User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
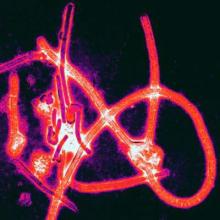
Postexposure prophylaxis may prevent Ebola disease development
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
Quit smoking for less chest pain, better mental health after MI
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
Patients who stopped smoking after their heart attack had less chest pain and experienced better mental health than did those who continued to smoke at 1 year after their acute myocardial infarction (AMI).
Moreover, the post-MI quitters had levels of angina and mental health similar to those who had never smoked, and scores improved with the passage of time after smoking cessation, according to a prospective, multicenter study.
Smoking cessation after a heart attack reduces mortality and the risk of recurrent MI by up to 50%, according to Donna Buchanan, Ph.D., and her coinvestigators. However, few high-quality studies to date have examined the effect of smoking cessation on overall health-related quality of life (HRQOL), she said.
For this study, Dr. Buchanan and her colleagues used data from two large multicenter AMI registries to address how smoking status after AMI is related to mental and physical health status. Using the Seattle Angina Questionnaire and the Medical Outcomes Study Short Form 12-item questionnaire, investigators tracked changes in chest pain and mental and physical health status at 1, 6, and 12 months post AMI according to smoking status.
The final cohort included 4,003 patients who were then grouped by smoking status.
Patients were grouped into never smokers (1,145), former smokers (1,374), and current smokers. A total of 1,484 patients were smokers at baseline; of those, 801 were still smoking at 1 year post-MI. The remaining 683 patients quit within the year after their AMI and were classified as recent quitters. In unadjusted analysis, never smokers had the highest health status scores and current smokers the worst, with a gradation across the four categories of smoking status that was statistically significant for all domains, said Dr. Buchanan of the University of Missouri–Kansas City.
Further statistical exploration with multivariable analysis showed that former smokers and never smokers looked similar in all HRQOL, while there was more variability across HRQOL domains for recent quitters. Recent quitters were significantly more likely to report good mental health status than current smokers, even when levels of depression and social support were taken into consideration (Circ Cardiovasc Qual Outcomes. 2015 Aug 25; doi: 10.1161/circoutcomes.114.001545).
In examining physical symptoms, recent quitters had levels of angina similar to those who had never smoked, while persistent smokers had more angina post-AMI than any other group. Dr. Buchanan and her colleagues noted that the oxidative stress, endothelial damage, and proinflammatory state that are caused by smoking all may contribute to ongoing angina. Smokers also experience increased adrenergic tone, and may have more coronary vasospasm.
The study elucidates an important aspect of care for the patient who has experienced a heart attack, said Dr. Buchanan. “Current educational efforts tend to focus on how continued smoking increases the risk of recurrent heart attack and death, but health-related quality of life is often equally or more important to patients than longevity,” she said in a statement. Her hope, she wrote, is that “These observations may help encourage patients to stop smoking after AMI.”
The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
On Twitter @karioakes
FROM CIRCULATION CARDIOVASCULAR QUALITY OUTCOMES
Key clinical point: Patients who quit smoking after acute myocardial infarction had better health-related quality of life and less chest pain than those who continued smoking.
Major finding: One year after acute MI, those who stopped smoking had similar mental health scores and angina levels to never-smokers.
Data source: 4,003 patients in two U.S., multicenter, prospective AMI registries who were assessed for smoking status, HRQOL, and angina at 1, 6, and 12 months post MI.
Disclosures: The study was funded by CV Therapeutics and the National Institutes of Health. A coinvestigator owns the copyright to the Seattle Angina Questionnaire, used to assess angina in the study.
New IPF guidelines limit treatment choices
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Pneumococcal vaccination rates increase with intervention
A pediatric rheumatology clinic substantially increased the pneumococcal vaccination rates of their high-risk patients through a targeted, multipart yearlong intervention, according to a recent study.
“This single-center quality improvement project to increase pneumococcal vaccination rates in eligible pediatric rheumatology clinic patients was a success that can serve as a model for other hospitals and divisions,” reported Dr. Julia G. Harris of Children’s Mercy-Kansas City in Missouri, and her associates (Pediatrics 2015 Aug. 24. [doi:10.1542/peds.2014-2512]). “Through simple quality improvement initiatives, our vaccination rates statistically increased over time and were sustained indicating a true change in practice.”
The Centers for Disease Control and Prevention recommends that all infants receive the 13-valent pneumococcal conjugate vaccine (PCV13) four times in early childhood, with high-risk patients aged 2-5 years receiving at least one dose. High-risk patients at least 2 years old should also receive the 23-valent pneumococcal polysaccharide vaccine (PPSV23) and continue to receive a dose every 5 years if they remain at high risk.
The researchers designed an intervention aimed at improving pneumococcal vaccination rates among children at least 2 years old and adults who had systemic lupus erythematosus and/or who were taking immunosuppressive medication.
Before the intervention, retrospective analysis of 90 patient visits in 88 patients during 4 weeks revealed that 6.7% of the patients had received the PCV13, and 8.9% had received PPSV23, but none had received both.
The intervention, which ran from September 2012 to October 2013, involved multiple components, beginning with stocking PCV13 and PPSV23 and then a formal presentation to providers and nurses about the recommendations for pneumococcal vaccines. An immunization algorithm posted throughout the clinic helped clinicians determine whether pneumococcal vaccination was indicated.
The office created a weekly email identifying patients in need of either vaccine; then the nurses would attach brightly colored pieces of paper with either PCV13 or PPSV23 written on them to patients’ clinic encounter forms to flag which patients should be immunized.
“Pneumococcal vaccines were often administered in clinic, and nurses provided an educational document regarding the specific vaccine to the patient and family,” the authors explained. Patients living out of state or who lacked an immunization record also received letters requesting immunization records to determine if they needed the pneumococcal vaccine.
During the year (53 weeks) after the intervention began, the coverage increased to 48.4% of 299 patients with 1,033 patient visits (P less than .001). Similarly, the vaccination rate with PPSV23 increased from 8.9% to 28.4%, and the combined vaccination rate for receiving both vaccines increased from 0% to 23.2%.
A pediatric rheumatology clinic substantially increased the pneumococcal vaccination rates of their high-risk patients through a targeted, multipart yearlong intervention, according to a recent study.
“This single-center quality improvement project to increase pneumococcal vaccination rates in eligible pediatric rheumatology clinic patients was a success that can serve as a model for other hospitals and divisions,” reported Dr. Julia G. Harris of Children’s Mercy-Kansas City in Missouri, and her associates (Pediatrics 2015 Aug. 24. [doi:10.1542/peds.2014-2512]). “Through simple quality improvement initiatives, our vaccination rates statistically increased over time and were sustained indicating a true change in practice.”
The Centers for Disease Control and Prevention recommends that all infants receive the 13-valent pneumococcal conjugate vaccine (PCV13) four times in early childhood, with high-risk patients aged 2-5 years receiving at least one dose. High-risk patients at least 2 years old should also receive the 23-valent pneumococcal polysaccharide vaccine (PPSV23) and continue to receive a dose every 5 years if they remain at high risk.
The researchers designed an intervention aimed at improving pneumococcal vaccination rates among children at least 2 years old and adults who had systemic lupus erythematosus and/or who were taking immunosuppressive medication.
Before the intervention, retrospective analysis of 90 patient visits in 88 patients during 4 weeks revealed that 6.7% of the patients had received the PCV13, and 8.9% had received PPSV23, but none had received both.
The intervention, which ran from September 2012 to October 2013, involved multiple components, beginning with stocking PCV13 and PPSV23 and then a formal presentation to providers and nurses about the recommendations for pneumococcal vaccines. An immunization algorithm posted throughout the clinic helped clinicians determine whether pneumococcal vaccination was indicated.
The office created a weekly email identifying patients in need of either vaccine; then the nurses would attach brightly colored pieces of paper with either PCV13 or PPSV23 written on them to patients’ clinic encounter forms to flag which patients should be immunized.
“Pneumococcal vaccines were often administered in clinic, and nurses provided an educational document regarding the specific vaccine to the patient and family,” the authors explained. Patients living out of state or who lacked an immunization record also received letters requesting immunization records to determine if they needed the pneumococcal vaccine.
During the year (53 weeks) after the intervention began, the coverage increased to 48.4% of 299 patients with 1,033 patient visits (P less than .001). Similarly, the vaccination rate with PPSV23 increased from 8.9% to 28.4%, and the combined vaccination rate for receiving both vaccines increased from 0% to 23.2%.
A pediatric rheumatology clinic substantially increased the pneumococcal vaccination rates of their high-risk patients through a targeted, multipart yearlong intervention, according to a recent study.
“This single-center quality improvement project to increase pneumococcal vaccination rates in eligible pediatric rheumatology clinic patients was a success that can serve as a model for other hospitals and divisions,” reported Dr. Julia G. Harris of Children’s Mercy-Kansas City in Missouri, and her associates (Pediatrics 2015 Aug. 24. [doi:10.1542/peds.2014-2512]). “Through simple quality improvement initiatives, our vaccination rates statistically increased over time and were sustained indicating a true change in practice.”
The Centers for Disease Control and Prevention recommends that all infants receive the 13-valent pneumococcal conjugate vaccine (PCV13) four times in early childhood, with high-risk patients aged 2-5 years receiving at least one dose. High-risk patients at least 2 years old should also receive the 23-valent pneumococcal polysaccharide vaccine (PPSV23) and continue to receive a dose every 5 years if they remain at high risk.
The researchers designed an intervention aimed at improving pneumococcal vaccination rates among children at least 2 years old and adults who had systemic lupus erythematosus and/or who were taking immunosuppressive medication.
Before the intervention, retrospective analysis of 90 patient visits in 88 patients during 4 weeks revealed that 6.7% of the patients had received the PCV13, and 8.9% had received PPSV23, but none had received both.
The intervention, which ran from September 2012 to October 2013, involved multiple components, beginning with stocking PCV13 and PPSV23 and then a formal presentation to providers and nurses about the recommendations for pneumococcal vaccines. An immunization algorithm posted throughout the clinic helped clinicians determine whether pneumococcal vaccination was indicated.
The office created a weekly email identifying patients in need of either vaccine; then the nurses would attach brightly colored pieces of paper with either PCV13 or PPSV23 written on them to patients’ clinic encounter forms to flag which patients should be immunized.
“Pneumococcal vaccines were often administered in clinic, and nurses provided an educational document regarding the specific vaccine to the patient and family,” the authors explained. Patients living out of state or who lacked an immunization record also received letters requesting immunization records to determine if they needed the pneumococcal vaccine.
During the year (53 weeks) after the intervention began, the coverage increased to 48.4% of 299 patients with 1,033 patient visits (P less than .001). Similarly, the vaccination rate with PPSV23 increased from 8.9% to 28.4%, and the combined vaccination rate for receiving both vaccines increased from 0% to 23.2%.
FROM PEDIATRICS
Key clinical point: Pneumococcal vaccination rates for high-risk pediatric rheumatology patients improved with a targeted intervention.
Major finding: PCV13 coverage increased from 6.7% to 48.4%, and PPSV23 increased from 8.9% to 28.4%.
Data source: The findings are based on retrospective baseline data and then prospectively collected data on patient pneumococcal immunization rates in a pediatric rheumatology clinic during a 53-week intervention.
Disclosures: The study did not use any external funding. Dr. Judyann C. Olson reported being a site coinvestigator for a multicenter clinical trial on an unrelated topic with a grant pending from Pfizer.
Evidence of a respiratory virus does not exclude Kawasaki disease
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
Many children with Kawasaki disease (KD) have respiratory viruses and a positive viral polymerase chain reaction should not exclude a KD diagnosis, according to a new study.
Kawasaki disease is a major cause of heart disease in children, however a specific etiology has yet to be found. A viral cause is suspected because of its seasonal presentation, clinical symptoms, and evidence from previous studies.
Dr. Jessica Turnier and her colleagues of the University of Colorado Denver and Children’s Hospital Colorado, both in Aurora, wanted to determine the rate of viral infections with KD, and if this coinfection was linked to variances in cardiac outcomes or clinical presentation (Pediatrics. 2015, Aug 24. [doi: 10.1542/peds.2015-0950]).
A chart review was performed of patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado. For patients suspected of having KD, it was the standard practice to obtain nasopharyngeal washes to detect the presence of 16 respiratory viruses.
During the study period, 222 patients were diagnosed with KD, and 86% (n = 192) had respiratory viral polymerase chain reactions (PCRs) obtained. These viral PCRs were positive in 42% of the 192 patients, with the most-common being enterovirus or rhinovirus (28%). Adenovirus, respiratory syncytial virus, and human metapneumovirus were found in 5% of patients.
The authors noted no significant differences in the clinical presentation of patients with KD whether or not they had concurrent viral infection. Upper respiratory infection was reported 63% (virus-positive KD) and 56% (virus-negative KD) of the time. Patients reported a recent history of gastrointestinal symptoms 67% (virus-negative KD) and 57% (virus-positive KD) of the time.
Furthermore, there were no differences between the groups with respect to C-reactive protein, erythrocyte sedimentation rate, WBC, frequency of coronary artery lesions, or immunoglobulin resistance.
Patients with positive viral results (11%) required care in the PICU more often than the viral-negative group (6%), but this was not significant. Incomplete KD was documented in 31% of viral-positive patients versus 25% in the viral-negative patients.
The authors conclude that patients with KD commonly have concurrent respiratory viral infections. They continued, “a large percentage of patients with KD have a concurrent or recent history of respiratory viral infections and [this study] suggests that clinicians should not dismiss the diagnosis of KD based on the presence of respiratory or gastrointestinal symptoms or solely on the results of a positive respiratory viral PCR test.”
The authors report no external funding sources or disclosures.
FROM PEDIATRICS
Key clinical point: A positive respiratory viral PCR does not exclude Kawasaki disease.
Major finding: There were no significant differences in clinical presentation, laboratory results, coronary artery lesions, or frequency of PICU admission between the viral-positive and viral-negative groups.
Data source: A chart review of 192 patients diagnosed with KD from January 2009 to May 2013 and admitted to the Children’s Hospital Colorado, Aurora.
Disclosures: The authors report no external funding sources or disclosures.
CT findings identify COPD phenotype with high risk for exacerbations
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
This study identified a group of COPD patients who may benefit from more access to health care resources, a finding that is especially opportune with the increased focus on reductions in COPD exacerbation and readmissions.
However, the question remains as to how to incorporate these findings into clinical practice and further research. CT images are quite variable due to differences in brands, variable protocols, and reconstruction algorithms.
The biomedical community needs to emphasize the need for stable estimates of disease severity between different CT brands and create standardization of CT derived measurements.
Dr. George R. Washko is affiliated with the Division of Pulmonary and Critical Care Medicine at Brighman and Women’s Hospital in Boston, MA. These comments are taken from an accompanying editorial. Dr. Washko reported consulting for GSK and Merck.
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
COPD patients who have emphysema and airway thickening on computed tomography findings have more hospitalizations and more severe dyspnea, according to the results of a study by Dr. Van Tho Nguyen and colleagues from the Shiga University of Medical Science, Otsu, Shiga, Japan, and the University Medical Center at Ho Chi Minh City, Vietnam.
Pulmonary function testing may not fully represent the heterogenous characteristics of COPD, according to the researchers, who used quantitative CT to develop a method to phenotype COPD and examine differences in clinical outcomes between mixed phenotype patients and those with emphysema- and airway-dominant phenotypes.
The mixed phenotype was associated with more severe dyspnea and more frequent hospitalizations, and these patients may need more attention and interventions, the researchers said (Ann Am Thorac Soc Vol 12, No 7, pp 988–996, Jul 2015).
The researchers performed pulmonary function testing and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD. Four phenotypical classifications were defined on the basis of measurements of airway thickening and percentage of low-attenuation volume (threshold of -950 Hounsfield units) – CT-normal, airway-dominant, emphysema-dominant, and mixed phenotype.
Of the 240 patients with COPD, 43% had the emphysema-dominant phenotype, 22% had the CT-normal phenotype, 19% had a mixed phenotype, and 16% had the airway-dominant phenotype.
Patients with mixed phenotype COPD were found to have more severe air trapping (residual volume/total lung capacity, RV/TLC) and airflow limitation (FEV1/FVC and FEV1% predicted) compared to the other phenotypes. Likewise, mixed phenotype COPD patients had lower percent predicted carbon monoxide diffusing capacity than the airway-dominant phenotype (P<0.0001) and the CT-normal phenotype (P<0.0001).
Furthermore, patients with mixed phenotype COPD had 2.0 to 3.6 more hospitalizations for COPD exacerbations (P<0.05) and more severe dyspnea (P<0.01) than the other CT-based COPD phenotypes. The differences persisted after adjusting for BMI, FEV1, age, smoking status, and pack-years.
Further, the mixed COPD phenotype was associated with a longer duration of disease and a higher blood neutrophil count, which has been linked to higher risk of recurrent exacerbations and may lead to emphysema progression.
The researchers theorize that these patients have more severe dyspnea and therefore are diagnosed earlier or it may take longer for both airway thickening and emphysema to develop.
Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quantitative CT can be used to classify COPD patients as having either airway-dominant, emphysema-dominant, or mixed-phenotype based on the severity of airway thickening versus emphysema. Frequent exacerbations and cough is found in the airway-dominant COPD phenotype, whereas, the emphysema-dominant phenotype have more severe dyspnea, lower BMI, rapid loss of FEV-1, and higher respiratory associated mortality.
FROM THE ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point: COPD patients with both airway thickening and emphysema have more hospitalizations and more severe dyspnea.
Major finding: Patients with mixed phenotype COPD had 2.0 to 3.6 more COPD exacerbation hospitalizations (P<0.05) and more severe dyspnea (P<0.01).
Data source: A cross-sectional study using pulmonary function testing (PFTs), medical interviews, and whole-lung CT scans on 240 male smokers with COPD and 187 male smokers without COPD.
Disclosures: Dr. Nakano and Ogawa reported receiving grants from the Japan Society for the Promotion of Science and Dr. Nakano reported receiving fees from GSK and Nippon Boehringer Ingelheim.
Quadrivalent flu vaccine administration nearly equal to trivalent usage in 2013-2014 season
Administration of the quadrivalent influenza vaccine in U.S. children nearly matched that of the trivalent vaccine during the 2013-2014 flu season, Loren Rodgers, Ph.D., and his coauthors from the Center for Disease Control and Prevention’s Immunization Services Division reported in a letter to the editor to Vaccine.
An analysis of 1,976,443 immunization records in patients aged 6 months to 18 years showed that 49.8% of vaccinations administered were trivalent, compared with 46.6% for the quadrivalent type. Another 3.7% of vaccines were an unknown or other type of influenza vaccine .
The report’s findings establish “a baseline for measuring uptake of quadrivalent influenza vaccines,” the authors said. “Trivalent vaccines were administered slightly more frequently, although use of quadrivalent vaccines is expected to increase.”
Read the full report here: (Vaccine 2015 http://dx.doi.org/10.1016/j.vaccine.2015.08.018)
Administration of the quadrivalent influenza vaccine in U.S. children nearly matched that of the trivalent vaccine during the 2013-2014 flu season, Loren Rodgers, Ph.D., and his coauthors from the Center for Disease Control and Prevention’s Immunization Services Division reported in a letter to the editor to Vaccine.
An analysis of 1,976,443 immunization records in patients aged 6 months to 18 years showed that 49.8% of vaccinations administered were trivalent, compared with 46.6% for the quadrivalent type. Another 3.7% of vaccines were an unknown or other type of influenza vaccine .
The report’s findings establish “a baseline for measuring uptake of quadrivalent influenza vaccines,” the authors said. “Trivalent vaccines were administered slightly more frequently, although use of quadrivalent vaccines is expected to increase.”
Read the full report here: (Vaccine 2015 http://dx.doi.org/10.1016/j.vaccine.2015.08.018)
Administration of the quadrivalent influenza vaccine in U.S. children nearly matched that of the trivalent vaccine during the 2013-2014 flu season, Loren Rodgers, Ph.D., and his coauthors from the Center for Disease Control and Prevention’s Immunization Services Division reported in a letter to the editor to Vaccine.
An analysis of 1,976,443 immunization records in patients aged 6 months to 18 years showed that 49.8% of vaccinations administered were trivalent, compared with 46.6% for the quadrivalent type. Another 3.7% of vaccines were an unknown or other type of influenza vaccine .
The report’s findings establish “a baseline for measuring uptake of quadrivalent influenza vaccines,” the authors said. “Trivalent vaccines were administered slightly more frequently, although use of quadrivalent vaccines is expected to increase.”
Read the full report here: (Vaccine 2015 http://dx.doi.org/10.1016/j.vaccine.2015.08.018)
CDC: Chinese study highlights need for smoke-free policies
Strictly enforced tobacco control regulations are necessary to effectively protect the public from the dangers of secondhand smoke, and results from a recently published report in China show strong public support for such policies, the CDC reported in a statement Aug. 19.
Findings from the survey of 31,151 respondents from 14 cities in China showed that more than 90% supported smoking bans in health care facilities and indoor areas of schools and universities. Also, 88% supported prohibiting smoking in workplaces and 86% supported a smoking ban in taxis.
However, in areas with smoke-free policies in effect in health care facilities and schools, awareness of these policies was as low as 34% in some cities, the authors noted. Other areas in need of attention are cessation rates, which remain low, and the cost of tobacco, which is very low in China, they added.
“Through the synergy of effective law enforcement and public-education campaigns, the acceptance of smoking could be reduced and eventually reversed,” the authors said in the report. “Cities could help transform the social norms regarding smoking in the surrounding areas and eliminate smoking in public places.”
The study was funded by the Chinese Center for Disease Control and Prevention.
Read the full report here.
Strictly enforced tobacco control regulations are necessary to effectively protect the public from the dangers of secondhand smoke, and results from a recently published report in China show strong public support for such policies, the CDC reported in a statement Aug. 19.
Findings from the survey of 31,151 respondents from 14 cities in China showed that more than 90% supported smoking bans in health care facilities and indoor areas of schools and universities. Also, 88% supported prohibiting smoking in workplaces and 86% supported a smoking ban in taxis.
However, in areas with smoke-free policies in effect in health care facilities and schools, awareness of these policies was as low as 34% in some cities, the authors noted. Other areas in need of attention are cessation rates, which remain low, and the cost of tobacco, which is very low in China, they added.
“Through the synergy of effective law enforcement and public-education campaigns, the acceptance of smoking could be reduced and eventually reversed,” the authors said in the report. “Cities could help transform the social norms regarding smoking in the surrounding areas and eliminate smoking in public places.”
The study was funded by the Chinese Center for Disease Control and Prevention.
Read the full report here.
Strictly enforced tobacco control regulations are necessary to effectively protect the public from the dangers of secondhand smoke, and results from a recently published report in China show strong public support for such policies, the CDC reported in a statement Aug. 19.
Findings from the survey of 31,151 respondents from 14 cities in China showed that more than 90% supported smoking bans in health care facilities and indoor areas of schools and universities. Also, 88% supported prohibiting smoking in workplaces and 86% supported a smoking ban in taxis.
However, in areas with smoke-free policies in effect in health care facilities and schools, awareness of these policies was as low as 34% in some cities, the authors noted. Other areas in need of attention are cessation rates, which remain low, and the cost of tobacco, which is very low in China, they added.
“Through the synergy of effective law enforcement and public-education campaigns, the acceptance of smoking could be reduced and eventually reversed,” the authors said in the report. “Cities could help transform the social norms regarding smoking in the surrounding areas and eliminate smoking in public places.”
The study was funded by the Chinese Center for Disease Control and Prevention.
Read the full report here.
E-cigarettes precede tobacco smoking in ninth-graders
Ninth-graders who have used electronic cigarettes are much more likely than are nonusers to try regular cigarettes, cigars, and hookahs during the subsequent year, according to a report published online Aug. 18 in JAMA.
E-cigarettes are handheld battery-operated devices that heat a liquid composed of nicotine, propylene glycol or glycerin, flavorings, and other chemicals to create a vapor that is inhaled, simulating the experience of cigarette smoking. Their main potential benefit is to help adult smokers switch from using the more unhealthy combustible tobacco.
However, critics argue that adolescents who use e-cigarettes may be more likely to try other products that deliver nicotine, which would perpetuate the current epidemic of tobacco-related illness, said Adam M. Leventhal, Ph.D., of the department of preventive medicine, University of Southern California, Los Angeles, and his associates.
The investigators analyzed data from a longitudinal survey of substance use and mental health among high school students. In their prospective observational study, they focused on 2,530 demographically diverse students in ninth grade at 10 Los Angeles–area public high schools. The students were nonsmokers at baseline. A total of 222 of these adolescents reported that they had used e-cigarettes, while 2,308 had not.
Adolescents who had used e-cigarettes were much more likely than were nonusers to report trying combustible tobacco products during the next 6 months (30.7% vs 8.1%) and during the next 12 months (25.2% vs 9.3%), for an odds ratio of 4.27 averaged across the two study periods. This association was strong for each of the combustible tobacco products assessed, with an OR of 2.65 for regular cigarettes, an OR of 4.85 for full-size cigars or cigarillos, and an OR of 3.25 for hookahs.
When the data were adjusted to account for many sociodemographic, environmental, and intrapersonal characteristics known to influence smoking, the ORs declined but the associations remained strong and statistically significant, ranging from 1.75 to 2.96, depending on the smoking product, Dr. Leventhal and his associates said (JAMA. 2015;314[7]:700-707). One possible explanation for these findings is that adolescents who used e-cigarettes enjoyed the experience and were more likely to experiment with other nicotine-containing products. However, “because this is an observational study, and one of the first to address this issue, inferences regarding whether this association is or is not causal cannot yet be made,” they noted.
The study by Leventhal et al. presents the “strongest evidence to date” that e-cigarettes may pose a health hazard by encouraging adolescents to start smoking conventional tobacco products.
But regardless of whether e-cigarettes are a “gateway” drug, there is no reason for adolescents to use a product for which the purported intent is to help adults quit smoking. To protect youths, the same sales, marketing, and use restrictions that apply to combustible cigarettes should – promptly and effectively – be applied to e-cigarettes.
The Food and Drug Administration should set a minimum age of sale, require health warnings on e-cigarettes, and consider regulatory activities such as banning e-cigarette flavorings and prohibiting advertising in youth-oriented media. And states and communities should restrict e-cigarette smoking in public places and workplaces to avoid normalizing the behavior.
Nancy A. Rigotti, M.D., is in the department of medicine at Massachusetts General Hospital and Harvard Medical School, Boston. She reported receiving grants and nonfinancial support from Pfizer, and nonfinancial support from Arena Pharmaceuticals. Dr. Rigotti made these remarks in an editorial accompanying Dr. Leventhal’s report (JAMA 2015;314[7]:673-4).
The study by Leventhal et al. presents the “strongest evidence to date” that e-cigarettes may pose a health hazard by encouraging adolescents to start smoking conventional tobacco products.
But regardless of whether e-cigarettes are a “gateway” drug, there is no reason for adolescents to use a product for which the purported intent is to help adults quit smoking. To protect youths, the same sales, marketing, and use restrictions that apply to combustible cigarettes should – promptly and effectively – be applied to e-cigarettes.
The Food and Drug Administration should set a minimum age of sale, require health warnings on e-cigarettes, and consider regulatory activities such as banning e-cigarette flavorings and prohibiting advertising in youth-oriented media. And states and communities should restrict e-cigarette smoking in public places and workplaces to avoid normalizing the behavior.
Nancy A. Rigotti, M.D., is in the department of medicine at Massachusetts General Hospital and Harvard Medical School, Boston. She reported receiving grants and nonfinancial support from Pfizer, and nonfinancial support from Arena Pharmaceuticals. Dr. Rigotti made these remarks in an editorial accompanying Dr. Leventhal’s report (JAMA 2015;314[7]:673-4).
The study by Leventhal et al. presents the “strongest evidence to date” that e-cigarettes may pose a health hazard by encouraging adolescents to start smoking conventional tobacco products.
But regardless of whether e-cigarettes are a “gateway” drug, there is no reason for adolescents to use a product for which the purported intent is to help adults quit smoking. To protect youths, the same sales, marketing, and use restrictions that apply to combustible cigarettes should – promptly and effectively – be applied to e-cigarettes.
The Food and Drug Administration should set a minimum age of sale, require health warnings on e-cigarettes, and consider regulatory activities such as banning e-cigarette flavorings and prohibiting advertising in youth-oriented media. And states and communities should restrict e-cigarette smoking in public places and workplaces to avoid normalizing the behavior.
Nancy A. Rigotti, M.D., is in the department of medicine at Massachusetts General Hospital and Harvard Medical School, Boston. She reported receiving grants and nonfinancial support from Pfizer, and nonfinancial support from Arena Pharmaceuticals. Dr. Rigotti made these remarks in an editorial accompanying Dr. Leventhal’s report (JAMA 2015;314[7]:673-4).
Ninth-graders who have used electronic cigarettes are much more likely than are nonusers to try regular cigarettes, cigars, and hookahs during the subsequent year, according to a report published online Aug. 18 in JAMA.
E-cigarettes are handheld battery-operated devices that heat a liquid composed of nicotine, propylene glycol or glycerin, flavorings, and other chemicals to create a vapor that is inhaled, simulating the experience of cigarette smoking. Their main potential benefit is to help adult smokers switch from using the more unhealthy combustible tobacco.
However, critics argue that adolescents who use e-cigarettes may be more likely to try other products that deliver nicotine, which would perpetuate the current epidemic of tobacco-related illness, said Adam M. Leventhal, Ph.D., of the department of preventive medicine, University of Southern California, Los Angeles, and his associates.
The investigators analyzed data from a longitudinal survey of substance use and mental health among high school students. In their prospective observational study, they focused on 2,530 demographically diverse students in ninth grade at 10 Los Angeles–area public high schools. The students were nonsmokers at baseline. A total of 222 of these adolescents reported that they had used e-cigarettes, while 2,308 had not.
Adolescents who had used e-cigarettes were much more likely than were nonusers to report trying combustible tobacco products during the next 6 months (30.7% vs 8.1%) and during the next 12 months (25.2% vs 9.3%), for an odds ratio of 4.27 averaged across the two study periods. This association was strong for each of the combustible tobacco products assessed, with an OR of 2.65 for regular cigarettes, an OR of 4.85 for full-size cigars or cigarillos, and an OR of 3.25 for hookahs.
When the data were adjusted to account for many sociodemographic, environmental, and intrapersonal characteristics known to influence smoking, the ORs declined but the associations remained strong and statistically significant, ranging from 1.75 to 2.96, depending on the smoking product, Dr. Leventhal and his associates said (JAMA. 2015;314[7]:700-707). One possible explanation for these findings is that adolescents who used e-cigarettes enjoyed the experience and were more likely to experiment with other nicotine-containing products. However, “because this is an observational study, and one of the first to address this issue, inferences regarding whether this association is or is not causal cannot yet be made,” they noted.
Ninth-graders who have used electronic cigarettes are much more likely than are nonusers to try regular cigarettes, cigars, and hookahs during the subsequent year, according to a report published online Aug. 18 in JAMA.
E-cigarettes are handheld battery-operated devices that heat a liquid composed of nicotine, propylene glycol or glycerin, flavorings, and other chemicals to create a vapor that is inhaled, simulating the experience of cigarette smoking. Their main potential benefit is to help adult smokers switch from using the more unhealthy combustible tobacco.
However, critics argue that adolescents who use e-cigarettes may be more likely to try other products that deliver nicotine, which would perpetuate the current epidemic of tobacco-related illness, said Adam M. Leventhal, Ph.D., of the department of preventive medicine, University of Southern California, Los Angeles, and his associates.
The investigators analyzed data from a longitudinal survey of substance use and mental health among high school students. In their prospective observational study, they focused on 2,530 demographically diverse students in ninth grade at 10 Los Angeles–area public high schools. The students were nonsmokers at baseline. A total of 222 of these adolescents reported that they had used e-cigarettes, while 2,308 had not.
Adolescents who had used e-cigarettes were much more likely than were nonusers to report trying combustible tobacco products during the next 6 months (30.7% vs 8.1%) and during the next 12 months (25.2% vs 9.3%), for an odds ratio of 4.27 averaged across the two study periods. This association was strong for each of the combustible tobacco products assessed, with an OR of 2.65 for regular cigarettes, an OR of 4.85 for full-size cigars or cigarillos, and an OR of 3.25 for hookahs.
When the data were adjusted to account for many sociodemographic, environmental, and intrapersonal characteristics known to influence smoking, the ORs declined but the associations remained strong and statistically significant, ranging from 1.75 to 2.96, depending on the smoking product, Dr. Leventhal and his associates said (JAMA. 2015;314[7]:700-707). One possible explanation for these findings is that adolescents who used e-cigarettes enjoyed the experience and were more likely to experiment with other nicotine-containing products. However, “because this is an observational study, and one of the first to address this issue, inferences regarding whether this association is or is not causal cannot yet be made,” they noted.
FROM JAMA
Key clinical point: Ninth-graders who use electronic cigarettes are much more likely than are nonusers to try regular cigarettes, cigars, and hookahs during the following year.
Major finding: Adolescents who had used e-cigarettes were much more likely than were nonusers to report trying combustible tobacco products during the next 6 months (30.7% vs. 8.1%) and during the next 12 months (25.2% vs. 9.3%), for an OR of 4.27 averaged across the two study periods.
Data source: A prospective observational study of 2,530 demographically diverse, nonsmoking ninth-graders at 10 Los Angeles public high schools who were followed up for 1 year.
Disclosures: The National Institutes of Health supported the study. Dr. Leventhal and his associates reported having no relevant disclosures.
In refractory asthma, think vocal cord dysfunction
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM