User login
Resuming DOAC therapy in AF patients after gastrointestinal bleed
Clinical question: For patients who develop a gastrointestinal bleed (GIB) while using direct oral anticoagulant (DOAC) therapy for atrial fibrillation (AF), does the risk of venous thromboembolism (VTE) or recurrent GIB increase after DOAC resumption?
Background: DOACs are increasingly used for stroke prophylaxis in nonvalvular AF and can increase the risk of GIB by 30% compared to warfarin. Although warfarin can be safely resumed within 14 days of GIB cessation, outcomes related to resuming DOAC therapy after hospitalization for GIB are lacking.
Study design: Retrospective analysis of claims data.
Setting: Patients with AF on DOAC therapy admitted for acute GIB in Michigan.
Synopsis: 1,338 adults, median age 79 years, on a DOAC for AF were hospitalized for GIB. After the index hospitalization, patients were followed for resumption of DOAC (defined by new prescription fill), recurrent bleeding, and VTE. 62% of patients resumed DOAC therapy.
Resuming a DOAC within 30 days did not lead to a statistically significant difference in VTE or recurrence of GIB at 90 days or 6 months. However, at 90 days recurrent GIB risk increased with concomitant use of antiplatelet agents (hazard ratio, 3.12; 95% confidence interval, 1.55-5.81; P = .002). Rivaroxaban had higher rates of rebleeding events, compared with the other DOACs (P = .04). History of VTE increased the risk for postdischarge VTE. Key limitations included lack of cerebrovascular accident rates, exclusion of patients who switched from DOAC to warfarin, and uncertainty surrounding the timing of actual DOAC resumption.
Bottom line: DOAC resumption within 30 days of GIB did not increase VTE or recurrent GIB, but concurrent antiplatelet agent use increased recurrent GIB rates.
Citation: Sengupta N et al. Rebleeding vs. thromboembolism after hospitalization for gastrointestinal bleeding in patients on direct oral anticoagulants. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.05.005.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: For patients who develop a gastrointestinal bleed (GIB) while using direct oral anticoagulant (DOAC) therapy for atrial fibrillation (AF), does the risk of venous thromboembolism (VTE) or recurrent GIB increase after DOAC resumption?
Background: DOACs are increasingly used for stroke prophylaxis in nonvalvular AF and can increase the risk of GIB by 30% compared to warfarin. Although warfarin can be safely resumed within 14 days of GIB cessation, outcomes related to resuming DOAC therapy after hospitalization for GIB are lacking.
Study design: Retrospective analysis of claims data.
Setting: Patients with AF on DOAC therapy admitted for acute GIB in Michigan.
Synopsis: 1,338 adults, median age 79 years, on a DOAC for AF were hospitalized for GIB. After the index hospitalization, patients were followed for resumption of DOAC (defined by new prescription fill), recurrent bleeding, and VTE. 62% of patients resumed DOAC therapy.
Resuming a DOAC within 30 days did not lead to a statistically significant difference in VTE or recurrence of GIB at 90 days or 6 months. However, at 90 days recurrent GIB risk increased with concomitant use of antiplatelet agents (hazard ratio, 3.12; 95% confidence interval, 1.55-5.81; P = .002). Rivaroxaban had higher rates of rebleeding events, compared with the other DOACs (P = .04). History of VTE increased the risk for postdischarge VTE. Key limitations included lack of cerebrovascular accident rates, exclusion of patients who switched from DOAC to warfarin, and uncertainty surrounding the timing of actual DOAC resumption.
Bottom line: DOAC resumption within 30 days of GIB did not increase VTE or recurrent GIB, but concurrent antiplatelet agent use increased recurrent GIB rates.
Citation: Sengupta N et al. Rebleeding vs. thromboembolism after hospitalization for gastrointestinal bleeding in patients on direct oral anticoagulants. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.05.005.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: For patients who develop a gastrointestinal bleed (GIB) while using direct oral anticoagulant (DOAC) therapy for atrial fibrillation (AF), does the risk of venous thromboembolism (VTE) or recurrent GIB increase after DOAC resumption?
Background: DOACs are increasingly used for stroke prophylaxis in nonvalvular AF and can increase the risk of GIB by 30% compared to warfarin. Although warfarin can be safely resumed within 14 days of GIB cessation, outcomes related to resuming DOAC therapy after hospitalization for GIB are lacking.
Study design: Retrospective analysis of claims data.
Setting: Patients with AF on DOAC therapy admitted for acute GIB in Michigan.
Synopsis: 1,338 adults, median age 79 years, on a DOAC for AF were hospitalized for GIB. After the index hospitalization, patients were followed for resumption of DOAC (defined by new prescription fill), recurrent bleeding, and VTE. 62% of patients resumed DOAC therapy.
Resuming a DOAC within 30 days did not lead to a statistically significant difference in VTE or recurrence of GIB at 90 days or 6 months. However, at 90 days recurrent GIB risk increased with concomitant use of antiplatelet agents (hazard ratio, 3.12; 95% confidence interval, 1.55-5.81; P = .002). Rivaroxaban had higher rates of rebleeding events, compared with the other DOACs (P = .04). History of VTE increased the risk for postdischarge VTE. Key limitations included lack of cerebrovascular accident rates, exclusion of patients who switched from DOAC to warfarin, and uncertainty surrounding the timing of actual DOAC resumption.
Bottom line: DOAC resumption within 30 days of GIB did not increase VTE or recurrent GIB, but concurrent antiplatelet agent use increased recurrent GIB rates.
Citation: Sengupta N et al. Rebleeding vs. thromboembolism after hospitalization for gastrointestinal bleeding in patients on direct oral anticoagulants. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2018.05.005.
Dr. Naderi is assistant professor in the division of hospital medicine, University of Colorado, Denver.
New pediatric therapies show promise for influenza, multidrug-resistant pathogens
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
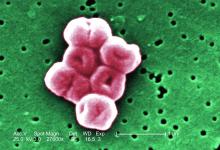
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
ORLANDO – John S. Bradley, MD, said at the annual meeting of the American Academy of Pediatrics.
Dr. Bradley, director of the division of infectious diseases at Rady Children’s Hospital–San Diego, discussed a therapy for influenza, baloxavir, which was recently approved as a fast-acting single-dose medication and currently is under study in children. Also, a recent double-blind, phase 3 trial in the New England Journal of Medicine recruited patients as young as 12 years old. In the study, patients in the intervention group resolved their fever in median 25 hours, compared with 42 hours in the placebo group. Baloxavir better reduced viral load at day 2, compared with oseltamivir and placebo, but there was a similar alleviation of symptoms between both groups. There was a greater incidence of nausea and vomiting among the oseltamivir group, while the baloxavir group had a higher rate of diarrhea (N Engl J Med 2018;379:913-23).
However, Dr. Bradley noted baloxavir is much more expensive than oseltamivir, which may not justify the better tolerance of the drug for influenza treatment.
You don’t get better with it faster, so I’m not going to be recommending you all run to baloxavir this flu season for kids 12 years of age and older,” Dr. Bradley said. “I think oseltamivir is still fine, unless we end up with oseltamivir resistance.”
Solithromycin, an intravenous and oral fluoroketolide, has shown promising results against gram-positive and gram-negative pathogens for community-acquired pneumonia and other infections. During the drug’s study period, Cempra sold solithromycin to Melinta. However, one trial showed elevated liver functions in a higher number of patients than expected, and the Food and Drug Administration asked Melinta to conduct additional studies. Investigations on solithromycin have currently stopped until Melinta secures funding. “Until they get better resources, this particular drug is on hold, but you’ll see it again, I’m sure,” said Dr. Bradley, who also is professor and chief of the division of infectious diseases at the University of California, San Diego.
Dr. Bradley also discussed the efficacy of tedizolid, a protein synthesis inhibitor similar to linezolid approved in adults for the treatment of skin infections. He noted tedizolid is more active than linezolid, but the treatment course is a shorter dose for a shorter amount of time. Compared with linezolid, which can cause thrombocytopenia or neutropenia if taken for more than 10 days to 14 days, there also are fewer side effects.
“The tedizolid is much, much safer,” Dr. Bradley said, who added that trials for efficacy of tedizolid are currently underway in pediatric patients. “We’re hoping that will end up being the pediatric oxazolidinone.”
Other investigative therapies approved for adults and under study for use in children include ceftazidime/avibactam for treatment of urinary tract and complicated intra-abdominal infections, which is effective against meropenem-resistant Enterobacteriaceae and resistant Escherichia coli with extended-spectrum beta-lactamases (ESBL); ceftolozane/tazobactam has also been approved for adults, is pending approval in pediatric patients, and is active against ESBLs such as Pseudomonas; and meropenem/vaborbactam, which is active against Klebsiella pneumoniae carbapenemase (KPC)–producing isolates. Plazomicin, an aminoglycoside similar to gentamicin used to treat KPC-producing isolates, is stable against enzymes that degrade gentamicin and tobramycin.
Therapies currently under study for adults and being considered for children include imipenem/relebactam for treatment against E. coli, Enterobacter species, and KPC-producing isolates, and cefiderocol, a siderophore cephalosporin antibiotic – commonly described as a “Trojan horse” antibiotic because it binds to iron and is actively transported into the organism – is effective against Pseudomonas and has finished phase 2 trials in adults, with researchers looking to do single-dose trials in children, Dr. Bradley noted.
More experimentally, phage therapy for multidrug-resistant Acinetobacter baumannii proved effective in a 68-year-old patient with necrotizing pancreatitis who continued to deteriorate over a 4-month period despite multiple courses of antibiotics and attempted drainage of a pancreatic pseudocyst. Researchers selected a phage-specific bacterium with specificity for A. baumannii and cured him. “This is like science fiction,” Dr. Bradley said.
Dr. Bradley reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 18
Preop anemia management saves blood, costs
BOSTON – A pilot anemia optimization program resulted in significant increases in day-of-surgery hemoglobin levels and reductions in RBC transfusion rates and costs in one center, but whether patient outcomes also improved is still not known.
By diagnosing anemia at the preanesthesia visit and providing anemic patients with dietary guidance and supplementation prior to cardiac surgery, blood program managers noticed a more than $360 reduction in per-patient blood-product acquisition costs, a more than $1,800 average reduction per patient in transfusion costs, and overall cost savings of more than $100,000 over 18 months, compared with historical data.
The findings were reported by Christine M. Cahill, RN, from Strong Memorial Hospital in Rochester, N.Y., and the University of Rochester (N.Y.), at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
“Anemia has been thought of as a relatively benign thing our patients live with traditionally, but what we have been finding lately is that anemia is actually more serious than we once thought, and is an independent risk factor for hospitalization, readmission, increased patient length of stay, loss of function, and diminished quality of life,” she said.
Anemia also increases the likelihood that a patient will require allogeneic transfusions and is an independent risk factor for morbidity and mortality, she added.
The pilot program, which ran from February 2016 to September 2017, was designed to test the feasibility of diagnosing anemia during a cardiology consult visit and implementing a management plan.
During the study period, 240 patients presenting for elective cardiac surgery were screened for anemia, and 58 were diagnosed as anemic, defined as a hemoglobin level of less than 12 g/dL. These patients were referred for anemia work-ups, which found that 33 patients had iron-deficient anemia and 25 had anemia from other causes. Controls were patients who underwent cardiac surgery from March to July 2015, matched by age, sex, and procedures.
Treatments for iron-deficient patients included oral iron (7 patients), intravenous iron with or without folate (20 patients), or oral folate with or without vitamin B12 (5 patients). One iron-deficient patient could not have surgery delayed for anemia management.
Of the iron-replete patients, one received oral iron and 17 received folate plus or minus vitamin B12. The remaining seven iron-replete patients were not treated for anemia.
One iron-deficient patient had a reaction to the infusion and did not receive a scheduled second dose due to the need for immediate surgery. A second patient scheduled for intravenous iron and folate broke an arm and therefore missed an intravenous infusion appointment. No other complications or reactions occurred.
Intraoperative transfusion units used in the anemia management group totaled 10, compared with 68 for controls. Postoperative transfusion units used were also significantly lower following anemia management at 13 versus 122, respectively.
The rate of RBC transfusions among patients with anemia management was 24%, compared with 60% for controls (P less than .0001). Patients in the management program also had significantly higher day-of-surgery hemoglobin, at 11.01 g/dL versus 10.16 g/dL (P less than .001), and less RBC utilization, at an average 0.40 units per patient versus 2.07 for controls (P less than .0001).
The average per patient savings in acquisition costs was $367.40, the average transfusion cost saving was $1,837, and the total cost savings over the life of the pilot program was $106,546.
The keys to success for similar programs is “to make sure you do your homework,” Ms. Cahill said. Specifically, she recommended feasibility studies, evaluation of the potential impact of infusions on the service, work flow analyses, and cost analyses. It’s also important to get high-level administrative support as well as buy-in from surgeons and patients.
Future studies should include assessment of patient outcomes, safety, and length of ICU and hospital stay, she emphasized.
The study was internally funded. Ms. Cahill reported having no conflicts of interest.
SOURCE: Cahill CM et al. AABB 2018, Abstract PBM4-ST4-22.
BOSTON – A pilot anemia optimization program resulted in significant increases in day-of-surgery hemoglobin levels and reductions in RBC transfusion rates and costs in one center, but whether patient outcomes also improved is still not known.
By diagnosing anemia at the preanesthesia visit and providing anemic patients with dietary guidance and supplementation prior to cardiac surgery, blood program managers noticed a more than $360 reduction in per-patient blood-product acquisition costs, a more than $1,800 average reduction per patient in transfusion costs, and overall cost savings of more than $100,000 over 18 months, compared with historical data.
The findings were reported by Christine M. Cahill, RN, from Strong Memorial Hospital in Rochester, N.Y., and the University of Rochester (N.Y.), at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
“Anemia has been thought of as a relatively benign thing our patients live with traditionally, but what we have been finding lately is that anemia is actually more serious than we once thought, and is an independent risk factor for hospitalization, readmission, increased patient length of stay, loss of function, and diminished quality of life,” she said.
Anemia also increases the likelihood that a patient will require allogeneic transfusions and is an independent risk factor for morbidity and mortality, she added.
The pilot program, which ran from February 2016 to September 2017, was designed to test the feasibility of diagnosing anemia during a cardiology consult visit and implementing a management plan.
During the study period, 240 patients presenting for elective cardiac surgery were screened for anemia, and 58 were diagnosed as anemic, defined as a hemoglobin level of less than 12 g/dL. These patients were referred for anemia work-ups, which found that 33 patients had iron-deficient anemia and 25 had anemia from other causes. Controls were patients who underwent cardiac surgery from March to July 2015, matched by age, sex, and procedures.
Treatments for iron-deficient patients included oral iron (7 patients), intravenous iron with or without folate (20 patients), or oral folate with or without vitamin B12 (5 patients). One iron-deficient patient could not have surgery delayed for anemia management.
Of the iron-replete patients, one received oral iron and 17 received folate plus or minus vitamin B12. The remaining seven iron-replete patients were not treated for anemia.
One iron-deficient patient had a reaction to the infusion and did not receive a scheduled second dose due to the need for immediate surgery. A second patient scheduled for intravenous iron and folate broke an arm and therefore missed an intravenous infusion appointment. No other complications or reactions occurred.
Intraoperative transfusion units used in the anemia management group totaled 10, compared with 68 for controls. Postoperative transfusion units used were also significantly lower following anemia management at 13 versus 122, respectively.
The rate of RBC transfusions among patients with anemia management was 24%, compared with 60% for controls (P less than .0001). Patients in the management program also had significantly higher day-of-surgery hemoglobin, at 11.01 g/dL versus 10.16 g/dL (P less than .001), and less RBC utilization, at an average 0.40 units per patient versus 2.07 for controls (P less than .0001).
The average per patient savings in acquisition costs was $367.40, the average transfusion cost saving was $1,837, and the total cost savings over the life of the pilot program was $106,546.
The keys to success for similar programs is “to make sure you do your homework,” Ms. Cahill said. Specifically, she recommended feasibility studies, evaluation of the potential impact of infusions on the service, work flow analyses, and cost analyses. It’s also important to get high-level administrative support as well as buy-in from surgeons and patients.
Future studies should include assessment of patient outcomes, safety, and length of ICU and hospital stay, she emphasized.
The study was internally funded. Ms. Cahill reported having no conflicts of interest.
SOURCE: Cahill CM et al. AABB 2018, Abstract PBM4-ST4-22.
BOSTON – A pilot anemia optimization program resulted in significant increases in day-of-surgery hemoglobin levels and reductions in RBC transfusion rates and costs in one center, but whether patient outcomes also improved is still not known.
By diagnosing anemia at the preanesthesia visit and providing anemic patients with dietary guidance and supplementation prior to cardiac surgery, blood program managers noticed a more than $360 reduction in per-patient blood-product acquisition costs, a more than $1,800 average reduction per patient in transfusion costs, and overall cost savings of more than $100,000 over 18 months, compared with historical data.
The findings were reported by Christine M. Cahill, RN, from Strong Memorial Hospital in Rochester, N.Y., and the University of Rochester (N.Y.), at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
“Anemia has been thought of as a relatively benign thing our patients live with traditionally, but what we have been finding lately is that anemia is actually more serious than we once thought, and is an independent risk factor for hospitalization, readmission, increased patient length of stay, loss of function, and diminished quality of life,” she said.
Anemia also increases the likelihood that a patient will require allogeneic transfusions and is an independent risk factor for morbidity and mortality, she added.
The pilot program, which ran from February 2016 to September 2017, was designed to test the feasibility of diagnosing anemia during a cardiology consult visit and implementing a management plan.
During the study period, 240 patients presenting for elective cardiac surgery were screened for anemia, and 58 were diagnosed as anemic, defined as a hemoglobin level of less than 12 g/dL. These patients were referred for anemia work-ups, which found that 33 patients had iron-deficient anemia and 25 had anemia from other causes. Controls were patients who underwent cardiac surgery from March to July 2015, matched by age, sex, and procedures.
Treatments for iron-deficient patients included oral iron (7 patients), intravenous iron with or without folate (20 patients), or oral folate with or without vitamin B12 (5 patients). One iron-deficient patient could not have surgery delayed for anemia management.
Of the iron-replete patients, one received oral iron and 17 received folate plus or minus vitamin B12. The remaining seven iron-replete patients were not treated for anemia.
One iron-deficient patient had a reaction to the infusion and did not receive a scheduled second dose due to the need for immediate surgery. A second patient scheduled for intravenous iron and folate broke an arm and therefore missed an intravenous infusion appointment. No other complications or reactions occurred.
Intraoperative transfusion units used in the anemia management group totaled 10, compared with 68 for controls. Postoperative transfusion units used were also significantly lower following anemia management at 13 versus 122, respectively.
The rate of RBC transfusions among patients with anemia management was 24%, compared with 60% for controls (P less than .0001). Patients in the management program also had significantly higher day-of-surgery hemoglobin, at 11.01 g/dL versus 10.16 g/dL (P less than .001), and less RBC utilization, at an average 0.40 units per patient versus 2.07 for controls (P less than .0001).
The average per patient savings in acquisition costs was $367.40, the average transfusion cost saving was $1,837, and the total cost savings over the life of the pilot program was $106,546.
The keys to success for similar programs is “to make sure you do your homework,” Ms. Cahill said. Specifically, she recommended feasibility studies, evaluation of the potential impact of infusions on the service, work flow analyses, and cost analyses. It’s also important to get high-level administrative support as well as buy-in from surgeons and patients.
Future studies should include assessment of patient outcomes, safety, and length of ICU and hospital stay, she emphasized.
The study was internally funded. Ms. Cahill reported having no conflicts of interest.
SOURCE: Cahill CM et al. AABB 2018, Abstract PBM4-ST4-22.
REPORTING FROM AABB 2018
Key clinical point:
Major finding: The total cost savings over the life of a pilot anemia management program was $106,546.
Study details: A case-control study with 58 patients scheduled for elective cardiac surgery and matched historical controls.
Disclosures: The study was internally funded. Ms. Cahill reported having no conflicts of interest.
Source: Cahill CM et al. AABB 2018, Abstract PBM4-ST4-22.
Children are vulnerable to diseases emerging because of climate change
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
ORLANDO – “Expect the unexpected” when considering the health impacts of climate change on children, Susan Pacheo, MD, advised in her presentation at the annual meeting of the American Academy of Pediatrics.
“We don’t know what we’re going to see, and we need to be ready,” said Dr. Pacheo of the University of Texas, Houston.
Climate change is categorized by an increase in droughts, fires, storms, floods, mudslides, and extreme temperatures. According to the Centers for Disease Control and Prevention, the impacts of climate change on human health are multiple, but can include an increased rate of infectious disease, respiratory conditions, injury, cardiovascular-related health issues, malnutrition, and mental health problems.
These problems can especially target children, Dr. Pacheo noted. “Kids are vulnerable. You’ve heard this, you’ve experienced this, you see this every day in your pediatric population.”
Children are more vulnerable because of the increased exposure they have to the environment. They spend more time outdoors, they are closer to the ground, and they are likely to put objects in their mouth. Children also tend to swallow more water when swimming, compared with adults. A 2014 study by de Man et al. found that children exposed to storm sewers and combined sewers swallowed 1.7 mL of water per exposure event and that the risk of infection from pathogens such as noroviruses, enteroviruses, Campylobacter jejuni, Cryptosporidium, and Giardia was 23%-33% per event, compared with 0.016 mL of water per exposure in adults and a mean infection risk of 0.58%-3.90% per event (Water Research. 2014 Jan 1. doi: 10.1016/j.watres.2013.09.022).
In addition, socioeconomic status and built environment as well as a child’s immature lung development and higher respiratory rate can lead to children being impacted by factors such as air pollution. Poverty, access to medical care, and the structure and dynamics of family also can affect children.
“We need to do something because this is a problem of social justice and we, as pediatricians, are advocates of the vulnerable,” Dr. Pacheo said.
Expect to see an increase in the number of vector-borne, airborne, and pollution-related disease, as well as water- and food-borne diseases, as a result of climate change, in addition to other issues such as hand, foot, and mouth disease and antibiotic resistance, she noted. As historically colder parts of the world continue to have milder winters, disease-carrying insects such as ticks and mosquitoes will expand their habitats and transmission of diseases such as Zika virus, malaria, dengue fever, and chikungunya will increase.
Leptospirosis and Naegleria fowleri, the latter which can cause primary amebic meningoencephalitis, are also becoming more common. Food-borne illnesses like vibriosis are being seen in more northern areas of the world like Alaska, and ciguatera fish poisoning is expected to be more prevalent in the southeastern United States and Gulf of Mexico, Dr. Pacheo said.
Air pollution carries a risk of respiratory diseases, pneumonia, and bronchiolitis, with a 2017 systematic review by Nhung et al. finding increased exposure to ambient air pollution markers such as sulfur dioxide, ozone, nitrogen dioxide, and carbon monoxide was associated with pneumonia in children (Environ Pollut. 2017 Jul 25. doi: 10.1016/j.envpol.2017.07.063). Coccidioidomycosis, or valley fever, is caused by inhaling a fungus in the soil and is associated with dust storms primarily in the southwestern United States. Warmer temperatures also have caused toxic algae blooms that have killed marine life and caused respiratory distress; children should not go near or play in water when algae blooms are growing, she noted.
Recent studies have linked an increase in temperature with incidence of Escherichia coli, with a 2016 study by Philipsborn et al. showing a 1° Celsius increase in mean monthly temperature was associated with an 8% increase in incidence of diarrheagenic E. coli (J Infect Dis. 2016 Feb 29. doi: 10.1093/infdis/jiw081). The incidence of hand, foot, and mouth disease also is linked to temperature and humidity, with a 2018 study by Cheng et al. showing a 1° Celsius increase in temperature and humidity was significantly associated with hand, foot, and mouth disease (Sci Total Environ. 2018 Jan 12. doi: 10.1016/j.scitotenv.2018.01.006). Rates of influenza are controlled by the changing environment as well, and increasing the number of vaccinations will help lower the number of influenza cases.
“We need to be advocates, we need to educate ourselves like we’re doing now so that we can educate our patients and to create a plan for preparedness,” Dr. Pacheo said.
She reported no relevant conflicts of interest.
EXPERT ANALYSIS FROM AAP 2018
Dialysis decision in elderly needs to factor in comorbidities
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
SAN DIEGO – The wider picture of the patient’s health and prognosis, not just chronologic age, should enter into the clinical decision to initiate dialysis, according to Bjorg Thorsteinsdottir, MD, a palliative care physician at the Mayo Clinic in Rochester, Minn.
“People perceive they have no choice [but treatment], and we perceive we have to do things to them until everything is lost, then we expect them to do a 180 [degree turn],” she said in a presentation at the meeting sponsored by the American Society of Nephrology.
“A 90-year-old fit individual, with minimal comorbidity living independently, would absolutely be a good candidate for dialysis, while a 75-year-old patient with bad peripheral vascular disease and dementia, living in a nursing home, would be unlikely to live longer on dialysis than off dialysis,” she said. “We need to weigh the risks and benefits for each individual patient against their goals and values. We need to be honest about the lack of benefit for certain subgroups of patients and the heavy treatment burdens of dialysis. Age, comorbidity, and frailty all factor into these deliberations and prognosis.”
More than 107,000 people over age 75 in the United States received dialysis in 2015, according to statistics gathered by the National Kidney Foundation. Yet the survival advantage of dialysis is more limited in elderly patients with multiple comorbidities, Dr. Thorsteinsdottir said. “It becomes important to think about the harms of treatment.”
A 2016 study from the Netherlands found no survival advantage to dialysis, compared with conservative management among kidney failure patients aged 80 and older. The survival advantage was limited with dialysis in patients aged 70 and older who also had multiple comorbidities. (Clin J Am Soc Nephrol. 2016 Apr;11(4):633-40)
In an interview, Dr. Thorsteinsdottir acknowledged that “determining who is unlikely to benefit from dialysis is complicated.” However, she said, “we know that the following comorbidities are the worst: dementia and peripheral vascular disease.”
“No one that I know of currently has an age cutoff for dialysis,” Dr. Thorsteinsdottir said in the interview, “and I do not believe the U.S. is ready for any kind of explicit limit setting by the government on dialysis treatment.”
“We must respond to legitimate concerns raised by recent studies that suggest that strong moral imperatives – to treat anyone we can treat – have created a situation where we are not pausing and asking hard questions about whether the patient in front of us is likely to benefit from dialysis,” she said in the interview. “Patients sense this and do not feel that they are given any alternatives to dialysis treatment. This needs to change.”
Dr. Thorsteinsdottir reported no relevant financial disclosures.
REPORTING FROM KIDNEY WEEK 2018
PIONEER-HF called “practice changing” for acute decompensated heart failure
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The rate of rehospitalization for heart failure during the next 2 months after initiation of sacubitril/valsartan during hospitalization for acute decompensated heart failure was 44% lower than with enalapril.
Study details: A randomized, multicenter trial involving 881 patients hospitalized for acute decompensated heart failure.
Disclosures: The PIONEER-HF trial was sponsored by Novartis. The presenter reported receiving research grants from and serving as a consultant to that company and others.
Burden of atrial fibrillation associated with stroke risk
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
How to slash colorectal surgery infection rates
BOSTON – driven mostly by a reduction in deep organ space infections from 5.5% to 1.7%.
It was a remarkable finding that got the attention of attendees at the annual clinical congress of the American College of Surgeons. The Cleveland Clinic had been an outlier, in the wrong direction, compared with other centers, and administrators wanted a solution.
I. Emre Gorgun, MD, FACS, a colorectal surgeon and quality improvement officer at Cleveland Clinic, led the search for evidence-based interventions. Eventually, big changes were made to perioperative antibiotics, mechanical bowel prep, preop shower routines, and intraoperative procedures. The efforts paid off (Dis Colon Rectum. 2018 Jan;61[1]:89-98).
To help surgeons lower their own infection rates, Dr. Gorgun agreed to an interview at the meeting to explain exactly what was done.
There was resistance at first from surgeons who wanted to stick with their routines, but they came around once they were shown the data backing the changes. Eventually, “everyone was on board. We believe in this,” Dr. Gorgun said.
BOSTON – driven mostly by a reduction in deep organ space infections from 5.5% to 1.7%.
It was a remarkable finding that got the attention of attendees at the annual clinical congress of the American College of Surgeons. The Cleveland Clinic had been an outlier, in the wrong direction, compared with other centers, and administrators wanted a solution.
I. Emre Gorgun, MD, FACS, a colorectal surgeon and quality improvement officer at Cleveland Clinic, led the search for evidence-based interventions. Eventually, big changes were made to perioperative antibiotics, mechanical bowel prep, preop shower routines, and intraoperative procedures. The efforts paid off (Dis Colon Rectum. 2018 Jan;61[1]:89-98).
To help surgeons lower their own infection rates, Dr. Gorgun agreed to an interview at the meeting to explain exactly what was done.
There was resistance at first from surgeons who wanted to stick with their routines, but they came around once they were shown the data backing the changes. Eventually, “everyone was on board. We believe in this,” Dr. Gorgun said.
BOSTON – driven mostly by a reduction in deep organ space infections from 5.5% to 1.7%.
It was a remarkable finding that got the attention of attendees at the annual clinical congress of the American College of Surgeons. The Cleveland Clinic had been an outlier, in the wrong direction, compared with other centers, and administrators wanted a solution.
I. Emre Gorgun, MD, FACS, a colorectal surgeon and quality improvement officer at Cleveland Clinic, led the search for evidence-based interventions. Eventually, big changes were made to perioperative antibiotics, mechanical bowel prep, preop shower routines, and intraoperative procedures. The efforts paid off (Dis Colon Rectum. 2018 Jan;61[1]:89-98).
To help surgeons lower their own infection rates, Dr. Gorgun agreed to an interview at the meeting to explain exactly what was done.
There was resistance at first from surgeons who wanted to stick with their routines, but they came around once they were shown the data backing the changes. Eventually, “everyone was on board. We believe in this,” Dr. Gorgun said.
REPORTING FROM THE ACS CLINICAL CONGRESS
PIONEER-HF secures place for sacubitril/valsartan in this heart failure doc’s practice
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
CHICAGO – Dr. Larry A. Allen will now have an easier time of treating hospitalized patients with acute decompensated heart failure because of the results of the PIONEER-HF trial.
That study examined whether in-hospital initiation of sacubitril/valsartan compared to enalapril is safe and effective in ADHF, a treatment that hasn’t been studied well or taken up in clinical practice.
, showed comparable safety, and reduced composite endpoint of death, rehospitalization for heart failure, implantation of a left-ventricular implant device, and need for a transplant by 46%.
Dr. Allen, of the University of Colorado, Denver, was the designated discussant for the PIONEER-HF presentation at the American Heart Association scientific sessions. In an interview, he explained how these results will change his practice as a heart failure specialist. “It simplifies things: I don’t have to start on an old therapy in the hospital, get the patients back in clinic, and switch the over to this newer therapy. I can just start from the beginning with the therapy that I think will be most effective.”
To find out why, watch the complete interview.
REPORTING FROM AHA 2018
Apixaban is safest effective DOAC for stroke prevention in Afib, per AHRQ report
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.