User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Physicians react: Should docs lose their licenses for spreading false COVID information?
Doctors providing “fraudulent” COVID-19 information became a hot-button issue for physicians responding to Medscape’s recent article, "Shouldn’t Doctors Who Spread False COVID-19 Information Lose Their Licenses?”
COVID-19 safety recommendations are set by mainstream medical organizations as new information becomes available, but some doctors consistently oppose advice from the Centers for Disease Control and Prevention and other medical authorities. These physicians often promote off-label, unapproved use of medications for COVID-19 and/or contradict mainstream safety guidelines such as vaccines, masks, and social distancing.
Some medical organizations are concerned that these doctors are hampering efforts to control the highly contagious coronavirus and are, at worst, placing lives in danger with their contrarian views that can spread like wildfire on social media sites. Their words are often used by those who refuse to be vaccinated or wear masks.
State licensing boards have mostly refused to discipline these doctors for making false and/or misleading claims, but as the virus spreads, there are calls to take action against them. However, others worry that such actions would violate free speech and critical thought.
Yes, those doctors are doing wrong
Several physicians took a strong stand against their fellow doctors who are spreading misinformation about COVID-19.
One doctor endorsed the idea of removing licenses for spreading misinformation and called for criminal prosecution: “It should certainly be grounds for cancellation of all licensing (after appropriate examination to rule out acute psychotic episodes, dementia, tumor, etc.) and very likely [include] a charge of manslaughter.”
Another health care provider said, “A person who does not accept science should not, of course, be allowed to practice medicine. One who argues publicly that vaccines and masks don’t work should be prosecuted for crimes ranging from reckless endangerment to attempted murder.”
One reader framed COVID-19 misinformers in stark terms: “These men and women are medical prostitutes. Their medical and surgical colleges [should] have a panel to track in-court testimony and the disinformation they spread ...”
“This is malpractice of the worst kind,” said a clinician. “Public health officials and science are quite clear on [the] best practices for safety during a pandemic, which is killing millions. This is a standard of care.”
“Medical Boards should suspend licenses and give the physician a chance to testify [about] the scientific basis for his comments,” added a health care provider. “Boards involve themselves in all kinds of perceived disciplinary infractions. We are in the midst of a lethal pandemic. I would think that would take precedence over many other issues?”
“I do believe that physicians have the responsibility to speak the truth and have scientifically displayed minds,” said a reader. “Not [to] promulgate misleading, false, and/or unverified information.”
“Any physician, who holds a license, should abide [by] government and state regulation,” asserted a doctor. “He should be disciplined by the board for spreading medical/public misinformation since he is creating potential harm to the population.”
One specialist insisted that “state boards do not do enough to restrict/limit the practice of physicians touting questionable therapies.”
“Any doctor who spreads false information about Covid is hurting our country, our individuals, and our economy and leading to needless deaths,” asserted a physician. “However, there are uncertainties, and where those exist, physicians [should] simply say ‘it is unknown.’”
No, those physicians have a right to speak their beliefs
However, many physicians worried that science and controversial thought were being muzzled.
“Absolutely no,” a doctor stated. “Who judges what is misinformation in this age where debate is canceled? Science advances with challenge, and it’s not about an authority dictating the allowable opinion.”
Another clinician claimed the “truth is very difficult to discern from less-than-truth in a country running on a profit-oriented economic ideology.”
One specialist warned that if disinformation doctors are held responsible, then “that means a lot of doctors” will be “gone” because “almost anything that is written or said about COVID can be contested.”
Another physician warned his colleagues about suppressing new ideas: “To condemn what we didn’t try, or purposefully ignore a different approach because [it] doesn’t agree with our opinion is suppression of information.”
Some doctors insisted the issue extended beyond medicine and into Constitutional freedoms. They also expressed their mistrust in the government to regulate physicians.
“There is a First Amendment in this country,” said one reader. “What you think is false may not be so. The people can listen to whoever they want to and make their own medical decisions. We do not need one iota more of politicizing medicine. Having an MD or DO does not mean you relinquish your First Amendment rights.”
“One of the fundamental problems with a system that allows government to ‘license’ physicians, or any other profession, is that politics inevitably turn to cronyism, and big businesses and wealthy people start controlling the government,” argued a doctor.
One clinician suggested enforcement against health food, drug company commercials, and talk shows: “What about all the [misinformation] at the health food stores and the like. Doctors of natural-whatever? Those info-commercials on tv. How many faxes do I get to ‘approve’ because ‘patients request’ braces and pain-treating expensive compounds advertised on TV? We tolerate those ... What about Dr. Oz and the docs on talk shows claiming BS?”
And the debate goes even further
Some physicians questioned the very notion of claiming “truth.”
“Nobody should be certain that they have the ‘absolute truth,’” said one reader. “In fact, the best clinical insights exceed so-called knowledge by at least one step.”
“Who can determine exactly what is truth?” asked another clinician. “For sure, the ‘Federal Government,’ who ‘is here to help you,’ is not qualified to make such determinations, and who are you to make such a suggestion as to remove someone’s license because they disagree with you? Give me a break!”
Another physician echoed that sentiment: “What’s true and false is often and certainly currently debatable. There are well-qualified physicians (with credentials such as the development of mRNA technology), virologists, and biostatisticians that have valid thoughts on this but do not necessarily agree with the drug company-sponsored journals and news channels (most of them). Their voices should be heard, and they should not lose their licenses. They are doing their work in good conscience.”
One reader commented that he wanted his “freedom of speech,” and offered this defiant advice: “You can take this license and shove it.”
Finally, a physician noted that the political climate has influenced medical directives: “If someone in a leadership role knowingly, and with intent, spread false information, that is wrong. However, during this global pandemic the active and the politics have combined. Red state no mandate, blue state mandate – what does that tell you about American leadership?”
A version of this article first appeared on Medscape.com.
Doctors providing “fraudulent” COVID-19 information became a hot-button issue for physicians responding to Medscape’s recent article, "Shouldn’t Doctors Who Spread False COVID-19 Information Lose Their Licenses?”
COVID-19 safety recommendations are set by mainstream medical organizations as new information becomes available, but some doctors consistently oppose advice from the Centers for Disease Control and Prevention and other medical authorities. These physicians often promote off-label, unapproved use of medications for COVID-19 and/or contradict mainstream safety guidelines such as vaccines, masks, and social distancing.
Some medical organizations are concerned that these doctors are hampering efforts to control the highly contagious coronavirus and are, at worst, placing lives in danger with their contrarian views that can spread like wildfire on social media sites. Their words are often used by those who refuse to be vaccinated or wear masks.
State licensing boards have mostly refused to discipline these doctors for making false and/or misleading claims, but as the virus spreads, there are calls to take action against them. However, others worry that such actions would violate free speech and critical thought.
Yes, those doctors are doing wrong
Several physicians took a strong stand against their fellow doctors who are spreading misinformation about COVID-19.
One doctor endorsed the idea of removing licenses for spreading misinformation and called for criminal prosecution: “It should certainly be grounds for cancellation of all licensing (after appropriate examination to rule out acute psychotic episodes, dementia, tumor, etc.) and very likely [include] a charge of manslaughter.”
Another health care provider said, “A person who does not accept science should not, of course, be allowed to practice medicine. One who argues publicly that vaccines and masks don’t work should be prosecuted for crimes ranging from reckless endangerment to attempted murder.”
One reader framed COVID-19 misinformers in stark terms: “These men and women are medical prostitutes. Their medical and surgical colleges [should] have a panel to track in-court testimony and the disinformation they spread ...”
“This is malpractice of the worst kind,” said a clinician. “Public health officials and science are quite clear on [the] best practices for safety during a pandemic, which is killing millions. This is a standard of care.”
“Medical Boards should suspend licenses and give the physician a chance to testify [about] the scientific basis for his comments,” added a health care provider. “Boards involve themselves in all kinds of perceived disciplinary infractions. We are in the midst of a lethal pandemic. I would think that would take precedence over many other issues?”
“I do believe that physicians have the responsibility to speak the truth and have scientifically displayed minds,” said a reader. “Not [to] promulgate misleading, false, and/or unverified information.”
“Any physician, who holds a license, should abide [by] government and state regulation,” asserted a doctor. “He should be disciplined by the board for spreading medical/public misinformation since he is creating potential harm to the population.”
One specialist insisted that “state boards do not do enough to restrict/limit the practice of physicians touting questionable therapies.”
“Any doctor who spreads false information about Covid is hurting our country, our individuals, and our economy and leading to needless deaths,” asserted a physician. “However, there are uncertainties, and where those exist, physicians [should] simply say ‘it is unknown.’”
No, those physicians have a right to speak their beliefs
However, many physicians worried that science and controversial thought were being muzzled.
“Absolutely no,” a doctor stated. “Who judges what is misinformation in this age where debate is canceled? Science advances with challenge, and it’s not about an authority dictating the allowable opinion.”
Another clinician claimed the “truth is very difficult to discern from less-than-truth in a country running on a profit-oriented economic ideology.”
One specialist warned that if disinformation doctors are held responsible, then “that means a lot of doctors” will be “gone” because “almost anything that is written or said about COVID can be contested.”
Another physician warned his colleagues about suppressing new ideas: “To condemn what we didn’t try, or purposefully ignore a different approach because [it] doesn’t agree with our opinion is suppression of information.”
Some doctors insisted the issue extended beyond medicine and into Constitutional freedoms. They also expressed their mistrust in the government to regulate physicians.
“There is a First Amendment in this country,” said one reader. “What you think is false may not be so. The people can listen to whoever they want to and make their own medical decisions. We do not need one iota more of politicizing medicine. Having an MD or DO does not mean you relinquish your First Amendment rights.”
“One of the fundamental problems with a system that allows government to ‘license’ physicians, or any other profession, is that politics inevitably turn to cronyism, and big businesses and wealthy people start controlling the government,” argued a doctor.
One clinician suggested enforcement against health food, drug company commercials, and talk shows: “What about all the [misinformation] at the health food stores and the like. Doctors of natural-whatever? Those info-commercials on tv. How many faxes do I get to ‘approve’ because ‘patients request’ braces and pain-treating expensive compounds advertised on TV? We tolerate those ... What about Dr. Oz and the docs on talk shows claiming BS?”
And the debate goes even further
Some physicians questioned the very notion of claiming “truth.”
“Nobody should be certain that they have the ‘absolute truth,’” said one reader. “In fact, the best clinical insights exceed so-called knowledge by at least one step.”
“Who can determine exactly what is truth?” asked another clinician. “For sure, the ‘Federal Government,’ who ‘is here to help you,’ is not qualified to make such determinations, and who are you to make such a suggestion as to remove someone’s license because they disagree with you? Give me a break!”
Another physician echoed that sentiment: “What’s true and false is often and certainly currently debatable. There are well-qualified physicians (with credentials such as the development of mRNA technology), virologists, and biostatisticians that have valid thoughts on this but do not necessarily agree with the drug company-sponsored journals and news channels (most of them). Their voices should be heard, and they should not lose their licenses. They are doing their work in good conscience.”
One reader commented that he wanted his “freedom of speech,” and offered this defiant advice: “You can take this license and shove it.”
Finally, a physician noted that the political climate has influenced medical directives: “If someone in a leadership role knowingly, and with intent, spread false information, that is wrong. However, during this global pandemic the active and the politics have combined. Red state no mandate, blue state mandate – what does that tell you about American leadership?”
A version of this article first appeared on Medscape.com.
Doctors providing “fraudulent” COVID-19 information became a hot-button issue for physicians responding to Medscape’s recent article, "Shouldn’t Doctors Who Spread False COVID-19 Information Lose Their Licenses?”
COVID-19 safety recommendations are set by mainstream medical organizations as new information becomes available, but some doctors consistently oppose advice from the Centers for Disease Control and Prevention and other medical authorities. These physicians often promote off-label, unapproved use of medications for COVID-19 and/or contradict mainstream safety guidelines such as vaccines, masks, and social distancing.
Some medical organizations are concerned that these doctors are hampering efforts to control the highly contagious coronavirus and are, at worst, placing lives in danger with their contrarian views that can spread like wildfire on social media sites. Their words are often used by those who refuse to be vaccinated or wear masks.
State licensing boards have mostly refused to discipline these doctors for making false and/or misleading claims, but as the virus spreads, there are calls to take action against them. However, others worry that such actions would violate free speech and critical thought.
Yes, those doctors are doing wrong
Several physicians took a strong stand against their fellow doctors who are spreading misinformation about COVID-19.
One doctor endorsed the idea of removing licenses for spreading misinformation and called for criminal prosecution: “It should certainly be grounds for cancellation of all licensing (after appropriate examination to rule out acute psychotic episodes, dementia, tumor, etc.) and very likely [include] a charge of manslaughter.”
Another health care provider said, “A person who does not accept science should not, of course, be allowed to practice medicine. One who argues publicly that vaccines and masks don’t work should be prosecuted for crimes ranging from reckless endangerment to attempted murder.”
One reader framed COVID-19 misinformers in stark terms: “These men and women are medical prostitutes. Their medical and surgical colleges [should] have a panel to track in-court testimony and the disinformation they spread ...”
“This is malpractice of the worst kind,” said a clinician. “Public health officials and science are quite clear on [the] best practices for safety during a pandemic, which is killing millions. This is a standard of care.”
“Medical Boards should suspend licenses and give the physician a chance to testify [about] the scientific basis for his comments,” added a health care provider. “Boards involve themselves in all kinds of perceived disciplinary infractions. We are in the midst of a lethal pandemic. I would think that would take precedence over many other issues?”
“I do believe that physicians have the responsibility to speak the truth and have scientifically displayed minds,” said a reader. “Not [to] promulgate misleading, false, and/or unverified information.”
“Any physician, who holds a license, should abide [by] government and state regulation,” asserted a doctor. “He should be disciplined by the board for spreading medical/public misinformation since he is creating potential harm to the population.”
One specialist insisted that “state boards do not do enough to restrict/limit the practice of physicians touting questionable therapies.”
“Any doctor who spreads false information about Covid is hurting our country, our individuals, and our economy and leading to needless deaths,” asserted a physician. “However, there are uncertainties, and where those exist, physicians [should] simply say ‘it is unknown.’”
No, those physicians have a right to speak their beliefs
However, many physicians worried that science and controversial thought were being muzzled.
“Absolutely no,” a doctor stated. “Who judges what is misinformation in this age where debate is canceled? Science advances with challenge, and it’s not about an authority dictating the allowable opinion.”
Another clinician claimed the “truth is very difficult to discern from less-than-truth in a country running on a profit-oriented economic ideology.”
One specialist warned that if disinformation doctors are held responsible, then “that means a lot of doctors” will be “gone” because “almost anything that is written or said about COVID can be contested.”
Another physician warned his colleagues about suppressing new ideas: “To condemn what we didn’t try, or purposefully ignore a different approach because [it] doesn’t agree with our opinion is suppression of information.”
Some doctors insisted the issue extended beyond medicine and into Constitutional freedoms. They also expressed their mistrust in the government to regulate physicians.
“There is a First Amendment in this country,” said one reader. “What you think is false may not be so. The people can listen to whoever they want to and make their own medical decisions. We do not need one iota more of politicizing medicine. Having an MD or DO does not mean you relinquish your First Amendment rights.”
“One of the fundamental problems with a system that allows government to ‘license’ physicians, or any other profession, is that politics inevitably turn to cronyism, and big businesses and wealthy people start controlling the government,” argued a doctor.
One clinician suggested enforcement against health food, drug company commercials, and talk shows: “What about all the [misinformation] at the health food stores and the like. Doctors of natural-whatever? Those info-commercials on tv. How many faxes do I get to ‘approve’ because ‘patients request’ braces and pain-treating expensive compounds advertised on TV? We tolerate those ... What about Dr. Oz and the docs on talk shows claiming BS?”
And the debate goes even further
Some physicians questioned the very notion of claiming “truth.”
“Nobody should be certain that they have the ‘absolute truth,’” said one reader. “In fact, the best clinical insights exceed so-called knowledge by at least one step.”
“Who can determine exactly what is truth?” asked another clinician. “For sure, the ‘Federal Government,’ who ‘is here to help you,’ is not qualified to make such determinations, and who are you to make such a suggestion as to remove someone’s license because they disagree with you? Give me a break!”
Another physician echoed that sentiment: “What’s true and false is often and certainly currently debatable. There are well-qualified physicians (with credentials such as the development of mRNA technology), virologists, and biostatisticians that have valid thoughts on this but do not necessarily agree with the drug company-sponsored journals and news channels (most of them). Their voices should be heard, and they should not lose their licenses. They are doing their work in good conscience.”
One reader commented that he wanted his “freedom of speech,” and offered this defiant advice: “You can take this license and shove it.”
Finally, a physician noted that the political climate has influenced medical directives: “If someone in a leadership role knowingly, and with intent, spread false information, that is wrong. However, during this global pandemic the active and the politics have combined. Red state no mandate, blue state mandate – what does that tell you about American leadership?”
A version of this article first appeared on Medscape.com.
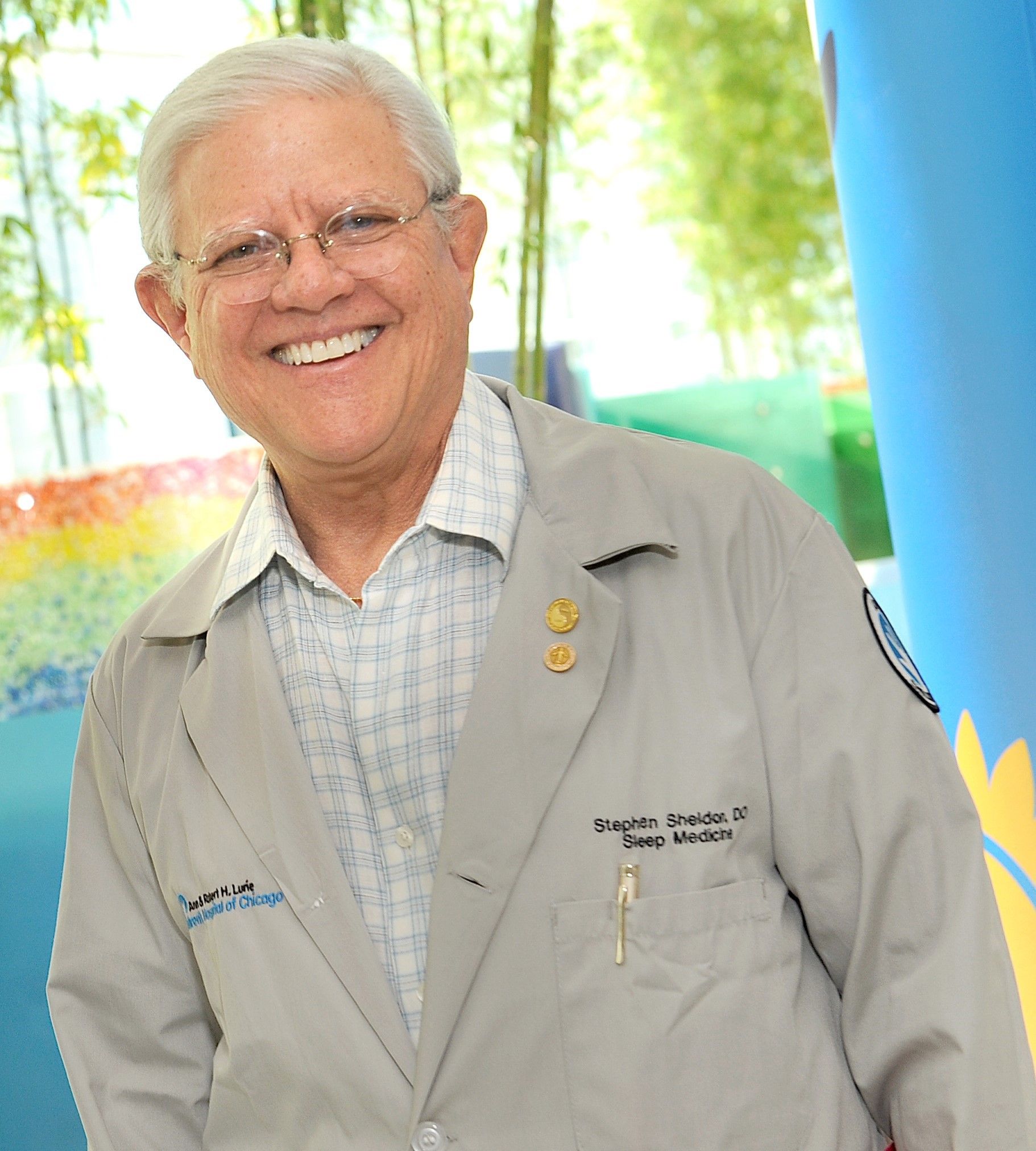
Sorting out sleep complaints in children with AD can be complex
according to Stephen H. Sheldon, DO.
“They wake up frequently,” Dr. Sheldon, professor of pediatrics and neurology at Northwestern University, Chicago, said during the Revolutionizing Atopic Dermatitis symposium. “They may not stay up for long periods of time, but they move about often. There’s a loss of about 50 minutes of sleep per night in children with AD. This loss can result in significant sleep debt the following day. They have difficulty settling at night. Once they get into bed, they have difficulty falling asleep, and many of them have difficulty staying asleep.”
At the sleep medicine center at Lurie Children’s Hospital of Chicago, he and his colleagues have observed that some children with AD complain of difficulty with limb movements. “Part of the issue has been that they have been diagnosed with different sleep-related disorders, such as period limb movement disorder, restless leg syndrome, and growing pain,” Dr. Sheldon said. “Often, they do not know how to describe the manifestations of their leg discomfort in restless leg syndrome and period limb movement disorder and limb movements of sleep.”
Children who complain of growing pains say that their legs hurt, he continued. Sometimes they’ll say that they feel like spiders are crawling on their legs, or that their legs itch, but they often say they have pain in their legs that wakes them up and keeps them from keeping their legs still.
According to the American Academy of Sleep Medicine, periodic limb movement disorder of sleep is characterized by frequent limb movements that last at least 0.5 seconds and are separated by no more than 90 seconds. “They’re four movements in a row that are at least 5 seconds apart,” Dr. Sheldon said.
Interestingly, he added, children who have limb movement disorder have symptoms during the day, similar to adults. “But we see many children with periodic limb movements of sleep whose arms and legs are moving all night, and they don’t have many symptoms during the day.” These children may have difficulty falling or staying asleep, but do not fulfill all of the American Academy of Sleep Medicine criteria for diagnosis of periodic limb movement disorder, he added.
In 2018, Lourdes M. DelRosso, MD, EdD, of Seattle Children’s Hospital, and colleagues described a new sleep problem they termed restless sleep disorder: those who do not fit the criteria for any other sleep disorder but have daytime impairment.
“On video they have very frequent movements – more than five movements an hour of major body activity,” Dr. Sheldon explained. “They’ll move their trunk, their legs, and reposition themselves. We have found that there are many children who presented to the sleep disorder center with restless sleep, limb movement disorder, periodic limb movements of sleep, and daytime symptoms that would fulfill the criteria of periodic limb movement disorder but also have atopic dermatitis.”
Recently, Dr. Sheldon and his colleagues used polysomnographic variables to study children who presented to Lurie Children’s Hospital with AD and symptoms such as difficulty maintaining sleep and snoring with allergic rhinitis. They found that there were increased periods of being awake after the onset of sleep, “meaning the children fell asleep fairly easily in the beginning of the night but they had significant wake after they fell asleep,” he said. “They would wake up in the middle of the night and stay awake for long periods of time – either one long session or multiple shorter sessions throughout the night. They had increased total limb movements per hour of sleep. This means that their limb movements were greater than five events per hour of sleep and it resulted in restless sleep and limb movements that would fulfill the criteria of periodic limb movement disorder.”
Most of these children had mild to moderate AD, he continued. “We feel that the sensory afferent loop in these youngsters doesn’t really turn off completely when they’re asleep. This is ripe for further study, but it makes intuitive sense that if the sensory afferent loop continues during sleep, it may affect the arousal system significantly.”
Dr. Sheldon recommended that any child who presents with a diagnosis of periodic limb movement disorder, periodic limb movements of sleep, or restless sleep disorder should be evaluated for AD. “The treatment then, would first require differentiation between periodic limb movement disorder of sleep and AD. Both should be addressed at the same time in order to solve the child’s daytime AD problem as well as the sleep-related issues that occur with an AD diagnosis.”
He reported having no financial disclosures.
according to Stephen H. Sheldon, DO.
“They wake up frequently,” Dr. Sheldon, professor of pediatrics and neurology at Northwestern University, Chicago, said during the Revolutionizing Atopic Dermatitis symposium. “They may not stay up for long periods of time, but they move about often. There’s a loss of about 50 minutes of sleep per night in children with AD. This loss can result in significant sleep debt the following day. They have difficulty settling at night. Once they get into bed, they have difficulty falling asleep, and many of them have difficulty staying asleep.”
At the sleep medicine center at Lurie Children’s Hospital of Chicago, he and his colleagues have observed that some children with AD complain of difficulty with limb movements. “Part of the issue has been that they have been diagnosed with different sleep-related disorders, such as period limb movement disorder, restless leg syndrome, and growing pain,” Dr. Sheldon said. “Often, they do not know how to describe the manifestations of their leg discomfort in restless leg syndrome and period limb movement disorder and limb movements of sleep.”
Children who complain of growing pains say that their legs hurt, he continued. Sometimes they’ll say that they feel like spiders are crawling on their legs, or that their legs itch, but they often say they have pain in their legs that wakes them up and keeps them from keeping their legs still.
According to the American Academy of Sleep Medicine, periodic limb movement disorder of sleep is characterized by frequent limb movements that last at least 0.5 seconds and are separated by no more than 90 seconds. “They’re four movements in a row that are at least 5 seconds apart,” Dr. Sheldon said.
Interestingly, he added, children who have limb movement disorder have symptoms during the day, similar to adults. “But we see many children with periodic limb movements of sleep whose arms and legs are moving all night, and they don’t have many symptoms during the day.” These children may have difficulty falling or staying asleep, but do not fulfill all of the American Academy of Sleep Medicine criteria for diagnosis of periodic limb movement disorder, he added.
In 2018, Lourdes M. DelRosso, MD, EdD, of Seattle Children’s Hospital, and colleagues described a new sleep problem they termed restless sleep disorder: those who do not fit the criteria for any other sleep disorder but have daytime impairment.
“On video they have very frequent movements – more than five movements an hour of major body activity,” Dr. Sheldon explained. “They’ll move their trunk, their legs, and reposition themselves. We have found that there are many children who presented to the sleep disorder center with restless sleep, limb movement disorder, periodic limb movements of sleep, and daytime symptoms that would fulfill the criteria of periodic limb movement disorder but also have atopic dermatitis.”
Recently, Dr. Sheldon and his colleagues used polysomnographic variables to study children who presented to Lurie Children’s Hospital with AD and symptoms such as difficulty maintaining sleep and snoring with allergic rhinitis. They found that there were increased periods of being awake after the onset of sleep, “meaning the children fell asleep fairly easily in the beginning of the night but they had significant wake after they fell asleep,” he said. “They would wake up in the middle of the night and stay awake for long periods of time – either one long session or multiple shorter sessions throughout the night. They had increased total limb movements per hour of sleep. This means that their limb movements were greater than five events per hour of sleep and it resulted in restless sleep and limb movements that would fulfill the criteria of periodic limb movement disorder.”
Most of these children had mild to moderate AD, he continued. “We feel that the sensory afferent loop in these youngsters doesn’t really turn off completely when they’re asleep. This is ripe for further study, but it makes intuitive sense that if the sensory afferent loop continues during sleep, it may affect the arousal system significantly.”
Dr. Sheldon recommended that any child who presents with a diagnosis of periodic limb movement disorder, periodic limb movements of sleep, or restless sleep disorder should be evaluated for AD. “The treatment then, would first require differentiation between periodic limb movement disorder of sleep and AD. Both should be addressed at the same time in order to solve the child’s daytime AD problem as well as the sleep-related issues that occur with an AD diagnosis.”
He reported having no financial disclosures.
according to Stephen H. Sheldon, DO.
“They wake up frequently,” Dr. Sheldon, professor of pediatrics and neurology at Northwestern University, Chicago, said during the Revolutionizing Atopic Dermatitis symposium. “They may not stay up for long periods of time, but they move about often. There’s a loss of about 50 minutes of sleep per night in children with AD. This loss can result in significant sleep debt the following day. They have difficulty settling at night. Once they get into bed, they have difficulty falling asleep, and many of them have difficulty staying asleep.”
At the sleep medicine center at Lurie Children’s Hospital of Chicago, he and his colleagues have observed that some children with AD complain of difficulty with limb movements. “Part of the issue has been that they have been diagnosed with different sleep-related disorders, such as period limb movement disorder, restless leg syndrome, and growing pain,” Dr. Sheldon said. “Often, they do not know how to describe the manifestations of their leg discomfort in restless leg syndrome and period limb movement disorder and limb movements of sleep.”
Children who complain of growing pains say that their legs hurt, he continued. Sometimes they’ll say that they feel like spiders are crawling on their legs, or that their legs itch, but they often say they have pain in their legs that wakes them up and keeps them from keeping their legs still.
According to the American Academy of Sleep Medicine, periodic limb movement disorder of sleep is characterized by frequent limb movements that last at least 0.5 seconds and are separated by no more than 90 seconds. “They’re four movements in a row that are at least 5 seconds apart,” Dr. Sheldon said.
Interestingly, he added, children who have limb movement disorder have symptoms during the day, similar to adults. “But we see many children with periodic limb movements of sleep whose arms and legs are moving all night, and they don’t have many symptoms during the day.” These children may have difficulty falling or staying asleep, but do not fulfill all of the American Academy of Sleep Medicine criteria for diagnosis of periodic limb movement disorder, he added.
In 2018, Lourdes M. DelRosso, MD, EdD, of Seattle Children’s Hospital, and colleagues described a new sleep problem they termed restless sleep disorder: those who do not fit the criteria for any other sleep disorder but have daytime impairment.
“On video they have very frequent movements – more than five movements an hour of major body activity,” Dr. Sheldon explained. “They’ll move their trunk, their legs, and reposition themselves. We have found that there are many children who presented to the sleep disorder center with restless sleep, limb movement disorder, periodic limb movements of sleep, and daytime symptoms that would fulfill the criteria of periodic limb movement disorder but also have atopic dermatitis.”
Recently, Dr. Sheldon and his colleagues used polysomnographic variables to study children who presented to Lurie Children’s Hospital with AD and symptoms such as difficulty maintaining sleep and snoring with allergic rhinitis. They found that there were increased periods of being awake after the onset of sleep, “meaning the children fell asleep fairly easily in the beginning of the night but they had significant wake after they fell asleep,” he said. “They would wake up in the middle of the night and stay awake for long periods of time – either one long session or multiple shorter sessions throughout the night. They had increased total limb movements per hour of sleep. This means that their limb movements were greater than five events per hour of sleep and it resulted in restless sleep and limb movements that would fulfill the criteria of periodic limb movement disorder.”
Most of these children had mild to moderate AD, he continued. “We feel that the sensory afferent loop in these youngsters doesn’t really turn off completely when they’re asleep. This is ripe for further study, but it makes intuitive sense that if the sensory afferent loop continues during sleep, it may affect the arousal system significantly.”
Dr. Sheldon recommended that any child who presents with a diagnosis of periodic limb movement disorder, periodic limb movements of sleep, or restless sleep disorder should be evaluated for AD. “The treatment then, would first require differentiation between periodic limb movement disorder of sleep and AD. Both should be addressed at the same time in order to solve the child’s daytime AD problem as well as the sleep-related issues that occur with an AD diagnosis.”
He reported having no financial disclosures.
FROM RAD 2021
Physician as trusted counselor
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Pediatricians play many roles as they fulfill their duties and responsibilities. Among these is the role of trusted counselor.
A pediatrician is a risk manager. Not the risk manager at a brokerage firm assessing financial risks. Not the hospital lawyer providing legal advice to minimize lawsuits against the hospital. The pediatrician, as risk manager, is a fiduciary, confidant, partner, and guide for parents seeking to protect and maximize the health of their children.
The practice of pediatrics deals with many low-probability, high-impact threats. This begins before birth. The obstetrician has already ordered a litany of prenatal screens, blood tests, and ultrasounds. Many of these have a positive predictive value of less than 20%. That means the alarming positive results are wrong more than 80% of the time. Tests done purportedly to reassure the parents are likely to falsely terrify them. This devilish process continues immediately after birth. The newborns are subjected to a wide variety of screening tests that they must pass before being stamped USDA Prime baby. Early in my career, a thorough newborn physical exam was the key means of identifying problems. Modern medicine employs a wide variety of blood tests, a hearing screen, a pulse ox check, and a transcutaneous bilirubin test before discharge. It is a gauntlet that few escape unscathed. Even the totally normal infant is going to flunk a handful of these screens. Then the nursery doctor is ready to erect additional hoops to jump through. Too big or too small? You need glucose checks. Breech presentation? A hip ultrasound. Too long in labor? Blood tests. Too pale or too ruddy? Blood tests. Not acting quite right? Temperature too high? Temperature too low? Too irritable? Too lethargic? Baby, you’ve hit the jackpot for extra blood tests, an app to estimate the risk of early-onset sepsis, and maybe a trip to the NICU.
Many of these protocols have poor positive predictive value results that are not easy to explain to lay people. The ideas are not easily taught to medical students. Those results can be even harder to communicate to new parents with health care careers. A little knowledge goes a long ways toward long, sleepless nights of worrying even though the baby is just fine. Even cute. Snuggly. A good baby! Parents, hug your baby! Feed the baby! Let the professional do most of the worrying.
What does a professional worrier offer? First, a comprehension of the science. The professional understands sensitivity and specificity, false-positive rates, prevalence, and positive predictive value. Second, particular knowledge of the various tests involved, including the confirmatory tests and the risk-benefit of treatment. Third, experienced clinical judgment that knows that lotteries are bad investments even though two people are splitting a $600 million lottery win this week. Most people don’t emotionally cope with small risks. Fourth, the ability to do values clarification. There is not a one-size-fits-all bedside approach in pediatrics. Parents have differing expectations, differing levels of risk aversion, and different methods for handling anxiety. First-time parents may be very risk intolerant with their baby. Some people deal with fear by seeking more information. Others are looking for evidence that the expert physician is committed to compassionately providing whatever is best for their child.
How has medicine evolved recently? I will highlight four items. First, as described earlier, there has been a large increase in the number of these screens that will be failed. Typical office practice continues the methodology with well child exams and developmental screening. Second, many screens have been introduced that have very low positive predictive value. This leads to many anxious parents who will benefit from pediatricians with the bedside manner to guide the parents and their precious baby through this maze of scientific interventions. The science is difficult enough to master during training. It takes more time to learn the art of counseling parents, listening to their concerns, and earning their trust. That art is practiced in face-to-face encounters with the parents. The classic approach to residency training limits the opportunity to observe and mentor the knowledge, skills, and empathy of a good bedside manner.
A third evolution, more recent, has been the widespread pollution of scientific knowledge with misinformation and disinformation through social media. I addressed that issue in my columns in January and March 2019.
Fourth, most recently, I believe the pandemic has emphasized to the public that nothing in life is totally risk free. Extreme efforts to reduce risk produce unwanted consequences. There is a window of opportunity here to work with parents and patients to build relationships that help people to assess risks and make more rational and beneficial choices. For example, when is the risk of meningitis in a febrile young infant low enough to manage at home? The risk will never be zero. But admission to the hospital “just in case” is not risk free either. People are acutely aware of that right now.
Health care professionals can position themselves as the trusted source of health information specific to a particular person’s situation. Health care professionals can be competent, committed, and compassionate listeners to what really worries people. In this way, we manage risk. This role also involves addressing the mental health crisis causing so much suicide and addiction. Severe problems should be referred to specialists, but I anticipate in the near future that most pediatricians will require more skills dealing with risk and anxiety rather than microbes.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The death of expertise
Unless your social circle is packed with medical professionals, I suspect you are the go-to gal/guy when there is a question about the pandemic. Seated around the fire pit trying to stay warm and socially distanced, inevitably the discussion will turn to COVID. Someone will report something they have read about vaccine side effects or the appropriate timing of isolation or quarantine and then turn to me assuming that I have inside information and ask: “But Will you know all about that. Tell us what have you heard.”
By now, well into our second year of the pandemic, my friends and neighbors should have come to expect my usual answer. “I don’t really know any more about this than you have read on the Internet or seen on television.” I am flattered that folks keep asking for my observations. I guess old habits die slowly. Although I usually introduce myself as an ex-pediatrician, the “doctor” descriptor still seems to command some respect, whether it is deserved or not.
It is not just my waning ability to speak authoritatively about the pandemic that has put expertise at death’s door. Although my formal medical education is more than a half-century old, like most physicians I have tried to stay abreast of what’s happening in health care. Keeping up to date with the new developments in pathophysiology and pharmacology does take some work, but the pandemic has shone a spotlight on how quickly these changes can occur.
With the pandemic, a sense of urgency has thrust onto the world stage opinions that in the past might have been quietly held theories based on preliminary studies. However, even the most careful scientists who might otherwise have been content to patiently wait for peer review are sharing their findings prematurely with international news sources and on social media. Not surprisingly, this rush to share has generated confusion and concern and in many cases resulted in retractions or corrections. Even more importantly, it has made us all skeptical about who these “experts” are, making often disproven pronouncements.
While my friends still persist in politely asking my opinion based on the same reports we are all reading on the Internet, I sense the nation as a whole has become wary of claimed expertise. I haven’t done a Google search but I wouldn’t be surprised if “expert” gets far fewer hits than the term “so-called expert.”
Even before we were engulfed by the pandemic, there has been an unfortunate phenomenon in which health care providers and other scientists are parlaying their degrees to promote products with little if any proven efficacy. Of course, this country has a long history of snake oil salesmen making their rounds. However, the electronic media and the Internet have increased the power to persuade so that we are awash in so-called experts. Many good scientists, in an attempt to be helpful, have succumbed to the sin of impatience. And there are a few who had never earned the moniker “expert.”
I hope that expertise returns to the landscape when the pandemic abates. But, I fear it may be a while.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Unless your social circle is packed with medical professionals, I suspect you are the go-to gal/guy when there is a question about the pandemic. Seated around the fire pit trying to stay warm and socially distanced, inevitably the discussion will turn to COVID. Someone will report something they have read about vaccine side effects or the appropriate timing of isolation or quarantine and then turn to me assuming that I have inside information and ask: “But Will you know all about that. Tell us what have you heard.”
By now, well into our second year of the pandemic, my friends and neighbors should have come to expect my usual answer. “I don’t really know any more about this than you have read on the Internet or seen on television.” I am flattered that folks keep asking for my observations. I guess old habits die slowly. Although I usually introduce myself as an ex-pediatrician, the “doctor” descriptor still seems to command some respect, whether it is deserved or not.
It is not just my waning ability to speak authoritatively about the pandemic that has put expertise at death’s door. Although my formal medical education is more than a half-century old, like most physicians I have tried to stay abreast of what’s happening in health care. Keeping up to date with the new developments in pathophysiology and pharmacology does take some work, but the pandemic has shone a spotlight on how quickly these changes can occur.
With the pandemic, a sense of urgency has thrust onto the world stage opinions that in the past might have been quietly held theories based on preliminary studies. However, even the most careful scientists who might otherwise have been content to patiently wait for peer review are sharing their findings prematurely with international news sources and on social media. Not surprisingly, this rush to share has generated confusion and concern and in many cases resulted in retractions or corrections. Even more importantly, it has made us all skeptical about who these “experts” are, making often disproven pronouncements.
While my friends still persist in politely asking my opinion based on the same reports we are all reading on the Internet, I sense the nation as a whole has become wary of claimed expertise. I haven’t done a Google search but I wouldn’t be surprised if “expert” gets far fewer hits than the term “so-called expert.”
Even before we were engulfed by the pandemic, there has been an unfortunate phenomenon in which health care providers and other scientists are parlaying their degrees to promote products with little if any proven efficacy. Of course, this country has a long history of snake oil salesmen making their rounds. However, the electronic media and the Internet have increased the power to persuade so that we are awash in so-called experts. Many good scientists, in an attempt to be helpful, have succumbed to the sin of impatience. And there are a few who had never earned the moniker “expert.”
I hope that expertise returns to the landscape when the pandemic abates. But, I fear it may be a while.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Unless your social circle is packed with medical professionals, I suspect you are the go-to gal/guy when there is a question about the pandemic. Seated around the fire pit trying to stay warm and socially distanced, inevitably the discussion will turn to COVID. Someone will report something they have read about vaccine side effects or the appropriate timing of isolation or quarantine and then turn to me assuming that I have inside information and ask: “But Will you know all about that. Tell us what have you heard.”
By now, well into our second year of the pandemic, my friends and neighbors should have come to expect my usual answer. “I don’t really know any more about this than you have read on the Internet or seen on television.” I am flattered that folks keep asking for my observations. I guess old habits die slowly. Although I usually introduce myself as an ex-pediatrician, the “doctor” descriptor still seems to command some respect, whether it is deserved or not.
It is not just my waning ability to speak authoritatively about the pandemic that has put expertise at death’s door. Although my formal medical education is more than a half-century old, like most physicians I have tried to stay abreast of what’s happening in health care. Keeping up to date with the new developments in pathophysiology and pharmacology does take some work, but the pandemic has shone a spotlight on how quickly these changes can occur.
With the pandemic, a sense of urgency has thrust onto the world stage opinions that in the past might have been quietly held theories based on preliminary studies. However, even the most careful scientists who might otherwise have been content to patiently wait for peer review are sharing their findings prematurely with international news sources and on social media. Not surprisingly, this rush to share has generated confusion and concern and in many cases resulted in retractions or corrections. Even more importantly, it has made us all skeptical about who these “experts” are, making often disproven pronouncements.
While my friends still persist in politely asking my opinion based on the same reports we are all reading on the Internet, I sense the nation as a whole has become wary of claimed expertise. I haven’t done a Google search but I wouldn’t be surprised if “expert” gets far fewer hits than the term “so-called expert.”
Even before we were engulfed by the pandemic, there has been an unfortunate phenomenon in which health care providers and other scientists are parlaying their degrees to promote products with little if any proven efficacy. Of course, this country has a long history of snake oil salesmen making their rounds. However, the electronic media and the Internet have increased the power to persuade so that we are awash in so-called experts. Many good scientists, in an attempt to be helpful, have succumbed to the sin of impatience. And there are a few who had never earned the moniker “expert.”
I hope that expertise returns to the landscape when the pandemic abates. But, I fear it may be a while.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Pediatric depression and parents
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
In October of 2021, the American Academy of Child and Adolescent Psychiatry, the American Academy of Pediatrics, and the Children’s Hospital Association jointly declared a National State of Emergency in Children’s Mental Health and called on policy makers to address a host of challenges that have impeded access to effective mental health care for youth.
In November, we wrote about how pediatricians may increase their use of screening for adolescent depression and initiate treatment when appropriate.
Now we complement that piece with guidance you may offer the parents of your depressed adolescent patients. Adolescent depression is a common pediatric disorder, especially in the COVID-19 era when so many relationships and activities have been limited or cut off. With treatment, most adolescents recover. Accepting that it may be taking longer to find a therapist, you can make treatment recommendations, support the teenager and parents, address safety concerns and, if the depression is of moderate or more serious severity, start medications. Parents are your natural partners as they are concerned about their children’s health and safety and eager for guidance on how to best support their recovery.
Adolescence is a time in which parents transition to more of a consulting than a controlling posture with their children, but illness calls for a shift toward setting rules and routines that will support health and healing. Prepare both the teenager (in a 1:1 discussion) and parents for this temporary shift, and for some teenagers, expect resistance. Depression will make the teenager more unhappy and irritable. It also causes withdrawal, by sapping energy and making one feel unwelcome at activities, believing his or her presence will be a burden to others. Treatment includes something called “behavioral activation,” or continuous nudging, to keep the patient involved in social, intellectual, and physical activities. Parents (and siblings) are the keys to this behavioral activation, whether nudging to participate in a board game or a walk. Reassure parents they should not take it personally when their teen resists, and not be discouraged if they fail sometimes. Their focus is on calmly, warmly, and repeatedly prompting their children with nudges toward these routines and activities. They should be ready to remind them why they are “nagging,” framing these efforts explicitly as supporting recovery from depression. If possible, applying these rules to everyone at home will help. They need to avoid being drawn into conflict, focusing instead on staying connected to their teens. Their task is to keep planning and cajoling, giving their children multiple opportunities to participate, pushing back against depression’s gravitational pull for total withdrawal.
Sleep
One of the most important thing parents can do for their depressed adolescents is to support their healthy restful sleep. During adolescence, the timing of sleep naturally shifts later, and the need for restful sleep increases. Working against the demands of homework, extracurricular activities, and social connections, sleep often suffers during adolescence. Further sleep disruptions, including difficulty falling asleep and frequent awakening during sleep or in the early morning, are typical of depression. Restful sleep is instrumental to recovery, and parents need to help their depressed teens set good sleep habits. This includes setting a time for bed that is realistic and consistent and turning off screens 30 minutes before lights out. A soothing, consistent bedtime routine, including a hot shower and reading in bed, is a powerful cue for sleep. Getting daily exercise and avoiding a heavy meal and caffeine in the hours before bed supports both falling and staying asleep. Having light reading near bed (magazines or comics) instead of screens can provide a way to pass 30 minutes if they wake up during the night (ideally reading out of bed), one that will not make it harder for them to go back to sleep. Finally, teens should not be allowed to spend all day in bed or nap in the afternoon. This may be the hardest task for parents, as adolescents naturally treat their beds like their center of operations and depression lowers their energy and initiative. If parents set these rules and routines for all members of the family, it can improve the chances that their depressed adolescents may begin to return to healthy sleep.
Exercise
Vigorous exercise (for 20 minutes three times weekly) is as effective as SSRIs in treating mild to moderate depression. Even in severe depression, exercise may accelerate recovery and certainly contributes to returning to restful sleep and a feeling of improved energy. Inviting their depressed teens to join them on a trip to the gym may seem like a fool’s errand to parents, but they should prioritize getting their children moving. Don’t offer choices or ask what activity they would like to do. Most invitations will be met with “no, thanks” (or probably something less polite). Instead, initiate simple activities and then cajole the children with “let’s go!” They should use loving persistence to get them out the door. Parents are the experts on their children and will know if there is an activity that they are more likely to enjoy. Make any activities group ones, easy to start and not too long. They could initiate family walks or bike rides in their neighborhood. If it helps, they can blame you, “these are doctor’s orders!” This approach of warm persistence should be applied across the board, helping their depressed teens participate in mealtimes and other activities. Prepare parents that this can feel unnatural, if they have been letting their healthy teenagers have more space and independence and less time in family activities.
Social connections
Behavioral activation includes keeping a depressed teen engaged in social activities. Friendships are a potent motivator in the lives of healthy adolescents. If depressed teens can stay connected to close friends, it is a powerful force for recovery. Find out if their friends know about their depression, whom do they trust to tell about it? Help them find comfortable language to speak about their depression with trusted friends. Parents can use their behavioral activation strategies to prompt their teenagers to participate in social activities. If texting, video chatting, or social media platforms are how they stay connected with close friends, support their use of these platforms. But be mindful that social media promotes social comparison over connection, and depression sets them up to feel less than others even without assistance. Parents should support real time with their friends in small groups, for short periods during the time of day when they have the most energy.
Safety
Suicide is the second leading cause of death for adolescents in the United States, and the rate of attempted and completed suicide in adolescents has been steadily climbing over the past decade according to the CDC. The rate is higher in older adolescents, though thankfully relatively uncommon (about 1 in 10,000 a year), and, although we know risk factors, no one has been able to predict reliably the risk for an individual teenager at a point in time. In a clinically referred sample, 85% of depressed adolescents will have suicidal ideation and 32% will make a suicide attempt. The risk is higher in those adolescents with more than one psychiatric diagnosis and with a history of impulsive behaviors, substance abuse, prior suicide attempts, and a family history of suicide. It is important that parents hear that asking about suicidal thoughts will not cause them. On the contrary, preserving open communication and a warm relationship is very protective. Adolescent suicide attempts are likely to be impulsive, so helping the family to consider ways to “put up obstacles” that would slow down any possible attempt is an effective way to improve safety. Ask your patients about suicidal thoughts, plans, and what keeps them safe. Find out if they worry about sharing these thoughts with their parents and why. Ask if there are ways their parents can check on them that “aren’t too annoying.” Determine if there are guns in the home, and if so, are they safely stored (locked, separate from ammunition)? More than 50% of completed adolescent suicides involve firearms, so this question is critical. What about access to medications that could be dangerous in overdose in your home or a relative’s home they may visit? Discussing these facts with your patients and their parents together will make it easier for them to continue the conversation outside of your office and can make an enormous difference in their recovery.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Reference
Kovacs M et al. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):8-20.
The etiology of acute otitis media in young children in recent years
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.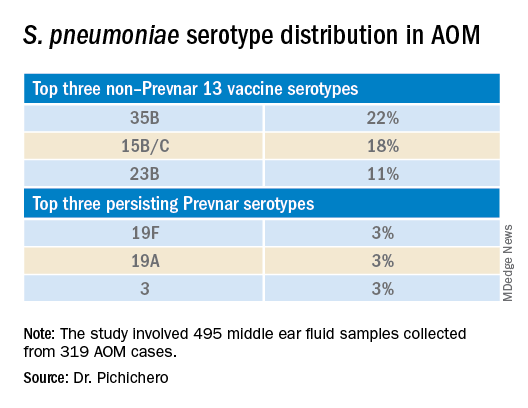
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.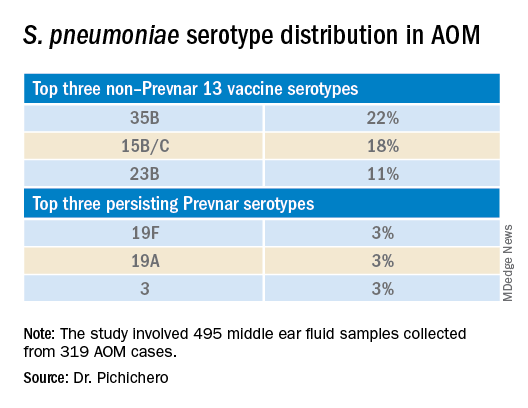
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Since the COVID-19 pandemic began, pediatricians have been seeing fewer cases of all respiratory illnesses, including acute otitis media (AOM). However, as I prepare this column, an uptick has commenced and likely will continue in an upward trajectory as we emerge from the pandemic into an endemic coronavirus era. Our group in Rochester, N.Y., has continued prospective studies of AOM throughout the pandemic. We found that nasopharyngeal colonization by Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and Moraxella catarrhalis remained prevalent in our study cohort of children aged 6-36 months. However, with all the precautions of masking, social distancing, hand washing, and quick exclusion from day care when illness occurred, the frequency of detecting these common otopathogens decreased, as one might expect.1
Leading up to the pandemic, we had an abundance of data to characterize AOM etiology and found that the cause of AOM continues to change following the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar 13). Our most recent report on otopathogen distribution and antibiotic susceptibility covered the years 2015-2019.2 A total of 589 children were enrolled prospectively and we collected 495 middle ear fluid samples (MEF) from 319 AOM cases using tympanocentesis. The frequency of isolates was H. influenzae (34%), pneumococcus (24%), and M. catarrhalis (15%). Beta-lactamase–positive H. influenzae strains were identified among 49% of the isolates, rendering them resistant to amoxicillin. PCV13 serotypes were infrequently isolated. However, we did isolate vaccine types (VTs) in some children from MEF, notably serotypes 19F, 19A, and 3. Non-PCV13 pneumococcus serotypes 35B, 23B, and 15B/C emerged as the most common serotypes. Amoxicillin resistance was identified among 25% of pneumococcal strains. Out of 16 antibiotics tested, 9 (56%) showed a significant increase in nonsusceptibility among pneumococcal isolates. 100% of M. catarrhalis isolates were beta-lactamase producers and therefore resistant to amoxicillin.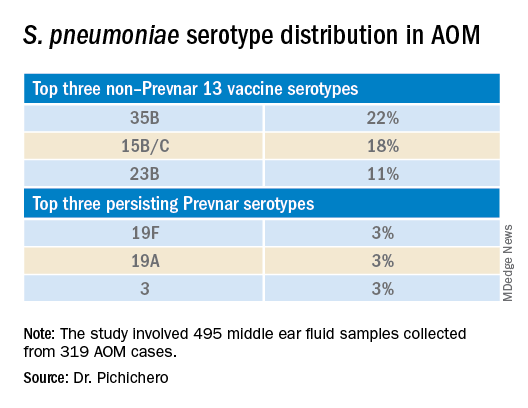
PCV13 has resulted in a decline in both invasive and noninvasive pneumococcal infections caused by strains expressing the 13 capsular serotypes included in the vaccine. However, the emergence of replacement serotypes occurred after introduction of PCV73,4 and continues to occur during the PCV13 era, as shown from the results presented here. Non-PCV13 serotypes accounted for more than 90% of MEF isolates during 2015-2019, with 35B, 21 and 23B being the most commonly isolated. Other emergent serotypes of potential importance were nonvaccine serotypes 15A, 15B, 15C, 23A and 11A. This is highly relevant because forthcoming higher-valency PCVs – PCV15 (manufactured by Merck) and PCV20 (manufactured by Pfizer) will not include many of the dominant capsular serotypes of pneumococcus strains causing AOM. Consequently, the impact of higher-valency PCVs on AOM will not be as great as was observed with the introduction of PCV7 or PCV13.
Of special interest, 22% of pneumococcus isolates from MEF were serotype 35B, making it the most prevalent. Recently we reported a significant rise in antibiotic nonsusceptibility in Spn isolates, contributed mainly by serotype 35B5 and we have been studying how 35B strains transitioned from commensal to otopathogen in children.6 Because serotype 35B strains are increasingly prevalent and often antibiotic resistant, absence of this serotype from PCV15 and PCV20 is cause for concern.
The frequency of isolation of H. influenzae and M. catarrhalis has remained stable across the PCV13 era as the No. 1 and No. 3 pathogens. Similarly, the production of beta-lactamase among strains causing AOM has remained stable at close to 50% and 100%, respectively. Use of amoxicillin, either high dose or standard dose, would not be expected to kill these bacteria.
Our study design has limitations. The population is derived from a predominantly middle-class, suburban population of children in upstate New York and may not be representative of other types of populations in the United States. The children are 6-36 months old, the age when most AOM occurs. MEF samples that were culture negative for bacteria were not further tested by polymerase chain reaction methods.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
References
1. Kaur R et al. Front Pediatr. 2021;9:722483.
2. Kaur R et al. Euro J Clin Microbiol Infect Dis. 2021;41:37-44
3. Pelton SI et al. Pediatr Infect Disease J. 2004;23:1015-22.
4. Farrell DJ et al. Pediatr Infect Disease J. 2007;26:123-8..
5. Kaur R et al. Clin Infect Dis 2021;72(5):797-805.
6. Fuji N et al. Front Cell Infect Microbiol. 2021;11:744742.
Children and COVID: New cases and hospital admissions skyrocket
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The total for the week of Dec. 31 to Jan. 6 – the highest since the pandemic began – was an increase of 78% over the previous week (325,000) and 192% higher than just 2 weeks before (199,000), the AAP and CHA said in their weekly COVID-19 report. No region of the country was spared, as all four saw at least 50,000 more cases than the week before, but the increase was largest in the West and smallest in the Midwest.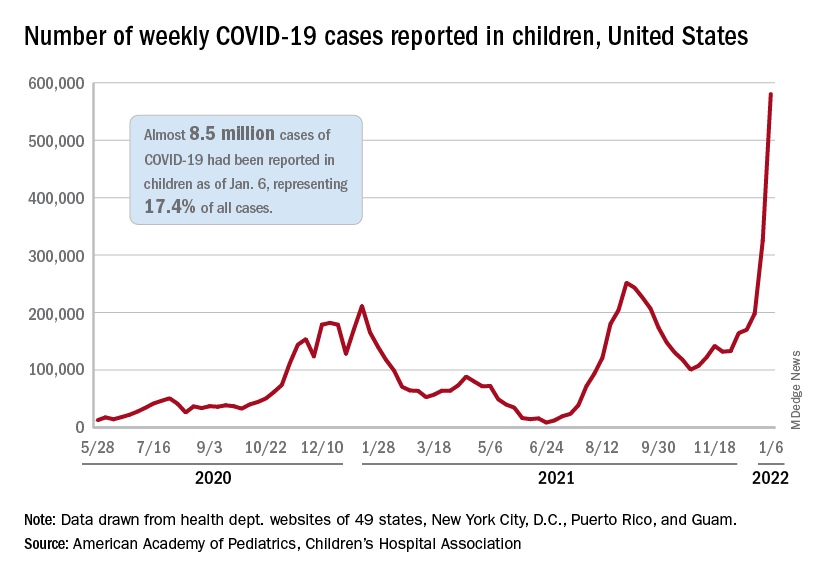
“Nearly 8.5 million children have tested positive for COVID-19 since the onset of the pandemic; nearly 11% of these cases have been added in the past 2 weeks,” the AAP said.
The situation is the same for hospitalizations. On Dec. 15, the daily rate of new admissions for children aged 0-17 years was 0.26 per 100,000, and by Jan. 7 it had more than quadrupled to 1.15 per 100,000, the Centers for Disease Control and Prevention reported. Before Omicron, the highest rate was 0.47 per 100,000 on Sept. 4, 2021.
The number of children occupying inpatient beds who had laboratory-confirmed COVID-19 went from 2,343 on Jan. 2 to 3,476 on Jan. 9, a jump of more than 48% in just 1 week. Texas had more hospitalized children (392) than any other state on Jan. 9, with California (339) and New York (313) the only other states over 300, according to data from the Department of Health & Human Services.
For vaccinations. however, the situation is definitely not the same. The number of children added to the ranks of those with at least one dose of COVID-19 vaccine was down in early 2022 (Jan. 3-9) for both 5- to 11-year-olds (–8.2%) and 16- to 17-year-olds (–12.2%) but higher among those aged 12-15 (12.2%), compared with the previous week (Dec. 27 to Jan. 2), the CDC said on its COVID Data Tracker.
Cumulative figures show that 26.3% of all children aged 5-11 had received at least one dose of vaccine and 17.2% were fully vaccinated as of Jan. 10, compared with 62.2% and 52.0% of 12- to 15-year-olds and 68.5% and 58.1% of those aged 16-17. Altogether, over 23.8 million children in those three age groups have received at least one dose and almost 18.6 million are fully vaccinated, the CDC said.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The total for the week of Dec. 31 to Jan. 6 – the highest since the pandemic began – was an increase of 78% over the previous week (325,000) and 192% higher than just 2 weeks before (199,000), the AAP and CHA said in their weekly COVID-19 report. No region of the country was spared, as all four saw at least 50,000 more cases than the week before, but the increase was largest in the West and smallest in the Midwest.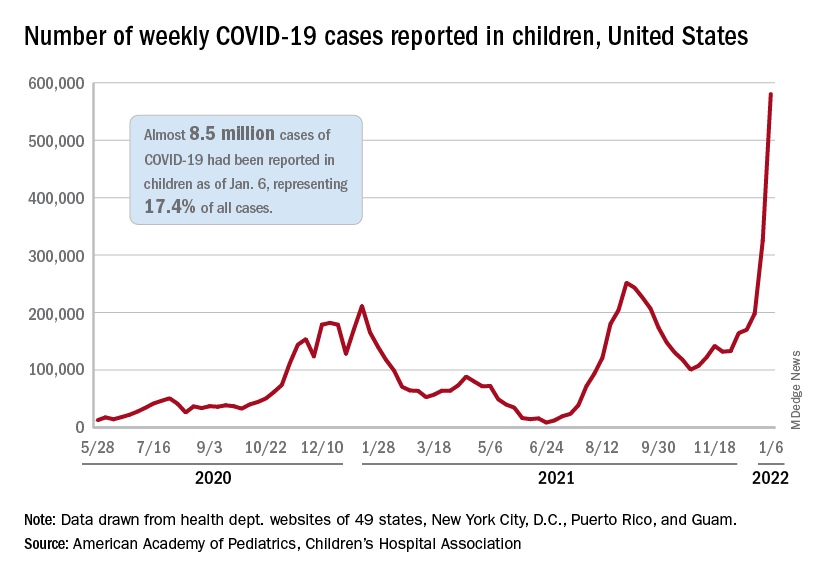
“Nearly 8.5 million children have tested positive for COVID-19 since the onset of the pandemic; nearly 11% of these cases have been added in the past 2 weeks,” the AAP said.
The situation is the same for hospitalizations. On Dec. 15, the daily rate of new admissions for children aged 0-17 years was 0.26 per 100,000, and by Jan. 7 it had more than quadrupled to 1.15 per 100,000, the Centers for Disease Control and Prevention reported. Before Omicron, the highest rate was 0.47 per 100,000 on Sept. 4, 2021.
The number of children occupying inpatient beds who had laboratory-confirmed COVID-19 went from 2,343 on Jan. 2 to 3,476 on Jan. 9, a jump of more than 48% in just 1 week. Texas had more hospitalized children (392) than any other state on Jan. 9, with California (339) and New York (313) the only other states over 300, according to data from the Department of Health & Human Services.
For vaccinations. however, the situation is definitely not the same. The number of children added to the ranks of those with at least one dose of COVID-19 vaccine was down in early 2022 (Jan. 3-9) for both 5- to 11-year-olds (–8.2%) and 16- to 17-year-olds (–12.2%) but higher among those aged 12-15 (12.2%), compared with the previous week (Dec. 27 to Jan. 2), the CDC said on its COVID Data Tracker.
Cumulative figures show that 26.3% of all children aged 5-11 had received at least one dose of vaccine and 17.2% were fully vaccinated as of Jan. 10, compared with 62.2% and 52.0% of 12- to 15-year-olds and 68.5% and 58.1% of those aged 16-17. Altogether, over 23.8 million children in those three age groups have received at least one dose and almost 18.6 million are fully vaccinated, the CDC said.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The total for the week of Dec. 31 to Jan. 6 – the highest since the pandemic began – was an increase of 78% over the previous week (325,000) and 192% higher than just 2 weeks before (199,000), the AAP and CHA said in their weekly COVID-19 report. No region of the country was spared, as all four saw at least 50,000 more cases than the week before, but the increase was largest in the West and smallest in the Midwest.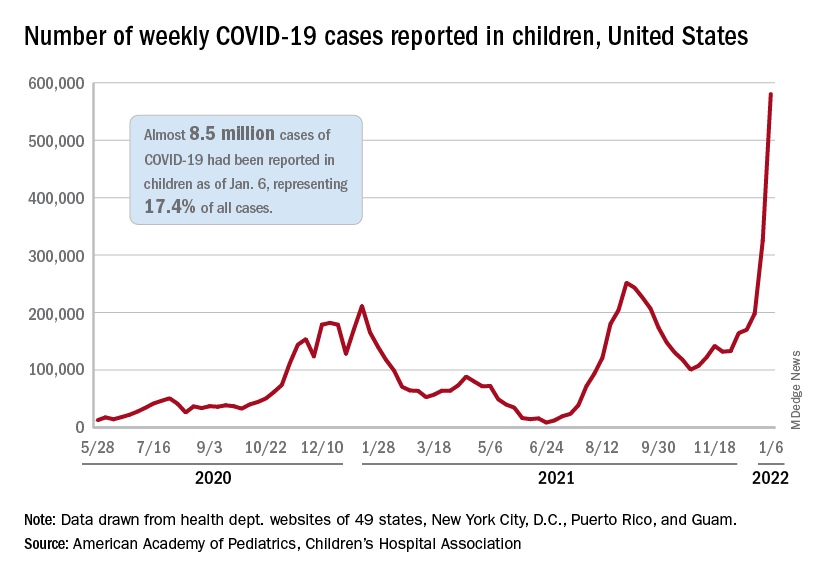
“Nearly 8.5 million children have tested positive for COVID-19 since the onset of the pandemic; nearly 11% of these cases have been added in the past 2 weeks,” the AAP said.
The situation is the same for hospitalizations. On Dec. 15, the daily rate of new admissions for children aged 0-17 years was 0.26 per 100,000, and by Jan. 7 it had more than quadrupled to 1.15 per 100,000, the Centers for Disease Control and Prevention reported. Before Omicron, the highest rate was 0.47 per 100,000 on Sept. 4, 2021.
The number of children occupying inpatient beds who had laboratory-confirmed COVID-19 went from 2,343 on Jan. 2 to 3,476 on Jan. 9, a jump of more than 48% in just 1 week. Texas had more hospitalized children (392) than any other state on Jan. 9, with California (339) and New York (313) the only other states over 300, according to data from the Department of Health & Human Services.
For vaccinations. however, the situation is definitely not the same. The number of children added to the ranks of those with at least one dose of COVID-19 vaccine was down in early 2022 (Jan. 3-9) for both 5- to 11-year-olds (–8.2%) and 16- to 17-year-olds (–12.2%) but higher among those aged 12-15 (12.2%), compared with the previous week (Dec. 27 to Jan. 2), the CDC said on its COVID Data Tracker.
Cumulative figures show that 26.3% of all children aged 5-11 had received at least one dose of vaccine and 17.2% were fully vaccinated as of Jan. 10, compared with 62.2% and 52.0% of 12- to 15-year-olds and 68.5% and 58.1% of those aged 16-17. Altogether, over 23.8 million children in those three age groups have received at least one dose and almost 18.6 million are fully vaccinated, the CDC said.
U.S. reports record-breaking 1.35 million new COVID cases in a day
The United States reported 1.35 million new COVID-19 cases on Jan. 10, logging the highest daily total for any country in the world during the pandemic.
The United States set the previous record of 1 million cases on Jan. 3. (A large number of cases are reported on Mondays, since many states don’t provide updates over the weekend, according to Reuters.)
Still, the 7-day average for new cases has surpassed 700,000, tripling in 2 weeks as the contagious Omicron variant continues to spread across the country.
The daily record of new cases came a day after the United States crossed the grim milestone of 60 million COVID-19 cases during the pandemic, according to the latest data from Johns Hopkins University. More than 11 million new cases were reported in the past 28 days, with 5 million reported since Jan. 2.
Globally, more than 310 million cases have been reported, resulting in nearly 5.5 million COVID-19 deaths. Almost 40 million cases have been confirmed worldwide during the past month, with the United States accounting for 28% of those.
Texas became the second state to report more than 5 million cases since the pandemic began, behind California’s total of 6 million cases. Florida has reported more than 4.6 million, while New York has reported more than 4.1 million.
The United States has also hit an all-time high for hospitalizations, with nearly 146,000 COVID-19 patients in hospitals across the country, according to the latest data from the U.S. Department of Health and Human Services. The previous record was 142,000 hospitalizations in January 2021.
Jan. 11’s hospitalizations are more than twice as many as 2 weeks ago, according to CNN. About 78% of inpatient beds are in use nationwide, and 21% are being used for COVID-19 patients.
Deaths are averaging about 1,700 per day, Reuters reported, which is up from 1,400 in recent days but not much higher than earlier this winter. The peak average was 3,400 daily deaths in mid-January 2021.
The surging numbers of cases and hospitalizations across the country are straining hospitals. On Jan. 10, Virginia Gov. Ralph Northam declared a state of emergency after the number of intensive care unit hospitalizations more than doubled since Dec. 1, CNN reported. The order allows hospitals to expand bed capacity, use telehealth options, and be more flexible with staffing.
Texas is hiring at least 2,700 medical staff to help with the surge, CNN reported, and Kentucky has mobilized the National Guard to provide support.
“Omicron continues to burn through the commonwealth, growing at levels we have never seen before. Omicron is significantly more contagious than even the Delta variant,” Kentucky Gov. Andy Beshear said during a news briefing Jan. 10.
Kentucky reported its highest weekly total of cases last week and has its highest rate of positive tests, at 26%. Mr. Beshear said the state is down to 134 available adult ICU beds.
“If it spreads at the rate we are seeing, it is certainly going to fill up our hospitals,” he said.
A version of this article first appeared on WebMD.com.
The United States reported 1.35 million new COVID-19 cases on Jan. 10, logging the highest daily total for any country in the world during the pandemic.
The United States set the previous record of 1 million cases on Jan. 3. (A large number of cases are reported on Mondays, since many states don’t provide updates over the weekend, according to Reuters.)
Still, the 7-day average for new cases has surpassed 700,000, tripling in 2 weeks as the contagious Omicron variant continues to spread across the country.
The daily record of new cases came a day after the United States crossed the grim milestone of 60 million COVID-19 cases during the pandemic, according to the latest data from Johns Hopkins University. More than 11 million new cases were reported in the past 28 days, with 5 million reported since Jan. 2.
Globally, more than 310 million cases have been reported, resulting in nearly 5.5 million COVID-19 deaths. Almost 40 million cases have been confirmed worldwide during the past month, with the United States accounting for 28% of those.
Texas became the second state to report more than 5 million cases since the pandemic began, behind California’s total of 6 million cases. Florida has reported more than 4.6 million, while New York has reported more than 4.1 million.
The United States has also hit an all-time high for hospitalizations, with nearly 146,000 COVID-19 patients in hospitals across the country, according to the latest data from the U.S. Department of Health and Human Services. The previous record was 142,000 hospitalizations in January 2021.
Jan. 11’s hospitalizations are more than twice as many as 2 weeks ago, according to CNN. About 78% of inpatient beds are in use nationwide, and 21% are being used for COVID-19 patients.
Deaths are averaging about 1,700 per day, Reuters reported, which is up from 1,400 in recent days but not much higher than earlier this winter. The peak average was 3,400 daily deaths in mid-January 2021.
The surging numbers of cases and hospitalizations across the country are straining hospitals. On Jan. 10, Virginia Gov. Ralph Northam declared a state of emergency after the number of intensive care unit hospitalizations more than doubled since Dec. 1, CNN reported. The order allows hospitals to expand bed capacity, use telehealth options, and be more flexible with staffing.
Texas is hiring at least 2,700 medical staff to help with the surge, CNN reported, and Kentucky has mobilized the National Guard to provide support.
“Omicron continues to burn through the commonwealth, growing at levels we have never seen before. Omicron is significantly more contagious than even the Delta variant,” Kentucky Gov. Andy Beshear said during a news briefing Jan. 10.
Kentucky reported its highest weekly total of cases last week and has its highest rate of positive tests, at 26%. Mr. Beshear said the state is down to 134 available adult ICU beds.
“If it spreads at the rate we are seeing, it is certainly going to fill up our hospitals,” he said.
A version of this article first appeared on WebMD.com.
The United States reported 1.35 million new COVID-19 cases on Jan. 10, logging the highest daily total for any country in the world during the pandemic.
The United States set the previous record of 1 million cases on Jan. 3. (A large number of cases are reported on Mondays, since many states don’t provide updates over the weekend, according to Reuters.)
Still, the 7-day average for new cases has surpassed 700,000, tripling in 2 weeks as the contagious Omicron variant continues to spread across the country.
The daily record of new cases came a day after the United States crossed the grim milestone of 60 million COVID-19 cases during the pandemic, according to the latest data from Johns Hopkins University. More than 11 million new cases were reported in the past 28 days, with 5 million reported since Jan. 2.
Globally, more than 310 million cases have been reported, resulting in nearly 5.5 million COVID-19 deaths. Almost 40 million cases have been confirmed worldwide during the past month, with the United States accounting for 28% of those.
Texas became the second state to report more than 5 million cases since the pandemic began, behind California’s total of 6 million cases. Florida has reported more than 4.6 million, while New York has reported more than 4.1 million.
The United States has also hit an all-time high for hospitalizations, with nearly 146,000 COVID-19 patients in hospitals across the country, according to the latest data from the U.S. Department of Health and Human Services. The previous record was 142,000 hospitalizations in January 2021.
Jan. 11’s hospitalizations are more than twice as many as 2 weeks ago, according to CNN. About 78% of inpatient beds are in use nationwide, and 21% are being used for COVID-19 patients.
Deaths are averaging about 1,700 per day, Reuters reported, which is up from 1,400 in recent days but not much higher than earlier this winter. The peak average was 3,400 daily deaths in mid-January 2021.
The surging numbers of cases and hospitalizations across the country are straining hospitals. On Jan. 10, Virginia Gov. Ralph Northam declared a state of emergency after the number of intensive care unit hospitalizations more than doubled since Dec. 1, CNN reported. The order allows hospitals to expand bed capacity, use telehealth options, and be more flexible with staffing.
Texas is hiring at least 2,700 medical staff to help with the surge, CNN reported, and Kentucky has mobilized the National Guard to provide support.
“Omicron continues to burn through the commonwealth, growing at levels we have never seen before. Omicron is significantly more contagious than even the Delta variant,” Kentucky Gov. Andy Beshear said during a news briefing Jan. 10.
Kentucky reported its highest weekly total of cases last week and has its highest rate of positive tests, at 26%. Mr. Beshear said the state is down to 134 available adult ICU beds.
“If it spreads at the rate we are seeing, it is certainly going to fill up our hospitals,” he said.
A version of this article first appeared on WebMD.com.
Augmented autism screening pays big dividends
A new, augmented autism-screening strategy boosted the number of boys diagnosed with the condition, especially Spanish speakers, a new study finds. The research was published in JAMA Pediatrics
The number of diagnoses in girls didn’t budge significantly, however, surprising researchers. Still, the findings suggest that “multistage screening and appropriate access to diagnostic services can really move the needle on the early detection of autism and reducing disparities in autism diagnosis and detection,” said lead author R. Christopher Sheldrick, PhD, a Boston University research associate professor of health law, policy, and management, in an interview.
While early intervention is considered crucial, U.S. research suggests that several groups of children – the poor, racial and ethnic minorities, and non-English speakers – are more likely to be diagnosed with autism spectrum disorder (ASD) later in life. “They have much lower access to appropriate services, both to get kids diagnosed and to get the kinds of interventions that can be helpful for families,” Dr. Sheldrick said. “Our study is about trying to close the gap around diagnosis, the first step.”
For the new study, the researchers implemented an intervention strategy in Massachusetts at three Early Intervention (EI) programs, which provide autism screening to children who are referred by pediatricians or parents. The researchers then tracked the programs, all in Boston, and nine comparison programs from the greater Boston area from 2012 to 2018.
Overall, 33,326 children were assessed, all aged 14-36 months. Those at the intervention programs were chosen because they had high levels of poverty. Children at those programs were more likely to be Black than those at the comparison programs (30.7% vs. 12.2%), to be Spanish speakers (28.9% vs. 12.5%), and to be in the lowest household income bracket (66.9% vs. 54.2%). In both groups, about 64% of the children were male.
The intervention strategy aimed to reduce the reliance on screening tests. Instead, the study authors write, “our protocol emphasizes ASD screening as a process that includes clinician and parent decision-making.”
As Dr. Sheldrick explained, parents and specialists observe children together “and then decide whether it’s worth taking the next step, which is a full diagnostic assessment with a licensed professional.” According to the study, either the parent(s) or the specialists could make the referral for a full, university-based assessment.
The goal was to help specialists use their professional judgment more, he said, and refer children who don’t show signs of ASD via a screening instrument but still spark concern, he said. “We’re really trying to create a system in which the screening tools support professional judgment, but don’t really replace it.”
After weighting, the researchers found that diagnoses of ASD were more common in the intervention sites vs. comparison sites (incidence rate ratio, 1.6; 95% confidence interval, 1.3-2.1, P < .001), accounting for an extra 8.1 diagnoses per 1,000 per quarter. Among Spanish-speaking families only, diagnoses grew even more in the intervention sites vs. comparison sites (IRR, 2.6; 95% CI, 1.6-4.3; P < .001), representing 15.4 additional diagnoses per 1,000 children per quarter.
There was also an increase in diagnoses among boys in the intervention sites vs. comparison sites (IRR, 1.8; 95% CI, 1.4-2.3; P < .001), accounting for 14.8 additional diagnoses per 1,000 children per quarter. However, there was no statistically significant increase in diagnosis among girls (IRR, 1.1; 95% CI, 0.6-1.7; P = .84).
The finding about girls surprised the researchers. “The program was highly effective for boys, but really didn’t have any effect for girls,” Dr. Sheldrick said. “Even though autism is considered to be more common in boys, there are questions about whether it’s underidentified in girls. These data would be consistent with that view. So there’s work to do to be able to recognize how a young girl with autism might present and how you might note that in a sensitive way and then respond appropriately.”
The overall message of the study is “that screening with appropriate supports can make a difference,” he said. However, he acknowledged that the extra cost of the program is unclear. “We did not systematically collect data on cost,” he said, noting that the funding for the study paid for both the intervention and the analysis.
For now, he said, researchers are following the children in the study to see if they were able to access treatment services. Some of the investigators are also taking part in a randomized study to evaluate an intervention in children with social communication disorders, he said.
In an accompanying commentary, three pediatric specialists noted that the study is the first to analyze ASD screening in EI. “This study supports the notion of ASD screening as an iterative, multistep process that optimally involves multiple community stakeholders with varying levels of developmental expertise who have done the work to build trust with families,” write pediatrician Kate E. Wallis, MD, MPH, of Children’s Hospital of Philadelphia, graduate student Monica M. Abdul-Chani, MA, of the University of Alabama at Birmingham, and pediatrician Katharine E. Zuckerman, MD, MPH, of Oregon Health & Science University, Portland.
In regard to disparities in diagnosis in Spanish-speaking families, the commentary authors write that “locating a greater proportion of the ASD identification process in EI, which families are already familiar with, has no to low cost for families, and is likely geographically closer for families, can reduce structural barriers to identification.”
They add that the emphasis within Latino families on the “building of warm and caring relationships with others based on mutual trust and respect” can allow EI specialists to “develop relationships with families who may be afraid or skeptical of sharing what could be considered personal details of their family life.”
The commentary authors also note that “it remains all too common for language delays to be attributed to child exposure to two languages, even though data do not support this attribution. Bilingual EI staff can help to demystify this perpetual myth and better estimate a child’s communication and social skills in both languages as they communicate and play.”
The study was funded by grants from the Health Resources Services Administration and the National Institute of Mental Health. Dr. Sheldrick is cocreator of the Parent’s Observations of Social Interaction (POSI), which is one of the two first-stage screeners used in this study. He conducts research related to this instrument but receives no royalties. He reports grants from the National Institutes of Health. Coauthor Alice S. Carter, PhD, is cocreator of the POSI but receives no royalties. She is also cocreator of the Brief Infant Toddler Social Emotional Assessment, which is one of the two first-stage screeners used in this study, and receives royalties on the sale of the instrument. She reports grants from the National Institutes of Health and the Health Resources and Services Administration. Study coauthor Thomas I. Mackie, PhD, MPH, reports grants from the National Institute of Mental Health. Study coauthor Noah Hoch reports grants from the Health Resources Services Administration and the National Institute of Mental Health. No other disclosures from study authors are reported. Dr. Zuckerman reported grants from the National Institutes of Health and National Institute of Mental Health and consulting fees from H2N related to autism. The other commentary authors report no disclosures.
A new, augmented autism-screening strategy boosted the number of boys diagnosed with the condition, especially Spanish speakers, a new study finds. The research was published in JAMA Pediatrics
The number of diagnoses in girls didn’t budge significantly, however, surprising researchers. Still, the findings suggest that “multistage screening and appropriate access to diagnostic services can really move the needle on the early detection of autism and reducing disparities in autism diagnosis and detection,” said lead author R. Christopher Sheldrick, PhD, a Boston University research associate professor of health law, policy, and management, in an interview.
While early intervention is considered crucial, U.S. research suggests that several groups of children – the poor, racial and ethnic minorities, and non-English speakers – are more likely to be diagnosed with autism spectrum disorder (ASD) later in life. “They have much lower access to appropriate services, both to get kids diagnosed and to get the kinds of interventions that can be helpful for families,” Dr. Sheldrick said. “Our study is about trying to close the gap around diagnosis, the first step.”
For the new study, the researchers implemented an intervention strategy in Massachusetts at three Early Intervention (EI) programs, which provide autism screening to children who are referred by pediatricians or parents. The researchers then tracked the programs, all in Boston, and nine comparison programs from the greater Boston area from 2012 to 2018.
Overall, 33,326 children were assessed, all aged 14-36 months. Those at the intervention programs were chosen because they had high levels of poverty. Children at those programs were more likely to be Black than those at the comparison programs (30.7% vs. 12.2%), to be Spanish speakers (28.9% vs. 12.5%), and to be in the lowest household income bracket (66.9% vs. 54.2%). In both groups, about 64% of the children were male.
The intervention strategy aimed to reduce the reliance on screening tests. Instead, the study authors write, “our protocol emphasizes ASD screening as a process that includes clinician and parent decision-making.”
As Dr. Sheldrick explained, parents and specialists observe children together “and then decide whether it’s worth taking the next step, which is a full diagnostic assessment with a licensed professional.” According to the study, either the parent(s) or the specialists could make the referral for a full, university-based assessment.
The goal was to help specialists use their professional judgment more, he said, and refer children who don’t show signs of ASD via a screening instrument but still spark concern, he said. “We’re really trying to create a system in which the screening tools support professional judgment, but don’t really replace it.”
After weighting, the researchers found that diagnoses of ASD were more common in the intervention sites vs. comparison sites (incidence rate ratio, 1.6; 95% confidence interval, 1.3-2.1, P < .001), accounting for an extra 8.1 diagnoses per 1,000 per quarter. Among Spanish-speaking families only, diagnoses grew even more in the intervention sites vs. comparison sites (IRR, 2.6; 95% CI, 1.6-4.3; P < .001), representing 15.4 additional diagnoses per 1,000 children per quarter.
There was also an increase in diagnoses among boys in the intervention sites vs. comparison sites (IRR, 1.8; 95% CI, 1.4-2.3; P < .001), accounting for 14.8 additional diagnoses per 1,000 children per quarter. However, there was no statistically significant increase in diagnosis among girls (IRR, 1.1; 95% CI, 0.6-1.7; P = .84).
The finding about girls surprised the researchers. “The program was highly effective for boys, but really didn’t have any effect for girls,” Dr. Sheldrick said. “Even though autism is considered to be more common in boys, there are questions about whether it’s underidentified in girls. These data would be consistent with that view. So there’s work to do to be able to recognize how a young girl with autism might present and how you might note that in a sensitive way and then respond appropriately.”
The overall message of the study is “that screening with appropriate supports can make a difference,” he said. However, he acknowledged that the extra cost of the program is unclear. “We did not systematically collect data on cost,” he said, noting that the funding for the study paid for both the intervention and the analysis.
For now, he said, researchers are following the children in the study to see if they were able to access treatment services. Some of the investigators are also taking part in a randomized study to evaluate an intervention in children with social communication disorders, he said.
In an accompanying commentary, three pediatric specialists noted that the study is the first to analyze ASD screening in EI. “This study supports the notion of ASD screening as an iterative, multistep process that optimally involves multiple community stakeholders with varying levels of developmental expertise who have done the work to build trust with families,” write pediatrician Kate E. Wallis, MD, MPH, of Children’s Hospital of Philadelphia, graduate student Monica M. Abdul-Chani, MA, of the University of Alabama at Birmingham, and pediatrician Katharine E. Zuckerman, MD, MPH, of Oregon Health & Science University, Portland.
In regard to disparities in diagnosis in Spanish-speaking families, the commentary authors write that “locating a greater proportion of the ASD identification process in EI, which families are already familiar with, has no to low cost for families, and is likely geographically closer for families, can reduce structural barriers to identification.”
They add that the emphasis within Latino families on the “building of warm and caring relationships with others based on mutual trust and respect” can allow EI specialists to “develop relationships with families who may be afraid or skeptical of sharing what could be considered personal details of their family life.”
The commentary authors also note that “it remains all too common for language delays to be attributed to child exposure to two languages, even though data do not support this attribution. Bilingual EI staff can help to demystify this perpetual myth and better estimate a child’s communication and social skills in both languages as they communicate and play.”
The study was funded by grants from the Health Resources Services Administration and the National Institute of Mental Health. Dr. Sheldrick is cocreator of the Parent’s Observations of Social Interaction (POSI), which is one of the two first-stage screeners used in this study. He conducts research related to this instrument but receives no royalties. He reports grants from the National Institutes of Health. Coauthor Alice S. Carter, PhD, is cocreator of the POSI but receives no royalties. She is also cocreator of the Brief Infant Toddler Social Emotional Assessment, which is one of the two first-stage screeners used in this study, and receives royalties on the sale of the instrument. She reports grants from the National Institutes of Health and the Health Resources and Services Administration. Study coauthor Thomas I. Mackie, PhD, MPH, reports grants from the National Institute of Mental Health. Study coauthor Noah Hoch reports grants from the Health Resources Services Administration and the National Institute of Mental Health. No other disclosures from study authors are reported. Dr. Zuckerman reported grants from the National Institutes of Health and National Institute of Mental Health and consulting fees from H2N related to autism. The other commentary authors report no disclosures.
A new, augmented autism-screening strategy boosted the number of boys diagnosed with the condition, especially Spanish speakers, a new study finds. The research was published in JAMA Pediatrics
The number of diagnoses in girls didn’t budge significantly, however, surprising researchers. Still, the findings suggest that “multistage screening and appropriate access to diagnostic services can really move the needle on the early detection of autism and reducing disparities in autism diagnosis and detection,” said lead author R. Christopher Sheldrick, PhD, a Boston University research associate professor of health law, policy, and management, in an interview.
While early intervention is considered crucial, U.S. research suggests that several groups of children – the poor, racial and ethnic minorities, and non-English speakers – are more likely to be diagnosed with autism spectrum disorder (ASD) later in life. “They have much lower access to appropriate services, both to get kids diagnosed and to get the kinds of interventions that can be helpful for families,” Dr. Sheldrick said. “Our study is about trying to close the gap around diagnosis, the first step.”
For the new study, the researchers implemented an intervention strategy in Massachusetts at three Early Intervention (EI) programs, which provide autism screening to children who are referred by pediatricians or parents. The researchers then tracked the programs, all in Boston, and nine comparison programs from the greater Boston area from 2012 to 2018.
Overall, 33,326 children were assessed, all aged 14-36 months. Those at the intervention programs were chosen because they had high levels of poverty. Children at those programs were more likely to be Black than those at the comparison programs (30.7% vs. 12.2%), to be Spanish speakers (28.9% vs. 12.5%), and to be in the lowest household income bracket (66.9% vs. 54.2%). In both groups, about 64% of the children were male.
The intervention strategy aimed to reduce the reliance on screening tests. Instead, the study authors write, “our protocol emphasizes ASD screening as a process that includes clinician and parent decision-making.”
As Dr. Sheldrick explained, parents and specialists observe children together “and then decide whether it’s worth taking the next step, which is a full diagnostic assessment with a licensed professional.” According to the study, either the parent(s) or the specialists could make the referral for a full, university-based assessment.
The goal was to help specialists use their professional judgment more, he said, and refer children who don’t show signs of ASD via a screening instrument but still spark concern, he said. “We’re really trying to create a system in which the screening tools support professional judgment, but don’t really replace it.”
After weighting, the researchers found that diagnoses of ASD were more common in the intervention sites vs. comparison sites (incidence rate ratio, 1.6; 95% confidence interval, 1.3-2.1, P < .001), accounting for an extra 8.1 diagnoses per 1,000 per quarter. Among Spanish-speaking families only, diagnoses grew even more in the intervention sites vs. comparison sites (IRR, 2.6; 95% CI, 1.6-4.3; P < .001), representing 15.4 additional diagnoses per 1,000 children per quarter.
There was also an increase in diagnoses among boys in the intervention sites vs. comparison sites (IRR, 1.8; 95% CI, 1.4-2.3; P < .001), accounting for 14.8 additional diagnoses per 1,000 children per quarter. However, there was no statistically significant increase in diagnosis among girls (IRR, 1.1; 95% CI, 0.6-1.7; P = .84).
The finding about girls surprised the researchers. “The program was highly effective for boys, but really didn’t have any effect for girls,” Dr. Sheldrick said. “Even though autism is considered to be more common in boys, there are questions about whether it’s underidentified in girls. These data would be consistent with that view. So there’s work to do to be able to recognize how a young girl with autism might present and how you might note that in a sensitive way and then respond appropriately.”
The overall message of the study is “that screening with appropriate supports can make a difference,” he said. However, he acknowledged that the extra cost of the program is unclear. “We did not systematically collect data on cost,” he said, noting that the funding for the study paid for both the intervention and the analysis.
For now, he said, researchers are following the children in the study to see if they were able to access treatment services. Some of the investigators are also taking part in a randomized study to evaluate an intervention in children with social communication disorders, he said.
In an accompanying commentary, three pediatric specialists noted that the study is the first to analyze ASD screening in EI. “This study supports the notion of ASD screening as an iterative, multistep process that optimally involves multiple community stakeholders with varying levels of developmental expertise who have done the work to build trust with families,” write pediatrician Kate E. Wallis, MD, MPH, of Children’s Hospital of Philadelphia, graduate student Monica M. Abdul-Chani, MA, of the University of Alabama at Birmingham, and pediatrician Katharine E. Zuckerman, MD, MPH, of Oregon Health & Science University, Portland.
In regard to disparities in diagnosis in Spanish-speaking families, the commentary authors write that “locating a greater proportion of the ASD identification process in EI, which families are already familiar with, has no to low cost for families, and is likely geographically closer for families, can reduce structural barriers to identification.”
They add that the emphasis within Latino families on the “building of warm and caring relationships with others based on mutual trust and respect” can allow EI specialists to “develop relationships with families who may be afraid or skeptical of sharing what could be considered personal details of their family life.”
The commentary authors also note that “it remains all too common for language delays to be attributed to child exposure to two languages, even though data do not support this attribution. Bilingual EI staff can help to demystify this perpetual myth and better estimate a child’s communication and social skills in both languages as they communicate and play.”
The study was funded by grants from the Health Resources Services Administration and the National Institute of Mental Health. Dr. Sheldrick is cocreator of the Parent’s Observations of Social Interaction (POSI), which is one of the two first-stage screeners used in this study. He conducts research related to this instrument but receives no royalties. He reports grants from the National Institutes of Health. Coauthor Alice S. Carter, PhD, is cocreator of the POSI but receives no royalties. She is also cocreator of the Brief Infant Toddler Social Emotional Assessment, which is one of the two first-stage screeners used in this study, and receives royalties on the sale of the instrument. She reports grants from the National Institutes of Health and the Health Resources and Services Administration. Study coauthor Thomas I. Mackie, PhD, MPH, reports grants from the National Institute of Mental Health. Study coauthor Noah Hoch reports grants from the Health Resources Services Administration and the National Institute of Mental Health. No other disclosures from study authors are reported. Dr. Zuckerman reported grants from the National Institutes of Health and National Institute of Mental Health and consulting fees from H2N related to autism. The other commentary authors report no disclosures.
FROM JAMA PEDIATRICS
CDC: More kids hospitalized with COVID since pandemic began
Hospital admissions of U.S. children younger than 5 – the only group ineligible for vaccination – have reached their peak since the start of the pandemic, according to new data from the Centers for Disease Control and Prevention.
CDC Director Rochelle Walensky, MD, said the higher numbers show the importance of vaccination for all eligible groups.
“This is the highest number of pediatric hospitalizations we’ve seen throughout the pandemic, which we said about Delta until now,” she said at a CDC briefing Friday. “This very well may be that there are just more cases out there, and our children are more vulnerable when they have more cases surrounding them.”
Despite the skyrocketing admissions, hospitalizations are still relatively low for children, she said. The hospitalization rate for children under 5 is 4 in 100,000, and it’s about 1 in 100,000 in children 5-17.
Dr. Walensky said not all children are being hospitalized for COVID-19 – some are admitted for unrelated issues and test positive but don’t have symptoms.
“We are still learning more about the severity of Omicron in children,” she said, noting that just over 50% of children 12-18 are fully vaccinated, while only 16% of those ages 5-11 are fully vaccinated.
Friday’s teleconference was the first CDC briefing in several months and comes on the heels of recent guideline updates for testing and isolation that have left the American public dumbfounded. When asked why the briefing was held, Dr. Walensky said there had been interest in hearing more from the CDC, saying, “I anticipate this will be the first of many briefings.”
She also defended the confusing guideline changes, saying, “We’re in an unprecedented time with the speed of Omicron cases rising. … This is hard, and I am committed to continuing to improve as we learn more about the science and communicate that to you.”
A version of this article first appeared on WebMD.com.
Hospital admissions of U.S. children younger than 5 – the only group ineligible for vaccination – have reached their peak since the start of the pandemic, according to new data from the Centers for Disease Control and Prevention.
CDC Director Rochelle Walensky, MD, said the higher numbers show the importance of vaccination for all eligible groups.
“This is the highest number of pediatric hospitalizations we’ve seen throughout the pandemic, which we said about Delta until now,” she said at a CDC briefing Friday. “This very well may be that there are just more cases out there, and our children are more vulnerable when they have more cases surrounding them.”
Despite the skyrocketing admissions, hospitalizations are still relatively low for children, she said. The hospitalization rate for children under 5 is 4 in 100,000, and it’s about 1 in 100,000 in children 5-17.
Dr. Walensky said not all children are being hospitalized for COVID-19 – some are admitted for unrelated issues and test positive but don’t have symptoms.
“We are still learning more about the severity of Omicron in children,” she said, noting that just over 50% of children 12-18 are fully vaccinated, while only 16% of those ages 5-11 are fully vaccinated.
Friday’s teleconference was the first CDC briefing in several months and comes on the heels of recent guideline updates for testing and isolation that have left the American public dumbfounded. When asked why the briefing was held, Dr. Walensky said there had been interest in hearing more from the CDC, saying, “I anticipate this will be the first of many briefings.”
She also defended the confusing guideline changes, saying, “We’re in an unprecedented time with the speed of Omicron cases rising. … This is hard, and I am committed to continuing to improve as we learn more about the science and communicate that to you.”
A version of this article first appeared on WebMD.com.
Hospital admissions of U.S. children younger than 5 – the only group ineligible for vaccination – have reached their peak since the start of the pandemic, according to new data from the Centers for Disease Control and Prevention.
CDC Director Rochelle Walensky, MD, said the higher numbers show the importance of vaccination for all eligible groups.
“This is the highest number of pediatric hospitalizations we’ve seen throughout the pandemic, which we said about Delta until now,” she said at a CDC briefing Friday. “This very well may be that there are just more cases out there, and our children are more vulnerable when they have more cases surrounding them.”
Despite the skyrocketing admissions, hospitalizations are still relatively low for children, she said. The hospitalization rate for children under 5 is 4 in 100,000, and it’s about 1 in 100,000 in children 5-17.
Dr. Walensky said not all children are being hospitalized for COVID-19 – some are admitted for unrelated issues and test positive but don’t have symptoms.
“We are still learning more about the severity of Omicron in children,” she said, noting that just over 50% of children 12-18 are fully vaccinated, while only 16% of those ages 5-11 are fully vaccinated.
Friday’s teleconference was the first CDC briefing in several months and comes on the heels of recent guideline updates for testing and isolation that have left the American public dumbfounded. When asked why the briefing was held, Dr. Walensky said there had been interest in hearing more from the CDC, saying, “I anticipate this will be the first of many briefings.”
She also defended the confusing guideline changes, saying, “We’re in an unprecedented time with the speed of Omicron cases rising. … This is hard, and I am committed to continuing to improve as we learn more about the science and communicate that to you.”
A version of this article first appeared on WebMD.com.