User login
More evidence links COVID vaccines to rare cases of myocarditis in youth
a Centers for Disease Control and Prevention expert reported on June 10, detailing data on cases of myocarditis and pericarditis detected through a government safety system.
The side effect seems to be more common in teen boys and young men than in older adults and women and may occur in 16 cases for every 1 million people who got a second dose, said Tom Shimabukuro, MD, MPH, deputy director of the CDC’s Immunization Safety Office, who presented information on the cases at a meeting of an expert panel that advises the U.S. Food and Drug Administration on vaccines.
Telltale symptoms include chest pain, shortness of breath, and fever.
William Schaffner, MD, an infectious diseases specialist from Vanderbilt University, Nashville, Tenn., thinks certain characteristics are pointing toward a “rare, but real” signal. First, the events are clustering, occurring within days of vaccination. Second, they tend to be more common in males and younger people. Third, he says, the number of events is above the so-called “background rate” – the cases that could be expected in this age group even without vaccination.
“I don’t think we’re quite there yet. We haven’t tied a ribbon around it, but I think the data are trending in that direction,” he said.
The issue of myocarditis weighed heavily on the Vaccines and Related Biological Products Advisory Committee’s considerations of what kind and how much data might be needed to green light use of a vaccine for COVID in children.
Because the rates of hospitalization for COVID are low in kids, some felt that the FDA should require at least a year of study of the vaccines in clinical trials, the amount of data typically required for full approval, instead of the 2 months currently required for emergency use authorization. Others wondered whether the risks of vaccination – as low as they are – might outweigh the benefits in this age group.
“I don’t really see this as an emergency in children,” said committee member Michael Kurilla, MD, PhD, the director of clinical innovation at the National Institutes of Health. Dr. Kurilla, however, did say he thought having an expanded access program for children at high risk might make sense.
Most of the young adults who experienced myocarditis recovered quickly, though three needed intensive care and rehabilitation after their episodes. Among cases with known outcomes, 81% got better and 19% still have ongoing symptoms.
Adverse events reports
The data on myocarditis come from the Vaccine Adverse Events Reporting System, or VAERS, a database of health problems reported after vaccination. This reporting system, open to anyone, has benefits and limits. It gives the CDC and FDA the ability to rapidly detect potential safety issues, and it is large enough that it can detect rare events, something that’s beyond the power of even large clinical trials.
But it is observational, so that there’s no way to know if problems reported were caused by the vaccines or a coincidence.
But because VAERS works on an honor system, it can also be spammed, and it carries the bias of the person who’s doing the reporting, from clinicians to average patients. For that reason, Dr. Shimabukuro said they are actively investigating and confirming each report they get.
Out of more than 12 million doses administered to youth ages 16-24, the CDC says it has 275 reports of heart inflammation following vaccination in this age group. The CDC has analyzed a total 475 cases of myocarditis after vaccination in people under age 30 that were reported to VAERS.
The vaccines linked to the events are the mRNA vaccines made by Pfizer and Moderna. The only vaccines currently authorized for use in adolescents are made by Pfizer. Because the Pfizer vaccine was authorized for use in kids as young as 12 last month, there’s not yet enough data to draw conclusions about the risk of myocarditis in kids ages 12-15.
Younger age groups have only received about 9% of the total doses of the vaccine so far, but they represent about 50% of the myocarditis cases reported after vaccination. “We clearly have an imbalance there,” Dr. Shimabukuro said.
The number of events in this age group appears to be above the rate that would be expected for these age groups without vaccines in the picture, he said, explaining that the number of events are in line with similar adverse events seen in young people in Israel and reported by the Department of Defense. Israel found the incidence of myocarditis after vaccination was 50 cases per million for men ages 18-30.
More study needed
Another system tracking adverse events through hospitals, the Vaccine Safety Datalink, didn’t show reports of heart inflammation above numbers that are normally seen in the population, but it did show that inflammation was more likely after a second dose of the vaccine.
“Should this be included in informed consent?” asked Cody Meissner, MD, a pediatric infectious disease specialist at Tufts University, Boston, and a member of the FDA committee.
“I think it’s hard to deny there seem to be some [events that seem] to be occurring in terms of myocarditis,” he said.
Dr. Meissner said later in the committee’s discussion that his own hospital had recently admitted a 12-year-old boy who developed heart swelling 2 days after the second dose of vaccine with a high level of troponin, an enzyme that indicates damage to the heart. His level was over 9. “A very high level,” Dr. Meissner said.
“Will there be scarring to the myocardium? Will there be a predisposition to arrhythmias later on? Will there be an early onset of heart failure? We think that’s unlikely, but [we] don’t know that,” he said.
The CDC has scheduled an emergency meeting next week to convene an expert panel on immunization practices to further review the events.
In addition to the information presented at the FDA’s meeting, doctors at Oregon Health & Science University, Portland, recently described seven cases in teens – all boys – who developed heart inflammation within 4 days of getting the second dose of the Pfizer vaccine.
The study was published June 10 in Pediatrics. All the boys were hospitalized and treated with anti-inflammatory medications including NSAIDs and steroids. Most were discharged within a few days and all recovered from their symptoms.
A version of this article first appeared on Medscape.com.
a Centers for Disease Control and Prevention expert reported on June 10, detailing data on cases of myocarditis and pericarditis detected through a government safety system.
The side effect seems to be more common in teen boys and young men than in older adults and women and may occur in 16 cases for every 1 million people who got a second dose, said Tom Shimabukuro, MD, MPH, deputy director of the CDC’s Immunization Safety Office, who presented information on the cases at a meeting of an expert panel that advises the U.S. Food and Drug Administration on vaccines.
Telltale symptoms include chest pain, shortness of breath, and fever.
William Schaffner, MD, an infectious diseases specialist from Vanderbilt University, Nashville, Tenn., thinks certain characteristics are pointing toward a “rare, but real” signal. First, the events are clustering, occurring within days of vaccination. Second, they tend to be more common in males and younger people. Third, he says, the number of events is above the so-called “background rate” – the cases that could be expected in this age group even without vaccination.
“I don’t think we’re quite there yet. We haven’t tied a ribbon around it, but I think the data are trending in that direction,” he said.
The issue of myocarditis weighed heavily on the Vaccines and Related Biological Products Advisory Committee’s considerations of what kind and how much data might be needed to green light use of a vaccine for COVID in children.
Because the rates of hospitalization for COVID are low in kids, some felt that the FDA should require at least a year of study of the vaccines in clinical trials, the amount of data typically required for full approval, instead of the 2 months currently required for emergency use authorization. Others wondered whether the risks of vaccination – as low as they are – might outweigh the benefits in this age group.
“I don’t really see this as an emergency in children,” said committee member Michael Kurilla, MD, PhD, the director of clinical innovation at the National Institutes of Health. Dr. Kurilla, however, did say he thought having an expanded access program for children at high risk might make sense.
Most of the young adults who experienced myocarditis recovered quickly, though three needed intensive care and rehabilitation after their episodes. Among cases with known outcomes, 81% got better and 19% still have ongoing symptoms.
Adverse events reports
The data on myocarditis come from the Vaccine Adverse Events Reporting System, or VAERS, a database of health problems reported after vaccination. This reporting system, open to anyone, has benefits and limits. It gives the CDC and FDA the ability to rapidly detect potential safety issues, and it is large enough that it can detect rare events, something that’s beyond the power of even large clinical trials.
But it is observational, so that there’s no way to know if problems reported were caused by the vaccines or a coincidence.
But because VAERS works on an honor system, it can also be spammed, and it carries the bias of the person who’s doing the reporting, from clinicians to average patients. For that reason, Dr. Shimabukuro said they are actively investigating and confirming each report they get.
Out of more than 12 million doses administered to youth ages 16-24, the CDC says it has 275 reports of heart inflammation following vaccination in this age group. The CDC has analyzed a total 475 cases of myocarditis after vaccination in people under age 30 that were reported to VAERS.
The vaccines linked to the events are the mRNA vaccines made by Pfizer and Moderna. The only vaccines currently authorized for use in adolescents are made by Pfizer. Because the Pfizer vaccine was authorized for use in kids as young as 12 last month, there’s not yet enough data to draw conclusions about the risk of myocarditis in kids ages 12-15.
Younger age groups have only received about 9% of the total doses of the vaccine so far, but they represent about 50% of the myocarditis cases reported after vaccination. “We clearly have an imbalance there,” Dr. Shimabukuro said.
The number of events in this age group appears to be above the rate that would be expected for these age groups without vaccines in the picture, he said, explaining that the number of events are in line with similar adverse events seen in young people in Israel and reported by the Department of Defense. Israel found the incidence of myocarditis after vaccination was 50 cases per million for men ages 18-30.
More study needed
Another system tracking adverse events through hospitals, the Vaccine Safety Datalink, didn’t show reports of heart inflammation above numbers that are normally seen in the population, but it did show that inflammation was more likely after a second dose of the vaccine.
“Should this be included in informed consent?” asked Cody Meissner, MD, a pediatric infectious disease specialist at Tufts University, Boston, and a member of the FDA committee.
“I think it’s hard to deny there seem to be some [events that seem] to be occurring in terms of myocarditis,” he said.
Dr. Meissner said later in the committee’s discussion that his own hospital had recently admitted a 12-year-old boy who developed heart swelling 2 days after the second dose of vaccine with a high level of troponin, an enzyme that indicates damage to the heart. His level was over 9. “A very high level,” Dr. Meissner said.
“Will there be scarring to the myocardium? Will there be a predisposition to arrhythmias later on? Will there be an early onset of heart failure? We think that’s unlikely, but [we] don’t know that,” he said.
The CDC has scheduled an emergency meeting next week to convene an expert panel on immunization practices to further review the events.
In addition to the information presented at the FDA’s meeting, doctors at Oregon Health & Science University, Portland, recently described seven cases in teens – all boys – who developed heart inflammation within 4 days of getting the second dose of the Pfizer vaccine.
The study was published June 10 in Pediatrics. All the boys were hospitalized and treated with anti-inflammatory medications including NSAIDs and steroids. Most were discharged within a few days and all recovered from their symptoms.
A version of this article first appeared on Medscape.com.
a Centers for Disease Control and Prevention expert reported on June 10, detailing data on cases of myocarditis and pericarditis detected through a government safety system.
The side effect seems to be more common in teen boys and young men than in older adults and women and may occur in 16 cases for every 1 million people who got a second dose, said Tom Shimabukuro, MD, MPH, deputy director of the CDC’s Immunization Safety Office, who presented information on the cases at a meeting of an expert panel that advises the U.S. Food and Drug Administration on vaccines.
Telltale symptoms include chest pain, shortness of breath, and fever.
William Schaffner, MD, an infectious diseases specialist from Vanderbilt University, Nashville, Tenn., thinks certain characteristics are pointing toward a “rare, but real” signal. First, the events are clustering, occurring within days of vaccination. Second, they tend to be more common in males and younger people. Third, he says, the number of events is above the so-called “background rate” – the cases that could be expected in this age group even without vaccination.
“I don’t think we’re quite there yet. We haven’t tied a ribbon around it, but I think the data are trending in that direction,” he said.
The issue of myocarditis weighed heavily on the Vaccines and Related Biological Products Advisory Committee’s considerations of what kind and how much data might be needed to green light use of a vaccine for COVID in children.
Because the rates of hospitalization for COVID are low in kids, some felt that the FDA should require at least a year of study of the vaccines in clinical trials, the amount of data typically required for full approval, instead of the 2 months currently required for emergency use authorization. Others wondered whether the risks of vaccination – as low as they are – might outweigh the benefits in this age group.
“I don’t really see this as an emergency in children,” said committee member Michael Kurilla, MD, PhD, the director of clinical innovation at the National Institutes of Health. Dr. Kurilla, however, did say he thought having an expanded access program for children at high risk might make sense.
Most of the young adults who experienced myocarditis recovered quickly, though three needed intensive care and rehabilitation after their episodes. Among cases with known outcomes, 81% got better and 19% still have ongoing symptoms.
Adverse events reports
The data on myocarditis come from the Vaccine Adverse Events Reporting System, or VAERS, a database of health problems reported after vaccination. This reporting system, open to anyone, has benefits and limits. It gives the CDC and FDA the ability to rapidly detect potential safety issues, and it is large enough that it can detect rare events, something that’s beyond the power of even large clinical trials.
But it is observational, so that there’s no way to know if problems reported were caused by the vaccines or a coincidence.
But because VAERS works on an honor system, it can also be spammed, and it carries the bias of the person who’s doing the reporting, from clinicians to average patients. For that reason, Dr. Shimabukuro said they are actively investigating and confirming each report they get.
Out of more than 12 million doses administered to youth ages 16-24, the CDC says it has 275 reports of heart inflammation following vaccination in this age group. The CDC has analyzed a total 475 cases of myocarditis after vaccination in people under age 30 that were reported to VAERS.
The vaccines linked to the events are the mRNA vaccines made by Pfizer and Moderna. The only vaccines currently authorized for use in adolescents are made by Pfizer. Because the Pfizer vaccine was authorized for use in kids as young as 12 last month, there’s not yet enough data to draw conclusions about the risk of myocarditis in kids ages 12-15.
Younger age groups have only received about 9% of the total doses of the vaccine so far, but they represent about 50% of the myocarditis cases reported after vaccination. “We clearly have an imbalance there,” Dr. Shimabukuro said.
The number of events in this age group appears to be above the rate that would be expected for these age groups without vaccines in the picture, he said, explaining that the number of events are in line with similar adverse events seen in young people in Israel and reported by the Department of Defense. Israel found the incidence of myocarditis after vaccination was 50 cases per million for men ages 18-30.
More study needed
Another system tracking adverse events through hospitals, the Vaccine Safety Datalink, didn’t show reports of heart inflammation above numbers that are normally seen in the population, but it did show that inflammation was more likely after a second dose of the vaccine.
“Should this be included in informed consent?” asked Cody Meissner, MD, a pediatric infectious disease specialist at Tufts University, Boston, and a member of the FDA committee.
“I think it’s hard to deny there seem to be some [events that seem] to be occurring in terms of myocarditis,” he said.
Dr. Meissner said later in the committee’s discussion that his own hospital had recently admitted a 12-year-old boy who developed heart swelling 2 days after the second dose of vaccine with a high level of troponin, an enzyme that indicates damage to the heart. His level was over 9. “A very high level,” Dr. Meissner said.
“Will there be scarring to the myocardium? Will there be a predisposition to arrhythmias later on? Will there be an early onset of heart failure? We think that’s unlikely, but [we] don’t know that,” he said.
The CDC has scheduled an emergency meeting next week to convene an expert panel on immunization practices to further review the events.
In addition to the information presented at the FDA’s meeting, doctors at Oregon Health & Science University, Portland, recently described seven cases in teens – all boys – who developed heart inflammation within 4 days of getting the second dose of the Pfizer vaccine.
The study was published June 10 in Pediatrics. All the boys were hospitalized and treated with anti-inflammatory medications including NSAIDs and steroids. Most were discharged within a few days and all recovered from their symptoms.
A version of this article first appeared on Medscape.com.
Migraine linked to more COVID-19 infections, symptoms but less health care utilization
, according to a study presented at the American Headache Society’s 2021 annual meeting.
“These data suggest that people with migraine are either more susceptible to contracting COVID-19, or that they may be more sensitive to the development of symptoms once COVID-19 has been contracted, or both,” Robert Shapiro, MD, PhD, professor of neurological science at the University of Vermont, Burlington. “Further, once COVID-19 has been contracted, people with migraine may be less likely to develop serious COVID-19 outcomes, or they may be less likely to seek health care for COVID-19, or both.”
In providing background information, Dr. Shapiro noted previous research showing that headache is associated with a positive prognosis in COVID-19 inpatients, including lower IL-6 levels throughout the disease course, a 1-week shorter disease course, and a 2.2 times greater relative risk of survival.
Yet in a study across 171 countries, a higher population prevalence of migraine is associated with higher COVID-19 mortality rates. It’s unclear what conclusions can be drawn from that association, however, said Deborah I. Friedman, MD, MPH, professor of neurology and ophthalmology at University of Texas, Dallas, who was not involved in the research.
Dr. Shapiro suggested a theoretical possibility, noting that two genes linked to migraine susceptibility – SCN1A and IFNAR2 – are among 15 host loci also associated with COVID-19 outcomes. Further, Dr. Shapiro noted in his background information, COVID-19 is linked to lower serum calcitonin gene-related peptide levels.
For the study, Dr. Shapiro and colleagues analyzed data from U.S. adults who responded to the National Health and Wellness Survey from April to July 2020. The researchers limited their analysis to the 41,155 participants who had not received the flu vaccine in 2020 since previous research has suggested reduced morbidity among those with COVID-19 who had been vaccinated against the flu. In this group, 4,550 participants had ever been diagnosed by a doctor with migraine (11%) and 36,605 participants had not (89%).
The majority of those with a history of migraine were female (78%), compared with the overall sample (50% female), and tended to be younger, with an average age of 39 compared with 45 for those without migraine (P < .001).
Among those with a previous migraine diagnosis, 3.8% self-reported having had a COVID-19 infection, compared with infection in 2.4% of those without a history of migraine (P < .001). That translated to a 58% increased risk of COVID-19 infection in those with migraine history, with a similar rate of test positivity in both groups (33.7% with migraine history vs. 34.5% without). Test negativity was also similar in both groups (15.9% vs. 17.8%).
Of 360 respondents who had tested positive for COVID-19, the 60 with a history of migraine reported more frequent symptoms than those without migraine. The increased frequency was statistically significant (P < .001 unless otherwise indicated) for the following symptoms:
- Difficulty breathing or shortness of breath (P = .005).
- Fever.
- Headache, sore throat, and/or congestion.
- Fatigue.
- Loss of smell and taste.
- Chills and body aches.
- Persistent pain or pressure in the chest.
- Confusion or inability to arouse.
- Digestive issues (P = .005).
- Bluish lips or face.
For several of these symptoms – such as headache/sore throat/congestion, persistent pain or pressure in the chest, confusion/inability to arouse, and digestive issues – more than twice as many respondents with migraine reported the symptom, vs. those without migraine.
Changes in health care utilization
“I think that people with migraine are aware of their bodies and aware of their symptoms more than the average person,” Dr. Friedman said. Yet those with migraine were less likely to use health care while diagnosed with COVID-19 than were those without migraine. Migraine sufferers with a COVID-19 infection were 1.2 times more likely to visit a health care provider than were those without an infection, but the similar relative risk was 1.35 greater for those with COVID-19 infections and no migraines.
Similarly, those with a migraine history were more than twice as likely to visit the emergency department when they had a COVID-19 vaccine infection than were those without an infection (RR = 2.6), but among those without a history of migraine, respondents were nearly five times more likely to visit the emergency department when they had a COVID-19 infection than when they didn’t (RR = 4.9).
Dr. Friedman suggested that the lower utilization rate may have to do with the nature of migraine itself. “There are people with migraine who go to the emergency room all the time, but then there’s most of the people with migraine, who would rather die than go to the emergency room because with the light and the noise, it’s just a horrible place to be if you have migraine,” Dr. Friedman said. “I think the majority of people would prefer not to go to the emergency room if given the choice.”
Increased likelihood of hospitalization among those with migraine and a COVID-19 infection was 4.6 compared with those with a migraine and no infection; the corresponding hospitalization risk for COVID-19 among those without migraine was 7.6 times greater than for those with no infection. All these risk ratios were statistically significant.
Dr. Shapiro then speculated on what it might mean that headache is a positive prognostic indicator for COVID-19 inpatients and that migraine population prevalence is linked to higher COVID-19 mortality.
“A hypothesis emerges that headache as a symptom, and migraine as a disease, may reflect adaptive processes associated with host defenses against viruses,” Dr. Shapiro said. “For example, migraine-driven behaviors, such as social distancing due to photophobia, in the setting of viral illness may play adaptive roles in reducing viral spread.”
The researchers did not receive external funding. Dr. Shapiro has consulted for Eli Lilly and Lundbeck. Dr. Friedman reports grant support and/or advisory board participation for Allergan, Biohaven Pharmaceuticals, Eli Lilly, Impel NeuroPharma, Invex, Lundbeck, Merck, Revance Therapeutics, Satsuma Pharmaceuticals, Teva Pharmaceuticals, Theranica, and Zosano Pharma.
, according to a study presented at the American Headache Society’s 2021 annual meeting.
“These data suggest that people with migraine are either more susceptible to contracting COVID-19, or that they may be more sensitive to the development of symptoms once COVID-19 has been contracted, or both,” Robert Shapiro, MD, PhD, professor of neurological science at the University of Vermont, Burlington. “Further, once COVID-19 has been contracted, people with migraine may be less likely to develop serious COVID-19 outcomes, or they may be less likely to seek health care for COVID-19, or both.”
In providing background information, Dr. Shapiro noted previous research showing that headache is associated with a positive prognosis in COVID-19 inpatients, including lower IL-6 levels throughout the disease course, a 1-week shorter disease course, and a 2.2 times greater relative risk of survival.
Yet in a study across 171 countries, a higher population prevalence of migraine is associated with higher COVID-19 mortality rates. It’s unclear what conclusions can be drawn from that association, however, said Deborah I. Friedman, MD, MPH, professor of neurology and ophthalmology at University of Texas, Dallas, who was not involved in the research.
Dr. Shapiro suggested a theoretical possibility, noting that two genes linked to migraine susceptibility – SCN1A and IFNAR2 – are among 15 host loci also associated with COVID-19 outcomes. Further, Dr. Shapiro noted in his background information, COVID-19 is linked to lower serum calcitonin gene-related peptide levels.
For the study, Dr. Shapiro and colleagues analyzed data from U.S. adults who responded to the National Health and Wellness Survey from April to July 2020. The researchers limited their analysis to the 41,155 participants who had not received the flu vaccine in 2020 since previous research has suggested reduced morbidity among those with COVID-19 who had been vaccinated against the flu. In this group, 4,550 participants had ever been diagnosed by a doctor with migraine (11%) and 36,605 participants had not (89%).
The majority of those with a history of migraine were female (78%), compared with the overall sample (50% female), and tended to be younger, with an average age of 39 compared with 45 for those without migraine (P < .001).
Among those with a previous migraine diagnosis, 3.8% self-reported having had a COVID-19 infection, compared with infection in 2.4% of those without a history of migraine (P < .001). That translated to a 58% increased risk of COVID-19 infection in those with migraine history, with a similar rate of test positivity in both groups (33.7% with migraine history vs. 34.5% without). Test negativity was also similar in both groups (15.9% vs. 17.8%).
Of 360 respondents who had tested positive for COVID-19, the 60 with a history of migraine reported more frequent symptoms than those without migraine. The increased frequency was statistically significant (P < .001 unless otherwise indicated) for the following symptoms:
- Difficulty breathing or shortness of breath (P = .005).
- Fever.
- Headache, sore throat, and/or congestion.
- Fatigue.
- Loss of smell and taste.
- Chills and body aches.
- Persistent pain or pressure in the chest.
- Confusion or inability to arouse.
- Digestive issues (P = .005).
- Bluish lips or face.
For several of these symptoms – such as headache/sore throat/congestion, persistent pain or pressure in the chest, confusion/inability to arouse, and digestive issues – more than twice as many respondents with migraine reported the symptom, vs. those without migraine.
Changes in health care utilization
“I think that people with migraine are aware of their bodies and aware of their symptoms more than the average person,” Dr. Friedman said. Yet those with migraine were less likely to use health care while diagnosed with COVID-19 than were those without migraine. Migraine sufferers with a COVID-19 infection were 1.2 times more likely to visit a health care provider than were those without an infection, but the similar relative risk was 1.35 greater for those with COVID-19 infections and no migraines.
Similarly, those with a migraine history were more than twice as likely to visit the emergency department when they had a COVID-19 vaccine infection than were those without an infection (RR = 2.6), but among those without a history of migraine, respondents were nearly five times more likely to visit the emergency department when they had a COVID-19 infection than when they didn’t (RR = 4.9).
Dr. Friedman suggested that the lower utilization rate may have to do with the nature of migraine itself. “There are people with migraine who go to the emergency room all the time, but then there’s most of the people with migraine, who would rather die than go to the emergency room because with the light and the noise, it’s just a horrible place to be if you have migraine,” Dr. Friedman said. “I think the majority of people would prefer not to go to the emergency room if given the choice.”
Increased likelihood of hospitalization among those with migraine and a COVID-19 infection was 4.6 compared with those with a migraine and no infection; the corresponding hospitalization risk for COVID-19 among those without migraine was 7.6 times greater than for those with no infection. All these risk ratios were statistically significant.
Dr. Shapiro then speculated on what it might mean that headache is a positive prognostic indicator for COVID-19 inpatients and that migraine population prevalence is linked to higher COVID-19 mortality.
“A hypothesis emerges that headache as a symptom, and migraine as a disease, may reflect adaptive processes associated with host defenses against viruses,” Dr. Shapiro said. “For example, migraine-driven behaviors, such as social distancing due to photophobia, in the setting of viral illness may play adaptive roles in reducing viral spread.”
The researchers did not receive external funding. Dr. Shapiro has consulted for Eli Lilly and Lundbeck. Dr. Friedman reports grant support and/or advisory board participation for Allergan, Biohaven Pharmaceuticals, Eli Lilly, Impel NeuroPharma, Invex, Lundbeck, Merck, Revance Therapeutics, Satsuma Pharmaceuticals, Teva Pharmaceuticals, Theranica, and Zosano Pharma.
, according to a study presented at the American Headache Society’s 2021 annual meeting.
“These data suggest that people with migraine are either more susceptible to contracting COVID-19, or that they may be more sensitive to the development of symptoms once COVID-19 has been contracted, or both,” Robert Shapiro, MD, PhD, professor of neurological science at the University of Vermont, Burlington. “Further, once COVID-19 has been contracted, people with migraine may be less likely to develop serious COVID-19 outcomes, or they may be less likely to seek health care for COVID-19, or both.”
In providing background information, Dr. Shapiro noted previous research showing that headache is associated with a positive prognosis in COVID-19 inpatients, including lower IL-6 levels throughout the disease course, a 1-week shorter disease course, and a 2.2 times greater relative risk of survival.
Yet in a study across 171 countries, a higher population prevalence of migraine is associated with higher COVID-19 mortality rates. It’s unclear what conclusions can be drawn from that association, however, said Deborah I. Friedman, MD, MPH, professor of neurology and ophthalmology at University of Texas, Dallas, who was not involved in the research.
Dr. Shapiro suggested a theoretical possibility, noting that two genes linked to migraine susceptibility – SCN1A and IFNAR2 – are among 15 host loci also associated with COVID-19 outcomes. Further, Dr. Shapiro noted in his background information, COVID-19 is linked to lower serum calcitonin gene-related peptide levels.
For the study, Dr. Shapiro and colleagues analyzed data from U.S. adults who responded to the National Health and Wellness Survey from April to July 2020. The researchers limited their analysis to the 41,155 participants who had not received the flu vaccine in 2020 since previous research has suggested reduced morbidity among those with COVID-19 who had been vaccinated against the flu. In this group, 4,550 participants had ever been diagnosed by a doctor with migraine (11%) and 36,605 participants had not (89%).
The majority of those with a history of migraine were female (78%), compared with the overall sample (50% female), and tended to be younger, with an average age of 39 compared with 45 for those without migraine (P < .001).
Among those with a previous migraine diagnosis, 3.8% self-reported having had a COVID-19 infection, compared with infection in 2.4% of those without a history of migraine (P < .001). That translated to a 58% increased risk of COVID-19 infection in those with migraine history, with a similar rate of test positivity in both groups (33.7% with migraine history vs. 34.5% without). Test negativity was also similar in both groups (15.9% vs. 17.8%).
Of 360 respondents who had tested positive for COVID-19, the 60 with a history of migraine reported more frequent symptoms than those without migraine. The increased frequency was statistically significant (P < .001 unless otherwise indicated) for the following symptoms:
- Difficulty breathing or shortness of breath (P = .005).
- Fever.
- Headache, sore throat, and/or congestion.
- Fatigue.
- Loss of smell and taste.
- Chills and body aches.
- Persistent pain or pressure in the chest.
- Confusion or inability to arouse.
- Digestive issues (P = .005).
- Bluish lips or face.
For several of these symptoms – such as headache/sore throat/congestion, persistent pain or pressure in the chest, confusion/inability to arouse, and digestive issues – more than twice as many respondents with migraine reported the symptom, vs. those without migraine.
Changes in health care utilization
“I think that people with migraine are aware of their bodies and aware of their symptoms more than the average person,” Dr. Friedman said. Yet those with migraine were less likely to use health care while diagnosed with COVID-19 than were those without migraine. Migraine sufferers with a COVID-19 infection were 1.2 times more likely to visit a health care provider than were those without an infection, but the similar relative risk was 1.35 greater for those with COVID-19 infections and no migraines.
Similarly, those with a migraine history were more than twice as likely to visit the emergency department when they had a COVID-19 vaccine infection than were those without an infection (RR = 2.6), but among those without a history of migraine, respondents were nearly five times more likely to visit the emergency department when they had a COVID-19 infection than when they didn’t (RR = 4.9).
Dr. Friedman suggested that the lower utilization rate may have to do with the nature of migraine itself. “There are people with migraine who go to the emergency room all the time, but then there’s most of the people with migraine, who would rather die than go to the emergency room because with the light and the noise, it’s just a horrible place to be if you have migraine,” Dr. Friedman said. “I think the majority of people would prefer not to go to the emergency room if given the choice.”
Increased likelihood of hospitalization among those with migraine and a COVID-19 infection was 4.6 compared with those with a migraine and no infection; the corresponding hospitalization risk for COVID-19 among those without migraine was 7.6 times greater than for those with no infection. All these risk ratios were statistically significant.
Dr. Shapiro then speculated on what it might mean that headache is a positive prognostic indicator for COVID-19 inpatients and that migraine population prevalence is linked to higher COVID-19 mortality.
“A hypothesis emerges that headache as a symptom, and migraine as a disease, may reflect adaptive processes associated with host defenses against viruses,” Dr. Shapiro said. “For example, migraine-driven behaviors, such as social distancing due to photophobia, in the setting of viral illness may play adaptive roles in reducing viral spread.”
The researchers did not receive external funding. Dr. Shapiro has consulted for Eli Lilly and Lundbeck. Dr. Friedman reports grant support and/or advisory board participation for Allergan, Biohaven Pharmaceuticals, Eli Lilly, Impel NeuroPharma, Invex, Lundbeck, Merck, Revance Therapeutics, Satsuma Pharmaceuticals, Teva Pharmaceuticals, Theranica, and Zosano Pharma.
FROM AHS 2021
Mavrilimumab may aid severe COVID-19 recovery
Inhibiting granulocyte/macrophage–colony stimulating factor (GM-CSF) with mavrilimumab prevented some patients with severe COVID-19 pneumonia and hyperinflammation from needing mechanical ventilation and reduced their risk of dying versus placebo in a phase 2 study.
There was no difference in outcomes between the two doses of mavrilimumab used in the trial (6 mg/kg or 10 mg/kg) and combined data showed a higher percentage of patients achieving the primary endpoint of being alive and free of mechanical ventilation at 29 days, at 87%, versus placebo, at 74%.
The P value was 0.12, “which achieved the prespecified evidentiary standard of 0.2,” according to Lara Pupim, MD, vice president of clinical research and development at Kiniksa Pharmaceuticals in Lexington, Mass.
Importantly, there was a 61% reduction in the risk of dying if patients had received mavrilimumab rather than placebo, she reported at the annual European Congress of Rheumatology. Mortality at day 29 was 21% in the placebo arm but just 8% in the combined mavrilimumab arms (P = .07).
Hendrik Schulze-Koops, MD, called it a “surprising study” and that “the outcome is very spectacular” in his short appraisal of the study during the Clinical Highlights session on the final day of the congress.
Mavrilimumab was “a compound that we would not have thought that would have such an impact on the outcome of COVID-19 infected patients,” Dr. Schulze-Koops of Ludwig Maximilian University of Munich added.
In this small study, “there was a consistent suggestion of a biological effect across key endpoints,” Richard Conway, MBChB, PhD, a consultant rheumatologist at St. James’s Hospital in Dublin, pointed out in an interview.
“Similar to tocilizumab, the benefits with mavrilimumab appear to be in addition to those seen with glucocorticoids, as 96% of patients received dexamethasone,” Dr. Conway observed. Furthermore, nearly one-third received antiviral or remdesivir treatment.
“This study was likely underpowered to assess a clinically meaningful benefit,” he said, adding that “there is insufficient evidence at present to begin using mavrilimumab as an alternative to currently available agents.” That said, “these results are promising for future studies.”
Rationale for GM-CSF inhibition with mavrilimumab in COVID-19 pneumonia
“The cytokine GM-CSF is vital to both lung homeostasis and regulation of inflammation in autoimmunity,” Dr. Pupim explained.
She added that “GM-CSF is implicated in the mechanism of aberrant immune cell infiltration and activation in the lungs, and it may contribute to respiratory failure and death in patients with severe COVID-19 pneumonia and systemic hyperinflammation.”
The efficacy and safety of blocking GM-CSF with mavrilimumab have been shown previously in phase 2 studies in other diseases, Dr. Pupim noted. This includes patients with rheumatoid arthritis and those with giant cell arteritis.
“It was hypothesized that GM-CSF receptor–alpha blockade may reduce infiltration of pathogenic cells into the lung and may suppress inflammation in COVID-19 pneumonia in hyperinflammation,” she explained.
Study details and other outcome results
The study presented by Dr. Pupim was a phase 2/3 double-blind, placebo-controlled trial predominantly conducted in Brazil, the United States, and South Africa, with some participation in Peru and Chile.
Patients were eligible for inclusion if they had had a positive COVID-19 test within 14 days of randomization and had been hospitalized but not ventilated. Evidence of bilateral pneumonia on chest x-ray or CT scan and clinical laboratory evidence indicative of hyperinflammation were also prerequisites for study enrollment.
The ongoing study comprised two cohorts, Dr. Pupim explained: patients who have not been ventilated and those who have recently been ventilated. Dr. Pupim presented the data on the nonventilated cohort, noting that there was a total of 116 patients aged a mean of 57 years.
Patients were randomized to one of three treatment arms: two groups received a single intravenous infusion of mavrilimumab, either 6 mg/kg or 10 mg/kg, and the third group got a placebo.
“Using a time-to-event approach, looking at mechanical ventilation-free survival, mavrilimumab recipients experienced a 65% reduction in the risk of mechanical ventilation or death,” Dr. Pupim said (P = .0175).
“Separation in the Kaplan-Meier curves was evident very early after study drug administration,” she added.
There were trends toward a faster benefit with mavrilimumab than placebo in two other key secondary endpoints: the median time to achieving a two-point clinical improvement (7 vs. 11 days) and the median time to room air (7 vs. 9 days).
Timing of mavrilimumab administration and safety
Study coauthor and chief clinical development officer at Kiniksa, Arian Pano, MD, answered questions on the presentation. When asked about the timing of giving mavrilimumab, he said: “Based on these data it is before they go to ventilation, as soon as you have symptoms of hyperinflammation and a need for oxygen.”
Mavrilimumab is given as a single infusion “and has been well tolerated; virtually no interruptions occurred in this study.”
No serious adverse events related to mavrilimumab were seen, and adverse events, including secondary infections, which are known complications of COVID-19, occurred less frequently in mavrilimumab recipients, compared with placebo.
Dr. Pupim reported that there was a case of tuberculosis in one patient treated with mavrilimumab (10 mg/kg). That case had occurred in an “endemic area for tuberculosis,” and the patient had been screened before entry but only via a sputum sample.
“Prior to these events, the patient received high-dose corticosteroids, a known risk factor for reactivation of TB, and thus the potential additive contribution of mavrilimumab, if any, is uncertain.” Dr. Pupim said.
“Thrombotic events, another known complication of COVID-19, occurred in the placebo arm only,” she added.
Dr. Pano commented that the study has now “seamlessly continued to phase 3. So, basically, we did not stop the study. At the end of phase 2, we just locked the database and collected the data.” Both the 6 mg/kg and 10 mg/kg are being studied, but it’s “very likely [that] 6 mg/kg could be the dose that we may bring forward to the clinic in terms of registration, but that’s at this point in time. We will need to wait for the phase 3 data,” he observed. Those findings will hopefully be available later this year.
Kiniksa funded the study. Dr. Pupim, Dr. Pano, and multiple study coinvestigators are employees of the company.
Dr. Schulze-Koops was not involved in the study and had no specific disclosures. Dr. Conway had no financial disclosures to make in relation to his comments.
Inhibiting granulocyte/macrophage–colony stimulating factor (GM-CSF) with mavrilimumab prevented some patients with severe COVID-19 pneumonia and hyperinflammation from needing mechanical ventilation and reduced their risk of dying versus placebo in a phase 2 study.
There was no difference in outcomes between the two doses of mavrilimumab used in the trial (6 mg/kg or 10 mg/kg) and combined data showed a higher percentage of patients achieving the primary endpoint of being alive and free of mechanical ventilation at 29 days, at 87%, versus placebo, at 74%.
The P value was 0.12, “which achieved the prespecified evidentiary standard of 0.2,” according to Lara Pupim, MD, vice president of clinical research and development at Kiniksa Pharmaceuticals in Lexington, Mass.
Importantly, there was a 61% reduction in the risk of dying if patients had received mavrilimumab rather than placebo, she reported at the annual European Congress of Rheumatology. Mortality at day 29 was 21% in the placebo arm but just 8% in the combined mavrilimumab arms (P = .07).
Hendrik Schulze-Koops, MD, called it a “surprising study” and that “the outcome is very spectacular” in his short appraisal of the study during the Clinical Highlights session on the final day of the congress.
Mavrilimumab was “a compound that we would not have thought that would have such an impact on the outcome of COVID-19 infected patients,” Dr. Schulze-Koops of Ludwig Maximilian University of Munich added.
In this small study, “there was a consistent suggestion of a biological effect across key endpoints,” Richard Conway, MBChB, PhD, a consultant rheumatologist at St. James’s Hospital in Dublin, pointed out in an interview.
“Similar to tocilizumab, the benefits with mavrilimumab appear to be in addition to those seen with glucocorticoids, as 96% of patients received dexamethasone,” Dr. Conway observed. Furthermore, nearly one-third received antiviral or remdesivir treatment.
“This study was likely underpowered to assess a clinically meaningful benefit,” he said, adding that “there is insufficient evidence at present to begin using mavrilimumab as an alternative to currently available agents.” That said, “these results are promising for future studies.”
Rationale for GM-CSF inhibition with mavrilimumab in COVID-19 pneumonia
“The cytokine GM-CSF is vital to both lung homeostasis and regulation of inflammation in autoimmunity,” Dr. Pupim explained.
She added that “GM-CSF is implicated in the mechanism of aberrant immune cell infiltration and activation in the lungs, and it may contribute to respiratory failure and death in patients with severe COVID-19 pneumonia and systemic hyperinflammation.”
The efficacy and safety of blocking GM-CSF with mavrilimumab have been shown previously in phase 2 studies in other diseases, Dr. Pupim noted. This includes patients with rheumatoid arthritis and those with giant cell arteritis.
“It was hypothesized that GM-CSF receptor–alpha blockade may reduce infiltration of pathogenic cells into the lung and may suppress inflammation in COVID-19 pneumonia in hyperinflammation,” she explained.
Study details and other outcome results
The study presented by Dr. Pupim was a phase 2/3 double-blind, placebo-controlled trial predominantly conducted in Brazil, the United States, and South Africa, with some participation in Peru and Chile.
Patients were eligible for inclusion if they had had a positive COVID-19 test within 14 days of randomization and had been hospitalized but not ventilated. Evidence of bilateral pneumonia on chest x-ray or CT scan and clinical laboratory evidence indicative of hyperinflammation were also prerequisites for study enrollment.
The ongoing study comprised two cohorts, Dr. Pupim explained: patients who have not been ventilated and those who have recently been ventilated. Dr. Pupim presented the data on the nonventilated cohort, noting that there was a total of 116 patients aged a mean of 57 years.
Patients were randomized to one of three treatment arms: two groups received a single intravenous infusion of mavrilimumab, either 6 mg/kg or 10 mg/kg, and the third group got a placebo.
“Using a time-to-event approach, looking at mechanical ventilation-free survival, mavrilimumab recipients experienced a 65% reduction in the risk of mechanical ventilation or death,” Dr. Pupim said (P = .0175).
“Separation in the Kaplan-Meier curves was evident very early after study drug administration,” she added.
There were trends toward a faster benefit with mavrilimumab than placebo in two other key secondary endpoints: the median time to achieving a two-point clinical improvement (7 vs. 11 days) and the median time to room air (7 vs. 9 days).
Timing of mavrilimumab administration and safety
Study coauthor and chief clinical development officer at Kiniksa, Arian Pano, MD, answered questions on the presentation. When asked about the timing of giving mavrilimumab, he said: “Based on these data it is before they go to ventilation, as soon as you have symptoms of hyperinflammation and a need for oxygen.”
Mavrilimumab is given as a single infusion “and has been well tolerated; virtually no interruptions occurred in this study.”
No serious adverse events related to mavrilimumab were seen, and adverse events, including secondary infections, which are known complications of COVID-19, occurred less frequently in mavrilimumab recipients, compared with placebo.
Dr. Pupim reported that there was a case of tuberculosis in one patient treated with mavrilimumab (10 mg/kg). That case had occurred in an “endemic area for tuberculosis,” and the patient had been screened before entry but only via a sputum sample.
“Prior to these events, the patient received high-dose corticosteroids, a known risk factor for reactivation of TB, and thus the potential additive contribution of mavrilimumab, if any, is uncertain.” Dr. Pupim said.
“Thrombotic events, another known complication of COVID-19, occurred in the placebo arm only,” she added.
Dr. Pano commented that the study has now “seamlessly continued to phase 3. So, basically, we did not stop the study. At the end of phase 2, we just locked the database and collected the data.” Both the 6 mg/kg and 10 mg/kg are being studied, but it’s “very likely [that] 6 mg/kg could be the dose that we may bring forward to the clinic in terms of registration, but that’s at this point in time. We will need to wait for the phase 3 data,” he observed. Those findings will hopefully be available later this year.
Kiniksa funded the study. Dr. Pupim, Dr. Pano, and multiple study coinvestigators are employees of the company.
Dr. Schulze-Koops was not involved in the study and had no specific disclosures. Dr. Conway had no financial disclosures to make in relation to his comments.
Inhibiting granulocyte/macrophage–colony stimulating factor (GM-CSF) with mavrilimumab prevented some patients with severe COVID-19 pneumonia and hyperinflammation from needing mechanical ventilation and reduced their risk of dying versus placebo in a phase 2 study.
There was no difference in outcomes between the two doses of mavrilimumab used in the trial (6 mg/kg or 10 mg/kg) and combined data showed a higher percentage of patients achieving the primary endpoint of being alive and free of mechanical ventilation at 29 days, at 87%, versus placebo, at 74%.
The P value was 0.12, “which achieved the prespecified evidentiary standard of 0.2,” according to Lara Pupim, MD, vice president of clinical research and development at Kiniksa Pharmaceuticals in Lexington, Mass.
Importantly, there was a 61% reduction in the risk of dying if patients had received mavrilimumab rather than placebo, she reported at the annual European Congress of Rheumatology. Mortality at day 29 was 21% in the placebo arm but just 8% in the combined mavrilimumab arms (P = .07).
Hendrik Schulze-Koops, MD, called it a “surprising study” and that “the outcome is very spectacular” in his short appraisal of the study during the Clinical Highlights session on the final day of the congress.
Mavrilimumab was “a compound that we would not have thought that would have such an impact on the outcome of COVID-19 infected patients,” Dr. Schulze-Koops of Ludwig Maximilian University of Munich added.
In this small study, “there was a consistent suggestion of a biological effect across key endpoints,” Richard Conway, MBChB, PhD, a consultant rheumatologist at St. James’s Hospital in Dublin, pointed out in an interview.
“Similar to tocilizumab, the benefits with mavrilimumab appear to be in addition to those seen with glucocorticoids, as 96% of patients received dexamethasone,” Dr. Conway observed. Furthermore, nearly one-third received antiviral or remdesivir treatment.
“This study was likely underpowered to assess a clinically meaningful benefit,” he said, adding that “there is insufficient evidence at present to begin using mavrilimumab as an alternative to currently available agents.” That said, “these results are promising for future studies.”
Rationale for GM-CSF inhibition with mavrilimumab in COVID-19 pneumonia
“The cytokine GM-CSF is vital to both lung homeostasis and regulation of inflammation in autoimmunity,” Dr. Pupim explained.
She added that “GM-CSF is implicated in the mechanism of aberrant immune cell infiltration and activation in the lungs, and it may contribute to respiratory failure and death in patients with severe COVID-19 pneumonia and systemic hyperinflammation.”
The efficacy and safety of blocking GM-CSF with mavrilimumab have been shown previously in phase 2 studies in other diseases, Dr. Pupim noted. This includes patients with rheumatoid arthritis and those with giant cell arteritis.
“It was hypothesized that GM-CSF receptor–alpha blockade may reduce infiltration of pathogenic cells into the lung and may suppress inflammation in COVID-19 pneumonia in hyperinflammation,” she explained.
Study details and other outcome results
The study presented by Dr. Pupim was a phase 2/3 double-blind, placebo-controlled trial predominantly conducted in Brazil, the United States, and South Africa, with some participation in Peru and Chile.
Patients were eligible for inclusion if they had had a positive COVID-19 test within 14 days of randomization and had been hospitalized but not ventilated. Evidence of bilateral pneumonia on chest x-ray or CT scan and clinical laboratory evidence indicative of hyperinflammation were also prerequisites for study enrollment.
The ongoing study comprised two cohorts, Dr. Pupim explained: patients who have not been ventilated and those who have recently been ventilated. Dr. Pupim presented the data on the nonventilated cohort, noting that there was a total of 116 patients aged a mean of 57 years.
Patients were randomized to one of three treatment arms: two groups received a single intravenous infusion of mavrilimumab, either 6 mg/kg or 10 mg/kg, and the third group got a placebo.
“Using a time-to-event approach, looking at mechanical ventilation-free survival, mavrilimumab recipients experienced a 65% reduction in the risk of mechanical ventilation or death,” Dr. Pupim said (P = .0175).
“Separation in the Kaplan-Meier curves was evident very early after study drug administration,” she added.
There were trends toward a faster benefit with mavrilimumab than placebo in two other key secondary endpoints: the median time to achieving a two-point clinical improvement (7 vs. 11 days) and the median time to room air (7 vs. 9 days).
Timing of mavrilimumab administration and safety
Study coauthor and chief clinical development officer at Kiniksa, Arian Pano, MD, answered questions on the presentation. When asked about the timing of giving mavrilimumab, he said: “Based on these data it is before they go to ventilation, as soon as you have symptoms of hyperinflammation and a need for oxygen.”
Mavrilimumab is given as a single infusion “and has been well tolerated; virtually no interruptions occurred in this study.”
No serious adverse events related to mavrilimumab were seen, and adverse events, including secondary infections, which are known complications of COVID-19, occurred less frequently in mavrilimumab recipients, compared with placebo.
Dr. Pupim reported that there was a case of tuberculosis in one patient treated with mavrilimumab (10 mg/kg). That case had occurred in an “endemic area for tuberculosis,” and the patient had been screened before entry but only via a sputum sample.
“Prior to these events, the patient received high-dose corticosteroids, a known risk factor for reactivation of TB, and thus the potential additive contribution of mavrilimumab, if any, is uncertain.” Dr. Pupim said.
“Thrombotic events, another known complication of COVID-19, occurred in the placebo arm only,” she added.
Dr. Pano commented that the study has now “seamlessly continued to phase 3. So, basically, we did not stop the study. At the end of phase 2, we just locked the database and collected the data.” Both the 6 mg/kg and 10 mg/kg are being studied, but it’s “very likely [that] 6 mg/kg could be the dose that we may bring forward to the clinic in terms of registration, but that’s at this point in time. We will need to wait for the phase 3 data,” he observed. Those findings will hopefully be available later this year.
Kiniksa funded the study. Dr. Pupim, Dr. Pano, and multiple study coinvestigators are employees of the company.
Dr. Schulze-Koops was not involved in the study and had no specific disclosures. Dr. Conway had no financial disclosures to make in relation to his comments.
FROM EULAR 2021 CONGRESS
New world order: Reflecting on a year of COVID
I remember sitting at the pool in San Diego. I had been there before many years prior – one of my first medical conferences. I remember the clinking of metal sail stays in the morning breeze.
Flying out this time I packed a few surgical masks. I guiltily picked up an N95 from the hospital floors the day before leaving, but then left it at home thinking it overkill. I still have it in a ziplock bag a year later – it’s our emergency “what-if-we-have-to-care-for-one-another-with-COVID-in-this-tiny-house-full-of-kids” N95. Not that my husband has been fit tested. At the time, neither was I.
I returned after the conference to befuddlement over how we might fit test thousands of people, racing COVID to the front door. An overly complicated task, as we didn’t even know who was supposed to be responsible for orchestrating such an effort. We didn’t even know if we could spare the N95s.
Still in California, I sat by the pool wondering if anyone would acknowledge the impending new reality. At the conference we were told “don’t shake hands, don’t touch your face, wash your hands a lot.” I gave a workshop without a mask. I ate dinner in an actual restaurant worried only about gluten free soy sauce. I sat in a lecture hall with almost 5,000 people. I started to have a conversation with a friend from Seattle, but he needed to leave because they found a positive patient in his hospital. I listened to a prerecorded webinar by the pool from our chief safety officer saying there was a plan. I was not reassured.
When we flew home the world had already changed. There were patients in New York now. Masks had appeared in the airport news stand. Yet we breathed the air in the closed space of the red eye and forgot to be concerned. At work that Monday I asked my team – fist to 5, how worried are you about this? Brave faces and side eyes at each other and a lot of 1s or 2s held up in the air. My job this week, I told them, is to get you all to a 5.
I was working with a resident who 2 months prior I had told, as we worked together in the lounge, I don’t think you’re going to China on vacation. She hadn’t gone, of course. I wasn’t going on spring break either. On one of my last train rides a commuter friend (remember those?) told me we’ll all feel a lot better once we realize that none of us are going to get to do any of the things we want to do.
The med students were still there, helping the team and hanging onto their education. I told everyone not to see any patient with a respiratory complaint until we first discussed the case. On the third day of service I had to call infection control because a hypoxic febrile patient had come to the floor without isolation orders. “Are we testing?” No, I was informed, she hadn’t had exposures, hadn’t travelled. Speechless that we were screening for travel to Italy while living with one tiny state between us and the American epicenter, I can now recall thinking that our infection control officer did not sound well rested.
My N95 was still in a baggy at home. The PAPRS hadn’t appeared yet. Literally no one could agree what kind of mask the CDC or infection control or the ID consultant of the day recommended – today we are using surgical masks, I was told. Thursday will likely be different. “Anyway, she doesn’t sound like she has it.” I walked to the floors.
My med student started presenting our septic viral pneumonia patient including the very well done exam that I previously forbade him from obtaining. What happened to not seeing respiratory patients, I asked. Oh, they said, well night float said it didn’t sound like COVID. Insufficiently convinced by our second year resident’s unjustifiably overconfident, though ultimately correct, assessment – I held my head in my hands and give my first hallway COVID chalk talk of the new era. Complete with telling the team to question everything they thought they knew now including everything I said except “be careful.” That was about when Philadelphia ran out of toilet paper.
That weekend I sat in front of a bay of computers as our Medical Officer of the Day. Air traffic control for ED patients coming in for a landing on medical teams, I watched the new biohazard warnings line up indicating respiratory isolation patients waiting for a bed. I watched CRPs and D-dimers, and looked for leukopenia. I vowed I would follow up on tests to hone my COVID illness script. I soon realized that tests lie anyway.
By the end of that week we’d fallen through the looking glass. The old rules didn’t apply. We weren’t going to China, or Arizona; we didn’t know when the med students were coming back; the jobs we had were not the jobs we signed up for but were those that the world needed us to do; we couldn’t trust our intuition or our tests; we had no experts – and yet we started to grow the humble beginnings of expertise like spring garden sprouts.
In a chaotic world, seeds of order take shape and then scatter like a screensaver. The skills needed to manage chaos are different from those that leaders use in simple ordered times. Order cannot be pulled from chaos by force of will or cleverness, nor can it be delegated, cascaded, demanded, or launched. Order emerges when communities that are receptive to learning see patterns through noise, and slowly, lovingly, coax moments of stability into being.
Dr. Jaffe is division director for hospital medicine in the Department of Medicine at Thomas Jefferson University Hospital in Philadelphia.
I remember sitting at the pool in San Diego. I had been there before many years prior – one of my first medical conferences. I remember the clinking of metal sail stays in the morning breeze.
Flying out this time I packed a few surgical masks. I guiltily picked up an N95 from the hospital floors the day before leaving, but then left it at home thinking it overkill. I still have it in a ziplock bag a year later – it’s our emergency “what-if-we-have-to-care-for-one-another-with-COVID-in-this-tiny-house-full-of-kids” N95. Not that my husband has been fit tested. At the time, neither was I.
I returned after the conference to befuddlement over how we might fit test thousands of people, racing COVID to the front door. An overly complicated task, as we didn’t even know who was supposed to be responsible for orchestrating such an effort. We didn’t even know if we could spare the N95s.
Still in California, I sat by the pool wondering if anyone would acknowledge the impending new reality. At the conference we were told “don’t shake hands, don’t touch your face, wash your hands a lot.” I gave a workshop without a mask. I ate dinner in an actual restaurant worried only about gluten free soy sauce. I sat in a lecture hall with almost 5,000 people. I started to have a conversation with a friend from Seattle, but he needed to leave because they found a positive patient in his hospital. I listened to a prerecorded webinar by the pool from our chief safety officer saying there was a plan. I was not reassured.
When we flew home the world had already changed. There were patients in New York now. Masks had appeared in the airport news stand. Yet we breathed the air in the closed space of the red eye and forgot to be concerned. At work that Monday I asked my team – fist to 5, how worried are you about this? Brave faces and side eyes at each other and a lot of 1s or 2s held up in the air. My job this week, I told them, is to get you all to a 5.
I was working with a resident who 2 months prior I had told, as we worked together in the lounge, I don’t think you’re going to China on vacation. She hadn’t gone, of course. I wasn’t going on spring break either. On one of my last train rides a commuter friend (remember those?) told me we’ll all feel a lot better once we realize that none of us are going to get to do any of the things we want to do.
The med students were still there, helping the team and hanging onto their education. I told everyone not to see any patient with a respiratory complaint until we first discussed the case. On the third day of service I had to call infection control because a hypoxic febrile patient had come to the floor without isolation orders. “Are we testing?” No, I was informed, she hadn’t had exposures, hadn’t travelled. Speechless that we were screening for travel to Italy while living with one tiny state between us and the American epicenter, I can now recall thinking that our infection control officer did not sound well rested.
My N95 was still in a baggy at home. The PAPRS hadn’t appeared yet. Literally no one could agree what kind of mask the CDC or infection control or the ID consultant of the day recommended – today we are using surgical masks, I was told. Thursday will likely be different. “Anyway, she doesn’t sound like she has it.” I walked to the floors.
My med student started presenting our septic viral pneumonia patient including the very well done exam that I previously forbade him from obtaining. What happened to not seeing respiratory patients, I asked. Oh, they said, well night float said it didn’t sound like COVID. Insufficiently convinced by our second year resident’s unjustifiably overconfident, though ultimately correct, assessment – I held my head in my hands and give my first hallway COVID chalk talk of the new era. Complete with telling the team to question everything they thought they knew now including everything I said except “be careful.” That was about when Philadelphia ran out of toilet paper.
That weekend I sat in front of a bay of computers as our Medical Officer of the Day. Air traffic control for ED patients coming in for a landing on medical teams, I watched the new biohazard warnings line up indicating respiratory isolation patients waiting for a bed. I watched CRPs and D-dimers, and looked for leukopenia. I vowed I would follow up on tests to hone my COVID illness script. I soon realized that tests lie anyway.
By the end of that week we’d fallen through the looking glass. The old rules didn’t apply. We weren’t going to China, or Arizona; we didn’t know when the med students were coming back; the jobs we had were not the jobs we signed up for but were those that the world needed us to do; we couldn’t trust our intuition or our tests; we had no experts – and yet we started to grow the humble beginnings of expertise like spring garden sprouts.
In a chaotic world, seeds of order take shape and then scatter like a screensaver. The skills needed to manage chaos are different from those that leaders use in simple ordered times. Order cannot be pulled from chaos by force of will or cleverness, nor can it be delegated, cascaded, demanded, or launched. Order emerges when communities that are receptive to learning see patterns through noise, and slowly, lovingly, coax moments of stability into being.
Dr. Jaffe is division director for hospital medicine in the Department of Medicine at Thomas Jefferson University Hospital in Philadelphia.
I remember sitting at the pool in San Diego. I had been there before many years prior – one of my first medical conferences. I remember the clinking of metal sail stays in the morning breeze.
Flying out this time I packed a few surgical masks. I guiltily picked up an N95 from the hospital floors the day before leaving, but then left it at home thinking it overkill. I still have it in a ziplock bag a year later – it’s our emergency “what-if-we-have-to-care-for-one-another-with-COVID-in-this-tiny-house-full-of-kids” N95. Not that my husband has been fit tested. At the time, neither was I.
I returned after the conference to befuddlement over how we might fit test thousands of people, racing COVID to the front door. An overly complicated task, as we didn’t even know who was supposed to be responsible for orchestrating such an effort. We didn’t even know if we could spare the N95s.
Still in California, I sat by the pool wondering if anyone would acknowledge the impending new reality. At the conference we were told “don’t shake hands, don’t touch your face, wash your hands a lot.” I gave a workshop without a mask. I ate dinner in an actual restaurant worried only about gluten free soy sauce. I sat in a lecture hall with almost 5,000 people. I started to have a conversation with a friend from Seattle, but he needed to leave because they found a positive patient in his hospital. I listened to a prerecorded webinar by the pool from our chief safety officer saying there was a plan. I was not reassured.
When we flew home the world had already changed. There were patients in New York now. Masks had appeared in the airport news stand. Yet we breathed the air in the closed space of the red eye and forgot to be concerned. At work that Monday I asked my team – fist to 5, how worried are you about this? Brave faces and side eyes at each other and a lot of 1s or 2s held up in the air. My job this week, I told them, is to get you all to a 5.
I was working with a resident who 2 months prior I had told, as we worked together in the lounge, I don’t think you’re going to China on vacation. She hadn’t gone, of course. I wasn’t going on spring break either. On one of my last train rides a commuter friend (remember those?) told me we’ll all feel a lot better once we realize that none of us are going to get to do any of the things we want to do.
The med students were still there, helping the team and hanging onto their education. I told everyone not to see any patient with a respiratory complaint until we first discussed the case. On the third day of service I had to call infection control because a hypoxic febrile patient had come to the floor without isolation orders. “Are we testing?” No, I was informed, she hadn’t had exposures, hadn’t travelled. Speechless that we were screening for travel to Italy while living with one tiny state between us and the American epicenter, I can now recall thinking that our infection control officer did not sound well rested.
My N95 was still in a baggy at home. The PAPRS hadn’t appeared yet. Literally no one could agree what kind of mask the CDC or infection control or the ID consultant of the day recommended – today we are using surgical masks, I was told. Thursday will likely be different. “Anyway, she doesn’t sound like she has it.” I walked to the floors.
My med student started presenting our septic viral pneumonia patient including the very well done exam that I previously forbade him from obtaining. What happened to not seeing respiratory patients, I asked. Oh, they said, well night float said it didn’t sound like COVID. Insufficiently convinced by our second year resident’s unjustifiably overconfident, though ultimately correct, assessment – I held my head in my hands and give my first hallway COVID chalk talk of the new era. Complete with telling the team to question everything they thought they knew now including everything I said except “be careful.” That was about when Philadelphia ran out of toilet paper.
That weekend I sat in front of a bay of computers as our Medical Officer of the Day. Air traffic control for ED patients coming in for a landing on medical teams, I watched the new biohazard warnings line up indicating respiratory isolation patients waiting for a bed. I watched CRPs and D-dimers, and looked for leukopenia. I vowed I would follow up on tests to hone my COVID illness script. I soon realized that tests lie anyway.
By the end of that week we’d fallen through the looking glass. The old rules didn’t apply. We weren’t going to China, or Arizona; we didn’t know when the med students were coming back; the jobs we had were not the jobs we signed up for but were those that the world needed us to do; we couldn’t trust our intuition or our tests; we had no experts – and yet we started to grow the humble beginnings of expertise like spring garden sprouts.
In a chaotic world, seeds of order take shape and then scatter like a screensaver. The skills needed to manage chaos are different from those that leaders use in simple ordered times. Order cannot be pulled from chaos by force of will or cleverness, nor can it be delegated, cascaded, demanded, or launched. Order emerges when communities that are receptive to learning see patterns through noise, and slowly, lovingly, coax moments of stability into being.
Dr. Jaffe is division director for hospital medicine in the Department of Medicine at Thomas Jefferson University Hospital in Philadelphia.
Free U.K. tool could help guide COVID-19 care for cancer patients
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
Mistrust and Mandates: COVID-19 Vaccination in the Military
It is June and most of us are looking forward to a more normal summer than the one we had in 2020. Many Americans have been vaccinated and states are rolling back some (or all) masking requirements and restrictions on gatherings. In many sectors, including the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA), worries from public health officials about vaccine supply and how to ethically allocate demand have given way to a new set of concerns: We have the shots, but for widespread protection we have to get them into arms.
The reluctance to roll up the sleeve is known as vaccine hesitancy. The National Academies of Science comments on vaccine hesitancy in its report on COVID-19 vaccination allocation. “Potential consequences of vaccine hesitancy—which the committee views as an attitude, preference, or motivational state—are the behaviors of vaccine refusal or delay.”2
On that count, there was encouraging albeit unexpected news in waning days of May. Media reported a sharp increase in the COVID-vaccination of military personnel. Unnamed DoD officials indicated, they had seen a 55% increase in the vaccination of active-duty service members over the previous month. This news represents a dramatic turnaround in a trend of vaccine hesitancy among military members that has persisted since the vaccine became available.3 Even last month, this would have been a very different column. The DoD has not disclosed the exact number of service members who have declined COVID-19 vaccination but multiple news outlets have documented that there was widespread and significant vaccine hesitancy among military personnel. In February, Military News reported that one-third of troops who were offered the vaccine declined it; and in April, USA Today stated that 40% of Marines had refused vaccination.4,5
Still, it is worth examining the data on vaccination among active duty service members. From December 2020 through March 2021, the military conducted the first study to evaluate rates of vaccine initiation and completion in the military in general and for service members from racial/ethnic minorities in particular. Black military personnel were 28% less likely than non-Hispanic White service members to initiate vaccination against coronavirus even after adjusting for other possible confounders. Just 29% of White, 25.5% of Hispanic, and 18.7% of Black service members had initiated the vaccine process in the survey.6
The authors suggest that in part, vaccine hesitancy explains the findings.4 Vaccine hesitancy among racial and ethnic minorities is even more tragic because these same already disadvantaged cohorts have disproportionately suffered from COVID-19 throughout the pandemic with higher rates of infection, serious illness requiring hospitalization, and infection-related morbidity.7
Vaccine hesitancy, delay, or refusal in Black Americans whether military or civilian often is attributed to the historical abuses like the Tuskegee syphilis experiments or the more recent example of cancer cell lines taken from Henrietta Lacks without consent.8 Such government sponsored betrayals no doubt are the soil in which hesitancy grows but recent commentators have opined that focusing solely on these infamous examples may ignore current systemic racism that is pervasively feeding Black Americans reluctance to consider or accept COVID-19 vaccination.9 Blaming infamous research also provides a convenient excuse for confronting contemporary racial discrimination in health care and taking responsibility as health care practitioners for reversing it. “Framing the conversation about distrust in COVID vaccines in terms of everyday racism rather than historical atrocities may increase underserved communities’ willingness to be vaccinated,” Bajaj and Stanford wrote in a recent recent New England Journal of Medicine commentary. “When we hyperfocus on Sims, Lacks, and Tuskegee, we ascribe the current Black health experience to past racism, rooting our present in immovable historical occurrences and undermining efforts to combat mistrust. Everyday racism, by contrast, can be tackled in the present.”9
The study of racial/ethnic disparities in COVID-19 vaccination in active-duty service members was a work product of the Armed Forces Health Surveillance Division. The authors underscore several factors that support the connection between discrimination and vaccine hesitancy in the military. Lack of access to and ability to obtain COVID-19 vaccination continues to be a major barrier that disadvantaged populations must overcome.10 The COVID-19 vaccine is widely available, easily obtained, and free of charge for all military personnel. Yet the vaccine hesitancy in the military parallels that of the civilian sector. This led the study authors to opine that, “forces external to the U.S. Military, such as interpersonal and societal factors also contribute to vaccine hesitancy among military service members.”6
Obviously, any unvaccinated active-duty service member reduces the combat readiness of the fighting force a consideration that led some in Congress to call for mandating vaccination. The vaccine is currently being administered under an emergency use authorization (EUA), which prevents even the military from mandating it.11 Even if President Joseph Biden obtained a waiver to make the vaccine mandatory, the implications of forcing service members who have volunteered to serve their country is ethically problematic. Those problems are exponentially amplified when applied to members of ethnic and racial minorities who have a past and present of health disparities and discrimination. Respecting the decision of those in uniform to decline COVID-19 vaccination is the first and perhaps most important step to rebuilding the trust that is the most promising means of reducing vaccine hesitancy.
Part of the accountability we all bear for health care inequity and racism is to continue the work of this landmark study to better understand vaccine hesitancy among military and veteran cohorts, develop counseling and education that target those attitudes, beliefs, and motivations with education, counseling, and support. All of us can in some small measure follow the ethical mandate “to dispel rumors and provide facts to people” of Secretary Austin, a Black retired 4-star Army general.1
1. Garmone J. Secretary of Defense Addresses Vaccine Hesitancy in the Military. Published February 25, 2021. Accessed May 26, 2021. https://www.defense.gov/Explore/News/Article/Article/2516511/secretary-of-defense-addresses-vaccine-hesitancy-in-military/
2. National Academies of Sciences, Engineering, and Medicine. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies of Science; 2020:188. doi:10.17226/25917
3. Liebermann O. US military sees 55% jump in COVID-19 vaccinations over last month. Published May 20, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/05/20/politics/us-military-covid-vaccinations/index.html
4. Kime P. Almost one-third of us troops are refusing COVID-19 vaccines, officials Say. Published February 17, 2021. Accessed May 26, 2021. https://www.military.com/daily-news/2021/02/17/almost-one-third-of-us-troops-are-refusing-covid-vaccines-officials-say.html
5. Elbeshbishi S. Nearly 40% of Marines decline COVID-19 vaccine, prompting some Democrats to urge Biden to set mandate for the military. USA Today. April 10, 2021. Accessed May 26, 2021. https://www.usatoday.com/story/news/politics/2021/04/10/covid-vaccine-nearly-forty-percent-us-marines-decline/7173918002/
6. Lang MA, Stahlman S, Wells NY, et al. Disparities in COVID-19 vaccine initiation and completion among active component service members and health care personnel, 11 December 2020-12 March 2021. MSMR. 2021;28(4):2-9.
7. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA . 2020;323(24):2466-2467. doi:10.1001/jama.2020.8598
8. Kum D. Fueled by a history of mistreatment, Black Americans distrust the new COVID-19 vaccines. TIME. December 8, 2020. Accessed May 26, 2021.https://time.com/5925074/black-americans-covid-19-vaccine-distrust/
9. Bajaj SS, Stanford FC. Beyond Tuskegee - Vaccine Distrust and Everyday Racism. N Engl J Med. 2021;384(5):e12. doi:10.1056/NEJMpv2035827
10. Feldman N. Why Black and Latino people still lag on COVID-19 vaccines-and how to fix it. NPR. April 26, 2021. Accessed May 26, 2021. https://www.npr.org/sections/health-shots/2021/04/26/989962041/why-black-and-latino-people-still-lag-on-covid-vaccines-and-how-to-fix-it
11. Kaufman E. Lawmakers ask Biden to issue waiver to make COVID-19 vaccination mandatory of members of the military. Updated March 24, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/03/24/politics/congress-letter-military-vaccine/index.html
It is June and most of us are looking forward to a more normal summer than the one we had in 2020. Many Americans have been vaccinated and states are rolling back some (or all) masking requirements and restrictions on gatherings. In many sectors, including the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA), worries from public health officials about vaccine supply and how to ethically allocate demand have given way to a new set of concerns: We have the shots, but for widespread protection we have to get them into arms.
The reluctance to roll up the sleeve is known as vaccine hesitancy. The National Academies of Science comments on vaccine hesitancy in its report on COVID-19 vaccination allocation. “Potential consequences of vaccine hesitancy—which the committee views as an attitude, preference, or motivational state—are the behaviors of vaccine refusal or delay.”2
On that count, there was encouraging albeit unexpected news in waning days of May. Media reported a sharp increase in the COVID-vaccination of military personnel. Unnamed DoD officials indicated, they had seen a 55% increase in the vaccination of active-duty service members over the previous month. This news represents a dramatic turnaround in a trend of vaccine hesitancy among military members that has persisted since the vaccine became available.3 Even last month, this would have been a very different column. The DoD has not disclosed the exact number of service members who have declined COVID-19 vaccination but multiple news outlets have documented that there was widespread and significant vaccine hesitancy among military personnel. In February, Military News reported that one-third of troops who were offered the vaccine declined it; and in April, USA Today stated that 40% of Marines had refused vaccination.4,5
Still, it is worth examining the data on vaccination among active duty service members. From December 2020 through March 2021, the military conducted the first study to evaluate rates of vaccine initiation and completion in the military in general and for service members from racial/ethnic minorities in particular. Black military personnel were 28% less likely than non-Hispanic White service members to initiate vaccination against coronavirus even after adjusting for other possible confounders. Just 29% of White, 25.5% of Hispanic, and 18.7% of Black service members had initiated the vaccine process in the survey.6
The authors suggest that in part, vaccine hesitancy explains the findings.4 Vaccine hesitancy among racial and ethnic minorities is even more tragic because these same already disadvantaged cohorts have disproportionately suffered from COVID-19 throughout the pandemic with higher rates of infection, serious illness requiring hospitalization, and infection-related morbidity.7
Vaccine hesitancy, delay, or refusal in Black Americans whether military or civilian often is attributed to the historical abuses like the Tuskegee syphilis experiments or the more recent example of cancer cell lines taken from Henrietta Lacks without consent.8 Such government sponsored betrayals no doubt are the soil in which hesitancy grows but recent commentators have opined that focusing solely on these infamous examples may ignore current systemic racism that is pervasively feeding Black Americans reluctance to consider or accept COVID-19 vaccination.9 Blaming infamous research also provides a convenient excuse for confronting contemporary racial discrimination in health care and taking responsibility as health care practitioners for reversing it. “Framing the conversation about distrust in COVID vaccines in terms of everyday racism rather than historical atrocities may increase underserved communities’ willingness to be vaccinated,” Bajaj and Stanford wrote in a recent recent New England Journal of Medicine commentary. “When we hyperfocus on Sims, Lacks, and Tuskegee, we ascribe the current Black health experience to past racism, rooting our present in immovable historical occurrences and undermining efforts to combat mistrust. Everyday racism, by contrast, can be tackled in the present.”9
The study of racial/ethnic disparities in COVID-19 vaccination in active-duty service members was a work product of the Armed Forces Health Surveillance Division. The authors underscore several factors that support the connection between discrimination and vaccine hesitancy in the military. Lack of access to and ability to obtain COVID-19 vaccination continues to be a major barrier that disadvantaged populations must overcome.10 The COVID-19 vaccine is widely available, easily obtained, and free of charge for all military personnel. Yet the vaccine hesitancy in the military parallels that of the civilian sector. This led the study authors to opine that, “forces external to the U.S. Military, such as interpersonal and societal factors also contribute to vaccine hesitancy among military service members.”6
Obviously, any unvaccinated active-duty service member reduces the combat readiness of the fighting force a consideration that led some in Congress to call for mandating vaccination. The vaccine is currently being administered under an emergency use authorization (EUA), which prevents even the military from mandating it.11 Even if President Joseph Biden obtained a waiver to make the vaccine mandatory, the implications of forcing service members who have volunteered to serve their country is ethically problematic. Those problems are exponentially amplified when applied to members of ethnic and racial minorities who have a past and present of health disparities and discrimination. Respecting the decision of those in uniform to decline COVID-19 vaccination is the first and perhaps most important step to rebuilding the trust that is the most promising means of reducing vaccine hesitancy.
Part of the accountability we all bear for health care inequity and racism is to continue the work of this landmark study to better understand vaccine hesitancy among military and veteran cohorts, develop counseling and education that target those attitudes, beliefs, and motivations with education, counseling, and support. All of us can in some small measure follow the ethical mandate “to dispel rumors and provide facts to people” of Secretary Austin, a Black retired 4-star Army general.1
It is June and most of us are looking forward to a more normal summer than the one we had in 2020. Many Americans have been vaccinated and states are rolling back some (or all) masking requirements and restrictions on gatherings. In many sectors, including the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA), worries from public health officials about vaccine supply and how to ethically allocate demand have given way to a new set of concerns: We have the shots, but for widespread protection we have to get them into arms.
The reluctance to roll up the sleeve is known as vaccine hesitancy. The National Academies of Science comments on vaccine hesitancy in its report on COVID-19 vaccination allocation. “Potential consequences of vaccine hesitancy—which the committee views as an attitude, preference, or motivational state—are the behaviors of vaccine refusal or delay.”2
On that count, there was encouraging albeit unexpected news in waning days of May. Media reported a sharp increase in the COVID-vaccination of military personnel. Unnamed DoD officials indicated, they had seen a 55% increase in the vaccination of active-duty service members over the previous month. This news represents a dramatic turnaround in a trend of vaccine hesitancy among military members that has persisted since the vaccine became available.3 Even last month, this would have been a very different column. The DoD has not disclosed the exact number of service members who have declined COVID-19 vaccination but multiple news outlets have documented that there was widespread and significant vaccine hesitancy among military personnel. In February, Military News reported that one-third of troops who were offered the vaccine declined it; and in April, USA Today stated that 40% of Marines had refused vaccination.4,5
Still, it is worth examining the data on vaccination among active duty service members. From December 2020 through March 2021, the military conducted the first study to evaluate rates of vaccine initiation and completion in the military in general and for service members from racial/ethnic minorities in particular. Black military personnel were 28% less likely than non-Hispanic White service members to initiate vaccination against coronavirus even after adjusting for other possible confounders. Just 29% of White, 25.5% of Hispanic, and 18.7% of Black service members had initiated the vaccine process in the survey.6
The authors suggest that in part, vaccine hesitancy explains the findings.4 Vaccine hesitancy among racial and ethnic minorities is even more tragic because these same already disadvantaged cohorts have disproportionately suffered from COVID-19 throughout the pandemic with higher rates of infection, serious illness requiring hospitalization, and infection-related morbidity.7
Vaccine hesitancy, delay, or refusal in Black Americans whether military or civilian often is attributed to the historical abuses like the Tuskegee syphilis experiments or the more recent example of cancer cell lines taken from Henrietta Lacks without consent.8 Such government sponsored betrayals no doubt are the soil in which hesitancy grows but recent commentators have opined that focusing solely on these infamous examples may ignore current systemic racism that is pervasively feeding Black Americans reluctance to consider or accept COVID-19 vaccination.9 Blaming infamous research also provides a convenient excuse for confronting contemporary racial discrimination in health care and taking responsibility as health care practitioners for reversing it. “Framing the conversation about distrust in COVID vaccines in terms of everyday racism rather than historical atrocities may increase underserved communities’ willingness to be vaccinated,” Bajaj and Stanford wrote in a recent recent New England Journal of Medicine commentary. “When we hyperfocus on Sims, Lacks, and Tuskegee, we ascribe the current Black health experience to past racism, rooting our present in immovable historical occurrences and undermining efforts to combat mistrust. Everyday racism, by contrast, can be tackled in the present.”9
The study of racial/ethnic disparities in COVID-19 vaccination in active-duty service members was a work product of the Armed Forces Health Surveillance Division. The authors underscore several factors that support the connection between discrimination and vaccine hesitancy in the military. Lack of access to and ability to obtain COVID-19 vaccination continues to be a major barrier that disadvantaged populations must overcome.10 The COVID-19 vaccine is widely available, easily obtained, and free of charge for all military personnel. Yet the vaccine hesitancy in the military parallels that of the civilian sector. This led the study authors to opine that, “forces external to the U.S. Military, such as interpersonal and societal factors also contribute to vaccine hesitancy among military service members.”6
Obviously, any unvaccinated active-duty service member reduces the combat readiness of the fighting force a consideration that led some in Congress to call for mandating vaccination. The vaccine is currently being administered under an emergency use authorization (EUA), which prevents even the military from mandating it.11 Even if President Joseph Biden obtained a waiver to make the vaccine mandatory, the implications of forcing service members who have volunteered to serve their country is ethically problematic. Those problems are exponentially amplified when applied to members of ethnic and racial minorities who have a past and present of health disparities and discrimination. Respecting the decision of those in uniform to decline COVID-19 vaccination is the first and perhaps most important step to rebuilding the trust that is the most promising means of reducing vaccine hesitancy.
Part of the accountability we all bear for health care inequity and racism is to continue the work of this landmark study to better understand vaccine hesitancy among military and veteran cohorts, develop counseling and education that target those attitudes, beliefs, and motivations with education, counseling, and support. All of us can in some small measure follow the ethical mandate “to dispel rumors and provide facts to people” of Secretary Austin, a Black retired 4-star Army general.1
1. Garmone J. Secretary of Defense Addresses Vaccine Hesitancy in the Military. Published February 25, 2021. Accessed May 26, 2021. https://www.defense.gov/Explore/News/Article/Article/2516511/secretary-of-defense-addresses-vaccine-hesitancy-in-military/
2. National Academies of Sciences, Engineering, and Medicine. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies of Science; 2020:188. doi:10.17226/25917
3. Liebermann O. US military sees 55% jump in COVID-19 vaccinations over last month. Published May 20, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/05/20/politics/us-military-covid-vaccinations/index.html
4. Kime P. Almost one-third of us troops are refusing COVID-19 vaccines, officials Say. Published February 17, 2021. Accessed May 26, 2021. https://www.military.com/daily-news/2021/02/17/almost-one-third-of-us-troops-are-refusing-covid-vaccines-officials-say.html
5. Elbeshbishi S. Nearly 40% of Marines decline COVID-19 vaccine, prompting some Democrats to urge Biden to set mandate for the military. USA Today. April 10, 2021. Accessed May 26, 2021. https://www.usatoday.com/story/news/politics/2021/04/10/covid-vaccine-nearly-forty-percent-us-marines-decline/7173918002/
6. Lang MA, Stahlman S, Wells NY, et al. Disparities in COVID-19 vaccine initiation and completion among active component service members and health care personnel, 11 December 2020-12 March 2021. MSMR. 2021;28(4):2-9.
7. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA . 2020;323(24):2466-2467. doi:10.1001/jama.2020.8598
8. Kum D. Fueled by a history of mistreatment, Black Americans distrust the new COVID-19 vaccines. TIME. December 8, 2020. Accessed May 26, 2021.https://time.com/5925074/black-americans-covid-19-vaccine-distrust/
9. Bajaj SS, Stanford FC. Beyond Tuskegee - Vaccine Distrust and Everyday Racism. N Engl J Med. 2021;384(5):e12. doi:10.1056/NEJMpv2035827
10. Feldman N. Why Black and Latino people still lag on COVID-19 vaccines-and how to fix it. NPR. April 26, 2021. Accessed May 26, 2021. https://www.npr.org/sections/health-shots/2021/04/26/989962041/why-black-and-latino-people-still-lag-on-covid-vaccines-and-how-to-fix-it
11. Kaufman E. Lawmakers ask Biden to issue waiver to make COVID-19 vaccination mandatory of members of the military. Updated March 24, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/03/24/politics/congress-letter-military-vaccine/index.html
1. Garmone J. Secretary of Defense Addresses Vaccine Hesitancy in the Military. Published February 25, 2021. Accessed May 26, 2021. https://www.defense.gov/Explore/News/Article/Article/2516511/secretary-of-defense-addresses-vaccine-hesitancy-in-military/
2. National Academies of Sciences, Engineering, and Medicine. Framework for Equitable Allocation of COVID-19 Vaccine . The National Academies of Science; 2020:188. doi:10.17226/25917
3. Liebermann O. US military sees 55% jump in COVID-19 vaccinations over last month. Published May 20, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/05/20/politics/us-military-covid-vaccinations/index.html
4. Kime P. Almost one-third of us troops are refusing COVID-19 vaccines, officials Say. Published February 17, 2021. Accessed May 26, 2021. https://www.military.com/daily-news/2021/02/17/almost-one-third-of-us-troops-are-refusing-covid-vaccines-officials-say.html
5. Elbeshbishi S. Nearly 40% of Marines decline COVID-19 vaccine, prompting some Democrats to urge Biden to set mandate for the military. USA Today. April 10, 2021. Accessed May 26, 2021. https://www.usatoday.com/story/news/politics/2021/04/10/covid-vaccine-nearly-forty-percent-us-marines-decline/7173918002/
6. Lang MA, Stahlman S, Wells NY, et al. Disparities in COVID-19 vaccine initiation and completion among active component service members and health care personnel, 11 December 2020-12 March 2021. MSMR. 2021;28(4):2-9.
7. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA . 2020;323(24):2466-2467. doi:10.1001/jama.2020.8598
8. Kum D. Fueled by a history of mistreatment, Black Americans distrust the new COVID-19 vaccines. TIME. December 8, 2020. Accessed May 26, 2021.https://time.com/5925074/black-americans-covid-19-vaccine-distrust/
9. Bajaj SS, Stanford FC. Beyond Tuskegee - Vaccine Distrust and Everyday Racism. N Engl J Med. 2021;384(5):e12. doi:10.1056/NEJMpv2035827
10. Feldman N. Why Black and Latino people still lag on COVID-19 vaccines-and how to fix it. NPR. April 26, 2021. Accessed May 26, 2021. https://www.npr.org/sections/health-shots/2021/04/26/989962041/why-black-and-latino-people-still-lag-on-covid-vaccines-and-how-to-fix-it
11. Kaufman E. Lawmakers ask Biden to issue waiver to make COVID-19 vaccination mandatory of members of the military. Updated March 24, 2021. Accessed May 26, 2021. https://www.cnn.com/2021/03/24/politics/congress-letter-military-vaccine/index.html
By the numbers: Children and COVID-19 prevention
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
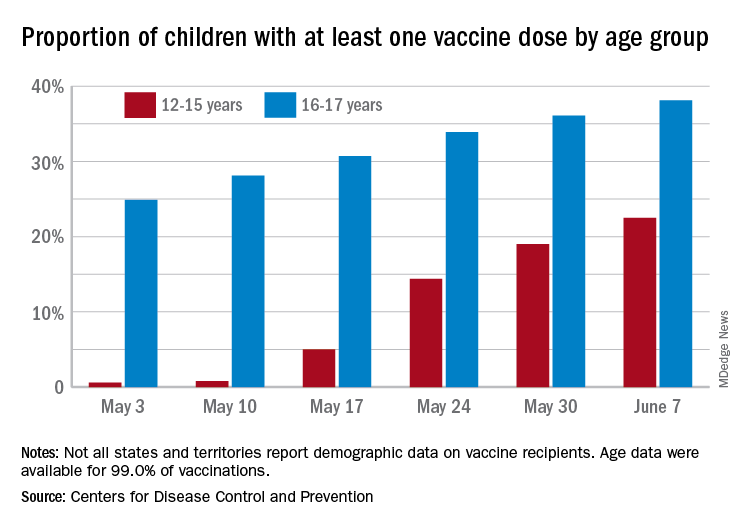
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
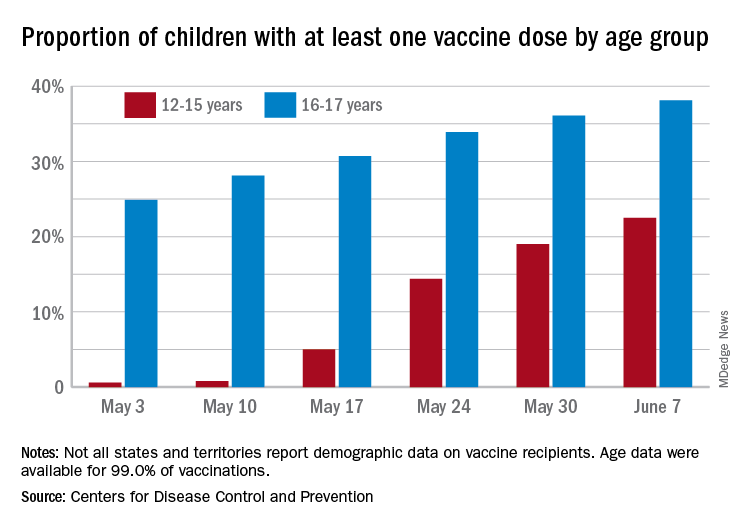
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
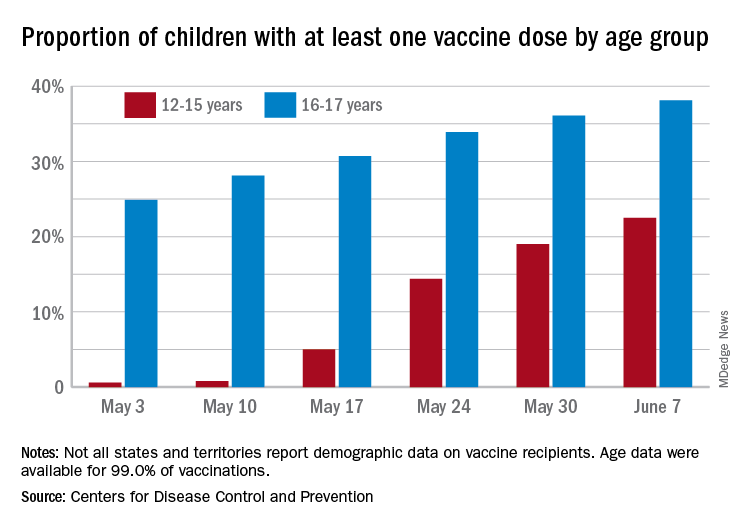
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
CDC director cites rise in hospitalizations in urging teen vaccinations
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
Patients with RA on rituximab at risk for worse COVID-19 outcomes
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
FROM THE EULAR 2021 CONGRESS
A primer on COVID-19 in hospitalized children
Converge 2021 session
COVID-19 in Children
Presenter
Philip Zachariah, MD, MPH
Session summary
Children have been less severely affected by COVID-19 than adults (hospitalization rates around 5%). However, once hospitalized, ICU admission rates in children have been similar to adults, around 30%. Mortality has been 1%-2%. Risk factors for more severe acute SARS CoV-2 infections include age extremes, minorities, obesity, medical complexity, immunocompromised pediatric patients, and asthma.
Multisystem-inflammatory-syndrome-in-children (MIS-C) continues to present among persistently febrile children with multisystem findings and the history of acute COVID-19 infection in prior 3-6 weeks. There seems to be a link between the immunological defects in type I and II interferon production, as autoantibodies to type I interferon may predispose to severe disease. Dr. Zachariah of Columbia University Medical Center in New York, discussed the recent study exploring intravenous immunoglobulin (IVIG) alone versus IVIG and steroids as treatment options for MIS-C. So far, the failure rates in IVIG-alone group were higher (51%) versus IVIG and steroids (9%).
Besides MIS-C, many neurological manifestations of COVID-19 have been seen among children including GBS, seizures, encephalitis, cranial neuropathies, and demyelination cases. Diabetic ketoacidosis (DKA), secondary hemophagocytic lymphohistiocytosis (HLH), and pseudo-appendicitis have all been described in the literature, however, larger case control studied are needed.
In children, clinical vascular thrombotic events (VTEs) are rare. Anticoagulant thromboprophylaxis is suggested for hospitalized patients with COVID-19–related illness, whose D-dimer is >5 times upper limit of normal values and who have one or more non–COVID-19 related clinical risk factors for hospital acquired VTEs.
Key takeaways
- Once hospitalized, the ICU admission rates for children have been similar to those in adults, ~30%.
- MIS-C is showing lower failure rates if treated with IVIG and steroids, and most reliable laboratory findings should be elevated C-reactive protein, lymphopenia, and elevated brain natriuretic peptide.
- In hospitalized children with COVID-19, clinical VTEs are rare.
Dr. Giordano is an associate professor of pediatrics at Columbia University Medical Center in New York. She is a pediatric hospitalist with expertise in pediatric surgical comanagement
Converge 2021 session
COVID-19 in Children
Presenter
Philip Zachariah, MD, MPH
Session summary
Children have been less severely affected by COVID-19 than adults (hospitalization rates around 5%). However, once hospitalized, ICU admission rates in children have been similar to adults, around 30%. Mortality has been 1%-2%. Risk factors for more severe acute SARS CoV-2 infections include age extremes, minorities, obesity, medical complexity, immunocompromised pediatric patients, and asthma.
Multisystem-inflammatory-syndrome-in-children (MIS-C) continues to present among persistently febrile children with multisystem findings and the history of acute COVID-19 infection in prior 3-6 weeks. There seems to be a link between the immunological defects in type I and II interferon production, as autoantibodies to type I interferon may predispose to severe disease. Dr. Zachariah of Columbia University Medical Center in New York, discussed the recent study exploring intravenous immunoglobulin (IVIG) alone versus IVIG and steroids as treatment options for MIS-C. So far, the failure rates in IVIG-alone group were higher (51%) versus IVIG and steroids (9%).
Besides MIS-C, many neurological manifestations of COVID-19 have been seen among children including GBS, seizures, encephalitis, cranial neuropathies, and demyelination cases. Diabetic ketoacidosis (DKA), secondary hemophagocytic lymphohistiocytosis (HLH), and pseudo-appendicitis have all been described in the literature, however, larger case control studied are needed.
In children, clinical vascular thrombotic events (VTEs) are rare. Anticoagulant thromboprophylaxis is suggested for hospitalized patients with COVID-19–related illness, whose D-dimer is >5 times upper limit of normal values and who have one or more non–COVID-19 related clinical risk factors for hospital acquired VTEs.
Key takeaways
- Once hospitalized, the ICU admission rates for children have been similar to those in adults, ~30%.
- MIS-C is showing lower failure rates if treated with IVIG and steroids, and most reliable laboratory findings should be elevated C-reactive protein, lymphopenia, and elevated brain natriuretic peptide.
- In hospitalized children with COVID-19, clinical VTEs are rare.
Dr. Giordano is an associate professor of pediatrics at Columbia University Medical Center in New York. She is a pediatric hospitalist with expertise in pediatric surgical comanagement
Converge 2021 session
COVID-19 in Children
Presenter
Philip Zachariah, MD, MPH
Session summary
Children have been less severely affected by COVID-19 than adults (hospitalization rates around 5%). However, once hospitalized, ICU admission rates in children have been similar to adults, around 30%. Mortality has been 1%-2%. Risk factors for more severe acute SARS CoV-2 infections include age extremes, minorities, obesity, medical complexity, immunocompromised pediatric patients, and asthma.
Multisystem-inflammatory-syndrome-in-children (MIS-C) continues to present among persistently febrile children with multisystem findings and the history of acute COVID-19 infection in prior 3-6 weeks. There seems to be a link between the immunological defects in type I and II interferon production, as autoantibodies to type I interferon may predispose to severe disease. Dr. Zachariah of Columbia University Medical Center in New York, discussed the recent study exploring intravenous immunoglobulin (IVIG) alone versus IVIG and steroids as treatment options for MIS-C. So far, the failure rates in IVIG-alone group were higher (51%) versus IVIG and steroids (9%).
Besides MIS-C, many neurological manifestations of COVID-19 have been seen among children including GBS, seizures, encephalitis, cranial neuropathies, and demyelination cases. Diabetic ketoacidosis (DKA), secondary hemophagocytic lymphohistiocytosis (HLH), and pseudo-appendicitis have all been described in the literature, however, larger case control studied are needed.
In children, clinical vascular thrombotic events (VTEs) are rare. Anticoagulant thromboprophylaxis is suggested for hospitalized patients with COVID-19–related illness, whose D-dimer is >5 times upper limit of normal values and who have one or more non–COVID-19 related clinical risk factors for hospital acquired VTEs.
Key takeaways
- Once hospitalized, the ICU admission rates for children have been similar to those in adults, ~30%.
- MIS-C is showing lower failure rates if treated with IVIG and steroids, and most reliable laboratory findings should be elevated C-reactive protein, lymphopenia, and elevated brain natriuretic peptide.
- In hospitalized children with COVID-19, clinical VTEs are rare.
Dr. Giordano is an associate professor of pediatrics at Columbia University Medical Center in New York. She is a pediatric hospitalist with expertise in pediatric surgical comanagement
FROM SHM CONVERGE 2021












