User login
CRC blood tests: A future without screening colonoscopies?
Most recently, Guardant Health announced the completion of its U.S. premarket approval application for its Shield blood test to screen for CRC. Approval by the Food and Drug Administration would position Guardant to later secure Medicare coverage for its test.
Rival companies, including CellMax Life, Freenome, and Exact Sciences, which already offers the stool-based Cologuard product, are pursuing similar paths in their development of blood tests for CRC.
If these companies succeed, clinicians and patients could have a choice of several FDA-approved tests in a few years.
“They’re coming, and they will be increasingly widely used,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who earlier in his career helped win broader insurance coverage of colonoscopy.
Blood tests for CRC have the potential to cause a shift in screening for colon cancer.
Screening colonoscopies ultimately could be largely phased out in the years ahead in favor of highly sensitive noninvasive tests, if the blood tests do as well as expected, said John M. Carethers, MD, AGAF, president of the American Gastroenterological Association.
‘Holy grail?’
“A blood test for cancer screening has been the ‘holy grail’ ever since the carcinoembryonic antigen blood test in the 1960s was claimed to have nearly 100% sensitivity and specificity – but turned out not to – for colorectal cancer,” wrote David F. Ransohoff, MD, a gastroenterologist at the University of North Carolina at Chapel Hill, in a 2021 article. Dr. Ransohoff has studied noninvasive CRC screening for decades.
There is a great allure in the idea of such multi-cancer detection (MCD) tests. “MCD technology offers the potential to detect asymptomatic cancer at several organ sites with a simple blood test, often called a liquid biopsy, ” according to a National Cancer Institute FY24 budget request report.
Several companies are selling MCD tests, some of which include CRC components. Among the best-known MCD tests now sold is Grail’s Galleri. At this time, however, the Galleri test, which tests for 50 types of cancer, should be used in addition to recommended colon cancer screening tests, such as colonoscopy, the company’s website says.
Guardant has also noted that its CRC-specific blood test should only complement screening tools, including colonoscopy, not replace them.
The prospect of phasing out more commonly used CRC screening – such as colonoscopy – may be appealing, but it would require a big shift for a field in which procedures have dominated. According to a report from the Centers for Disease Control and Prevention, in 2018, 67% of U.S. adults aged 50-75 years met the U.S. Preventive Services Task Force recommendations for CRC screening, and overall, 60.6% had a colonoscopy in the past 10 years.
Still, the NCI and the FDA have signaled the potential they see in MCD tests. The NCI highlighted its plans to aid MCD test development as part of its budget request for fiscal year 2024. The NCI is preparing to launch a 4-year pilot study for MCD tests to enroll 24,000 people aged 45-70 years. The study is intended as groundwork for a randomized controlled trial that will enroll 225,000 people.
The FDA has shown an interest in helping companies bring blood tests for cancer detection to market through its breakthrough device designation – a sign that the FDA places great priority on a product and seeks to streamline the application and review process.
CellMax Life appears to be the only CRC-specific screening blood test to have received a breakthrough device designation from the FDA, Atul Sharan, MS, MBA, cofounder and chief executive officer of CellMax Life, said in an email.
Lance Baldo, MD, Freenome’s chief medical officer, said in an interview that the FDA may be reviewing parts of their application in 2024, allowing for a potential 2025 launch of a blood test for asymptomatic people at average risk for CRC.
A spotty track record
Before anyone gets too excited about the prospect of phasing out screening colonoscopy, it’s important to remember that CRC blood tests have proven disappointing in the past.
Germany’s Epigenomics, for example, secured the first FDA approval for a CRC blood test, Epi ProColon, in 2016. But the company did not receive Medicare coverage for the test. In a 2021 memo explaining the decision, the Centers for Medicare & Medicaid Services noted that, given more reliable alternatives, including stool-based tests, the Epi ProColon would result in harm to some patients.
CMS also does not cover Grail’s blood test, which has a list price of $949, though the company has secured reimbursement arrangements with several self-insured employers and insurers, such as Point32Health.
But CMS officials have acknowledged the strong interest in CRC blood tests.
In that 2021 memo, the agency also outlined its requirements for Medicare coverage. CMS said it will cover blood-based screening tests for certain patients if these products meet the following standards:
- Receive FDA market authorization with an indication for CRC screening.
- Have proven test performance characteristics for a blood-based screening test with sensitivity of at least 74% and specificity of at least 90% in the detection of CRC, compared with the recognized standard (which at this time is colonoscopy) as minimal threshold levels, based on the pivotal studies included in the FDA labeling.
In February 2023, CellLife Max presented data at ASCO Gastrointestinal Cancers Symposium that its blood test had sensitivity of 92.1% for detection of CRC and 54.5% for detection of advanced adenomas, at 91% specificity.
Prior to that, in December 2022, Guardant issued a press release with study results that met the CMS standard. The test had sensitivity of 83% in detecting individuals with CRC. Specificity was 90%, the company said. That translates to a false positive rate of just 10%.
While such results look promising, Asad Umar, DVM, PhD, the chief of gastrointestinal and other cancers at NCI’s division of cancer prevention, said physicians should be cautious when giving advice or answering questions about MCD tests, given limited data from prospective studies about their effect on health outcomes.
Even among physicians already using some MCD tests to screen patients, there is a lot of concern about false-positive results that require diagnostic workup and false negative results that lead to a false sense of assurance, Dr. Umar said.
“Screening is a process and not just a test. The process involves follow-up testing for any positive test findings,” Dr. Umar said. “At this point, doctors should inform patients that there is not sufficient data to know how best to use these tests.”
Hurdles to broad acceptance
For companies seeking broad acceptance of a CRC blood test, two of the three major steps needed are securing FDA approval and Medicare coverage. The last step would be getting an A or B recommendation from the USPSTF, which would mandate coverage by health plans.
This is the “big trifecta,” Dr. Baldo said.
In the USPSTF’s current colon cancer screening recommendations, issued in 2021, it gave an A grade for CRC screening for adults aged 50-75 years and a B grade for those aged 45-49 years.
The USPSTF’s recommended forms of screening include colonoscopy, high-sensitivity guaiac fecal occult blood (gFOBT), fecal immunochemical test (FIT), flexible sigmoidoscopy (FS), stool DNA, and/or computed tomographic colonography (CTC).
The USPSTF says more research is needed to establish the accuracy and effectiveness of emerging screening technologies, such as blood or serum tests.
If CRC blood tests eventually win FDA approval, the USPSTF would likely provide guidance to clinicians on how patients can use them as a screening option.
Dr. Ransohoff noted that the mission of the USPSTF is different from that of the FDA and CMS. The FDA’s approach on medical tests is to consider overall safety and efficacy, as does CMS, but neither agency makes recommendations, nor does it perform its own rigorous quantitative assessment of benefit versus harm. The USPSTF, however, does its own detailed evidence-based reviews of the benefit versus harm of products, Dr. Ransohoff said.
“To me, the Task Force is the gold standard,” Dr. Ransohoff said. “You have to jump through the hoops with the FDA and CMS for making claims, to enable use, and to help get payment. But the Task Force looks at the choices and the consequences in a quantitative way and makes specific practice recommendations.”
What the future may hold
Dr. Carethers sees a future in which highly sensitive blood tests are able to largely replace screening colonoscopies. He said that colonoscopies would be used for people who are most in need of diagnosis and treatment. Dr. Carethers addressed these points during an AGA podcast released in January 2023.
In 20-25 years, colonoscopies may be only a therapeutic procedure, much like endoscopic retrograde cholangiopancreatography is now, Dr. Carethers added.
Even if CRC-specific blood tests prove to be effective screening tools, Dr. Ransohoff stressed that colonoscopy will survive. Many people will eventually need to undergo colonoscopy as a diagnostic procedure following a positive blood-based test result, and some may also opt for screening colonoscopies in lieu of frequent blood tests.
And, overall, physicians and patients will need to weigh the trade-offs of a noninvasive test that can only diagnose CRC versus a screening colonoscopy that offers preventative treatment as well.
“The best intent for screening is prevention of cancer, not detection of cancer,” said Dr. Johnson.
Dr. Carethers, Dr. Johnson, and Dr. Ransohoff reporting having no relevant financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
Most recently, Guardant Health announced the completion of its U.S. premarket approval application for its Shield blood test to screen for CRC. Approval by the Food and Drug Administration would position Guardant to later secure Medicare coverage for its test.
Rival companies, including CellMax Life, Freenome, and Exact Sciences, which already offers the stool-based Cologuard product, are pursuing similar paths in their development of blood tests for CRC.
If these companies succeed, clinicians and patients could have a choice of several FDA-approved tests in a few years.
“They’re coming, and they will be increasingly widely used,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who earlier in his career helped win broader insurance coverage of colonoscopy.
Blood tests for CRC have the potential to cause a shift in screening for colon cancer.
Screening colonoscopies ultimately could be largely phased out in the years ahead in favor of highly sensitive noninvasive tests, if the blood tests do as well as expected, said John M. Carethers, MD, AGAF, president of the American Gastroenterological Association.
‘Holy grail?’
“A blood test for cancer screening has been the ‘holy grail’ ever since the carcinoembryonic antigen blood test in the 1960s was claimed to have nearly 100% sensitivity and specificity – but turned out not to – for colorectal cancer,” wrote David F. Ransohoff, MD, a gastroenterologist at the University of North Carolina at Chapel Hill, in a 2021 article. Dr. Ransohoff has studied noninvasive CRC screening for decades.
There is a great allure in the idea of such multi-cancer detection (MCD) tests. “MCD technology offers the potential to detect asymptomatic cancer at several organ sites with a simple blood test, often called a liquid biopsy, ” according to a National Cancer Institute FY24 budget request report.
Several companies are selling MCD tests, some of which include CRC components. Among the best-known MCD tests now sold is Grail’s Galleri. At this time, however, the Galleri test, which tests for 50 types of cancer, should be used in addition to recommended colon cancer screening tests, such as colonoscopy, the company’s website says.
Guardant has also noted that its CRC-specific blood test should only complement screening tools, including colonoscopy, not replace them.
The prospect of phasing out more commonly used CRC screening – such as colonoscopy – may be appealing, but it would require a big shift for a field in which procedures have dominated. According to a report from the Centers for Disease Control and Prevention, in 2018, 67% of U.S. adults aged 50-75 years met the U.S. Preventive Services Task Force recommendations for CRC screening, and overall, 60.6% had a colonoscopy in the past 10 years.
Still, the NCI and the FDA have signaled the potential they see in MCD tests. The NCI highlighted its plans to aid MCD test development as part of its budget request for fiscal year 2024. The NCI is preparing to launch a 4-year pilot study for MCD tests to enroll 24,000 people aged 45-70 years. The study is intended as groundwork for a randomized controlled trial that will enroll 225,000 people.
The FDA has shown an interest in helping companies bring blood tests for cancer detection to market through its breakthrough device designation – a sign that the FDA places great priority on a product and seeks to streamline the application and review process.
CellMax Life appears to be the only CRC-specific screening blood test to have received a breakthrough device designation from the FDA, Atul Sharan, MS, MBA, cofounder and chief executive officer of CellMax Life, said in an email.
Lance Baldo, MD, Freenome’s chief medical officer, said in an interview that the FDA may be reviewing parts of their application in 2024, allowing for a potential 2025 launch of a blood test for asymptomatic people at average risk for CRC.
A spotty track record
Before anyone gets too excited about the prospect of phasing out screening colonoscopy, it’s important to remember that CRC blood tests have proven disappointing in the past.
Germany’s Epigenomics, for example, secured the first FDA approval for a CRC blood test, Epi ProColon, in 2016. But the company did not receive Medicare coverage for the test. In a 2021 memo explaining the decision, the Centers for Medicare & Medicaid Services noted that, given more reliable alternatives, including stool-based tests, the Epi ProColon would result in harm to some patients.
CMS also does not cover Grail’s blood test, which has a list price of $949, though the company has secured reimbursement arrangements with several self-insured employers and insurers, such as Point32Health.
But CMS officials have acknowledged the strong interest in CRC blood tests.
In that 2021 memo, the agency also outlined its requirements for Medicare coverage. CMS said it will cover blood-based screening tests for certain patients if these products meet the following standards:
- Receive FDA market authorization with an indication for CRC screening.
- Have proven test performance characteristics for a blood-based screening test with sensitivity of at least 74% and specificity of at least 90% in the detection of CRC, compared with the recognized standard (which at this time is colonoscopy) as minimal threshold levels, based on the pivotal studies included in the FDA labeling.
In February 2023, CellLife Max presented data at ASCO Gastrointestinal Cancers Symposium that its blood test had sensitivity of 92.1% for detection of CRC and 54.5% for detection of advanced adenomas, at 91% specificity.
Prior to that, in December 2022, Guardant issued a press release with study results that met the CMS standard. The test had sensitivity of 83% in detecting individuals with CRC. Specificity was 90%, the company said. That translates to a false positive rate of just 10%.
While such results look promising, Asad Umar, DVM, PhD, the chief of gastrointestinal and other cancers at NCI’s division of cancer prevention, said physicians should be cautious when giving advice or answering questions about MCD tests, given limited data from prospective studies about their effect on health outcomes.
Even among physicians already using some MCD tests to screen patients, there is a lot of concern about false-positive results that require diagnostic workup and false negative results that lead to a false sense of assurance, Dr. Umar said.
“Screening is a process and not just a test. The process involves follow-up testing for any positive test findings,” Dr. Umar said. “At this point, doctors should inform patients that there is not sufficient data to know how best to use these tests.”
Hurdles to broad acceptance
For companies seeking broad acceptance of a CRC blood test, two of the three major steps needed are securing FDA approval and Medicare coverage. The last step would be getting an A or B recommendation from the USPSTF, which would mandate coverage by health plans.
This is the “big trifecta,” Dr. Baldo said.
In the USPSTF’s current colon cancer screening recommendations, issued in 2021, it gave an A grade for CRC screening for adults aged 50-75 years and a B grade for those aged 45-49 years.
The USPSTF’s recommended forms of screening include colonoscopy, high-sensitivity guaiac fecal occult blood (gFOBT), fecal immunochemical test (FIT), flexible sigmoidoscopy (FS), stool DNA, and/or computed tomographic colonography (CTC).
The USPSTF says more research is needed to establish the accuracy and effectiveness of emerging screening technologies, such as blood or serum tests.
If CRC blood tests eventually win FDA approval, the USPSTF would likely provide guidance to clinicians on how patients can use them as a screening option.
Dr. Ransohoff noted that the mission of the USPSTF is different from that of the FDA and CMS. The FDA’s approach on medical tests is to consider overall safety and efficacy, as does CMS, but neither agency makes recommendations, nor does it perform its own rigorous quantitative assessment of benefit versus harm. The USPSTF, however, does its own detailed evidence-based reviews of the benefit versus harm of products, Dr. Ransohoff said.
“To me, the Task Force is the gold standard,” Dr. Ransohoff said. “You have to jump through the hoops with the FDA and CMS for making claims, to enable use, and to help get payment. But the Task Force looks at the choices and the consequences in a quantitative way and makes specific practice recommendations.”
What the future may hold
Dr. Carethers sees a future in which highly sensitive blood tests are able to largely replace screening colonoscopies. He said that colonoscopies would be used for people who are most in need of diagnosis and treatment. Dr. Carethers addressed these points during an AGA podcast released in January 2023.
In 20-25 years, colonoscopies may be only a therapeutic procedure, much like endoscopic retrograde cholangiopancreatography is now, Dr. Carethers added.
Even if CRC-specific blood tests prove to be effective screening tools, Dr. Ransohoff stressed that colonoscopy will survive. Many people will eventually need to undergo colonoscopy as a diagnostic procedure following a positive blood-based test result, and some may also opt for screening colonoscopies in lieu of frequent blood tests.
And, overall, physicians and patients will need to weigh the trade-offs of a noninvasive test that can only diagnose CRC versus a screening colonoscopy that offers preventative treatment as well.
“The best intent for screening is prevention of cancer, not detection of cancer,” said Dr. Johnson.
Dr. Carethers, Dr. Johnson, and Dr. Ransohoff reporting having no relevant financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
Most recently, Guardant Health announced the completion of its U.S. premarket approval application for its Shield blood test to screen for CRC. Approval by the Food and Drug Administration would position Guardant to later secure Medicare coverage for its test.
Rival companies, including CellMax Life, Freenome, and Exact Sciences, which already offers the stool-based Cologuard product, are pursuing similar paths in their development of blood tests for CRC.
If these companies succeed, clinicians and patients could have a choice of several FDA-approved tests in a few years.
“They’re coming, and they will be increasingly widely used,” said David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who earlier in his career helped win broader insurance coverage of colonoscopy.
Blood tests for CRC have the potential to cause a shift in screening for colon cancer.
Screening colonoscopies ultimately could be largely phased out in the years ahead in favor of highly sensitive noninvasive tests, if the blood tests do as well as expected, said John M. Carethers, MD, AGAF, president of the American Gastroenterological Association.
‘Holy grail?’
“A blood test for cancer screening has been the ‘holy grail’ ever since the carcinoembryonic antigen blood test in the 1960s was claimed to have nearly 100% sensitivity and specificity – but turned out not to – for colorectal cancer,” wrote David F. Ransohoff, MD, a gastroenterologist at the University of North Carolina at Chapel Hill, in a 2021 article. Dr. Ransohoff has studied noninvasive CRC screening for decades.
There is a great allure in the idea of such multi-cancer detection (MCD) tests. “MCD technology offers the potential to detect asymptomatic cancer at several organ sites with a simple blood test, often called a liquid biopsy, ” according to a National Cancer Institute FY24 budget request report.
Several companies are selling MCD tests, some of which include CRC components. Among the best-known MCD tests now sold is Grail’s Galleri. At this time, however, the Galleri test, which tests for 50 types of cancer, should be used in addition to recommended colon cancer screening tests, such as colonoscopy, the company’s website says.
Guardant has also noted that its CRC-specific blood test should only complement screening tools, including colonoscopy, not replace them.
The prospect of phasing out more commonly used CRC screening – such as colonoscopy – may be appealing, but it would require a big shift for a field in which procedures have dominated. According to a report from the Centers for Disease Control and Prevention, in 2018, 67% of U.S. adults aged 50-75 years met the U.S. Preventive Services Task Force recommendations for CRC screening, and overall, 60.6% had a colonoscopy in the past 10 years.
Still, the NCI and the FDA have signaled the potential they see in MCD tests. The NCI highlighted its plans to aid MCD test development as part of its budget request for fiscal year 2024. The NCI is preparing to launch a 4-year pilot study for MCD tests to enroll 24,000 people aged 45-70 years. The study is intended as groundwork for a randomized controlled trial that will enroll 225,000 people.
The FDA has shown an interest in helping companies bring blood tests for cancer detection to market through its breakthrough device designation – a sign that the FDA places great priority on a product and seeks to streamline the application and review process.
CellMax Life appears to be the only CRC-specific screening blood test to have received a breakthrough device designation from the FDA, Atul Sharan, MS, MBA, cofounder and chief executive officer of CellMax Life, said in an email.
Lance Baldo, MD, Freenome’s chief medical officer, said in an interview that the FDA may be reviewing parts of their application in 2024, allowing for a potential 2025 launch of a blood test for asymptomatic people at average risk for CRC.
A spotty track record
Before anyone gets too excited about the prospect of phasing out screening colonoscopy, it’s important to remember that CRC blood tests have proven disappointing in the past.
Germany’s Epigenomics, for example, secured the first FDA approval for a CRC blood test, Epi ProColon, in 2016. But the company did not receive Medicare coverage for the test. In a 2021 memo explaining the decision, the Centers for Medicare & Medicaid Services noted that, given more reliable alternatives, including stool-based tests, the Epi ProColon would result in harm to some patients.
CMS also does not cover Grail’s blood test, which has a list price of $949, though the company has secured reimbursement arrangements with several self-insured employers and insurers, such as Point32Health.
But CMS officials have acknowledged the strong interest in CRC blood tests.
In that 2021 memo, the agency also outlined its requirements for Medicare coverage. CMS said it will cover blood-based screening tests for certain patients if these products meet the following standards:
- Receive FDA market authorization with an indication for CRC screening.
- Have proven test performance characteristics for a blood-based screening test with sensitivity of at least 74% and specificity of at least 90% in the detection of CRC, compared with the recognized standard (which at this time is colonoscopy) as minimal threshold levels, based on the pivotal studies included in the FDA labeling.
In February 2023, CellLife Max presented data at ASCO Gastrointestinal Cancers Symposium that its blood test had sensitivity of 92.1% for detection of CRC and 54.5% for detection of advanced adenomas, at 91% specificity.
Prior to that, in December 2022, Guardant issued a press release with study results that met the CMS standard. The test had sensitivity of 83% in detecting individuals with CRC. Specificity was 90%, the company said. That translates to a false positive rate of just 10%.
While such results look promising, Asad Umar, DVM, PhD, the chief of gastrointestinal and other cancers at NCI’s division of cancer prevention, said physicians should be cautious when giving advice or answering questions about MCD tests, given limited data from prospective studies about their effect on health outcomes.
Even among physicians already using some MCD tests to screen patients, there is a lot of concern about false-positive results that require diagnostic workup and false negative results that lead to a false sense of assurance, Dr. Umar said.
“Screening is a process and not just a test. The process involves follow-up testing for any positive test findings,” Dr. Umar said. “At this point, doctors should inform patients that there is not sufficient data to know how best to use these tests.”
Hurdles to broad acceptance
For companies seeking broad acceptance of a CRC blood test, two of the three major steps needed are securing FDA approval and Medicare coverage. The last step would be getting an A or B recommendation from the USPSTF, which would mandate coverage by health plans.
This is the “big trifecta,” Dr. Baldo said.
In the USPSTF’s current colon cancer screening recommendations, issued in 2021, it gave an A grade for CRC screening for adults aged 50-75 years and a B grade for those aged 45-49 years.
The USPSTF’s recommended forms of screening include colonoscopy, high-sensitivity guaiac fecal occult blood (gFOBT), fecal immunochemical test (FIT), flexible sigmoidoscopy (FS), stool DNA, and/or computed tomographic colonography (CTC).
The USPSTF says more research is needed to establish the accuracy and effectiveness of emerging screening technologies, such as blood or serum tests.
If CRC blood tests eventually win FDA approval, the USPSTF would likely provide guidance to clinicians on how patients can use them as a screening option.
Dr. Ransohoff noted that the mission of the USPSTF is different from that of the FDA and CMS. The FDA’s approach on medical tests is to consider overall safety and efficacy, as does CMS, but neither agency makes recommendations, nor does it perform its own rigorous quantitative assessment of benefit versus harm. The USPSTF, however, does its own detailed evidence-based reviews of the benefit versus harm of products, Dr. Ransohoff said.
“To me, the Task Force is the gold standard,” Dr. Ransohoff said. “You have to jump through the hoops with the FDA and CMS for making claims, to enable use, and to help get payment. But the Task Force looks at the choices and the consequences in a quantitative way and makes specific practice recommendations.”
What the future may hold
Dr. Carethers sees a future in which highly sensitive blood tests are able to largely replace screening colonoscopies. He said that colonoscopies would be used for people who are most in need of diagnosis and treatment. Dr. Carethers addressed these points during an AGA podcast released in January 2023.
In 20-25 years, colonoscopies may be only a therapeutic procedure, much like endoscopic retrograde cholangiopancreatography is now, Dr. Carethers added.
Even if CRC-specific blood tests prove to be effective screening tools, Dr. Ransohoff stressed that colonoscopy will survive. Many people will eventually need to undergo colonoscopy as a diagnostic procedure following a positive blood-based test result, and some may also opt for screening colonoscopies in lieu of frequent blood tests.
And, overall, physicians and patients will need to weigh the trade-offs of a noninvasive test that can only diagnose CRC versus a screening colonoscopy that offers preventative treatment as well.
“The best intent for screening is prevention of cancer, not detection of cancer,” said Dr. Johnson.
Dr. Carethers, Dr. Johnson, and Dr. Ransohoff reporting having no relevant financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
Lack of food for thought: Starve a bacterium, feed an infection
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
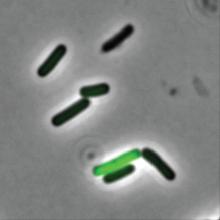
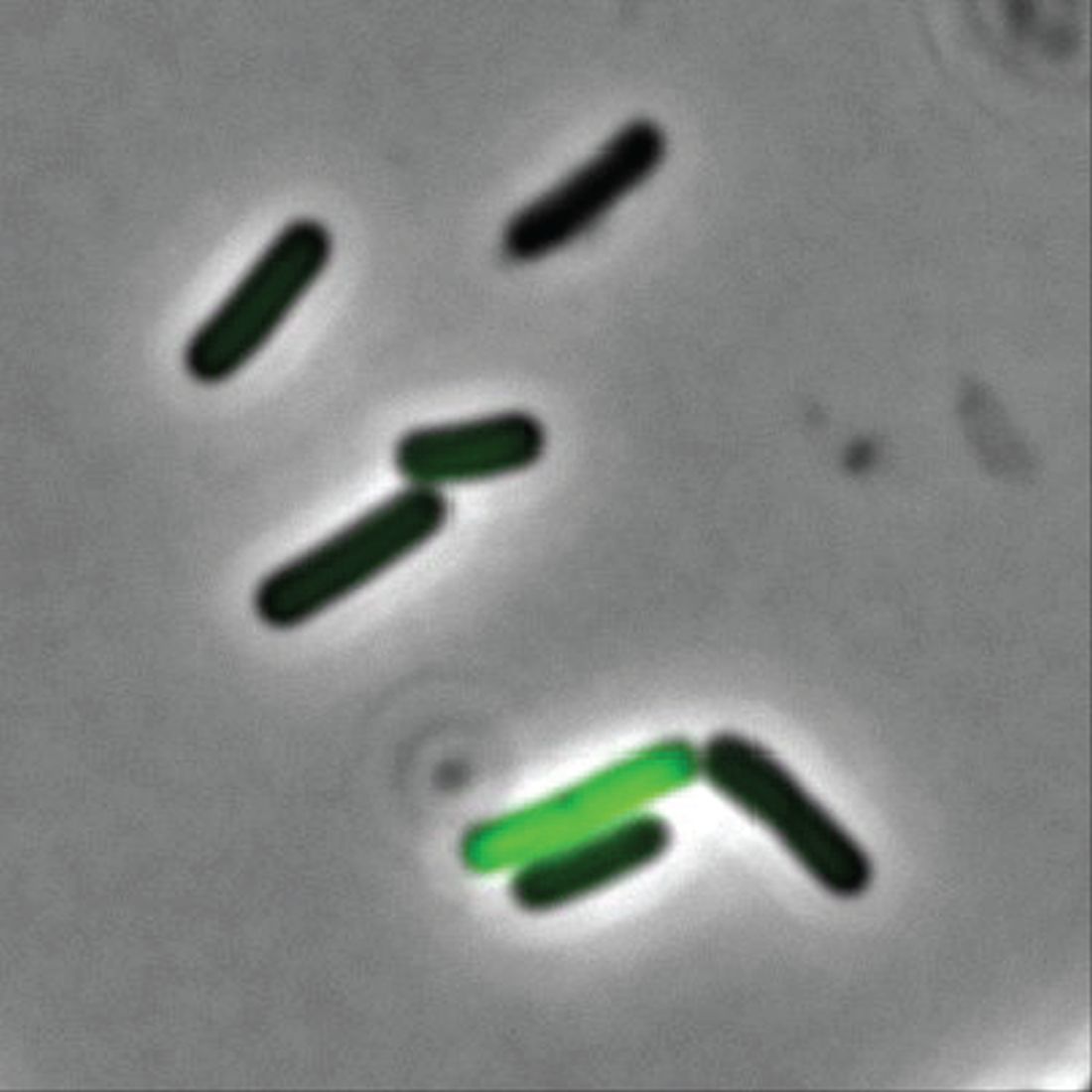
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
Doctor’s checklist for treating long COVID patients
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Lisa McCorkell had a mild bout of COVID-19 in March 2020. Young and healthy, she assumed that she would bounce back quickly. But when her fatigue, shortness of breath, and brain fog persisted, she realized that she most likely had long COVID.
“Back then, we as patients basically coined the term,” she said. While her first primary care provider was sympathetic, they were unsure how to treat her. After her insurance changed, she ended up with a second primary care provider who didn’t take her symptoms seriously. “They dismissed my complaints and told me they were all in my head. I didn’t seek care for a while after that.”
Ms. McCorkell’s symptoms improved after her first COVID vaccine in the spring of 2021. She also finally found a new primary care doctor she could trust. But as one of the founders of the Patient-Led Research Collaborative, a group of researchers who study long COVID, she said many doctors still don’t know the hallmark symptoms of the condition or how to treat it.
“There’s still a lack of education on what long COVID is, and the symptoms associated with it,” she said. “Many of the symptoms that occur in long COVID are symptoms of other chronic conditions, such as chronic fatigue syndrome, that are often dismissed. And even if providers believe patients and send them for a workup, many of the routine blood and imaging tests come back normal.”
The term “long COVID” emerged in May 2020. And though the condition was recognized within a few months of the start of the pandemic, doctors weren’t sure how to screen or treat it.
While knowledge has developed since then, primary care doctors are still in a tough spot. They’re often the first providers that patients turn to when they have symptoms of long COVID.
“There’s no clear algorithm to pick up long COVID – there are no definite blood tests or biomarkers, or specific things to look for on a physical exam,” said Lawrence Purpura, MD, an infectious disease specialist and director of the long COVID clinic at Columbia University Medical Center, New York. “It’s a complicated disease that can impact every organ system of the body.”
Even so, emerging research has identified a checklist of sorts that doctors should consider when a patient seeks care for what appears to be long COVID. Among them: the key systems and organs impacted by the disease, the most common symptoms, useful therapeutic options for symptom management that have been found to help people with long COVID, and the best healthy lifestyle choices that doctors can recommend to help their patients
Here’s a closer look at each of these aspects, based on research and interviews with experts, patients, and doctors.
Key systems, organs impacted
About 10% of people who are infected with COVID-19 go on to have long COVID, according to a recent study that Ms. McCorkell helped coauthor. But more than 3 years into the pandemic, much about the condition is still a mystery.
COVID is a unique virus because it can spread far and wide in a patient’s body. A December 2022 study, published in Nature, autopsied 44 people who died of COVID and found that the virus could spread throughout the body and persist, in one case as long as 230 days after symptoms started.
“We know that there are dozens of symptoms across multiple organ systems,” said Ms. McCorkell. “That makes it harder for a primary care physician to connect the dots and associate it with COVID.”
A paper published in Nature Medicine proposed one way to help guide diagnosis. It divided symptoms into four groups:
- Cardiac and renal issues such as heart palpitations, chest pain, and kidney damage
- Sleep and anxiety problems like insomnia, waking up in the middle of the night, and anxiety
- In the musculoskeletal and nervous systems: musculoskeletal pain, osteoarthritis, and problems with mental skills
- In the digestive and respiratory systems: trouble breathing, asthma, stomach pain, nausea, and vomiting
There were also specific patterns in these groups. People in the first group were more likely to be older, male, have other conditions and to have been infected during the first wave of the COVID pandemic. People in the second group were over 60% female, and were more likely to have had previous allergies or asthma. The third group was also about 60% female, and many of them already had autoimmune conditions such as rheumatoid arthritis. Members of the fourth group – also 60% female – were the least likely of all the groups to have another condition.
This research is helpful, because it gives doctors a better sense of what conditions might make a patient more likely to get long COVID, as well as specific symptoms to look out for, said Steven Flanagan, MD, a physical medicine and rehabilitation specialist at New York University Langone Medical Center who also specializes in treating patients with long COVID.
But the “challenge there, though, for health care providers is that not everyone will fall neatly into one of these categories,” he stressed.
Checklist of symptoms
Although long COVID can be confusing, doctors say there are several symptoms that appear consistently that primary care providers should look out for, that could flag long COVID.
Postexertional malaise (PEM). This is different from simply feeling tired. “This term is often conflated with fatigue, but it’s very different,” said David Putrino, PhD, director of rehabilitation innovation at the Mount Sinai Health System in New York, who says that he sees it in about 90% of patients who come to his long COVID clinic.
PEM is the worsening of symptoms after physical or mental exertion. This usually occurs a day or 2 after the activity, but it can last for days, and sometimes weeks.
“It’s very different from fatigue, which is just a generalized tiredness, and exercise intolerance, where someone complains of not being able to do their usual workout on the treadmill,” he noted. “People with PEM are able to push through and do what they need to do, and then are hit with symptoms anywhere from 12 to 72 hours later.”
Dysautonomia. This is an umbrella term used to describe a dysfunction of the autonomic nervous system, which regulates bodily functions that you can’t control, like your blood pressure, heart rate, and breathing. This can cause symptoms such as heart palpitations, along with orthostatic intolerance, which means you can’t stand up for long without feeling faint or dizzy.
“In my practice, about 80% of patients meet criteria for dysautonomia,” said Dr. Putrino. Other research has found that it’s present in about two-thirds of long COVID patients.
One relatively easy way primary care providers can diagnose dysautonomia is to do the tilt table test. This helps check for postural orthostatic tachycardia syndrome (POTS), one of the most common forms of dysautonomia. During this exam, the patient lies flat on a table. As the head of the table is raised to an almost upright position, their heart rate and blood pressure are measured. Signs of POTS include an abnormal heart rate when you’re upright, as well as a worsening of symptoms.
Exercise intolerance. A review published in the journal JAMA Network Open analyzed 38 studies on long COVID and exercise and found that patients with the condition had a much harder time doing physical activity. Exercise capacity was reduced to levels that would be expected about a decade later in life, according to study authors.
“This is especially important because it can’t be explained just by deconditioning,” said Dr. Purpura. “Sometimes these patients are encouraged to ramp up exercise as a way to help with symptoms, but in these cases, encouraging them to push through can cause postexertional malaise, which sets patients back and delays recovery.”
While long COVID can cause dozens of symptoms, a paper Ms. McCorkell coauthored zeroed in on some of the most common ones: chest pain, heart palpitations, coughing, shortness of breath, belly pain, nausea, problems with mental skills, fatigue, disordered sleep, memory loss, ringing in the ears (tinnitus), erectile dysfunction, irregular menstruation, and worsened premenstrual syndrome.
While most primary care providers are familiar with some of these long COVID symptoms, they may not be aware of others.
“COVID itself seems to cause hormonal changes that can lead to erection and menstrual cycle problems,” explained Dr. Putrino. “But these may not be picked up in a visit if the patient is complaining of other signs of long COVID.”
It’s not just what symptoms are, but when they began to occur, he added. “Usually, these symptoms either start with the initial COVID infection, or begin sometime within 3 months after the acute COVID infection. That’s why it’s important for people with COVID to take notice of anything unusual that crops up within a month or 2 after getting sick.”
Can you prevent long COVID?
You can’t, but one of the best ways to reduce your risk is to get vaccinated. Getting at least one dose of a COVID vaccine before you test positive for COVID lowers your risk of long COVID by about 35% according to a study published in Antimicrobial Stewardship & Healthcare Epidemiology. Unvaccinated people who recovered from COVID, and then got a vaccine, lowered their own long COVID risk by 27%.
In addition, a study published in JAMA Internal Medicine found that women who were infected with COVID were less likely to go on to get long COVID and/or have less debilitating symptoms if they had a healthy lifestyle, which included the following: a healthy weight (a body mass index between 18.5 and 24.7 kg/m2), never-smoker, moderate alcohol consumption, a high-quality diet, 7-9 hours of sleep a night, and at least 150 minutes per week of physical activity
But Ms. McCorkell noted that she herself had a healthy preinfection lifestyle but got long COVID anyway, suggesting these approaches don’t work for everyone.
“I think one reason my symptoms weren’t addressed by primary care physicians for so long is because they looked at me and saw that I was young and healthy, so they dismissed my reports as being all in my head,” she explained. “But we know now anyone can get long COVID, regardless of age, health status, or disease severity. That’s why it’s so important that primary care physicians be able to recognize symptoms.”
A version of this article first appeared on WebMD.com.
Too high: Can you ID pot-induced psychosis?
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
Cervical screening often stops at 65, but should it?
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
“Did you love your wife?” asks a character in “Rose,” a book by Martin Cruz Smith.
“No, but she became a fact through perseverance,” the man replied.
Medicine also has such relationships, it seems – tentative ideas that turned into fact simply by existing long enough.
Age 65 as the cutoff for cervical screening may be one such example. It has existed for 27 years with limited science to back it up. That may soon change with the launch of a $3.3 million study that is being funded by the National Institutes of Health (NIH). The study is intended to provide a more solid foundation for the benefits and harms of cervical screening for women older than 65.
It’s an important issue: 20% of all cervical cancer cases are found in women who are older than 65. Most of these patients have late-stage disease, which can be fatal. In the United States, 35% of cervical cancer deaths occur after age 65. But women in this age group are usually no longer screened for cervical cancer.
Back in 1996, the U.S. Preventive Services Task Force recommended that for women at average risk with adequate prior screening, cervical screening should stop at the age of 65. This recommendation has been carried forward year after year and has been incorporated into several other guidelines.
For example, current guidelines from the American Cancer Society, the American College of Obstetricians and Gynecologists, and the USPSTF recommend that cervical screening stop at aged 65 for patients with adequate prior screening.
“Adequate screening” is defined as three consecutive normal Pap tests or two consecutive negative human papillomavirus tests or two consecutive negative co-tests within the prior 10 years, with the most recent screening within 5 years and with no precancerous lesions in the past 25 years.
This all sounds reasonable; however, for most women, medical records aren’t up to the task of providing a clean bill of cervical health over many decades.
Explained Sarah Feldman, MD, an associate professor in obstetrics, gynecology, and reproductive biology at Harvard Medical School, Boston: “You know, when a patient says to me at 65, ‘Should I continue screening?’ I say, ‘Do you have all your results?’ And they’ll say, ‘Well, I remember I had a sort of abnormal pap 15 years ago,’ and I say, ‘All right; well, who knows what that was?’ So I’ll continue screening.”
According to George Sawaya, MD, professor of obstetrics, gynecology, and reproductive sciences at the University of California, San Francisco, up to 60% of women do not meet the criteria to end screening at age 65. This means that each year in the United States, approximately 1.7 million women turn 65 and should, in theory, continue to undergo screening for cervical cancer.
Unfortunately, the evidence base for the harms and benefits of cervical screening after age 65 is almost nonexistent – at least by the current standards of evidence-based medicine.
“We need to be clear that we don’t really know the appropriateness of the screening after 65,” said Dr. Sawaya, “which is ironic, because cervical cancer screening is probably the most commonly implemented cancer screening test in the country because it starts so early and ends so late and it’s applied so frequently.”
Dr. Feldman agrees that the age 65 cutoff is “somewhat arbitrary.” She said, “Why don’t they want to consider it continuing past 65? I don’t really understand, I have to be honest with you.”
So what’s the scientific evidence backing up the 27-year-old recommendation?
In 2018, the USPSTF’s cervical-screening guidelines concluded “with moderate certainty that the benefits of screening in women older than 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer do not outweigh the potential harms.”
This recommendation was based on a new decision model commissioned by the USPSTF. The model was needed because, as noted by the guidelines’ authors, “None of the screening trials enrolled women older than 65 years, so direct evidence on when to stop screening is not available.”
In 2020, the ACS carried out a fresh literature review and published its own recommendations. The ACS concluded that “the evidence for the effectiveness of screening beyond age 65 is limited, based solely on observational and modeling studies.”
As a result, the ACS assigned a “qualified recommendation” to the age-65 moratorium (defined as “less certainty about the balance of benefits and harms or about patients’ values and preferences”).
Most recently, the 2021 Updated Cervical Cancer Screening Guidelines, published by the American College of Obstetricians and Gynecologists, endorsed the recommendations of the USPSTF.
Dr. Sawaya said, “The whole issue about screening over 65 is complicated from a lot of perspectives. We don’t know a lot about the safety. We don’t really know a lot about patients’ perceptions of it. But we do know that there has to be an upper age limit after which screening is just simply imprudent.”
Dr. Sawaya acknowledges that there exists a “heck-why-not” attitude toward cervical screening after 65 among some physicians, given that the tests are quick and cheap and could save a life, but he sounds a note of caution.
“It’s like when we used to use old cameras: the film was cheap, but the developing was really expensive,” Dr. Sawaya said. “So it’s not necessarily about the tests being cheap, it’s about the cascade of events [that follow].”
Follow-up for cervical cancer can be more hazardous for a postmenopausal patient than for a younger woman, explained Dr. Sawaya, because the transformation zone of the cervix may be difficult to see on colposcopy. Instead of a straightforward 5-minute procedure in the doctor’s office, the older patient may need the operating room simply to provide the first biopsy.
In addition, treatments such as cone biopsy, loop excision, or ablation are also more worrying for older women, said Dr. Sawaya, “So you start thinking about the risks of anesthesia, you start thinking about the risks of bleeding and infection, etc. And these have not been well described in older people.”
To add to the uncertainty about the merits and risks of hunting out cervical cancer in older women, a lot has changed in women’s health since 1996.
Explained Dr. Sawaya, “This stake was put in the ground in 1996, ... but since that time, life expectancy has gained 5 years. So a logical person would say, ‘Oh, well, let’s just say it should be 70 now, right?’ [But] can we even use old studies to inform the current cohort of women who are entering this 65-year-and-older age group?”
To answer all these questions, a 5-year, $3.3 million study funded by the NIH through the National Cancer Institute is now underway.
The project, named Comparative Effectiveness Research to Validate and Improve Cervical Cancer Screening (CERVICCS 2), will be led by Dr. Sawaya and Michael Silverberg, PhD, associate director of the Behavioral Health, Aging and Infectious Diseases Section of Kaiser Permanente Northern California’s Division of Research.
It’s not possible to conduct a true randomized controlled trial in this field of medicine for ethical reasons, so CERVICCS 2 will emulate a randomized study by following the fate of approximately 280,000 women older than 65 who were long-term members of two large health systems during 2005-2022. – both before and after the crucial age 65 cutoff.
The California study will also look at the downsides of diagnostic procedures and surgical interventions that follow a positive screening result after the age of 65 and the personal experiences of the women involved.
Dr. Sawaya and Dr. Silverberg’s team will use software that emulates a clinical trial by utilizing observational data to compare the benefits and risks of screening continuation or screening cessation after age 65.
In effect, after 27 years of loyalty to a recommendation supported by low-quality evidence, medicine will finally have a reliable answer to the question, Should we continue to look for cervical cancer in women over 65?
Dr. Sawaya concluded: “There’s very few things that are packaged away and thought to be just the truth. And this is why we always have to be vigilant. ... And that’s what keeps science so interesting and exciting.”
Dr. Sawaya has disclosed no relevant financial relationships. Dr. Feldman writes for UpToDate and receives several NIH grants.
A version of this article first appeared on Medscape.com.
SGLT2 inhibitors: Real-world data show benefits outweigh risks
Starting therapy with an SGLT2 inhibitor versus a glucagon-like peptide-1 (GLP-1) receptor agonist was associated with more lower limb amputations, nonvertebral fractures, and genital infections, but these risks need to be balanced against cardiovascular and renoprotective benefits, according to the researchers.
The analysis showed that there would be 2.1 more lower limb amputations, 2.5 more nonvertebral fractures, and 41 more genital infections per 1,000 patients per year among those receiving SGLT2 inhibitors versus an equal number of patients receiving GLP-1 agonists, lead author Edouard Fu, PhD, explained to this news organization in an email.
“On the other hand, we know from the evidence from randomized controlled trials that taking an SGLT2 inhibitor compared with placebo lowers the risk of developing kidney failure,” said Dr. Fu, who is a research fellow in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
“For instance,” he continued, “in the DAPA-CKD clinical trial, dapagliflozin versus placebo led to 29 fewer events per 1,000 patients per year of the composite outcome (50% decline in estimated glomerular filtration rate [eGFR], kidney failure, cardiovascular or kidney death).”
In the CREDENCE trial, canagliflozin versus placebo led to 18 fewer events per 1,000 person-years for the composite outcome of doubling of serum creatinine, kidney failure, and cardiovascular or kidney death.
And in the EMPA-KIDNEY study, empagliflozin versus placebo led to 21 fewer events per 1,000 person-years for the composite outcome of progression of kidney disease or cardiovascular death.
“Thus, benefits would still outweigh the risks,” Dr. Fu emphasized.
‘Quantifies absolute rate of events among routine care patients’
“The importance of our paper,” he summarized, “is that it quantifies the absolute rate of events among routine care patients and may be used to inform shared decision-making.”
The analysis also found that the risks of diabetic ketoacidosis (DKA), hypovolemia, hypoglycemia, and severe urinary tract infection (UTI) were similar with SGLT2 inhibitors versus GLP-1 agonists, but the risk of developing acute kidney injury (AKI) was lower with an SGLT2 inhibitor.
“Our study can help inform patient-physician decision-making regarding risks and benefits before prescribing SGLT2 inhibitors in this population” of patients with CKD and diabetes treated in clinical practice, the researchers conclude, “but needs to be interpreted in light of its limitations, including residual confounding, short follow-up time, and the use of diagnosis codes to identify patients with CKD.”
The study was recently published in the Clinical Journal of the American Society of Nephrology.
Slow uptake, safety concerns
SGLT2 inhibitors are recommended as first-line therapy in patients with type 2 diabetes and CKD who have an eGFR equal to or greater than 20 mL/min per 1.73 m2, and thus are at high risk for cardiovascular disease and kidney disease progression, Dr. Fu and colleagues write.
However, studies report that as few as 6% of patients with CKD and type 2 diabetes are currently prescribed SGLT2 inhibitors in the United States.
This slow uptake of SGLT2 inhibitors among patients with CKD may be partly due to concerns about DKA, fractures, amputations, and urogenital infections observed in clinical trials.
However, such trials are generally underpowered to assess rare adverse events, use monitoring protocols to lower the risk of adverse events, and include a highly selected patient population, and so safety in routine clinical practice is often unclear.
To examine this, the researchers identified health insurance claims data from 96,128 individuals (from Optum, IBM MarketScan, and Medicare databases) who were 18 years or older (65 years or older for Medicare) and had type 2 diabetes and at least one inpatient or two outpatient diagnostic codes for stage 3 or 4 CKD.
Of these patients, 32,192 had a newly filled prescription for an SGLT2 inhibitor (empagliflozin, dapagliflozin, canagliflozin, or ertugliflozin) and 63,936 had a newly filled prescription for a GLP-1 agonist (liraglutide, dulaglutide, semaglutide, exenatide, albiglutide, or lixisenatide) between April 2013, when the first SGLT2 inhibitor was available in the United States, and 2021.
The researchers matched 28,847 individuals who were initiated on an SGLT2 inhibitor with an equal number who were initiated on a GLP-1 agonist, based on propensity scores, adjusting for more than 120 baseline characteristics.
Safety outcomes were based on previously identified potential safety signals.
Patients who were initiated on an SGLT2 inhibitor had 1.30-fold, 2.13-fold, and 3.08-fold higher risks of having a nonvertebral fracture, a lower limb amputation, and a genital infection, respectively, compared with patients who were initiated on a GLP-1 agonist, after a mean on-treatment time of 7.5 months,
Risks of DKA, hypovolemia, hypoglycemia, and severe UTI were similar in both groups.
Patients initiated on an SGLT2 inhibitor versus a GLP-1 agonist had a lower risk of AKI (hazard ratio, 0.93) equivalent to 6.75 fewer cases of AKI per 1,000 patients per year.
Patients had higher risks for lower limb amputation, genital infections, and nonvertebral fractures with SGLT2 inhibitors versus GLP-1 agonists across most of the prespecified subgroups by age, sex, cardiovascular disease, heart failure, and use of metformin, insulin, or sulfonylurea, but with wider confidence intervals.
Dr. Fu was supported by a Rubicon grant from the Dutch Research Council and has reported no relevant financial relationships. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Starting therapy with an SGLT2 inhibitor versus a glucagon-like peptide-1 (GLP-1) receptor agonist was associated with more lower limb amputations, nonvertebral fractures, and genital infections, but these risks need to be balanced against cardiovascular and renoprotective benefits, according to the researchers.
The analysis showed that there would be 2.1 more lower limb amputations, 2.5 more nonvertebral fractures, and 41 more genital infections per 1,000 patients per year among those receiving SGLT2 inhibitors versus an equal number of patients receiving GLP-1 agonists, lead author Edouard Fu, PhD, explained to this news organization in an email.
“On the other hand, we know from the evidence from randomized controlled trials that taking an SGLT2 inhibitor compared with placebo lowers the risk of developing kidney failure,” said Dr. Fu, who is a research fellow in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
“For instance,” he continued, “in the DAPA-CKD clinical trial, dapagliflozin versus placebo led to 29 fewer events per 1,000 patients per year of the composite outcome (50% decline in estimated glomerular filtration rate [eGFR], kidney failure, cardiovascular or kidney death).”
In the CREDENCE trial, canagliflozin versus placebo led to 18 fewer events per 1,000 person-years for the composite outcome of doubling of serum creatinine, kidney failure, and cardiovascular or kidney death.
And in the EMPA-KIDNEY study, empagliflozin versus placebo led to 21 fewer events per 1,000 person-years for the composite outcome of progression of kidney disease or cardiovascular death.
“Thus, benefits would still outweigh the risks,” Dr. Fu emphasized.
‘Quantifies absolute rate of events among routine care patients’
“The importance of our paper,” he summarized, “is that it quantifies the absolute rate of events among routine care patients and may be used to inform shared decision-making.”
The analysis also found that the risks of diabetic ketoacidosis (DKA), hypovolemia, hypoglycemia, and severe urinary tract infection (UTI) were similar with SGLT2 inhibitors versus GLP-1 agonists, but the risk of developing acute kidney injury (AKI) was lower with an SGLT2 inhibitor.
“Our study can help inform patient-physician decision-making regarding risks and benefits before prescribing SGLT2 inhibitors in this population” of patients with CKD and diabetes treated in clinical practice, the researchers conclude, “but needs to be interpreted in light of its limitations, including residual confounding, short follow-up time, and the use of diagnosis codes to identify patients with CKD.”
The study was recently published in the Clinical Journal of the American Society of Nephrology.
Slow uptake, safety concerns
SGLT2 inhibitors are recommended as first-line therapy in patients with type 2 diabetes and CKD who have an eGFR equal to or greater than 20 mL/min per 1.73 m2, and thus are at high risk for cardiovascular disease and kidney disease progression, Dr. Fu and colleagues write.
However, studies report that as few as 6% of patients with CKD and type 2 diabetes are currently prescribed SGLT2 inhibitors in the United States.
This slow uptake of SGLT2 inhibitors among patients with CKD may be partly due to concerns about DKA, fractures, amputations, and urogenital infections observed in clinical trials.
However, such trials are generally underpowered to assess rare adverse events, use monitoring protocols to lower the risk of adverse events, and include a highly selected patient population, and so safety in routine clinical practice is often unclear.
To examine this, the researchers identified health insurance claims data from 96,128 individuals (from Optum, IBM MarketScan, and Medicare databases) who were 18 years or older (65 years or older for Medicare) and had type 2 diabetes and at least one inpatient or two outpatient diagnostic codes for stage 3 or 4 CKD.
Of these patients, 32,192 had a newly filled prescription for an SGLT2 inhibitor (empagliflozin, dapagliflozin, canagliflozin, or ertugliflozin) and 63,936 had a newly filled prescription for a GLP-1 agonist (liraglutide, dulaglutide, semaglutide, exenatide, albiglutide, or lixisenatide) between April 2013, when the first SGLT2 inhibitor was available in the United States, and 2021.
The researchers matched 28,847 individuals who were initiated on an SGLT2 inhibitor with an equal number who were initiated on a GLP-1 agonist, based on propensity scores, adjusting for more than 120 baseline characteristics.
Safety outcomes were based on previously identified potential safety signals.
Patients who were initiated on an SGLT2 inhibitor had 1.30-fold, 2.13-fold, and 3.08-fold higher risks of having a nonvertebral fracture, a lower limb amputation, and a genital infection, respectively, compared with patients who were initiated on a GLP-1 agonist, after a mean on-treatment time of 7.5 months,
Risks of DKA, hypovolemia, hypoglycemia, and severe UTI were similar in both groups.
Patients initiated on an SGLT2 inhibitor versus a GLP-1 agonist had a lower risk of AKI (hazard ratio, 0.93) equivalent to 6.75 fewer cases of AKI per 1,000 patients per year.
Patients had higher risks for lower limb amputation, genital infections, and nonvertebral fractures with SGLT2 inhibitors versus GLP-1 agonists across most of the prespecified subgroups by age, sex, cardiovascular disease, heart failure, and use of metformin, insulin, or sulfonylurea, but with wider confidence intervals.
Dr. Fu was supported by a Rubicon grant from the Dutch Research Council and has reported no relevant financial relationships. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Starting therapy with an SGLT2 inhibitor versus a glucagon-like peptide-1 (GLP-1) receptor agonist was associated with more lower limb amputations, nonvertebral fractures, and genital infections, but these risks need to be balanced against cardiovascular and renoprotective benefits, according to the researchers.
The analysis showed that there would be 2.1 more lower limb amputations, 2.5 more nonvertebral fractures, and 41 more genital infections per 1,000 patients per year among those receiving SGLT2 inhibitors versus an equal number of patients receiving GLP-1 agonists, lead author Edouard Fu, PhD, explained to this news organization in an email.
“On the other hand, we know from the evidence from randomized controlled trials that taking an SGLT2 inhibitor compared with placebo lowers the risk of developing kidney failure,” said Dr. Fu, who is a research fellow in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston.
“For instance,” he continued, “in the DAPA-CKD clinical trial, dapagliflozin versus placebo led to 29 fewer events per 1,000 patients per year of the composite outcome (50% decline in estimated glomerular filtration rate [eGFR], kidney failure, cardiovascular or kidney death).”
In the CREDENCE trial, canagliflozin versus placebo led to 18 fewer events per 1,000 person-years for the composite outcome of doubling of serum creatinine, kidney failure, and cardiovascular or kidney death.
And in the EMPA-KIDNEY study, empagliflozin versus placebo led to 21 fewer events per 1,000 person-years for the composite outcome of progression of kidney disease or cardiovascular death.
“Thus, benefits would still outweigh the risks,” Dr. Fu emphasized.
‘Quantifies absolute rate of events among routine care patients’
“The importance of our paper,” he summarized, “is that it quantifies the absolute rate of events among routine care patients and may be used to inform shared decision-making.”
The analysis also found that the risks of diabetic ketoacidosis (DKA), hypovolemia, hypoglycemia, and severe urinary tract infection (UTI) were similar with SGLT2 inhibitors versus GLP-1 agonists, but the risk of developing acute kidney injury (AKI) was lower with an SGLT2 inhibitor.
“Our study can help inform patient-physician decision-making regarding risks and benefits before prescribing SGLT2 inhibitors in this population” of patients with CKD and diabetes treated in clinical practice, the researchers conclude, “but needs to be interpreted in light of its limitations, including residual confounding, short follow-up time, and the use of diagnosis codes to identify patients with CKD.”
The study was recently published in the Clinical Journal of the American Society of Nephrology.
Slow uptake, safety concerns
SGLT2 inhibitors are recommended as first-line therapy in patients with type 2 diabetes and CKD who have an eGFR equal to or greater than 20 mL/min per 1.73 m2, and thus are at high risk for cardiovascular disease and kidney disease progression, Dr. Fu and colleagues write.
However, studies report that as few as 6% of patients with CKD and type 2 diabetes are currently prescribed SGLT2 inhibitors in the United States.
This slow uptake of SGLT2 inhibitors among patients with CKD may be partly due to concerns about DKA, fractures, amputations, and urogenital infections observed in clinical trials.
However, such trials are generally underpowered to assess rare adverse events, use monitoring protocols to lower the risk of adverse events, and include a highly selected patient population, and so safety in routine clinical practice is often unclear.
To examine this, the researchers identified health insurance claims data from 96,128 individuals (from Optum, IBM MarketScan, and Medicare databases) who were 18 years or older (65 years or older for Medicare) and had type 2 diabetes and at least one inpatient or two outpatient diagnostic codes for stage 3 or 4 CKD.
Of these patients, 32,192 had a newly filled prescription for an SGLT2 inhibitor (empagliflozin, dapagliflozin, canagliflozin, or ertugliflozin) and 63,936 had a newly filled prescription for a GLP-1 agonist (liraglutide, dulaglutide, semaglutide, exenatide, albiglutide, or lixisenatide) between April 2013, when the first SGLT2 inhibitor was available in the United States, and 2021.
The researchers matched 28,847 individuals who were initiated on an SGLT2 inhibitor with an equal number who were initiated on a GLP-1 agonist, based on propensity scores, adjusting for more than 120 baseline characteristics.
Safety outcomes were based on previously identified potential safety signals.
Patients who were initiated on an SGLT2 inhibitor had 1.30-fold, 2.13-fold, and 3.08-fold higher risks of having a nonvertebral fracture, a lower limb amputation, and a genital infection, respectively, compared with patients who were initiated on a GLP-1 agonist, after a mean on-treatment time of 7.5 months,
Risks of DKA, hypovolemia, hypoglycemia, and severe UTI were similar in both groups.
Patients initiated on an SGLT2 inhibitor versus a GLP-1 agonist had a lower risk of AKI (hazard ratio, 0.93) equivalent to 6.75 fewer cases of AKI per 1,000 patients per year.
Patients had higher risks for lower limb amputation, genital infections, and nonvertebral fractures with SGLT2 inhibitors versus GLP-1 agonists across most of the prespecified subgroups by age, sex, cardiovascular disease, heart failure, and use of metformin, insulin, or sulfonylurea, but with wider confidence intervals.
Dr. Fu was supported by a Rubicon grant from the Dutch Research Council and has reported no relevant financial relationships. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
New coalition aims to revolutionize stalled lupus research
Clinical research into lupus has long been hampered by failures of medications that initially seemed promising. Now, a coalition of drugmakers, federal regulators, and activists has come together to forge a path toward better-designed studies and – potentially – groundbreaking new drugs.
“We have an opportunity to work collaboratively in lupus to address the challenges in drug development,” Teodora Staeva, PhD, vice president and chief scientific officer of the Lupus Research Alliance, said in an interview.
The alliance held a press conference on March 29 to announce the formation of the public-private Lupus Accelerating Breakthroughs Consortium. Coalition members include several major drugmakers, lupus organizations such as the LRA, the American College of Rheumatology, the Food and Drug Administration, and other federal agencies. Academic researchers, people living with lupus, caregivers and family members, and other members of the lupus community are also on board.
As Dr. Staeva explained, research into lupus has been marked by a high rate of failure. “Often, phase 2 trial successes have not translated into phase 3 successes,” she said.
But researchers, she said, don’t tend to think this is because the drugs themselves are useless.
Instead, it appears that “trial designs are not adequate to capture meaningful readouts of the drug effects, and that may have contributed to the multiple failures,” she said.
According to her, this may because the trials aren’t yet designed to fully detect whether drugs are useful. This is difficult to accomplish since patients have so many manifestations of the disease and trial participants already take a variety of existing drugs.
“Another major limitation has been the lack of integration of the patient’s voice and needs in the drug development process,” she said. It’s also challenging to recruit patients with the most severe lupus to participate in studies, especially since the trials often last 52 weeks.
The new coalition will not directly develop or favor specific drugs. Instead, it will focus on clinical research priorities. “It’s all open and collaborative,” Dr. Staeva explained, and a patient council will provide input. “We have a unique opportunity to bring the voice of people [living with lupus] to the table for the first time and be able to integrate their needs and priorities into the infrastructure.”
The new coalition was inspired by existing public-private partnerships such as the Kidney Health Initiative, she said. That initiative was founded in 2012 by the FDA and the American Society of Nephrology and has dozens of members, including multiple drugmakers and medical societies.
The leadership of the Lupus ABC coalition will include three nonvoting members from the FDA. They’ll offer guidance, Dr. Staeva said. At the press conference, Albert T. Roy, president and CEO of the LRA, said drug companies will appreciate the opportunity to speak with FDA representatives “in a space that is not competitive with respect to intellectual property or anything like that.”
The coalition will meet later in spring 2023, Dr. Staeva said. She hopes it will launch a couple of projects by the end of 2023 and be able to release preliminary results by the end of 2024.
One challenge will be figuring out how to stratify trial subjects so drug studies will more easily detect medications that may work in smaller populations of patients, Hoang Nguyen, PhD, director of scientific partnerships at the LRA, said in an interview. “Now we lump [patients] all together, and that’s not the optimal way to test drugs on patients who have a lot of differences.”
According to Dr. Staeva, the LRA funded the development of the coalition, and drugmakers will primarily provide financial support going forward. The pharmaceutical company members of the coalition are Biogen, Bristol-Myers Squibb, Eli Lilly, EMD Serono, Genentech, Gilead, GlaxoSmithKline, Merck, and Takeda.
Dr. Staeva, Dr. Nguyen, and Mr. Roy have no disclosures.
Clinical research into lupus has long been hampered by failures of medications that initially seemed promising. Now, a coalition of drugmakers, federal regulators, and activists has come together to forge a path toward better-designed studies and – potentially – groundbreaking new drugs.
“We have an opportunity to work collaboratively in lupus to address the challenges in drug development,” Teodora Staeva, PhD, vice president and chief scientific officer of the Lupus Research Alliance, said in an interview.
The alliance held a press conference on March 29 to announce the formation of the public-private Lupus Accelerating Breakthroughs Consortium. Coalition members include several major drugmakers, lupus organizations such as the LRA, the American College of Rheumatology, the Food and Drug Administration, and other federal agencies. Academic researchers, people living with lupus, caregivers and family members, and other members of the lupus community are also on board.
As Dr. Staeva explained, research into lupus has been marked by a high rate of failure. “Often, phase 2 trial successes have not translated into phase 3 successes,” she said.
But researchers, she said, don’t tend to think this is because the drugs themselves are useless.
Instead, it appears that “trial designs are not adequate to capture meaningful readouts of the drug effects, and that may have contributed to the multiple failures,” she said.
According to her, this may because the trials aren’t yet designed to fully detect whether drugs are useful. This is difficult to accomplish since patients have so many manifestations of the disease and trial participants already take a variety of existing drugs.
“Another major limitation has been the lack of integration of the patient’s voice and needs in the drug development process,” she said. It’s also challenging to recruit patients with the most severe lupus to participate in studies, especially since the trials often last 52 weeks.
The new coalition will not directly develop or favor specific drugs. Instead, it will focus on clinical research priorities. “It’s all open and collaborative,” Dr. Staeva explained, and a patient council will provide input. “We have a unique opportunity to bring the voice of people [living with lupus] to the table for the first time and be able to integrate their needs and priorities into the infrastructure.”
The new coalition was inspired by existing public-private partnerships such as the Kidney Health Initiative, she said. That initiative was founded in 2012 by the FDA and the American Society of Nephrology and has dozens of members, including multiple drugmakers and medical societies.
The leadership of the Lupus ABC coalition will include three nonvoting members from the FDA. They’ll offer guidance, Dr. Staeva said. At the press conference, Albert T. Roy, president and CEO of the LRA, said drug companies will appreciate the opportunity to speak with FDA representatives “in a space that is not competitive with respect to intellectual property or anything like that.”
The coalition will meet later in spring 2023, Dr. Staeva said. She hopes it will launch a couple of projects by the end of 2023 and be able to release preliminary results by the end of 2024.
One challenge will be figuring out how to stratify trial subjects so drug studies will more easily detect medications that may work in smaller populations of patients, Hoang Nguyen, PhD, director of scientific partnerships at the LRA, said in an interview. “Now we lump [patients] all together, and that’s not the optimal way to test drugs on patients who have a lot of differences.”
According to Dr. Staeva, the LRA funded the development of the coalition, and drugmakers will primarily provide financial support going forward. The pharmaceutical company members of the coalition are Biogen, Bristol-Myers Squibb, Eli Lilly, EMD Serono, Genentech, Gilead, GlaxoSmithKline, Merck, and Takeda.
Dr. Staeva, Dr. Nguyen, and Mr. Roy have no disclosures.
Clinical research into lupus has long been hampered by failures of medications that initially seemed promising. Now, a coalition of drugmakers, federal regulators, and activists has come together to forge a path toward better-designed studies and – potentially – groundbreaking new drugs.
“We have an opportunity to work collaboratively in lupus to address the challenges in drug development,” Teodora Staeva, PhD, vice president and chief scientific officer of the Lupus Research Alliance, said in an interview.
The alliance held a press conference on March 29 to announce the formation of the public-private Lupus Accelerating Breakthroughs Consortium. Coalition members include several major drugmakers, lupus organizations such as the LRA, the American College of Rheumatology, the Food and Drug Administration, and other federal agencies. Academic researchers, people living with lupus, caregivers and family members, and other members of the lupus community are also on board.
As Dr. Staeva explained, research into lupus has been marked by a high rate of failure. “Often, phase 2 trial successes have not translated into phase 3 successes,” she said.
But researchers, she said, don’t tend to think this is because the drugs themselves are useless.
Instead, it appears that “trial designs are not adequate to capture meaningful readouts of the drug effects, and that may have contributed to the multiple failures,” she said.
According to her, this may because the trials aren’t yet designed to fully detect whether drugs are useful. This is difficult to accomplish since patients have so many manifestations of the disease and trial participants already take a variety of existing drugs.
“Another major limitation has been the lack of integration of the patient’s voice and needs in the drug development process,” she said. It’s also challenging to recruit patients with the most severe lupus to participate in studies, especially since the trials often last 52 weeks.
The new coalition will not directly develop or favor specific drugs. Instead, it will focus on clinical research priorities. “It’s all open and collaborative,” Dr. Staeva explained, and a patient council will provide input. “We have a unique opportunity to bring the voice of people [living with lupus] to the table for the first time and be able to integrate their needs and priorities into the infrastructure.”
The new coalition was inspired by existing public-private partnerships such as the Kidney Health Initiative, she said. That initiative was founded in 2012 by the FDA and the American Society of Nephrology and has dozens of members, including multiple drugmakers and medical societies.
The leadership of the Lupus ABC coalition will include three nonvoting members from the FDA. They’ll offer guidance, Dr. Staeva said. At the press conference, Albert T. Roy, president and CEO of the LRA, said drug companies will appreciate the opportunity to speak with FDA representatives “in a space that is not competitive with respect to intellectual property or anything like that.”
The coalition will meet later in spring 2023, Dr. Staeva said. She hopes it will launch a couple of projects by the end of 2023 and be able to release preliminary results by the end of 2024.
One challenge will be figuring out how to stratify trial subjects so drug studies will more easily detect medications that may work in smaller populations of patients, Hoang Nguyen, PhD, director of scientific partnerships at the LRA, said in an interview. “Now we lump [patients] all together, and that’s not the optimal way to test drugs on patients who have a lot of differences.”
According to Dr. Staeva, the LRA funded the development of the coalition, and drugmakers will primarily provide financial support going forward. The pharmaceutical company members of the coalition are Biogen, Bristol-Myers Squibb, Eli Lilly, EMD Serono, Genentech, Gilead, GlaxoSmithKline, Merck, and Takeda.
Dr. Staeva, Dr. Nguyen, and Mr. Roy have no disclosures.
Biosimilars and patients: Discussions should address safety, cost, and anxiety about change
Rheumatologist Marcus Snow, MD, is comfortable with prescribing biosimilars as a first-line, first-time biologic, and discussing them with patients.
“If a biosimilar is on the market, it has gone through rigorous study proving its effectiveness and equivalence to a bio-originator,” said Dr. Snow, a rheumatologist with the University of Nebraska Medical Center, Omaha, and chair of the American College of Rheumatology’s Committee on Rheumatologic Care.
The formulary makes a big difference in the conversation about options, he said. “The formularies dictate what we can prescribe. It may not be appropriate, but it is reality. The cost of biologics for a patient without insurance coverage makes it impossible to afford.”
He will often tell patients that he’ll fight any changes or formulary restrictions he does not agree with. “However, when I see patients in follow-up, even if there is no known change on the horizon, I may bring up biosimilars when we have a moment to chat about them to familiarize them with what may happen in the future.”
The need for patient education on biosimilars presents a barrier to realizing their potential to save money and expand choice, noted Cardinal Health in its 2023 biosimilars report. Of 103 rheumatologists who responded to a Cardinal Health survey, 85% agreed that patient education was important. But those conversations can take an uncomfortable turn if the patient pushes back against taking a biosimilar owing to cost or safety concerns.
It’s not uncommon for a patient to express some anxiety about biosimilars, especially if they’re doing well on a current treatment plan. Most patients do not want any changes that may lead to worsening disease control, Dr. Snow said.
Patients and physicians alike often don’t understand the mechanics of biosimilars. “There’s a lot of misinformation about this,” said Sameer Awsare, MD, an associate executive director for The Permanente Medical Group in Campbell, Calif. Patients should know that a biosimilar will be as clinically efficacious as the medicine they’ve been on, with the same safety profiles, said Dr. Awsare, who works with Kaiser Permanente’s pharmacy partners on biosimilars.
Insurance often drives the conversation
The global anti-inflammatory biologics market is anticipated to reach $150 billion by 2027, according to a recent CVS report. As of March 2023, the Food and Drug Administration had approved 40 biosimilars to 11 different reference products. There are 28 on the U.S. market and 100 more in development. Projected to save more than $180 billion over the next 5 years, they are anticipated to expand choice and drive competition.
Rheumatologists, dermatologists, and gastroenterologists are frequent prescribers, although their choices for immune-mediated inflammatory diseases are limited to tumor necrosis factor inhibitors (infliximab [Remicade] originator and adalimumab [Humira] originator) and anti-CD20 agents, such as rituximab (Rituxan) originator.
Benefit design or formulary usually dictates what medicine a patient receives. “Because of significantly higher out-of-pocket cost or formulary positioning, patients may end up with a generic or a biosimilar instead of a brand-name medicine or branded biologic,” said Robert Popovian, PharmD, MS, chief science policy officer of the Global Healthy Living Foundation.
Insurers rarely offer both Remicade and biosimilar infliximab, allowing the doctor to choose, said Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, who prescribes infliximab biosimilars. Most often, the payer will choose the lower-cost biosimilar. “I am fine with the biosimilar, either as a new start or a switch from the reference product.”
However, the patient might feel differently. They can form an attachment to the reference medication if it has prevented severe illness. “They do not want to change, as they feel they are going on a ‘new’ medication that will not work as well,” Dr. Regueiro said.
This is where the education comes in: to reassure patients that a biosimilar will work just as well as the reference product. “For patients who have done well for years on a biologic, more time needs to be spent reassuring them and answering questions,” compared with a patient just starting on a biosimilar, he advised.
But not all physicians are quick to prescribe biosimilars.
Especially with psoriasis, which has so many strong options for reference drugs, a switch may be hard to justify, said dermatologist Stephanie K. Fabbro, MD, assistant professor at Northeast Ohio Medical University, Rootstown. “If I have a preference, I would rather switch a patient to a drug from a different class without a biosimilar option to reduce the possibility of pushback.”
Dr. Fabbro, part of the core faculty in the Riverside Methodist Hospital Dermatology Residency Program in Columbus, will share data from clinical trials and postmarket surveillance with patients to support her decision.
Conversations about cost
Patients may also push back if they don’t save money when switching to a biosimilar. “This dilemma raises the question of who is profiting when a biosimilar is dispensed,” Dr. Popovian said. Insurers and pharmacy benefit managers (PBMs) that take additional concessions from biopharmaceutical manufacturers in the form of rebates and fees will often pocket this money as profit instead of passing savings back to the patient to help reduce their out-of-pocket requirement, he added.
If an originator biologic and a biosimilar are available, “as a pharmacist, I will choose the medicine that will incur the lowest out-of-pocket cost for the patient,” Dr. Popovian said.
Discussing cost – and who dictates which biosimilar is on the formulary – is an important conversation to have with patients, said Vivek Kaul, MD, Segal-Watson Professor of Medicine at the University of Rochester (N.Y.) Medical Center.
Providing equivalent clinical efficacy while saving costs is the economic reality of biosimilars, Dr. Kaul said. Third-party payers regularly evaluate how to provide the same quality of care while saving money. Physicians and patients alike “must be mindful that as time goes on, if the science on biosimilars stays robust, if the adoption is more widespread and the cost-saving proposition turns out to be true, more formularies will be attracted to replacing the reference product with the biosimilar counterpart.”
Providers and patients can weigh the options if a formulary suddenly switches to a biosimilar, Dr. Kaul continued. “You can accept the novel product on the formulary or may have to face out-of-pocket expenses as a patient.” If providers and patients have concerns about the biosimilar, they can always appeal if there’s solid scientific evidence that supports reverting back to the reference product.
“If you think the biosimilar is equally efficacious, comes at a lower cost, and is right for the patient, then the providers should tell the patient that,” he added.
Some studies have questioned whether the biosimilars will save money, compared with the reference drug, Dr. Fabbro noted. Medicare, for example, may pay only for a certain percentage of an approved biosimilar, saddling the patient with a monthly copay costing thousands of dollars. “It is unclear whether biosimilar manufacturers will have the same level of patient support programs as the reference drug companies.”
For that reason, physicians should also inform patients about the robust patient assistance and copay assistance programs many reference drug manufacturers offer, she said.
Biosimilars 101: Familiarizing patients
Safety and ease of use are other common concerns about biosimilars. Patients may ask if the application is different, or why it’s advantageous to switch to a biosimilar, Dr. Awsare said.
Sometimes the syringe or injector for a biosimilar might look different from that of the originator drug, he said.
Anecdotally, Dr. Fabbro has heard stories of patients having injection reactions that they did not experience with the reference drug or having a disease flare-up after starting a biosimilar.
As is the case with reference products, in their conversations with patients, clinicians should address the adverse event profile of biosimilars, offering data points from published studies and clinical guidelines that support the use of these products. “There should be an emphasis on patient education around efficacy and any side effects, and how the profile of the reference product compares with a proposed biosimilar,” Dr. Kaul suggested.
When Dr. Snow discusses biosimilars and generics, “I make sure to share this in an understandable way based on the patient’s scientific background, or lack thereof,” he said. If there is enough time, he also discusses how European- and U.S.-sourced biologics are slightly different.
Pharmacists should tell patients to expect the same clinical outcomes from a biosimilar, Dr. Popovian said. However, if they have any reduction in efficacy or potential safety concerns, they should communicate with their physician or pharmacist immediately.
In Dr. Regueiro’s practice, a pharmacist specializing in inflammatory bowel disease often has a one-on-one meeting with patients to educate and answer questions. “Additionally, we provide them the Crohn’s and Colitis Foundation web link on biosimilars,” said Dr. Regueiro.
A village approach to education
When biosimilars first came out, there were no formal education materials, Dr. Awsare said. Kaiser Permanente decided to create its own educational materials, not just for patients but also to help educate its primary care doctors; the rheumatologists, dermatologists, and gastroenterologists using the biosimilars; the nurses infusing patients; and the pharmacists preparing the biosimilars.
The health system also has a different approach to choosing medication. Instead of having an insurance company or PBM decide what’s in the formulary, clinicians work with the pharmacists at Kaiser to look at clinical evidence and decide which biosimilar to use. Most of its plans also provide lower copays to patients when they use the biosimilar.
This was the approach for Humira biosimilars, Dr. Awsare said. Eight will be on the market in 2023. “Our rheumatologists, dermatologists, and gastroenterologists looked at the data from Europe, looked at some real-world evidence, and then said: ‘We think this one’s going to be the best one for our patients.’ ”
Having clinicians choose the biosimilar instead of a health plan makes it a lot easier to have conversations with patients, he said. “Once we’ve moved that market share to that particular biosimilar, we give our physicians the time to have those discussions.”
Clinical pharmacists also provide educational support, offering guidance on issues such as side effects, as patients transition to the biosimilar. “We like to use the word ‘transition’ because it’s essentially the same biologic. So, you’re not actually switching,” Dr. Awsare said.
No consensus on interchangeability
Whether the conversation on interchangeability will affect patient conversations with physicians depends on who you ask.
If a biosimilar has an interchangeability designation, it means that the pharmacist can substitute it without the intervention of the clinician who prescribed the reference product. It does not relate to the quality, safety, or effectiveness of biosimilars or interchangeable biosimilar products, Dr. Popovian said.
The United States is the only country that has this designation. Even though it’s not identical to the originator drug, a biosimilar has the same clinical efficacy and safety profile. “So clinically, interchangeability is meaningless,” Dr. Awsare said.
In its report on biosimilars in the autoimmune category, CVS acknowledged that interchangeability was important but would not be a significant factor in driving adoption of biosimilars. However, in a Cardinal Health survey of 72 gastroenterologists, 38% cited the interchangeability of biosimilars as a top concern for adalimumab biosimilars, along with transitioning patients from Humira to a biosimilar (44%).
“Patient education regarding biosimilar safety, efficacy, and interchangeability appears paramount to the acceptance of these products, particularly for patients who are switched from a reference product,” Dr. Kaul noted in the Cardinal Health report.
Wherever supported by data, Dr. Kaul recommends incorporating biosimilar use and interchangeability into best practice guidelines going forward. “That will go a long way in disseminating the latest information on this topic and position this paradigm for increased adoption among providers.”
Some physicians like Dr. Snow aren’t that concerned with interchangeability. This hasn’t affected conversations with patients, he said. Multiple studies demonstrating the lack of antibody formation with multiple switches from different biosimilar drugs has eased his concern about multiple switches causing problems.
“Initially, there was a gap in demonstrating the long-term effect of multiple switches on antibody production and drug effectiveness. That gap has started to close as more data from Europe’s experience with biosimilars becomes available,” Dr. Snow said.
Resources for physicians, patients
The federal government has taken steps to advance biosimilars education and adoption. In 2021, President Biden signed the Advancing Education on Biosimilars Act into law, which directs the FDA to develop or improve continuing education programs that address prescribing of biosimilars and biological products.
The FDA provides educational materials on its website, including a comprehensive curriculum toolkit. The Accreditation Council for Medical Affairs has also created an online 40-hour curriculum for health care professionals called the Board-Certified Biologics and Biosimilars Specialist Program.
Dr. Fabbro recommended patients use the FDA page Biosimilar Basics for Patients to educate themselves on biosimilars. The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars, is another free resource for patients.
“While much has changed, the continued need for multistakeholder education, awareness, and dedicated research remains even more important as we expand into newer therapeutic areas and classes,” wrote the authors of the Cardinal Health report.
Help patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars.
Dr. Regueiro is on advisory boards and consults for AbbVie, Janssen, UCB, Takeda, Pfizer, Bristol-Myers Squibb, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET PharmaSolutions, Trellis, and Boehringer Ingelheim. Dr. Fabbro is a principal investigator for Castle Biosciences, on the speakers bureau for Valchlor, and on the advisory boards of Janssen and Bristol-Myers Squibb. Dr. Popovian, Dr. Snow, Dr. Awsare, and Dr. Kaul had no disclosures.
A version of this article originally appeared on Medscape.com.
Rheumatologist Marcus Snow, MD, is comfortable with prescribing biosimilars as a first-line, first-time biologic, and discussing them with patients.
“If a biosimilar is on the market, it has gone through rigorous study proving its effectiveness and equivalence to a bio-originator,” said Dr. Snow, a rheumatologist with the University of Nebraska Medical Center, Omaha, and chair of the American College of Rheumatology’s Committee on Rheumatologic Care.
The formulary makes a big difference in the conversation about options, he said. “The formularies dictate what we can prescribe. It may not be appropriate, but it is reality. The cost of biologics for a patient without insurance coverage makes it impossible to afford.”
He will often tell patients that he’ll fight any changes or formulary restrictions he does not agree with. “However, when I see patients in follow-up, even if there is no known change on the horizon, I may bring up biosimilars when we have a moment to chat about them to familiarize them with what may happen in the future.”
The need for patient education on biosimilars presents a barrier to realizing their potential to save money and expand choice, noted Cardinal Health in its 2023 biosimilars report. Of 103 rheumatologists who responded to a Cardinal Health survey, 85% agreed that patient education was important. But those conversations can take an uncomfortable turn if the patient pushes back against taking a biosimilar owing to cost or safety concerns.
It’s not uncommon for a patient to express some anxiety about biosimilars, especially if they’re doing well on a current treatment plan. Most patients do not want any changes that may lead to worsening disease control, Dr. Snow said.
Patients and physicians alike often don’t understand the mechanics of biosimilars. “There’s a lot of misinformation about this,” said Sameer Awsare, MD, an associate executive director for The Permanente Medical Group in Campbell, Calif. Patients should know that a biosimilar will be as clinically efficacious as the medicine they’ve been on, with the same safety profiles, said Dr. Awsare, who works with Kaiser Permanente’s pharmacy partners on biosimilars.
Insurance often drives the conversation
The global anti-inflammatory biologics market is anticipated to reach $150 billion by 2027, according to a recent CVS report. As of March 2023, the Food and Drug Administration had approved 40 biosimilars to 11 different reference products. There are 28 on the U.S. market and 100 more in development. Projected to save more than $180 billion over the next 5 years, they are anticipated to expand choice and drive competition.
Rheumatologists, dermatologists, and gastroenterologists are frequent prescribers, although their choices for immune-mediated inflammatory diseases are limited to tumor necrosis factor inhibitors (infliximab [Remicade] originator and adalimumab [Humira] originator) and anti-CD20 agents, such as rituximab (Rituxan) originator.
Benefit design or formulary usually dictates what medicine a patient receives. “Because of significantly higher out-of-pocket cost or formulary positioning, patients may end up with a generic or a biosimilar instead of a brand-name medicine or branded biologic,” said Robert Popovian, PharmD, MS, chief science policy officer of the Global Healthy Living Foundation.
Insurers rarely offer both Remicade and biosimilar infliximab, allowing the doctor to choose, said Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, who prescribes infliximab biosimilars. Most often, the payer will choose the lower-cost biosimilar. “I am fine with the biosimilar, either as a new start or a switch from the reference product.”
However, the patient might feel differently. They can form an attachment to the reference medication if it has prevented severe illness. “They do not want to change, as they feel they are going on a ‘new’ medication that will not work as well,” Dr. Regueiro said.
This is where the education comes in: to reassure patients that a biosimilar will work just as well as the reference product. “For patients who have done well for years on a biologic, more time needs to be spent reassuring them and answering questions,” compared with a patient just starting on a biosimilar, he advised.
But not all physicians are quick to prescribe biosimilars.
Especially with psoriasis, which has so many strong options for reference drugs, a switch may be hard to justify, said dermatologist Stephanie K. Fabbro, MD, assistant professor at Northeast Ohio Medical University, Rootstown. “If I have a preference, I would rather switch a patient to a drug from a different class without a biosimilar option to reduce the possibility of pushback.”
Dr. Fabbro, part of the core faculty in the Riverside Methodist Hospital Dermatology Residency Program in Columbus, will share data from clinical trials and postmarket surveillance with patients to support her decision.
Conversations about cost
Patients may also push back if they don’t save money when switching to a biosimilar. “This dilemma raises the question of who is profiting when a biosimilar is dispensed,” Dr. Popovian said. Insurers and pharmacy benefit managers (PBMs) that take additional concessions from biopharmaceutical manufacturers in the form of rebates and fees will often pocket this money as profit instead of passing savings back to the patient to help reduce their out-of-pocket requirement, he added.
If an originator biologic and a biosimilar are available, “as a pharmacist, I will choose the medicine that will incur the lowest out-of-pocket cost for the patient,” Dr. Popovian said.
Discussing cost – and who dictates which biosimilar is on the formulary – is an important conversation to have with patients, said Vivek Kaul, MD, Segal-Watson Professor of Medicine at the University of Rochester (N.Y.) Medical Center.
Providing equivalent clinical efficacy while saving costs is the economic reality of biosimilars, Dr. Kaul said. Third-party payers regularly evaluate how to provide the same quality of care while saving money. Physicians and patients alike “must be mindful that as time goes on, if the science on biosimilars stays robust, if the adoption is more widespread and the cost-saving proposition turns out to be true, more formularies will be attracted to replacing the reference product with the biosimilar counterpart.”
Providers and patients can weigh the options if a formulary suddenly switches to a biosimilar, Dr. Kaul continued. “You can accept the novel product on the formulary or may have to face out-of-pocket expenses as a patient.” If providers and patients have concerns about the biosimilar, they can always appeal if there’s solid scientific evidence that supports reverting back to the reference product.
“If you think the biosimilar is equally efficacious, comes at a lower cost, and is right for the patient, then the providers should tell the patient that,” he added.
Some studies have questioned whether the biosimilars will save money, compared with the reference drug, Dr. Fabbro noted. Medicare, for example, may pay only for a certain percentage of an approved biosimilar, saddling the patient with a monthly copay costing thousands of dollars. “It is unclear whether biosimilar manufacturers will have the same level of patient support programs as the reference drug companies.”
For that reason, physicians should also inform patients about the robust patient assistance and copay assistance programs many reference drug manufacturers offer, she said.
Biosimilars 101: Familiarizing patients
Safety and ease of use are other common concerns about biosimilars. Patients may ask if the application is different, or why it’s advantageous to switch to a biosimilar, Dr. Awsare said.
Sometimes the syringe or injector for a biosimilar might look different from that of the originator drug, he said.
Anecdotally, Dr. Fabbro has heard stories of patients having injection reactions that they did not experience with the reference drug or having a disease flare-up after starting a biosimilar.
As is the case with reference products, in their conversations with patients, clinicians should address the adverse event profile of biosimilars, offering data points from published studies and clinical guidelines that support the use of these products. “There should be an emphasis on patient education around efficacy and any side effects, and how the profile of the reference product compares with a proposed biosimilar,” Dr. Kaul suggested.
When Dr. Snow discusses biosimilars and generics, “I make sure to share this in an understandable way based on the patient’s scientific background, or lack thereof,” he said. If there is enough time, he also discusses how European- and U.S.-sourced biologics are slightly different.
Pharmacists should tell patients to expect the same clinical outcomes from a biosimilar, Dr. Popovian said. However, if they have any reduction in efficacy or potential safety concerns, they should communicate with their physician or pharmacist immediately.
In Dr. Regueiro’s practice, a pharmacist specializing in inflammatory bowel disease often has a one-on-one meeting with patients to educate and answer questions. “Additionally, we provide them the Crohn’s and Colitis Foundation web link on biosimilars,” said Dr. Regueiro.
A village approach to education
When biosimilars first came out, there were no formal education materials, Dr. Awsare said. Kaiser Permanente decided to create its own educational materials, not just for patients but also to help educate its primary care doctors; the rheumatologists, dermatologists, and gastroenterologists using the biosimilars; the nurses infusing patients; and the pharmacists preparing the biosimilars.
The health system also has a different approach to choosing medication. Instead of having an insurance company or PBM decide what’s in the formulary, clinicians work with the pharmacists at Kaiser to look at clinical evidence and decide which biosimilar to use. Most of its plans also provide lower copays to patients when they use the biosimilar.
This was the approach for Humira biosimilars, Dr. Awsare said. Eight will be on the market in 2023. “Our rheumatologists, dermatologists, and gastroenterologists looked at the data from Europe, looked at some real-world evidence, and then said: ‘We think this one’s going to be the best one for our patients.’ ”
Having clinicians choose the biosimilar instead of a health plan makes it a lot easier to have conversations with patients, he said. “Once we’ve moved that market share to that particular biosimilar, we give our physicians the time to have those discussions.”
Clinical pharmacists also provide educational support, offering guidance on issues such as side effects, as patients transition to the biosimilar. “We like to use the word ‘transition’ because it’s essentially the same biologic. So, you’re not actually switching,” Dr. Awsare said.
No consensus on interchangeability
Whether the conversation on interchangeability will affect patient conversations with physicians depends on who you ask.
If a biosimilar has an interchangeability designation, it means that the pharmacist can substitute it without the intervention of the clinician who prescribed the reference product. It does not relate to the quality, safety, or effectiveness of biosimilars or interchangeable biosimilar products, Dr. Popovian said.
The United States is the only country that has this designation. Even though it’s not identical to the originator drug, a biosimilar has the same clinical efficacy and safety profile. “So clinically, interchangeability is meaningless,” Dr. Awsare said.
In its report on biosimilars in the autoimmune category, CVS acknowledged that interchangeability was important but would not be a significant factor in driving adoption of biosimilars. However, in a Cardinal Health survey of 72 gastroenterologists, 38% cited the interchangeability of biosimilars as a top concern for adalimumab biosimilars, along with transitioning patients from Humira to a biosimilar (44%).
“Patient education regarding biosimilar safety, efficacy, and interchangeability appears paramount to the acceptance of these products, particularly for patients who are switched from a reference product,” Dr. Kaul noted in the Cardinal Health report.
Wherever supported by data, Dr. Kaul recommends incorporating biosimilar use and interchangeability into best practice guidelines going forward. “That will go a long way in disseminating the latest information on this topic and position this paradigm for increased adoption among providers.”
Some physicians like Dr. Snow aren’t that concerned with interchangeability. This hasn’t affected conversations with patients, he said. Multiple studies demonstrating the lack of antibody formation with multiple switches from different biosimilar drugs has eased his concern about multiple switches causing problems.
“Initially, there was a gap in demonstrating the long-term effect of multiple switches on antibody production and drug effectiveness. That gap has started to close as more data from Europe’s experience with biosimilars becomes available,” Dr. Snow said.
Resources for physicians, patients
The federal government has taken steps to advance biosimilars education and adoption. In 2021, President Biden signed the Advancing Education on Biosimilars Act into law, which directs the FDA to develop or improve continuing education programs that address prescribing of biosimilars and biological products.
The FDA provides educational materials on its website, including a comprehensive curriculum toolkit. The Accreditation Council for Medical Affairs has also created an online 40-hour curriculum for health care professionals called the Board-Certified Biologics and Biosimilars Specialist Program.
Dr. Fabbro recommended patients use the FDA page Biosimilar Basics for Patients to educate themselves on biosimilars. The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars, is another free resource for patients.
“While much has changed, the continued need for multistakeholder education, awareness, and dedicated research remains even more important as we expand into newer therapeutic areas and classes,” wrote the authors of the Cardinal Health report.
Help patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars.
Dr. Regueiro is on advisory boards and consults for AbbVie, Janssen, UCB, Takeda, Pfizer, Bristol-Myers Squibb, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET PharmaSolutions, Trellis, and Boehringer Ingelheim. Dr. Fabbro is a principal investigator for Castle Biosciences, on the speakers bureau for Valchlor, and on the advisory boards of Janssen and Bristol-Myers Squibb. Dr. Popovian, Dr. Snow, Dr. Awsare, and Dr. Kaul had no disclosures.
A version of this article originally appeared on Medscape.com.
Rheumatologist Marcus Snow, MD, is comfortable with prescribing biosimilars as a first-line, first-time biologic, and discussing them with patients.
“If a biosimilar is on the market, it has gone through rigorous study proving its effectiveness and equivalence to a bio-originator,” said Dr. Snow, a rheumatologist with the University of Nebraska Medical Center, Omaha, and chair of the American College of Rheumatology’s Committee on Rheumatologic Care.
The formulary makes a big difference in the conversation about options, he said. “The formularies dictate what we can prescribe. It may not be appropriate, but it is reality. The cost of biologics for a patient without insurance coverage makes it impossible to afford.”
He will often tell patients that he’ll fight any changes or formulary restrictions he does not agree with. “However, when I see patients in follow-up, even if there is no known change on the horizon, I may bring up biosimilars when we have a moment to chat about them to familiarize them with what may happen in the future.”
The need for patient education on biosimilars presents a barrier to realizing their potential to save money and expand choice, noted Cardinal Health in its 2023 biosimilars report. Of 103 rheumatologists who responded to a Cardinal Health survey, 85% agreed that patient education was important. But those conversations can take an uncomfortable turn if the patient pushes back against taking a biosimilar owing to cost or safety concerns.
It’s not uncommon for a patient to express some anxiety about biosimilars, especially if they’re doing well on a current treatment plan. Most patients do not want any changes that may lead to worsening disease control, Dr. Snow said.
Patients and physicians alike often don’t understand the mechanics of biosimilars. “There’s a lot of misinformation about this,” said Sameer Awsare, MD, an associate executive director for The Permanente Medical Group in Campbell, Calif. Patients should know that a biosimilar will be as clinically efficacious as the medicine they’ve been on, with the same safety profiles, said Dr. Awsare, who works with Kaiser Permanente’s pharmacy partners on biosimilars.
Insurance often drives the conversation
The global anti-inflammatory biologics market is anticipated to reach $150 billion by 2027, according to a recent CVS report. As of March 2023, the Food and Drug Administration had approved 40 biosimilars to 11 different reference products. There are 28 on the U.S. market and 100 more in development. Projected to save more than $180 billion over the next 5 years, they are anticipated to expand choice and drive competition.
Rheumatologists, dermatologists, and gastroenterologists are frequent prescribers, although their choices for immune-mediated inflammatory diseases are limited to tumor necrosis factor inhibitors (infliximab [Remicade] originator and adalimumab [Humira] originator) and anti-CD20 agents, such as rituximab (Rituxan) originator.
Benefit design or formulary usually dictates what medicine a patient receives. “Because of significantly higher out-of-pocket cost or formulary positioning, patients may end up with a generic or a biosimilar instead of a brand-name medicine or branded biologic,” said Robert Popovian, PharmD, MS, chief science policy officer of the Global Healthy Living Foundation.
Insurers rarely offer both Remicade and biosimilar infliximab, allowing the doctor to choose, said Miguel Regueiro, MD, chair of the Cleveland Clinic’s Digestive Disease & Surgery Institute, who prescribes infliximab biosimilars. Most often, the payer will choose the lower-cost biosimilar. “I am fine with the biosimilar, either as a new start or a switch from the reference product.”
However, the patient might feel differently. They can form an attachment to the reference medication if it has prevented severe illness. “They do not want to change, as they feel they are going on a ‘new’ medication that will not work as well,” Dr. Regueiro said.
This is where the education comes in: to reassure patients that a biosimilar will work just as well as the reference product. “For patients who have done well for years on a biologic, more time needs to be spent reassuring them and answering questions,” compared with a patient just starting on a biosimilar, he advised.
But not all physicians are quick to prescribe biosimilars.
Especially with psoriasis, which has so many strong options for reference drugs, a switch may be hard to justify, said dermatologist Stephanie K. Fabbro, MD, assistant professor at Northeast Ohio Medical University, Rootstown. “If I have a preference, I would rather switch a patient to a drug from a different class without a biosimilar option to reduce the possibility of pushback.”
Dr. Fabbro, part of the core faculty in the Riverside Methodist Hospital Dermatology Residency Program in Columbus, will share data from clinical trials and postmarket surveillance with patients to support her decision.
Conversations about cost
Patients may also push back if they don’t save money when switching to a biosimilar. “This dilemma raises the question of who is profiting when a biosimilar is dispensed,” Dr. Popovian said. Insurers and pharmacy benefit managers (PBMs) that take additional concessions from biopharmaceutical manufacturers in the form of rebates and fees will often pocket this money as profit instead of passing savings back to the patient to help reduce their out-of-pocket requirement, he added.
If an originator biologic and a biosimilar are available, “as a pharmacist, I will choose the medicine that will incur the lowest out-of-pocket cost for the patient,” Dr. Popovian said.
Discussing cost – and who dictates which biosimilar is on the formulary – is an important conversation to have with patients, said Vivek Kaul, MD, Segal-Watson Professor of Medicine at the University of Rochester (N.Y.) Medical Center.
Providing equivalent clinical efficacy while saving costs is the economic reality of biosimilars, Dr. Kaul said. Third-party payers regularly evaluate how to provide the same quality of care while saving money. Physicians and patients alike “must be mindful that as time goes on, if the science on biosimilars stays robust, if the adoption is more widespread and the cost-saving proposition turns out to be true, more formularies will be attracted to replacing the reference product with the biosimilar counterpart.”
Providers and patients can weigh the options if a formulary suddenly switches to a biosimilar, Dr. Kaul continued. “You can accept the novel product on the formulary or may have to face out-of-pocket expenses as a patient.” If providers and patients have concerns about the biosimilar, they can always appeal if there’s solid scientific evidence that supports reverting back to the reference product.
“If you think the biosimilar is equally efficacious, comes at a lower cost, and is right for the patient, then the providers should tell the patient that,” he added.
Some studies have questioned whether the biosimilars will save money, compared with the reference drug, Dr. Fabbro noted. Medicare, for example, may pay only for a certain percentage of an approved biosimilar, saddling the patient with a monthly copay costing thousands of dollars. “It is unclear whether biosimilar manufacturers will have the same level of patient support programs as the reference drug companies.”
For that reason, physicians should also inform patients about the robust patient assistance and copay assistance programs many reference drug manufacturers offer, she said.
Biosimilars 101: Familiarizing patients
Safety and ease of use are other common concerns about biosimilars. Patients may ask if the application is different, or why it’s advantageous to switch to a biosimilar, Dr. Awsare said.
Sometimes the syringe or injector for a biosimilar might look different from that of the originator drug, he said.
Anecdotally, Dr. Fabbro has heard stories of patients having injection reactions that they did not experience with the reference drug or having a disease flare-up after starting a biosimilar.
As is the case with reference products, in their conversations with patients, clinicians should address the adverse event profile of biosimilars, offering data points from published studies and clinical guidelines that support the use of these products. “There should be an emphasis on patient education around efficacy and any side effects, and how the profile of the reference product compares with a proposed biosimilar,” Dr. Kaul suggested.
When Dr. Snow discusses biosimilars and generics, “I make sure to share this in an understandable way based on the patient’s scientific background, or lack thereof,” he said. If there is enough time, he also discusses how European- and U.S.-sourced biologics are slightly different.
Pharmacists should tell patients to expect the same clinical outcomes from a biosimilar, Dr. Popovian said. However, if they have any reduction in efficacy or potential safety concerns, they should communicate with their physician or pharmacist immediately.
In Dr. Regueiro’s practice, a pharmacist specializing in inflammatory bowel disease often has a one-on-one meeting with patients to educate and answer questions. “Additionally, we provide them the Crohn’s and Colitis Foundation web link on biosimilars,” said Dr. Regueiro.
A village approach to education
When biosimilars first came out, there were no formal education materials, Dr. Awsare said. Kaiser Permanente decided to create its own educational materials, not just for patients but also to help educate its primary care doctors; the rheumatologists, dermatologists, and gastroenterologists using the biosimilars; the nurses infusing patients; and the pharmacists preparing the biosimilars.
The health system also has a different approach to choosing medication. Instead of having an insurance company or PBM decide what’s in the formulary, clinicians work with the pharmacists at Kaiser to look at clinical evidence and decide which biosimilar to use. Most of its plans also provide lower copays to patients when they use the biosimilar.
This was the approach for Humira biosimilars, Dr. Awsare said. Eight will be on the market in 2023. “Our rheumatologists, dermatologists, and gastroenterologists looked at the data from Europe, looked at some real-world evidence, and then said: ‘We think this one’s going to be the best one for our patients.’ ”
Having clinicians choose the biosimilar instead of a health plan makes it a lot easier to have conversations with patients, he said. “Once we’ve moved that market share to that particular biosimilar, we give our physicians the time to have those discussions.”
Clinical pharmacists also provide educational support, offering guidance on issues such as side effects, as patients transition to the biosimilar. “We like to use the word ‘transition’ because it’s essentially the same biologic. So, you’re not actually switching,” Dr. Awsare said.
No consensus on interchangeability
Whether the conversation on interchangeability will affect patient conversations with physicians depends on who you ask.
If a biosimilar has an interchangeability designation, it means that the pharmacist can substitute it without the intervention of the clinician who prescribed the reference product. It does not relate to the quality, safety, or effectiveness of biosimilars or interchangeable biosimilar products, Dr. Popovian said.
The United States is the only country that has this designation. Even though it’s not identical to the originator drug, a biosimilar has the same clinical efficacy and safety profile. “So clinically, interchangeability is meaningless,” Dr. Awsare said.
In its report on biosimilars in the autoimmune category, CVS acknowledged that interchangeability was important but would not be a significant factor in driving adoption of biosimilars. However, in a Cardinal Health survey of 72 gastroenterologists, 38% cited the interchangeability of biosimilars as a top concern for adalimumab biosimilars, along with transitioning patients from Humira to a biosimilar (44%).
“Patient education regarding biosimilar safety, efficacy, and interchangeability appears paramount to the acceptance of these products, particularly for patients who are switched from a reference product,” Dr. Kaul noted in the Cardinal Health report.
Wherever supported by data, Dr. Kaul recommends incorporating biosimilar use and interchangeability into best practice guidelines going forward. “That will go a long way in disseminating the latest information on this topic and position this paradigm for increased adoption among providers.”
Some physicians like Dr. Snow aren’t that concerned with interchangeability. This hasn’t affected conversations with patients, he said. Multiple studies demonstrating the lack of antibody formation with multiple switches from different biosimilar drugs has eased his concern about multiple switches causing problems.
“Initially, there was a gap in demonstrating the long-term effect of multiple switches on antibody production and drug effectiveness. That gap has started to close as more data from Europe’s experience with biosimilars becomes available,” Dr. Snow said.
Resources for physicians, patients
The federal government has taken steps to advance biosimilars education and adoption. In 2021, President Biden signed the Advancing Education on Biosimilars Act into law, which directs the FDA to develop or improve continuing education programs that address prescribing of biosimilars and biological products.
The FDA provides educational materials on its website, including a comprehensive curriculum toolkit. The Accreditation Council for Medical Affairs has also created an online 40-hour curriculum for health care professionals called the Board-Certified Biologics and Biosimilars Specialist Program.
Dr. Fabbro recommended patients use the FDA page Biosimilar Basics for Patients to educate themselves on biosimilars. The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars, is another free resource for patients.
“While much has changed, the continued need for multistakeholder education, awareness, and dedicated research remains even more important as we expand into newer therapeutic areas and classes,” wrote the authors of the Cardinal Health report.
Help patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars.
Dr. Regueiro is on advisory boards and consults for AbbVie, Janssen, UCB, Takeda, Pfizer, Bristol-Myers Squibb, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET PharmaSolutions, Trellis, and Boehringer Ingelheim. Dr. Fabbro is a principal investigator for Castle Biosciences, on the speakers bureau for Valchlor, and on the advisory boards of Janssen and Bristol-Myers Squibb. Dr. Popovian, Dr. Snow, Dr. Awsare, and Dr. Kaul had no disclosures.
A version of this article originally appeared on Medscape.com.
Sweaty treatment for social anxiety could pass the sniff test
Getting sweet on sweat
Are you the sort of person who struggles in social situations? Have the past 3 years been a secret respite from the terror and exhaustion of meeting new people? We understand your plight. People kind of suck. And you don’t have to look far to be reminded of it.
Unfortunately, on occasion we all have to interact with other human beings. If you suffer from social anxiety, this is not a fun thing to do. But new research indicates that there may be a way to alleviate the stress for those with social anxiety: armpits.
Specifically, sweat from the armpits of other people. Yes, this means a group of scientists gathered up some volunteers and collected their armpit sweat while the volunteers watched a variety of movies (horror, comedy, romance, etc.). Our condolences to the poor unpaid interns tasked with gathering the sweat.
Once they had their precious new medicine, the researchers took a group of women and administered a round of mindfulness therapy. Some of the participants then received the various sweats, while the rest were forced to smell only clean air. (The horror!) Lo and behold, the sweat groups had their anxiety scores reduced by about 40% after their therapy, compared with just 17% in the control group.
The researchers also found that the source of the sweat didn’t matter. Their study subjects responded the same to sweat excreted during a scary movie as they did to sweat from a comedy, a result that surprised the researchers. They suggested chemosignals in the sweat may affect the treatment response and advised further research. Which means more sweat collection! They plan on testing emotionally neutral movies next time, and if we can make a humble suggestion, they also should try the sweatiest movies.
Before the Food and Drug Administration can approve armpit sweat as a treatment for social anxiety, we have some advice for those shut-in introverts out there. Next time you have to interact with rabid extroverts, instead of shaking their hands, walk up to them and take a deep whiff of their armpits. Establish dominance. Someone will feel awkward, and science has proved it won’t be you.
The puff that vaccinates
Ever been shot with a Nerf gun or hit with a foam pool tube? More annoying than painful, right? If we asked if you’d rather get pelted with one of those than receive a traditional vaccine injection, you would choose the former. Maybe someday you actually will.
During the boredom of the early pandemic lockdown, Jeremiah Gassensmith, PhD, of the department of chemistry and biochemistry at the University of Texas, Dallas, ordered a compressed gas–powered jet injection system to fool around with at home. Hey, who didn’t? Anyway, when it was time to go back to the lab he handed it over to one of his grad students, Yalini Wijesundara, and asked her to see what could be done with it.
In her tinkering she found that the jet injector could deliver metal-organic frameworks (MOFs) that can hold a bunch of different materials, like proteins and nucleic acids, through the skin.
Thus the “MOF-Jet” was born!
Jet injectors are nothing new, but they hurt. The MOF-Jet, however, is practically painless and cheaper than the gene guns that veterinarians use to inject biological cargo attached to the surface of a metal microparticle.
Changing the carrier gas also changes the time needed to break down the MOF and thus alters delivery of the drug inside. “If you shoot it with carbon dioxide, it will release its cargo faster within cells; if you use regular air, it will take 4 or 5 days,” Ms. Wijesundara explained in a written statement. That means the same drug could be released over different timescales without changing its formulation.
While testing on onion cells and mice, Ms. Wijesundara noted that it was as easy as “pointing and shooting” to distribute the puff of gas into the cells. A saving grace to those with needle anxiety. Not that we would know anything about needle anxiety.
More testing needs to be done before bringing this technology to human use, obviously, but we’re looking forward to saying goodbye to that dreaded prick and hello to a puff.
Your hippocampus is showing
Brain anatomy is one of the many, many things that’s not really our thing, but we do know a cool picture when we see one. Case in point: The image just below, which happens to be a full-scale, single-cell resolution model of the CA1 region of the hippocampus that “replicates the structure and architecture of the area, along with the position and relative connectivity of the neurons,” according to a statement from the Human Brain Project.
“We have performed a data mining operation on high resolution images of the human hippocampus, obtained from the BigBrain database. The position of individual neurons has been derived from a detailed analysis of these images,” said senior author Michele Migliore, PhD, of the Italian National Research Council’s Institute of Biophysics in Palermo.
Yes, he did say BigBrain database. BigBrain is – we checked and it’s definitely not this – a 3D model of a brain that was sectioned into 7,404 slices just 20 micrometers thick and then scanned by MRI. Digital reconstruction of those slices was done by supercomputer and the results are now available for analysis.
Dr. Migliore and his associates developed an image-processing algorithm to obtain neuronal positioning distribution and an algorithm to generate neuronal connectivity by approximating the shapes of dendrites and axons. (Our brains are starting to hurt just trying to write this.) “Some fit into narrow cones, others have a broad complex extension that can be approximated by dedicated geometrical volumes, and the connectivity to nearby neurons changes accordingly,” explained lead author Daniela Gandolfi of the University of Modena (Italy) and Reggio Emilia.
The investigators have made their dataset and the extraction methodology available on the EBRAINS platform and through the Human Brain Project and are moving on to other brain regions. And then, once everyone can find their way in and around the old gray matter, it should bring an end to conversations like this, which no doubt occur between male and female neuroscientists every day:
“Arnold, I think we’re lost.”
“Don’t worry, Bev, I know where I’m going.”
“Stop and ask this lady for directions.”
“I said I can find it.”
“Just ask her.”
“Fine. Excuse me, ma’am, can you tell us how to get to the corpora quadrigemina from here?
Getting sweet on sweat
Are you the sort of person who struggles in social situations? Have the past 3 years been a secret respite from the terror and exhaustion of meeting new people? We understand your plight. People kind of suck. And you don’t have to look far to be reminded of it.
Unfortunately, on occasion we all have to interact with other human beings. If you suffer from social anxiety, this is not a fun thing to do. But new research indicates that there may be a way to alleviate the stress for those with social anxiety: armpits.
Specifically, sweat from the armpits of other people. Yes, this means a group of scientists gathered up some volunteers and collected their armpit sweat while the volunteers watched a variety of movies (horror, comedy, romance, etc.). Our condolences to the poor unpaid interns tasked with gathering the sweat.
Once they had their precious new medicine, the researchers took a group of women and administered a round of mindfulness therapy. Some of the participants then received the various sweats, while the rest were forced to smell only clean air. (The horror!) Lo and behold, the sweat groups had their anxiety scores reduced by about 40% after their therapy, compared with just 17% in the control group.
The researchers also found that the source of the sweat didn’t matter. Their study subjects responded the same to sweat excreted during a scary movie as they did to sweat from a comedy, a result that surprised the researchers. They suggested chemosignals in the sweat may affect the treatment response and advised further research. Which means more sweat collection! They plan on testing emotionally neutral movies next time, and if we can make a humble suggestion, they also should try the sweatiest movies.
Before the Food and Drug Administration can approve armpit sweat as a treatment for social anxiety, we have some advice for those shut-in introverts out there. Next time you have to interact with rabid extroverts, instead of shaking their hands, walk up to them and take a deep whiff of their armpits. Establish dominance. Someone will feel awkward, and science has proved it won’t be you.
The puff that vaccinates
Ever been shot with a Nerf gun or hit with a foam pool tube? More annoying than painful, right? If we asked if you’d rather get pelted with one of those than receive a traditional vaccine injection, you would choose the former. Maybe someday you actually will.
During the boredom of the early pandemic lockdown, Jeremiah Gassensmith, PhD, of the department of chemistry and biochemistry at the University of Texas, Dallas, ordered a compressed gas–powered jet injection system to fool around with at home. Hey, who didn’t? Anyway, when it was time to go back to the lab he handed it over to one of his grad students, Yalini Wijesundara, and asked her to see what could be done with it.
In her tinkering she found that the jet injector could deliver metal-organic frameworks (MOFs) that can hold a bunch of different materials, like proteins and nucleic acids, through the skin.
Thus the “MOF-Jet” was born!
Jet injectors are nothing new, but they hurt. The MOF-Jet, however, is practically painless and cheaper than the gene guns that veterinarians use to inject biological cargo attached to the surface of a metal microparticle.
Changing the carrier gas also changes the time needed to break down the MOF and thus alters delivery of the drug inside. “If you shoot it with carbon dioxide, it will release its cargo faster within cells; if you use regular air, it will take 4 or 5 days,” Ms. Wijesundara explained in a written statement. That means the same drug could be released over different timescales without changing its formulation.
While testing on onion cells and mice, Ms. Wijesundara noted that it was as easy as “pointing and shooting” to distribute the puff of gas into the cells. A saving grace to those with needle anxiety. Not that we would know anything about needle anxiety.
More testing needs to be done before bringing this technology to human use, obviously, but we’re looking forward to saying goodbye to that dreaded prick and hello to a puff.
Your hippocampus is showing
Brain anatomy is one of the many, many things that’s not really our thing, but we do know a cool picture when we see one. Case in point: The image just below, which happens to be a full-scale, single-cell resolution model of the CA1 region of the hippocampus that “replicates the structure and architecture of the area, along with the position and relative connectivity of the neurons,” according to a statement from the Human Brain Project.
“We have performed a data mining operation on high resolution images of the human hippocampus, obtained from the BigBrain database. The position of individual neurons has been derived from a detailed analysis of these images,” said senior author Michele Migliore, PhD, of the Italian National Research Council’s Institute of Biophysics in Palermo.
Yes, he did say BigBrain database. BigBrain is – we checked and it’s definitely not this – a 3D model of a brain that was sectioned into 7,404 slices just 20 micrometers thick and then scanned by MRI. Digital reconstruction of those slices was done by supercomputer and the results are now available for analysis.
Dr. Migliore and his associates developed an image-processing algorithm to obtain neuronal positioning distribution and an algorithm to generate neuronal connectivity by approximating the shapes of dendrites and axons. (Our brains are starting to hurt just trying to write this.) “Some fit into narrow cones, others have a broad complex extension that can be approximated by dedicated geometrical volumes, and the connectivity to nearby neurons changes accordingly,” explained lead author Daniela Gandolfi of the University of Modena (Italy) and Reggio Emilia.
The investigators have made their dataset and the extraction methodology available on the EBRAINS platform and through the Human Brain Project and are moving on to other brain regions. And then, once everyone can find their way in and around the old gray matter, it should bring an end to conversations like this, which no doubt occur between male and female neuroscientists every day:
“Arnold, I think we’re lost.”
“Don’t worry, Bev, I know where I’m going.”
“Stop and ask this lady for directions.”
“I said I can find it.”
“Just ask her.”
“Fine. Excuse me, ma’am, can you tell us how to get to the corpora quadrigemina from here?
Getting sweet on sweat
Are you the sort of person who struggles in social situations? Have the past 3 years been a secret respite from the terror and exhaustion of meeting new people? We understand your plight. People kind of suck. And you don’t have to look far to be reminded of it.
Unfortunately, on occasion we all have to interact with other human beings. If you suffer from social anxiety, this is not a fun thing to do. But new research indicates that there may be a way to alleviate the stress for those with social anxiety: armpits.
Specifically, sweat from the armpits of other people. Yes, this means a group of scientists gathered up some volunteers and collected their armpit sweat while the volunteers watched a variety of movies (horror, comedy, romance, etc.). Our condolences to the poor unpaid interns tasked with gathering the sweat.
Once they had their precious new medicine, the researchers took a group of women and administered a round of mindfulness therapy. Some of the participants then received the various sweats, while the rest were forced to smell only clean air. (The horror!) Lo and behold, the sweat groups had their anxiety scores reduced by about 40% after their therapy, compared with just 17% in the control group.
The researchers also found that the source of the sweat didn’t matter. Their study subjects responded the same to sweat excreted during a scary movie as they did to sweat from a comedy, a result that surprised the researchers. They suggested chemosignals in the sweat may affect the treatment response and advised further research. Which means more sweat collection! They plan on testing emotionally neutral movies next time, and if we can make a humble suggestion, they also should try the sweatiest movies.
Before the Food and Drug Administration can approve armpit sweat as a treatment for social anxiety, we have some advice for those shut-in introverts out there. Next time you have to interact with rabid extroverts, instead of shaking their hands, walk up to them and take a deep whiff of their armpits. Establish dominance. Someone will feel awkward, and science has proved it won’t be you.
The puff that vaccinates
Ever been shot with a Nerf gun or hit with a foam pool tube? More annoying than painful, right? If we asked if you’d rather get pelted with one of those than receive a traditional vaccine injection, you would choose the former. Maybe someday you actually will.
During the boredom of the early pandemic lockdown, Jeremiah Gassensmith, PhD, of the department of chemistry and biochemistry at the University of Texas, Dallas, ordered a compressed gas–powered jet injection system to fool around with at home. Hey, who didn’t? Anyway, when it was time to go back to the lab he handed it over to one of his grad students, Yalini Wijesundara, and asked her to see what could be done with it.
In her tinkering she found that the jet injector could deliver metal-organic frameworks (MOFs) that can hold a bunch of different materials, like proteins and nucleic acids, through the skin.
Thus the “MOF-Jet” was born!
Jet injectors are nothing new, but they hurt. The MOF-Jet, however, is practically painless and cheaper than the gene guns that veterinarians use to inject biological cargo attached to the surface of a metal microparticle.
Changing the carrier gas also changes the time needed to break down the MOF and thus alters delivery of the drug inside. “If you shoot it with carbon dioxide, it will release its cargo faster within cells; if you use regular air, it will take 4 or 5 days,” Ms. Wijesundara explained in a written statement. That means the same drug could be released over different timescales without changing its formulation.
While testing on onion cells and mice, Ms. Wijesundara noted that it was as easy as “pointing and shooting” to distribute the puff of gas into the cells. A saving grace to those with needle anxiety. Not that we would know anything about needle anxiety.
More testing needs to be done before bringing this technology to human use, obviously, but we’re looking forward to saying goodbye to that dreaded prick and hello to a puff.
Your hippocampus is showing
Brain anatomy is one of the many, many things that’s not really our thing, but we do know a cool picture when we see one. Case in point: The image just below, which happens to be a full-scale, single-cell resolution model of the CA1 region of the hippocampus that “replicates the structure and architecture of the area, along with the position and relative connectivity of the neurons,” according to a statement from the Human Brain Project.
“We have performed a data mining operation on high resolution images of the human hippocampus, obtained from the BigBrain database. The position of individual neurons has been derived from a detailed analysis of these images,” said senior author Michele Migliore, PhD, of the Italian National Research Council’s Institute of Biophysics in Palermo.
Yes, he did say BigBrain database. BigBrain is – we checked and it’s definitely not this – a 3D model of a brain that was sectioned into 7,404 slices just 20 micrometers thick and then scanned by MRI. Digital reconstruction of those slices was done by supercomputer and the results are now available for analysis.
Dr. Migliore and his associates developed an image-processing algorithm to obtain neuronal positioning distribution and an algorithm to generate neuronal connectivity by approximating the shapes of dendrites and axons. (Our brains are starting to hurt just trying to write this.) “Some fit into narrow cones, others have a broad complex extension that can be approximated by dedicated geometrical volumes, and the connectivity to nearby neurons changes accordingly,” explained lead author Daniela Gandolfi of the University of Modena (Italy) and Reggio Emilia.
The investigators have made their dataset and the extraction methodology available on the EBRAINS platform and through the Human Brain Project and are moving on to other brain regions. And then, once everyone can find their way in and around the old gray matter, it should bring an end to conversations like this, which no doubt occur between male and female neuroscientists every day:
“Arnold, I think we’re lost.”
“Don’t worry, Bev, I know where I’m going.”
“Stop and ask this lady for directions.”
“I said I can find it.”
“Just ask her.”
“Fine. Excuse me, ma’am, can you tell us how to get to the corpora quadrigemina from here?
Dupilumab moves forward as possible COPD treatment
of more than 900 adults with uncontrolled chronic obstructive pulmonary disease.
In the study, known as the BOREAS trial, dupilumab met its primary and secondary endpoints, with a significant reduction compared with placebo in exacerbations for adults with chronic obstructive pulmonary disease (COPD) that was uncontrolled despite use of the maximal standard-of-care inhaled therapy (triple therapy), according to a press release from manufacturers Regeneron and Sanofi.
Dupilumab, which inhibits the signaling of the interleukin-4 (IL-4) and interleukin-13 (IL-13) pathways, is currently approved in multiple countries for certain patients with conditions including atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps, eosinophilic esophagitis, or prurigo nodularis in different age groups. The drug is not an immunosuppressant, and would be the first biologic approved for COPD, according to the manufacturers.
In the BOREAS trial, 468 adults with COPD who were current or former smokers aged 40-80 years were randomized to dupilumab and 471 to placebo; both groups continued to receive maximal standard of care.
Over 52 weeks, patients in the dupilumab group experienced a 30% reduction in moderate to severe COPD exacerbations compared with placebo (P = .0005).
In addition, patients treated with dupilumab met the key secondary endpoints of significant improvement in lung function from baseline to 12 weeks compared with placebo (160 mL vs. 77 mL, P < .0001); this difference persisted at 52 weeks (P = .0003).
Dupilumab also met endpoints for improvement in patient-reported health-related quality of life based on the St. George’s Respiratory Questionnaire (SGRQ) and reduction in the severity of respiratory symptoms of COPD based on the Evaluation Respiratory Symptoms: COPD (E-RS: COPD) Scale, according to the companies’ statement.
The results represent a previously unreported magnitude of improvement for COPD patients treated with a biologic, principal investigator George D. Yancopoulos, MD, said in the statement. “These results also validate the role type 2 inflammation plays in driving COPD in these patients, advancing the scientific community’s understanding of the underlying biology of this disease,” he added.
The safety results in the BOREAS trial were generally consistent with the known safety profile of Dupixent in its approved indications. Overall adverse event rates were similar for dupilumab and placebo patients (77% and 76%, respectively) and the overall safety profiles were consistent with the currently approved dupilumab indications, according to the manufacturers.
The adverse events that were more common in dupilumab patients compared with placebo patients were headache (8.1% vs. 6.8%), diarrhea (5.3% vs. 3.6%), and back pain (5.1% vs. 3.4%).
Adverse events leading to deaths were similar between the groups (1.7% in placebo patients and 1.5% in dupilumab patients).
Complete safety and efficacy results from the BOREAS trial are scheduled to be presented in a future scientific forum, and a second phase 3 trial of dupilumab for COPD, known as NOTUS, is ongoing, with data expected in 2024, according to the manufacturers.
The Boreas trial was sponsored by Sanofi and Regeneron Pharmaceuticals.
of more than 900 adults with uncontrolled chronic obstructive pulmonary disease.
In the study, known as the BOREAS trial, dupilumab met its primary and secondary endpoints, with a significant reduction compared with placebo in exacerbations for adults with chronic obstructive pulmonary disease (COPD) that was uncontrolled despite use of the maximal standard-of-care inhaled therapy (triple therapy), according to a press release from manufacturers Regeneron and Sanofi.
Dupilumab, which inhibits the signaling of the interleukin-4 (IL-4) and interleukin-13 (IL-13) pathways, is currently approved in multiple countries for certain patients with conditions including atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps, eosinophilic esophagitis, or prurigo nodularis in different age groups. The drug is not an immunosuppressant, and would be the first biologic approved for COPD, according to the manufacturers.
In the BOREAS trial, 468 adults with COPD who were current or former smokers aged 40-80 years were randomized to dupilumab and 471 to placebo; both groups continued to receive maximal standard of care.
Over 52 weeks, patients in the dupilumab group experienced a 30% reduction in moderate to severe COPD exacerbations compared with placebo (P = .0005).
In addition, patients treated with dupilumab met the key secondary endpoints of significant improvement in lung function from baseline to 12 weeks compared with placebo (160 mL vs. 77 mL, P < .0001); this difference persisted at 52 weeks (P = .0003).
Dupilumab also met endpoints for improvement in patient-reported health-related quality of life based on the St. George’s Respiratory Questionnaire (SGRQ) and reduction in the severity of respiratory symptoms of COPD based on the Evaluation Respiratory Symptoms: COPD (E-RS: COPD) Scale, according to the companies’ statement.
The results represent a previously unreported magnitude of improvement for COPD patients treated with a biologic, principal investigator George D. Yancopoulos, MD, said in the statement. “These results also validate the role type 2 inflammation plays in driving COPD in these patients, advancing the scientific community’s understanding of the underlying biology of this disease,” he added.
The safety results in the BOREAS trial were generally consistent with the known safety profile of Dupixent in its approved indications. Overall adverse event rates were similar for dupilumab and placebo patients (77% and 76%, respectively) and the overall safety profiles were consistent with the currently approved dupilumab indications, according to the manufacturers.
The adverse events that were more common in dupilumab patients compared with placebo patients were headache (8.1% vs. 6.8%), diarrhea (5.3% vs. 3.6%), and back pain (5.1% vs. 3.4%).
Adverse events leading to deaths were similar between the groups (1.7% in placebo patients and 1.5% in dupilumab patients).
Complete safety and efficacy results from the BOREAS trial are scheduled to be presented in a future scientific forum, and a second phase 3 trial of dupilumab for COPD, known as NOTUS, is ongoing, with data expected in 2024, according to the manufacturers.
The Boreas trial was sponsored by Sanofi and Regeneron Pharmaceuticals.
of more than 900 adults with uncontrolled chronic obstructive pulmonary disease.
In the study, known as the BOREAS trial, dupilumab met its primary and secondary endpoints, with a significant reduction compared with placebo in exacerbations for adults with chronic obstructive pulmonary disease (COPD) that was uncontrolled despite use of the maximal standard-of-care inhaled therapy (triple therapy), according to a press release from manufacturers Regeneron and Sanofi.
Dupilumab, which inhibits the signaling of the interleukin-4 (IL-4) and interleukin-13 (IL-13) pathways, is currently approved in multiple countries for certain patients with conditions including atopic dermatitis, asthma, chronic rhinosinusitis with nasal polyps, eosinophilic esophagitis, or prurigo nodularis in different age groups. The drug is not an immunosuppressant, and would be the first biologic approved for COPD, according to the manufacturers.
In the BOREAS trial, 468 adults with COPD who were current or former smokers aged 40-80 years were randomized to dupilumab and 471 to placebo; both groups continued to receive maximal standard of care.
Over 52 weeks, patients in the dupilumab group experienced a 30% reduction in moderate to severe COPD exacerbations compared with placebo (P = .0005).
In addition, patients treated with dupilumab met the key secondary endpoints of significant improvement in lung function from baseline to 12 weeks compared with placebo (160 mL vs. 77 mL, P < .0001); this difference persisted at 52 weeks (P = .0003).
Dupilumab also met endpoints for improvement in patient-reported health-related quality of life based on the St. George’s Respiratory Questionnaire (SGRQ) and reduction in the severity of respiratory symptoms of COPD based on the Evaluation Respiratory Symptoms: COPD (E-RS: COPD) Scale, according to the companies’ statement.
The results represent a previously unreported magnitude of improvement for COPD patients treated with a biologic, principal investigator George D. Yancopoulos, MD, said in the statement. “These results also validate the role type 2 inflammation plays in driving COPD in these patients, advancing the scientific community’s understanding of the underlying biology of this disease,” he added.
The safety results in the BOREAS trial were generally consistent with the known safety profile of Dupixent in its approved indications. Overall adverse event rates were similar for dupilumab and placebo patients (77% and 76%, respectively) and the overall safety profiles were consistent with the currently approved dupilumab indications, according to the manufacturers.
The adverse events that were more common in dupilumab patients compared with placebo patients were headache (8.1% vs. 6.8%), diarrhea (5.3% vs. 3.6%), and back pain (5.1% vs. 3.4%).
Adverse events leading to deaths were similar between the groups (1.7% in placebo patients and 1.5% in dupilumab patients).
Complete safety and efficacy results from the BOREAS trial are scheduled to be presented in a future scientific forum, and a second phase 3 trial of dupilumab for COPD, known as NOTUS, is ongoing, with data expected in 2024, according to the manufacturers.
The Boreas trial was sponsored by Sanofi and Regeneron Pharmaceuticals.