User login
Jornay PM improves classroom functioning in ADHD
SEATTLE – A novel formulation of methylphenidate could provide morning relief to pediatric patients with attention-deficit/hyperactivity disorder, according to results of a pivotal phase 3 classroom trial.
In the study, delayed release/extended release methylphenidate (DR/ER MPH), when taken the night before, improved ADHD symptoms throughout a 12-hour laboratory classroom period – including in the late afternoons and early mornings.
The formulation, also known as Jornay PM, received Food and Drug Administration approval for ADHD in August for patients aged 6 and older. “For kids who have a horrendous time in the morning, getting up out of bed, and getting ready for school, they get up and they’re ready to rock and roll. [The drug] makes the mornings go better,” Ann Childress, MD, said in an interview at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
In a previous phase 3 trial, DR/ER MPH proved beneficial in late afternoon and early morning symptoms in a naturalistic sample over a 3- week treatment course (J Child Adolesc Pharmacol. 2017 Aug 1;27[6]:474-82). The current work sought to show its value in a classroom setting. And in yet another earlier survey, 77% of parents rated early morning functional impairment in children with ADHD as moderate to severe (J Child Adolesc Pharmacol. 2017 Oct 1;27[8]:715-22).
“,” said Dr. Childress, president of the Center for Psychiatry and Behavioral Medicine in Las Vegas.
In the current study, presented by Dr. Childress at the meeting, 117 children aged 6-12 years with ADHD and morning behavioral problems, after a 5-day washout period, were started on an evening DR/ER MPH dose of 20 mg or 40 mg. They were then seen for up to 4 more weeks, and doses optimized (maximum 100 mg/day).
Adjustments also were made in the evening dose schedule to determine an optimal dosing time, which had to range from 6:30 pm to 9:30 pm, at least 1 hour after dinner. Clinicians optimized the dose and timing to achieve maximum symptom control throughout the day (minimum 30% improvement in total symptom score from baseline), while remaining safe and well-tolerated.The participants were then randomized to maintain the current drug dose, or to switch to placebo for 1 week. The primary endpoint was the average of all post-dose SKAMP-CS (Swanson, Kotkin, Agler, M-Flynn, and Pelham combined scale) measurements, as recorded by a trained, independent observer during the 12-hour period on the last classroom day.
There was a significant improvement in the primary measure, with the treatment group averaging 14.8 on the SKAMP-CS, compared with 20.7 for the placebo group (P less than .001). The improved outcomes were steady throughout the day, failing to achieve statistical significance at 8 a.m., but achieving significance in measurements taken at 9 a.m.,10 a.m., 12 p.m., 2 pm, 4 p.m., 6 p.m., and 7 p.m.
The formulation also achieved significant difference in morning and late afternoon measurements of the Parent Rating of Evening and Morning Behavior Scale, Revised (PREMB-R AM and PREMB-R PM). The treatment group scored a mean of 0.9 on PREMB-R AM, compared with 2.7 for placebo (P less than .001), and 6.1 vs. 9.3 in the PREMB-R PM scale (P = .003).
Most treatment emergent adverse events were considered mild or moderate, and occurred in 36.9% of the treatment group and 40.7% of placebo subjects.
The study was funded by Ironshore Pharmaceuticals, which said in a press statement that it plans to launch the drug early next year. In addition to Ironshore, Dr. Childress has served on the advisory board for, consulted for, or received research support from Aevi Genomic Medicine, Akili Interactive, Alcobra, Arbor Pharmaceuticals, Eli Lilly, Forest Laboratories, Lundbeck, KemPharm, Neos Therapeutics, Noven Pharmaceuticals, Otsuka America Pharmaceutical, Pearson, Pfizer, Purdue Pharma, Rhodes Pharmaceuticals, Shire, Sunovion, and Tris Pharma.
SEATTLE – A novel formulation of methylphenidate could provide morning relief to pediatric patients with attention-deficit/hyperactivity disorder, according to results of a pivotal phase 3 classroom trial.
In the study, delayed release/extended release methylphenidate (DR/ER MPH), when taken the night before, improved ADHD symptoms throughout a 12-hour laboratory classroom period – including in the late afternoons and early mornings.
The formulation, also known as Jornay PM, received Food and Drug Administration approval for ADHD in August for patients aged 6 and older. “For kids who have a horrendous time in the morning, getting up out of bed, and getting ready for school, they get up and they’re ready to rock and roll. [The drug] makes the mornings go better,” Ann Childress, MD, said in an interview at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
In a previous phase 3 trial, DR/ER MPH proved beneficial in late afternoon and early morning symptoms in a naturalistic sample over a 3- week treatment course (J Child Adolesc Pharmacol. 2017 Aug 1;27[6]:474-82). The current work sought to show its value in a classroom setting. And in yet another earlier survey, 77% of parents rated early morning functional impairment in children with ADHD as moderate to severe (J Child Adolesc Pharmacol. 2017 Oct 1;27[8]:715-22).
“,” said Dr. Childress, president of the Center for Psychiatry and Behavioral Medicine in Las Vegas.
In the current study, presented by Dr. Childress at the meeting, 117 children aged 6-12 years with ADHD and morning behavioral problems, after a 5-day washout period, were started on an evening DR/ER MPH dose of 20 mg or 40 mg. They were then seen for up to 4 more weeks, and doses optimized (maximum 100 mg/day).
Adjustments also were made in the evening dose schedule to determine an optimal dosing time, which had to range from 6:30 pm to 9:30 pm, at least 1 hour after dinner. Clinicians optimized the dose and timing to achieve maximum symptom control throughout the day (minimum 30% improvement in total symptom score from baseline), while remaining safe and well-tolerated.The participants were then randomized to maintain the current drug dose, or to switch to placebo for 1 week. The primary endpoint was the average of all post-dose SKAMP-CS (Swanson, Kotkin, Agler, M-Flynn, and Pelham combined scale) measurements, as recorded by a trained, independent observer during the 12-hour period on the last classroom day.
There was a significant improvement in the primary measure, with the treatment group averaging 14.8 on the SKAMP-CS, compared with 20.7 for the placebo group (P less than .001). The improved outcomes were steady throughout the day, failing to achieve statistical significance at 8 a.m., but achieving significance in measurements taken at 9 a.m.,10 a.m., 12 p.m., 2 pm, 4 p.m., 6 p.m., and 7 p.m.
The formulation also achieved significant difference in morning and late afternoon measurements of the Parent Rating of Evening and Morning Behavior Scale, Revised (PREMB-R AM and PREMB-R PM). The treatment group scored a mean of 0.9 on PREMB-R AM, compared with 2.7 for placebo (P less than .001), and 6.1 vs. 9.3 in the PREMB-R PM scale (P = .003).
Most treatment emergent adverse events were considered mild or moderate, and occurred in 36.9% of the treatment group and 40.7% of placebo subjects.
The study was funded by Ironshore Pharmaceuticals, which said in a press statement that it plans to launch the drug early next year. In addition to Ironshore, Dr. Childress has served on the advisory board for, consulted for, or received research support from Aevi Genomic Medicine, Akili Interactive, Alcobra, Arbor Pharmaceuticals, Eli Lilly, Forest Laboratories, Lundbeck, KemPharm, Neos Therapeutics, Noven Pharmaceuticals, Otsuka America Pharmaceutical, Pearson, Pfizer, Purdue Pharma, Rhodes Pharmaceuticals, Shire, Sunovion, and Tris Pharma.
SEATTLE – A novel formulation of methylphenidate could provide morning relief to pediatric patients with attention-deficit/hyperactivity disorder, according to results of a pivotal phase 3 classroom trial.
In the study, delayed release/extended release methylphenidate (DR/ER MPH), when taken the night before, improved ADHD symptoms throughout a 12-hour laboratory classroom period – including in the late afternoons and early mornings.
The formulation, also known as Jornay PM, received Food and Drug Administration approval for ADHD in August for patients aged 6 and older. “For kids who have a horrendous time in the morning, getting up out of bed, and getting ready for school, they get up and they’re ready to rock and roll. [The drug] makes the mornings go better,” Ann Childress, MD, said in an interview at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
In a previous phase 3 trial, DR/ER MPH proved beneficial in late afternoon and early morning symptoms in a naturalistic sample over a 3- week treatment course (J Child Adolesc Pharmacol. 2017 Aug 1;27[6]:474-82). The current work sought to show its value in a classroom setting. And in yet another earlier survey, 77% of parents rated early morning functional impairment in children with ADHD as moderate to severe (J Child Adolesc Pharmacol. 2017 Oct 1;27[8]:715-22).
“,” said Dr. Childress, president of the Center for Psychiatry and Behavioral Medicine in Las Vegas.
In the current study, presented by Dr. Childress at the meeting, 117 children aged 6-12 years with ADHD and morning behavioral problems, after a 5-day washout period, were started on an evening DR/ER MPH dose of 20 mg or 40 mg. They were then seen for up to 4 more weeks, and doses optimized (maximum 100 mg/day).
Adjustments also were made in the evening dose schedule to determine an optimal dosing time, which had to range from 6:30 pm to 9:30 pm, at least 1 hour after dinner. Clinicians optimized the dose and timing to achieve maximum symptom control throughout the day (minimum 30% improvement in total symptom score from baseline), while remaining safe and well-tolerated.The participants were then randomized to maintain the current drug dose, or to switch to placebo for 1 week. The primary endpoint was the average of all post-dose SKAMP-CS (Swanson, Kotkin, Agler, M-Flynn, and Pelham combined scale) measurements, as recorded by a trained, independent observer during the 12-hour period on the last classroom day.
There was a significant improvement in the primary measure, with the treatment group averaging 14.8 on the SKAMP-CS, compared with 20.7 for the placebo group (P less than .001). The improved outcomes were steady throughout the day, failing to achieve statistical significance at 8 a.m., but achieving significance in measurements taken at 9 a.m.,10 a.m., 12 p.m., 2 pm, 4 p.m., 6 p.m., and 7 p.m.
The formulation also achieved significant difference in morning and late afternoon measurements of the Parent Rating of Evening and Morning Behavior Scale, Revised (PREMB-R AM and PREMB-R PM). The treatment group scored a mean of 0.9 on PREMB-R AM, compared with 2.7 for placebo (P less than .001), and 6.1 vs. 9.3 in the PREMB-R PM scale (P = .003).
Most treatment emergent adverse events were considered mild or moderate, and occurred in 36.9% of the treatment group and 40.7% of placebo subjects.
The study was funded by Ironshore Pharmaceuticals, which said in a press statement that it plans to launch the drug early next year. In addition to Ironshore, Dr. Childress has served on the advisory board for, consulted for, or received research support from Aevi Genomic Medicine, Akili Interactive, Alcobra, Arbor Pharmaceuticals, Eli Lilly, Forest Laboratories, Lundbeck, KemPharm, Neos Therapeutics, Noven Pharmaceuticals, Otsuka America Pharmaceutical, Pearson, Pfizer, Purdue Pharma, Rhodes Pharmaceuticals, Shire, Sunovion, and Tris Pharma.
REPORTING FROM AACAP 2018
Key clinical point: Children who took the formulation experienced improved, steady outcomes throughout the day.
Major finding: The treatment group scored an average of 0.9 on the PREMB-R morning test, compared with 2.7 in the placebo group.
Study details: Randomized, controlled trial involving 117 patients.
Disclosures: The study was funded by Ironshore Pharmaceuticals, which said in a press statement that it plans to launch the drug early next year. In addition to Ironshore, Dr. Childress has served on the advisory board for, consulted for, or received research support from Aevi Genomic Medicine, Akili Interactive, Alcobra, Arbor Pharmaceuticals, Eli Lilly, Forest Laboratories, Lundbeck, KemPharm, Neos Therapeutics, Noven Pharmaceuticals, Otsuka America Pharmaceutical, Pearson, Pfizer, Purdue Pharma, Rhodes Pharmaceuticals, Shire, Sunovion, and Tris Pharma.
Adult ADHD? Screen for hoarding symptoms
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
BARCELONA – Clinically meaningful hoarding symptoms are present in roughly one in four adults with attention-deficit/hyperactivity disorder, Sharon Morein-Zamir, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
Her message to her fellow clinicians: “Nobody tends to ask about hoarding problems in adult ADHD clinics. Ask your ADHD patients carefully and routinely about hoarding symptoms. Screen them for it, ask their family members about it, and see whether it could be a problem contributing to daily impairment,” urged Dr. Morein-Zamir, a senior lecturer in clinical psychology at Anglia Ruskin University in Cambridge, England.
The clinician must broach the subject, because hoarding often is characterized by lack of insight.
“Patients don’t complain about it. You’ll have family members complain about it, neighbors complain about it, maybe social services, but the individuals themselves often don’t think they have a problem. And if they acknowledge it, they don’t seek treatment for it. So you really need to actively ask about the issue. They won’t raise it themselves,” she said.
Hoarding disorder and ADHD are considered two separate entities. But her study demonstrated that they share a common link: inattention symptoms.
the psychologist continued.
Indeed, one of the reasons why hoarding disorder is no longer grouped with obsessive-compulsive disorder in diagnostic schema is that inattention symptoms are not characteristic of OCD.
Dr. Morein-Zamir presented a cross-sectional study of 50 patients in an adult ADHD clinic and 46 age- and sex-matched controls. A total of 22 of the ADHD patients were on methylphenidate, 15 on selective serotonin reuptake inhibitors, 6 on amphetamine, and 7 were unmedicated.
Participants were assessed for hoarding using two validated measures well-suited for screening in daily practice: the Saving Inventory–Revised (SIR) and the Clutter Image Rating (CIR). Clinically meaningful hoarding symptoms – a designation requiring both a score of at least 42 on the SIR and 12 on the CIR – were present in 11 of 50 adult ADHD patients and none of the controls.
The group with clinically meaningful hoarding symptoms differed from the 39 ADHD patients without hoarding most noticeably in their more pronounced inattention symptoms as scored on the Adult ADHD Self-Report Scale (ASRS): a mean score of 32.8, compared with 28.8 in ADHD patients without clinically important hoarding. In contrast, the two groups scored similarly for hyperactivity/impulsivity on the patient-completed 18-item ASRS, as well as for depression and anxiety on the Depression Anxiety Stress Scales (DASS).
Within the ADHD group, only inattention as measured on the ASRS predicted hoarding severity on the SIR. In a multivariate regression analysis controlling for age, sex, hyperactivity/impulsivity on the ASRS, and DASS scores, inattention correlated strongly with all of the key hoarding dimensions: clutter, excessive acquisition, and difficulty discarding. Hyperactivity/impulsivity showed a modest correlation with clutter but not with the other hoarding dimensions.
Dr. Morein-Zamir observed that, while the last 3 or so years have seen booming interest in the development of manualized cognitive-behavioral therapy strategies for hoarding disorder, it’s not yet known whether those tools will be effective for treating high-level hoarding symptoms in patients with ADHD.
She reported having no financial conflicts regarding her study, which was funded by the British Academy.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Routinely screen adults with ADHD for hoarding disorder.
Major finding: Eleven of 50 (22%) unselected adults with ADHD displayed clinically meaningful hoarding symptoms.
Study details: This cross-sectional study included 50 adult ADHD patients and 46 matched controls who were assessed for hoarding symptoms and inattention.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was funded by the British Academy.
ADHD in the long term
Parents whose kids are diagnosed with ADHD face important questions about what to expect in the long term and how that might inform treatment. Studies find that ADHD diagnosed in childhood tends to persist in up to 65% of adolescents (some estimates are lower depending on criteria used),1 and about 50% of people are estimated to continue to meet criteria for ADHD as adults.2 Many studies have attempted to understand what long-term risks are associated with ADHD, as well as the factors that help better predict which characteristics in childhood might predict those risks. A recent article was published on a cohort of boys followed over 33 years.3 This, as well as other large prospective studies, such as the Multimodal Treatment of ADHD (MTA) provide us with helpful long-range data that inform this article.4-6 This article reviews risks in adolescence and adulthood and the factors thought to be associated with them.
What predicts persistence of ADHD symptoms in adolescence?
Several factors emerge consistently, including higher symptom severity, comorbid conduct disorder, and lower childhood IQ; other findings include family-related factors, such as lower parental mental health, less-positive parenting, and lower rates of parental education. In general, hyperactivity and impulsivity wanes, while inattention symptoms remain more stable.
What does ADHD predict for adolescents?
Adolescents with ADHD are more than twice as likely to be involved in pregnancies under the age of 18 years, true for both male and female genders.7 This finding also is associated with increased substance use and low academic achievement but not completely explained by it. Adolescents with persistent ADHD symptoms experience poorer educational success than do kids without ADHD symptoms, according to teacher reports of performance and measurements of grade point average. They are more likely to repeat a grade.8 Related but independent is the relationship of substance use disorders in kids with ADHD. Adolescents with ADHD are more likely to use nicotine or marijuana or meet criteria for any substance use disorder than adolescents without ADHD. Finally, adolescents aged 12-18 years with ADHD are at higher risk for motor vehicle accidents and all types of accidental injuries.9
What predicts persistence of ADHD symptoms in adulthood?
A follow-up study of the MTA trial 16 years later looked at ADHD diagnosed before age 12 years and the association with symptom persistence in adulthood, defined by the DSM-5 cutoff criteria of five symptoms. The following factors related to symptom persistence: childhood psychiatric comorbidity, higher ADHD symptom severity, and parental mental health problems. Notably, family socioeconomic status, child IQ, and parental education were not associated. In addition to looking at symptom persistence, other studies have looked at predictors of functional impairment in adulthood following a childhood ADHD diagnosis (independent of whether people continue to meet criteria for the disorder). The main findings that seem consistently related to all functional outcomes, including social, occupational, and educational, are lower childhood IQ and history of conduct problems (in the absence of meeting criteria for full childhood conduct disorder). Educational family-related factors, such as socioeconomic status and lower parental education, were related to lower educational functioning only.
What does ADHD predict for adults?
It appears that overall, adults who were diagnosed with ADHD as children show poorer functional outcomes than did those who weren’t, and there is a step-wise relationship when considering adults whose symptoms persist, with more severe outcomes compared with adults whose symptoms have desisted, who in turn have worse outcomes than adults who were never diagnosed with ADHD. Educational attainments follow this pattern with the highest average levels of education in the non-ADHD group and the lowest average years in the group with persistent symptoms. Occupational success and percent receiving public assistance again separated between each group, with the symptom persisters faring the worst, the symptom desisters better, and those never affected by ADHD, the best. In terms of emotional disorders, it was only the symptom persisters who suffered from higher rates of mood and anxiety disorders. Similarly, only the symptom persisters had significantly more marijuana use disorders. No other substance use disorders or legal outcomes were significant.
How does this affect how we approach treatment?
Clinicians and researchers who specialize in ADHD have been arguing for ADHD to be treated as more of a chronic disease and for impairment to be the focus of treatment, rather than simply symptom control.10 With what we know about long-term functional impairment, there is reason to consider a more holistic picture of a child or an adolescent and how they are functioning in their academic, emotional, and social domains. A meta-analysis of treatment and long-term outcomes suggests that psychostimulant treatment, psychotherapy treatment, and combined treatment all improve long-term functioning, especially self-esteem, social functioning, and academic functioning, with combined psychotherapeutic and pharmacologic treatments associated with the highest effect sizes.11
For those who treat ADHD, it is our job to provide education to families about the chronic risks associated with the diagnosis, and the importance of offering multimodal therapy that can address family factors that might be contributing to risks, as well as the child’s overall well-being. If we are to make sense of how adults may experience impairment even in the absence of ongoing symptoms, we might look at how their overall wellness was interrupted during development. Maybe they fell into a different crowd of kids? Maybe they stopped achieving at school in a way that changed the achievement trajectory they were on? Maybe they impulsively picked up substances or got in trouble with the law? These events can have lasting impacts on well-being. We must use medicine and psychotherapy to help with symptoms, but we must look beyond treating illness and use evidence-based strategies to promote wellness at the level of the entire family.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. She works with children and adolescents as well as women in the perinatal period. She has no relevant financial disclosures.
References
1. Psychol Med. 2006 Feb;36(2):159-65.
2. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):937-44.e4.
3. J Am Acad Child Adolesc Psychiatry. 2018 Aug;57(8):571-82.e1.
4. J Am Acad Child Adolesc Psychiatry. 2017 Aug;56(8):687-95.e7.
5. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):945-52.e2.
6. J Am Acad Child Adolesc Psychiatry. 2009 May;48(5):484-500.
7. J Atten Disord. 2017 Sep 1:1087054717730610. doi: 10.1177/1087054717730610.
8. J Atten Disord. 2016 May;20(5):383-9.
9. Eur Child Adolesc Psychiatry. 2014 Feb;23(2):95-102.
10. JAMA Pediatr. 2018 Aug 13. doi: 10.1001/jamapediatrics.2018.1642.
11. PLoS One. 2015 Feb 25;10(2):e0116407.
Parents whose kids are diagnosed with ADHD face important questions about what to expect in the long term and how that might inform treatment. Studies find that ADHD diagnosed in childhood tends to persist in up to 65% of adolescents (some estimates are lower depending on criteria used),1 and about 50% of people are estimated to continue to meet criteria for ADHD as adults.2 Many studies have attempted to understand what long-term risks are associated with ADHD, as well as the factors that help better predict which characteristics in childhood might predict those risks. A recent article was published on a cohort of boys followed over 33 years.3 This, as well as other large prospective studies, such as the Multimodal Treatment of ADHD (MTA) provide us with helpful long-range data that inform this article.4-6 This article reviews risks in adolescence and adulthood and the factors thought to be associated with them.
What predicts persistence of ADHD symptoms in adolescence?
Several factors emerge consistently, including higher symptom severity, comorbid conduct disorder, and lower childhood IQ; other findings include family-related factors, such as lower parental mental health, less-positive parenting, and lower rates of parental education. In general, hyperactivity and impulsivity wanes, while inattention symptoms remain more stable.
What does ADHD predict for adolescents?
Adolescents with ADHD are more than twice as likely to be involved in pregnancies under the age of 18 years, true for both male and female genders.7 This finding also is associated with increased substance use and low academic achievement but not completely explained by it. Adolescents with persistent ADHD symptoms experience poorer educational success than do kids without ADHD symptoms, according to teacher reports of performance and measurements of grade point average. They are more likely to repeat a grade.8 Related but independent is the relationship of substance use disorders in kids with ADHD. Adolescents with ADHD are more likely to use nicotine or marijuana or meet criteria for any substance use disorder than adolescents without ADHD. Finally, adolescents aged 12-18 years with ADHD are at higher risk for motor vehicle accidents and all types of accidental injuries.9
What predicts persistence of ADHD symptoms in adulthood?
A follow-up study of the MTA trial 16 years later looked at ADHD diagnosed before age 12 years and the association with symptom persistence in adulthood, defined by the DSM-5 cutoff criteria of five symptoms. The following factors related to symptom persistence: childhood psychiatric comorbidity, higher ADHD symptom severity, and parental mental health problems. Notably, family socioeconomic status, child IQ, and parental education were not associated. In addition to looking at symptom persistence, other studies have looked at predictors of functional impairment in adulthood following a childhood ADHD diagnosis (independent of whether people continue to meet criteria for the disorder). The main findings that seem consistently related to all functional outcomes, including social, occupational, and educational, are lower childhood IQ and history of conduct problems (in the absence of meeting criteria for full childhood conduct disorder). Educational family-related factors, such as socioeconomic status and lower parental education, were related to lower educational functioning only.
What does ADHD predict for adults?
It appears that overall, adults who were diagnosed with ADHD as children show poorer functional outcomes than did those who weren’t, and there is a step-wise relationship when considering adults whose symptoms persist, with more severe outcomes compared with adults whose symptoms have desisted, who in turn have worse outcomes than adults who were never diagnosed with ADHD. Educational attainments follow this pattern with the highest average levels of education in the non-ADHD group and the lowest average years in the group with persistent symptoms. Occupational success and percent receiving public assistance again separated between each group, with the symptom persisters faring the worst, the symptom desisters better, and those never affected by ADHD, the best. In terms of emotional disorders, it was only the symptom persisters who suffered from higher rates of mood and anxiety disorders. Similarly, only the symptom persisters had significantly more marijuana use disorders. No other substance use disorders or legal outcomes were significant.
How does this affect how we approach treatment?
Clinicians and researchers who specialize in ADHD have been arguing for ADHD to be treated as more of a chronic disease and for impairment to be the focus of treatment, rather than simply symptom control.10 With what we know about long-term functional impairment, there is reason to consider a more holistic picture of a child or an adolescent and how they are functioning in their academic, emotional, and social domains. A meta-analysis of treatment and long-term outcomes suggests that psychostimulant treatment, psychotherapy treatment, and combined treatment all improve long-term functioning, especially self-esteem, social functioning, and academic functioning, with combined psychotherapeutic and pharmacologic treatments associated with the highest effect sizes.11
For those who treat ADHD, it is our job to provide education to families about the chronic risks associated with the diagnosis, and the importance of offering multimodal therapy that can address family factors that might be contributing to risks, as well as the child’s overall well-being. If we are to make sense of how adults may experience impairment even in the absence of ongoing symptoms, we might look at how their overall wellness was interrupted during development. Maybe they fell into a different crowd of kids? Maybe they stopped achieving at school in a way that changed the achievement trajectory they were on? Maybe they impulsively picked up substances or got in trouble with the law? These events can have lasting impacts on well-being. We must use medicine and psychotherapy to help with symptoms, but we must look beyond treating illness and use evidence-based strategies to promote wellness at the level of the entire family.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. She works with children and adolescents as well as women in the perinatal period. She has no relevant financial disclosures.
References
1. Psychol Med. 2006 Feb;36(2):159-65.
2. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):937-44.e4.
3. J Am Acad Child Adolesc Psychiatry. 2018 Aug;57(8):571-82.e1.
4. J Am Acad Child Adolesc Psychiatry. 2017 Aug;56(8):687-95.e7.
5. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):945-52.e2.
6. J Am Acad Child Adolesc Psychiatry. 2009 May;48(5):484-500.
7. J Atten Disord. 2017 Sep 1:1087054717730610. doi: 10.1177/1087054717730610.
8. J Atten Disord. 2016 May;20(5):383-9.
9. Eur Child Adolesc Psychiatry. 2014 Feb;23(2):95-102.
10. JAMA Pediatr. 2018 Aug 13. doi: 10.1001/jamapediatrics.2018.1642.
11. PLoS One. 2015 Feb 25;10(2):e0116407.
Parents whose kids are diagnosed with ADHD face important questions about what to expect in the long term and how that might inform treatment. Studies find that ADHD diagnosed in childhood tends to persist in up to 65% of adolescents (some estimates are lower depending on criteria used),1 and about 50% of people are estimated to continue to meet criteria for ADHD as adults.2 Many studies have attempted to understand what long-term risks are associated with ADHD, as well as the factors that help better predict which characteristics in childhood might predict those risks. A recent article was published on a cohort of boys followed over 33 years.3 This, as well as other large prospective studies, such as the Multimodal Treatment of ADHD (MTA) provide us with helpful long-range data that inform this article.4-6 This article reviews risks in adolescence and adulthood and the factors thought to be associated with them.
What predicts persistence of ADHD symptoms in adolescence?
Several factors emerge consistently, including higher symptom severity, comorbid conduct disorder, and lower childhood IQ; other findings include family-related factors, such as lower parental mental health, less-positive parenting, and lower rates of parental education. In general, hyperactivity and impulsivity wanes, while inattention symptoms remain more stable.
What does ADHD predict for adolescents?
Adolescents with ADHD are more than twice as likely to be involved in pregnancies under the age of 18 years, true for both male and female genders.7 This finding also is associated with increased substance use and low academic achievement but not completely explained by it. Adolescents with persistent ADHD symptoms experience poorer educational success than do kids without ADHD symptoms, according to teacher reports of performance and measurements of grade point average. They are more likely to repeat a grade.8 Related but independent is the relationship of substance use disorders in kids with ADHD. Adolescents with ADHD are more likely to use nicotine or marijuana or meet criteria for any substance use disorder than adolescents without ADHD. Finally, adolescents aged 12-18 years with ADHD are at higher risk for motor vehicle accidents and all types of accidental injuries.9
What predicts persistence of ADHD symptoms in adulthood?
A follow-up study of the MTA trial 16 years later looked at ADHD diagnosed before age 12 years and the association with symptom persistence in adulthood, defined by the DSM-5 cutoff criteria of five symptoms. The following factors related to symptom persistence: childhood psychiatric comorbidity, higher ADHD symptom severity, and parental mental health problems. Notably, family socioeconomic status, child IQ, and parental education were not associated. In addition to looking at symptom persistence, other studies have looked at predictors of functional impairment in adulthood following a childhood ADHD diagnosis (independent of whether people continue to meet criteria for the disorder). The main findings that seem consistently related to all functional outcomes, including social, occupational, and educational, are lower childhood IQ and history of conduct problems (in the absence of meeting criteria for full childhood conduct disorder). Educational family-related factors, such as socioeconomic status and lower parental education, were related to lower educational functioning only.
What does ADHD predict for adults?
It appears that overall, adults who were diagnosed with ADHD as children show poorer functional outcomes than did those who weren’t, and there is a step-wise relationship when considering adults whose symptoms persist, with more severe outcomes compared with adults whose symptoms have desisted, who in turn have worse outcomes than adults who were never diagnosed with ADHD. Educational attainments follow this pattern with the highest average levels of education in the non-ADHD group and the lowest average years in the group with persistent symptoms. Occupational success and percent receiving public assistance again separated between each group, with the symptom persisters faring the worst, the symptom desisters better, and those never affected by ADHD, the best. In terms of emotional disorders, it was only the symptom persisters who suffered from higher rates of mood and anxiety disorders. Similarly, only the symptom persisters had significantly more marijuana use disorders. No other substance use disorders or legal outcomes were significant.
How does this affect how we approach treatment?
Clinicians and researchers who specialize in ADHD have been arguing for ADHD to be treated as more of a chronic disease and for impairment to be the focus of treatment, rather than simply symptom control.10 With what we know about long-term functional impairment, there is reason to consider a more holistic picture of a child or an adolescent and how they are functioning in their academic, emotional, and social domains. A meta-analysis of treatment and long-term outcomes suggests that psychostimulant treatment, psychotherapy treatment, and combined treatment all improve long-term functioning, especially self-esteem, social functioning, and academic functioning, with combined psychotherapeutic and pharmacologic treatments associated with the highest effect sizes.11
For those who treat ADHD, it is our job to provide education to families about the chronic risks associated with the diagnosis, and the importance of offering multimodal therapy that can address family factors that might be contributing to risks, as well as the child’s overall well-being. If we are to make sense of how adults may experience impairment even in the absence of ongoing symptoms, we might look at how their overall wellness was interrupted during development. Maybe they fell into a different crowd of kids? Maybe they stopped achieving at school in a way that changed the achievement trajectory they were on? Maybe they impulsively picked up substances or got in trouble with the law? These events can have lasting impacts on well-being. We must use medicine and psychotherapy to help with symptoms, but we must look beyond treating illness and use evidence-based strategies to promote wellness at the level of the entire family.
Dr. Guth is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and the University of Vermont, both in Burlington. She works with children and adolescents as well as women in the perinatal period. She has no relevant financial disclosures.
References
1. Psychol Med. 2006 Feb;36(2):159-65.
2. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):937-44.e4.
3. J Am Acad Child Adolesc Psychiatry. 2018 Aug;57(8):571-82.e1.
4. J Am Acad Child Adolesc Psychiatry. 2017 Aug;56(8):687-95.e7.
5. J Am Acad Child Adolesc Psychiatry. 2016 Nov;55(11):945-52.e2.
6. J Am Acad Child Adolesc Psychiatry. 2009 May;48(5):484-500.
7. J Atten Disord. 2017 Sep 1:1087054717730610. doi: 10.1177/1087054717730610.
8. J Atten Disord. 2016 May;20(5):383-9.
9. Eur Child Adolesc Psychiatry. 2014 Feb;23(2):95-102.
10. JAMA Pediatr. 2018 Aug 13. doi: 10.1001/jamapediatrics.2018.1642.
11. PLoS One. 2015 Feb 25;10(2):e0116407.
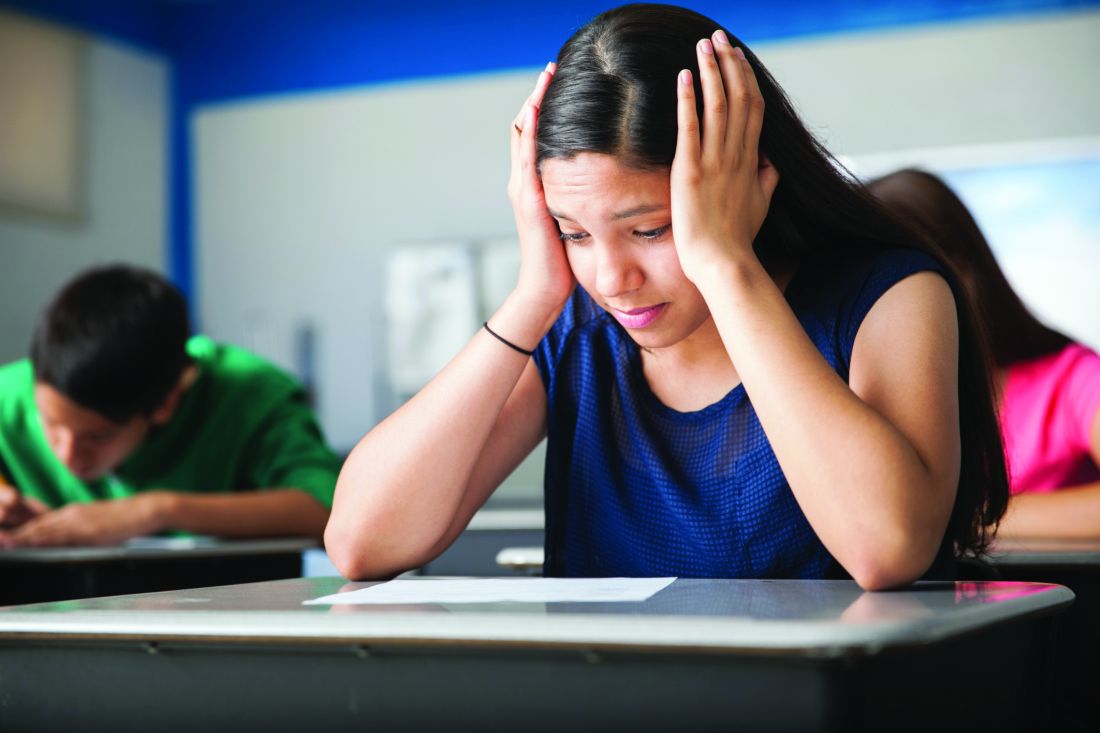
Over past 20 years, the percentage of children with ADHD nearly doubles
The number of children diagnosed with ADHD has reached more than 10%, a significant increase during the past 20 years, according to a recent study in JAMA.
The rise was most pronounced in minority groups, suggesting that better access to health insurance and mental health treatment through the Affordable Care Act might have played some role in the increase. The rate of diagnosis during that time period doubled in girls, although it was still much lower than in boys.
But the researchers say they found no evidence confirming frequent complaints that the condition is overdiagnosed or misdiagnosed.
The United States has significantly more instances of ADHD than do other developed countries, which researchers said has led some to think Americans are overdiagnosing children. Wei Bao, MD, PhD, lead author of the study, said in an interview that a review of studies around the world does not support that.
”I don’t think overdiagnosis is the main issue,” he said.
Nonetheless, those doubts persist. Stephen Hinshaw, MD, who coauthored a 2014 book called “The ADHD Explosion: Myths, Medication, Money, and Today’s Push for Performance,” compared ADHD with depression. He said in an interview that neither condition has unequivocal biological markers, which makes it hard to determine if a patient truly has the condition without lengthy psychological evaluations. Symptoms of ADHD can include inattention, fidgety behavior, and impulsivity.
“It’s probably not a true epidemic of ADHD,” said Dr. Hinshaw, a professor of psychology at the University of California, Berkeley, and a professor of psychiatry at University of California, San Francisco. “It might be an epidemic of diagnosing it.”
In interpreting their results, however, the study’s authors tied the higher numbers to better understanding of the condition by doctors and the public, new standards for diagnosis and an increase in access to health insurance through the ACA.
Because of the ACA, “some low-income families have improved access to services and referrals,” said Dr. Bao, an epidemiologist at the University of Iowa College of Public Health in Iowa City.
The study, published in JAMA Network Open, used data from the National Health Interview Survey, an annual federal survey of about 35,000 households. It found a steady increase in diagnoses in children from about 6% during 1997-1998 to more than 10% during 2015-2016.
Advances in medical technology also may have contributed to the increase, according to the research. Twenty years ago, preterm or low-birth-weight babies had a harder time surviving. Those factors increase the risk of being diagnosed with ADHD.
The study also suggests that fewer stigmas about mental health care in minority communities also may lead to more people receiving an ADHD diagnosis.
In the late 1990s, 7.2% of non-Hispanic white children, 4.7% of non-Hispanic black children, and 3.6% of Hispanic children were diagnosed with ADHD, according to the study. By 2016, it was 12% of white kids, 12.8% of blacks, and 6.1% of Hispanics.
Over the past several decades, Dr. Hinshaw said, there’s been an expanded view of who can develop ADHD. It’s no longer viewed as a disease that affects only white middle-class boys, as eating disorders are no longer seen as afflicting only white middle-class girls.
Still, he cautioned against overdiagnosing ADHD in communities in which behavioral issues could be the result of social or environmental factors such as overcrowded classrooms.
The study found rates of ADHD among girls rose from 3% to more than 6% over the study period. It said that was partly a result of a change in how the condition is classified. For years, ADHD pertained to children who were hyperactive. But in recent years, the American Psychiatric Association added to its guide of mental health conditions that diagnosis should also include some children who are inattentive, Dr. Bao said. That raised the number of girls, he explained, because it seems they are more likely to be in that second subtype.
“If we compare these two, you can easily imagine people will easily recognize hyperactivity,” he said.
That rang true for Ruth Hay, a 25-year-old student and cook from New York who now lives in Jerusalem. She was diagnosed with what was then called ADD the summer between second and third grade.
Ms. Hay said her hyperactive tendencies aren’t as “loud” as some people’s. She’s less likely to bounce around a room than she is to bounce in her chair, she said.
Yet, despite her early diagnosis, Ms. Hay said, no one ever told her about other symptoms. For example, she said, she suffers from executive dysfunction, which leaves her feeling unable to accomplish tasks, no matter how much she wanted to or tried.
“I grew up being called lazy in periods of time when I wasn’t,” Ms. Hay said. “If you look at a list of all the various ADHD symptoms, I have all of them to one degree or another, but the only ones ever discussed with me was you might be less focused and more fidgety.”
“I don’t know how my brain would be if I didn’t have it,” she added. “I don’t know if I’d still be me, but all it has been for me is a disability.”
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The number of children diagnosed with ADHD has reached more than 10%, a significant increase during the past 20 years, according to a recent study in JAMA.
The rise was most pronounced in minority groups, suggesting that better access to health insurance and mental health treatment through the Affordable Care Act might have played some role in the increase. The rate of diagnosis during that time period doubled in girls, although it was still much lower than in boys.
But the researchers say they found no evidence confirming frequent complaints that the condition is overdiagnosed or misdiagnosed.
The United States has significantly more instances of ADHD than do other developed countries, which researchers said has led some to think Americans are overdiagnosing children. Wei Bao, MD, PhD, lead author of the study, said in an interview that a review of studies around the world does not support that.
”I don’t think overdiagnosis is the main issue,” he said.
Nonetheless, those doubts persist. Stephen Hinshaw, MD, who coauthored a 2014 book called “The ADHD Explosion: Myths, Medication, Money, and Today’s Push for Performance,” compared ADHD with depression. He said in an interview that neither condition has unequivocal biological markers, which makes it hard to determine if a patient truly has the condition without lengthy psychological evaluations. Symptoms of ADHD can include inattention, fidgety behavior, and impulsivity.
“It’s probably not a true epidemic of ADHD,” said Dr. Hinshaw, a professor of psychology at the University of California, Berkeley, and a professor of psychiatry at University of California, San Francisco. “It might be an epidemic of diagnosing it.”
In interpreting their results, however, the study’s authors tied the higher numbers to better understanding of the condition by doctors and the public, new standards for diagnosis and an increase in access to health insurance through the ACA.
Because of the ACA, “some low-income families have improved access to services and referrals,” said Dr. Bao, an epidemiologist at the University of Iowa College of Public Health in Iowa City.
The study, published in JAMA Network Open, used data from the National Health Interview Survey, an annual federal survey of about 35,000 households. It found a steady increase in diagnoses in children from about 6% during 1997-1998 to more than 10% during 2015-2016.
Advances in medical technology also may have contributed to the increase, according to the research. Twenty years ago, preterm or low-birth-weight babies had a harder time surviving. Those factors increase the risk of being diagnosed with ADHD.
The study also suggests that fewer stigmas about mental health care in minority communities also may lead to more people receiving an ADHD diagnosis.
In the late 1990s, 7.2% of non-Hispanic white children, 4.7% of non-Hispanic black children, and 3.6% of Hispanic children were diagnosed with ADHD, according to the study. By 2016, it was 12% of white kids, 12.8% of blacks, and 6.1% of Hispanics.
Over the past several decades, Dr. Hinshaw said, there’s been an expanded view of who can develop ADHD. It’s no longer viewed as a disease that affects only white middle-class boys, as eating disorders are no longer seen as afflicting only white middle-class girls.
Still, he cautioned against overdiagnosing ADHD in communities in which behavioral issues could be the result of social or environmental factors such as overcrowded classrooms.
The study found rates of ADHD among girls rose from 3% to more than 6% over the study period. It said that was partly a result of a change in how the condition is classified. For years, ADHD pertained to children who were hyperactive. But in recent years, the American Psychiatric Association added to its guide of mental health conditions that diagnosis should also include some children who are inattentive, Dr. Bao said. That raised the number of girls, he explained, because it seems they are more likely to be in that second subtype.
“If we compare these two, you can easily imagine people will easily recognize hyperactivity,” he said.
That rang true for Ruth Hay, a 25-year-old student and cook from New York who now lives in Jerusalem. She was diagnosed with what was then called ADD the summer between second and third grade.
Ms. Hay said her hyperactive tendencies aren’t as “loud” as some people’s. She’s less likely to bounce around a room than she is to bounce in her chair, she said.
Yet, despite her early diagnosis, Ms. Hay said, no one ever told her about other symptoms. For example, she said, she suffers from executive dysfunction, which leaves her feeling unable to accomplish tasks, no matter how much she wanted to or tried.
“I grew up being called lazy in periods of time when I wasn’t,” Ms. Hay said. “If you look at a list of all the various ADHD symptoms, I have all of them to one degree or another, but the only ones ever discussed with me was you might be less focused and more fidgety.”
“I don’t know how my brain would be if I didn’t have it,” she added. “I don’t know if I’d still be me, but all it has been for me is a disability.”
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The number of children diagnosed with ADHD has reached more than 10%, a significant increase during the past 20 years, according to a recent study in JAMA.
The rise was most pronounced in minority groups, suggesting that better access to health insurance and mental health treatment through the Affordable Care Act might have played some role in the increase. The rate of diagnosis during that time period doubled in girls, although it was still much lower than in boys.
But the researchers say they found no evidence confirming frequent complaints that the condition is overdiagnosed or misdiagnosed.
The United States has significantly more instances of ADHD than do other developed countries, which researchers said has led some to think Americans are overdiagnosing children. Wei Bao, MD, PhD, lead author of the study, said in an interview that a review of studies around the world does not support that.
”I don’t think overdiagnosis is the main issue,” he said.
Nonetheless, those doubts persist. Stephen Hinshaw, MD, who coauthored a 2014 book called “The ADHD Explosion: Myths, Medication, Money, and Today’s Push for Performance,” compared ADHD with depression. He said in an interview that neither condition has unequivocal biological markers, which makes it hard to determine if a patient truly has the condition without lengthy psychological evaluations. Symptoms of ADHD can include inattention, fidgety behavior, and impulsivity.
“It’s probably not a true epidemic of ADHD,” said Dr. Hinshaw, a professor of psychology at the University of California, Berkeley, and a professor of psychiatry at University of California, San Francisco. “It might be an epidemic of diagnosing it.”
In interpreting their results, however, the study’s authors tied the higher numbers to better understanding of the condition by doctors and the public, new standards for diagnosis and an increase in access to health insurance through the ACA.
Because of the ACA, “some low-income families have improved access to services and referrals,” said Dr. Bao, an epidemiologist at the University of Iowa College of Public Health in Iowa City.
The study, published in JAMA Network Open, used data from the National Health Interview Survey, an annual federal survey of about 35,000 households. It found a steady increase in diagnoses in children from about 6% during 1997-1998 to more than 10% during 2015-2016.
Advances in medical technology also may have contributed to the increase, according to the research. Twenty years ago, preterm or low-birth-weight babies had a harder time surviving. Those factors increase the risk of being diagnosed with ADHD.
The study also suggests that fewer stigmas about mental health care in minority communities also may lead to more people receiving an ADHD diagnosis.
In the late 1990s, 7.2% of non-Hispanic white children, 4.7% of non-Hispanic black children, and 3.6% of Hispanic children were diagnosed with ADHD, according to the study. By 2016, it was 12% of white kids, 12.8% of blacks, and 6.1% of Hispanics.
Over the past several decades, Dr. Hinshaw said, there’s been an expanded view of who can develop ADHD. It’s no longer viewed as a disease that affects only white middle-class boys, as eating disorders are no longer seen as afflicting only white middle-class girls.
Still, he cautioned against overdiagnosing ADHD in communities in which behavioral issues could be the result of social or environmental factors such as overcrowded classrooms.
The study found rates of ADHD among girls rose from 3% to more than 6% over the study period. It said that was partly a result of a change in how the condition is classified. For years, ADHD pertained to children who were hyperactive. But in recent years, the American Psychiatric Association added to its guide of mental health conditions that diagnosis should also include some children who are inattentive, Dr. Bao said. That raised the number of girls, he explained, because it seems they are more likely to be in that second subtype.
“If we compare these two, you can easily imagine people will easily recognize hyperactivity,” he said.
That rang true for Ruth Hay, a 25-year-old student and cook from New York who now lives in Jerusalem. She was diagnosed with what was then called ADD the summer between second and third grade.
Ms. Hay said her hyperactive tendencies aren’t as “loud” as some people’s. She’s less likely to bounce around a room than she is to bounce in her chair, she said.
Yet, despite her early diagnosis, Ms. Hay said, no one ever told her about other symptoms. For example, she said, she suffers from executive dysfunction, which leaves her feeling unable to accomplish tasks, no matter how much she wanted to or tried.
“I grew up being called lazy in periods of time when I wasn’t,” Ms. Hay said. “If you look at a list of all the various ADHD symptoms, I have all of them to one degree or another, but the only ones ever discussed with me was you might be less focused and more fidgety.”
“I don’t know how my brain would be if I didn’t have it,” she added. “I don’t know if I’d still be me, but all it has been for me is a disability.”
KHN’s coverage of children’s health care issues is supported in part by the Heising-Simons Foundation.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Schools’ cell phone policies: What’s best for students?
Schools across the country – or around the world, for that matter – are grappling with policies and regulations tied to their students’ use of cell phones during school hours.
These policies run the gamut, from allowing students to use smartphones as learning tools to requiring them to keep the devices turned off. One public high school’s action on cell phones, initiated this year by a parent, has prompted one parent’s thumbs-up. This school is phasing in a lock-up-your-cell-phone policy.
NPR reporter Jennifer Ludden said that when the idea was first floated toward the end of the last school year, it provoked a parental outcry at her sons’ school. “My generation is used to 24/7 access to our kids, wherever they are. I confess, I’ve texted mine at school. It was about a doctor’s appointment,” Ms. Ludden says.
Meanwhile, she says, some asked: “ ‘What if there’s an emergency?’ It’s a fair question. We’ve all heard about students hiding from a gunman, posting updates, and texting to let friends and family know they’re safe,” she says.
Yet, evidence suggests that a cell-free classroom is a safer classroom, without the distraction of that screen to divert attention instructions that come in the wake of a school emergency. And, in a chilling mental image, a phone’s ringtone or vibration on a desk could be a beacon for a shooter.
Putting aside the horrific potential of school violence, a no-phone policy could have other tangible benefits that would help students in real life. The rejigging of adolescent brains away from the umbilical cord of their phone would be welcome. Imagine social interactions, instead of that face-down, thumbs-poised posture that is everywhere! And it could also help curb the electronic version of passing notes during tests.
Ms. Ludden mentions another benefit. “ Invaluable time to relax, and connect, without phones. I’m grateful to see some schools investing in that,” Ms. Ludden says.
Click here to listen to Ms. Ludden’s take.
Schools across the country – or around the world, for that matter – are grappling with policies and regulations tied to their students’ use of cell phones during school hours.
These policies run the gamut, from allowing students to use smartphones as learning tools to requiring them to keep the devices turned off. One public high school’s action on cell phones, initiated this year by a parent, has prompted one parent’s thumbs-up. This school is phasing in a lock-up-your-cell-phone policy.
NPR reporter Jennifer Ludden said that when the idea was first floated toward the end of the last school year, it provoked a parental outcry at her sons’ school. “My generation is used to 24/7 access to our kids, wherever they are. I confess, I’ve texted mine at school. It was about a doctor’s appointment,” Ms. Ludden says.
Meanwhile, she says, some asked: “ ‘What if there’s an emergency?’ It’s a fair question. We’ve all heard about students hiding from a gunman, posting updates, and texting to let friends and family know they’re safe,” she says.
Yet, evidence suggests that a cell-free classroom is a safer classroom, without the distraction of that screen to divert attention instructions that come in the wake of a school emergency. And, in a chilling mental image, a phone’s ringtone or vibration on a desk could be a beacon for a shooter.
Putting aside the horrific potential of school violence, a no-phone policy could have other tangible benefits that would help students in real life. The rejigging of adolescent brains away from the umbilical cord of their phone would be welcome. Imagine social interactions, instead of that face-down, thumbs-poised posture that is everywhere! And it could also help curb the electronic version of passing notes during tests.
Ms. Ludden mentions another benefit. “ Invaluable time to relax, and connect, without phones. I’m grateful to see some schools investing in that,” Ms. Ludden says.
Click here to listen to Ms. Ludden’s take.
Schools across the country – or around the world, for that matter – are grappling with policies and regulations tied to their students’ use of cell phones during school hours.
These policies run the gamut, from allowing students to use smartphones as learning tools to requiring them to keep the devices turned off. One public high school’s action on cell phones, initiated this year by a parent, has prompted one parent’s thumbs-up. This school is phasing in a lock-up-your-cell-phone policy.
NPR reporter Jennifer Ludden said that when the idea was first floated toward the end of the last school year, it provoked a parental outcry at her sons’ school. “My generation is used to 24/7 access to our kids, wherever they are. I confess, I’ve texted mine at school. It was about a doctor’s appointment,” Ms. Ludden says.
Meanwhile, she says, some asked: “ ‘What if there’s an emergency?’ It’s a fair question. We’ve all heard about students hiding from a gunman, posting updates, and texting to let friends and family know they’re safe,” she says.
Yet, evidence suggests that a cell-free classroom is a safer classroom, without the distraction of that screen to divert attention instructions that come in the wake of a school emergency. And, in a chilling mental image, a phone’s ringtone or vibration on a desk could be a beacon for a shooter.
Putting aside the horrific potential of school violence, a no-phone policy could have other tangible benefits that would help students in real life. The rejigging of adolescent brains away from the umbilical cord of their phone would be welcome. Imagine social interactions, instead of that face-down, thumbs-poised posture that is everywhere! And it could also help curb the electronic version of passing notes during tests.
Ms. Ludden mentions another benefit. “ Invaluable time to relax, and connect, without phones. I’m grateful to see some schools investing in that,” Ms. Ludden says.
Click here to listen to Ms. Ludden’s take.
Alopecia areata linked to mental health disorders
Alopecia areata is associated with greater frequency of mental health disorders, according to a new analysis of U.S. hospitalizations.
Specifically, the analysis found, alopecia areata patients are at risk for any mental health disorder, anxiety disorders, attention-deficit/hyperactivity disorder, dementia, mood disorders, personality disorders, and suicide or intentionally self-inflicted injury. The report was published in the Journal of the American Academy of Dermatology.
The researchers worked with 87,053,155 adult and child records from the 2002-2012 National Inpatient Sample, which represents 20% of U.S. hospitalizations.
Overall, 5,605 patients had alopecia areata, which was the secondary diagnosis more than 99% of the time. Compared with inpatients without alopecia areata, those with the disorder were more likely to be younger (42.2 vs. 47.9 years; P less than .0001), female (61.7% vs. 58.6%; P = .0297), and uninsured (8.1% vs. 5.5%; P less than .0001). In addition, inpatients with alopecia areata had a greater frequency of mental health disorders (32.8% vs. 20.0%; P less than .0001) and were more likely to have a primary mental health diagnosis (5.5% vs. 2.2%; P less than .0001), reported Vivek Singam of Northwestern University, Chicago, and his associates.
Among 15 mental health or classes of disorders examined, alopecia areata patients were at greater risk in 13 of them. The only exceptions were delirium/dementia/amnestic/cognitive disorders and disorders diagnosed in infancy, childhood, or adolescence.
Alopecia areata patients with a mental health disorder had a mean hospital stay of 6.0 days (95% confidence interval, 5.4.-6.6) and hospitalization cost of $11,907 (95% CI, $10,312-$13,503).
Previous studies had shown similar relationships. However, previous studies showed lower risk of alopecia areata and schizophrenia and no increased risk of ADHD, compared with the current study’s findings. The authors could offer no explanation for those differences.
The strengths of the current analysis include its use of a large-scale, nationally representative cohort and its large sample size, as well its inclusion of a broad range of mental health disorders. Because of its cross-sectional design, the study could not establish the temporal relationship between alopecia areata and mental health disorders.
It is unclear whether psychosocial stress might cause or exacerbate alopecia areata, or whether alopecia areata can lead to or worsen mental health disorders.
The researchers called for additional studies to understand this relationship and potential mechanisms.
The Agency for Healthcare Research and Quality and the Dermatology Foundation funded the study. The researchers declared having no conflicts of interest.
SOURCE: Singam V et al. J Am Acad Dermatol. 2018 Aug 6. doi: 10.1016/j.jaad.2018.07.044.
Alopecia areata is associated with greater frequency of mental health disorders, according to a new analysis of U.S. hospitalizations.
Specifically, the analysis found, alopecia areata patients are at risk for any mental health disorder, anxiety disorders, attention-deficit/hyperactivity disorder, dementia, mood disorders, personality disorders, and suicide or intentionally self-inflicted injury. The report was published in the Journal of the American Academy of Dermatology.
The researchers worked with 87,053,155 adult and child records from the 2002-2012 National Inpatient Sample, which represents 20% of U.S. hospitalizations.
Overall, 5,605 patients had alopecia areata, which was the secondary diagnosis more than 99% of the time. Compared with inpatients without alopecia areata, those with the disorder were more likely to be younger (42.2 vs. 47.9 years; P less than .0001), female (61.7% vs. 58.6%; P = .0297), and uninsured (8.1% vs. 5.5%; P less than .0001). In addition, inpatients with alopecia areata had a greater frequency of mental health disorders (32.8% vs. 20.0%; P less than .0001) and were more likely to have a primary mental health diagnosis (5.5% vs. 2.2%; P less than .0001), reported Vivek Singam of Northwestern University, Chicago, and his associates.
Among 15 mental health or classes of disorders examined, alopecia areata patients were at greater risk in 13 of them. The only exceptions were delirium/dementia/amnestic/cognitive disorders and disorders diagnosed in infancy, childhood, or adolescence.
Alopecia areata patients with a mental health disorder had a mean hospital stay of 6.0 days (95% confidence interval, 5.4.-6.6) and hospitalization cost of $11,907 (95% CI, $10,312-$13,503).
Previous studies had shown similar relationships. However, previous studies showed lower risk of alopecia areata and schizophrenia and no increased risk of ADHD, compared with the current study’s findings. The authors could offer no explanation for those differences.
The strengths of the current analysis include its use of a large-scale, nationally representative cohort and its large sample size, as well its inclusion of a broad range of mental health disorders. Because of its cross-sectional design, the study could not establish the temporal relationship between alopecia areata and mental health disorders.
It is unclear whether psychosocial stress might cause or exacerbate alopecia areata, or whether alopecia areata can lead to or worsen mental health disorders.
The researchers called for additional studies to understand this relationship and potential mechanisms.
The Agency for Healthcare Research and Quality and the Dermatology Foundation funded the study. The researchers declared having no conflicts of interest.
SOURCE: Singam V et al. J Am Acad Dermatol. 2018 Aug 6. doi: 10.1016/j.jaad.2018.07.044.
Alopecia areata is associated with greater frequency of mental health disorders, according to a new analysis of U.S. hospitalizations.
Specifically, the analysis found, alopecia areata patients are at risk for any mental health disorder, anxiety disorders, attention-deficit/hyperactivity disorder, dementia, mood disorders, personality disorders, and suicide or intentionally self-inflicted injury. The report was published in the Journal of the American Academy of Dermatology.
The researchers worked with 87,053,155 adult and child records from the 2002-2012 National Inpatient Sample, which represents 20% of U.S. hospitalizations.
Overall, 5,605 patients had alopecia areata, which was the secondary diagnosis more than 99% of the time. Compared with inpatients without alopecia areata, those with the disorder were more likely to be younger (42.2 vs. 47.9 years; P less than .0001), female (61.7% vs. 58.6%; P = .0297), and uninsured (8.1% vs. 5.5%; P less than .0001). In addition, inpatients with alopecia areata had a greater frequency of mental health disorders (32.8% vs. 20.0%; P less than .0001) and were more likely to have a primary mental health diagnosis (5.5% vs. 2.2%; P less than .0001), reported Vivek Singam of Northwestern University, Chicago, and his associates.
Among 15 mental health or classes of disorders examined, alopecia areata patients were at greater risk in 13 of them. The only exceptions were delirium/dementia/amnestic/cognitive disorders and disorders diagnosed in infancy, childhood, or adolescence.
Alopecia areata patients with a mental health disorder had a mean hospital stay of 6.0 days (95% confidence interval, 5.4.-6.6) and hospitalization cost of $11,907 (95% CI, $10,312-$13,503).
Previous studies had shown similar relationships. However, previous studies showed lower risk of alopecia areata and schizophrenia and no increased risk of ADHD, compared with the current study’s findings. The authors could offer no explanation for those differences.
The strengths of the current analysis include its use of a large-scale, nationally representative cohort and its large sample size, as well its inclusion of a broad range of mental health disorders. Because of its cross-sectional design, the study could not establish the temporal relationship between alopecia areata and mental health disorders.
It is unclear whether psychosocial stress might cause or exacerbate alopecia areata, or whether alopecia areata can lead to or worsen mental health disorders.
The researchers called for additional studies to understand this relationship and potential mechanisms.
The Agency for Healthcare Research and Quality and the Dermatology Foundation funded the study. The researchers declared having no conflicts of interest.
SOURCE: Singam V et al. J Am Acad Dermatol. 2018 Aug 6. doi: 10.1016/j.jaad.2018.07.044.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: Alopecia areata patients should be monitored closely for mental health disorders.
Major finding: Overall, 32.8% of hospitalized alopecia areata patients had a mental health disorder, compared with 20.0% of controls.
Study details: Retrospective analysis of 87,053,155 U.S. adults and children.
Disclosures: The Agency for Healthcare Research & Quality and the Dermatology Foundation funded the study. The researchers declared having no conflicts of interest.
Source: Singam V et al. J Am Acad Dermatol. 2018 Aug 6. doi: 10.1016/j.jaad.2018.07.044.
Concurrent stimulant and opioid use ‘common’ in adult ADHD
A significant number of adults with attention-deficit/hyperactivity disorder are concurrently using stimulants and opioids, highlighting a need for research into the risks and benefits of long-term coadministration of these medications.
Researchers reported the results of a cross-sectional study using Medicaid Analytic eXtract data from 66,406 adults with ADHD across 29 states.
Overall, 32.7% used stimulants, and 5.4% had used both stimulants and opioids long term, defined as at least 30 consecutive days of use. Long-term opioid use was more common among adults who used stimulants, compared with those who did not use stimulants (16.5% vs. 13%), wrote Yu-Jung “Jenny” Wei, PhD, and her associates. The report was published in JAMA Network Open.
Most of the adults who used both stimulants and opioids concurrently long term were using short-acting opioids (81.8%) rather than long-acting (20.6%). However, nearly one-quarter (23.2%) had prescriptions for both long- and short-acting opioids.
The researchers noted a significant 12% increase in the prevalence of concurrent use of stimulants and opioids from 1999 to 2010.
“Our findings suggest that long-term concurrent use of stimulants and opioids has become an increasingly common practice among adult patients with ADHD,” wrote Dr. Wei, of the College of Pharmacy at the University of Florida, Gainesville, and her associates.
The researchers also found an increase in these trends with age: Adults in their 30s showed a 7% higher prevalence of long-term concurrent use, compared with adults in their 20s. In addition, those aged 41-50 years had a 14% higher prevalence, and those aged 51-64 years had a 17% higher prevalence.
Adults with pain had a 10% higher prevalence of concurrent use, while other People with schizophrenia appeared to have a 5% lower incidence of concurrent use.
“Although the concurrent use of stimulants and opioids may initially have been prompted by ADHD symptoms and comorbid chronic pain, continued use of opioids alone or combined with central nervous system stimulants may result in drug dependence and other adverse effects (e.g., overdose) because of the high potential for abuse and misuse,” the authors wrote. “Identifying these high-risk patients allows for early intervention and may reduce the number of adverse events associated with the long-term use of these medications.”
Among the limitations cited is that only prescription medications filled and reimbursed by Medicaid were included in the analysis. “Considering that opioid prescription fills are commonly paid out of pocket, our reported prevalence of concurrent stimulant-opioid use may be too low,” they wrote.
The authors reported no conflicts of interest. One author was supported by an award from the National Institute on Aging.
SOURCE: Wei Y-J et al. JAMA Network Open. 2018. Aug 10. doi: 10.1001/jamanetworkopen.2018.1152.
A significant number of adults with attention-deficit/hyperactivity disorder are concurrently using stimulants and opioids, highlighting a need for research into the risks and benefits of long-term coadministration of these medications.
Researchers reported the results of a cross-sectional study using Medicaid Analytic eXtract data from 66,406 adults with ADHD across 29 states.
Overall, 32.7% used stimulants, and 5.4% had used both stimulants and opioids long term, defined as at least 30 consecutive days of use. Long-term opioid use was more common among adults who used stimulants, compared with those who did not use stimulants (16.5% vs. 13%), wrote Yu-Jung “Jenny” Wei, PhD, and her associates. The report was published in JAMA Network Open.
Most of the adults who used both stimulants and opioids concurrently long term were using short-acting opioids (81.8%) rather than long-acting (20.6%). However, nearly one-quarter (23.2%) had prescriptions for both long- and short-acting opioids.
The researchers noted a significant 12% increase in the prevalence of concurrent use of stimulants and opioids from 1999 to 2010.
“Our findings suggest that long-term concurrent use of stimulants and opioids has become an increasingly common practice among adult patients with ADHD,” wrote Dr. Wei, of the College of Pharmacy at the University of Florida, Gainesville, and her associates.
The researchers also found an increase in these trends with age: Adults in their 30s showed a 7% higher prevalence of long-term concurrent use, compared with adults in their 20s. In addition, those aged 41-50 years had a 14% higher prevalence, and those aged 51-64 years had a 17% higher prevalence.
Adults with pain had a 10% higher prevalence of concurrent use, while other People with schizophrenia appeared to have a 5% lower incidence of concurrent use.
“Although the concurrent use of stimulants and opioids may initially have been prompted by ADHD symptoms and comorbid chronic pain, continued use of opioids alone or combined with central nervous system stimulants may result in drug dependence and other adverse effects (e.g., overdose) because of the high potential for abuse and misuse,” the authors wrote. “Identifying these high-risk patients allows for early intervention and may reduce the number of adverse events associated with the long-term use of these medications.”
Among the limitations cited is that only prescription medications filled and reimbursed by Medicaid were included in the analysis. “Considering that opioid prescription fills are commonly paid out of pocket, our reported prevalence of concurrent stimulant-opioid use may be too low,” they wrote.
The authors reported no conflicts of interest. One author was supported by an award from the National Institute on Aging.
SOURCE: Wei Y-J et al. JAMA Network Open. 2018. Aug 10. doi: 10.1001/jamanetworkopen.2018.1152.
A significant number of adults with attention-deficit/hyperactivity disorder are concurrently using stimulants and opioids, highlighting a need for research into the risks and benefits of long-term coadministration of these medications.
Researchers reported the results of a cross-sectional study using Medicaid Analytic eXtract data from 66,406 adults with ADHD across 29 states.
Overall, 32.7% used stimulants, and 5.4% had used both stimulants and opioids long term, defined as at least 30 consecutive days of use. Long-term opioid use was more common among adults who used stimulants, compared with those who did not use stimulants (16.5% vs. 13%), wrote Yu-Jung “Jenny” Wei, PhD, and her associates. The report was published in JAMA Network Open.
Most of the adults who used both stimulants and opioids concurrently long term were using short-acting opioids (81.8%) rather than long-acting (20.6%). However, nearly one-quarter (23.2%) had prescriptions for both long- and short-acting opioids.
The researchers noted a significant 12% increase in the prevalence of concurrent use of stimulants and opioids from 1999 to 2010.
“Our findings suggest that long-term concurrent use of stimulants and opioids has become an increasingly common practice among adult patients with ADHD,” wrote Dr. Wei, of the College of Pharmacy at the University of Florida, Gainesville, and her associates.
The researchers also found an increase in these trends with age: Adults in their 30s showed a 7% higher prevalence of long-term concurrent use, compared with adults in their 20s. In addition, those aged 41-50 years had a 14% higher prevalence, and those aged 51-64 years had a 17% higher prevalence.
Adults with pain had a 10% higher prevalence of concurrent use, while other People with schizophrenia appeared to have a 5% lower incidence of concurrent use.
“Although the concurrent use of stimulants and opioids may initially have been prompted by ADHD symptoms and comorbid chronic pain, continued use of opioids alone or combined with central nervous system stimulants may result in drug dependence and other adverse effects (e.g., overdose) because of the high potential for abuse and misuse,” the authors wrote. “Identifying these high-risk patients allows for early intervention and may reduce the number of adverse events associated with the long-term use of these medications.”
Among the limitations cited is that only prescription medications filled and reimbursed by Medicaid were included in the analysis. “Considering that opioid prescription fills are commonly paid out of pocket, our reported prevalence of concurrent stimulant-opioid use may be too low,” they wrote.
The authors reported no conflicts of interest. One author was supported by an award from the National Institute on Aging.
SOURCE: Wei Y-J et al. JAMA Network Open. 2018. Aug 10. doi: 10.1001/jamanetworkopen.2018.1152.
FROM JAMA NETWORK OPEN
Key clinical point: Identifying high-risk patients “allows for early intervention and may reduce the number of adverse events associated with the long-term use.”
Major finding: About 5% of adults with ADHD are on both opioids and stimulants long term.
Study details: Cross-sectional study of 66,406 adults with ADHD.
Disclosures: The authors reported no conflicts of interest. One author was supported by an award from the National Institute on Aging.
Source: Wei Y-J et al. JAMA Network Open. 2018. Aug 10. doi: 10.1001/jamanetworkopen.2018.1152.
Methylphenidate deemed best first-line option for ADHD in children
Methylphenidate appears to be the safest and most effective treatment option for attention-deficit/hyperactivity disorder in children and adolescents, while amphetamines are the preferred first-line choice in adults, a systematic review and meta-analysis have found.
Researchers reported the results of a network meta-analysis of 133 double-blind randomized controlled trials – 81 in children and adolescents, 51 in adults, and 1 in both – involving a total of 10,068 children and adolescents, and 8,131 adults. The included studies all compared a range of medications to placebo or in head-to-head trials. The meta-analysis was published online Aug. 7 in The Lancet Psychiatry.
At 12 weeks, all the medications, which included amphetamines, atomoxetine, bupropion, clonidine, guanfacine, methylphenidate, and modafinil, were found to be better than placebo in reducing core ADHD symptoms in children and adolescents, according to clinicians’ ratings. However, when teachers’ ratings were used, only methylphenidate and modafinil were better than placebo.
In adults, clinicians’ ratings found that amphetamines, methylphenidate, bupropion, and atomoxetine – but not modafinil – were better than placebo.
In head-to-head trials, clinicians’ ratings favored amphetamines over modafinil, atomoxetine, and methylphenidate in children, adolescents, and adults.
But in adults, amphetamines, bupropion, and methylphenidate all beat placebo.
When it came to tolerability in children and adolescents, guanfacine and amphetamines were the only two treatments that were less well tolerated than placebo. However, a post hoc analysis suggested lisdexamfetamine had a lower tolerability relative to other amphetamines, at least in children and adolescents. In adults, modafinil, amphetamines, methylphenidate, and atomoxetine were beaten by placebo for tolerability.
“Overall, all medications, except modafinil in adults, were more efficacious than placebo for the short-term treatment of ADHD, and they were less efficacious and less well tolerated in adults than in children and adolescents,” wrote Samuele Cortese, MD, PhD, of the University of Southampton (England), and his coauthors. “However, the included medications were not equivalent in relation to their mean effect size, which ranged from moderate to high and varied according to the type of rater.”
For example, while atomoxetine had the lowest mean effect size in children and adolescents based on clinicians’ ratings, in adults, it was on par with methylphenidate. Amphetamines increased diastolic blood pressure in children but not in adults.
“Taking into account both efficacy and safety, evidence from this meta-analysis supports methylphenidate in children and adolescents, and amphetamines in adults, as preferred first-choice medications for the short-term treatment of ADHD,” the authors wrote.
Dr. Cortese and his coauthors cited a few limitations. One is that the most recent study included in their meta-analysis was published in April 2017. When the researchers conducted a PubMed search in May 2018, they found three additional studies that met their criteria. “Since we already had 133 included studies, we decided that adding these three studies would not have changed the final results materially,” they wrote.
The study was supported by the Stichting Eunethydis (European Network for Hyperkinetic Disorders), and the U.K. National Institute for Health Research Oxford Health Biomedical Research Centre. Nine authors declared support, funding, or advisory roles with a range of organizations or the pharmaceutical industry.
SOURCE: Cortese S et al. Lancet Psychiatry. 2018 Aug 7. doi: 10.1016/S2215-0366(18)30269-4.
Methylphenidate appears to be the safest and most effective treatment option for attention-deficit/hyperactivity disorder in children and adolescents, while amphetamines are the preferred first-line choice in adults, a systematic review and meta-analysis have found.
Researchers reported the results of a network meta-analysis of 133 double-blind randomized controlled trials – 81 in children and adolescents, 51 in adults, and 1 in both – involving a total of 10,068 children and adolescents, and 8,131 adults. The included studies all compared a range of medications to placebo or in head-to-head trials. The meta-analysis was published online Aug. 7 in The Lancet Psychiatry.
At 12 weeks, all the medications, which included amphetamines, atomoxetine, bupropion, clonidine, guanfacine, methylphenidate, and modafinil, were found to be better than placebo in reducing core ADHD symptoms in children and adolescents, according to clinicians’ ratings. However, when teachers’ ratings were used, only methylphenidate and modafinil were better than placebo.
In adults, clinicians’ ratings found that amphetamines, methylphenidate, bupropion, and atomoxetine – but not modafinil – were better than placebo.
In head-to-head trials, clinicians’ ratings favored amphetamines over modafinil, atomoxetine, and methylphenidate in children, adolescents, and adults.
But in adults, amphetamines, bupropion, and methylphenidate all beat placebo.
When it came to tolerability in children and adolescents, guanfacine and amphetamines were the only two treatments that were less well tolerated than placebo. However, a post hoc analysis suggested lisdexamfetamine had a lower tolerability relative to other amphetamines, at least in children and adolescents. In adults, modafinil, amphetamines, methylphenidate, and atomoxetine were beaten by placebo for tolerability.
“Overall, all medications, except modafinil in adults, were more efficacious than placebo for the short-term treatment of ADHD, and they were less efficacious and less well tolerated in adults than in children and adolescents,” wrote Samuele Cortese, MD, PhD, of the University of Southampton (England), and his coauthors. “However, the included medications were not equivalent in relation to their mean effect size, which ranged from moderate to high and varied according to the type of rater.”
For example, while atomoxetine had the lowest mean effect size in children and adolescents based on clinicians’ ratings, in adults, it was on par with methylphenidate. Amphetamines increased diastolic blood pressure in children but not in adults.
“Taking into account both efficacy and safety, evidence from this meta-analysis supports methylphenidate in children and adolescents, and amphetamines in adults, as preferred first-choice medications for the short-term treatment of ADHD,” the authors wrote.
Dr. Cortese and his coauthors cited a few limitations. One is that the most recent study included in their meta-analysis was published in April 2017. When the researchers conducted a PubMed search in May 2018, they found three additional studies that met their criteria. “Since we already had 133 included studies, we decided that adding these three studies would not have changed the final results materially,” they wrote.
The study was supported by the Stichting Eunethydis (European Network for Hyperkinetic Disorders), and the U.K. National Institute for Health Research Oxford Health Biomedical Research Centre. Nine authors declared support, funding, or advisory roles with a range of organizations or the pharmaceutical industry.
SOURCE: Cortese S et al. Lancet Psychiatry. 2018 Aug 7. doi: 10.1016/S2215-0366(18)30269-4.
Methylphenidate appears to be the safest and most effective treatment option for attention-deficit/hyperactivity disorder in children and adolescents, while amphetamines are the preferred first-line choice in adults, a systematic review and meta-analysis have found.
Researchers reported the results of a network meta-analysis of 133 double-blind randomized controlled trials – 81 in children and adolescents, 51 in adults, and 1 in both – involving a total of 10,068 children and adolescents, and 8,131 adults. The included studies all compared a range of medications to placebo or in head-to-head trials. The meta-analysis was published online Aug. 7 in The Lancet Psychiatry.
At 12 weeks, all the medications, which included amphetamines, atomoxetine, bupropion, clonidine, guanfacine, methylphenidate, and modafinil, were found to be better than placebo in reducing core ADHD symptoms in children and adolescents, according to clinicians’ ratings. However, when teachers’ ratings were used, only methylphenidate and modafinil were better than placebo.
In adults, clinicians’ ratings found that amphetamines, methylphenidate, bupropion, and atomoxetine – but not modafinil – were better than placebo.
In head-to-head trials, clinicians’ ratings favored amphetamines over modafinil, atomoxetine, and methylphenidate in children, adolescents, and adults.
But in adults, amphetamines, bupropion, and methylphenidate all beat placebo.
When it came to tolerability in children and adolescents, guanfacine and amphetamines were the only two treatments that were less well tolerated than placebo. However, a post hoc analysis suggested lisdexamfetamine had a lower tolerability relative to other amphetamines, at least in children and adolescents. In adults, modafinil, amphetamines, methylphenidate, and atomoxetine were beaten by placebo for tolerability.
“Overall, all medications, except modafinil in adults, were more efficacious than placebo for the short-term treatment of ADHD, and they were less efficacious and less well tolerated in adults than in children and adolescents,” wrote Samuele Cortese, MD, PhD, of the University of Southampton (England), and his coauthors. “However, the included medications were not equivalent in relation to their mean effect size, which ranged from moderate to high and varied according to the type of rater.”
For example, while atomoxetine had the lowest mean effect size in children and adolescents based on clinicians’ ratings, in adults, it was on par with methylphenidate. Amphetamines increased diastolic blood pressure in children but not in adults.
“Taking into account both efficacy and safety, evidence from this meta-analysis supports methylphenidate in children and adolescents, and amphetamines in adults, as preferred first-choice medications for the short-term treatment of ADHD,” the authors wrote.
Dr. Cortese and his coauthors cited a few limitations. One is that the most recent study included in their meta-analysis was published in April 2017. When the researchers conducted a PubMed search in May 2018, they found three additional studies that met their criteria. “Since we already had 133 included studies, we decided that adding these three studies would not have changed the final results materially,” they wrote.
The study was supported by the Stichting Eunethydis (European Network for Hyperkinetic Disorders), and the U.K. National Institute for Health Research Oxford Health Biomedical Research Centre. Nine authors declared support, funding, or advisory roles with a range of organizations or the pharmaceutical industry.
SOURCE: Cortese S et al. Lancet Psychiatry. 2018 Aug 7. doi: 10.1016/S2215-0366(18)30269-4.
FROM THE LANCET PSYCHIATRY
Key clinical point: “All medications, except modafinil in adults, were more efficacious than placebo for the short-term treatment of ADHD.”
Major finding: Methylphenidate showed the greatest tolerability and efficacy of ADHD treatments for children and adolescents.
Study details: Systematic review and meta-analysis of 133 double-blind randomized controlled trials.
Disclosures: The study was supported by the Stichting Eunethydis (European Network for Hyperkinetic Disorders), and the U.K. National Institute for Health Research Oxford Health Biomedical Research Centre. Nine authors declared support, funding, or advisory roles with a range of organizations or the pharmaceutical industry.
Source: Cortese S et al. Lancet Psychiatry. 2018 Aug 7. doi: 10.1016/S2215-0366(18)30269-4.
Social media use linked to 10% increase in risk of new ADHD symptoms among teens
according to results from a prospective, longitudinal cohort study published in JAMA.
“Further research is needed to determine whether this association is causal,” cautioned the investigators.
Between fall 2014 (10th grade) and fall 2016 (12th grade), researchers studied 3,051 students from 10 different Los Angeles schools who were enrolled in the Happiness & Health Study and did not have significant ADHD symptoms; of these students, 2,587 adolescents (mean age 16 years, 54% girls) self-reported digital media use activities from 14 different types through surveys administered at baseline and again at 6-month, 12-month, 18-month and 24-month follow-up. Digital use activities included checking social media sites, engaging with social media content, texting, streaming music, and browsing or viewing images or videos, among others.
“Although some emerging research indicates that ADHD levels and use of certain forms of modern media may be concurrently associated, the role of modern digital media use in ADHD risk largely remains unclear from the prior literature due to limitations in exposure assessment and the application of designs incapable of supporting temporal or causal inferences,” wrote Chaelin K. Ra, MPH, of the University of Southern California, Los Angeles, and his colleagues. “The current study provides new longitudinal evidence on this topic using a 5-wave prospective design and comprehensive assessment across a wide continuum of digital media exposure, including numerous media platforms currently popular among youth.”
Students ranked their activities in a cumulative index and indicated whether they participated in those activities “0, 1-2 times per week, 1-2 times per day, or many times per day.” They also filled out the DSM-IV Current Symptoms Self-Report Form, which asked them to report whether they experienced any of nine different hyperactivity-impulsivity symptoms such as “difficulty organizing and completing tasks.”
Mr. Ra and his colleagues found that 81% of adolescents reported at least one digital media activity performed at a high-frequency rate, with 54% reporting they checked social media at a high-frequency rate. There was a mean of four baseline digital media activities performed at a high-frequency rate among students surveyed. Each additional digital media activity used at a high-frequency rate carried a statistically significant association of subsequent ADHD symptoms over the follow-up period (odds ratio 1.1; 95% confidence interval, 1.06-1.16), which remained after adjustment for covariates including age, sex, and subsidized lunch availability tied to family income (OR 1.1; 95% CI, 1.05-1.15). The researchers noted that there was a 5% mean prevalence of subsequent ADHD symptoms in follow-up among patients who reported no baseline high-frequency rate of digital media use, compared with 10% in students indicating 7 high-frequency activities and 11% in students indicating 14 high-frequency activities.
Limitations of the study included potential inaccuracies in self-reporting ADHD symptoms as opposed to students receiving a diagnosis through a clinical interview, the possibility of the association being influenced by ADHD symptoms not detected in the study, the fact that the media use measure in the study had not been validated, and use of a targeted age range in the sample of students that excluded students without surveys who had differing demographic data from the rest of the cohort, according to the researchers.
The authors reported having no relevant financial disclosures. The study was supported by a grant from the National Institutes of Health.
SOURCE: Ra CK et al. JAMA. 2018 Jul 17. doi: 10.1001/jama.2018.8931.
This study is among the first to capture current media use because technology tends to outpace researchers’ ability to publish data “within relevant time frames,” Jenny Radesky, MD of the University of Michigan in Ann Arbor, said in an editorial.
While previous studies linking ADHD symptoms and media use analyzed use of media such as television shows and video games, this study analyzes smartphone use and “always-on” media such as social media in addition to traditional media, she said.
It should be noted that “high-frequency media use was associated with only a 10% increased risk of later ADHD symptoms overall.
“Although the authors were able to adjust for income and mental health symptoms, they did not assess parent media use or whether the parents were involved in how the adolescents used media,” Dr. Radesky said. “Parent media use correlates with child media use, may interrupt parent-child activities, and is associated with child behavior difficulties in younger children.”
She said the study affirms guidelines from the American Academy of Pediatrics to “prioritize activities that promote adolescent executive functioning and well-being, including sleep, physical activity, distraction-free homework, and positive interactions with family and friends.
“Although not directly addressed by this study, the American Academy of Pediatrics recommendations for parent involvement in their adolescent’s media use – including discussions about prosocial uses of media, digital citizenship, misinformation, and persuasion awareness – are relevant to the cognitive and emotional reactions to digital media of adolescents,” she added.
Dr. Radesky noted that the potential for the association between media use and ADHD symptoms to be influenced by confounders not measured in the study is a “major limitation.”
Dr. Radesky is at the University of Michigan, Ann Arbor. She receives grant support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. These comments summarize her editorial accompanying the article by Ra et al. ( JAMA. 2018;320:237-39 ).
This study is among the first to capture current media use because technology tends to outpace researchers’ ability to publish data “within relevant time frames,” Jenny Radesky, MD of the University of Michigan in Ann Arbor, said in an editorial.
While previous studies linking ADHD symptoms and media use analyzed use of media such as television shows and video games, this study analyzes smartphone use and “always-on” media such as social media in addition to traditional media, she said.
It should be noted that “high-frequency media use was associated with only a 10% increased risk of later ADHD symptoms overall.
“Although the authors were able to adjust for income and mental health symptoms, they did not assess parent media use or whether the parents were involved in how the adolescents used media,” Dr. Radesky said. “Parent media use correlates with child media use, may interrupt parent-child activities, and is associated with child behavior difficulties in younger children.”
She said the study affirms guidelines from the American Academy of Pediatrics to “prioritize activities that promote adolescent executive functioning and well-being, including sleep, physical activity, distraction-free homework, and positive interactions with family and friends.
“Although not directly addressed by this study, the American Academy of Pediatrics recommendations for parent involvement in their adolescent’s media use – including discussions about prosocial uses of media, digital citizenship, misinformation, and persuasion awareness – are relevant to the cognitive and emotional reactions to digital media of adolescents,” she added.
Dr. Radesky noted that the potential for the association between media use and ADHD symptoms to be influenced by confounders not measured in the study is a “major limitation.”
Dr. Radesky is at the University of Michigan, Ann Arbor. She receives grant support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. These comments summarize her editorial accompanying the article by Ra et al. ( JAMA. 2018;320:237-39 ).
This study is among the first to capture current media use because technology tends to outpace researchers’ ability to publish data “within relevant time frames,” Jenny Radesky, MD of the University of Michigan in Ann Arbor, said in an editorial.
While previous studies linking ADHD symptoms and media use analyzed use of media such as television shows and video games, this study analyzes smartphone use and “always-on” media such as social media in addition to traditional media, she said.
It should be noted that “high-frequency media use was associated with only a 10% increased risk of later ADHD symptoms overall.
“Although the authors were able to adjust for income and mental health symptoms, they did not assess parent media use or whether the parents were involved in how the adolescents used media,” Dr. Radesky said. “Parent media use correlates with child media use, may interrupt parent-child activities, and is associated with child behavior difficulties in younger children.”
She said the study affirms guidelines from the American Academy of Pediatrics to “prioritize activities that promote adolescent executive functioning and well-being, including sleep, physical activity, distraction-free homework, and positive interactions with family and friends.
“Although not directly addressed by this study, the American Academy of Pediatrics recommendations for parent involvement in their adolescent’s media use – including discussions about prosocial uses of media, digital citizenship, misinformation, and persuasion awareness – are relevant to the cognitive and emotional reactions to digital media of adolescents,” she added.
Dr. Radesky noted that the potential for the association between media use and ADHD symptoms to be influenced by confounders not measured in the study is a “major limitation.”
Dr. Radesky is at the University of Michigan, Ann Arbor. She receives grant support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. These comments summarize her editorial accompanying the article by Ra et al. ( JAMA. 2018;320:237-39 ).
according to results from a prospective, longitudinal cohort study published in JAMA.
“Further research is needed to determine whether this association is causal,” cautioned the investigators.
Between fall 2014 (10th grade) and fall 2016 (12th grade), researchers studied 3,051 students from 10 different Los Angeles schools who were enrolled in the Happiness & Health Study and did not have significant ADHD symptoms; of these students, 2,587 adolescents (mean age 16 years, 54% girls) self-reported digital media use activities from 14 different types through surveys administered at baseline and again at 6-month, 12-month, 18-month and 24-month follow-up. Digital use activities included checking social media sites, engaging with social media content, texting, streaming music, and browsing or viewing images or videos, among others.
“Although some emerging research indicates that ADHD levels and use of certain forms of modern media may be concurrently associated, the role of modern digital media use in ADHD risk largely remains unclear from the prior literature due to limitations in exposure assessment and the application of designs incapable of supporting temporal or causal inferences,” wrote Chaelin K. Ra, MPH, of the University of Southern California, Los Angeles, and his colleagues. “The current study provides new longitudinal evidence on this topic using a 5-wave prospective design and comprehensive assessment across a wide continuum of digital media exposure, including numerous media platforms currently popular among youth.”
Students ranked their activities in a cumulative index and indicated whether they participated in those activities “0, 1-2 times per week, 1-2 times per day, or many times per day.” They also filled out the DSM-IV Current Symptoms Self-Report Form, which asked them to report whether they experienced any of nine different hyperactivity-impulsivity symptoms such as “difficulty organizing and completing tasks.”
Mr. Ra and his colleagues found that 81% of adolescents reported at least one digital media activity performed at a high-frequency rate, with 54% reporting they checked social media at a high-frequency rate. There was a mean of four baseline digital media activities performed at a high-frequency rate among students surveyed. Each additional digital media activity used at a high-frequency rate carried a statistically significant association of subsequent ADHD symptoms over the follow-up period (odds ratio 1.1; 95% confidence interval, 1.06-1.16), which remained after adjustment for covariates including age, sex, and subsidized lunch availability tied to family income (OR 1.1; 95% CI, 1.05-1.15). The researchers noted that there was a 5% mean prevalence of subsequent ADHD symptoms in follow-up among patients who reported no baseline high-frequency rate of digital media use, compared with 10% in students indicating 7 high-frequency activities and 11% in students indicating 14 high-frequency activities.
Limitations of the study included potential inaccuracies in self-reporting ADHD symptoms as opposed to students receiving a diagnosis through a clinical interview, the possibility of the association being influenced by ADHD symptoms not detected in the study, the fact that the media use measure in the study had not been validated, and use of a targeted age range in the sample of students that excluded students without surveys who had differing demographic data from the rest of the cohort, according to the researchers.
The authors reported having no relevant financial disclosures. The study was supported by a grant from the National Institutes of Health.
SOURCE: Ra CK et al. JAMA. 2018 Jul 17. doi: 10.1001/jama.2018.8931.
according to results from a prospective, longitudinal cohort study published in JAMA.
“Further research is needed to determine whether this association is causal,” cautioned the investigators.
Between fall 2014 (10th grade) and fall 2016 (12th grade), researchers studied 3,051 students from 10 different Los Angeles schools who were enrolled in the Happiness & Health Study and did not have significant ADHD symptoms; of these students, 2,587 adolescents (mean age 16 years, 54% girls) self-reported digital media use activities from 14 different types through surveys administered at baseline and again at 6-month, 12-month, 18-month and 24-month follow-up. Digital use activities included checking social media sites, engaging with social media content, texting, streaming music, and browsing or viewing images or videos, among others.
“Although some emerging research indicates that ADHD levels and use of certain forms of modern media may be concurrently associated, the role of modern digital media use in ADHD risk largely remains unclear from the prior literature due to limitations in exposure assessment and the application of designs incapable of supporting temporal or causal inferences,” wrote Chaelin K. Ra, MPH, of the University of Southern California, Los Angeles, and his colleagues. “The current study provides new longitudinal evidence on this topic using a 5-wave prospective design and comprehensive assessment across a wide continuum of digital media exposure, including numerous media platforms currently popular among youth.”
Students ranked their activities in a cumulative index and indicated whether they participated in those activities “0, 1-2 times per week, 1-2 times per day, or many times per day.” They also filled out the DSM-IV Current Symptoms Self-Report Form, which asked them to report whether they experienced any of nine different hyperactivity-impulsivity symptoms such as “difficulty organizing and completing tasks.”
Mr. Ra and his colleagues found that 81% of adolescents reported at least one digital media activity performed at a high-frequency rate, with 54% reporting they checked social media at a high-frequency rate. There was a mean of four baseline digital media activities performed at a high-frequency rate among students surveyed. Each additional digital media activity used at a high-frequency rate carried a statistically significant association of subsequent ADHD symptoms over the follow-up period (odds ratio 1.1; 95% confidence interval, 1.06-1.16), which remained after adjustment for covariates including age, sex, and subsidized lunch availability tied to family income (OR 1.1; 95% CI, 1.05-1.15). The researchers noted that there was a 5% mean prevalence of subsequent ADHD symptoms in follow-up among patients who reported no baseline high-frequency rate of digital media use, compared with 10% in students indicating 7 high-frequency activities and 11% in students indicating 14 high-frequency activities.
Limitations of the study included potential inaccuracies in self-reporting ADHD symptoms as opposed to students receiving a diagnosis through a clinical interview, the possibility of the association being influenced by ADHD symptoms not detected in the study, the fact that the media use measure in the study had not been validated, and use of a targeted age range in the sample of students that excluded students without surveys who had differing demographic data from the rest of the cohort, according to the researchers.
The authors reported having no relevant financial disclosures. The study was supported by a grant from the National Institutes of Health.
SOURCE: Ra CK et al. JAMA. 2018 Jul 17. doi: 10.1001/jama.2018.8931.
FROM JAMA
Key clinical point: High-frequency digital media use carries a statistically significant association with subsequent ADHD symptoms in adolescent students without previous significant ADHD symptoms at baseline.
Major finding: Of the adolescent students without significant ADHD symptoms,
Study details: A prospective, longitudinal study of 3,051 adolescent students (mean age, 16 years) in the Happiness & Health Study, followed for 24 months.
Disclosures: The authors reported having no relevant financial disclosures. The study was supported by a grant from the National Institutes of Health.
Source: Ra CK et al. JAMA. 2018 Jul 17. doi: 10.1001/jama.2018.8931.
It’s not about time
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Like most couples of retirement age, rituals dominate our breakfasts. I eat eggs. Marilyn leans toward baked goods. We each have a bowl of fruit and finish by working the New York Times mini-crossword on our electronic devices. Solving it usually takes somewhere between 40 seconds and 4 minutes. The challenge lies in how fast one can complete the puzzle. And, being who we are, Marilyn and I have ritualized this into a serious competition. She usually takes the first turn and then tries to psyche me out by announcing, “I did it in 2:34, but you should be able to solve it in less than 2 minutes.” This bit of gamesmanship often means that I am going to start the day with thin layer of nervous perspiration.
The claimed disabilities range from an anxiety disorder and ADHD to a problem with reading comprehension. The number of students requesting a test environment modification at Pomona College, Claremont, Calif., is 22% up from 5% in 2014. At Marlboro College in Vermont, one in three students asks for more time or a less distracting setting.
This phenomenon raises two obvious questions. First, what has happened to the bell-shaped curve? Was it too boring hanging out with all those people under the bell? Do folks feel safer and more secure in the tails? I guess we have to be happy that young people are less afraid to admit they are different. But it does make one wonder how we should go about defining a disability.
The second question is whether timed tests deserve a place in our educational toolbox? How often is processing speed important? I would like the woman piloting my flight to San Francisco to be quick-witted. But what about the research chemist working on a more durable tire compound? Is it a problem that it took him 30% longer than his classmates to successfully finish his college statistics final exam?
What about the lawyer who bills you $500 per hour to review the contract with your employer? It might have been helpful to know before you hired him that he routinely requested an extra hour and a half to complete his exams in law school. But I suspect that for the most part timed tests probably don’t produce better graduates. In the past they may have been used to thin oversubscribed disciplines, and certainly time limits have been the norm at every level of education I encountered. However, the best taught courses had exams with an abundance of time. Either you knew the information or you didn’t. An extra 2 hours wasn’t going to make a difference.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].