User login
Inflammation and immunity troubles top long-COVID suspect list
“I think that it’s a much more complex picture than just inflammation, or just autoimmunity, or just immune dysregulation. And it’s probably a combination of all three causing a cascade of effects that then manifests itself as brain fog, or shortness of breath, or chronic fatigue,” says Alexander Truong, MD, a pulmonologist and assistant professor at Emory University, Atlanta, who also runs a long-COVID clinic.
Long COVID, post–COVID-19 condition, and postacute sequelae of SARS-CoV-2 (PASC) are among the terms used by the National Institutes of Health to describe the long-term health issues faced by an estimated 10%-30% of people infected with COVID-19. Symptoms – as many as 200 – can range from inconvenient to crippling, damage multiple organ systems, come and go, and relapse. Long COVID increases the risk of worsening existing health problems and triggering new ones, including cardiovascular disease and type 2 diabetes.
So far, research suggests there is no single cause, condition, or disease that explains why some people have an extensive range of symptoms long after the early COVID-19 infection has cleared up. Many experts believe some combination of biological processes – including the virus hanging around in our bodies, inflammation, autoimmunity, tiny blood clots, immune system problems, and even the reactivation of dormant viruses such as the Epstein-Barr virus – could be the culprit, a theory also supported by a comprehensive and in-depth review of long-COVID studies published in the journal Nature Reviews Microbiology.
“It’s become clear over the last couple of years that there are different [symptoms] of long COVID … that cannot all be lumped together,” says Michael Peluso, MD, an assistant professor of medicine and an infectious diseases doctor at the University of California, San Francisco.
Inflammation and a virus that hangs around
Multiple studies have shown that the virus or pieces of it can remain in many parts of the body, including the kidneys, brain, heart, and gastrointestinal system, long after the early infection.
“One major question that I think is the area of most intense investigation now is whether there is viral persistence that is driving immune dysregulation and therefore symptoms,” says Dr. Peluso.
A small Harvard University study, for example, found evidence that reservoirs of the coronavirus could linger in patients up to a year after they’re first diagnosed.
An earlier German study found that patients with post-COVID-19 symptoms had higher levels of three cytokines – small proteins that tell the body’s immune system what to do and are involved in the growth and activity of immune system cells and blood cells. Researchers said the results supported the theory that there is persistent reprogramming of certain immune cells, and that the uncontrolled “self-fueled hyperinflammation” during the early COVID-19 infection can become continued immune cell disruption that drives long-COVID symptoms.
“Long COVID is more likely due to either an inflammatory response by the body or reservoirs of virus that the body is still trying to clear … and the symptoms we’re seeing are a side effect of that,” says Rainu Kaushal, MD, senior associate dean for clinical research at Weill Cornell Medicine in New York.
Australian researchers found that immune system recovery appeared different, compared with those who were infected with other common coronaviruses.
These findings also support concerns that some experts express over the long-term risks of COVID-19 infections in general, but especially repeat infections.
“Anything that kind of revs up inflammation in the body can boil that pot over and make the symptoms worse. That’s very easily an infection or some other insult to the body. So that’s the generalized hypothesis as to why insults to the body may worsen the symptoms,” says Dr. Truong.
An autoimmune condition?
But inflammation alone does not fully explain post–COVID-19 problems.
Dr. Truong and his team, for example, have been documenting inflammatory markers in patients at the post-COVID clinic he cofounded more than 2 years ago at Emory Executive Park in Atlanta. When the clinic was first launched, high-dose nonsteroidal anti-inflammatory drugs – including ibuprofen – and prednisone were prescribed to long-COVID patients.
“It didn’t make a difference at all for any of these folks,” he says, adding that there are signs that autoimmunity is at play. But he cautions that it is still too early to suggest treating long-COVID patients with medications used for other autoimmune conditions.
In autoimmune conditions such as rheumatoid arthritis, lupus, and type 1 diabetes, a person’s immune system can’t tell normal cells from foreign pathogens and attacks healthy cells. There is typically no single diagnostic test, and many share similar symptoms, making detection and diagnosis potentially difficult, according to Johns Hopkins Medicine.
A small study published in the journal Science Translational Medicine found that, among patients who failed to regain their sense of smell long after their initial infection, there was inflammation in the nose tissue where smell nerve cells are found, even though no detectable virus remained. Fewer olfactory sensory neurons were seen, as well – findings that researchers said resembled some kind of “autoimmune-like process.”
Meanwhile, scientists in Canada found signs of autoimmunity in blood samples taken from patients who still had fatigue and shortness of breath after their initial COVID-19 infection. Two specific proteins were present a year after infection in up to 30% of patients, many of whom still had shortness of breath and fatigue, the researchers reported in the Jan. 1 issue of the European Respiratory Journal. These patients had been healthy and had no autoimmune condition or other diseases before they were infected.
Immune system problems
A number of studies have suggested that a problematic immune response could also explain why symptoms persist for some people.
Researchers in France, for example, found that the immune response problems in those with severe COVID-19 infections caused exaggerated or uncontrolled formation of a type of bug-fighting defense mechanism called a neutrophil extracellular trap (NET), which in turn triggers harmful inflammation that can result in multiorgan damage. These traps are netlike structures made from fibers composed mostly of DNA strings that bind, or trap, pathogens.
Long COVID is not like an acute infectious disease, says Alexander Charney, MD, PhD, the lead principal investigator of the RECOVER adult cohort at Mount Sinai in New York, and an associate professor at Icahn School of Medicine at Mount Sinai. It is more similar to other complex chronic diseases that have taken decades to understand, such as heart disease, mental illness, and rheumatologic diseases, he says.
Biomarkers and blood clots
Scientists are homing in on biomarkers, or detectable and measurable traits – in this case, molecular indicators – that can make diagnosing long COVID easier and give better direction for treatment. These biomarkers are also key to helping sort out the complex biology of long COVID.
In one study, data from blood samples taken from hundreds of hospitalized COVID-19 patients suggests changes are happening at the molecular level during initial severe infections. These changes may be tied to the development of longer-term symptoms, according to the study by Dr. Charney and his team at Mount Sinai published in Nature Medicine
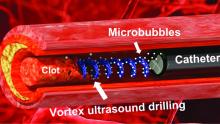
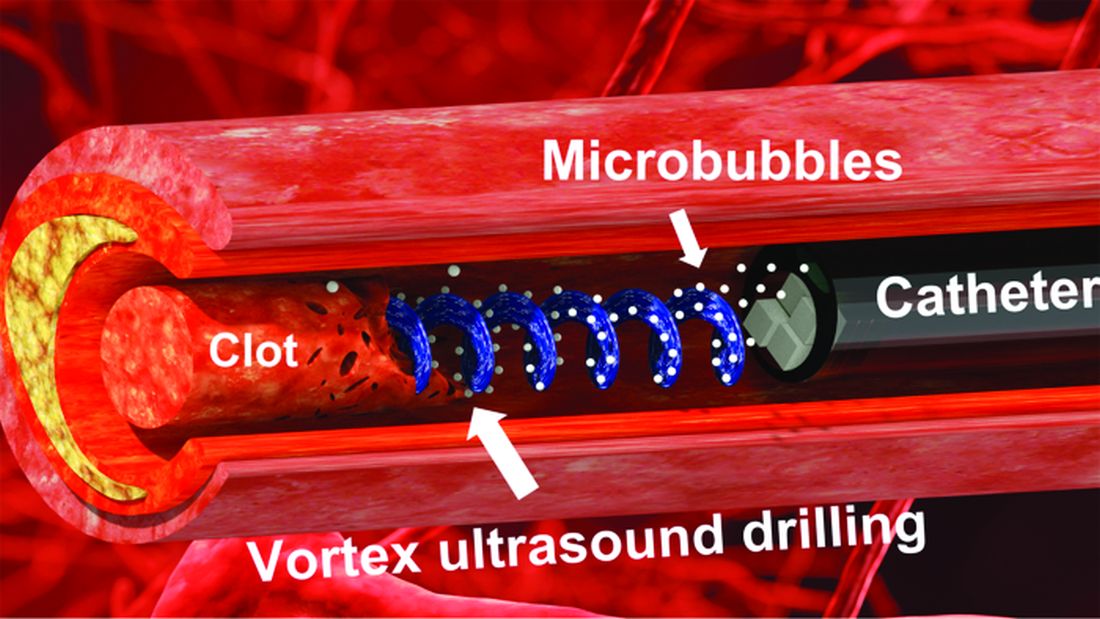
Blood clotting issues have also been detected in long COVID patients. At least one study found signs that long-COVID patients had higher levels of a type of auto-antibody linked to the abnormal formation of clots. Researchers suspect that tiny, persistent microclots – undetectable via regular pathology tests – may be cutting off oxygen flow to tissue by blocking capillaries – and could explain many of the post-COVID symptoms described by patients.
While enormous progress has been made toward understanding long COVID, the research is still considered early and faces many challenges, including varying criteria used to define the condition, the types and quality of data used, differences in how patients are defined and recruited, and the small size of many studies. Some research also appears to conflict with other studies. And while there are specialized tools for diagnosing some aspects of the condition, standard tests often don’t detect many of the signs seen in long-COVID patients. But given the urgency and global scale of the problem, experts say more funding and support should be prioritized.
“People are suffering now, and they want answers now. ... It’s not like with COVID, where the path towards a great and meaningful solution to this unbelievable problem was clear – we need a vaccine,” says Dr. Charney.
“It’s going to be a long haul to figure out what is going on.”
A version of this article originally appeared on WebMD.com.
“I think that it’s a much more complex picture than just inflammation, or just autoimmunity, or just immune dysregulation. And it’s probably a combination of all three causing a cascade of effects that then manifests itself as brain fog, or shortness of breath, or chronic fatigue,” says Alexander Truong, MD, a pulmonologist and assistant professor at Emory University, Atlanta, who also runs a long-COVID clinic.
Long COVID, post–COVID-19 condition, and postacute sequelae of SARS-CoV-2 (PASC) are among the terms used by the National Institutes of Health to describe the long-term health issues faced by an estimated 10%-30% of people infected with COVID-19. Symptoms – as many as 200 – can range from inconvenient to crippling, damage multiple organ systems, come and go, and relapse. Long COVID increases the risk of worsening existing health problems and triggering new ones, including cardiovascular disease and type 2 diabetes.
So far, research suggests there is no single cause, condition, or disease that explains why some people have an extensive range of symptoms long after the early COVID-19 infection has cleared up. Many experts believe some combination of biological processes – including the virus hanging around in our bodies, inflammation, autoimmunity, tiny blood clots, immune system problems, and even the reactivation of dormant viruses such as the Epstein-Barr virus – could be the culprit, a theory also supported by a comprehensive and in-depth review of long-COVID studies published in the journal Nature Reviews Microbiology.
“It’s become clear over the last couple of years that there are different [symptoms] of long COVID … that cannot all be lumped together,” says Michael Peluso, MD, an assistant professor of medicine and an infectious diseases doctor at the University of California, San Francisco.
Inflammation and a virus that hangs around
Multiple studies have shown that the virus or pieces of it can remain in many parts of the body, including the kidneys, brain, heart, and gastrointestinal system, long after the early infection.
“One major question that I think is the area of most intense investigation now is whether there is viral persistence that is driving immune dysregulation and therefore symptoms,” says Dr. Peluso.
A small Harvard University study, for example, found evidence that reservoirs of the coronavirus could linger in patients up to a year after they’re first diagnosed.
An earlier German study found that patients with post-COVID-19 symptoms had higher levels of three cytokines – small proteins that tell the body’s immune system what to do and are involved in the growth and activity of immune system cells and blood cells. Researchers said the results supported the theory that there is persistent reprogramming of certain immune cells, and that the uncontrolled “self-fueled hyperinflammation” during the early COVID-19 infection can become continued immune cell disruption that drives long-COVID symptoms.
“Long COVID is more likely due to either an inflammatory response by the body or reservoirs of virus that the body is still trying to clear … and the symptoms we’re seeing are a side effect of that,” says Rainu Kaushal, MD, senior associate dean for clinical research at Weill Cornell Medicine in New York.
Australian researchers found that immune system recovery appeared different, compared with those who were infected with other common coronaviruses.
These findings also support concerns that some experts express over the long-term risks of COVID-19 infections in general, but especially repeat infections.
“Anything that kind of revs up inflammation in the body can boil that pot over and make the symptoms worse. That’s very easily an infection or some other insult to the body. So that’s the generalized hypothesis as to why insults to the body may worsen the symptoms,” says Dr. Truong.
An autoimmune condition?
But inflammation alone does not fully explain post–COVID-19 problems.
Dr. Truong and his team, for example, have been documenting inflammatory markers in patients at the post-COVID clinic he cofounded more than 2 years ago at Emory Executive Park in Atlanta. When the clinic was first launched, high-dose nonsteroidal anti-inflammatory drugs – including ibuprofen – and prednisone were prescribed to long-COVID patients.
“It didn’t make a difference at all for any of these folks,” he says, adding that there are signs that autoimmunity is at play. But he cautions that it is still too early to suggest treating long-COVID patients with medications used for other autoimmune conditions.
In autoimmune conditions such as rheumatoid arthritis, lupus, and type 1 diabetes, a person’s immune system can’t tell normal cells from foreign pathogens and attacks healthy cells. There is typically no single diagnostic test, and many share similar symptoms, making detection and diagnosis potentially difficult, according to Johns Hopkins Medicine.
A small study published in the journal Science Translational Medicine found that, among patients who failed to regain their sense of smell long after their initial infection, there was inflammation in the nose tissue where smell nerve cells are found, even though no detectable virus remained. Fewer olfactory sensory neurons were seen, as well – findings that researchers said resembled some kind of “autoimmune-like process.”
Meanwhile, scientists in Canada found signs of autoimmunity in blood samples taken from patients who still had fatigue and shortness of breath after their initial COVID-19 infection. Two specific proteins were present a year after infection in up to 30% of patients, many of whom still had shortness of breath and fatigue, the researchers reported in the Jan. 1 issue of the European Respiratory Journal. These patients had been healthy and had no autoimmune condition or other diseases before they were infected.
Immune system problems
A number of studies have suggested that a problematic immune response could also explain why symptoms persist for some people.
Researchers in France, for example, found that the immune response problems in those with severe COVID-19 infections caused exaggerated or uncontrolled formation of a type of bug-fighting defense mechanism called a neutrophil extracellular trap (NET), which in turn triggers harmful inflammation that can result in multiorgan damage. These traps are netlike structures made from fibers composed mostly of DNA strings that bind, or trap, pathogens.
Long COVID is not like an acute infectious disease, says Alexander Charney, MD, PhD, the lead principal investigator of the RECOVER adult cohort at Mount Sinai in New York, and an associate professor at Icahn School of Medicine at Mount Sinai. It is more similar to other complex chronic diseases that have taken decades to understand, such as heart disease, mental illness, and rheumatologic diseases, he says.
Biomarkers and blood clots
Scientists are homing in on biomarkers, or detectable and measurable traits – in this case, molecular indicators – that can make diagnosing long COVID easier and give better direction for treatment. These biomarkers are also key to helping sort out the complex biology of long COVID.
In one study, data from blood samples taken from hundreds of hospitalized COVID-19 patients suggests changes are happening at the molecular level during initial severe infections. These changes may be tied to the development of longer-term symptoms, according to the study by Dr. Charney and his team at Mount Sinai published in Nature Medicine
Blood clotting issues have also been detected in long COVID patients. At least one study found signs that long-COVID patients had higher levels of a type of auto-antibody linked to the abnormal formation of clots. Researchers suspect that tiny, persistent microclots – undetectable via regular pathology tests – may be cutting off oxygen flow to tissue by blocking capillaries – and could explain many of the post-COVID symptoms described by patients.
While enormous progress has been made toward understanding long COVID, the research is still considered early and faces many challenges, including varying criteria used to define the condition, the types and quality of data used, differences in how patients are defined and recruited, and the small size of many studies. Some research also appears to conflict with other studies. And while there are specialized tools for diagnosing some aspects of the condition, standard tests often don’t detect many of the signs seen in long-COVID patients. But given the urgency and global scale of the problem, experts say more funding and support should be prioritized.
“People are suffering now, and they want answers now. ... It’s not like with COVID, where the path towards a great and meaningful solution to this unbelievable problem was clear – we need a vaccine,” says Dr. Charney.
“It’s going to be a long haul to figure out what is going on.”
A version of this article originally appeared on WebMD.com.
“I think that it’s a much more complex picture than just inflammation, or just autoimmunity, or just immune dysregulation. And it’s probably a combination of all three causing a cascade of effects that then manifests itself as brain fog, or shortness of breath, or chronic fatigue,” says Alexander Truong, MD, a pulmonologist and assistant professor at Emory University, Atlanta, who also runs a long-COVID clinic.
Long COVID, post–COVID-19 condition, and postacute sequelae of SARS-CoV-2 (PASC) are among the terms used by the National Institutes of Health to describe the long-term health issues faced by an estimated 10%-30% of people infected with COVID-19. Symptoms – as many as 200 – can range from inconvenient to crippling, damage multiple organ systems, come and go, and relapse. Long COVID increases the risk of worsening existing health problems and triggering new ones, including cardiovascular disease and type 2 diabetes.
So far, research suggests there is no single cause, condition, or disease that explains why some people have an extensive range of symptoms long after the early COVID-19 infection has cleared up. Many experts believe some combination of biological processes – including the virus hanging around in our bodies, inflammation, autoimmunity, tiny blood clots, immune system problems, and even the reactivation of dormant viruses such as the Epstein-Barr virus – could be the culprit, a theory also supported by a comprehensive and in-depth review of long-COVID studies published in the journal Nature Reviews Microbiology.
“It’s become clear over the last couple of years that there are different [symptoms] of long COVID … that cannot all be lumped together,” says Michael Peluso, MD, an assistant professor of medicine and an infectious diseases doctor at the University of California, San Francisco.
Inflammation and a virus that hangs around
Multiple studies have shown that the virus or pieces of it can remain in many parts of the body, including the kidneys, brain, heart, and gastrointestinal system, long after the early infection.
“One major question that I think is the area of most intense investigation now is whether there is viral persistence that is driving immune dysregulation and therefore symptoms,” says Dr. Peluso.
A small Harvard University study, for example, found evidence that reservoirs of the coronavirus could linger in patients up to a year after they’re first diagnosed.
An earlier German study found that patients with post-COVID-19 symptoms had higher levels of three cytokines – small proteins that tell the body’s immune system what to do and are involved in the growth and activity of immune system cells and blood cells. Researchers said the results supported the theory that there is persistent reprogramming of certain immune cells, and that the uncontrolled “self-fueled hyperinflammation” during the early COVID-19 infection can become continued immune cell disruption that drives long-COVID symptoms.
“Long COVID is more likely due to either an inflammatory response by the body or reservoirs of virus that the body is still trying to clear … and the symptoms we’re seeing are a side effect of that,” says Rainu Kaushal, MD, senior associate dean for clinical research at Weill Cornell Medicine in New York.
Australian researchers found that immune system recovery appeared different, compared with those who were infected with other common coronaviruses.
These findings also support concerns that some experts express over the long-term risks of COVID-19 infections in general, but especially repeat infections.
“Anything that kind of revs up inflammation in the body can boil that pot over and make the symptoms worse. That’s very easily an infection or some other insult to the body. So that’s the generalized hypothesis as to why insults to the body may worsen the symptoms,” says Dr. Truong.
An autoimmune condition?
But inflammation alone does not fully explain post–COVID-19 problems.
Dr. Truong and his team, for example, have been documenting inflammatory markers in patients at the post-COVID clinic he cofounded more than 2 years ago at Emory Executive Park in Atlanta. When the clinic was first launched, high-dose nonsteroidal anti-inflammatory drugs – including ibuprofen – and prednisone were prescribed to long-COVID patients.
“It didn’t make a difference at all for any of these folks,” he says, adding that there are signs that autoimmunity is at play. But he cautions that it is still too early to suggest treating long-COVID patients with medications used for other autoimmune conditions.
In autoimmune conditions such as rheumatoid arthritis, lupus, and type 1 diabetes, a person’s immune system can’t tell normal cells from foreign pathogens and attacks healthy cells. There is typically no single diagnostic test, and many share similar symptoms, making detection and diagnosis potentially difficult, according to Johns Hopkins Medicine.
A small study published in the journal Science Translational Medicine found that, among patients who failed to regain their sense of smell long after their initial infection, there was inflammation in the nose tissue where smell nerve cells are found, even though no detectable virus remained. Fewer olfactory sensory neurons were seen, as well – findings that researchers said resembled some kind of “autoimmune-like process.”
Meanwhile, scientists in Canada found signs of autoimmunity in blood samples taken from patients who still had fatigue and shortness of breath after their initial COVID-19 infection. Two specific proteins were present a year after infection in up to 30% of patients, many of whom still had shortness of breath and fatigue, the researchers reported in the Jan. 1 issue of the European Respiratory Journal. These patients had been healthy and had no autoimmune condition or other diseases before they were infected.
Immune system problems
A number of studies have suggested that a problematic immune response could also explain why symptoms persist for some people.
Researchers in France, for example, found that the immune response problems in those with severe COVID-19 infections caused exaggerated or uncontrolled formation of a type of bug-fighting defense mechanism called a neutrophil extracellular trap (NET), which in turn triggers harmful inflammation that can result in multiorgan damage. These traps are netlike structures made from fibers composed mostly of DNA strings that bind, or trap, pathogens.
Long COVID is not like an acute infectious disease, says Alexander Charney, MD, PhD, the lead principal investigator of the RECOVER adult cohort at Mount Sinai in New York, and an associate professor at Icahn School of Medicine at Mount Sinai. It is more similar to other complex chronic diseases that have taken decades to understand, such as heart disease, mental illness, and rheumatologic diseases, he says.
Biomarkers and blood clots
Scientists are homing in on biomarkers, or detectable and measurable traits – in this case, molecular indicators – that can make diagnosing long COVID easier and give better direction for treatment. These biomarkers are also key to helping sort out the complex biology of long COVID.
In one study, data from blood samples taken from hundreds of hospitalized COVID-19 patients suggests changes are happening at the molecular level during initial severe infections. These changes may be tied to the development of longer-term symptoms, according to the study by Dr. Charney and his team at Mount Sinai published in Nature Medicine
Blood clotting issues have also been detected in long COVID patients. At least one study found signs that long-COVID patients had higher levels of a type of auto-antibody linked to the abnormal formation of clots. Researchers suspect that tiny, persistent microclots – undetectable via regular pathology tests – may be cutting off oxygen flow to tissue by blocking capillaries – and could explain many of the post-COVID symptoms described by patients.
While enormous progress has been made toward understanding long COVID, the research is still considered early and faces many challenges, including varying criteria used to define the condition, the types and quality of data used, differences in how patients are defined and recruited, and the small size of many studies. Some research also appears to conflict with other studies. And while there are specialized tools for diagnosing some aspects of the condition, standard tests often don’t detect many of the signs seen in long-COVID patients. But given the urgency and global scale of the problem, experts say more funding and support should be prioritized.
“People are suffering now, and they want answers now. ... It’s not like with COVID, where the path towards a great and meaningful solution to this unbelievable problem was clear – we need a vaccine,” says Dr. Charney.
“It’s going to be a long haul to figure out what is going on.”
A version of this article originally appeared on WebMD.com.
Using live pigs in residency training sparks heated debate
Pigs have been long used in medical schools to teach surgical techniques and, more recently, in research trials and experimental xenotransplantation procedures. But
Just last month, the Physicians Committee for Responsible Medicine, a nonprofit group with a decades-long stance against the use of animals in medical education and research, placed billboards around the Portland, Ore., area demanding that Oregon Health and Science University stop using pigs to teach surgical residents.
Undergraduate medical programs no longer use live animals. But a small number of graduate medical education programs still use animals, predominantly pigs, to train physicians in subspecialties like internal medicine, emergency medicine, surgery, and anesthesiology, John Pippin, MD, FACC, director of academic affairs at PCRM, told this news organization.
Dr. Pippin says residents practice establishing emergency airways, inserting chest tubes, and accessing blood vessels on anesthetized pigs before euthanizing them.
Swine lab advocates say pigs make ideal training subjects because of their similarities to humans, including comparably sized organs like the heart, lungs, and kidneys. Pigs share about 85% of their DNA with people. Where pig skin alternatives may suffice for less invasive procedures, supporters say residents’ experiences with live tissue are irreplaceable.
In a statement, Sara Hottman, associate director of media relations at Oregon Health and Science University, told this news organization the school “only uses animal models in its surgical training program when nonanimal methods are inadequate or too dangerous for human participants.”
“We believe that the education and experience surgical trainees gain through the use of relevant animal models are essential to ensuring future surgeons have the knowledge and skills necessary to provide safe, high-quality care.”
Ms. Hottman also noted that the university continues to evaluate alternatives and looks forward to when nonanimal “surgical training methods are capable of faithfully modeling the complexity of a living system,” such as in the management of critical internal complications.
But Dr. Pippin argues that residents can gain sufficient expertise through simulators and hands-on training in the operating room, and that the differences between humans and pigs are too vast to provide meaningful clinical data or skills.
“Pigs have different genetic influences and very thick, tough skin,” he said. If you use the same pressure on a human that you learned on a pig, he added, “you’d slice right through the trachea. Whatever you think you find out in animals, you have to learn all over again with humans.”
Undergraduate medical education programs in the United States and Canada abandoned the practice of using live animals, including pigs, by 2016, with Johns Hopkins University, Baltimore, and the University of Tennessee, Chattanooga, last to announce their shift away from the controversial teaching model following campaigns by PCRM.
Today, most residency training programs have followed suit. Pippin said that pediatric residencies no longer use animals, and all trauma and anesthesiology programs have ceased such practices except two. Just 3% of emergency medicine programs continue to use animals, as do about 21% of surgical residencies, he said, based on PCRM’s latest surveys.
A public debate
Occasionally, PCRM goes public with a campaign against a residency program “if that’s the only way to win,” Dr. Pippin said.
In addition to billboards, the group has held protests, circulated petitions, and filed complaints with the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service, the entity responsible for overseeing the health and welfare of animals used in medical training and research.
In 2021, spurred by a complaint from PCRM, APHIS launched an investigation into the University of Cincinnati’s surgical residency program. At the time, a university spokesperson acknowledged the school’s limited use of pigs to train “highly-skilled, well-prepared surgeons in the most advanced, complex, real-world needs, procedures, and techniques,” adding that the training methods were endorsed by the American College of Surgeons and in compliance with federal guidelines.
Residency programs have caught the attention of state lawmakers, too. In 2020, bills introduced in both the Rhode Island House and Senate sought to ban the use of live animals in medical training when “there is an alternate teaching method that teaches the medical procedure or lesson without the use of an animal.” Violators would incur misdemeanor charges and monetary fines of up to $1,000 per animal.
The bills – backed by PCRM – targeted Brown University’s emergency medicine residency program, Providence, R.I., which sponsoring legislators said was the last program in New England still using the “outdated” and “unnecessary” method.
In testimony before lawmakers, the school said fewer than 15 pigs participate in the annual training, and faculty spoke about the benefits of the experience.
“If it was your brother or sister, or your mother or father who had to come in and get this procedure done, would you want the physician who’s doing it to be the one who does it for the very first time on a human being, on live tissue? Or do you want that provider to have only practiced on plastic and rubber?” said Nicholas Musisca, MD, an assistant program director with Brown University’s emergency medicine residency, NBC affiliate WJAR reported.
The bills have since stalled, and PCRM held a protest at Brown University in October 2022. In response, a university spokesperson told the Brown Daily Herald, “effective synthetic model alternatives simply do not exist for every complex medical procedure that an emergency physician must be prepared to perform,” including establishing an airway in adults and pediatric patients with severe facial trauma.
By the numbers
Annual reports from APHIS do not show the number of pigs dedicated solely to residency training. Instead, reporting indicates the number of animals “upon which experiments, teaching, research, surgery, or tests were conducted involving accompanying pain or distress to the animals and for which appropriate anesthetic, analgesic, or tranquilizing drugs were used.”
For fiscal year 2021 – the most recent data available – Oregon Health and Science University had 154 pigs under its control, while the University of Cincinnati and Brown University had 118 and 71 pigs, respectively, according to APHIS. Primates were more commonly used at Oregon Health and Science University and guinea pigs at the University of Cincinnati.
Similarly, the Association of American Medical Colleges supports the “use of animals to meet essential educational objectives [across] the medical education continuum. ... Further restrictions on the use of animals in biomedical and behavioral research and education threatens progress in health care and disease prevention.”
The debate will likely rage on. “The one thing we don’t do is give up,” Dr. Pippin said.
A version of this article originally appeared on Medscape.com.
Pigs have been long used in medical schools to teach surgical techniques and, more recently, in research trials and experimental xenotransplantation procedures. But
Just last month, the Physicians Committee for Responsible Medicine, a nonprofit group with a decades-long stance against the use of animals in medical education and research, placed billboards around the Portland, Ore., area demanding that Oregon Health and Science University stop using pigs to teach surgical residents.
Undergraduate medical programs no longer use live animals. But a small number of graduate medical education programs still use animals, predominantly pigs, to train physicians in subspecialties like internal medicine, emergency medicine, surgery, and anesthesiology, John Pippin, MD, FACC, director of academic affairs at PCRM, told this news organization.
Dr. Pippin says residents practice establishing emergency airways, inserting chest tubes, and accessing blood vessels on anesthetized pigs before euthanizing them.
Swine lab advocates say pigs make ideal training subjects because of their similarities to humans, including comparably sized organs like the heart, lungs, and kidneys. Pigs share about 85% of their DNA with people. Where pig skin alternatives may suffice for less invasive procedures, supporters say residents’ experiences with live tissue are irreplaceable.
In a statement, Sara Hottman, associate director of media relations at Oregon Health and Science University, told this news organization the school “only uses animal models in its surgical training program when nonanimal methods are inadequate or too dangerous for human participants.”
“We believe that the education and experience surgical trainees gain through the use of relevant animal models are essential to ensuring future surgeons have the knowledge and skills necessary to provide safe, high-quality care.”
Ms. Hottman also noted that the university continues to evaluate alternatives and looks forward to when nonanimal “surgical training methods are capable of faithfully modeling the complexity of a living system,” such as in the management of critical internal complications.
But Dr. Pippin argues that residents can gain sufficient expertise through simulators and hands-on training in the operating room, and that the differences between humans and pigs are too vast to provide meaningful clinical data or skills.
“Pigs have different genetic influences and very thick, tough skin,” he said. If you use the same pressure on a human that you learned on a pig, he added, “you’d slice right through the trachea. Whatever you think you find out in animals, you have to learn all over again with humans.”
Undergraduate medical education programs in the United States and Canada abandoned the practice of using live animals, including pigs, by 2016, with Johns Hopkins University, Baltimore, and the University of Tennessee, Chattanooga, last to announce their shift away from the controversial teaching model following campaigns by PCRM.
Today, most residency training programs have followed suit. Pippin said that pediatric residencies no longer use animals, and all trauma and anesthesiology programs have ceased such practices except two. Just 3% of emergency medicine programs continue to use animals, as do about 21% of surgical residencies, he said, based on PCRM’s latest surveys.
A public debate
Occasionally, PCRM goes public with a campaign against a residency program “if that’s the only way to win,” Dr. Pippin said.
In addition to billboards, the group has held protests, circulated petitions, and filed complaints with the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service, the entity responsible for overseeing the health and welfare of animals used in medical training and research.
In 2021, spurred by a complaint from PCRM, APHIS launched an investigation into the University of Cincinnati’s surgical residency program. At the time, a university spokesperson acknowledged the school’s limited use of pigs to train “highly-skilled, well-prepared surgeons in the most advanced, complex, real-world needs, procedures, and techniques,” adding that the training methods were endorsed by the American College of Surgeons and in compliance with federal guidelines.
Residency programs have caught the attention of state lawmakers, too. In 2020, bills introduced in both the Rhode Island House and Senate sought to ban the use of live animals in medical training when “there is an alternate teaching method that teaches the medical procedure or lesson without the use of an animal.” Violators would incur misdemeanor charges and monetary fines of up to $1,000 per animal.
The bills – backed by PCRM – targeted Brown University’s emergency medicine residency program, Providence, R.I., which sponsoring legislators said was the last program in New England still using the “outdated” and “unnecessary” method.
In testimony before lawmakers, the school said fewer than 15 pigs participate in the annual training, and faculty spoke about the benefits of the experience.
“If it was your brother or sister, or your mother or father who had to come in and get this procedure done, would you want the physician who’s doing it to be the one who does it for the very first time on a human being, on live tissue? Or do you want that provider to have only practiced on plastic and rubber?” said Nicholas Musisca, MD, an assistant program director with Brown University’s emergency medicine residency, NBC affiliate WJAR reported.
The bills have since stalled, and PCRM held a protest at Brown University in October 2022. In response, a university spokesperson told the Brown Daily Herald, “effective synthetic model alternatives simply do not exist for every complex medical procedure that an emergency physician must be prepared to perform,” including establishing an airway in adults and pediatric patients with severe facial trauma.
By the numbers
Annual reports from APHIS do not show the number of pigs dedicated solely to residency training. Instead, reporting indicates the number of animals “upon which experiments, teaching, research, surgery, or tests were conducted involving accompanying pain or distress to the animals and for which appropriate anesthetic, analgesic, or tranquilizing drugs were used.”
For fiscal year 2021 – the most recent data available – Oregon Health and Science University had 154 pigs under its control, while the University of Cincinnati and Brown University had 118 and 71 pigs, respectively, according to APHIS. Primates were more commonly used at Oregon Health and Science University and guinea pigs at the University of Cincinnati.
Similarly, the Association of American Medical Colleges supports the “use of animals to meet essential educational objectives [across] the medical education continuum. ... Further restrictions on the use of animals in biomedical and behavioral research and education threatens progress in health care and disease prevention.”
The debate will likely rage on. “The one thing we don’t do is give up,” Dr. Pippin said.
A version of this article originally appeared on Medscape.com.
Pigs have been long used in medical schools to teach surgical techniques and, more recently, in research trials and experimental xenotransplantation procedures. But
Just last month, the Physicians Committee for Responsible Medicine, a nonprofit group with a decades-long stance against the use of animals in medical education and research, placed billboards around the Portland, Ore., area demanding that Oregon Health and Science University stop using pigs to teach surgical residents.
Undergraduate medical programs no longer use live animals. But a small number of graduate medical education programs still use animals, predominantly pigs, to train physicians in subspecialties like internal medicine, emergency medicine, surgery, and anesthesiology, John Pippin, MD, FACC, director of academic affairs at PCRM, told this news organization.
Dr. Pippin says residents practice establishing emergency airways, inserting chest tubes, and accessing blood vessels on anesthetized pigs before euthanizing them.
Swine lab advocates say pigs make ideal training subjects because of their similarities to humans, including comparably sized organs like the heart, lungs, and kidneys. Pigs share about 85% of their DNA with people. Where pig skin alternatives may suffice for less invasive procedures, supporters say residents’ experiences with live tissue are irreplaceable.
In a statement, Sara Hottman, associate director of media relations at Oregon Health and Science University, told this news organization the school “only uses animal models in its surgical training program when nonanimal methods are inadequate or too dangerous for human participants.”
“We believe that the education and experience surgical trainees gain through the use of relevant animal models are essential to ensuring future surgeons have the knowledge and skills necessary to provide safe, high-quality care.”
Ms. Hottman also noted that the university continues to evaluate alternatives and looks forward to when nonanimal “surgical training methods are capable of faithfully modeling the complexity of a living system,” such as in the management of critical internal complications.
But Dr. Pippin argues that residents can gain sufficient expertise through simulators and hands-on training in the operating room, and that the differences between humans and pigs are too vast to provide meaningful clinical data or skills.
“Pigs have different genetic influences and very thick, tough skin,” he said. If you use the same pressure on a human that you learned on a pig, he added, “you’d slice right through the trachea. Whatever you think you find out in animals, you have to learn all over again with humans.”
Undergraduate medical education programs in the United States and Canada abandoned the practice of using live animals, including pigs, by 2016, with Johns Hopkins University, Baltimore, and the University of Tennessee, Chattanooga, last to announce their shift away from the controversial teaching model following campaigns by PCRM.
Today, most residency training programs have followed suit. Pippin said that pediatric residencies no longer use animals, and all trauma and anesthesiology programs have ceased such practices except two. Just 3% of emergency medicine programs continue to use animals, as do about 21% of surgical residencies, he said, based on PCRM’s latest surveys.
A public debate
Occasionally, PCRM goes public with a campaign against a residency program “if that’s the only way to win,” Dr. Pippin said.
In addition to billboards, the group has held protests, circulated petitions, and filed complaints with the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service, the entity responsible for overseeing the health and welfare of animals used in medical training and research.
In 2021, spurred by a complaint from PCRM, APHIS launched an investigation into the University of Cincinnati’s surgical residency program. At the time, a university spokesperson acknowledged the school’s limited use of pigs to train “highly-skilled, well-prepared surgeons in the most advanced, complex, real-world needs, procedures, and techniques,” adding that the training methods were endorsed by the American College of Surgeons and in compliance with federal guidelines.
Residency programs have caught the attention of state lawmakers, too. In 2020, bills introduced in both the Rhode Island House and Senate sought to ban the use of live animals in medical training when “there is an alternate teaching method that teaches the medical procedure or lesson without the use of an animal.” Violators would incur misdemeanor charges and monetary fines of up to $1,000 per animal.
The bills – backed by PCRM – targeted Brown University’s emergency medicine residency program, Providence, R.I., which sponsoring legislators said was the last program in New England still using the “outdated” and “unnecessary” method.
In testimony before lawmakers, the school said fewer than 15 pigs participate in the annual training, and faculty spoke about the benefits of the experience.
“If it was your brother or sister, or your mother or father who had to come in and get this procedure done, would you want the physician who’s doing it to be the one who does it for the very first time on a human being, on live tissue? Or do you want that provider to have only practiced on plastic and rubber?” said Nicholas Musisca, MD, an assistant program director with Brown University’s emergency medicine residency, NBC affiliate WJAR reported.
The bills have since stalled, and PCRM held a protest at Brown University in October 2022. In response, a university spokesperson told the Brown Daily Herald, “effective synthetic model alternatives simply do not exist for every complex medical procedure that an emergency physician must be prepared to perform,” including establishing an airway in adults and pediatric patients with severe facial trauma.
By the numbers
Annual reports from APHIS do not show the number of pigs dedicated solely to residency training. Instead, reporting indicates the number of animals “upon which experiments, teaching, research, surgery, or tests were conducted involving accompanying pain or distress to the animals and for which appropriate anesthetic, analgesic, or tranquilizing drugs were used.”
For fiscal year 2021 – the most recent data available – Oregon Health and Science University had 154 pigs under its control, while the University of Cincinnati and Brown University had 118 and 71 pigs, respectively, according to APHIS. Primates were more commonly used at Oregon Health and Science University and guinea pigs at the University of Cincinnati.
Similarly, the Association of American Medical Colleges supports the “use of animals to meet essential educational objectives [across] the medical education continuum. ... Further restrictions on the use of animals in biomedical and behavioral research and education threatens progress in health care and disease prevention.”
The debate will likely rage on. “The one thing we don’t do is give up,” Dr. Pippin said.
A version of this article originally appeared on Medscape.com.
COVID emergency orders ending: What’s next?
It’s the end of an era.
The orders spanned two presidencies. The Trump administration’s Health and Human Services Secretary Alex Azar issued a public health emergency in January 2020. Then-President Donald Trump declared the COVID-19 pandemic a national emergency 2 months later. Both emergency declarations – which remained in effect under President Joe Biden – are set to expire May 11.
Read on for an overview of how the end of the public health emergency will trigger multiple federal policy changes.
Changes that affect everyone
- There will be cost-sharing changes for COVID-19 vaccines, testing, and certain treatments. One hundred–percent coverage for COVID testing, including free at-home tests, will expire May 11.
- Telemedicine cannot be used to prescribe controlled substances after May 11, 2023.
- Enhanced federal funding will be phased down through Dec. 31, 2023. This extends the time states must receive federally matched funds for COVID-related services and products, through the Consolidated Appropriations Act of 2023. Otherwise, this would have expired June 30, 2023.
- Emergency use authorizations for COVID-19 treatments and vaccinations will not be affected and/or end on May 11.
Changes that affect people with private health insurance
- Many will likely see higher costs for COVID-19 tests, as free testing expires and cost-sharing begins in the coming months.
- COVID-19 vaccinations and boosters will continue to be covered until the federal government’s vaccination supply is depleted. If that happens, you will need an in-network provider.
- You will still have access to COVID-19 treatments – but that could change when the federal supply dwindles.
Changes that affect Medicare recipients
- Medicare telehealth flexibilities will be extended through Dec. 31, 2024, regardless of public health emergency status. This means people can access telehealth services from anywhere, not just rural areas; can use a smartphone for telehealth; and can access telehealth in their homes.
- Medicare cost-sharing for testing and treatments will expire May 11, except for oral antivirals.
Changes that affect Medicaid/CHIP recipients
- Medicaid and Children’s Health Insurance Program (CHIP) recipients will continue to receive approved vaccinations free of charge, but testing and treatment without cost-sharing will expire during the third quarter of 2024.
- The Medicaid continuous enrollment provision will be separated from the public health emergency, and continuous enrollment will end March 31, 2023.
Changes that affect uninsured people
- The uninsured will no longer have access to 100% coverage for these products and services (free COVID-19 treatments, vaccines, and testing).
Changes that affect health care providers
- There will be changes to how much providers get paid for diagnosing people with COVID-19, ending the enhanced Inpatient Prospective Payment System reimbursement rate, as of May 11, 2023.
- Health Insurance Portability and Accountability Act (HIPAA) potential penalty waivers will end. This allows providers to communicate with patients through telehealth on a smartphone, for example, without violating privacy laws and incurring penalties.
What the experts are saying
This news organization asked several health experts for their thoughts on ending the emergency health declarations for COVID, and what effects this could have. Many expressed concerns about the timing of the ending, saying that the move could limit access to COVID-related treatments. Others said the move was inevitable but raised concerns about federal guidance related to the decision.
Question: Do you agree with the timing of the end to the emergency order?
Answer: Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston: “A lead time to prepare and anticipate these consequences may ease the transition, compared to an abrupt declaration that ends the declaration.”
Answer: Georges C. Benjamin, MD, executive director of the American Public Health Association: “I think it’s time to do so. It has to be done in a great, thoughtful, and organized way because we’ve attached so many different things to this public health emergency. It’s going to take time for the system to adapt. [Centers for Disease Control and Prevention] data collection most likely will continue. People are used to reporting now. The CDC needs to give guidance to the states so that we’re clear about what we’re reporting, what we’re not. If we did that abruptly, it would just be a mess.”
Answer: Bruce Farber, MD, chief public health and epidemiology officer at Northwell Health in Manhasset, N.Y.: “I would have hoped to see it delayed.”
Answer: Steven Newmark, JD, chief legal officer and director of policy at the Global Healthy Living Foundation: “While we understand that an emergency cannot last forever, we hope that expanded services such as free vaccination, promotion of widespread vaccination, increased use of pharmacists to administer vaccines, telehealth availability and reimbursement, flexibility in work-from-home opportunities, and more continues. Access to equitable health care should never backtrack or be reduced.”
Q: What will the end of free COVID vaccinations and free testing mean?
A: Dr. Farber: “There will likely be a decrease in vaccinations and testing. The vaccination rates are very low to begin with, and this will likely lower it further.”
A: Dr. Atmar: “I think it will mean that fewer people will get tested and vaccinated,” which “could lead to increased transmission, although wastewater testing suggests that there is a lot of unrecognized infection already occurring.”
A: Dr. Benjamin: “That is a big concern. It means that for people, particularly for people who are uninsured and underinsured, we’ve got to make sure they have access to those. There’s a lot of discussion and debate about what the cost of those tests and vaccines will be, and it looks like the companies are going to impose very steep, increasing costs.”
Q: How will this affect higher-risk populations, like people with weakened immune systems?
A: Dr. Farber: “Without monoclonals [drugs to treat COVID] and free Paxlovid,” people with weakened immune systems “may be undertreated.”
A: Dr. Atmar: “The implications of ongoing widespread virus transmission are that immunocompromised individuals may be more likely to be exposed and infected and to suffer the consequences of such infection, including severe illness. However, to a certain degree, this may already be happening. We are still seeing about 500 deaths/day, primarily in persons at highest risk of severe disease.”
A: Dr. Benjamin: “People who have good insurance, can afford to get immunized, and have good relations with practitioners probably will continue to be covered. But lower-income individuals and people who really can’t afford to get tested or get immunized would likely become underimmunized and more infected.
“So even though the federal emergency declaration will go away, I’m hoping that the federal government will continue to encourage all of us to emphasize those populations at the highest risk – those with chronic disease and those who are immunocompromised.”
A: Mr. Newmark: “People who are immunocompromised by their chronic illness or the medicines they take to treat acute or chronic conditions remain at higher risk for COVID-19 and its serious complications. The administration needs to support continued development of effective treatments and updated vaccines to protect the individual and public health. We’re also concerned that increased health care services - such as vaccination or telehealth – may fall back to prepandemic levels while the burden of protection, such as masking, may fall to chronic disease patients alone, which adds to the burden of living with disease.”
Q: What effect will ending Medicaid expansion money have?
A: Dr. Benjamin: Anywhere from 16 to 20 million people are going to lose in coverage. I’m hoping that states will look at their experience over these last 2 years or so and come to the decision that there were improvements in healthier populations.
Q: Will this have any effect on how the public perceives the pandemic?
A: Dr. Farber: “It is likely to give the impression that COVID is gone, which clearly is not the case.”
A: Dr. Benjamin: “It’ll be another argument by some that the pandemic is over. People should think about this as kind of like a hurricane. A hurricane comes through and tragically tears up communities, and we have an emergency during that time. But then we have to go through a period of recovery. I’m hoping people will realize that even though the public health emergencies have gone away, that we still need to go through a period of transition ... and that means that they still need to protect themselves, get vaccinated, and wear a mask when appropriate.”
A: Dr. Atmar: “There needs to be messaging that while we are transitioning away from emergency management of COVID-19, it is still a significant public health concern.”
A version of this article originally appeared on WebMD.com.
It’s the end of an era.
The orders spanned two presidencies. The Trump administration’s Health and Human Services Secretary Alex Azar issued a public health emergency in January 2020. Then-President Donald Trump declared the COVID-19 pandemic a national emergency 2 months later. Both emergency declarations – which remained in effect under President Joe Biden – are set to expire May 11.
Read on for an overview of how the end of the public health emergency will trigger multiple federal policy changes.
Changes that affect everyone
- There will be cost-sharing changes for COVID-19 vaccines, testing, and certain treatments. One hundred–percent coverage for COVID testing, including free at-home tests, will expire May 11.
- Telemedicine cannot be used to prescribe controlled substances after May 11, 2023.
- Enhanced federal funding will be phased down through Dec. 31, 2023. This extends the time states must receive federally matched funds for COVID-related services and products, through the Consolidated Appropriations Act of 2023. Otherwise, this would have expired June 30, 2023.
- Emergency use authorizations for COVID-19 treatments and vaccinations will not be affected and/or end on May 11.
Changes that affect people with private health insurance
- Many will likely see higher costs for COVID-19 tests, as free testing expires and cost-sharing begins in the coming months.
- COVID-19 vaccinations and boosters will continue to be covered until the federal government’s vaccination supply is depleted. If that happens, you will need an in-network provider.
- You will still have access to COVID-19 treatments – but that could change when the federal supply dwindles.
Changes that affect Medicare recipients
- Medicare telehealth flexibilities will be extended through Dec. 31, 2024, regardless of public health emergency status. This means people can access telehealth services from anywhere, not just rural areas; can use a smartphone for telehealth; and can access telehealth in their homes.
- Medicare cost-sharing for testing and treatments will expire May 11, except for oral antivirals.
Changes that affect Medicaid/CHIP recipients
- Medicaid and Children’s Health Insurance Program (CHIP) recipients will continue to receive approved vaccinations free of charge, but testing and treatment without cost-sharing will expire during the third quarter of 2024.
- The Medicaid continuous enrollment provision will be separated from the public health emergency, and continuous enrollment will end March 31, 2023.
Changes that affect uninsured people
- The uninsured will no longer have access to 100% coverage for these products and services (free COVID-19 treatments, vaccines, and testing).
Changes that affect health care providers
- There will be changes to how much providers get paid for diagnosing people with COVID-19, ending the enhanced Inpatient Prospective Payment System reimbursement rate, as of May 11, 2023.
- Health Insurance Portability and Accountability Act (HIPAA) potential penalty waivers will end. This allows providers to communicate with patients through telehealth on a smartphone, for example, without violating privacy laws and incurring penalties.
What the experts are saying
This news organization asked several health experts for their thoughts on ending the emergency health declarations for COVID, and what effects this could have. Many expressed concerns about the timing of the ending, saying that the move could limit access to COVID-related treatments. Others said the move was inevitable but raised concerns about federal guidance related to the decision.
Question: Do you agree with the timing of the end to the emergency order?
Answer: Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston: “A lead time to prepare and anticipate these consequences may ease the transition, compared to an abrupt declaration that ends the declaration.”
Answer: Georges C. Benjamin, MD, executive director of the American Public Health Association: “I think it’s time to do so. It has to be done in a great, thoughtful, and organized way because we’ve attached so many different things to this public health emergency. It’s going to take time for the system to adapt. [Centers for Disease Control and Prevention] data collection most likely will continue. People are used to reporting now. The CDC needs to give guidance to the states so that we’re clear about what we’re reporting, what we’re not. If we did that abruptly, it would just be a mess.”
Answer: Bruce Farber, MD, chief public health and epidemiology officer at Northwell Health in Manhasset, N.Y.: “I would have hoped to see it delayed.”
Answer: Steven Newmark, JD, chief legal officer and director of policy at the Global Healthy Living Foundation: “While we understand that an emergency cannot last forever, we hope that expanded services such as free vaccination, promotion of widespread vaccination, increased use of pharmacists to administer vaccines, telehealth availability and reimbursement, flexibility in work-from-home opportunities, and more continues. Access to equitable health care should never backtrack or be reduced.”
Q: What will the end of free COVID vaccinations and free testing mean?
A: Dr. Farber: “There will likely be a decrease in vaccinations and testing. The vaccination rates are very low to begin with, and this will likely lower it further.”
A: Dr. Atmar: “I think it will mean that fewer people will get tested and vaccinated,” which “could lead to increased transmission, although wastewater testing suggests that there is a lot of unrecognized infection already occurring.”
A: Dr. Benjamin: “That is a big concern. It means that for people, particularly for people who are uninsured and underinsured, we’ve got to make sure they have access to those. There’s a lot of discussion and debate about what the cost of those tests and vaccines will be, and it looks like the companies are going to impose very steep, increasing costs.”
Q: How will this affect higher-risk populations, like people with weakened immune systems?
A: Dr. Farber: “Without monoclonals [drugs to treat COVID] and free Paxlovid,” people with weakened immune systems “may be undertreated.”
A: Dr. Atmar: “The implications of ongoing widespread virus transmission are that immunocompromised individuals may be more likely to be exposed and infected and to suffer the consequences of such infection, including severe illness. However, to a certain degree, this may already be happening. We are still seeing about 500 deaths/day, primarily in persons at highest risk of severe disease.”
A: Dr. Benjamin: “People who have good insurance, can afford to get immunized, and have good relations with practitioners probably will continue to be covered. But lower-income individuals and people who really can’t afford to get tested or get immunized would likely become underimmunized and more infected.
“So even though the federal emergency declaration will go away, I’m hoping that the federal government will continue to encourage all of us to emphasize those populations at the highest risk – those with chronic disease and those who are immunocompromised.”
A: Mr. Newmark: “People who are immunocompromised by their chronic illness or the medicines they take to treat acute or chronic conditions remain at higher risk for COVID-19 and its serious complications. The administration needs to support continued development of effective treatments and updated vaccines to protect the individual and public health. We’re also concerned that increased health care services - such as vaccination or telehealth – may fall back to prepandemic levels while the burden of protection, such as masking, may fall to chronic disease patients alone, which adds to the burden of living with disease.”
Q: What effect will ending Medicaid expansion money have?
A: Dr. Benjamin: Anywhere from 16 to 20 million people are going to lose in coverage. I’m hoping that states will look at their experience over these last 2 years or so and come to the decision that there were improvements in healthier populations.
Q: Will this have any effect on how the public perceives the pandemic?
A: Dr. Farber: “It is likely to give the impression that COVID is gone, which clearly is not the case.”
A: Dr. Benjamin: “It’ll be another argument by some that the pandemic is over. People should think about this as kind of like a hurricane. A hurricane comes through and tragically tears up communities, and we have an emergency during that time. But then we have to go through a period of recovery. I’m hoping people will realize that even though the public health emergencies have gone away, that we still need to go through a period of transition ... and that means that they still need to protect themselves, get vaccinated, and wear a mask when appropriate.”
A: Dr. Atmar: “There needs to be messaging that while we are transitioning away from emergency management of COVID-19, it is still a significant public health concern.”
A version of this article originally appeared on WebMD.com.
It’s the end of an era.
The orders spanned two presidencies. The Trump administration’s Health and Human Services Secretary Alex Azar issued a public health emergency in January 2020. Then-President Donald Trump declared the COVID-19 pandemic a national emergency 2 months later. Both emergency declarations – which remained in effect under President Joe Biden – are set to expire May 11.
Read on for an overview of how the end of the public health emergency will trigger multiple federal policy changes.
Changes that affect everyone
- There will be cost-sharing changes for COVID-19 vaccines, testing, and certain treatments. One hundred–percent coverage for COVID testing, including free at-home tests, will expire May 11.
- Telemedicine cannot be used to prescribe controlled substances after May 11, 2023.
- Enhanced federal funding will be phased down through Dec. 31, 2023. This extends the time states must receive federally matched funds for COVID-related services and products, through the Consolidated Appropriations Act of 2023. Otherwise, this would have expired June 30, 2023.
- Emergency use authorizations for COVID-19 treatments and vaccinations will not be affected and/or end on May 11.
Changes that affect people with private health insurance
- Many will likely see higher costs for COVID-19 tests, as free testing expires and cost-sharing begins in the coming months.
- COVID-19 vaccinations and boosters will continue to be covered until the federal government’s vaccination supply is depleted. If that happens, you will need an in-network provider.
- You will still have access to COVID-19 treatments – but that could change when the federal supply dwindles.
Changes that affect Medicare recipients
- Medicare telehealth flexibilities will be extended through Dec. 31, 2024, regardless of public health emergency status. This means people can access telehealth services from anywhere, not just rural areas; can use a smartphone for telehealth; and can access telehealth in their homes.
- Medicare cost-sharing for testing and treatments will expire May 11, except for oral antivirals.
Changes that affect Medicaid/CHIP recipients
- Medicaid and Children’s Health Insurance Program (CHIP) recipients will continue to receive approved vaccinations free of charge, but testing and treatment without cost-sharing will expire during the third quarter of 2024.
- The Medicaid continuous enrollment provision will be separated from the public health emergency, and continuous enrollment will end March 31, 2023.
Changes that affect uninsured people
- The uninsured will no longer have access to 100% coverage for these products and services (free COVID-19 treatments, vaccines, and testing).
Changes that affect health care providers
- There will be changes to how much providers get paid for diagnosing people with COVID-19, ending the enhanced Inpatient Prospective Payment System reimbursement rate, as of May 11, 2023.
- Health Insurance Portability and Accountability Act (HIPAA) potential penalty waivers will end. This allows providers to communicate with patients through telehealth on a smartphone, for example, without violating privacy laws and incurring penalties.
What the experts are saying
This news organization asked several health experts for their thoughts on ending the emergency health declarations for COVID, and what effects this could have. Many expressed concerns about the timing of the ending, saying that the move could limit access to COVID-related treatments. Others said the move was inevitable but raised concerns about federal guidance related to the decision.
Question: Do you agree with the timing of the end to the emergency order?
Answer: Robert Atmar, MD, professor of infectious diseases at Baylor College of Medicine in Houston: “A lead time to prepare and anticipate these consequences may ease the transition, compared to an abrupt declaration that ends the declaration.”
Answer: Georges C. Benjamin, MD, executive director of the American Public Health Association: “I think it’s time to do so. It has to be done in a great, thoughtful, and organized way because we’ve attached so many different things to this public health emergency. It’s going to take time for the system to adapt. [Centers for Disease Control and Prevention] data collection most likely will continue. People are used to reporting now. The CDC needs to give guidance to the states so that we’re clear about what we’re reporting, what we’re not. If we did that abruptly, it would just be a mess.”
Answer: Bruce Farber, MD, chief public health and epidemiology officer at Northwell Health in Manhasset, N.Y.: “I would have hoped to see it delayed.”
Answer: Steven Newmark, JD, chief legal officer and director of policy at the Global Healthy Living Foundation: “While we understand that an emergency cannot last forever, we hope that expanded services such as free vaccination, promotion of widespread vaccination, increased use of pharmacists to administer vaccines, telehealth availability and reimbursement, flexibility in work-from-home opportunities, and more continues. Access to equitable health care should never backtrack or be reduced.”
Q: What will the end of free COVID vaccinations and free testing mean?
A: Dr. Farber: “There will likely be a decrease in vaccinations and testing. The vaccination rates are very low to begin with, and this will likely lower it further.”
A: Dr. Atmar: “I think it will mean that fewer people will get tested and vaccinated,” which “could lead to increased transmission, although wastewater testing suggests that there is a lot of unrecognized infection already occurring.”
A: Dr. Benjamin: “That is a big concern. It means that for people, particularly for people who are uninsured and underinsured, we’ve got to make sure they have access to those. There’s a lot of discussion and debate about what the cost of those tests and vaccines will be, and it looks like the companies are going to impose very steep, increasing costs.”
Q: How will this affect higher-risk populations, like people with weakened immune systems?
A: Dr. Farber: “Without monoclonals [drugs to treat COVID] and free Paxlovid,” people with weakened immune systems “may be undertreated.”
A: Dr. Atmar: “The implications of ongoing widespread virus transmission are that immunocompromised individuals may be more likely to be exposed and infected and to suffer the consequences of such infection, including severe illness. However, to a certain degree, this may already be happening. We are still seeing about 500 deaths/day, primarily in persons at highest risk of severe disease.”
A: Dr. Benjamin: “People who have good insurance, can afford to get immunized, and have good relations with practitioners probably will continue to be covered. But lower-income individuals and people who really can’t afford to get tested or get immunized would likely become underimmunized and more infected.
“So even though the federal emergency declaration will go away, I’m hoping that the federal government will continue to encourage all of us to emphasize those populations at the highest risk – those with chronic disease and those who are immunocompromised.”
A: Mr. Newmark: “People who are immunocompromised by their chronic illness or the medicines they take to treat acute or chronic conditions remain at higher risk for COVID-19 and its serious complications. The administration needs to support continued development of effective treatments and updated vaccines to protect the individual and public health. We’re also concerned that increased health care services - such as vaccination or telehealth – may fall back to prepandemic levels while the burden of protection, such as masking, may fall to chronic disease patients alone, which adds to the burden of living with disease.”
Q: What effect will ending Medicaid expansion money have?
A: Dr. Benjamin: Anywhere from 16 to 20 million people are going to lose in coverage. I’m hoping that states will look at their experience over these last 2 years or so and come to the decision that there were improvements in healthier populations.
Q: Will this have any effect on how the public perceives the pandemic?
A: Dr. Farber: “It is likely to give the impression that COVID is gone, which clearly is not the case.”
A: Dr. Benjamin: “It’ll be another argument by some that the pandemic is over. People should think about this as kind of like a hurricane. A hurricane comes through and tragically tears up communities, and we have an emergency during that time. But then we have to go through a period of recovery. I’m hoping people will realize that even though the public health emergencies have gone away, that we still need to go through a period of transition ... and that means that they still need to protect themselves, get vaccinated, and wear a mask when appropriate.”
A: Dr. Atmar: “There needs to be messaging that while we are transitioning away from emergency management of COVID-19, it is still a significant public health concern.”
A version of this article originally appeared on WebMD.com.
Decoding endometriosis: Recent research fosters hope
Roughly 4 decades after she first started menstruating, Elizabeth Flanagan finally underwent surgery to repair damage wreaked on her body by endometriosis. She’d spent years struggling with a variety of seemingly random symptoms, from migraines to excruciatingly painful periods to fatigue and irritable bowel syndrome. She’d worried about abnormal labs, including “extremely high” ANA, creatinine, and BUN blood test results that had been out of normal range for more than 10 years.
She was diagnosed with endometriosis in 2016, at age 47, after surgery to remove an ovarian cyst. Still, it took 5 more years before she landed in the office of a surgeon with the proper training to excise the lesions that continued to cause her so much anguish. That physician, Matthew Siedhoff, MD, at Cedars-Sinai Medical Center in Los Angeles, explained why her creatinine and BUN results were so far out of range: The endometriosis was impinging on her ureters.
The appointment left Ms. Flanagan with a range of emotions. “I was shocked that no doctor had identified this before, relieved knowing that I was finally in the hands of an expert who understood my condition, and saddened by the dearth of knowledge and proper treatment of endometriosis,” she wrote in an email.
Although the disease afflicts at least 1 out of every 10 women, endometriosis remains a conundrum for patients and their physicians. It often masquerades as other problems, from mental health issues such as anxiety and depression to physical issues such as irritable bowel syndrome. It often coexists with autoimmune conditions. Short of performing surgery, it can be a diagnosis of exclusion. And the existing, state-of-the-art treatment – hormone therapy that shuts down the reproductive system – doesn’t work for every woman every time.
“It is no wonder that it takes 10 years on average, from the time someone has symptoms of endometriosis, until they get a definitive diagnosis,” said Hugh Taylor, MD, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn. “It’s a combination of [physicians] not taking painful menses seriously and getting distracted by all these other manifestations of the disease throughout the whole body.”
Endometriosis, he said, “is a whole-body disease.”
But recent genetic research offers the tantalizing prospect of new diagnostic tools and treatments. In 5-10 years, scientists say, physicians may be able to diagnose the disease with a simple blood test, and treat it, for example, by preventing a gene receptor from initiating a cascade of inflammatory effects, or crafting treatments tailored to the molecular makeup of a patient’s disease.
“Tomorrow’s therapies will target specifically the molecular defects of endometriosis and be nonhormonal,” Dr. Taylor said.
Guidelines published last year by the European Society of Human Reproduction and Embryology detail the latest standards for diagnosis and treatment of endometriosis.
According to the guidelines, physicians should consider the diagnosis of endometriosis in individuals presenting with the following cyclical and noncyclical signs and symptoms: dysmenorrhea, deep dyspareunia, dysuria, dyschezia, painful rectal bleeding or hematuria, shoulder tip pain, catamenial pneumothorax, cyclical cough/hemoptysis/chest pain, cyclical scar swelling, and pain, fatigue, and infertility.
A clinical exam should be considered, as well as imaging such as ultrasound and/or MRI, the guidelines state, although negative findings should not rule out a diagnosis. Laparoscopy is also an option, particularly for patients who desire a definitive diagnosis or cannot be diagnosed any other way, “although negative histology [of endometriotic lesions] does not entirely rule out the disease,” the guidelines state.
To treat the pain associated with endometriosis, the guidelines advise, as a first-line therapy, beginning with NSAIDs and combined hormonal contraceptives (in oral, vaginal, or transdermal form). Another option is progesterone, including progesterone-only contraceptives, with a recommendation to prescribe a levonorgestrel-releasing intrauterine system or an etonogestrel-releasing subdermal implant to reduce endometriosis-associated pain.
However, progestins and low-dose oral contraceptives are “unsuccessful in a third of women,” Dr. Taylor and his coauthors wrote in a paper published in 2021 in The Lancet.
Until recently, the gold standard for second-line treatment of endometriosis was oral gonadotropin-releasing hormone (GnRH) agonists. These manage the disease by inducing medical menopause – they downregulate pituitary GnRH receptors to create a hypoestrogenic state characterized by low serum levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). GnRH agonists may be administered nasally, or through daily, monthly, or trimonthly injections. But the Food and Drug Administration advises that, when used for longer than 6 months, GnRH agonists be paired with add-back hormone replacement therapy to reduce the risk of bone loss associated with the plunge in hormone levels. Also, treatment may not be appropriate for patients who, when suddenly forced into menopause, suffer from bothersome symptoms.
The latest treatment, GnRH antagonists, are new options for patients who either do not respond adequately to progestins and low-dose contraceptives or develop progesterone resistance, and want to avoid some of the risks and/or symptoms associated with GnRH agonists. Two advantages of GnRH antagonists for patients, Dr. Taylor said, are that they have a fast onset of action and are oral rather than injectable.
“These drugs [GnRH antagonists] cause competitive blockage of the GnRH receptor and hence dose-dependently suppress production of FSH and LH and inhibit secretion of ovarian steroid hormones without inducing a flare-up effect,” Belgian physicians and researchers Jacques Donnez, MD, and Marie-Madeleine Dolmans, MD, PhD, wrote in a paper published last year in the Journal of Clinical Medicine. “The mechanism is different from that of the GnRH agonist which, after a first phase of stimulation, desensitizes GnRH receptors, leading to full suppression of LH and FSH production and subsequently to complete suppression of [estrogen] to levels similar to those observed after bilateral oophorectomy.”
Patients who took Elagolix, the first oral nonpeptide GnRH antagonist available for the treatment of moderate to severe endometriosis-associated pain, had fewer vasomotor side effects and less bone density loss than those on the GnRH agonist leuprorelin, according to a 2018 study in Obstetrics and Gynecology. However, without add-back hormone-replacement therapy, GnRH antagonist use may need to be limited to 24 months, because of loss of bone density, a study in Cell Reports Medicine reported in 2022.
Attempting to explain the pathogenesis of endometriosis, and frustrated by the shortcomings of currently available therapies, researchers have turned to genetics for insight. A team of scientists led by Thomas Tapmeier, PhD, now a senior research fellow at Monash University in Australia, and Prof. Krina Zondervan at the University of Oxford, ran genetic analyses of families with a history of endometriosis, as well as rhesus macaques that spontaneously developed endometriosis. The research, published in Science Translational Medicine, identified NPSR1, the gene encoding neuropeptide S receptor 1, as one commonly associated with endometriosis. In trials with mouse models, they found that the NPSR1 inhibitor SHA 68R was able to reduce endometriosis-related inflammation and pain.
“It’s important to stress that there is no single gene that is responsible for endometriosis,” Dr. Tapmeier said in an interview. “This gene just has a higher frequency in people with endometriosis.”
The next step, then, would be to try to find a compound that would inhibit NPSR1 at some point, or a competitor to the ligand that binds to the receptor and blocks it, he said.
“We’re currently looking at compounds that might be able to inhibit the receptor signaling,” he said.
Such a therapy could potentially reduce the symptoms of endometriosis without interfering with the menstrual cycle and without introducing hormones that cause undesirable side effects in some patients.
“This might be a way to treat the pain and inflammation that goes with endometriosis, as well as leaving the possibility of pregnancy open,” he said.
Other researchers are searching for biomarkers of the disease, both to provide a definitive, nonsurgical diagnostic tool, and for potential, individualized treatment.
In a study published in Nature Genetics, researchers at Cedars-Sinai created a “cellular atlas” of endometriosis by analyzing nearly 400,000 individual cells from 21 patients, some of whom had the disease and some of whom did not. A new technology, single-cell genomics, allowed the scientists to profile the multiple cell types contributing to the disease.
“So the initial question we wanted to ask was about understanding how the cells look in endometriosis, compared to endometrium,” said Kate Lawrenson, PhD, an associate professor in the department of obstetrics and gynecology at Cedars-Sinai, and co–senior author of the study. “We know that they resemble the cells of the womb, but we really don’t understand if they behave the same. We had a good inkling that they would behave differently.”
It turned out they did: Cells of endometriosis interacted atypically with female hormones, compared with cells in the uterus, Dr. Lawrenson said.
“That helps us understand how, even when patients take contraceptive pills, which is a commonly prescribed therapy, it doesn’t always work, or sometimes it stops working after a while,” she said. The next step for researchers, she said, will be to pinpoint the specific causes of these altered interactions.
Meanwhile, the current research also points to diagnostic possibilities. “We were quite excited to see that multiple cell types and endometriosis are upregulating the same sets of genes,” she said. “That makes us optimistic that hopefully there are some protein gene products that are being made in abundance, and hopefully we can detect them in the blood stream. It might be that we could use that information to develop new biomarkers, or even risk stratification tools.”
In the future, a simple blood test could identify signs of endometriosis in at-risk patients and get them “fast-tracked to a specialist for evaluation,” she said. “Whereas now, they might go from PCP to gynecologist to a different gynecologist over the course of 5-10 years before they get that referral.”
This discovery, that endometrial cells use genes differently and cross-talk with nearby cells differently, presents new treatment possibilities. Maybe we can physically block how cells interact with nearby cells, Dr. Lawrenson said. One model for doing that, she said, would be antibody-based therapy, similar to the therapies now changing the treatment of cancer.
What’s most exciting, looking ahead 5-10 years, is that treatment for endometriosis in the future may be significantly more individualized, and less hormone-based, than it is today.
“What we need for endometriosis is more options for patients and something that is tailored to the molecular makeup of their disease rather than a process of trial and error,” she said.
Roughly 4 decades after she first started menstruating, Elizabeth Flanagan finally underwent surgery to repair damage wreaked on her body by endometriosis. She’d spent years struggling with a variety of seemingly random symptoms, from migraines to excruciatingly painful periods to fatigue and irritable bowel syndrome. She’d worried about abnormal labs, including “extremely high” ANA, creatinine, and BUN blood test results that had been out of normal range for more than 10 years.
She was diagnosed with endometriosis in 2016, at age 47, after surgery to remove an ovarian cyst. Still, it took 5 more years before she landed in the office of a surgeon with the proper training to excise the lesions that continued to cause her so much anguish. That physician, Matthew Siedhoff, MD, at Cedars-Sinai Medical Center in Los Angeles, explained why her creatinine and BUN results were so far out of range: The endometriosis was impinging on her ureters.
The appointment left Ms. Flanagan with a range of emotions. “I was shocked that no doctor had identified this before, relieved knowing that I was finally in the hands of an expert who understood my condition, and saddened by the dearth of knowledge and proper treatment of endometriosis,” she wrote in an email.
Although the disease afflicts at least 1 out of every 10 women, endometriosis remains a conundrum for patients and their physicians. It often masquerades as other problems, from mental health issues such as anxiety and depression to physical issues such as irritable bowel syndrome. It often coexists with autoimmune conditions. Short of performing surgery, it can be a diagnosis of exclusion. And the existing, state-of-the-art treatment – hormone therapy that shuts down the reproductive system – doesn’t work for every woman every time.
“It is no wonder that it takes 10 years on average, from the time someone has symptoms of endometriosis, until they get a definitive diagnosis,” said Hugh Taylor, MD, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn. “It’s a combination of [physicians] not taking painful menses seriously and getting distracted by all these other manifestations of the disease throughout the whole body.”
Endometriosis, he said, “is a whole-body disease.”
But recent genetic research offers the tantalizing prospect of new diagnostic tools and treatments. In 5-10 years, scientists say, physicians may be able to diagnose the disease with a simple blood test, and treat it, for example, by preventing a gene receptor from initiating a cascade of inflammatory effects, or crafting treatments tailored to the molecular makeup of a patient’s disease.
“Tomorrow’s therapies will target specifically the molecular defects of endometriosis and be nonhormonal,” Dr. Taylor said.
Guidelines published last year by the European Society of Human Reproduction and Embryology detail the latest standards for diagnosis and treatment of endometriosis.
According to the guidelines, physicians should consider the diagnosis of endometriosis in individuals presenting with the following cyclical and noncyclical signs and symptoms: dysmenorrhea, deep dyspareunia, dysuria, dyschezia, painful rectal bleeding or hematuria, shoulder tip pain, catamenial pneumothorax, cyclical cough/hemoptysis/chest pain, cyclical scar swelling, and pain, fatigue, and infertility.
A clinical exam should be considered, as well as imaging such as ultrasound and/or MRI, the guidelines state, although negative findings should not rule out a diagnosis. Laparoscopy is also an option, particularly for patients who desire a definitive diagnosis or cannot be diagnosed any other way, “although negative histology [of endometriotic lesions] does not entirely rule out the disease,” the guidelines state.
To treat the pain associated with endometriosis, the guidelines advise, as a first-line therapy, beginning with NSAIDs and combined hormonal contraceptives (in oral, vaginal, or transdermal form). Another option is progesterone, including progesterone-only contraceptives, with a recommendation to prescribe a levonorgestrel-releasing intrauterine system or an etonogestrel-releasing subdermal implant to reduce endometriosis-associated pain.
However, progestins and low-dose oral contraceptives are “unsuccessful in a third of women,” Dr. Taylor and his coauthors wrote in a paper published in 2021 in The Lancet.
Until recently, the gold standard for second-line treatment of endometriosis was oral gonadotropin-releasing hormone (GnRH) agonists. These manage the disease by inducing medical menopause – they downregulate pituitary GnRH receptors to create a hypoestrogenic state characterized by low serum levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). GnRH agonists may be administered nasally, or through daily, monthly, or trimonthly injections. But the Food and Drug Administration advises that, when used for longer than 6 months, GnRH agonists be paired with add-back hormone replacement therapy to reduce the risk of bone loss associated with the plunge in hormone levels. Also, treatment may not be appropriate for patients who, when suddenly forced into menopause, suffer from bothersome symptoms.
The latest treatment, GnRH antagonists, are new options for patients who either do not respond adequately to progestins and low-dose contraceptives or develop progesterone resistance, and want to avoid some of the risks and/or symptoms associated with GnRH agonists. Two advantages of GnRH antagonists for patients, Dr. Taylor said, are that they have a fast onset of action and are oral rather than injectable.
“These drugs [GnRH antagonists] cause competitive blockage of the GnRH receptor and hence dose-dependently suppress production of FSH and LH and inhibit secretion of ovarian steroid hormones without inducing a flare-up effect,” Belgian physicians and researchers Jacques Donnez, MD, and Marie-Madeleine Dolmans, MD, PhD, wrote in a paper published last year in the Journal of Clinical Medicine. “The mechanism is different from that of the GnRH agonist which, after a first phase of stimulation, desensitizes GnRH receptors, leading to full suppression of LH and FSH production and subsequently to complete suppression of [estrogen] to levels similar to those observed after bilateral oophorectomy.”
Patients who took Elagolix, the first oral nonpeptide GnRH antagonist available for the treatment of moderate to severe endometriosis-associated pain, had fewer vasomotor side effects and less bone density loss than those on the GnRH agonist leuprorelin, according to a 2018 study in Obstetrics and Gynecology. However, without add-back hormone-replacement therapy, GnRH antagonist use may need to be limited to 24 months, because of loss of bone density, a study in Cell Reports Medicine reported in 2022.
Attempting to explain the pathogenesis of endometriosis, and frustrated by the shortcomings of currently available therapies, researchers have turned to genetics for insight. A team of scientists led by Thomas Tapmeier, PhD, now a senior research fellow at Monash University in Australia, and Prof. Krina Zondervan at the University of Oxford, ran genetic analyses of families with a history of endometriosis, as well as rhesus macaques that spontaneously developed endometriosis. The research, published in Science Translational Medicine, identified NPSR1, the gene encoding neuropeptide S receptor 1, as one commonly associated with endometriosis. In trials with mouse models, they found that the NPSR1 inhibitor SHA 68R was able to reduce endometriosis-related inflammation and pain.
“It’s important to stress that there is no single gene that is responsible for endometriosis,” Dr. Tapmeier said in an interview. “This gene just has a higher frequency in people with endometriosis.”
The next step, then, would be to try to find a compound that would inhibit NPSR1 at some point, or a competitor to the ligand that binds to the receptor and blocks it, he said.
“We’re currently looking at compounds that might be able to inhibit the receptor signaling,” he said.
Such a therapy could potentially reduce the symptoms of endometriosis without interfering with the menstrual cycle and without introducing hormones that cause undesirable side effects in some patients.
“This might be a way to treat the pain and inflammation that goes with endometriosis, as well as leaving the possibility of pregnancy open,” he said.
Other researchers are searching for biomarkers of the disease, both to provide a definitive, nonsurgical diagnostic tool, and for potential, individualized treatment.
In a study published in Nature Genetics, researchers at Cedars-Sinai created a “cellular atlas” of endometriosis by analyzing nearly 400,000 individual cells from 21 patients, some of whom had the disease and some of whom did not. A new technology, single-cell genomics, allowed the scientists to profile the multiple cell types contributing to the disease.
“So the initial question we wanted to ask was about understanding how the cells look in endometriosis, compared to endometrium,” said Kate Lawrenson, PhD, an associate professor in the department of obstetrics and gynecology at Cedars-Sinai, and co–senior author of the study. “We know that they resemble the cells of the womb, but we really don’t understand if they behave the same. We had a good inkling that they would behave differently.”
It turned out they did: Cells of endometriosis interacted atypically with female hormones, compared with cells in the uterus, Dr. Lawrenson said.
“That helps us understand how, even when patients take contraceptive pills, which is a commonly prescribed therapy, it doesn’t always work, or sometimes it stops working after a while,” she said. The next step for researchers, she said, will be to pinpoint the specific causes of these altered interactions.
Meanwhile, the current research also points to diagnostic possibilities. “We were quite excited to see that multiple cell types and endometriosis are upregulating the same sets of genes,” she said. “That makes us optimistic that hopefully there are some protein gene products that are being made in abundance, and hopefully we can detect them in the blood stream. It might be that we could use that information to develop new biomarkers, or even risk stratification tools.”
In the future, a simple blood test could identify signs of endometriosis in at-risk patients and get them “fast-tracked to a specialist for evaluation,” she said. “Whereas now, they might go from PCP to gynecologist to a different gynecologist over the course of 5-10 years before they get that referral.”
This discovery, that endometrial cells use genes differently and cross-talk with nearby cells differently, presents new treatment possibilities. Maybe we can physically block how cells interact with nearby cells, Dr. Lawrenson said. One model for doing that, she said, would be antibody-based therapy, similar to the therapies now changing the treatment of cancer.
What’s most exciting, looking ahead 5-10 years, is that treatment for endometriosis in the future may be significantly more individualized, and less hormone-based, than it is today.
“What we need for endometriosis is more options for patients and something that is tailored to the molecular makeup of their disease rather than a process of trial and error,” she said.
Roughly 4 decades after she first started menstruating, Elizabeth Flanagan finally underwent surgery to repair damage wreaked on her body by endometriosis. She’d spent years struggling with a variety of seemingly random symptoms, from migraines to excruciatingly painful periods to fatigue and irritable bowel syndrome. She’d worried about abnormal labs, including “extremely high” ANA, creatinine, and BUN blood test results that had been out of normal range for more than 10 years.
She was diagnosed with endometriosis in 2016, at age 47, after surgery to remove an ovarian cyst. Still, it took 5 more years before she landed in the office of a surgeon with the proper training to excise the lesions that continued to cause her so much anguish. That physician, Matthew Siedhoff, MD, at Cedars-Sinai Medical Center in Los Angeles, explained why her creatinine and BUN results were so far out of range: The endometriosis was impinging on her ureters.
The appointment left Ms. Flanagan with a range of emotions. “I was shocked that no doctor had identified this before, relieved knowing that I was finally in the hands of an expert who understood my condition, and saddened by the dearth of knowledge and proper treatment of endometriosis,” she wrote in an email.
Although the disease afflicts at least 1 out of every 10 women, endometriosis remains a conundrum for patients and their physicians. It often masquerades as other problems, from mental health issues such as anxiety and depression to physical issues such as irritable bowel syndrome. It often coexists with autoimmune conditions. Short of performing surgery, it can be a diagnosis of exclusion. And the existing, state-of-the-art treatment – hormone therapy that shuts down the reproductive system – doesn’t work for every woman every time.
“It is no wonder that it takes 10 years on average, from the time someone has symptoms of endometriosis, until they get a definitive diagnosis,” said Hugh Taylor, MD, chair of obstetrics, gynecology, and reproductive sciences at Yale University, New Haven, Conn. “It’s a combination of [physicians] not taking painful menses seriously and getting distracted by all these other manifestations of the disease throughout the whole body.”
Endometriosis, he said, “is a whole-body disease.”
But recent genetic research offers the tantalizing prospect of new diagnostic tools and treatments. In 5-10 years, scientists say, physicians may be able to diagnose the disease with a simple blood test, and treat it, for example, by preventing a gene receptor from initiating a cascade of inflammatory effects, or crafting treatments tailored to the molecular makeup of a patient’s disease.
“Tomorrow’s therapies will target specifically the molecular defects of endometriosis and be nonhormonal,” Dr. Taylor said.
Guidelines published last year by the European Society of Human Reproduction and Embryology detail the latest standards for diagnosis and treatment of endometriosis.
According to the guidelines, physicians should consider the diagnosis of endometriosis in individuals presenting with the following cyclical and noncyclical signs and symptoms: dysmenorrhea, deep dyspareunia, dysuria, dyschezia, painful rectal bleeding or hematuria, shoulder tip pain, catamenial pneumothorax, cyclical cough/hemoptysis/chest pain, cyclical scar swelling, and pain, fatigue, and infertility.
A clinical exam should be considered, as well as imaging such as ultrasound and/or MRI, the guidelines state, although negative findings should not rule out a diagnosis. Laparoscopy is also an option, particularly for patients who desire a definitive diagnosis or cannot be diagnosed any other way, “although negative histology [of endometriotic lesions] does not entirely rule out the disease,” the guidelines state.
To treat the pain associated with endometriosis, the guidelines advise, as a first-line therapy, beginning with NSAIDs and combined hormonal contraceptives (in oral, vaginal, or transdermal form). Another option is progesterone, including progesterone-only contraceptives, with a recommendation to prescribe a levonorgestrel-releasing intrauterine system or an etonogestrel-releasing subdermal implant to reduce endometriosis-associated pain.
However, progestins and low-dose oral contraceptives are “unsuccessful in a third of women,” Dr. Taylor and his coauthors wrote in a paper published in 2021 in The Lancet.
Until recently, the gold standard for second-line treatment of endometriosis was oral gonadotropin-releasing hormone (GnRH) agonists. These manage the disease by inducing medical menopause – they downregulate pituitary GnRH receptors to create a hypoestrogenic state characterized by low serum levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). GnRH agonists may be administered nasally, or through daily, monthly, or trimonthly injections. But the Food and Drug Administration advises that, when used for longer than 6 months, GnRH agonists be paired with add-back hormone replacement therapy to reduce the risk of bone loss associated with the plunge in hormone levels. Also, treatment may not be appropriate for patients who, when suddenly forced into menopause, suffer from bothersome symptoms.
The latest treatment, GnRH antagonists, are new options for patients who either do not respond adequately to progestins and low-dose contraceptives or develop progesterone resistance, and want to avoid some of the risks and/or symptoms associated with GnRH agonists. Two advantages of GnRH antagonists for patients, Dr. Taylor said, are that they have a fast onset of action and are oral rather than injectable.
“These drugs [GnRH antagonists] cause competitive blockage of the GnRH receptor and hence dose-dependently suppress production of FSH and LH and inhibit secretion of ovarian steroid hormones without inducing a flare-up effect,” Belgian physicians and researchers Jacques Donnez, MD, and Marie-Madeleine Dolmans, MD, PhD, wrote in a paper published last year in the Journal of Clinical Medicine. “The mechanism is different from that of the GnRH agonist which, after a first phase of stimulation, desensitizes GnRH receptors, leading to full suppression of LH and FSH production and subsequently to complete suppression of [estrogen] to levels similar to those observed after bilateral oophorectomy.”
Patients who took Elagolix, the first oral nonpeptide GnRH antagonist available for the treatment of moderate to severe endometriosis-associated pain, had fewer vasomotor side effects and less bone density loss than those on the GnRH agonist leuprorelin, according to a 2018 study in Obstetrics and Gynecology. However, without add-back hormone-replacement therapy, GnRH antagonist use may need to be limited to 24 months, because of loss of bone density, a study in Cell Reports Medicine reported in 2022.
Attempting to explain the pathogenesis of endometriosis, and frustrated by the shortcomings of currently available therapies, researchers have turned to genetics for insight. A team of scientists led by Thomas Tapmeier, PhD, now a senior research fellow at Monash University in Australia, and Prof. Krina Zondervan at the University of Oxford, ran genetic analyses of families with a history of endometriosis, as well as rhesus macaques that spontaneously developed endometriosis. The research, published in Science Translational Medicine, identified NPSR1, the gene encoding neuropeptide S receptor 1, as one commonly associated with endometriosis. In trials with mouse models, they found that the NPSR1 inhibitor SHA 68R was able to reduce endometriosis-related inflammation and pain.
“It’s important to stress that there is no single gene that is responsible for endometriosis,” Dr. Tapmeier said in an interview. “This gene just has a higher frequency in people with endometriosis.”
The next step, then, would be to try to find a compound that would inhibit NPSR1 at some point, or a competitor to the ligand that binds to the receptor and blocks it, he said.
“We’re currently looking at compounds that might be able to inhibit the receptor signaling,” he said.
Such a therapy could potentially reduce the symptoms of endometriosis without interfering with the menstrual cycle and without introducing hormones that cause undesirable side effects in some patients.
“This might be a way to treat the pain and inflammation that goes with endometriosis, as well as leaving the possibility of pregnancy open,” he said.
Other researchers are searching for biomarkers of the disease, both to provide a definitive, nonsurgical diagnostic tool, and for potential, individualized treatment.
In a study published in Nature Genetics, researchers at Cedars-Sinai created a “cellular atlas” of endometriosis by analyzing nearly 400,000 individual cells from 21 patients, some of whom had the disease and some of whom did not. A new technology, single-cell genomics, allowed the scientists to profile the multiple cell types contributing to the disease.
“So the initial question we wanted to ask was about understanding how the cells look in endometriosis, compared to endometrium,” said Kate Lawrenson, PhD, an associate professor in the department of obstetrics and gynecology at Cedars-Sinai, and co–senior author of the study. “We know that they resemble the cells of the womb, but we really don’t understand if they behave the same. We had a good inkling that they would behave differently.”
It turned out they did: Cells of endometriosis interacted atypically with female hormones, compared with cells in the uterus, Dr. Lawrenson said.
“That helps us understand how, even when patients take contraceptive pills, which is a commonly prescribed therapy, it doesn’t always work, or sometimes it stops working after a while,” she said. The next step for researchers, she said, will be to pinpoint the specific causes of these altered interactions.
Meanwhile, the current research also points to diagnostic possibilities. “We were quite excited to see that multiple cell types and endometriosis are upregulating the same sets of genes,” she said. “That makes us optimistic that hopefully there are some protein gene products that are being made in abundance, and hopefully we can detect them in the blood stream. It might be that we could use that information to develop new biomarkers, or even risk stratification tools.”
In the future, a simple blood test could identify signs of endometriosis in at-risk patients and get them “fast-tracked to a specialist for evaluation,” she said. “Whereas now, they might go from PCP to gynecologist to a different gynecologist over the course of 5-10 years before they get that referral.”
This discovery, that endometrial cells use genes differently and cross-talk with nearby cells differently, presents new treatment possibilities. Maybe we can physically block how cells interact with nearby cells, Dr. Lawrenson said. One model for doing that, she said, would be antibody-based therapy, similar to the therapies now changing the treatment of cancer.
What’s most exciting, looking ahead 5-10 years, is that treatment for endometriosis in the future may be significantly more individualized, and less hormone-based, than it is today.
“What we need for endometriosis is more options for patients and something that is tailored to the molecular makeup of their disease rather than a process of trial and error,” she said.
The long-range thrombolysis forecast calls for tiny ultrasonic tornadoes
Sticks and stones may break my bones, but clots will never hurt me
You’ve probably seen “Ghostbusters” or at least heard the theme song. Maybe you even know about the Discovery Channel’s “Mythbusters.” But now there’s a new buster in town, and it eats platitudes for breakfast: Meet Cliche-busters, LOTME’s new recurring feature.
This week, Cliche-busters takes on “Two wrongs don’t make a right.” Yum.
We start with blood clots, which are bad. Doctors go to a lot of trouble to get rid of the things because they are dangerous. A blood clot, then, is a bodily function gone wrong.
Tornadoes are also bad. Out there in the world, these violently rotating columns of air can destroy buildings, toss large objects long distances, and inspire mediocre action movies. They are examples of nature gone wrong.
Seemingly, these two wrongs – blood clots and tornadoes – are not about to make a right. Has Cliche-busters bitten off more than it can chew?
Not according to Xiaoning Jiang of North Carolina State University, Raleigh, and his team of researchers. They’ve figured out a way to use a tiny ultrasonic tornado to break down clots in the brain. “Our new work uses vortex ultrasound, where the ultrasound waves have a helical wavefront. In other words, the ultrasound is swirling as it moves forward,” he said in a statement from the university.
Their new tool’s single transducer is small enough to fit in a catheter, and its “vortex ultrasound-induced shear force has the potential to break down clots safely and improve the efficacy of thrombolysis,” they explained in the open-access journal Research.
The investigators used cow blood in a 3D-printed model of the cerebral venous sinus for the proof-of-concept study and were able to dissolve an acute blood clot in less than 30 minutes, compared with the 15-30 hours needed with a pharmaceutical intervention, according to the written statement.
Can you hear the sound of two wrongs making a right? We can, and that closes the curtain on this cliche.
With age does not come wisdom
We’ve all met this person before. The sort of person who takes a 10-minute IQ test on a shifty-looking website and then proceeds to brag about a 180 IQ until the heat death of the universe. The one who worships at the altar of Mensa. Yeah, that guy. They’re never as smart as they think they are, but they’ll never, ever admit it.
It’s not exactly a secret that IQ as a measurement of intelligence is highly overrated. A lot of scientists doubt we should bother measuring it at all. That said, a higher IQ is associated with greater success in academic and financial endeavors, so it’s not absolutely worthless. And if we’re stuck with it, we may as well study it.
That brings us neatly to new research published in Brain and Behavior. Most studies into IQ and self-estimated intelligence have focused on younger adults, and the author of this study was curious if the stereotype of young men inflating their IQ, a stereotype backed up by research, persisted into older adulthood. So she conducted a survey of 159 younger adults and 152 older adults to find out.
The results in younger adults were not surprising: Younger men overestimated their actual IQ by 5-15 points, which tracks with previous research. We’re in for a bit of a surprise with the older adults, though, because the older men were more humble about their intelligence, with their estimation falling in line with their actual IQ. Older women, however, not so much. In fact, they overestimated their intelligence just as much as the younger men.
In addition, older women who perceived themselves as more attractive reported the highest self-estimated intelligence of all. That isn’t how intelligence works, but honestly, if Grandma’s out and about thinking she looks good and has the brains to go and win “Jeopardy!” do you really have the heart to tell her otherwise?
Fight temptation with empathy … and shoes
Relationships are tough. They all go through their respective ups and downs, but what happens when one person is feeling so down in the partnership that cheating comes to mind? Is there any way to stop it from happening?
Well, a recent study suggests that there is, and it’s as simple as putting yourself in the other person’s shoes. By observing 408 heterosexual, monogamous participants in a series of experiments, psychologists in Israel and New York found that practicing empathy and “perspective taking” doesn’t necessarily stop people from cheating but it does reduces the desire.
People cheat on their significant others for many different reasons – men for a lack of sexual needs being met and women for shortfalls regarding emotional needs – but prioritizing the other person’s perspective gives the idea of being unfaithful a different view and could make one act differently, the investigators said.
Perspective taking also promotes other positive attributes to the relationship, such as the promotion of compassion and the feeling of being understood, lead author Gurit Birnbaum of Reichman University in Herzliya, Israel, said in a written statement. These things ultimately help couples navigate the rough patches and strengthen bonds, making them even less likely to cheat.
The researchers noted that even people in satisfying relationships do cheat, but this approach does encourage people to stop and think before they act. It could ultimately prevent what might be a huge mistake.
Think before they act. Hmm, that’s kind of like look before they leap, right? Sounds like a job for the Cliche-busters.
Sticks and stones may break my bones, but clots will never hurt me
You’ve probably seen “Ghostbusters” or at least heard the theme song. Maybe you even know about the Discovery Channel’s “Mythbusters.” But now there’s a new buster in town, and it eats platitudes for breakfast: Meet Cliche-busters, LOTME’s new recurring feature.
This week, Cliche-busters takes on “Two wrongs don’t make a right.” Yum.
We start with blood clots, which are bad. Doctors go to a lot of trouble to get rid of the things because they are dangerous. A blood clot, then, is a bodily function gone wrong.
Tornadoes are also bad. Out there in the world, these violently rotating columns of air can destroy buildings, toss large objects long distances, and inspire mediocre action movies. They are examples of nature gone wrong.
Seemingly, these two wrongs – blood clots and tornadoes – are not about to make a right. Has Cliche-busters bitten off more than it can chew?
Not according to Xiaoning Jiang of North Carolina State University, Raleigh, and his team of researchers. They’ve figured out a way to use a tiny ultrasonic tornado to break down clots in the brain. “Our new work uses vortex ultrasound, where the ultrasound waves have a helical wavefront. In other words, the ultrasound is swirling as it moves forward,” he said in a statement from the university.
Their new tool’s single transducer is small enough to fit in a catheter, and its “vortex ultrasound-induced shear force has the potential to break down clots safely and improve the efficacy of thrombolysis,” they explained in the open-access journal Research.
The investigators used cow blood in a 3D-printed model of the cerebral venous sinus for the proof-of-concept study and were able to dissolve an acute blood clot in less than 30 minutes, compared with the 15-30 hours needed with a pharmaceutical intervention, according to the written statement.
Can you hear the sound of two wrongs making a right? We can, and that closes the curtain on this cliche.
With age does not come wisdom
We’ve all met this person before. The sort of person who takes a 10-minute IQ test on a shifty-looking website and then proceeds to brag about a 180 IQ until the heat death of the universe. The one who worships at the altar of Mensa. Yeah, that guy. They’re never as smart as they think they are, but they’ll never, ever admit it.
It’s not exactly a secret that IQ as a measurement of intelligence is highly overrated. A lot of scientists doubt we should bother measuring it at all. That said, a higher IQ is associated with greater success in academic and financial endeavors, so it’s not absolutely worthless. And if we’re stuck with it, we may as well study it.
That brings us neatly to new research published in Brain and Behavior. Most studies into IQ and self-estimated intelligence have focused on younger adults, and the author of this study was curious if the stereotype of young men inflating their IQ, a stereotype backed up by research, persisted into older adulthood. So she conducted a survey of 159 younger adults and 152 older adults to find out.
The results in younger adults were not surprising: Younger men overestimated their actual IQ by 5-15 points, which tracks with previous research. We’re in for a bit of a surprise with the older adults, though, because the older men were more humble about their intelligence, with their estimation falling in line with their actual IQ. Older women, however, not so much. In fact, they overestimated their intelligence just as much as the younger men.
In addition, older women who perceived themselves as more attractive reported the highest self-estimated intelligence of all. That isn’t how intelligence works, but honestly, if Grandma’s out and about thinking she looks good and has the brains to go and win “Jeopardy!” do you really have the heart to tell her otherwise?
Fight temptation with empathy … and shoes
Relationships are tough. They all go through their respective ups and downs, but what happens when one person is feeling so down in the partnership that cheating comes to mind? Is there any way to stop it from happening?
Well, a recent study suggests that there is, and it’s as simple as putting yourself in the other person’s shoes. By observing 408 heterosexual, monogamous participants in a series of experiments, psychologists in Israel and New York found that practicing empathy and “perspective taking” doesn’t necessarily stop people from cheating but it does reduces the desire.
People cheat on their significant others for many different reasons – men for a lack of sexual needs being met and women for shortfalls regarding emotional needs – but prioritizing the other person’s perspective gives the idea of being unfaithful a different view and could make one act differently, the investigators said.
Perspective taking also promotes other positive attributes to the relationship, such as the promotion of compassion and the feeling of being understood, lead author Gurit Birnbaum of Reichman University in Herzliya, Israel, said in a written statement. These things ultimately help couples navigate the rough patches and strengthen bonds, making them even less likely to cheat.
The researchers noted that even people in satisfying relationships do cheat, but this approach does encourage people to stop and think before they act. It could ultimately prevent what might be a huge mistake.
Think before they act. Hmm, that’s kind of like look before they leap, right? Sounds like a job for the Cliche-busters.
Sticks and stones may break my bones, but clots will never hurt me
You’ve probably seen “Ghostbusters” or at least heard the theme song. Maybe you even know about the Discovery Channel’s “Mythbusters.” But now there’s a new buster in town, and it eats platitudes for breakfast: Meet Cliche-busters, LOTME’s new recurring feature.
This week, Cliche-busters takes on “Two wrongs don’t make a right.” Yum.
We start with blood clots, which are bad. Doctors go to a lot of trouble to get rid of the things because they are dangerous. A blood clot, then, is a bodily function gone wrong.
Tornadoes are also bad. Out there in the world, these violently rotating columns of air can destroy buildings, toss large objects long distances, and inspire mediocre action movies. They are examples of nature gone wrong.
Seemingly, these two wrongs – blood clots and tornadoes – are not about to make a right. Has Cliche-busters bitten off more than it can chew?
Not according to Xiaoning Jiang of North Carolina State University, Raleigh, and his team of researchers. They’ve figured out a way to use a tiny ultrasonic tornado to break down clots in the brain. “Our new work uses vortex ultrasound, where the ultrasound waves have a helical wavefront. In other words, the ultrasound is swirling as it moves forward,” he said in a statement from the university.
Their new tool’s single transducer is small enough to fit in a catheter, and its “vortex ultrasound-induced shear force has the potential to break down clots safely and improve the efficacy of thrombolysis,” they explained in the open-access journal Research.
The investigators used cow blood in a 3D-printed model of the cerebral venous sinus for the proof-of-concept study and were able to dissolve an acute blood clot in less than 30 minutes, compared with the 15-30 hours needed with a pharmaceutical intervention, according to the written statement.
Can you hear the sound of two wrongs making a right? We can, and that closes the curtain on this cliche.
With age does not come wisdom
We’ve all met this person before. The sort of person who takes a 10-minute IQ test on a shifty-looking website and then proceeds to brag about a 180 IQ until the heat death of the universe. The one who worships at the altar of Mensa. Yeah, that guy. They’re never as smart as they think they are, but they’ll never, ever admit it.
It’s not exactly a secret that IQ as a measurement of intelligence is highly overrated. A lot of scientists doubt we should bother measuring it at all. That said, a higher IQ is associated with greater success in academic and financial endeavors, so it’s not absolutely worthless. And if we’re stuck with it, we may as well study it.
That brings us neatly to new research published in Brain and Behavior. Most studies into IQ and self-estimated intelligence have focused on younger adults, and the author of this study was curious if the stereotype of young men inflating their IQ, a stereotype backed up by research, persisted into older adulthood. So she conducted a survey of 159 younger adults and 152 older adults to find out.
The results in younger adults were not surprising: Younger men overestimated their actual IQ by 5-15 points, which tracks with previous research. We’re in for a bit of a surprise with the older adults, though, because the older men were more humble about their intelligence, with their estimation falling in line with their actual IQ. Older women, however, not so much. In fact, they overestimated their intelligence just as much as the younger men.
In addition, older women who perceived themselves as more attractive reported the highest self-estimated intelligence of all. That isn’t how intelligence works, but honestly, if Grandma’s out and about thinking she looks good and has the brains to go and win “Jeopardy!” do you really have the heart to tell her otherwise?
Fight temptation with empathy … and shoes
Relationships are tough. They all go through their respective ups and downs, but what happens when one person is feeling so down in the partnership that cheating comes to mind? Is there any way to stop it from happening?
Well, a recent study suggests that there is, and it’s as simple as putting yourself in the other person’s shoes. By observing 408 heterosexual, monogamous participants in a series of experiments, psychologists in Israel and New York found that practicing empathy and “perspective taking” doesn’t necessarily stop people from cheating but it does reduces the desire.
People cheat on their significant others for many different reasons – men for a lack of sexual needs being met and women for shortfalls regarding emotional needs – but prioritizing the other person’s perspective gives the idea of being unfaithful a different view and could make one act differently, the investigators said.
Perspective taking also promotes other positive attributes to the relationship, such as the promotion of compassion and the feeling of being understood, lead author Gurit Birnbaum of Reichman University in Herzliya, Israel, said in a written statement. These things ultimately help couples navigate the rough patches and strengthen bonds, making them even less likely to cheat.
The researchers noted that even people in satisfying relationships do cheat, but this approach does encourage people to stop and think before they act. It could ultimately prevent what might be a huge mistake.
Think before they act. Hmm, that’s kind of like look before they leap, right? Sounds like a job for the Cliche-busters.
Exercise halves T2D risk in adults with obesity
“Physical exercise combined with diet restriction has been proven to be effective in prevention of diabetes. However, the long-term effect of exercise on prevention of diabetes, and the difference of exercise intensity in prevention of diabetes have not been well studied,” said corresponding author Xiaoying Li, MD, of Zhongshan Hospital, Fudan University, Shanghai, in an interview.
In the research letter published in JAMA Internal Medicine, Dr. Li and colleagues analyzed the results of a study of 220 adults with central obesity and nonalcoholic fatty liver disease, but no incident diabetes, randomized to a 12-month program of vigorous exercise (73 patients), moderate aerobic exercise (73 patients) or no exercise (74 patients).
A total of 208 participants completed the 1-year intervention; of these, 195 and 178 remained to provide data at 2 years and 10 years, respectively. The mean age of the participants was 53.9 years, 32.3% were male, and the mean waist circumference was 96.1 cm at baseline.
The cumulative incidence of type 2 diabetes in the vigorous exercise, moderate exercise, and nonexercise groups was 2.1 per 100 person-years 1.9 per 100 person-years, and 4.1 per 100 person-years, respectively, over the 10-year follow-up period. This translated to a reduction in type 2 diabetes risk of 49% in the vigorous exercise group and 53% in the moderate exercise group compared with the nonexercise group.
In addition, individuals in the vigorous and moderate exercise groups significantly reduced their HbA1c and waist circumference compared with the nonexercisers. Levels of plasma fasting glucose and weight regain were lower in both exercise groups compared with nonexercisers, but these differences were not significant.
The exercise intervention was described in a 2016 study, which was also published in JAMA Internal Medicine. That study’s purpose was to compare the effects of exercise on patients with nonalcoholic fatty liver disease. Participants were coached and supervised for their exercise programs. The program for the vigorous group involved jogging for 150 minutes per week at 65%-80% of maximum heart rate for 6 months and brisk walking 150 minutes per week at 45%-55% of maximum heart rate for another 6 months. The program for the moderate exercise group involved brisk walking 150 minutes per week for 12 months.
Both exercise groups showed a trend towards higher levels of leisure time physical activity after 10 years compared with the nonexercise groups, although the difference was not significant.
The main limitation of the study was that incident prediabetes was not prespecified, which may have led to some confounding, the researchers noted. In addition, the participants were highly supervised for a 12-month program only. However, the results support the long-term value of physical exercise as a method of obesity management and to delay progression to type 2 diabetes in obese individuals, they said. Vigorous and moderate aerobic exercise programs could be implemented for this patient population, they concluded.
“Surprisingly, our findings demonstrated that a 12-month vigorous aerobic exercise or moderate aerobic exercise could significantly reduce the risk of incident diabetes by 50% over the 10-year follow-up,” Dr. Li said in an interview. The results suggest that physical exercise for some period of time can produce a long-term beneficial effect in prevention of type 2 diabetes, he said.
Potential barriers to the routine use of an exercise intervention in patients with obesity include the unwillingness of this population to engage in vigorous exercise, and the potential for musculoskeletal injury, said Dr. Li. In these cases, obese patients should be encouraged to pursue moderate exercise, Dr. Li said.
Looking ahead, more research is needed to examine the potential mechanism behind the effect of exercise on diabetes prevention, said Dr. Li.
Findings fill gap in long-term outcome data
The current study is important because of the long-term follow-up data, said Jill Kanaley, PhD, professor and interim chair of nutrition and exercise physiology at the University of Missouri, in an interview. “We seldom follow up on our training studies, thus it is important to see if there is any long-term impact of these interventions,” she said.
Dr. Kanaley said she was surprised to see the residual benefits of the exercise intervention 10 years later.
“We often wonder how long the impact of the exercise training will stay with someone so that they continue to exercise and watch their weight; this study seems to indicate that there is an educational component that stays with them,” she said.
The main clinical takeaway from the current study was the minimal weight gain over time, Dr. Kanaley said.
Although time may be a barrier to the routine use of an exercise intervention, patients have to realize that they can usually find the time, especially given the multiple benefits, said Dr. Kanaley. “The exercise interventions provide more benefits than just weight control and glucose levels,” she said.
“The 30-60 minutes of exercise does not have to come all at the same time,” Dr. Kanaley noted. “It could be three 15-minute bouts of exercise/physical activity to get their 45 minutes in,” she noted. Exercise does not have to be heavy vigorous exercise, even walking is beneficial, she said. For people who complain of boredom with an exercise routine, Dr. Kanaley encourages mixing it up, with activities such as different exercise classes, running, or walking on a different day of any given week.
Although the current study was conducted in China, the findings may translate to a U.S. population, Dr. Kanaley said in an interview. However, “frequently our Western diet is less healthy than the traditional Chinese diet. This may have provided an immeasurable benefit to these subjects,” although study participants did not make specific adjustments to their diets, she said.
Additional research is needed to confirm the findings, said Dr. Kanaley. “Ideally, the study should be repeated in a population with a Western diet,” she noted.
Next steps for research include maintenance of activity
Evidence on the long-term benefits of exercise programs is limited, said Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, in an interview.
“Chronic diseases such as diabetes can take years to develop, so understanding these important health outcomes requires years of follow-up. This study followed their study participants for 10 years, which gives us a nice glimpse of the long-term benefits of exercise training on diabetes prevention,” she said.
Data from previous observational studies of individuals’ current activity levels (without an intervention) suggest that adults who are more physically active have a lower risk of diabetes over time, said Dr. Paluch. However, the current study is one of the few with rigorous exercise interventions with extensive follow-up on diabetes risk, and it provides important evidence that a 12-month structured exercise program in inactive adults with obesity can result in meaningful long-term health benefits by lowering the risk of diabetes, she said.
“The individuals in the current study participated in a structured exercise program where their exercise sessions were supervised and coached,” Dr. Paluch noted. “Having a personalized coach may not be within the budget or time constraints for many people,” she said. Her message to clinicians for their patients: “When looking to start an exercise routine, identify an activity you enjoy and find feasible to fit into your existing life and schedule,” she said.
“Although this study was conducted in China, the results are meaningful for the U.S. population, as we would expect the physiological benefit of exercise to be consistent across various populations,” Dr. Paluch said. “However, there are certainly differences across countries at the individual level to the larger community-wide level that may influence a person’s ability to maintain physical activity and prevent diabetes, so replicating similar studies in other countries, including the U.S., would be of value.”
“Additionally, we need more research on how to encourage maintenance of physical activity in the long-term, after the initial exercise program is over,” she said.
“From this current study, we cannot tease out whether diabetes risk is reduced because of the 12-month exercise intervention or the benefit is from maintaining physical activity regularly over the 10 years of follow-up, or a combination of the two,” said Dr. Paluch. Future studies should consider teasing out participants who were only active during the exercise intervention, then ceased being active vs. participants who continued with vigorous activity long-term, she said.
The study was supported by the National Nature Science Foundation, the National Key Research and Development Program of China, and the Shanghai Municipal Science and Technology Major Project. The researchers, Dr. Kanaley, and Dr. Paluch had no financial conflicts to disclose.
“Physical exercise combined with diet restriction has been proven to be effective in prevention of diabetes. However, the long-term effect of exercise on prevention of diabetes, and the difference of exercise intensity in prevention of diabetes have not been well studied,” said corresponding author Xiaoying Li, MD, of Zhongshan Hospital, Fudan University, Shanghai, in an interview.
In the research letter published in JAMA Internal Medicine, Dr. Li and colleagues analyzed the results of a study of 220 adults with central obesity and nonalcoholic fatty liver disease, but no incident diabetes, randomized to a 12-month program of vigorous exercise (73 patients), moderate aerobic exercise (73 patients) or no exercise (74 patients).
A total of 208 participants completed the 1-year intervention; of these, 195 and 178 remained to provide data at 2 years and 10 years, respectively. The mean age of the participants was 53.9 years, 32.3% were male, and the mean waist circumference was 96.1 cm at baseline.
The cumulative incidence of type 2 diabetes in the vigorous exercise, moderate exercise, and nonexercise groups was 2.1 per 100 person-years 1.9 per 100 person-years, and 4.1 per 100 person-years, respectively, over the 10-year follow-up period. This translated to a reduction in type 2 diabetes risk of 49% in the vigorous exercise group and 53% in the moderate exercise group compared with the nonexercise group.
In addition, individuals in the vigorous and moderate exercise groups significantly reduced their HbA1c and waist circumference compared with the nonexercisers. Levels of plasma fasting glucose and weight regain were lower in both exercise groups compared with nonexercisers, but these differences were not significant.
The exercise intervention was described in a 2016 study, which was also published in JAMA Internal Medicine. That study’s purpose was to compare the effects of exercise on patients with nonalcoholic fatty liver disease. Participants were coached and supervised for their exercise programs. The program for the vigorous group involved jogging for 150 minutes per week at 65%-80% of maximum heart rate for 6 months and brisk walking 150 minutes per week at 45%-55% of maximum heart rate for another 6 months. The program for the moderate exercise group involved brisk walking 150 minutes per week for 12 months.
Both exercise groups showed a trend towards higher levels of leisure time physical activity after 10 years compared with the nonexercise groups, although the difference was not significant.
The main limitation of the study was that incident prediabetes was not prespecified, which may have led to some confounding, the researchers noted. In addition, the participants were highly supervised for a 12-month program only. However, the results support the long-term value of physical exercise as a method of obesity management and to delay progression to type 2 diabetes in obese individuals, they said. Vigorous and moderate aerobic exercise programs could be implemented for this patient population, they concluded.
“Surprisingly, our findings demonstrated that a 12-month vigorous aerobic exercise or moderate aerobic exercise could significantly reduce the risk of incident diabetes by 50% over the 10-year follow-up,” Dr. Li said in an interview. The results suggest that physical exercise for some period of time can produce a long-term beneficial effect in prevention of type 2 diabetes, he said.
Potential barriers to the routine use of an exercise intervention in patients with obesity include the unwillingness of this population to engage in vigorous exercise, and the potential for musculoskeletal injury, said Dr. Li. In these cases, obese patients should be encouraged to pursue moderate exercise, Dr. Li said.
Looking ahead, more research is needed to examine the potential mechanism behind the effect of exercise on diabetes prevention, said Dr. Li.
Findings fill gap in long-term outcome data
The current study is important because of the long-term follow-up data, said Jill Kanaley, PhD, professor and interim chair of nutrition and exercise physiology at the University of Missouri, in an interview. “We seldom follow up on our training studies, thus it is important to see if there is any long-term impact of these interventions,” she said.
Dr. Kanaley said she was surprised to see the residual benefits of the exercise intervention 10 years later.
“We often wonder how long the impact of the exercise training will stay with someone so that they continue to exercise and watch their weight; this study seems to indicate that there is an educational component that stays with them,” she said.
The main clinical takeaway from the current study was the minimal weight gain over time, Dr. Kanaley said.
Although time may be a barrier to the routine use of an exercise intervention, patients have to realize that they can usually find the time, especially given the multiple benefits, said Dr. Kanaley. “The exercise interventions provide more benefits than just weight control and glucose levels,” she said.
“The 30-60 minutes of exercise does not have to come all at the same time,” Dr. Kanaley noted. “It could be three 15-minute bouts of exercise/physical activity to get their 45 minutes in,” she noted. Exercise does not have to be heavy vigorous exercise, even walking is beneficial, she said. For people who complain of boredom with an exercise routine, Dr. Kanaley encourages mixing it up, with activities such as different exercise classes, running, or walking on a different day of any given week.
Although the current study was conducted in China, the findings may translate to a U.S. population, Dr. Kanaley said in an interview. However, “frequently our Western diet is less healthy than the traditional Chinese diet. This may have provided an immeasurable benefit to these subjects,” although study participants did not make specific adjustments to their diets, she said.
Additional research is needed to confirm the findings, said Dr. Kanaley. “Ideally, the study should be repeated in a population with a Western diet,” she noted.
Next steps for research include maintenance of activity
Evidence on the long-term benefits of exercise programs is limited, said Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, in an interview.
“Chronic diseases such as diabetes can take years to develop, so understanding these important health outcomes requires years of follow-up. This study followed their study participants for 10 years, which gives us a nice glimpse of the long-term benefits of exercise training on diabetes prevention,” she said.
Data from previous observational studies of individuals’ current activity levels (without an intervention) suggest that adults who are more physically active have a lower risk of diabetes over time, said Dr. Paluch. However, the current study is one of the few with rigorous exercise interventions with extensive follow-up on diabetes risk, and it provides important evidence that a 12-month structured exercise program in inactive adults with obesity can result in meaningful long-term health benefits by lowering the risk of diabetes, she said.
“The individuals in the current study participated in a structured exercise program where their exercise sessions were supervised and coached,” Dr. Paluch noted. “Having a personalized coach may not be within the budget or time constraints for many people,” she said. Her message to clinicians for their patients: “When looking to start an exercise routine, identify an activity you enjoy and find feasible to fit into your existing life and schedule,” she said.
“Although this study was conducted in China, the results are meaningful for the U.S. population, as we would expect the physiological benefit of exercise to be consistent across various populations,” Dr. Paluch said. “However, there are certainly differences across countries at the individual level to the larger community-wide level that may influence a person’s ability to maintain physical activity and prevent diabetes, so replicating similar studies in other countries, including the U.S., would be of value.”
“Additionally, we need more research on how to encourage maintenance of physical activity in the long-term, after the initial exercise program is over,” she said.
“From this current study, we cannot tease out whether diabetes risk is reduced because of the 12-month exercise intervention or the benefit is from maintaining physical activity regularly over the 10 years of follow-up, or a combination of the two,” said Dr. Paluch. Future studies should consider teasing out participants who were only active during the exercise intervention, then ceased being active vs. participants who continued with vigorous activity long-term, she said.
The study was supported by the National Nature Science Foundation, the National Key Research and Development Program of China, and the Shanghai Municipal Science and Technology Major Project. The researchers, Dr. Kanaley, and Dr. Paluch had no financial conflicts to disclose.
“Physical exercise combined with diet restriction has been proven to be effective in prevention of diabetes. However, the long-term effect of exercise on prevention of diabetes, and the difference of exercise intensity in prevention of diabetes have not been well studied,” said corresponding author Xiaoying Li, MD, of Zhongshan Hospital, Fudan University, Shanghai, in an interview.
In the research letter published in JAMA Internal Medicine, Dr. Li and colleagues analyzed the results of a study of 220 adults with central obesity and nonalcoholic fatty liver disease, but no incident diabetes, randomized to a 12-month program of vigorous exercise (73 patients), moderate aerobic exercise (73 patients) or no exercise (74 patients).
A total of 208 participants completed the 1-year intervention; of these, 195 and 178 remained to provide data at 2 years and 10 years, respectively. The mean age of the participants was 53.9 years, 32.3% were male, and the mean waist circumference was 96.1 cm at baseline.
The cumulative incidence of type 2 diabetes in the vigorous exercise, moderate exercise, and nonexercise groups was 2.1 per 100 person-years 1.9 per 100 person-years, and 4.1 per 100 person-years, respectively, over the 10-year follow-up period. This translated to a reduction in type 2 diabetes risk of 49% in the vigorous exercise group and 53% in the moderate exercise group compared with the nonexercise group.
In addition, individuals in the vigorous and moderate exercise groups significantly reduced their HbA1c and waist circumference compared with the nonexercisers. Levels of plasma fasting glucose and weight regain were lower in both exercise groups compared with nonexercisers, but these differences were not significant.
The exercise intervention was described in a 2016 study, which was also published in JAMA Internal Medicine. That study’s purpose was to compare the effects of exercise on patients with nonalcoholic fatty liver disease. Participants were coached and supervised for their exercise programs. The program for the vigorous group involved jogging for 150 minutes per week at 65%-80% of maximum heart rate for 6 months and brisk walking 150 minutes per week at 45%-55% of maximum heart rate for another 6 months. The program for the moderate exercise group involved brisk walking 150 minutes per week for 12 months.
Both exercise groups showed a trend towards higher levels of leisure time physical activity after 10 years compared with the nonexercise groups, although the difference was not significant.
The main limitation of the study was that incident prediabetes was not prespecified, which may have led to some confounding, the researchers noted. In addition, the participants were highly supervised for a 12-month program only. However, the results support the long-term value of physical exercise as a method of obesity management and to delay progression to type 2 diabetes in obese individuals, they said. Vigorous and moderate aerobic exercise programs could be implemented for this patient population, they concluded.
“Surprisingly, our findings demonstrated that a 12-month vigorous aerobic exercise or moderate aerobic exercise could significantly reduce the risk of incident diabetes by 50% over the 10-year follow-up,” Dr. Li said in an interview. The results suggest that physical exercise for some period of time can produce a long-term beneficial effect in prevention of type 2 diabetes, he said.
Potential barriers to the routine use of an exercise intervention in patients with obesity include the unwillingness of this population to engage in vigorous exercise, and the potential for musculoskeletal injury, said Dr. Li. In these cases, obese patients should be encouraged to pursue moderate exercise, Dr. Li said.
Looking ahead, more research is needed to examine the potential mechanism behind the effect of exercise on diabetes prevention, said Dr. Li.
Findings fill gap in long-term outcome data
The current study is important because of the long-term follow-up data, said Jill Kanaley, PhD, professor and interim chair of nutrition and exercise physiology at the University of Missouri, in an interview. “We seldom follow up on our training studies, thus it is important to see if there is any long-term impact of these interventions,” she said.
Dr. Kanaley said she was surprised to see the residual benefits of the exercise intervention 10 years later.
“We often wonder how long the impact of the exercise training will stay with someone so that they continue to exercise and watch their weight; this study seems to indicate that there is an educational component that stays with them,” she said.
The main clinical takeaway from the current study was the minimal weight gain over time, Dr. Kanaley said.
Although time may be a barrier to the routine use of an exercise intervention, patients have to realize that they can usually find the time, especially given the multiple benefits, said Dr. Kanaley. “The exercise interventions provide more benefits than just weight control and glucose levels,” she said.
“The 30-60 minutes of exercise does not have to come all at the same time,” Dr. Kanaley noted. “It could be three 15-minute bouts of exercise/physical activity to get their 45 minutes in,” she noted. Exercise does not have to be heavy vigorous exercise, even walking is beneficial, she said. For people who complain of boredom with an exercise routine, Dr. Kanaley encourages mixing it up, with activities such as different exercise classes, running, or walking on a different day of any given week.
Although the current study was conducted in China, the findings may translate to a U.S. population, Dr. Kanaley said in an interview. However, “frequently our Western diet is less healthy than the traditional Chinese diet. This may have provided an immeasurable benefit to these subjects,” although study participants did not make specific adjustments to their diets, she said.
Additional research is needed to confirm the findings, said Dr. Kanaley. “Ideally, the study should be repeated in a population with a Western diet,” she noted.
Next steps for research include maintenance of activity
Evidence on the long-term benefits of exercise programs is limited, said Amanda Paluch, PhD, a physical activity epidemiologist at the University of Massachusetts, Amherst, in an interview.
“Chronic diseases such as diabetes can take years to develop, so understanding these important health outcomes requires years of follow-up. This study followed their study participants for 10 years, which gives us a nice glimpse of the long-term benefits of exercise training on diabetes prevention,” she said.
Data from previous observational studies of individuals’ current activity levels (without an intervention) suggest that adults who are more physically active have a lower risk of diabetes over time, said Dr. Paluch. However, the current study is one of the few with rigorous exercise interventions with extensive follow-up on diabetes risk, and it provides important evidence that a 12-month structured exercise program in inactive adults with obesity can result in meaningful long-term health benefits by lowering the risk of diabetes, she said.
“The individuals in the current study participated in a structured exercise program where their exercise sessions were supervised and coached,” Dr. Paluch noted. “Having a personalized coach may not be within the budget or time constraints for many people,” she said. Her message to clinicians for their patients: “When looking to start an exercise routine, identify an activity you enjoy and find feasible to fit into your existing life and schedule,” she said.
“Although this study was conducted in China, the results are meaningful for the U.S. population, as we would expect the physiological benefit of exercise to be consistent across various populations,” Dr. Paluch said. “However, there are certainly differences across countries at the individual level to the larger community-wide level that may influence a person’s ability to maintain physical activity and prevent diabetes, so replicating similar studies in other countries, including the U.S., would be of value.”
“Additionally, we need more research on how to encourage maintenance of physical activity in the long-term, after the initial exercise program is over,” she said.
“From this current study, we cannot tease out whether diabetes risk is reduced because of the 12-month exercise intervention or the benefit is from maintaining physical activity regularly over the 10 years of follow-up, or a combination of the two,” said Dr. Paluch. Future studies should consider teasing out participants who were only active during the exercise intervention, then ceased being active vs. participants who continued with vigorous activity long-term, she said.
The study was supported by the National Nature Science Foundation, the National Key Research and Development Program of China, and the Shanghai Municipal Science and Technology Major Project. The researchers, Dr. Kanaley, and Dr. Paluch had no financial conflicts to disclose.
FROM JAMA INTERNAL MEDICINE
Massive rise in drug overdose deaths driven by opioids
The 376% represents the change in age-adjusted overdose deaths per 100,000 population, which went from 6.9 in 2001 to 32.4 in 2021, as the total number of deaths rose from 19,394 to 106,699 (450%) over that time period, the NCHS said in a recent data brief. That total made 2021 the first year ever with more than 100,000 overdose deaths.
Since the age-adjusted rate stood at 21.6 per 100,000 in 2019, that means 42% of the total increase over 20 years actually occurred in 2020 and 2021. The number of deaths increased by about 36,000 over those 2 years, accounting for 41% of the total annual increase from 2001 to 2021, based on data from the National Vital Statistics System mortality files.
The overdose death rate was significantly higher for males than females for all of the years from 2001 to 2021, with males seeing an increase from 9.0 to 45.1 per 100,000 and females going from 4.6 to 19.6 deaths per 100,000. In the single year from 2020 to 2021, the age-adjusted rate was up by 14% for males and 15% for females, the mortality-file data show.
Analysis by age showed an even larger effect in some groups from 2020 to 2021. Drug overdose deaths jumped 28% among adults aged 65 years and older, more than any other group, and by 21% in those aged 55-64 years, according to the NCHS.
The only age group for which deaths didn’t increase significantly from 2020 to 2021 was 15- to 24-year-olds, whose rate rose by just 3%. The age group with the highest rate in both 2020 and 2021, however, was the 35- to 44-year-olds: 53.9 and 62.0 overdose deaths per 100,000, respectively, for an increase of 15%, the NCHS said in the report.
The drugs now involved in overdose deaths are most often opioids, a change from 2001. That year, opioids were involved in 49% of all overdose deaths, but by 2021 that share had increased to 75%. The trend for opioid-related deaths almost matches that of overall deaths over the 20-year span, and the significantly increasing trend that began for all overdose deaths in 2013 closely follows that of synthetic opioids such as fentanyl and tramadol, the report shows.
Overdose deaths involving cocaine and psychostimulants such as methamphetamine, amphetamine, and methylphenidate also show similar increases. The cocaine-related death rate rose 22% from 2020 to 2021 and is up by 421% since 2012, while the corresponding increases for psychostimulant deaths were 33% and 2,400%, the NCHS said.
The 376% represents the change in age-adjusted overdose deaths per 100,000 population, which went from 6.9 in 2001 to 32.4 in 2021, as the total number of deaths rose from 19,394 to 106,699 (450%) over that time period, the NCHS said in a recent data brief. That total made 2021 the first year ever with more than 100,000 overdose deaths.
Since the age-adjusted rate stood at 21.6 per 100,000 in 2019, that means 42% of the total increase over 20 years actually occurred in 2020 and 2021. The number of deaths increased by about 36,000 over those 2 years, accounting for 41% of the total annual increase from 2001 to 2021, based on data from the National Vital Statistics System mortality files.
The overdose death rate was significantly higher for males than females for all of the years from 2001 to 2021, with males seeing an increase from 9.0 to 45.1 per 100,000 and females going from 4.6 to 19.6 deaths per 100,000. In the single year from 2020 to 2021, the age-adjusted rate was up by 14% for males and 15% for females, the mortality-file data show.
Analysis by age showed an even larger effect in some groups from 2020 to 2021. Drug overdose deaths jumped 28% among adults aged 65 years and older, more than any other group, and by 21% in those aged 55-64 years, according to the NCHS.
The only age group for which deaths didn’t increase significantly from 2020 to 2021 was 15- to 24-year-olds, whose rate rose by just 3%. The age group with the highest rate in both 2020 and 2021, however, was the 35- to 44-year-olds: 53.9 and 62.0 overdose deaths per 100,000, respectively, for an increase of 15%, the NCHS said in the report.
The drugs now involved in overdose deaths are most often opioids, a change from 2001. That year, opioids were involved in 49% of all overdose deaths, but by 2021 that share had increased to 75%. The trend for opioid-related deaths almost matches that of overall deaths over the 20-year span, and the significantly increasing trend that began for all overdose deaths in 2013 closely follows that of synthetic opioids such as fentanyl and tramadol, the report shows.
Overdose deaths involving cocaine and psychostimulants such as methamphetamine, amphetamine, and methylphenidate also show similar increases. The cocaine-related death rate rose 22% from 2020 to 2021 and is up by 421% since 2012, while the corresponding increases for psychostimulant deaths were 33% and 2,400%, the NCHS said.
The 376% represents the change in age-adjusted overdose deaths per 100,000 population, which went from 6.9 in 2001 to 32.4 in 2021, as the total number of deaths rose from 19,394 to 106,699 (450%) over that time period, the NCHS said in a recent data brief. That total made 2021 the first year ever with more than 100,000 overdose deaths.
Since the age-adjusted rate stood at 21.6 per 100,000 in 2019, that means 42% of the total increase over 20 years actually occurred in 2020 and 2021. The number of deaths increased by about 36,000 over those 2 years, accounting for 41% of the total annual increase from 2001 to 2021, based on data from the National Vital Statistics System mortality files.
The overdose death rate was significantly higher for males than females for all of the years from 2001 to 2021, with males seeing an increase from 9.0 to 45.1 per 100,000 and females going from 4.6 to 19.6 deaths per 100,000. In the single year from 2020 to 2021, the age-adjusted rate was up by 14% for males and 15% for females, the mortality-file data show.
Analysis by age showed an even larger effect in some groups from 2020 to 2021. Drug overdose deaths jumped 28% among adults aged 65 years and older, more than any other group, and by 21% in those aged 55-64 years, according to the NCHS.
The only age group for which deaths didn’t increase significantly from 2020 to 2021 was 15- to 24-year-olds, whose rate rose by just 3%. The age group with the highest rate in both 2020 and 2021, however, was the 35- to 44-year-olds: 53.9 and 62.0 overdose deaths per 100,000, respectively, for an increase of 15%, the NCHS said in the report.
The drugs now involved in overdose deaths are most often opioids, a change from 2001. That year, opioids were involved in 49% of all overdose deaths, but by 2021 that share had increased to 75%. The trend for opioid-related deaths almost matches that of overall deaths over the 20-year span, and the significantly increasing trend that began for all overdose deaths in 2013 closely follows that of synthetic opioids such as fentanyl and tramadol, the report shows.
Overdose deaths involving cocaine and psychostimulants such as methamphetamine, amphetamine, and methylphenidate also show similar increases. The cocaine-related death rate rose 22% from 2020 to 2021 and is up by 421% since 2012, while the corresponding increases for psychostimulant deaths were 33% and 2,400%, the NCHS said.
Washington medical board charges doctor with spreading COVID misinformation
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Difficulty fitting family into career: Female oncologists
In a survey of just over 1,000 female oncologists, 95% said their career plans were at least somewhat associated with the timing of when to start a family.
The most striking finding was that one third of respondents had miscarried and another one third reported difficulty with infertility that required fertility counseling and/or treatment.
One third reported experiencing discrimination during pregnancy, and another third said they experienced discrimination for taking maternity leave, and having more than one child increased the likelihood of this.
The most common negative factor associated with family planning was long work hours and heavy workload (66.6%),
These findings suggest there are systemic changes needed not only in the healthcare setting but in society as a whole around women in the workplace and their choices of childbearing, say the authors.
The study was published online in JAMA Network Open and led by Anna Lee MD, MPH, from the department of radiation oncology, University of Texas MD Anderson Cancer Center, Houston.
In an invited commentary, Mona Saleh, MD, and Stephanie Blank, MD, from the department of obstetrics, gynecology, and reproductive science at the Icahn School of Medicine at Mount Sinai in New York, suggest that cultural changes are needed that go beyond women in medicine.
“These cultural values are so deeply pervasive (one could also say invasive) that they affect even these most educated and wealthy professional women, such as those who participated in this survey,” the editorialists write.
“[The researchers] advocate for early education on assisted reproductive technology (ART) risks, benefits, and success rates, but this is not getting at the underlying issue: Pregnancy discrimination and unfair distribution of childbearing responsibilities are a reflection of a larger problematic culture rather than an issue specific to women in medicine,” they add.
Survey details
The survey comprised a novel 39-item questionnaire distributed to 1,004 U.S. female oncologists from May 7 to June 30, 2020, via email and social media channels.
Most respondents (84.4%) were married, and 71% were currently working full-time.
About one-third (35%) worked in radiation oncology, another third (34.3%) in medical oncology, 18.4% in surgical oncology, and 9.1% in pediatric oncology.
A total of 768 respondents (76.5%) had children, and of these, 415 (41.3%) first gave birth during postgraduate training and 275 (27.4%) gave birth in years 1-5 as an attending physician.
Of all respondents who had been pregnant, approximately two-thirds (65.7%) had some type of pregnancy complication. About one-third of respondents (31.7%) reported having experienced a miscarriage after a confirmed pregnancy; of those, 61.6% reported one miscarriage, while the remainder had two or more miscarriages (38.4%).
Approximately one-third (31.4%) of respondents reported difficulty with infertility that required fertility counseling and/or treatment.
The questionnaire also asked about assisted reproductive technology, and 164 participants (16.3%) reported the use of fertility medications, and 53 (5.3%) reported cryopreservation of eggs. Nearly 13% reported the use of intrauterine insemination and 13.2% reported the use of in vivo fertilization. Among those who experienced fertility concerns, 36.6% (232 of 634) reported facing financial burdens because of fertility or pregnancy that was in some way associated with their career choice.
When asked on the survey if fertility preservation should be discussed with women during medical school and/or residency, 65.7% of respondents stated that it should.
However, the editorialists suggest that “encouraging formal and directed education regarding the infertility risks specifically toward female physicians (which Lee et al. recommend) could be perceived as a blanket recommendation that it is best for women in medicine to delay childbearing and pursue ART.”
“Medical schools and residency and fellowship training programs should instead focus their energy on creating a framework and culture that normalizes conception during these points in training while also subsidizing and supporting trainees and physicians who prefer to use ART and delay fertility until after training,” they suggest.
The editorialists also emphasized that women may choose to become pregnant at any point during the years that it takes to go from being a medical student to resident/fellow to attending physician, and they should be supported by their workplace on their decisions.
The study was funded by grants from National Institutes of Health/National Cancer Institute Cancer Center.
Dr. Lee and coauthors reported no relevant financial relationships. Dr. Blank reported receiving grants from AstraZeneca, Aravive, Akesobio, GlaxoSmithKline, Merck, and Seattle Genetics outside the submitted work. Dr. Saleh reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a survey of just over 1,000 female oncologists, 95% said their career plans were at least somewhat associated with the timing of when to start a family.
The most striking finding was that one third of respondents had miscarried and another one third reported difficulty with infertility that required fertility counseling and/or treatment.
One third reported experiencing discrimination during pregnancy, and another third said they experienced discrimination for taking maternity leave, and having more than one child increased the likelihood of this.
The most common negative factor associated with family planning was long work hours and heavy workload (66.6%),
These findings suggest there are systemic changes needed not only in the healthcare setting but in society as a whole around women in the workplace and their choices of childbearing, say the authors.
The study was published online in JAMA Network Open and led by Anna Lee MD, MPH, from the department of radiation oncology, University of Texas MD Anderson Cancer Center, Houston.
In an invited commentary, Mona Saleh, MD, and Stephanie Blank, MD, from the department of obstetrics, gynecology, and reproductive science at the Icahn School of Medicine at Mount Sinai in New York, suggest that cultural changes are needed that go beyond women in medicine.
“These cultural values are so deeply pervasive (one could also say invasive) that they affect even these most educated and wealthy professional women, such as those who participated in this survey,” the editorialists write.
“[The researchers] advocate for early education on assisted reproductive technology (ART) risks, benefits, and success rates, but this is not getting at the underlying issue: Pregnancy discrimination and unfair distribution of childbearing responsibilities are a reflection of a larger problematic culture rather than an issue specific to women in medicine,” they add.
Survey details
The survey comprised a novel 39-item questionnaire distributed to 1,004 U.S. female oncologists from May 7 to June 30, 2020, via email and social media channels.
Most respondents (84.4%) were married, and 71% were currently working full-time.
About one-third (35%) worked in radiation oncology, another third (34.3%) in medical oncology, 18.4% in surgical oncology, and 9.1% in pediatric oncology.
A total of 768 respondents (76.5%) had children, and of these, 415 (41.3%) first gave birth during postgraduate training and 275 (27.4%) gave birth in years 1-5 as an attending physician.
Of all respondents who had been pregnant, approximately two-thirds (65.7%) had some type of pregnancy complication. About one-third of respondents (31.7%) reported having experienced a miscarriage after a confirmed pregnancy; of those, 61.6% reported one miscarriage, while the remainder had two or more miscarriages (38.4%).
Approximately one-third (31.4%) of respondents reported difficulty with infertility that required fertility counseling and/or treatment.
The questionnaire also asked about assisted reproductive technology, and 164 participants (16.3%) reported the use of fertility medications, and 53 (5.3%) reported cryopreservation of eggs. Nearly 13% reported the use of intrauterine insemination and 13.2% reported the use of in vivo fertilization. Among those who experienced fertility concerns, 36.6% (232 of 634) reported facing financial burdens because of fertility or pregnancy that was in some way associated with their career choice.
When asked on the survey if fertility preservation should be discussed with women during medical school and/or residency, 65.7% of respondents stated that it should.
However, the editorialists suggest that “encouraging formal and directed education regarding the infertility risks specifically toward female physicians (which Lee et al. recommend) could be perceived as a blanket recommendation that it is best for women in medicine to delay childbearing and pursue ART.”
“Medical schools and residency and fellowship training programs should instead focus their energy on creating a framework and culture that normalizes conception during these points in training while also subsidizing and supporting trainees and physicians who prefer to use ART and delay fertility until after training,” they suggest.
The editorialists also emphasized that women may choose to become pregnant at any point during the years that it takes to go from being a medical student to resident/fellow to attending physician, and they should be supported by their workplace on their decisions.
The study was funded by grants from National Institutes of Health/National Cancer Institute Cancer Center.
Dr. Lee and coauthors reported no relevant financial relationships. Dr. Blank reported receiving grants from AstraZeneca, Aravive, Akesobio, GlaxoSmithKline, Merck, and Seattle Genetics outside the submitted work. Dr. Saleh reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a survey of just over 1,000 female oncologists, 95% said their career plans were at least somewhat associated with the timing of when to start a family.
The most striking finding was that one third of respondents had miscarried and another one third reported difficulty with infertility that required fertility counseling and/or treatment.
One third reported experiencing discrimination during pregnancy, and another third said they experienced discrimination for taking maternity leave, and having more than one child increased the likelihood of this.
The most common negative factor associated with family planning was long work hours and heavy workload (66.6%),
These findings suggest there are systemic changes needed not only in the healthcare setting but in society as a whole around women in the workplace and their choices of childbearing, say the authors.
The study was published online in JAMA Network Open and led by Anna Lee MD, MPH, from the department of radiation oncology, University of Texas MD Anderson Cancer Center, Houston.
In an invited commentary, Mona Saleh, MD, and Stephanie Blank, MD, from the department of obstetrics, gynecology, and reproductive science at the Icahn School of Medicine at Mount Sinai in New York, suggest that cultural changes are needed that go beyond women in medicine.
“These cultural values are so deeply pervasive (one could also say invasive) that they affect even these most educated and wealthy professional women, such as those who participated in this survey,” the editorialists write.
“[The researchers] advocate for early education on assisted reproductive technology (ART) risks, benefits, and success rates, but this is not getting at the underlying issue: Pregnancy discrimination and unfair distribution of childbearing responsibilities are a reflection of a larger problematic culture rather than an issue specific to women in medicine,” they add.
Survey details
The survey comprised a novel 39-item questionnaire distributed to 1,004 U.S. female oncologists from May 7 to June 30, 2020, via email and social media channels.
Most respondents (84.4%) were married, and 71% were currently working full-time.
About one-third (35%) worked in radiation oncology, another third (34.3%) in medical oncology, 18.4% in surgical oncology, and 9.1% in pediatric oncology.
A total of 768 respondents (76.5%) had children, and of these, 415 (41.3%) first gave birth during postgraduate training and 275 (27.4%) gave birth in years 1-5 as an attending physician.
Of all respondents who had been pregnant, approximately two-thirds (65.7%) had some type of pregnancy complication. About one-third of respondents (31.7%) reported having experienced a miscarriage after a confirmed pregnancy; of those, 61.6% reported one miscarriage, while the remainder had two or more miscarriages (38.4%).
Approximately one-third (31.4%) of respondents reported difficulty with infertility that required fertility counseling and/or treatment.
The questionnaire also asked about assisted reproductive technology, and 164 participants (16.3%) reported the use of fertility medications, and 53 (5.3%) reported cryopreservation of eggs. Nearly 13% reported the use of intrauterine insemination and 13.2% reported the use of in vivo fertilization. Among those who experienced fertility concerns, 36.6% (232 of 634) reported facing financial burdens because of fertility or pregnancy that was in some way associated with their career choice.
When asked on the survey if fertility preservation should be discussed with women during medical school and/or residency, 65.7% of respondents stated that it should.
However, the editorialists suggest that “encouraging formal and directed education regarding the infertility risks specifically toward female physicians (which Lee et al. recommend) could be perceived as a blanket recommendation that it is best for women in medicine to delay childbearing and pursue ART.”
“Medical schools and residency and fellowship training programs should instead focus their energy on creating a framework and culture that normalizes conception during these points in training while also subsidizing and supporting trainees and physicians who prefer to use ART and delay fertility until after training,” they suggest.
The editorialists also emphasized that women may choose to become pregnant at any point during the years that it takes to go from being a medical student to resident/fellow to attending physician, and they should be supported by their workplace on their decisions.
The study was funded by grants from National Institutes of Health/National Cancer Institute Cancer Center.
Dr. Lee and coauthors reported no relevant financial relationships. Dr. Blank reported receiving grants from AstraZeneca, Aravive, Akesobio, GlaxoSmithKline, Merck, and Seattle Genetics outside the submitted work. Dr. Saleh reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Can a nationwide liver paired donation program work?
For a patient who needs a liver, living donation offers an alternative to staying on a list of more than 10,000 people waiting for a transplant. But what happens when your donor is not a match?
“It’s an exciting time to be caring for patients who need liver transplants,” Benjamin Samstein, MD, chief of liver transplantation at New York–Presbyterian/Weill Cornell Medical Center, New York, said in an interview. He is the principal investigator for the UNOS pilot program. “I do believe it is within our grasp to make sure that nobody dies while waiting for an organ,” he said.
The initiative involves 15 U.S. transplant centers. So far, one recipient-donor pair has enrolled in the program. The pilot program has three main goals: Increase access to living donor transplants; increase access to transplants earlier, when recipients are in better health; and work out how to create and sustain a national program.
What is paired donation?
In 2020, 1,095 people died while waiting for a liver transplant, according to a report from the Organ Procurement and Transplant Network (OPTN) – a public-private partnership that includes more than 250 transplant centers and 50 organ procurement organizations across the country.
Most liver transplants involve deceased donors. One way to improve access to lifesaving transplants is through living donation, by which a healthy individual donates part of his or her liver. Someone can participate in nondirected or “altruistic” donation, in which someone donates a liver to someone they don’t know, or they can donate to a specific individual (usually a blood relative or a spouse).
With living liver donation, someone may receive a liver earlier, before getting sick enough to be given priority on the wait-list for deceased donation. Because the recipients are in better health, they may have an easier time recovering from the surgery, Ruthanne Leishman, who manages paired donation programs at UNOS, said in an interview.
In some cases, an individual will want to donate an organ to a specific person, but testing reveals that the two would not be a good match. Paired donation allows incompatible donors and recipients to find matches with other incompatible pairs. Each donor matches with the other pairs’ recipient, so the organs are essentially swapped or exchanged between the two pairs.
“People who want to donate get excited about the fact that they are not just helping their loved one but they’re also helping somebody else,” Ms. Leishman said.
Paired kidney donation programs have been running since 2002, but paired liver donation is relatively new. Since the first U.S. living-donor liver transplant in 1989, the procedure has become safer and is a viable alternative to deceased liver donation. A growing number of living donor programs are popping up at transplant centers across the country.
Still, living-donor liver donation makes up a small percentage of the liver transplants that are performed every year. In 2022, 603 living-donor liver transplants were performed in the United States, compared to 8,925 liver transplants from deceased donors, according to OPTN data. Dr. Samstein estimates a couple dozen paired liver exchanges may have been performed in the United States over the past few years within individual hospital systems. A goal of this pilot program, along with increasing access to liver transplants, is to see whether paired liver donation works on a national level, Ms. Leishman said.
Challenges to building a national program
There are several notable differences between living donor kidney transplants and living donor liver transplants. For example, living donor liver transplant is a more complicated surgery and poses greater risk to the donor. According to the OPTN 2020 Annual Report, from 2015 to 2019, the rehospitalization rate for living liver donors was twice that of living kidney donors up to 6 weeks after transplant (4.7% vs. 2.4%). One year post transplant, the cumulative rehospitalization rate was 11.0% for living liver donors and 4.8% for living kidney donors.
The risk of dying because of living donation is also higher for liver donors compared to kidney donors. The National Kidney Association states that the odds of dying during kidney donation are about 3 in 100,000, while estimates for risk of death for living liver donors range from 1 in 500 to 1 in 1,000. But some of these estimates are from 10 or more years ago, and outcomes have likely improved, said Whitney Jackson, MD, medical director of living donor liver transplant at UCHealth University of Colorado Hospital, Aurora. Her program is participating in the UNOS pilot.
More recent data from OPTN provides some idea of risk: Of 3,967 liver donors who donated between March 1, 2008, to Sept. 30, 2022, three deaths were reported within 30 days of transplant. However, the causes of death were not specified and therefore may be unrelated to the surgery. By comparison, of 74,555 kidney donors during that date range, 10 deaths were reported at 30 days post surgery.
In addition to a more complex surgery, surgeons also have a smaller time window in which to transplant a liver than than they do to transplant a kidney. A kidney can remain viable in cold storage for 24-36 hours, and it can be transported via commercial airlines cross country. Livers have to be transplanted within 8-12 hours, according to the OPTN website. For living donation, the graft needs to be transplanted within about 4 hours, Dr. Samstein noted; this poses a logistical challenge for a national organ paired donation program.
“We worked around that with the idea that we would move the donor rather than the organ,” he said. The program will require a donor (and a support person) to travel to the recipient’s transplant center where the surgery will be performed. While 3 of the 15 pilot paired donation transplant centers are in New York City, the other programs are scattered across the country, meaning a donor may have to fly to a different city to undergo surgery.
Including the preoperative evaluation, meeting the surgical team, the surgery itself, and follow-up, the donor could stay for about a month. The program offers up to $10,000 of financial assistance for travel expenses (for both the donor and support person), as well as lost wages and dependent care (for the donor only). Health insurance coverage will also be provided by the pilot program, in partnership with the American Foundation for Donation and Transplant.
The program requires that transplant candidates (the recipients) be at least 12 years old, be on the waiting list for deceased liver donation at one of the pilot’s transplant centers, and have a Model for End-Stage Liver Disease (MELD) score of 25 or less. All potential donors must be 18 years or older and must undergo a medical and psychosocial evaluation. Nondirected donors can register with the program, and they will be paired with a candidate on the liver transplant waiting list at the same transplant center.
The 1-year pilot program is set to begin when the program conducts its first match run – an algorithm will help match pairs who are enrolled in the program. About five to seven enrolled pairs would be ideal for the first match run, a UNOS spokesperson said. It is possible that the 1-year pilot program could run without performing any paired transplants, but that’s unlikely if multiple pairs are enrolled in the system, the spokesperson said. At the time of this story’s publication, the one enrolled pair are a mother and daughter who are registered at the UCHealth Transplant Center in Colorado.
Is a national liver paired donor program feasible?
While the UNOS pilot program offers financial assistance for expenses related to liver donation, some transplant surgeons are skeptical about the potential travel component of the pilot program.
The pilot program requires that the donor bring one support person if there is a need to travel for the surgery, but undergoing major abdominal surgery from a transplant team they are not familiar with may be stressful, said Peter Abt, MD, a transplant surgeon at the Hospital of the University of Pennsylvania and the Children’s Hospital of Philadelphia. “That’s a big ask,” he said, “and I’m not sure many potential donors would be up to that.”
John Roberts, MD, a transplant surgeon at the University of California, San Francisco, agreed that the travel component may put additional stress on the donor, but “if it’s the only way for the recipient to get a transplant, then the donor might be motivated,” he added.
Dr. Jackson remains optimistic. “Our experience so far has been that, yes, some people have been hesitant for things like traveling, but a lot of people who seem to be genuinely dedicated to the idea of living donation have been very enthusiastic,” she noted.
Dr. Leishman agreed that the travel aspect appears to one of the greatest barriers to participants entering the program but noted that a goal of the pilot program is to understand better what works - and what doesn’t – when considering a liver paired donation program on a national scale. “[Our] steering committee has put together a really nice framework that they think will work, but they know it’s not perfect. We’re going to have to tweak it along the way,” she said.
More information on the paired liver donation pilot program can be found on the UNOS website.
The sources interviewed for this article reported no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
This article was updated 2/15/23.
For a patient who needs a liver, living donation offers an alternative to staying on a list of more than 10,000 people waiting for a transplant. But what happens when your donor is not a match?
“It’s an exciting time to be caring for patients who need liver transplants,” Benjamin Samstein, MD, chief of liver transplantation at New York–Presbyterian/Weill Cornell Medical Center, New York, said in an interview. He is the principal investigator for the UNOS pilot program. “I do believe it is within our grasp to make sure that nobody dies while waiting for an organ,” he said.
The initiative involves 15 U.S. transplant centers. So far, one recipient-donor pair has enrolled in the program. The pilot program has three main goals: Increase access to living donor transplants; increase access to transplants earlier, when recipients are in better health; and work out how to create and sustain a national program.
What is paired donation?
In 2020, 1,095 people died while waiting for a liver transplant, according to a report from the Organ Procurement and Transplant Network (OPTN) – a public-private partnership that includes more than 250 transplant centers and 50 organ procurement organizations across the country.
Most liver transplants involve deceased donors. One way to improve access to lifesaving transplants is through living donation, by which a healthy individual donates part of his or her liver. Someone can participate in nondirected or “altruistic” donation, in which someone donates a liver to someone they don’t know, or they can donate to a specific individual (usually a blood relative or a spouse).
With living liver donation, someone may receive a liver earlier, before getting sick enough to be given priority on the wait-list for deceased donation. Because the recipients are in better health, they may have an easier time recovering from the surgery, Ruthanne Leishman, who manages paired donation programs at UNOS, said in an interview.
In some cases, an individual will want to donate an organ to a specific person, but testing reveals that the two would not be a good match. Paired donation allows incompatible donors and recipients to find matches with other incompatible pairs. Each donor matches with the other pairs’ recipient, so the organs are essentially swapped or exchanged between the two pairs.
“People who want to donate get excited about the fact that they are not just helping their loved one but they’re also helping somebody else,” Ms. Leishman said.
Paired kidney donation programs have been running since 2002, but paired liver donation is relatively new. Since the first U.S. living-donor liver transplant in 1989, the procedure has become safer and is a viable alternative to deceased liver donation. A growing number of living donor programs are popping up at transplant centers across the country.
Still, living-donor liver donation makes up a small percentage of the liver transplants that are performed every year. In 2022, 603 living-donor liver transplants were performed in the United States, compared to 8,925 liver transplants from deceased donors, according to OPTN data. Dr. Samstein estimates a couple dozen paired liver exchanges may have been performed in the United States over the past few years within individual hospital systems. A goal of this pilot program, along with increasing access to liver transplants, is to see whether paired liver donation works on a national level, Ms. Leishman said.
Challenges to building a national program
There are several notable differences between living donor kidney transplants and living donor liver transplants. For example, living donor liver transplant is a more complicated surgery and poses greater risk to the donor. According to the OPTN 2020 Annual Report, from 2015 to 2019, the rehospitalization rate for living liver donors was twice that of living kidney donors up to 6 weeks after transplant (4.7% vs. 2.4%). One year post transplant, the cumulative rehospitalization rate was 11.0% for living liver donors and 4.8% for living kidney donors.
The risk of dying because of living donation is also higher for liver donors compared to kidney donors. The National Kidney Association states that the odds of dying during kidney donation are about 3 in 100,000, while estimates for risk of death for living liver donors range from 1 in 500 to 1 in 1,000. But some of these estimates are from 10 or more years ago, and outcomes have likely improved, said Whitney Jackson, MD, medical director of living donor liver transplant at UCHealth University of Colorado Hospital, Aurora. Her program is participating in the UNOS pilot.
More recent data from OPTN provides some idea of risk: Of 3,967 liver donors who donated between March 1, 2008, to Sept. 30, 2022, three deaths were reported within 30 days of transplant. However, the causes of death were not specified and therefore may be unrelated to the surgery. By comparison, of 74,555 kidney donors during that date range, 10 deaths were reported at 30 days post surgery.
In addition to a more complex surgery, surgeons also have a smaller time window in which to transplant a liver than than they do to transplant a kidney. A kidney can remain viable in cold storage for 24-36 hours, and it can be transported via commercial airlines cross country. Livers have to be transplanted within 8-12 hours, according to the OPTN website. For living donation, the graft needs to be transplanted within about 4 hours, Dr. Samstein noted; this poses a logistical challenge for a national organ paired donation program.
“We worked around that with the idea that we would move the donor rather than the organ,” he said. The program will require a donor (and a support person) to travel to the recipient’s transplant center where the surgery will be performed. While 3 of the 15 pilot paired donation transplant centers are in New York City, the other programs are scattered across the country, meaning a donor may have to fly to a different city to undergo surgery.
Including the preoperative evaluation, meeting the surgical team, the surgery itself, and follow-up, the donor could stay for about a month. The program offers up to $10,000 of financial assistance for travel expenses (for both the donor and support person), as well as lost wages and dependent care (for the donor only). Health insurance coverage will also be provided by the pilot program, in partnership with the American Foundation for Donation and Transplant.
The program requires that transplant candidates (the recipients) be at least 12 years old, be on the waiting list for deceased liver donation at one of the pilot’s transplant centers, and have a Model for End-Stage Liver Disease (MELD) score of 25 or less. All potential donors must be 18 years or older and must undergo a medical and psychosocial evaluation. Nondirected donors can register with the program, and they will be paired with a candidate on the liver transplant waiting list at the same transplant center.
The 1-year pilot program is set to begin when the program conducts its first match run – an algorithm will help match pairs who are enrolled in the program. About five to seven enrolled pairs would be ideal for the first match run, a UNOS spokesperson said. It is possible that the 1-year pilot program could run without performing any paired transplants, but that’s unlikely if multiple pairs are enrolled in the system, the spokesperson said. At the time of this story’s publication, the one enrolled pair are a mother and daughter who are registered at the UCHealth Transplant Center in Colorado.
Is a national liver paired donor program feasible?
While the UNOS pilot program offers financial assistance for expenses related to liver donation, some transplant surgeons are skeptical about the potential travel component of the pilot program.
The pilot program requires that the donor bring one support person if there is a need to travel for the surgery, but undergoing major abdominal surgery from a transplant team they are not familiar with may be stressful, said Peter Abt, MD, a transplant surgeon at the Hospital of the University of Pennsylvania and the Children’s Hospital of Philadelphia. “That’s a big ask,” he said, “and I’m not sure many potential donors would be up to that.”
John Roberts, MD, a transplant surgeon at the University of California, San Francisco, agreed that the travel component may put additional stress on the donor, but “if it’s the only way for the recipient to get a transplant, then the donor might be motivated,” he added.
Dr. Jackson remains optimistic. “Our experience so far has been that, yes, some people have been hesitant for things like traveling, but a lot of people who seem to be genuinely dedicated to the idea of living donation have been very enthusiastic,” she noted.
Dr. Leishman agreed that the travel aspect appears to one of the greatest barriers to participants entering the program but noted that a goal of the pilot program is to understand better what works - and what doesn’t – when considering a liver paired donation program on a national scale. “[Our] steering committee has put together a really nice framework that they think will work, but they know it’s not perfect. We’re going to have to tweak it along the way,” she said.
More information on the paired liver donation pilot program can be found on the UNOS website.
The sources interviewed for this article reported no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
This article was updated 2/15/23.
For a patient who needs a liver, living donation offers an alternative to staying on a list of more than 10,000 people waiting for a transplant. But what happens when your donor is not a match?
“It’s an exciting time to be caring for patients who need liver transplants,” Benjamin Samstein, MD, chief of liver transplantation at New York–Presbyterian/Weill Cornell Medical Center, New York, said in an interview. He is the principal investigator for the UNOS pilot program. “I do believe it is within our grasp to make sure that nobody dies while waiting for an organ,” he said.
The initiative involves 15 U.S. transplant centers. So far, one recipient-donor pair has enrolled in the program. The pilot program has three main goals: Increase access to living donor transplants; increase access to transplants earlier, when recipients are in better health; and work out how to create and sustain a national program.
What is paired donation?
In 2020, 1,095 people died while waiting for a liver transplant, according to a report from the Organ Procurement and Transplant Network (OPTN) – a public-private partnership that includes more than 250 transplant centers and 50 organ procurement organizations across the country.
Most liver transplants involve deceased donors. One way to improve access to lifesaving transplants is through living donation, by which a healthy individual donates part of his or her liver. Someone can participate in nondirected or “altruistic” donation, in which someone donates a liver to someone they don’t know, or they can donate to a specific individual (usually a blood relative or a spouse).
With living liver donation, someone may receive a liver earlier, before getting sick enough to be given priority on the wait-list for deceased donation. Because the recipients are in better health, they may have an easier time recovering from the surgery, Ruthanne Leishman, who manages paired donation programs at UNOS, said in an interview.
In some cases, an individual will want to donate an organ to a specific person, but testing reveals that the two would not be a good match. Paired donation allows incompatible donors and recipients to find matches with other incompatible pairs. Each donor matches with the other pairs’ recipient, so the organs are essentially swapped or exchanged between the two pairs.
“People who want to donate get excited about the fact that they are not just helping their loved one but they’re also helping somebody else,” Ms. Leishman said.
Paired kidney donation programs have been running since 2002, but paired liver donation is relatively new. Since the first U.S. living-donor liver transplant in 1989, the procedure has become safer and is a viable alternative to deceased liver donation. A growing number of living donor programs are popping up at transplant centers across the country.
Still, living-donor liver donation makes up a small percentage of the liver transplants that are performed every year. In 2022, 603 living-donor liver transplants were performed in the United States, compared to 8,925 liver transplants from deceased donors, according to OPTN data. Dr. Samstein estimates a couple dozen paired liver exchanges may have been performed in the United States over the past few years within individual hospital systems. A goal of this pilot program, along with increasing access to liver transplants, is to see whether paired liver donation works on a national level, Ms. Leishman said.
Challenges to building a national program
There are several notable differences between living donor kidney transplants and living donor liver transplants. For example, living donor liver transplant is a more complicated surgery and poses greater risk to the donor. According to the OPTN 2020 Annual Report, from 2015 to 2019, the rehospitalization rate for living liver donors was twice that of living kidney donors up to 6 weeks after transplant (4.7% vs. 2.4%). One year post transplant, the cumulative rehospitalization rate was 11.0% for living liver donors and 4.8% for living kidney donors.
The risk of dying because of living donation is also higher for liver donors compared to kidney donors. The National Kidney Association states that the odds of dying during kidney donation are about 3 in 100,000, while estimates for risk of death for living liver donors range from 1 in 500 to 1 in 1,000. But some of these estimates are from 10 or more years ago, and outcomes have likely improved, said Whitney Jackson, MD, medical director of living donor liver transplant at UCHealth University of Colorado Hospital, Aurora. Her program is participating in the UNOS pilot.
More recent data from OPTN provides some idea of risk: Of 3,967 liver donors who donated between March 1, 2008, to Sept. 30, 2022, three deaths were reported within 30 days of transplant. However, the causes of death were not specified and therefore may be unrelated to the surgery. By comparison, of 74,555 kidney donors during that date range, 10 deaths were reported at 30 days post surgery.
In addition to a more complex surgery, surgeons also have a smaller time window in which to transplant a liver than than they do to transplant a kidney. A kidney can remain viable in cold storage for 24-36 hours, and it can be transported via commercial airlines cross country. Livers have to be transplanted within 8-12 hours, according to the OPTN website. For living donation, the graft needs to be transplanted within about 4 hours, Dr. Samstein noted; this poses a logistical challenge for a national organ paired donation program.
“We worked around that with the idea that we would move the donor rather than the organ,” he said. The program will require a donor (and a support person) to travel to the recipient’s transplant center where the surgery will be performed. While 3 of the 15 pilot paired donation transplant centers are in New York City, the other programs are scattered across the country, meaning a donor may have to fly to a different city to undergo surgery.
Including the preoperative evaluation, meeting the surgical team, the surgery itself, and follow-up, the donor could stay for about a month. The program offers up to $10,000 of financial assistance for travel expenses (for both the donor and support person), as well as lost wages and dependent care (for the donor only). Health insurance coverage will also be provided by the pilot program, in partnership with the American Foundation for Donation and Transplant.
The program requires that transplant candidates (the recipients) be at least 12 years old, be on the waiting list for deceased liver donation at one of the pilot’s transplant centers, and have a Model for End-Stage Liver Disease (MELD) score of 25 or less. All potential donors must be 18 years or older and must undergo a medical and psychosocial evaluation. Nondirected donors can register with the program, and they will be paired with a candidate on the liver transplant waiting list at the same transplant center.
The 1-year pilot program is set to begin when the program conducts its first match run – an algorithm will help match pairs who are enrolled in the program. About five to seven enrolled pairs would be ideal for the first match run, a UNOS spokesperson said. It is possible that the 1-year pilot program could run without performing any paired transplants, but that’s unlikely if multiple pairs are enrolled in the system, the spokesperson said. At the time of this story’s publication, the one enrolled pair are a mother and daughter who are registered at the UCHealth Transplant Center in Colorado.
Is a national liver paired donor program feasible?
While the UNOS pilot program offers financial assistance for expenses related to liver donation, some transplant surgeons are skeptical about the potential travel component of the pilot program.
The pilot program requires that the donor bring one support person if there is a need to travel for the surgery, but undergoing major abdominal surgery from a transplant team they are not familiar with may be stressful, said Peter Abt, MD, a transplant surgeon at the Hospital of the University of Pennsylvania and the Children’s Hospital of Philadelphia. “That’s a big ask,” he said, “and I’m not sure many potential donors would be up to that.”
John Roberts, MD, a transplant surgeon at the University of California, San Francisco, agreed that the travel component may put additional stress on the donor, but “if it’s the only way for the recipient to get a transplant, then the donor might be motivated,” he added.
Dr. Jackson remains optimistic. “Our experience so far has been that, yes, some people have been hesitant for things like traveling, but a lot of people who seem to be genuinely dedicated to the idea of living donation have been very enthusiastic,” she noted.
Dr. Leishman agreed that the travel aspect appears to one of the greatest barriers to participants entering the program but noted that a goal of the pilot program is to understand better what works - and what doesn’t – when considering a liver paired donation program on a national scale. “[Our] steering committee has put together a really nice framework that they think will work, but they know it’s not perfect. We’re going to have to tweak it along the way,” she said.
More information on the paired liver donation pilot program can be found on the UNOS website.
The sources interviewed for this article reported no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
This article was updated 2/15/23.