User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Increased electronic media use and youth suicidality: What can clinicians do?
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Pediatric suicide was an emerging public health crisis prior to COVID-19, and recent data indicate that pediatric suicide attempts continued to increase during the pandemic.1 In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for pediatric mental health because of a surge in youth suicide attempts.2 Isolation mediated by the degradation of community and exacerbated by the pandemic, has been identified as a contributor to increasing pediatric suicidality.
It is impossible to understand this current public health crisis and to seek solutions without recognizing the ways in which the degradation of community and consequent social isolation play a central role. While the degradation of community and the isolation epidemic that preceded COVID-19 have been mediated by multiple factors, one factor associated with mental health problems in youth is electronic media use.3 During COVID-19, when physical distancing and virtual learning have been necessary to curb the spread, electronic media use has increased exponentially in the pediatric demographic. Some of this increase in screen time has been attributable to virtual schooling, but electronic devices also have become the only means by which kids can stay in contact with one another. While electronic communication has been viewed as an antidote to isolation, disturbing consequences associated with electronic media use have also been noted in our pediatric population.
In the health care system where I (P.L.L.) work as a pediatrician and a child and adolescent psychiatrist, electronic media use has been implicated in more than 90% of our inpatient admissions for suicidal ideation. Use of electronic devices has contributed to suicidal thoughts and attempts in most patients admitted to our acute crisis stabilization unit over the past year. During the pandemic, and in the absence of meaningful interpersonal interactions, many in our pediatric population have become even more dependent on electronic devices to cope with isolation. This has created an often-devastating irony, where the very devices already associated with mental health problems in youth are now being endorsed as “necessary” by mental health professionals.
So how does electronic media use relate to isolation and the continued degradation of community, and why might electronic media use be exacerbating pediatric suicide? One way we have coped with the deterioration of our communities has been the creation of the synthetic community-substitutes found on electronic devices. Unfortunately, our electronic devices create only an illusion of community, where interpersonal interaction occurs by way of inanimate objects, and by electronic text and ideograms. These become substitutes for genuine intimacy, personal contact, and reciprocity. Instead of engaging with one another, our youth are spending hours daily in isolation engaging with a piece of plastic. The mirage generated by pixels on a plastic screen creates an illusion of connectivity, but in reality, this only increases the isolation of our youth.
Human evolution and connection
Intimate social connectivity, woven together in our communities, was a fundamental mechanism for human survival. Historically, for our hunter-gatherer ancestors, the community provided access to our fundamental needs, such as safety from predators and access to substantive nutrition.4 Community allowed our ancestors to survive and procreate, and facilitated their triumph over predation and disease.5 Our distinction as the dominant species on Earth has been afforded by our social connectivity. Unfortunately, in the virtual worlds of our electronic devices the intimate social connectivity of community is absent. Our children wander in isolation, left to navigate age-old evolutionary pressures in the absence of the fundamental advantage for our survival as a species.
Unlike the living, breathing bears and wolves that threatened our ancestors, in the virtual world of the electronic device children are stalked by invisible predators seeking sexual or monetary exploitation. Children are being consumed by digital advertising and social media platforms that perpetually reinforce the requirement of perfection, and they fall prey to cyberbullies who mercilessly disparage their imperfections. In their virtual worlds, where their value is predicated upon anonymous others’ opinions, they succumb to the idea that they will never be enough.6 Their fundamental needs of competence and relatedness go unmet, and they lose their sense of purpose, belonging, and often their will to live. More importantly, absent from their children’s virtual worlds, and preoccupied within their own, parents cannot protect their children from online predators, deflect the vicious attacks of cyberbullies, or reframe their children’s imperfections as distinctive or empowering. They are unable to provide their children with the substantive interpersonal contact necessary for resilience and that bolsters their self-worth.
Human beings are inherently social creatures, who regardless of era require community to meet their fundamental needs. As the duration of daily screen time steadily increases, our youth are spending more and more of their waking hours living in isolation in an electronic world. Without the protective social connectivity of community, they are hunted by online predators, and they are consumed by the predatory culture of perfectionism that is contradictory to the reciprocal caretaking necessary to support their healthy development. Evolutionary biology informs us that, when children are isolated, they are susceptible to predation and disease. And in the socialized isolation of their electronic worlds, they are succumbing to predation and to the depressive diseases that are exacerbating the pediatric mental health crisis.
Creating and building community amid a pandemic has been challenging at best. However, now that we have better tools to fight COVID, it is important to encourage our young patients to reduce their nonacademic screen time, and to get outside and engage with others. Their mental health depends on it.
Dr. Loper is a pediatrician and child and adolescent psychiatrist at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. Dr. Loper has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
References
1. MMWR. 2021 Jun 18;70(24):888-94.
2. Ray G. “Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health.” Childrenshospitals.org. 2021 Oct 19.
3. JAMA Netw Open. 2020(8):e2011381.
4. Am J Phys Anthropol. 2018 April:165(4):777-800.
5. The influence of predation on primate and early human evolution: Impetus for cooperation, in “Origins of Altruism and Cooperation. Developments in Primatology: Progress and Prospects.” (Basingstoke, England: Springer Nature, 2011, pp. 19-40).
6. Media Psychology. 2020;23(1):52-78.
Pediatric antibiotic prescriptions plummeted in pandemic
Antibiotic prescribing in pediatric primary care decreased dramatically when the COVID-19 pandemic hit, and new research indicates that drop was sustained through June of 2021.
Lauren Dutcher, MD, with the division of infectious diseases at Hospital of the University of Pennsylvania in Philadelphia, led a study of 27 pediatric primary care practices in the United States. Encounters from Jan. 1, 2018, through June 30, 2021, were included.
Researchers found a 72.7% drop in antibiotic prescriptions when they compared prepandemic April 2019 through December 2019 with the same period in 2020.
Prescriptions remained at the lower levels, primarily driven by reductions in respiratory tract infection (RTI) encounters, and began to rise only in April of 2021, the authors write.
Findings were published online Jan. 11 in Pediatrics.
Researchers report there were 69,327 antibiotic prescriptions from April through December in 2019 and 18,935 antibiotic prescriptions during the same months in 2020.
“The reduction in prescriptions at visits for respiratory tract infection (RTI) accounted for 87.3% of this decrease,” the authors write.
Both prescribing and acute non–COVID-19 respiratory tract infection diagnoses decreased.
Researchers conclude reductions in viral RTI transmission likely played a large role in reduced RTI pediatric visits and antibiotic prescriptions.
Dr. Dutcher told this publication the reduction was likely caused by a combination of less viral transmission of respiratory infections, helped in part by masking and distancing, but also avoidance of health care in the pandemic.
She said the data reinforce the need for appropriate prescribing.
“Antibiotic prescribing is really heavily driven by respiratory infections so this should continue to clue providers in on how frequently that can be unnecessary,“ she said.
Dr. Dutcher said there was probably a reduction in secondary bacterial infections as well as the viral infections.
The research is more comprehensive than some other previous studies, the authors write.
“Although other studies demonstrated early reductions in RTIs and antibiotic prescribing during the COVID-19 pandemic, to our knowledge, this is the first study to demonstrate a sustained decrease in antibiotic prescribing in pediatric primary care throughout 2020 and early 2021,” they write.
The findings also suggest benefits of preventive measures during the pandemic, the authors say.
“Our data suggest that reducing community viral RTI transmission through social distancing and masking corresponds with a reduction in antibiotic prescribing,” they write.
Kao-Ping Chua, MD, a pediatrician and an assistant professor of pediatrics at the University of Michigan in Ann Arbor, said the reductions indicate one of two things is happening: either children aren’t getting sick as often during the pandemic or they are getting sick, but not coming in.
But if they were sick and not coming in, the expectation would be that they would show up in large numbers in emergency departments from untreated infections, he said.
“We just haven’t seen that,” he said.
He said one of the main points the authors make is that masks, distancing, and hand washing may be keeping kids from diseases beyond COVID-19.
He said longer-term data will be needed to show if the trend highlighted in this paper lasts, given children have now returned to school and pediatricians started to see lots of respiratory syncytial virus (RSV) cases this summer.
Anecdotally, he said, he has been prescribing more antibiotics of late for presentations such as ear infections.
Dr. Dutcher said that, though her team doesn’t have data yet since the end of the study period, she agreed that anecdotally it is likely that the prescriptions have been on the rise since June.
Dr. Chua said the reduction in visits also reduces the chance that a physician will be tempted to give in to families’ demands to prescribe an antibiotic.
“Every visit for a sick child represents an opportunity to inappropriately prescribe antibiotics,” Dr. Chua said. Dr. Chua’s own research has found that up to one-quarter of pediatric and adult antibiotic prescriptions are unnecessary.
This work was supported by a Centers for Disease Control and Prevention cooperative agreement, Epicenters for the Prevention of Healthcare Associated Infections. Dr. Dutcher and Dr. Chua had no relevant financial disclosures.
This article was updated 1/11/22.
Antibiotic prescribing in pediatric primary care decreased dramatically when the COVID-19 pandemic hit, and new research indicates that drop was sustained through June of 2021.
Lauren Dutcher, MD, with the division of infectious diseases at Hospital of the University of Pennsylvania in Philadelphia, led a study of 27 pediatric primary care practices in the United States. Encounters from Jan. 1, 2018, through June 30, 2021, were included.
Researchers found a 72.7% drop in antibiotic prescriptions when they compared prepandemic April 2019 through December 2019 with the same period in 2020.
Prescriptions remained at the lower levels, primarily driven by reductions in respiratory tract infection (RTI) encounters, and began to rise only in April of 2021, the authors write.
Findings were published online Jan. 11 in Pediatrics.
Researchers report there were 69,327 antibiotic prescriptions from April through December in 2019 and 18,935 antibiotic prescriptions during the same months in 2020.
“The reduction in prescriptions at visits for respiratory tract infection (RTI) accounted for 87.3% of this decrease,” the authors write.
Both prescribing and acute non–COVID-19 respiratory tract infection diagnoses decreased.
Researchers conclude reductions in viral RTI transmission likely played a large role in reduced RTI pediatric visits and antibiotic prescriptions.
Dr. Dutcher told this publication the reduction was likely caused by a combination of less viral transmission of respiratory infections, helped in part by masking and distancing, but also avoidance of health care in the pandemic.
She said the data reinforce the need for appropriate prescribing.
“Antibiotic prescribing is really heavily driven by respiratory infections so this should continue to clue providers in on how frequently that can be unnecessary,“ she said.
Dr. Dutcher said there was probably a reduction in secondary bacterial infections as well as the viral infections.
The research is more comprehensive than some other previous studies, the authors write.
“Although other studies demonstrated early reductions in RTIs and antibiotic prescribing during the COVID-19 pandemic, to our knowledge, this is the first study to demonstrate a sustained decrease in antibiotic prescribing in pediatric primary care throughout 2020 and early 2021,” they write.
The findings also suggest benefits of preventive measures during the pandemic, the authors say.
“Our data suggest that reducing community viral RTI transmission through social distancing and masking corresponds with a reduction in antibiotic prescribing,” they write.
Kao-Ping Chua, MD, a pediatrician and an assistant professor of pediatrics at the University of Michigan in Ann Arbor, said the reductions indicate one of two things is happening: either children aren’t getting sick as often during the pandemic or they are getting sick, but not coming in.
But if they were sick and not coming in, the expectation would be that they would show up in large numbers in emergency departments from untreated infections, he said.
“We just haven’t seen that,” he said.
He said one of the main points the authors make is that masks, distancing, and hand washing may be keeping kids from diseases beyond COVID-19.
He said longer-term data will be needed to show if the trend highlighted in this paper lasts, given children have now returned to school and pediatricians started to see lots of respiratory syncytial virus (RSV) cases this summer.
Anecdotally, he said, he has been prescribing more antibiotics of late for presentations such as ear infections.
Dr. Dutcher said that, though her team doesn’t have data yet since the end of the study period, she agreed that anecdotally it is likely that the prescriptions have been on the rise since June.
Dr. Chua said the reduction in visits also reduces the chance that a physician will be tempted to give in to families’ demands to prescribe an antibiotic.
“Every visit for a sick child represents an opportunity to inappropriately prescribe antibiotics,” Dr. Chua said. Dr. Chua’s own research has found that up to one-quarter of pediatric and adult antibiotic prescriptions are unnecessary.
This work was supported by a Centers for Disease Control and Prevention cooperative agreement, Epicenters for the Prevention of Healthcare Associated Infections. Dr. Dutcher and Dr. Chua had no relevant financial disclosures.
This article was updated 1/11/22.
Antibiotic prescribing in pediatric primary care decreased dramatically when the COVID-19 pandemic hit, and new research indicates that drop was sustained through June of 2021.
Lauren Dutcher, MD, with the division of infectious diseases at Hospital of the University of Pennsylvania in Philadelphia, led a study of 27 pediatric primary care practices in the United States. Encounters from Jan. 1, 2018, through June 30, 2021, were included.
Researchers found a 72.7% drop in antibiotic prescriptions when they compared prepandemic April 2019 through December 2019 with the same period in 2020.
Prescriptions remained at the lower levels, primarily driven by reductions in respiratory tract infection (RTI) encounters, and began to rise only in April of 2021, the authors write.
Findings were published online Jan. 11 in Pediatrics.
Researchers report there were 69,327 antibiotic prescriptions from April through December in 2019 and 18,935 antibiotic prescriptions during the same months in 2020.
“The reduction in prescriptions at visits for respiratory tract infection (RTI) accounted for 87.3% of this decrease,” the authors write.
Both prescribing and acute non–COVID-19 respiratory tract infection diagnoses decreased.
Researchers conclude reductions in viral RTI transmission likely played a large role in reduced RTI pediatric visits and antibiotic prescriptions.
Dr. Dutcher told this publication the reduction was likely caused by a combination of less viral transmission of respiratory infections, helped in part by masking and distancing, but also avoidance of health care in the pandemic.
She said the data reinforce the need for appropriate prescribing.
“Antibiotic prescribing is really heavily driven by respiratory infections so this should continue to clue providers in on how frequently that can be unnecessary,“ she said.
Dr. Dutcher said there was probably a reduction in secondary bacterial infections as well as the viral infections.
The research is more comprehensive than some other previous studies, the authors write.
“Although other studies demonstrated early reductions in RTIs and antibiotic prescribing during the COVID-19 pandemic, to our knowledge, this is the first study to demonstrate a sustained decrease in antibiotic prescribing in pediatric primary care throughout 2020 and early 2021,” they write.
The findings also suggest benefits of preventive measures during the pandemic, the authors say.
“Our data suggest that reducing community viral RTI transmission through social distancing and masking corresponds with a reduction in antibiotic prescribing,” they write.
Kao-Ping Chua, MD, a pediatrician and an assistant professor of pediatrics at the University of Michigan in Ann Arbor, said the reductions indicate one of two things is happening: either children aren’t getting sick as often during the pandemic or they are getting sick, but not coming in.
But if they were sick and not coming in, the expectation would be that they would show up in large numbers in emergency departments from untreated infections, he said.
“We just haven’t seen that,” he said.
He said one of the main points the authors make is that masks, distancing, and hand washing may be keeping kids from diseases beyond COVID-19.
He said longer-term data will be needed to show if the trend highlighted in this paper lasts, given children have now returned to school and pediatricians started to see lots of respiratory syncytial virus (RSV) cases this summer.
Anecdotally, he said, he has been prescribing more antibiotics of late for presentations such as ear infections.
Dr. Dutcher said that, though her team doesn’t have data yet since the end of the study period, she agreed that anecdotally it is likely that the prescriptions have been on the rise since June.
Dr. Chua said the reduction in visits also reduces the chance that a physician will be tempted to give in to families’ demands to prescribe an antibiotic.
“Every visit for a sick child represents an opportunity to inappropriately prescribe antibiotics,” Dr. Chua said. Dr. Chua’s own research has found that up to one-quarter of pediatric and adult antibiotic prescriptions are unnecessary.
This work was supported by a Centers for Disease Control and Prevention cooperative agreement, Epicenters for the Prevention of Healthcare Associated Infections. Dr. Dutcher and Dr. Chua had no relevant financial disclosures.
This article was updated 1/11/22.
FROM PEDIATRICS
COVID-vaccine myocarditis: Rare, mild, and usually in young men
The risk of myocarditis after immunization with mRNA-based vaccines against SARS-CoV-2 raised concerns when it came to light in early 2021. But as report after report showed such cases to be rare and usually mild and self-limited, focus has turned to the “how and why.”
The mechanism linking the BNT162b2 (Pfizer-BioNTech) and especially mRNA-1273 (Moderna) vaccines to the occurrence of myocarditis is unclear for now, but one potential driver may be tied to a peculiarity that became apparent early: It occurs overwhelmingly in younger males, from 16 to perhaps 40 or 50 years of age. Excess risk has not been consistently seen among women, girls, and older men.
That observation has led to speculation that higher testosterone levels in adolescent boys and young men may somehow promote the adverse vaccine effect, whereas greater levels of estrogen among girls and women in the same age range may be cardioprotective.
Unlikely, brief, and ‘benign’
“Most of the myocarditis is benign, by which I mean that maybe the patients are admitted due to chest pain, but without reduction in ventricular function,” Enrico Ammirati, MD, PhD, a myocarditis expert at De Gasperis Cardio Center and Transplant Center, Niguarda Hospital, Milan, said in an interview.
In a Nov. 14 address on this topic at the annual scientific sessions of the American Heart Association, Dror Mevorach, MD, described the typical case presentation as “mild” and one that clears in fairly short order based on resolution of “clinical symptoms, inflammatory markers and troponin decline, EKG normalization, echo normalization, and a relatively short length of hospital stay.”
Dr. Mevorach, of Hadassah Hebrew University Medical Center, Jerusalem, subsequently published the findings in a report in the New England Journal of Medicine that described 136 confirmed myocarditis cases among more than 5 million people in Israel immunized with the Pfizer-BioNTech vaccine. Myocarditis was considered “mild” in 129 cases, or 95%.
And the risk is tiny, compared with myocarditis from infection by SARS-CoV-2, not to mention the possibility of nasty clinical COVID-19 complications such as pneumonia and pulmonary embolism, Dr. Mevorach observed.
Many other reports agree that the incidence is minimal, especially given the rewards of vaccination. In a separate NEJM publication in September 2021 – from Noam Barda, MD, Clalit (Israel) Research Institute, and colleagues on 1.7 million people in that country, about half unvaccinated and half given the Pfizer-BioNTech vaccine – there were an estimated 2.7 cases of myocarditis per 100,000 vaccinated persons. There were also 11 cases of myocarditis per 100,000 persons who were positive for SARS-CoV-2 infection.
And in a recent case series of vaccinated people aged 16 or older, the myocarditis rate after a first or second Pfizer-BioNTech or Moderna injection was estimated at 1 or fewer per 100,000. The corresponding estimate was 4 such cases per 100,000 after a positive SARS-CoV-2 test among the same population, notes a report published Dec.14, 2021, in Nature Medicine.
In general, “the risk of any kind of cardiac injury is vastly lower with a vaccine than it is with the actual viral infection,” Leslie T. Cooper Jr., MD, a myocarditis expert and clinical trialist at the Mayo Clinic, Jacksonville, Fla., said in an interview. With the mRNA-based vaccines, “we do not have any conceivable danger signal that would outweigh the benefit of vaccination.”
Males of a certain age
Evidence that such myocarditis predominates in young adult men and adolescent boys, especially following a second vaccine dose, is remarkably consistent.
The risk was elevated only among mRNA-based vaccine recipients who were younger than 40 in the recent Nature Medicine analysis. Among that group, estimates after a second dose numbered fewer than 1 case per 100,000 for Pfizer-BioNTech and 1.5 per 100,000 for Moderna.
In a third analysis from Israel – also in NEJM, from Guy Witberg, MD, Rabin Medical Center, Petah Tikva, and colleagues, based on 2.5 million people aged 16 and older with at least one Pfizer-BioNTech injection – 2.1 cases per 100,000 were estimated overall, but the number rose to 10.7 per 100,000 among those aged 16-29 years.
In Dr. Mevorach’s NEJM report, estimates after a second Pfizer-BioNTech vaccine dose were 1 per 26,000 males versus 1 in 218,000 females, compared with 1 myocarditis case in 10,857 persons among “the general unvaccinated population.”
Most recipients of a first vaccine dose were younger than 50, and 16- to 29-year-olds accounted for most who completed two doses, noted Dr. Mevorach. Younger males bore the brunt of any myocarditis: the estimated prevalence after a second dose among males aged 16-19 was 1 per 6,637, compared with 1 per 99,853 females in the same age range, the group reported.
In the BMJ report, based on about 5 million people 12 years of age or older in Denmark, the estimated rates of myocarditis or pericarditis associated with Moderna immunization were 2 per 100,000 among women but 6.3 per 100,000 for men. The incidence and sex difference was much lower among those getting the Pfizer-BioNTech vaccine: 1.3 per 100,000 and 1.5 per 100,000 in women and men, respectively.
Sex hormones may be key
The predominance of vaccine-associated myocarditis among adolescent and young adult males is probably more about the myocarditis itself than the vaccines, observed Biykem Bozkurt, MD, PhD, who has been studying COVID-related myocarditis at Baylor College of Medicine, Houston.
Male sex historically is associated in both epidemiologic studies and experimental models with a greater propensity for most any form of myocarditis, Dr. Bozkurt said in an interview. Given that males aged 16-19 or so appear to be at highest risk of myocarditis as a complication of SARS-CoV-2 vaccination, the mechanism may well be related to sex hormones.
“Therefore, testosterone is implicated as a player in their higher risk of inflammation and injury and lack of adaptive response in terms of healing, and in terms of prevention of injury,” Dr. Bozkurt said. For its part, estrogen inhibits proinflammatory processes and, in particular, “blunts cell-mediated immune responses.”
“We don’t know the mechanism, but a theory that attributes a protective role to estrogen, or a risk associated with testosterone, is reasonable. It makes sense, at least based on epidemiological data,” Dr. Ammirati agreed. Still, “we do not have any direct evidence in human beings.”
Sex-associated differences in experimental myocarditis have been reported in the journals for at least 70 years, but “the testosterone literature and the estrogen literature have not been evaluated in detail in vaccine-associated myocarditis,” Dr. Cooper said.
Most myocarditis in the laboratory is viral, Dr. Cooper observed, and “the links between testosterone, viruses, and inflammation have been pretty well worked out, I would say, if you’re a mouse. If you’re a human, I think it’s still a bit uncertain.”
Were it to apply in humans, greater testosterone levels might independently promote myocarditis, “and if estrogen is cardioprotective, it would be another mechanism,” Dr. Cooper said. “That would translate to slight male predominance in most kinds of myocarditis.”
In males, compared with females, “the heart can be more vulnerable to events such as arrhythmias or to immune-mediated phenomena. So, probably there is also higher vulnerability to myocarditis in men,” Dr. Ammirati noted.
Male predominance in vaccine-related myocarditis is provocative, so it’s worth considering whether testosterone is part of the mechanism as well as the possibility of estrogen cardioprotection, Dr. Ammirati said. But given limitations of the animal models, “we don’t really have robust data to support any part of that.”
Although myocarditis is in some way immune mediated, “and hormones can modulate the response,” the mechanism has to be more than just sex hormones, he said. “They probably cannot explain the specificity for the heart. It’s not a systemic response, it’s an organ-specific response.”
Modulation of immune responses
Details about the immune processes underlying mRNA-vaccine myocarditis, hormone modulated or not, have been elusive. The complication doesn’t resemble serum sickness, nor does it seem to be a reaction to infection by other cardiotropic viruses, such as coxsackie virus B, a cause of viral myocarditis, Dr. Bozkurt said. The latter had been a compelling possibility because such hypersensitivity to smallpox vaccination is well recognized.
“We don’t know the mechanism, that’s the short answer. But there are many hypotheses,” she said. One candidate widely proposed in the literature: autoantibodies driven by molecular mimicry between the SARS-CoV-2 spike protein targeted by the mRNA vaccines and a structurally similar myocardial protein, possibly alpha-myosin, noted Dr. Bozkurt and colleagues in a recent publication.
But elevations in specific “antiheart antibodies” have not been documented in recipients of the two mRNA-based vaccines, said Dr. Cooper. “So, I would say that – although molecular mimicry is a well-established mechanism of, for example, rheumatic carditis after a streptococcal A infection – that has not been demonstrated yet for COVID-19 mRNA vaccination–related myocarditis.”
“We probably won’t know, ever, with a huge level of certainty, the exact mechanisms,” Dr. Cooper added. There is no animal model for vaccine-induced myocarditis, and “We’re still talking very, very small numbers of patients. The vast majority of them recover,” and so don’t generally provide mechanistic clues.
Prospects for younger children
Vaccination against SARS-CoV-2 has now been authorized by the Centers for Disease Control and Prevention for kids as young as 5-11 years, using the Pfizer-BioNTech vaccine. Experience so far suggests the immunization is safe in that age group with negligible risk of myocarditis or other complications. But with prospects of possible authorization in children younger than 5, should myocarditis be a concern for them?
Probably not, if the complication is driven primarily by sex hormones, Dr. Cooper proposed. “One would predict that before puberty you would have a lower – much, much lower – rate of myocarditis in males than you would in the 16- to 19-year-old range, and that it would be roughly equal to females.” Dr. Ammirati and Dr. Bozkurt largely agreed.
It remains to be seen whether the vaccine-related myocarditis risk applies to children younger than 12, “but I doubt it. I think it’s going to be puberty-related,” Dr. Bozkurt said. Still, “I don’t want to hypothesize without data.”
A version of this article first appeared on Medscape.com.
The risk of myocarditis after immunization with mRNA-based vaccines against SARS-CoV-2 raised concerns when it came to light in early 2021. But as report after report showed such cases to be rare and usually mild and self-limited, focus has turned to the “how and why.”
The mechanism linking the BNT162b2 (Pfizer-BioNTech) and especially mRNA-1273 (Moderna) vaccines to the occurrence of myocarditis is unclear for now, but one potential driver may be tied to a peculiarity that became apparent early: It occurs overwhelmingly in younger males, from 16 to perhaps 40 or 50 years of age. Excess risk has not been consistently seen among women, girls, and older men.
That observation has led to speculation that higher testosterone levels in adolescent boys and young men may somehow promote the adverse vaccine effect, whereas greater levels of estrogen among girls and women in the same age range may be cardioprotective.
Unlikely, brief, and ‘benign’
“Most of the myocarditis is benign, by which I mean that maybe the patients are admitted due to chest pain, but without reduction in ventricular function,” Enrico Ammirati, MD, PhD, a myocarditis expert at De Gasperis Cardio Center and Transplant Center, Niguarda Hospital, Milan, said in an interview.
In a Nov. 14 address on this topic at the annual scientific sessions of the American Heart Association, Dror Mevorach, MD, described the typical case presentation as “mild” and one that clears in fairly short order based on resolution of “clinical symptoms, inflammatory markers and troponin decline, EKG normalization, echo normalization, and a relatively short length of hospital stay.”
Dr. Mevorach, of Hadassah Hebrew University Medical Center, Jerusalem, subsequently published the findings in a report in the New England Journal of Medicine that described 136 confirmed myocarditis cases among more than 5 million people in Israel immunized with the Pfizer-BioNTech vaccine. Myocarditis was considered “mild” in 129 cases, or 95%.
And the risk is tiny, compared with myocarditis from infection by SARS-CoV-2, not to mention the possibility of nasty clinical COVID-19 complications such as pneumonia and pulmonary embolism, Dr. Mevorach observed.
Many other reports agree that the incidence is minimal, especially given the rewards of vaccination. In a separate NEJM publication in September 2021 – from Noam Barda, MD, Clalit (Israel) Research Institute, and colleagues on 1.7 million people in that country, about half unvaccinated and half given the Pfizer-BioNTech vaccine – there were an estimated 2.7 cases of myocarditis per 100,000 vaccinated persons. There were also 11 cases of myocarditis per 100,000 persons who were positive for SARS-CoV-2 infection.
And in a recent case series of vaccinated people aged 16 or older, the myocarditis rate after a first or second Pfizer-BioNTech or Moderna injection was estimated at 1 or fewer per 100,000. The corresponding estimate was 4 such cases per 100,000 after a positive SARS-CoV-2 test among the same population, notes a report published Dec.14, 2021, in Nature Medicine.
In general, “the risk of any kind of cardiac injury is vastly lower with a vaccine than it is with the actual viral infection,” Leslie T. Cooper Jr., MD, a myocarditis expert and clinical trialist at the Mayo Clinic, Jacksonville, Fla., said in an interview. With the mRNA-based vaccines, “we do not have any conceivable danger signal that would outweigh the benefit of vaccination.”
Males of a certain age
Evidence that such myocarditis predominates in young adult men and adolescent boys, especially following a second vaccine dose, is remarkably consistent.
The risk was elevated only among mRNA-based vaccine recipients who were younger than 40 in the recent Nature Medicine analysis. Among that group, estimates after a second dose numbered fewer than 1 case per 100,000 for Pfizer-BioNTech and 1.5 per 100,000 for Moderna.
In a third analysis from Israel – also in NEJM, from Guy Witberg, MD, Rabin Medical Center, Petah Tikva, and colleagues, based on 2.5 million people aged 16 and older with at least one Pfizer-BioNTech injection – 2.1 cases per 100,000 were estimated overall, but the number rose to 10.7 per 100,000 among those aged 16-29 years.
In Dr. Mevorach’s NEJM report, estimates after a second Pfizer-BioNTech vaccine dose were 1 per 26,000 males versus 1 in 218,000 females, compared with 1 myocarditis case in 10,857 persons among “the general unvaccinated population.”
Most recipients of a first vaccine dose were younger than 50, and 16- to 29-year-olds accounted for most who completed two doses, noted Dr. Mevorach. Younger males bore the brunt of any myocarditis: the estimated prevalence after a second dose among males aged 16-19 was 1 per 6,637, compared with 1 per 99,853 females in the same age range, the group reported.
In the BMJ report, based on about 5 million people 12 years of age or older in Denmark, the estimated rates of myocarditis or pericarditis associated with Moderna immunization were 2 per 100,000 among women but 6.3 per 100,000 for men. The incidence and sex difference was much lower among those getting the Pfizer-BioNTech vaccine: 1.3 per 100,000 and 1.5 per 100,000 in women and men, respectively.
Sex hormones may be key
The predominance of vaccine-associated myocarditis among adolescent and young adult males is probably more about the myocarditis itself than the vaccines, observed Biykem Bozkurt, MD, PhD, who has been studying COVID-related myocarditis at Baylor College of Medicine, Houston.
Male sex historically is associated in both epidemiologic studies and experimental models with a greater propensity for most any form of myocarditis, Dr. Bozkurt said in an interview. Given that males aged 16-19 or so appear to be at highest risk of myocarditis as a complication of SARS-CoV-2 vaccination, the mechanism may well be related to sex hormones.
“Therefore, testosterone is implicated as a player in their higher risk of inflammation and injury and lack of adaptive response in terms of healing, and in terms of prevention of injury,” Dr. Bozkurt said. For its part, estrogen inhibits proinflammatory processes and, in particular, “blunts cell-mediated immune responses.”
“We don’t know the mechanism, but a theory that attributes a protective role to estrogen, or a risk associated with testosterone, is reasonable. It makes sense, at least based on epidemiological data,” Dr. Ammirati agreed. Still, “we do not have any direct evidence in human beings.”
Sex-associated differences in experimental myocarditis have been reported in the journals for at least 70 years, but “the testosterone literature and the estrogen literature have not been evaluated in detail in vaccine-associated myocarditis,” Dr. Cooper said.
Most myocarditis in the laboratory is viral, Dr. Cooper observed, and “the links between testosterone, viruses, and inflammation have been pretty well worked out, I would say, if you’re a mouse. If you’re a human, I think it’s still a bit uncertain.”
Were it to apply in humans, greater testosterone levels might independently promote myocarditis, “and if estrogen is cardioprotective, it would be another mechanism,” Dr. Cooper said. “That would translate to slight male predominance in most kinds of myocarditis.”
In males, compared with females, “the heart can be more vulnerable to events such as arrhythmias or to immune-mediated phenomena. So, probably there is also higher vulnerability to myocarditis in men,” Dr. Ammirati noted.
Male predominance in vaccine-related myocarditis is provocative, so it’s worth considering whether testosterone is part of the mechanism as well as the possibility of estrogen cardioprotection, Dr. Ammirati said. But given limitations of the animal models, “we don’t really have robust data to support any part of that.”
Although myocarditis is in some way immune mediated, “and hormones can modulate the response,” the mechanism has to be more than just sex hormones, he said. “They probably cannot explain the specificity for the heart. It’s not a systemic response, it’s an organ-specific response.”
Modulation of immune responses
Details about the immune processes underlying mRNA-vaccine myocarditis, hormone modulated or not, have been elusive. The complication doesn’t resemble serum sickness, nor does it seem to be a reaction to infection by other cardiotropic viruses, such as coxsackie virus B, a cause of viral myocarditis, Dr. Bozkurt said. The latter had been a compelling possibility because such hypersensitivity to smallpox vaccination is well recognized.
“We don’t know the mechanism, that’s the short answer. But there are many hypotheses,” she said. One candidate widely proposed in the literature: autoantibodies driven by molecular mimicry between the SARS-CoV-2 spike protein targeted by the mRNA vaccines and a structurally similar myocardial protein, possibly alpha-myosin, noted Dr. Bozkurt and colleagues in a recent publication.
But elevations in specific “antiheart antibodies” have not been documented in recipients of the two mRNA-based vaccines, said Dr. Cooper. “So, I would say that – although molecular mimicry is a well-established mechanism of, for example, rheumatic carditis after a streptococcal A infection – that has not been demonstrated yet for COVID-19 mRNA vaccination–related myocarditis.”
“We probably won’t know, ever, with a huge level of certainty, the exact mechanisms,” Dr. Cooper added. There is no animal model for vaccine-induced myocarditis, and “We’re still talking very, very small numbers of patients. The vast majority of them recover,” and so don’t generally provide mechanistic clues.
Prospects for younger children
Vaccination against SARS-CoV-2 has now been authorized by the Centers for Disease Control and Prevention for kids as young as 5-11 years, using the Pfizer-BioNTech vaccine. Experience so far suggests the immunization is safe in that age group with negligible risk of myocarditis or other complications. But with prospects of possible authorization in children younger than 5, should myocarditis be a concern for them?
Probably not, if the complication is driven primarily by sex hormones, Dr. Cooper proposed. “One would predict that before puberty you would have a lower – much, much lower – rate of myocarditis in males than you would in the 16- to 19-year-old range, and that it would be roughly equal to females.” Dr. Ammirati and Dr. Bozkurt largely agreed.
It remains to be seen whether the vaccine-related myocarditis risk applies to children younger than 12, “but I doubt it. I think it’s going to be puberty-related,” Dr. Bozkurt said. Still, “I don’t want to hypothesize without data.”
A version of this article first appeared on Medscape.com.
The risk of myocarditis after immunization with mRNA-based vaccines against SARS-CoV-2 raised concerns when it came to light in early 2021. But as report after report showed such cases to be rare and usually mild and self-limited, focus has turned to the “how and why.”
The mechanism linking the BNT162b2 (Pfizer-BioNTech) and especially mRNA-1273 (Moderna) vaccines to the occurrence of myocarditis is unclear for now, but one potential driver may be tied to a peculiarity that became apparent early: It occurs overwhelmingly in younger males, from 16 to perhaps 40 or 50 years of age. Excess risk has not been consistently seen among women, girls, and older men.
That observation has led to speculation that higher testosterone levels in adolescent boys and young men may somehow promote the adverse vaccine effect, whereas greater levels of estrogen among girls and women in the same age range may be cardioprotective.
Unlikely, brief, and ‘benign’
“Most of the myocarditis is benign, by which I mean that maybe the patients are admitted due to chest pain, but without reduction in ventricular function,” Enrico Ammirati, MD, PhD, a myocarditis expert at De Gasperis Cardio Center and Transplant Center, Niguarda Hospital, Milan, said in an interview.
In a Nov. 14 address on this topic at the annual scientific sessions of the American Heart Association, Dror Mevorach, MD, described the typical case presentation as “mild” and one that clears in fairly short order based on resolution of “clinical symptoms, inflammatory markers and troponin decline, EKG normalization, echo normalization, and a relatively short length of hospital stay.”
Dr. Mevorach, of Hadassah Hebrew University Medical Center, Jerusalem, subsequently published the findings in a report in the New England Journal of Medicine that described 136 confirmed myocarditis cases among more than 5 million people in Israel immunized with the Pfizer-BioNTech vaccine. Myocarditis was considered “mild” in 129 cases, or 95%.
And the risk is tiny, compared with myocarditis from infection by SARS-CoV-2, not to mention the possibility of nasty clinical COVID-19 complications such as pneumonia and pulmonary embolism, Dr. Mevorach observed.
Many other reports agree that the incidence is minimal, especially given the rewards of vaccination. In a separate NEJM publication in September 2021 – from Noam Barda, MD, Clalit (Israel) Research Institute, and colleagues on 1.7 million people in that country, about half unvaccinated and half given the Pfizer-BioNTech vaccine – there were an estimated 2.7 cases of myocarditis per 100,000 vaccinated persons. There were also 11 cases of myocarditis per 100,000 persons who were positive for SARS-CoV-2 infection.
And in a recent case series of vaccinated people aged 16 or older, the myocarditis rate after a first or second Pfizer-BioNTech or Moderna injection was estimated at 1 or fewer per 100,000. The corresponding estimate was 4 such cases per 100,000 after a positive SARS-CoV-2 test among the same population, notes a report published Dec.14, 2021, in Nature Medicine.
In general, “the risk of any kind of cardiac injury is vastly lower with a vaccine than it is with the actual viral infection,” Leslie T. Cooper Jr., MD, a myocarditis expert and clinical trialist at the Mayo Clinic, Jacksonville, Fla., said in an interview. With the mRNA-based vaccines, “we do not have any conceivable danger signal that would outweigh the benefit of vaccination.”
Males of a certain age
Evidence that such myocarditis predominates in young adult men and adolescent boys, especially following a second vaccine dose, is remarkably consistent.
The risk was elevated only among mRNA-based vaccine recipients who were younger than 40 in the recent Nature Medicine analysis. Among that group, estimates after a second dose numbered fewer than 1 case per 100,000 for Pfizer-BioNTech and 1.5 per 100,000 for Moderna.
In a third analysis from Israel – also in NEJM, from Guy Witberg, MD, Rabin Medical Center, Petah Tikva, and colleagues, based on 2.5 million people aged 16 and older with at least one Pfizer-BioNTech injection – 2.1 cases per 100,000 were estimated overall, but the number rose to 10.7 per 100,000 among those aged 16-29 years.
In Dr. Mevorach’s NEJM report, estimates after a second Pfizer-BioNTech vaccine dose were 1 per 26,000 males versus 1 in 218,000 females, compared with 1 myocarditis case in 10,857 persons among “the general unvaccinated population.”
Most recipients of a first vaccine dose were younger than 50, and 16- to 29-year-olds accounted for most who completed two doses, noted Dr. Mevorach. Younger males bore the brunt of any myocarditis: the estimated prevalence after a second dose among males aged 16-19 was 1 per 6,637, compared with 1 per 99,853 females in the same age range, the group reported.
In the BMJ report, based on about 5 million people 12 years of age or older in Denmark, the estimated rates of myocarditis or pericarditis associated with Moderna immunization were 2 per 100,000 among women but 6.3 per 100,000 for men. The incidence and sex difference was much lower among those getting the Pfizer-BioNTech vaccine: 1.3 per 100,000 and 1.5 per 100,000 in women and men, respectively.
Sex hormones may be key
The predominance of vaccine-associated myocarditis among adolescent and young adult males is probably more about the myocarditis itself than the vaccines, observed Biykem Bozkurt, MD, PhD, who has been studying COVID-related myocarditis at Baylor College of Medicine, Houston.
Male sex historically is associated in both epidemiologic studies and experimental models with a greater propensity for most any form of myocarditis, Dr. Bozkurt said in an interview. Given that males aged 16-19 or so appear to be at highest risk of myocarditis as a complication of SARS-CoV-2 vaccination, the mechanism may well be related to sex hormones.
“Therefore, testosterone is implicated as a player in their higher risk of inflammation and injury and lack of adaptive response in terms of healing, and in terms of prevention of injury,” Dr. Bozkurt said. For its part, estrogen inhibits proinflammatory processes and, in particular, “blunts cell-mediated immune responses.”
“We don’t know the mechanism, but a theory that attributes a protective role to estrogen, or a risk associated with testosterone, is reasonable. It makes sense, at least based on epidemiological data,” Dr. Ammirati agreed. Still, “we do not have any direct evidence in human beings.”
Sex-associated differences in experimental myocarditis have been reported in the journals for at least 70 years, but “the testosterone literature and the estrogen literature have not been evaluated in detail in vaccine-associated myocarditis,” Dr. Cooper said.
Most myocarditis in the laboratory is viral, Dr. Cooper observed, and “the links between testosterone, viruses, and inflammation have been pretty well worked out, I would say, if you’re a mouse. If you’re a human, I think it’s still a bit uncertain.”
Were it to apply in humans, greater testosterone levels might independently promote myocarditis, “and if estrogen is cardioprotective, it would be another mechanism,” Dr. Cooper said. “That would translate to slight male predominance in most kinds of myocarditis.”
In males, compared with females, “the heart can be more vulnerable to events such as arrhythmias or to immune-mediated phenomena. So, probably there is also higher vulnerability to myocarditis in men,” Dr. Ammirati noted.
Male predominance in vaccine-related myocarditis is provocative, so it’s worth considering whether testosterone is part of the mechanism as well as the possibility of estrogen cardioprotection, Dr. Ammirati said. But given limitations of the animal models, “we don’t really have robust data to support any part of that.”
Although myocarditis is in some way immune mediated, “and hormones can modulate the response,” the mechanism has to be more than just sex hormones, he said. “They probably cannot explain the specificity for the heart. It’s not a systemic response, it’s an organ-specific response.”
Modulation of immune responses
Details about the immune processes underlying mRNA-vaccine myocarditis, hormone modulated or not, have been elusive. The complication doesn’t resemble serum sickness, nor does it seem to be a reaction to infection by other cardiotropic viruses, such as coxsackie virus B, a cause of viral myocarditis, Dr. Bozkurt said. The latter had been a compelling possibility because such hypersensitivity to smallpox vaccination is well recognized.
“We don’t know the mechanism, that’s the short answer. But there are many hypotheses,” she said. One candidate widely proposed in the literature: autoantibodies driven by molecular mimicry between the SARS-CoV-2 spike protein targeted by the mRNA vaccines and a structurally similar myocardial protein, possibly alpha-myosin, noted Dr. Bozkurt and colleagues in a recent publication.
But elevations in specific “antiheart antibodies” have not been documented in recipients of the two mRNA-based vaccines, said Dr. Cooper. “So, I would say that – although molecular mimicry is a well-established mechanism of, for example, rheumatic carditis after a streptococcal A infection – that has not been demonstrated yet for COVID-19 mRNA vaccination–related myocarditis.”
“We probably won’t know, ever, with a huge level of certainty, the exact mechanisms,” Dr. Cooper added. There is no animal model for vaccine-induced myocarditis, and “We’re still talking very, very small numbers of patients. The vast majority of them recover,” and so don’t generally provide mechanistic clues.
Prospects for younger children
Vaccination against SARS-CoV-2 has now been authorized by the Centers for Disease Control and Prevention for kids as young as 5-11 years, using the Pfizer-BioNTech vaccine. Experience so far suggests the immunization is safe in that age group with negligible risk of myocarditis or other complications. But with prospects of possible authorization in children younger than 5, should myocarditis be a concern for them?
Probably not, if the complication is driven primarily by sex hormones, Dr. Cooper proposed. “One would predict that before puberty you would have a lower – much, much lower – rate of myocarditis in males than you would in the 16- to 19-year-old range, and that it would be roughly equal to females.” Dr. Ammirati and Dr. Bozkurt largely agreed.
It remains to be seen whether the vaccine-related myocarditis risk applies to children younger than 12, “but I doubt it. I think it’s going to be puberty-related,” Dr. Bozkurt said. Still, “I don’t want to hypothesize without data.”
A version of this article first appeared on Medscape.com.
PA name change bad for patients and the profession
Physician assistants (PAs) are angry with me, and with good reason. I had the audacity to lump them together with nurse practitioners (NPs) in my book “Patients at Risk,” an act which one highly placed PA leader called “distasteful” in a private conversation with me.
I will admit that PAs have reason to be upset. With competitive acceptance rates including a requirement for extensive health care experience before PA school, standardized training, and at least 2,000 hours of clinical experience before graduation, the profession is a stark contrast to the haphazard training and 500 clinical hours required of NPs today. Further, unlike NPs, who have sought independent practice since the 1980s, PAs have traditionally been close allies with physicians, generally working in a 1:1 supervision model.
The truth is that it hurt to include PAs with NPs in my book. I’ve had my own close relationships with PAs over the years and found the PAs I worked with to be outstanding clinicians. Unfortunately, the profession has given me no choice. Following a model set by the NP profession,
Their efforts began with a change in terminology. “Optimal team practice” (OTP) was supposed to give PAs more flexibility, allowing them to work for hospitals or physician groups rather than under the responsibility of one physician. Not surprisingly, corporations and even academic centers have been quick to take advantage, hiring PAs and placing them in positions without adequate physician support. OTP paved the way for independent practice, as PAs sought and gained independence from any physician supervision in North Dakota, the first state to grant them that right.
Most recently, PAs have determined to change their name entirely, calling themselves physician associates. This move by the American Academy of Physician Assistants is the culmination of a years-long marketing study on how to increase the relevance and improve patient perception of the PA profession. The AAPA decision is expected to galvanize state and local PA organizations to lobby legislators for legal and regulatory changes that allow the use of the “physician associate” title, which is not currently a legal representation of PA licensure.
PAs’ latest attempt at title and branding reform follows years of advocacy to not be referred to as physician extenders or midlevel providers. For example, to gain more public acceptance of the PA model, the profession launched the public relations campaign “Your PA Can,” closely mirroring the “We Choose NPs” media blitz. PAs have also followed other dangerous precedents set by NPs, including 100% online training and a new “Doctor of Medical Science” degree, allowing PAs, as well as NPs, to now be called “doctors.”
I can understand PA reasoning even if I don’t agree with it. PAs are frustrated to be treated as second-class citizens compared with NPs, who have been granted independent practice in half the states in the union despite having a fraction of PA training. Frankly, it’s unfair that NPs are being hired preferentially over PAs simply because of looser legal requirements for physician oversight. The bottom line is that NPs have been more successful at persuading legislators to allow them independence – but that doesn’t make it right for either group.
While PAs have more clinical training upon graduation than NPs, they still have far less than physicians. PAs generally attend a 2-year master’s degree program after college which includes 2,000 hours of hands-on clinical work. By comparison, the average medical student spends 4 years and receives 5,000-6,000 hours of supervised clinical training upon graduation. But this isn’t considered enough for a graduate medical student to practice medicine independently.
Physicians must complete at least 3 years of postgraduate residency training in most states to receive a medical license, and by the time a physician is permitted to practice medicine unsupervised, they will have attained no fewer than 15,000-20,000 hours of supervised clinical practice, with years of specialty-specific training.
Patients want and deserve access to truly physician-led care, but in many parts of the country, physicians are being replaced by nonphysician practitioners to boost corporate profits. In many cases, patients are kept in the dark about the differences in training between the medical professionals now in charge of their care. The American Medical Association and other critics have expressed concern that the proposed title of “physician associate” is likely to further obscure the training and roles of medical professionals, already a source of confusion to patients.
One specific criticism is that a physician associate has historically referred to a physician (MD or DO) in a private practice group who has not yet achieved the status of partner. These physician associates are fully licensed medical doctors who have completed medical school and residency training and are in the process of completing a partnership track with their group to participate fully in financial and administrative processes. This nomenclature is similar to that of attorneys on a partnership track. Thus, the use of the term “physician associate” for someone other than a medical doctor is seen as misleading, particularly to patients who cannot be expected to have familiarity with the differences in training.
Efforts to separate the PA profession from a close-working relationship with a physician are bad not only for patients but for PAs as well. Many PAs who desire physician involvement may find themselves hung out to dry, hired by companies and expected to perform outside of their comfort level. The profession also risks ostracizing physician allies, many of whom have preferentially sought to work with PAs.
My sincere hope is that the PA profession will return to its traditional roots of a physician-PA relationship, a model that has been demonstrated to result in high-quality patient care. When that day comes, I will happily re-title my book. But as long as the AAPA continues to work to remove physicians from the equation, patients are indeed at risk.
Rebekah Bernard, MD, is a family physician in Fort Myers, Florida, and president of Physicians for Patient Protection. She is the coauthor of Patients at Risk: The Rise of the Nurse Practitioner and Physician Assistant in Healthcare (Irvine, Calif.: Universal Publishers, 2020). She had no relevant financial disclosures. A version of this article first appeared on Medscape.com.
Physician assistants (PAs) are angry with me, and with good reason. I had the audacity to lump them together with nurse practitioners (NPs) in my book “Patients at Risk,” an act which one highly placed PA leader called “distasteful” in a private conversation with me.
I will admit that PAs have reason to be upset. With competitive acceptance rates including a requirement for extensive health care experience before PA school, standardized training, and at least 2,000 hours of clinical experience before graduation, the profession is a stark contrast to the haphazard training and 500 clinical hours required of NPs today. Further, unlike NPs, who have sought independent practice since the 1980s, PAs have traditionally been close allies with physicians, generally working in a 1:1 supervision model.
The truth is that it hurt to include PAs with NPs in my book. I’ve had my own close relationships with PAs over the years and found the PAs I worked with to be outstanding clinicians. Unfortunately, the profession has given me no choice. Following a model set by the NP profession,
Their efforts began with a change in terminology. “Optimal team practice” (OTP) was supposed to give PAs more flexibility, allowing them to work for hospitals or physician groups rather than under the responsibility of one physician. Not surprisingly, corporations and even academic centers have been quick to take advantage, hiring PAs and placing them in positions without adequate physician support. OTP paved the way for independent practice, as PAs sought and gained independence from any physician supervision in North Dakota, the first state to grant them that right.
Most recently, PAs have determined to change their name entirely, calling themselves physician associates. This move by the American Academy of Physician Assistants is the culmination of a years-long marketing study on how to increase the relevance and improve patient perception of the PA profession. The AAPA decision is expected to galvanize state and local PA organizations to lobby legislators for legal and regulatory changes that allow the use of the “physician associate” title, which is not currently a legal representation of PA licensure.
PAs’ latest attempt at title and branding reform follows years of advocacy to not be referred to as physician extenders or midlevel providers. For example, to gain more public acceptance of the PA model, the profession launched the public relations campaign “Your PA Can,” closely mirroring the “We Choose NPs” media blitz. PAs have also followed other dangerous precedents set by NPs, including 100% online training and a new “Doctor of Medical Science” degree, allowing PAs, as well as NPs, to now be called “doctors.”
I can understand PA reasoning even if I don’t agree with it. PAs are frustrated to be treated as second-class citizens compared with NPs, who have been granted independent practice in half the states in the union despite having a fraction of PA training. Frankly, it’s unfair that NPs are being hired preferentially over PAs simply because of looser legal requirements for physician oversight. The bottom line is that NPs have been more successful at persuading legislators to allow them independence – but that doesn’t make it right for either group.
While PAs have more clinical training upon graduation than NPs, they still have far less than physicians. PAs generally attend a 2-year master’s degree program after college which includes 2,000 hours of hands-on clinical work. By comparison, the average medical student spends 4 years and receives 5,000-6,000 hours of supervised clinical training upon graduation. But this isn’t considered enough for a graduate medical student to practice medicine independently.
Physicians must complete at least 3 years of postgraduate residency training in most states to receive a medical license, and by the time a physician is permitted to practice medicine unsupervised, they will have attained no fewer than 15,000-20,000 hours of supervised clinical practice, with years of specialty-specific training.
Patients want and deserve access to truly physician-led care, but in many parts of the country, physicians are being replaced by nonphysician practitioners to boost corporate profits. In many cases, patients are kept in the dark about the differences in training between the medical professionals now in charge of their care. The American Medical Association and other critics have expressed concern that the proposed title of “physician associate” is likely to further obscure the training and roles of medical professionals, already a source of confusion to patients.
One specific criticism is that a physician associate has historically referred to a physician (MD or DO) in a private practice group who has not yet achieved the status of partner. These physician associates are fully licensed medical doctors who have completed medical school and residency training and are in the process of completing a partnership track with their group to participate fully in financial and administrative processes. This nomenclature is similar to that of attorneys on a partnership track. Thus, the use of the term “physician associate” for someone other than a medical doctor is seen as misleading, particularly to patients who cannot be expected to have familiarity with the differences in training.
Efforts to separate the PA profession from a close-working relationship with a physician are bad not only for patients but for PAs as well. Many PAs who desire physician involvement may find themselves hung out to dry, hired by companies and expected to perform outside of their comfort level. The profession also risks ostracizing physician allies, many of whom have preferentially sought to work with PAs.
My sincere hope is that the PA profession will return to its traditional roots of a physician-PA relationship, a model that has been demonstrated to result in high-quality patient care. When that day comes, I will happily re-title my book. But as long as the AAPA continues to work to remove physicians from the equation, patients are indeed at risk.
Rebekah Bernard, MD, is a family physician in Fort Myers, Florida, and president of Physicians for Patient Protection. She is the coauthor of Patients at Risk: The Rise of the Nurse Practitioner and Physician Assistant in Healthcare (Irvine, Calif.: Universal Publishers, 2020). She had no relevant financial disclosures. A version of this article first appeared on Medscape.com.
Physician assistants (PAs) are angry with me, and with good reason. I had the audacity to lump them together with nurse practitioners (NPs) in my book “Patients at Risk,” an act which one highly placed PA leader called “distasteful” in a private conversation with me.
I will admit that PAs have reason to be upset. With competitive acceptance rates including a requirement for extensive health care experience before PA school, standardized training, and at least 2,000 hours of clinical experience before graduation, the profession is a stark contrast to the haphazard training and 500 clinical hours required of NPs today. Further, unlike NPs, who have sought independent practice since the 1980s, PAs have traditionally been close allies with physicians, generally working in a 1:1 supervision model.
The truth is that it hurt to include PAs with NPs in my book. I’ve had my own close relationships with PAs over the years and found the PAs I worked with to be outstanding clinicians. Unfortunately, the profession has given me no choice. Following a model set by the NP profession,
Their efforts began with a change in terminology. “Optimal team practice” (OTP) was supposed to give PAs more flexibility, allowing them to work for hospitals or physician groups rather than under the responsibility of one physician. Not surprisingly, corporations and even academic centers have been quick to take advantage, hiring PAs and placing them in positions without adequate physician support. OTP paved the way for independent practice, as PAs sought and gained independence from any physician supervision in North Dakota, the first state to grant them that right.
Most recently, PAs have determined to change their name entirely, calling themselves physician associates. This move by the American Academy of Physician Assistants is the culmination of a years-long marketing study on how to increase the relevance and improve patient perception of the PA profession. The AAPA decision is expected to galvanize state and local PA organizations to lobby legislators for legal and regulatory changes that allow the use of the “physician associate” title, which is not currently a legal representation of PA licensure.
PAs’ latest attempt at title and branding reform follows years of advocacy to not be referred to as physician extenders or midlevel providers. For example, to gain more public acceptance of the PA model, the profession launched the public relations campaign “Your PA Can,” closely mirroring the “We Choose NPs” media blitz. PAs have also followed other dangerous precedents set by NPs, including 100% online training and a new “Doctor of Medical Science” degree, allowing PAs, as well as NPs, to now be called “doctors.”
I can understand PA reasoning even if I don’t agree with it. PAs are frustrated to be treated as second-class citizens compared with NPs, who have been granted independent practice in half the states in the union despite having a fraction of PA training. Frankly, it’s unfair that NPs are being hired preferentially over PAs simply because of looser legal requirements for physician oversight. The bottom line is that NPs have been more successful at persuading legislators to allow them independence – but that doesn’t make it right for either group.
While PAs have more clinical training upon graduation than NPs, they still have far less than physicians. PAs generally attend a 2-year master’s degree program after college which includes 2,000 hours of hands-on clinical work. By comparison, the average medical student spends 4 years and receives 5,000-6,000 hours of supervised clinical training upon graduation. But this isn’t considered enough for a graduate medical student to practice medicine independently.
Physicians must complete at least 3 years of postgraduate residency training in most states to receive a medical license, and by the time a physician is permitted to practice medicine unsupervised, they will have attained no fewer than 15,000-20,000 hours of supervised clinical practice, with years of specialty-specific training.
Patients want and deserve access to truly physician-led care, but in many parts of the country, physicians are being replaced by nonphysician practitioners to boost corporate profits. In many cases, patients are kept in the dark about the differences in training between the medical professionals now in charge of their care. The American Medical Association and other critics have expressed concern that the proposed title of “physician associate” is likely to further obscure the training and roles of medical professionals, already a source of confusion to patients.
One specific criticism is that a physician associate has historically referred to a physician (MD or DO) in a private practice group who has not yet achieved the status of partner. These physician associates are fully licensed medical doctors who have completed medical school and residency training and are in the process of completing a partnership track with their group to participate fully in financial and administrative processes. This nomenclature is similar to that of attorneys on a partnership track. Thus, the use of the term “physician associate” for someone other than a medical doctor is seen as misleading, particularly to patients who cannot be expected to have familiarity with the differences in training.
Efforts to separate the PA profession from a close-working relationship with a physician are bad not only for patients but for PAs as well. Many PAs who desire physician involvement may find themselves hung out to dry, hired by companies and expected to perform outside of their comfort level. The profession also risks ostracizing physician allies, many of whom have preferentially sought to work with PAs.
My sincere hope is that the PA profession will return to its traditional roots of a physician-PA relationship, a model that has been demonstrated to result in high-quality patient care. When that day comes, I will happily re-title my book. But as long as the AAPA continues to work to remove physicians from the equation, patients are indeed at risk.
Rebekah Bernard, MD, is a family physician in Fort Myers, Florida, and president of Physicians for Patient Protection. She is the coauthor of Patients at Risk: The Rise of the Nurse Practitioner and Physician Assistant in Healthcare (Irvine, Calif.: Universal Publishers, 2020). She had no relevant financial disclosures. A version of this article first appeared on Medscape.com.
COVID-19 linked to increased diabetes risk in youth
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
SARS-CoV-2 infection was associated with an increased risk for diabetes among youth, whereas other acute respiratory infections were not, new data from the U.S. Centers for Disease Control and Prevention indicate.
The results from two large U.S. health claims databases were published in an early release in the CDC’s Morbidity and Mortality Weekly Report by Catherine E. Barrett, PhD, and colleagues of the CDC’s COVID-19 Emergency Response Team and Division of Diabetes Translation.
Clinicians should monitor individuals younger than 18 years in the months following a SARS-CoV-2 infection for new diabetes onset, they advise.
The findings, which are supported by independent studies in adults, “underscore the importance of COVID-19 prevention among all age groups, including vaccination for all eligible children and adolescents, and chronic disease prevention and treatment,” Dr. Barrett and colleagues say.
Diabetes type couldn’t be reliably distinguished from the databases, which is noted as an important study limitation.
“SARS-CoV-2 infection might lead to type 1 or type 2 diabetes through complex and differing mechanisms,” they say.
Emerging evidence began to suggest, in mid-2020, that COVID-19 may trigger the onset of diabetes in healthy people. A new global registry was subsequently established to collect data on patients with COVID-19–related diabetes, called the CoviDiab registry.
Not clear if diabetes after COVID-19 is transient or permanent
From one of the databases used in the new study, known as IQVIA, 80,893 individuals aged younger than 18 years diagnosed with COVID-19 during March 2020 to February 26, 2021, were compared with age- and sex-matched people during that period who did not have COVID-19 and to prepandemic groups with and without a diagnosis of acute respiratory illness during March 1, 2017, to February 26, 2018.
From the second database, HealthVerity, 439,439 youth diagnosed with COVID-19 during March 1, 2020, to June 28, 2021, were compared with age- and sex-matched youth without COVID-19. Here, there was no prepandemic comparison group.
Diabetes diagnoses were coded in 0.08% with COVID-19 vs. 0.03% without COVID-19 in IQVIA and in 0.25% vs. 0.19% in HealthVerity.
Thus, new diabetes diagnoses were 166% and 31% more likely to occur in those with COVID-19 in IQVIA and HealthVerity, respectively. And in IQVIA, those with COVID-19 were 116% more likely to develop diabetes than were those with prepandemic acute respiratory illnesses. Those differences were all significant, whereas non–SARS-CoV-2 respiratory infections were not associated with diabetes, Dr. Barrett and colleagues say.
In both databases, diabetic ketoacidosis (DKA) was more common at diabetes onset among those with, vs. without, COVID-19: 48.5% vs. 13.6% in IQVIA and 40.2% vs. 29.7% in HealthVerity. In IQVIA, 22.0% with prepandemic acute respiratory illness presented with DKA.
Dr. Barrett and colleagues offer several potential explanations for the observed association between COVID-19 and diabetes, including a direct attack on pancreatic beta cells expressing angiotensin-converting enzyme 2 receptors, or via stress hyperglycemia resulting from cytokine storm and alterations in glucose metabolism.
Another possibility is the precipitation to diabetes from prediabetes; the latter is a condition present in one in five U.S. adolescents.
Steroid treatment during hospitalization might have led to transient hyperglycemia, but only 1.5% to 2.2% of diabetes codes were for drug- or chemical-induced diabetes. The majority were for type 1 or 2.
Alternatively, pandemic-associated weight gain might have also contributed to risks for both severe COVID-19 and type 2 diabetes.
“Although this study can provide information on the risk for diabetes following SARS-CoV-2 infection, additional data are needed to understand underlying pathogenic mechanisms, either those caused by SARS-CoV-2 infection itself or resulting from treatments, and whether a COVID-19–associated diabetes diagnosis is transient or leads to a chronic condition,” Dr. Barrett and colleagues conclude.
A version of this article first appeared on Medscape.com.
FROM MMWR
As pandemic regs expire, states get tougher on telehealth: report
Among the most important restrictions that have been reinstated in some states are those barring requirements for insurers to cover telehealth and regulations that prohibit telehealth visits across state lines, unless the physician is licensed in both states.
“Only three states – Arizona, Florida, and Indiana – allow all health care providers to easily practice telehealth across state lines,” says a news release on the think tanks’ report. “Forty-seven others have arbitrary barriers in place that limit patients’ access to specialists and available appointments based purely on residency.”
“Once the [state-based] public health emergency declarations started to end or executive orders were withdrawn, many of the new flexibilities for providers, insurers, and patients were lost overnight,” Vittorio Nastasi, a policy analyst at Reason Foundation and a co-author of the report, says in the news release. “States need to adopt a number of telehealth reforms to provide their residents better access to this safe and effective virtual care.”
On a positive note, the report says, most states have removed the requirement that a patient must first see a provider in person before they can use telehealth services. The exceptions are Tennessee, Alaska, and West Virginia, which require an in-person visit before certain telehealth services can be provided.
In addition, 20 states allow nurse practitioners to conduct telehealth visits without being under the supervision of a physician. Prior to the pandemic, some states allowed only doctors to use telehealth, the report says, but, during the COVID crisis, “the acute shortage of providers in many counties adds to the need for more kinds of providers to be able to use it.”
A number of states place restrictions on the telehealth modalities that can be utilized. Under the definition by the American Telemedicine Association, telehealth includes audio-video visits, remote patient monitoring, and “store and forward” telemedicine, which entails collecting clinical information and sending it to another site for evaluation. The latter method is particularly useful for consultations with specialists, the report notes.
Coverage mandates and payment parity
The report also examines other parameters of telehealth regulations in each state, including whether they have telehealth coverage mandates and whether they require physicians to be paid the same amount for similar types of in-person and telehealth visits.
The report views insurance mandates as beneficial, but not if they require coverage of all virtual services. While telehealth can be a game changer for post-stroke care and for other “treatment-intensive conditions,” the report says, the evidence of better outcomes for other conditions treated through telehealth is far less certain. Therefore, it advises states to “protect flexibility so that new innovative models can emerge.”
Ateev Mehrotra, MD, a professor at Harvard Medical School who studies telehealth, agrees that it offers more value in some clinical situations than in others. “High value is improving quality or outcomes at a reasonable cost,” he told this news organization. “If a telemedicine visit for stroke can save a person’s life and prevent disability, let’s pay for it. A telemedicine visit for a cold may not be necessary. Mom’s chicken soup is fine.”
A little over half of the states still require payment parity, according to the report. While these regulations are intended to promote the use of telehealth, the authors note, they can increase the growth of health care costs. Moreover, they argue, it’s hard to defend equal payments for virtual visits when the overhead required to deliver them – such as office rental, utility, and labor costs – is much lower than that for in-person visits. Also, it makes no sense for health systems to charge facility fees for telehealth visits when these visits can be initiated from anywhere, they say.
Dr. Mehrotra concurs with this view. “If you see someone in your office, your fee includes all the overhead for your office, and it’s a substantial cost,” he says. “For many procedures, it’s more than half of the cost. If you have a telemedicine visit and you’re at home, why would you pay the same amount? The visit may take the same amount of time, but all the money that goes for overhead is not accounted for.”
Telemedicine across state lines
The report’s contention about the difficulty of conducting telehealth encounters across most state lines seems to be at odds with the growth in the Interstate Medical Licensure Compact, which makes it easier for physicians in one compact member state to get licensed in others. Currently, 35 states belong to the compact, Joe Knickrehm, vice president of communications for the Federation of State Medical Boards, told this news organization.
In addition, he says, “12 state boards issue a special purpose license, telemedicine license or certificate, or license to practice medicine across state lines to allow for the practice of telemedicine.”
The catch, Dr. Mehrotra says, is that, despite the streamlining of license applications in compact member states, the fees charged by the state boards are still very high – a point that the report also makes. “If I want to have broad scope of practice, I’d have to pay thousands of dollars to many states. The license fees start to add up. Also, I have to keep track of each state’s CME requirements, which are all different. Keeping up with all of that is an administration burden, and it’s a pain.”
Mr. Knickrehm contends that obtaining multiple licenses via the compact “is generally less expensive for physicians than the cost of requesting transcripts, fingerprints, and other necessary paperwork each time they apply for licensure in a new state. Physicians are seeing the benefits of an expedited process that allows them to begin practicing more quickly [in other states].”
Dr. Mehrotra says he has seen the same retrenchment in state telehealth regulations that the report references. However, he says, “CMS [the Centers for Medicare & Medicaid Services] has signaled that at least through 2022 and maybe into 2023, they’ll continue their extensions of telemedicine [pandemic regulations].” After that, Congress would have to decide whether to make the changes permanent.
“Right now, it’s hard for me to see how a payer is going to pull back on telehealth, unless there’s ample evidence of overuse of telehealth,” he argues. “With the public and providers liking telehealth, it’s hard to say on theoretical grounds that we should stop using it. That’s why Medicare and others have extended it and why Congress will too.”
A version of this article first appeared on Medscape.com.
Among the most important restrictions that have been reinstated in some states are those barring requirements for insurers to cover telehealth and regulations that prohibit telehealth visits across state lines, unless the physician is licensed in both states.
“Only three states – Arizona, Florida, and Indiana – allow all health care providers to easily practice telehealth across state lines,” says a news release on the think tanks’ report. “Forty-seven others have arbitrary barriers in place that limit patients’ access to specialists and available appointments based purely on residency.”
“Once the [state-based] public health emergency declarations started to end or executive orders were withdrawn, many of the new flexibilities for providers, insurers, and patients were lost overnight,” Vittorio Nastasi, a policy analyst at Reason Foundation and a co-author of the report, says in the news release. “States need to adopt a number of telehealth reforms to provide their residents better access to this safe and effective virtual care.”
On a positive note, the report says, most states have removed the requirement that a patient must first see a provider in person before they can use telehealth services. The exceptions are Tennessee, Alaska, and West Virginia, which require an in-person visit before certain telehealth services can be provided.
In addition, 20 states allow nurse practitioners to conduct telehealth visits without being under the supervision of a physician. Prior to the pandemic, some states allowed only doctors to use telehealth, the report says, but, during the COVID crisis, “the acute shortage of providers in many counties adds to the need for more kinds of providers to be able to use it.”
A number of states place restrictions on the telehealth modalities that can be utilized. Under the definition by the American Telemedicine Association, telehealth includes audio-video visits, remote patient monitoring, and “store and forward” telemedicine, which entails collecting clinical information and sending it to another site for evaluation. The latter method is particularly useful for consultations with specialists, the report notes.
Coverage mandates and payment parity
The report also examines other parameters of telehealth regulations in each state, including whether they have telehealth coverage mandates and whether they require physicians to be paid the same amount for similar types of in-person and telehealth visits.
The report views insurance mandates as beneficial, but not if they require coverage of all virtual services. While telehealth can be a game changer for post-stroke care and for other “treatment-intensive conditions,” the report says, the evidence of better outcomes for other conditions treated through telehealth is far less certain. Therefore, it advises states to “protect flexibility so that new innovative models can emerge.”
Ateev Mehrotra, MD, a professor at Harvard Medical School who studies telehealth, agrees that it offers more value in some clinical situations than in others. “High value is improving quality or outcomes at a reasonable cost,” he told this news organization. “If a telemedicine visit for stroke can save a person’s life and prevent disability, let’s pay for it. A telemedicine visit for a cold may not be necessary. Mom’s chicken soup is fine.”
A little over half of the states still require payment parity, according to the report. While these regulations are intended to promote the use of telehealth, the authors note, they can increase the growth of health care costs. Moreover, they argue, it’s hard to defend equal payments for virtual visits when the overhead required to deliver them – such as office rental, utility, and labor costs – is much lower than that for in-person visits. Also, it makes no sense for health systems to charge facility fees for telehealth visits when these visits can be initiated from anywhere, they say.
Dr. Mehrotra concurs with this view. “If you see someone in your office, your fee includes all the overhead for your office, and it’s a substantial cost,” he says. “For many procedures, it’s more than half of the cost. If you have a telemedicine visit and you’re at home, why would you pay the same amount? The visit may take the same amount of time, but all the money that goes for overhead is not accounted for.”
Telemedicine across state lines
The report’s contention about the difficulty of conducting telehealth encounters across most state lines seems to be at odds with the growth in the Interstate Medical Licensure Compact, which makes it easier for physicians in one compact member state to get licensed in others. Currently, 35 states belong to the compact, Joe Knickrehm, vice president of communications for the Federation of State Medical Boards, told this news organization.
In addition, he says, “12 state boards issue a special purpose license, telemedicine license or certificate, or license to practice medicine across state lines to allow for the practice of telemedicine.”
The catch, Dr. Mehrotra says, is that, despite the streamlining of license applications in compact member states, the fees charged by the state boards are still very high – a point that the report also makes. “If I want to have broad scope of practice, I’d have to pay thousands of dollars to many states. The license fees start to add up. Also, I have to keep track of each state’s CME requirements, which are all different. Keeping up with all of that is an administration burden, and it’s a pain.”
Mr. Knickrehm contends that obtaining multiple licenses via the compact “is generally less expensive for physicians than the cost of requesting transcripts, fingerprints, and other necessary paperwork each time they apply for licensure in a new state. Physicians are seeing the benefits of an expedited process that allows them to begin practicing more quickly [in other states].”
Dr. Mehrotra says he has seen the same retrenchment in state telehealth regulations that the report references. However, he says, “CMS [the Centers for Medicare & Medicaid Services] has signaled that at least through 2022 and maybe into 2023, they’ll continue their extensions of telemedicine [pandemic regulations].” After that, Congress would have to decide whether to make the changes permanent.
“Right now, it’s hard for me to see how a payer is going to pull back on telehealth, unless there’s ample evidence of overuse of telehealth,” he argues. “With the public and providers liking telehealth, it’s hard to say on theoretical grounds that we should stop using it. That’s why Medicare and others have extended it and why Congress will too.”
A version of this article first appeared on Medscape.com.
Among the most important restrictions that have been reinstated in some states are those barring requirements for insurers to cover telehealth and regulations that prohibit telehealth visits across state lines, unless the physician is licensed in both states.
“Only three states – Arizona, Florida, and Indiana – allow all health care providers to easily practice telehealth across state lines,” says a news release on the think tanks’ report. “Forty-seven others have arbitrary barriers in place that limit patients’ access to specialists and available appointments based purely on residency.”
“Once the [state-based] public health emergency declarations started to end or executive orders were withdrawn, many of the new flexibilities for providers, insurers, and patients were lost overnight,” Vittorio Nastasi, a policy analyst at Reason Foundation and a co-author of the report, says in the news release. “States need to adopt a number of telehealth reforms to provide their residents better access to this safe and effective virtual care.”
On a positive note, the report says, most states have removed the requirement that a patient must first see a provider in person before they can use telehealth services. The exceptions are Tennessee, Alaska, and West Virginia, which require an in-person visit before certain telehealth services can be provided.
In addition, 20 states allow nurse practitioners to conduct telehealth visits without being under the supervision of a physician. Prior to the pandemic, some states allowed only doctors to use telehealth, the report says, but, during the COVID crisis, “the acute shortage of providers in many counties adds to the need for more kinds of providers to be able to use it.”
A number of states place restrictions on the telehealth modalities that can be utilized. Under the definition by the American Telemedicine Association, telehealth includes audio-video visits, remote patient monitoring, and “store and forward” telemedicine, which entails collecting clinical information and sending it to another site for evaluation. The latter method is particularly useful for consultations with specialists, the report notes.
Coverage mandates and payment parity
The report also examines other parameters of telehealth regulations in each state, including whether they have telehealth coverage mandates and whether they require physicians to be paid the same amount for similar types of in-person and telehealth visits.
The report views insurance mandates as beneficial, but not if they require coverage of all virtual services. While telehealth can be a game changer for post-stroke care and for other “treatment-intensive conditions,” the report says, the evidence of better outcomes for other conditions treated through telehealth is far less certain. Therefore, it advises states to “protect flexibility so that new innovative models can emerge.”
Ateev Mehrotra, MD, a professor at Harvard Medical School who studies telehealth, agrees that it offers more value in some clinical situations than in others. “High value is improving quality or outcomes at a reasonable cost,” he told this news organization. “If a telemedicine visit for stroke can save a person’s life and prevent disability, let’s pay for it. A telemedicine visit for a cold may not be necessary. Mom’s chicken soup is fine.”
A little over half of the states still require payment parity, according to the report. While these regulations are intended to promote the use of telehealth, the authors note, they can increase the growth of health care costs. Moreover, they argue, it’s hard to defend equal payments for virtual visits when the overhead required to deliver them – such as office rental, utility, and labor costs – is much lower than that for in-person visits. Also, it makes no sense for health systems to charge facility fees for telehealth visits when these visits can be initiated from anywhere, they say.
Dr. Mehrotra concurs with this view. “If you see someone in your office, your fee includes all the overhead for your office, and it’s a substantial cost,” he says. “For many procedures, it’s more than half of the cost. If you have a telemedicine visit and you’re at home, why would you pay the same amount? The visit may take the same amount of time, but all the money that goes for overhead is not accounted for.”
Telemedicine across state lines
The report’s contention about the difficulty of conducting telehealth encounters across most state lines seems to be at odds with the growth in the Interstate Medical Licensure Compact, which makes it easier for physicians in one compact member state to get licensed in others. Currently, 35 states belong to the compact, Joe Knickrehm, vice president of communications for the Federation of State Medical Boards, told this news organization.
In addition, he says, “12 state boards issue a special purpose license, telemedicine license or certificate, or license to practice medicine across state lines to allow for the practice of telemedicine.”
The catch, Dr. Mehrotra says, is that, despite the streamlining of license applications in compact member states, the fees charged by the state boards are still very high – a point that the report also makes. “If I want to have broad scope of practice, I’d have to pay thousands of dollars to many states. The license fees start to add up. Also, I have to keep track of each state’s CME requirements, which are all different. Keeping up with all of that is an administration burden, and it’s a pain.”
Mr. Knickrehm contends that obtaining multiple licenses via the compact “is generally less expensive for physicians than the cost of requesting transcripts, fingerprints, and other necessary paperwork each time they apply for licensure in a new state. Physicians are seeing the benefits of an expedited process that allows them to begin practicing more quickly [in other states].”
Dr. Mehrotra says he has seen the same retrenchment in state telehealth regulations that the report references. However, he says, “CMS [the Centers for Medicare & Medicaid Services] has signaled that at least through 2022 and maybe into 2023, they’ll continue their extensions of telemedicine [pandemic regulations].” After that, Congress would have to decide whether to make the changes permanent.
“Right now, it’s hard for me to see how a payer is going to pull back on telehealth, unless there’s ample evidence of overuse of telehealth,” he argues. “With the public and providers liking telehealth, it’s hard to say on theoretical grounds that we should stop using it. That’s why Medicare and others have extended it and why Congress will too.”
A version of this article first appeared on Medscape.com.
Neonatal sepsis: WHO-recommended Rx needs a major rethink
First-line treatment of neonatal sepsis in low- and middle-income countries (LMICs) with ampicillin-gentamicin – as recommended by the World Health Organization – needs to be reassessed, a retrospective, observational cohort study suggests. Rates of resistance to this particular antibiotic combination are extremely high in LMICs, and this treatment is unlikely to save many neonatal patients, according to the study’s results.
“The WHO guidelines are over 10 years old, and they are actually based on high-income country data, whereas data reported from low-income countries are reported by private labs, and they do not cater to the lower socioeconomic groups within these countries, which is important data to capture,” Timothy Walsh, MD, University of Oxford, United Kingdom, told this news organization.
“The main take-home message from our data is that ampicillin-gentamicin doesn’t work for most of the Gram-negative isolates we tested, and while there are alternatives, their use is confounded by [a lack of] financial support,” he added.
The study was published online in The Lancet Infectious Diseases.
BARNARDS study
In this substudy of the Burden of Antibiotic Resistance in Neonates from Developing Societies (BARNARDS) study, investigators focused on the effectiveness of antibiotic therapies after taking into account the high prevalence of pathogen resistance to ampicillin-gentamicin. Participating countries included Bangladesh, Ethiopia, India, Nigeria, Pakistan, Rwanda, and South Africa.
“Blood samples were obtained from neonates presenting with clinical signs of sepsis,” the authors note, “and WGS [whole-genome sequencing] and MICs [minimum inhibitory concentrations] for antibiotic treatment were determined for bacterial isolates from culture-confirmed sepsis.” Between Nov. 2015 and Feb. 2018, 36,285 neonates were enrolled into the main BARNARDS study, of whom 9,874 had clinically diagnosed sepsis and 5,749 had antibiotic data.
A total of 2,483 neonates had culture-confirmed sepsis, and WGS data were available for 457 isolates taken from 442 neonates. Slightly over three-quarters of the 5,749 neonates who had antibiotic data received first-line ampicillin-gentamicin. The other three most commonly prescribed antibiotic combinations were ceftazidime-amikacin, piperacillin-tazobactam-amikacin, and amoxicillin-clavulanate-amikacin.
Neonates treated with ceftazidime-amikacin had a 68% lower reported mortality than those treated with ampicillin-gentamicin at an adjusted hazard ratio of 0.32 (95% confidence interval, 0.14-0.72; P = .006), the investigators report. In contrast, no significant differences in mortality rates were reported for neonates treated with amoxicillin-clavulanate-amikacin or piperacillin-tazobactam-amikacin compared to those treated with ampicillin-gentamicin.
Investigators were careful to suggest that mortality effects associated with the different antibiotic combinations might have been confounded by either country-specific effects or underreporting of mortality, as a large proportion of neonates who were treated with ampicillin-gentamicin were followed for fewer than 10 days. However, in an unreported aspect of the same study, neonatal mortality from sepsis dropped by over 50% in two federally funded sites in Nigeria that changed their treatment from the WHO-recommended ampicillin-gentamicin regimen to ceftazidime-amikacin – which Dr. Walsh suggested was an endorsement of ceftazidime-amikacin over ampicillin-gentamicin if ever there was one.
Gram-negative resistance
In looking at resistance patterns to the antibiotic combinations used in these countries, investigators found that almost all Gram-negative isolates tested were “overwhelmingly resistant” to ampicillin, and over 70% of them were resistant to gentamicin as well. Extremely high resistance rates were also found against Staphylococcus spp, which are regarded as intrinsically resistant to ampicillin, rendering it basically useless in this particular treatment setting.
Amikacin had much lower level of resistance, with only about 26% of Gram-negative isolates showing resistance. In terms of coverage against Gram-negative isolates, the lowest level of coverage was provided by ampicillin-gentamicin at slightly over 28%, compared with about 73% for amoxicillin-clavulanate-amikacin, 77% for ceftazidime-amikacin, and 80% for piperacillin-tazobactam-amikacin.
In contrast, “Gram-positive isolates generally had reduced levels of resistance,” the authors state. As Dr. Walsh noted, the consortium also did an analysis assessing how much the antibiotic combinations cost and how much payment was deferred to the parents. For example, in Nigeria, the entire cost of treatment is passed down to the parents, “so if they are earning, say, $5.00 a day and the infant needs ceftazidime-amikacin, where the cost per dose is about $6.00 or $7.00 a day, parents can’t afford it,” Dr. Walsh observed.
This part of the conversation, he added, tends to get lost in many studies of antibiotic resistance in LMICs, which is a critical omission, because in many instances, the choice of treatment does come down to affordability. “It’s all very well for the WHO to sit there and say, ampicillin-gentamicin is perfect, but the combination actually doesn’t work in over 70% of the Gram-negative bacteria we looked at in these countries,” Dr. Walsh emphasized.
“The fact is that we have to be a lot more internationally engaged as to what’s actually happening in poorer populations, because unless we do, neonates are going to continue to die,” he said.
Editorial commentary
Commenting on the findings, lead editorialist Luregn Schlapbach, MD, PhD, of University Children’s Hospital Zurich, Switzerland, pointed out that the study has a number of limitations, including a high rate of dropouts from follow-up. This could possibly result in underestimation of neonatal mortality as well as country-specific biases. Nevertheless, Dr. Schlapbach feels that the integration of sequential clinical, genomic, microbiologic, drug, and cost data across a large network in LMIC settings is “exceptional” and will serve to inform “urgently needed” clinical trials in the field of neonatal sepsis.
“At present, increasing global antibiotic resistance is threatening progress against neonatal sepsis, prompting urgency to develop improved measures to effectively prevent and treat life-threatening infections in this high-risk group,” Dr. Schlapbach and colleagues write.
“The findings from the BARNARDS study call for randomized trials comparing mortality benefit and cost efficiency of different antibiotic combinations and management algorithms to safely reduce unnecessary antibiotic exposure for neonatal sepsis,” the editorialists concluded.
The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
First-line treatment of neonatal sepsis in low- and middle-income countries (LMICs) with ampicillin-gentamicin – as recommended by the World Health Organization – needs to be reassessed, a retrospective, observational cohort study suggests. Rates of resistance to this particular antibiotic combination are extremely high in LMICs, and this treatment is unlikely to save many neonatal patients, according to the study’s results.
“The WHO guidelines are over 10 years old, and they are actually based on high-income country data, whereas data reported from low-income countries are reported by private labs, and they do not cater to the lower socioeconomic groups within these countries, which is important data to capture,” Timothy Walsh, MD, University of Oxford, United Kingdom, told this news organization.
“The main take-home message from our data is that ampicillin-gentamicin doesn’t work for most of the Gram-negative isolates we tested, and while there are alternatives, their use is confounded by [a lack of] financial support,” he added.
The study was published online in The Lancet Infectious Diseases.
BARNARDS study
In this substudy of the Burden of Antibiotic Resistance in Neonates from Developing Societies (BARNARDS) study, investigators focused on the effectiveness of antibiotic therapies after taking into account the high prevalence of pathogen resistance to ampicillin-gentamicin. Participating countries included Bangladesh, Ethiopia, India, Nigeria, Pakistan, Rwanda, and South Africa.
“Blood samples were obtained from neonates presenting with clinical signs of sepsis,” the authors note, “and WGS [whole-genome sequencing] and MICs [minimum inhibitory concentrations] for antibiotic treatment were determined for bacterial isolates from culture-confirmed sepsis.” Between Nov. 2015 and Feb. 2018, 36,285 neonates were enrolled into the main BARNARDS study, of whom 9,874 had clinically diagnosed sepsis and 5,749 had antibiotic data.
A total of 2,483 neonates had culture-confirmed sepsis, and WGS data were available for 457 isolates taken from 442 neonates. Slightly over three-quarters of the 5,749 neonates who had antibiotic data received first-line ampicillin-gentamicin. The other three most commonly prescribed antibiotic combinations were ceftazidime-amikacin, piperacillin-tazobactam-amikacin, and amoxicillin-clavulanate-amikacin.
Neonates treated with ceftazidime-amikacin had a 68% lower reported mortality than those treated with ampicillin-gentamicin at an adjusted hazard ratio of 0.32 (95% confidence interval, 0.14-0.72; P = .006), the investigators report. In contrast, no significant differences in mortality rates were reported for neonates treated with amoxicillin-clavulanate-amikacin or piperacillin-tazobactam-amikacin compared to those treated with ampicillin-gentamicin.
Investigators were careful to suggest that mortality effects associated with the different antibiotic combinations might have been confounded by either country-specific effects or underreporting of mortality, as a large proportion of neonates who were treated with ampicillin-gentamicin were followed for fewer than 10 days. However, in an unreported aspect of the same study, neonatal mortality from sepsis dropped by over 50% in two federally funded sites in Nigeria that changed their treatment from the WHO-recommended ampicillin-gentamicin regimen to ceftazidime-amikacin – which Dr. Walsh suggested was an endorsement of ceftazidime-amikacin over ampicillin-gentamicin if ever there was one.
Gram-negative resistance
In looking at resistance patterns to the antibiotic combinations used in these countries, investigators found that almost all Gram-negative isolates tested were “overwhelmingly resistant” to ampicillin, and over 70% of them were resistant to gentamicin as well. Extremely high resistance rates were also found against Staphylococcus spp, which are regarded as intrinsically resistant to ampicillin, rendering it basically useless in this particular treatment setting.
Amikacin had much lower level of resistance, with only about 26% of Gram-negative isolates showing resistance. In terms of coverage against Gram-negative isolates, the lowest level of coverage was provided by ampicillin-gentamicin at slightly over 28%, compared with about 73% for amoxicillin-clavulanate-amikacin, 77% for ceftazidime-amikacin, and 80% for piperacillin-tazobactam-amikacin.
In contrast, “Gram-positive isolates generally had reduced levels of resistance,” the authors state. As Dr. Walsh noted, the consortium also did an analysis assessing how much the antibiotic combinations cost and how much payment was deferred to the parents. For example, in Nigeria, the entire cost of treatment is passed down to the parents, “so if they are earning, say, $5.00 a day and the infant needs ceftazidime-amikacin, where the cost per dose is about $6.00 or $7.00 a day, parents can’t afford it,” Dr. Walsh observed.
This part of the conversation, he added, tends to get lost in many studies of antibiotic resistance in LMICs, which is a critical omission, because in many instances, the choice of treatment does come down to affordability. “It’s all very well for the WHO to sit there and say, ampicillin-gentamicin is perfect, but the combination actually doesn’t work in over 70% of the Gram-negative bacteria we looked at in these countries,” Dr. Walsh emphasized.
“The fact is that we have to be a lot more internationally engaged as to what’s actually happening in poorer populations, because unless we do, neonates are going to continue to die,” he said.
Editorial commentary
Commenting on the findings, lead editorialist Luregn Schlapbach, MD, PhD, of University Children’s Hospital Zurich, Switzerland, pointed out that the study has a number of limitations, including a high rate of dropouts from follow-up. This could possibly result in underestimation of neonatal mortality as well as country-specific biases. Nevertheless, Dr. Schlapbach feels that the integration of sequential clinical, genomic, microbiologic, drug, and cost data across a large network in LMIC settings is “exceptional” and will serve to inform “urgently needed” clinical trials in the field of neonatal sepsis.
“At present, increasing global antibiotic resistance is threatening progress against neonatal sepsis, prompting urgency to develop improved measures to effectively prevent and treat life-threatening infections in this high-risk group,” Dr. Schlapbach and colleagues write.
“The findings from the BARNARDS study call for randomized trials comparing mortality benefit and cost efficiency of different antibiotic combinations and management algorithms to safely reduce unnecessary antibiotic exposure for neonatal sepsis,” the editorialists concluded.
The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
First-line treatment of neonatal sepsis in low- and middle-income countries (LMICs) with ampicillin-gentamicin – as recommended by the World Health Organization – needs to be reassessed, a retrospective, observational cohort study suggests. Rates of resistance to this particular antibiotic combination are extremely high in LMICs, and this treatment is unlikely to save many neonatal patients, according to the study’s results.
“The WHO guidelines are over 10 years old, and they are actually based on high-income country data, whereas data reported from low-income countries are reported by private labs, and they do not cater to the lower socioeconomic groups within these countries, which is important data to capture,” Timothy Walsh, MD, University of Oxford, United Kingdom, told this news organization.
“The main take-home message from our data is that ampicillin-gentamicin doesn’t work for most of the Gram-negative isolates we tested, and while there are alternatives, their use is confounded by [a lack of] financial support,” he added.
The study was published online in The Lancet Infectious Diseases.
BARNARDS study
In this substudy of the Burden of Antibiotic Resistance in Neonates from Developing Societies (BARNARDS) study, investigators focused on the effectiveness of antibiotic therapies after taking into account the high prevalence of pathogen resistance to ampicillin-gentamicin. Participating countries included Bangladesh, Ethiopia, India, Nigeria, Pakistan, Rwanda, and South Africa.
“Blood samples were obtained from neonates presenting with clinical signs of sepsis,” the authors note, “and WGS [whole-genome sequencing] and MICs [minimum inhibitory concentrations] for antibiotic treatment were determined for bacterial isolates from culture-confirmed sepsis.” Between Nov. 2015 and Feb. 2018, 36,285 neonates were enrolled into the main BARNARDS study, of whom 9,874 had clinically diagnosed sepsis and 5,749 had antibiotic data.
A total of 2,483 neonates had culture-confirmed sepsis, and WGS data were available for 457 isolates taken from 442 neonates. Slightly over three-quarters of the 5,749 neonates who had antibiotic data received first-line ampicillin-gentamicin. The other three most commonly prescribed antibiotic combinations were ceftazidime-amikacin, piperacillin-tazobactam-amikacin, and amoxicillin-clavulanate-amikacin.
Neonates treated with ceftazidime-amikacin had a 68% lower reported mortality than those treated with ampicillin-gentamicin at an adjusted hazard ratio of 0.32 (95% confidence interval, 0.14-0.72; P = .006), the investigators report. In contrast, no significant differences in mortality rates were reported for neonates treated with amoxicillin-clavulanate-amikacin or piperacillin-tazobactam-amikacin compared to those treated with ampicillin-gentamicin.
Investigators were careful to suggest that mortality effects associated with the different antibiotic combinations might have been confounded by either country-specific effects or underreporting of mortality, as a large proportion of neonates who were treated with ampicillin-gentamicin were followed for fewer than 10 days. However, in an unreported aspect of the same study, neonatal mortality from sepsis dropped by over 50% in two federally funded sites in Nigeria that changed their treatment from the WHO-recommended ampicillin-gentamicin regimen to ceftazidime-amikacin – which Dr. Walsh suggested was an endorsement of ceftazidime-amikacin over ampicillin-gentamicin if ever there was one.
Gram-negative resistance
In looking at resistance patterns to the antibiotic combinations used in these countries, investigators found that almost all Gram-negative isolates tested were “overwhelmingly resistant” to ampicillin, and over 70% of them were resistant to gentamicin as well. Extremely high resistance rates were also found against Staphylococcus spp, which are regarded as intrinsically resistant to ampicillin, rendering it basically useless in this particular treatment setting.
Amikacin had much lower level of resistance, with only about 26% of Gram-negative isolates showing resistance. In terms of coverage against Gram-negative isolates, the lowest level of coverage was provided by ampicillin-gentamicin at slightly over 28%, compared with about 73% for amoxicillin-clavulanate-amikacin, 77% for ceftazidime-amikacin, and 80% for piperacillin-tazobactam-amikacin.
In contrast, “Gram-positive isolates generally had reduced levels of resistance,” the authors state. As Dr. Walsh noted, the consortium also did an analysis assessing how much the antibiotic combinations cost and how much payment was deferred to the parents. For example, in Nigeria, the entire cost of treatment is passed down to the parents, “so if they are earning, say, $5.00 a day and the infant needs ceftazidime-amikacin, where the cost per dose is about $6.00 or $7.00 a day, parents can’t afford it,” Dr. Walsh observed.
This part of the conversation, he added, tends to get lost in many studies of antibiotic resistance in LMICs, which is a critical omission, because in many instances, the choice of treatment does come down to affordability. “It’s all very well for the WHO to sit there and say, ampicillin-gentamicin is perfect, but the combination actually doesn’t work in over 70% of the Gram-negative bacteria we looked at in these countries,” Dr. Walsh emphasized.
“The fact is that we have to be a lot more internationally engaged as to what’s actually happening in poorer populations, because unless we do, neonates are going to continue to die,” he said.
Editorial commentary
Commenting on the findings, lead editorialist Luregn Schlapbach, MD, PhD, of University Children’s Hospital Zurich, Switzerland, pointed out that the study has a number of limitations, including a high rate of dropouts from follow-up. This could possibly result in underestimation of neonatal mortality as well as country-specific biases. Nevertheless, Dr. Schlapbach feels that the integration of sequential clinical, genomic, microbiologic, drug, and cost data across a large network in LMIC settings is “exceptional” and will serve to inform “urgently needed” clinical trials in the field of neonatal sepsis.
“At present, increasing global antibiotic resistance is threatening progress against neonatal sepsis, prompting urgency to develop improved measures to effectively prevent and treat life-threatening infections in this high-risk group,” Dr. Schlapbach and colleagues write.
“The findings from the BARNARDS study call for randomized trials comparing mortality benefit and cost efficiency of different antibiotic combinations and management algorithms to safely reduce unnecessary antibiotic exposure for neonatal sepsis,” the editorialists concluded.
The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Changing terminology in LGBTQ+ spaces: How to keep up with the lingo
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
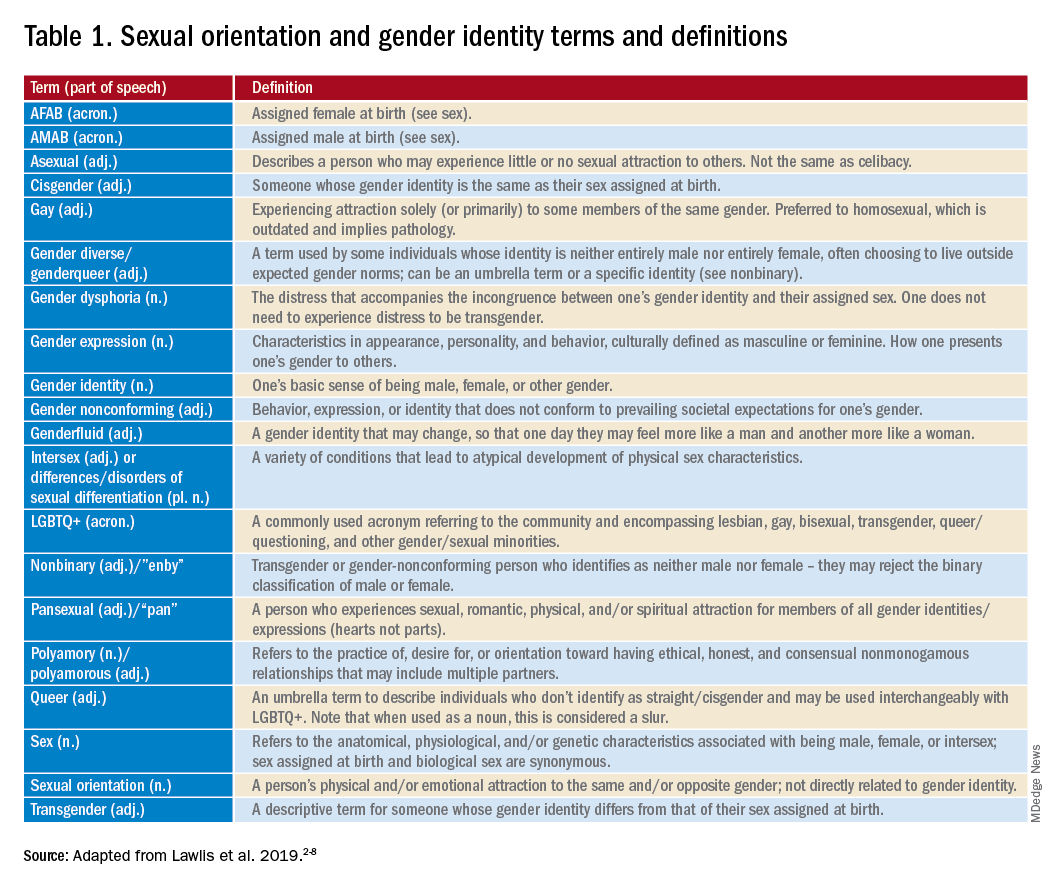
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
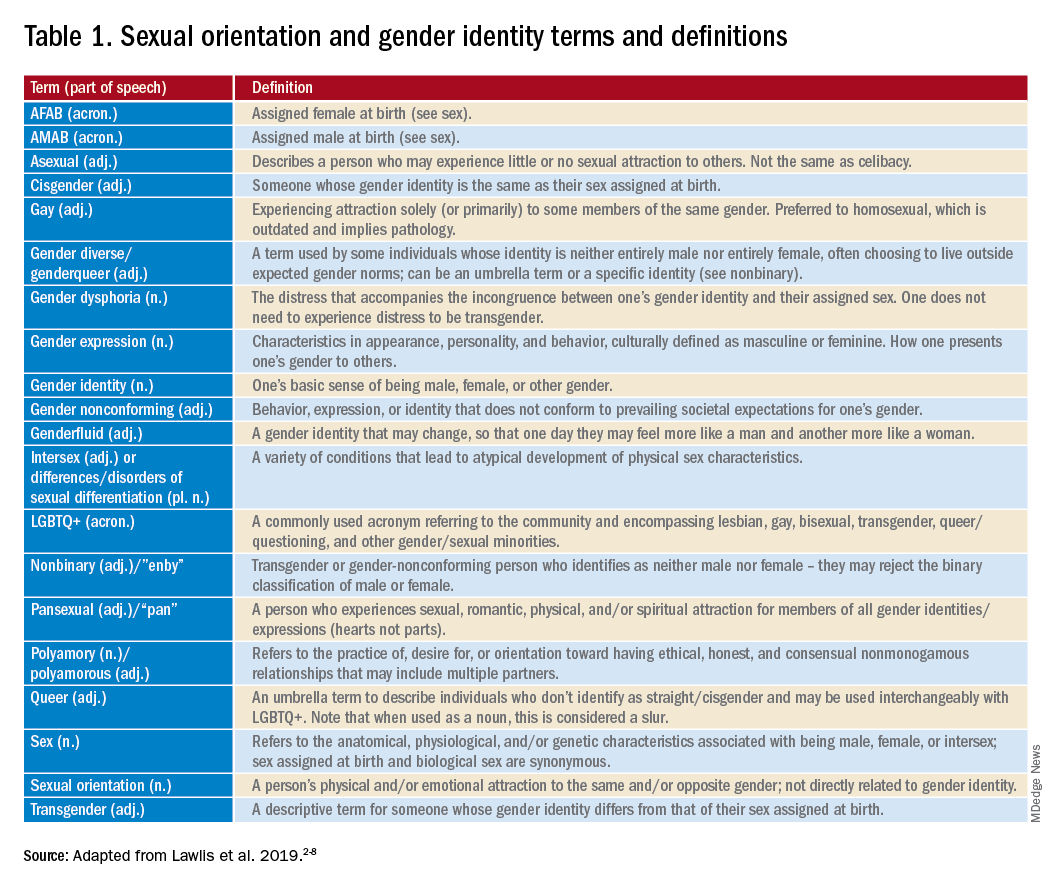
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
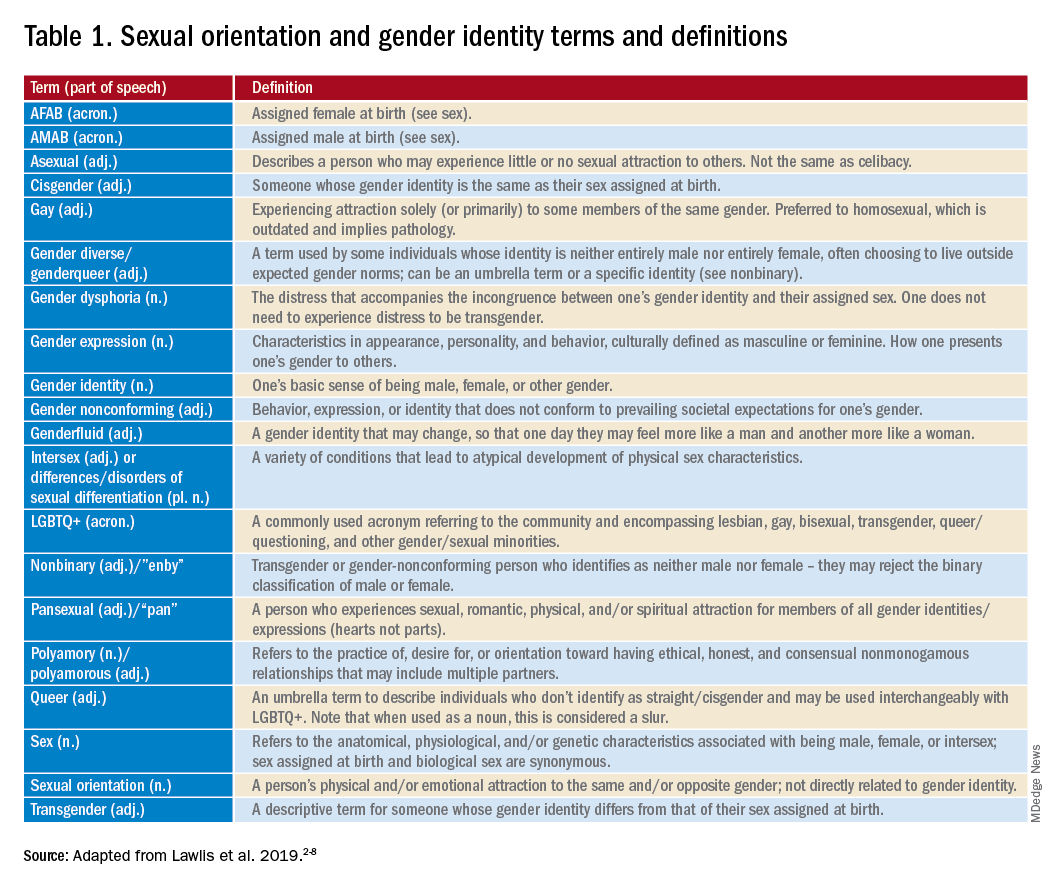
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
The child with hypertension: Diagnosis and management
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
Experts plead for more pediatric telehealth
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.
A specialty group is asking federal and state governments to preserve and expand access to telehealth services for children with developmental and behavioral problems.
Citing the success during the COVID-19 pandemic of telehealth for these patients, the Society for Developmental and Behavioral Pediatrics (SDBP) has issued a position statement in its official journal calling for continued use of video and telephone for home-based diagnostic assessments, medication management follow-ups, and therapeutic interventions for children with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other neurodevelopmental conditions.
“Telehealth offers plenty of opportunities for quick check-ins. It can offer some crisis management opportunities ... to address a parent’s concern about challenging behaviors or navigating school system issues or developmental needs,” lead author Robert D. Keder, MD, assistant professor of pediatrics at University of Connecticut, Farmington, and cochair of SDBP’s Advocacy Committee, told this news organization.
“The video visit does really offer us so much more. It’s so enriching and lets us as providers meet the child in their natural home environment. The real magic of a video visit is we haven’t done house calls as a medical society for decades. But now, literally, the power of telehealth lets us do a house call.”
In the face of the pandemic, emergency government policies allowed care to continue remotely via telehealth, including video and phone calls. The policies have allowed patients to have video visits in their own home, lifted provider licensure requirements for visits across state lines, and allowed reimbursement not only for video visits but also for telephone encounters.
As a result, the field of developmental and behavioral pediatrics (DBP) has recognized telehealth as a viable and useful model of care for children with neurodevelopmental disorders, said Neelkamal Soares, MD, a member of the society’s board and a coauthor of the position paper.
“Telehealth has been helpful in mitigating barriers families often face when attending in-person visits,” such as the lack of transportation and child care, missed work hours, and other issues, said Dr. Soares, professor of pediatric and adolescent medicine at Western Michigan University Stryker in Kalamazoo. At the same time, the growth in the use of the technology has highlighted additional obstacles to equitable access to care, including broadband connectivity, digital literacy, and the availability of interpretation and sign language services, he said.
Dr. Keder said telehealth has enabled him to better help with behavior management by observing children where they are most comfortable. Remote visits also allow him to consider information such as furniture arrangements and how that can affect the patient’s living conditions, and also sibling interactions, learning and homework, eating, and sleep.
Telemedicine conferences enable DBP specialists to facilitate care collaboration with different members of the patient’s care team. Consent from a family and a click of a button allows for therapists, early intervention specialists, teachers, school nurses, or even primary care providers the capacity to participate in a telehealth visit, he said.
Dr. Keder said the future of telehealth is uncertain. The policies from the pandemic may expire in the near term and vary from state to state. The goal of the policy statement is to advocate for legislation and policies that support ongoing, equitable, home-based telehealth care for patients seen by DBP providers while ensuring equitable access to DBP in general.
Kate Benton, PhD, a clinical psychologist with Lurie Children’s Hospital at Northwestern Medicine Central DuPage Hospital in Winfield, Ill., said the society has done an excellent job of explaining the need to maintain telehealth in light of the shortage of pediatricians, clinical psychologists, and other professionals in the field.
“Telehealth has opened new avenues for these patients who otherwise have difficulty seeing specialists. This is a population of children who without telehealth have significant challenges in getting access to care,” she said.
Wendy Fournier, mother of an autistic child and president of the National Autism Association, said telehealth can be beneficial for some individuals with the disorder.
“There are many aspects of in-person doctor visits that can be overwhelming, including bright lights, many people talking, waiting for the doctor, being comfortable with the doctor’s touch, etc.,” Ms. Fournier said in an interview. “All of these things can cause sensory and emotional dysregulation leading to overwhelming anxiety and fear.”
Visits to the doctor can be especially difficult for people who are nonverbal and unable to express their discomfort, said.
“At my daughter’s last medical appointment, she could not stay in the exam room and pulled me out the door. Thankfully, we have an understanding and compassionate physician who finished our appointment in our car. I believe that telehealth visits should remain available as a necessary and vital accommodation for people with disabilities,” Ms. Fournier said.
False equivalence?
Dr. Soares said researchers have attempted to assess the evidence of telehealth benefits in such situations as ADHD, cognitive behavioral therapy, and parent training.
“There is a paucity of published studies that specifically look at different conditions and compare in-person to telehealth visits, but these are ongoing in autism diagnostics and other areas by several SDBP members,” he said. “Stay tuned.”
Dr. Keder added that telehealth will never replace in-person visits, but the availability of this new option gives developmental pediatricians flexibility in strategies in treating and evaluating patients.
“Both are helpful and viable models. In the pandemic, we were forced out of necessity to embrace telehealth,” he said. “Because of this, we are seeing the power and benefits telehealth offers. Now many families like a mixture of alternating in person with telehealth visits.”
The policy statement cites research that finds patients are highly satisfied with telehealth and that telehealth may cost less than in-office visits.
The report stresses that equitable access to devices needed for telehealth visits is a concern because there is disproportionate access to required technology, especially in rural and underserved communities. The Federal Communications Commission has provided grants to eligible families to offset the cost, in part, for a laptop, desktop computer, or tablet. However, more is still needed, the group said.
The position paper calls for:
- Equitable access to the infrastructure and technology for telehealth, including greater access to broadband services in rural and underserved areas.
- Increased access to devices needed to connect children with neurodevelopmental disorders with critical health care services.
- Reimbursement of interpretation services for the people who are deaf and/or have limited English proficiency.
- Mitigation of geographic barriers to accessing DBP care.
- Permitting patients to access telehealth from their home or whichever physical location provides opportunities for safe and timely care, especially for established patients.
- Ensuring more engagement by state medical licensing boards to join the Interstate Medical Licensing Compact to provide care by telehealth when there is already an insufficient geographic distribution of that type of provider in a state, as is being conducted in the field of psychology.
- Ensuring ongoing reimbursement.
- Parity in reimbursement for telehealth in-person visits.
- Increased funding for research looking into outcomes, quality, and effectiveness of telehealth services at the federal and state levels.
“Our organization can work with families to educate lawmakers, insurance administrators, and organizational leaders about the value that telehealth holds in the care of their child and family,” Dr. Soares said. “We can also conduct research to add to the evidence based around the topic to further the science around telehealth outcomes and equivalency to in-person settings.”
“With the current workforce shortage in DBP and behavioral health it is more critical than ever to maintain access to care,” Dr. Keder added. “The pandemic has provided an opportunity to better harness the amazing power of telehealth to allow for access to equitable care for families. We hope that this statement moves legislators, leaders, and voters to continue to advocate for ongoing telehealth at both the state, federal, and organizational levels.”
Dr. Benton, Dr. Keder, and Dr. Soares have disclosed no financial conflicts of interest.
A version of this article first appeared on Medscape.com.