User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'medstat-accordion-set article-series')]
SGLT2 inhibitors for diabetes: No link to fractures in older adults
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors does not appear to raise the risk for fractures in older adults, new research suggests.
The data come from a nationwide propensity score-matched study of U.S. Medicare recipients with type 2 diabetes who were new users of either an SGLT2 inhibitor, a dipeptidyl peptidase 4 (DPP-4) inhibitor, or a glucagon-like peptide (GLP-1) receptor agonist.
“The use of SGLT2 inhibitors was not associated with an increased risk of nontraumatic fractures compared with DPP-4 inhibitors or GLP-1 agonists. Results were consistent across categories of sex, frailty, age, and insulin use,” say Min Zhuo, MD, of Harvard Medical School, Boston, and colleagues, who published their work online October 27 in JAMA Network Open.
“Our results add to the evidence base evaluating the safety profile of SGLT2 inhibitors in older adults outside of [randomized controlled trials] and further characterize the risk-benefit balance of SGLT2 inhibitors in clinical practice,” they write.
Asked to comment, Simeon I. Taylor, MD, PhD, told this news organization, “This is a high-quality study that is generally reassuring that relatively short, less than 1 year, treatment with an SGLT2 inhibitor does not appear to significantly increase the risk of bone fractures.”
However, Dr. Taylor, of the Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, Baltimore, also noted: “Notwithstanding these reassuring data, the paper also does a good job of pointing out important limitations.”
“Most importantly, these data do not address questions related to the risk of long-term chronic therapy. It is instructive to refer back to the published data demonstrating an approximately 2-year lag before a significant increase in the risk of fracture was observed in rosiglitazone-treated patients in the ADOPT study. The length of the lag is likely related to the baseline bone mineral density at the time drug therapy is initiated. These considerations may contribute to the observed variation in bone-related outcomes in different studies.”
Concern about SGLT2 inhibitors and fractures first arose in 2017 from the CANVAS study, in which the overall fracture risk with canagliflozin was a significant 26% higher than placebo. However, subsequent larger randomized trials of canagliflozin and other SGLT2 inhibitors did not find the same risk.
In addition, previous observational studies in younger adults have also not found use of SGLT2 inhibitors to be associated with increased fracture risk compared with DPP-4 inhibitors or GLP-1 agonists.
Understanding fracture risk with SGLT2 inhibitors is ‘critical’
Older adults with type 2 diabetes may benefit from reductions in atherosclerotic cardiovascular events, hospitalization for heart failure, end-stage kidney disease, and death associated with SGLT2 inhibitors, but the fact that aging may have negative effects on bone metabolism means “understanding the fracture risk associated with SGLT2 inhibitors in older adults with type 2 diabetes is critical,” say Dr. Zhuo and colleagues.
In the current study, they analyzed claims data for Medicare beneficiaries aged 66 years and older (1 year past Medicare eligibility) who were newly prescribed an SGLT2 inhibitor, DPP-4 inhibitor, or GLP-1 agonist between April 1, 2013 and Dec. 31, 2017.
A total of 45,889 patients from each treatment group were propensity-matched using 58 baseline characteristics, for a total of 137,667 patients.
After matching, there were 501 events of the primary composite outcome (nontraumatic pelvic fracture, hip fracture requiring surgery, or humerus, radius, or ulna fracture requiring intervention) within 30 days. By treatment group, fracture rates per 1,000 person-years were 4.69, 5.26, and 4.71 for SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 agonists respectively.
The differences between patients taking DPP-4 inhibitors or GLP-1 agonists compared with SGLT2 inhibitors were not significant, with hazard ratios of 0.90 and 1.00, respectively.
Results remained consistent in various sensitivity and subgroup analyses, including limiting the data to just the canagliflozin group. Overall, the fracture rate was greater with female sex, frailty, older age, and insulin use, consistent across drug classes.
The risks for falls and hypoglycemia were lower in the SGLT2 inhibitor versus matched DPP-4 inhibitor groups (hazard ratio, 0.82), and there was no difference in syncope. None of those differences were significant for the SGLT2 inhibitor group compared with the GLP-1 agonist group.
Consistent with previous data, the risk for diabetic ketoacidosis was higher with SGLT2 inhibitors versus DPP-4 inhibitors and GLP-1 agonists (HR, 1.29 and 1.58), and the risk for heart failure hospitalization was lower (HR, 0.42 and 0.69).
The study was funded by the Division of Pharmacoepidemiology and Pharmacoeconomics, department of medicine, Brigham and Women’s Hospital, Harvard Medical School. Dr. Zhuo was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Taylor is a consultant for Ionis Pharmaceuticals.
A version of this article first appeared on Medscape.com.
The devil in the (masking) details
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
Which specialties get the biggest markups over Medicare rates?
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .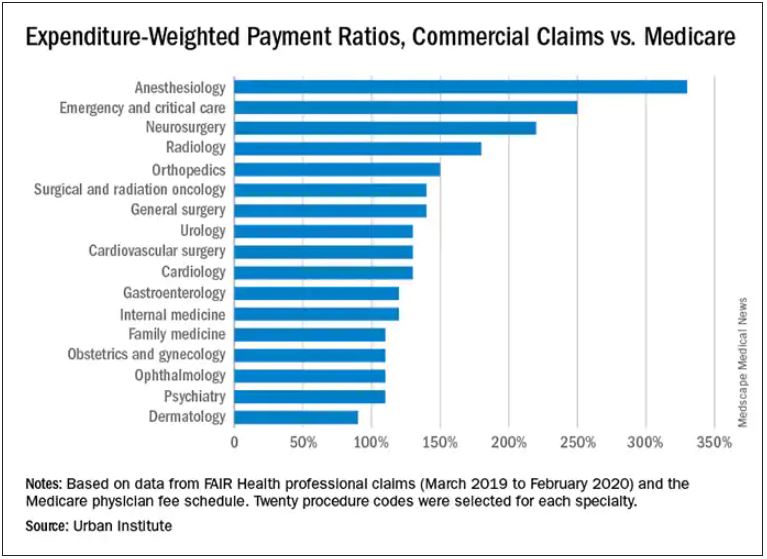
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .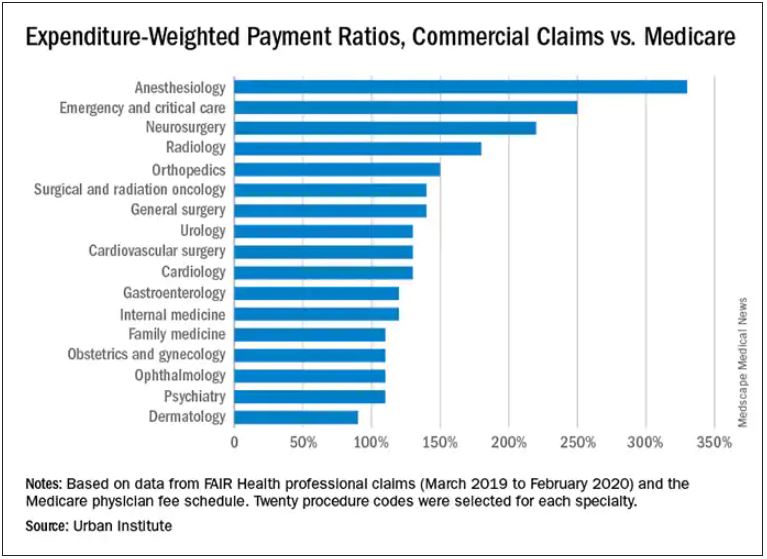
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .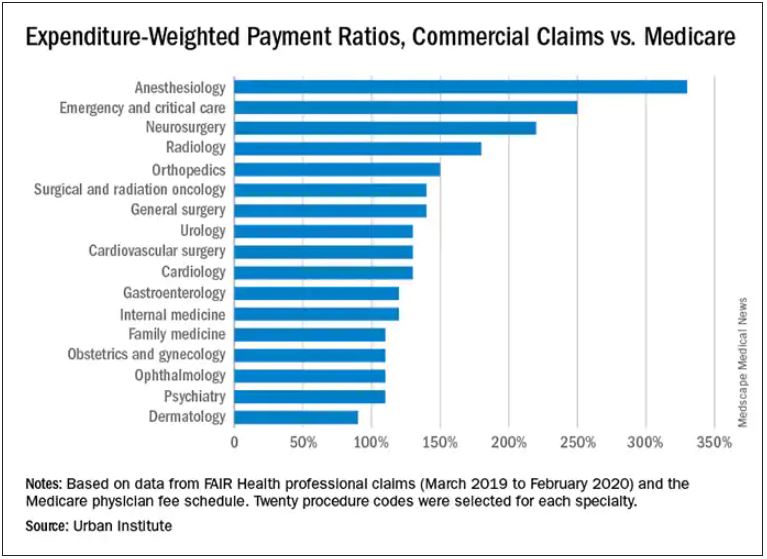
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Hot temperatures in outdoor lockboxes increase sample errors
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA panel votes to approve Pfizer’s vaccine for children
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
Seventeen of the 18 members of the Vaccines and Related Biological Products Advisory Committee (VRBPAC) on Oct. 26 voted to recommend the 10-microgram shot for kids, which is one-third the dose given to adults.
One member, Michael Kurilla, MD, director of the division of clinical innovation at the National Institutes of Health, Bethesda, Md., abstained from voting.
If the FDA follows the recommendation, as it typically does, and issues an Emergency Use Authorization for the vaccine, the shots could be available within days.
After the FDA’s final decision, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will meet to make specific recommendations for its use. The CDC committee must stick closely to the conditions for use spelled out in the EUA, so their recommendations are likely to be similar to those made by the FDA. Their next meeting is scheduled for Nov. 2 and 3.
In the end, some on the panel felt uneasy with their decision.
“I voted yes primarily because I wanted to make sure that children who really need this vaccine, the Black and brown children of our country, get the vaccine,” said James Hildreth, MD, PhD, president and CEO of Meharry Medical College in Nashville.
“But to be honest, the best way to protect the health of some children will be to do nothing because they will be just fine,” he said.
Others said they were surprised by how difficult the decision had been.
“This is a much tougher one than we had expected going into it,” said committee member Eric Rubin, MD, editor and chief of the New England Journal of Medicine, during the FDA advisory committee’s meeting.
Ahead of the vote, the committee heard presentations outlining the expected benefits of vaccinating children along with potential risks.
“Children have been greatly impacted by the pandemic,” said Fiona Havers, MD, a medical officer with the CDC in Atlanta who reviewed the epidemiology of COVID-19 in kids.
In the second year of the pandemic, as more seniors have been vaccinated against the virus, COVID cases have largely shifted from older to younger age groups.
So far, there have been more than 1.9 million COVID-19 cases in children ages 5 through 11 in the United States.. Cases in kids saw a big jump in July and August with summer travel, schools reopening, and the dominance of the Delta variant.
And those are just the cases reported to the CDC. Regular testing of anonymous blood samples collected at sites across the United States indicates that 6 times as many kids have had COVID than what is reflected in official counts.
Last winter, blood sample testing showed about 13% of children had antibodies against the virus, suggesting they’d been infected. By this summer, that number had risen to 42%.
That figure clearly made an impression on many members of the committee who asked the FDA’s vaccine reviewers if they had tried to account for immunity from past infections in their modeling. They had not.
Some felt that even with a highly effective vaccine — new data presented by Pfizer showed the children’s dose was 90% effective at preventing symptomatic infections in kids — caution was warranted as much is still unknown about myocarditis, a rare side effect of the mRNA vaccines.
Myocarditis has been more common in younger age groups. It usually goes away over time but requires hospital care. It’s not known if myocarditis could have lingering effects for those who experience it.
There were no cases of myocarditis seen in Pfizer’s studies of the vaccine in children, and no other serious events were seen. Vaccine side effects reported in the Pfizer studies were mostly mild and included fatigue, headache, and pain at the injection site.
“We think we have optimized the immune response and minimized our reactions,” said William Gruber, MD, senior vice president vaccine research and clinical development at Pfizer.
But the studies didn’t include enough participants to pick up rare, but serious adverse events like myocarditis.
“We’re worried about a side effect that we can’t measure yet, but it’s probably real, and we see a benefit that isn’t the same as it is in older age groups,” said Dr. Rubin.
Benefits vs. risks
FDA modeled the benefits and risks for children under a variety of scenarios. The benefits of the vaccines to children very much depend on the amount of transmission in the community.
When transmission is high, the benefits to children — in terms of infections, hospitalizations, ICU admissions — clearly outweigh its risks.
But when COVID-19 rates are low in the community, as they were in June, FDA analysts predicted the vaccines might send more children to the hospital for myocarditis than the virus would.
The FDA noted that kids who are hospitalized for myocarditis tend not to be as ill as children with COVID-19, however.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” Dr. Hildreth said.
But others warned against complacency.
“Thinking that this is going to be the end of the wave permanently may be a little overly optimistic,” said committee chairman Arnold Monto, MD, a professor of public health and epidemiology at the University of Michigan, Ann Arbor.
The majority of COVID-19 cases in children are mild. Only about 1% of kids are hospitalized for their infections, according to CDC data. But the rates of hospitalizations in kids are about 3 times higher for people of color — including Blacks, Hispanics, and Native Americans, as compared to Whites and Asian Americans.
Since the start of the pandemic, 94 children ages 5 to 11 have died, making it the eighth leading cause of death for kids this age last year.
More than 5,200 children have developed a delayed complication from their infections called Multi-System Inflammatory Syndrome (MIS-C).
MIS-C can be severe and require hospital care and can lead to myocarditis. Children ages 5 to 11 are the age group at greatest risk for this complication.
Kids can also get long COVID. There’s not a lot of data on how often this happens, though it appears to be less frequent in children than in adults.
But a survey in the United Kingdom found that 7%-8% of kids have symptoms from their infections that last longer than 12 weeks, Dr. Havers said. Symptoms that can linger for kids include fatigue, cough, muscle and joint pain, headaches, and insomnia.
More than 1 million children have been impacted by school closures so far this year, and quarantines have had lasting impacts on learning, social development, and mental health.
Even though kids aren’t usually COVID superspreaders, they can still pass the infection on to others.
“What is clear is that secondary transmission from children, both to other children and to adults, does occur,” Dr. Havers said.
For that reason, they can continue the spread of the virus and give it opportunities to mutate and become more dangerous.
Safety monitoring to continue
Some committee members referenced thousands of letters they had received within the past few days urging them to vote against the vaccine.
Jay Portnoy, MD, a professor of pediatrics at Children’s Mercy Hospital in Kansas City, Mo., said he had personally received about 4,000 emails.
“But I feel like I need to also represent the consumers, the parents that I see every day in the clinic who are terrified of sending their children to school because they’re not protected against COVID,” he said, explaining his vote to recommend authorization.
“Our kids are going to be dealing with this virus for many years to come. It’s going to come repeatedly. Getting this vaccine is just the first step that they can take to protect themselves from having bad outcomes,” Dr. Portnoy said.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, reminded members of the committee that there were several government surveillance systems in place to catch any potential safety issues in near real time.
“I really appreciate very much the concern here. The safety monitoring of this vaccine will continue,” Dr. Marks said. “I do view this as one of our greatest responsibilities.”
“I really am so grateful that we had this discussion and voted to approve,” said Capt. Amanda Cohn, MD, chief medical officer at the National Center for Immunization and Respiratory Diseases.
“I think the benefits in this age group really are super important even if they are lower than for other age groups.”
This article was updated 10/27/21.
A version of this article first appeared on WebMD.com.
PRP injections don’t top placebo for ankle osteoarthritis
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Judge dismisses Lyme disease lawsuit against IDSA, doctors, but the ordeal has left its scars
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.
Unvaccinated people likely to catch COVID repeatedly
according to a recent study published in The Lancet Microbe.
Since COVID-19 hasn’t existed for long enough to perform a long-term study, researchers at Yale University and the University of North Carolina at Charlotte looked at reinfection data for six other human-infecting coronaviruses, including SARS and MERS.
“Reinfection can reasonably happen in three months or less,” Jeffrey Townsend, PhD, lead study author and a biostatistics professor at the Yale School of Public Health, said in a statement.
“Therefore, those who have been naturally infected should get vaccinated,” he said. “Previous infection alone can offer very little long-term protection against subsequent infections.”
The research team looked at post-infection data for six coronaviruses between 1984-2020 and found reinfection ranged from 128 days to 28 years. They calculated that reinfection with COVID-19 would likely occur between 3 months to 5 years after peak antibody response, with an average of 16 months. This is less than half the duration seen for other coronaviruses that circulate among humans.
The risk of COVID-19 reinfection is about 5% at three months, which jumps to 50% after 17 months, the research team found. Reinfection could become increasingly common as immunity wanes and new variants develop, they said.
“We tend to think about immunity as being immune or not immune. Our study cautions that we instead should be more focused on the risk of reinfection through time,” Alex Dornburg, PhD, senior study author and assistant professor of bioinformatics and genomics at UNC, said in the statement.
“As new variants arise, previous immune responses become less effective at combating the virus,” he said. “Those who were naturally infected early in the pandemic are increasingly likely to become reinfected in the near future.”
Study estimates are based on average times of declining immunity across different coronaviruses, the researchers told the Yale Daily News. At the individual level, people have different levels of immunity, which can provide shorter or longer duration of protection based on immune status, immunity within a community, age, underlying health conditions, environmental exposure, and other factors.
The research team said that preventive health measures and global distribution of vaccines will be “critical” in minimizing reinfection and COVID-19 deaths. In areas with low vaccination rates, for instance, unvaccinated people should continue safety practices such as social distancing, wearing masks, and proper indoor ventilation to avoid reinfection.
“We need to be very aware of the fact that this disease is likely to be circulating over the long term and that we don’t have this long-term immunity that many people seem to be hoping to rely on in order to protect them from disease,” Dr. Townsend told the newspaper.
A version of this article first appeared on WebMD.com.
according to a recent study published in The Lancet Microbe.
Since COVID-19 hasn’t existed for long enough to perform a long-term study, researchers at Yale University and the University of North Carolina at Charlotte looked at reinfection data for six other human-infecting coronaviruses, including SARS and MERS.
“Reinfection can reasonably happen in three months or less,” Jeffrey Townsend, PhD, lead study author and a biostatistics professor at the Yale School of Public Health, said in a statement.
“Therefore, those who have been naturally infected should get vaccinated,” he said. “Previous infection alone can offer very little long-term protection against subsequent infections.”
The research team looked at post-infection data for six coronaviruses between 1984-2020 and found reinfection ranged from 128 days to 28 years. They calculated that reinfection with COVID-19 would likely occur between 3 months to 5 years after peak antibody response, with an average of 16 months. This is less than half the duration seen for other coronaviruses that circulate among humans.
The risk of COVID-19 reinfection is about 5% at three months, which jumps to 50% after 17 months, the research team found. Reinfection could become increasingly common as immunity wanes and new variants develop, they said.
“We tend to think about immunity as being immune or not immune. Our study cautions that we instead should be more focused on the risk of reinfection through time,” Alex Dornburg, PhD, senior study author and assistant professor of bioinformatics and genomics at UNC, said in the statement.
“As new variants arise, previous immune responses become less effective at combating the virus,” he said. “Those who were naturally infected early in the pandemic are increasingly likely to become reinfected in the near future.”
Study estimates are based on average times of declining immunity across different coronaviruses, the researchers told the Yale Daily News. At the individual level, people have different levels of immunity, which can provide shorter or longer duration of protection based on immune status, immunity within a community, age, underlying health conditions, environmental exposure, and other factors.
The research team said that preventive health measures and global distribution of vaccines will be “critical” in minimizing reinfection and COVID-19 deaths. In areas with low vaccination rates, for instance, unvaccinated people should continue safety practices such as social distancing, wearing masks, and proper indoor ventilation to avoid reinfection.
“We need to be very aware of the fact that this disease is likely to be circulating over the long term and that we don’t have this long-term immunity that many people seem to be hoping to rely on in order to protect them from disease,” Dr. Townsend told the newspaper.
A version of this article first appeared on WebMD.com.
according to a recent study published in The Lancet Microbe.
Since COVID-19 hasn’t existed for long enough to perform a long-term study, researchers at Yale University and the University of North Carolina at Charlotte looked at reinfection data for six other human-infecting coronaviruses, including SARS and MERS.
“Reinfection can reasonably happen in three months or less,” Jeffrey Townsend, PhD, lead study author and a biostatistics professor at the Yale School of Public Health, said in a statement.
“Therefore, those who have been naturally infected should get vaccinated,” he said. “Previous infection alone can offer very little long-term protection against subsequent infections.”
The research team looked at post-infection data for six coronaviruses between 1984-2020 and found reinfection ranged from 128 days to 28 years. They calculated that reinfection with COVID-19 would likely occur between 3 months to 5 years after peak antibody response, with an average of 16 months. This is less than half the duration seen for other coronaviruses that circulate among humans.
The risk of COVID-19 reinfection is about 5% at three months, which jumps to 50% after 17 months, the research team found. Reinfection could become increasingly common as immunity wanes and new variants develop, they said.
“We tend to think about immunity as being immune or not immune. Our study cautions that we instead should be more focused on the risk of reinfection through time,” Alex Dornburg, PhD, senior study author and assistant professor of bioinformatics and genomics at UNC, said in the statement.
“As new variants arise, previous immune responses become less effective at combating the virus,” he said. “Those who were naturally infected early in the pandemic are increasingly likely to become reinfected in the near future.”
Study estimates are based on average times of declining immunity across different coronaviruses, the researchers told the Yale Daily News. At the individual level, people have different levels of immunity, which can provide shorter or longer duration of protection based on immune status, immunity within a community, age, underlying health conditions, environmental exposure, and other factors.
The research team said that preventive health measures and global distribution of vaccines will be “critical” in minimizing reinfection and COVID-19 deaths. In areas with low vaccination rates, for instance, unvaccinated people should continue safety practices such as social distancing, wearing masks, and proper indoor ventilation to avoid reinfection.
“We need to be very aware of the fact that this disease is likely to be circulating over the long term and that we don’t have this long-term immunity that many people seem to be hoping to rely on in order to protect them from disease,” Dr. Townsend told the newspaper.
A version of this article first appeared on WebMD.com.
What if your patient refuses to disrobe?
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Progressive muscle relaxation enhances sleep quality and decreases fatigue in RA
Key clinical point: Progressive muscle relaxation (PMR) effectively improved sleep quality and reduced fatigue in patients with rheumatoid arthritis (RA).
Major finding: The total Pittsburgh Sleep Quality Index and total Fatigue Severity Scale mean score decreased significantly from 11.37 to 4.97 and 6.48 to 2.15 (both P = .001), respectively, in the PMR intervention group. However, no significant difference was observed among patients in the control group.
Study details: This was a randomized controlled study of 72 patients with RA who were categorized into the PMR intervention group (n = 35) or the control group (n = 37).
Disclosures: The Fırat University Rectorate Scientific Research Projects Coordination Unit provided funding to this research. None of the authors declared any conflict of interest.
Source: Kılıç N et al. Int J Nurs Pract. 2021 Sep 26. doi: 10.1111/ijn.13015.
Key clinical point: Progressive muscle relaxation (PMR) effectively improved sleep quality and reduced fatigue in patients with rheumatoid arthritis (RA).
Major finding: The total Pittsburgh Sleep Quality Index and total Fatigue Severity Scale mean score decreased significantly from 11.37 to 4.97 and 6.48 to 2.15 (both P = .001), respectively, in the PMR intervention group. However, no significant difference was observed among patients in the control group.
Study details: This was a randomized controlled study of 72 patients with RA who were categorized into the PMR intervention group (n = 35) or the control group (n = 37).
Disclosures: The Fırat University Rectorate Scientific Research Projects Coordination Unit provided funding to this research. None of the authors declared any conflict of interest.
Source: Kılıç N et al. Int J Nurs Pract. 2021 Sep 26. doi: 10.1111/ijn.13015.
Key clinical point: Progressive muscle relaxation (PMR) effectively improved sleep quality and reduced fatigue in patients with rheumatoid arthritis (RA).
Major finding: The total Pittsburgh Sleep Quality Index and total Fatigue Severity Scale mean score decreased significantly from 11.37 to 4.97 and 6.48 to 2.15 (both P = .001), respectively, in the PMR intervention group. However, no significant difference was observed among patients in the control group.
Study details: This was a randomized controlled study of 72 patients with RA who were categorized into the PMR intervention group (n = 35) or the control group (n = 37).
Disclosures: The Fırat University Rectorate Scientific Research Projects Coordination Unit provided funding to this research. None of the authors declared any conflict of interest.
Source: Kılıç N et al. Int J Nurs Pract. 2021 Sep 26. doi: 10.1111/ijn.13015.