User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
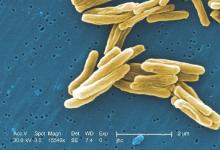
Number of TB-caused deaths fall, but disease still kills 1 million-plus
Tuberculosis (TB) mortality has fallen 47% since 1990, and the reporting on incidences of the disease has improved, says a global report by the World Health Organization (WHO). News about this disease is not all positive, however; TB continues to be one of the world’s deadliest diseases and many cases of TB went unreported last year, according to the WHO report.
Most improvements in mortality rate for TB patients occurred at the beginning of the 21st century, when the United Nations established the Millennium Development Goals, says the report. Such goals included halting and reversing TB incidence on a worldwide basis, in each of the 6 WHO regions, and in 16 of the 22 high-burden countries that collectively account for 80% of TB cases.
“In all, effective diagnosis and treatment of TB saved an estimated 43 million lives between 2000 and 2014,” says the report.
Better reporting on TB’s prevalence led to the first increase in the number of TB cases reported since 2007.
“The annual total of new TB cases, which had been about 5.7 million until 2013, rose to slightly more than 6 million in 2014 (an increase of 6%). This was mostly due to a 29% increase in notification in India, which followed the introduction of a policy of mandatory notification in May 2012, creation of a national Web-based reporting system in June 2012, and intensified efforts to engage the private health sector,” according to the report.
Despite these improvements in data collection of TB incidents, 37% of new TB cases were undiagnosed or not reported last year, with 9.6 million people having fallen sick to TB during a year when just 6 million new cases were reported, according to estimates. Regarding multidrug-resistant TB cases specifically, only 123,000 of an estimated 480,000 cases were detected and reported.
As for the deadliness of the disease, TB killed 1.5 million people in 2014.
Read the full report on the WHO website.
Tuberculosis (TB) mortality has fallen 47% since 1990, and the reporting on incidences of the disease has improved, says a global report by the World Health Organization (WHO). News about this disease is not all positive, however; TB continues to be one of the world’s deadliest diseases and many cases of TB went unreported last year, according to the WHO report.
Most improvements in mortality rate for TB patients occurred at the beginning of the 21st century, when the United Nations established the Millennium Development Goals, says the report. Such goals included halting and reversing TB incidence on a worldwide basis, in each of the 6 WHO regions, and in 16 of the 22 high-burden countries that collectively account for 80% of TB cases.
“In all, effective diagnosis and treatment of TB saved an estimated 43 million lives between 2000 and 2014,” says the report.
Better reporting on TB’s prevalence led to the first increase in the number of TB cases reported since 2007.
“The annual total of new TB cases, which had been about 5.7 million until 2013, rose to slightly more than 6 million in 2014 (an increase of 6%). This was mostly due to a 29% increase in notification in India, which followed the introduction of a policy of mandatory notification in May 2012, creation of a national Web-based reporting system in June 2012, and intensified efforts to engage the private health sector,” according to the report.
Despite these improvements in data collection of TB incidents, 37% of new TB cases were undiagnosed or not reported last year, with 9.6 million people having fallen sick to TB during a year when just 6 million new cases were reported, according to estimates. Regarding multidrug-resistant TB cases specifically, only 123,000 of an estimated 480,000 cases were detected and reported.
As for the deadliness of the disease, TB killed 1.5 million people in 2014.
Read the full report on the WHO website.
Tuberculosis (TB) mortality has fallen 47% since 1990, and the reporting on incidences of the disease has improved, says a global report by the World Health Organization (WHO). News about this disease is not all positive, however; TB continues to be one of the world’s deadliest diseases and many cases of TB went unreported last year, according to the WHO report.
Most improvements in mortality rate for TB patients occurred at the beginning of the 21st century, when the United Nations established the Millennium Development Goals, says the report. Such goals included halting and reversing TB incidence on a worldwide basis, in each of the 6 WHO regions, and in 16 of the 22 high-burden countries that collectively account for 80% of TB cases.
“In all, effective diagnosis and treatment of TB saved an estimated 43 million lives between 2000 and 2014,” says the report.
Better reporting on TB’s prevalence led to the first increase in the number of TB cases reported since 2007.
“The annual total of new TB cases, which had been about 5.7 million until 2013, rose to slightly more than 6 million in 2014 (an increase of 6%). This was mostly due to a 29% increase in notification in India, which followed the introduction of a policy of mandatory notification in May 2012, creation of a national Web-based reporting system in June 2012, and intensified efforts to engage the private health sector,” according to the report.
Despite these improvements in data collection of TB incidents, 37% of new TB cases were undiagnosed or not reported last year, with 9.6 million people having fallen sick to TB during a year when just 6 million new cases were reported, according to estimates. Regarding multidrug-resistant TB cases specifically, only 123,000 of an estimated 480,000 cases were detected and reported.
As for the deadliness of the disease, TB killed 1.5 million people in 2014.
Read the full report on the WHO website.
FDA approves mepolizumab for use in combination with other asthma drugs
Nucala (mepolizumab) has been approved for use with other asthma medicines as maintenance therapy for patients aged 12 years and older with a history of asthma exacerbations despite adherence with their current asthma medicines, the U.S. Food and Drug Administration announced Nov. 4.
“This approval offers patients with severe asthma an additional therapy when current treatments cannot maintain adequate control of their asthma,” Dr. Badrul Chowdhury, director of the Division of Pulmonary, Allergy, and Rheumatology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Nucala is a humanized interleukin-5 antagonist monoclonal antibody that limits severe asthma attacks by reducing the levels of blood eosinophils. Nucala is administered subcutaneously once every 4 weeks by a health care professional.
This innovation in precision medicine is the first and only approved, biologic therapy specifically developed for people with severe asthma with an eosinophilic phenotype, according to a statement from GlaxoSmithKline, the maker of Nucala.
The safety and efficacy of Nucala were established in three double-blind, randomized, placebo‑controlled trials in patients with severe asthma on currently available therapies. Nucala or a placebo was administered to patients every 4 weeks as an add-on asthma treatment. Compared with placebo, patients with severe asthma receiving Nucala had fewer exacerbations requiring hospitalization or emergency department visits, and a longer time to their first exacerbation. In addition, patients with severe asthma receiving Nucala experienced greater reductions in their daily maintenance oral corticosteroid dose, while maintaining asthma control, compared with patients receiving placebo. Treatment with mepolizumab did not result in a significant improvement in lung function, as measured by the volume of air exhaled by patients in 1 second, the FDA said in their statement.
The most common side effects of Nucala include headache, injection site reactions, back pain, and weakness. Hypersensitivity reactions can occur within hours or days of receiving Nucala.
Nucala (mepolizumab) has been approved for use with other asthma medicines as maintenance therapy for patients aged 12 years and older with a history of asthma exacerbations despite adherence with their current asthma medicines, the U.S. Food and Drug Administration announced Nov. 4.
“This approval offers patients with severe asthma an additional therapy when current treatments cannot maintain adequate control of their asthma,” Dr. Badrul Chowdhury, director of the Division of Pulmonary, Allergy, and Rheumatology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Nucala is a humanized interleukin-5 antagonist monoclonal antibody that limits severe asthma attacks by reducing the levels of blood eosinophils. Nucala is administered subcutaneously once every 4 weeks by a health care professional.
This innovation in precision medicine is the first and only approved, biologic therapy specifically developed for people with severe asthma with an eosinophilic phenotype, according to a statement from GlaxoSmithKline, the maker of Nucala.
The safety and efficacy of Nucala were established in three double-blind, randomized, placebo‑controlled trials in patients with severe asthma on currently available therapies. Nucala or a placebo was administered to patients every 4 weeks as an add-on asthma treatment. Compared with placebo, patients with severe asthma receiving Nucala had fewer exacerbations requiring hospitalization or emergency department visits, and a longer time to their first exacerbation. In addition, patients with severe asthma receiving Nucala experienced greater reductions in their daily maintenance oral corticosteroid dose, while maintaining asthma control, compared with patients receiving placebo. Treatment with mepolizumab did not result in a significant improvement in lung function, as measured by the volume of air exhaled by patients in 1 second, the FDA said in their statement.
The most common side effects of Nucala include headache, injection site reactions, back pain, and weakness. Hypersensitivity reactions can occur within hours or days of receiving Nucala.
Nucala (mepolizumab) has been approved for use with other asthma medicines as maintenance therapy for patients aged 12 years and older with a history of asthma exacerbations despite adherence with their current asthma medicines, the U.S. Food and Drug Administration announced Nov. 4.
“This approval offers patients with severe asthma an additional therapy when current treatments cannot maintain adequate control of their asthma,” Dr. Badrul Chowdhury, director of the Division of Pulmonary, Allergy, and Rheumatology Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Nucala is a humanized interleukin-5 antagonist monoclonal antibody that limits severe asthma attacks by reducing the levels of blood eosinophils. Nucala is administered subcutaneously once every 4 weeks by a health care professional.
This innovation in precision medicine is the first and only approved, biologic therapy specifically developed for people with severe asthma with an eosinophilic phenotype, according to a statement from GlaxoSmithKline, the maker of Nucala.
The safety and efficacy of Nucala were established in three double-blind, randomized, placebo‑controlled trials in patients with severe asthma on currently available therapies. Nucala or a placebo was administered to patients every 4 weeks as an add-on asthma treatment. Compared with placebo, patients with severe asthma receiving Nucala had fewer exacerbations requiring hospitalization or emergency department visits, and a longer time to their first exacerbation. In addition, patients with severe asthma receiving Nucala experienced greater reductions in their daily maintenance oral corticosteroid dose, while maintaining asthma control, compared with patients receiving placebo. Treatment with mepolizumab did not result in a significant improvement in lung function, as measured by the volume of air exhaled by patients in 1 second, the FDA said in their statement.
The most common side effects of Nucala include headache, injection site reactions, back pain, and weakness. Hypersensitivity reactions can occur within hours or days of receiving Nucala.
CHEST: Catheter-directed thrombolysis shows pulmonary embolism efficacy
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 U.S. patients.
The review also found evidence that U.S. pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 U.S. clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national U.S. registry of hospitalized patients, Dr. Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score–matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr. Saqib, a researcher at Staten Island (N.Y.) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,” Dr. Saqib said.
The U.S. data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
“We need to more systematically identify the patients with an acute PE who could benefit from catheter-directed thrombolysis, especially patients with a massive PE,” commented Dr. Muthiah P. Muthiah, a critical-care medicine physician at the University of Tennessee Health Science Center in Memphis. “This may be something to offer to patients who have an absolute contraindication for systemic thrombolysis, such as recent surgery, but it is not available everywhere,” Dr. Muthiah said in an interview.
Dr. Saqib and her associates used data collected by the Federal National Inpatient Sample. Among U.S. patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score–adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr. Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr. Saqib said.
Dr. Saqib and Dr. Muthiah had no disclosures.
On Twitter @mitchelzoler
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 U.S. patients.
The review also found evidence that U.S. pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 U.S. clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national U.S. registry of hospitalized patients, Dr. Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score–matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr. Saqib, a researcher at Staten Island (N.Y.) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,” Dr. Saqib said.
The U.S. data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
“We need to more systematically identify the patients with an acute PE who could benefit from catheter-directed thrombolysis, especially patients with a massive PE,” commented Dr. Muthiah P. Muthiah, a critical-care medicine physician at the University of Tennessee Health Science Center in Memphis. “This may be something to offer to patients who have an absolute contraindication for systemic thrombolysis, such as recent surgery, but it is not available everywhere,” Dr. Muthiah said in an interview.
Dr. Saqib and her associates used data collected by the Federal National Inpatient Sample. Among U.S. patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score–adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr. Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr. Saqib said.
Dr. Saqib and Dr. Muthiah had no disclosures.
On Twitter @mitchelzoler
MONTREAL – Catheter-directed thrombolysis surpassed systemic thrombolysis for minimizing in-hospital mortality of patients with an acute pulmonary embolism in a review of more than 1,500 U.S. patients.
The review also found evidence that U.S. pulmonary embolism (PE) patients increasingly undergo catheter-directed thrombolysis, with usage jumping by more than 50% from 2010 to 2012, although in 2012 U.S. clinicians performed catheter-directed thrombolysis on 160 patients with an acute pulmonary embolism (PE) who were included in a national U.S. registry of hospitalized patients, Dr. Amina Saqib said at the annual meeting of the American College of Chest Physicians.
Catheter-directed thrombolysis resulted in a 9% in-hospital mortality rate and a 10% combined rate of in-hospital mortality plus intracerebral hemorrhages, rates significantly below those tallied in propensity score–matched patients who underwent systemic thrombolysis of their acute PE. The matched group with systemic thrombolysis had a 17% in-hospital mortality rate and a 17% combined mortality plus intracerebral hemorrhage rate, said Dr. Saqib, a researcher at Staten Island (N.Y.) University Hospital.
“To the best of our knowledge, this is the first, large, nationwide, observational study that compared safety and efficacy outcomes between systemic thrombolysis and catheter-directed thrombolysis in acute PE,” Dr. Saqib said.
The U.S. data, collected during 2010-2012, also showed that, after adjustment for clinical and demographic variables, each acute PE treatment by catheter-directed thrombolysis cost an average $9,428 above the cost for systemic thrombolysis, she said.
“We need to more systematically identify the patients with an acute PE who could benefit from catheter-directed thrombolysis, especially patients with a massive PE,” commented Dr. Muthiah P. Muthiah, a critical-care medicine physician at the University of Tennessee Health Science Center in Memphis. “This may be something to offer to patients who have an absolute contraindication for systemic thrombolysis, such as recent surgery, but it is not available everywhere,” Dr. Muthiah said in an interview.
Dr. Saqib and her associates used data collected by the Federal National Inpatient Sample. Among U.S. patients hospitalized during 2010-2012 and entered into this database, they identified 1,169 adult acute PE patients who underwent systemic thrombolysis and 352 patients who received catheter-directed thrombolysis. The patients averaged about 58 years old and just under half were men.
The propensity score–adjusted analysis also showed no statistically significant difference between the two treatment approaches for the incidence of intracerebral hemorrhage, any hemorrhages requiring a transfusion, new-onset acute renal failure, or hospital length of stay. Among the patients treated by catheter-directed thrombolysis, all the intracerebral hemorrhages occurred during 2010; during 2011 and 2012 none of the patients treated this way had an intracerebral hemorrhage, Dr. Saqib noted.
Although the findings were consistent with results from prior analyses, the propensity-score adjustment used in the current study cannot fully account for all unmeasured confounding factors. The best way to compare catheter-directed thrombolysis and systemic thrombolysis for treating acute PE would be in a prospective, randomized study, Dr. Saqib said.
Dr. Saqib and Dr. Muthiah had no disclosures.
On Twitter @mitchelzoler
AT CHEST 2015
Key clinical point: Catheter-directed thrombolysis was linked to reduced mortality, compared with systemic thrombolysis in patients with an acute pulmonary embolism.
Major finding: In-hospital mortality in acute pulmonary embolism patients ran 10% with catheter-directed thrombolysis and 17% with systemic thrombolysis.
Data source: Review of 1,521 U.S. patients treated for acute pulmonary embolism during 2010-2012 in the National Inpatient Sample.
Disclosures: Dr. Saqib and Dr. Muthiah had no disclosures.
AHA Releases First-ever Pediatric Pulmonary Hypertension Guideline
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
FROM CIRCULATION
AHA releases first-ever pediatric pulmonary hypertension guideline
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The pediatric pulmonary, pediatric cardiology, and neonatal and pediatric intensivists all have greatly anticipated directions for the care of pediatric pulmonary hypertension. The guidelines have excellent care maps for the diagnosis and evaluation of the various etiologies of pulmonary hypertension.
The new guidelines also should help also with insurance authorizations for the expensive medications for pulmonary hypertension! Dr. Robyn J. Barst, a renowned leader in pediatric pulmonary hypertension, who passed away in 2013, would be so proud of this AHA guideline!
Dr. Susan L. Millard is director of research, pediatric pulmonary & sleep medicine at Helen DeVos Children’s Hospital in Grand Rapids, MI.
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
The American Heart Association and the American Thoracic Society jointly released the first-ever clinical practice guideline for assessing and managing pulmonary hypertension (PH) in the pediatric population, which was published online Nov. 3 in Circulation.
The two organizations developed this guideline because the causes and treatments of PH in neonates, infants, and children are often different from those in adults. The literature for adult PH is “robust,” and there are several treatment guidelines available, whereas pediatric PH has not been well studied, “and little is understood about the natural history, fundamental mechanisms, and treatment of childhood PH,” said Dr. Steven H. Abman, cochair of the guideline committee and a pediatric pulmonologist at the University of Colorado and Children’s Hospital, both in Denver.
“It’s important to note that, although these guidelines provide a foundation for taking care of children with pulmonary hypertension, we still have a huge need for more specific data and research to further improve outcomes,” he said in a statement accompanying the guideline.
This guideline was developed by a working group of 27 clinicians and researchers with expertise in pediatric pulmonology, pediatric and adult cardiology, pediatric intensivism, neonatology, and translational science. They reviewed more than 600 articles in the literature, but given the paucity of high-quality data regarding pediatric PH, the guideline relies heavily on expert opinion and primarily describes “generally acceptable approaches” to diagnosis and management; more specific and detailed recommendations await the findings of future research, Dr. Abman and his associates said (Circulation. 2015 Oct 26. doi:10.1161/CIR.0000000000000329).
In the pediatric population, PH is defined as a resting mean pulmonary artery pressure greater than 25 mm Hg after the first few months of life and is usually related to cardiac, lung, or systemic diseases. Idiopathic PH, a pulmonary vasculopathy, is a diagnosis of exclusion after diseases of the left side of the heart, lung parenchyma, heart valves, thromboembolism, and other miscellaneous causes have been ruled out.
The guideline emphasizes that children thought to have PH should be evaluated and treated at comprehensive, multidisciplinary clinics at specialized pediatric centers. “When children are diagnosed, parents often feel helpless. However, it’s important that parents seek doctors and centers that see these children on a regular basis and can offer them access to new molecular diagnostics, new drug therapies, and new devices, as well as surgeries that have recently been developed,” Dr. Stephen L. Archer, cochair of the guideline committee and head of medicine at Queen’s University, Kingston, Ont., said in the statement.
“These children suffer with health issues throughout their lives or die prematurely, particularly if they’re not properly diagnosed and managed. But with the proper diagnosis and treatment at a specialized center for PH, the prognosis for many of these children is excellent,” he noted.
Properly classifying the type of PH is a key first step in determining treatment. The guideline addresses numerous methods for diagnosing and monitoring PH, including imaging studies, echocardiograms, cardiac catheterization, brain natriuretic peptide and other laboratory testing, 6-minute walk distance (at appropriate ages), sleep studies, and genetic testing. It specifically deals with persistent PH of the newborn and PH arising from congenital diaphragmatic hernia; bronchopulmonary dysplasia or other lung diseases; heart disease such as atrial-septal defect or patent ductus arteriosus; and systemic diseases such as hemolytic hemoglobinopathies and hepatic, renal, or metabolic illness; as well as idiopathic PH and PH related to high-altitude pulmonary edema.
Regarding ongoing outpatient care, the guideline recommends that children with PH receive influenza and pneumococcal vaccinations and prophylaxis for respiratory syncytial virus (if they are eligible), as well as antibiotic prophylaxis to prevent subacute bacterial endocarditis in those who are cyanotic or have indwelling central lines. Growth must be monitored rigorously, and infections and respiratory illnesses must be recognized and treated promptly. Any surgeries require careful preoperative planning and should be performed at hospitals with expertise in PH.
The guideline includes an extensive section on pharmacotherapy for childhood PH, including the use of digitalis, diuretics, long-term anticoagulation, oxygen therapy, calcium channel blockers, phosphodiesterase type 5 inhibitors, endothelin receptor antagonists, intravenous and subcutaneous prostacyclin therapy, and the transition from parenteral to oral or inhaled treatment.
In addition, the guideline addresses exercise and sports participation, travel restrictions, and contraceptive counseling for adolescent patients. Finally, “given the impact of childhood PH on the entire family, [patients], siblings, and caregivers should be assessed for psychosocial stress and be readily provided support and referral as needed,” the guideline recommends.
A copy of the guideline is available at http://my.americanheart.org/statements.
FROM CIRCULATION
VIDEO: MMF equals cyclophosphamide’s efficacy in sclerodermal lung disease
MONTREAL – The immunosuppressant mycophenolate mofetil worked as effectively as cyclophosphamide for treating scleroderma-related interstitial lung disease while being better tolerated and causing fewer adverse effects in a multicenter, head-to-head comparison with 142 randomized patients.
“The findings support the increasingly common clinical practice of prescribing MMF [mycophenolate mofetil] for this disease,” said Dr. Donald P. Tashkin at the annual meeting of the American College of Chest Physicians.
Another limitation of cyclophosphamide is that it is usually not used for more than 1 year because of concerns that longer use substantially increases a patient’s risk for developing malignancy. That’s another reason why there is a “strong need for longer and safer immunosuppressive treatment with a drug like MMF,” said Dr. Tashkin, a pulmonologist at the University of California, Los Angeles.
When used in this trial on patients with scleroderma, as defined by the American College of Rheumatology and with a baseline forced vital capacity of no more than 80% of predicted, “MMF was effective at reducing the rate of decline in vital capacity, improving symptoms such as dyspnea – the cardinal symptom of interstitial lung disease, and reducing lung fibrosis seen on CT scans, and MMF was better tolerated” than cyclophosphamide, Dr. Tashkin said in an interview. Cyclophosphamide treatment in this new trial “was associated with more toxicity, especially hematologic toxicity, an was not nearly as well tolerated, with more patients withdrawing because of side effects or a perceived lack of benefit.”
“Cyclophosphamide has a lot of side effects. MMF is just now coming into increased use. I think we’ll see it being used more for first-line treatment because the side effects with cyclophosphamide are so bad,” commented Dr. Thomas Fuhrman, chief of anesthesiology at the Bay Pines (Fla.) VA Healthcare System.
Dr. Tashkin and his associates conceived the Scleroderma Lung Study II (SLSII) as a follow-up to the first SLS run about a decade ago that compared cyclosphosphamide against placebo for controlling progression of interstitial lung disease in scleroderma patients. The results from the first SLS trial established cyclosphosphamide as a treatment that could preserve forced vital capacity percent predicted in patients with scleroderma-induced interstitial lung disease (N Engl J Med. 2006 Jun 22;354[25]:2655-666).
For the new study they enrolled patients who averaged 52 years old, with an average scleroderma duration of almost 3 years. Their average percent predicted forced vital capacity was 67%, and their baseline dyspnea index was 7.1.
Patients received either a target oral MMF dosage of 1.5 g b.i.d. for 2 years, or a target cyclophosphamide dosage of 2 mg/kg/day for up to 1 year, followed by a year of placebo. Cyclophosphamide treatment was capped at 1 year to protect against causing malignancy. Among the 73 patients randomized to the cyclophosphamide arm, 58 had data available after 12 months with 48 patients continuing on cyclophosphamide, and 53 had data available out to 2 years, with 37 patients remaining on their assigned regimen. Among 69 patients randomized to MMF 58 had data available after 12 months with 53 continuing on MMF, and 53 patients had data available through 24 months with 49 remaining on their MMF regimen.
After 24 months, the average percent predicted forced vital capacity, the study’s primary endpoint, had increased by 3.3% among patients on MMF and 3.0% among those in the cyclophosphamide arm in an intention-to-treat analysis, a nonsignificant difference. After 24 months 72% of patients in the MMF arm and 65% in the cyclophosphamide arm had a positive change, compared with baseline, in their percent predicted forced vital capacity, Dr. Tashkin reported.
MMF also showed a superior overall safety profile. Patients on cyclophosphamide had a significantly increased rate of withdrawal from the study medication. Drug discontinuations occurred in 36 of the cyclophosphamide patients and in 20 of those on MMF. Serious adverse events attributable to study medication occurred in eight patients on cyclophosphamide and three patients on MMF. The most frequent protocol-defined adverse event was leukopenia, which occurred in 30 patients on cyclophosphamide and four patients on MMF.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
MONTREAL – The immunosuppressant mycophenolate mofetil worked as effectively as cyclophosphamide for treating scleroderma-related interstitial lung disease while being better tolerated and causing fewer adverse effects in a multicenter, head-to-head comparison with 142 randomized patients.
“The findings support the increasingly common clinical practice of prescribing MMF [mycophenolate mofetil] for this disease,” said Dr. Donald P. Tashkin at the annual meeting of the American College of Chest Physicians.
Another limitation of cyclophosphamide is that it is usually not used for more than 1 year because of concerns that longer use substantially increases a patient’s risk for developing malignancy. That’s another reason why there is a “strong need for longer and safer immunosuppressive treatment with a drug like MMF,” said Dr. Tashkin, a pulmonologist at the University of California, Los Angeles.
When used in this trial on patients with scleroderma, as defined by the American College of Rheumatology and with a baseline forced vital capacity of no more than 80% of predicted, “MMF was effective at reducing the rate of decline in vital capacity, improving symptoms such as dyspnea – the cardinal symptom of interstitial lung disease, and reducing lung fibrosis seen on CT scans, and MMF was better tolerated” than cyclophosphamide, Dr. Tashkin said in an interview. Cyclophosphamide treatment in this new trial “was associated with more toxicity, especially hematologic toxicity, an was not nearly as well tolerated, with more patients withdrawing because of side effects or a perceived lack of benefit.”
“Cyclophosphamide has a lot of side effects. MMF is just now coming into increased use. I think we’ll see it being used more for first-line treatment because the side effects with cyclophosphamide are so bad,” commented Dr. Thomas Fuhrman, chief of anesthesiology at the Bay Pines (Fla.) VA Healthcare System.
Dr. Tashkin and his associates conceived the Scleroderma Lung Study II (SLSII) as a follow-up to the first SLS run about a decade ago that compared cyclosphosphamide against placebo for controlling progression of interstitial lung disease in scleroderma patients. The results from the first SLS trial established cyclosphosphamide as a treatment that could preserve forced vital capacity percent predicted in patients with scleroderma-induced interstitial lung disease (N Engl J Med. 2006 Jun 22;354[25]:2655-666).
For the new study they enrolled patients who averaged 52 years old, with an average scleroderma duration of almost 3 years. Their average percent predicted forced vital capacity was 67%, and their baseline dyspnea index was 7.1.
Patients received either a target oral MMF dosage of 1.5 g b.i.d. for 2 years, or a target cyclophosphamide dosage of 2 mg/kg/day for up to 1 year, followed by a year of placebo. Cyclophosphamide treatment was capped at 1 year to protect against causing malignancy. Among the 73 patients randomized to the cyclophosphamide arm, 58 had data available after 12 months with 48 patients continuing on cyclophosphamide, and 53 had data available out to 2 years, with 37 patients remaining on their assigned regimen. Among 69 patients randomized to MMF 58 had data available after 12 months with 53 continuing on MMF, and 53 patients had data available through 24 months with 49 remaining on their MMF regimen.
After 24 months, the average percent predicted forced vital capacity, the study’s primary endpoint, had increased by 3.3% among patients on MMF and 3.0% among those in the cyclophosphamide arm in an intention-to-treat analysis, a nonsignificant difference. After 24 months 72% of patients in the MMF arm and 65% in the cyclophosphamide arm had a positive change, compared with baseline, in their percent predicted forced vital capacity, Dr. Tashkin reported.
MMF also showed a superior overall safety profile. Patients on cyclophosphamide had a significantly increased rate of withdrawal from the study medication. Drug discontinuations occurred in 36 of the cyclophosphamide patients and in 20 of those on MMF. Serious adverse events attributable to study medication occurred in eight patients on cyclophosphamide and three patients on MMF. The most frequent protocol-defined adverse event was leukopenia, which occurred in 30 patients on cyclophosphamide and four patients on MMF.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
MONTREAL – The immunosuppressant mycophenolate mofetil worked as effectively as cyclophosphamide for treating scleroderma-related interstitial lung disease while being better tolerated and causing fewer adverse effects in a multicenter, head-to-head comparison with 142 randomized patients.
“The findings support the increasingly common clinical practice of prescribing MMF [mycophenolate mofetil] for this disease,” said Dr. Donald P. Tashkin at the annual meeting of the American College of Chest Physicians.
Another limitation of cyclophosphamide is that it is usually not used for more than 1 year because of concerns that longer use substantially increases a patient’s risk for developing malignancy. That’s another reason why there is a “strong need for longer and safer immunosuppressive treatment with a drug like MMF,” said Dr. Tashkin, a pulmonologist at the University of California, Los Angeles.
When used in this trial on patients with scleroderma, as defined by the American College of Rheumatology and with a baseline forced vital capacity of no more than 80% of predicted, “MMF was effective at reducing the rate of decline in vital capacity, improving symptoms such as dyspnea – the cardinal symptom of interstitial lung disease, and reducing lung fibrosis seen on CT scans, and MMF was better tolerated” than cyclophosphamide, Dr. Tashkin said in an interview. Cyclophosphamide treatment in this new trial “was associated with more toxicity, especially hematologic toxicity, an was not nearly as well tolerated, with more patients withdrawing because of side effects or a perceived lack of benefit.”
“Cyclophosphamide has a lot of side effects. MMF is just now coming into increased use. I think we’ll see it being used more for first-line treatment because the side effects with cyclophosphamide are so bad,” commented Dr. Thomas Fuhrman, chief of anesthesiology at the Bay Pines (Fla.) VA Healthcare System.
Dr. Tashkin and his associates conceived the Scleroderma Lung Study II (SLSII) as a follow-up to the first SLS run about a decade ago that compared cyclosphosphamide against placebo for controlling progression of interstitial lung disease in scleroderma patients. The results from the first SLS trial established cyclosphosphamide as a treatment that could preserve forced vital capacity percent predicted in patients with scleroderma-induced interstitial lung disease (N Engl J Med. 2006 Jun 22;354[25]:2655-666).
For the new study they enrolled patients who averaged 52 years old, with an average scleroderma duration of almost 3 years. Their average percent predicted forced vital capacity was 67%, and their baseline dyspnea index was 7.1.
Patients received either a target oral MMF dosage of 1.5 g b.i.d. for 2 years, or a target cyclophosphamide dosage of 2 mg/kg/day for up to 1 year, followed by a year of placebo. Cyclophosphamide treatment was capped at 1 year to protect against causing malignancy. Among the 73 patients randomized to the cyclophosphamide arm, 58 had data available after 12 months with 48 patients continuing on cyclophosphamide, and 53 had data available out to 2 years, with 37 patients remaining on their assigned regimen. Among 69 patients randomized to MMF 58 had data available after 12 months with 53 continuing on MMF, and 53 patients had data available through 24 months with 49 remaining on their MMF regimen.
After 24 months, the average percent predicted forced vital capacity, the study’s primary endpoint, had increased by 3.3% among patients on MMF and 3.0% among those in the cyclophosphamide arm in an intention-to-treat analysis, a nonsignificant difference. After 24 months 72% of patients in the MMF arm and 65% in the cyclophosphamide arm had a positive change, compared with baseline, in their percent predicted forced vital capacity, Dr. Tashkin reported.
MMF also showed a superior overall safety profile. Patients on cyclophosphamide had a significantly increased rate of withdrawal from the study medication. Drug discontinuations occurred in 36 of the cyclophosphamide patients and in 20 of those on MMF. Serious adverse events attributable to study medication occurred in eight patients on cyclophosphamide and three patients on MMF. The most frequent protocol-defined adverse event was leukopenia, which occurred in 30 patients on cyclophosphamide and four patients on MMF.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT CHEST 2015
Key clinical point: Mycophenolate mofetil controlled scleroderma-induced interstitial lung disease as well as cyclosphosphamide did but with reduced toxicity.
Major finding: Average percent predicted forced vital capacity rose 3.0% in patients treated with cyclosphosphamide and 3.3% in those on MMF.
Data source: SLSII, a randomized trial that enrolled 142 scleroderma patients at 13 U.S. centers.
Disclosures: SLSII received partial funding from Hoffman-La Roche, a company that markets a formulation of mycophenolate mofetil (CellCept). Dr. Tashkin had no disclosures. Dr. Fuhrman had no disclosures.
Pediatric pertussis tied to minor elevation in epilepsy risk
Danish researchers reported a slightly heightened vulnerability to child-onset epilepsy in infants who contract pertussis, which strikes an estimated 16 million children globally on an annual basis, in a study published in the Nov. 3 issue of JAMA.
Dr. Morten Olsen of the department of clinical epidemiology, Aarhus (Denmark) University Hospital, and his colleagues collected data from population-based medical registries encompassing every hospital and citizen in Denmark (roughly 5.6 million people) to catalogue all patients presenting with pertussis born between 1978 and 2011. Subjects were tracked for a maximum of 15 years, beginning with their respective initial pertussis diagnosis dates, up until their first-time epilepsy diagnosis, emigration, death, or Dec. 31, 2011 (whichever occurred first). To establish a control cohort, the national Danish Civil Registration System database was mined to identify and select 10 age- and sex-matched individuals from the general population for each patient with pertussis (JAMA. 2015 Nov 3;314[17]:1844-9).
Of the 4,700 identified pertussis patients (53% of whom were younger than 6 months of age when initially diagnosed with pertussis), 90 (2%) subsequently developed epilepsy (incidence rate, 1.56/1,000 person-years; 95% confidence interval, 1.55-1.57), compared with 511 (0.1%) in the 47,000-subject comparison arm (incidence rate, 0.88/1,000 person-years; 95% CI, 0.88-0.88). Pertussis patients were found to have a cumulative epilepsy incidence rate of 1.7% (95% CI, 1.4%-2.1%) at age 10 years; cumulative epilepsy incidence at age 10 years was 0.9% (95% CI, 0.8%-1%) in the control population. Moreover, epilepsy risk was demonstrated to be dependent on age of pertussis onset; a pertussis diagnosis was not associated with increased epilepsy risk in patients over the age of 3 years (hazard ratio, 1; 95% CI, 0.5-1.8).
According to study investigators, one explanation for the role that pertussis could potentially play in the pathophysiology of epilepsy may center on the occurrence of hypoxic brain damage resulting from severe pertussis-related coughing, “perhaps via increased intrathoracic and intra-abdominal pressure and central nervous system hemorrhages.”
The study was funded by the Program for Clinical Research Infrastructure established by the Lundbeck Foundation and the Novo Nordisk Foundation. The department of clinical epidemiology, Aarhus (Denmark) University Hospital, receives funding for other studies from companies in the form of research grants.
Danish researchers reported a slightly heightened vulnerability to child-onset epilepsy in infants who contract pertussis, which strikes an estimated 16 million children globally on an annual basis, in a study published in the Nov. 3 issue of JAMA.
Dr. Morten Olsen of the department of clinical epidemiology, Aarhus (Denmark) University Hospital, and his colleagues collected data from population-based medical registries encompassing every hospital and citizen in Denmark (roughly 5.6 million people) to catalogue all patients presenting with pertussis born between 1978 and 2011. Subjects were tracked for a maximum of 15 years, beginning with their respective initial pertussis diagnosis dates, up until their first-time epilepsy diagnosis, emigration, death, or Dec. 31, 2011 (whichever occurred first). To establish a control cohort, the national Danish Civil Registration System database was mined to identify and select 10 age- and sex-matched individuals from the general population for each patient with pertussis (JAMA. 2015 Nov 3;314[17]:1844-9).
Of the 4,700 identified pertussis patients (53% of whom were younger than 6 months of age when initially diagnosed with pertussis), 90 (2%) subsequently developed epilepsy (incidence rate, 1.56/1,000 person-years; 95% confidence interval, 1.55-1.57), compared with 511 (0.1%) in the 47,000-subject comparison arm (incidence rate, 0.88/1,000 person-years; 95% CI, 0.88-0.88). Pertussis patients were found to have a cumulative epilepsy incidence rate of 1.7% (95% CI, 1.4%-2.1%) at age 10 years; cumulative epilepsy incidence at age 10 years was 0.9% (95% CI, 0.8%-1%) in the control population. Moreover, epilepsy risk was demonstrated to be dependent on age of pertussis onset; a pertussis diagnosis was not associated with increased epilepsy risk in patients over the age of 3 years (hazard ratio, 1; 95% CI, 0.5-1.8).
According to study investigators, one explanation for the role that pertussis could potentially play in the pathophysiology of epilepsy may center on the occurrence of hypoxic brain damage resulting from severe pertussis-related coughing, “perhaps via increased intrathoracic and intra-abdominal pressure and central nervous system hemorrhages.”
The study was funded by the Program for Clinical Research Infrastructure established by the Lundbeck Foundation and the Novo Nordisk Foundation. The department of clinical epidemiology, Aarhus (Denmark) University Hospital, receives funding for other studies from companies in the form of research grants.
Danish researchers reported a slightly heightened vulnerability to child-onset epilepsy in infants who contract pertussis, which strikes an estimated 16 million children globally on an annual basis, in a study published in the Nov. 3 issue of JAMA.
Dr. Morten Olsen of the department of clinical epidemiology, Aarhus (Denmark) University Hospital, and his colleagues collected data from population-based medical registries encompassing every hospital and citizen in Denmark (roughly 5.6 million people) to catalogue all patients presenting with pertussis born between 1978 and 2011. Subjects were tracked for a maximum of 15 years, beginning with their respective initial pertussis diagnosis dates, up until their first-time epilepsy diagnosis, emigration, death, or Dec. 31, 2011 (whichever occurred first). To establish a control cohort, the national Danish Civil Registration System database was mined to identify and select 10 age- and sex-matched individuals from the general population for each patient with pertussis (JAMA. 2015 Nov 3;314[17]:1844-9).
Of the 4,700 identified pertussis patients (53% of whom were younger than 6 months of age when initially diagnosed with pertussis), 90 (2%) subsequently developed epilepsy (incidence rate, 1.56/1,000 person-years; 95% confidence interval, 1.55-1.57), compared with 511 (0.1%) in the 47,000-subject comparison arm (incidence rate, 0.88/1,000 person-years; 95% CI, 0.88-0.88). Pertussis patients were found to have a cumulative epilepsy incidence rate of 1.7% (95% CI, 1.4%-2.1%) at age 10 years; cumulative epilepsy incidence at age 10 years was 0.9% (95% CI, 0.8%-1%) in the control population. Moreover, epilepsy risk was demonstrated to be dependent on age of pertussis onset; a pertussis diagnosis was not associated with increased epilepsy risk in patients over the age of 3 years (hazard ratio, 1; 95% CI, 0.5-1.8).
According to study investigators, one explanation for the role that pertussis could potentially play in the pathophysiology of epilepsy may center on the occurrence of hypoxic brain damage resulting from severe pertussis-related coughing, “perhaps via increased intrathoracic and intra-abdominal pressure and central nervous system hemorrhages.”
The study was funded by the Program for Clinical Research Infrastructure established by the Lundbeck Foundation and the Novo Nordisk Foundation. The department of clinical epidemiology, Aarhus (Denmark) University Hospital, receives funding for other studies from companies in the form of research grants.
FROM JAMA
Key clinical point: Early-onset pertussis (older than age 3 years) has been linked to an increase, albeit small, in epilepsy risk.
Major finding: Pertussis patients were found to have a cumulative epilepsy incidence of 1.7% (95% confidence interval, 1.4%-2.1%) at age 10 years, compared with .9% (95% CI, 0.8%-1%) in the control population.
Data source: A comparative, retrospective analysis that identified and tracked 4,700 pertussis patients for up to 15 years from population-based medical registries encompassing every hospital and citizen in Denmark (roughly 5.6 million people) and a control population of 47,000 derived from the national Danish Civil Registration System.
Disclosures: The study was funded by the Program for Clinical Research Infrastructure established by the Lundbeck Foundation and the Novo Nordisk Foundation. The Department of Clinical Epidemiology, Aarhus (Denmark) University Hospital, receives funding for other studies from companies in the form of research grants.
Off-label prescriptions frequently cause adverse events
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published online Nov. 2 in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. But recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events in the Canadian province of Quebec, which provides health insurance for all 8.5 million residents. There, physicians must provide the indication(s) for every new prescription, the reason(s) for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr. Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
In what they described as the first large study of its kind, the investigators analyzed the prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions during a 5-year period. Physicians reported off-label use in 17,847 (11.8%) of these prescriptions, and that off-label use lacked strong scientific evidence in the great majority of cases (80.9%). The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
Prescribed drugs were discontinued because of adverse events in 3,484 cases. The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months). Moreover, the incidence of adverse events was 54% higher for off-label use unsupported by strong scientific evidence (21.7 per 10,000 person-months) than for off-label use supported by strong scientific evidence (13.2 per 10,000 person-months), the investigators said (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6058).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors added.
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr. Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr. Tewodros Eguale and his associates reported having no relevant financial disclosures.
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr. Chester B. Good is in pharmacy benefits management services at the U.S. Department of Veterans Affairs in Hines, Ill., and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr. Good and Dr. Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr. Good and Dr. Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr. Eguale’s report (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6068).
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr. Chester B. Good is in pharmacy benefits management services at the U.S. Department of Veterans Affairs in Hines, Ill., and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr. Good and Dr. Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr. Good and Dr. Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr. Eguale’s report (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6068).
This study, the most extensive and informative one to evaluate the safety of off-label drug use in adults to date, shows that clinicians often enter an arena of the unknown when they expand prescribing beyond the carefully devised confines of the labeled indication. It provides compelling evidence that off-label prescribing is frequently inappropriate and substantially raises the risk for an adverse event.
Even in cases in which an off-label indication has been studied, the pharmacokinetics, drug-disease interactions, drug-drug interactions, and other safety considerations weren’t studied to the degree required during the drug approval process. Moreover, how many clinicians have the time or motivation to review the evidence for those off-label indications, arriving at a balanced assessment of risks and benefits?
Dr. Chester B. Good is in pharmacy benefits management services at the U.S. Department of Veterans Affairs in Hines, Ill., and the department of pharmacy and therapeutics at the University of Pittsburgh. Dr. Good and Dr. Walid F. Gellad are in the department of medicine at the University of Pittsburgh and at the Center for Health Equity Research and Promotion in the Veterans Affairs Pittsburgh Healthcare System. Dr. Good and Dr. Gellad reported serving as unpaid advisers to the Food and Drug Administration’s Drug Safety Oversight Board. They made these remarks in an Invited Commentary accompanying Dr. Eguale’s report (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6068).
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published online Nov. 2 in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. But recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events in the Canadian province of Quebec, which provides health insurance for all 8.5 million residents. There, physicians must provide the indication(s) for every new prescription, the reason(s) for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr. Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
In what they described as the first large study of its kind, the investigators analyzed the prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions during a 5-year period. Physicians reported off-label use in 17,847 (11.8%) of these prescriptions, and that off-label use lacked strong scientific evidence in the great majority of cases (80.9%). The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
Prescribed drugs were discontinued because of adverse events in 3,484 cases. The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months). Moreover, the incidence of adverse events was 54% higher for off-label use unsupported by strong scientific evidence (21.7 per 10,000 person-months) than for off-label use supported by strong scientific evidence (13.2 per 10,000 person-months), the investigators said (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6058).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors added.
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr. Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr. Tewodros Eguale and his associates reported having no relevant financial disclosures.
Off-label prescribing of drugs is common and very likely to cause adverse events, particularly when no strong scientific evidence supports the off-label use, according to a report published online Nov. 2 in JAMA Internal Medicine.
No systematic investigation of the off-label use of prescription drugs has been done to date, in part because physicians aren’t required to document intended indications. But recent innovations in electronic health records provided an opportunity to track off-label prescribing and its influence on adverse drug events in the Canadian province of Quebec, which provides health insurance for all 8.5 million residents. There, physicians must provide the indication(s) for every new prescription, the reason(s) for any dose changes or drug discontinuation, and the nature of any adverse events, said Dr. Tewodros Eguale of the department of epidemiology, biostatistics, and occupational health at McGill University, Montreal, and his associates.
In what they described as the first large study of its kind, the investigators analyzed the prescribing information in electronic medical records of 46,021 adults (mean age 58 years) given 151,305 new prescriptions during a 5-year period. Physicians reported off-label use in 17,847 (11.8%) of these prescriptions, and that off-label use lacked strong scientific evidence in the great majority of cases (80.9%). The median follow-up time for use of prescribed medications was 386 days (range, 1 day to 6 years).
Prescribed drugs were discontinued because of adverse events in 3,484 cases. The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months). Moreover, the incidence of adverse events was 54% higher for off-label use unsupported by strong scientific evidence (21.7 per 10,000 person-months) than for off-label use supported by strong scientific evidence (13.2 per 10,000 person-months), the investigators said (JAMA Intern Med. 2015 Nov 2. doi:10.1001/jamainternmed.2015.6058).
The class of drugs with the highest rate of adverse effects was anti-infective agents (66.2 per 10,000 person-months), followed by central nervous system drugs such as antidepressants, anxiolytics, and antimigraine medicine (18.1 per 10,000); cardiovascular drugs (15.9 per 10,000); hormonal agents (12.7); autonomic drugs including albuterol and terbutaline (8.4); gastrointestinal drugs (6.1); ear, nose, and throat medications (2.8); and “other” agents such as antihistamines, blood thinners, and antineoplastics (1.3).
“Selected examples of adverse events associated with the most frequently used off-label drugs include akathisia resulting from the use of gabapentin for neurogenic pain; agitation associated with the use of amitriptyline hydrochloride for migraine; hallucinations with the use of trazodone hydrochloride for insomnia; QT interval prolongation with the use of quetiapine fumarate for depression; and weight gain with the use of olanzapine for depression,” the authors added.
“Off-label use may be clinically appropriate given the complexity of the patient’s condition, the lack of alternative effective drugs, or after exhausting approved drugs.” However, previous research has shown that physicians’ lack of knowledge of approved treatment indications was one important factor contributing to off-label prescribing. And one study showed that physicians are finding it difficult to keep up with rapidly changing medication information, and this lack of knowledge is affecting treatment, Dr. Eguale and his associates said.
That knowledge gap could be filled by supplying clinicians with information regarding drug approval status and the quality of supporting scientific evidence at the point of care, when they write prescriptions into patients’ electronic health records, the investigators noted. This would have the added advantage of facilitating communication among physicians, pharmacists, and patients, and could reduce medication errors such as those caused by giving drugs to the wrong patients or by giving patients sound-alike or look-alike drugs.
No sponsors were identified for this study. Dr. Tewodros Eguale and his associates reported having no relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Off-label prescribing in adults is common and very likely to cause adverse events.
Major finding: The incidence of adverse events was 44% higher for off-label use (19.7 per 10,000 person-months) than for on-label use (12.5 per 10,000 person-months) of prescription drugs.
Data source: A prospective cohort study of 46,021 adults who received 151,305 incident prescriptions from primary care clinicians in Quebec during a 5-year period.
Disclosures: No sponsors were identified for this study. Dr. Tewodros Eguale and his associates reported having no relevant financial disclosures.
This Adjunct Medication Can Speed CAP Recovery
PRACTICE CHANGER
Prescribe oral prednisone 50 mg/d to hospitalized patients with mild-to-moderate community-acquired pneumonia. It decreases time to clinical stability and length of hospital stay.1
STRENGTH OF RECOMMENDATION
A: Based on a single good-quality randomized controlled trial (RCT) and meta-analysis.1
ILLUSTRATIVE CASE
A 75-year-old woman with hypertension and diabetes presents to the emergency department with shortness of breath, cough, and fever that she’s had for four days. On examination, her temperature is 38.2°C; heart rate, 110 beats/min; respiratory rate, 28 breaths/min; and O2 saturation, 91%. Rhonchi are heard in her right lower lung field; chest x-ray reveals infiltrate in her right lower lobe. The patient is admitted and started on IV antibiotics, IV fluids, acetaminophen for fever, and oxygen. Can anything else be done to speed her recovery?
Community-acquired pneumonia (CAP) is responsible for more than 1 million hospitalizations annually in the United States and is the eighth leading cause of death.2,3 Treatment of CAP typically consists of antibiotics and supportive measures (eg, IV fluids and antipyretics). Because the disease process involves extensive inflammation, adjunct treatment with corticosteroids may be beneficial.
Multiple studies have shown that treatment with corticosteroids can help patients with severe CAP, but the potential benefit in patients with less severe CAP has been uncertain.4,5 A Cochrane systematic review published in 2011 identified six small RCTs that evaluated the impact of corticosteroids on CAP recovery.4 It suggested that corticosteroids may decrease time to recovery, but the studies that included patients with less severe CAP had a relatively high risk for bias.
Subsequently, a 2012 meta-analysis of nine RCTs explored whether corticosteroids affected mortality in CAP; no benefit was observed in patients with less severe CAP.5 Most recently, a 2013 meta-analysis of eight moderate-quality RCTs showed that corticosteroid use was associated with shorter hospital stays but no change in mortality.6
The synthesis of small or moderate-quality studies suggests some potential benefit in treating less severe CAP with corticosteroids, but there has been a need for a large, definitive, high-quality RCT. This study investigated the impact of a short course of oral steroids on inpatients with less severe CAP.
STUDY SUMMARY
Prednisone hastens clinical stabilization, cuts hospital stay
In a multicenter, double-blind RCT, Blum et al1 enrolled 785 patients with CAP who were admitted to one of seven tertiary care hospitals in Switzerland from 2009 to 2014. Patients were eligible if they were 18 or older, had a new infiltrate on chest x-ray, and had at least one additional sign or symptom of respiratory illness (eg, cough, dyspnea, fever, abnormal breathing signs or rales, or elevated or decreased white blood cell count). Patients were excluded if they had a contraindication to corticosteroids, cystic fibrosis, or active tuberculosis.
Patients were randomized to receive either prednisone 50 mg/d or placebo for seven days. They were treated with antibiotics according to accepted local guidelines; most patients received either amoxicillin/clavulanic acid or ceftriaxone. Antibiotic treatment was adjusted according to susceptibility whenever a specific pathogen was identified. Nurses assessed all patients every 12 hours during hospitalization, and laboratory tests were obtained on hospital days 1, 3, 5, and 7, and before discharge. Follow-up telephone interviews were conducted on day 30.
The primary outcome was length of time to clinical stability (eg, at least 24 hours of stable vital signs). This composite endpoint required all of the following: temperature ≤ 37.8°C; heart rate ≤ 100 beats/min; spontaneous respiratory rate ≤ 24 breaths/min; systolic blood pressure ≥ 90 mm Hg (≥ 100 mm Hg for patients diagnosed with hypertension) without vasopressor support; mental status back to baseline; ability to take food by mouth; and adequate oxygenation on room air.
Secondary outcomes included length of hospital stay, pneumonia recurrence, hospital readmission, intensive care unit (ICU) admission, all-cause mortality, and duration of antibiotic treatment. Researchers also explored whether the rates of complications from pneumonia or corticosteroid use differed between the prednisone and placebo groups.
In an intention-to-treat analysis, the median time to clinical stability was shorter for the prednisone group at 3 days (interquartile range [IQR], 2.5 to 3.4) compared to the placebo group at 4.4 days (IQR, 4 - 5; hazard ratio [HR], 1.33). Median time to hospital discharge was also shorter for the prednisone group (6 d vs 7 d; HR, 1.19), as was duration of IV antibiotic treatment (4 d vs 5 d; difference, –0.89 d).
There were no statistically significant differences in pneumonia recurrence, hospital readmission, ICU admission, or all-cause mortality. Patients treated with prednisone were more likely to experience hyperglycemia that required insulin treatment during admission (19% vs 11%; odds ratio, 1.96).
WHAT’S NEW
This large, good-quality study reinforces previous evidence
This is the first rigorous study to show a clear decrease in both time to clinical stability and length of hospital stay. It also used an easy-to-administer dose of oral steroids, instead of the several-day course of IV steroids used in most other studies. The findings from this study were incorporated into a 2015 meta-analysis that confirmed that corticosteroid treatment in patients with less severe CAP results in a shorter length of hospital stay and decreased time to clinical stability.7
CAVEATS
It’s unclear if steroids benefit nonhospitalized patients
Because this study included hospitalized patients only, it’s not clear whether corticosteroids have a role in outpatient treatment of CAP. Additionally, although this was a large, well-designed study, it did not have a sufficient number of patients to examine whether corticosteroids impact mortality among patients with CAP.
Finally, the average length of hospital stay reported in this study was approximately 1.5 days longer than the typical length of stay in the US.2 The average length of stay has varied widely in studies examining corticosteroids in CAP, but good-quality studies have consistently shown a median reduction in length of stay of one day.7
CHALLENGES TO IMPLEMENTATION
Risk for adverse events
Treatment with prednisone increases risk for corticosteroid-related adverse events, primarily hyperglycemia and the need for insulin. This may not be well received by patients or providers. However, these effects appear to resolve quickly after treatment and do not impact the overall time to clinical stability.
REFERENCES
1. Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomized, placebo-controlled trial. Lancet. 2015;385:1511-1518.
2. CDC. FastStats: Pneumonia. www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed September 29, 2015.
3. CDC/National Center for Health Statistics. Top 10 leading causes of death: United States, 1999–2013. http://blogs.cdc.gov/nchs-data-visualization/2015/06/01/leading-causes-of-death. Accessed September 29, 2015.
4. Chen Y, Li K, Pu H, et al. Corticosteroids for pneumonia. Cochrane Database Syst Rev. 2011;3:CD007720.
5. Nie W, Zhang Y, Cheng J, et al. Corticosteroids in the treatment of community-acquired pneumonia in adults: a meta-analysis. PLoS One. 2012;7:e47926.
6. Shafiq M, Mansoor MS, Khan AA, et al. Adjuvant steroid therapy in community-acquired pneumonia: a systematic review and meta-analysis. J Hosp Med. 2013;8:68-75.
7. Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med. 2015;163:519-528.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(10):648-650.
PRACTICE CHANGER
Prescribe oral prednisone 50 mg/d to hospitalized patients with mild-to-moderate community-acquired pneumonia. It decreases time to clinical stability and length of hospital stay.1
STRENGTH OF RECOMMENDATION
A: Based on a single good-quality randomized controlled trial (RCT) and meta-analysis.1
ILLUSTRATIVE CASE
A 75-year-old woman with hypertension and diabetes presents to the emergency department with shortness of breath, cough, and fever that she’s had for four days. On examination, her temperature is 38.2°C; heart rate, 110 beats/min; respiratory rate, 28 breaths/min; and O2 saturation, 91%. Rhonchi are heard in her right lower lung field; chest x-ray reveals infiltrate in her right lower lobe. The patient is admitted and started on IV antibiotics, IV fluids, acetaminophen for fever, and oxygen. Can anything else be done to speed her recovery?
Community-acquired pneumonia (CAP) is responsible for more than 1 million hospitalizations annually in the United States and is the eighth leading cause of death.2,3 Treatment of CAP typically consists of antibiotics and supportive measures (eg, IV fluids and antipyretics). Because the disease process involves extensive inflammation, adjunct treatment with corticosteroids may be beneficial.
Multiple studies have shown that treatment with corticosteroids can help patients with severe CAP, but the potential benefit in patients with less severe CAP has been uncertain.4,5 A Cochrane systematic review published in 2011 identified six small RCTs that evaluated the impact of corticosteroids on CAP recovery.4 It suggested that corticosteroids may decrease time to recovery, but the studies that included patients with less severe CAP had a relatively high risk for bias.
Subsequently, a 2012 meta-analysis of nine RCTs explored whether corticosteroids affected mortality in CAP; no benefit was observed in patients with less severe CAP.5 Most recently, a 2013 meta-analysis of eight moderate-quality RCTs showed that corticosteroid use was associated with shorter hospital stays but no change in mortality.6
The synthesis of small or moderate-quality studies suggests some potential benefit in treating less severe CAP with corticosteroids, but there has been a need for a large, definitive, high-quality RCT. This study investigated the impact of a short course of oral steroids on inpatients with less severe CAP.
STUDY SUMMARY
Prednisone hastens clinical stabilization, cuts hospital stay
In a multicenter, double-blind RCT, Blum et al1 enrolled 785 patients with CAP who were admitted to one of seven tertiary care hospitals in Switzerland from 2009 to 2014. Patients were eligible if they were 18 or older, had a new infiltrate on chest x-ray, and had at least one additional sign or symptom of respiratory illness (eg, cough, dyspnea, fever, abnormal breathing signs or rales, or elevated or decreased white blood cell count). Patients were excluded if they had a contraindication to corticosteroids, cystic fibrosis, or active tuberculosis.
Patients were randomized to receive either prednisone 50 mg/d or placebo for seven days. They were treated with antibiotics according to accepted local guidelines; most patients received either amoxicillin/clavulanic acid or ceftriaxone. Antibiotic treatment was adjusted according to susceptibility whenever a specific pathogen was identified. Nurses assessed all patients every 12 hours during hospitalization, and laboratory tests were obtained on hospital days 1, 3, 5, and 7, and before discharge. Follow-up telephone interviews were conducted on day 30.
The primary outcome was length of time to clinical stability (eg, at least 24 hours of stable vital signs). This composite endpoint required all of the following: temperature ≤ 37.8°C; heart rate ≤ 100 beats/min; spontaneous respiratory rate ≤ 24 breaths/min; systolic blood pressure ≥ 90 mm Hg (≥ 100 mm Hg for patients diagnosed with hypertension) without vasopressor support; mental status back to baseline; ability to take food by mouth; and adequate oxygenation on room air.
Secondary outcomes included length of hospital stay, pneumonia recurrence, hospital readmission, intensive care unit (ICU) admission, all-cause mortality, and duration of antibiotic treatment. Researchers also explored whether the rates of complications from pneumonia or corticosteroid use differed between the prednisone and placebo groups.
In an intention-to-treat analysis, the median time to clinical stability was shorter for the prednisone group at 3 days (interquartile range [IQR], 2.5 to 3.4) compared to the placebo group at 4.4 days (IQR, 4 - 5; hazard ratio [HR], 1.33). Median time to hospital discharge was also shorter for the prednisone group (6 d vs 7 d; HR, 1.19), as was duration of IV antibiotic treatment (4 d vs 5 d; difference, –0.89 d).
There were no statistically significant differences in pneumonia recurrence, hospital readmission, ICU admission, or all-cause mortality. Patients treated with prednisone were more likely to experience hyperglycemia that required insulin treatment during admission (19% vs 11%; odds ratio, 1.96).
WHAT’S NEW
This large, good-quality study reinforces previous evidence
This is the first rigorous study to show a clear decrease in both time to clinical stability and length of hospital stay. It also used an easy-to-administer dose of oral steroids, instead of the several-day course of IV steroids used in most other studies. The findings from this study were incorporated into a 2015 meta-analysis that confirmed that corticosteroid treatment in patients with less severe CAP results in a shorter length of hospital stay and decreased time to clinical stability.7
CAVEATS
It’s unclear if steroids benefit nonhospitalized patients
Because this study included hospitalized patients only, it’s not clear whether corticosteroids have a role in outpatient treatment of CAP. Additionally, although this was a large, well-designed study, it did not have a sufficient number of patients to examine whether corticosteroids impact mortality among patients with CAP.
Finally, the average length of hospital stay reported in this study was approximately 1.5 days longer than the typical length of stay in the US.2 The average length of stay has varied widely in studies examining corticosteroids in CAP, but good-quality studies have consistently shown a median reduction in length of stay of one day.7
CHALLENGES TO IMPLEMENTATION
Risk for adverse events
Treatment with prednisone increases risk for corticosteroid-related adverse events, primarily hyperglycemia and the need for insulin. This may not be well received by patients or providers. However, these effects appear to resolve quickly after treatment and do not impact the overall time to clinical stability.
REFERENCES
1. Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomized, placebo-controlled trial. Lancet. 2015;385:1511-1518.
2. CDC. FastStats: Pneumonia. www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed September 29, 2015.
3. CDC/National Center for Health Statistics. Top 10 leading causes of death: United States, 1999–2013. http://blogs.cdc.gov/nchs-data-visualization/2015/06/01/leading-causes-of-death. Accessed September 29, 2015.
4. Chen Y, Li K, Pu H, et al. Corticosteroids for pneumonia. Cochrane Database Syst Rev. 2011;3:CD007720.
5. Nie W, Zhang Y, Cheng J, et al. Corticosteroids in the treatment of community-acquired pneumonia in adults: a meta-analysis. PLoS One. 2012;7:e47926.
6. Shafiq M, Mansoor MS, Khan AA, et al. Adjuvant steroid therapy in community-acquired pneumonia: a systematic review and meta-analysis. J Hosp Med. 2013;8:68-75.
7. Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med. 2015;163:519-528.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(10):648-650.
PRACTICE CHANGER
Prescribe oral prednisone 50 mg/d to hospitalized patients with mild-to-moderate community-acquired pneumonia. It decreases time to clinical stability and length of hospital stay.1
STRENGTH OF RECOMMENDATION
A: Based on a single good-quality randomized controlled trial (RCT) and meta-analysis.1
ILLUSTRATIVE CASE
A 75-year-old woman with hypertension and diabetes presents to the emergency department with shortness of breath, cough, and fever that she’s had for four days. On examination, her temperature is 38.2°C; heart rate, 110 beats/min; respiratory rate, 28 breaths/min; and O2 saturation, 91%. Rhonchi are heard in her right lower lung field; chest x-ray reveals infiltrate in her right lower lobe. The patient is admitted and started on IV antibiotics, IV fluids, acetaminophen for fever, and oxygen. Can anything else be done to speed her recovery?
Community-acquired pneumonia (CAP) is responsible for more than 1 million hospitalizations annually in the United States and is the eighth leading cause of death.2,3 Treatment of CAP typically consists of antibiotics and supportive measures (eg, IV fluids and antipyretics). Because the disease process involves extensive inflammation, adjunct treatment with corticosteroids may be beneficial.
Multiple studies have shown that treatment with corticosteroids can help patients with severe CAP, but the potential benefit in patients with less severe CAP has been uncertain.4,5 A Cochrane systematic review published in 2011 identified six small RCTs that evaluated the impact of corticosteroids on CAP recovery.4 It suggested that corticosteroids may decrease time to recovery, but the studies that included patients with less severe CAP had a relatively high risk for bias.
Subsequently, a 2012 meta-analysis of nine RCTs explored whether corticosteroids affected mortality in CAP; no benefit was observed in patients with less severe CAP.5 Most recently, a 2013 meta-analysis of eight moderate-quality RCTs showed that corticosteroid use was associated with shorter hospital stays but no change in mortality.6
The synthesis of small or moderate-quality studies suggests some potential benefit in treating less severe CAP with corticosteroids, but there has been a need for a large, definitive, high-quality RCT. This study investigated the impact of a short course of oral steroids on inpatients with less severe CAP.
STUDY SUMMARY
Prednisone hastens clinical stabilization, cuts hospital stay
In a multicenter, double-blind RCT, Blum et al1 enrolled 785 patients with CAP who were admitted to one of seven tertiary care hospitals in Switzerland from 2009 to 2014. Patients were eligible if they were 18 or older, had a new infiltrate on chest x-ray, and had at least one additional sign or symptom of respiratory illness (eg, cough, dyspnea, fever, abnormal breathing signs or rales, or elevated or decreased white blood cell count). Patients were excluded if they had a contraindication to corticosteroids, cystic fibrosis, or active tuberculosis.
Patients were randomized to receive either prednisone 50 mg/d or placebo for seven days. They were treated with antibiotics according to accepted local guidelines; most patients received either amoxicillin/clavulanic acid or ceftriaxone. Antibiotic treatment was adjusted according to susceptibility whenever a specific pathogen was identified. Nurses assessed all patients every 12 hours during hospitalization, and laboratory tests were obtained on hospital days 1, 3, 5, and 7, and before discharge. Follow-up telephone interviews were conducted on day 30.
The primary outcome was length of time to clinical stability (eg, at least 24 hours of stable vital signs). This composite endpoint required all of the following: temperature ≤ 37.8°C; heart rate ≤ 100 beats/min; spontaneous respiratory rate ≤ 24 breaths/min; systolic blood pressure ≥ 90 mm Hg (≥ 100 mm Hg for patients diagnosed with hypertension) without vasopressor support; mental status back to baseline; ability to take food by mouth; and adequate oxygenation on room air.
Secondary outcomes included length of hospital stay, pneumonia recurrence, hospital readmission, intensive care unit (ICU) admission, all-cause mortality, and duration of antibiotic treatment. Researchers also explored whether the rates of complications from pneumonia or corticosteroid use differed between the prednisone and placebo groups.
In an intention-to-treat analysis, the median time to clinical stability was shorter for the prednisone group at 3 days (interquartile range [IQR], 2.5 to 3.4) compared to the placebo group at 4.4 days (IQR, 4 - 5; hazard ratio [HR], 1.33). Median time to hospital discharge was also shorter for the prednisone group (6 d vs 7 d; HR, 1.19), as was duration of IV antibiotic treatment (4 d vs 5 d; difference, –0.89 d).
There were no statistically significant differences in pneumonia recurrence, hospital readmission, ICU admission, or all-cause mortality. Patients treated with prednisone were more likely to experience hyperglycemia that required insulin treatment during admission (19% vs 11%; odds ratio, 1.96).
WHAT’S NEW
This large, good-quality study reinforces previous evidence
This is the first rigorous study to show a clear decrease in both time to clinical stability and length of hospital stay. It also used an easy-to-administer dose of oral steroids, instead of the several-day course of IV steroids used in most other studies. The findings from this study were incorporated into a 2015 meta-analysis that confirmed that corticosteroid treatment in patients with less severe CAP results in a shorter length of hospital stay and decreased time to clinical stability.7
CAVEATS
It’s unclear if steroids benefit nonhospitalized patients
Because this study included hospitalized patients only, it’s not clear whether corticosteroids have a role in outpatient treatment of CAP. Additionally, although this was a large, well-designed study, it did not have a sufficient number of patients to examine whether corticosteroids impact mortality among patients with CAP.
Finally, the average length of hospital stay reported in this study was approximately 1.5 days longer than the typical length of stay in the US.2 The average length of stay has varied widely in studies examining corticosteroids in CAP, but good-quality studies have consistently shown a median reduction in length of stay of one day.7
CHALLENGES TO IMPLEMENTATION
Risk for adverse events
Treatment with prednisone increases risk for corticosteroid-related adverse events, primarily hyperglycemia and the need for insulin. This may not be well received by patients or providers. However, these effects appear to resolve quickly after treatment and do not impact the overall time to clinical stability.
REFERENCES
1. Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomized, placebo-controlled trial. Lancet. 2015;385:1511-1518.
2. CDC. FastStats: Pneumonia. www.cdc.gov/nchs/fastats/pneumonia.htm. Accessed September 29, 2015.
3. CDC/National Center for Health Statistics. Top 10 leading causes of death: United States, 1999–2013. http://blogs.cdc.gov/nchs-data-visualization/2015/06/01/leading-causes-of-death. Accessed September 29, 2015.
4. Chen Y, Li K, Pu H, et al. Corticosteroids for pneumonia. Cochrane Database Syst Rev. 2011;3:CD007720.
5. Nie W, Zhang Y, Cheng J, et al. Corticosteroids in the treatment of community-acquired pneumonia in adults: a meta-analysis. PLoS One. 2012;7:e47926.
6. Shafiq M, Mansoor MS, Khan AA, et al. Adjuvant steroid therapy in community-acquired pneumonia: a systematic review and meta-analysis. J Hosp Med. 2013;8:68-75.
7. Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med. 2015;163:519-528.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2015. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2015;64(10):648-650.
CHEST: Losartan slows emphysema progression in pilot trial
MONTREAL – Daily treatment with the antihypertensive drug losartan for a year appeared to slow progression of emphysema, compared with placebo, in a controlled pilot study involving 46 patients at one U.S. center, Dr. Allison Lambert reported at the annual meeting of the American College of Chest Physicians.
One year of daily, 100-mg oral treatment with the angiotensin receptor–blocking drug losartan in patients with emphysema produced a statistically significant regression of the disease in their right-middle lung lobes, compared with progression of right-middle lung lobe disease among control patients, as assessed by CT lung scans. In this lung segment, emphysema regressed by 0.72% in patients on losartan (Cozaar), compared with an average 3.34% rate of progression in patients on placebo.
The losartan-treated patients also showed a consistent pattern of either substantially slowed or reversed emphysema throughout multiple lung segments, although the between-group differences did not reach statistical significance in any other segment, said Dr. Lambert, a pulmonologist at Johns Hopkins Hospital in Baltimore.
Throughout the entire lung, 12 months of losartan treatment was linked to an average 0.32% reduction in emphysema extent from baseline when measured by CT, compared with a 2.18% rate of emphysema progression in control patients on usual care, which just missed statistical significance (P = .064).
Data from other researchers “suggest the right-middle lobe most commonly progresses in emphysema,” which may explain why that lung segment showed the most dramatic effect from treatment, she suggested. Another finding Dr. Lambert found striking was the consistent trend toward slowed emphysema progression in multiple segments throughout patients’ lungs.
Dr. Lambert called this a phase II, “proof of concept” trial. She and her associates have begun a larger, phase III version that will study the effect of 100-mg daily losartan during 1 year of treatment in 220 patients with emphysema, she said. This trial received funding from the Pulmonary Trials Cooperative of the National Heart Lung and Blood Institute.
“These are some of the most interesting and exciting data I’ve seen,” commented Dr. David P.L. Sachs, a pulmonologist who practices in Stanford, Calif., and cochaired the session in which Dr. Lambert gave her report. “Having an agent that could slow progression of emphysema would be unique,” he said in an interview. One aspect that makes this treatment especially attractive is losartan’s extensive safety record as an antihypertensive drug that is also often used to treat patients with heart failure, Dr. Sachs noted.
To put the 100-mg/day dosage used in the current study in perspective, results from a multicenter randomized trial of more than 3,800 heart failure patients published in 2009 showed that a losartan dosage of 150 mg once daily was safe and effective and produced outcomes superior to those seen with a 50 mg once-daily dosage (Lancet. 2009;374[9704]:1840-8).
Dr. Lambert and her associates designed this pilot study because of previously reported results from other groups showing favorable effects of losartan on animal models of emphysema or other lung disease, as well as suggestions from nonprospective clinical studies of benefits from angiotensin-receptor blockers on lung function and on chronic obstructive pulmonary disease (COPD) in particular.
The current study enrolled patients with mild to severe COPD who were current or former cigarette smokers who had at least a 10 pack-year history and were on stable treatment for their COPD. The researchers excluded patients already taking an angiotensin-receptor blocker or angiotensin-converting enzyme inhibitor.
The study included a total of 106 patients with COPD, including the 46 with emphysema at baseline. Their average age was about 58 years old, the enrolled patients included roughly equal numbers of men and women, and about two-thirds were current smokers. All patients underwent CT lung scans at baseline and after 6 and 12 months, as well as other lung function assessments. The study’s primary endpoint was the amount of additional emphysema in their lungs beyond that seen at baseline using CT imaging.
The entire group of 106 COPD patients showed no significant differences in emphysema progression at either 6 or 12 months between the 54 patients treated with losartan and the 52 controls on placebo, but a second, prespecified analysis that focused only on the 46 enrolled patients who had visible emphysema at baseline showed a significant slowing of progression at the 1-year follow-up, Dr. Lambert said.
The study received partial funding from Merck, which markets losartan (Cozaar). Dr. Lambert had no disclosures. Dr. Sachs had no disclosures.
On Twitter @mitchelzoler
MONTREAL – Daily treatment with the antihypertensive drug losartan for a year appeared to slow progression of emphysema, compared with placebo, in a controlled pilot study involving 46 patients at one U.S. center, Dr. Allison Lambert reported at the annual meeting of the American College of Chest Physicians.
One year of daily, 100-mg oral treatment with the angiotensin receptor–blocking drug losartan in patients with emphysema produced a statistically significant regression of the disease in their right-middle lung lobes, compared with progression of right-middle lung lobe disease among control patients, as assessed by CT lung scans. In this lung segment, emphysema regressed by 0.72% in patients on losartan (Cozaar), compared with an average 3.34% rate of progression in patients on placebo.
The losartan-treated patients also showed a consistent pattern of either substantially slowed or reversed emphysema throughout multiple lung segments, although the between-group differences did not reach statistical significance in any other segment, said Dr. Lambert, a pulmonologist at Johns Hopkins Hospital in Baltimore.
Throughout the entire lung, 12 months of losartan treatment was linked to an average 0.32% reduction in emphysema extent from baseline when measured by CT, compared with a 2.18% rate of emphysema progression in control patients on usual care, which just missed statistical significance (P = .064).
Data from other researchers “suggest the right-middle lobe most commonly progresses in emphysema,” which may explain why that lung segment showed the most dramatic effect from treatment, she suggested. Another finding Dr. Lambert found striking was the consistent trend toward slowed emphysema progression in multiple segments throughout patients’ lungs.
Dr. Lambert called this a phase II, “proof of concept” trial. She and her associates have begun a larger, phase III version that will study the effect of 100-mg daily losartan during 1 year of treatment in 220 patients with emphysema, she said. This trial received funding from the Pulmonary Trials Cooperative of the National Heart Lung and Blood Institute.
“These are some of the most interesting and exciting data I’ve seen,” commented Dr. David P.L. Sachs, a pulmonologist who practices in Stanford, Calif., and cochaired the session in which Dr. Lambert gave her report. “Having an agent that could slow progression of emphysema would be unique,” he said in an interview. One aspect that makes this treatment especially attractive is losartan’s extensive safety record as an antihypertensive drug that is also often used to treat patients with heart failure, Dr. Sachs noted.
To put the 100-mg/day dosage used in the current study in perspective, results from a multicenter randomized trial of more than 3,800 heart failure patients published in 2009 showed that a losartan dosage of 150 mg once daily was safe and effective and produced outcomes superior to those seen with a 50 mg once-daily dosage (Lancet. 2009;374[9704]:1840-8).
Dr. Lambert and her associates designed this pilot study because of previously reported results from other groups showing favorable effects of losartan on animal models of emphysema or other lung disease, as well as suggestions from nonprospective clinical studies of benefits from angiotensin-receptor blockers on lung function and on chronic obstructive pulmonary disease (COPD) in particular.
The current study enrolled patients with mild to severe COPD who were current or former cigarette smokers who had at least a 10 pack-year history and were on stable treatment for their COPD. The researchers excluded patients already taking an angiotensin-receptor blocker or angiotensin-converting enzyme inhibitor.
The study included a total of 106 patients with COPD, including the 46 with emphysema at baseline. Their average age was about 58 years old, the enrolled patients included roughly equal numbers of men and women, and about two-thirds were current smokers. All patients underwent CT lung scans at baseline and after 6 and 12 months, as well as other lung function assessments. The study’s primary endpoint was the amount of additional emphysema in their lungs beyond that seen at baseline using CT imaging.
The entire group of 106 COPD patients showed no significant differences in emphysema progression at either 6 or 12 months between the 54 patients treated with losartan and the 52 controls on placebo, but a second, prespecified analysis that focused only on the 46 enrolled patients who had visible emphysema at baseline showed a significant slowing of progression at the 1-year follow-up, Dr. Lambert said.
The study received partial funding from Merck, which markets losartan (Cozaar). Dr. Lambert had no disclosures. Dr. Sachs had no disclosures.
On Twitter @mitchelzoler
MONTREAL – Daily treatment with the antihypertensive drug losartan for a year appeared to slow progression of emphysema, compared with placebo, in a controlled pilot study involving 46 patients at one U.S. center, Dr. Allison Lambert reported at the annual meeting of the American College of Chest Physicians.
One year of daily, 100-mg oral treatment with the angiotensin receptor–blocking drug losartan in patients with emphysema produced a statistically significant regression of the disease in their right-middle lung lobes, compared with progression of right-middle lung lobe disease among control patients, as assessed by CT lung scans. In this lung segment, emphysema regressed by 0.72% in patients on losartan (Cozaar), compared with an average 3.34% rate of progression in patients on placebo.
The losartan-treated patients also showed a consistent pattern of either substantially slowed or reversed emphysema throughout multiple lung segments, although the between-group differences did not reach statistical significance in any other segment, said Dr. Lambert, a pulmonologist at Johns Hopkins Hospital in Baltimore.
Throughout the entire lung, 12 months of losartan treatment was linked to an average 0.32% reduction in emphysema extent from baseline when measured by CT, compared with a 2.18% rate of emphysema progression in control patients on usual care, which just missed statistical significance (P = .064).
Data from other researchers “suggest the right-middle lobe most commonly progresses in emphysema,” which may explain why that lung segment showed the most dramatic effect from treatment, she suggested. Another finding Dr. Lambert found striking was the consistent trend toward slowed emphysema progression in multiple segments throughout patients’ lungs.
Dr. Lambert called this a phase II, “proof of concept” trial. She and her associates have begun a larger, phase III version that will study the effect of 100-mg daily losartan during 1 year of treatment in 220 patients with emphysema, she said. This trial received funding from the Pulmonary Trials Cooperative of the National Heart Lung and Blood Institute.
“These are some of the most interesting and exciting data I’ve seen,” commented Dr. David P.L. Sachs, a pulmonologist who practices in Stanford, Calif., and cochaired the session in which Dr. Lambert gave her report. “Having an agent that could slow progression of emphysema would be unique,” he said in an interview. One aspect that makes this treatment especially attractive is losartan’s extensive safety record as an antihypertensive drug that is also often used to treat patients with heart failure, Dr. Sachs noted.
To put the 100-mg/day dosage used in the current study in perspective, results from a multicenter randomized trial of more than 3,800 heart failure patients published in 2009 showed that a losartan dosage of 150 mg once daily was safe and effective and produced outcomes superior to those seen with a 50 mg once-daily dosage (Lancet. 2009;374[9704]:1840-8).
Dr. Lambert and her associates designed this pilot study because of previously reported results from other groups showing favorable effects of losartan on animal models of emphysema or other lung disease, as well as suggestions from nonprospective clinical studies of benefits from angiotensin-receptor blockers on lung function and on chronic obstructive pulmonary disease (COPD) in particular.
The current study enrolled patients with mild to severe COPD who were current or former cigarette smokers who had at least a 10 pack-year history and were on stable treatment for their COPD. The researchers excluded patients already taking an angiotensin-receptor blocker or angiotensin-converting enzyme inhibitor.
The study included a total of 106 patients with COPD, including the 46 with emphysema at baseline. Their average age was about 58 years old, the enrolled patients included roughly equal numbers of men and women, and about two-thirds were current smokers. All patients underwent CT lung scans at baseline and after 6 and 12 months, as well as other lung function assessments. The study’s primary endpoint was the amount of additional emphysema in their lungs beyond that seen at baseline using CT imaging.
The entire group of 106 COPD patients showed no significant differences in emphysema progression at either 6 or 12 months between the 54 patients treated with losartan and the 52 controls on placebo, but a second, prespecified analysis that focused only on the 46 enrolled patients who had visible emphysema at baseline showed a significant slowing of progression at the 1-year follow-up, Dr. Lambert said.
The study received partial funding from Merck, which markets losartan (Cozaar). Dr. Lambert had no disclosures. Dr. Sachs had no disclosures.
On Twitter @mitchelzoler
AT CHEST 2015
Key clinical point: A year of daily treatment with losartan produced significant slowing of emphysema progression in a placebo-controlled pilot study with 46 patients.
Major finding: Right middle-lobe emphysema regressed by 0.72% in patients using losartan, compared with 3.34% progression in controls, measured by CT imaging.
Data source: A single-center, prospective, controlled study involving 46 patients with emphysema and 60 additional patients with less severe COPD.
Disclosures: The study received partial funding from Merck, which markets losartan (Cozaar). Dr. Lambert had no disclosures. Dr. Sachs had no disclosures.