User login
E-cigarettes beat nicotine patch for smoking cessation
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
Any smoking cessation benefit of e-cigarettes needs to be balanced against short- and long-term safety risks of using these products, according to authors of an editorial.
In the study by Hajek et al., the 1-year abstinence rate of 18% in the e-cigarette group compares favorably to what has been reported for Food and Drug Administration–approved smoking cessation treatments, according to Belinda Borelli, PhD, and George T. O’Connor, MD.
The short-term safety data in the trial are “reassuring,” with a low incidence of oropharyngeal irritation, no excess wheezing or dyspnea, and greater declines in cough and phlegm production versus the nicotine replacement group, Dr. Borelli and Dr. O’Connor said.
However, a notable finding was that 80% of participants in the e-cigarette group were still using the product at 1 year, versus just 9% in the nicotine replacement group. “This differential pattern of long-term use raises concerns about the health consequences of long-term e-cigarette use,” they said.
E-cigarette vapor generally has lower levels of toxins and fewer biologic effects than does tobacco smoke, but it has produced adverse biologic effects in animal models and human cells in vitro, according to the authors.
“These findings argue against complacency in accepting the transition from tobacco smoking to indefinite e-cigarette use as a completely successful smoking cessation outcome,” they wrote. Policy analysts need to be careful and do their due diligence to ensure all consequences of the policy options are fully understood, especially as pharmaceuticals account for greater costs in the Medicare program. Future policy analyses must account for changes to Medicare costs as well as beneficiary costs to understand the overall effects of policy changes.
Dr. Borelli is with the Center for Behavioral Science Research, department of health policy and health services research at the Henry M. Goldman School of Dental Medicine, Boston University. Dr. O’Connor is with the Pulmonary Center at Boston University and with the division of pulmonary, allergy, sleep, and critical care medicine at Boston Medical Center. Dr. Borelli had no disclosures; Dr. O’Connor reported disclosures with AstraZeneca and Janssen Pharmaceuticals. They made these comments in an accompanying editorial (N Eng J Med. 2019. doi: 10.1056/NEJMe1816406).
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
E-cigarettes might be more effective for smoking cessation than nicotine replacement therapy, results of a randomized study of almost 900 adults suggest.
Rates of abstinence at 1 year were 18% for adults who used refillable e-cigarettes to wean themselves off smoking, according to the reported results, compared with about 10% for those who tried nicotine replacement therapies.
“This is particularly noteworthy given that nicotine replacement was used under expert guidance, with access to the full range of nicotine replacement products, and with 88.1% of participants using combination treatments,” said investigator Peter Hajek, PhD, of Queen Mary University of London, and his coauthors in the New England Journal of Medicine.
The findings contrast with those of earlier studies, which showed a lesser effect of e-cigarettes as a stop-smoking strategy, Dr. Hajek and coauthors wrote.
In previous studies, participants used first-generation cartridge-based e-cigarettes, while in the present study, they were given second-generation refillable e-cigarettes and free choice of e-liquids, the authors noted. Moreover, those previous studies provided limited face-to-face support, they said, but
The randomized study by Dr. Hajek and his colleagues included 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service. They were randomized to receive either an e-cigarette starter pack and one bottle of nicotine-containing e-liquid, or 3 months’ worth of nicotine replacement products of their own choosing. At the 52-week validation visits, the study participants received about the equivalence of about $26 U.S. dollars for their travel and time.
Abstinence from smoking at 52 weeks, which was verified by measuring expired carbon monoxide levels, was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001), according to the report.
However, the rate of continued e-cigarette use was “fairly high,” investigators wrote. Eighty percent of the e-cigarette group was still using their assigned product at 52 weeks, compared with just 9% in the nicotine replacement group.
“This can be seen as problematic if e-cigarette use for a year signals long-term use, which may pose as-yet-unknown health risks,” they said.
Tobacco withdrawal symptoms were less severe and satisfaction ratings were higher with e-cigarettes versus nicotine replacement therapy, similar to what had been observed in previous studies, investigators said.
They cited several limitations. For example, product assignments were not blinded. However, the investigators said they tried to “limit expectation effects by recruiting only participants with no strong product preference.”
Dr. Hajek reported grants and fees from Pfizer unrelated to the present study. Coauthors reported disclosures related to Pfizer and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
SOURCE: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The rate of smokers who continued to use e-cigarettes after 1 year was “fairly high,” which might be problematic.
Major finding: Abstinence from smoking at 52 weeks was achieved in 18.0% of the e-cigarette group and 9.9% of the nicotine replacement group (relative risk, 1.83; 95% confidence interval, 1.30-2.58; P less than .001).
Study details: Randomized study of 886 adults in the United Kingdom attending stop-smoking services provided by the U.K. National Health Service.
Disclosures: Dr. Hajek reported grants and fees from Pfizer unrelated to the present study.The coauthors reported disclosures related to Pfizer, and Johnson and Johnson, along with grants from the U.K. National Institute for Health Research.
Source: Hajek P et al. N Engl J Med. 2019;380:629-37. doi: 10.1056/NEJMoa1808779.
Conservatism spreads in prostate cancer
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
In California, opioids most often prescribed in low-income, mostly white areas
There is a higher prevalence of opioid prescribing and opioid-related overdose deaths concentrated in regions with mostly low-income, white residents, compared with regions with high income and the lowest proportion of white residents, according to a new analysis of data on people living in California.
The findings of this study provide further evidence that the opioid epidemic affects a large proportion of low-income white communities (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6721).
“Whereas most epidemics predominate within social minority groups and previous US drug epidemics have typically been concentrated in nonwhite communities, Joseph Friedman, MPH, from the University of California, Los Angeles, and his colleagues wrote in their study. “Our analysis suggests that, at least in California, an important determinant of this phenomenon may be that white individuals have a higher level of exposure than nonwhite individuals to opioid prescriptions on a per capita basis through the health care system.”
Mr. Friedman and his colleagues analyzed 29.7 million prescription drug records from California’s Controlled Substance Utilization Review and Evaluation System in and examined the prevalence of opioids, benzodiazepines, and stimulants by race, ethnicity, and income level in 1,760 zip codes during 2011-2015. The researchers estimated the prevalence of opioid prescriptions in each zip code by calculating the number of people per zip code receiving an opioid prescription divided by the population of the zip code during each year.
Overall, 23.6% of California residents received at least one opioid prescription each year of the study. The researchers found 44.2% of individuals in zip codes with the lowest income but highest proportion of white residents and 16.1% of individuals in areas with the highest income and lowest proportion of white residents had received a minimum of one opioid prescription each year. The prevalence of stimulant prescriptions was 3.8% in zip codes with high income, and a high proportion of white population, compared with a prevalence of 0.6% in areas with low income and a low proportion of white residents. The researchers noted there was no association between income and benzodiazepine prescription, but the prevalence of benzodiazepine prescriptions was 15.7% in zip codes with the highest proportion of white residents, compared with 7.0% in zip codes with a low proportion of white residents.
During the same time period, there were 9,534 opioid overdose deaths in California from causes such as fentanyl, synthetic opioids, and prescription opioids. “Overdose deaths were highly concentrated in lower-income and mostly white areas,” Mr. Friedman and his colleagues wrote. “We observed an approximate 10-fold difference in overdose rates across the race/ethnicity–income gradient in California.”
Although the number of opioids prescribed each year has decreased since 2012, in a research letter published in the same issue noted that the rate of prescribing is still higher than it was in 1999 (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6989). The authors also pointed out increases in the duration of opioid prescriptions and wide regional variations in opioid prescribing rates.
In their study, Gery P. Guy Jr., PhD, and his colleagues used data from the IQVIA Xponent database from approximately 50,400 retail pharmacies and discovered the average morphine milligram equivalent (MME) per capita had decreased from 641.4 MME per capita in 2015 to 512.6 MME per capita in 2017 (20.1%). The number of opioid prescriptions also decreased from 6.7 per 100 persons in 2015 to 5.0 per 100 persons in 2017 (25.3%). However, during 2015-2017, the average duration of opioid prescriptions increased from 17.7 days to 18.3 days (3.4%), while the median duration increased during the same time from 15.0 days to 20.0 days (33.3%).
While 74.7% of counties reduced the number of opioids prescribed during 2015-2017 and there also were reductions in the rate of high-dose prescribing (76.6%) and overall prescribing rates (74.7%), Dr. Guy of the Centers for Disease Control and Prevention and his colleagues found “substantial variation” in 2017 prescription rates at the county level, with opioids prescribed at 1,061.0 MME per capita at the highest quartile, compared with 182.8 MME per capita at the lowest quartile.
“Recent reductions could be related to policies and strategies aimed at reducing inappropriate prescribing, increased awareness of the risks associated with opioids, and release of the CDC Guideline for Prescribing Opioids for Chronic Pain–United States, 2016,” Dr. Guy and his colleagues noted.
In an additional article published in the same JAMA Internal Medicine issue, Bennett Allen, a research associate at the New York City Department of Health and Mental Hygiene and his colleagues examined the rate of opioid overdose deaths for non-Hispanic white, non-Hispanic black, Hispanic, and undefined other races in New York (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7700). They identified 1,487 deaths in 2017, which included 556 white (37.0%), 421 black (28.0%), 455 Hispanic (31.0%), and 55 undefined (4.0%) opioid overdose deaths. There was a higher rate of fentanyl and/or heroin overdose deaths from younger (aged 15-34 years) white New Yorkers (22.2/100,000 persons; 95% confidence interval, 19.0-25.5), compared with younger black New Yorkers (5.8/100,000; 95% CI, 4.0-8.2) and Hispanic (9.7/100,000; 95% CI, 7.6-12.1).
Among older residents (aged 55-84 years), Mr. Allen and his colleagues found higher rates of fentanyl and/or heroin overdose for black New Yorkers (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with older white New Yorkers (9.4/100,000 persons; 95% CI, 7.3-11.8), as well as significantly higher rates of cocaine overdose (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with white (5.1/100,000 persons; 95% CI, 3.6-7.0) and Hispanic residents (11.8/100,000 persons; 95% CI, 8.9-15.4).
“The distinct age distribution and drug involvement of overdose deaths among New York City blacks, Latinos, and whites, along with complementary evidence about drug use trajectories, highlight the need for heterogeneous approaches to treatment and the equitable allocation of treatment and health care resources to reach diverse populations at risk of overdose,” Mr. Allen and his colleagues wrote.
Dr. Schriger reported support from Korein Foundation for his time working on the study by Friedman et al. The other authors reported no conflicts of interest.
The results published by Friedman et al. are a reminder that we can use regional prescribing trends to identify communities most susceptible to the opioid epidemic and give them the resources they need to combat opioid addiction, Vice Adm. Jerome M. Adams, MD, MPH, and Adm. Brett P. Giroir, MD, wrote in a related editorial.
“Discussion of overdose risks and coprescribing of naloxone must become routine if we are to make opioid prescribing safer,” the authors wrote.
Physicians also can help respond to the opioid epidemic outside of prescribing by promoting evidence-based nonopioid and nonpharmaceutical pain treatments, screening their patients for OUD and OUD risks, and acknowledging “that the problem cannot be solved by medical interventions alone.” Individual, environmental, and societal factors also contribute to the opioid epidemic, and physicians are uniquely suited to spearhead efforts aimed at addressing comprehensive opioid misuse.
“Physicians stand out as natural leaders to help solve the crises because of the depth of their knowledge, immediacy of their contact with patients, and relatively high level of respect their profession enjoys,” Dr. Adams and Dr. Giroir wrote. “We thereby call on our nation’s doctors to embrace their roles in the clinic and beyond to help educate communities, bring together stakeholders, and be part of the cultural change to support people living free from addiction.”
Dr. Adams is the 20th surgeon general of the United States at the U.S. Public Health Service and HHS; Dr. Giroir is the 16th U.S. assistant secretary for health at the U.S. Public Health Service and HHS. They reported no relevant conflicts of interest. Their invited commentary accompanied the three related articles in the publication (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7934 ).
The results published by Friedman et al. are a reminder that we can use regional prescribing trends to identify communities most susceptible to the opioid epidemic and give them the resources they need to combat opioid addiction, Vice Adm. Jerome M. Adams, MD, MPH, and Adm. Brett P. Giroir, MD, wrote in a related editorial.
“Discussion of overdose risks and coprescribing of naloxone must become routine if we are to make opioid prescribing safer,” the authors wrote.
Physicians also can help respond to the opioid epidemic outside of prescribing by promoting evidence-based nonopioid and nonpharmaceutical pain treatments, screening their patients for OUD and OUD risks, and acknowledging “that the problem cannot be solved by medical interventions alone.” Individual, environmental, and societal factors also contribute to the opioid epidemic, and physicians are uniquely suited to spearhead efforts aimed at addressing comprehensive opioid misuse.
“Physicians stand out as natural leaders to help solve the crises because of the depth of their knowledge, immediacy of their contact with patients, and relatively high level of respect their profession enjoys,” Dr. Adams and Dr. Giroir wrote. “We thereby call on our nation’s doctors to embrace their roles in the clinic and beyond to help educate communities, bring together stakeholders, and be part of the cultural change to support people living free from addiction.”
Dr. Adams is the 20th surgeon general of the United States at the U.S. Public Health Service and HHS; Dr. Giroir is the 16th U.S. assistant secretary for health at the U.S. Public Health Service and HHS. They reported no relevant conflicts of interest. Their invited commentary accompanied the three related articles in the publication (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7934 ).
The results published by Friedman et al. are a reminder that we can use regional prescribing trends to identify communities most susceptible to the opioid epidemic and give them the resources they need to combat opioid addiction, Vice Adm. Jerome M. Adams, MD, MPH, and Adm. Brett P. Giroir, MD, wrote in a related editorial.
“Discussion of overdose risks and coprescribing of naloxone must become routine if we are to make opioid prescribing safer,” the authors wrote.
Physicians also can help respond to the opioid epidemic outside of prescribing by promoting evidence-based nonopioid and nonpharmaceutical pain treatments, screening their patients for OUD and OUD risks, and acknowledging “that the problem cannot be solved by medical interventions alone.” Individual, environmental, and societal factors also contribute to the opioid epidemic, and physicians are uniquely suited to spearhead efforts aimed at addressing comprehensive opioid misuse.
“Physicians stand out as natural leaders to help solve the crises because of the depth of their knowledge, immediacy of their contact with patients, and relatively high level of respect their profession enjoys,” Dr. Adams and Dr. Giroir wrote. “We thereby call on our nation’s doctors to embrace their roles in the clinic and beyond to help educate communities, bring together stakeholders, and be part of the cultural change to support people living free from addiction.”
Dr. Adams is the 20th surgeon general of the United States at the U.S. Public Health Service and HHS; Dr. Giroir is the 16th U.S. assistant secretary for health at the U.S. Public Health Service and HHS. They reported no relevant conflicts of interest. Their invited commentary accompanied the three related articles in the publication (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7934 ).
There is a higher prevalence of opioid prescribing and opioid-related overdose deaths concentrated in regions with mostly low-income, white residents, compared with regions with high income and the lowest proportion of white residents, according to a new analysis of data on people living in California.
The findings of this study provide further evidence that the opioid epidemic affects a large proportion of low-income white communities (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6721).
“Whereas most epidemics predominate within social minority groups and previous US drug epidemics have typically been concentrated in nonwhite communities, Joseph Friedman, MPH, from the University of California, Los Angeles, and his colleagues wrote in their study. “Our analysis suggests that, at least in California, an important determinant of this phenomenon may be that white individuals have a higher level of exposure than nonwhite individuals to opioid prescriptions on a per capita basis through the health care system.”
Mr. Friedman and his colleagues analyzed 29.7 million prescription drug records from California’s Controlled Substance Utilization Review and Evaluation System in and examined the prevalence of opioids, benzodiazepines, and stimulants by race, ethnicity, and income level in 1,760 zip codes during 2011-2015. The researchers estimated the prevalence of opioid prescriptions in each zip code by calculating the number of people per zip code receiving an opioid prescription divided by the population of the zip code during each year.
Overall, 23.6% of California residents received at least one opioid prescription each year of the study. The researchers found 44.2% of individuals in zip codes with the lowest income but highest proportion of white residents and 16.1% of individuals in areas with the highest income and lowest proportion of white residents had received a minimum of one opioid prescription each year. The prevalence of stimulant prescriptions was 3.8% in zip codes with high income, and a high proportion of white population, compared with a prevalence of 0.6% in areas with low income and a low proportion of white residents. The researchers noted there was no association between income and benzodiazepine prescription, but the prevalence of benzodiazepine prescriptions was 15.7% in zip codes with the highest proportion of white residents, compared with 7.0% in zip codes with a low proportion of white residents.
During the same time period, there were 9,534 opioid overdose deaths in California from causes such as fentanyl, synthetic opioids, and prescription opioids. “Overdose deaths were highly concentrated in lower-income and mostly white areas,” Mr. Friedman and his colleagues wrote. “We observed an approximate 10-fold difference in overdose rates across the race/ethnicity–income gradient in California.”
Although the number of opioids prescribed each year has decreased since 2012, in a research letter published in the same issue noted that the rate of prescribing is still higher than it was in 1999 (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6989). The authors also pointed out increases in the duration of opioid prescriptions and wide regional variations in opioid prescribing rates.
In their study, Gery P. Guy Jr., PhD, and his colleagues used data from the IQVIA Xponent database from approximately 50,400 retail pharmacies and discovered the average morphine milligram equivalent (MME) per capita had decreased from 641.4 MME per capita in 2015 to 512.6 MME per capita in 2017 (20.1%). The number of opioid prescriptions also decreased from 6.7 per 100 persons in 2015 to 5.0 per 100 persons in 2017 (25.3%). However, during 2015-2017, the average duration of opioid prescriptions increased from 17.7 days to 18.3 days (3.4%), while the median duration increased during the same time from 15.0 days to 20.0 days (33.3%).
While 74.7% of counties reduced the number of opioids prescribed during 2015-2017 and there also were reductions in the rate of high-dose prescribing (76.6%) and overall prescribing rates (74.7%), Dr. Guy of the Centers for Disease Control and Prevention and his colleagues found “substantial variation” in 2017 prescription rates at the county level, with opioids prescribed at 1,061.0 MME per capita at the highest quartile, compared with 182.8 MME per capita at the lowest quartile.
“Recent reductions could be related to policies and strategies aimed at reducing inappropriate prescribing, increased awareness of the risks associated with opioids, and release of the CDC Guideline for Prescribing Opioids for Chronic Pain–United States, 2016,” Dr. Guy and his colleagues noted.
In an additional article published in the same JAMA Internal Medicine issue, Bennett Allen, a research associate at the New York City Department of Health and Mental Hygiene and his colleagues examined the rate of opioid overdose deaths for non-Hispanic white, non-Hispanic black, Hispanic, and undefined other races in New York (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7700). They identified 1,487 deaths in 2017, which included 556 white (37.0%), 421 black (28.0%), 455 Hispanic (31.0%), and 55 undefined (4.0%) opioid overdose deaths. There was a higher rate of fentanyl and/or heroin overdose deaths from younger (aged 15-34 years) white New Yorkers (22.2/100,000 persons; 95% confidence interval, 19.0-25.5), compared with younger black New Yorkers (5.8/100,000; 95% CI, 4.0-8.2) and Hispanic (9.7/100,000; 95% CI, 7.6-12.1).
Among older residents (aged 55-84 years), Mr. Allen and his colleagues found higher rates of fentanyl and/or heroin overdose for black New Yorkers (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with older white New Yorkers (9.4/100,000 persons; 95% CI, 7.3-11.8), as well as significantly higher rates of cocaine overdose (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with white (5.1/100,000 persons; 95% CI, 3.6-7.0) and Hispanic residents (11.8/100,000 persons; 95% CI, 8.9-15.4).
“The distinct age distribution and drug involvement of overdose deaths among New York City blacks, Latinos, and whites, along with complementary evidence about drug use trajectories, highlight the need for heterogeneous approaches to treatment and the equitable allocation of treatment and health care resources to reach diverse populations at risk of overdose,” Mr. Allen and his colleagues wrote.
Dr. Schriger reported support from Korein Foundation for his time working on the study by Friedman et al. The other authors reported no conflicts of interest.
There is a higher prevalence of opioid prescribing and opioid-related overdose deaths concentrated in regions with mostly low-income, white residents, compared with regions with high income and the lowest proportion of white residents, according to a new analysis of data on people living in California.
The findings of this study provide further evidence that the opioid epidemic affects a large proportion of low-income white communities (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6721).
“Whereas most epidemics predominate within social minority groups and previous US drug epidemics have typically been concentrated in nonwhite communities, Joseph Friedman, MPH, from the University of California, Los Angeles, and his colleagues wrote in their study. “Our analysis suggests that, at least in California, an important determinant of this phenomenon may be that white individuals have a higher level of exposure than nonwhite individuals to opioid prescriptions on a per capita basis through the health care system.”
Mr. Friedman and his colleagues analyzed 29.7 million prescription drug records from California’s Controlled Substance Utilization Review and Evaluation System in and examined the prevalence of opioids, benzodiazepines, and stimulants by race, ethnicity, and income level in 1,760 zip codes during 2011-2015. The researchers estimated the prevalence of opioid prescriptions in each zip code by calculating the number of people per zip code receiving an opioid prescription divided by the population of the zip code during each year.
Overall, 23.6% of California residents received at least one opioid prescription each year of the study. The researchers found 44.2% of individuals in zip codes with the lowest income but highest proportion of white residents and 16.1% of individuals in areas with the highest income and lowest proportion of white residents had received a minimum of one opioid prescription each year. The prevalence of stimulant prescriptions was 3.8% in zip codes with high income, and a high proportion of white population, compared with a prevalence of 0.6% in areas with low income and a low proportion of white residents. The researchers noted there was no association between income and benzodiazepine prescription, but the prevalence of benzodiazepine prescriptions was 15.7% in zip codes with the highest proportion of white residents, compared with 7.0% in zip codes with a low proportion of white residents.
During the same time period, there were 9,534 opioid overdose deaths in California from causes such as fentanyl, synthetic opioids, and prescription opioids. “Overdose deaths were highly concentrated in lower-income and mostly white areas,” Mr. Friedman and his colleagues wrote. “We observed an approximate 10-fold difference in overdose rates across the race/ethnicity–income gradient in California.”
Although the number of opioids prescribed each year has decreased since 2012, in a research letter published in the same issue noted that the rate of prescribing is still higher than it was in 1999 (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.6989). The authors also pointed out increases in the duration of opioid prescriptions and wide regional variations in opioid prescribing rates.
In their study, Gery P. Guy Jr., PhD, and his colleagues used data from the IQVIA Xponent database from approximately 50,400 retail pharmacies and discovered the average morphine milligram equivalent (MME) per capita had decreased from 641.4 MME per capita in 2015 to 512.6 MME per capita in 2017 (20.1%). The number of opioid prescriptions also decreased from 6.7 per 100 persons in 2015 to 5.0 per 100 persons in 2017 (25.3%). However, during 2015-2017, the average duration of opioid prescriptions increased from 17.7 days to 18.3 days (3.4%), while the median duration increased during the same time from 15.0 days to 20.0 days (33.3%).
While 74.7% of counties reduced the number of opioids prescribed during 2015-2017 and there also were reductions in the rate of high-dose prescribing (76.6%) and overall prescribing rates (74.7%), Dr. Guy of the Centers for Disease Control and Prevention and his colleagues found “substantial variation” in 2017 prescription rates at the county level, with opioids prescribed at 1,061.0 MME per capita at the highest quartile, compared with 182.8 MME per capita at the lowest quartile.
“Recent reductions could be related to policies and strategies aimed at reducing inappropriate prescribing, increased awareness of the risks associated with opioids, and release of the CDC Guideline for Prescribing Opioids for Chronic Pain–United States, 2016,” Dr. Guy and his colleagues noted.
In an additional article published in the same JAMA Internal Medicine issue, Bennett Allen, a research associate at the New York City Department of Health and Mental Hygiene and his colleagues examined the rate of opioid overdose deaths for non-Hispanic white, non-Hispanic black, Hispanic, and undefined other races in New York (JAMA Intern Med. 2019 Feb 11. doi: 10.1001/jamainternmed.2018.7700). They identified 1,487 deaths in 2017, which included 556 white (37.0%), 421 black (28.0%), 455 Hispanic (31.0%), and 55 undefined (4.0%) opioid overdose deaths. There was a higher rate of fentanyl and/or heroin overdose deaths from younger (aged 15-34 years) white New Yorkers (22.2/100,000 persons; 95% confidence interval, 19.0-25.5), compared with younger black New Yorkers (5.8/100,000; 95% CI, 4.0-8.2) and Hispanic (9.7/100,000; 95% CI, 7.6-12.1).
Among older residents (aged 55-84 years), Mr. Allen and his colleagues found higher rates of fentanyl and/or heroin overdose for black New Yorkers (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with older white New Yorkers (9.4/100,000 persons; 95% CI, 7.3-11.8), as well as significantly higher rates of cocaine overdose (25.4/100,000 persons; 95% CI, 20.9-30.0), compared with white (5.1/100,000 persons; 95% CI, 3.6-7.0) and Hispanic residents (11.8/100,000 persons; 95% CI, 8.9-15.4).
“The distinct age distribution and drug involvement of overdose deaths among New York City blacks, Latinos, and whites, along with complementary evidence about drug use trajectories, highlight the need for heterogeneous approaches to treatment and the equitable allocation of treatment and health care resources to reach diverse populations at risk of overdose,” Mr. Allen and his colleagues wrote.
Dr. Schriger reported support from Korein Foundation for his time working on the study by Friedman et al. The other authors reported no conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Key clinical point: The most common users of opioids according to prescription drug records are residents of mostly low-income, white neighborhoods.
Major finding: Compared with 23.6% of all Californians, 44.2% of individuals in zip codes containing mostly low-income, white residents had at least one opioid prescription each year, compared with 16.1% of individuals in high-income zip codes with the lowest population of white residents.
Study details: An analysis of 29.7 million opioid prescription drug records by race and income in California during 2011-2015.
Disclosures: Dr. Schriger reported support from the Korein Foundation for his time working on the study by Friedman et al. The other authors from Friedman et al. reported no conflicts of interest.
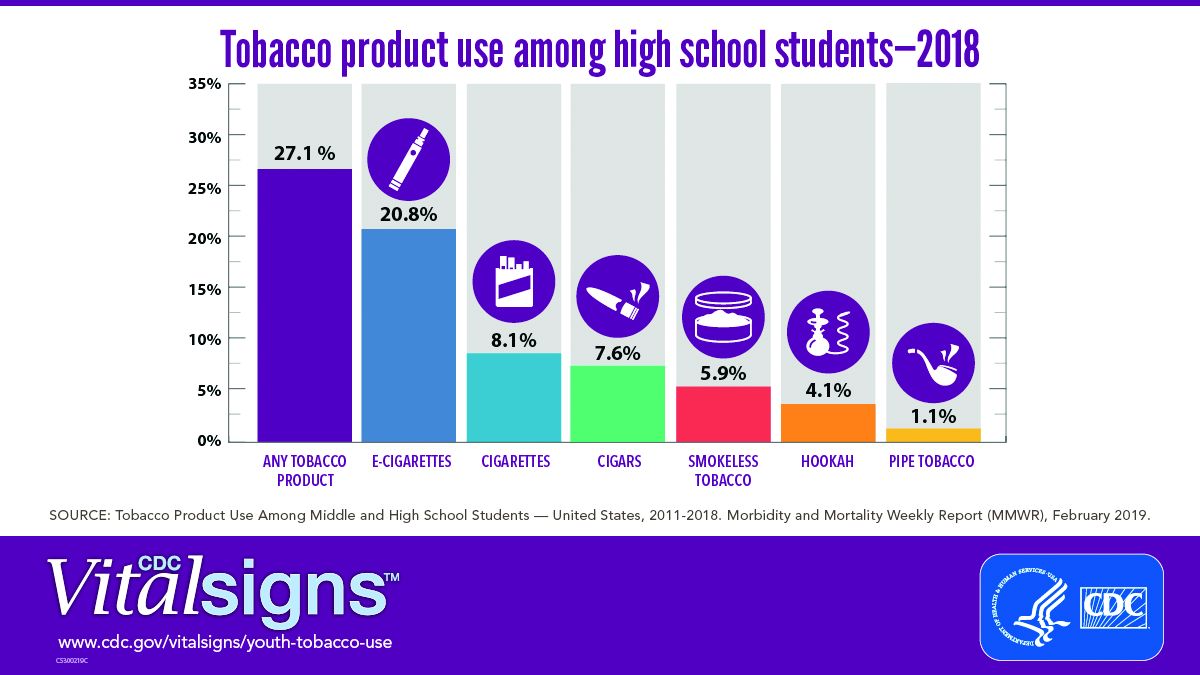
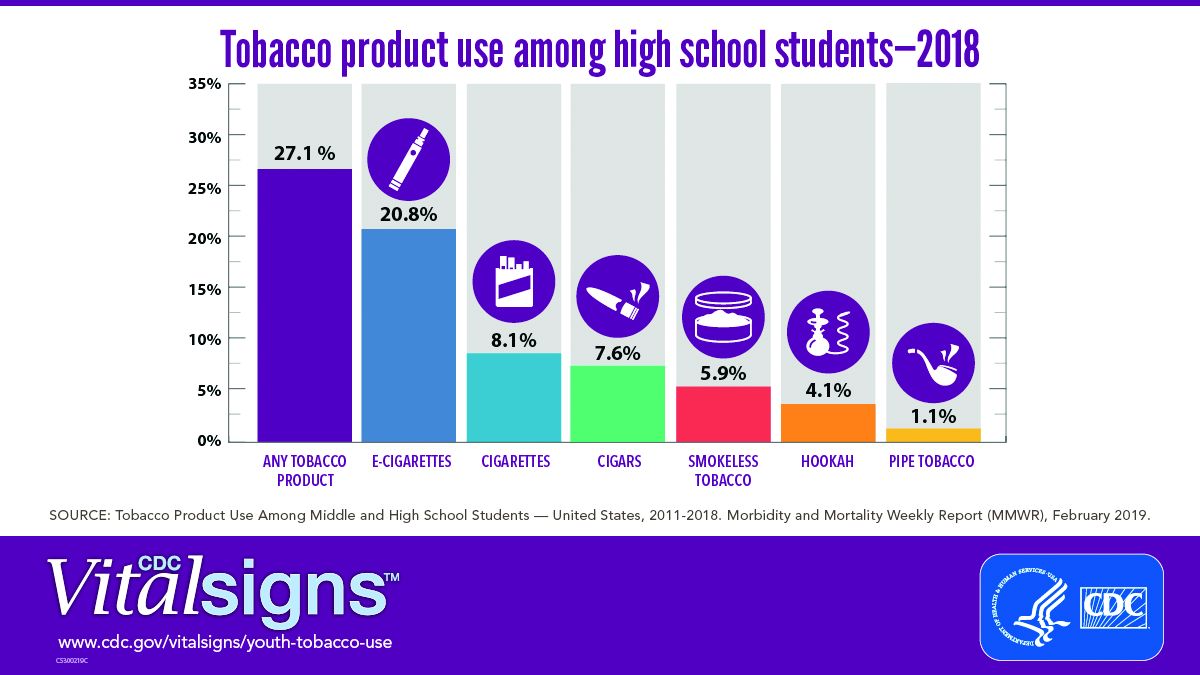
E-cig use reverses progress in reducing tobacco use in teens
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
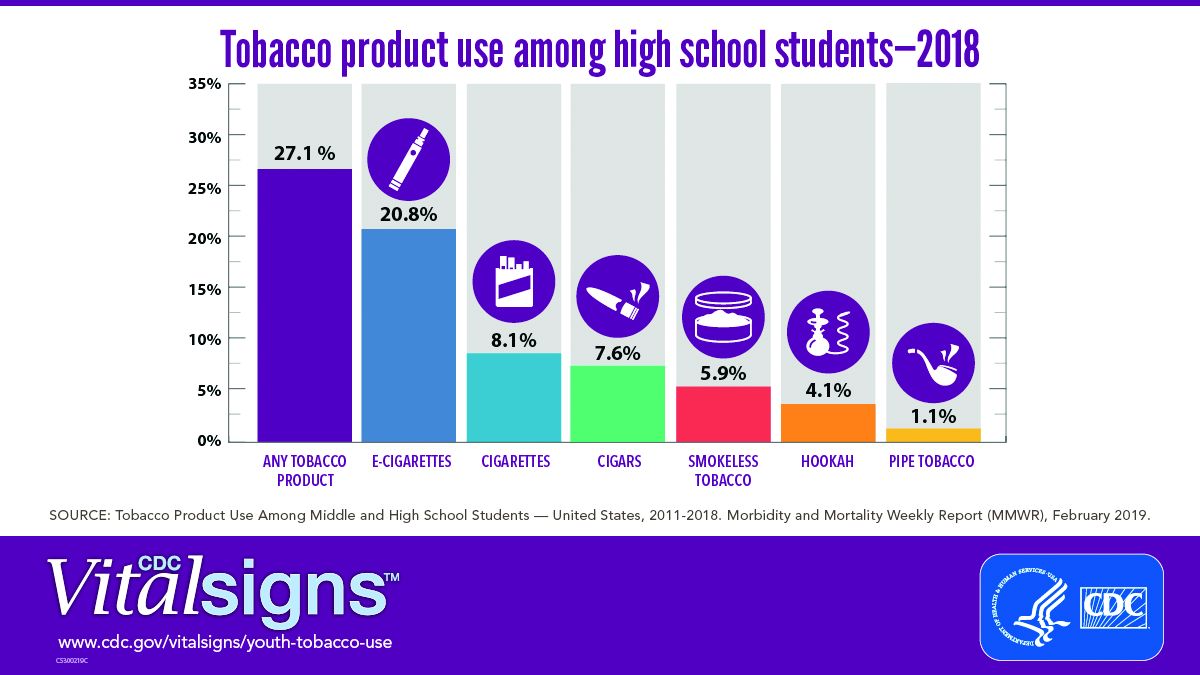
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
A significant increase during 2017-2018 in e-cigarette use among U.S. youths has erased recent progress in reducing overall tobacco product use in this age group, a study from the Centers for Disease Control and Prevention has found.
E-cigarettes are driving the trend. About 4 million high school students in the United States reported using any tobacco product in the last 30 days, and 3 million of them reported using e-cigarettes, according to a Vital Signs document published by the CDC on Feb. 11 in its Morbidity and Mortality Weekly Report.*
In addition, many high school students who use e-cigarettes use them often; 28% reported using the products at least 20 times in the past 28 days, up from 20% in 2017.
“Any use of any tobacco product is unsafe for teens,” Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference to present the findings. Nicotine is highly addictive and can harm brain development in youth, including capacity for learning, memory, and attention, she said.
The rise in e-cigarette use corresponds with the rise in marketing and availability of e-cigarette devices such as JUUL, which dispense nicotine via liquid refill pods available in flavors including strawberry and cotton candy, said Brian King, MPH, PhD, deputy director for research translation at the CDC’s Office on Smoking and Health.
“The advertising will lead a horse to water, the flavors will make them drink, and the nicotine will keep them coming back for more,” said Dr. King.
Approximately 27.1% of high school students and 7.2% of middle school students used a tobacco product in 2018, a significant increase from 2017 data, and with a major increase in e-cigarette use.
No change was noted in the use of other tobacco products, including cigarettes, from 2017 to 2018, according to the report. However, conventional cigarettes remained the most common companion product to e-cigarettes for youth who use two or more tobacco products (two in five high school students and one in three middle school students in 2018). From a demographic standpoint, e-cigarette use was highest among males, whites, and high school students.
Tobacco use in teens is trending in the direction of wiping out the progress made in recent years to reduce exposure to youths. The report noted, “The prevalence of e-cigarette use by U.S. high school students had peaked in 2015 before declining by 29% during 2015-2016 (from 16% to 11.3%); this decline was the first ever recorded for e-cigarette use among youths in the NYTS since monitoring began, and it was subsequently sustained during 2016-2017). However, current e-cigarette use increased by 77.8% among high school students and 48.5% among middle school students during 2017-2018, erasing the progress in reducing e-cigarette use, as well as any tobacco product use, that had occurred in prior years.”
The CDC and the Food and Drug Administration are taking action to curb the rise in e-cigarette use in youth in particular by seeking regulations to make the products less accessible, raising prices, and banning most flavorings, said Dr. Schuchat.
“We have targeted companies engaged in kid friendly marketing,” said Mitch Zeller, JD, director of the Center for Tobacco Products for the FDA.
In a statement published simultaneously with the Vital Signs study, FDA Commissioner Scott Gottlieb, MD, emphasized the link between e-cigarette use in teens and the potential for future tobacco use. “The kids using e-cigarettes are children who rejected conventional cigarettes, but don’t see the same stigma associated with the use of e-cigarettes. But now, having become exposed to nicotine through e-cigs, they will be more likely to smoke.” Dr. Gottlieb declared, “I will not allow a generation of children to become addicted to nicotine through e-cigarettes. We must stop the trends of youth e-cigarette use from continuing to build and will take whatever action is necessary to ensure these kids don’t become future smokers.” He reviewed steps taken in the past year by the FDA to counter tobacco use in teens but he warned of future actions that may need to be taken: “If these youth use trends continue, we’ll be forced to consider regulatory steps that could constrain or even foreclose the opportunities for currently addicted adult smokers to have the same level of access to these products that they now enjoy. I recognize that such a move could come with significant impacts to adult smokers.”
In the meantime, however, parents, teachers, community leaders, and health care providers are on the front lines and can make a difference in protecting youth and curbing nicotine use, Dr. King said.
One of the most important things clinicians can do is to ask young patients specifically about e-cigarette use, he emphasized. Learn and use the terminology the kids are using; ask, “Do you use JUUL?” If they are using these products, “make sure they know they are dangerous,” and can harm the developing brain, he said.
Although there are no currently approved medications to treat nicotine addiction in youth, research suggests that behavioral counseling, as well as reinforcement of the danger of nicotine from parents and other people of influence, can help, Dr. King said.
The Vital Signs report is based on data from the 2011-2018 National Youth Tobacco Survey, which assesses current use of cigarettes, cigars, smokeless tobacco, e-cigarettes, hookahs, pipe tobacco, and bidis among a nationally representative sample of middle and high school students in the United States. The findings were analyzed by the CDC, FDA, and the National Cancer Institute.
SOURCE: Gentzke AS et al. MMWR 2019 Feb 11. doi: 10.15585/mmwr.mm6806e1.
*Correction 2/13/2019 An earlier version of this article misstated the number of students using e-cigarettes as a proportion of all teen tobacco users.
FROM CDC VITAL SIGNS REPORT
The Underrecognized Risk for Drug Overdose Deaths
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
Loan Repayment Plan for Substance Use Clinicians
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
Legal marijuana may complicate SUD treatment in adolescents
BROOKLYN, N.Y. – The legalization of marijuana almost certainly will complicate the treatment of substance use disorder in adolescents, particularly when SUD occurs as a comorbidity of bipolar disorder or other psychiatric diseases, according to an expert review at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
The full effects of marijuana legalization on SUD have not yet been comprehensively studied in children or adults, but the consequences of easier access, diminished stigma, and potential for a diminished sense of harm are widely considered to be an important obstacle to successful therapy in children, said Timothy E. Wilens, MD, chief of the division of child and adolescent psychiatry at Massachusetts General Hospital, Boston.
Comorbid substance use in children with mood disorders or ADHD has long been understood as a form of self-medication. However, use of marijuana, alcohol, or other mood-altering drugs also are known to interfere with treatment, Dr. Wilens said.
The problem is common among adults as well, but adolescents pose a greater challenge.
“Youths are more vulnerable to developing a substance use disorder because reward pathways develop before control pathways,” Dr. Wilens said. He cited data showing that about half of individuals who develop SUD, many of whom have other psychiatric diagnoses, do so by age 18 years, and 80% do so by age 26 years.
“Substance use disorder is a pediatric issue,” he emphasized.
The problem with legalization of marijuana is that adolescents are likely to conclude that what is safe for adults is safe for children. Citing a study that associated increased use of marijuana with reduced perception of harm (and the opposite), Dr. Wilens predicted that adolescents with comorbid SUD would resist treatment.
Because of those concerns, Massachusetts General Hospital, which is based in a state where recreational marijuana use is permitted, has issued a position statement. The statement endorses the study of marijuana for benefit and for harm but expresses specific concern about “the recreational use of marijuana at any age because of the potential downstream effects on children.”
Dr. Wilens expressed particular concern about parental use of marijuana in front of children because of the implication that it is safe and acceptable. For children at risk of comorbid substance use because of a mood disorder, he cautioned parents against even concealed use of marijuana because of the low likelihood that it will go unnoticed.
“Substance use disorders are associated with a more pernicious and longer course in adolescents than children,” said Dr. Wilens, paraphrasing one of the bullet points from the Massachusetts General position statement, which outlines the potential harms for children. Another of the bullet points maintains, “there are known structural and functional brain changes” that have been documented when marijuana use begins in childhood.
Citing a correlation between parental and adolescent marijuana use, He noted that a very high proportion of adolescents with or without mood disorders experiment with marijuana at some point in high school, so there already is resistance to a characterization that it is harmful.
A realistic approach is therefore required in helping adolescents with comorbid substance use to curb this form of self-medication. It is essential to set priorities, he said, when treating adolescents with SUD and comorbid psychiatric disorders. “Don’t even think about treating substance use disorder until you treat the bipolar disease,” he said.
As the symptoms are relieved, the need for self-medication is likely to diminish, but Dr. Wilens cautioned against being too rigid when helping adolescents move away from marijuana and alcohol. He believes a zero tolerance approach can be counterproductive. Rather, he advocates a “harm reduction” approach in which adolescents agree to reasonable reductions, like avoiding marijuana during the week, while they eliminate dependence.
In an overview of pharmacotherapy to reduce cravings for drugs, he cited evidence, as well as personal experience, that over-the-counter N-acetylcysteine can be a useful tool. However, adolescents in particular should be warned about the pungent smell, which has been a barrier to adherence. He also suggested that psychotherapy, with or without pharmacotherapy, is helpful.
Treatment of comorbid SUD is a critical part of achieving control of accompanying psychiatric diseases, but this task might be complicated by legalized recreational marijuana, Dr. Wilens concluded. He encouraged clinicians to recognize that challenge.
Dr. Wilens reported financial relationships with Ironshore Pharmaceuticals, Janssen, KemPharm, and Otsuka Pharmaceutical.
BROOKLYN, N.Y. – The legalization of marijuana almost certainly will complicate the treatment of substance use disorder in adolescents, particularly when SUD occurs as a comorbidity of bipolar disorder or other psychiatric diseases, according to an expert review at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
The full effects of marijuana legalization on SUD have not yet been comprehensively studied in children or adults, but the consequences of easier access, diminished stigma, and potential for a diminished sense of harm are widely considered to be an important obstacle to successful therapy in children, said Timothy E. Wilens, MD, chief of the division of child and adolescent psychiatry at Massachusetts General Hospital, Boston.
Comorbid substance use in children with mood disorders or ADHD has long been understood as a form of self-medication. However, use of marijuana, alcohol, or other mood-altering drugs also are known to interfere with treatment, Dr. Wilens said.
The problem is common among adults as well, but adolescents pose a greater challenge.
“Youths are more vulnerable to developing a substance use disorder because reward pathways develop before control pathways,” Dr. Wilens said. He cited data showing that about half of individuals who develop SUD, many of whom have other psychiatric diagnoses, do so by age 18 years, and 80% do so by age 26 years.
“Substance use disorder is a pediatric issue,” he emphasized.
The problem with legalization of marijuana is that adolescents are likely to conclude that what is safe for adults is safe for children. Citing a study that associated increased use of marijuana with reduced perception of harm (and the opposite), Dr. Wilens predicted that adolescents with comorbid SUD would resist treatment.
Because of those concerns, Massachusetts General Hospital, which is based in a state where recreational marijuana use is permitted, has issued a position statement. The statement endorses the study of marijuana for benefit and for harm but expresses specific concern about “the recreational use of marijuana at any age because of the potential downstream effects on children.”
Dr. Wilens expressed particular concern about parental use of marijuana in front of children because of the implication that it is safe and acceptable. For children at risk of comorbid substance use because of a mood disorder, he cautioned parents against even concealed use of marijuana because of the low likelihood that it will go unnoticed.
“Substance use disorders are associated with a more pernicious and longer course in adolescents than children,” said Dr. Wilens, paraphrasing one of the bullet points from the Massachusetts General position statement, which outlines the potential harms for children. Another of the bullet points maintains, “there are known structural and functional brain changes” that have been documented when marijuana use begins in childhood.
Citing a correlation between parental and adolescent marijuana use, He noted that a very high proportion of adolescents with or without mood disorders experiment with marijuana at some point in high school, so there already is resistance to a characterization that it is harmful.
A realistic approach is therefore required in helping adolescents with comorbid substance use to curb this form of self-medication. It is essential to set priorities, he said, when treating adolescents with SUD and comorbid psychiatric disorders. “Don’t even think about treating substance use disorder until you treat the bipolar disease,” he said.
As the symptoms are relieved, the need for self-medication is likely to diminish, but Dr. Wilens cautioned against being too rigid when helping adolescents move away from marijuana and alcohol. He believes a zero tolerance approach can be counterproductive. Rather, he advocates a “harm reduction” approach in which adolescents agree to reasonable reductions, like avoiding marijuana during the week, while they eliminate dependence.
In an overview of pharmacotherapy to reduce cravings for drugs, he cited evidence, as well as personal experience, that over-the-counter N-acetylcysteine can be a useful tool. However, adolescents in particular should be warned about the pungent smell, which has been a barrier to adherence. He also suggested that psychotherapy, with or without pharmacotherapy, is helpful.
Treatment of comorbid SUD is a critical part of achieving control of accompanying psychiatric diseases, but this task might be complicated by legalized recreational marijuana, Dr. Wilens concluded. He encouraged clinicians to recognize that challenge.
Dr. Wilens reported financial relationships with Ironshore Pharmaceuticals, Janssen, KemPharm, and Otsuka Pharmaceutical.
BROOKLYN, N.Y. – The legalization of marijuana almost certainly will complicate the treatment of substance use disorder in adolescents, particularly when SUD occurs as a comorbidity of bipolar disorder or other psychiatric diseases, according to an expert review at a pediatric psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
The full effects of marijuana legalization on SUD have not yet been comprehensively studied in children or adults, but the consequences of easier access, diminished stigma, and potential for a diminished sense of harm are widely considered to be an important obstacle to successful therapy in children, said Timothy E. Wilens, MD, chief of the division of child and adolescent psychiatry at Massachusetts General Hospital, Boston.
Comorbid substance use in children with mood disorders or ADHD has long been understood as a form of self-medication. However, use of marijuana, alcohol, or other mood-altering drugs also are known to interfere with treatment, Dr. Wilens said.
The problem is common among adults as well, but adolescents pose a greater challenge.
“Youths are more vulnerable to developing a substance use disorder because reward pathways develop before control pathways,” Dr. Wilens said. He cited data showing that about half of individuals who develop SUD, many of whom have other psychiatric diagnoses, do so by age 18 years, and 80% do so by age 26 years.
“Substance use disorder is a pediatric issue,” he emphasized.
The problem with legalization of marijuana is that adolescents are likely to conclude that what is safe for adults is safe for children. Citing a study that associated increased use of marijuana with reduced perception of harm (and the opposite), Dr. Wilens predicted that adolescents with comorbid SUD would resist treatment.
Because of those concerns, Massachusetts General Hospital, which is based in a state where recreational marijuana use is permitted, has issued a position statement. The statement endorses the study of marijuana for benefit and for harm but expresses specific concern about “the recreational use of marijuana at any age because of the potential downstream effects on children.”
Dr. Wilens expressed particular concern about parental use of marijuana in front of children because of the implication that it is safe and acceptable. For children at risk of comorbid substance use because of a mood disorder, he cautioned parents against even concealed use of marijuana because of the low likelihood that it will go unnoticed.
“Substance use disorders are associated with a more pernicious and longer course in adolescents than children,” said Dr. Wilens, paraphrasing one of the bullet points from the Massachusetts General position statement, which outlines the potential harms for children. Another of the bullet points maintains, “there are known structural and functional brain changes” that have been documented when marijuana use begins in childhood.
Citing a correlation between parental and adolescent marijuana use, He noted that a very high proportion of adolescents with or without mood disorders experiment with marijuana at some point in high school, so there already is resistance to a characterization that it is harmful.
A realistic approach is therefore required in helping adolescents with comorbid substance use to curb this form of self-medication. It is essential to set priorities, he said, when treating adolescents with SUD and comorbid psychiatric disorders. “Don’t even think about treating substance use disorder until you treat the bipolar disease,” he said.
As the symptoms are relieved, the need for self-medication is likely to diminish, but Dr. Wilens cautioned against being too rigid when helping adolescents move away from marijuana and alcohol. He believes a zero tolerance approach can be counterproductive. Rather, he advocates a “harm reduction” approach in which adolescents agree to reasonable reductions, like avoiding marijuana during the week, while they eliminate dependence.
In an overview of pharmacotherapy to reduce cravings for drugs, he cited evidence, as well as personal experience, that over-the-counter N-acetylcysteine can be a useful tool. However, adolescents in particular should be warned about the pungent smell, which has been a barrier to adherence. He also suggested that psychotherapy, with or without pharmacotherapy, is helpful.
Treatment of comorbid SUD is a critical part of achieving control of accompanying psychiatric diseases, but this task might be complicated by legalized recreational marijuana, Dr. Wilens concluded. He encouraged clinicians to recognize that challenge.
Dr. Wilens reported financial relationships with Ironshore Pharmaceuticals, Janssen, KemPharm, and Otsuka Pharmaceutical.
EXPERT ANALYSIS FROM THE PSYCHOPHARMACOLOGY UPDATE INSTITUTE
Rise in HCV infection rates linked to OxyContin reformulation
Public health experts have attributed the alarming rise in hepatitis C virus (HCV) infection rates in recent years to the opioid epidemic, and a new Rand study suggests that an effort to deter opioid abuse – namely the 2010 abuse-deterrent reformulation of OxyContin – is partly to blame.
Between 2004 and 2015, HCV infection rates in the United States nearly tripled, but a closer look showed that states with above-median rates of OxyContin misuse prior to the reformulation had a 222% increase in HCV rates, compared with a 75% increase in states with below-median OxyContin misuse, said David Powell, PhD, a senior economist at Rand in Arlington, Va., and his colleagues, Abby Alpert, PhD, and Rosalie L. Pacula, PhD. The report was published in Health Affairs.
The coauthors found that hepatitis C infection rates were not significantly different between the two groups of states before the reformulation (0.350 vs. 0.260). But after 2010, there were large and statistically significant differences in the rates (1.128 vs. 0.455; P less than 0.01), they wrote, noting that the above-median states experienced an additional 0.58 HCV infections per 100,000 population through 2015 relative to the below-median states).
HCV infection rates declined during the 1990s followed by a plateau beginning around 2003, then rose sharply beginning in 2010, coinciding with the introduction of the release of the abuse-deterrent formulation of OxyContin, which is one of the most commonly misused opioid analgesics, the investigators said, explaining that the reformulated version was harder to crush or dissolve, making it more difficult to inhale or inject.
“Prior studies have shown that, after OxyContin became more difficult to abuse, some nonmedical users of OxyContin switched to heroin (a pharmacologically similar opiate),” they noted.
This led to a decline of more than 40% in OxyContin misuse but also to a sharp increase in heroin overdoses after 2010.
The investigators assessed whether the related increase in heroin use might explain the increase in HCV infections, which can be transmitted through shared needle use.
Using a quasi-experimental difference-in-differences approach, they examined whether states with higher exposure to the reformulated OxyContin had faster growth of HCV infection rates after the reformulations, and as a falsification exercise, they also looked at whether the nonmedical use of pain relievers other than OxyContin predicted post-reformulation HCV infection rate increases.
HCV infection rates for each calendar year from 2004 to 2015 were assessed using confirmed case reports collected by the Centers for Disease Control and Prevention, and nonmedical OxyContin use was measured using self-reported data from the National Survey on Drug Use and Health, which is the largest U.S. survey on substance use disorder.
The two groups of states had similar demographic and economic conditions, except that the above-median misuse states had smaller populations and a larger proportion of white residents.
Of note, the patterns of HCV infection mirrored those of heroin overdoses. There was small relative increase in HCV infection rates in 2010 in the above-median OxyContin misuse states, and the gap between above- and below-median misuse states widened more rapidly from 2011 to 2013. “This striking inflection point in the trend of hepatitis C infections for high-misuse states after 2010 mimics the inflection in heroin overdoses that occurred as a result of the reformulation,” they said, noting that heroin morality per 100,000 population was nearly identical in the two groups of states in the pre-reformulation period (0.859 and 0.847).
The falsification exercise looking at nonmedical use of pain relievers other than OxyContin in the two groups of states showed that after 2010 groups’ rates of hepatitis C infections grew at virtually identical rates.
“Thus, the differential risk in hepatitis C infections was uniquely associated with OxyContin misuse, rather than prescription pain reliever misuse more generally,” they said. “This suggests that it was the OxyContin reformulation, not other policies broadly affecting opioids, that drove much of the differential growth.”
The investigators controlled for numerous other factors, including opioid policies that might have an impact on OxyContin and heroin use, prescription drug monitoring programs and pain clinic regulations, as well as the role of major pill-mill crackdowns in 2010 and 2011.
The findings represent a “substantial public health concern,” they said, explaining that, while “considerable policy attention is being given to managing the opioid epidemic ... a ‘silent epidemic’ of hepatitis C has emerged as a result of a transition in the mode of administration toward injection drug use.”
In 2017, the CDC reported on this link between the opioid epidemic and rising HCV infection rates, as well.
Dr. Powell and his colleagues wrote.
Their findings regarding the unintended consequences of the OxyContin reformulation suggest that caution is warranted with respect to future interventions that limit the supply of abusable prescription opioids, they said, adding that “such interventions must be paired with polices that alleviate the harms associated with switching to illicit drugs, such as improved access to substance use disorder treatment and increased efforts aimed at identifying and treating diseases associated with injection drug use.”
However, policy makers and medical professionals also must recognize that reducing opioid-related mortality and increasing access to drug treatment might not be sufficient to fully address all of the public health consequences associated with the opioid crisis. As additional reformulations of opioids are promoted and more policies seek to limit access to prescription opioids, “both the medical and the law enforcement communities must recognize the critical transition from prescription opioids to other drugs, particularly those that are injected, and be prepared to consider complementary strategies that can effectively reduce the additional harms from the particular mode of drug use,” they concluded.
The coauthors cited several limitations, including the possibility that true hepatitis C infection rates might have been underestimated in the study.
He and Dr. Pacula received funding from the National Institute on Drug Abuse. Dr. Powell also cited funding from the Rand Alumni Impact Award.
SOURCE: Powell D et al. Health Aff. 2019;38(2):287-94.
Increases have been seen not only in infectious diseases but also in cardiovascular diseases as intravenous opioid use has risen, Mark S. Gold, MD, said in an interview. “These emerging co-occurring diseases tend to lag behind drug deaths and other data,” he said.
The study by Powell et al. shows that drugs of abuse are dangerous, and that, with addictive use, we find consequences. “Each change appears to bring with it intended consequences we study, but over time, unintended consequences emerge,” he said. “It is important to remain vigilant.”
Dr. Gold is 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis.
Increases have been seen not only in infectious diseases but also in cardiovascular diseases as intravenous opioid use has risen, Mark S. Gold, MD, said in an interview. “These emerging co-occurring diseases tend to lag behind drug deaths and other data,” he said.
The study by Powell et al. shows that drugs of abuse are dangerous, and that, with addictive use, we find consequences. “Each change appears to bring with it intended consequences we study, but over time, unintended consequences emerge,” he said. “It is important to remain vigilant.”
Dr. Gold is 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis.
Increases have been seen not only in infectious diseases but also in cardiovascular diseases as intravenous opioid use has risen, Mark S. Gold, MD, said in an interview. “These emerging co-occurring diseases tend to lag behind drug deaths and other data,” he said.
The study by Powell et al. shows that drugs of abuse are dangerous, and that, with addictive use, we find consequences. “Each change appears to bring with it intended consequences we study, but over time, unintended consequences emerge,” he said. “It is important to remain vigilant.”
Dr. Gold is 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis.
Public health experts have attributed the alarming rise in hepatitis C virus (HCV) infection rates in recent years to the opioid epidemic, and a new Rand study suggests that an effort to deter opioid abuse – namely the 2010 abuse-deterrent reformulation of OxyContin – is partly to blame.
Between 2004 and 2015, HCV infection rates in the United States nearly tripled, but a closer look showed that states with above-median rates of OxyContin misuse prior to the reformulation had a 222% increase in HCV rates, compared with a 75% increase in states with below-median OxyContin misuse, said David Powell, PhD, a senior economist at Rand in Arlington, Va., and his colleagues, Abby Alpert, PhD, and Rosalie L. Pacula, PhD. The report was published in Health Affairs.
The coauthors found that hepatitis C infection rates were not significantly different between the two groups of states before the reformulation (0.350 vs. 0.260). But after 2010, there were large and statistically significant differences in the rates (1.128 vs. 0.455; P less than 0.01), they wrote, noting that the above-median states experienced an additional 0.58 HCV infections per 100,000 population through 2015 relative to the below-median states).
HCV infection rates declined during the 1990s followed by a plateau beginning around 2003, then rose sharply beginning in 2010, coinciding with the introduction of the release of the abuse-deterrent formulation of OxyContin, which is one of the most commonly misused opioid analgesics, the investigators said, explaining that the reformulated version was harder to crush or dissolve, making it more difficult to inhale or inject.
“Prior studies have shown that, after OxyContin became more difficult to abuse, some nonmedical users of OxyContin switched to heroin (a pharmacologically similar opiate),” they noted.
This led to a decline of more than 40% in OxyContin misuse but also to a sharp increase in heroin overdoses after 2010.
The investigators assessed whether the related increase in heroin use might explain the increase in HCV infections, which can be transmitted through shared needle use.
Using a quasi-experimental difference-in-differences approach, they examined whether states with higher exposure to the reformulated OxyContin had faster growth of HCV infection rates after the reformulations, and as a falsification exercise, they also looked at whether the nonmedical use of pain relievers other than OxyContin predicted post-reformulation HCV infection rate increases.
HCV infection rates for each calendar year from 2004 to 2015 were assessed using confirmed case reports collected by the Centers for Disease Control and Prevention, and nonmedical OxyContin use was measured using self-reported data from the National Survey on Drug Use and Health, which is the largest U.S. survey on substance use disorder.
The two groups of states had similar demographic and economic conditions, except that the above-median misuse states had smaller populations and a larger proportion of white residents.
Of note, the patterns of HCV infection mirrored those of heroin overdoses. There was small relative increase in HCV infection rates in 2010 in the above-median OxyContin misuse states, and the gap between above- and below-median misuse states widened more rapidly from 2011 to 2013. “This striking inflection point in the trend of hepatitis C infections for high-misuse states after 2010 mimics the inflection in heroin overdoses that occurred as a result of the reformulation,” they said, noting that heroin morality per 100,000 population was nearly identical in the two groups of states in the pre-reformulation period (0.859 and 0.847).
The falsification exercise looking at nonmedical use of pain relievers other than OxyContin in the two groups of states showed that after 2010 groups’ rates of hepatitis C infections grew at virtually identical rates.
“Thus, the differential risk in hepatitis C infections was uniquely associated with OxyContin misuse, rather than prescription pain reliever misuse more generally,” they said. “This suggests that it was the OxyContin reformulation, not other policies broadly affecting opioids, that drove much of the differential growth.”
The investigators controlled for numerous other factors, including opioid policies that might have an impact on OxyContin and heroin use, prescription drug monitoring programs and pain clinic regulations, as well as the role of major pill-mill crackdowns in 2010 and 2011.
The findings represent a “substantial public health concern,” they said, explaining that, while “considerable policy attention is being given to managing the opioid epidemic ... a ‘silent epidemic’ of hepatitis C has emerged as a result of a transition in the mode of administration toward injection drug use.”
In 2017, the CDC reported on this link between the opioid epidemic and rising HCV infection rates, as well.
Dr. Powell and his colleagues wrote.
Their findings regarding the unintended consequences of the OxyContin reformulation suggest that caution is warranted with respect to future interventions that limit the supply of abusable prescription opioids, they said, adding that “such interventions must be paired with polices that alleviate the harms associated with switching to illicit drugs, such as improved access to substance use disorder treatment and increased efforts aimed at identifying and treating diseases associated with injection drug use.”
However, policy makers and medical professionals also must recognize that reducing opioid-related mortality and increasing access to drug treatment might not be sufficient to fully address all of the public health consequences associated with the opioid crisis. As additional reformulations of opioids are promoted and more policies seek to limit access to prescription opioids, “both the medical and the law enforcement communities must recognize the critical transition from prescription opioids to other drugs, particularly those that are injected, and be prepared to consider complementary strategies that can effectively reduce the additional harms from the particular mode of drug use,” they concluded.
The coauthors cited several limitations, including the possibility that true hepatitis C infection rates might have been underestimated in the study.
He and Dr. Pacula received funding from the National Institute on Drug Abuse. Dr. Powell also cited funding from the Rand Alumni Impact Award.
SOURCE: Powell D et al. Health Aff. 2019;38(2):287-94.
Public health experts have attributed the alarming rise in hepatitis C virus (HCV) infection rates in recent years to the opioid epidemic, and a new Rand study suggests that an effort to deter opioid abuse – namely the 2010 abuse-deterrent reformulation of OxyContin – is partly to blame.
Between 2004 and 2015, HCV infection rates in the United States nearly tripled, but a closer look showed that states with above-median rates of OxyContin misuse prior to the reformulation had a 222% increase in HCV rates, compared with a 75% increase in states with below-median OxyContin misuse, said David Powell, PhD, a senior economist at Rand in Arlington, Va., and his colleagues, Abby Alpert, PhD, and Rosalie L. Pacula, PhD. The report was published in Health Affairs.
The coauthors found that hepatitis C infection rates were not significantly different between the two groups of states before the reformulation (0.350 vs. 0.260). But after 2010, there were large and statistically significant differences in the rates (1.128 vs. 0.455; P less than 0.01), they wrote, noting that the above-median states experienced an additional 0.58 HCV infections per 100,000 population through 2015 relative to the below-median states).
HCV infection rates declined during the 1990s followed by a plateau beginning around 2003, then rose sharply beginning in 2010, coinciding with the introduction of the release of the abuse-deterrent formulation of OxyContin, which is one of the most commonly misused opioid analgesics, the investigators said, explaining that the reformulated version was harder to crush or dissolve, making it more difficult to inhale or inject.
“Prior studies have shown that, after OxyContin became more difficult to abuse, some nonmedical users of OxyContin switched to heroin (a pharmacologically similar opiate),” they noted.
This led to a decline of more than 40% in OxyContin misuse but also to a sharp increase in heroin overdoses after 2010.
The investigators assessed whether the related increase in heroin use might explain the increase in HCV infections, which can be transmitted through shared needle use.
Using a quasi-experimental difference-in-differences approach, they examined whether states with higher exposure to the reformulated OxyContin had faster growth of HCV infection rates after the reformulations, and as a falsification exercise, they also looked at whether the nonmedical use of pain relievers other than OxyContin predicted post-reformulation HCV infection rate increases.
HCV infection rates for each calendar year from 2004 to 2015 were assessed using confirmed case reports collected by the Centers for Disease Control and Prevention, and nonmedical OxyContin use was measured using self-reported data from the National Survey on Drug Use and Health, which is the largest U.S. survey on substance use disorder.
The two groups of states had similar demographic and economic conditions, except that the above-median misuse states had smaller populations and a larger proportion of white residents.
Of note, the patterns of HCV infection mirrored those of heroin overdoses. There was small relative increase in HCV infection rates in 2010 in the above-median OxyContin misuse states, and the gap between above- and below-median misuse states widened more rapidly from 2011 to 2013. “This striking inflection point in the trend of hepatitis C infections for high-misuse states after 2010 mimics the inflection in heroin overdoses that occurred as a result of the reformulation,” they said, noting that heroin morality per 100,000 population was nearly identical in the two groups of states in the pre-reformulation period (0.859 and 0.847).
The falsification exercise looking at nonmedical use of pain relievers other than OxyContin in the two groups of states showed that after 2010 groups’ rates of hepatitis C infections grew at virtually identical rates.
“Thus, the differential risk in hepatitis C infections was uniquely associated with OxyContin misuse, rather than prescription pain reliever misuse more generally,” they said. “This suggests that it was the OxyContin reformulation, not other policies broadly affecting opioids, that drove much of the differential growth.”
The investigators controlled for numerous other factors, including opioid policies that might have an impact on OxyContin and heroin use, prescription drug monitoring programs and pain clinic regulations, as well as the role of major pill-mill crackdowns in 2010 and 2011.
The findings represent a “substantial public health concern,” they said, explaining that, while “considerable policy attention is being given to managing the opioid epidemic ... a ‘silent epidemic’ of hepatitis C has emerged as a result of a transition in the mode of administration toward injection drug use.”
In 2017, the CDC reported on this link between the opioid epidemic and rising HCV infection rates, as well.
Dr. Powell and his colleagues wrote.
Their findings regarding the unintended consequences of the OxyContin reformulation suggest that caution is warranted with respect to future interventions that limit the supply of abusable prescription opioids, they said, adding that “such interventions must be paired with polices that alleviate the harms associated with switching to illicit drugs, such as improved access to substance use disorder treatment and increased efforts aimed at identifying and treating diseases associated with injection drug use.”
However, policy makers and medical professionals also must recognize that reducing opioid-related mortality and increasing access to drug treatment might not be sufficient to fully address all of the public health consequences associated with the opioid crisis. As additional reformulations of opioids are promoted and more policies seek to limit access to prescription opioids, “both the medical and the law enforcement communities must recognize the critical transition from prescription opioids to other drugs, particularly those that are injected, and be prepared to consider complementary strategies that can effectively reduce the additional harms from the particular mode of drug use,” they concluded.
The coauthors cited several limitations, including the possibility that true hepatitis C infection rates might have been underestimated in the study.
He and Dr. Pacula received funding from the National Institute on Drug Abuse. Dr. Powell also cited funding from the Rand Alumni Impact Award.
SOURCE: Powell D et al. Health Aff. 2019;38(2):287-94.
FROM HEALTH AFFAIRS
Key clinical point: Physicians and others must be “prepared to consider complementary strategies that can effectively reduce the additional harms from the particular mode of drug use.”
Major finding: HCV rates increased 222% in states that had above-median OxyContin misuse rates, compared with an increase of 75% in states with below-median misuse.
Study details: A review of data from 2004 to 2015.
Disclosures: Dr. Powell and Dr. Pacula received funding from the National Institute on Drug Abuse. Dr. Powell also cited funding from the Rand Alumni Impact Award.
Source: Powell D et al. Health Aff. 2019;38(2):287-94.
Lifetime cost of tobacco use tops $1.9 million per smoker
according to the personal financial website WalletHub.
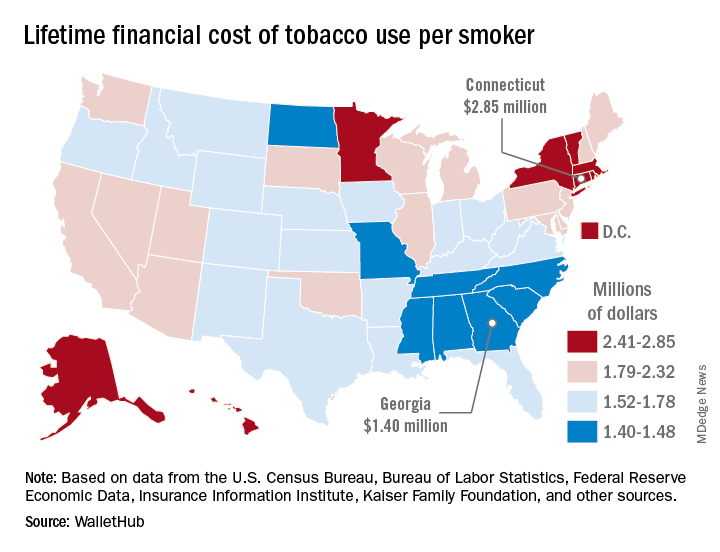
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
according to the personal financial website WalletHub.
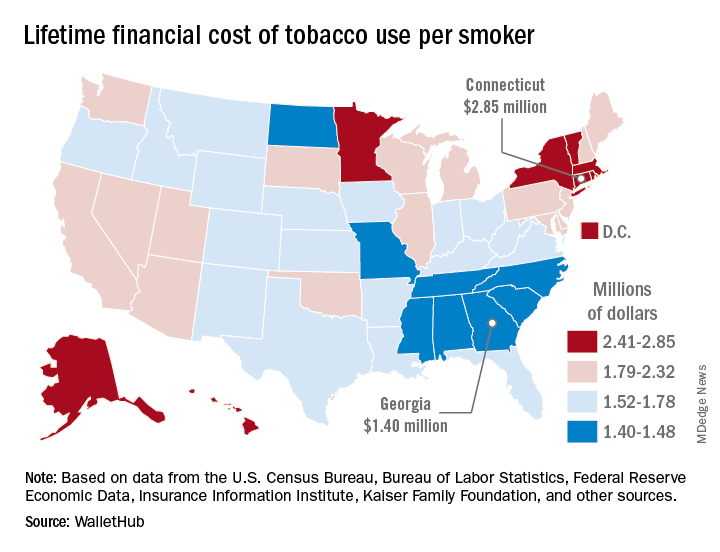
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
according to the personal financial website WalletHub.
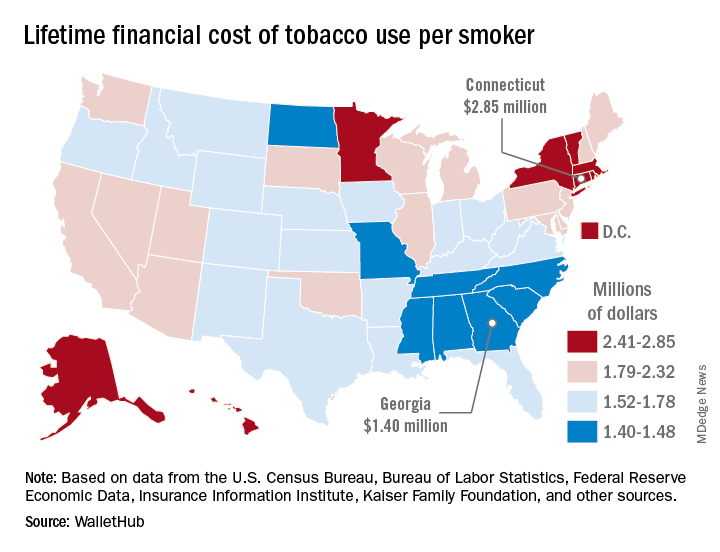
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
Residential HCV program improves veterans’ diagnosis and care
Integrating comprehensive and collaborative hepatitis C virus (HCV) care within a Veterans Affairs residential treatment program can substantially increase diagnosis and treatment of HCV-infected veterans with substance use disorder (SUD), according to the results of an evaluation study for the period from December 2014 to April 2018.
A total of 97.5% (582/597) of patient admissions to the program were screened for HCV infection, and 12.7% (74/582) of the cases were confirmed to be HCV positive. All of the positive cases were sent to an infectious disease (ID) clinic for further evaluation and, if appropriate, to begin HCV pharmacotherapy, according to the report, published in the Journal of Substance Abuse Treatment.
Of the HCV-positive cases, 78.4% (58/74) received pharmacotherapy, with a sustained virologic response rate of 82.8% (48/58), wrote Mary Jane Burton, MD, of the G.V. (Sonny) Montgomery VA Medical Center, Jackson, Miss., and her colleagues.
As part of the program, all veterans admitted to the SUD residential program were offered screening for HCV. Veterans with negative screening results received education about how to remain HCV negative via handouts and veterans who screened positive received brief supportive counseling and were referred to the ID clinic via a consult. Veterans confirmed to have chronic HCV infection receive education and evaluation in the HCV clinic while they attend the residential SUD program. Treatment for HCV is instituted as early as feasible and prescribing is in accordance with VA guidelines (Department of Veterans Affairs, 2018), with the goal of initiating pharmacotherapy treatment for HCV while the veteran is still in the residential program, according to the researchers.
Following discharge from the program, veterans on HCV treatment are scheduled for follow-up every 2 weeks in the HCV treatment clinic for the remainder of their pharmacotherapy, the researchers added.
Patient-level barriers to HCV treatment among the SUD population include reduced health literacy, low health care utilization, comorbid mental health conditions, and poor social support, according to the literature. Because multidisciplinary approaches to HCV treatment that mitigate these barriers have been shown to increase treatment uptake among these patients, the VA program was initiated, the researchers stated. Dr. Burton and her colleagues reported that 18.9% (14/74) of the HCV-positive cases were newly diagnosed and would have likely gone undetected without this program (J Substance Abuse Treatment. 2019;98:9-14).
“We have demonstrated that integrating a comprehensive HCV screening, education, referral, and treatment program within residential SUD treatment is feasible and effective in diagnosing previously unrecognized HCV infections, transitioning veterans into HCV care, and promoting treatment initiation,” the researchers concluded.
The Department of Veterans Affairs and the VA Center for Innovation supported the study. Dr. Burton reported research support from Merck Sharpe & Dohme.
Integrating comprehensive and collaborative hepatitis C virus (HCV) care within a Veterans Affairs residential treatment program can substantially increase diagnosis and treatment of HCV-infected veterans with substance use disorder (SUD), according to the results of an evaluation study for the period from December 2014 to April 2018.
A total of 97.5% (582/597) of patient admissions to the program were screened for HCV infection, and 12.7% (74/582) of the cases were confirmed to be HCV positive. All of the positive cases were sent to an infectious disease (ID) clinic for further evaluation and, if appropriate, to begin HCV pharmacotherapy, according to the report, published in the Journal of Substance Abuse Treatment.
Of the HCV-positive cases, 78.4% (58/74) received pharmacotherapy, with a sustained virologic response rate of 82.8% (48/58), wrote Mary Jane Burton, MD, of the G.V. (Sonny) Montgomery VA Medical Center, Jackson, Miss., and her colleagues.
As part of the program, all veterans admitted to the SUD residential program were offered screening for HCV. Veterans with negative screening results received education about how to remain HCV negative via handouts and veterans who screened positive received brief supportive counseling and were referred to the ID clinic via a consult. Veterans confirmed to have chronic HCV infection receive education and evaluation in the HCV clinic while they attend the residential SUD program. Treatment for HCV is instituted as early as feasible and prescribing is in accordance with VA guidelines (Department of Veterans Affairs, 2018), with the goal of initiating pharmacotherapy treatment for HCV while the veteran is still in the residential program, according to the researchers.
Following discharge from the program, veterans on HCV treatment are scheduled for follow-up every 2 weeks in the HCV treatment clinic for the remainder of their pharmacotherapy, the researchers added.
Patient-level barriers to HCV treatment among the SUD population include reduced health literacy, low health care utilization, comorbid mental health conditions, and poor social support, according to the literature. Because multidisciplinary approaches to HCV treatment that mitigate these barriers have been shown to increase treatment uptake among these patients, the VA program was initiated, the researchers stated. Dr. Burton and her colleagues reported that 18.9% (14/74) of the HCV-positive cases were newly diagnosed and would have likely gone undetected without this program (J Substance Abuse Treatment. 2019;98:9-14).
“We have demonstrated that integrating a comprehensive HCV screening, education, referral, and treatment program within residential SUD treatment is feasible and effective in diagnosing previously unrecognized HCV infections, transitioning veterans into HCV care, and promoting treatment initiation,” the researchers concluded.
The Department of Veterans Affairs and the VA Center for Innovation supported the study. Dr. Burton reported research support from Merck Sharpe & Dohme.
Integrating comprehensive and collaborative hepatitis C virus (HCV) care within a Veterans Affairs residential treatment program can substantially increase diagnosis and treatment of HCV-infected veterans with substance use disorder (SUD), according to the results of an evaluation study for the period from December 2014 to April 2018.
A total of 97.5% (582/597) of patient admissions to the program were screened for HCV infection, and 12.7% (74/582) of the cases were confirmed to be HCV positive. All of the positive cases were sent to an infectious disease (ID) clinic for further evaluation and, if appropriate, to begin HCV pharmacotherapy, according to the report, published in the Journal of Substance Abuse Treatment.
Of the HCV-positive cases, 78.4% (58/74) received pharmacotherapy, with a sustained virologic response rate of 82.8% (48/58), wrote Mary Jane Burton, MD, of the G.V. (Sonny) Montgomery VA Medical Center, Jackson, Miss., and her colleagues.
As part of the program, all veterans admitted to the SUD residential program were offered screening for HCV. Veterans with negative screening results received education about how to remain HCV negative via handouts and veterans who screened positive received brief supportive counseling and were referred to the ID clinic via a consult. Veterans confirmed to have chronic HCV infection receive education and evaluation in the HCV clinic while they attend the residential SUD program. Treatment for HCV is instituted as early as feasible and prescribing is in accordance with VA guidelines (Department of Veterans Affairs, 2018), with the goal of initiating pharmacotherapy treatment for HCV while the veteran is still in the residential program, according to the researchers.
Following discharge from the program, veterans on HCV treatment are scheduled for follow-up every 2 weeks in the HCV treatment clinic for the remainder of their pharmacotherapy, the researchers added.
Patient-level barriers to HCV treatment among the SUD population include reduced health literacy, low health care utilization, comorbid mental health conditions, and poor social support, according to the literature. Because multidisciplinary approaches to HCV treatment that mitigate these barriers have been shown to increase treatment uptake among these patients, the VA program was initiated, the researchers stated. Dr. Burton and her colleagues reported that 18.9% (14/74) of the HCV-positive cases were newly diagnosed and would have likely gone undetected without this program (J Substance Abuse Treatment. 2019;98:9-14).
“We have demonstrated that integrating a comprehensive HCV screening, education, referral, and treatment program within residential SUD treatment is feasible and effective in diagnosing previously unrecognized HCV infections, transitioning veterans into HCV care, and promoting treatment initiation,” the researchers concluded.
The Department of Veterans Affairs and the VA Center for Innovation supported the study. Dr. Burton reported research support from Merck Sharpe & Dohme.
FROM THE JOURNAL OF SUBSTANCE ABUSE TREATMENT











