User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
West African Ebola–virus transmission ends, then resumes
A day after the World Health Organization declared on Jan. 14 that no known cases of Ebola-virus transmission or active infection had been identified in West Africa for more than 42 days, the agency revealed the existence of a new, single case of Ebola-virus infection in Sierra Leone.
The appearance of the new case highlighted the challenges that remain in fully stamping out the West African Ebola–virus outbreak. The crisis began in December 2013, raged throughout 2014, and only wound down toward a sputtering halt near the end of 2015.
When Dr. Rick Brennan, the World Health Organization (WHO) director for Emergency Risk Management and Humanitarian Response, announced during a press conference on Jan. 14, “the end of Ebola-virus transmission in West Africa” and “the first time since 2014 that all know chains of transmission have stopped in Guinea, Liberia, and Sierra Leone,” he and his colleague, Dr. Peter Graaff, also underscored the ongoing risk for sporadic, isolated cases. The main threat for new cases comes from men who survived Ebola-virus infection but harbored significant quantities of infectious virus in various body fluids and tissues, including their semen, for a period of about 1 year following their infection.
During the press conference, both Dr. Brennan and Dr. Graaff spoke of a new, strengthened infrastructure that WHO had placed in West Africa to better monitor and react quickly to these flare-up cases – the mechanism that led to quick identification of the new Sierra Leone case.
“I think you’ll see a more responsive and effective WHO,” said Dr. Graaff, WHO’s director of Ebola response. “We will use the Ebola experience to be more agile, more operational, and better able to react more quickly to whatever future problems come our way,” including infectious-disease outbreaks by pathogens other than Ebola virus.
The 42-day period without new infections that had led to the announcement of an end to Ebola-virus transmission in West Africa represents two 21-day incubation cycles for the virus. Until the Sierra Leone case reported on Jan. 15, the last confirmed West African case had been identified in Liberia in mid-November. Liberia had previously been declared Ebola free in last May, but four new, isolated infections appeared subsequent to that transmitted by Ebola-infection survivors who still harbored infectious virus. Before the Jan. 15 case, an additional three such flare-ups occurred in Sierra Leone and another three in Guinea since last March, Dr. Brennan said.
The current tally on the West African Ebola outbreak stands at roughly 28,500 confirmed cases identified, and about 11,300 deaths. Nearly three-quarters of infections occurred during 2014. The case fatality rate at the start of the outbreak ran about 80%, noted Dr. Graaff, but gradually fell as infected patients began receiving better care. Near the outbreak’s end, the case fatality rate stood at roughly 35%, when most patients were receiving optimal clinical care.
WHO staffers are maintaining close surveillance of people who recently survived Ebola-virus infection so that they can identify and isolate any new infections. WHO personnel have also counseled these survivors on the risk they pose for potential transmission, primarily by unprotected sex by men for up to 12 months following the end of active infection. The WHO also plans to launch an investigational protocol to vaccinate sexual partners and other close contacts of adult male survivors with an as-yet unapproved Ebola vaccine to further reduce risk of new infections.
“The WHO and world community reacted slowly at the start of the Ebola outbreak” in early 2014, admitted Dr. Brennan. “Without question, the disease got away from us. In retrospect, there were a number of things that we should have done better and sooner,” he said. “We have done a lot of soul-searching and we [at WHO] have identified a number of weaknesses in our structures and systems. We have already taken several important steps, and we are undergoing major reforms of our emergency operations. I think you’ll see a much more effective WHO in the future.”
Reform of WHO systems for infection prevention and control “will be much better able to detect new cases, not only of Ebola, but of other important diseases,” said Dr. Graaff.
The United States is also strengthening its health screening and monitoring system for travelers coming from affected countries and improving its hospital preparedness to manage cases, said Alice C. Hill, senior adviser for preparedness and resilience at the National Security Council and special assistant to President Obama. Hill, who spoke Jan. 6 at the Public Health Emergency Medical Countermeasures Enterprise stakeholders workshop, acknowledged that challenges still exist that must be addressed, including the development of safe and effective diagnostics, treatments, and vaccines for existing infectious diseases such as influenza and more emerging threats such as Ebola or MERS (Middle East Respiratory Syndrome), developing accurate disease forecasting capabilities to predict what will be the next threat, building rapid clinical trial networks and manufacturing capabilities, and the abilities for mass dispensing of medical countermeasures.
Gregory Twachtman also contributed to this story.
On Twitter @mitchelzoler
A day after the World Health Organization declared on Jan. 14 that no known cases of Ebola-virus transmission or active infection had been identified in West Africa for more than 42 days, the agency revealed the existence of a new, single case of Ebola-virus infection in Sierra Leone.
The appearance of the new case highlighted the challenges that remain in fully stamping out the West African Ebola–virus outbreak. The crisis began in December 2013, raged throughout 2014, and only wound down toward a sputtering halt near the end of 2015.
When Dr. Rick Brennan, the World Health Organization (WHO) director for Emergency Risk Management and Humanitarian Response, announced during a press conference on Jan. 14, “the end of Ebola-virus transmission in West Africa” and “the first time since 2014 that all know chains of transmission have stopped in Guinea, Liberia, and Sierra Leone,” he and his colleague, Dr. Peter Graaff, also underscored the ongoing risk for sporadic, isolated cases. The main threat for new cases comes from men who survived Ebola-virus infection but harbored significant quantities of infectious virus in various body fluids and tissues, including their semen, for a period of about 1 year following their infection.
During the press conference, both Dr. Brennan and Dr. Graaff spoke of a new, strengthened infrastructure that WHO had placed in West Africa to better monitor and react quickly to these flare-up cases – the mechanism that led to quick identification of the new Sierra Leone case.
“I think you’ll see a more responsive and effective WHO,” said Dr. Graaff, WHO’s director of Ebola response. “We will use the Ebola experience to be more agile, more operational, and better able to react more quickly to whatever future problems come our way,” including infectious-disease outbreaks by pathogens other than Ebola virus.
The 42-day period without new infections that had led to the announcement of an end to Ebola-virus transmission in West Africa represents two 21-day incubation cycles for the virus. Until the Sierra Leone case reported on Jan. 15, the last confirmed West African case had been identified in Liberia in mid-November. Liberia had previously been declared Ebola free in last May, but four new, isolated infections appeared subsequent to that transmitted by Ebola-infection survivors who still harbored infectious virus. Before the Jan. 15 case, an additional three such flare-ups occurred in Sierra Leone and another three in Guinea since last March, Dr. Brennan said.
The current tally on the West African Ebola outbreak stands at roughly 28,500 confirmed cases identified, and about 11,300 deaths. Nearly three-quarters of infections occurred during 2014. The case fatality rate at the start of the outbreak ran about 80%, noted Dr. Graaff, but gradually fell as infected patients began receiving better care. Near the outbreak’s end, the case fatality rate stood at roughly 35%, when most patients were receiving optimal clinical care.
WHO staffers are maintaining close surveillance of people who recently survived Ebola-virus infection so that they can identify and isolate any new infections. WHO personnel have also counseled these survivors on the risk they pose for potential transmission, primarily by unprotected sex by men for up to 12 months following the end of active infection. The WHO also plans to launch an investigational protocol to vaccinate sexual partners and other close contacts of adult male survivors with an as-yet unapproved Ebola vaccine to further reduce risk of new infections.
“The WHO and world community reacted slowly at the start of the Ebola outbreak” in early 2014, admitted Dr. Brennan. “Without question, the disease got away from us. In retrospect, there were a number of things that we should have done better and sooner,” he said. “We have done a lot of soul-searching and we [at WHO] have identified a number of weaknesses in our structures and systems. We have already taken several important steps, and we are undergoing major reforms of our emergency operations. I think you’ll see a much more effective WHO in the future.”
Reform of WHO systems for infection prevention and control “will be much better able to detect new cases, not only of Ebola, but of other important diseases,” said Dr. Graaff.
The United States is also strengthening its health screening and monitoring system for travelers coming from affected countries and improving its hospital preparedness to manage cases, said Alice C. Hill, senior adviser for preparedness and resilience at the National Security Council and special assistant to President Obama. Hill, who spoke Jan. 6 at the Public Health Emergency Medical Countermeasures Enterprise stakeholders workshop, acknowledged that challenges still exist that must be addressed, including the development of safe and effective diagnostics, treatments, and vaccines for existing infectious diseases such as influenza and more emerging threats such as Ebola or MERS (Middle East Respiratory Syndrome), developing accurate disease forecasting capabilities to predict what will be the next threat, building rapid clinical trial networks and manufacturing capabilities, and the abilities for mass dispensing of medical countermeasures.
Gregory Twachtman also contributed to this story.
On Twitter @mitchelzoler
A day after the World Health Organization declared on Jan. 14 that no known cases of Ebola-virus transmission or active infection had been identified in West Africa for more than 42 days, the agency revealed the existence of a new, single case of Ebola-virus infection in Sierra Leone.
The appearance of the new case highlighted the challenges that remain in fully stamping out the West African Ebola–virus outbreak. The crisis began in December 2013, raged throughout 2014, and only wound down toward a sputtering halt near the end of 2015.
When Dr. Rick Brennan, the World Health Organization (WHO) director for Emergency Risk Management and Humanitarian Response, announced during a press conference on Jan. 14, “the end of Ebola-virus transmission in West Africa” and “the first time since 2014 that all know chains of transmission have stopped in Guinea, Liberia, and Sierra Leone,” he and his colleague, Dr. Peter Graaff, also underscored the ongoing risk for sporadic, isolated cases. The main threat for new cases comes from men who survived Ebola-virus infection but harbored significant quantities of infectious virus in various body fluids and tissues, including their semen, for a period of about 1 year following their infection.
During the press conference, both Dr. Brennan and Dr. Graaff spoke of a new, strengthened infrastructure that WHO had placed in West Africa to better monitor and react quickly to these flare-up cases – the mechanism that led to quick identification of the new Sierra Leone case.
“I think you’ll see a more responsive and effective WHO,” said Dr. Graaff, WHO’s director of Ebola response. “We will use the Ebola experience to be more agile, more operational, and better able to react more quickly to whatever future problems come our way,” including infectious-disease outbreaks by pathogens other than Ebola virus.
The 42-day period without new infections that had led to the announcement of an end to Ebola-virus transmission in West Africa represents two 21-day incubation cycles for the virus. Until the Sierra Leone case reported on Jan. 15, the last confirmed West African case had been identified in Liberia in mid-November. Liberia had previously been declared Ebola free in last May, but four new, isolated infections appeared subsequent to that transmitted by Ebola-infection survivors who still harbored infectious virus. Before the Jan. 15 case, an additional three such flare-ups occurred in Sierra Leone and another three in Guinea since last March, Dr. Brennan said.
The current tally on the West African Ebola outbreak stands at roughly 28,500 confirmed cases identified, and about 11,300 deaths. Nearly three-quarters of infections occurred during 2014. The case fatality rate at the start of the outbreak ran about 80%, noted Dr. Graaff, but gradually fell as infected patients began receiving better care. Near the outbreak’s end, the case fatality rate stood at roughly 35%, when most patients were receiving optimal clinical care.
WHO staffers are maintaining close surveillance of people who recently survived Ebola-virus infection so that they can identify and isolate any new infections. WHO personnel have also counseled these survivors on the risk they pose for potential transmission, primarily by unprotected sex by men for up to 12 months following the end of active infection. The WHO also plans to launch an investigational protocol to vaccinate sexual partners and other close contacts of adult male survivors with an as-yet unapproved Ebola vaccine to further reduce risk of new infections.
“The WHO and world community reacted slowly at the start of the Ebola outbreak” in early 2014, admitted Dr. Brennan. “Without question, the disease got away from us. In retrospect, there were a number of things that we should have done better and sooner,” he said. “We have done a lot of soul-searching and we [at WHO] have identified a number of weaknesses in our structures and systems. We have already taken several important steps, and we are undergoing major reforms of our emergency operations. I think you’ll see a much more effective WHO in the future.”
Reform of WHO systems for infection prevention and control “will be much better able to detect new cases, not only of Ebola, but of other important diseases,” said Dr. Graaff.
The United States is also strengthening its health screening and monitoring system for travelers coming from affected countries and improving its hospital preparedness to manage cases, said Alice C. Hill, senior adviser for preparedness and resilience at the National Security Council and special assistant to President Obama. Hill, who spoke Jan. 6 at the Public Health Emergency Medical Countermeasures Enterprise stakeholders workshop, acknowledged that challenges still exist that must be addressed, including the development of safe and effective diagnostics, treatments, and vaccines for existing infectious diseases such as influenza and more emerging threats such as Ebola or MERS (Middle East Respiratory Syndrome), developing accurate disease forecasting capabilities to predict what will be the next threat, building rapid clinical trial networks and manufacturing capabilities, and the abilities for mass dispensing of medical countermeasures.
Gregory Twachtman also contributed to this story.
On Twitter @mitchelzoler
Many physicians don’t teach epinephrine use for food allergies
Many pediatricians and allergists failed to provide instructions for when and how to use epinephrine and a written emergency action plan to the parents of children with food allergies, a study found.
Researchers asked the parents of 859 children with allergies to share their level of satisfaction with the care and delivery of care from the pediatricians and allergists treating their children over the course of the previous 6 months. While more than 75% of the doctors treated the parents courteously and respectfully and provided clear explanations of children’s allergies, a high percentage of the doctors neglected to provide other information essential for caring for children with food allergies, the parents reported.
The parents most often said they were missing explanations on when and how their children should be receiving epinephrine to treat allergic reactions and instructions on exactly what to do if their children had a medical emergency related to their specific allergies and circumstances. More pediatricians than allergists failed to share such information.
Among allergists, 68% explained when to use epinephrine, while 37% of pediatricians provided such information, the parents reported. Instructions on how to use epinephrine were provided to parents by 47% of allergists and 20% of pediatricians. Written emergency health care plans customized to each child were provided by 56% of the allergists and 24% of the pediatricians
“Although pediatricians might be relying on allergists to deliver [an emergency action plan and training in epinephrine autoinjectors use], with the rise in food allergies, guidelines recommend that pediatricians conduct these steps and not rely solely on the allergist,” said Jesse A. Blumenstock of Northwestern University, Chicago, and colleagues. “With our understanding of food allergy and anaphylaxis constantly evolving, guidelines and recommendations for how and when to give epinephrine and the need for an action plan need to be reinforced by physicians.”
Read the study in the Journal of Allergy and Clinical Immunology: In Practice (doi: 10.1016/j.jaip.2015.10.011).
Many pediatricians and allergists failed to provide instructions for when and how to use epinephrine and a written emergency action plan to the parents of children with food allergies, a study found.
Researchers asked the parents of 859 children with allergies to share their level of satisfaction with the care and delivery of care from the pediatricians and allergists treating their children over the course of the previous 6 months. While more than 75% of the doctors treated the parents courteously and respectfully and provided clear explanations of children’s allergies, a high percentage of the doctors neglected to provide other information essential for caring for children with food allergies, the parents reported.
The parents most often said they were missing explanations on when and how their children should be receiving epinephrine to treat allergic reactions and instructions on exactly what to do if their children had a medical emergency related to their specific allergies and circumstances. More pediatricians than allergists failed to share such information.
Among allergists, 68% explained when to use epinephrine, while 37% of pediatricians provided such information, the parents reported. Instructions on how to use epinephrine were provided to parents by 47% of allergists and 20% of pediatricians. Written emergency health care plans customized to each child were provided by 56% of the allergists and 24% of the pediatricians
“Although pediatricians might be relying on allergists to deliver [an emergency action plan and training in epinephrine autoinjectors use], with the rise in food allergies, guidelines recommend that pediatricians conduct these steps and not rely solely on the allergist,” said Jesse A. Blumenstock of Northwestern University, Chicago, and colleagues. “With our understanding of food allergy and anaphylaxis constantly evolving, guidelines and recommendations for how and when to give epinephrine and the need for an action plan need to be reinforced by physicians.”
Read the study in the Journal of Allergy and Clinical Immunology: In Practice (doi: 10.1016/j.jaip.2015.10.011).
Many pediatricians and allergists failed to provide instructions for when and how to use epinephrine and a written emergency action plan to the parents of children with food allergies, a study found.
Researchers asked the parents of 859 children with allergies to share their level of satisfaction with the care and delivery of care from the pediatricians and allergists treating their children over the course of the previous 6 months. While more than 75% of the doctors treated the parents courteously and respectfully and provided clear explanations of children’s allergies, a high percentage of the doctors neglected to provide other information essential for caring for children with food allergies, the parents reported.
The parents most often said they were missing explanations on when and how their children should be receiving epinephrine to treat allergic reactions and instructions on exactly what to do if their children had a medical emergency related to their specific allergies and circumstances. More pediatricians than allergists failed to share such information.
Among allergists, 68% explained when to use epinephrine, while 37% of pediatricians provided such information, the parents reported. Instructions on how to use epinephrine were provided to parents by 47% of allergists and 20% of pediatricians. Written emergency health care plans customized to each child were provided by 56% of the allergists and 24% of the pediatricians
“Although pediatricians might be relying on allergists to deliver [an emergency action plan and training in epinephrine autoinjectors use], with the rise in food allergies, guidelines recommend that pediatricians conduct these steps and not rely solely on the allergist,” said Jesse A. Blumenstock of Northwestern University, Chicago, and colleagues. “With our understanding of food allergy and anaphylaxis constantly evolving, guidelines and recommendations for how and when to give epinephrine and the need for an action plan need to be reinforced by physicians.”
Read the study in the Journal of Allergy and Clinical Immunology: In Practice (doi: 10.1016/j.jaip.2015.10.011).
Bronchoscopic nitinol coils improve severe emphysema
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
FROM JAMA
Key clinical point: Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance in severe emphysema.
Major finding: 36% of patients who underwent coil placement achieved an improvement of at least 54 m in the 6-minute walk test, compared with only 18% who received usual care.
Data source: A preliminary randomized trial involving 100 patients treated at 10 university hospitals in France and followed for 1 year.
Disclosures: This study was supported by the French Ministry of Health. Dr. Deslee reported ties to PneumRx, maker of the coils tested in this study; his associates reported ties to PneumRx, Novatech, GlaxoSmithKline, Boehringer Ingelheim, Novartis, AstraZeneca, and Pulmonix.
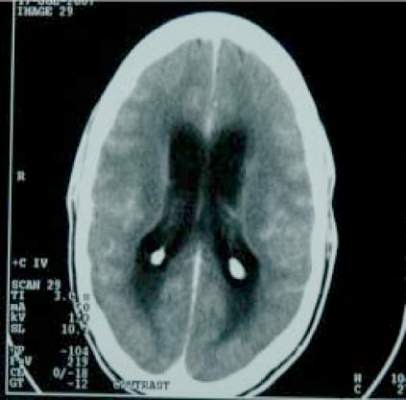
Tuberculous meningitis: Intensified anti-TB therapy not useful
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
These findings are disappointing and suggest that fluoroquinolones are not going to revolutionize the treatment of tuberculous meningitis, even though they may replace isoniazid because of their bactericidal activity. The 28% mortality and other measures of illness in both study groups were no better than those achieved by the standard therapy used in the 1950s.
It is also disappointing that three new drugs finally becoming available for this indication – bedaquiline, delamanid, and pretomanid – are highly protein bound and unlikely to freely penetrate the blood-brain barrier.
Dr. Peter R. Donald is at the Desmond Tutu TB Center and the department of pediatrics and child health at Stellenbosch University, Tygerberg (South Africa). He reported having no relevant financial disclosures. Dr. Donald made these remarks in an editorial accompanying Dr. Heemskerk’s report (New Engl J Med. 2016 Jan 14. doi:10.1056/NEJMe1511990).
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
Intensified antituberculosis therapy doesn’t appear to improve survival in adults with tuberculous meningitis, compared with standard treatment, according to a report published online Jan. 14 in the New England Journal of Medicine.
This result, from a 3-year randomized double-blind placebo controlled clinical trial involving 817 adults in Vietnam, contradicts findings from previous small studies which suggested that increasing the rifampin dose and adding a fluoroquinolone to the standard regimen might improve outcomes, said Dr. A. Dorothee Heemskerk of the Oxford University Clinical Research Unit, Ho Chi Minh City, Vietnam, and her associates.
Current guidelines recommend at least 2 months of therapy with four antituberculosis agents, followed by treatment with rifampin (10 mg/kg) and isoniazid for an additional 7-10 months. “However, these recommendations are based on data from pulmonary tuberculosis and do not take into account the differential ability of antituberculosis drugs to penetrate the brain,” the investigators noted.
The concentration of rifampin in cerebrospinal fluid reaches only 30% of that in the plasma, so it has been proposed that higher-dose rifampin (15 mg/kg) might be more effective for tuberculous meningitis. Fluoroquinolones such as levofloxacin were proposed because they are active against tuberculosis and achieve good penetration of the blood-brain barrier.
Dr. Heemskerk and her associates tested this hypothesis at two tertiary referral centers for severe cases of tuberculosis or infectious diseases in Vietnam. All the study participants received standard daily isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg), and ethambutol (20 mg/kg) for 3 months, followed by the same doses of rifampin and isoniazid for an additional 6 months. Approximately half (408 patients in the intensive-therapy group) received additional rifampin (5 mg/kg) and levofloxacin (20 mg/kg), while the other half (409 patients in the control group) received matching placebos.
The median patient age was 35 years. Approximately 43% of patients were coinfected with HIV.
The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94). The intensified treatment was no better than was standard treatment in any subgroup of patients or in any secondary outcomes, including neurologic disability and time to a new neurologic event or death, the investigators said (N Engl J Med. 2016 Jan 14. doi:10.1056/NEJMoa1507062).
However, intensive therapy was associated with a higher frequency of seizures (23 vs. 11 patients), visual impairment (14 vs. 4 patients), allergic reactions (30 patients vs. 17 patients), jaundice (19 vs. 7 patients), grade 3 or 4 hyponatremia (112 patients vs. 81 patients), and adverse events leading to treatment interruptions (95 patients vs. 64 patients).
It is possible that raising the dose of rifampin by only 5 mg/kg may not have increased intracerebral drug concentrations “sufficiently to enhance bacterial killing. Recent data suggest that much higher doses (up to 35 mg/kg per day) may have an acceptable side-effect profile and may be necessary to significantly increase the killing of M. tuberculosis in pulmonary tuberculosis,” Dr. Heemskerk and her associates noted.
“Although the results of our study do not support a change in the currently recommended treatment regimens for tuberculous meningitis, enhanced antituberculosis treatment with higher doses of first-line drugs, including intravenous rifampin, or the newer antituberculosis drugs bedaquiline and delamanid, still require investigation,” they added.
Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Intensified anti-TB therapy doesn’t improve survival, compared with standard treatment, in adults with tuberculous meningitis.
Major finding: The primary outcome measure – death at 9-month follow-up – occurred in 113 of the intensive-therapy group and 114 of the control group, a nonsignificant difference (HR, 0.94).
Data source: A 3-year randomized double-blind placebo-controlled trial involving 817 Vietnamese adults followed for 9 months.
Disclosures: Wellcome Trust and the Li Ka Shing Foundation supported the study. Dr. Heemskerk and her associates reported having no relevant disclosures.
Short sleep duration in hypertensives ups mortality
ORLANDO – Hypertensive persons who sleep 5 hours or less per night have a significantly higher all-cause mortality rate than those who get more shut-eye, according to an analysis from the Penn State Adult Cohort Study.
“We found that the odds of all-cause mortality associated with hypertension increased in a dose-response manner as a function of the degree of objective short sleep duration, even after adjusting for a multitude of factors,” Julio Fernandez-Mendoza, Ph.D., reported at the American Heart Association scientific sessions.
The Penn State Adult Cohort consists of a random, general population sample of 1,741 men and women who enrolled in the study back in the 1990s, at a mean age of 48.7 years. As part of their comprehensive evaluation they were studied in the overnight sleep laboratory. The cohort has been followed for 15.5 years, during which 20% of subjects died.
As expected, hypertension was associated with increased risk of all-cause mortality in the Penn State Adult Cohort. But Dr. Fernandez-Mendoza and coinvestigators further dissected this association by incorporating the subjects’ objective sleep lab data, something that hadn’t been done in other studies. They found that while as a group the roughly 35% of study participants with hypertension had an adjusted 2.54-fold increased risk of all-cause mortality, compared with normotensive subjects, those who slept 6 or more hours at night – placing them at or above the 50th percentile for sleep duration – had a 1.75-fold increased risk, which just barely reached statistical significance.
In contrast, those who slept 5-6 hours per night were at 2.36-fold increased risk of all-cause mortality, while hypertensives in the bottom quartile for sleep duration with 5 hours or less of sleep had an even more robust 4.04-fold increased risk. All risk figures were determined in a multivariate logistic regression analysis extensively adjusted for age, gender, race, diabetes, obesity, smoking, depression, insomnia, sleep apnea, and history of heart disease or stroke.
This finding of an inverse association between sleep duration and all-cause mortality was consistent with the investigators’ study hypothesis that short sleep duration in hypertensive patients may be a marker of the severity of autonomic dysfunction. After all, it is known that the autonomic nervous system not only controls cardiovascular function, it also regulates sleep, explained Dr. Fernandez-Mendoza, a behavioral psychologist at Pennsylvania State University in Hershey.
Other possible explanations for the findings are that short sleep duration in hypertensive patients might be genetically driven or behaviorally induced, but he considers these less plausible.
In an interview, Dr. Fernandez-Mendoza said he and his coinvestigators have found the same relationship between short sleep duration and increased all-cause mortality in Penn State Adult Cohort members with diabetes or dyslipidemia, although he didn’t present those data at the AHA meeting.
If indeed short sleep duration is a marker of autonomic dysfunction, it would have important clinical implications: “Objective sleep duration may allow for refinement of estimates of mortality risk. I predict that someday cardiovascular risk calculators will incorporate sleep duration,” he said.
The Penn State Adult Cohort findings bring a measure of clarity to what has been a somewhat cloudy area, Dr. Fernandez-Mendoza said. Most prior epidemiologic studies of sleep’s impact on health have relied upon self-reported sleep duration, which is considerably less reliable than objectively measured sleep lab data. And many studies have looked at sleep duration as an isolated variable in relation to morbidity and mortality risk. This, he said, has contributed to public misunderstanding.
“We have people coming into the sleep lab thinking, ‘If I don’t get 7 hours of sleep I’m going to die,’ ” according to the sleep scientist. “But the paradigm we’ve developed, tied to what we know about autonomic control, is that the cardiovascular system and the sleep system are connected to each other. It doesn’t mean that short sleep kills you, it’s that the combination of the traditional cardiometabolic risk factors and short sleep increases risk of morbidity and mortality.”
Dr. Fernandez-Mendoza’s study was funded by an AHA Scientist Development Grant. He reported having no financial conflicts of interest.
ORLANDO – Hypertensive persons who sleep 5 hours or less per night have a significantly higher all-cause mortality rate than those who get more shut-eye, according to an analysis from the Penn State Adult Cohort Study.
“We found that the odds of all-cause mortality associated with hypertension increased in a dose-response manner as a function of the degree of objective short sleep duration, even after adjusting for a multitude of factors,” Julio Fernandez-Mendoza, Ph.D., reported at the American Heart Association scientific sessions.
The Penn State Adult Cohort consists of a random, general population sample of 1,741 men and women who enrolled in the study back in the 1990s, at a mean age of 48.7 years. As part of their comprehensive evaluation they were studied in the overnight sleep laboratory. The cohort has been followed for 15.5 years, during which 20% of subjects died.
As expected, hypertension was associated with increased risk of all-cause mortality in the Penn State Adult Cohort. But Dr. Fernandez-Mendoza and coinvestigators further dissected this association by incorporating the subjects’ objective sleep lab data, something that hadn’t been done in other studies. They found that while as a group the roughly 35% of study participants with hypertension had an adjusted 2.54-fold increased risk of all-cause mortality, compared with normotensive subjects, those who slept 6 or more hours at night – placing them at or above the 50th percentile for sleep duration – had a 1.75-fold increased risk, which just barely reached statistical significance.
In contrast, those who slept 5-6 hours per night were at 2.36-fold increased risk of all-cause mortality, while hypertensives in the bottom quartile for sleep duration with 5 hours or less of sleep had an even more robust 4.04-fold increased risk. All risk figures were determined in a multivariate logistic regression analysis extensively adjusted for age, gender, race, diabetes, obesity, smoking, depression, insomnia, sleep apnea, and history of heart disease or stroke.
This finding of an inverse association between sleep duration and all-cause mortality was consistent with the investigators’ study hypothesis that short sleep duration in hypertensive patients may be a marker of the severity of autonomic dysfunction. After all, it is known that the autonomic nervous system not only controls cardiovascular function, it also regulates sleep, explained Dr. Fernandez-Mendoza, a behavioral psychologist at Pennsylvania State University in Hershey.
Other possible explanations for the findings are that short sleep duration in hypertensive patients might be genetically driven or behaviorally induced, but he considers these less plausible.
In an interview, Dr. Fernandez-Mendoza said he and his coinvestigators have found the same relationship between short sleep duration and increased all-cause mortality in Penn State Adult Cohort members with diabetes or dyslipidemia, although he didn’t present those data at the AHA meeting.
If indeed short sleep duration is a marker of autonomic dysfunction, it would have important clinical implications: “Objective sleep duration may allow for refinement of estimates of mortality risk. I predict that someday cardiovascular risk calculators will incorporate sleep duration,” he said.
The Penn State Adult Cohort findings bring a measure of clarity to what has been a somewhat cloudy area, Dr. Fernandez-Mendoza said. Most prior epidemiologic studies of sleep’s impact on health have relied upon self-reported sleep duration, which is considerably less reliable than objectively measured sleep lab data. And many studies have looked at sleep duration as an isolated variable in relation to morbidity and mortality risk. This, he said, has contributed to public misunderstanding.
“We have people coming into the sleep lab thinking, ‘If I don’t get 7 hours of sleep I’m going to die,’ ” according to the sleep scientist. “But the paradigm we’ve developed, tied to what we know about autonomic control, is that the cardiovascular system and the sleep system are connected to each other. It doesn’t mean that short sleep kills you, it’s that the combination of the traditional cardiometabolic risk factors and short sleep increases risk of morbidity and mortality.”
Dr. Fernandez-Mendoza’s study was funded by an AHA Scientist Development Grant. He reported having no financial conflicts of interest.
ORLANDO – Hypertensive persons who sleep 5 hours or less per night have a significantly higher all-cause mortality rate than those who get more shut-eye, according to an analysis from the Penn State Adult Cohort Study.
“We found that the odds of all-cause mortality associated with hypertension increased in a dose-response manner as a function of the degree of objective short sleep duration, even after adjusting for a multitude of factors,” Julio Fernandez-Mendoza, Ph.D., reported at the American Heart Association scientific sessions.
The Penn State Adult Cohort consists of a random, general population sample of 1,741 men and women who enrolled in the study back in the 1990s, at a mean age of 48.7 years. As part of their comprehensive evaluation they were studied in the overnight sleep laboratory. The cohort has been followed for 15.5 years, during which 20% of subjects died.
As expected, hypertension was associated with increased risk of all-cause mortality in the Penn State Adult Cohort. But Dr. Fernandez-Mendoza and coinvestigators further dissected this association by incorporating the subjects’ objective sleep lab data, something that hadn’t been done in other studies. They found that while as a group the roughly 35% of study participants with hypertension had an adjusted 2.54-fold increased risk of all-cause mortality, compared with normotensive subjects, those who slept 6 or more hours at night – placing them at or above the 50th percentile for sleep duration – had a 1.75-fold increased risk, which just barely reached statistical significance.
In contrast, those who slept 5-6 hours per night were at 2.36-fold increased risk of all-cause mortality, while hypertensives in the bottom quartile for sleep duration with 5 hours or less of sleep had an even more robust 4.04-fold increased risk. All risk figures were determined in a multivariate logistic regression analysis extensively adjusted for age, gender, race, diabetes, obesity, smoking, depression, insomnia, sleep apnea, and history of heart disease or stroke.
This finding of an inverse association between sleep duration and all-cause mortality was consistent with the investigators’ study hypothesis that short sleep duration in hypertensive patients may be a marker of the severity of autonomic dysfunction. After all, it is known that the autonomic nervous system not only controls cardiovascular function, it also regulates sleep, explained Dr. Fernandez-Mendoza, a behavioral psychologist at Pennsylvania State University in Hershey.
Other possible explanations for the findings are that short sleep duration in hypertensive patients might be genetically driven or behaviorally induced, but he considers these less plausible.
In an interview, Dr. Fernandez-Mendoza said he and his coinvestigators have found the same relationship between short sleep duration and increased all-cause mortality in Penn State Adult Cohort members with diabetes or dyslipidemia, although he didn’t present those data at the AHA meeting.
If indeed short sleep duration is a marker of autonomic dysfunction, it would have important clinical implications: “Objective sleep duration may allow for refinement of estimates of mortality risk. I predict that someday cardiovascular risk calculators will incorporate sleep duration,” he said.
The Penn State Adult Cohort findings bring a measure of clarity to what has been a somewhat cloudy area, Dr. Fernandez-Mendoza said. Most prior epidemiologic studies of sleep’s impact on health have relied upon self-reported sleep duration, which is considerably less reliable than objectively measured sleep lab data. And many studies have looked at sleep duration as an isolated variable in relation to morbidity and mortality risk. This, he said, has contributed to public misunderstanding.
“We have people coming into the sleep lab thinking, ‘If I don’t get 7 hours of sleep I’m going to die,’ ” according to the sleep scientist. “But the paradigm we’ve developed, tied to what we know about autonomic control, is that the cardiovascular system and the sleep system are connected to each other. It doesn’t mean that short sleep kills you, it’s that the combination of the traditional cardiometabolic risk factors and short sleep increases risk of morbidity and mortality.”
Dr. Fernandez-Mendoza’s study was funded by an AHA Scientist Development Grant. He reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The shorter a hypertensive patient’s objectively measured sleep duration, the greater the all-cause mortality risk, compared with normotensives.
Major finding: Hypertensive persons with 5 hours of sleep or less were at 4.04-fold increased risk of all-cause mortality, compared with normotensives. Those with a sleep duration of 5-6 hours were at 2.36-fold increased risk, while hypertensives with a sleep duration of 6 hours or more were at 1.75-fold increased risk.
Data source: This study involved 1,741 participants in the Penn State Adult Cohort followed prospectively for 15.5 years.
Disclosures: The presenter’s study was funded by an AHA Scientist Development Grant. He reported having no financial conflicts of interest.
HIV-TB coinfection strongly associated with poor TB treatment outcomes
A large European study published in the journal AIDS has confirmed that HIV-positive status is a strong risk factor for an adverse tuberculosis treatment outcome.
Researchers at the Robert Koch Institute in Berlin analyzed the treatment outcomes of 61,138 TB cases reported from nine European countries during 2010-2012, and investigated the effect of HIV on TB outcomes using multilevel and multinomial logistic models. They also considered the interaction between HIV and multidrug-resistant TB (MDR-TB).
According to lead author Basel Karo and his colleagues, 5.5% of the TB cases analyzed were HIV positive. HIV coinfected cases had a significantly lower TB treatment success rate, compared with HIV-negative cases (57% vs. 79%). In the multilevel model adjusted for age and an interaction with MDR-TB, HIV was significantly associated with lower treatment success in all MDR strata, while in the multinomial regression model, HIV-positive cases had significantly higher relative risk ratio for death. Mr. Karo and coauthors said an increased risk of still being on treatment (more than 12 months for non-MDR-TB; more than 24 months for MDR-TB) is another indicator of less successful TB regimens in HIV-positive patients. The research team did not find any significant association between HIV and TB treatment failure.
Negative treatment outcomes may be explained by difficulties in diagnosis of TB, sometimes due to “alternation of the clinical manifestation of TB and lack of a rapid and sensitive TB diagnostic test” in HIV coinfected patients, which may lead to a delayed diagnosis and treatment. TB treatment of TB in HIV coinfected patients also “presents with major challenges regarding the drug interactions between the rifamycins and some antiretroviral agents, overlapping toxic effects, and the occurrence of immune reconstitution inflammatory syndrome (IRIS),” the investigators said.
The results of the trial should encourage future studies “including randomized clinical trials to investigate the optimal duration of TB treatment in HIV coinfected individuals,” Mr. Karo said.
Read the study in the journal AIDS (AIDS. 2016 Jan 8. doi:10.1097/QAD.0000000000001016).
On Twitter @richpizzi
A large European study published in the journal AIDS has confirmed that HIV-positive status is a strong risk factor for an adverse tuberculosis treatment outcome.
Researchers at the Robert Koch Institute in Berlin analyzed the treatment outcomes of 61,138 TB cases reported from nine European countries during 2010-2012, and investigated the effect of HIV on TB outcomes using multilevel and multinomial logistic models. They also considered the interaction between HIV and multidrug-resistant TB (MDR-TB).
According to lead author Basel Karo and his colleagues, 5.5% of the TB cases analyzed were HIV positive. HIV coinfected cases had a significantly lower TB treatment success rate, compared with HIV-negative cases (57% vs. 79%). In the multilevel model adjusted for age and an interaction with MDR-TB, HIV was significantly associated with lower treatment success in all MDR strata, while in the multinomial regression model, HIV-positive cases had significantly higher relative risk ratio for death. Mr. Karo and coauthors said an increased risk of still being on treatment (more than 12 months for non-MDR-TB; more than 24 months for MDR-TB) is another indicator of less successful TB regimens in HIV-positive patients. The research team did not find any significant association between HIV and TB treatment failure.
Negative treatment outcomes may be explained by difficulties in diagnosis of TB, sometimes due to “alternation of the clinical manifestation of TB and lack of a rapid and sensitive TB diagnostic test” in HIV coinfected patients, which may lead to a delayed diagnosis and treatment. TB treatment of TB in HIV coinfected patients also “presents with major challenges regarding the drug interactions between the rifamycins and some antiretroviral agents, overlapping toxic effects, and the occurrence of immune reconstitution inflammatory syndrome (IRIS),” the investigators said.
The results of the trial should encourage future studies “including randomized clinical trials to investigate the optimal duration of TB treatment in HIV coinfected individuals,” Mr. Karo said.
Read the study in the journal AIDS (AIDS. 2016 Jan 8. doi:10.1097/QAD.0000000000001016).
On Twitter @richpizzi
A large European study published in the journal AIDS has confirmed that HIV-positive status is a strong risk factor for an adverse tuberculosis treatment outcome.
Researchers at the Robert Koch Institute in Berlin analyzed the treatment outcomes of 61,138 TB cases reported from nine European countries during 2010-2012, and investigated the effect of HIV on TB outcomes using multilevel and multinomial logistic models. They also considered the interaction between HIV and multidrug-resistant TB (MDR-TB).
According to lead author Basel Karo and his colleagues, 5.5% of the TB cases analyzed were HIV positive. HIV coinfected cases had a significantly lower TB treatment success rate, compared with HIV-negative cases (57% vs. 79%). In the multilevel model adjusted for age and an interaction with MDR-TB, HIV was significantly associated with lower treatment success in all MDR strata, while in the multinomial regression model, HIV-positive cases had significantly higher relative risk ratio for death. Mr. Karo and coauthors said an increased risk of still being on treatment (more than 12 months for non-MDR-TB; more than 24 months for MDR-TB) is another indicator of less successful TB regimens in HIV-positive patients. The research team did not find any significant association between HIV and TB treatment failure.
Negative treatment outcomes may be explained by difficulties in diagnosis of TB, sometimes due to “alternation of the clinical manifestation of TB and lack of a rapid and sensitive TB diagnostic test” in HIV coinfected patients, which may lead to a delayed diagnosis and treatment. TB treatment of TB in HIV coinfected patients also “presents with major challenges regarding the drug interactions between the rifamycins and some antiretroviral agents, overlapping toxic effects, and the occurrence of immune reconstitution inflammatory syndrome (IRIS),” the investigators said.
The results of the trial should encourage future studies “including randomized clinical trials to investigate the optimal duration of TB treatment in HIV coinfected individuals,” Mr. Karo said.
Read the study in the journal AIDS (AIDS. 2016 Jan 8. doi:10.1097/QAD.0000000000001016).
On Twitter @richpizzi
FROM AIDS
Pertussis vaccine possibly ineffective in preschoolers
Preschool-age children who have been fully vaccinated against pertussis can still develop symptoms of illness consistent with a whooping cough diagnosis, according to a study of toddlers in a Tallahassee, Fla., school that experienced an outbreak of pertussis in late 2013 (Emerg Infect Dis. 2016 Feb;22[2]. doi: 10.3201/eid2202.150325)
The study, published in Emerging Infectious Diseases by the Centers for Disease Control and Prevention, is the result of an outbreak investigation at the preschool that began after a 1-year-old and two 3-year-old children developed illness consistent with pertussis, and were confirmed to have pertussis after undergoing a polymerase chain reaction (PCR) test.
The Florida Department of Health administered a questionnaire to be completed by families of the 117 students (ages 10 months to 6 years) and 26 staff members. Questionnaire completion rate was 98%, with three student households and one staff household failing to complete it.
Overall, 28 cases were determined to be “probable” pertussis and 11 were confirmed as pertussis via PCR or other laboratory testing methods. Of these, 26 were students aged 1-5 years (22% of total student population), 2 were attributed to the staff (7%), and 11 were linked to the preschool, of which 9 originated from the households of the individual students and 2 from “camp counselors who had contact with a sibling of a laboratory-confirmed case-patient who attended the preschool.”
However, 28 of the students who had pertussis had received at least three vaccinations, with 23 of them having received at least four vaccinations, meaning they were classified as being fully vaccinated against the disease. Only 5 out of the school’s 117 children had not received the complete series of vaccinations, out of which 2 ended up being case-patients; both of those children, however, had received at least one vaccination prior to falling sick.
“Poor performance of a vaccine in a defined cohort might suggest a provider-level failure to store, use, and administer the vaccine properly,” noted the researchers, led by Dr. James Matthias of the Florida Department of Health. “Although we did not assess vaccine storage and handling practices, children from this investigation were seen by multiple providers in the community [and] no general increase in reported pertussis incidence was observed in the county at the same time as this outbreak.”
The bottom line, the authors concluded, is for pediatricians and primary care doctors to be wary that vaccination against pertussis doesn’t necessarily mean patients can’t ever get it. If pertussis symptoms arise in a vaccinated child, especially one 5 years old or younger, it may still be whooping cough.
The CDC supported the study. Dr. Matthias and his coauthors are all affiliated with the Florida Department of Health and the CDC, but reported no other relevant financial disclosures.
Preschool-age children who have been fully vaccinated against pertussis can still develop symptoms of illness consistent with a whooping cough diagnosis, according to a study of toddlers in a Tallahassee, Fla., school that experienced an outbreak of pertussis in late 2013 (Emerg Infect Dis. 2016 Feb;22[2]. doi: 10.3201/eid2202.150325)
The study, published in Emerging Infectious Diseases by the Centers for Disease Control and Prevention, is the result of an outbreak investigation at the preschool that began after a 1-year-old and two 3-year-old children developed illness consistent with pertussis, and were confirmed to have pertussis after undergoing a polymerase chain reaction (PCR) test.
The Florida Department of Health administered a questionnaire to be completed by families of the 117 students (ages 10 months to 6 years) and 26 staff members. Questionnaire completion rate was 98%, with three student households and one staff household failing to complete it.
Overall, 28 cases were determined to be “probable” pertussis and 11 were confirmed as pertussis via PCR or other laboratory testing methods. Of these, 26 were students aged 1-5 years (22% of total student population), 2 were attributed to the staff (7%), and 11 were linked to the preschool, of which 9 originated from the households of the individual students and 2 from “camp counselors who had contact with a sibling of a laboratory-confirmed case-patient who attended the preschool.”
However, 28 of the students who had pertussis had received at least three vaccinations, with 23 of them having received at least four vaccinations, meaning they were classified as being fully vaccinated against the disease. Only 5 out of the school’s 117 children had not received the complete series of vaccinations, out of which 2 ended up being case-patients; both of those children, however, had received at least one vaccination prior to falling sick.
“Poor performance of a vaccine in a defined cohort might suggest a provider-level failure to store, use, and administer the vaccine properly,” noted the researchers, led by Dr. James Matthias of the Florida Department of Health. “Although we did not assess vaccine storage and handling practices, children from this investigation were seen by multiple providers in the community [and] no general increase in reported pertussis incidence was observed in the county at the same time as this outbreak.”
The bottom line, the authors concluded, is for pediatricians and primary care doctors to be wary that vaccination against pertussis doesn’t necessarily mean patients can’t ever get it. If pertussis symptoms arise in a vaccinated child, especially one 5 years old or younger, it may still be whooping cough.
The CDC supported the study. Dr. Matthias and his coauthors are all affiliated with the Florida Department of Health and the CDC, but reported no other relevant financial disclosures.
Preschool-age children who have been fully vaccinated against pertussis can still develop symptoms of illness consistent with a whooping cough diagnosis, according to a study of toddlers in a Tallahassee, Fla., school that experienced an outbreak of pertussis in late 2013 (Emerg Infect Dis. 2016 Feb;22[2]. doi: 10.3201/eid2202.150325)
The study, published in Emerging Infectious Diseases by the Centers for Disease Control and Prevention, is the result of an outbreak investigation at the preschool that began after a 1-year-old and two 3-year-old children developed illness consistent with pertussis, and were confirmed to have pertussis after undergoing a polymerase chain reaction (PCR) test.
The Florida Department of Health administered a questionnaire to be completed by families of the 117 students (ages 10 months to 6 years) and 26 staff members. Questionnaire completion rate was 98%, with three student households and one staff household failing to complete it.
Overall, 28 cases were determined to be “probable” pertussis and 11 were confirmed as pertussis via PCR or other laboratory testing methods. Of these, 26 were students aged 1-5 years (22% of total student population), 2 were attributed to the staff (7%), and 11 were linked to the preschool, of which 9 originated from the households of the individual students and 2 from “camp counselors who had contact with a sibling of a laboratory-confirmed case-patient who attended the preschool.”
However, 28 of the students who had pertussis had received at least three vaccinations, with 23 of them having received at least four vaccinations, meaning they were classified as being fully vaccinated against the disease. Only 5 out of the school’s 117 children had not received the complete series of vaccinations, out of which 2 ended up being case-patients; both of those children, however, had received at least one vaccination prior to falling sick.
“Poor performance of a vaccine in a defined cohort might suggest a provider-level failure to store, use, and administer the vaccine properly,” noted the researchers, led by Dr. James Matthias of the Florida Department of Health. “Although we did not assess vaccine storage and handling practices, children from this investigation were seen by multiple providers in the community [and] no general increase in reported pertussis incidence was observed in the county at the same time as this outbreak.”
The bottom line, the authors concluded, is for pediatricians and primary care doctors to be wary that vaccination against pertussis doesn’t necessarily mean patients can’t ever get it. If pertussis symptoms arise in a vaccinated child, especially one 5 years old or younger, it may still be whooping cough.
The CDC supported the study. Dr. Matthias and his coauthors are all affiliated with the Florida Department of Health and the CDC, but reported no other relevant financial disclosures.
FROM EMERGING INFECTIOUS DISEASES
Key clinical point: Preschoolers vaccinated against pertussis may still develop whooping cough or similar symptoms.
Major finding: Children who had received full series of pertussis vaccinations still developed whooping cough during an outbreak at a school of 117 children.
Data source: Survey of 117 students and 26 staff members at a Tallahassee, Fla., school in 2014.
Disclosures: The CDC supported the study. Dr. Matthias and his coauthors are all affiliated with the Florida Department of Health and the CDC, but reported no other relevant financial disclosures.
Flu activity high in New Jersey, South Carolina
Week 12 of the 2015-2016 U.S. flu season saw two states in the “high” range of the influenza-like illness (ILI) activity scale, the Centers for Disease Control and Prevention reported.
New Jersey was at level 10 on the CDC’s 1-10 scale for the week ending Jan. 2, 2016, and South Carolina was at level 9. The next-most-active state, Texas, was at level 7, putting it in the “moderate” range along with Maryland, which was at level 6, the CDC said.
States in the “low” range were Arizona, Oklahoma, Pennsylvania, and Virginia at level 5 and California, Colorado, and Georgia at level 4. Altogether, there were 24 states at level 2 or higher, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
Puerto Rico also moved up to level 10 for the week ending Jan. 2 and, in a case of geographic concentration, New York City was at level 6 even though New York State was still at level 1.
The proportion of outpatient visits for ILI nationally was 2.8% at the end of week 12, which is above the national baseline of 2.1%. For comparison, at this point in the 2014-2015 flu season, the proportion of visits for ILI was about 6%, and in 2013-2014 it was around 4.5%.
There were two flu-related pediatric deaths reported during the week, bringing the total to six for the 2015-2016 season. One death was associated with an influenza A (H3) virus and the other was associated with
an influenza A (H1N1)pdm09 virus. Looking again at previous years, there had been single weeks with at least six pediatric deaths by week 12 in each of the last three seasons, the CDC report showed.
Week 12 of the 2015-2016 U.S. flu season saw two states in the “high” range of the influenza-like illness (ILI) activity scale, the Centers for Disease Control and Prevention reported.
New Jersey was at level 10 on the CDC’s 1-10 scale for the week ending Jan. 2, 2016, and South Carolina was at level 9. The next-most-active state, Texas, was at level 7, putting it in the “moderate” range along with Maryland, which was at level 6, the CDC said.
States in the “low” range were Arizona, Oklahoma, Pennsylvania, and Virginia at level 5 and California, Colorado, and Georgia at level 4. Altogether, there were 24 states at level 2 or higher, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
Puerto Rico also moved up to level 10 for the week ending Jan. 2 and, in a case of geographic concentration, New York City was at level 6 even though New York State was still at level 1.
The proportion of outpatient visits for ILI nationally was 2.8% at the end of week 12, which is above the national baseline of 2.1%. For comparison, at this point in the 2014-2015 flu season, the proportion of visits for ILI was about 6%, and in 2013-2014 it was around 4.5%.
There were two flu-related pediatric deaths reported during the week, bringing the total to six for the 2015-2016 season. One death was associated with an influenza A (H3) virus and the other was associated with
an influenza A (H1N1)pdm09 virus. Looking again at previous years, there had been single weeks with at least six pediatric deaths by week 12 in each of the last three seasons, the CDC report showed.
Week 12 of the 2015-2016 U.S. flu season saw two states in the “high” range of the influenza-like illness (ILI) activity scale, the Centers for Disease Control and Prevention reported.
New Jersey was at level 10 on the CDC’s 1-10 scale for the week ending Jan. 2, 2016, and South Carolina was at level 9. The next-most-active state, Texas, was at level 7, putting it in the “moderate” range along with Maryland, which was at level 6, the CDC said.
States in the “low” range were Arizona, Oklahoma, Pennsylvania, and Virginia at level 5 and California, Colorado, and Georgia at level 4. Altogether, there were 24 states at level 2 or higher, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
Puerto Rico also moved up to level 10 for the week ending Jan. 2 and, in a case of geographic concentration, New York City was at level 6 even though New York State was still at level 1.
The proportion of outpatient visits for ILI nationally was 2.8% at the end of week 12, which is above the national baseline of 2.1%. For comparison, at this point in the 2014-2015 flu season, the proportion of visits for ILI was about 6%, and in 2013-2014 it was around 4.5%.
There were two flu-related pediatric deaths reported during the week, bringing the total to six for the 2015-2016 season. One death was associated with an influenza A (H3) virus and the other was associated with
an influenza A (H1N1)pdm09 virus. Looking again at previous years, there had been single weeks with at least six pediatric deaths by week 12 in each of the last three seasons, the CDC report showed.
Infectious disease in elderly a significant burden for EDs
More U.S. adults over the age of 65 visited an emergency department because of an infectious disease than for myocardial infarction and congestive heart failure combined, according to a new study.
Based on a nationwide ED sample, adults over 65 visited the ED just over 3.1 million times in 2012 due to infectious diseases (ID), more than three times the estimated amount for myocardial infarction and congestive heart failure. The most common diagnoses were lower respiratory infections (26.2%), urinary tract infections (25.3%), and septicemia (18.9%).
Of the 3.1 million cases brought to the ED, nearly 1.8 million cases were hospitalized, with septicemia the most common cause for hospitalization, accounting for 32.2% of ID-related hospitalizations, followed by lower respiratory infections. Septicemia was also the most common cause of mortality, accounting for 74.7% of the nearly 124,000 deaths.
“These observations underscore the importance of integrated strategies aimed at reducing ID-related morbidity and health care use of elderly adults as a national priority for research, health policy, and community action,” Dr. Tadahiro Goto of the University of Fukui (Japan) Hospital and his associates concluded.
Find the full study in the Journal of the American Geriatrics Society (2015 Dec 23. doi: 101111/jgs.13836).
More U.S. adults over the age of 65 visited an emergency department because of an infectious disease than for myocardial infarction and congestive heart failure combined, according to a new study.
Based on a nationwide ED sample, adults over 65 visited the ED just over 3.1 million times in 2012 due to infectious diseases (ID), more than three times the estimated amount for myocardial infarction and congestive heart failure. The most common diagnoses were lower respiratory infections (26.2%), urinary tract infections (25.3%), and septicemia (18.9%).
Of the 3.1 million cases brought to the ED, nearly 1.8 million cases were hospitalized, with septicemia the most common cause for hospitalization, accounting for 32.2% of ID-related hospitalizations, followed by lower respiratory infections. Septicemia was also the most common cause of mortality, accounting for 74.7% of the nearly 124,000 deaths.
“These observations underscore the importance of integrated strategies aimed at reducing ID-related morbidity and health care use of elderly adults as a national priority for research, health policy, and community action,” Dr. Tadahiro Goto of the University of Fukui (Japan) Hospital and his associates concluded.
Find the full study in the Journal of the American Geriatrics Society (2015 Dec 23. doi: 101111/jgs.13836).
More U.S. adults over the age of 65 visited an emergency department because of an infectious disease than for myocardial infarction and congestive heart failure combined, according to a new study.
Based on a nationwide ED sample, adults over 65 visited the ED just over 3.1 million times in 2012 due to infectious diseases (ID), more than three times the estimated amount for myocardial infarction and congestive heart failure. The most common diagnoses were lower respiratory infections (26.2%), urinary tract infections (25.3%), and septicemia (18.9%).
Of the 3.1 million cases brought to the ED, nearly 1.8 million cases were hospitalized, with septicemia the most common cause for hospitalization, accounting for 32.2% of ID-related hospitalizations, followed by lower respiratory infections. Septicemia was also the most common cause of mortality, accounting for 74.7% of the nearly 124,000 deaths.
“These observations underscore the importance of integrated strategies aimed at reducing ID-related morbidity and health care use of elderly adults as a national priority for research, health policy, and community action,” Dr. Tadahiro Goto of the University of Fukui (Japan) Hospital and his associates concluded.
Find the full study in the Journal of the American Geriatrics Society (2015 Dec 23. doi: 101111/jgs.13836).
FROM JOURNAL OF THE AMERICAN GERIATRICS SOCIETY
LAIV, IIV almost equally effective against influenza
When vaccinating children against influenza, inactivated and live attenuated influenza vaccines show little significant difference in effectiveness against nearly all strains of the virus, according to a new study in Pediatrics.
However, the study – which examined the effectiveness of IIV and LAIV across four consecutive influenza seasons between 2010 and 2014 – cautions that the 2013-2014 season’s A/(H1N1)pdm09 showed an uncharacteristically large gap in effectiveness favoring IIV, a discrepancy likely due to a problem with a vaccine component in LAIV. (Pediatrics. 2016;137(2):e20153279)
“We found that lower LAIV effectiveness in 2013-2014 was specific to the A/(H1N1)pdm09 vaccine component and was consistent with a previously unexamined effect during the 2010-2011 influenza season,” Jessie R. Chung of the influenza division at the Centers for Disease Control and Prevention and associates wrote, adding that the impetus for the study was the lack of available data “from observational studies after the 2009 pandemic on relative effectiveness of LAIV and IIV in children and adolescents.”
Ms. Chung* and coinvestigators enrolled children aged 2-17 years from clinics and hospitals in Michigan, New York, Pennsylvania, Tennessee, Texas, Washington, and Wisconsin during the 2010-2011, 2011-2012, 2012-2013, and 2013-2014 influenza seasons. Children brought in with symptoms of acute respiratory illness – cough, fever, or feverishness – had nasal and throat swabs collected to test for presence and type of influenza.
In total, 7,718 subjects were evaluated across the four influenza seasons, but after excluding subjects for various reasons – unknown vaccine type, indeterminate vaccine status, and inconclusive reverse transcription polymerase chain reaction results, among others – 6,819 subjects were included for vaccine effectiveness analysis, of which 2,703 were ultimately matched age appropriately and placed into IIV and LAIV cohorts for comparison. The IIV cohort consisted of 2,066 individuals (76.4%), while the LAIV cohort had 637 (23.6%).
During the 2010-2011 season, 66 of the 477 IIV subjects contracted influenza, versus 21 of 116 who received LAIV (14% vs. 18%, respectively). In the 2011-2012 season, 51 of the 499 IIV subjects (10%) contracted influenza, compared with 12 of the 152 LAIV subjects (8%). In the 2012-2013 season, 198 of the 622 IIV subjects (32%) contracted influenza, versus 61 of the 205 LAIV subjects (30%). But, in the 2013-2014 season, 36 of the 468 IIV subjects (8%) contracted influenza, versus 34 of the 164 LAIV subjects (21%).
After adjustment for age and season, the odds ratio for the 2013-2014 season was significantly higher than those of the other seasons across the entire age spectrum of 2-17 years: 2.88, compared with 1.49 (2010-2011), 0.67 (2011-2012), and 0.92 (2012-2013).
When comparing influenza type/subtype, adjusted odds ratio was 5.53 for those with A/(H1N1)pdm09 in the 2010-2011 season, compared with 2.65 for those with the same in the 2013-2014 season. Those with A/H3N2 did not show as significant a difference across seasons (2010-2013), nor did those with influenza type B (2010-2011, 2012-2013).
“We found no statistically significant difference in LAIV effectiveness compared with IIV against medically attended, laboratory-confirmed influenza illness due to A/H3N2 or B viruses,” Ms. Chung and colleagues concluded. “We found significantly higher odds of influenza A/(H1N1)pdm09 among participants vaccinated with LAIV, compared with IIV, [but] reasons for lower effectiveness of LAIV against the A/(H1N1)pdm09 virus, compared with IIV are not fully understood.”
The investigators added that “the finding appears to be specific to the A/(H1N1)pdm09 vaccine component; we did not detect any statistically significant differences in effectiveness for the other components.” Three previous randomized controlled trials indicated that trivalent LAIV was just as effective, if not more so, than IIV, making the findings of this study surprising and “unexpected,” the authors noted.
This study was supported by the CDC through cooperative agreements with a variety of universities and foundations, and funded by the National Institutes of Health. Ms. Chung and associates reported no relevant financial disclosures.
*A previous version of this story misstated Jessie Chung’s academic title. Ms. Chung holds a Master’s in public health.
Influenza vaccination has been recommended for everyone for the past few years. Acceptance of this recommendation has been variable, and vaccine failures do not help the cause of convincing our patients to accept vaccination. In the paper by Chung et al. from the CDC and other coinvestigators who are prominent in influenza research, we learn that the live attenuated intranasally administered flu vaccine was significantly inferior to the killed injection administered flu vaccine for one of the type A flu strains. As a consequence, more kids vaccinated with the live attenuated vaccine got the flu. So parents who claim “the flu shot does not work” were partially correct more often since the 2009 flu season, if their child got the intranasal flu vaccine. However, neither the intranasal nor the injectable flu vaccine have an exceptionally high efficacy because the calculations by the authors for the study described and by citation of prior studies we are reminded that vaccine efficacy varies by strain and yearly by the season between 45% and 71%. We need to have better flu vaccines.

|
Dr. Michael E. Pichichero |
At Legacy Pediatrics, where I am in part-time private practice, we have seen increasing requests for the intranasal flu vaccine each year because parents and kids who can voice their wishes don’t want the shot. Our nurses like it, too, because the crying, wailing, and fighting to hold the kid down is avoided. There had been some reports before 2009 that the intranasal flu vaccine was more effective than the shot. But those of us who have been around long enough practicing medicine have learned about the pendulum of data and opinion sometimes swings back and forth. The article by Chung et al. reminds us once again of this reality.
Dr. Michael E. Pichichero is at the University of Rochester (N.Y.) Medical Center. He has received investigator-initiated grants from Sanofi Pasteur to study novel pneumococcal protein vaccines over the past 3 years and currently but has received no funding from Sanofi regarding injectable influenza vaccine. He also has conducted research with study coauthor Dr. John J. Treanor that was supported by MedImmune, who makes the intranasal flu vaccine.
Influenza vaccination has been recommended for everyone for the past few years. Acceptance of this recommendation has been variable, and vaccine failures do not help the cause of convincing our patients to accept vaccination. In the paper by Chung et al. from the CDC and other coinvestigators who are prominent in influenza research, we learn that the live attenuated intranasally administered flu vaccine was significantly inferior to the killed injection administered flu vaccine for one of the type A flu strains. As a consequence, more kids vaccinated with the live attenuated vaccine got the flu. So parents who claim “the flu shot does not work” were partially correct more often since the 2009 flu season, if their child got the intranasal flu vaccine. However, neither the intranasal nor the injectable flu vaccine have an exceptionally high efficacy because the calculations by the authors for the study described and by citation of prior studies we are reminded that vaccine efficacy varies by strain and yearly by the season between 45% and 71%. We need to have better flu vaccines.

|
Dr. Michael E. Pichichero |
At Legacy Pediatrics, where I am in part-time private practice, we have seen increasing requests for the intranasal flu vaccine each year because parents and kids who can voice their wishes don’t want the shot. Our nurses like it, too, because the crying, wailing, and fighting to hold the kid down is avoided. There had been some reports before 2009 that the intranasal flu vaccine was more effective than the shot. But those of us who have been around long enough practicing medicine have learned about the pendulum of data and opinion sometimes swings back and forth. The article by Chung et al. reminds us once again of this reality.
Dr. Michael E. Pichichero is at the University of Rochester (N.Y.) Medical Center. He has received investigator-initiated grants from Sanofi Pasteur to study novel pneumococcal protein vaccines over the past 3 years and currently but has received no funding from Sanofi regarding injectable influenza vaccine. He also has conducted research with study coauthor Dr. John J. Treanor that was supported by MedImmune, who makes the intranasal flu vaccine.
Influenza vaccination has been recommended for everyone for the past few years. Acceptance of this recommendation has been variable, and vaccine failures do not help the cause of convincing our patients to accept vaccination. In the paper by Chung et al. from the CDC and other coinvestigators who are prominent in influenza research, we learn that the live attenuated intranasally administered flu vaccine was significantly inferior to the killed injection administered flu vaccine for one of the type A flu strains. As a consequence, more kids vaccinated with the live attenuated vaccine got the flu. So parents who claim “the flu shot does not work” were partially correct more often since the 2009 flu season, if their child got the intranasal flu vaccine. However, neither the intranasal nor the injectable flu vaccine have an exceptionally high efficacy because the calculations by the authors for the study described and by citation of prior studies we are reminded that vaccine efficacy varies by strain and yearly by the season between 45% and 71%. We need to have better flu vaccines.

|
Dr. Michael E. Pichichero |
At Legacy Pediatrics, where I am in part-time private practice, we have seen increasing requests for the intranasal flu vaccine each year because parents and kids who can voice their wishes don’t want the shot. Our nurses like it, too, because the crying, wailing, and fighting to hold the kid down is avoided. There had been some reports before 2009 that the intranasal flu vaccine was more effective than the shot. But those of us who have been around long enough practicing medicine have learned about the pendulum of data and opinion sometimes swings back and forth. The article by Chung et al. reminds us once again of this reality.
Dr. Michael E. Pichichero is at the University of Rochester (N.Y.) Medical Center. He has received investigator-initiated grants from Sanofi Pasteur to study novel pneumococcal protein vaccines over the past 3 years and currently but has received no funding from Sanofi regarding injectable influenza vaccine. He also has conducted research with study coauthor Dr. John J. Treanor that was supported by MedImmune, who makes the intranasal flu vaccine.
When vaccinating children against influenza, inactivated and live attenuated influenza vaccines show little significant difference in effectiveness against nearly all strains of the virus, according to a new study in Pediatrics.
However, the study – which examined the effectiveness of IIV and LAIV across four consecutive influenza seasons between 2010 and 2014 – cautions that the 2013-2014 season’s A/(H1N1)pdm09 showed an uncharacteristically large gap in effectiveness favoring IIV, a discrepancy likely due to a problem with a vaccine component in LAIV. (Pediatrics. 2016;137(2):e20153279)
“We found that lower LAIV effectiveness in 2013-2014 was specific to the A/(H1N1)pdm09 vaccine component and was consistent with a previously unexamined effect during the 2010-2011 influenza season,” Jessie R. Chung of the influenza division at the Centers for Disease Control and Prevention and associates wrote, adding that the impetus for the study was the lack of available data “from observational studies after the 2009 pandemic on relative effectiveness of LAIV and IIV in children and adolescents.”
Ms. Chung* and coinvestigators enrolled children aged 2-17 years from clinics and hospitals in Michigan, New York, Pennsylvania, Tennessee, Texas, Washington, and Wisconsin during the 2010-2011, 2011-2012, 2012-2013, and 2013-2014 influenza seasons. Children brought in with symptoms of acute respiratory illness – cough, fever, or feverishness – had nasal and throat swabs collected to test for presence and type of influenza.
In total, 7,718 subjects were evaluated across the four influenza seasons, but after excluding subjects for various reasons – unknown vaccine type, indeterminate vaccine status, and inconclusive reverse transcription polymerase chain reaction results, among others – 6,819 subjects were included for vaccine effectiveness analysis, of which 2,703 were ultimately matched age appropriately and placed into IIV and LAIV cohorts for comparison. The IIV cohort consisted of 2,066 individuals (76.4%), while the LAIV cohort had 637 (23.6%).
During the 2010-2011 season, 66 of the 477 IIV subjects contracted influenza, versus 21 of 116 who received LAIV (14% vs. 18%, respectively). In the 2011-2012 season, 51 of the 499 IIV subjects (10%) contracted influenza, compared with 12 of the 152 LAIV subjects (8%). In the 2012-2013 season, 198 of the 622 IIV subjects (32%) contracted influenza, versus 61 of the 205 LAIV subjects (30%). But, in the 2013-2014 season, 36 of the 468 IIV subjects (8%) contracted influenza, versus 34 of the 164 LAIV subjects (21%).
After adjustment for age and season, the odds ratio for the 2013-2014 season was significantly higher than those of the other seasons across the entire age spectrum of 2-17 years: 2.88, compared with 1.49 (2010-2011), 0.67 (2011-2012), and 0.92 (2012-2013).
When comparing influenza type/subtype, adjusted odds ratio was 5.53 for those with A/(H1N1)pdm09 in the 2010-2011 season, compared with 2.65 for those with the same in the 2013-2014 season. Those with A/H3N2 did not show as significant a difference across seasons (2010-2013), nor did those with influenza type B (2010-2011, 2012-2013).
“We found no statistically significant difference in LAIV effectiveness compared with IIV against medically attended, laboratory-confirmed influenza illness due to A/H3N2 or B viruses,” Ms. Chung and colleagues concluded. “We found significantly higher odds of influenza A/(H1N1)pdm09 among participants vaccinated with LAIV, compared with IIV, [but] reasons for lower effectiveness of LAIV against the A/(H1N1)pdm09 virus, compared with IIV are not fully understood.”
The investigators added that “the finding appears to be specific to the A/(H1N1)pdm09 vaccine component; we did not detect any statistically significant differences in effectiveness for the other components.” Three previous randomized controlled trials indicated that trivalent LAIV was just as effective, if not more so, than IIV, making the findings of this study surprising and “unexpected,” the authors noted.
This study was supported by the CDC through cooperative agreements with a variety of universities and foundations, and funded by the National Institutes of Health. Ms. Chung and associates reported no relevant financial disclosures.
*A previous version of this story misstated Jessie Chung’s academic title. Ms. Chung holds a Master’s in public health.
When vaccinating children against influenza, inactivated and live attenuated influenza vaccines show little significant difference in effectiveness against nearly all strains of the virus, according to a new study in Pediatrics.
However, the study – which examined the effectiveness of IIV and LAIV across four consecutive influenza seasons between 2010 and 2014 – cautions that the 2013-2014 season’s A/(H1N1)pdm09 showed an uncharacteristically large gap in effectiveness favoring IIV, a discrepancy likely due to a problem with a vaccine component in LAIV. (Pediatrics. 2016;137(2):e20153279)
“We found that lower LAIV effectiveness in 2013-2014 was specific to the A/(H1N1)pdm09 vaccine component and was consistent with a previously unexamined effect during the 2010-2011 influenza season,” Jessie R. Chung of the influenza division at the Centers for Disease Control and Prevention and associates wrote, adding that the impetus for the study was the lack of available data “from observational studies after the 2009 pandemic on relative effectiveness of LAIV and IIV in children and adolescents.”
Ms. Chung* and coinvestigators enrolled children aged 2-17 years from clinics and hospitals in Michigan, New York, Pennsylvania, Tennessee, Texas, Washington, and Wisconsin during the 2010-2011, 2011-2012, 2012-2013, and 2013-2014 influenza seasons. Children brought in with symptoms of acute respiratory illness – cough, fever, or feverishness – had nasal and throat swabs collected to test for presence and type of influenza.
In total, 7,718 subjects were evaluated across the four influenza seasons, but after excluding subjects for various reasons – unknown vaccine type, indeterminate vaccine status, and inconclusive reverse transcription polymerase chain reaction results, among others – 6,819 subjects were included for vaccine effectiveness analysis, of which 2,703 were ultimately matched age appropriately and placed into IIV and LAIV cohorts for comparison. The IIV cohort consisted of 2,066 individuals (76.4%), while the LAIV cohort had 637 (23.6%).
During the 2010-2011 season, 66 of the 477 IIV subjects contracted influenza, versus 21 of 116 who received LAIV (14% vs. 18%, respectively). In the 2011-2012 season, 51 of the 499 IIV subjects (10%) contracted influenza, compared with 12 of the 152 LAIV subjects (8%). In the 2012-2013 season, 198 of the 622 IIV subjects (32%) contracted influenza, versus 61 of the 205 LAIV subjects (30%). But, in the 2013-2014 season, 36 of the 468 IIV subjects (8%) contracted influenza, versus 34 of the 164 LAIV subjects (21%).
After adjustment for age and season, the odds ratio for the 2013-2014 season was significantly higher than those of the other seasons across the entire age spectrum of 2-17 years: 2.88, compared with 1.49 (2010-2011), 0.67 (2011-2012), and 0.92 (2012-2013).
When comparing influenza type/subtype, adjusted odds ratio was 5.53 for those with A/(H1N1)pdm09 in the 2010-2011 season, compared with 2.65 for those with the same in the 2013-2014 season. Those with A/H3N2 did not show as significant a difference across seasons (2010-2013), nor did those with influenza type B (2010-2011, 2012-2013).
“We found no statistically significant difference in LAIV effectiveness compared with IIV against medically attended, laboratory-confirmed influenza illness due to A/H3N2 or B viruses,” Ms. Chung and colleagues concluded. “We found significantly higher odds of influenza A/(H1N1)pdm09 among participants vaccinated with LAIV, compared with IIV, [but] reasons for lower effectiveness of LAIV against the A/(H1N1)pdm09 virus, compared with IIV are not fully understood.”
The investigators added that “the finding appears to be specific to the A/(H1N1)pdm09 vaccine component; we did not detect any statistically significant differences in effectiveness for the other components.” Three previous randomized controlled trials indicated that trivalent LAIV was just as effective, if not more so, than IIV, making the findings of this study surprising and “unexpected,” the authors noted.
This study was supported by the CDC through cooperative agreements with a variety of universities and foundations, and funded by the National Institutes of Health. Ms. Chung and associates reported no relevant financial disclosures.
*A previous version of this story misstated Jessie Chung’s academic title. Ms. Chung holds a Master’s in public health.
FROM PEDIATRICS
Key clinical point: Inactivated influenza vaccine was significantly more effective against at least one strain of influenza than live attenuated influenza vaccine in 2013-2014.
Major finding: While no significant differences were seen in influenza rates between the IIV and LAIV cohorts for three consecutive seasons (2010-2013), the A/(H1N1)pdm09 strain of 2013-2014 affected subjects with LAIV at a significantly higher rate than did those with IIV.
Data source: Prospective cohort study of 2,703 children aged 2-17 years vaccinated between 2010 and 2014 with either IIV or LAIV.
Disclosures: This study was supported by the CDC through cooperative agreements with a variety of universities and foundations, and funded by the National Institutes of Health. Dr. Chung and his associates reported no relevant financial disclosures.