500-600 years ago in Europe,” the castle’s marketing director said.
While it may not be kind of the jabbing ole Vladdy got his name for – fully impaling people on hundreds of wooden stakes while you eat a nice dinner isn’t exactly smiled upon in today’s world – we’re sure he’d approve of this more limited but ultimately beneficial version. Jabbing people while helping them really is the dream.
Fuzzy little COVID detectors
Before we get started, we need a moment to get our deep, movie trailer announcer-type voice ready. Okay, here goes.
“In a world where an organism too tiny to see brings entire economies to a standstill and pits scientists against doofuses, who can humanity turn to for help?”
How about bees? That’s right, we said bees. But not just any bees. Specially trained bees. Specially trained Dutch bees. Bees trained to sniff out our greatest nemesis. No, we’re not talking about Ted Cruz anymore. Let it go, that was just a joke. We’re talking COVID.
We’ll let Wim van der Poel, professor of virology at Wageningen (the Netherlands) University, explain the process: “We collect normal honeybees from a beekeeper, and we put the bees in harnesses.” And you thought their tulips were pretty great – the Dutch are putting harnesses on bees! (Which is much better than our previous story of bees involving a Taiwanese patient.)
The researchers presented the bees with two types of samples: COVID infected and non–COVID infected. The infected samples came with a sugary water reward and the noninfected samples did not, so the bees quickly learned to tell the difference.
The bees, then, could cut the waiting time for test results down to seconds, and at a fraction of the cost, making them an option in countries without a lot of testing infrastructure, the research team suggested.
The plan is not without its flaws, of course, but we’re convinced. More than that, we are true bee-lievers.
A little slice of … well, not heaven
If you’ve been around for the last 2 decades, you’ve seen your share of Internet trends: Remember the ice bucket challenge? Tide pod eating? We know what you’re thinking: Sigh, what could they be doing now?
Well, people are eating old meat, and before you think about the expired ground beef you got on special from the grocery store yesterday, that’s not quite what we mean. We all know expiration dates are “suggestions,” like yield signs and yellow lights. People are eating rotten, decomposing, borderline moldy meat.
They claim that the meat tastes better. We’re not so sure, but don’t worry, because it gets weirder. Some folks, apparently, are getting high from eating this meat, experiencing a feeling of euphoria. Personally, we think that rotten fumes probably knocked these people out and made them hallucinate.
Singaporean dietitian Naras Lapsys says that eating rotten meat can possibly cause a person to go into another state of consciousness, but it’s not a good thing. We don’t think you have to be a dietitian to know that.
It has not been definitively proven that eating rotting meat makes you high, but it’s definitely proven that this is disgusting … and very dangerous.
CDC recommends use of Pfizer’s COVID vaccine in 12- to 15-year-olds
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.













