User login
Living the introvert’s dream: Alone for 500 days, but never lonely
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
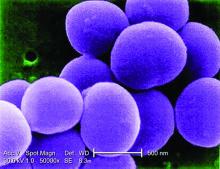
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Beating the allegory of the cave
When Beatriz Flamini spoke with reporters on April 14, she knew nothing of the previous 18 months. The Russian invasion of Ukraine? Nope. The death of Queen Elizabeth? Also no. But before you make fun of her, she has an excuse. She’s been living under a rock.
As part of an experiment to test how social isolation and disorientation affect a person’s mind, sense of time, and sleeping patterns, Ms. Flamini lived in a 70-meter-deep cave in southern Spain for 500 days, starting in November 2021. Alone. No outside communication with the outside world in any way, though she was constantly monitored by a team of researchers. She also had multiple cameras filming her for an upcoming documentary.
This is a massive step up from the previous record for time spent underground for science: A team of 15 spent 50 days underground in 2021 to similar study of isolation and how it affected circadian rhythms. It’s also almost certainly a world record for time spent underground.
All that time alone certainly sounds like some sort of medieval torture, but Ms. Flamini had access to food, water, and a library of books. Which she made liberal use of, reading at least 60 books during her stay. She also had a panic button in case the isolation became too much or an emergency developed, but she never considered using it.
She lost track of time after 2 months, flies invaded the cave on occasion, and maintaining coherence was occasionally a struggle, but she kept things together very well. In fact, she didn’t even want to leave when her team came for her. She wasn’t even finished with her 61st book.
When she spoke with gathered reporters after the ordeal, words were obviously difficult to come by for her, having not spoken in nearly 18 months, but her mind was clearly still sharp and she had a very important question for everyone gathered around her.
Who’s buying the beer?
We approve of this request.
Staphylococcus and the speed of evolution
Bacteria, we know, are tough little buggers that are hard to see and even harder to get rid of. So hard, actually, that human bodies eventually gave up on the task and decided to just incorporate them into our organ systems. But why are bacteria so hard to eliminate?
Two words: rapid evolution. How rapid? For the first time, scientists have directly observed adaptive evolution by Staphylococcus aureus in a single person’s skin microbiome. That’s how rapid.
For their study, the researchers collected samples from the nostrils, backs of knees, insides of elbows, and forearms of 23 children with eczema. They eventually cultured almost 1,500 unique colonies of S. aureus cells from those samples and sequenced the cells’ genomes.
All that sampling and culturing and sequencing showed that it was rare for a new S. aureus strain to come in and replace the existing strain. “Despite the stability at the lineage level, we see a lot of dynamics at the whole genome level, where new mutations are constantly arising in these bacteria and then spreading throughout the entire body,” Tami D. Lieberman, PhD, of the Massachusetts Institute of Technology, Cambridge, said in a written statement from MIT.
One frequent mutation involved a gene called capD, which encodes an enzyme necessary for synthesizing the capsular polysaccharide – a coating that protects S. aureus from recognition by immune cells. In one patient, four different mutations of capD arose independently in different samples before one variant became dominant and spread over the entire microbiome, MIT reported.
The mutation, which actually results in the loss of the polysaccharide capsule, may allow cells to grow faster than those without the mutation because they have more fuel to power their own growth, the researchers suggested. It’s also possible that loss of the capsule allows S. aureus cells to stick to the skin better because proteins that allow them to adhere to the skin are more exposed.
Dr. Lieberman and her associates hope that these variant-containing cells could be a new target for eczema treatments, but we’re never optimistic when it comes to bacteria. That’s because some of us are old enough to remember evolutionary biologist Stephen Jay Gould, who wrote in his book “Full House”: “Our planet has always been in the ‘Age of Bacteria,’ ever since the first fossils – bacteria, of course – were entombed in rocks more than 3 billion years ago. On any possible, reasonable or fair criterion, bacteria are – and always have been – the dominant forms of life on Earth.”
In the distant future, long after humans have left the scene, the bacteria will be laughing at the last rats and cockroaches scurrying across the landscape. Wanna bet?
The height of genetic prediction
Genetics are practically a DNA Scrabble bag. Traits like eye color and hair texture are chosen in the same fashion, based on what gets pulled from our own genetic bag of letters, but what about height? Researchers may now have a way to predict adult height and make it more than just an educated guess.
How? By looking at the genes in our growth plates. The cartilage on the ends of our bones hardens as we age, eventually deciding an individual’s stature. In a recently published study, a research team looked at 600 million cartilage cells linked to maturation and cell growth in mice. Because everything starts with rodents.
After that search identified 145 genes linked to growth plate maturation and formation of the bones, they compared the mouse genes with data from genome-wide association studies (GWAS) of human height to look for hotspots where the height genes exist in human DNA.
The results showed which genes play a role in deciding height, and the GWAS data also suggested that genetic changes affecting cartilage cell maturation may strongly influence adult height, said the investigators, who hope that earlier interventions can improve outcomes in patients with conditions such as skeletal dysplasia.
So, yeah, you may want to be a little taller or shorter, but the outcome of that particular Scrabble game was determined when your parents, you know, dropped the letters in the bag.
Optimal time period for weight loss drugs: Debate continues
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
Forgotten but not gone: EVALI epidemic continues
Rashelle Bernal vaped and ended up in an induced coma for a week. She was one of almost 3,000 people who were hospitalized during 2019 and early 2020 with severe lung damage from vaping and became part of what is now known as the epidemic of e-cigarette, or vaping, product use–associated lung injury (EVALI).
For many, the EVALI epidemic is a distant, pre-COVID memory.
But the vaping-related injuries are still happening. And for Ms. Bernal, the aftermath is her reality. Her pulmonologist from that time described the harm from the vape ingredients as an oil spill in her lungs. Eventually, the toxins would probably clear. But she will likely wrestle with the injuries for a very long time.
More than 3 years later, she frequently finds herself in the emergency department.
“If I get sick, if there’s anything that irritates my lungs – it could be something as simple as pollen in the air – it will cause me to get like a bacterial infection or other issues, and I can’t breathe,” Ms. Ms. Bernal, now 30, said in a recent interview. “I get really winded, to the point where I’ll walk up the stairs and I feel like I just ran a mile.”
In 2019 and 2020, a media firestorm erupted as hospitals notified the public of outbreaks of vaping-related lung injuries. News headlines reported e-cigarettes were killing teens from Texas to the Bronx. Investigators at the U.S. Centers for Disease Control and Prevention tracked most of the cases to vitamin E acetate, an additive in illicit cannabis vaping products intended to promote the metabolism of tetrahydrocannabinol (THC). The agency stopped tracking EVALI in February 2020.
But 2 months later, in April 2020, the agency’s National Center for Health Statistics implemented a diagnostic code, U07.0, for health care professionals in the United States to diagnose EVALI for the first time. The code is also used for lung damage related to use of electronic cigarettes and “dabbing” – a method of inhaling cannabis. Damage could include inflammation of the lungs, pulmonary hemorrhage, and eosinophilic pneumonia.
The incidence of these diagnoses appears to have risen sharply since 2020. In the last three months of 2020, a total of 11,300 medical claims included the U07.0 code. That figure rose to 22,000 in 2021 and hit 31,600 in 2022, according to data compiled for and provided to Medscape by Komodo Health, a health care technology company that holds a database of more than 330 million U.S. patients from Medicare, Medicaid, and commercial insurers’ medical, pharmacy, and laboratory claims.
Harm from vaping, including EVALI, has continued.
said Usha Periyanayagam, MD, MPH, head of clinic product and real-world evidence for Komodo and a former emergency medicine physician.
Where it started
Devika Rao, MD, a pediatric pulmonology specialist at UT Southwestern Medical Center, Dallas, has cared for most of her EVALI patients in the hospital, with the most recent case in early 2023. But in January, for the first time, she saw an EVALI patient in an outpatient clinic. The person had not been admitted to the hospital – like most were pre-pandemic. And like most who were seen during the pandemic, this patient had milder symptoms, not requiring intubation or take-home oxygen.
In 2019 and the beginning of 2020, many EVALI patients who were eventually hospitalized first sought help at urgent care centers or with primary care doctors and were presumed to have pneumonia or gastroenteritis and sent home.
“But they got worse, and they would present to our emergency room; their chest X-rays and CT scans showed extensive lung disease,” Dr. Rao said, adding that the damage was striking among patients all under age 18. “They were short of breath. Their oxygen levels were low. They had diminished lung function. And they had a lot of GI issues like abdominal pain and weight loss from nausea and vomiting.”
“These overwhelming inflammatory reactions that we see with EVALI,” said Karen M. Wilson, MD, MPH, a pediatric hospitalist at the University of Rochester (N.Y.) Medical Center and a tobacco use researcher. “You might find some microvascular changes with normal inhaling of smoke or aerosol, but you’re not going to find macro changes like we see with the EVALI.”
In late 2019, images of the CT scans of patients with EVALI were published, grabbing the attention of Arun Kannappan, MD, an assistant professor of pulmonary sciences and critical care at the University of Colorado Anschutz School of Medicine, Aurora. Dr. Kannappan knew a patient with such severe lung damage could develop acute respiratory distress syndrome, which means a patient would be put on a ventilator because their inflamed lungs could not oxygenate blood.
“That confers within somewhere between 30% to 50% chance of dying; it made all of the pulmonary specialists really turn their heads to make sure that we keep a lookout for it,” said Dr. Kannappan.
CT scans of lungs proved to be a critical diagnostic tool for doctors. Most of the images from patients showed acute inflammation and diffuse lung damage. Ehab Ali, MD, a critical care and pulmonary disease medicine specialist in Louisville, Ky., said the damage was often spread across both lungs in many areas and appeared opaque and hazy, known as “ground glass.” COVID-19, meanwhile, appeared differently in lung scans, often with damage that was more isolated.
But many diseases carry a “ground glass” appearance, with many potential causes, like infections, cigarette smoke, or an autoimmune condition.
“Before you even talk to the patient, you can immediately put it in your mind that ‘I’m going to ask this patient if they vape,’ when I see the distribution of ground glass appearance,” Dr. Ali said.
Dr. Ali said other factors, like the age of the patient – about three-quarters of EVALI patients are under age 34, according to the CDC – would spur him to ask about vaping. But because so many patients were young, discerning vape usage wasn’t always easy.
“When you’re talking to teenagers, if you ask them upon admission, with the parents in the room, they’re going say ‘no,’ ” said Rachel Boykan, MD, a pediatric hospitalist at Stony Brook (N.Y.) Children’s. She added that her hospital is still seeing cases.
Dr. Rao said it often takes two to three people asking a patient about any vape usage before they confess.
Ms. Bernal, who was 27 at the time of her hospital admission for EVALI, said she bought vapes with THC at a retail shop in California. She’d been a traditional marijuana smoker, using the leaf product, but switched when someone told her it was healthier to vape THC than inhale smoke from burned marijuana leaves into her lungs. “I thought this was safe.”
Dr. Rao and her colleagues recently published a study of 41 teenage patients with EVALI who were seen at Children’s Medical Center Dallas between December 2018 and July 2021. All but one reported using e-cigarettes containing THC, and the CDC in its most recent report from February 2020 said about 80% of patients had used vapes containing THC.
The CDC also found that vitamin E acetate, an oily substance that allows THC to travel from the lungs to the brain quickly and an ingredient used in the food and cosmetics industries, was found in many of the lungs of EVALI patients, though not all.
The aftermath
The outcomes of the thousands of patients who had EVALI – and those who may still be developing it – are largely untracked.
Bonnie Halpern-Felsher, PhD, director at the Stanford (Calif.) Reach Lab that bears her name and a researcher on tobacco in youth, said she and many of her colleagues are frustrated that the CDC is not continuing to collect data on EVALI.
“I know a lot of colleagues who’ve said that they’re still seeing EVALI, but because of COVID-19 they stopped collecting the data. And that’s been very frustrating because it’s hard to say whether the kinds of lung issues you’re having are related to e-cigarettes, generally, or EVALI,” Dr. Halpern-Felsher said.
Researchers and doctors affiliated with the American Thoracic Society published a report with solutions on how to better track EVALI. They recommended that a national case registry and biorepository be created.
Doctors also worry that many cases were missed. Dr. Boykan said that while protocol dictated nurses and other clinicians ask about a history of vaping – a key part of EVALI diagnosis – many did not. Dr. Ali, the Louisville critical care physician, said EVALI symptoms of nausea, cough, and fever are associated with viral infections.
“I’m sure that some of these cases might be discharged from the emergency room as a virus,” Dr. Ali said. “Most of the time patients would get prescribed steroids for viral infections, which may help EVALI patients even though it’s never been studied.”
Dr. Rao also said the treatment regimen at Children’s MC Dallas, which included high doses of intravenous steroids, seemed to help. But the best management approach for treatment, or long-term follow up care, has not been studied.
The report in the Annals of the American Thoracic Society said prospective studies are showing that a significant portion of patients with EVALI experience prolonged respiratory issues and cognitive and mood impairment. Dr. Rao said a common thread for many of her EVALI patients has been significant stress in their lives with school or family, which led them to vape in an attempt to reduce stress.
That was certainly the case for Ms. Bernal before her hospital admission. She had recently moved across the country for her husband’s job, was trying to buy a house, and had spent months in a hotel with three children. She vaped to cope.
But she said her mental and cognitive health has worsened. Back in Louisville, she saw a neurologist, who told her that her brain had shrunk, she said. She hasn’t found a new neurologist in Portland, Ore., where her family moved a year after the EVALI episode.
But she often finds herself overwhelmed and overstimulated with tasks that she said she never had problems with before. She tears up while talking about the newfound limitations. She struggled to find a primary care physician who could medically manage her mental health and a counselor who can understand what she’s been through with EVALI.
But, “a lot of doctors aren’t educated in it, and they don’t know how to respond or they don’t know what to do,” Ms. Bernal said. “And that makes me feel like, I guess, what I had wasn’t important.”
Ms. Bernal does have a new pulmonologist and is going in for a round of pulmonary tests soon because she often finds herself unable to breathe while completing simple tasks. She is tired of rushing to the ER. She wants answers, or some kind of treatment to help her feel normal again.
“I feel like this is my fault,” Ms. Bernal said. “Had I not smoked, I would be fine, and that’s hard to live with. Every day. Telling yourself, ‘It’s your fault.’ It’s been how many years now? And I still haven’t found peace yet. I don’t know if ever will.”
A version of this article first appeared on Medscape.com.
Rashelle Bernal vaped and ended up in an induced coma for a week. She was one of almost 3,000 people who were hospitalized during 2019 and early 2020 with severe lung damage from vaping and became part of what is now known as the epidemic of e-cigarette, or vaping, product use–associated lung injury (EVALI).
For many, the EVALI epidemic is a distant, pre-COVID memory.
But the vaping-related injuries are still happening. And for Ms. Bernal, the aftermath is her reality. Her pulmonologist from that time described the harm from the vape ingredients as an oil spill in her lungs. Eventually, the toxins would probably clear. But she will likely wrestle with the injuries for a very long time.
More than 3 years later, she frequently finds herself in the emergency department.
“If I get sick, if there’s anything that irritates my lungs – it could be something as simple as pollen in the air – it will cause me to get like a bacterial infection or other issues, and I can’t breathe,” Ms. Ms. Bernal, now 30, said in a recent interview. “I get really winded, to the point where I’ll walk up the stairs and I feel like I just ran a mile.”
In 2019 and 2020, a media firestorm erupted as hospitals notified the public of outbreaks of vaping-related lung injuries. News headlines reported e-cigarettes were killing teens from Texas to the Bronx. Investigators at the U.S. Centers for Disease Control and Prevention tracked most of the cases to vitamin E acetate, an additive in illicit cannabis vaping products intended to promote the metabolism of tetrahydrocannabinol (THC). The agency stopped tracking EVALI in February 2020.
But 2 months later, in April 2020, the agency’s National Center for Health Statistics implemented a diagnostic code, U07.0, for health care professionals in the United States to diagnose EVALI for the first time. The code is also used for lung damage related to use of electronic cigarettes and “dabbing” – a method of inhaling cannabis. Damage could include inflammation of the lungs, pulmonary hemorrhage, and eosinophilic pneumonia.
The incidence of these diagnoses appears to have risen sharply since 2020. In the last three months of 2020, a total of 11,300 medical claims included the U07.0 code. That figure rose to 22,000 in 2021 and hit 31,600 in 2022, according to data compiled for and provided to Medscape by Komodo Health, a health care technology company that holds a database of more than 330 million U.S. patients from Medicare, Medicaid, and commercial insurers’ medical, pharmacy, and laboratory claims.
Harm from vaping, including EVALI, has continued.
said Usha Periyanayagam, MD, MPH, head of clinic product and real-world evidence for Komodo and a former emergency medicine physician.
Where it started
Devika Rao, MD, a pediatric pulmonology specialist at UT Southwestern Medical Center, Dallas, has cared for most of her EVALI patients in the hospital, with the most recent case in early 2023. But in January, for the first time, she saw an EVALI patient in an outpatient clinic. The person had not been admitted to the hospital – like most were pre-pandemic. And like most who were seen during the pandemic, this patient had milder symptoms, not requiring intubation or take-home oxygen.
In 2019 and the beginning of 2020, many EVALI patients who were eventually hospitalized first sought help at urgent care centers or with primary care doctors and were presumed to have pneumonia or gastroenteritis and sent home.
“But they got worse, and they would present to our emergency room; their chest X-rays and CT scans showed extensive lung disease,” Dr. Rao said, adding that the damage was striking among patients all under age 18. “They were short of breath. Their oxygen levels were low. They had diminished lung function. And they had a lot of GI issues like abdominal pain and weight loss from nausea and vomiting.”
“These overwhelming inflammatory reactions that we see with EVALI,” said Karen M. Wilson, MD, MPH, a pediatric hospitalist at the University of Rochester (N.Y.) Medical Center and a tobacco use researcher. “You might find some microvascular changes with normal inhaling of smoke or aerosol, but you’re not going to find macro changes like we see with the EVALI.”
In late 2019, images of the CT scans of patients with EVALI were published, grabbing the attention of Arun Kannappan, MD, an assistant professor of pulmonary sciences and critical care at the University of Colorado Anschutz School of Medicine, Aurora. Dr. Kannappan knew a patient with such severe lung damage could develop acute respiratory distress syndrome, which means a patient would be put on a ventilator because their inflamed lungs could not oxygenate blood.
“That confers within somewhere between 30% to 50% chance of dying; it made all of the pulmonary specialists really turn their heads to make sure that we keep a lookout for it,” said Dr. Kannappan.
CT scans of lungs proved to be a critical diagnostic tool for doctors. Most of the images from patients showed acute inflammation and diffuse lung damage. Ehab Ali, MD, a critical care and pulmonary disease medicine specialist in Louisville, Ky., said the damage was often spread across both lungs in many areas and appeared opaque and hazy, known as “ground glass.” COVID-19, meanwhile, appeared differently in lung scans, often with damage that was more isolated.
But many diseases carry a “ground glass” appearance, with many potential causes, like infections, cigarette smoke, or an autoimmune condition.
“Before you even talk to the patient, you can immediately put it in your mind that ‘I’m going to ask this patient if they vape,’ when I see the distribution of ground glass appearance,” Dr. Ali said.
Dr. Ali said other factors, like the age of the patient – about three-quarters of EVALI patients are under age 34, according to the CDC – would spur him to ask about vaping. But because so many patients were young, discerning vape usage wasn’t always easy.
“When you’re talking to teenagers, if you ask them upon admission, with the parents in the room, they’re going say ‘no,’ ” said Rachel Boykan, MD, a pediatric hospitalist at Stony Brook (N.Y.) Children’s. She added that her hospital is still seeing cases.
Dr. Rao said it often takes two to three people asking a patient about any vape usage before they confess.
Ms. Bernal, who was 27 at the time of her hospital admission for EVALI, said she bought vapes with THC at a retail shop in California. She’d been a traditional marijuana smoker, using the leaf product, but switched when someone told her it was healthier to vape THC than inhale smoke from burned marijuana leaves into her lungs. “I thought this was safe.”
Dr. Rao and her colleagues recently published a study of 41 teenage patients with EVALI who were seen at Children’s Medical Center Dallas between December 2018 and July 2021. All but one reported using e-cigarettes containing THC, and the CDC in its most recent report from February 2020 said about 80% of patients had used vapes containing THC.
The CDC also found that vitamin E acetate, an oily substance that allows THC to travel from the lungs to the brain quickly and an ingredient used in the food and cosmetics industries, was found in many of the lungs of EVALI patients, though not all.
The aftermath
The outcomes of the thousands of patients who had EVALI – and those who may still be developing it – are largely untracked.
Bonnie Halpern-Felsher, PhD, director at the Stanford (Calif.) Reach Lab that bears her name and a researcher on tobacco in youth, said she and many of her colleagues are frustrated that the CDC is not continuing to collect data on EVALI.
“I know a lot of colleagues who’ve said that they’re still seeing EVALI, but because of COVID-19 they stopped collecting the data. And that’s been very frustrating because it’s hard to say whether the kinds of lung issues you’re having are related to e-cigarettes, generally, or EVALI,” Dr. Halpern-Felsher said.
Researchers and doctors affiliated with the American Thoracic Society published a report with solutions on how to better track EVALI. They recommended that a national case registry and biorepository be created.
Doctors also worry that many cases were missed. Dr. Boykan said that while protocol dictated nurses and other clinicians ask about a history of vaping – a key part of EVALI diagnosis – many did not. Dr. Ali, the Louisville critical care physician, said EVALI symptoms of nausea, cough, and fever are associated with viral infections.
“I’m sure that some of these cases might be discharged from the emergency room as a virus,” Dr. Ali said. “Most of the time patients would get prescribed steroids for viral infections, which may help EVALI patients even though it’s never been studied.”
Dr. Rao also said the treatment regimen at Children’s MC Dallas, which included high doses of intravenous steroids, seemed to help. But the best management approach for treatment, or long-term follow up care, has not been studied.
The report in the Annals of the American Thoracic Society said prospective studies are showing that a significant portion of patients with EVALI experience prolonged respiratory issues and cognitive and mood impairment. Dr. Rao said a common thread for many of her EVALI patients has been significant stress in their lives with school or family, which led them to vape in an attempt to reduce stress.
That was certainly the case for Ms. Bernal before her hospital admission. She had recently moved across the country for her husband’s job, was trying to buy a house, and had spent months in a hotel with three children. She vaped to cope.
But she said her mental and cognitive health has worsened. Back in Louisville, she saw a neurologist, who told her that her brain had shrunk, she said. She hasn’t found a new neurologist in Portland, Ore., where her family moved a year after the EVALI episode.
But she often finds herself overwhelmed and overstimulated with tasks that she said she never had problems with before. She tears up while talking about the newfound limitations. She struggled to find a primary care physician who could medically manage her mental health and a counselor who can understand what she’s been through with EVALI.
But, “a lot of doctors aren’t educated in it, and they don’t know how to respond or they don’t know what to do,” Ms. Bernal said. “And that makes me feel like, I guess, what I had wasn’t important.”
Ms. Bernal does have a new pulmonologist and is going in for a round of pulmonary tests soon because she often finds herself unable to breathe while completing simple tasks. She is tired of rushing to the ER. She wants answers, or some kind of treatment to help her feel normal again.
“I feel like this is my fault,” Ms. Bernal said. “Had I not smoked, I would be fine, and that’s hard to live with. Every day. Telling yourself, ‘It’s your fault.’ It’s been how many years now? And I still haven’t found peace yet. I don’t know if ever will.”
A version of this article first appeared on Medscape.com.
Rashelle Bernal vaped and ended up in an induced coma for a week. She was one of almost 3,000 people who were hospitalized during 2019 and early 2020 with severe lung damage from vaping and became part of what is now known as the epidemic of e-cigarette, or vaping, product use–associated lung injury (EVALI).
For many, the EVALI epidemic is a distant, pre-COVID memory.
But the vaping-related injuries are still happening. And for Ms. Bernal, the aftermath is her reality. Her pulmonologist from that time described the harm from the vape ingredients as an oil spill in her lungs. Eventually, the toxins would probably clear. But she will likely wrestle with the injuries for a very long time.
More than 3 years later, she frequently finds herself in the emergency department.
“If I get sick, if there’s anything that irritates my lungs – it could be something as simple as pollen in the air – it will cause me to get like a bacterial infection or other issues, and I can’t breathe,” Ms. Ms. Bernal, now 30, said in a recent interview. “I get really winded, to the point where I’ll walk up the stairs and I feel like I just ran a mile.”
In 2019 and 2020, a media firestorm erupted as hospitals notified the public of outbreaks of vaping-related lung injuries. News headlines reported e-cigarettes were killing teens from Texas to the Bronx. Investigators at the U.S. Centers for Disease Control and Prevention tracked most of the cases to vitamin E acetate, an additive in illicit cannabis vaping products intended to promote the metabolism of tetrahydrocannabinol (THC). The agency stopped tracking EVALI in February 2020.
But 2 months later, in April 2020, the agency’s National Center for Health Statistics implemented a diagnostic code, U07.0, for health care professionals in the United States to diagnose EVALI for the first time. The code is also used for lung damage related to use of electronic cigarettes and “dabbing” – a method of inhaling cannabis. Damage could include inflammation of the lungs, pulmonary hemorrhage, and eosinophilic pneumonia.
The incidence of these diagnoses appears to have risen sharply since 2020. In the last three months of 2020, a total of 11,300 medical claims included the U07.0 code. That figure rose to 22,000 in 2021 and hit 31,600 in 2022, according to data compiled for and provided to Medscape by Komodo Health, a health care technology company that holds a database of more than 330 million U.S. patients from Medicare, Medicaid, and commercial insurers’ medical, pharmacy, and laboratory claims.
Harm from vaping, including EVALI, has continued.
said Usha Periyanayagam, MD, MPH, head of clinic product and real-world evidence for Komodo and a former emergency medicine physician.
Where it started
Devika Rao, MD, a pediatric pulmonology specialist at UT Southwestern Medical Center, Dallas, has cared for most of her EVALI patients in the hospital, with the most recent case in early 2023. But in January, for the first time, she saw an EVALI patient in an outpatient clinic. The person had not been admitted to the hospital – like most were pre-pandemic. And like most who were seen during the pandemic, this patient had milder symptoms, not requiring intubation or take-home oxygen.
In 2019 and the beginning of 2020, many EVALI patients who were eventually hospitalized first sought help at urgent care centers or with primary care doctors and were presumed to have pneumonia or gastroenteritis and sent home.
“But they got worse, and they would present to our emergency room; their chest X-rays and CT scans showed extensive lung disease,” Dr. Rao said, adding that the damage was striking among patients all under age 18. “They were short of breath. Their oxygen levels were low. They had diminished lung function. And they had a lot of GI issues like abdominal pain and weight loss from nausea and vomiting.”
“These overwhelming inflammatory reactions that we see with EVALI,” said Karen M. Wilson, MD, MPH, a pediatric hospitalist at the University of Rochester (N.Y.) Medical Center and a tobacco use researcher. “You might find some microvascular changes with normal inhaling of smoke or aerosol, but you’re not going to find macro changes like we see with the EVALI.”
In late 2019, images of the CT scans of patients with EVALI were published, grabbing the attention of Arun Kannappan, MD, an assistant professor of pulmonary sciences and critical care at the University of Colorado Anschutz School of Medicine, Aurora. Dr. Kannappan knew a patient with such severe lung damage could develop acute respiratory distress syndrome, which means a patient would be put on a ventilator because their inflamed lungs could not oxygenate blood.
“That confers within somewhere between 30% to 50% chance of dying; it made all of the pulmonary specialists really turn their heads to make sure that we keep a lookout for it,” said Dr. Kannappan.
CT scans of lungs proved to be a critical diagnostic tool for doctors. Most of the images from patients showed acute inflammation and diffuse lung damage. Ehab Ali, MD, a critical care and pulmonary disease medicine specialist in Louisville, Ky., said the damage was often spread across both lungs in many areas and appeared opaque and hazy, known as “ground glass.” COVID-19, meanwhile, appeared differently in lung scans, often with damage that was more isolated.
But many diseases carry a “ground glass” appearance, with many potential causes, like infections, cigarette smoke, or an autoimmune condition.
“Before you even talk to the patient, you can immediately put it in your mind that ‘I’m going to ask this patient if they vape,’ when I see the distribution of ground glass appearance,” Dr. Ali said.
Dr. Ali said other factors, like the age of the patient – about three-quarters of EVALI patients are under age 34, according to the CDC – would spur him to ask about vaping. But because so many patients were young, discerning vape usage wasn’t always easy.
“When you’re talking to teenagers, if you ask them upon admission, with the parents in the room, they’re going say ‘no,’ ” said Rachel Boykan, MD, a pediatric hospitalist at Stony Brook (N.Y.) Children’s. She added that her hospital is still seeing cases.
Dr. Rao said it often takes two to three people asking a patient about any vape usage before they confess.
Ms. Bernal, who was 27 at the time of her hospital admission for EVALI, said she bought vapes with THC at a retail shop in California. She’d been a traditional marijuana smoker, using the leaf product, but switched when someone told her it was healthier to vape THC than inhale smoke from burned marijuana leaves into her lungs. “I thought this was safe.”
Dr. Rao and her colleagues recently published a study of 41 teenage patients with EVALI who were seen at Children’s Medical Center Dallas between December 2018 and July 2021. All but one reported using e-cigarettes containing THC, and the CDC in its most recent report from February 2020 said about 80% of patients had used vapes containing THC.
The CDC also found that vitamin E acetate, an oily substance that allows THC to travel from the lungs to the brain quickly and an ingredient used in the food and cosmetics industries, was found in many of the lungs of EVALI patients, though not all.
The aftermath
The outcomes of the thousands of patients who had EVALI – and those who may still be developing it – are largely untracked.
Bonnie Halpern-Felsher, PhD, director at the Stanford (Calif.) Reach Lab that bears her name and a researcher on tobacco in youth, said she and many of her colleagues are frustrated that the CDC is not continuing to collect data on EVALI.
“I know a lot of colleagues who’ve said that they’re still seeing EVALI, but because of COVID-19 they stopped collecting the data. And that’s been very frustrating because it’s hard to say whether the kinds of lung issues you’re having are related to e-cigarettes, generally, or EVALI,” Dr. Halpern-Felsher said.
Researchers and doctors affiliated with the American Thoracic Society published a report with solutions on how to better track EVALI. They recommended that a national case registry and biorepository be created.
Doctors also worry that many cases were missed. Dr. Boykan said that while protocol dictated nurses and other clinicians ask about a history of vaping – a key part of EVALI diagnosis – many did not. Dr. Ali, the Louisville critical care physician, said EVALI symptoms of nausea, cough, and fever are associated with viral infections.
“I’m sure that some of these cases might be discharged from the emergency room as a virus,” Dr. Ali said. “Most of the time patients would get prescribed steroids for viral infections, which may help EVALI patients even though it’s never been studied.”
Dr. Rao also said the treatment regimen at Children’s MC Dallas, which included high doses of intravenous steroids, seemed to help. But the best management approach for treatment, or long-term follow up care, has not been studied.
The report in the Annals of the American Thoracic Society said prospective studies are showing that a significant portion of patients with EVALI experience prolonged respiratory issues and cognitive and mood impairment. Dr. Rao said a common thread for many of her EVALI patients has been significant stress in their lives with school or family, which led them to vape in an attempt to reduce stress.
That was certainly the case for Ms. Bernal before her hospital admission. She had recently moved across the country for her husband’s job, was trying to buy a house, and had spent months in a hotel with three children. She vaped to cope.
But she said her mental and cognitive health has worsened. Back in Louisville, she saw a neurologist, who told her that her brain had shrunk, she said. She hasn’t found a new neurologist in Portland, Ore., where her family moved a year after the EVALI episode.
But she often finds herself overwhelmed and overstimulated with tasks that she said she never had problems with before. She tears up while talking about the newfound limitations. She struggled to find a primary care physician who could medically manage her mental health and a counselor who can understand what she’s been through with EVALI.
But, “a lot of doctors aren’t educated in it, and they don’t know how to respond or they don’t know what to do,” Ms. Bernal said. “And that makes me feel like, I guess, what I had wasn’t important.”
Ms. Bernal does have a new pulmonologist and is going in for a round of pulmonary tests soon because she often finds herself unable to breathe while completing simple tasks. She is tired of rushing to the ER. She wants answers, or some kind of treatment to help her feel normal again.
“I feel like this is my fault,” Ms. Bernal said. “Had I not smoked, I would be fine, and that’s hard to live with. Every day. Telling yourself, ‘It’s your fault.’ It’s been how many years now? And I still haven’t found peace yet. I don’t know if ever will.”
A version of this article first appeared on Medscape.com.
Suicidal thoughts decline in endocrinologists: Survey
Rates of suicidal thoughts and attempted suicide among endocrinologists declined from 2022 and now rank similar to the average rate among physicians overall, but these rates are still higher than the general public, according to survey findings.
The current report about suicide among endocrinologists, titled, “Doctors’ Burden: Endocrinologist Suicide Report 2023,” was recently published.
A report about suicide among physicians overall, based on the same survey, titled, “Doctors’ Burden: Medscape Physician Suicide Report 2023,” was published previously.
Improved rates among 28 medical specialties
In the 2022 survey of a representative national sample of 13,069 U.S. physicians, 10% of endocrinologists reported having suicidal thoughts, ranking the specialty sixth among 29 medical specialties that year.
The 2023 survey found that in a representative national sample of 9,175 U.S. physicians, 8% of endocrinologists reported having suicidal thoughts, roughly the average rate among clinicians overall, ranking it 20th among 29 medical specialties.
The highest rates of thoughts of suicide in the latest survey were reported by physicians in otolaryngology (13%), followed by physicians in psychiatry, family medicine, anesthesiology, obstetrics/gynecology, and emergency medicine (roughly 12% in each specialty).
The rate of attempted suicide was 1% among endocrinologists, which was also the rate among physicians overall.
More female than male endocrinologists reported contemplating suicide (8% versus 5%). In addition, 1% of male endocrinologists reported that they had attempted suicide and 2% of female endocrinologists replied they preferred not to answer the question about attempted suicide.
In contrast, in 2020, an estimated 4.9% of U.S. adults aged 18 and older had serious thoughts about suicide and 0.5% attempted suicide, according to the National Institutes of Health website, the latest report states.
Rates of suicidal thoughts and suicide attempts among physicians overall “are worryingly high numbers,” Peter Yellowlees, MBBS, MD, emeritus professor of psychiatry at University of California, Davis, Health, and chief executive officer, Asynchealth, said in the report.
Confiding in others, good mental health habits, resources
In the 2023 survey, half of the endocrinologists who had thought about suicide had confided in a therapist and 41% had spoken to a family member, but none had told a colleague or a friend, or phoned a suicide hotline.
On the other hand, 7% of male and 10% of female endocrinologists, and 9% of male and 11% of female physicians overall, reported that a colleague had shared suicidal thoughts with them.
“It’s pleasing that physicians overall have shown themselves slightly more likely to bring ideas about suicide to a therapist and less likely to keep their distress entirely to themselves,” Dr. Yellowlees said.
“It’s possible that the need for health care is becoming less stigmatized nationally, with large and increasing emphasis on physician well-being during and after the COVID-19 pandemic,” he suggested.
Endocrinologists reported that to keep happy and have good mental health, they engaged in activities and hobbies (70%), exercised (66%), spent time with family and friends (63%), got enough sleep (56%), ate healthy (48%), went to therapy (11%), or did other things (8%), which was similar to that reported by physicians overall.
The report lists several resources that are specific for physicians having suicidal thoughts (Physician Support Line, 988 Suicide and Crisis Lifeline, Peer RxMed, International Association for Suicide Prevention, and the American Foundation for Suicide Prevention) along with contact information.
The 2023 survey was conducted from June 28, 2022, to Oct. 3, 2022, and the 2022 survey was conducted from June 29, 2021, to Sept. 26, 2021.
A version of this article first appeared on Medscape.com.
Rates of suicidal thoughts and attempted suicide among endocrinologists declined from 2022 and now rank similar to the average rate among physicians overall, but these rates are still higher than the general public, according to survey findings.
The current report about suicide among endocrinologists, titled, “Doctors’ Burden: Endocrinologist Suicide Report 2023,” was recently published.
A report about suicide among physicians overall, based on the same survey, titled, “Doctors’ Burden: Medscape Physician Suicide Report 2023,” was published previously.
Improved rates among 28 medical specialties
In the 2022 survey of a representative national sample of 13,069 U.S. physicians, 10% of endocrinologists reported having suicidal thoughts, ranking the specialty sixth among 29 medical specialties that year.
The 2023 survey found that in a representative national sample of 9,175 U.S. physicians, 8% of endocrinologists reported having suicidal thoughts, roughly the average rate among clinicians overall, ranking it 20th among 29 medical specialties.
The highest rates of thoughts of suicide in the latest survey were reported by physicians in otolaryngology (13%), followed by physicians in psychiatry, family medicine, anesthesiology, obstetrics/gynecology, and emergency medicine (roughly 12% in each specialty).
The rate of attempted suicide was 1% among endocrinologists, which was also the rate among physicians overall.
More female than male endocrinologists reported contemplating suicide (8% versus 5%). In addition, 1% of male endocrinologists reported that they had attempted suicide and 2% of female endocrinologists replied they preferred not to answer the question about attempted suicide.
In contrast, in 2020, an estimated 4.9% of U.S. adults aged 18 and older had serious thoughts about suicide and 0.5% attempted suicide, according to the National Institutes of Health website, the latest report states.
Rates of suicidal thoughts and suicide attempts among physicians overall “are worryingly high numbers,” Peter Yellowlees, MBBS, MD, emeritus professor of psychiatry at University of California, Davis, Health, and chief executive officer, Asynchealth, said in the report.
Confiding in others, good mental health habits, resources
In the 2023 survey, half of the endocrinologists who had thought about suicide had confided in a therapist and 41% had spoken to a family member, but none had told a colleague or a friend, or phoned a suicide hotline.
On the other hand, 7% of male and 10% of female endocrinologists, and 9% of male and 11% of female physicians overall, reported that a colleague had shared suicidal thoughts with them.
“It’s pleasing that physicians overall have shown themselves slightly more likely to bring ideas about suicide to a therapist and less likely to keep their distress entirely to themselves,” Dr. Yellowlees said.
“It’s possible that the need for health care is becoming less stigmatized nationally, with large and increasing emphasis on physician well-being during and after the COVID-19 pandemic,” he suggested.
Endocrinologists reported that to keep happy and have good mental health, they engaged in activities and hobbies (70%), exercised (66%), spent time with family and friends (63%), got enough sleep (56%), ate healthy (48%), went to therapy (11%), or did other things (8%), which was similar to that reported by physicians overall.
The report lists several resources that are specific for physicians having suicidal thoughts (Physician Support Line, 988 Suicide and Crisis Lifeline, Peer RxMed, International Association for Suicide Prevention, and the American Foundation for Suicide Prevention) along with contact information.
The 2023 survey was conducted from June 28, 2022, to Oct. 3, 2022, and the 2022 survey was conducted from June 29, 2021, to Sept. 26, 2021.
A version of this article first appeared on Medscape.com.
Rates of suicidal thoughts and attempted suicide among endocrinologists declined from 2022 and now rank similar to the average rate among physicians overall, but these rates are still higher than the general public, according to survey findings.
The current report about suicide among endocrinologists, titled, “Doctors’ Burden: Endocrinologist Suicide Report 2023,” was recently published.
A report about suicide among physicians overall, based on the same survey, titled, “Doctors’ Burden: Medscape Physician Suicide Report 2023,” was published previously.
Improved rates among 28 medical specialties
In the 2022 survey of a representative national sample of 13,069 U.S. physicians, 10% of endocrinologists reported having suicidal thoughts, ranking the specialty sixth among 29 medical specialties that year.
The 2023 survey found that in a representative national sample of 9,175 U.S. physicians, 8% of endocrinologists reported having suicidal thoughts, roughly the average rate among clinicians overall, ranking it 20th among 29 medical specialties.
The highest rates of thoughts of suicide in the latest survey were reported by physicians in otolaryngology (13%), followed by physicians in psychiatry, family medicine, anesthesiology, obstetrics/gynecology, and emergency medicine (roughly 12% in each specialty).
The rate of attempted suicide was 1% among endocrinologists, which was also the rate among physicians overall.
More female than male endocrinologists reported contemplating suicide (8% versus 5%). In addition, 1% of male endocrinologists reported that they had attempted suicide and 2% of female endocrinologists replied they preferred not to answer the question about attempted suicide.
In contrast, in 2020, an estimated 4.9% of U.S. adults aged 18 and older had serious thoughts about suicide and 0.5% attempted suicide, according to the National Institutes of Health website, the latest report states.
Rates of suicidal thoughts and suicide attempts among physicians overall “are worryingly high numbers,” Peter Yellowlees, MBBS, MD, emeritus professor of psychiatry at University of California, Davis, Health, and chief executive officer, Asynchealth, said in the report.
Confiding in others, good mental health habits, resources
In the 2023 survey, half of the endocrinologists who had thought about suicide had confided in a therapist and 41% had spoken to a family member, but none had told a colleague or a friend, or phoned a suicide hotline.
On the other hand, 7% of male and 10% of female endocrinologists, and 9% of male and 11% of female physicians overall, reported that a colleague had shared suicidal thoughts with them.
“It’s pleasing that physicians overall have shown themselves slightly more likely to bring ideas about suicide to a therapist and less likely to keep their distress entirely to themselves,” Dr. Yellowlees said.
“It’s possible that the need for health care is becoming less stigmatized nationally, with large and increasing emphasis on physician well-being during and after the COVID-19 pandemic,” he suggested.
Endocrinologists reported that to keep happy and have good mental health, they engaged in activities and hobbies (70%), exercised (66%), spent time with family and friends (63%), got enough sleep (56%), ate healthy (48%), went to therapy (11%), or did other things (8%), which was similar to that reported by physicians overall.
The report lists several resources that are specific for physicians having suicidal thoughts (Physician Support Line, 988 Suicide and Crisis Lifeline, Peer RxMed, International Association for Suicide Prevention, and the American Foundation for Suicide Prevention) along with contact information.
The 2023 survey was conducted from June 28, 2022, to Oct. 3, 2022, and the 2022 survey was conducted from June 29, 2021, to Sept. 26, 2021.
A version of this article first appeared on Medscape.com.
As COVID tracking wanes, are we letting our guard down too soon?
The 30-second commercial, part of the government’s We Can Do This campaign, shows everyday people going about their lives, then reminds them that, “because COVID is still out there and so are you,” it might be time to update your vaccine.
Many data tracking sources, both federal and others, are no longer reporting, as often, the number of COVID cases, hospitalizations, and deaths.
The Department of Health & Human Services in February stopped updating its public COVID data site, instead directing all queries to the Centers for Disease Control and Prevention, which itself has been updating only weekly instead of daily since 2022.
Nongovernmental sources, such as John Hopkins University, stopped reporting pandemic data in March, The New York Times also ended its COVID data-gathering project in March, stating that “the comprehensive real-time reporting that The Times has prioritized is no longer possible.” It will rely on reporting weekly CDC data moving forward.
Along with the tracking sites, masking and social distancing mandates have mostly disappeared. President Joe Biden signed a bipartisan bill on April 10 that ended the national emergency for COVID. While some programs will stay in place for now, such as free vaccines, treatments, and tests, that too will go away when the federal public health emergency expires on May 11. The HHS already has issued its transition roadmap.
Many Americans, meanwhile, are still on the fence about the pandemic. A Gallup poll from March shows that about half of the American public say it’s over, and about half disagree.
Are we closing up shop on COVID-19 too soon, or is it time? Not surprisingly, experts don’t agree. Some say the pandemic is now endemic – which broadly means the virus and its patterns are predictable and steady in designated regions – and that it’s critical to catch up on health needs neglected during the pandemic, such as screenings and other vaccinations
But others don’t think it’s reached that stage yet, saying that we are letting our guard down too soon and we can’t be blind to the possibility of another strong variant – or pandemic – emerging. Surveillance must continue, not decline, and be improved.
Time to move on?
In its transition roadmap released in February, the HHS notes that daily COVID reported cases are down over 90%, compared with the peak of the Omicron surge at the end of January 2022; deaths have declined by over 80%; and new hospitalizations caused by COVID have dropped by nearly 80%.
It is time to move on, said Ali Mokdad, PhD, a professor and chief strategy officer of population health at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle.
“Many people were delaying a lot of medical care, because they were afraid” during COVID’s height, he said, explaining that elective surgeries were postponed, prenatal care went down, as did screenings for blood pressure and diabetes.
His institute was tracking COVID projections every week but stopped in December.
As for emerging variants, “we haven’t seen a variant that scares us since Omicron” in November 2021, said Dr. Mokdad, who agrees that COVID is endemic now. The subvariants that followed it are very similar, and the current vaccines are working.
“We can move on, but we cannot drop the ball on keeping an eye on the genetic sequencing of the virus,” he said. That will enable quick identification of new variants.
If a worrisome new variant does surface, Dr. Mokdad said, certain locations and resources will be able to gear up quickly, while others won’t be as fast, but overall the United States is in a much better position now.
Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, also believes the pandemic phase is behind us
“This can’t be an emergency in perpetuity,” he said “Just because something is not a pandemic [anymore] does not mean that all activities related to it cease.”
COVID is highly unlikely to overwhelm hospitals again, and that was the main reason for the emergency declaration, he said.
“It’s not all or none – collapsing COVID-related [monitoring] activities into the routine monitoring that is done for other infectious disease should be seen as an achievement in taming the virus,” he said.
Not endemic yet
Closing up shop too early could mean we are blindsided, said Rajendram Rajnarayanan, PhD, an assistant dean of research and associate professor at the New York Institute of Technology College of Osteopathic Medicine at Arkansas State University in Jonesboro.
Already, he said, large labs have closed or scaled down as testing demand has declined, and many centers that offered community testing have also closed. Plus, home test results are often not reported.
Continued monitoring is key, he said. “You have to maintain a base level of sequencing for new variants,” he said. “Right now, the variant that is ‘top dog’ in the world is XBB.1.16.”
That’s an Omicron subvariant that the World Health Organization is currently keeping its eye on, according to a media briefing on March 29. There are about 800 sequences of it from 22 countries, mostly India, and it’s been in circulation a few months.
Dr. Rajnarayanan said he’s not overly worried about this variant, but surveillance must continue. His own breakdown of XBB.1.16 found the subvariant in 27 countries, including the United States, as of April 10.
Ideally, Dr. Rajnarayanan would suggest four areas to keep focusing on, moving forward:
- Active, random surveillance for new variants, especially in hot spots.
- Hospital surveillance and surveillance of long-term care, especially in congregate settings where people can more easily spread the virus.
- Travelers’ surveillance, now at , according to the CDC.
- Surveillance of animals such as mink and deer, because these animals can not only pick up the virus, but the virus can mutate in the animals, which could then transmit it back to people.
With less testing, baseline surveillance for new variants has declined. The other three surveillance areas need improvement, too, he said, as the reporting is often delayed.
Continued surveillance is crucial, agreed Katelyn Jetelina, PhD, an epidemiologist and data scientist who publishes a newsletter, Your Local Epidemiologist, updating developments in COVID and other pressing health issues.
“It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars,” said Dr. Jetelina, who is also director of population health analytics for the Meadows Mental Health Policy Institute. “COVID-19 is still going to be here, it’s still going to mutate,” and still cause grief for those affected. “I’m most concerned about our ability to track the virus. It’s not clear what surveillance we will still have in the states and around the globe.”
It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars.
For surveillance, she calls wastewater monitoring “the lowest-hanging fruit.” That’s because it “is not based on bias testing and has the potential to help with other outbreaks, too.” Hospitalization data is also essential, she said, as that information is the basis for public health decisions on updated vaccines and other protective measures.
While Dr. Jetelina is hopeful that COVID will someday be universally viewed as endemic, with predictable seasonal patterns, “I don’t think we are there yet. We still need to approach this virus with humility; that’s at least what I will continue to do.”
Dr. Rajnarayanan agreed that the pandemic has not yet reached endemic phase, though the situation is much improved. “Our vaccines are still protecting us from severe disease and hospitalization, and [the antiviral drug] Paxlovid is a great tool that works.”
Keeping tabs
While some data tracking has been eliminated, not all has, or will be. The CDC, as mentioned, continues to post cases, deaths, and a daily average of new hospital admissions weekly. The WHO’s dashboard tracks deaths, cases, and vaccine doses globally.
In March, the WHO updated its working definitions and tracking system for SARS-CoV-2 variants of concern and variants of interest, with goals of evaluating the sublineages independently and to classify new variants more clearly when that’s needed.
Still, WHO is considering ending its declaration of COVID as a public health emergency of international concern sometime in 2023.
Some public companies are staying vigilant. The drugstore chain Walgreens said it plans to maintain its COVID-19 Index, which launched in January 2022.
“Data regarding spread of variants is important to our understanding of viral transmission and, as new variants emerge, it will be critical to continue to track this information quickly to predict which communities are most at risk,” Anita Patel, PharmD, vice president of pharmacy services development for Walgreens, said in a statement.
The data also reinforces the importance of vaccinations and testing in helping to stop the spread of COVID-19, she said.
A version of this article first appeared on WebMD.com.
The 30-second commercial, part of the government’s We Can Do This campaign, shows everyday people going about their lives, then reminds them that, “because COVID is still out there and so are you,” it might be time to update your vaccine.
Many data tracking sources, both federal and others, are no longer reporting, as often, the number of COVID cases, hospitalizations, and deaths.
The Department of Health & Human Services in February stopped updating its public COVID data site, instead directing all queries to the Centers for Disease Control and Prevention, which itself has been updating only weekly instead of daily since 2022.
Nongovernmental sources, such as John Hopkins University, stopped reporting pandemic data in March, The New York Times also ended its COVID data-gathering project in March, stating that “the comprehensive real-time reporting that The Times has prioritized is no longer possible.” It will rely on reporting weekly CDC data moving forward.
Along with the tracking sites, masking and social distancing mandates have mostly disappeared. President Joe Biden signed a bipartisan bill on April 10 that ended the national emergency for COVID. While some programs will stay in place for now, such as free vaccines, treatments, and tests, that too will go away when the federal public health emergency expires on May 11. The HHS already has issued its transition roadmap.
Many Americans, meanwhile, are still on the fence about the pandemic. A Gallup poll from March shows that about half of the American public say it’s over, and about half disagree.
Are we closing up shop on COVID-19 too soon, or is it time? Not surprisingly, experts don’t agree. Some say the pandemic is now endemic – which broadly means the virus and its patterns are predictable and steady in designated regions – and that it’s critical to catch up on health needs neglected during the pandemic, such as screenings and other vaccinations
But others don’t think it’s reached that stage yet, saying that we are letting our guard down too soon and we can’t be blind to the possibility of another strong variant – or pandemic – emerging. Surveillance must continue, not decline, and be improved.
Time to move on?
In its transition roadmap released in February, the HHS notes that daily COVID reported cases are down over 90%, compared with the peak of the Omicron surge at the end of January 2022; deaths have declined by over 80%; and new hospitalizations caused by COVID have dropped by nearly 80%.
It is time to move on, said Ali Mokdad, PhD, a professor and chief strategy officer of population health at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle.
“Many people were delaying a lot of medical care, because they were afraid” during COVID’s height, he said, explaining that elective surgeries were postponed, prenatal care went down, as did screenings for blood pressure and diabetes.
His institute was tracking COVID projections every week but stopped in December.
As for emerging variants, “we haven’t seen a variant that scares us since Omicron” in November 2021, said Dr. Mokdad, who agrees that COVID is endemic now. The subvariants that followed it are very similar, and the current vaccines are working.
“We can move on, but we cannot drop the ball on keeping an eye on the genetic sequencing of the virus,” he said. That will enable quick identification of new variants.
If a worrisome new variant does surface, Dr. Mokdad said, certain locations and resources will be able to gear up quickly, while others won’t be as fast, but overall the United States is in a much better position now.
Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, also believes the pandemic phase is behind us
“This can’t be an emergency in perpetuity,” he said “Just because something is not a pandemic [anymore] does not mean that all activities related to it cease.”
COVID is highly unlikely to overwhelm hospitals again, and that was the main reason for the emergency declaration, he said.
“It’s not all or none – collapsing COVID-related [monitoring] activities into the routine monitoring that is done for other infectious disease should be seen as an achievement in taming the virus,” he said.
Not endemic yet
Closing up shop too early could mean we are blindsided, said Rajendram Rajnarayanan, PhD, an assistant dean of research and associate professor at the New York Institute of Technology College of Osteopathic Medicine at Arkansas State University in Jonesboro.
Already, he said, large labs have closed or scaled down as testing demand has declined, and many centers that offered community testing have also closed. Plus, home test results are often not reported.
Continued monitoring is key, he said. “You have to maintain a base level of sequencing for new variants,” he said. “Right now, the variant that is ‘top dog’ in the world is XBB.1.16.”
That’s an Omicron subvariant that the World Health Organization is currently keeping its eye on, according to a media briefing on March 29. There are about 800 sequences of it from 22 countries, mostly India, and it’s been in circulation a few months.
Dr. Rajnarayanan said he’s not overly worried about this variant, but surveillance must continue. His own breakdown of XBB.1.16 found the subvariant in 27 countries, including the United States, as of April 10.
Ideally, Dr. Rajnarayanan would suggest four areas to keep focusing on, moving forward:
- Active, random surveillance for new variants, especially in hot spots.
- Hospital surveillance and surveillance of long-term care, especially in congregate settings where people can more easily spread the virus.
- Travelers’ surveillance, now at , according to the CDC.
- Surveillance of animals such as mink and deer, because these animals can not only pick up the virus, but the virus can mutate in the animals, which could then transmit it back to people.
With less testing, baseline surveillance for new variants has declined. The other three surveillance areas need improvement, too, he said, as the reporting is often delayed.
Continued surveillance is crucial, agreed Katelyn Jetelina, PhD, an epidemiologist and data scientist who publishes a newsletter, Your Local Epidemiologist, updating developments in COVID and other pressing health issues.
“It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars,” said Dr. Jetelina, who is also director of population health analytics for the Meadows Mental Health Policy Institute. “COVID-19 is still going to be here, it’s still going to mutate,” and still cause grief for those affected. “I’m most concerned about our ability to track the virus. It’s not clear what surveillance we will still have in the states and around the globe.”
It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars.
For surveillance, she calls wastewater monitoring “the lowest-hanging fruit.” That’s because it “is not based on bias testing and has the potential to help with other outbreaks, too.” Hospitalization data is also essential, she said, as that information is the basis for public health decisions on updated vaccines and other protective measures.
While Dr. Jetelina is hopeful that COVID will someday be universally viewed as endemic, with predictable seasonal patterns, “I don’t think we are there yet. We still need to approach this virus with humility; that’s at least what I will continue to do.”
Dr. Rajnarayanan agreed that the pandemic has not yet reached endemic phase, though the situation is much improved. “Our vaccines are still protecting us from severe disease and hospitalization, and [the antiviral drug] Paxlovid is a great tool that works.”
Keeping tabs
While some data tracking has been eliminated, not all has, or will be. The CDC, as mentioned, continues to post cases, deaths, and a daily average of new hospital admissions weekly. The WHO’s dashboard tracks deaths, cases, and vaccine doses globally.
In March, the WHO updated its working definitions and tracking system for SARS-CoV-2 variants of concern and variants of interest, with goals of evaluating the sublineages independently and to classify new variants more clearly when that’s needed.
Still, WHO is considering ending its declaration of COVID as a public health emergency of international concern sometime in 2023.
Some public companies are staying vigilant. The drugstore chain Walgreens said it plans to maintain its COVID-19 Index, which launched in January 2022.
“Data regarding spread of variants is important to our understanding of viral transmission and, as new variants emerge, it will be critical to continue to track this information quickly to predict which communities are most at risk,” Anita Patel, PharmD, vice president of pharmacy services development for Walgreens, said in a statement.
The data also reinforces the importance of vaccinations and testing in helping to stop the spread of COVID-19, she said.
A version of this article first appeared on WebMD.com.
The 30-second commercial, part of the government’s We Can Do This campaign, shows everyday people going about their lives, then reminds them that, “because COVID is still out there and so are you,” it might be time to update your vaccine.
Many data tracking sources, both federal and others, are no longer reporting, as often, the number of COVID cases, hospitalizations, and deaths.
The Department of Health & Human Services in February stopped updating its public COVID data site, instead directing all queries to the Centers for Disease Control and Prevention, which itself has been updating only weekly instead of daily since 2022.
Nongovernmental sources, such as John Hopkins University, stopped reporting pandemic data in March, The New York Times also ended its COVID data-gathering project in March, stating that “the comprehensive real-time reporting that The Times has prioritized is no longer possible.” It will rely on reporting weekly CDC data moving forward.
Along with the tracking sites, masking and social distancing mandates have mostly disappeared. President Joe Biden signed a bipartisan bill on April 10 that ended the national emergency for COVID. While some programs will stay in place for now, such as free vaccines, treatments, and tests, that too will go away when the federal public health emergency expires on May 11. The HHS already has issued its transition roadmap.
Many Americans, meanwhile, are still on the fence about the pandemic. A Gallup poll from March shows that about half of the American public say it’s over, and about half disagree.
Are we closing up shop on COVID-19 too soon, or is it time? Not surprisingly, experts don’t agree. Some say the pandemic is now endemic – which broadly means the virus and its patterns are predictable and steady in designated regions – and that it’s critical to catch up on health needs neglected during the pandemic, such as screenings and other vaccinations
But others don’t think it’s reached that stage yet, saying that we are letting our guard down too soon and we can’t be blind to the possibility of another strong variant – or pandemic – emerging. Surveillance must continue, not decline, and be improved.
Time to move on?
In its transition roadmap released in February, the HHS notes that daily COVID reported cases are down over 90%, compared with the peak of the Omicron surge at the end of January 2022; deaths have declined by over 80%; and new hospitalizations caused by COVID have dropped by nearly 80%.
It is time to move on, said Ali Mokdad, PhD, a professor and chief strategy officer of population health at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle.
“Many people were delaying a lot of medical care, because they were afraid” during COVID’s height, he said, explaining that elective surgeries were postponed, prenatal care went down, as did screenings for blood pressure and diabetes.
His institute was tracking COVID projections every week but stopped in December.
As for emerging variants, “we haven’t seen a variant that scares us since Omicron” in November 2021, said Dr. Mokdad, who agrees that COVID is endemic now. The subvariants that followed it are very similar, and the current vaccines are working.
“We can move on, but we cannot drop the ball on keeping an eye on the genetic sequencing of the virus,” he said. That will enable quick identification of new variants.
If a worrisome new variant does surface, Dr. Mokdad said, certain locations and resources will be able to gear up quickly, while others won’t be as fast, but overall the United States is in a much better position now.
Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, also believes the pandemic phase is behind us
“This can’t be an emergency in perpetuity,” he said “Just because something is not a pandemic [anymore] does not mean that all activities related to it cease.”
COVID is highly unlikely to overwhelm hospitals again, and that was the main reason for the emergency declaration, he said.
“It’s not all or none – collapsing COVID-related [monitoring] activities into the routine monitoring that is done for other infectious disease should be seen as an achievement in taming the virus,” he said.
Not endemic yet
Closing up shop too early could mean we are blindsided, said Rajendram Rajnarayanan, PhD, an assistant dean of research and associate professor at the New York Institute of Technology College of Osteopathic Medicine at Arkansas State University in Jonesboro.
Already, he said, large labs have closed or scaled down as testing demand has declined, and many centers that offered community testing have also closed. Plus, home test results are often not reported.
Continued monitoring is key, he said. “You have to maintain a base level of sequencing for new variants,” he said. “Right now, the variant that is ‘top dog’ in the world is XBB.1.16.”
That’s an Omicron subvariant that the World Health Organization is currently keeping its eye on, according to a media briefing on March 29. There are about 800 sequences of it from 22 countries, mostly India, and it’s been in circulation a few months.
Dr. Rajnarayanan said he’s not overly worried about this variant, but surveillance must continue. His own breakdown of XBB.1.16 found the subvariant in 27 countries, including the United States, as of April 10.
Ideally, Dr. Rajnarayanan would suggest four areas to keep focusing on, moving forward:
- Active, random surveillance for new variants, especially in hot spots.
- Hospital surveillance and surveillance of long-term care, especially in congregate settings where people can more easily spread the virus.
- Travelers’ surveillance, now at , according to the CDC.
- Surveillance of animals such as mink and deer, because these animals can not only pick up the virus, but the virus can mutate in the animals, which could then transmit it back to people.
With less testing, baseline surveillance for new variants has declined. The other three surveillance areas need improvement, too, he said, as the reporting is often delayed.
Continued surveillance is crucial, agreed Katelyn Jetelina, PhD, an epidemiologist and data scientist who publishes a newsletter, Your Local Epidemiologist, updating developments in COVID and other pressing health issues.
“It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars,” said Dr. Jetelina, who is also director of population health analytics for the Meadows Mental Health Policy Institute. “COVID-19 is still going to be here, it’s still going to mutate,” and still cause grief for those affected. “I’m most concerned about our ability to track the virus. It’s not clear what surveillance we will still have in the states and around the globe.”
It’s a bit ironic to have a date for the end of a public health emergency; viruses don’t care about calendars.
For surveillance, she calls wastewater monitoring “the lowest-hanging fruit.” That’s because it “is not based on bias testing and has the potential to help with other outbreaks, too.” Hospitalization data is also essential, she said, as that information is the basis for public health decisions on updated vaccines and other protective measures.
While Dr. Jetelina is hopeful that COVID will someday be universally viewed as endemic, with predictable seasonal patterns, “I don’t think we are there yet. We still need to approach this virus with humility; that’s at least what I will continue to do.”
Dr. Rajnarayanan agreed that the pandemic has not yet reached endemic phase, though the situation is much improved. “Our vaccines are still protecting us from severe disease and hospitalization, and [the antiviral drug] Paxlovid is a great tool that works.”
Keeping tabs
While some data tracking has been eliminated, not all has, or will be. The CDC, as mentioned, continues to post cases, deaths, and a daily average of new hospital admissions weekly. The WHO’s dashboard tracks deaths, cases, and vaccine doses globally.
In March, the WHO updated its working definitions and tracking system for SARS-CoV-2 variants of concern and variants of interest, with goals of evaluating the sublineages independently and to classify new variants more clearly when that’s needed.
Still, WHO is considering ending its declaration of COVID as a public health emergency of international concern sometime in 2023.
Some public companies are staying vigilant. The drugstore chain Walgreens said it plans to maintain its COVID-19 Index, which launched in January 2022.
“Data regarding spread of variants is important to our understanding of viral transmission and, as new variants emerge, it will be critical to continue to track this information quickly to predict which communities are most at risk,” Anita Patel, PharmD, vice president of pharmacy services development for Walgreens, said in a statement.
The data also reinforces the importance of vaccinations and testing in helping to stop the spread of COVID-19, she said.
A version of this article first appeared on WebMD.com.
You’ve quit smoking with vaping. Now what?
This article is part of a series from Medscape on vaping.
Every day, Sonia Sharma, PA, meets people like Natalie H., who is trying to quit vaping.
Natalie, a member of the nicotine addiction support group at the University of California San Francisco’s Fontana Tobacco Treatment Center, switched from traditional cigarettes to vaping but found the electronic version just as addictive and eventually decided to quit using nicotine completely.
“I went from being an occasional cigarette smoker, a few a month, to a daily vaper,” said Natalie, who preferred not to give her last name to protect her privacy. “Vaping made my nicotine addiction worse, not better.”
“We have people tell us they vape before their feet hit the ground in the morning,” said Ms. Sharma, who coleads Natalie’s support group at UCSF. Ms. Sharma has met individuals who had smoked four to five cigarettes a day, switched to e-cigarettes to quit smoking, then vaped the equivalent of a pack a day. Others had switched to vapes to quit but ended up both vaping and smoking again. And others picked up vaping without ever smoking. They want to quit, she said, but are not sure how.
Researchers from the National Institutes of Health in 2020 reported that 5.6 million adults in the United States vaped. A little over 57% of people said they started using e-cigarettes to quit smoking traditional cigarettes. Another study in 2021 based on survey data found that about 60% of e-cigarette users wanted to quit their vaping habit.
Vaping has been marketed as a way to help people kick their smoking habit. Research is inconclusive on this claim. But unlike cessation tools like nicotine gums or lozenges, using vapes for cessation is uncharted territory. Vapers lack guidance for how to use the devices to quit, and they have even less direction on what to do if they develop an addiction to the vapes themselves.
A new addiction?
Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery in New Jersey, said she has witnessed a higher level of nicotine addiction in the vapers with whom she has worked.
“When someone takes a hit from a vaping device, it doesn’t generate the burn it would from traditional tobacco,” Ms. Hanna said. “This causes people to take a deeper pull, and when they take a deeper pull, they establish a higher level of nicotine dependence over time.”
A 2019 study of nearly 900 people published in the New England Journal of Medicine found that smokers who used vapes for cessation were twice as likely to have quit smoking cigarettes as those who used other nicotine replacement therapy. However, 80% of people who switched to vaping were using e-cigarettes a year after they tried to quit smoking.
Given that potential for addiction, Nancy Rigotti, MD, director of Massachusetts General Hospital’s Tobacco Research and Treatment Center in Boston, said patients must use vapes “properly” for cessation. That means giving up smoking completely and quitting vapes as soon as patients are sure they will not go back to smoking tobacco.
“We are going to need to help these people to stop vaping,” said Dr. Rigotti, who is working with Achieve Life Sciences, a pharmaceutical company developing a prescription drug to treat nicotine addiction from vapes and cigarettes.
And many nicotine users who have tried vaping to quit smoking end up becoming dual users.
“It’s important to stress that health benefits [of switching to vaping] only occur if the switch to vapes is complete and permanent. So far, that appears difficult to do for most people who smoke, and in my anecdotal experience it has not worked,” said J. Taylor Hays, MD, the former medical director of Mayo Clinic’s Nicotine Dependence Center in Rochester, Minn.
Besides challenges in communicating the current evidence, no established method exists to help vapers quit, according to Nigar Nargis, PhD, senior scientific director of tobacco control research at the American Cancer Society.
“There are some experimental methods like using social interventions, counseling, and some educational campaigns,” Dr. Nargis said. “[Little] progress has been done in terms of clinical interventions.”
Unlike cessation products such as gum or a nicotine patch, which have clear recommendations for duration of use, similar guidelines don’t exist for vapes, in part because the U.S. Food and Drug Administration hasn’t yet granted approval of vapes as cessation products.
Alex Clark, the CEO of Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping, said people could vape for longer and still benefit from making the switch from traditional cigarettes.
“The most important thing is that people start replacing cigarettes with a smoke-free product and continue until they’ve completely switched,” said Mr. Clark, whose group accepts donations from the e-cigarette industry. “Following switching, people are encouraged to continue with the product for as long as they feel necessary.”
But 2013 guidelines from the FDA advised makers of nicotine-replacement therapies – including gums, patches, and lozenges – to include labeling that advises users to complete treatment. According to the agency, if a person feels like they “need to use [the NRT product] for a longer period to keep from smoking, talk to your health care provider.”
Dr. Hays, who is now an emeritus professor at the Mayo Clinic, said he would not recommend patients try vaping as a cessation device given the availability of more proven techniques such as patches and gums. If a patient insists, vaping could be considered under the medical guidance of a cessation professional. He also advised people purchase products only from large tobacco companies that are likely to have “reasonable quality control.” Hundreds of vaping devices are on the market, and they are not all equivalent, he said.
But when an e-cigarette user wants to quit vaping, guidance might boil down to using traditional tobacco cessation methods like gums and lozenges because few tools exist to help people with a vaping-specific addiction.
The long-term health outcomes of vaping are also unclear, and decades will pass before scientists are able to make conclusions, according to Thomas Eissenberg, PhD, codirector of Virginia Commonwealth University’s Center for the Study of Tobacco Products in Richmond.
“I don’t think anyone knows what the long-term effects of heated propylene glycol and vegetable glycerin and flavors intended as food ingredients are, especially when these compounds are inhaled hundreds of times a day, week after week, year after year,” Dr. Eissenberg said.
Dr. Rigotti reported that she receives no funding from the tobacco or e-cigarette industry. She is working with Achieve Life Sciences to develop a tool for vaping cessation. Dr. Eissenberg, Ms. Hanna, Dr. Hays, Dr. Nargis, and Ms. Sharma reported no funding from the tobacco or e-cigarette industry.
A version of this article first appeared on Medscape.com.
This article is part of a series from Medscape on vaping.
Every day, Sonia Sharma, PA, meets people like Natalie H., who is trying to quit vaping.
Natalie, a member of the nicotine addiction support group at the University of California San Francisco’s Fontana Tobacco Treatment Center, switched from traditional cigarettes to vaping but found the electronic version just as addictive and eventually decided to quit using nicotine completely.
“I went from being an occasional cigarette smoker, a few a month, to a daily vaper,” said Natalie, who preferred not to give her last name to protect her privacy. “Vaping made my nicotine addiction worse, not better.”
“We have people tell us they vape before their feet hit the ground in the morning,” said Ms. Sharma, who coleads Natalie’s support group at UCSF. Ms. Sharma has met individuals who had smoked four to five cigarettes a day, switched to e-cigarettes to quit smoking, then vaped the equivalent of a pack a day. Others had switched to vapes to quit but ended up both vaping and smoking again. And others picked up vaping without ever smoking. They want to quit, she said, but are not sure how.
Researchers from the National Institutes of Health in 2020 reported that 5.6 million adults in the United States vaped. A little over 57% of people said they started using e-cigarettes to quit smoking traditional cigarettes. Another study in 2021 based on survey data found that about 60% of e-cigarette users wanted to quit their vaping habit.
Vaping has been marketed as a way to help people kick their smoking habit. Research is inconclusive on this claim. But unlike cessation tools like nicotine gums or lozenges, using vapes for cessation is uncharted territory. Vapers lack guidance for how to use the devices to quit, and they have even less direction on what to do if they develop an addiction to the vapes themselves.
A new addiction?
Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery in New Jersey, said she has witnessed a higher level of nicotine addiction in the vapers with whom she has worked.
“When someone takes a hit from a vaping device, it doesn’t generate the burn it would from traditional tobacco,” Ms. Hanna said. “This causes people to take a deeper pull, and when they take a deeper pull, they establish a higher level of nicotine dependence over time.”
A 2019 study of nearly 900 people published in the New England Journal of Medicine found that smokers who used vapes for cessation were twice as likely to have quit smoking cigarettes as those who used other nicotine replacement therapy. However, 80% of people who switched to vaping were using e-cigarettes a year after they tried to quit smoking.
Given that potential for addiction, Nancy Rigotti, MD, director of Massachusetts General Hospital’s Tobacco Research and Treatment Center in Boston, said patients must use vapes “properly” for cessation. That means giving up smoking completely and quitting vapes as soon as patients are sure they will not go back to smoking tobacco.
“We are going to need to help these people to stop vaping,” said Dr. Rigotti, who is working with Achieve Life Sciences, a pharmaceutical company developing a prescription drug to treat nicotine addiction from vapes and cigarettes.
And many nicotine users who have tried vaping to quit smoking end up becoming dual users.
“It’s important to stress that health benefits [of switching to vaping] only occur if the switch to vapes is complete and permanent. So far, that appears difficult to do for most people who smoke, and in my anecdotal experience it has not worked,” said J. Taylor Hays, MD, the former medical director of Mayo Clinic’s Nicotine Dependence Center in Rochester, Minn.
Besides challenges in communicating the current evidence, no established method exists to help vapers quit, according to Nigar Nargis, PhD, senior scientific director of tobacco control research at the American Cancer Society.
“There are some experimental methods like using social interventions, counseling, and some educational campaigns,” Dr. Nargis said. “[Little] progress has been done in terms of clinical interventions.”
Unlike cessation products such as gum or a nicotine patch, which have clear recommendations for duration of use, similar guidelines don’t exist for vapes, in part because the U.S. Food and Drug Administration hasn’t yet granted approval of vapes as cessation products.
Alex Clark, the CEO of Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping, said people could vape for longer and still benefit from making the switch from traditional cigarettes.
“The most important thing is that people start replacing cigarettes with a smoke-free product and continue until they’ve completely switched,” said Mr. Clark, whose group accepts donations from the e-cigarette industry. “Following switching, people are encouraged to continue with the product for as long as they feel necessary.”
But 2013 guidelines from the FDA advised makers of nicotine-replacement therapies – including gums, patches, and lozenges – to include labeling that advises users to complete treatment. According to the agency, if a person feels like they “need to use [the NRT product] for a longer period to keep from smoking, talk to your health care provider.”
Dr. Hays, who is now an emeritus professor at the Mayo Clinic, said he would not recommend patients try vaping as a cessation device given the availability of more proven techniques such as patches and gums. If a patient insists, vaping could be considered under the medical guidance of a cessation professional. He also advised people purchase products only from large tobacco companies that are likely to have “reasonable quality control.” Hundreds of vaping devices are on the market, and they are not all equivalent, he said.
But when an e-cigarette user wants to quit vaping, guidance might boil down to using traditional tobacco cessation methods like gums and lozenges because few tools exist to help people with a vaping-specific addiction.
The long-term health outcomes of vaping are also unclear, and decades will pass before scientists are able to make conclusions, according to Thomas Eissenberg, PhD, codirector of Virginia Commonwealth University’s Center for the Study of Tobacco Products in Richmond.
“I don’t think anyone knows what the long-term effects of heated propylene glycol and vegetable glycerin and flavors intended as food ingredients are, especially when these compounds are inhaled hundreds of times a day, week after week, year after year,” Dr. Eissenberg said.
Dr. Rigotti reported that she receives no funding from the tobacco or e-cigarette industry. She is working with Achieve Life Sciences to develop a tool for vaping cessation. Dr. Eissenberg, Ms. Hanna, Dr. Hays, Dr. Nargis, and Ms. Sharma reported no funding from the tobacco or e-cigarette industry.
A version of this article first appeared on Medscape.com.
This article is part of a series from Medscape on vaping.
Every day, Sonia Sharma, PA, meets people like Natalie H., who is trying to quit vaping.
Natalie, a member of the nicotine addiction support group at the University of California San Francisco’s Fontana Tobacco Treatment Center, switched from traditional cigarettes to vaping but found the electronic version just as addictive and eventually decided to quit using nicotine completely.
“I went from being an occasional cigarette smoker, a few a month, to a daily vaper,” said Natalie, who preferred not to give her last name to protect her privacy. “Vaping made my nicotine addiction worse, not better.”
“We have people tell us they vape before their feet hit the ground in the morning,” said Ms. Sharma, who coleads Natalie’s support group at UCSF. Ms. Sharma has met individuals who had smoked four to five cigarettes a day, switched to e-cigarettes to quit smoking, then vaped the equivalent of a pack a day. Others had switched to vapes to quit but ended up both vaping and smoking again. And others picked up vaping without ever smoking. They want to quit, she said, but are not sure how.
Researchers from the National Institutes of Health in 2020 reported that 5.6 million adults in the United States vaped. A little over 57% of people said they started using e-cigarettes to quit smoking traditional cigarettes. Another study in 2021 based on survey data found that about 60% of e-cigarette users wanted to quit their vaping habit.
Vaping has been marketed as a way to help people kick their smoking habit. Research is inconclusive on this claim. But unlike cessation tools like nicotine gums or lozenges, using vapes for cessation is uncharted territory. Vapers lack guidance for how to use the devices to quit, and they have even less direction on what to do if they develop an addiction to the vapes themselves.
A new addiction?
Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery in New Jersey, said she has witnessed a higher level of nicotine addiction in the vapers with whom she has worked.
“When someone takes a hit from a vaping device, it doesn’t generate the burn it would from traditional tobacco,” Ms. Hanna said. “This causes people to take a deeper pull, and when they take a deeper pull, they establish a higher level of nicotine dependence over time.”
A 2019 study of nearly 900 people published in the New England Journal of Medicine found that smokers who used vapes for cessation were twice as likely to have quit smoking cigarettes as those who used other nicotine replacement therapy. However, 80% of people who switched to vaping were using e-cigarettes a year after they tried to quit smoking.
Given that potential for addiction, Nancy Rigotti, MD, director of Massachusetts General Hospital’s Tobacco Research and Treatment Center in Boston, said patients must use vapes “properly” for cessation. That means giving up smoking completely and quitting vapes as soon as patients are sure they will not go back to smoking tobacco.
“We are going to need to help these people to stop vaping,” said Dr. Rigotti, who is working with Achieve Life Sciences, a pharmaceutical company developing a prescription drug to treat nicotine addiction from vapes and cigarettes.
And many nicotine users who have tried vaping to quit smoking end up becoming dual users.
“It’s important to stress that health benefits [of switching to vaping] only occur if the switch to vapes is complete and permanent. So far, that appears difficult to do for most people who smoke, and in my anecdotal experience it has not worked,” said J. Taylor Hays, MD, the former medical director of Mayo Clinic’s Nicotine Dependence Center in Rochester, Minn.
Besides challenges in communicating the current evidence, no established method exists to help vapers quit, according to Nigar Nargis, PhD, senior scientific director of tobacco control research at the American Cancer Society.
“There are some experimental methods like using social interventions, counseling, and some educational campaigns,” Dr. Nargis said. “[Little] progress has been done in terms of clinical interventions.”
Unlike cessation products such as gum or a nicotine patch, which have clear recommendations for duration of use, similar guidelines don’t exist for vapes, in part because the U.S. Food and Drug Administration hasn’t yet granted approval of vapes as cessation products.
Alex Clark, the CEO of Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping, said people could vape for longer and still benefit from making the switch from traditional cigarettes.
“The most important thing is that people start replacing cigarettes with a smoke-free product and continue until they’ve completely switched,” said Mr. Clark, whose group accepts donations from the e-cigarette industry. “Following switching, people are encouraged to continue with the product for as long as they feel necessary.”
But 2013 guidelines from the FDA advised makers of nicotine-replacement therapies – including gums, patches, and lozenges – to include labeling that advises users to complete treatment. According to the agency, if a person feels like they “need to use [the NRT product] for a longer period to keep from smoking, talk to your health care provider.”
Dr. Hays, who is now an emeritus professor at the Mayo Clinic, said he would not recommend patients try vaping as a cessation device given the availability of more proven techniques such as patches and gums. If a patient insists, vaping could be considered under the medical guidance of a cessation professional. He also advised people purchase products only from large tobacco companies that are likely to have “reasonable quality control.” Hundreds of vaping devices are on the market, and they are not all equivalent, he said.
But when an e-cigarette user wants to quit vaping, guidance might boil down to using traditional tobacco cessation methods like gums and lozenges because few tools exist to help people with a vaping-specific addiction.
The long-term health outcomes of vaping are also unclear, and decades will pass before scientists are able to make conclusions, according to Thomas Eissenberg, PhD, codirector of Virginia Commonwealth University’s Center for the Study of Tobacco Products in Richmond.
“I don’t think anyone knows what the long-term effects of heated propylene glycol and vegetable glycerin and flavors intended as food ingredients are, especially when these compounds are inhaled hundreds of times a day, week after week, year after year,” Dr. Eissenberg said.
Dr. Rigotti reported that she receives no funding from the tobacco or e-cigarette industry. She is working with Achieve Life Sciences to develop a tool for vaping cessation. Dr. Eissenberg, Ms. Hanna, Dr. Hays, Dr. Nargis, and Ms. Sharma reported no funding from the tobacco or e-cigarette industry.
A version of this article first appeared on Medscape.com.
Should you recommend e-cigs to help patients quit smoking?
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
In 2014, after smoking cigarettes for 40 years, Kati Markowitz decided to switch to vaping. She had heard the newer electronic cigarettes might be less harmful. And, at the time, she said, she wasn’t aware of other options to try to quit smoking.
For 7 years, she vaped every day.
Then Ms. Markowitz received news she’d hoped never to hear: She had lung cancer. A nodule detected in a CT scan had grown. She was scheduled for treatment – the removal of an entire lobe from her right lung. But first, she said, her surgeon told her she had to quit vaping, which reduces the risk for post-operative complications and enables a healthy recovery.
Ms. Markowitz had thought switching to vaping would be less harmful than smoking cigarettes. Now, she no longer believes that’s true.
“Did I fool myself by hoping to get lucky and not have any bad repercussions? Yes, I did,” Ms. Markowitz said, adding that she wonders if vaping contributed to her lung cancer or if she’ll experience other negative health effects in the future.
Researchers are divided on if e-cigarettes are as effective in smoking cessation as other nicotine replacement therapies like gums and lozenges. They also say more research is needed on the long-term health impacts of vaping to ultimately determine if vapes are a safe replacement for cigarettes.
“There is scientific research to support vaping as a cessation tool, but we wouldn’t use it as a first line of defense because we still need longitudinal studies to understand the long-term risk of e-cigarettes,” said Monica Hanna, MPH, assistant director of the Nicotine and Tobacco Recovery Program at RWJBarnabas Health’s Institute for Prevention and Recovery, Eatontown, N.J. “We also need research to understand exactly how we could use e-cigarettes as a cessation device.”
Vaping to quit
The first prototypes of e-cigarettes were developed in the 1930s, although what are now known as vapes weren’t sold by manufacturers until the 2000s in the United States, following an invention by a former health official in China. The vape was touted by both researchers and manufacturers over the years of development as a way to quit smoking cigarettes.
The Consumer Advocates for Smoke-free Alternatives Association, a nonprofit group that supports vaping and accepts donations from the e-cigarette industry, has compiled more than 13,000 testimonials from people who say vaping helped them give up smoking.
Studies show mixed results that using vapes can help traditional smokers quit.
A November 2022 Cochrane review showed a “high certainty of evidence that people are more likely to stop smoking traditional cigarettes for at least 6 months using e-cigarettes, or ‘vapes,’ than using nicotine replacement therapies, such as patches and gums.” The meta-analysis examined 78 studies with more than 22,000 participants. And a 2019 study with 886 participants, published in the New England Journal Medicine, found smokers who tried vaping to quit were twice as likely after a year to have stopped smoking cigarettes than those who used nicotine replacement therapy.
“In terms of the global research, it’s pretty clear that vaping can help smokers quit,” said Peter Shields, MD, a professor in the department of internal medicine at The Ohio State University College of Medicine, Columbus, who specializes in the treatment of lung cancer.
But a 2013 study published in the Lancet, and another from the Lancet in 2019, found only a modest improvement in cessation outcomes when participants used e-cigarettes paired with patches, compared with patches alone.
“For a disruptive technology that was supposed to end combustible tobacco use, there seems very little large-scale disruption,” said Thomas Eissenberg, PhD, co-director of Virginia Commonwealth University’s Center for the Study of Tobacco Products, Richmond.
Michael Joseph Blaha, MD, MPH, director of clinical research at the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, Baltimore, pointed to research that shows a portion of people who start vaping to quit smoking end up using both products – or become so-called “dual” users.
“I do think there is fairly high-quality evidence that vaping can lead to more cessation, but at the tradeoff of more long-term dual users and more overall nicotine addiction,” Dr. Blaha said. “Vaping remains a third-line clinical tool after nicotine replacement therapy and FDA-approved cessation medications.”
The U.S. Food and Drug Administration has not approved any e-cigarette or vaping device for smoking cessation, like it has for patches and gums, which means manufacturers cannot market their products as helping tobacco smokers quit.
“ Ms. Hanna, from RWJBarnabas Health’s Institute for Prevention and Recovery, said.
Reducing harm and improving health?
Vapes have also been touted as a boon to individual and public health since cigarette smoking is the leading cause of preventable disease and disability in the United States, responsible for more than 480,000 deaths per year in the U.S., according to the U.S. Centers for Disease Control and Prevention.
Quitting smoking lowers the risk of developing various cancers, heart disease, stroke, and other serious diseases. The aim of nicotine replacement therapy is to help smokers quit by gradually providing the body with smaller doses of nicotine over time, without exposing the body to toxic chemicals found in cigarettes.
“No one should say that e-cigarettes are safe, but compared to cigarettes, the data is consistent: They are not as harmful, and when a smoker switches, it’s better for them,” Dr. Shields said. “Like with other nicotine replacement therapies, if there is a risk that someone stops vaping and returns to smoking, I would rather have them as long-term vapers since it is generally considered to be less harmful than combustible tobacco.”
The FDA has allowed a handful of companies to market their electronic nicotine delivery systems as safer than traditional cigarettes by gaining approval through the Premarket Tobacco Product Applications process. In 2021, the agency announced its first PMTA authorization of an electronic cigarette to R.J. Reynolds for three of its tobacco-flavored vaping products. Regulators approved more products from three additional companies in 2022.
But the FDA has also denied others, including two products in 2023 from R.J. Reynolds, stating that, “the applications lacked sufficient evidence to demonstrate that permitting the marketing of the products would be appropriate for the protection of the public health.”
Questions remain among some researchers on the effects of vaping if used long term. Data on the health effects of vapes are just beginning to emerge and are mainly from studies of animals or cells. Measuring health effects among vape users will entail decades more of study, since Americans only gained access to the products in the 2000s.
Dr. Eissenberg said vaping likely does not cause the same diseases as cigarette smoking, but that does not mean they are not harmful. Ingredients found in e-cigarettes, such as heated propylene glycol, vegetable glycerin, and flavors, have only been used as food ingredients. The potential diseases caused by vapes are still unknown, because inhaling these heated ingredients is new. He also said he had “no issue” with an adult smoker vaping to help them quit smoking – as long they do so for a short period.
“I am very concerned that long-term use in adults could lead to considerable disease and death,” Dr. Eissenberg said. “Simply put, the human lung evolved for one purpose: gas exchange of oxygen in, carbon dioxide out. Anything else that enters the lung is a challenge to the organ.”
But Kenneth Warner, PhD, dean emeritus at the University of Michigan School of Public Health, Ann Arbor, said breaking the addiction to traditional cigarettes could reduce high rates of lung cancer in lower income communities where rates of smoking are comparatively high.
About three times as many Americans smoked (12.6%) than vaped (4.7%) in 2021, but those who live in households with lower incomes are more likely to smoke. According to the CDC, use of tobacco is higher among adults who were uninsured (27.3%) or who had Medicaid coverage (28.6%) than among those with private insurance (16.4%). People with annual family incomes of less than $12,500 also are more likely to be diagnosed with lung cancer than those with family incomes of $50,000 or more. Public health researchers have attributed those disparities in part to higher rates of smoking in lower-income households.
Dr. Warner said many lower-income and other Americans may never quit smoking cigarettes because they believe making the switch to e-cigarettes will not benefit their health. A 2022 study, published in the American Journal of Preventive Medicine, found that the percent of Americans who thought vaping was more harmful than smoking quadrupled between 2018 and 2020, from 6.8% to 28.3%. A third of respondents thought vaping was as harmful as smoking.
“We’ve convinced a large percentage of the American public that vaping is as harmful as smoking when it could be helping people quit smoking,” Dr. Warner said. “People are dying right now.”
Ms. Markowitz did quit smoking by taking up vaping. But now she questions if her lung cancer prognosis would have been delayed, or even avoided, if she’d tried a traditional method like a lozenge or gum instead. She vaped once an hour for most of her 7 years of using the devices.
“For people who are trying to stop smoking, I would recommend something like the patch instead,” Ms. Markowitz said.
The Consumer Advocates for Smoke-free Alternatives receives funding from the vaping industry. Dr. Blaha, Dr. Eissenberg, Ms. Hanna, Dr. Shields, and Dr. Warner reported no funding from the tobacco or e-cigarette industry. Dr. Blaha and Dr. Warner receive tobacco-related research funding from the FDA. Dr. Warner is a member of the FDA’s Tobacco Products Scientific Advisory Committee.
A version of this article first appeared on Medscape.com.
Long COVID: ‘On par’ with heart disease, cancer, book says
Filmmaker Gez Medinger and immunologist Danny Altmann have been dubbed by British media as “COVID’s odd couple,” and they don’t mind at all. Discussing their recent book, The Long COVID Handbook, the authors lean into their animated roles: Medinger is a passionate patient-researcher and “guinea pig” (his words) in search of his own healing, and Altmann is a no-nonsense, data-driven scientist and “Professor Boring” (as he puts it).
And the message they have about the impact of long COVID is stunning.
“The clinical burden [of long COVID] is somewhere on par with the whole of heart disease all over again, or the whole of oncology all over again, which are our biggest clinical bills concurrently,” Altmann said.
The pair met early in the pandemic, after Medinger became infected during the first wave and interviewed Altmann for his YouTube channel, which has more than 5 million views.
“Danny was one of the first people from the medical establishment to sort of stand up on the parapet and wave a flag and say, ‘Hey, guys, there’s a problem here.’ And that was incredibly validating for 2 million people in the U.K. alone who were suffering with long COVID,” Medinger said.
Their relationship works, not just for publishing one of the first definitive guides to long COVID, but also as a model for how patients with lived experiences can lead the way in medicine – from giving the condition its name to driving the medical establishment for recognition, clinical research, and therapeutic answers.
With Altmann currently leading a major research project at Imperial College London on long COVID and Medinger’s social media platform and communication skills, they’re both advancing the world’s understanding of the disease in their own way.
“We’re now more than 3 years into this completely mysterious, uncharted disease process with a whole globe full of really desperate people,” said Altmann. “It’s a living, organic thing, and yet that also demands some kind of order and collation and pulling together into some kind of sense. So I was very pleased when Gez approached me to help him with the book.”
In it, they translate everything they’ve learned about the condition that’s “scattered in 100,000 places around the globe” into a digestible format. It tells two sides of the same story: the anecdotal experiences Medinger has undergone or observed in the long COVID community through more than a dozen of his own patient-led studies, as well the hard science and research that’s amassing in the medical world.
In an interview,
What are the book’s key takeaways for you?
Medinger: “I would say we put together an incredibly comprehensive couple of chapters on the hypotheses, big picture, what’s causing long COVID. And then the nitty-gritty research for everything that we’ve found out that is going on. ... And the other part of the book that I think is particularly important, beyond the tips for managing symptoms, is the content on mental health and the impact on your emotional state and your capacity and just how huge that is. ... That has been the most powerful thing for patients when they’ve read it. And they’ve said that they’ve just been crying all the way through those chapters because suddenly they feel heard and seen.”
Altmann: “Obviously, you’d expect me to say that the parts of the book that I love most are the kind of hard-nosed, medical, mechanistic bits. ... We’ve got 150 million-plus desperate people deciding or not deciding to go and see their general practitioner, getting a fair hearing or not getting a fair hearing. And the poor doctor has never learned this in medical school, has never read a textbook on it, and hasn’t a clue what’s coming through the door.
How are they expected to know what to do? So I think the least we can do in some of those chapters is feed into their knowledge of general medicine and give them some clues. ... I think if we can explain to people what might be going on in them, and to their doctors, what on earth they might do about it, what kind of tests they might order, that helps a bit.”
How did you balance the more controversial parts of the book, including the chapter about so-called “treatments”? For instance, the book recounts Gez’s harrowing experience with ivermectin as a frightening warning. But Danny, you were nervous about even mentioning unproven and potentially dangerous treatments as things people have tried and have looked into.
Medinger: “We had to try and work out how to handle the topic, how to handle those points of view, whilst at the same time still being informative. I think the book is stronger for that chapter, too. The other thing would certainly have been to just not address the subject, but it’s one of the things that people want to know the most about. And there’s also a lot of bad information floating around out there about certain treatments. Ivermectin, for example, and this is what happened to me when I tried it. ‘Don’t do it. It’s not recommended. Please don’t.’
I think it was also very important to include because that cautionary tale really applies to every single one of those treatments that people might be hearing about that hasn’t been backed up by efficacy and safety studies.”
Altmann: “I think Gez has been quite diplomatic. That chapter was, I think, a testament to the power of the book. And the biggest test of our marriage as ‘the odd couple.’ Because when I first read the first draft of what Gez had written, I said, ‘my name can’t even be on this book. Otherwise, I’ll be sacked.’
And we had to find marriage counseling after that, and a way back to write a version of that chapter that expressed both halves of those concerns in a way that did justice to those different viewpoints. And I think that makes it quite a strong chapter.”
What do you think are the most urgent next steps in the search for solving long COVID?
Medinger: “I would personally like to try and get some sort of answer on viral persistence. ... If there’s one thing that feels like it would be treatable in theory, and would make sense why we’re still getting all of these symptoms this whole time later, it’s that, so I would like to try and establish or eliminate viral persistence. So if you gave me Elon Musk’s wealth, that’s what I would throw a bunch of the money at, trying to either eliminate or establish that.
And then, you know, the other important thing is a diagnostic test. Danny always talks about how important it is. Once you have that, it helps you suddenly open the doors to all these other things that you can do. And treatment trials. Let’s throw some meds at this so that we have an educated guess at what might work and put them into high-powered, randomized, controlled trials and see if anything comes out because from the patient perspective, I don’t think any of us wants to wait for 5 years for that stuff to start happening.”
Altmann: “I completely agree. If you go to a website, like clinicaltrials.gov, you’ll find an immense number of clinical trials on COVID. There isn’t really a shortage of them, some of them better-powered to get an answer than others.”
How do you think public policy needs to adapt for long COVID, including social safety nets such as workers’ compensation and disability benefits?
Medinger: “In terms of public policy, what I would like would be some public acknowledgment that it’s real from government sources. Just the acknowledgment that it’s real and it remains a risk even now.”
Altmann: “Nobody in politics asks my opinion. I think they’d hate to hear it. Because if I went to see them and said, well, actually, if you thought the COVID pandemic was bad, wait till you see what’s on the table now. We’ve created a disabled population in our country of 2 million, at least a portion if not more of people who are not fully contributory to the workforce anymore ... [with] legal wrangles about retirement and health insurance and pensions, and a human right to adequate health care. Which means, ideally, a purpose-built clinic where they can have their respiratory opinion and their rheumatology opinion and their endocrine opinion and their neurology opinion, all under one roof.”
You’ve both shown so much optimism. Why is that?
Altmann: “I’ve been an immunologist for a long time now, and written all my decades of grant applications, where as a community we made what, at the time, were kind of wild promises and wildly optimistic projections of how our knowledge of tumor immunity would revolutionize cancer care, and how knowledge of autoimmunity would revolutionize care of all the autoimmune diseases.
And weirdly almost every word we wrote over those 25 or 30 years came true. Cancer immunotherapy was revolutionized, and biologics for diabetes, multiple sclerosis, and arthritis were revolutionized. So if I have faith that those things came true, I have complete faith in this as well.”
Medinger: “From the patient perspective, what I would say is that we are seeing people who’ve been ill for more than 2 years recover. People are suddenly turning the corner when they might not have expected to.
And while we don’t quite know exactly why yet, and it’s not everyone, every single time I hear the story of someone saying, ‘I’m pretty much back to where I was, I feel like I’ve recovered,’ I feel great. Even if I haven’t. Because I know that every single time I hear someone say that, that just increases the probability that I will, too.”
A version of this article first appeared on WebMD.com.
Filmmaker Gez Medinger and immunologist Danny Altmann have been dubbed by British media as “COVID’s odd couple,” and they don’t mind at all. Discussing their recent book, The Long COVID Handbook, the authors lean into their animated roles: Medinger is a passionate patient-researcher and “guinea pig” (his words) in search of his own healing, and Altmann is a no-nonsense, data-driven scientist and “Professor Boring” (as he puts it).
And the message they have about the impact of long COVID is stunning.
“The clinical burden [of long COVID] is somewhere on par with the whole of heart disease all over again, or the whole of oncology all over again, which are our biggest clinical bills concurrently,” Altmann said.
The pair met early in the pandemic, after Medinger became infected during the first wave and interviewed Altmann for his YouTube channel, which has more than 5 million views.
“Danny was one of the first people from the medical establishment to sort of stand up on the parapet and wave a flag and say, ‘Hey, guys, there’s a problem here.’ And that was incredibly validating for 2 million people in the U.K. alone who were suffering with long COVID,” Medinger said.
Their relationship works, not just for publishing one of the first definitive guides to long COVID, but also as a model for how patients with lived experiences can lead the way in medicine – from giving the condition its name to driving the medical establishment for recognition, clinical research, and therapeutic answers.
With Altmann currently leading a major research project at Imperial College London on long COVID and Medinger’s social media platform and communication skills, they’re both advancing the world’s understanding of the disease in their own way.
“We’re now more than 3 years into this completely mysterious, uncharted disease process with a whole globe full of really desperate people,” said Altmann. “It’s a living, organic thing, and yet that also demands some kind of order and collation and pulling together into some kind of sense. So I was very pleased when Gez approached me to help him with the book.”
In it, they translate everything they’ve learned about the condition that’s “scattered in 100,000 places around the globe” into a digestible format. It tells two sides of the same story: the anecdotal experiences Medinger has undergone or observed in the long COVID community through more than a dozen of his own patient-led studies, as well the hard science and research that’s amassing in the medical world.
In an interview,
What are the book’s key takeaways for you?
Medinger: “I would say we put together an incredibly comprehensive couple of chapters on the hypotheses, big picture, what’s causing long COVID. And then the nitty-gritty research for everything that we’ve found out that is going on. ... And the other part of the book that I think is particularly important, beyond the tips for managing symptoms, is the content on mental health and the impact on your emotional state and your capacity and just how huge that is. ... That has been the most powerful thing for patients when they’ve read it. And they’ve said that they’ve just been crying all the way through those chapters because suddenly they feel heard and seen.”
Altmann: “Obviously, you’d expect me to say that the parts of the book that I love most are the kind of hard-nosed, medical, mechanistic bits. ... We’ve got 150 million-plus desperate people deciding or not deciding to go and see their general practitioner, getting a fair hearing or not getting a fair hearing. And the poor doctor has never learned this in medical school, has never read a textbook on it, and hasn’t a clue what’s coming through the door.
How are they expected to know what to do? So I think the least we can do in some of those chapters is feed into their knowledge of general medicine and give them some clues. ... I think if we can explain to people what might be going on in them, and to their doctors, what on earth they might do about it, what kind of tests they might order, that helps a bit.”
How did you balance the more controversial parts of the book, including the chapter about so-called “treatments”? For instance, the book recounts Gez’s harrowing experience with ivermectin as a frightening warning. But Danny, you were nervous about even mentioning unproven and potentially dangerous treatments as things people have tried and have looked into.
Medinger: “We had to try and work out how to handle the topic, how to handle those points of view, whilst at the same time still being informative. I think the book is stronger for that chapter, too. The other thing would certainly have been to just not address the subject, but it’s one of the things that people want to know the most about. And there’s also a lot of bad information floating around out there about certain treatments. Ivermectin, for example, and this is what happened to me when I tried it. ‘Don’t do it. It’s not recommended. Please don’t.’
I think it was also very important to include because that cautionary tale really applies to every single one of those treatments that people might be hearing about that hasn’t been backed up by efficacy and safety studies.”
Altmann: “I think Gez has been quite diplomatic. That chapter was, I think, a testament to the power of the book. And the biggest test of our marriage as ‘the odd couple.’ Because when I first read the first draft of what Gez had written, I said, ‘my name can’t even be on this book. Otherwise, I’ll be sacked.’
And we had to find marriage counseling after that, and a way back to write a version of that chapter that expressed both halves of those concerns in a way that did justice to those different viewpoints. And I think that makes it quite a strong chapter.”
What do you think are the most urgent next steps in the search for solving long COVID?
Medinger: “I would personally like to try and get some sort of answer on viral persistence. ... If there’s one thing that feels like it would be treatable in theory, and would make sense why we’re still getting all of these symptoms this whole time later, it’s that, so I would like to try and establish or eliminate viral persistence. So if you gave me Elon Musk’s wealth, that’s what I would throw a bunch of the money at, trying to either eliminate or establish that.
And then, you know, the other important thing is a diagnostic test. Danny always talks about how important it is. Once you have that, it helps you suddenly open the doors to all these other things that you can do. And treatment trials. Let’s throw some meds at this so that we have an educated guess at what might work and put them into high-powered, randomized, controlled trials and see if anything comes out because from the patient perspective, I don’t think any of us wants to wait for 5 years for that stuff to start happening.”
Altmann: “I completely agree. If you go to a website, like clinicaltrials.gov, you’ll find an immense number of clinical trials on COVID. There isn’t really a shortage of them, some of them better-powered to get an answer than others.”
How do you think public policy needs to adapt for long COVID, including social safety nets such as workers’ compensation and disability benefits?
Medinger: “In terms of public policy, what I would like would be some public acknowledgment that it’s real from government sources. Just the acknowledgment that it’s real and it remains a risk even now.”
Altmann: “Nobody in politics asks my opinion. I think they’d hate to hear it. Because if I went to see them and said, well, actually, if you thought the COVID pandemic was bad, wait till you see what’s on the table now. We’ve created a disabled population in our country of 2 million, at least a portion if not more of people who are not fully contributory to the workforce anymore ... [with] legal wrangles about retirement and health insurance and pensions, and a human right to adequate health care. Which means, ideally, a purpose-built clinic where they can have their respiratory opinion and their rheumatology opinion and their endocrine opinion and their neurology opinion, all under one roof.”
You’ve both shown so much optimism. Why is that?
Altmann: “I’ve been an immunologist for a long time now, and written all my decades of grant applications, where as a community we made what, at the time, were kind of wild promises and wildly optimistic projections of how our knowledge of tumor immunity would revolutionize cancer care, and how knowledge of autoimmunity would revolutionize care of all the autoimmune diseases.
And weirdly almost every word we wrote over those 25 or 30 years came true. Cancer immunotherapy was revolutionized, and biologics for diabetes, multiple sclerosis, and arthritis were revolutionized. So if I have faith that those things came true, I have complete faith in this as well.”
Medinger: “From the patient perspective, what I would say is that we are seeing people who’ve been ill for more than 2 years recover. People are suddenly turning the corner when they might not have expected to.
And while we don’t quite know exactly why yet, and it’s not everyone, every single time I hear the story of someone saying, ‘I’m pretty much back to where I was, I feel like I’ve recovered,’ I feel great. Even if I haven’t. Because I know that every single time I hear someone say that, that just increases the probability that I will, too.”
A version of this article first appeared on WebMD.com.
Filmmaker Gez Medinger and immunologist Danny Altmann have been dubbed by British media as “COVID’s odd couple,” and they don’t mind at all. Discussing their recent book, The Long COVID Handbook, the authors lean into their animated roles: Medinger is a passionate patient-researcher and “guinea pig” (his words) in search of his own healing, and Altmann is a no-nonsense, data-driven scientist and “Professor Boring” (as he puts it).
And the message they have about the impact of long COVID is stunning.
“The clinical burden [of long COVID] is somewhere on par with the whole of heart disease all over again, or the whole of oncology all over again, which are our biggest clinical bills concurrently,” Altmann said.
The pair met early in the pandemic, after Medinger became infected during the first wave and interviewed Altmann for his YouTube channel, which has more than 5 million views.
“Danny was one of the first people from the medical establishment to sort of stand up on the parapet and wave a flag and say, ‘Hey, guys, there’s a problem here.’ And that was incredibly validating for 2 million people in the U.K. alone who were suffering with long COVID,” Medinger said.
Their relationship works, not just for publishing one of the first definitive guides to long COVID, but also as a model for how patients with lived experiences can lead the way in medicine – from giving the condition its name to driving the medical establishment for recognition, clinical research, and therapeutic answers.
With Altmann currently leading a major research project at Imperial College London on long COVID and Medinger’s social media platform and communication skills, they’re both advancing the world’s understanding of the disease in their own way.
“We’re now more than 3 years into this completely mysterious, uncharted disease process with a whole globe full of really desperate people,” said Altmann. “It’s a living, organic thing, and yet that also demands some kind of order and collation and pulling together into some kind of sense. So I was very pleased when Gez approached me to help him with the book.”
In it, they translate everything they’ve learned about the condition that’s “scattered in 100,000 places around the globe” into a digestible format. It tells two sides of the same story: the anecdotal experiences Medinger has undergone or observed in the long COVID community through more than a dozen of his own patient-led studies, as well the hard science and research that’s amassing in the medical world.
In an interview,
What are the book’s key takeaways for you?
Medinger: “I would say we put together an incredibly comprehensive couple of chapters on the hypotheses, big picture, what’s causing long COVID. And then the nitty-gritty research for everything that we’ve found out that is going on. ... And the other part of the book that I think is particularly important, beyond the tips for managing symptoms, is the content on mental health and the impact on your emotional state and your capacity and just how huge that is. ... That has been the most powerful thing for patients when they’ve read it. And they’ve said that they’ve just been crying all the way through those chapters because suddenly they feel heard and seen.”
Altmann: “Obviously, you’d expect me to say that the parts of the book that I love most are the kind of hard-nosed, medical, mechanistic bits. ... We’ve got 150 million-plus desperate people deciding or not deciding to go and see their general practitioner, getting a fair hearing or not getting a fair hearing. And the poor doctor has never learned this in medical school, has never read a textbook on it, and hasn’t a clue what’s coming through the door.
How are they expected to know what to do? So I think the least we can do in some of those chapters is feed into their knowledge of general medicine and give them some clues. ... I think if we can explain to people what might be going on in them, and to their doctors, what on earth they might do about it, what kind of tests they might order, that helps a bit.”
How did you balance the more controversial parts of the book, including the chapter about so-called “treatments”? For instance, the book recounts Gez’s harrowing experience with ivermectin as a frightening warning. But Danny, you were nervous about even mentioning unproven and potentially dangerous treatments as things people have tried and have looked into.
Medinger: “We had to try and work out how to handle the topic, how to handle those points of view, whilst at the same time still being informative. I think the book is stronger for that chapter, too. The other thing would certainly have been to just not address the subject, but it’s one of the things that people want to know the most about. And there’s also a lot of bad information floating around out there about certain treatments. Ivermectin, for example, and this is what happened to me when I tried it. ‘Don’t do it. It’s not recommended. Please don’t.’
I think it was also very important to include because that cautionary tale really applies to every single one of those treatments that people might be hearing about that hasn’t been backed up by efficacy and safety studies.”
Altmann: “I think Gez has been quite diplomatic. That chapter was, I think, a testament to the power of the book. And the biggest test of our marriage as ‘the odd couple.’ Because when I first read the first draft of what Gez had written, I said, ‘my name can’t even be on this book. Otherwise, I’ll be sacked.’
And we had to find marriage counseling after that, and a way back to write a version of that chapter that expressed both halves of those concerns in a way that did justice to those different viewpoints. And I think that makes it quite a strong chapter.”
What do you think are the most urgent next steps in the search for solving long COVID?
Medinger: “I would personally like to try and get some sort of answer on viral persistence. ... If there’s one thing that feels like it would be treatable in theory, and would make sense why we’re still getting all of these symptoms this whole time later, it’s that, so I would like to try and establish or eliminate viral persistence. So if you gave me Elon Musk’s wealth, that’s what I would throw a bunch of the money at, trying to either eliminate or establish that.
And then, you know, the other important thing is a diagnostic test. Danny always talks about how important it is. Once you have that, it helps you suddenly open the doors to all these other things that you can do. And treatment trials. Let’s throw some meds at this so that we have an educated guess at what might work and put them into high-powered, randomized, controlled trials and see if anything comes out because from the patient perspective, I don’t think any of us wants to wait for 5 years for that stuff to start happening.”
Altmann: “I completely agree. If you go to a website, like clinicaltrials.gov, you’ll find an immense number of clinical trials on COVID. There isn’t really a shortage of them, some of them better-powered to get an answer than others.”
How do you think public policy needs to adapt for long COVID, including social safety nets such as workers’ compensation and disability benefits?
Medinger: “In terms of public policy, what I would like would be some public acknowledgment that it’s real from government sources. Just the acknowledgment that it’s real and it remains a risk even now.”
Altmann: “Nobody in politics asks my opinion. I think they’d hate to hear it. Because if I went to see them and said, well, actually, if you thought the COVID pandemic was bad, wait till you see what’s on the table now. We’ve created a disabled population in our country of 2 million, at least a portion if not more of people who are not fully contributory to the workforce anymore ... [with] legal wrangles about retirement and health insurance and pensions, and a human right to adequate health care. Which means, ideally, a purpose-built clinic where they can have their respiratory opinion and their rheumatology opinion and their endocrine opinion and their neurology opinion, all under one roof.”
You’ve both shown so much optimism. Why is that?
Altmann: “I’ve been an immunologist for a long time now, and written all my decades of grant applications, where as a community we made what, at the time, were kind of wild promises and wildly optimistic projections of how our knowledge of tumor immunity would revolutionize cancer care, and how knowledge of autoimmunity would revolutionize care of all the autoimmune diseases.
And weirdly almost every word we wrote over those 25 or 30 years came true. Cancer immunotherapy was revolutionized, and biologics for diabetes, multiple sclerosis, and arthritis were revolutionized. So if I have faith that those things came true, I have complete faith in this as well.”
Medinger: “From the patient perspective, what I would say is that we are seeing people who’ve been ill for more than 2 years recover. People are suddenly turning the corner when they might not have expected to.
And while we don’t quite know exactly why yet, and it’s not everyone, every single time I hear the story of someone saying, ‘I’m pretty much back to where I was, I feel like I’ve recovered,’ I feel great. Even if I haven’t. Because I know that every single time I hear someone say that, that just increases the probability that I will, too.”
A version of this article first appeared on WebMD.com.
Previously unknown viral families hide in the darnedest places
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
Malpractice risks for docs who oversee NPs or PAs
Even in states that have abolished requirements that NPs be physician-supervised, physicians may still be liable by virtue of employing the NP, according to William P. Sullivan, DO, an attorney and emergency physician in Frankfort, Ill.
Indeed, the vast majority of lawsuits against NPs and PAs name the supervising physician. According to a study of claims against NPs from 2011 to 2016, 82% of the cases also named the supervising physician.
Employed or contracted physicians assigned to supervise NPs or PAs are also affected, Dr. Sullivan said. “The employed physicians’ contract with a hospital or staffing company may require them to assist in the selection, supervision, and/or training of NPs or PAs,” he said. He added that supervisory duties may also be assigned through hospital bylaws.
“The physician is usually not paid anything extra for this work and may not be given extra time to perform it,” Dr. Sullivan said. But still, he said, that physician could be named in a lawsuit and wind up bearing some responsibility for an NP’s or PA’s mistake.
In addition to facing medical malpractice suits, Dr. Sullivan said, doctors are often sanctioned by state licensure boards for improperly supervising NPs and PAs. Licensure boards often require extensive protocols for supervision of NPs and PAs.
Yet more states are removing supervision requirements
With the addition of Kansas and New York in 2022 and California in 2023, 27 states no longer require supervision for all or most NPs. Sixteen of those states, including New York and California, have instituted progressive practice authority that requires temporary supervision of new NPs but then removes supervision after a period of 6 months to 4 years, depending on the state, for the rest of their career.
“When it comes to NP independence, the horse is already out of the barn,” Dr. Sullivan said. “It’s unlikely that states will repeal laws granting NPs independence, and in fact, more states are likely to pass them.”
*PAs, in contrast, are well behind NPs in achieving independence, but the American Academy of Physician Associates (AAPA) is calling to eliminate a mandated relationship with a specific physician. So far, Utah, North Dakota and Wyoming have ended physician supervision of PAs, while California and Hawaii have eliminated mandated chart review. Other states are considering eliminating physician supervision of PAs, according to the AAPA.
In states that have abolished oversight requirements for NPs, “liability can then shift to the NP when the NP is fully independent,” Cathy Klein, an advanced practice registered nurse who helped found the NP profession 50 years ago, told this news organization. “More NPs are starting their own practices, and in many cases, patients actually prefer to see an NP.”
As more NPs became more autonomous, the average payment that NPs incurred in professional liability lawsuits rose by 10.5% from 2017 to 2022, to $332,187, according to the Nurses Service Organization (NSO), a nursing malpractice insurer.
The number of malpractice judgments against autonomous NPs alone has also been rising. From 2012 to 2017, autonomous NPs’ share of all NP cases rose from 7% to 16.4%, the NSO reported.
The good news for physicians is that states’ removal of restrictions on NPs has reduced physicians’ liability to some extent. A 2017 study found that enacting less restrictive scope-of-practice laws for NPs decreased the number of payments made by physicians in NP cases by as much as 31%.
However, the top location for NP payouts remains the physician’s office, not the autonomous NP’s practice, according to the latter NSO report. Plaintiffs sue NPs’ and PAs’ supervising physicians on the basis of legal concepts, such as vicarious liability and respondeat superior. Even if the physician-employer never saw the patient, he or she can be held liable.
Court cases in which supervising physician was found liable
There are plenty of judgments against supervising or collaborating physicians when the NP or PA made the error. Typically, the doctor was faulted for paying little attention to the NP or PA he or she was supposed to supervise.
Dr. Sullivan points to a 2016 case in which a New York jury held a physician 40% liable for a $7 million judgment in a malpractice case involving a PA’s care of a patient in the emergency department. The case is Shajan v. South Nassau Community Hospital in New York.
“The patient presented with nontraumatic leg pain to his lower leg, was diagnosed by the PA with a muscle strain, and discharged without a physician evaluation,” Dr. Sullivan said. The next day, the patient visited an orthopedist who immediately diagnosed compartment syndrome, an emergent condition in which pressure builds up in an affected extremity, damaging the muscles and nerves. “The patient developed irreversible nerve damage and chronic regional pain syndrome,” he said.
A malpractice lawsuit named the PA and the emergency physician he was supposed to be reporting to. Even though the physician had never seen the patient, he had signed off on the PA’s note from a patient’s ED visit. “Testimony during the trial focused on hospital protocols that the supervising physician was supposed to take,” Dr. Sullivan said.
When doctors share fault, they frequently failed to follow the collaborative agreement with the NP or PA. In Collip v. Ratts, a 2015 Indiana case in which the patient died from a drug interaction, the doctor’s certified public accountant stated that the doctor was required to review at least 5% of the NP’s charts every week to evaluate her prescriptive practices.
The doctor admitted that he never reviewed the NP’s charts on a weekly basis. He did conduct some cursory reviews of some of the NP’s notes, and in them he noted concerns for her prescribing practices and suggested she attend a narcotics-prescribing seminar, but he did not follow up to make sure she had done this.
Sometimes the NP or PA who made the mistake may actually be dropped from the lawsuit, leaving the supervising physician fully liable. In these cases, courts reason that a fully engaged supervisor could have prevented the error. In the 2006 case of Husak v. Siegal, the Florida Supreme Court dropped the NP from the case, ruling that the NP had provided the supervising doctor all the information he needed in order to tell her what to do for the patient.
The court noted the physician had failed to look at the chart, even though he was required to do so under his supervisory agreement with the NP. The doctor “could have made the correct diagnosis or referral had he been attentive,” the court said. Therefore, there was “no evidence of independent negligence” by the NP, even though she was the one who had made the incorrect diagnosis that harmed the patient.
When states require an autonomous NP to have a supervisory relationship with a doctor, the supervisor may be unavailable and may fail to designate a substitute. In Texas in January 2019, a 7-year-old girl died of pneumonia after being treated by an NP in an urgent care clinic. The NP had told the parents that the child could safely go home and only needed ibuprofen. The parents brought the girl back home, and she died 15 hours later. The Wattenbargers sued the NP, and the doctor’s supervision was a topic in the trial.
The supervising physician for the NP was out of the country at the time. He said that he had found a substitute, but the substitute doctor testified she had no idea she was designated to be the substitute, according to Niran Al-Agba, MD, a family physician in Silverdale, Wash., who has written on the Texas case. Dr. Al-Agba told this news organization the case appears to have been settled confidentially.
Different standards for expert witnesses
In many states, courts do not allow physicians to testify as expert witnesses in malpractice cases against NPs, arguing that nurses have a different set of standards than doctors have, Dr. Sullivan reported.
These states include Arkansas, Illinois, North Carolina, and New York, according to a report by SEAK Inc., an expert witness training program. The report said most other states allow physician experts in these cases, but they may still require that they have experience with the nursing standard of care.
Dr. Sullivan said some courts are whittling away at the ban on physician experts, and the ban may eventually disappear. He reported that in Oklahoma, which normally upholds the ban, a judge recently allowed a physician-expert to testify in a case involving the death of a 19-year-old woman, Alexus Ochoa, in an ED staffed by an NP. The judge reasoned that Ms. Ochoa’s parents assumed the ED was staffed by physicians and would adhere to medical standards.
Supervision pointers from a physician
Physicians who supervise NPs or PAs say it is important to keep track of their skills and help them sharpen their expertise. Their scope of practice and physicians’ supervisory responsibilities are included in the collaborative agreement.
Arthur Apolinario, MD, a family physician in Clinton, N.C., says his 10-physician practice, which employs six NPs and one PA, works under a collaborative agreement. “The agreement defines each person’s scope of practice. They can’t do certain procedures, such as surgery, and they need extra training before doing certain tasks alone, such as joint injection.
“You have to always figure that if there is a lawsuit against one of them, you as the supervising physician would be named,” said Dr. Apolinario, who is also president of the North Carolina Medical Society. “We try to avert mistakes by meeting regularly with our NPs and PAs and making sure they keep up to date.”
Collaborating with autonomous NPs
Even when NPs operate independently in states that have abolished supervision, physicians may still have some liability if they give NPs advice, Dr. Al-Agba said.
At her Washington state practice, Dr. Al-Agba shares an office with an autonomous NP. “We share overhead and a front desk, but we have separate patients,” Dr. Al-Agba said. “This arrangement works very well for both of us.”
The NP sometimes asks her for advice. When this occurs, Dr. Al-Agba said she always makes sure to see the patient first. “If you don’t actually see the patient, there could be a misunderstanding that could lead to an error,” she said.
Conclusion
Even though NPs now have autonomy in most states, supervising physicians may still be liable for NP malpractice by virtue of being their employers, and physicians in the remaining states are liable for NPs through state law and for PAs in virtually all the states. To determine the supervising physician’s fault, courts often study whether the physician has met the terms of the collaborative agreement.
Physicians can reduce collaborating NPs’ and PAs’ liability by properly training them, by verifying their scope of practice, by making themselves easily available for consultation, and by occasionally seeing their patients. If their NPs and PAs do commit malpractice, supervising physicians may be able to protect themselves from liability by adhering to all requirements of the collaborative agreement.
*Correction, 4/19/2023: An earlier version of this story misstated the name of the AAPA and the states that have ended physician supervision of PAs.
A version of this article first appeared on Medscape.com.
Even in states that have abolished requirements that NPs be physician-supervised, physicians may still be liable by virtue of employing the NP, according to William P. Sullivan, DO, an attorney and emergency physician in Frankfort, Ill.
Indeed, the vast majority of lawsuits against NPs and PAs name the supervising physician. According to a study of claims against NPs from 2011 to 2016, 82% of the cases also named the supervising physician.
Employed or contracted physicians assigned to supervise NPs or PAs are also affected, Dr. Sullivan said. “The employed physicians’ contract with a hospital or staffing company may require them to assist in the selection, supervision, and/or training of NPs or PAs,” he said. He added that supervisory duties may also be assigned through hospital bylaws.
“The physician is usually not paid anything extra for this work and may not be given extra time to perform it,” Dr. Sullivan said. But still, he said, that physician could be named in a lawsuit and wind up bearing some responsibility for an NP’s or PA’s mistake.
In addition to facing medical malpractice suits, Dr. Sullivan said, doctors are often sanctioned by state licensure boards for improperly supervising NPs and PAs. Licensure boards often require extensive protocols for supervision of NPs and PAs.
Yet more states are removing supervision requirements
With the addition of Kansas and New York in 2022 and California in 2023, 27 states no longer require supervision for all or most NPs. Sixteen of those states, including New York and California, have instituted progressive practice authority that requires temporary supervision of new NPs but then removes supervision after a period of 6 months to 4 years, depending on the state, for the rest of their career.
“When it comes to NP independence, the horse is already out of the barn,” Dr. Sullivan said. “It’s unlikely that states will repeal laws granting NPs independence, and in fact, more states are likely to pass them.”
*PAs, in contrast, are well behind NPs in achieving independence, but the American Academy of Physician Associates (AAPA) is calling to eliminate a mandated relationship with a specific physician. So far, Utah, North Dakota and Wyoming have ended physician supervision of PAs, while California and Hawaii have eliminated mandated chart review. Other states are considering eliminating physician supervision of PAs, according to the AAPA.
In states that have abolished oversight requirements for NPs, “liability can then shift to the NP when the NP is fully independent,” Cathy Klein, an advanced practice registered nurse who helped found the NP profession 50 years ago, told this news organization. “More NPs are starting their own practices, and in many cases, patients actually prefer to see an NP.”
As more NPs became more autonomous, the average payment that NPs incurred in professional liability lawsuits rose by 10.5% from 2017 to 2022, to $332,187, according to the Nurses Service Organization (NSO), a nursing malpractice insurer.
The number of malpractice judgments against autonomous NPs alone has also been rising. From 2012 to 2017, autonomous NPs’ share of all NP cases rose from 7% to 16.4%, the NSO reported.
The good news for physicians is that states’ removal of restrictions on NPs has reduced physicians’ liability to some extent. A 2017 study found that enacting less restrictive scope-of-practice laws for NPs decreased the number of payments made by physicians in NP cases by as much as 31%.
However, the top location for NP payouts remains the physician’s office, not the autonomous NP’s practice, according to the latter NSO report. Plaintiffs sue NPs’ and PAs’ supervising physicians on the basis of legal concepts, such as vicarious liability and respondeat superior. Even if the physician-employer never saw the patient, he or she can be held liable.
Court cases in which supervising physician was found liable
There are plenty of judgments against supervising or collaborating physicians when the NP or PA made the error. Typically, the doctor was faulted for paying little attention to the NP or PA he or she was supposed to supervise.
Dr. Sullivan points to a 2016 case in which a New York jury held a physician 40% liable for a $7 million judgment in a malpractice case involving a PA’s care of a patient in the emergency department. The case is Shajan v. South Nassau Community Hospital in New York.
“The patient presented with nontraumatic leg pain to his lower leg, was diagnosed by the PA with a muscle strain, and discharged without a physician evaluation,” Dr. Sullivan said. The next day, the patient visited an orthopedist who immediately diagnosed compartment syndrome, an emergent condition in which pressure builds up in an affected extremity, damaging the muscles and nerves. “The patient developed irreversible nerve damage and chronic regional pain syndrome,” he said.
A malpractice lawsuit named the PA and the emergency physician he was supposed to be reporting to. Even though the physician had never seen the patient, he had signed off on the PA’s note from a patient’s ED visit. “Testimony during the trial focused on hospital protocols that the supervising physician was supposed to take,” Dr. Sullivan said.
When doctors share fault, they frequently failed to follow the collaborative agreement with the NP or PA. In Collip v. Ratts, a 2015 Indiana case in which the patient died from a drug interaction, the doctor’s certified public accountant stated that the doctor was required to review at least 5% of the NP’s charts every week to evaluate her prescriptive practices.
The doctor admitted that he never reviewed the NP’s charts on a weekly basis. He did conduct some cursory reviews of some of the NP’s notes, and in them he noted concerns for her prescribing practices and suggested she attend a narcotics-prescribing seminar, but he did not follow up to make sure she had done this.
Sometimes the NP or PA who made the mistake may actually be dropped from the lawsuit, leaving the supervising physician fully liable. In these cases, courts reason that a fully engaged supervisor could have prevented the error. In the 2006 case of Husak v. Siegal, the Florida Supreme Court dropped the NP from the case, ruling that the NP had provided the supervising doctor all the information he needed in order to tell her what to do for the patient.
The court noted the physician had failed to look at the chart, even though he was required to do so under his supervisory agreement with the NP. The doctor “could have made the correct diagnosis or referral had he been attentive,” the court said. Therefore, there was “no evidence of independent negligence” by the NP, even though she was the one who had made the incorrect diagnosis that harmed the patient.
When states require an autonomous NP to have a supervisory relationship with a doctor, the supervisor may be unavailable and may fail to designate a substitute. In Texas in January 2019, a 7-year-old girl died of pneumonia after being treated by an NP in an urgent care clinic. The NP had told the parents that the child could safely go home and only needed ibuprofen. The parents brought the girl back home, and she died 15 hours later. The Wattenbargers sued the NP, and the doctor’s supervision was a topic in the trial.
The supervising physician for the NP was out of the country at the time. He said that he had found a substitute, but the substitute doctor testified she had no idea she was designated to be the substitute, according to Niran Al-Agba, MD, a family physician in Silverdale, Wash., who has written on the Texas case. Dr. Al-Agba told this news organization the case appears to have been settled confidentially.
Different standards for expert witnesses
In many states, courts do not allow physicians to testify as expert witnesses in malpractice cases against NPs, arguing that nurses have a different set of standards than doctors have, Dr. Sullivan reported.
These states include Arkansas, Illinois, North Carolina, and New York, according to a report by SEAK Inc., an expert witness training program. The report said most other states allow physician experts in these cases, but they may still require that they have experience with the nursing standard of care.
Dr. Sullivan said some courts are whittling away at the ban on physician experts, and the ban may eventually disappear. He reported that in Oklahoma, which normally upholds the ban, a judge recently allowed a physician-expert to testify in a case involving the death of a 19-year-old woman, Alexus Ochoa, in an ED staffed by an NP. The judge reasoned that Ms. Ochoa’s parents assumed the ED was staffed by physicians and would adhere to medical standards.
Supervision pointers from a physician
Physicians who supervise NPs or PAs say it is important to keep track of their skills and help them sharpen their expertise. Their scope of practice and physicians’ supervisory responsibilities are included in the collaborative agreement.
Arthur Apolinario, MD, a family physician in Clinton, N.C., says his 10-physician practice, which employs six NPs and one PA, works under a collaborative agreement. “The agreement defines each person’s scope of practice. They can’t do certain procedures, such as surgery, and they need extra training before doing certain tasks alone, such as joint injection.
“You have to always figure that if there is a lawsuit against one of them, you as the supervising physician would be named,” said Dr. Apolinario, who is also president of the North Carolina Medical Society. “We try to avert mistakes by meeting regularly with our NPs and PAs and making sure they keep up to date.”
Collaborating with autonomous NPs
Even when NPs operate independently in states that have abolished supervision, physicians may still have some liability if they give NPs advice, Dr. Al-Agba said.
At her Washington state practice, Dr. Al-Agba shares an office with an autonomous NP. “We share overhead and a front desk, but we have separate patients,” Dr. Al-Agba said. “This arrangement works very well for both of us.”
The NP sometimes asks her for advice. When this occurs, Dr. Al-Agba said she always makes sure to see the patient first. “If you don’t actually see the patient, there could be a misunderstanding that could lead to an error,” she said.
Conclusion
Even though NPs now have autonomy in most states, supervising physicians may still be liable for NP malpractice by virtue of being their employers, and physicians in the remaining states are liable for NPs through state law and for PAs in virtually all the states. To determine the supervising physician’s fault, courts often study whether the physician has met the terms of the collaborative agreement.
Physicians can reduce collaborating NPs’ and PAs’ liability by properly training them, by verifying their scope of practice, by making themselves easily available for consultation, and by occasionally seeing their patients. If their NPs and PAs do commit malpractice, supervising physicians may be able to protect themselves from liability by adhering to all requirements of the collaborative agreement.
*Correction, 4/19/2023: An earlier version of this story misstated the name of the AAPA and the states that have ended physician supervision of PAs.
A version of this article first appeared on Medscape.com.
Even in states that have abolished requirements that NPs be physician-supervised, physicians may still be liable by virtue of employing the NP, according to William P. Sullivan, DO, an attorney and emergency physician in Frankfort, Ill.
Indeed, the vast majority of lawsuits against NPs and PAs name the supervising physician. According to a study of claims against NPs from 2011 to 2016, 82% of the cases also named the supervising physician.
Employed or contracted physicians assigned to supervise NPs or PAs are also affected, Dr. Sullivan said. “The employed physicians’ contract with a hospital or staffing company may require them to assist in the selection, supervision, and/or training of NPs or PAs,” he said. He added that supervisory duties may also be assigned through hospital bylaws.
“The physician is usually not paid anything extra for this work and may not be given extra time to perform it,” Dr. Sullivan said. But still, he said, that physician could be named in a lawsuit and wind up bearing some responsibility for an NP’s or PA’s mistake.
In addition to facing medical malpractice suits, Dr. Sullivan said, doctors are often sanctioned by state licensure boards for improperly supervising NPs and PAs. Licensure boards often require extensive protocols for supervision of NPs and PAs.
Yet more states are removing supervision requirements
With the addition of Kansas and New York in 2022 and California in 2023, 27 states no longer require supervision for all or most NPs. Sixteen of those states, including New York and California, have instituted progressive practice authority that requires temporary supervision of new NPs but then removes supervision after a period of 6 months to 4 years, depending on the state, for the rest of their career.
“When it comes to NP independence, the horse is already out of the barn,” Dr. Sullivan said. “It’s unlikely that states will repeal laws granting NPs independence, and in fact, more states are likely to pass them.”
*PAs, in contrast, are well behind NPs in achieving independence, but the American Academy of Physician Associates (AAPA) is calling to eliminate a mandated relationship with a specific physician. So far, Utah, North Dakota and Wyoming have ended physician supervision of PAs, while California and Hawaii have eliminated mandated chart review. Other states are considering eliminating physician supervision of PAs, according to the AAPA.
In states that have abolished oversight requirements for NPs, “liability can then shift to the NP when the NP is fully independent,” Cathy Klein, an advanced practice registered nurse who helped found the NP profession 50 years ago, told this news organization. “More NPs are starting their own practices, and in many cases, patients actually prefer to see an NP.”
As more NPs became more autonomous, the average payment that NPs incurred in professional liability lawsuits rose by 10.5% from 2017 to 2022, to $332,187, according to the Nurses Service Organization (NSO), a nursing malpractice insurer.
The number of malpractice judgments against autonomous NPs alone has also been rising. From 2012 to 2017, autonomous NPs’ share of all NP cases rose from 7% to 16.4%, the NSO reported.
The good news for physicians is that states’ removal of restrictions on NPs has reduced physicians’ liability to some extent. A 2017 study found that enacting less restrictive scope-of-practice laws for NPs decreased the number of payments made by physicians in NP cases by as much as 31%.
However, the top location for NP payouts remains the physician’s office, not the autonomous NP’s practice, according to the latter NSO report. Plaintiffs sue NPs’ and PAs’ supervising physicians on the basis of legal concepts, such as vicarious liability and respondeat superior. Even if the physician-employer never saw the patient, he or she can be held liable.
Court cases in which supervising physician was found liable
There are plenty of judgments against supervising or collaborating physicians when the NP or PA made the error. Typically, the doctor was faulted for paying little attention to the NP or PA he or she was supposed to supervise.
Dr. Sullivan points to a 2016 case in which a New York jury held a physician 40% liable for a $7 million judgment in a malpractice case involving a PA’s care of a patient in the emergency department. The case is Shajan v. South Nassau Community Hospital in New York.
“The patient presented with nontraumatic leg pain to his lower leg, was diagnosed by the PA with a muscle strain, and discharged without a physician evaluation,” Dr. Sullivan said. The next day, the patient visited an orthopedist who immediately diagnosed compartment syndrome, an emergent condition in which pressure builds up in an affected extremity, damaging the muscles and nerves. “The patient developed irreversible nerve damage and chronic regional pain syndrome,” he said.
A malpractice lawsuit named the PA and the emergency physician he was supposed to be reporting to. Even though the physician had never seen the patient, he had signed off on the PA’s note from a patient’s ED visit. “Testimony during the trial focused on hospital protocols that the supervising physician was supposed to take,” Dr. Sullivan said.
When doctors share fault, they frequently failed to follow the collaborative agreement with the NP or PA. In Collip v. Ratts, a 2015 Indiana case in which the patient died from a drug interaction, the doctor’s certified public accountant stated that the doctor was required to review at least 5% of the NP’s charts every week to evaluate her prescriptive practices.
The doctor admitted that he never reviewed the NP’s charts on a weekly basis. He did conduct some cursory reviews of some of the NP’s notes, and in them he noted concerns for her prescribing practices and suggested she attend a narcotics-prescribing seminar, but he did not follow up to make sure she had done this.
Sometimes the NP or PA who made the mistake may actually be dropped from the lawsuit, leaving the supervising physician fully liable. In these cases, courts reason that a fully engaged supervisor could have prevented the error. In the 2006 case of Husak v. Siegal, the Florida Supreme Court dropped the NP from the case, ruling that the NP had provided the supervising doctor all the information he needed in order to tell her what to do for the patient.
The court noted the physician had failed to look at the chart, even though he was required to do so under his supervisory agreement with the NP. The doctor “could have made the correct diagnosis or referral had he been attentive,” the court said. Therefore, there was “no evidence of independent negligence” by the NP, even though she was the one who had made the incorrect diagnosis that harmed the patient.
When states require an autonomous NP to have a supervisory relationship with a doctor, the supervisor may be unavailable and may fail to designate a substitute. In Texas in January 2019, a 7-year-old girl died of pneumonia after being treated by an NP in an urgent care clinic. The NP had told the parents that the child could safely go home and only needed ibuprofen. The parents brought the girl back home, and she died 15 hours later. The Wattenbargers sued the NP, and the doctor’s supervision was a topic in the trial.
The supervising physician for the NP was out of the country at the time. He said that he had found a substitute, but the substitute doctor testified she had no idea she was designated to be the substitute, according to Niran Al-Agba, MD, a family physician in Silverdale, Wash., who has written on the Texas case. Dr. Al-Agba told this news organization the case appears to have been settled confidentially.
Different standards for expert witnesses
In many states, courts do not allow physicians to testify as expert witnesses in malpractice cases against NPs, arguing that nurses have a different set of standards than doctors have, Dr. Sullivan reported.
These states include Arkansas, Illinois, North Carolina, and New York, according to a report by SEAK Inc., an expert witness training program. The report said most other states allow physician experts in these cases, but they may still require that they have experience with the nursing standard of care.
Dr. Sullivan said some courts are whittling away at the ban on physician experts, and the ban may eventually disappear. He reported that in Oklahoma, which normally upholds the ban, a judge recently allowed a physician-expert to testify in a case involving the death of a 19-year-old woman, Alexus Ochoa, in an ED staffed by an NP. The judge reasoned that Ms. Ochoa’s parents assumed the ED was staffed by physicians and would adhere to medical standards.
Supervision pointers from a physician
Physicians who supervise NPs or PAs say it is important to keep track of their skills and help them sharpen their expertise. Their scope of practice and physicians’ supervisory responsibilities are included in the collaborative agreement.
Arthur Apolinario, MD, a family physician in Clinton, N.C., says his 10-physician practice, which employs six NPs and one PA, works under a collaborative agreement. “The agreement defines each person’s scope of practice. They can’t do certain procedures, such as surgery, and they need extra training before doing certain tasks alone, such as joint injection.
“You have to always figure that if there is a lawsuit against one of them, you as the supervising physician would be named,” said Dr. Apolinario, who is also president of the North Carolina Medical Society. “We try to avert mistakes by meeting regularly with our NPs and PAs and making sure they keep up to date.”
Collaborating with autonomous NPs
Even when NPs operate independently in states that have abolished supervision, physicians may still have some liability if they give NPs advice, Dr. Al-Agba said.
At her Washington state practice, Dr. Al-Agba shares an office with an autonomous NP. “We share overhead and a front desk, but we have separate patients,” Dr. Al-Agba said. “This arrangement works very well for both of us.”
The NP sometimes asks her for advice. When this occurs, Dr. Al-Agba said she always makes sure to see the patient first. “If you don’t actually see the patient, there could be a misunderstanding that could lead to an error,” she said.
Conclusion
Even though NPs now have autonomy in most states, supervising physicians may still be liable for NP malpractice by virtue of being their employers, and physicians in the remaining states are liable for NPs through state law and for PAs in virtually all the states. To determine the supervising physician’s fault, courts often study whether the physician has met the terms of the collaborative agreement.
Physicians can reduce collaborating NPs’ and PAs’ liability by properly training them, by verifying their scope of practice, by making themselves easily available for consultation, and by occasionally seeing their patients. If their NPs and PAs do commit malpractice, supervising physicians may be able to protect themselves from liability by adhering to all requirements of the collaborative agreement.
*Correction, 4/19/2023: An earlier version of this story misstated the name of the AAPA and the states that have ended physician supervision of PAs.
A version of this article first appeared on Medscape.com.