User login
The body of evidence for Paxlovid therapy
Dear Colleagues,
We have a mismatch. The evidence supporting treatment for Paxlovid is compelling for people aged 60 or over, but the older patients in the United States are much less likely to be treated. Not only was there a randomized, placebo-controlled trial of high-risk patients which showed 89% reduction of hospitalizations and deaths (median age, 45), but there have been multiple real-world effectiveness studies subsequently published that have partitioned the benefit for age 65 or older, such as the ones from Israel and Hong Kong (age 60+). Overall, the real-world effectiveness in the first month after treatment is at least as good, if not better, than in the high-risk randomized trial.
We’re doing the current survey to find out, but the most likely reasons include (1) lack of confidence of benefit; (2) medication interactions; and (3) concerns over rebound.
Let me address each of these briefly. The lack of confidence in benefit stems from the fact that the initial high-risk trial was in unvaccinated individuals. That concern can now be put aside because all of the several real-world studies confirming the protective benefit against hospitalizations and deaths are in people who have been vaccinated, and a significant proportion received booster shots.
The potential medication interactions due to the ritonavir component of the Paxlovid drug combination, attributable to its cytochrome P450 3A4 inhibition, have been unduly emphasized. There are many drug-interaction checkers for Paxlovid, but this one from the University of Liverpool is user friendly, color- and icon-coded, and shows that the vast majority of interactions can be sidestepped by discontinuing the medication of concern for the length of the Paxlovid treatment, 5 days. The simple chart is provided in my recent substack newsletter.
As far as rebound, this problem has unfortunately been exaggerated because of lack of prospective systematic studies and appreciation that a positive test of clinical symptom rebound can occur without Paxlovid. There are soon to be multiple reports that the incidence of Paxlovid rebound is fairly low, in the range of 10%. That concern should not be a reason to withhold treatment.
Now the plot thickens. A new preprint report from the Veterans Health Administration, the largest health care system in the United States, looks at 90-day outcomes of about 9,000 Paxlovid-treated patients and approximately 47,000 controls. Not only was there a 26% reduction in long COVID, but of the breakdown of 12 organs/systems and symptoms, 10 of 12 were significantly reduced with Paxlovid, including pulmonary embolism, deep vein thrombosis, and neurocognitive impairment. There was also a 48% reduction in death and a 30% reduction in hospitalizations after the first 30 days. I have reviewed all of these data and put them in context in a recent newsletter. A key point is that the magnitude of benefit was unaffected by vaccination or booster status, or prior COVID infections, or unvaccinated status. Also, it was the same for men and women, as well as for age > 70 and age < 60. These findings all emphasize a new reason to be using Paxlovid therapy, and if replicated, Paxlovid may even be indicated for younger patients (who are at low risk for hospitalizations and deaths but at increased risk for long COVID).
In summary, for older patients, we should be thinking of why we should be using Paxlovid rather than the reason not to treat. We’ll be interested in the survey results to understand the mismatch better, and we look forward to your ideas and feedback to make better use of this treatment for the people who need it the most.
Sincerely yours, Eric J. Topol, MD
Dr. Topol reports no conflicts of interest with Pfizer; he receives no honoraria or speaker fees, does not serve in an advisory role, and has no financial association with the company.
A version of this article first appeared on Medscape.com.
Dear Colleagues,
We have a mismatch. The evidence supporting treatment for Paxlovid is compelling for people aged 60 or over, but the older patients in the United States are much less likely to be treated. Not only was there a randomized, placebo-controlled trial of high-risk patients which showed 89% reduction of hospitalizations and deaths (median age, 45), but there have been multiple real-world effectiveness studies subsequently published that have partitioned the benefit for age 65 or older, such as the ones from Israel and Hong Kong (age 60+). Overall, the real-world effectiveness in the first month after treatment is at least as good, if not better, than in the high-risk randomized trial.
We’re doing the current survey to find out, but the most likely reasons include (1) lack of confidence of benefit; (2) medication interactions; and (3) concerns over rebound.
Let me address each of these briefly. The lack of confidence in benefit stems from the fact that the initial high-risk trial was in unvaccinated individuals. That concern can now be put aside because all of the several real-world studies confirming the protective benefit against hospitalizations and deaths are in people who have been vaccinated, and a significant proportion received booster shots.
The potential medication interactions due to the ritonavir component of the Paxlovid drug combination, attributable to its cytochrome P450 3A4 inhibition, have been unduly emphasized. There are many drug-interaction checkers for Paxlovid, but this one from the University of Liverpool is user friendly, color- and icon-coded, and shows that the vast majority of interactions can be sidestepped by discontinuing the medication of concern for the length of the Paxlovid treatment, 5 days. The simple chart is provided in my recent substack newsletter.
As far as rebound, this problem has unfortunately been exaggerated because of lack of prospective systematic studies and appreciation that a positive test of clinical symptom rebound can occur without Paxlovid. There are soon to be multiple reports that the incidence of Paxlovid rebound is fairly low, in the range of 10%. That concern should not be a reason to withhold treatment.
Now the plot thickens. A new preprint report from the Veterans Health Administration, the largest health care system in the United States, looks at 90-day outcomes of about 9,000 Paxlovid-treated patients and approximately 47,000 controls. Not only was there a 26% reduction in long COVID, but of the breakdown of 12 organs/systems and symptoms, 10 of 12 were significantly reduced with Paxlovid, including pulmonary embolism, deep vein thrombosis, and neurocognitive impairment. There was also a 48% reduction in death and a 30% reduction in hospitalizations after the first 30 days. I have reviewed all of these data and put them in context in a recent newsletter. A key point is that the magnitude of benefit was unaffected by vaccination or booster status, or prior COVID infections, or unvaccinated status. Also, it was the same for men and women, as well as for age > 70 and age < 60. These findings all emphasize a new reason to be using Paxlovid therapy, and if replicated, Paxlovid may even be indicated for younger patients (who are at low risk for hospitalizations and deaths but at increased risk for long COVID).
In summary, for older patients, we should be thinking of why we should be using Paxlovid rather than the reason not to treat. We’ll be interested in the survey results to understand the mismatch better, and we look forward to your ideas and feedback to make better use of this treatment for the people who need it the most.
Sincerely yours, Eric J. Topol, MD
Dr. Topol reports no conflicts of interest with Pfizer; he receives no honoraria or speaker fees, does not serve in an advisory role, and has no financial association with the company.
A version of this article first appeared on Medscape.com.
Dear Colleagues,
We have a mismatch. The evidence supporting treatment for Paxlovid is compelling for people aged 60 or over, but the older patients in the United States are much less likely to be treated. Not only was there a randomized, placebo-controlled trial of high-risk patients which showed 89% reduction of hospitalizations and deaths (median age, 45), but there have been multiple real-world effectiveness studies subsequently published that have partitioned the benefit for age 65 or older, such as the ones from Israel and Hong Kong (age 60+). Overall, the real-world effectiveness in the first month after treatment is at least as good, if not better, than in the high-risk randomized trial.
We’re doing the current survey to find out, but the most likely reasons include (1) lack of confidence of benefit; (2) medication interactions; and (3) concerns over rebound.
Let me address each of these briefly. The lack of confidence in benefit stems from the fact that the initial high-risk trial was in unvaccinated individuals. That concern can now be put aside because all of the several real-world studies confirming the protective benefit against hospitalizations and deaths are in people who have been vaccinated, and a significant proportion received booster shots.
The potential medication interactions due to the ritonavir component of the Paxlovid drug combination, attributable to its cytochrome P450 3A4 inhibition, have been unduly emphasized. There are many drug-interaction checkers for Paxlovid, but this one from the University of Liverpool is user friendly, color- and icon-coded, and shows that the vast majority of interactions can be sidestepped by discontinuing the medication of concern for the length of the Paxlovid treatment, 5 days. The simple chart is provided in my recent substack newsletter.
As far as rebound, this problem has unfortunately been exaggerated because of lack of prospective systematic studies and appreciation that a positive test of clinical symptom rebound can occur without Paxlovid. There are soon to be multiple reports that the incidence of Paxlovid rebound is fairly low, in the range of 10%. That concern should not be a reason to withhold treatment.
Now the plot thickens. A new preprint report from the Veterans Health Administration, the largest health care system in the United States, looks at 90-day outcomes of about 9,000 Paxlovid-treated patients and approximately 47,000 controls. Not only was there a 26% reduction in long COVID, but of the breakdown of 12 organs/systems and symptoms, 10 of 12 were significantly reduced with Paxlovid, including pulmonary embolism, deep vein thrombosis, and neurocognitive impairment. There was also a 48% reduction in death and a 30% reduction in hospitalizations after the first 30 days. I have reviewed all of these data and put them in context in a recent newsletter. A key point is that the magnitude of benefit was unaffected by vaccination or booster status, or prior COVID infections, or unvaccinated status. Also, it was the same for men and women, as well as for age > 70 and age < 60. These findings all emphasize a new reason to be using Paxlovid therapy, and if replicated, Paxlovid may even be indicated for younger patients (who are at low risk for hospitalizations and deaths but at increased risk for long COVID).
In summary, for older patients, we should be thinking of why we should be using Paxlovid rather than the reason not to treat. We’ll be interested in the survey results to understand the mismatch better, and we look forward to your ideas and feedback to make better use of this treatment for the people who need it the most.
Sincerely yours, Eric J. Topol, MD
Dr. Topol reports no conflicts of interest with Pfizer; he receives no honoraria or speaker fees, does not serve in an advisory role, and has no financial association with the company.
A version of this article first appeared on Medscape.com.
Use 2022’s advocacy successes and frustrations as a catalyst for the new year
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
A new ultrabrief screening scale for pediatric OCD
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.
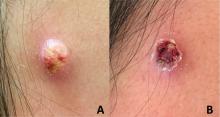
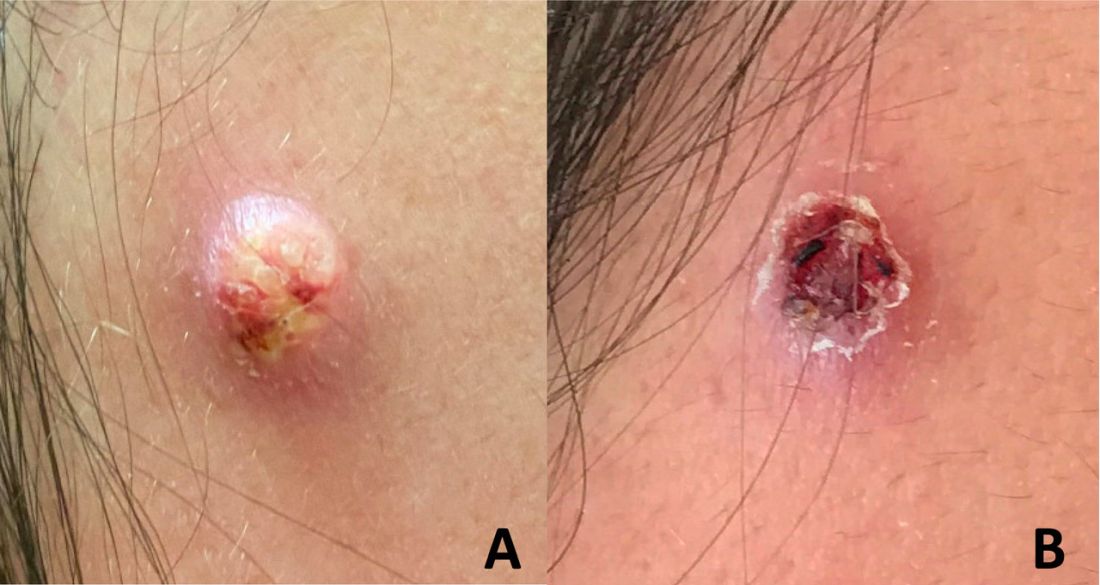
An adolescent male presents with an eroded bump on the temple
The correct answer is (D), molluscum contagiosum. Upon surgical excision, the pathology indicated the lesion was consistent with molluscum contagiosum.
Molluscum contagiosum is a benign skin disorder caused by a pox virus and is frequently seen in children. This disease is transmitted primarily through direct skin contact with an infected individual.1 Contaminated fomites have been suggested as another source of infection.2 The typical lesion appears dome-shaped, round, and pinkish-purple in color.1 The incubation period ranges from 2 weeks to 6 months and is typically self-limited in immunocompetent hosts; however, in immunocompromised persons, molluscum contagiosum lesions may present atypically such that they are larger in size and/or resemble malignancies, such as basal cell carcinoma or keratoacanthoma (for single lesions), or other infectious diseases, such as cryptococcosis and histoplasmosis (for more numerous lesions).3,4 A giant atypical molluscum contagiosum is rarely seen in healthy individuals.
What’s on the differential?
The recent episode of bleeding raises concern for other neoplastic processes of the skin including squamous cell carcinoma or basal cell carcinoma as well as cutaneous metastatic rhabdoid tumor, given the patient’s history.
Eruptive keratoacanthomas are also reported in patients taking nivolumab, an anti-PD-1 immunotherapy, which the patient has received for treatment of his recurrent metastatic rhabdoid tumor.5 More common entities such as a pyogenic granuloma or verruca are also included on the differential. The initial presentation of the lesion, however, is more consistent with the pearly umbilicated papules associated with molluscum contagiosum.
Comments from Dr. Eichenfield
This is a very hard diagnosis to make with the clinical findings and history.
Molluscum contagiosum infections are common, but with this patient’s medical history, biopsy and excision with pathologic examination was an appropriate approach to make a certain diagnosis.
Ms. Moyal is a research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego.
References
1. Brown J et al. Int J Dermatol. 2006 Feb;45(2):93-9.
2. Hanson D and Diven DG. Dermatol Online J. 2003 Mar;9(2).
3. Badri T and Gandhi GR. Molluscum contagiosum. 2022. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing.
4. Schwartz JJ and Myskowski PL. J Am Acad Dermatol. 1992 Oct 1;27(4):583-8.
5. Antonov NK et al. JAAD Case Rep. 2019 Apr 5;5(4):342-5.
The correct answer is (D), molluscum contagiosum. Upon surgical excision, the pathology indicated the lesion was consistent with molluscum contagiosum.
Molluscum contagiosum is a benign skin disorder caused by a pox virus and is frequently seen in children. This disease is transmitted primarily through direct skin contact with an infected individual.1 Contaminated fomites have been suggested as another source of infection.2 The typical lesion appears dome-shaped, round, and pinkish-purple in color.1 The incubation period ranges from 2 weeks to 6 months and is typically self-limited in immunocompetent hosts; however, in immunocompromised persons, molluscum contagiosum lesions may present atypically such that they are larger in size and/or resemble malignancies, such as basal cell carcinoma or keratoacanthoma (for single lesions), or other infectious diseases, such as cryptococcosis and histoplasmosis (for more numerous lesions).3,4 A giant atypical molluscum contagiosum is rarely seen in healthy individuals.
What’s on the differential?
The recent episode of bleeding raises concern for other neoplastic processes of the skin including squamous cell carcinoma or basal cell carcinoma as well as cutaneous metastatic rhabdoid tumor, given the patient’s history.
Eruptive keratoacanthomas are also reported in patients taking nivolumab, an anti-PD-1 immunotherapy, which the patient has received for treatment of his recurrent metastatic rhabdoid tumor.5 More common entities such as a pyogenic granuloma or verruca are also included on the differential. The initial presentation of the lesion, however, is more consistent with the pearly umbilicated papules associated with molluscum contagiosum.
Comments from Dr. Eichenfield
This is a very hard diagnosis to make with the clinical findings and history.
Molluscum contagiosum infections are common, but with this patient’s medical history, biopsy and excision with pathologic examination was an appropriate approach to make a certain diagnosis.
Ms. Moyal is a research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego.
References
1. Brown J et al. Int J Dermatol. 2006 Feb;45(2):93-9.
2. Hanson D and Diven DG. Dermatol Online J. 2003 Mar;9(2).
3. Badri T and Gandhi GR. Molluscum contagiosum. 2022. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing.
4. Schwartz JJ and Myskowski PL. J Am Acad Dermatol. 1992 Oct 1;27(4):583-8.
5. Antonov NK et al. JAAD Case Rep. 2019 Apr 5;5(4):342-5.
The correct answer is (D), molluscum contagiosum. Upon surgical excision, the pathology indicated the lesion was consistent with molluscum contagiosum.
Molluscum contagiosum is a benign skin disorder caused by a pox virus and is frequently seen in children. This disease is transmitted primarily through direct skin contact with an infected individual.1 Contaminated fomites have been suggested as another source of infection.2 The typical lesion appears dome-shaped, round, and pinkish-purple in color.1 The incubation period ranges from 2 weeks to 6 months and is typically self-limited in immunocompetent hosts; however, in immunocompromised persons, molluscum contagiosum lesions may present atypically such that they are larger in size and/or resemble malignancies, such as basal cell carcinoma or keratoacanthoma (for single lesions), or other infectious diseases, such as cryptococcosis and histoplasmosis (for more numerous lesions).3,4 A giant atypical molluscum contagiosum is rarely seen in healthy individuals.
What’s on the differential?
The recent episode of bleeding raises concern for other neoplastic processes of the skin including squamous cell carcinoma or basal cell carcinoma as well as cutaneous metastatic rhabdoid tumor, given the patient’s history.
Eruptive keratoacanthomas are also reported in patients taking nivolumab, an anti-PD-1 immunotherapy, which the patient has received for treatment of his recurrent metastatic rhabdoid tumor.5 More common entities such as a pyogenic granuloma or verruca are also included on the differential. The initial presentation of the lesion, however, is more consistent with the pearly umbilicated papules associated with molluscum contagiosum.
Comments from Dr. Eichenfield
This is a very hard diagnosis to make with the clinical findings and history.
Molluscum contagiosum infections are common, but with this patient’s medical history, biopsy and excision with pathologic examination was an appropriate approach to make a certain diagnosis.
Ms. Moyal is a research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital, San Diego. Dr. Eichenfield is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego, and Rady Children’s Hospital, San Diego.
References
1. Brown J et al. Int J Dermatol. 2006 Feb;45(2):93-9.
2. Hanson D and Diven DG. Dermatol Online J. 2003 Mar;9(2).
3. Badri T and Gandhi GR. Molluscum contagiosum. 2022. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing.
4. Schwartz JJ and Myskowski PL. J Am Acad Dermatol. 1992 Oct 1;27(4):583-8.
5. Antonov NK et al. JAAD Case Rep. 2019 Apr 5;5(4):342-5.
Will Congress step up to save primary care?
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
More children should be getting flu vaccines
Cold and flu season came early in 2022.
On Nov. 4, 2022, the Centers for Disease Control and Prevention issued a Health Alert Network Health Advisory about early, elevated respiratory disease incidence caused by multiple viruses other than SARS-CoV-2.
Interseasonal spread of respiratory syncytial virus has continued in 2022, with RSV-associated hospitalizations increasing in the late spring and continuing throughout the summer and into the fall. In October, some regions of the country were seeing RSV activity near the peak seasonal levels typically observed in December and January.
Cases of severe respiratory infection in children who tested positive for rhinovirus or enterovirus spiked in August; further testing confirmed the presence of EV-D68 in some children. Rhinovirus and enterovirus continue to circulate and are isolated in hospitalized children with respiratory illness.
In some parts of the country, influenza cases have rapidly increased ahead of what we normally anticipate. According to preliminary estimates from the CDC, between Oct. 1 and Oct. 22, 880,000 people were sickened with flu, 420,000 people visited a health care provider for flu illness, and 6,900 people were hospitalized for flu. The cumulative hospitalization rate is higher than observed at this time of year in every previous flu season since 2010-2011. Hospitalization rates are highest in children aged 0-4 years and adults 65 years and older.
Of course, this report came as no surprise to pediatric health care providers. Many children’s hospitals had been operating at or over capacity for weeks. While a systematic assessment of the surge on children’s hospitals has not been published, anecdotally, hospitals from around the country have described record emergency department visits and inpatient census numbers. Some have set up tents or other temporary facilities to see ambulatory patients and have canceled elective surgeries because of a lack of beds.
There is no quick or easy solution to stem the tide of RSV-related or enterovirus/rhinovirus admissions, but many flu-related hospitalizations are vaccine preventable. Unfortunately, too few children are receiving influenza vaccine. As of the week ending Oct. 15, only about 22.1% of eligible children had been immunized. The American Academy of Pediatrics and the CDC recommend that all children are vaccinated, preferably by the end of October so they have time to develop immunity before influenza starts circulating. As it stands now, the majority of the nation’s children are facing a flu season without the benefits of vaccine.
There is still time to take steps to prevent this flu season from becoming one of the worst in recent memory. A strong provider recommendation for influenza vaccine is consistently associated with higher rates of vaccine acceptance. We need to recommend influenza vaccine to all eligible patients at every visit and in every setting. It will help if we can say it like we mean it. Some of us are tired of debating the merits of COVID-19 vaccine with families and may be leery of additional debates about flu. Some of us may just be tired, as many practices have already expanded office hours to care for the influx of kids with respiratory illness. On the heels of two atypical flu seasons, a few of us may be quietly complacent about the importance of flu vaccines for children.
Anyone in need of a little motivation should check out a paper recently published in Clinical Infectious Diseases that reinforces the value of flu vaccine, even in a year when there is a poor match between the vaccine and circulating viruses.
The 2019-2020 flu season was a bad flu season for children. Two antigenically drifted influenza viruses predominated and cases of influenza soared, resulting in the largest influenza epidemic in children in the United States since 1992. Pediatric Intensive Care Influenza Study investigators used a test-negative design to estimate the effectiveness of influenza vaccine in preventing critical and life-threatening influenza in children during that season. The good news: vaccination reduced the risk of critical influenza by 78% against H1N1pdm09 viruses that were well-matched to vaccine and by 47% against mismatched viruses. Vaccination was estimated to be 75% protective against antigenically drifted B-Victoria viruses. Overall vaccine effectiveness against critical illness from any influenza virus was 63% (95% confidence interval, 38%-78%).
While it might be tempting to attribute suboptimal immunization rates to vaccine hesitancy, ready availability remains an issue for some families. We need to eliminate barriers to access. While the AAP continues to emphasize immunization in the medical home, especially for the youngest infants, the 2022 policy statement suggests that vaccinating children in schools, pharmacies, and other nontraditional settings could improve immunization rates. To the extent feasible, we need to work with partners to support community-based initiatives and promote these to families who struggle to make it into the office.
Improving access is just one potential way to reduce health disparities related to influenza and influenza vaccination. Over 10 influenza seasons, higher rates of influenza-associated hospitalizations and intensive care unit admissions were observed in Black, Hispanic, and American Indian/Alaska Native people. These disparities were highest in children aged younger than 4 years and influenza-associated in-hospital deaths were three- to fourfold higher in Black, Hispanic, and Asian/Pacific Islander children, compared with White children. The reason for the disparities isn’t completely clear but increasing immunization rates may be part of the solution. During the 2020-2021 influenza season, flu immunization rates in Black children (51.6%) were lower than those seen in White (57.4%) and Hispanic children (58.9%).
The AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023, highlight a variety of evidence-based strategies to increase influenza immunization rates. These may provide a little inspiration for clinicians looking to try a new approach. If you wish to share your experience with increasing influenza immunization rates in your practice setting, please email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead.
Cold and flu season came early in 2022.
On Nov. 4, 2022, the Centers for Disease Control and Prevention issued a Health Alert Network Health Advisory about early, elevated respiratory disease incidence caused by multiple viruses other than SARS-CoV-2.
Interseasonal spread of respiratory syncytial virus has continued in 2022, with RSV-associated hospitalizations increasing in the late spring and continuing throughout the summer and into the fall. In October, some regions of the country were seeing RSV activity near the peak seasonal levels typically observed in December and January.
Cases of severe respiratory infection in children who tested positive for rhinovirus or enterovirus spiked in August; further testing confirmed the presence of EV-D68 in some children. Rhinovirus and enterovirus continue to circulate and are isolated in hospitalized children with respiratory illness.
In some parts of the country, influenza cases have rapidly increased ahead of what we normally anticipate. According to preliminary estimates from the CDC, between Oct. 1 and Oct. 22, 880,000 people were sickened with flu, 420,000 people visited a health care provider for flu illness, and 6,900 people were hospitalized for flu. The cumulative hospitalization rate is higher than observed at this time of year in every previous flu season since 2010-2011. Hospitalization rates are highest in children aged 0-4 years and adults 65 years and older.
Of course, this report came as no surprise to pediatric health care providers. Many children’s hospitals had been operating at or over capacity for weeks. While a systematic assessment of the surge on children’s hospitals has not been published, anecdotally, hospitals from around the country have described record emergency department visits and inpatient census numbers. Some have set up tents or other temporary facilities to see ambulatory patients and have canceled elective surgeries because of a lack of beds.
There is no quick or easy solution to stem the tide of RSV-related or enterovirus/rhinovirus admissions, but many flu-related hospitalizations are vaccine preventable. Unfortunately, too few children are receiving influenza vaccine. As of the week ending Oct. 15, only about 22.1% of eligible children had been immunized. The American Academy of Pediatrics and the CDC recommend that all children are vaccinated, preferably by the end of October so they have time to develop immunity before influenza starts circulating. As it stands now, the majority of the nation’s children are facing a flu season without the benefits of vaccine.
There is still time to take steps to prevent this flu season from becoming one of the worst in recent memory. A strong provider recommendation for influenza vaccine is consistently associated with higher rates of vaccine acceptance. We need to recommend influenza vaccine to all eligible patients at every visit and in every setting. It will help if we can say it like we mean it. Some of us are tired of debating the merits of COVID-19 vaccine with families and may be leery of additional debates about flu. Some of us may just be tired, as many practices have already expanded office hours to care for the influx of kids with respiratory illness. On the heels of two atypical flu seasons, a few of us may be quietly complacent about the importance of flu vaccines for children.
Anyone in need of a little motivation should check out a paper recently published in Clinical Infectious Diseases that reinforces the value of flu vaccine, even in a year when there is a poor match between the vaccine and circulating viruses.
The 2019-2020 flu season was a bad flu season for children. Two antigenically drifted influenza viruses predominated and cases of influenza soared, resulting in the largest influenza epidemic in children in the United States since 1992. Pediatric Intensive Care Influenza Study investigators used a test-negative design to estimate the effectiveness of influenza vaccine in preventing critical and life-threatening influenza in children during that season. The good news: vaccination reduced the risk of critical influenza by 78% against H1N1pdm09 viruses that were well-matched to vaccine and by 47% against mismatched viruses. Vaccination was estimated to be 75% protective against antigenically drifted B-Victoria viruses. Overall vaccine effectiveness against critical illness from any influenza virus was 63% (95% confidence interval, 38%-78%).
While it might be tempting to attribute suboptimal immunization rates to vaccine hesitancy, ready availability remains an issue for some families. We need to eliminate barriers to access. While the AAP continues to emphasize immunization in the medical home, especially for the youngest infants, the 2022 policy statement suggests that vaccinating children in schools, pharmacies, and other nontraditional settings could improve immunization rates. To the extent feasible, we need to work with partners to support community-based initiatives and promote these to families who struggle to make it into the office.
Improving access is just one potential way to reduce health disparities related to influenza and influenza vaccination. Over 10 influenza seasons, higher rates of influenza-associated hospitalizations and intensive care unit admissions were observed in Black, Hispanic, and American Indian/Alaska Native people. These disparities were highest in children aged younger than 4 years and influenza-associated in-hospital deaths were three- to fourfold higher in Black, Hispanic, and Asian/Pacific Islander children, compared with White children. The reason for the disparities isn’t completely clear but increasing immunization rates may be part of the solution. During the 2020-2021 influenza season, flu immunization rates in Black children (51.6%) were lower than those seen in White (57.4%) and Hispanic children (58.9%).
The AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023, highlight a variety of evidence-based strategies to increase influenza immunization rates. These may provide a little inspiration for clinicians looking to try a new approach. If you wish to share your experience with increasing influenza immunization rates in your practice setting, please email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead.
Cold and flu season came early in 2022.
On Nov. 4, 2022, the Centers for Disease Control and Prevention issued a Health Alert Network Health Advisory about early, elevated respiratory disease incidence caused by multiple viruses other than SARS-CoV-2.
Interseasonal spread of respiratory syncytial virus has continued in 2022, with RSV-associated hospitalizations increasing in the late spring and continuing throughout the summer and into the fall. In October, some regions of the country were seeing RSV activity near the peak seasonal levels typically observed in December and January.
Cases of severe respiratory infection in children who tested positive for rhinovirus or enterovirus spiked in August; further testing confirmed the presence of EV-D68 in some children. Rhinovirus and enterovirus continue to circulate and are isolated in hospitalized children with respiratory illness.
In some parts of the country, influenza cases have rapidly increased ahead of what we normally anticipate. According to preliminary estimates from the CDC, between Oct. 1 and Oct. 22, 880,000 people were sickened with flu, 420,000 people visited a health care provider for flu illness, and 6,900 people were hospitalized for flu. The cumulative hospitalization rate is higher than observed at this time of year in every previous flu season since 2010-2011. Hospitalization rates are highest in children aged 0-4 years and adults 65 years and older.
Of course, this report came as no surprise to pediatric health care providers. Many children’s hospitals had been operating at or over capacity for weeks. While a systematic assessment of the surge on children’s hospitals has not been published, anecdotally, hospitals from around the country have described record emergency department visits and inpatient census numbers. Some have set up tents or other temporary facilities to see ambulatory patients and have canceled elective surgeries because of a lack of beds.
There is no quick or easy solution to stem the tide of RSV-related or enterovirus/rhinovirus admissions, but many flu-related hospitalizations are vaccine preventable. Unfortunately, too few children are receiving influenza vaccine. As of the week ending Oct. 15, only about 22.1% of eligible children had been immunized. The American Academy of Pediatrics and the CDC recommend that all children are vaccinated, preferably by the end of October so they have time to develop immunity before influenza starts circulating. As it stands now, the majority of the nation’s children are facing a flu season without the benefits of vaccine.
There is still time to take steps to prevent this flu season from becoming one of the worst in recent memory. A strong provider recommendation for influenza vaccine is consistently associated with higher rates of vaccine acceptance. We need to recommend influenza vaccine to all eligible patients at every visit and in every setting. It will help if we can say it like we mean it. Some of us are tired of debating the merits of COVID-19 vaccine with families and may be leery of additional debates about flu. Some of us may just be tired, as many practices have already expanded office hours to care for the influx of kids with respiratory illness. On the heels of two atypical flu seasons, a few of us may be quietly complacent about the importance of flu vaccines for children.
Anyone in need of a little motivation should check out a paper recently published in Clinical Infectious Diseases that reinforces the value of flu vaccine, even in a year when there is a poor match between the vaccine and circulating viruses.
The 2019-2020 flu season was a bad flu season for children. Two antigenically drifted influenza viruses predominated and cases of influenza soared, resulting in the largest influenza epidemic in children in the United States since 1992. Pediatric Intensive Care Influenza Study investigators used a test-negative design to estimate the effectiveness of influenza vaccine in preventing critical and life-threatening influenza in children during that season. The good news: vaccination reduced the risk of critical influenza by 78% against H1N1pdm09 viruses that were well-matched to vaccine and by 47% against mismatched viruses. Vaccination was estimated to be 75% protective against antigenically drifted B-Victoria viruses. Overall vaccine effectiveness against critical illness from any influenza virus was 63% (95% confidence interval, 38%-78%).
While it might be tempting to attribute suboptimal immunization rates to vaccine hesitancy, ready availability remains an issue for some families. We need to eliminate barriers to access. While the AAP continues to emphasize immunization in the medical home, especially for the youngest infants, the 2022 policy statement suggests that vaccinating children in schools, pharmacies, and other nontraditional settings could improve immunization rates. To the extent feasible, we need to work with partners to support community-based initiatives and promote these to families who struggle to make it into the office.
Improving access is just one potential way to reduce health disparities related to influenza and influenza vaccination. Over 10 influenza seasons, higher rates of influenza-associated hospitalizations and intensive care unit admissions were observed in Black, Hispanic, and American Indian/Alaska Native people. These disparities were highest in children aged younger than 4 years and influenza-associated in-hospital deaths were three- to fourfold higher in Black, Hispanic, and Asian/Pacific Islander children, compared with White children. The reason for the disparities isn’t completely clear but increasing immunization rates may be part of the solution. During the 2020-2021 influenza season, flu immunization rates in Black children (51.6%) were lower than those seen in White (57.4%) and Hispanic children (58.9%).
The AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023, highlight a variety of evidence-based strategies to increase influenza immunization rates. These may provide a little inspiration for clinicians looking to try a new approach. If you wish to share your experience with increasing influenza immunization rates in your practice setting, please email me at [email protected].
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She is a member of the AAP’s Committee on Infectious Diseases and one of the lead authors of the AAP’s Recommendations for Prevention and Control of Influenza in Children, 2022–2023. The opinions expressed in this article are her own. Dr. Bryant discloses that she has served as an investigator on clinical trials funded by Pfizer, Enanta, and Gilead.
Do scare tactics work?
I suspect that you have heard about or maybe read the recent Associated Press story reporting that four daycare workers in Hamilton, Miss., have been charged with felony child abuse for intentionally scaring the children “who didn’t clean up or act good” by wearing a Halloween mask and yelling in their faces. I can have some sympathy for those among us who choose to spend their days tending a flock of sometimes unruly and mischievous toddlers and preschoolers. But, I think one would be hard pressed to find very many adults who would condone the strategy of these misguided daycare providers. Not surprisingly, the parents of some of these children describe their children as traumatized and having disordered sleep.
The news report of this incident in Mississippi doesn’t tell us if these daycare providers had used this tactic in the past. One wonders whether they had found less dramatic verbal threats just weren’t as effective as they had hoped and so decided to go all out.
How effective is fear in changing behavior? Certainly, we have all experienced situations in which a frightening experience has caused us to avoid places, people, and activities. But, is a fear-focused strategy one that health care providers should include in their quiver as we try to mold patient behavior? As luck would have it, 2 weeks before this news story broke I encountered a global study from 84 countries that sought to answer this question (Affect Sci. 2022 Sep. doi: 10.1007/s42761-022-00128-3).
Using the WHO four-point advice about COVID prevention (stay home/avoid shops/use face covering/isolate if exposed) as a model the researchers around the world reviewed the responses of 16,000 individuals. They found that there was no difference in the effectiveness of the message whether it was framed as a negative (“you have so much to lose”) or a positive (“you have so much to gain”). However, investigators observed that the negatively framed presentations generated significantly more anxiety in the respondents. The authors of the paper conclude that if there is no significant difference in the effectiveness, why would we chose a negatively framed presentation that is likely to generate anxiety that we know is associated with increased morbidity and mortality. From a purely public health perspective, it doesn’t make sense and is counterproductive.
I guess if we look back to the old carrot and stick metaphor we shouldn’t be surprised by the findings in this paper. If one’s only goal is to get a group of young preschoolers to behave by scaring the b’geezes out of them with a mask or a threat of bodily punishment, then go for it. Scare tactics will probably work just as well as offering a well-chosen reward system. However, the devil is in the side effects. It’s the same argument that I give to parents who argue that spanking works. Of course it does, but it has a narrow margin for safety and can set up ripples of negative side effects that can destroy healthy parent-child relationships.
The bottom line of this story is the sad truth that somewhere along the line someone failed to effectively train these four daycare workers. But, do we as health care providers need to rethink our training? Have we forgotten our commitment to “First do no harm?” As we craft our messaging have we thought enough about the potential side effects of our attempts at scaring the public into following our suggestions?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that you have heard about or maybe read the recent Associated Press story reporting that four daycare workers in Hamilton, Miss., have been charged with felony child abuse for intentionally scaring the children “who didn’t clean up or act good” by wearing a Halloween mask and yelling in their faces. I can have some sympathy for those among us who choose to spend their days tending a flock of sometimes unruly and mischievous toddlers and preschoolers. But, I think one would be hard pressed to find very many adults who would condone the strategy of these misguided daycare providers. Not surprisingly, the parents of some of these children describe their children as traumatized and having disordered sleep.
The news report of this incident in Mississippi doesn’t tell us if these daycare providers had used this tactic in the past. One wonders whether they had found less dramatic verbal threats just weren’t as effective as they had hoped and so decided to go all out.
How effective is fear in changing behavior? Certainly, we have all experienced situations in which a frightening experience has caused us to avoid places, people, and activities. But, is a fear-focused strategy one that health care providers should include in their quiver as we try to mold patient behavior? As luck would have it, 2 weeks before this news story broke I encountered a global study from 84 countries that sought to answer this question (Affect Sci. 2022 Sep. doi: 10.1007/s42761-022-00128-3).
Using the WHO four-point advice about COVID prevention (stay home/avoid shops/use face covering/isolate if exposed) as a model the researchers around the world reviewed the responses of 16,000 individuals. They found that there was no difference in the effectiveness of the message whether it was framed as a negative (“you have so much to lose”) or a positive (“you have so much to gain”). However, investigators observed that the negatively framed presentations generated significantly more anxiety in the respondents. The authors of the paper conclude that if there is no significant difference in the effectiveness, why would we chose a negatively framed presentation that is likely to generate anxiety that we know is associated with increased morbidity and mortality. From a purely public health perspective, it doesn’t make sense and is counterproductive.
I guess if we look back to the old carrot and stick metaphor we shouldn’t be surprised by the findings in this paper. If one’s only goal is to get a group of young preschoolers to behave by scaring the b’geezes out of them with a mask or a threat of bodily punishment, then go for it. Scare tactics will probably work just as well as offering a well-chosen reward system. However, the devil is in the side effects. It’s the same argument that I give to parents who argue that spanking works. Of course it does, but it has a narrow margin for safety and can set up ripples of negative side effects that can destroy healthy parent-child relationships.
The bottom line of this story is the sad truth that somewhere along the line someone failed to effectively train these four daycare workers. But, do we as health care providers need to rethink our training? Have we forgotten our commitment to “First do no harm?” As we craft our messaging have we thought enough about the potential side effects of our attempts at scaring the public into following our suggestions?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that you have heard about or maybe read the recent Associated Press story reporting that four daycare workers in Hamilton, Miss., have been charged with felony child abuse for intentionally scaring the children “who didn’t clean up or act good” by wearing a Halloween mask and yelling in their faces. I can have some sympathy for those among us who choose to spend their days tending a flock of sometimes unruly and mischievous toddlers and preschoolers. But, I think one would be hard pressed to find very many adults who would condone the strategy of these misguided daycare providers. Not surprisingly, the parents of some of these children describe their children as traumatized and having disordered sleep.
The news report of this incident in Mississippi doesn’t tell us if these daycare providers had used this tactic in the past. One wonders whether they had found less dramatic verbal threats just weren’t as effective as they had hoped and so decided to go all out.
How effective is fear in changing behavior? Certainly, we have all experienced situations in which a frightening experience has caused us to avoid places, people, and activities. But, is a fear-focused strategy one that health care providers should include in their quiver as we try to mold patient behavior? As luck would have it, 2 weeks before this news story broke I encountered a global study from 84 countries that sought to answer this question (Affect Sci. 2022 Sep. doi: 10.1007/s42761-022-00128-3).
Using the WHO four-point advice about COVID prevention (stay home/avoid shops/use face covering/isolate if exposed) as a model the researchers around the world reviewed the responses of 16,000 individuals. They found that there was no difference in the effectiveness of the message whether it was framed as a negative (“you have so much to lose”) or a positive (“you have so much to gain”). However, investigators observed that the negatively framed presentations generated significantly more anxiety in the respondents. The authors of the paper conclude that if there is no significant difference in the effectiveness, why would we chose a negatively framed presentation that is likely to generate anxiety that we know is associated with increased morbidity and mortality. From a purely public health perspective, it doesn’t make sense and is counterproductive.
I guess if we look back to the old carrot and stick metaphor we shouldn’t be surprised by the findings in this paper. If one’s only goal is to get a group of young preschoolers to behave by scaring the b’geezes out of them with a mask or a threat of bodily punishment, then go for it. Scare tactics will probably work just as well as offering a well-chosen reward system. However, the devil is in the side effects. It’s the same argument that I give to parents who argue that spanking works. Of course it does, but it has a narrow margin for safety and can set up ripples of negative side effects that can destroy healthy parent-child relationships.
The bottom line of this story is the sad truth that somewhere along the line someone failed to effectively train these four daycare workers. But, do we as health care providers need to rethink our training? Have we forgotten our commitment to “First do no harm?” As we craft our messaging have we thought enough about the potential side effects of our attempts at scaring the public into following our suggestions?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Four methods to chip away at imposter syndrome
Regardless of the setting, one of the most frequently discussed topics in health care is imposter syndrome.
Imposter syndrome was first defined by Clance and Imes as an inability to internalize success, and the tendency to attribute success to external causes such as luck, error, or knowing the appropriate individual.1 This definition is essential because most health care professionals have had a sense of doubt or questioned the full extent of their competencies in various situations. I would argue that this is normal and – within reason – helpful to the practice of medicine. The problem with true imposter syndrome is that the individual does not incorporate success in a way that builds healthy self-esteem and self-efficacy.2
Imposter syndrome has a very nasty way of interacting with burnout. Studies have shown that imposter syndrome can be associated with high levels of emotional exhaustion at work.3 In my experience, this makes clinical sense. Professionals suffering from imposter syndrome can spend a great deal of time and energy trying to maintain a particular image.4 They are acting a part 24/7. Have you ever seriously tried to act? It’s arduous work. A friend once asked me to read a role for a play because “you’d be great; you’re a natural.” By the time I was done with rehearsal, I felt like I had run a 4-by-400-meter relay, by myself, in Victoria, Tex.
And any talk of imposter syndrome must include its running mate, perfectionism. These two conditions exist together so commonly it can be a bit of a chicken or egg question as to which came first.
Imposter syndrome, perfectionism, and burnout can form a deadly triad if not recognized and addressed quickly. In medicine, perfectionism can be a coping strategy that sets up unrelenting standards. Failure to meet unrelenting standards then serves as fuel and validation for imposter syndrome and emotional exhaustion. The consequences of this cycle going unchecked over a health care professional’s career are seismic and can include downstream effects ranging from depression to suicide.
Some readers will relate to this, while others will shrug their shoulders and say that this has never happened in their professional life. I get it. However, I would now ask if you have ever felt like an imposter in your personal life. I’ll make a cup of tea and wait for you to figure out precisely what is the boundary between your personal and professional life. Okay, all done? Great. Now I’ll give you some more time to sincerely reflect if any of the traits of imposter syndrome have described you at times in your personal life. Hmmm, interesting to think about, isn’t it?
I believe that health care professionals frequently use one credit card to pay off another, but the debt remains the same. So even if things are going well at work, we may have just shifted the debt to our personal lives. (At some point in the future, I’ll share my 10 greatest father fails to date to elucidate my point.)
In my work at the GW Resiliency and Well-Being Center, I’ve gravitated toward a few methods supported by evidence that help alleviate imposter syndrome symptoms and potentially serve as protective factors against the future development of imposter syndrome.4 These include but are not limited to:
- Keep a record of small personal success that is yours alone.
- Have a mentor to share failures with.
- Use personal reflection to examine what it means to successfully reach your goals and fulfill your purpose, not a relative value unit target.
- Share experiences with each other, so you know you’re not alone.
The last method is one of my favorites because it involves connecting to others and shining a light on our shared experiences and, coincidentally, our collective strengths. Once this collective strength is realized, the circumstances of that 4-by-400-meter relay change drastically. Be safe and well, everyone.
Lorenzo Norris, MD, is a psychiatrist and chief wellness officer for the George Washington University Medical Enterprise and serves as associate dean of student affairs and administration for the George Washington University School of Medicine and Health Sciences. A version of this article first appeared on Medscape.com.
References
1. Clance PR, Imes SA. The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy: Theory, Research & Practice. 1978;15(3): 241-7. doi: 10.1037/h0086006.
2. Thomas M, Bigatti S. Perfectionism, impostor phenomenon, and mental health in medicine: A literature review. Int J Med Educ. 2020 Sep 28;11:201-3. doi: 10.5116/ijme.5f54.c8f8.
3. Liu RQ et al. Impostorism and anxiety contribute to burnout among resident physicians. Med Teach. 2022 Jul;44(7):758-64. doi: 10.1080/0142159X.2022.2028751.
4. Gottlieb M et al. Impostor syndrome among physicians and physicians in training: A scoping review. Med Educ. 2020 Feb;54(2):116-24. doi: 10.1111/medu.13956.
Regardless of the setting, one of the most frequently discussed topics in health care is imposter syndrome.
Imposter syndrome was first defined by Clance and Imes as an inability to internalize success, and the tendency to attribute success to external causes such as luck, error, or knowing the appropriate individual.1 This definition is essential because most health care professionals have had a sense of doubt or questioned the full extent of their competencies in various situations. I would argue that this is normal and – within reason – helpful to the practice of medicine. The problem with true imposter syndrome is that the individual does not incorporate success in a way that builds healthy self-esteem and self-efficacy.2
Imposter syndrome has a very nasty way of interacting with burnout. Studies have shown that imposter syndrome can be associated with high levels of emotional exhaustion at work.3 In my experience, this makes clinical sense. Professionals suffering from imposter syndrome can spend a great deal of time and energy trying to maintain a particular image.4 They are acting a part 24/7. Have you ever seriously tried to act? It’s arduous work. A friend once asked me to read a role for a play because “you’d be great; you’re a natural.” By the time I was done with rehearsal, I felt like I had run a 4-by-400-meter relay, by myself, in Victoria, Tex.
And any talk of imposter syndrome must include its running mate, perfectionism. These two conditions exist together so commonly it can be a bit of a chicken or egg question as to which came first.
Imposter syndrome, perfectionism, and burnout can form a deadly triad if not recognized and addressed quickly. In medicine, perfectionism can be a coping strategy that sets up unrelenting standards. Failure to meet unrelenting standards then serves as fuel and validation for imposter syndrome and emotional exhaustion. The consequences of this cycle going unchecked over a health care professional’s career are seismic and can include downstream effects ranging from depression to suicide.
Some readers will relate to this, while others will shrug their shoulders and say that this has never happened in their professional life. I get it. However, I would now ask if you have ever felt like an imposter in your personal life. I’ll make a cup of tea and wait for you to figure out precisely what is the boundary between your personal and professional life. Okay, all done? Great. Now I’ll give you some more time to sincerely reflect if any of the traits of imposter syndrome have described you at times in your personal life. Hmmm, interesting to think about, isn’t it?
I believe that health care professionals frequently use one credit card to pay off another, but the debt remains the same. So even if things are going well at work, we may have just shifted the debt to our personal lives. (At some point in the future, I’ll share my 10 greatest father fails to date to elucidate my point.)
In my work at the GW Resiliency and Well-Being Center, I’ve gravitated toward a few methods supported by evidence that help alleviate imposter syndrome symptoms and potentially serve as protective factors against the future development of imposter syndrome.4 These include but are not limited to:
- Keep a record of small personal success that is yours alone.
- Have a mentor to share failures with.
- Use personal reflection to examine what it means to successfully reach your goals and fulfill your purpose, not a relative value unit target.
- Share experiences with each other, so you know you’re not alone.
The last method is one of my favorites because it involves connecting to others and shining a light on our shared experiences and, coincidentally, our collective strengths. Once this collective strength is realized, the circumstances of that 4-by-400-meter relay change drastically. Be safe and well, everyone.
Lorenzo Norris, MD, is a psychiatrist and chief wellness officer for the George Washington University Medical Enterprise and serves as associate dean of student affairs and administration for the George Washington University School of Medicine and Health Sciences. A version of this article first appeared on Medscape.com.
References
1. Clance PR, Imes SA. The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy: Theory, Research & Practice. 1978;15(3): 241-7. doi: 10.1037/h0086006.
2. Thomas M, Bigatti S. Perfectionism, impostor phenomenon, and mental health in medicine: A literature review. Int J Med Educ. 2020 Sep 28;11:201-3. doi: 10.5116/ijme.5f54.c8f8.
3. Liu RQ et al. Impostorism and anxiety contribute to burnout among resident physicians. Med Teach. 2022 Jul;44(7):758-64. doi: 10.1080/0142159X.2022.2028751.
4. Gottlieb M et al. Impostor syndrome among physicians and physicians in training: A scoping review. Med Educ. 2020 Feb;54(2):116-24. doi: 10.1111/medu.13956.
Regardless of the setting, one of the most frequently discussed topics in health care is imposter syndrome.
Imposter syndrome was first defined by Clance and Imes as an inability to internalize success, and the tendency to attribute success to external causes such as luck, error, or knowing the appropriate individual.1 This definition is essential because most health care professionals have had a sense of doubt or questioned the full extent of their competencies in various situations. I would argue that this is normal and – within reason – helpful to the practice of medicine. The problem with true imposter syndrome is that the individual does not incorporate success in a way that builds healthy self-esteem and self-efficacy.2
Imposter syndrome has a very nasty way of interacting with burnout. Studies have shown that imposter syndrome can be associated with high levels of emotional exhaustion at work.3 In my experience, this makes clinical sense. Professionals suffering from imposter syndrome can spend a great deal of time and energy trying to maintain a particular image.4 They are acting a part 24/7. Have you ever seriously tried to act? It’s arduous work. A friend once asked me to read a role for a play because “you’d be great; you’re a natural.” By the time I was done with rehearsal, I felt like I had run a 4-by-400-meter relay, by myself, in Victoria, Tex.
And any talk of imposter syndrome must include its running mate, perfectionism. These two conditions exist together so commonly it can be a bit of a chicken or egg question as to which came first.
Imposter syndrome, perfectionism, and burnout can form a deadly triad if not recognized and addressed quickly. In medicine, perfectionism can be a coping strategy that sets up unrelenting standards. Failure to meet unrelenting standards then serves as fuel and validation for imposter syndrome and emotional exhaustion. The consequences of this cycle going unchecked over a health care professional’s career are seismic and can include downstream effects ranging from depression to suicide.
Some readers will relate to this, while others will shrug their shoulders and say that this has never happened in their professional life. I get it. However, I would now ask if you have ever felt like an imposter in your personal life. I’ll make a cup of tea and wait for you to figure out precisely what is the boundary between your personal and professional life. Okay, all done? Great. Now I’ll give you some more time to sincerely reflect if any of the traits of imposter syndrome have described you at times in your personal life. Hmmm, interesting to think about, isn’t it?
I believe that health care professionals frequently use one credit card to pay off another, but the debt remains the same. So even if things are going well at work, we may have just shifted the debt to our personal lives. (At some point in the future, I’ll share my 10 greatest father fails to date to elucidate my point.)
In my work at the GW Resiliency and Well-Being Center, I’ve gravitated toward a few methods supported by evidence that help alleviate imposter syndrome symptoms and potentially serve as protective factors against the future development of imposter syndrome.4 These include but are not limited to:
- Keep a record of small personal success that is yours alone.
- Have a mentor to share failures with.
- Use personal reflection to examine what it means to successfully reach your goals and fulfill your purpose, not a relative value unit target.
- Share experiences with each other, so you know you’re not alone.
The last method is one of my favorites because it involves connecting to others and shining a light on our shared experiences and, coincidentally, our collective strengths. Once this collective strength is realized, the circumstances of that 4-by-400-meter relay change drastically. Be safe and well, everyone.
Lorenzo Norris, MD, is a psychiatrist and chief wellness officer for the George Washington University Medical Enterprise and serves as associate dean of student affairs and administration for the George Washington University School of Medicine and Health Sciences. A version of this article first appeared on Medscape.com.
References
1. Clance PR, Imes SA. The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention. Psychotherapy: Theory, Research & Practice. 1978;15(3): 241-7. doi: 10.1037/h0086006.
2. Thomas M, Bigatti S. Perfectionism, impostor phenomenon, and mental health in medicine: A literature review. Int J Med Educ. 2020 Sep 28;11:201-3. doi: 10.5116/ijme.5f54.c8f8.
3. Liu RQ et al. Impostorism and anxiety contribute to burnout among resident physicians. Med Teach. 2022 Jul;44(7):758-64. doi: 10.1080/0142159X.2022.2028751.
4. Gottlieb M et al. Impostor syndrome among physicians and physicians in training: A scoping review. Med Educ. 2020 Feb;54(2):116-24. doi: 10.1111/medu.13956.
Fitness trackers: Useful in sleep medicine?
Who doesn’t love data, especially their own? With that thought in mind, over the years I have owned several activity trackers, including at least two Fitbits, and I frequently check my iPhone to see how far I’ve walked or how many steps I have taken. My most recent acquisition is an Oura (smart ring, third generation), which includes my first sleep tracker.
Sleep trackers are not unique to the Oura Ring; they are included on many of the newer activity trackers and smart watches, but the design and breakdown of daily sleep, activity, and readiness scores are hallmarks of Oura Rings.
The ring generates data for different phases of sleep, movements, oxygen saturation, disturbances in breathing, heart rate, and heart rate variability. I began to wonder how useful this information would be clinically and whether it might be helpful in either the diagnosis or treatment of sleep disorders.
David Neubauer, MD, is a psychiatrist at the Johns Hopkins Sleep Disorders Center. “Sleep tracking devices are more than just toys but less than medical devices. They do have clinical utility and might show findings that warrant further medical workup,” Dr. Neubauer said. “It is impressive that these devices estimate sleep as well as they do, but there is a problem with how they divide sleep stages that can lead people to believe their sleep is worse than it really is.”
For more than 50 years, he explained, sleep researchers and clinicians have categorized sleep as non–rapid eye movement (NREM) sleep stages 1-4 and REM sleep. More recently, sleep was reorganized to N1, N2, and N3 (which combines the older stages 3 and 4, representing “deep sleep” or “slow wave sleep”) and REM sleep. We normally spend more time in N2 than the other stages. However, the device companies often categorize their sleep estimates as “light sleep,” “deep sleep,” or “REM.” With “light sleep,” they are lumping together N1 and N2 sleep, and this is misleading, said Dr. Neubauer. “Understandably, people often think that there is something wrong if their tracker reports they are spending a lot of time in light sleep, when actually their sleep may be entirely normal.”
Sleep tracker validity
A study by Massimiliano de Zambotti, PhD, and colleagues, “The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography”, looked at sleep patterns of 41 adolescents and young adults and concluded that the second-generation tracker was accurate in terms of total sleep but underestimated time spent in N3 stage sleep by approximately 20 minutes while overestimating time spent in REM sleep by 17 minutes. They concluded that the ring had potential to be clinically useful but that further studies and validation were needed.
A larger study of the newest, third-generation Oura tracker, conducted by Altini and Kinnunen at Oura Health, found that the added sensors with the newer-generation ring led to improved accuracy, but they noted that the study was done with a healthy population and might not generalize to clinical populations.
Fernando Goes, MD, and Matthew Reid, PhD, both at Johns Hopkins, are working on a multicenter study using the Oura Ring and the mindLAMP app to look at the impact of sleep on mood in people with mood disorders as well as healthy controls. Dr. Reid said that “validation of sleep stages takes a hit when the ring is used in people with insomnia. We find it useful for total sleep time, but when you look at sleep architecture, the concordance is only 60%. And oxygen saturation measures are less accurate in people with dark skin.”
Clinical uses for sleep trackers
More accurate information might prove reassuring to patients. Dr. Goes added, “One use, for example, might be to help patients to limit or come off of long-term hypnotics with a more benign intervention that incorporates passive monitoring such as that in the Oura Ring. Some patients worry excessively about not being able to sleep, and sleep monitoring data can be helpful to reduce some of these concerns so patients can focus on safer interventions, such as cognitive behavioral therapy for insomnia.” Dr. Reid believes that wearable trackers have potential usefulness in monitoring sleep in patients with insomnia. “In insomnia, sleep state misperception is common. They are hyper-aroused, and they perceive that they are awake when in fact they are sleeping.”
Dr. Goes mentioned another use for sleep trackers in clinical settings: “In our inpatient units, the nurses open the door to look in on patients every hour to monitor and document if they are sleeping. If they look in and the patient isn’t moving, they will ask the patient to raise their hand, which of course is not going to help someone to fall back asleep.” Wearable devices might provide data on sleep without the risk of waking patients every hour through the night.
Not medical devices
However, Dr. Neubauer emphasized that current sleep trackers are not medical devices, saying “they may be measuring the same parameters that are measured with medical devices, for example pulse oximetry or sleep states, but there’s no simple answer yet to the question of whether the devices provide reliable data for clinical decision-making.”
Dr. Neubauer is skeptical about the accuracy of some of the measures the device provides. “I would not use the information from a consumer device to rule out obstructive sleep apnea based on good oxygen saturation numbers. So much depends on the history – snoring, gasping awakenings, reports from bed partners, and daytime sleepiness. These devices do not measure respiratory effort or nasal airflow as sleep studies do. But big drops in oxygen saturation from a consumer device certainly warrant attention for further evaluation.” Dr. Neubauer also noted that the parameters on sleep trackers do not differentiate between central or obstructive sleep apnea and that insurers won’t pay for continuous positive airway pressure to treat sleep apnea without a sleep study.
I enjoy looking at the data, even knowing that they are not entirely accurate. and we may find more clinical uses for these devices. For now, I’m off to get more exercise, at the suggestion of my tracker!
Dinah Miller, MD, is assistant professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore.
A version of this article first appeared on Medscape.com.
Who doesn’t love data, especially their own? With that thought in mind, over the years I have owned several activity trackers, including at least two Fitbits, and I frequently check my iPhone to see how far I’ve walked or how many steps I have taken. My most recent acquisition is an Oura (smart ring, third generation), which includes my first sleep tracker.
Sleep trackers are not unique to the Oura Ring; they are included on many of the newer activity trackers and smart watches, but the design and breakdown of daily sleep, activity, and readiness scores are hallmarks of Oura Rings.
The ring generates data for different phases of sleep, movements, oxygen saturation, disturbances in breathing, heart rate, and heart rate variability. I began to wonder how useful this information would be clinically and whether it might be helpful in either the diagnosis or treatment of sleep disorders.
David Neubauer, MD, is a psychiatrist at the Johns Hopkins Sleep Disorders Center. “Sleep tracking devices are more than just toys but less than medical devices. They do have clinical utility and might show findings that warrant further medical workup,” Dr. Neubauer said. “It is impressive that these devices estimate sleep as well as they do, but there is a problem with how they divide sleep stages that can lead people to believe their sleep is worse than it really is.”
For more than 50 years, he explained, sleep researchers and clinicians have categorized sleep as non–rapid eye movement (NREM) sleep stages 1-4 and REM sleep. More recently, sleep was reorganized to N1, N2, and N3 (which combines the older stages 3 and 4, representing “deep sleep” or “slow wave sleep”) and REM sleep. We normally spend more time in N2 than the other stages. However, the device companies often categorize their sleep estimates as “light sleep,” “deep sleep,” or “REM.” With “light sleep,” they are lumping together N1 and N2 sleep, and this is misleading, said Dr. Neubauer. “Understandably, people often think that there is something wrong if their tracker reports they are spending a lot of time in light sleep, when actually their sleep may be entirely normal.”
Sleep tracker validity
A study by Massimiliano de Zambotti, PhD, and colleagues, “The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography”, looked at sleep patterns of 41 adolescents and young adults and concluded that the second-generation tracker was accurate in terms of total sleep but underestimated time spent in N3 stage sleep by approximately 20 minutes while overestimating time spent in REM sleep by 17 minutes. They concluded that the ring had potential to be clinically useful but that further studies and validation were needed.
A larger study of the newest, third-generation Oura tracker, conducted by Altini and Kinnunen at Oura Health, found that the added sensors with the newer-generation ring led to improved accuracy, but they noted that the study was done with a healthy population and might not generalize to clinical populations.
Fernando Goes, MD, and Matthew Reid, PhD, both at Johns Hopkins, are working on a multicenter study using the Oura Ring and the mindLAMP app to look at the impact of sleep on mood in people with mood disorders as well as healthy controls. Dr. Reid said that “validation of sleep stages takes a hit when the ring is used in people with insomnia. We find it useful for total sleep time, but when you look at sleep architecture, the concordance is only 60%. And oxygen saturation measures are less accurate in people with dark skin.”
Clinical uses for sleep trackers
More accurate information might prove reassuring to patients. Dr. Goes added, “One use, for example, might be to help patients to limit or come off of long-term hypnotics with a more benign intervention that incorporates passive monitoring such as that in the Oura Ring. Some patients worry excessively about not being able to sleep, and sleep monitoring data can be helpful to reduce some of these concerns so patients can focus on safer interventions, such as cognitive behavioral therapy for insomnia.” Dr. Reid believes that wearable trackers have potential usefulness in monitoring sleep in patients with insomnia. “In insomnia, sleep state misperception is common. They are hyper-aroused, and they perceive that they are awake when in fact they are sleeping.”
Dr. Goes mentioned another use for sleep trackers in clinical settings: “In our inpatient units, the nurses open the door to look in on patients every hour to monitor and document if they are sleeping. If they look in and the patient isn’t moving, they will ask the patient to raise their hand, which of course is not going to help someone to fall back asleep.” Wearable devices might provide data on sleep without the risk of waking patients every hour through the night.
Not medical devices
However, Dr. Neubauer emphasized that current sleep trackers are not medical devices, saying “they may be measuring the same parameters that are measured with medical devices, for example pulse oximetry or sleep states, but there’s no simple answer yet to the question of whether the devices provide reliable data for clinical decision-making.”
Dr. Neubauer is skeptical about the accuracy of some of the measures the device provides. “I would not use the information from a consumer device to rule out obstructive sleep apnea based on good oxygen saturation numbers. So much depends on the history – snoring, gasping awakenings, reports from bed partners, and daytime sleepiness. These devices do not measure respiratory effort or nasal airflow as sleep studies do. But big drops in oxygen saturation from a consumer device certainly warrant attention for further evaluation.” Dr. Neubauer also noted that the parameters on sleep trackers do not differentiate between central or obstructive sleep apnea and that insurers won’t pay for continuous positive airway pressure to treat sleep apnea without a sleep study.
I enjoy looking at the data, even knowing that they are not entirely accurate. and we may find more clinical uses for these devices. For now, I’m off to get more exercise, at the suggestion of my tracker!
Dinah Miller, MD, is assistant professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore.
A version of this article first appeared on Medscape.com.
Who doesn’t love data, especially their own? With that thought in mind, over the years I have owned several activity trackers, including at least two Fitbits, and I frequently check my iPhone to see how far I’ve walked or how many steps I have taken. My most recent acquisition is an Oura (smart ring, third generation), which includes my first sleep tracker.
Sleep trackers are not unique to the Oura Ring; they are included on many of the newer activity trackers and smart watches, but the design and breakdown of daily sleep, activity, and readiness scores are hallmarks of Oura Rings.
The ring generates data for different phases of sleep, movements, oxygen saturation, disturbances in breathing, heart rate, and heart rate variability. I began to wonder how useful this information would be clinically and whether it might be helpful in either the diagnosis or treatment of sleep disorders.
David Neubauer, MD, is a psychiatrist at the Johns Hopkins Sleep Disorders Center. “Sleep tracking devices are more than just toys but less than medical devices. They do have clinical utility and might show findings that warrant further medical workup,” Dr. Neubauer said. “It is impressive that these devices estimate sleep as well as they do, but there is a problem with how they divide sleep stages that can lead people to believe their sleep is worse than it really is.”
For more than 50 years, he explained, sleep researchers and clinicians have categorized sleep as non–rapid eye movement (NREM) sleep stages 1-4 and REM sleep. More recently, sleep was reorganized to N1, N2, and N3 (which combines the older stages 3 and 4, representing “deep sleep” or “slow wave sleep”) and REM sleep. We normally spend more time in N2 than the other stages. However, the device companies often categorize their sleep estimates as “light sleep,” “deep sleep,” or “REM.” With “light sleep,” they are lumping together N1 and N2 sleep, and this is misleading, said Dr. Neubauer. “Understandably, people often think that there is something wrong if their tracker reports they are spending a lot of time in light sleep, when actually their sleep may be entirely normal.”
Sleep tracker validity
A study by Massimiliano de Zambotti, PhD, and colleagues, “The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography”, looked at sleep patterns of 41 adolescents and young adults and concluded that the second-generation tracker was accurate in terms of total sleep but underestimated time spent in N3 stage sleep by approximately 20 minutes while overestimating time spent in REM sleep by 17 minutes. They concluded that the ring had potential to be clinically useful but that further studies and validation were needed.
A larger study of the newest, third-generation Oura tracker, conducted by Altini and Kinnunen at Oura Health, found that the added sensors with the newer-generation ring led to improved accuracy, but they noted that the study was done with a healthy population and might not generalize to clinical populations.
Fernando Goes, MD, and Matthew Reid, PhD, both at Johns Hopkins, are working on a multicenter study using the Oura Ring and the mindLAMP app to look at the impact of sleep on mood in people with mood disorders as well as healthy controls. Dr. Reid said that “validation of sleep stages takes a hit when the ring is used in people with insomnia. We find it useful for total sleep time, but when you look at sleep architecture, the concordance is only 60%. And oxygen saturation measures are less accurate in people with dark skin.”
Clinical uses for sleep trackers
More accurate information might prove reassuring to patients. Dr. Goes added, “One use, for example, might be to help patients to limit or come off of long-term hypnotics with a more benign intervention that incorporates passive monitoring such as that in the Oura Ring. Some patients worry excessively about not being able to sleep, and sleep monitoring data can be helpful to reduce some of these concerns so patients can focus on safer interventions, such as cognitive behavioral therapy for insomnia.” Dr. Reid believes that wearable trackers have potential usefulness in monitoring sleep in patients with insomnia. “In insomnia, sleep state misperception is common. They are hyper-aroused, and they perceive that they are awake when in fact they are sleeping.”
Dr. Goes mentioned another use for sleep trackers in clinical settings: “In our inpatient units, the nurses open the door to look in on patients every hour to monitor and document if they are sleeping. If they look in and the patient isn’t moving, they will ask the patient to raise their hand, which of course is not going to help someone to fall back asleep.” Wearable devices might provide data on sleep without the risk of waking patients every hour through the night.
Not medical devices
However, Dr. Neubauer emphasized that current sleep trackers are not medical devices, saying “they may be measuring the same parameters that are measured with medical devices, for example pulse oximetry or sleep states, but there’s no simple answer yet to the question of whether the devices provide reliable data for clinical decision-making.”
Dr. Neubauer is skeptical about the accuracy of some of the measures the device provides. “I would not use the information from a consumer device to rule out obstructive sleep apnea based on good oxygen saturation numbers. So much depends on the history – snoring, gasping awakenings, reports from bed partners, and daytime sleepiness. These devices do not measure respiratory effort or nasal airflow as sleep studies do. But big drops in oxygen saturation from a consumer device certainly warrant attention for further evaluation.” Dr. Neubauer also noted that the parameters on sleep trackers do not differentiate between central or obstructive sleep apnea and that insurers won’t pay for continuous positive airway pressure to treat sleep apnea without a sleep study.
I enjoy looking at the data, even knowing that they are not entirely accurate. and we may find more clinical uses for these devices. For now, I’m off to get more exercise, at the suggestion of my tracker!
Dinah Miller, MD, is assistant professor of psychiatry and behavioral sciences, Johns Hopkins Medicine, Baltimore.
A version of this article first appeared on Medscape.com.
Should health care be a right?
Is health care a human right?
This year voters in Oregon are being asked to decide that.
It brings up some interesting questions. Should it be a right? Food, water, shelter, and oxygen aren’t, as far as I know, considered such. So why health care?
Probably the main argument against the idea is that, if it’s a right, shouldn’t the government (and therefore taxpayers) be tasked with paying for it all?
Good question, and not one that I can answer. If my neighbor refuses to buy insurance, then has a health crisis he can’t afford, why should I have to pay for his obstinacy and lack of foresight? Isn’t it his problem?
Of course, the truth is that not everyone can afford health care, or insurance. They ain’t cheap. Even if you get coverage through your job, part of your earnings, and part of the company’s profits, are being taken out to pay for it.
This raises the question of whether health care is something that should be rationed only to the working, successfully retired, or wealthy. Heaven knows I have plenty of patients tell me that. Their point is that if you’re not contributing to society, why should society contribute to you?
One even said that our distant ancestors didn’t see an issue with this: If you were unable to hunt, or outrun a cave lion, you probably weren’t helping the rest of the tribe anyway and deserved what happened to you.
Perhaps true, but we aren’t our distant ancestors. Over the millennia we’ve developed into a remarkably social, and increasingly interconnected, species. Somewhat paradoxically we often care more about famines on the other side of the world than we do in our own cities. If you’re going to use the argument of “we didn’t used to do this,” we also didn’t used to have cars, planes, or computers, but I don’t see anyone giving them up.
Another thing to keep in mind is that we are all paying for the uninsured under pretty much any system of health care there is. Whether it’s through taxes, insurance premiums, or both, our own costs go up to pay the bills of those who don’t have coverage. So in that respect the financial aspect of declaring it a right probably doesn’t change the de facto truth of the situation. It just makes it more official-ish.
Maybe the statement has more philosophical or political meaning than it does practical. If it passes it may change a lot of things, or nothing at all, depending how it’s legally interpreted.
Like so many things, we won’t know where it goes unless it happens. And even then it’s uncertain where it will lead.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Is health care a human right?
This year voters in Oregon are being asked to decide that.
It brings up some interesting questions. Should it be a right? Food, water, shelter, and oxygen aren’t, as far as I know, considered such. So why health care?
Probably the main argument against the idea is that, if it’s a right, shouldn’t the government (and therefore taxpayers) be tasked with paying for it all?
Good question, and not one that I can answer. If my neighbor refuses to buy insurance, then has a health crisis he can’t afford, why should I have to pay for his obstinacy and lack of foresight? Isn’t it his problem?
Of course, the truth is that not everyone can afford health care, or insurance. They ain’t cheap. Even if you get coverage through your job, part of your earnings, and part of the company’s profits, are being taken out to pay for it.
This raises the question of whether health care is something that should be rationed only to the working, successfully retired, or wealthy. Heaven knows I have plenty of patients tell me that. Their point is that if you’re not contributing to society, why should society contribute to you?
One even said that our distant ancestors didn’t see an issue with this: If you were unable to hunt, or outrun a cave lion, you probably weren’t helping the rest of the tribe anyway and deserved what happened to you.
Perhaps true, but we aren’t our distant ancestors. Over the millennia we’ve developed into a remarkably social, and increasingly interconnected, species. Somewhat paradoxically we often care more about famines on the other side of the world than we do in our own cities. If you’re going to use the argument of “we didn’t used to do this,” we also didn’t used to have cars, planes, or computers, but I don’t see anyone giving them up.
Another thing to keep in mind is that we are all paying for the uninsured under pretty much any system of health care there is. Whether it’s through taxes, insurance premiums, or both, our own costs go up to pay the bills of those who don’t have coverage. So in that respect the financial aspect of declaring it a right probably doesn’t change the de facto truth of the situation. It just makes it more official-ish.
Maybe the statement has more philosophical or political meaning than it does practical. If it passes it may change a lot of things, or nothing at all, depending how it’s legally interpreted.
Like so many things, we won’t know where it goes unless it happens. And even then it’s uncertain where it will lead.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Is health care a human right?
This year voters in Oregon are being asked to decide that.
It brings up some interesting questions. Should it be a right? Food, water, shelter, and oxygen aren’t, as far as I know, considered such. So why health care?
Probably the main argument against the idea is that, if it’s a right, shouldn’t the government (and therefore taxpayers) be tasked with paying for it all?
Good question, and not one that I can answer. If my neighbor refuses to buy insurance, then has a health crisis he can’t afford, why should I have to pay for his obstinacy and lack of foresight? Isn’t it his problem?
Of course, the truth is that not everyone can afford health care, or insurance. They ain’t cheap. Even if you get coverage through your job, part of your earnings, and part of the company’s profits, are being taken out to pay for it.
This raises the question of whether health care is something that should be rationed only to the working, successfully retired, or wealthy. Heaven knows I have plenty of patients tell me that. Their point is that if you’re not contributing to society, why should society contribute to you?
One even said that our distant ancestors didn’t see an issue with this: If you were unable to hunt, or outrun a cave lion, you probably weren’t helping the rest of the tribe anyway and deserved what happened to you.
Perhaps true, but we aren’t our distant ancestors. Over the millennia we’ve developed into a remarkably social, and increasingly interconnected, species. Somewhat paradoxically we often care more about famines on the other side of the world than we do in our own cities. If you’re going to use the argument of “we didn’t used to do this,” we also didn’t used to have cars, planes, or computers, but I don’t see anyone giving them up.
Another thing to keep in mind is that we are all paying for the uninsured under pretty much any system of health care there is. Whether it’s through taxes, insurance premiums, or both, our own costs go up to pay the bills of those who don’t have coverage. So in that respect the financial aspect of declaring it a right probably doesn’t change the de facto truth of the situation. It just makes it more official-ish.
Maybe the statement has more philosophical or political meaning than it does practical. If it passes it may change a lot of things, or nothing at all, depending how it’s legally interpreted.
Like so many things, we won’t know where it goes unless it happens. And even then it’s uncertain where it will lead.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.