User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Decline in child COVID-19 cases picks up after 2-week slowdown
, according to data gathered by the American Academy of Pediatrics and the Children’s Hospital Association.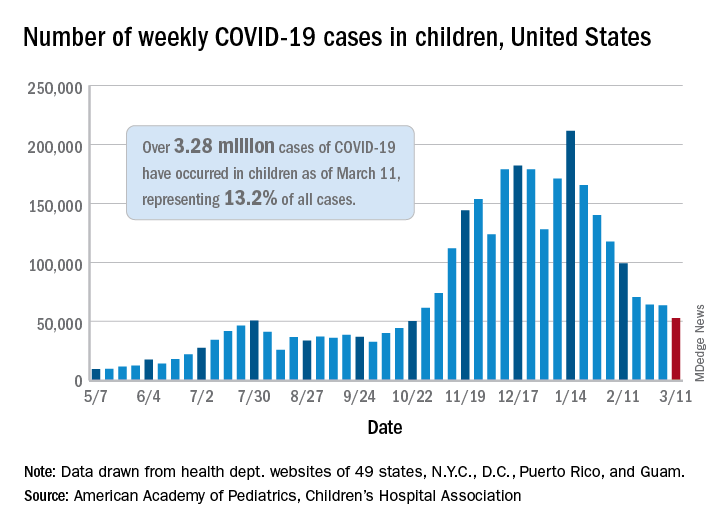
From Feb. 19 to March 4, the drop in new cases averaged just 5% each week, compared with 13.3% per week over the 5-week period from Jan. 15 to Feb. 18. For the week of March 5-11, a total of 52,695 COVID-19 cases were reported in children, down from 63,562 the previous week and the lowest number since late October, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
In those jurisdictions, 3.28 million children have been infected with SARS-CoV-2, representing 13.2% of all cases since the beginning of the pandemic. The cumulative rate of COVID-19 has now risen to 4,364 cases per 100,000 children nationally, with state rates ranging from 1,062 per 100,000 in Hawaii to 8,692 per 100,000 in North Dakota, the AAP and CHA said in their weekly COVID-19 report.
Hospitalization data are more limited – 24 states and New York City – but continue to show that serious illness is much less common in younger individuals: Children represent just 1.9% of all hospitalizations, and only 0.8% of the children who have been infected were hospitalized. Neither rate has changed since early February, the AAP and CHA said.
The number of deaths in children, however, rose from 253 to 266, the largest 1-week increase since early February in the 43 states (along with New York City, Puerto Rico, and Guam) that are tracking mortality data by age, the AAP and CHA reported.
Among those 46 jurisdictions, there are 10 (9 states and the District of Columbia) that have not yet reported a COVID-19–related child death, while Texas has almost twice as many deaths, 47, as the next state, Arizona, which has 24. Meanwhile, California’s total of 452,000 cases is almost 2½ times higher than the 183,000 recorded by Illinois, according to the report.
, according to data gathered by the American Academy of Pediatrics and the Children’s Hospital Association.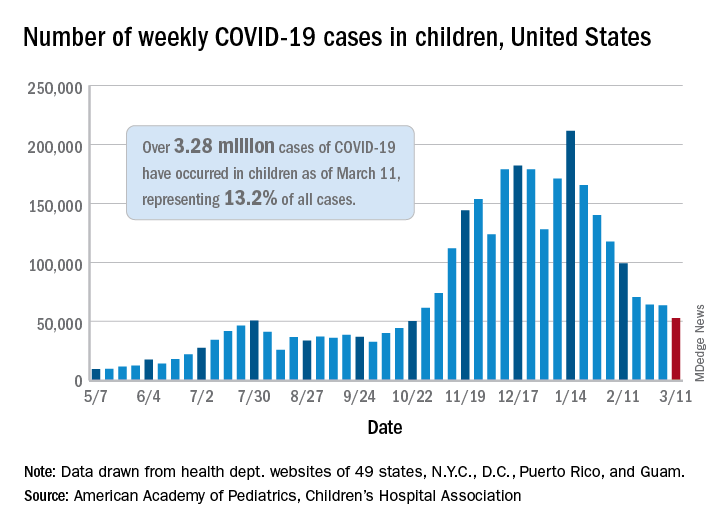
From Feb. 19 to March 4, the drop in new cases averaged just 5% each week, compared with 13.3% per week over the 5-week period from Jan. 15 to Feb. 18. For the week of March 5-11, a total of 52,695 COVID-19 cases were reported in children, down from 63,562 the previous week and the lowest number since late October, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
In those jurisdictions, 3.28 million children have been infected with SARS-CoV-2, representing 13.2% of all cases since the beginning of the pandemic. The cumulative rate of COVID-19 has now risen to 4,364 cases per 100,000 children nationally, with state rates ranging from 1,062 per 100,000 in Hawaii to 8,692 per 100,000 in North Dakota, the AAP and CHA said in their weekly COVID-19 report.
Hospitalization data are more limited – 24 states and New York City – but continue to show that serious illness is much less common in younger individuals: Children represent just 1.9% of all hospitalizations, and only 0.8% of the children who have been infected were hospitalized. Neither rate has changed since early February, the AAP and CHA said.
The number of deaths in children, however, rose from 253 to 266, the largest 1-week increase since early February in the 43 states (along with New York City, Puerto Rico, and Guam) that are tracking mortality data by age, the AAP and CHA reported.
Among those 46 jurisdictions, there are 10 (9 states and the District of Columbia) that have not yet reported a COVID-19–related child death, while Texas has almost twice as many deaths, 47, as the next state, Arizona, which has 24. Meanwhile, California’s total of 452,000 cases is almost 2½ times higher than the 183,000 recorded by Illinois, according to the report.
, according to data gathered by the American Academy of Pediatrics and the Children’s Hospital Association.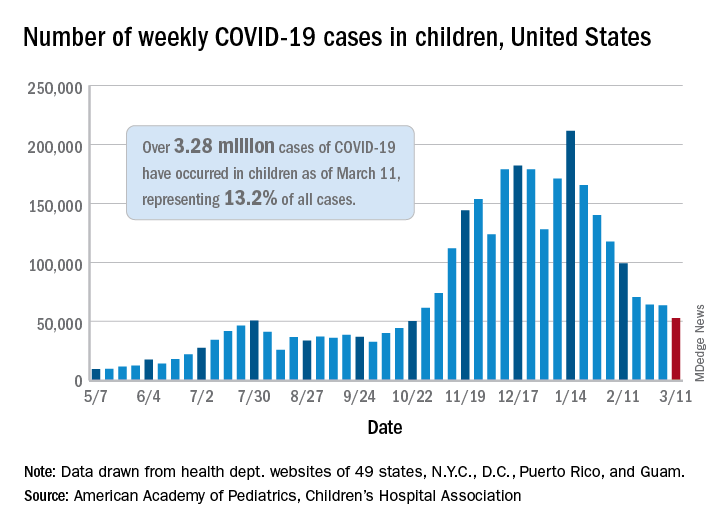
From Feb. 19 to March 4, the drop in new cases averaged just 5% each week, compared with 13.3% per week over the 5-week period from Jan. 15 to Feb. 18. For the week of March 5-11, a total of 52,695 COVID-19 cases were reported in children, down from 63,562 the previous week and the lowest number since late October, based on data from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
In those jurisdictions, 3.28 million children have been infected with SARS-CoV-2, representing 13.2% of all cases since the beginning of the pandemic. The cumulative rate of COVID-19 has now risen to 4,364 cases per 100,000 children nationally, with state rates ranging from 1,062 per 100,000 in Hawaii to 8,692 per 100,000 in North Dakota, the AAP and CHA said in their weekly COVID-19 report.
Hospitalization data are more limited – 24 states and New York City – but continue to show that serious illness is much less common in younger individuals: Children represent just 1.9% of all hospitalizations, and only 0.8% of the children who have been infected were hospitalized. Neither rate has changed since early February, the AAP and CHA said.
The number of deaths in children, however, rose from 253 to 266, the largest 1-week increase since early February in the 43 states (along with New York City, Puerto Rico, and Guam) that are tracking mortality data by age, the AAP and CHA reported.
Among those 46 jurisdictions, there are 10 (9 states and the District of Columbia) that have not yet reported a COVID-19–related child death, while Texas has almost twice as many deaths, 47, as the next state, Arizona, which has 24. Meanwhile, California’s total of 452,000 cases is almost 2½ times higher than the 183,000 recorded by Illinois, according to the report.
First pill for COVID-19 could be ready by year’s end
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
Is pediatric subspecialty training financially worth it?
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Infantile hemangiomas: Accurate diagnosis is crucial
The first rule about infantile hemangiomas: Make sure they’re actually infantile hemangiomas, a pediatric dermatologist urged colleagues. Then watch patients closely, refer to specialists when appropriate, and consider propranolol in complicated or high-risk cases, Andrea L. Zaenglein, MD, said at MedscapeLive’s Women’s & Pediatric Dermatology Seminar.
“In my career as a pediatric dermatologist, propranolol has been a life changer for us more than any other medicine,” said Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, Hershey.
Before the point where propranolol is prescribed, confirm the diagnosis and use the correct terminology, she advised. It’s still appropriate to use the International Society for the Study of Vascular Anomalies (ISSVA) vascular lesion classification system released in 1982. “For most people, it serves the purpose well,” she said. Another option is an updated and more complex classification system from 2015.
Dr. Zaenglein highlighted two studies – one published in 2011 and the other published in 2020 – that revealed high levels of misclassification of vascular malformations in research reports. The earlier study found that 21% of patients with misclassified lesions were mistreated, compared with none of those who were classified using ISSVA terminology.
“I cannot stress [proper classification] enough when you’re dealing with babies and children with vascular lesions. If not sure, be vague. Say ‘a vascular tumor’ or a ‘vascular malformation.’ But only reserve ‘infantile hemangioma’ for that very diagnosis,” she said.
As Dr. Zaenglein noted, infantile hemangiomas affect 5%-10% of 1-year-olds, of whom 20% have multiple lesions. They’re more common in females by a 3-to-1 margin, and also seen more in premature infants, and in cases of multiple births, higher maternal age, and low birth weight.
The pathogenesis of these lesions is unclear, she said, although there are hints about genetic components and tissue hypoxia, among other possible causes. “Importantly, you get 80% of the growth by 3-4 months of age. Then it’ll slow in its growth and kind of slowly go away over time, but it’s not linear regression. It’s more that you get more improvement up front, usually until about 5, and then you can get some continued gradual evolution up until about 7 or 10 years of age.”
Complications can include ulceration, infection and – in rare cases – hemorrhage and high-output cardiac failure, she said. “Knowing which ones are at high risk for complications is important, and also there are systemic associations that we have to be mindful of. We also want to think about aesthetic outcomes as well when we talk about management of infantile hemangiomas.”
High-risk infantile hemangiomas include those with the following features:
- Extensive facial involvement. Dr. Zaenglein highlighted a case of a 2-year-old baby with a large, bulky hemangioma that distorted facial features around the eye. “This would be a medical emergency” requiring immediate evaluation and treatment, she said.
- Periocular involvement. Refer to ophthalmology, she recommended. “Even smaller hemangiomas can cause refractive errors or amblyopia, and oftentimes need to be treated with either systemic or topical therapy depending on the size and extent,” she said.
- PHACE syndrome (Posterior fossa malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, eye abnormalities). “Propranolol has been safely used in PHACE, but every patient is different,” she said. “You need to make sure to do a good risk assessment before starting because if they have narrowed blood flow or limited blood flow, there is a question of whether there is potential risk for stroke if you drop a baby’s blood pressure. Make sure that the vasculature is evaluated before started on propranolol. Also, there are recent reports of risk of long-term risk of stroke with PHACE syndrome as patients are getting into their adulthood.”
- Beard distribution. Be aware of possible airway involvement that can be revealed by biphasic stridor. In those cases, immediate treatment – perhaps even with tracheostomy – is needed to avoid mortality, she said.
- Multiple sites: Patients with five or more hemangiomas may have liver involvement, she said, and should undergo hepatic evaluation. Consider evaluating if this is suspected, even if the number of hemangiomas is under five, she said.
- Perineal/lumbosacral involvement: A third of these cases are associated with spinal dysraphism. Refer to neurosurgery, she recommended.
Dr. Zaenglein highlighted a report on the use of propranolol published in 2008 and noted that clinical practice guidelines for managing infantile hemangiomas published in 2019 are also helpful.
Flat hemangiomas, meanwhile, can benefit from timolol maleate 0.5% solution or gel-forming solution – 1 drop twice daily or 2 drops once daily, she said. This treatment should be avoided in thick hemangiomas, she said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Zaenglein disclosed consulting fees (Dermata, Cassiopea, and Regeneron), and fees for contracted research support (Incyte).
The first rule about infantile hemangiomas: Make sure they’re actually infantile hemangiomas, a pediatric dermatologist urged colleagues. Then watch patients closely, refer to specialists when appropriate, and consider propranolol in complicated or high-risk cases, Andrea L. Zaenglein, MD, said at MedscapeLive’s Women’s & Pediatric Dermatology Seminar.
“In my career as a pediatric dermatologist, propranolol has been a life changer for us more than any other medicine,” said Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, Hershey.
Before the point where propranolol is prescribed, confirm the diagnosis and use the correct terminology, she advised. It’s still appropriate to use the International Society for the Study of Vascular Anomalies (ISSVA) vascular lesion classification system released in 1982. “For most people, it serves the purpose well,” she said. Another option is an updated and more complex classification system from 2015.
Dr. Zaenglein highlighted two studies – one published in 2011 and the other published in 2020 – that revealed high levels of misclassification of vascular malformations in research reports. The earlier study found that 21% of patients with misclassified lesions were mistreated, compared with none of those who were classified using ISSVA terminology.
“I cannot stress [proper classification] enough when you’re dealing with babies and children with vascular lesions. If not sure, be vague. Say ‘a vascular tumor’ or a ‘vascular malformation.’ But only reserve ‘infantile hemangioma’ for that very diagnosis,” she said.
As Dr. Zaenglein noted, infantile hemangiomas affect 5%-10% of 1-year-olds, of whom 20% have multiple lesions. They’re more common in females by a 3-to-1 margin, and also seen more in premature infants, and in cases of multiple births, higher maternal age, and low birth weight.
The pathogenesis of these lesions is unclear, she said, although there are hints about genetic components and tissue hypoxia, among other possible causes. “Importantly, you get 80% of the growth by 3-4 months of age. Then it’ll slow in its growth and kind of slowly go away over time, but it’s not linear regression. It’s more that you get more improvement up front, usually until about 5, and then you can get some continued gradual evolution up until about 7 or 10 years of age.”
Complications can include ulceration, infection and – in rare cases – hemorrhage and high-output cardiac failure, she said. “Knowing which ones are at high risk for complications is important, and also there are systemic associations that we have to be mindful of. We also want to think about aesthetic outcomes as well when we talk about management of infantile hemangiomas.”
High-risk infantile hemangiomas include those with the following features:
- Extensive facial involvement. Dr. Zaenglein highlighted a case of a 2-year-old baby with a large, bulky hemangioma that distorted facial features around the eye. “This would be a medical emergency” requiring immediate evaluation and treatment, she said.
- Periocular involvement. Refer to ophthalmology, she recommended. “Even smaller hemangiomas can cause refractive errors or amblyopia, and oftentimes need to be treated with either systemic or topical therapy depending on the size and extent,” she said.
- PHACE syndrome (Posterior fossa malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, eye abnormalities). “Propranolol has been safely used in PHACE, but every patient is different,” she said. “You need to make sure to do a good risk assessment before starting because if they have narrowed blood flow or limited blood flow, there is a question of whether there is potential risk for stroke if you drop a baby’s blood pressure. Make sure that the vasculature is evaluated before started on propranolol. Also, there are recent reports of risk of long-term risk of stroke with PHACE syndrome as patients are getting into their adulthood.”
- Beard distribution. Be aware of possible airway involvement that can be revealed by biphasic stridor. In those cases, immediate treatment – perhaps even with tracheostomy – is needed to avoid mortality, she said.
- Multiple sites: Patients with five or more hemangiomas may have liver involvement, she said, and should undergo hepatic evaluation. Consider evaluating if this is suspected, even if the number of hemangiomas is under five, she said.
- Perineal/lumbosacral involvement: A third of these cases are associated with spinal dysraphism. Refer to neurosurgery, she recommended.
Dr. Zaenglein highlighted a report on the use of propranolol published in 2008 and noted that clinical practice guidelines for managing infantile hemangiomas published in 2019 are also helpful.
Flat hemangiomas, meanwhile, can benefit from timolol maleate 0.5% solution or gel-forming solution – 1 drop twice daily or 2 drops once daily, she said. This treatment should be avoided in thick hemangiomas, she said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Zaenglein disclosed consulting fees (Dermata, Cassiopea, and Regeneron), and fees for contracted research support (Incyte).
The first rule about infantile hemangiomas: Make sure they’re actually infantile hemangiomas, a pediatric dermatologist urged colleagues. Then watch patients closely, refer to specialists when appropriate, and consider propranolol in complicated or high-risk cases, Andrea L. Zaenglein, MD, said at MedscapeLive’s Women’s & Pediatric Dermatology Seminar.
“In my career as a pediatric dermatologist, propranolol has been a life changer for us more than any other medicine,” said Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, Hershey.
Before the point where propranolol is prescribed, confirm the diagnosis and use the correct terminology, she advised. It’s still appropriate to use the International Society for the Study of Vascular Anomalies (ISSVA) vascular lesion classification system released in 1982. “For most people, it serves the purpose well,” she said. Another option is an updated and more complex classification system from 2015.
Dr. Zaenglein highlighted two studies – one published in 2011 and the other published in 2020 – that revealed high levels of misclassification of vascular malformations in research reports. The earlier study found that 21% of patients with misclassified lesions were mistreated, compared with none of those who were classified using ISSVA terminology.
“I cannot stress [proper classification] enough when you’re dealing with babies and children with vascular lesions. If not sure, be vague. Say ‘a vascular tumor’ or a ‘vascular malformation.’ But only reserve ‘infantile hemangioma’ for that very diagnosis,” she said.
As Dr. Zaenglein noted, infantile hemangiomas affect 5%-10% of 1-year-olds, of whom 20% have multiple lesions. They’re more common in females by a 3-to-1 margin, and also seen more in premature infants, and in cases of multiple births, higher maternal age, and low birth weight.
The pathogenesis of these lesions is unclear, she said, although there are hints about genetic components and tissue hypoxia, among other possible causes. “Importantly, you get 80% of the growth by 3-4 months of age. Then it’ll slow in its growth and kind of slowly go away over time, but it’s not linear regression. It’s more that you get more improvement up front, usually until about 5, and then you can get some continued gradual evolution up until about 7 or 10 years of age.”
Complications can include ulceration, infection and – in rare cases – hemorrhage and high-output cardiac failure, she said. “Knowing which ones are at high risk for complications is important, and also there are systemic associations that we have to be mindful of. We also want to think about aesthetic outcomes as well when we talk about management of infantile hemangiomas.”
High-risk infantile hemangiomas include those with the following features:
- Extensive facial involvement. Dr. Zaenglein highlighted a case of a 2-year-old baby with a large, bulky hemangioma that distorted facial features around the eye. “This would be a medical emergency” requiring immediate evaluation and treatment, she said.
- Periocular involvement. Refer to ophthalmology, she recommended. “Even smaller hemangiomas can cause refractive errors or amblyopia, and oftentimes need to be treated with either systemic or topical therapy depending on the size and extent,” she said.
- PHACE syndrome (Posterior fossa malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, eye abnormalities). “Propranolol has been safely used in PHACE, but every patient is different,” she said. “You need to make sure to do a good risk assessment before starting because if they have narrowed blood flow or limited blood flow, there is a question of whether there is potential risk for stroke if you drop a baby’s blood pressure. Make sure that the vasculature is evaluated before started on propranolol. Also, there are recent reports of risk of long-term risk of stroke with PHACE syndrome as patients are getting into their adulthood.”
- Beard distribution. Be aware of possible airway involvement that can be revealed by biphasic stridor. In those cases, immediate treatment – perhaps even with tracheostomy – is needed to avoid mortality, she said.
- Multiple sites: Patients with five or more hemangiomas may have liver involvement, she said, and should undergo hepatic evaluation. Consider evaluating if this is suspected, even if the number of hemangiomas is under five, she said.
- Perineal/lumbosacral involvement: A third of these cases are associated with spinal dysraphism. Refer to neurosurgery, she recommended.
Dr. Zaenglein highlighted a report on the use of propranolol published in 2008 and noted that clinical practice guidelines for managing infantile hemangiomas published in 2019 are also helpful.
Flat hemangiomas, meanwhile, can benefit from timolol maleate 0.5% solution or gel-forming solution – 1 drop twice daily or 2 drops once daily, she said. This treatment should be avoided in thick hemangiomas, she said.
MedscapeLive and this news organization are owned by the same parent company. Dr. Zaenglein disclosed consulting fees (Dermata, Cassiopea, and Regeneron), and fees for contracted research support (Incyte).
FROM MEDSCAPELIVE WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Helping parents deal with children’s transition to in-person school
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
This spring may bring an unusual transition for families: a return to in-person school after nearly a year in a virtual classroom. This will undoubtedly come as a welcome relief to many parents worried about their children’s education and development and struggling with running school from home. But it is important for parents to remember that transitions, even happy ones, are difficult. You can help parents to anticipate what may be challenging about this transition for their children so that they are all prepared and can diminish struggles and support their children’s mastery.
Be curious about their children’s thoughts and feelings
Parents should adopt a truly curious and open-minded approach with their children. Remind parents that, while they are experts on their own children, they should not assume they know what their children are thinking or feeling about the return to school. Some children, especially ones struggling with learning problems or difficulty with peers, will have grown very comfortable being at home with parents or siblings. Some children, especially pre- and early teens, may have changed substantially in the year and might feel uncertain about returning to a prior team or group of friends. Some children may feel concerned about leaving a pet at home alone. Some children may be going to a new school and be anxious about facing such a big transition without the usual planning and supports. Those on a college track may be worried they are “behind” academically or in college preparation.
Parents can show up when and where their children are most likely to talk, perhaps bath time or bedtime for younger children or in the car together with their adolescents. They can ask: “Have you been thinking about what it might be like to go back to school? Have your friends been chatting about it?” They might be curious together about what might have changed in a year. What might be really great about being back in a classroom? What might they miss about home school? And what might be new? Are you worried about the work, any of your friends, or not being home? If children can begin to anticipate both the good and the difficult, they will be better equipped to face and manage the challenges and appreciate the delights.
Children in elementary school are built to master new situations but are also prone to anxiety about new expectations and demands. Parents can be calmly curious about what their thoughts, feelings, and questions are and look for answers together. Often all they need is to see parents being calm in the face of uncertainty, bearing the strong feelings that may come, and preserving curiosity and compassion. Adolescents may be grieving the things they have missed, or they may have concerns about relationships and practical matters such as the implications for applying to college. Parents can offer compassion and validation and help them to devise their own strategies to face the practical challenges they are concerned about.
Be mindful of their children’s vulnerabilities
While most children will find the transition back to school easier than they may anticipate, there will be some for whom the transition will be very challenging. Children who have been bullied at school may have found themselves able to concentrate and learn free of the fear and stress of a classmate’s taunts or stares. Children with learning disabilities or ADHD have probably struggled with online school, but they have also likely established strategies and supports during the year that have enabled them to get enough individualized help to get their work done. These children are vulnerable to falling behind and getting discouraged when these supports are lost, and possibly not replaced with new ones in the chaos of transition. Parents should reassure their children that they will work with the school to make sure that they can succeed in the classroom as they did at home.
Children with an inhibited or shy temperament might have found that it was easier to focus and listen in the comfortable setting of home than in a busy, stimulating classroom. Children who suffer from anxiety disorders that may make separating from parents or managing the performance and social demands of school extra difficult will find the return to school especially challenging. Some younger children may have experienced the emergence of an anxiety disorder during the past year, and the return to school may mark the challenge that brings heretofore quiet symptoms into full relief.
These children have all enjoyed being able to avoid the discomfort of certain anxiety-provoking situations, and they may be particularly stressed by anticipating a return to school. Younger children may begin to have stomach aches and other physical complaints as the return to school gets close, older children may seem more withdrawn or irritable or begin discussing ways to continue school from home. Parents should help their children try to identify and describe their worries. For anxious children, having a chance to practice may be very helpful. Visiting their school, especially if it is a new school, or having a planned hangout with a friend (with appropriate precautions) is the kind of exposure that can lessen anticipatory anxiety. If this is not enough, parents should not hesitate to bring in other caring, supportive adults, such as school counselors or therapists that may be essential to helping their children face and manage what may be intense anxiety.
Consider routines to support their transition
Just as parents begin to return their children to an earlier bedtime toward the end of summer, it will be helpful to consider how changing certain routines will support their children now. If children will need to get up earlier to be ready for a bus or a team practice, they should start moving bedtime and wake-up time earlier gradually. Uniforms or backpacks that have not been seen for a year should be dug out. Children who are planning a return to a sport may benefit from gradually increasing their exercise or starting training now. This will have the added benefit of improving sleep and energy and fortifying children for the challenges of change. Parents might consider reaching out to other parents in the same class as their children and having a virtual conversation to share their thoughts.
If their family has developed some new “COVID routines” that they have come to enjoy, they should find a way to preserve them. Perhaps they are having dinner together more often or have established a family game night or Netflix night. Help parents consider how to avoid falling back into overscheduling their children and themselves. If they created a time to Zoom with distant or vulnerable loved ones, they might decide to continue this. School may determine some of their routines, but they should also prioritize their family connections and well-being in deciding how to schedule their days.
Find opportunity for mastery and meaning
As parents are listening, validating, and planning with their children, they might use this time to reflect on valuable lessons. They might point out the value of patience: Adjusting to change takes time and happens in fits and starts. It has been 12 months since many of the pandemic changes started and it will take more than a few days to adjust as schools reopen. They might point out how proud they are of what their children have been able to learn, build, or do during this year, what they admire about them. It may be a time to consider what their family may have lost and gained during the past year, what they are eager to leave behind, and what they might like to keep. And it is also a chance for parents to observe that change is an inevitable part of life (especially when growing up). It is always challenging, and often brings loss and sadness. But if we pay attention, there are also the green shoots of what is new and possible.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
COVID-related immunization gaps portend return of preventable infections
Because of significant reduction in delivery of recommended childhood immunization during the pandemic, there is a risk for resurgence of vaccine preventable infections, including measles, pertussis, and polio, which can result in significant morbidity and mortality in children, reported Amy G. Feldman, MD, of Children’s Hospital Colorado, Aurora, and associates.
Will loss of herd immunity lead to vaccine deserts?
When asked to comment, pediatric infectious disease specialist Christopher J. Harrison, MD, said, “My concern is that we may see expansion of what I call ‘vaccine deserts.’ Vaccine deserts occur in underserved communities, areas with pockets of vaccine-hesitant families or among selected groups with difficult access to health care. These vaccine deserts have held a higher density of vulnerables due to low vaccine uptake, often giving rise to outbreaks of vaccine-preventable diseases, e.g., measles, mumps, pertussis. They are usually due to an index case arriving from another vaccine desert (a developing country or a developed country, U.S. or foreign) where the disease is still endemic or pockets of vaccine hesitancy/refusal exist. When detected, local outbreaks result in rapid responses from public/private health collaborations that limit the outbreak. But what if vaccine deserts became more generalized in the U.S. because of loss of vaccine-induced herd immunity in many more or larger areas of our communities because of pandemic-driven lack of vaccinations? That pandemic-driven indirect damage would further stress the health care system and the economy. And it may first show up in the older children whose vaccines were deferred in the first 4-6 months of the pandemic.”
Dr. Feldman and associates cited findings from a collaborative survey conducted by UNICEF, the World Health Organization, Gavi the Vaccine Alliance, the CDC, the Sabin Vaccine Institute, and the Johns Hopkins Bloomberg School of Public Health, which found that immunization programs experienced moderate to severe disruptions or terminations in at least 68 of 129 low and middle-income countries surveyed. According to the WHO, CDC, Red Cross, and GAVI, 94 million people presently are estimated to be at risk as a consequence of not receiving their measles vaccines following the suspensions.
“These national and international declines in routine immunizations have placed the global community at significant risk for outbreaks of vaccine-preventable infections (VPIs) including measles, polio, and pertussis, diseases which are more deadly, more contagious and have a higher reproductive factor (R0) amongst children than COVID-19,” the authors observed.
Dr. Feldman and associates outlined the horrible devastation that these VPI can cause in children, including significantly higher morbidity and mortality than adults, especially among those with immunodeficiencies. Neurologic deficits, paralysis, intellectual disabilities, and vision and hearing loss are just some of the permanent effects conveyed. “It is concerning to imagine how measles could spread across the United States when social distancing restriction[s] are relaxed and unvaccinated children return to school and usual community engagement,” they noted.
Collaborative engagement key to course correction
The authors found that primary care providers and public health communities are working not only to restore vaccine administration but also to restore confidence that vaccine delivery is safe in spite of COVID. In addition to recommending specific risk mitigation strategies for clinicians, they also suggested individual practitioners use electronic health records to identify patients with COVID-related lapses in vaccination, employ electronic health record–based parent notification of overdue immunizations, and offer distance-friendly vaccination options that include parking lot or drive-up window vaccine delivery.
Additionally, Dr. Feldman and colleagues recommended that local, state, regional, and national health systems use public service announcements via television and digital as well as social media platforms to convey important messages about the considerable health risks associated with vaccine avoidance and the availability of free or reduced-cost vaccination programs through the federally funded Vaccines For Children program for parents out of work or without insurance. Equally important is messaging around encouraging vaccine opportunities during all health care visits, whether they be subspecialty, urgent care, emergency room, or inpatient visits. In areas where access to clinics is limited, they urged the use of mobile clinics as well as additional focus on providing medical homes to children with poor access to care.
“A partial but expanding safety net may be developing spontaneously, i.e., practices and clinics based on a patient-centered medical home (PCMH) model,” noted Dr. Harrison, professor of pediatrics, University of Missouri-Kansas City, in an interview. “When lagging vaccinations were reported in mid-2020, we checked with a local hospital–based urban clinic and two suburban private practices modeled on PCMH. Each had noted a drastic drop in well checks in the first months of the pandemic. But with ill visits nearly nonexistent, they doubled down on maintaining health maintenance visits. Even though staff and provider work hours were limited, and families were less enthusiastic about well checks, momentum appears to have grown so that, by later in 2020, vaccine uptake rates were again comparable to 2019. So, some already seem to have answered the call, but practices/clinics remain hampered by months of reduced revenue needed to support staff, providers, PPE supplies, and added infection control needs,” he said.The study was funded by the Agency for Healthcare Research Quality. Dr. Isakov disclosed relationships with various pharmaceutical companies outside the submitted work. The other authors had no relevant disclosures. Dr. Harrison’s institution receives grant funding from GSK, Merck, and Pfizer for pediatric vaccine trials and pneumococcal seroprevalence studies on which he is an investigator.
Because of significant reduction in delivery of recommended childhood immunization during the pandemic, there is a risk for resurgence of vaccine preventable infections, including measles, pertussis, and polio, which can result in significant morbidity and mortality in children, reported Amy G. Feldman, MD, of Children’s Hospital Colorado, Aurora, and associates.
Will loss of herd immunity lead to vaccine deserts?
When asked to comment, pediatric infectious disease specialist Christopher J. Harrison, MD, said, “My concern is that we may see expansion of what I call ‘vaccine deserts.’ Vaccine deserts occur in underserved communities, areas with pockets of vaccine-hesitant families or among selected groups with difficult access to health care. These vaccine deserts have held a higher density of vulnerables due to low vaccine uptake, often giving rise to outbreaks of vaccine-preventable diseases, e.g., measles, mumps, pertussis. They are usually due to an index case arriving from another vaccine desert (a developing country or a developed country, U.S. or foreign) where the disease is still endemic or pockets of vaccine hesitancy/refusal exist. When detected, local outbreaks result in rapid responses from public/private health collaborations that limit the outbreak. But what if vaccine deserts became more generalized in the U.S. because of loss of vaccine-induced herd immunity in many more or larger areas of our communities because of pandemic-driven lack of vaccinations? That pandemic-driven indirect damage would further stress the health care system and the economy. And it may first show up in the older children whose vaccines were deferred in the first 4-6 months of the pandemic.”
Dr. Feldman and associates cited findings from a collaborative survey conducted by UNICEF, the World Health Organization, Gavi the Vaccine Alliance, the CDC, the Sabin Vaccine Institute, and the Johns Hopkins Bloomberg School of Public Health, which found that immunization programs experienced moderate to severe disruptions or terminations in at least 68 of 129 low and middle-income countries surveyed. According to the WHO, CDC, Red Cross, and GAVI, 94 million people presently are estimated to be at risk as a consequence of not receiving their measles vaccines following the suspensions.
“These national and international declines in routine immunizations have placed the global community at significant risk for outbreaks of vaccine-preventable infections (VPIs) including measles, polio, and pertussis, diseases which are more deadly, more contagious and have a higher reproductive factor (R0) amongst children than COVID-19,” the authors observed.
Dr. Feldman and associates outlined the horrible devastation that these VPI can cause in children, including significantly higher morbidity and mortality than adults, especially among those with immunodeficiencies. Neurologic deficits, paralysis, intellectual disabilities, and vision and hearing loss are just some of the permanent effects conveyed. “It is concerning to imagine how measles could spread across the United States when social distancing restriction[s] are relaxed and unvaccinated children return to school and usual community engagement,” they noted.
Collaborative engagement key to course correction
The authors found that primary care providers and public health communities are working not only to restore vaccine administration but also to restore confidence that vaccine delivery is safe in spite of COVID. In addition to recommending specific risk mitigation strategies for clinicians, they also suggested individual practitioners use electronic health records to identify patients with COVID-related lapses in vaccination, employ electronic health record–based parent notification of overdue immunizations, and offer distance-friendly vaccination options that include parking lot or drive-up window vaccine delivery.
Additionally, Dr. Feldman and colleagues recommended that local, state, regional, and national health systems use public service announcements via television and digital as well as social media platforms to convey important messages about the considerable health risks associated with vaccine avoidance and the availability of free or reduced-cost vaccination programs through the federally funded Vaccines For Children program for parents out of work or without insurance. Equally important is messaging around encouraging vaccine opportunities during all health care visits, whether they be subspecialty, urgent care, emergency room, or inpatient visits. In areas where access to clinics is limited, they urged the use of mobile clinics as well as additional focus on providing medical homes to children with poor access to care.
“A partial but expanding safety net may be developing spontaneously, i.e., practices and clinics based on a patient-centered medical home (PCMH) model,” noted Dr. Harrison, professor of pediatrics, University of Missouri-Kansas City, in an interview. “When lagging vaccinations were reported in mid-2020, we checked with a local hospital–based urban clinic and two suburban private practices modeled on PCMH. Each had noted a drastic drop in well checks in the first months of the pandemic. But with ill visits nearly nonexistent, they doubled down on maintaining health maintenance visits. Even though staff and provider work hours were limited, and families were less enthusiastic about well checks, momentum appears to have grown so that, by later in 2020, vaccine uptake rates were again comparable to 2019. So, some already seem to have answered the call, but practices/clinics remain hampered by months of reduced revenue needed to support staff, providers, PPE supplies, and added infection control needs,” he said.The study was funded by the Agency for Healthcare Research Quality. Dr. Isakov disclosed relationships with various pharmaceutical companies outside the submitted work. The other authors had no relevant disclosures. Dr. Harrison’s institution receives grant funding from GSK, Merck, and Pfizer for pediatric vaccine trials and pneumococcal seroprevalence studies on which he is an investigator.
Because of significant reduction in delivery of recommended childhood immunization during the pandemic, there is a risk for resurgence of vaccine preventable infections, including measles, pertussis, and polio, which can result in significant morbidity and mortality in children, reported Amy G. Feldman, MD, of Children’s Hospital Colorado, Aurora, and associates.
Will loss of herd immunity lead to vaccine deserts?
When asked to comment, pediatric infectious disease specialist Christopher J. Harrison, MD, said, “My concern is that we may see expansion of what I call ‘vaccine deserts.’ Vaccine deserts occur in underserved communities, areas with pockets of vaccine-hesitant families or among selected groups with difficult access to health care. These vaccine deserts have held a higher density of vulnerables due to low vaccine uptake, often giving rise to outbreaks of vaccine-preventable diseases, e.g., measles, mumps, pertussis. They are usually due to an index case arriving from another vaccine desert (a developing country or a developed country, U.S. or foreign) where the disease is still endemic or pockets of vaccine hesitancy/refusal exist. When detected, local outbreaks result in rapid responses from public/private health collaborations that limit the outbreak. But what if vaccine deserts became more generalized in the U.S. because of loss of vaccine-induced herd immunity in many more or larger areas of our communities because of pandemic-driven lack of vaccinations? That pandemic-driven indirect damage would further stress the health care system and the economy. And it may first show up in the older children whose vaccines were deferred in the first 4-6 months of the pandemic.”
Dr. Feldman and associates cited findings from a collaborative survey conducted by UNICEF, the World Health Organization, Gavi the Vaccine Alliance, the CDC, the Sabin Vaccine Institute, and the Johns Hopkins Bloomberg School of Public Health, which found that immunization programs experienced moderate to severe disruptions or terminations in at least 68 of 129 low and middle-income countries surveyed. According to the WHO, CDC, Red Cross, and GAVI, 94 million people presently are estimated to be at risk as a consequence of not receiving their measles vaccines following the suspensions.
“These national and international declines in routine immunizations have placed the global community at significant risk for outbreaks of vaccine-preventable infections (VPIs) including measles, polio, and pertussis, diseases which are more deadly, more contagious and have a higher reproductive factor (R0) amongst children than COVID-19,” the authors observed.
Dr. Feldman and associates outlined the horrible devastation that these VPI can cause in children, including significantly higher morbidity and mortality than adults, especially among those with immunodeficiencies. Neurologic deficits, paralysis, intellectual disabilities, and vision and hearing loss are just some of the permanent effects conveyed. “It is concerning to imagine how measles could spread across the United States when social distancing restriction[s] are relaxed and unvaccinated children return to school and usual community engagement,” they noted.
Collaborative engagement key to course correction
The authors found that primary care providers and public health communities are working not only to restore vaccine administration but also to restore confidence that vaccine delivery is safe in spite of COVID. In addition to recommending specific risk mitigation strategies for clinicians, they also suggested individual practitioners use electronic health records to identify patients with COVID-related lapses in vaccination, employ electronic health record–based parent notification of overdue immunizations, and offer distance-friendly vaccination options that include parking lot or drive-up window vaccine delivery.
Additionally, Dr. Feldman and colleagues recommended that local, state, regional, and national health systems use public service announcements via television and digital as well as social media platforms to convey important messages about the considerable health risks associated with vaccine avoidance and the availability of free or reduced-cost vaccination programs through the federally funded Vaccines For Children program for parents out of work or without insurance. Equally important is messaging around encouraging vaccine opportunities during all health care visits, whether they be subspecialty, urgent care, emergency room, or inpatient visits. In areas where access to clinics is limited, they urged the use of mobile clinics as well as additional focus on providing medical homes to children with poor access to care.
“A partial but expanding safety net may be developing spontaneously, i.e., practices and clinics based on a patient-centered medical home (PCMH) model,” noted Dr. Harrison, professor of pediatrics, University of Missouri-Kansas City, in an interview. “When lagging vaccinations were reported in mid-2020, we checked with a local hospital–based urban clinic and two suburban private practices modeled on PCMH. Each had noted a drastic drop in well checks in the first months of the pandemic. But with ill visits nearly nonexistent, they doubled down on maintaining health maintenance visits. Even though staff and provider work hours were limited, and families were less enthusiastic about well checks, momentum appears to have grown so that, by later in 2020, vaccine uptake rates were again comparable to 2019. So, some already seem to have answered the call, but practices/clinics remain hampered by months of reduced revenue needed to support staff, providers, PPE supplies, and added infection control needs,” he said.The study was funded by the Agency for Healthcare Research Quality. Dr. Isakov disclosed relationships with various pharmaceutical companies outside the submitted work. The other authors had no relevant disclosures. Dr. Harrison’s institution receives grant funding from GSK, Merck, and Pfizer for pediatric vaccine trials and pneumococcal seroprevalence studies on which he is an investigator.
FROM CLINICAL INFECTIOUS DISEASES
JAMA editor resigns over controversial podcast
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
The vanguard of HIV care: Don’t forget this screening
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.
In response, clinical care is continually adapting to the dramatically altered natural history of disease.
Today, the cutting edge of clinical care overlaps with primary care. The clinical vanguard addresses the medical vulnerabilities of patients with HIV, seeking to eliminate preventable morbidity and premature death. Among this clinical vanguard is the screening for and prevention of anal cancer. With the increased longevity of people living with HIV and the nearly universal exposure to human papillomavirus (HPV), there is now potential for progression to mucosal cellular dysplasia and eventual malignancy.
We know that prevention is possible because of the example of cervical cancer, the etiology of which is exposure to oncogenic serotypes of HPV (16 and 18 are most common). Screenings for cervical cancer (regular clinical examinations and Pap smears) and treatments to eliminate high-grade dysplasia have decreased the incidence rate by over 50% since the 1970s. Vaccination against HPV has been available since 2006 and offers the prospect of preventing HPV-associated malignancies, including head and neck cancer, in future decades.
However, rates of anal cancer are increasing. The CDC estimates that about 4,700 new cases of HPV-associated anal cancers are diagnosed in women and about 2,300 are diagnosed in men each year in the United States. Anal cancer rates in individuals with HIV have increased in the era of effective antiretrovirals and greater longevity. The highest rates, at 95 per 100,000, are in HIV-positive men who have sex with men. Very similar rates were noted in a more recent study that found increased risk with advancing age and in those with an AIDS diagnosis.
All patients with HIV should be screened
The New York State AIDS Institute Clinical Guidelines Program recommends screening for anal dysplasia in all patients with HIV. A proactive approach similar to cervical cancer screening is appropriate and includes measures easily implemented by all clinicians.
- History: Assess for rectal symptoms, anal pain, discharge, and lumps.
- Physical exam: Assess for presence of perianal lesions; perform a thorough digital rectal exam.
- Anal Pap test for anal cytology: Insert a Dacron swab moistened with tap water about 3 inches into the anal canal, applying pressure to lateral anal walls and rotating the swab. Then remove and place the swab into liquid cytology solution, shake vigorously for a full 30 seconds, and assess for any dysplasia (high-grade squamous intraepithelial lesion, low-grade intraepithelial lesion, atypical squamous cells of undetermined significance), which would warrant further evaluation by high-resolution anoscopy (HRA).
High-resolution anoscopy
HRA for anal dysplasia corresponds to colposcopy for cervical dysplasia. The ability to treat and eliminate high-risk precursor lesions interrupts the progression to malignancy. The efficacy of this strategy is being evaluated in a National Institutes of Health prospective trial called the Anchor Study. The epidemiology of HPV; the clinical horror of witnessing the painful, preventable deaths of young patients with well-controlled HIV caused by anal cancer; and the example of controlling cervical cancer have motivated my practice to assure comprehensive care for our patients.
Unfortunately, establishing HRA in one’s practice is challenging. Barriers to practice include the expense of required equipment and the absence of consensus on specific products. In addition, hands-on precepting to ease newcomers to competence is not generally available. Considerable skill is required for complete visualization of the anal transformative zone in the folds of the anal canal, and recognizing high-risk lesions requires study and accumulated experience. The International Anal Neoplasia Society is a useful resource that also offers a training course. We are invited to train ourselves, and to rely on the eventual feedback of biopsy results and the forbearance of our early patients.
The expanding scope of our medical practices must shift to meet the evolving needs of the growing population of virologically suppressed patients who are living longer. HIV care involves curing life-threatening opportunistic infections, encouraging antiretroviral adherence, and providing comprehensive care – which now includes preventing anal cancer.
A version of this article first appeared on Medscape.com.
Smartphone ‘addiction’ tied to poor sleep in young adults
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smartphone “addiction” may explain poor sleep quality in a significant proportion of young adults, new research suggests.
Investigators found that almost 40% of adults aged 18-30 years who self-reported excessive smartphone use also reported poor sleep.
“Our study provides further support to the growing body of evidence that smartphone addiction has a deleterious impact on sleep,” wrote the researchers.
The study was published online March 2 in Frontiers of Psychiatry.
Not a clinical diagnosis
Smartphone addiction is not formally recognized as a clinical diagnosis, but it’s an “active” area of research, lead investigator Ben Carter, PhD, King’s College London, noted in the report.
In a cross-sectional survey, 1,043 college students (aged 18-30 years, 73% women) completed the 10-question validated Smartphone Addiction Scale Short Version (SAS-SV) and the adapted Pittsburgh Sleep Quality Score Index.
On the SAS-SV, 406 students (38.9%) reported “addiction” to their smartphones. This estimated prevalence is consistent with other reported studies in young adult populations globally, which is in the range of 30%-45%, the researchers noted.
Overall, 61.6% of participants surveyed reported poor sleep; among those who reported smartphone addiction, 68.7% had poor sleep quality, vs. 57.1% of those who did not report smartphone addiction.
In multivariable analysis that adjusted for a variety of relevant factors, among those for whom there was evidence of smartphone addiction, the odds of poor sleep were increased by 41% (adjusted odds ratio [aOR] = 1.41; 95% confidence interval, 1.06-1.87, P = .018).
The findings also suggest that a greater amount of time spent using the phone and greater use late at night can raise the risk for smartphone addiction.
“Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for four or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV,” the researchers wrote.
Caveats, cautions, and concerns
Reached for comment, Paul Weigle, MD, psychiatrist with Hartford HealthCare and Hartford (Conn.) Hospital, and member of the American Academy of Child and Adolescent Psychiatry, said the finding of a relationship between addictive smartphone usage and poor sleep quality is not surprising.
“Great increases in adolescent screen media habits in recent decades have seen a concurrent increase in rates of insomnia among this population,” he said in an interview.
Dr. Weigle also noted that young people who use the phone excessively often do so in bed, “which decreases sleep onset by disrupting conditioning (the tendency for our bodies to relate bed with sleep) and by increasing physiological arousal, which makes it more difficult to fall asleep. The blue light from smartphones used at night disrupts our body’s natural circadian rhythms, confusing our brains regarding whether it is night or day, and further worsens sleep.”
Dr. Weigle said in an interview that some of his patients come to him seeking sleep medications, although the best treatment is to perform a “smartphone-ectomy” every evening.
Teenage patients will “beg, borrow, or steal” to be allowed to keep their phones by the bed with the promise not to use them overnight. Three-quarters of the time, when the parents are able to charge the phone in another room, “the sleep problem resolves,” Dr. Weigle said.
One caveat, he said, is that it’s “somewhat unclear whether this is best classified as an addiction or simply a seriously problematic habit. Either way, this type of habit causes a great deal of distress and dysfunction in the lives of those it affects, so it is important to understand,” he said.
In a statement, Bob Patton, PhD, lecturer in clinical psychology, University of Surrey, Guildford, England, noted that this is a cross-sectional study “and as such cannot lead to any firm conclusions about phone usage as the cause of reduced sleep quality.
“It does, however, provide some compelling evidence,” Dr. Patton said, “that the nature of smartphone usage and its related consequences are important considerations in addressing the emerging phenomenon of ‘smartphone addiction.’ ”
Also weighing in, Andrew Przybylski, PhD, director of research, Oxford (England) Internet Institute, University of Oxford, said by any global health body and is not a psychiatric disorder.
“The study is a correlational analysis of a sample of participants recruited on university campuses and therefore only reflects the experiences of those who had the purpose of the study explained to them. It can say nothing about behaviors in the general population,” Dr. Przybylski said in a statement.
“Readers should be cautious of making any firm conclusions about the impact of smartphone use in the general population, or the idea that they’re addictive in any objective sense, on the basis of this work,” he added. The study had no specific funding. Dr. Carter, Dr. Weigle, Dr. Patton, and Dr. Przybylski have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Delay surgery by 7 weeks after COVID-19 diagnosis, study shows
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.