User login
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
Preventing arrhythmias and QTc prolongation in COVID-19 patients on psychotropics
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Over the last few weeks, several conflicting reports about the efficacy of SARS-CoV-2 treatments have emerged, including high-profile papers that were placed in the limelight and groundbreaking retractions that were issued by the Lancet and New England Journal of Medicine, involving the potential dangers of COVID therapy with findings derived from the Surgisphere database. Hydroxychloroquine has garnered considerable media attention and was touted earlier by President Trump for its therapeutic effects.1 Naturally, there are political connotations associated with the agent, and it is unlikely that hydroxychloroquine will be supplanted in the near future as ongoing clinical trials have demonstrated mixed results amid the controversy.
As clinicians navigating unchartered territory within the hospital setting, we have to come to terms with these new challenges, tailoring treatment protocols accordingly with the best clinical practices in mind. Patients with preexisting mental health conditions and who are being treated for COVID-19 are particularly susceptible to clinical deterioration. Recent studies have indicated that psychiatric patients are more prone to feelings of isolation and/or estrangement as well as exacerbation of symptoms such as paranoia.2 Even more concerning is the medication regimen, namely, the novel combination therapies that arise when agents such as hydroxychloroquine are used in tandem with certain antipsychotics or antidepressants.
What’s at stake for COVID-19–positive mental health care patients?
Although the efficacy of hydroxychloroquine is currently being investigated,3 the antimalarial is usually prescribed in tandem with azithromycin for people with COVID-19. The National Institute of Allergy and Infectious Diseases has advised against that particular combination therapy because of ongoing concerns about toxicities.3,4
In another study, azithromycin was effectively substituted with doxycycline to help minimize systemic effects for patients with cardiac and/or pulmonary issues.5 Azithromycin is notorious in the literature for influencing the electrical activity of the heart with the potential for fatal arrhythmia and sudden cardiac death in individuals at risk for cardiovascular disease.5,6,7 It should be noted that both of these commonly prescribed COVID-19 medications (for example, hydroxychloroquine and azithromycin) could lead to QT interval prolongation especially within the context of combination therapy. This is largely concerning for psychiatrists and various other mental health practitioners for the following reasons: (1) higher rates of metabolic syndrome and cardiovascular diseases among psychiatric patients8 and/or (2) effects of certain antipsychotics (for example, IV haloperidol, thioridazine, and ziprasidone) and antidepressants (for example, citalopram and escitalopram) on the QT interval.9
SARS-CoV-2 and clinical judgment: Evaluating patients at higher risk
Although COVID-19 medication guidelines are still being actively developed, hydroxychloroquine appears to be commonly prescribed by physicians. The medication is known myriad untoward effects, including potential behavioral dysfunction (for example, irritability, agitation, suicidal ideation)10 as well as the aforementioned issues concerning arrhythmia (for example, torsades de pointes). Health care professionals might not have much control over the choice of COVID-19 agents because of a lack of available resources or limited options, but they can exercise clinical judgment with respect to selecting the appropriate psychotropic medications.
Treatment recommendations
1. Establish a baseline EKG
A baseline 12-lead EKG is the standard of care for patients currently being screened for COVID-19. It is necessary to rule out the presence of an underlying cardiovascular disease or a rhythm irregularity. A prolonged QTc interval is generally regarded as being around greater than 450-470 msecs with variations attributable to gender;11 numerous studies have affirmed that the risk of acquiring torsades de pointes is substantial when the QTc interval exceeds 500 msecs.12
2. Medical management and risk assessment
Commonly prescribed antipsychotics such as IV haloperidol and ziprasidone are known for exerting a negative effect on the interval and should readily be substituted with other agents in patients who are being treated for COVID-19; the combination of these antipsychotics alongside some COVID-19 medication regimens (for example, hydroxychloroquine/azithromycin) might prove to be fatal. The same logic applies to COVID-19 patients previously on antidepressant therapeutics such as citalopram and escitalopram.
3. Embrace an individually tailored approach to therapeutics
While American Psychiatric Association guidelines historically supported a cessation or reduction in the offending agent under normal circumstances,12 our team is recommending that the psychotropics associated with QTc interval prolongation are discontinued altogether (or substituted with a low-risk agent) in the event that a patient presents with suspected COVID-19. However, after the patients tests negative with COVID-19, they may resume therapy as indicated under the discretion of the mental health practitioner.
References
1. Offard C. “Lancet, NEJM Retract Surgisphere Studies on COVID-19 Patients.” The Scientist Magazine. 2020 Jun 4.
2. Shigemura J et al. Psychiatry Clin Neurosci. 2020 Apr;74(4):281-2.
3. Keshtkar-Jahromi M and Bavari S. Am J Trop Med Hyg. 2020 May;102(5):932-3.
4. Palca J. “NIH panel recommends against drug combination promoted by Trump for COVID-19.” NPR. 2020 Apr 21.
5. Mongelli L. “Long Island doctor tries new twist on hydroxychloroquine for elderly COVID-19 patients.” New York Post. 2020 Apr 4.
6. Hancox JC et al. Ther Adv Infect Dis. 2013 Oct;(5):155-65.
7. Giudicessi JR and Ackerman MJ. Cleve Clin J Med. 2013 Sep;80(9):539-44.
8. Casey DE. Am J Med. 2005 Apr 1;118(Suppl 2):15S-22S.
9. Beach SR et al. Psychosomatics. 2013 Jan 1;54(1):1-3.
10. Bogaczewicz A and Sobów T. Psychiatria i Psychologia Kliniczna. 2017;17(2):111-4.
11. Chohan PS et al. Pak J Med Sci. 2015 Sep-Oct;31(5):1269-71.
12. Lieberman JA et al. APA guidance on the use of antipsychotic drugs and cardiac sudden death. NYS Office of Mental Health. 2012.
Dr. Faisal A. Islam is medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Faisal Islam disclosed no relevant financial relationships.
Dr. Mohammed Islam is affiliated with the department of psychiatry at the Interfaith Medical Center, New York. He disclosed no relevant financial relationships.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He disclosed no relevant financial relationships.
Getting unstuck: Helping patients with behavior change
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at [email protected].
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at [email protected].
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).
Kyle is a 14-year-old cisgender male who just moved to your town. At his first well-check, his single father brings him in reluctantly, stating, “We’ve never liked doctors.” Kyle has a history of asthma and obesity that have been relatively unchanged over time. He is an average student, an avid gamer, and seems somewhat shy. Privately he admits to occasional cannabis use. His father has no concerns, lamenting, “He’s always been pretty healthy for a fat kid.” Next patient?
Of course there is a lot to work with here. You might be concerned with Kyle’s asthma; his weight, sedentary nature, and body image; the criticism from his father and concerns about self-esteem; the possibility of anxiety in relation to his shyness; and the health effects of his cannabis use. In the end, recommendations for behavior change seem likely. These might take the form of tips on exercise, nutrition, substance use, study habits, parenting, social activities, or mental health support; the literature on behavior change would suggest that any success will be predicated on trust. How can we learn from someone we do not trust?1
To build trust is no easy task, and yet is perhaps the foundation on which the entire clinical relationship rests. Guidance from decades of evidence supporting the use of motivational interviewing2 suggests that the process of building rapport can be neatly summed up in an acronym as PACE. This represents Partnership, Acceptance, Compassion, and Evocation. Almost too clichéd to repeat, the most powerful change agent is the person making the change. In the setting of pediatric health care, we sometimes lean on caregivers to initiate or promote change because they are an intimate part of the patient’s microsystem, and thus moving one gear (the parents) inevitably shifts something in connected gears (the children).
So Partnership is centered on the patient, but inclusive of any important person in the patient’s sphere. In a family-based approach, this might show up as leveraging Kyle’s father’s motivation for behavior change by having the father start an exercise routine. This role models behavior change, shifts the home environment around the behavior, and builds empathy in the parent for the inherent challenges of change processes.
Acceptance can be distilled into knowing that the patient and family are doing the best they can. This does not preclude the possibility of change, but it seats this possibility in an attitude of assumed adequacy. There is nothing wrong with the patient, nothing to be fixed, just the possibility for change.
Similarly, Compassion takes a nonjudgmental viewpoint. With the stance of “this could happen to anybody,” the patient can feel responsible without feeling blamed. Noting the patient’s suffering without blame allows the clinician to be motivated not just to empathize, but to help.
And from this basis of compassionate partnership, the work of Evocation begins. What is happening in the patient’s life and relationships? What are their own goals and values? Where are the discrepancies between what the patient wants and what the patient does? For teenagers, this often brings into conflict developmentally appropriate wishes for autonomy – wanting to drive or get a car or stay out later or have more privacy – with developmentally typical challenges regarding responsibility.3 For example:
Clinician: “You want to use the car, and your parents want you to pay for the gas, but you’re out of money from buying weed. I see how you’re stuck.”
Teen: “Yeah, they really need to give me more allowance. It’s not like we’re living in the 1990s anymore!”
Clinician: “So you could ask for more allowance to get more money for gas. Any other ideas?”
Teen: “I could give up smoking pot and just be miserable all the time.”
Clinician: “Yeah, that sounds too difficult right now; if anything it sounds like you’d like to smoke more pot if you had more money.”
Teen: “Nah, I’m not that hooked on it. ... I could probably smoke a bit less each week and save some gas money.”
The PACE acronym also serves as a reminder of the patience required to grow connection where none has previously existed – pace yourself. Here are some skills-based tips to foster the spirit of motivational interviewing to help balance patience with the time frame of a pediatric check-in. The OARS skills represent the fundamental building blocks of motivational interviewing in practice. Taking the case of Kyle as an example, an Open-Ended Question makes space for the child or parent to express their views with less interviewer bias. Reflections expand this space by underscoring and, in the case of complex Reflections, adding some nuance to what the patient has to say.
Clinician: “How do you feel about your body?”
Teen: “Well, I’m fat. Nobody really wants to be fat. It sucks. But what can I do?”
Clinician: “You feel fat and kind of hopeless.”
Teen: “Yeah, I know you’re going to tell me to go on a diet and start exercising. Doesn’t work. My dad says I was born fat; I guess I’m going to stay that way.”
Clinician: “Sounds like you and your dad can get down on you for your weight. That must feel terrible.”
Teen: “Ah, it’s not that bad. I’m kind of used to it. Fat kid at home, fat kid at school.”
Affirmations are statements focusing on positive actions or attributes of the patient. They tend to build rapport by demonstrating that the clinician sees the strengths of the patient, not just the problems.
Clinician: “I’m pretty impressed that you’re able to show up here and talk about this. It can’t be easy when it sounds like your family and friends have put you down so much that you’re even putting yourself down about your body.”
Teen: “I didn’t really want to come, but then I thought, maybe this new doctor will have some new ideas. I actually want to do something about it, I just don’t know if anything will help. Plus my dad said if I showed up, we could go to McDonald’s afterward.”
Summaries are multipurpose. They demonstrate that you have been listening closely, which builds rapport. They provide a chance to put information together so that both clinician and patient can reflect on the sum of the data and notice what may be missing. And they provide a pause to consider where to go next.
Clinician: “So if I’m getting it right, you’ve been worried about your weight for a long time now. Your dad and your friends give you a hard time about it, which makes you feel down and hopeless, but somehow you stay brave and keep trying to figure it out. You feel ready to do something, you just don’t know what, and you were hoping maybe coming here could give you a place to work on your health. Does that sound about right?”
Teen: “I think that’s pretty much it. Plus the McDonald’s.”
Clinician: “Right, that’s important too – we have to consider your motivation! I wonder if we could talk about this more at our next visit – would that be alright?”
Offices with additional resources might be able to offer some of those as well, if timing seems appropriate; for example, referral to a wellness coach or social worker or nutritionist could be helpful int his case. With the spirit of PACE and the skills of OARS, you can be well on your way to fostering behavior changes that could last a lifetime! Check out the resources from the American Academy of Pediatrics with video and narrative demonstrations of motivational interviewing in pediatrics.
Dr. Rosenfeld is assistant professor in the departments of psychiatry and pediatrics at the University of Vermont Medical Center and the university’s Robert Larner College of Medicine, Burlington. He reported no relevant disclosures. Email him at [email protected].
References
1. Miller WR, Rollnick S. “Engagement and disengagement,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
2. Miller WR, Rollnick S. “The spirit of motivational interviewing,” in “Motivational interviewing: Helping people change,” 3rd ed. (New York: Guilford, 2013).
3. Naar S, Suarez M. “Adolescence and emerging adulthood: A brief review of development,” in “Motivational interviewing with adolescents and young adults” (New York: Guilford, 2011).
Racism: Developmental perspective can inform tough conversations
Can we help our pediatric patients with the complicated problems of racism, especially if we are privileged (and even white) professionals? We may not have experienced discrimination, but we can still advise and address it. Racist discrimination, fear, trauma, or distress may produce or exacerbate conditions we are treating.
Three levels of racism impact children’s health and health care: “structural or institutional” policies that influence social determinants of health; “personally mediated” differential treatment based on assumptions about one’s abilities, motives, or intents; and the resulting “internalization” of stereotypes into one’s identity, undermining confidence, self-esteem, and mental health. We can help advocate about structural racism and ensure equity within our offices, but how best to counsel the families and children themselves?
Racism includes actions of “assigning value based on the social interpretation of how a person looks” (Ethn Dis. 2008;18[4]:496-504). “Social interpretations” develop from an early age. Newborns detect differences in appearance and may startle or cry seeing a parent’s drastic haircut or new hat. Parents generally know to use soothing words and tone, bring the difference into view gradually, smile and comfort the child, and explain the change; these are good skills for later, too. Infants notice skin color, which, unlike clothes, is a stable feature by which to recognize parents. Social interpretation of these differences is cued from the parents’ feelings and reactions. Adults naturally transmit biases from their own past unless they work to dampen them. If the parent was taught to regard “other” as negative or is generally fearful, the child mirrors this. Working to reduce racism thus requires parents (and professionals) to examine their prejudices to be able to convey positive or neutral reactions to people who are different. Parents need to show curiosity, positive affect, and comfort about people who are different, and do well to seek contact and friendships with people from other groups and include their children in these relationships. We can encourage this outreach plus ensure diversity and respectful interactions in our offices.
Children from age 3 years value fairness and are upset seeing others treated unfairly – easily understanding “not fair” or “mean.” If the person being hurt is like them in race, ethnicity, religion, gender, or sexual preference, they also fear for themselves, family, and friends. Balance is needed in discussing racism to avoid increasing fear or overpromising as risks are real and solutions difficult. Children look to adults for understanding and evidence of action to feel safer, rather than helpless. We should state that leaders are working on “making the rules more fair,” ensuring that people “won’t be allowed do it again,” and “teaching that everyone deserves respect.” Even better, parents and children can generate ideas about child actions, giving them some power as an antidote to anxiety. Age-related possibilities might include drawing a picture of people getting along, talking at show-and-tell, writing a note to officials, making a protest sign, posting thoughts on Facebook, or protesting.
With age, the culture increasingly influences a child’s attitudes. Children see lots of teasing and bullying based on differences from being overweight or wearing glasses, to skin color. It is helpful to interpret for children that bullies are insecure, or sometimes have been hurt, and they put other people down to feel better than someone else. Thinking about racist acts this way may reduce the desire for revenge and a cycle of aggression. Effective anti-bullying programs help children recognize bullying, see it as an emergency that requires their action, tell adults, and take action. This action could be surrounding the bully, standing tall, making eye contact, having a dismissive retort, or asking questions that require the bully to think, such as “What do you want to happen by doing this?” We can coach our patients and their parents on these principles as well as advising schools.
Children need to be told that those being put down or held down – especially those like them – have strengths; have made discoveries; have produced writings, art, and music; have shown military bravery, moral leadership, and resistance to discrimination, but it is not the time to show strength when confronted by a gun or police. We can use and arm parents with examples to discuss strengths and accomplishments to help buffer the child from internalization of racist stereotypes. Children need positive role models who look like them; parents can seek out diverse professionals in their children’s lives, such as dentists, doctors, teachers, clergy, mentors, or coaches. We, and parents, can ensure that dolls and books are available, and that the children’s shows, movies, and video games are watched together and include diverse people doing good or brave things. These exposures also are key to all children becoming anti-racist.
Parents can be advised to initiate discussion of racism because children, detecting adult discomfort, may avoid the topic. We can encourage families to give their point of view; otherwise children simply absorb those of peers or the press. Parents should tell their children, “I want you to be able to talk about it if someone is mean or treats you unfairly because of [the color of your skin, your religion, your sex, your disability, etc.]. You might feel helpless, or angry, which is natural. We need to talk about this so you can feel strong. Then we can plan on what we are going to do.” The “sandwich” method of “ask-give information-ask what they think” can encourage discussion and correct misperceptions.
Racist policies have succeeded partly by adult “bullies” dehumanizing the “other.” Most children can consider someone else’s point of view by 4½ years old, shaped with adult help. Parents can begin by telling babies, “That hurts, doesn’t it?” asking toddlers and older, “How would you feel if ... [someone called you a name just because of having red hair]?” or “How do you think she feels when ... [someone pushes her out of line because she wears certain clothes]?” in cases of grabbing, not sharing, hitting, bullying, etc. Older children and teens can analyze more abstract situations when asked, “What if you were the one who ... [got expelled for mumbling about the teacher]?” or “What if that were your sister?” or “How would the world be if everyone ... [got a chance to go to college]?” We can encourage parents to propose these mental exercises to build the child’s perspective-taking while conveying their opinions.
Experiences, including through media, may increase or decrease fear; the child needs to have a supportive person moderating the exposure, providing a positive interpretation, and protecting the child from overwhelm, if needed.
Experiences are insufficient for developing anti-racist attitudes; listening and talking are needed. The first step is to ask children about what they notice, think, and feel about situations reflecting racism, especially as they lack words for these complicated observations. There are television, Internet, and newspaper examples of both racism and anti-racism that can be fruitfully discussed. We can recommend watching or reading together, and asking questions such as, “Why do you think they are shouting [protesting]?” “How do you think the [victim, police] felt?” or “What do you think should be done about this?”
It is important to acknowledge the child’s confusion, fear, anxiety, sadness, or anger as normal and appropriate, not dismissing, too quickly reassuring, or changing the subject, even though it’s uncomfortable.
Physicians and nurse practitioners can make a difference by being aware of our privilege and biases, being open, modeling discussion, screening for impact, offering strategies, advocating with schools, and providing resources such as therapy or legal counsel, as for other social determinants of health.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (https://www.site.chadis.com/). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Can we help our pediatric patients with the complicated problems of racism, especially if we are privileged (and even white) professionals? We may not have experienced discrimination, but we can still advise and address it. Racist discrimination, fear, trauma, or distress may produce or exacerbate conditions we are treating.
Three levels of racism impact children’s health and health care: “structural or institutional” policies that influence social determinants of health; “personally mediated” differential treatment based on assumptions about one’s abilities, motives, or intents; and the resulting “internalization” of stereotypes into one’s identity, undermining confidence, self-esteem, and mental health. We can help advocate about structural racism and ensure equity within our offices, but how best to counsel the families and children themselves?
Racism includes actions of “assigning value based on the social interpretation of how a person looks” (Ethn Dis. 2008;18[4]:496-504). “Social interpretations” develop from an early age. Newborns detect differences in appearance and may startle or cry seeing a parent’s drastic haircut or new hat. Parents generally know to use soothing words and tone, bring the difference into view gradually, smile and comfort the child, and explain the change; these are good skills for later, too. Infants notice skin color, which, unlike clothes, is a stable feature by which to recognize parents. Social interpretation of these differences is cued from the parents’ feelings and reactions. Adults naturally transmit biases from their own past unless they work to dampen them. If the parent was taught to regard “other” as negative or is generally fearful, the child mirrors this. Working to reduce racism thus requires parents (and professionals) to examine their prejudices to be able to convey positive or neutral reactions to people who are different. Parents need to show curiosity, positive affect, and comfort about people who are different, and do well to seek contact and friendships with people from other groups and include their children in these relationships. We can encourage this outreach plus ensure diversity and respectful interactions in our offices.
Children from age 3 years value fairness and are upset seeing others treated unfairly – easily understanding “not fair” or “mean.” If the person being hurt is like them in race, ethnicity, religion, gender, or sexual preference, they also fear for themselves, family, and friends. Balance is needed in discussing racism to avoid increasing fear or overpromising as risks are real and solutions difficult. Children look to adults for understanding and evidence of action to feel safer, rather than helpless. We should state that leaders are working on “making the rules more fair,” ensuring that people “won’t be allowed do it again,” and “teaching that everyone deserves respect.” Even better, parents and children can generate ideas about child actions, giving them some power as an antidote to anxiety. Age-related possibilities might include drawing a picture of people getting along, talking at show-and-tell, writing a note to officials, making a protest sign, posting thoughts on Facebook, or protesting.
With age, the culture increasingly influences a child’s attitudes. Children see lots of teasing and bullying based on differences from being overweight or wearing glasses, to skin color. It is helpful to interpret for children that bullies are insecure, or sometimes have been hurt, and they put other people down to feel better than someone else. Thinking about racist acts this way may reduce the desire for revenge and a cycle of aggression. Effective anti-bullying programs help children recognize bullying, see it as an emergency that requires their action, tell adults, and take action. This action could be surrounding the bully, standing tall, making eye contact, having a dismissive retort, or asking questions that require the bully to think, such as “What do you want to happen by doing this?” We can coach our patients and their parents on these principles as well as advising schools.
Children need to be told that those being put down or held down – especially those like them – have strengths; have made discoveries; have produced writings, art, and music; have shown military bravery, moral leadership, and resistance to discrimination, but it is not the time to show strength when confronted by a gun or police. We can use and arm parents with examples to discuss strengths and accomplishments to help buffer the child from internalization of racist stereotypes. Children need positive role models who look like them; parents can seek out diverse professionals in their children’s lives, such as dentists, doctors, teachers, clergy, mentors, or coaches. We, and parents, can ensure that dolls and books are available, and that the children’s shows, movies, and video games are watched together and include diverse people doing good or brave things. These exposures also are key to all children becoming anti-racist.
Parents can be advised to initiate discussion of racism because children, detecting adult discomfort, may avoid the topic. We can encourage families to give their point of view; otherwise children simply absorb those of peers or the press. Parents should tell their children, “I want you to be able to talk about it if someone is mean or treats you unfairly because of [the color of your skin, your religion, your sex, your disability, etc.]. You might feel helpless, or angry, which is natural. We need to talk about this so you can feel strong. Then we can plan on what we are going to do.” The “sandwich” method of “ask-give information-ask what they think” can encourage discussion and correct misperceptions.
Racist policies have succeeded partly by adult “bullies” dehumanizing the “other.” Most children can consider someone else’s point of view by 4½ years old, shaped with adult help. Parents can begin by telling babies, “That hurts, doesn’t it?” asking toddlers and older, “How would you feel if ... [someone called you a name just because of having red hair]?” or “How do you think she feels when ... [someone pushes her out of line because she wears certain clothes]?” in cases of grabbing, not sharing, hitting, bullying, etc. Older children and teens can analyze more abstract situations when asked, “What if you were the one who ... [got expelled for mumbling about the teacher]?” or “What if that were your sister?” or “How would the world be if everyone ... [got a chance to go to college]?” We can encourage parents to propose these mental exercises to build the child’s perspective-taking while conveying their opinions.
Experiences, including through media, may increase or decrease fear; the child needs to have a supportive person moderating the exposure, providing a positive interpretation, and protecting the child from overwhelm, if needed.
Experiences are insufficient for developing anti-racist attitudes; listening and talking are needed. The first step is to ask children about what they notice, think, and feel about situations reflecting racism, especially as they lack words for these complicated observations. There are television, Internet, and newspaper examples of both racism and anti-racism that can be fruitfully discussed. We can recommend watching or reading together, and asking questions such as, “Why do you think they are shouting [protesting]?” “How do you think the [victim, police] felt?” or “What do you think should be done about this?”
It is important to acknowledge the child’s confusion, fear, anxiety, sadness, or anger as normal and appropriate, not dismissing, too quickly reassuring, or changing the subject, even though it’s uncomfortable.
Physicians and nurse practitioners can make a difference by being aware of our privilege and biases, being open, modeling discussion, screening for impact, offering strategies, advocating with schools, and providing resources such as therapy or legal counsel, as for other social determinants of health.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (https://www.site.chadis.com/). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Can we help our pediatric patients with the complicated problems of racism, especially if we are privileged (and even white) professionals? We may not have experienced discrimination, but we can still advise and address it. Racist discrimination, fear, trauma, or distress may produce or exacerbate conditions we are treating.
Three levels of racism impact children’s health and health care: “structural or institutional” policies that influence social determinants of health; “personally mediated” differential treatment based on assumptions about one’s abilities, motives, or intents; and the resulting “internalization” of stereotypes into one’s identity, undermining confidence, self-esteem, and mental health. We can help advocate about structural racism and ensure equity within our offices, but how best to counsel the families and children themselves?
Racism includes actions of “assigning value based on the social interpretation of how a person looks” (Ethn Dis. 2008;18[4]:496-504). “Social interpretations” develop from an early age. Newborns detect differences in appearance and may startle or cry seeing a parent’s drastic haircut or new hat. Parents generally know to use soothing words and tone, bring the difference into view gradually, smile and comfort the child, and explain the change; these are good skills for later, too. Infants notice skin color, which, unlike clothes, is a stable feature by which to recognize parents. Social interpretation of these differences is cued from the parents’ feelings and reactions. Adults naturally transmit biases from their own past unless they work to dampen them. If the parent was taught to regard “other” as negative or is generally fearful, the child mirrors this. Working to reduce racism thus requires parents (and professionals) to examine their prejudices to be able to convey positive or neutral reactions to people who are different. Parents need to show curiosity, positive affect, and comfort about people who are different, and do well to seek contact and friendships with people from other groups and include their children in these relationships. We can encourage this outreach plus ensure diversity and respectful interactions in our offices.
Children from age 3 years value fairness and are upset seeing others treated unfairly – easily understanding “not fair” or “mean.” If the person being hurt is like them in race, ethnicity, religion, gender, or sexual preference, they also fear for themselves, family, and friends. Balance is needed in discussing racism to avoid increasing fear or overpromising as risks are real and solutions difficult. Children look to adults for understanding and evidence of action to feel safer, rather than helpless. We should state that leaders are working on “making the rules more fair,” ensuring that people “won’t be allowed do it again,” and “teaching that everyone deserves respect.” Even better, parents and children can generate ideas about child actions, giving them some power as an antidote to anxiety. Age-related possibilities might include drawing a picture of people getting along, talking at show-and-tell, writing a note to officials, making a protest sign, posting thoughts on Facebook, or protesting.
With age, the culture increasingly influences a child’s attitudes. Children see lots of teasing and bullying based on differences from being overweight or wearing glasses, to skin color. It is helpful to interpret for children that bullies are insecure, or sometimes have been hurt, and they put other people down to feel better than someone else. Thinking about racist acts this way may reduce the desire for revenge and a cycle of aggression. Effective anti-bullying programs help children recognize bullying, see it as an emergency that requires their action, tell adults, and take action. This action could be surrounding the bully, standing tall, making eye contact, having a dismissive retort, or asking questions that require the bully to think, such as “What do you want to happen by doing this?” We can coach our patients and their parents on these principles as well as advising schools.
Children need to be told that those being put down or held down – especially those like them – have strengths; have made discoveries; have produced writings, art, and music; have shown military bravery, moral leadership, and resistance to discrimination, but it is not the time to show strength when confronted by a gun or police. We can use and arm parents with examples to discuss strengths and accomplishments to help buffer the child from internalization of racist stereotypes. Children need positive role models who look like them; parents can seek out diverse professionals in their children’s lives, such as dentists, doctors, teachers, clergy, mentors, or coaches. We, and parents, can ensure that dolls and books are available, and that the children’s shows, movies, and video games are watched together and include diverse people doing good or brave things. These exposures also are key to all children becoming anti-racist.
Parents can be advised to initiate discussion of racism because children, detecting adult discomfort, may avoid the topic. We can encourage families to give their point of view; otherwise children simply absorb those of peers or the press. Parents should tell their children, “I want you to be able to talk about it if someone is mean or treats you unfairly because of [the color of your skin, your religion, your sex, your disability, etc.]. You might feel helpless, or angry, which is natural. We need to talk about this so you can feel strong. Then we can plan on what we are going to do.” The “sandwich” method of “ask-give information-ask what they think” can encourage discussion and correct misperceptions.
Racist policies have succeeded partly by adult “bullies” dehumanizing the “other.” Most children can consider someone else’s point of view by 4½ years old, shaped with adult help. Parents can begin by telling babies, “That hurts, doesn’t it?” asking toddlers and older, “How would you feel if ... [someone called you a name just because of having red hair]?” or “How do you think she feels when ... [someone pushes her out of line because she wears certain clothes]?” in cases of grabbing, not sharing, hitting, bullying, etc. Older children and teens can analyze more abstract situations when asked, “What if you were the one who ... [got expelled for mumbling about the teacher]?” or “What if that were your sister?” or “How would the world be if everyone ... [got a chance to go to college]?” We can encourage parents to propose these mental exercises to build the child’s perspective-taking while conveying their opinions.
Experiences, including through media, may increase or decrease fear; the child needs to have a supportive person moderating the exposure, providing a positive interpretation, and protecting the child from overwhelm, if needed.
Experiences are insufficient for developing anti-racist attitudes; listening and talking are needed. The first step is to ask children about what they notice, think, and feel about situations reflecting racism, especially as they lack words for these complicated observations. There are television, Internet, and newspaper examples of both racism and anti-racism that can be fruitfully discussed. We can recommend watching or reading together, and asking questions such as, “Why do you think they are shouting [protesting]?” “How do you think the [victim, police] felt?” or “What do you think should be done about this?”
It is important to acknowledge the child’s confusion, fear, anxiety, sadness, or anger as normal and appropriate, not dismissing, too quickly reassuring, or changing the subject, even though it’s uncomfortable.
Physicians and nurse practitioners can make a difference by being aware of our privilege and biases, being open, modeling discussion, screening for impact, offering strategies, advocating with schools, and providing resources such as therapy or legal counsel, as for other social determinants of health.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (https://www.site.chadis.com/). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Consider the stresses experienced by LGBTQ people of color
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Perfect storm of SARS-CoV-2 during flu season
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
If you reopen it, will they come?
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Perspectives of a black physician in the time of two pandemics
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
“Hey there – just checking on you and letting you know I’m thinking of you."
"I know words don't suffice right now. You are in my thoughts."
"If there's any way that I can be of support or if there's something you need, just let me know."
The texts and emails have come in waves. Pinging into my already distracted headspace when, like them, I’m supposed to be focused on a Zoom or WebEx department meeting. These somber reminders underscore what I have known for years but struggled to describe with each new “justice for” hashtag accompanying the name of the latest unarmed black person to die. This is grief.
With every headline in prior years, as black Americans we have usually found solace in our collective fellowship of suffering. Social media timelines become flooded with our own amen choirs and outrage along with words of comfort and inspiration. We remind ourselves of the prior atrocities survived by our people. And like them, we vow to rally; clinging to one other and praying to make it to shore. Though intermittently joined by a smattering of allies, our suffering has mostly been a private, repetitive mourning.
The two pandemics
The year 2020 ushered in a new decade along with the novel SARS-CoV2 (COVID-19) global pandemic. In addition to the thousands of lives that have been lost in the United States alone, COVID-19 brought with it a disruption of life in ways never seen by most generations. Schools and businesses were closed to mitigate spread. Mandatory shelter-in-place orders coupled with physical distancing recommendations limited human interactions and canceled everything from hospital visitations to graduations, intergenerational family gatherings, conferences, and weddings. As the data expanded, it quickly became apparent that minorities, particularly black Americans, shouldered a disproportionate burden of COVID-19. Known health disparities were amplified.
While caring for our patients as black physicians in the time of coronavirus, silently we mourned again. The connection and trust once found through racial concordance was now masked figuratively and literally by personal protective equipment (PPE). We ignored the sting of intimations that the staggering numbers of African Americans hospitalized and dying from COVID-19 could be explained by lack of discipline or, worse, genetic differences by race. Years of disenfranchisement and missed economic opportunities forced large numbers of our patients and loved ones out on the front lines to do essential jobs – but without the celebratory cheers or fanfare enjoyed by others. Frantic phone calls from family and acquaintances interrupted our quiet drives home from emotionally grueling shifts in the hospital – each conversation serving as our personal evidence of COVID-19 and her ruthless ravage of the black community. Add to this trying to serve as cultural bridges between the complexities of medical distrust and patient advocacy along with wrestling with our own vulnerability as potential COVID-19 patients, these have been overwhelming times to say the least.
Then came the acute decompensation of the chronic racism we’d always known in the form of three recent killings of more unarmed African Americans. On March 13, 2020, 26-year-old Breonna Taylor was shot after police forcibly entered her home after midnight on a “no knock” warrant. The story was buried in the news of COVID-19 – but we knew. Later we’d learn that 26-year-old Ahmaud Arbery was shot and killed by armed neighbors while running through a Brunswick, Georgia, neighborhood. His death on Feb. 23, 2020, initially yielded no criminal charges. Then, on May 25, 2020, George Floyd, a 46-year-old father arrested for suspected use of a counterfeit $20 bill, died after a law enforcement official kneeled with his full body weight upon Floyd’s neck for more than 8 minutes. The deaths of Arbery and Floyd were captured by cell phone cameras which, aided by social media, quickly reached the eyes of the entire world.
At first, it seemed plausible that this would be like it always has been. A black mother would stand before a podium filled with multiple microphones crying out in anguish. She would be flanked by community leaders and attorneys demanding justice. Hashtags would be formed. Our people would stand up or kneel down in solidarity – holding fast to our historic resilience. Evanescent allies would appear with signs on lawns and held high over heads. A few weeks would pass by and things would go back to normal. Black people would be left with what always remains: heads bowed and praying at dinner tables petitioning a higher power for protection followed by reaffirmations of what, if anything, could be done to keep our own mamas away from that podium. We’ve learned to treat the grief of racism as endemic to us alone, knowing that it has been a pandemic all along.
Dr. Manning is a professor of medicine and the associate vice chair of diversity, equity, and inclusion at Emory University in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. To read the full version of this article, visit the Journal of Hospital Medicine, where it first appeared (doi: 10.12788/jhm.3481).
Time for grit and resilience
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
Medical ethics in the time of COVID-19
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
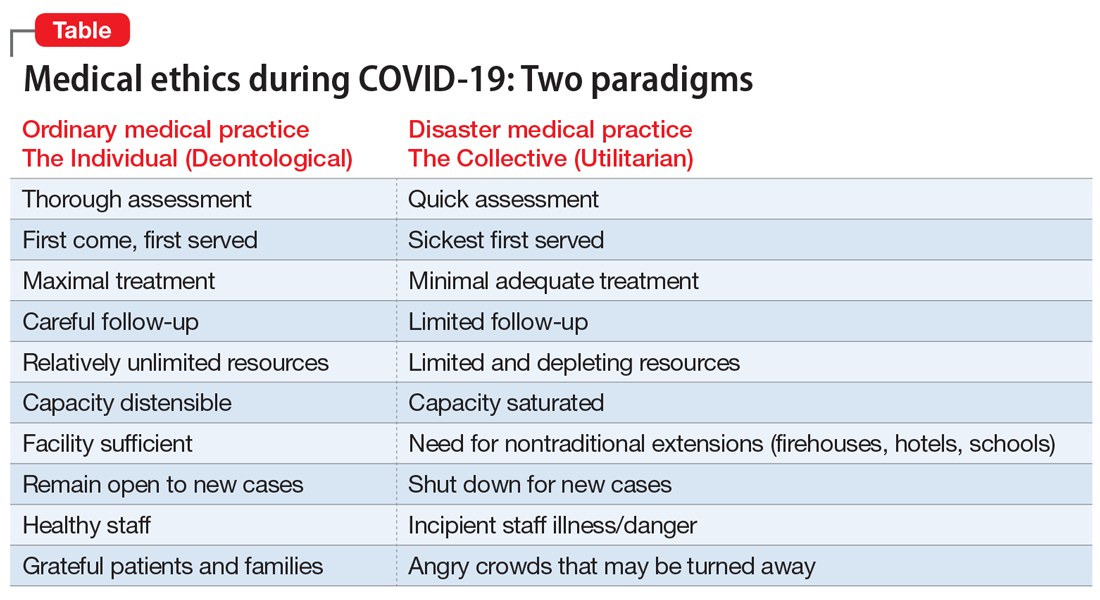
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
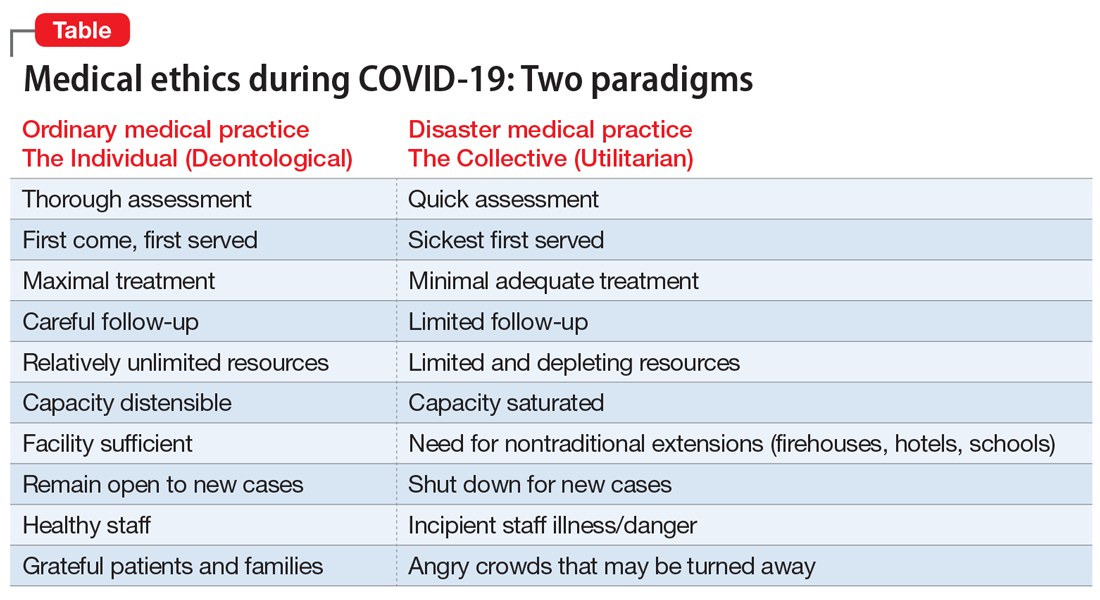
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
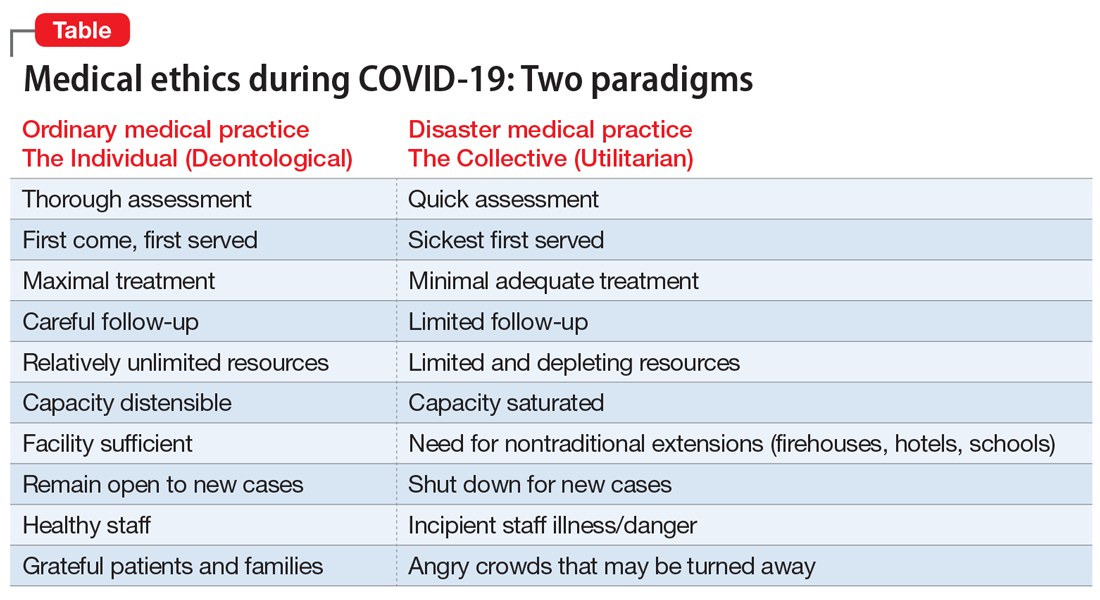
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.





















