User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
HIV infection an independent risk factor for AECOPD
HIV infection is an independent risk factor for an acute exacerbation of chronic obstructive pulmonary disease (AECOPD), particularly in those with severe immune suppression, new research shows.
The longitudinal study, led by Dr. Kristina Crothers, a pulmonary and critical care specialist at Harborview Medical Center in Seattle, compared the incidence of AECOPD in 43,618 HIV-infected patients with 86,492 uninfected patients participating in the Veterans Aging Cohort Study (AIDS. 2016 Jan 28;30[3]:455-63).
Over 234,099 person-years of follow-up, the research team found that HIV-infected individuals had an increased rate of AECOPD compared with uninfected individuals (18.8 vs. 13.3 per 1,000 person-years, P less than .001).
Adjusted models showed that AECOPD risk was greater in HIV-infected individuals overall (IRR 1.54; 95% CI 1.44-1.65), particularly in those with more severe immune suppression when stratified by CD4+ cell count (cells/mcL) compared with uninfected individuals (HIV-infected CD4+ <200: IRR 2.30, 95% CI 2.10-2.53, HIV-infected CD4+ ≥ 200-349: IRR 1.32, 95% CI 1.15-1.51, HIV-infected CD4+ ≥350: IRR 0.99, 95% CI 0.88-1.10).
“These findings support that severity of immune suppression increases risk for AECOPD, likely through greater risk of infection,” Dr. Crothers and her coauthors wrote.
The researchers also found a significant interaction between HIV infection and current smoking and alcohol use, with both conferring a substantially greater risk for AECOPD. This suggests that the increased risk of AECOPD in HIV may be related to enhanced susceptibility to harms from the modifiable risk factors of smoking and unhealthy alcohol use.
Infection with HIV coupled with alcohol use could serve as a ‘double hit’ to increase susceptibility to exacerbations of lung disease, the authors suggested.
“Intervening on these contributing factors may decrease morbidity and costs associated with COPD, particularly in a vulnerable HIV-infected population,” they concluded.
The authors declared no conflicts of interest.
HIV infection is an independent risk factor for an acute exacerbation of chronic obstructive pulmonary disease (AECOPD), particularly in those with severe immune suppression, new research shows.
The longitudinal study, led by Dr. Kristina Crothers, a pulmonary and critical care specialist at Harborview Medical Center in Seattle, compared the incidence of AECOPD in 43,618 HIV-infected patients with 86,492 uninfected patients participating in the Veterans Aging Cohort Study (AIDS. 2016 Jan 28;30[3]:455-63).
Over 234,099 person-years of follow-up, the research team found that HIV-infected individuals had an increased rate of AECOPD compared with uninfected individuals (18.8 vs. 13.3 per 1,000 person-years, P less than .001).
Adjusted models showed that AECOPD risk was greater in HIV-infected individuals overall (IRR 1.54; 95% CI 1.44-1.65), particularly in those with more severe immune suppression when stratified by CD4+ cell count (cells/mcL) compared with uninfected individuals (HIV-infected CD4+ <200: IRR 2.30, 95% CI 2.10-2.53, HIV-infected CD4+ ≥ 200-349: IRR 1.32, 95% CI 1.15-1.51, HIV-infected CD4+ ≥350: IRR 0.99, 95% CI 0.88-1.10).
“These findings support that severity of immune suppression increases risk for AECOPD, likely through greater risk of infection,” Dr. Crothers and her coauthors wrote.
The researchers also found a significant interaction between HIV infection and current smoking and alcohol use, with both conferring a substantially greater risk for AECOPD. This suggests that the increased risk of AECOPD in HIV may be related to enhanced susceptibility to harms from the modifiable risk factors of smoking and unhealthy alcohol use.
Infection with HIV coupled with alcohol use could serve as a ‘double hit’ to increase susceptibility to exacerbations of lung disease, the authors suggested.
“Intervening on these contributing factors may decrease morbidity and costs associated with COPD, particularly in a vulnerable HIV-infected population,” they concluded.
The authors declared no conflicts of interest.
HIV infection is an independent risk factor for an acute exacerbation of chronic obstructive pulmonary disease (AECOPD), particularly in those with severe immune suppression, new research shows.
The longitudinal study, led by Dr. Kristina Crothers, a pulmonary and critical care specialist at Harborview Medical Center in Seattle, compared the incidence of AECOPD in 43,618 HIV-infected patients with 86,492 uninfected patients participating in the Veterans Aging Cohort Study (AIDS. 2016 Jan 28;30[3]:455-63).
Over 234,099 person-years of follow-up, the research team found that HIV-infected individuals had an increased rate of AECOPD compared with uninfected individuals (18.8 vs. 13.3 per 1,000 person-years, P less than .001).
Adjusted models showed that AECOPD risk was greater in HIV-infected individuals overall (IRR 1.54; 95% CI 1.44-1.65), particularly in those with more severe immune suppression when stratified by CD4+ cell count (cells/mcL) compared with uninfected individuals (HIV-infected CD4+ <200: IRR 2.30, 95% CI 2.10-2.53, HIV-infected CD4+ ≥ 200-349: IRR 1.32, 95% CI 1.15-1.51, HIV-infected CD4+ ≥350: IRR 0.99, 95% CI 0.88-1.10).
“These findings support that severity of immune suppression increases risk for AECOPD, likely through greater risk of infection,” Dr. Crothers and her coauthors wrote.
The researchers also found a significant interaction between HIV infection and current smoking and alcohol use, with both conferring a substantially greater risk for AECOPD. This suggests that the increased risk of AECOPD in HIV may be related to enhanced susceptibility to harms from the modifiable risk factors of smoking and unhealthy alcohol use.
Infection with HIV coupled with alcohol use could serve as a ‘double hit’ to increase susceptibility to exacerbations of lung disease, the authors suggested.
“Intervening on these contributing factors may decrease morbidity and costs associated with COPD, particularly in a vulnerable HIV-infected population,” they concluded.
The authors declared no conflicts of interest.
FROM AIDS
Key clinical point: HIV-infected individuals are at a higher risk of AECOPD if they have severe immune suppression, and/or smoke cigarettes and drink alcohol.
Major finding: HIV-infected individuals had an increased rate of AECOPD compared with uninfected individuals (18.8 vs. 13.3 per 1,000 person-years, P less than .001).
Data source: Longitudinal study involving 43,618 HIV-infected individuals and 86,492 uninfected individuals participating in the Veterans Aging Cohort Study.
Disclosures: No conflicts of interest are declared.
What Matters: Probiotics for colds
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
In the midst of the cold and flu season, we should reflect on the fact that our patients are laying down billions of dollars annually on preventions and cures for respiratory tract infections.
An aside: I am frequently turned down on my offer of the influenza vaccine, for which we probably have the best evidence. But $60 per month for a completely unproven preventive/curative agent made in some random factory in some random foreign land with no guarantee of good manufacturing practices (never mind the lack of active ingredients)? Stores can’t keep it in stock.
But I digress.
Our patients may lack the awareness of where to access evidence-based information when seeking answers about efficacy for cold remedies. So, it’s up to us to have at least some sense of where to get reliable information.
Truth be told, I am an enormous fan of safe and effective nonmedication therapies for the treatment and prevention of disease. So, when time permits, I will do a quick PubMed.gov search limiting my articles to randomized trials or systematic reviews on the latest and greatest home remedy.
Probiotics have been around for a while, and I think of them as a cure in search of a disease. The Cochrane Collaboration conducted a systematic review evaluating probiotics for the prevention of upper respiratory tract infection. In this review, 13 randomized, controlled trials were included (Explore [NY]. 2015 Sep-Oct;11[5]:418-20).
Probiotics were observed to be significantly better than placebo for reducing episodes of upper respiratory tract infection, the mean duration of episodes, antibiotic prescription rates, and cold-related absences. The evidence was of moderate to low quality.
Some may wonder how an ingested probiotic helps the respiratory tract stave off or fight infection. The prevailing theory appears to be that probiotics may function by mobilizing cells from the intestine to immunomodulate respiratory mucosa.
As for what probiotic/organism to prescribe? On this issue, there is a lot of smoke and not a lot of heat.
In general, the product should be encapsulated, and the label should include the genus and species of the strains (e.g., Lactobacillus acidophilus), the number of organisms (e.g., 5 billion), storage conditions (e.g., refrigerated or room temperature), and the shelf life. Pharmacy chain house brands may be cheaper. Gummy and chewable products tend to have 92% fewer beneficial bacteria than standard formulations.
How can we ensure purity?
That is tough, because supplements like probiotics are not regulated by the Food and Drug Administration above and beyond the agency’s trying to ensure good manufacturing practices. However, companies such as LabDoor (which generates revenue through affiliate links) test and grade supplements for label accuracy and purity. Websites like this might be the best place to start.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no financial disclosures relevant to this article.
High-dose vitamin D in pregnancy fails to prevent wheezing risk in children
Among pregnant women at high risk for having a child with asthma, high doses of vitamin D administered during the third trimester failed to prevent persistent wheezing illness in their children at age 3, according to two separate reports published online Jan. 26 in JAMA.
Both studies were conducted because vitamin D insufficiency during pregnancy is commonplace and is thought to affect fetal immune programming and to contribute to asthma pathogenesis. In addition, observational studies have found an association between low levels of vitamin D in cord blood and later asthma in the child.
The two randomized, double-blind placebo-controlled clinical trials found that neither 2,800 IU/day nor 4,400 IU/day of vitamin D significantly reduced the risk of persistent wheeze in the offspring through 3 years of age. However, both research groups noted that their studies may have been underpowered to detect a clinically important protective effect, and both recommended longer-term observation of their study participants, as well as further studies using larger sample sizes, higher doses of vitamin D, administration earlier in pregnancy, and postnatal supplementation to establish a definitive result.
In the first study – conducted as part of the Copenhagen Prospective Studies on Asthma in Childhood 2010 cohort – 623 Danish women already taking the standard 400 IU of vitamin D3 during pregnancy were randomly assigned to receive an additional 2,400 IU (315 women) or a matching placebo (308 women) from 22 to 26 weeks’ gestation until delivery. After exclusions, researchers analyzed data on 581 children.
Maternal serum vitamin D levels increased markedly in the active-treatment group. “Correspondingly, the percentage of women with sufficient levels of vitamin D (greater than 30 ng/mL) after the intervention was 81% in the vitamin D group, compared with 44% in the control group,” wrote Dr. Bo L. Chawes of Copenhagen Prospective Studies on Asthma in Childhood, University of Copenhagen, and his associates.
Persistent wheeze developed in 104 (18%) of the 581 children: 47 (16%) in the vitamin D group and 57 (20%) in the control group, a nonsignificant difference. Similarly, asthma was diagnosed in 79 children: 32 (12%) in the vitamin D group and 47 (14%) in the control group, another nonsignificant difference.
Vitamin D supplementation also made no difference in infants’ levels of C-reactive protein, interleukin-6, tumor necrosis factor–alpha, or CXCL8, nor in the number of upper respiratory tract infections (5.2 per year vs 5.3 per year), the number of lower respiratory tract infections (32% vs 33%), the risk of allergic sensitization as measured by skin prick test or specific IgE level, or the development of eczema (23% vs 25%).
However, the risk of persistent wheeze was higher in children whose mothers’ vitamin D levels were lowest, compared with those whose mothers’ vitamin D levels were in the middle and upper tertiles. And high-dose vitamin D was protective with regard to some secondary endpoints, such as preventing more episodes of “troublesome lung symptoms” (5.9 vs. 7.2).
This finding, together with the study’s somewhat reduced statistical power, mean that a clinically important protective effect cannot be ruled out. In addition, the supplementation dose may have been too low or may have been given too late in the course of pregnancy to produce a significant effect, Dr. Chawes and his associates wrote (JAMA. 2016;315[4]:353-61. doi: 10.1001/jama.2015.18318).In the second study – the Vitamin D Antenatal Asthma Reduction Trial – 876 pregnant women in Boston, St. Louis, and San Diego who were already taking the standard 400 IU of vitamin D were randomly assigned to receive either an additional 4,000 IU/day (440 participants) or a matching placebo (436 participants). Maternal levels of vitamin D rose markedly in the active-treatment group (mean, 39.2 ng/mL), compared with the control group (mean, 26.8 ng/mL), and the proportion of women who achieved higher than “inadequate” levels was much greater (74.9% vs 34.0%), reported Dr. Augusto A. Litonjua of Brigham and Women’s Hospital, Boston, and his associates.
A total of 24.3% of the vitamin D group and 30.4% of the control group developed asthma or recurrent wheeze by age 3 years, a nonsignificant difference. However, the incidence of asthma was so much lower than anticipated in both study groups that the study may have lost statistical power to detect a clinically meaningful difference, according to the investigators (JAMA. 2016;315[4]:362-70. doi: 10.1001/jama.2015.18589).
It remains unclear whether vitamin D supplementation during pregnancy will reduce asthma and persistent wheezing in the offspring. “Larger studies and longer follow-up of the children in this study will be needed to answer the question,” the investigators wrote. “If additional studies identify a significant effect, given the high prevalence of low vitamin D levels in pregnant women, the effect of this inexpensive intervention on child health could be substantial.”
The first study was supported by the Copenhagen Prospective Study on Asthma in Childhood, which is funded by private and public research groups. One of the coauthors reported receiving consulting fees from Chiesi. The Vitamin D Antenatal Asthma Reduction Trial was supported by the U.S. National Heart, Lung, and Blood Institute and the National Centers for Advancing Translational Sciences. The lead author, Dr. Litonjua, reported receiving personal fees from UpToDate and Springer Humana Press; his associates reported ties to numerous industry sources.
These are sobering findings. Even if we assume that prenatal vitamin D supplementation will prove more protective as the children in these studies grow older, vitamin D insufficiency still would explain only a small portion of the current asthma epidemic.
But neither study showed any unwanted effects from supplementation, so it seems reasonable for clinicians to prescribe vitamin D to mothers at high risk of having children with asthma by virtue of their own asthma, eczema, or allergic rhinitis – especially if those mothers are deficient in vitamin D. However, the data in these two clinical trials do not support the use of very high-dose vitamin D, since any beneficial effects achieved with 4,400 IU/day were identical to those achieved with approximately half as high a dose.
Dr. Erika von Mutius is at Ludwig Maximilians University, Munich. Dr. Fernando D. Martinez is at the asthma and airway disease research center and the department of pediatrics at the University of Arizona, Tucson. Both reported having no relevant financial disclosures. Their remarks are adapted from an editorial accompanying the two reports (JAMA 2016;315[4]:347-8.).
These are sobering findings. Even if we assume that prenatal vitamin D supplementation will prove more protective as the children in these studies grow older, vitamin D insufficiency still would explain only a small portion of the current asthma epidemic.
But neither study showed any unwanted effects from supplementation, so it seems reasonable for clinicians to prescribe vitamin D to mothers at high risk of having children with asthma by virtue of their own asthma, eczema, or allergic rhinitis – especially if those mothers are deficient in vitamin D. However, the data in these two clinical trials do not support the use of very high-dose vitamin D, since any beneficial effects achieved with 4,400 IU/day were identical to those achieved with approximately half as high a dose.
Dr. Erika von Mutius is at Ludwig Maximilians University, Munich. Dr. Fernando D. Martinez is at the asthma and airway disease research center and the department of pediatrics at the University of Arizona, Tucson. Both reported having no relevant financial disclosures. Their remarks are adapted from an editorial accompanying the two reports (JAMA 2016;315[4]:347-8.).
These are sobering findings. Even if we assume that prenatal vitamin D supplementation will prove more protective as the children in these studies grow older, vitamin D insufficiency still would explain only a small portion of the current asthma epidemic.
But neither study showed any unwanted effects from supplementation, so it seems reasonable for clinicians to prescribe vitamin D to mothers at high risk of having children with asthma by virtue of their own asthma, eczema, or allergic rhinitis – especially if those mothers are deficient in vitamin D. However, the data in these two clinical trials do not support the use of very high-dose vitamin D, since any beneficial effects achieved with 4,400 IU/day were identical to those achieved with approximately half as high a dose.
Dr. Erika von Mutius is at Ludwig Maximilians University, Munich. Dr. Fernando D. Martinez is at the asthma and airway disease research center and the department of pediatrics at the University of Arizona, Tucson. Both reported having no relevant financial disclosures. Their remarks are adapted from an editorial accompanying the two reports (JAMA 2016;315[4]:347-8.).
Among pregnant women at high risk for having a child with asthma, high doses of vitamin D administered during the third trimester failed to prevent persistent wheezing illness in their children at age 3, according to two separate reports published online Jan. 26 in JAMA.
Both studies were conducted because vitamin D insufficiency during pregnancy is commonplace and is thought to affect fetal immune programming and to contribute to asthma pathogenesis. In addition, observational studies have found an association between low levels of vitamin D in cord blood and later asthma in the child.
The two randomized, double-blind placebo-controlled clinical trials found that neither 2,800 IU/day nor 4,400 IU/day of vitamin D significantly reduced the risk of persistent wheeze in the offspring through 3 years of age. However, both research groups noted that their studies may have been underpowered to detect a clinically important protective effect, and both recommended longer-term observation of their study participants, as well as further studies using larger sample sizes, higher doses of vitamin D, administration earlier in pregnancy, and postnatal supplementation to establish a definitive result.
In the first study – conducted as part of the Copenhagen Prospective Studies on Asthma in Childhood 2010 cohort – 623 Danish women already taking the standard 400 IU of vitamin D3 during pregnancy were randomly assigned to receive an additional 2,400 IU (315 women) or a matching placebo (308 women) from 22 to 26 weeks’ gestation until delivery. After exclusions, researchers analyzed data on 581 children.
Maternal serum vitamin D levels increased markedly in the active-treatment group. “Correspondingly, the percentage of women with sufficient levels of vitamin D (greater than 30 ng/mL) after the intervention was 81% in the vitamin D group, compared with 44% in the control group,” wrote Dr. Bo L. Chawes of Copenhagen Prospective Studies on Asthma in Childhood, University of Copenhagen, and his associates.
Persistent wheeze developed in 104 (18%) of the 581 children: 47 (16%) in the vitamin D group and 57 (20%) in the control group, a nonsignificant difference. Similarly, asthma was diagnosed in 79 children: 32 (12%) in the vitamin D group and 47 (14%) in the control group, another nonsignificant difference.
Vitamin D supplementation also made no difference in infants’ levels of C-reactive protein, interleukin-6, tumor necrosis factor–alpha, or CXCL8, nor in the number of upper respiratory tract infections (5.2 per year vs 5.3 per year), the number of lower respiratory tract infections (32% vs 33%), the risk of allergic sensitization as measured by skin prick test or specific IgE level, or the development of eczema (23% vs 25%).
However, the risk of persistent wheeze was higher in children whose mothers’ vitamin D levels were lowest, compared with those whose mothers’ vitamin D levels were in the middle and upper tertiles. And high-dose vitamin D was protective with regard to some secondary endpoints, such as preventing more episodes of “troublesome lung symptoms” (5.9 vs. 7.2).
This finding, together with the study’s somewhat reduced statistical power, mean that a clinically important protective effect cannot be ruled out. In addition, the supplementation dose may have been too low or may have been given too late in the course of pregnancy to produce a significant effect, Dr. Chawes and his associates wrote (JAMA. 2016;315[4]:353-61. doi: 10.1001/jama.2015.18318).In the second study – the Vitamin D Antenatal Asthma Reduction Trial – 876 pregnant women in Boston, St. Louis, and San Diego who were already taking the standard 400 IU of vitamin D were randomly assigned to receive either an additional 4,000 IU/day (440 participants) or a matching placebo (436 participants). Maternal levels of vitamin D rose markedly in the active-treatment group (mean, 39.2 ng/mL), compared with the control group (mean, 26.8 ng/mL), and the proportion of women who achieved higher than “inadequate” levels was much greater (74.9% vs 34.0%), reported Dr. Augusto A. Litonjua of Brigham and Women’s Hospital, Boston, and his associates.
A total of 24.3% of the vitamin D group and 30.4% of the control group developed asthma or recurrent wheeze by age 3 years, a nonsignificant difference. However, the incidence of asthma was so much lower than anticipated in both study groups that the study may have lost statistical power to detect a clinically meaningful difference, according to the investigators (JAMA. 2016;315[4]:362-70. doi: 10.1001/jama.2015.18589).
It remains unclear whether vitamin D supplementation during pregnancy will reduce asthma and persistent wheezing in the offspring. “Larger studies and longer follow-up of the children in this study will be needed to answer the question,” the investigators wrote. “If additional studies identify a significant effect, given the high prevalence of low vitamin D levels in pregnant women, the effect of this inexpensive intervention on child health could be substantial.”
The first study was supported by the Copenhagen Prospective Study on Asthma in Childhood, which is funded by private and public research groups. One of the coauthors reported receiving consulting fees from Chiesi. The Vitamin D Antenatal Asthma Reduction Trial was supported by the U.S. National Heart, Lung, and Blood Institute and the National Centers for Advancing Translational Sciences. The lead author, Dr. Litonjua, reported receiving personal fees from UpToDate and Springer Humana Press; his associates reported ties to numerous industry sources.
Among pregnant women at high risk for having a child with asthma, high doses of vitamin D administered during the third trimester failed to prevent persistent wheezing illness in their children at age 3, according to two separate reports published online Jan. 26 in JAMA.
Both studies were conducted because vitamin D insufficiency during pregnancy is commonplace and is thought to affect fetal immune programming and to contribute to asthma pathogenesis. In addition, observational studies have found an association between low levels of vitamin D in cord blood and later asthma in the child.
The two randomized, double-blind placebo-controlled clinical trials found that neither 2,800 IU/day nor 4,400 IU/day of vitamin D significantly reduced the risk of persistent wheeze in the offspring through 3 years of age. However, both research groups noted that their studies may have been underpowered to detect a clinically important protective effect, and both recommended longer-term observation of their study participants, as well as further studies using larger sample sizes, higher doses of vitamin D, administration earlier in pregnancy, and postnatal supplementation to establish a definitive result.
In the first study – conducted as part of the Copenhagen Prospective Studies on Asthma in Childhood 2010 cohort – 623 Danish women already taking the standard 400 IU of vitamin D3 during pregnancy were randomly assigned to receive an additional 2,400 IU (315 women) or a matching placebo (308 women) from 22 to 26 weeks’ gestation until delivery. After exclusions, researchers analyzed data on 581 children.
Maternal serum vitamin D levels increased markedly in the active-treatment group. “Correspondingly, the percentage of women with sufficient levels of vitamin D (greater than 30 ng/mL) after the intervention was 81% in the vitamin D group, compared with 44% in the control group,” wrote Dr. Bo L. Chawes of Copenhagen Prospective Studies on Asthma in Childhood, University of Copenhagen, and his associates.
Persistent wheeze developed in 104 (18%) of the 581 children: 47 (16%) in the vitamin D group and 57 (20%) in the control group, a nonsignificant difference. Similarly, asthma was diagnosed in 79 children: 32 (12%) in the vitamin D group and 47 (14%) in the control group, another nonsignificant difference.
Vitamin D supplementation also made no difference in infants’ levels of C-reactive protein, interleukin-6, tumor necrosis factor–alpha, or CXCL8, nor in the number of upper respiratory tract infections (5.2 per year vs 5.3 per year), the number of lower respiratory tract infections (32% vs 33%), the risk of allergic sensitization as measured by skin prick test or specific IgE level, or the development of eczema (23% vs 25%).
However, the risk of persistent wheeze was higher in children whose mothers’ vitamin D levels were lowest, compared with those whose mothers’ vitamin D levels were in the middle and upper tertiles. And high-dose vitamin D was protective with regard to some secondary endpoints, such as preventing more episodes of “troublesome lung symptoms” (5.9 vs. 7.2).
This finding, together with the study’s somewhat reduced statistical power, mean that a clinically important protective effect cannot be ruled out. In addition, the supplementation dose may have been too low or may have been given too late in the course of pregnancy to produce a significant effect, Dr. Chawes and his associates wrote (JAMA. 2016;315[4]:353-61. doi: 10.1001/jama.2015.18318).In the second study – the Vitamin D Antenatal Asthma Reduction Trial – 876 pregnant women in Boston, St. Louis, and San Diego who were already taking the standard 400 IU of vitamin D were randomly assigned to receive either an additional 4,000 IU/day (440 participants) or a matching placebo (436 participants). Maternal levels of vitamin D rose markedly in the active-treatment group (mean, 39.2 ng/mL), compared with the control group (mean, 26.8 ng/mL), and the proportion of women who achieved higher than “inadequate” levels was much greater (74.9% vs 34.0%), reported Dr. Augusto A. Litonjua of Brigham and Women’s Hospital, Boston, and his associates.
A total of 24.3% of the vitamin D group and 30.4% of the control group developed asthma or recurrent wheeze by age 3 years, a nonsignificant difference. However, the incidence of asthma was so much lower than anticipated in both study groups that the study may have lost statistical power to detect a clinically meaningful difference, according to the investigators (JAMA. 2016;315[4]:362-70. doi: 10.1001/jama.2015.18589).
It remains unclear whether vitamin D supplementation during pregnancy will reduce asthma and persistent wheezing in the offspring. “Larger studies and longer follow-up of the children in this study will be needed to answer the question,” the investigators wrote. “If additional studies identify a significant effect, given the high prevalence of low vitamin D levels in pregnant women, the effect of this inexpensive intervention on child health could be substantial.”
The first study was supported by the Copenhagen Prospective Study on Asthma in Childhood, which is funded by private and public research groups. One of the coauthors reported receiving consulting fees from Chiesi. The Vitamin D Antenatal Asthma Reduction Trial was supported by the U.S. National Heart, Lung, and Blood Institute and the National Centers for Advancing Translational Sciences. The lead author, Dr. Litonjua, reported receiving personal fees from UpToDate and Springer Humana Press; his associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: High doses of vitamin D administered during the third trimester didn’t prevent wheezing in children at age 3.
Major finding: In a study of 581 children, persistent wheeze developed in 16% in the vitamin D group and in 20% in the control group. In a separate trial of 806 infants, there was a 6.1% reduction in asthma or recurrent wheezing at age 3, which was not statistically significant.
Data source: Two separate randomized, double-blind placebo-controlled trials involving a total of nearly 1,500 pregnant women.
Disclosures: The first study was supported by the Copenhagen Prospective Study on Asthma in Childhood, which is funded by private and public research groups. One of the coauthors reported receiving consulting fees from Chiesi. The Vitamin D Antenatal Asthma Reduction Trial was supported by the U.S. National Heart, Lung, and Blood Institute and the National Centers for Advancing Translational Sciences. The lead author, Dr. Litonjua, reported receiving personal fees from UpToDate and Springer Humana Press; his associates reported ties to numerous industry sources.
Poor adherence to quality indicators found for NSCLC surgery
PHOENIX – National adherence to quality indicators for surgery in stage I non–small cell lung cancer is suboptimal, results from a large analysis of national data suggest.
“Compliance with such guidelines is a strong predictor of long-term survival, and vigorous efforts should be instituted at the level of national societies to improve such adherence,” researchers led by Dr. Pamela P. Samson wrote in an abstract presented at the annual meeting of the Society of Thoracic Surgeons. “National organizations, including American College of Chest Physicians, the National Comprehensive Cancer Network, and the American College of Surgeons Commission on Cancer, have recommended quality standards for surgery in early-stage non–small cell lung cancer (NSCLC). The determinants and outcomes of adherence to these guidelines for early-stage lung cancer patients are largely unknown.”
Dr. Samson, a general surgery resident at Washington University in St. Louis, and her associates used the National Cancer Data Base to evaluate data from 146,908 patients undergoing surgery for clinical stage I NSCLC between 2004 and 2013. They selected the following four quality measures for evaluation: performing an anatomical pulmonary resection, surgery within 8 weeks of diagnosis, R0 resection, and evaluation of 10 or more lymph nodes. Next, the researchers fitted multivariate models to identify variables independently associated with adherence to quality measures, and created a Cox multivariate model to evaluate long-term overall survival.
Dr. Varun Puri, senior author of the study, presented the findings at the STS meeting on behalf of Dr. Samson, and discussed the findings in a video interview. The researchers found that between 2004 and 2013, nearly 100% of patients met at least one of the four recommended criteria, 95% met two, 69% met three, and 22% met all four. Sampling of 10 or more lymph nodes was the least frequently met measure, occurring in only 31% of surgical patients. Patient factors associated with a greater likelihood of receiving all four quality measures included average income in ZIP code of at least $38,000 (odds ratio, 1.20), private insurance (OR, 1.22), or having Medicare (OR, 1.16). Institutional factors associated with a greater likelihood of meeting all four quality measures included higher-volume centers, defined as treating at least 38 cases per year (OR, 1.18), or being an academic institution (OR, 1.31).
At the same time, factors associated with a lower likelihood of recommended surgical care included increasing age (per year increase, OR, 0.99) and a higher Charlson/Deyo comorbidity score (OR, 0.90 for a score of 1 and OR, 0.82 for a score of 2 or more). The strongest determinant of long-term overall survival included pathologic upstaging (HR 1.84) and meeting all four quality indicators (HR 0.39). Every additional quality met was associated with a significant reduction in overall mortality.
“We believe this study can be a starting point to draw attention to institution- and surgeon-specific practice patterns that may vary widely,” Dr. Samson said in an interview prior to the meeting. “At our own institution, we are working to decrease time to surgery, as well as implementing quality improvement measures to increase nodal sampling rates. Improving these trends nationally must start at the local level, with a tailored approach.”
Dr. Samson is currently supported by a T32 NIH training grant for research fellows in cardiothoracic surgery. Study coauthor Dr. Bryan Meyers, has received honoraria from Varian Medical Systems and is a consultant/advisory board member of Ethicon. Senior author Dr. Varun Puri is supported by NIH career awards.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – National adherence to quality indicators for surgery in stage I non–small cell lung cancer is suboptimal, results from a large analysis of national data suggest.
“Compliance with such guidelines is a strong predictor of long-term survival, and vigorous efforts should be instituted at the level of national societies to improve such adherence,” researchers led by Dr. Pamela P. Samson wrote in an abstract presented at the annual meeting of the Society of Thoracic Surgeons. “National organizations, including American College of Chest Physicians, the National Comprehensive Cancer Network, and the American College of Surgeons Commission on Cancer, have recommended quality standards for surgery in early-stage non–small cell lung cancer (NSCLC). The determinants and outcomes of adherence to these guidelines for early-stage lung cancer patients are largely unknown.”
Dr. Samson, a general surgery resident at Washington University in St. Louis, and her associates used the National Cancer Data Base to evaluate data from 146,908 patients undergoing surgery for clinical stage I NSCLC between 2004 and 2013. They selected the following four quality measures for evaluation: performing an anatomical pulmonary resection, surgery within 8 weeks of diagnosis, R0 resection, and evaluation of 10 or more lymph nodes. Next, the researchers fitted multivariate models to identify variables independently associated with adherence to quality measures, and created a Cox multivariate model to evaluate long-term overall survival.
Dr. Varun Puri, senior author of the study, presented the findings at the STS meeting on behalf of Dr. Samson, and discussed the findings in a video interview. The researchers found that between 2004 and 2013, nearly 100% of patients met at least one of the four recommended criteria, 95% met two, 69% met three, and 22% met all four. Sampling of 10 or more lymph nodes was the least frequently met measure, occurring in only 31% of surgical patients. Patient factors associated with a greater likelihood of receiving all four quality measures included average income in ZIP code of at least $38,000 (odds ratio, 1.20), private insurance (OR, 1.22), or having Medicare (OR, 1.16). Institutional factors associated with a greater likelihood of meeting all four quality measures included higher-volume centers, defined as treating at least 38 cases per year (OR, 1.18), or being an academic institution (OR, 1.31).
At the same time, factors associated with a lower likelihood of recommended surgical care included increasing age (per year increase, OR, 0.99) and a higher Charlson/Deyo comorbidity score (OR, 0.90 for a score of 1 and OR, 0.82 for a score of 2 or more). The strongest determinant of long-term overall survival included pathologic upstaging (HR 1.84) and meeting all four quality indicators (HR 0.39). Every additional quality met was associated with a significant reduction in overall mortality.
“We believe this study can be a starting point to draw attention to institution- and surgeon-specific practice patterns that may vary widely,” Dr. Samson said in an interview prior to the meeting. “At our own institution, we are working to decrease time to surgery, as well as implementing quality improvement measures to increase nodal sampling rates. Improving these trends nationally must start at the local level, with a tailored approach.”
Dr. Samson is currently supported by a T32 NIH training grant for research fellows in cardiothoracic surgery. Study coauthor Dr. Bryan Meyers, has received honoraria from Varian Medical Systems and is a consultant/advisory board member of Ethicon. Senior author Dr. Varun Puri is supported by NIH career awards.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – National adherence to quality indicators for surgery in stage I non–small cell lung cancer is suboptimal, results from a large analysis of national data suggest.
“Compliance with such guidelines is a strong predictor of long-term survival, and vigorous efforts should be instituted at the level of national societies to improve such adherence,” researchers led by Dr. Pamela P. Samson wrote in an abstract presented at the annual meeting of the Society of Thoracic Surgeons. “National organizations, including American College of Chest Physicians, the National Comprehensive Cancer Network, and the American College of Surgeons Commission on Cancer, have recommended quality standards for surgery in early-stage non–small cell lung cancer (NSCLC). The determinants and outcomes of adherence to these guidelines for early-stage lung cancer patients are largely unknown.”
Dr. Samson, a general surgery resident at Washington University in St. Louis, and her associates used the National Cancer Data Base to evaluate data from 146,908 patients undergoing surgery for clinical stage I NSCLC between 2004 and 2013. They selected the following four quality measures for evaluation: performing an anatomical pulmonary resection, surgery within 8 weeks of diagnosis, R0 resection, and evaluation of 10 or more lymph nodes. Next, the researchers fitted multivariate models to identify variables independently associated with adherence to quality measures, and created a Cox multivariate model to evaluate long-term overall survival.
Dr. Varun Puri, senior author of the study, presented the findings at the STS meeting on behalf of Dr. Samson, and discussed the findings in a video interview. The researchers found that between 2004 and 2013, nearly 100% of patients met at least one of the four recommended criteria, 95% met two, 69% met three, and 22% met all four. Sampling of 10 or more lymph nodes was the least frequently met measure, occurring in only 31% of surgical patients. Patient factors associated with a greater likelihood of receiving all four quality measures included average income in ZIP code of at least $38,000 (odds ratio, 1.20), private insurance (OR, 1.22), or having Medicare (OR, 1.16). Institutional factors associated with a greater likelihood of meeting all four quality measures included higher-volume centers, defined as treating at least 38 cases per year (OR, 1.18), or being an academic institution (OR, 1.31).
At the same time, factors associated with a lower likelihood of recommended surgical care included increasing age (per year increase, OR, 0.99) and a higher Charlson/Deyo comorbidity score (OR, 0.90 for a score of 1 and OR, 0.82 for a score of 2 or more). The strongest determinant of long-term overall survival included pathologic upstaging (HR 1.84) and meeting all four quality indicators (HR 0.39). Every additional quality met was associated with a significant reduction in overall mortality.
“We believe this study can be a starting point to draw attention to institution- and surgeon-specific practice patterns that may vary widely,” Dr. Samson said in an interview prior to the meeting. “At our own institution, we are working to decrease time to surgery, as well as implementing quality improvement measures to increase nodal sampling rates. Improving these trends nationally must start at the local level, with a tailored approach.”
Dr. Samson is currently supported by a T32 NIH training grant for research fellows in cardiothoracic surgery. Study coauthor Dr. Bryan Meyers, has received honoraria from Varian Medical Systems and is a consultant/advisory board member of Ethicon. Senior author Dr. Varun Puri is supported by NIH career awards.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE STS ANNUAL MEETING
Key clinical point: At the national level, compliance with core indicators for surgery in stage I NSCLC is poor.
Major finding: Between 2004 and 2013, nearly 100% of patients met at least one of four recommended criteria for evaluation of stage I NSCLC, 95% met two, 69% met three, and 22% met all four.
Data source: An analysis of 146,908 patients undergoing surgery for clinical stage I NSCLC between 2004 and 2013.
Disclosures: Dr. Samson is currently supported by a T32 NIH training grant for research fellows in cardiothoracic surgery. Study coauthor Dr. Bryan Meyers, has received honoraria from Varian Medical Systems and is a consultant/advisory board member of Ethicon. Senior author Dr. Varun Puri is supported by NIH career awards.
Ivacaftor appears safe for young children with cystic fibrosis
Ivacaftor, a cystic fibrosis transmembrane conductance regulator potentiator, appears generally safe for young children with cystic fibrosis and a CFTR gating mutation, an open-label, single-arm study shows.
The study, published online Jan. 20, is the first to assess ivacaftor in children aged 2-5 years, suggests that the drug is well tolerated, somewhat improves sweat chloride and nutritional measures, and also might improve pancreatic function, reported Dr. Jane C. Davies of the National Heart & Lung Institute of Imperial College London, and her associates. “Reported side effects are similar to those in the general cystic fibrosis population, although children with previous cystic fibrosis liver disease might have transient rises in transaminase concentrations,” they added.
Ivacaftor is approved by the Food and Drug Administration for children aged 6 years and older with cystic fibrosis, and it should be even more beneficial if given before patients develop infections and inflammation as a result of cystic fibrosis transmembrane conductance regulator (CFTR) dysfunction, the researchers noted.
The investigators enrolled children aged 2 to 5 years with cystic fibrosis and a CFTR gating mutation on at least one allele from 15 hospitals in the United States, the United Kingdom, and Canada. To establish short-term safety and pharmacokinetics of ivacaftor and its metabolites, nine patients received an oral dose of 50 mg (if they weighed less than 14 kg) or 75 mg (if they weighed 14 kg or more) every 12 hours for 4 days.
To assess longer-term safety, 34 patients received these doses for 24 weeks, followed by an open-label extension study that remains underway (Lancet Respir Med. 2016 Jan 20. doi: 10.1016/S2213-2600[15]00545-7).
The pharmacokinetic analyses indicated that exposure was similar to that reported in adults, the researchers reported. The median Cmin was 536 ng per mL for the 50-mg dose and 580 ng per mL for the 75-mg dose, and median ivacaftor AUC values were 9,840 ng×h/mL and 10,200 ngxh/mL, respectively. The most common adverse events over 6 weeks of treatment included cough (56% of patients) and vomiting (29%). In addition five (15%) patients had liver function test results that were more than eight-fold higher than the upper limit of normal. As a result, four had the study drug interrupted and one discontinued. Hypertransaminasemia was the only serious adverse event considered related to ivacaftor, and the only adverse event leading to treatment discontinuation. By week 24, sweat chloride levels had dropped an average of 47 mmol per L from baseline (standard deviation, 26.2, P less than .0001), weight had dropped by a z score factor of 0.2 (P less than .0001), and BMI had fallen by a factor of 0.4 (P less than .0001).
“Unfortunately, this study could not generate meaningful data on pulmonary function, because only three patients produced research-quality measurements, and we did not provide specific training or quality control in preschool lung function testing,” the investigators said. The results “confirmed a safe and tolerable dose of an acceptable formulation of ivacaftor in children aged 2 to 5 years with a CFTR gating mutation, although liver function seems to require closer monitoring in this age range than in adults, particularly among those with a history of elevated [liver function tests].”
Vertex Pharmaceuticals funded the study. Dr. Davies reported serving on advisory boards for Proteostasis, Pharmaxis, Pulmocide, Novartis, and Vertex Pharmaceuticals, and participating in educational activities for which her institution received payment. Seven coinvestigators also reported financial relationships with Vertex, including three who reported employment with the company.
The study results are “groundbreaking” for cystic fibrosis care in young children, Dr. Sophie Yammine, Dr. Philipp Latzin, and Dr. Florian Singer wrote in an accompanying editorial. “Targeted treatment of this basic defect has potential for both prevention of damage and functional improvement of affected organs,” they wrote.
However, they said that many unknowns remain, “such as the earliest age of possible application, data for natural fluctuation of new outcome variables, and other points that have been reviewed previously. “In any case, the results published by Davies and colleagues are good news for young children with cystic fibrosis and their families, who often have an insufficient amount of advocacy,” they wrote.
Dr. Yammine and Dr. Latzin are affiliated with University Children’s Hospital Bern in Switzerland. Dr. Latzin is also at University Children’s Hospital Basel in Switzerland, and Dr. Singer is with University Children’s Hospital Zurich in Switzerland.
The study results are “groundbreaking” for cystic fibrosis care in young children, Dr. Sophie Yammine, Dr. Philipp Latzin, and Dr. Florian Singer wrote in an accompanying editorial. “Targeted treatment of this basic defect has potential for both prevention of damage and functional improvement of affected organs,” they wrote.
However, they said that many unknowns remain, “such as the earliest age of possible application, data for natural fluctuation of new outcome variables, and other points that have been reviewed previously. “In any case, the results published by Davies and colleagues are good news for young children with cystic fibrosis and their families, who often have an insufficient amount of advocacy,” they wrote.
Dr. Yammine and Dr. Latzin are affiliated with University Children’s Hospital Bern in Switzerland. Dr. Latzin is also at University Children’s Hospital Basel in Switzerland, and Dr. Singer is with University Children’s Hospital Zurich in Switzerland.
The study results are “groundbreaking” for cystic fibrosis care in young children, Dr. Sophie Yammine, Dr. Philipp Latzin, and Dr. Florian Singer wrote in an accompanying editorial. “Targeted treatment of this basic defect has potential for both prevention of damage and functional improvement of affected organs,” they wrote.
However, they said that many unknowns remain, “such as the earliest age of possible application, data for natural fluctuation of new outcome variables, and other points that have been reviewed previously. “In any case, the results published by Davies and colleagues are good news for young children with cystic fibrosis and their families, who often have an insufficient amount of advocacy,” they wrote.
Dr. Yammine and Dr. Latzin are affiliated with University Children’s Hospital Bern in Switzerland. Dr. Latzin is also at University Children’s Hospital Basel in Switzerland, and Dr. Singer is with University Children’s Hospital Zurich in Switzerland.
Ivacaftor, a cystic fibrosis transmembrane conductance regulator potentiator, appears generally safe for young children with cystic fibrosis and a CFTR gating mutation, an open-label, single-arm study shows.
The study, published online Jan. 20, is the first to assess ivacaftor in children aged 2-5 years, suggests that the drug is well tolerated, somewhat improves sweat chloride and nutritional measures, and also might improve pancreatic function, reported Dr. Jane C. Davies of the National Heart & Lung Institute of Imperial College London, and her associates. “Reported side effects are similar to those in the general cystic fibrosis population, although children with previous cystic fibrosis liver disease might have transient rises in transaminase concentrations,” they added.
Ivacaftor is approved by the Food and Drug Administration for children aged 6 years and older with cystic fibrosis, and it should be even more beneficial if given before patients develop infections and inflammation as a result of cystic fibrosis transmembrane conductance regulator (CFTR) dysfunction, the researchers noted.
The investigators enrolled children aged 2 to 5 years with cystic fibrosis and a CFTR gating mutation on at least one allele from 15 hospitals in the United States, the United Kingdom, and Canada. To establish short-term safety and pharmacokinetics of ivacaftor and its metabolites, nine patients received an oral dose of 50 mg (if they weighed less than 14 kg) or 75 mg (if they weighed 14 kg or more) every 12 hours for 4 days.
To assess longer-term safety, 34 patients received these doses for 24 weeks, followed by an open-label extension study that remains underway (Lancet Respir Med. 2016 Jan 20. doi: 10.1016/S2213-2600[15]00545-7).
The pharmacokinetic analyses indicated that exposure was similar to that reported in adults, the researchers reported. The median Cmin was 536 ng per mL for the 50-mg dose and 580 ng per mL for the 75-mg dose, and median ivacaftor AUC values were 9,840 ng×h/mL and 10,200 ngxh/mL, respectively. The most common adverse events over 6 weeks of treatment included cough (56% of patients) and vomiting (29%). In addition five (15%) patients had liver function test results that were more than eight-fold higher than the upper limit of normal. As a result, four had the study drug interrupted and one discontinued. Hypertransaminasemia was the only serious adverse event considered related to ivacaftor, and the only adverse event leading to treatment discontinuation. By week 24, sweat chloride levels had dropped an average of 47 mmol per L from baseline (standard deviation, 26.2, P less than .0001), weight had dropped by a z score factor of 0.2 (P less than .0001), and BMI had fallen by a factor of 0.4 (P less than .0001).
“Unfortunately, this study could not generate meaningful data on pulmonary function, because only three patients produced research-quality measurements, and we did not provide specific training or quality control in preschool lung function testing,” the investigators said. The results “confirmed a safe and tolerable dose of an acceptable formulation of ivacaftor in children aged 2 to 5 years with a CFTR gating mutation, although liver function seems to require closer monitoring in this age range than in adults, particularly among those with a history of elevated [liver function tests].”
Vertex Pharmaceuticals funded the study. Dr. Davies reported serving on advisory boards for Proteostasis, Pharmaxis, Pulmocide, Novartis, and Vertex Pharmaceuticals, and participating in educational activities for which her institution received payment. Seven coinvestigators also reported financial relationships with Vertex, including three who reported employment with the company.
Ivacaftor, a cystic fibrosis transmembrane conductance regulator potentiator, appears generally safe for young children with cystic fibrosis and a CFTR gating mutation, an open-label, single-arm study shows.
The study, published online Jan. 20, is the first to assess ivacaftor in children aged 2-5 years, suggests that the drug is well tolerated, somewhat improves sweat chloride and nutritional measures, and also might improve pancreatic function, reported Dr. Jane C. Davies of the National Heart & Lung Institute of Imperial College London, and her associates. “Reported side effects are similar to those in the general cystic fibrosis population, although children with previous cystic fibrosis liver disease might have transient rises in transaminase concentrations,” they added.
Ivacaftor is approved by the Food and Drug Administration for children aged 6 years and older with cystic fibrosis, and it should be even more beneficial if given before patients develop infections and inflammation as a result of cystic fibrosis transmembrane conductance regulator (CFTR) dysfunction, the researchers noted.
The investigators enrolled children aged 2 to 5 years with cystic fibrosis and a CFTR gating mutation on at least one allele from 15 hospitals in the United States, the United Kingdom, and Canada. To establish short-term safety and pharmacokinetics of ivacaftor and its metabolites, nine patients received an oral dose of 50 mg (if they weighed less than 14 kg) or 75 mg (if they weighed 14 kg or more) every 12 hours for 4 days.
To assess longer-term safety, 34 patients received these doses for 24 weeks, followed by an open-label extension study that remains underway (Lancet Respir Med. 2016 Jan 20. doi: 10.1016/S2213-2600[15]00545-7).
The pharmacokinetic analyses indicated that exposure was similar to that reported in adults, the researchers reported. The median Cmin was 536 ng per mL for the 50-mg dose and 580 ng per mL for the 75-mg dose, and median ivacaftor AUC values were 9,840 ng×h/mL and 10,200 ngxh/mL, respectively. The most common adverse events over 6 weeks of treatment included cough (56% of patients) and vomiting (29%). In addition five (15%) patients had liver function test results that were more than eight-fold higher than the upper limit of normal. As a result, four had the study drug interrupted and one discontinued. Hypertransaminasemia was the only serious adverse event considered related to ivacaftor, and the only adverse event leading to treatment discontinuation. By week 24, sweat chloride levels had dropped an average of 47 mmol per L from baseline (standard deviation, 26.2, P less than .0001), weight had dropped by a z score factor of 0.2 (P less than .0001), and BMI had fallen by a factor of 0.4 (P less than .0001).
“Unfortunately, this study could not generate meaningful data on pulmonary function, because only three patients produced research-quality measurements, and we did not provide specific training or quality control in preschool lung function testing,” the investigators said. The results “confirmed a safe and tolerable dose of an acceptable formulation of ivacaftor in children aged 2 to 5 years with a CFTR gating mutation, although liver function seems to require closer monitoring in this age range than in adults, particularly among those with a history of elevated [liver function tests].”
Vertex Pharmaceuticals funded the study. Dr. Davies reported serving on advisory boards for Proteostasis, Pharmaxis, Pulmocide, Novartis, and Vertex Pharmaceuticals, and participating in educational activities for which her institution received payment. Seven coinvestigators also reported financial relationships with Vertex, including three who reported employment with the company.
Key clinical point: Ivacaftor appeared generally safe and well tolerated in young children with cystic fibrosis and a CFTR gating mutation.
Major finding: The only serious adverse event considered related to treatment was elevated transaminase levels on liver function tests.
Data source: A phase III, single-arm study of 9 children treated in part 1 (4 days) and 34 children treated in part 2 (24 weeks).
Disclosures: Vertex Pharmaceuticals funded the study. Dr. Davies reported serving on advisory boards for Proteostasis, Pharmaxis, Pulmocide, Novartis, and Vertex Pharmaceuticals, and participating in educational activities for which her institution received payment. Seven coinvestigators also reported financial relationships with Vertex, including three who reported employment with the company.
VIDEO: Treating your atopic dermatitis patients more effectively
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ORLANDO – A “hard and soft” approach to treating atopic dermatitis – treating more frequently while symptoms persist, then pulling back on treatment to keep symptoms at bay – is an effective way to keep the condition manageable for your patients.
“This is not an easy disease to manage, and that’s the key,” explained Dr. Adam Friedman of the George Washington University in Washington, at the Orlando Dermatology Aesthetic and Clinical annual meeting, adding that it’s important to educate patients that atopic dermatitis is “something that they will always have” and does not have one-shot cures.
In this video interview, Dr. Friedman, who is a Dermatology News board member, discusses the best way to talk to new patients about what atopic dermatitis treatment will entail, and offers methods to make management of the disease more effective and, consequently, improve patients’ quality of life.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ODAC 2016
Research refining radiomic features for lung cancer screening
SAN DIEGO – A series of radiomics-derived imaging features may improve the diagnostic accuracy of low-dose CT lung cancer screening and help predict which nodules are at risk of becoming cancers.
“We are providing pretty compelling evidence that there is some utility in this science,” Matthew Schabath, Ph.D., said at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
Radiomics is an emerging field that uses high-throughput extraction to identify hundreds of quantitative features from standard computed tomography (CT) images and mines that data to develop diagnostic, predictive, or prognostic models.
Radiologists first identify a region of interest (ROI) on the CT scan containing either the whole tumor or spatially explicit regions of the tumor called “habitats.” These ROIs are then segmented via computer software before being rendered in three dimensions. Quantitative features are extracted from the rendered volumes and entered into the models, along with other clinical and patient data.
“Right now our tool box is about 219, but by the end of the year we are hoping to have close to 1,000 radiomic features we can extract from a 3-D rendered nodule or tumor,” said Dr. Schabath, of the Moffitt Cancer Center in Tampa, Fla.
Although not without its own challenges, radiomics is a far cry from the current practice that relies on a single CT feature, nodule size, and clinical guidelines to evaluate and follow-up pulmonary nodules, none of which provides clinicians tools to accurately predict the risk or probability of lung cancer development.
CT images are typically thought of as pictures, but in radiomics, “the images are data. That’s really the underlying principle,” he said.
Led by Dr. Robert Gillies, often referred to as the father of radiomics, the researchers extracted and analyzed the 219 radiomic features from nodules in 196 lung cancer cases and in 392 controls who had a positive but benign nodule at the baseline scan and were matched for age, sex, smoking status, and race.
The post hoc, nested case-control study used images and data from the pivotal National Lung Screening Trial, which identified a 20% reduction in lung cancer mortality for low-dose CT screening compared with chest x-rays, but with a 96% false-positive rate, which also highlighted the challenges of LDCT as a screening tool.
Two classes of features were extracted from the images: semantic features, which are commonly used in radiology to describe ROIs, and agnostic features, which are mathematically extracted quantitative descriptors that capture lesion heterogeneity.
Univariable analyses were used to identify statistically significant features (threshold P value less than .05) and a backward elimination process (threshold P less than 0.1) performed to generate the final set of features, Dr. Schabath said.
Separate analyses were performed for predictive and diagnostic features.
In the risk prediction model, eight “highly informative features” were identified, Dr. Schabath said. Five were agnostic and three were semantic – circularity of the nodule, volume, and distance from or pleural attachment.
The receiver operating characteristic (ROC) area under the curve for the model was 0.92, with 75% sensitivity and 89% specificity. When the model included only patient demographics, it was no better than flipping a coin for predicting nodules at risk of becoming cancerous (ROC 0.58), he said.
Six highly informative features were identified in the agnostic model, which extracted features from the nodules found at the first and second follow-up interval, Dr. Schabath said. Three were agnostic and three semantic – longest diameter, volume, and distance from or pleural attachment.
The ROC for the diagnostic model was 0.89, with 74% sensitivity and 89% specificity.
When an additional analysis was performed using a nodule threshold of less than 15 mm to account for nodule growth over time and smaller nodule size at baseline in controls, the ROC and specificity held steady, but sensitivity dropped off to 59%, he said.
“I think we’re showing a rigorous [statistical] approach by identifying really unique, highly informative features,” Dr. Schabath concluded.
The overlap of volume and distance from or pleural attachment in both the diagnostic and predictive models suggests “there might be something very important about these two features,” he added.
Dr. Schabath stressed that the findings are preliminary and said additional analyses will be run before the results are ready for prime time. Long-term goals are to implement radiomic-based decision support tools and models into radiology reading rooms.
“In the future, we envision that all medical images will be converted to mineable data with the process of radiomics as part of standard of care,” Dr. Gillies said in an interview. “Such data have already shown promise to increase the precision and accuracy of diagnostic images, and hence, will increasingly be used in therapy decision support.”
Among the many challenges that first need to be resolved are that images are often captured with settings and filters that can be different even within a single institution. The inconsistency adds noise to the data that are extracted by computers.
“Hence, the most robust data we have today are generated by radiologists themselves, although this has its own challenges of being time-consuming with inter-reader variability,” Dr. Gillies noted.
Another major challenge is sharing of the image data. Right now, radiomics is practiced at only a few research hospitals and thus, building large cohort studies requires that the images be moved across site. In the future, the researchers anticipate that software can be deployed across sites to enable radiomic feature extraction, which would mean that only the extracted data will have to be shared, he said.
SAN DIEGO – A series of radiomics-derived imaging features may improve the diagnostic accuracy of low-dose CT lung cancer screening and help predict which nodules are at risk of becoming cancers.
“We are providing pretty compelling evidence that there is some utility in this science,” Matthew Schabath, Ph.D., said at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
Radiomics is an emerging field that uses high-throughput extraction to identify hundreds of quantitative features from standard computed tomography (CT) images and mines that data to develop diagnostic, predictive, or prognostic models.
Radiologists first identify a region of interest (ROI) on the CT scan containing either the whole tumor or spatially explicit regions of the tumor called “habitats.” These ROIs are then segmented via computer software before being rendered in three dimensions. Quantitative features are extracted from the rendered volumes and entered into the models, along with other clinical and patient data.
“Right now our tool box is about 219, but by the end of the year we are hoping to have close to 1,000 radiomic features we can extract from a 3-D rendered nodule or tumor,” said Dr. Schabath, of the Moffitt Cancer Center in Tampa, Fla.
Although not without its own challenges, radiomics is a far cry from the current practice that relies on a single CT feature, nodule size, and clinical guidelines to evaluate and follow-up pulmonary nodules, none of which provides clinicians tools to accurately predict the risk or probability of lung cancer development.
CT images are typically thought of as pictures, but in radiomics, “the images are data. That’s really the underlying principle,” he said.
Led by Dr. Robert Gillies, often referred to as the father of radiomics, the researchers extracted and analyzed the 219 radiomic features from nodules in 196 lung cancer cases and in 392 controls who had a positive but benign nodule at the baseline scan and were matched for age, sex, smoking status, and race.
The post hoc, nested case-control study used images and data from the pivotal National Lung Screening Trial, which identified a 20% reduction in lung cancer mortality for low-dose CT screening compared with chest x-rays, but with a 96% false-positive rate, which also highlighted the challenges of LDCT as a screening tool.
Two classes of features were extracted from the images: semantic features, which are commonly used in radiology to describe ROIs, and agnostic features, which are mathematically extracted quantitative descriptors that capture lesion heterogeneity.
Univariable analyses were used to identify statistically significant features (threshold P value less than .05) and a backward elimination process (threshold P less than 0.1) performed to generate the final set of features, Dr. Schabath said.
Separate analyses were performed for predictive and diagnostic features.
In the risk prediction model, eight “highly informative features” were identified, Dr. Schabath said. Five were agnostic and three were semantic – circularity of the nodule, volume, and distance from or pleural attachment.
The receiver operating characteristic (ROC) area under the curve for the model was 0.92, with 75% sensitivity and 89% specificity. When the model included only patient demographics, it was no better than flipping a coin for predicting nodules at risk of becoming cancerous (ROC 0.58), he said.
Six highly informative features were identified in the agnostic model, which extracted features from the nodules found at the first and second follow-up interval, Dr. Schabath said. Three were agnostic and three semantic – longest diameter, volume, and distance from or pleural attachment.
The ROC for the diagnostic model was 0.89, with 74% sensitivity and 89% specificity.
When an additional analysis was performed using a nodule threshold of less than 15 mm to account for nodule growth over time and smaller nodule size at baseline in controls, the ROC and specificity held steady, but sensitivity dropped off to 59%, he said.
“I think we’re showing a rigorous [statistical] approach by identifying really unique, highly informative features,” Dr. Schabath concluded.
The overlap of volume and distance from or pleural attachment in both the diagnostic and predictive models suggests “there might be something very important about these two features,” he added.
Dr. Schabath stressed that the findings are preliminary and said additional analyses will be run before the results are ready for prime time. Long-term goals are to implement radiomic-based decision support tools and models into radiology reading rooms.
“In the future, we envision that all medical images will be converted to mineable data with the process of radiomics as part of standard of care,” Dr. Gillies said in an interview. “Such data have already shown promise to increase the precision and accuracy of diagnostic images, and hence, will increasingly be used in therapy decision support.”
Among the many challenges that first need to be resolved are that images are often captured with settings and filters that can be different even within a single institution. The inconsistency adds noise to the data that are extracted by computers.
“Hence, the most robust data we have today are generated by radiologists themselves, although this has its own challenges of being time-consuming with inter-reader variability,” Dr. Gillies noted.
Another major challenge is sharing of the image data. Right now, radiomics is practiced at only a few research hospitals and thus, building large cohort studies requires that the images be moved across site. In the future, the researchers anticipate that software can be deployed across sites to enable radiomic feature extraction, which would mean that only the extracted data will have to be shared, he said.
SAN DIEGO – A series of radiomics-derived imaging features may improve the diagnostic accuracy of low-dose CT lung cancer screening and help predict which nodules are at risk of becoming cancers.
“We are providing pretty compelling evidence that there is some utility in this science,” Matthew Schabath, Ph.D., said at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
Radiomics is an emerging field that uses high-throughput extraction to identify hundreds of quantitative features from standard computed tomography (CT) images and mines that data to develop diagnostic, predictive, or prognostic models.
Radiologists first identify a region of interest (ROI) on the CT scan containing either the whole tumor or spatially explicit regions of the tumor called “habitats.” These ROIs are then segmented via computer software before being rendered in three dimensions. Quantitative features are extracted from the rendered volumes and entered into the models, along with other clinical and patient data.
“Right now our tool box is about 219, but by the end of the year we are hoping to have close to 1,000 radiomic features we can extract from a 3-D rendered nodule or tumor,” said Dr. Schabath, of the Moffitt Cancer Center in Tampa, Fla.
Although not without its own challenges, radiomics is a far cry from the current practice that relies on a single CT feature, nodule size, and clinical guidelines to evaluate and follow-up pulmonary nodules, none of which provides clinicians tools to accurately predict the risk or probability of lung cancer development.
CT images are typically thought of as pictures, but in radiomics, “the images are data. That’s really the underlying principle,” he said.
Led by Dr. Robert Gillies, often referred to as the father of radiomics, the researchers extracted and analyzed the 219 radiomic features from nodules in 196 lung cancer cases and in 392 controls who had a positive but benign nodule at the baseline scan and were matched for age, sex, smoking status, and race.
The post hoc, nested case-control study used images and data from the pivotal National Lung Screening Trial, which identified a 20% reduction in lung cancer mortality for low-dose CT screening compared with chest x-rays, but with a 96% false-positive rate, which also highlighted the challenges of LDCT as a screening tool.
Two classes of features were extracted from the images: semantic features, which are commonly used in radiology to describe ROIs, and agnostic features, which are mathematically extracted quantitative descriptors that capture lesion heterogeneity.
Univariable analyses were used to identify statistically significant features (threshold P value less than .05) and a backward elimination process (threshold P less than 0.1) performed to generate the final set of features, Dr. Schabath said.
Separate analyses were performed for predictive and diagnostic features.
In the risk prediction model, eight “highly informative features” were identified, Dr. Schabath said. Five were agnostic and three were semantic – circularity of the nodule, volume, and distance from or pleural attachment.
The receiver operating characteristic (ROC) area under the curve for the model was 0.92, with 75% sensitivity and 89% specificity. When the model included only patient demographics, it was no better than flipping a coin for predicting nodules at risk of becoming cancerous (ROC 0.58), he said.
Six highly informative features were identified in the agnostic model, which extracted features from the nodules found at the first and second follow-up interval, Dr. Schabath said. Three were agnostic and three semantic – longest diameter, volume, and distance from or pleural attachment.
The ROC for the diagnostic model was 0.89, with 74% sensitivity and 89% specificity.
When an additional analysis was performed using a nodule threshold of less than 15 mm to account for nodule growth over time and smaller nodule size at baseline in controls, the ROC and specificity held steady, but sensitivity dropped off to 59%, he said.
“I think we’re showing a rigorous [statistical] approach by identifying really unique, highly informative features,” Dr. Schabath concluded.
The overlap of volume and distance from or pleural attachment in both the diagnostic and predictive models suggests “there might be something very important about these two features,” he added.
Dr. Schabath stressed that the findings are preliminary and said additional analyses will be run before the results are ready for prime time. Long-term goals are to implement radiomic-based decision support tools and models into radiology reading rooms.
“In the future, we envision that all medical images will be converted to mineable data with the process of radiomics as part of standard of care,” Dr. Gillies said in an interview. “Such data have already shown promise to increase the precision and accuracy of diagnostic images, and hence, will increasingly be used in therapy decision support.”
Among the many challenges that first need to be resolved are that images are often captured with settings and filters that can be different even within a single institution. The inconsistency adds noise to the data that are extracted by computers.
“Hence, the most robust data we have today are generated by radiologists themselves, although this has its own challenges of being time-consuming with inter-reader variability,” Dr. Gillies noted.
Another major challenge is sharing of the image data. Right now, radiomics is practiced at only a few research hospitals and thus, building large cohort studies requires that the images be moved across site. In the future, the researchers anticipate that software can be deployed across sites to enable radiomic feature extraction, which would mean that only the extracted data will have to be shared, he said.
AT AN AACR/IASLC JOINT CONFERENCE
Key clinical point: Non-invasive radiomics is showing potential for reducing false positives by differentiating between benign and cancerous lung nodules and quantitatively predicting future risk of lung cancer incidence.
Major finding: The receiver operating characteristic area under the curve for the risk prediction model was 0.92, with 75% sensitivity and 89% specificity.
Data source: Post hoc case-control analysis in 588 persons at high risk for lung cancer in the National Lung Screening Trial.
Disclosures: Dr. Schabath reported having no relevant conflicts of interest. Dr. Gillies reported serving as a speaker for HealthMyne.
Deciphering lung cancer biomarkers shrouded in tobacco smoke
SAN DIEGO – Tobacco researchers are getting one step closer to identifying young smokers particularly susceptible to the carcinogenic effects of smoking, by using large-scale epidemiology studies and DNA adducts data.
“This is not lung cancer screening; this is not early detection of lung cancer; this is detection of susceptible, high-risk individuals, so they can be targeted for cessation, surveillance, and prevention,” said Stephen S. Hecht, Ph.D., professor of cancer prevention at the University of Minnesota Masonic Cancer Center in Minneapolis.
While nicotine itself is not a carcinogen, each puff of tobacco smoke delivers a mixture of more than 70 established carcinogens, including the potent lung-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK).
Some of these carcinogens are excreted, but many will undergo metabolic activation and interact with a patient’s DNA.
The product of this interaction, called DNA adducts, causes persistent miscoding during DNA replication, leading to the thousands of mutations we see in lung cancer, he explained at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
The biomarkers of tobacco exposure and metabolism are very well developed, with blood and urinary biomarker panels applied in many studies and validated by mass spectrometry.
Using the Shanghai cohort study, the researchers identified three urinary biomarkers – PheT (r-1,t-2,3,c-4-tetrahydroxy-1,2,3,4-tetrahydrophenanthrene), total NNAL (a metabolite of NNK and its glucuronides), and total cotinine (a surrogate for nicotine that includes cotinine and its glucuronides) – that were significantly associated with lung cancer in 950 smokers, even after adjustment for smoking duration and intensity (Cancer Res. 2011;71:6749-57).
A more recent, deeper dive of 735 of those urinary samples, still stable about 20 years after they were taken, looked specifically at polymorphisms in cytochrome P450 2A6 (CYP2A6), the primary enzyme responsible for the oxidation of nicotine and cotinine.
Data currently in press show that CYP2A6 poor metabolizers had a lower risk of lung cancer than the combined group of normal, intermediate, or slow metabolizers (odds ratio, 0.64; P value for trend = .034).
“This is logical because poor metabolizers of nicotine have more unchanged nicotine on board, so they don’t need to smoke as intensely in order to get more nicotine because that nicotine is remaining to a greater extent in its natural form, rather than being metabolized into cotinine, which is not addictive,” Dr. Hecht said.
Recent genomewide-association studies by Dr. Hecht and his colleagues of smokers in the Multiethnic Cohort Study revealed that Japanese Americans had the highest number of low nicotine CYP2A6 metabolizing genotypes of the five ethnic groups analyzed, consistent with their low lung cancer risk.
Urinary biomarker studies showed that levels of total NNAL, 3-hydroxy phenanthrene, a biomarker of polycyclic aromatic hydrocarbon uptake, and S-phenylmercapturic acid (SPMA), a biomarker of benzene exposure, were also significantly higher among African Americans than whites and significantly lower in Japanese Americans than whites, he said.
The findings are consistent with the initial study results published a decade ago (N Engl J Med. 2006;354:333-342), showing that at low levels of smoking (10 cigarettes per day), Japanese Americans and Hispanics had one-third the risk of lung cancer of African Americans or Native Hawaiians (P less than .001). The differences disappeared at higher levels of smoking (30 cigarettes per day).
Results from the new analyses for Native Hawaiians and Hispanics, however, did not fit this pattern, and “we’re not sure what’s going on there and need to do more work,” Dr. Hecht said.
Nicotine equivalent levels in Native Hawaiians were actually lower than would be expected based on their high lung cancer risk, while Hispanics had higher levels than would be expected based on their low risk.
Interestingly, urinary levels of 3-hydroxypropylmercapturic acid (3-HPMA), a metabolite of acrolein, were found to be unusually high in Native Hawaiians and relatively low in Hispanics, “which may play into their lung cancer risk because acrolein is a very strong toxicant and there is evidence to suggest it is involved in lung cancer,” he said.
While tobacco exposure and metabolism biomarkers have hit their stride, less well developed are the DNA adducts and repair biomarkers that can predict lung cancer susceptibility. This is a critical step because of the role DNA adducts play in the formation of lung cancer mutations, Dr. Hecht said.
A smoker may have a high tobacco exposure as indicated by the urinary biomarkers, but have a low metabolism to form DNA adducts or high DNA repair, which would mean their DNA adduct levels would be low. Conversely, another smoker with low exposure and poor DNA repair may have higher DNA adduct levels, and thus, a greater risk for developing lung cancer.
In addition, the exposure biomarkers are not entirely predictive and thus, will need to be combined with multiple DNA adducts and repair if susceptible smokers are to be identified and targeted for state-of-the art cessation approaches and surveillance, he said.
Using high-level mass spectrometry, the researchers have been able to readily measure formaldehyde DNA adducts and tobacco-specific 4-hydroxy-1-(3-pyridyl)-1-butanone (HPB)–releasing DNA adducts in human oral cells. Levels of the HPB adduct were unusually high at 12-45 pmol/mg, which is similar to what is seen in animals when exposed to NNK at a much higher dose than smokers take in.
“So this is a real lead,” said Dr. Hecht, who reported having no relevant conflicts of interest.
SAN DIEGO – Tobacco researchers are getting one step closer to identifying young smokers particularly susceptible to the carcinogenic effects of smoking, by using large-scale epidemiology studies and DNA adducts data.
“This is not lung cancer screening; this is not early detection of lung cancer; this is detection of susceptible, high-risk individuals, so they can be targeted for cessation, surveillance, and prevention,” said Stephen S. Hecht, Ph.D., professor of cancer prevention at the University of Minnesota Masonic Cancer Center in Minneapolis.
While nicotine itself is not a carcinogen, each puff of tobacco smoke delivers a mixture of more than 70 established carcinogens, including the potent lung-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK).
Some of these carcinogens are excreted, but many will undergo metabolic activation and interact with a patient’s DNA.
The product of this interaction, called DNA adducts, causes persistent miscoding during DNA replication, leading to the thousands of mutations we see in lung cancer, he explained at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
The biomarkers of tobacco exposure and metabolism are very well developed, with blood and urinary biomarker panels applied in many studies and validated by mass spectrometry.
Using the Shanghai cohort study, the researchers identified three urinary biomarkers – PheT (r-1,t-2,3,c-4-tetrahydroxy-1,2,3,4-tetrahydrophenanthrene), total NNAL (a metabolite of NNK and its glucuronides), and total cotinine (a surrogate for nicotine that includes cotinine and its glucuronides) – that were significantly associated with lung cancer in 950 smokers, even after adjustment for smoking duration and intensity (Cancer Res. 2011;71:6749-57).
A more recent, deeper dive of 735 of those urinary samples, still stable about 20 years after they were taken, looked specifically at polymorphisms in cytochrome P450 2A6 (CYP2A6), the primary enzyme responsible for the oxidation of nicotine and cotinine.
Data currently in press show that CYP2A6 poor metabolizers had a lower risk of lung cancer than the combined group of normal, intermediate, or slow metabolizers (odds ratio, 0.64; P value for trend = .034).
“This is logical because poor metabolizers of nicotine have more unchanged nicotine on board, so they don’t need to smoke as intensely in order to get more nicotine because that nicotine is remaining to a greater extent in its natural form, rather than being metabolized into cotinine, which is not addictive,” Dr. Hecht said.
Recent genomewide-association studies by Dr. Hecht and his colleagues of smokers in the Multiethnic Cohort Study revealed that Japanese Americans had the highest number of low nicotine CYP2A6 metabolizing genotypes of the five ethnic groups analyzed, consistent with their low lung cancer risk.
Urinary biomarker studies showed that levels of total NNAL, 3-hydroxy phenanthrene, a biomarker of polycyclic aromatic hydrocarbon uptake, and S-phenylmercapturic acid (SPMA), a biomarker of benzene exposure, were also significantly higher among African Americans than whites and significantly lower in Japanese Americans than whites, he said.
The findings are consistent with the initial study results published a decade ago (N Engl J Med. 2006;354:333-342), showing that at low levels of smoking (10 cigarettes per day), Japanese Americans and Hispanics had one-third the risk of lung cancer of African Americans or Native Hawaiians (P less than .001). The differences disappeared at higher levels of smoking (30 cigarettes per day).
Results from the new analyses for Native Hawaiians and Hispanics, however, did not fit this pattern, and “we’re not sure what’s going on there and need to do more work,” Dr. Hecht said.
Nicotine equivalent levels in Native Hawaiians were actually lower than would be expected based on their high lung cancer risk, while Hispanics had higher levels than would be expected based on their low risk.
Interestingly, urinary levels of 3-hydroxypropylmercapturic acid (3-HPMA), a metabolite of acrolein, were found to be unusually high in Native Hawaiians and relatively low in Hispanics, “which may play into their lung cancer risk because acrolein is a very strong toxicant and there is evidence to suggest it is involved in lung cancer,” he said.
While tobacco exposure and metabolism biomarkers have hit their stride, less well developed are the DNA adducts and repair biomarkers that can predict lung cancer susceptibility. This is a critical step because of the role DNA adducts play in the formation of lung cancer mutations, Dr. Hecht said.
A smoker may have a high tobacco exposure as indicated by the urinary biomarkers, but have a low metabolism to form DNA adducts or high DNA repair, which would mean their DNA adduct levels would be low. Conversely, another smoker with low exposure and poor DNA repair may have higher DNA adduct levels, and thus, a greater risk for developing lung cancer.
In addition, the exposure biomarkers are not entirely predictive and thus, will need to be combined with multiple DNA adducts and repair if susceptible smokers are to be identified and targeted for state-of-the art cessation approaches and surveillance, he said.
Using high-level mass spectrometry, the researchers have been able to readily measure formaldehyde DNA adducts and tobacco-specific 4-hydroxy-1-(3-pyridyl)-1-butanone (HPB)–releasing DNA adducts in human oral cells. Levels of the HPB adduct were unusually high at 12-45 pmol/mg, which is similar to what is seen in animals when exposed to NNK at a much higher dose than smokers take in.
“So this is a real lead,” said Dr. Hecht, who reported having no relevant conflicts of interest.
SAN DIEGO – Tobacco researchers are getting one step closer to identifying young smokers particularly susceptible to the carcinogenic effects of smoking, by using large-scale epidemiology studies and DNA adducts data.
“This is not lung cancer screening; this is not early detection of lung cancer; this is detection of susceptible, high-risk individuals, so they can be targeted for cessation, surveillance, and prevention,” said Stephen S. Hecht, Ph.D., professor of cancer prevention at the University of Minnesota Masonic Cancer Center in Minneapolis.
While nicotine itself is not a carcinogen, each puff of tobacco smoke delivers a mixture of more than 70 established carcinogens, including the potent lung-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK).
Some of these carcinogens are excreted, but many will undergo metabolic activation and interact with a patient’s DNA.
The product of this interaction, called DNA adducts, causes persistent miscoding during DNA replication, leading to the thousands of mutations we see in lung cancer, he explained at a conference on lung cancer translational science sponsored by the American Association for Cancer Research and the International Association for the Study of Lung Cancer.
The biomarkers of tobacco exposure and metabolism are very well developed, with blood and urinary biomarker panels applied in many studies and validated by mass spectrometry.
Using the Shanghai cohort study, the researchers identified three urinary biomarkers – PheT (r-1,t-2,3,c-4-tetrahydroxy-1,2,3,4-tetrahydrophenanthrene), total NNAL (a metabolite of NNK and its glucuronides), and total cotinine (a surrogate for nicotine that includes cotinine and its glucuronides) – that were significantly associated with lung cancer in 950 smokers, even after adjustment for smoking duration and intensity (Cancer Res. 2011;71:6749-57).
A more recent, deeper dive of 735 of those urinary samples, still stable about 20 years after they were taken, looked specifically at polymorphisms in cytochrome P450 2A6 (CYP2A6), the primary enzyme responsible for the oxidation of nicotine and cotinine.
Data currently in press show that CYP2A6 poor metabolizers had a lower risk of lung cancer than the combined group of normal, intermediate, or slow metabolizers (odds ratio, 0.64; P value for trend = .034).
“This is logical because poor metabolizers of nicotine have more unchanged nicotine on board, so they don’t need to smoke as intensely in order to get more nicotine because that nicotine is remaining to a greater extent in its natural form, rather than being metabolized into cotinine, which is not addictive,” Dr. Hecht said.
Recent genomewide-association studies by Dr. Hecht and his colleagues of smokers in the Multiethnic Cohort Study revealed that Japanese Americans had the highest number of low nicotine CYP2A6 metabolizing genotypes of the five ethnic groups analyzed, consistent with their low lung cancer risk.
Urinary biomarker studies showed that levels of total NNAL, 3-hydroxy phenanthrene, a biomarker of polycyclic aromatic hydrocarbon uptake, and S-phenylmercapturic acid (SPMA), a biomarker of benzene exposure, were also significantly higher among African Americans than whites and significantly lower in Japanese Americans than whites, he said.
The findings are consistent with the initial study results published a decade ago (N Engl J Med. 2006;354:333-342), showing that at low levels of smoking (10 cigarettes per day), Japanese Americans and Hispanics had one-third the risk of lung cancer of African Americans or Native Hawaiians (P less than .001). The differences disappeared at higher levels of smoking (30 cigarettes per day).
Results from the new analyses for Native Hawaiians and Hispanics, however, did not fit this pattern, and “we’re not sure what’s going on there and need to do more work,” Dr. Hecht said.
Nicotine equivalent levels in Native Hawaiians were actually lower than would be expected based on their high lung cancer risk, while Hispanics had higher levels than would be expected based on their low risk.
Interestingly, urinary levels of 3-hydroxypropylmercapturic acid (3-HPMA), a metabolite of acrolein, were found to be unusually high in Native Hawaiians and relatively low in Hispanics, “which may play into their lung cancer risk because acrolein is a very strong toxicant and there is evidence to suggest it is involved in lung cancer,” he said.
While tobacco exposure and metabolism biomarkers have hit their stride, less well developed are the DNA adducts and repair biomarkers that can predict lung cancer susceptibility. This is a critical step because of the role DNA adducts play in the formation of lung cancer mutations, Dr. Hecht said.
A smoker may have a high tobacco exposure as indicated by the urinary biomarkers, but have a low metabolism to form DNA adducts or high DNA repair, which would mean their DNA adduct levels would be low. Conversely, another smoker with low exposure and poor DNA repair may have higher DNA adduct levels, and thus, a greater risk for developing lung cancer.
In addition, the exposure biomarkers are not entirely predictive and thus, will need to be combined with multiple DNA adducts and repair if susceptible smokers are to be identified and targeted for state-of-the art cessation approaches and surveillance, he said.
Using high-level mass spectrometry, the researchers have been able to readily measure formaldehyde DNA adducts and tobacco-specific 4-hydroxy-1-(3-pyridyl)-1-butanone (HPB)–releasing DNA adducts in human oral cells. Levels of the HPB adduct were unusually high at 12-45 pmol/mg, which is similar to what is seen in animals when exposed to NNK at a much higher dose than smokers take in.
“So this is a real lead,” said Dr. Hecht, who reported having no relevant conflicts of interest.
AT AN AACR/IASLC JOINT CONFERENCE
Gene signatures aid diagnosis of acute respiratory infection etiology
Pathogen-specific host gene expression patterns accurately discriminated most noninfectious from infectious illnesses, and bacterial from viral causes of acute respiratory infection (ARI) in an observational study conducted in acute care settings.
The findings could have important implications for combating inappropriate antibiotic use and emerging antibiotic resistance, Dr. Ephraim L. Tsalik of the department of medicine at Duke University, Durham, N.C., and his colleagues reported online Jan. 20 in Science Translational Medicine.
The investigators analyzed peripheral whole-blood gene expression from 273 subjects with community-onset viral ARI (115 subjects), bacterial ARI (70 subjects), or noninfectious illness (88 subjects) who were seen in an emergency department, and from 44 healthy control subjects. Classifiers for bacterial ARI, viral ARI, and noninfectious causes of illness were developed, and were 87% accurate overall (Sci Transl Med. 2016;8[322]:322ra11. doi/ 10.1126/scitranslmed.aad6873).
“Bacterial ARI was identified in 83% of patients and excluded in 94% without bacterial infection. Viral ARI was identified in 90% and excluded in 92% of cases. Using the noninfectious illness classifier, infection was excluded in 86% of cases,” they wrote.
The classifiers were more accurate than procalcitonin – a widely used biomarker with some specificity for bacterial infection (86% vs. 78% accuracy in 238 available samples), and three published classifiers of bacterial vs. viral infection, and were validated in five publicly available data sets, they noted.
The gene signature patterns identified in the course of this study mark an important step toward development of a rapid blood test that could be used in clinics to guide appropriate treatment for ARIs, the investigators said.
Precision treatment of viruses
More precise ways to distinguish infections could reduce unnecessary antibiotic use and lead to more precise treatment of viruses, senior author Dr. Geoffrey S. Ginsburg, director of Duke’s Center for Applied Genomics & Precision Medicine, said in a press statement.
“Right now, we can give patients [oseltamivir] Tamiflu to help them recover from an influenza infection, but for most viral infections, the treatment is fluids and rest until it resolves. In the next 5-10 years, we will likely see new antiviral medications for common bugs like respiratory syncytial virus and even rhinovirus, and guiding treatment choices will be even more important,” he added.
Senior author Dr. Christopher W. Woods, also of Duke University, further explained in an interview that the findings are particularly exciting because “there isn’t much out there that accomplishes what we’ve done. So just about any level of accuracy is an improvement.” Further, he said the test is “a tool to aid in diagnosis, used in conjunction with the patient’s symptoms, examination, and other testing. So an imperfect test is okay, because it does not stand alone.”
Next steps include putting the assay on a testing platform that can be used at the point of care, and validating the findings in all populations, including infants, the elderly, and across ethnic groups, he said.
“The work is ongoing, and we expect to have results available within the course of an outpatient visit in the near future,” Dr. Woods, also a professor of medicine and global health, added, noting that efforts also are underway to “expand the repertoire of this approach to many different types of viral and bacterial infections and also to fungal infections, and to address the challenges of critically ill patients in intensive care units.”
This study was supported by the U.S. Defense Advanced Research Projects Agency, the National Institutes of Health, the Agency for Healthcare Research and Quality, the U.S. Department of Veterans Affairs Office of Research and Development, and an in-kind contribution from bioMérieux. The authors reported having no relevant competing interests.
Pathogen-specific host gene expression patterns accurately discriminated most noninfectious from infectious illnesses, and bacterial from viral causes of acute respiratory infection (ARI) in an observational study conducted in acute care settings.
The findings could have important implications for combating inappropriate antibiotic use and emerging antibiotic resistance, Dr. Ephraim L. Tsalik of the department of medicine at Duke University, Durham, N.C., and his colleagues reported online Jan. 20 in Science Translational Medicine.
The investigators analyzed peripheral whole-blood gene expression from 273 subjects with community-onset viral ARI (115 subjects), bacterial ARI (70 subjects), or noninfectious illness (88 subjects) who were seen in an emergency department, and from 44 healthy control subjects. Classifiers for bacterial ARI, viral ARI, and noninfectious causes of illness were developed, and were 87% accurate overall (Sci Transl Med. 2016;8[322]:322ra11. doi/ 10.1126/scitranslmed.aad6873).
“Bacterial ARI was identified in 83% of patients and excluded in 94% without bacterial infection. Viral ARI was identified in 90% and excluded in 92% of cases. Using the noninfectious illness classifier, infection was excluded in 86% of cases,” they wrote.
The classifiers were more accurate than procalcitonin – a widely used biomarker with some specificity for bacterial infection (86% vs. 78% accuracy in 238 available samples), and three published classifiers of bacterial vs. viral infection, and were validated in five publicly available data sets, they noted.
The gene signature patterns identified in the course of this study mark an important step toward development of a rapid blood test that could be used in clinics to guide appropriate treatment for ARIs, the investigators said.
Precision treatment of viruses
More precise ways to distinguish infections could reduce unnecessary antibiotic use and lead to more precise treatment of viruses, senior author Dr. Geoffrey S. Ginsburg, director of Duke’s Center for Applied Genomics & Precision Medicine, said in a press statement.
“Right now, we can give patients [oseltamivir] Tamiflu to help them recover from an influenza infection, but for most viral infections, the treatment is fluids and rest until it resolves. In the next 5-10 years, we will likely see new antiviral medications for common bugs like respiratory syncytial virus and even rhinovirus, and guiding treatment choices will be even more important,” he added.
Senior author Dr. Christopher W. Woods, also of Duke University, further explained in an interview that the findings are particularly exciting because “there isn’t much out there that accomplishes what we’ve done. So just about any level of accuracy is an improvement.” Further, he said the test is “a tool to aid in diagnosis, used in conjunction with the patient’s symptoms, examination, and other testing. So an imperfect test is okay, because it does not stand alone.”
Next steps include putting the assay on a testing platform that can be used at the point of care, and validating the findings in all populations, including infants, the elderly, and across ethnic groups, he said.
“The work is ongoing, and we expect to have results available within the course of an outpatient visit in the near future,” Dr. Woods, also a professor of medicine and global health, added, noting that efforts also are underway to “expand the repertoire of this approach to many different types of viral and bacterial infections and also to fungal infections, and to address the challenges of critically ill patients in intensive care units.”
This study was supported by the U.S. Defense Advanced Research Projects Agency, the National Institutes of Health, the Agency for Healthcare Research and Quality, the U.S. Department of Veterans Affairs Office of Research and Development, and an in-kind contribution from bioMérieux. The authors reported having no relevant competing interests.
Pathogen-specific host gene expression patterns accurately discriminated most noninfectious from infectious illnesses, and bacterial from viral causes of acute respiratory infection (ARI) in an observational study conducted in acute care settings.
The findings could have important implications for combating inappropriate antibiotic use and emerging antibiotic resistance, Dr. Ephraim L. Tsalik of the department of medicine at Duke University, Durham, N.C., and his colleagues reported online Jan. 20 in Science Translational Medicine.
The investigators analyzed peripheral whole-blood gene expression from 273 subjects with community-onset viral ARI (115 subjects), bacterial ARI (70 subjects), or noninfectious illness (88 subjects) who were seen in an emergency department, and from 44 healthy control subjects. Classifiers for bacterial ARI, viral ARI, and noninfectious causes of illness were developed, and were 87% accurate overall (Sci Transl Med. 2016;8[322]:322ra11. doi/ 10.1126/scitranslmed.aad6873).
“Bacterial ARI was identified in 83% of patients and excluded in 94% without bacterial infection. Viral ARI was identified in 90% and excluded in 92% of cases. Using the noninfectious illness classifier, infection was excluded in 86% of cases,” they wrote.
The classifiers were more accurate than procalcitonin – a widely used biomarker with some specificity for bacterial infection (86% vs. 78% accuracy in 238 available samples), and three published classifiers of bacterial vs. viral infection, and were validated in five publicly available data sets, they noted.
The gene signature patterns identified in the course of this study mark an important step toward development of a rapid blood test that could be used in clinics to guide appropriate treatment for ARIs, the investigators said.
Precision treatment of viruses
More precise ways to distinguish infections could reduce unnecessary antibiotic use and lead to more precise treatment of viruses, senior author Dr. Geoffrey S. Ginsburg, director of Duke’s Center for Applied Genomics & Precision Medicine, said in a press statement.
“Right now, we can give patients [oseltamivir] Tamiflu to help them recover from an influenza infection, but for most viral infections, the treatment is fluids and rest until it resolves. In the next 5-10 years, we will likely see new antiviral medications for common bugs like respiratory syncytial virus and even rhinovirus, and guiding treatment choices will be even more important,” he added.
Senior author Dr. Christopher W. Woods, also of Duke University, further explained in an interview that the findings are particularly exciting because “there isn’t much out there that accomplishes what we’ve done. So just about any level of accuracy is an improvement.” Further, he said the test is “a tool to aid in diagnosis, used in conjunction with the patient’s symptoms, examination, and other testing. So an imperfect test is okay, because it does not stand alone.”
Next steps include putting the assay on a testing platform that can be used at the point of care, and validating the findings in all populations, including infants, the elderly, and across ethnic groups, he said.
“The work is ongoing, and we expect to have results available within the course of an outpatient visit in the near future,” Dr. Woods, also a professor of medicine and global health, added, noting that efforts also are underway to “expand the repertoire of this approach to many different types of viral and bacterial infections and also to fungal infections, and to address the challenges of critically ill patients in intensive care units.”
This study was supported by the U.S. Defense Advanced Research Projects Agency, the National Institutes of Health, the Agency for Healthcare Research and Quality, the U.S. Department of Veterans Affairs Office of Research and Development, and an in-kind contribution from bioMérieux. The authors reported having no relevant competing interests.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Pathogen-specific host gene expression patterns accurately discriminated most noninfectious from infectious illnesses, and bacterial from viral causes of acute respiratory infection (ARI) in an observational study.
Major finding: Classifiers for bacterial ARI, viral ARI, and noninfectious causes of illness were 87% accurate overall.
Data source: An observational cohort study involving 273 patients and 44 controls.
Disclosures: This study was supported by the U.S. Defense Advanced Research Projects Agency, the National Institutes of Health, the Agency for Healthcare Research and Quality, the U.S. Department of Veterans Affairs Office of Research and Development, and an in-kind contribution from bioMérieux. The authors reported having no relevant competing interests..
New year brings reduced flu activity
Influenza-like illness (ILI) activity was down during the first full week in January – a not-so-unlucky week 13 of the 2015-2016 flu season, the Centers for Disease Control and Prevention reported.
South Carolina was at level 8, making it the only state in the “high” range of activity for the week ending Jan. 9. Puerto Rico was also at level 8, but there was no state in the “moderate” range and only seven states in the “low” range: Arizona and Maryland at level 5 and Connecticut, Illinois, Pennsylvania, Texas, and Virginia at level 4. There were 18 states at level 2 or higher, compared with 24 the previous week, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
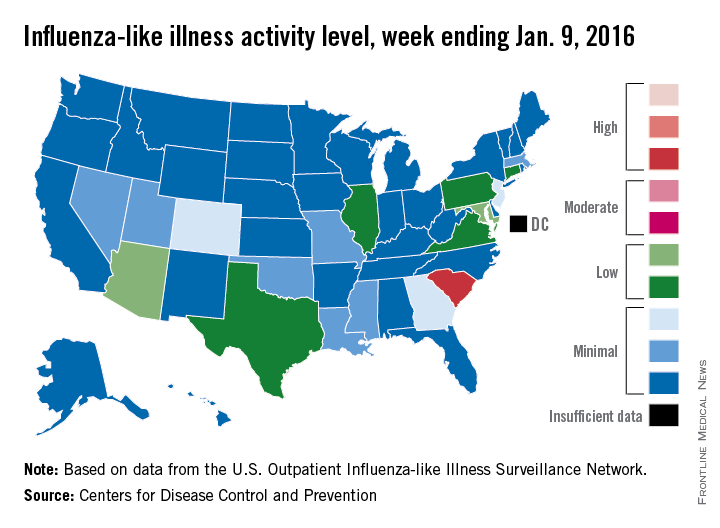
The proportion of outpatient visits for ILI was 2% for week 13, which was down from 2.8% in week 12 and below the national baseline of 2.1%, the CDC said. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
One ILI-related pediatric death was reported during week 13, although it actually occurred in December. So far, there have been seven pediatric deaths reported during the 2015-2016 flu season, the CDC report noted.
Since Oct. 1, 2015, there have been 423 laboratory-confirmed influenza-associated hospitalizations reported in the 13 states – including California, New York, and Ohio – of the CDC’s Influenza Hospitalization Surveillance Network, for an overall hospitalization rate of 1.5 per 100,000 population. That rate, however, is “likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications,” the CDC said.
Influenza-like illness (ILI) activity was down during the first full week in January – a not-so-unlucky week 13 of the 2015-2016 flu season, the Centers for Disease Control and Prevention reported.
South Carolina was at level 8, making it the only state in the “high” range of activity for the week ending Jan. 9. Puerto Rico was also at level 8, but there was no state in the “moderate” range and only seven states in the “low” range: Arizona and Maryland at level 5 and Connecticut, Illinois, Pennsylvania, Texas, and Virginia at level 4. There were 18 states at level 2 or higher, compared with 24 the previous week, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
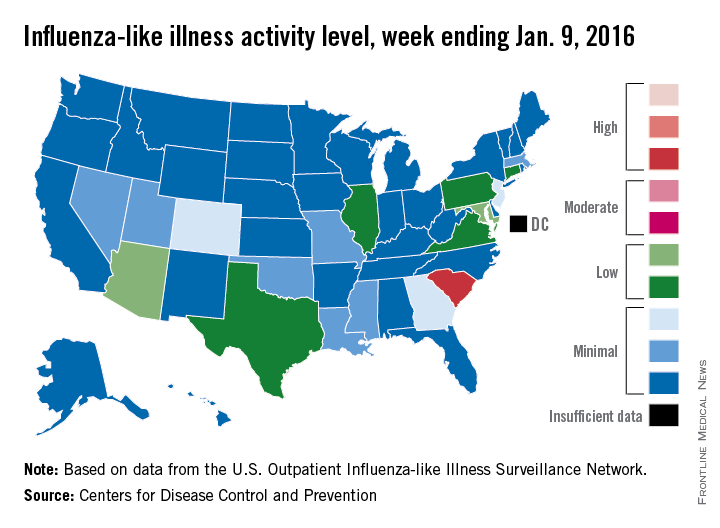
The proportion of outpatient visits for ILI was 2% for week 13, which was down from 2.8% in week 12 and below the national baseline of 2.1%, the CDC said. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
One ILI-related pediatric death was reported during week 13, although it actually occurred in December. So far, there have been seven pediatric deaths reported during the 2015-2016 flu season, the CDC report noted.
Since Oct. 1, 2015, there have been 423 laboratory-confirmed influenza-associated hospitalizations reported in the 13 states – including California, New York, and Ohio – of the CDC’s Influenza Hospitalization Surveillance Network, for an overall hospitalization rate of 1.5 per 100,000 population. That rate, however, is “likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications,” the CDC said.
Influenza-like illness (ILI) activity was down during the first full week in January – a not-so-unlucky week 13 of the 2015-2016 flu season, the Centers for Disease Control and Prevention reported.
South Carolina was at level 8, making it the only state in the “high” range of activity for the week ending Jan. 9. Puerto Rico was also at level 8, but there was no state in the “moderate” range and only seven states in the “low” range: Arizona and Maryland at level 5 and Connecticut, Illinois, Pennsylvania, Texas, and Virginia at level 4. There were 18 states at level 2 or higher, compared with 24 the previous week, according to data from the CDC’s Outpatient Influenza-like Illness Surveillance Network.
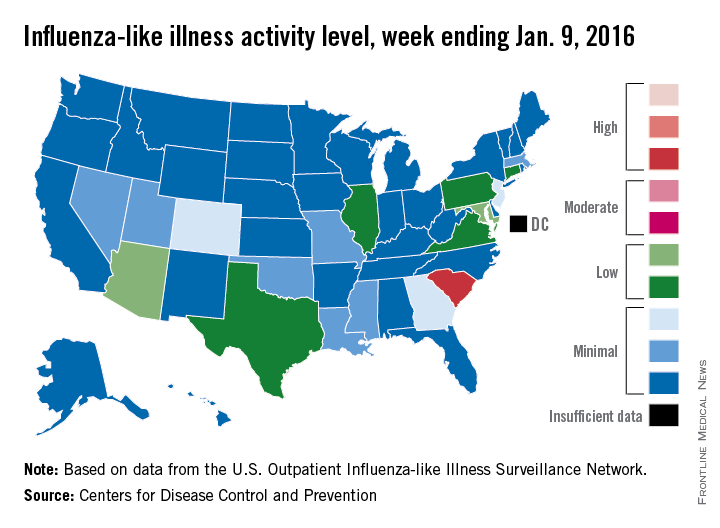
The proportion of outpatient visits for ILI was 2% for week 13, which was down from 2.8% in week 12 and below the national baseline of 2.1%, the CDC said. ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.
One ILI-related pediatric death was reported during week 13, although it actually occurred in December. So far, there have been seven pediatric deaths reported during the 2015-2016 flu season, the CDC report noted.
Since Oct. 1, 2015, there have been 423 laboratory-confirmed influenza-associated hospitalizations reported in the 13 states – including California, New York, and Ohio – of the CDC’s Influenza Hospitalization Surveillance Network, for an overall hospitalization rate of 1.5 per 100,000 population. That rate, however, is “likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications,” the CDC said.