User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Washington medical board charges doctor with spreading COVID misinformation
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Doctors and professional organizations are standing guard, hoping to protect patients from any harm that results from mistruths spread by colleagues.
Case in point: Several physicians and the American Board of Pathology filed complaints with Washington and Idaho medical boards alleging that Ryan Cole, MD, a board-certified pathologist who practices in Boise, Idaho, but who also holds a license in Washington, has spread antivaccine and pro-ivermectin statements on social media. Dr. Cole is one of the founders of America’s Frontline Doctors, a right-wing political organization. Dr. Cole did not respond to a request for comment.
Gary W. Procop, MD, CEO, American Board of Pathology, told this news organization that “as physicians and board-certified pathologists, we have a public trust, and we must be accountable to patients, society, and the profession. Misinformation can cause real harm to patients, which may include death. Misinformation diverts patients away from lifesaving vaccination and other preventive measures, promotes viral transmission, and recommends ineffective therapies that may be toxic instead of evidence-based medical care.”
Cavalcade of complaints
Several doctors also chimed in with formal complaints alleging that Cole is spreading unreliable information, according to a report from KTVB News. For example, a Boise doctor wrote in his complaint that Dr. Cole is “a major purveyor of misinformation” and called it “amazing” that the physician was continuing to publicly support debunked information about COVID-19 more than a year into the pandemic. The doctor also stated, “Cole is a health menace, abusing his status as a physician to mislead the public.”
As a result of such complaints, the Washington medical board has charged Cole with COVID-19–related violations. It is unclear whether or not the Idaho medical board will sanction the doctor. At least 12 medical boards have sanctioned doctors for similar violations since the start of the pandemic.
The statement of charges from the Washington medical board contends that since March 2021, Dr. Cole has made numerous misleading statements regarding the COVID-19 pandemic, vaccines, the use of ivermectin to treat COVID-19, and the effectiveness of masks.
In addition, the statement alleges that Dr. Cole treated several COVID-19 patients via telemedicine. During these sessions, he prescribed ivermectin, an antiparasite drug that has not been found to have any effectiveness in treating, curing, or preventing COVID-19. One of the patients died after receiving this treatment, according to the complaint.
Citing a study published in the New England Journal of Medicine, Dr. Procop pointed out that use of ivermectin, which is not approved by the U.S. Food and Drug Administration to treat COVID-19, is particularly troubling.
“There is a concern whenever an ineffective treatment is prescribed when more effective and scientifically proven therapies are available. Therapeutics have potential side effects, and toxicities have been associated with the use of ivermectin,” Dr. Procop said. “The benefits of therapy should always outweigh the risks of treatment.”
If the Washington medical board finds that Dr. Cole has engaged in unprofessional conduct, possible sanctions include revocation or suspension of his license. Washington state law also provides for a range of other possible sanctions, including restriction or limitation of his practice, requiring that he complete a specific program of remedial education or treatment, monitoring of his practice, censure or reprimand, probation, a fine of up to $5,000 for each violation, or refunding fees that his practice has billed to and collected from patients. Dr. Cole had until January 30 to respond to the medical board’s statement.
“The American Board of Pathology supports the actions of the Washington State Medical Board regarding their inquiries into any physician that holds license in their state who makes false and misleading medical claims, or provides medical care beyond their scope of practice, as indicated by their training,” Dr. Procop said.
Law in limbo
While medical boards are seeking to sanction professionals who spread falsehoods, the pause button has been hit on the California law that allows regulators to punish doctors for spreading false information about COVID-19 vaccinations and treatments.
The law went into effect Jan. 1 but was temporarily halted when U.S. District Judge William B. Shubb of the Eastern District of California granted a preliminary injunction against the law on Jan. 25, according to a report in the Sacramento Bee.
Mr. Shubb said the measure’s definition of “misinformation” was “unconstitutionally vague” under the due process clause of the 14th Amendment. He also criticized the law’s definition of “misinformation” as being “grammatically incoherent.”
A version of this article first appeared on Medscape.com.
Kid with glasses: Many children live far from pediatric eye care
More than 2,800 counties in the United States lack a practicing pediatric ophthalmologist, limiting easy access to specialized eye care, a new study found.
The review of public, online pediatric ophthalmology directories found 1,056 pediatric ophthalmologists registered. The majority of these doctors practiced in densely populated areas, leaving many poor and rural residents across the United States without a nearby doctor to visit, and with the burden of spending time and money to get care for their children.
Travel for that care may be out of reach for some, according to Hannah Walsh, a medical student at the University of Miami, who led the study published in JAMA Ophthalmology.
Ms. Walsh’s research found that the median income of families living in a county without a pediatric ophthalmologist was nearly $17,000 lower than that for families with access to such specialists (95% confidence interval, −$18,544 to −$14,389; P < .001). These families were also less likely to own a car.
“We found that counties that didn’t have access to ophthalmic care for pediatrics were already disproportionately affected by lower socioeconomic status,” she said.
Children often receive routine vision screenings through their primary care clinician, but children who fail a routine screening may need to visit a pediatric ophthalmologist for a full eye examination, according to the American Academy of Ophthalmology.
Ms. Walsh and colleagues pulled data in March 2022 on the demographics of pediatric ophthalmologists from online directories hosted by the AAO and the American Association of Pediatric Ophthalmology and Strabismus. Ms. Walsh cautioned that the directories might include eye doctors who are no longer practicing, or there might be specialists who had not registered for the databases.
Yasmin Bradfield, MD, a pediatric ophthalmologist at the University of Wisconsin–Madison, noted that after the study published, pediatric ophthalmologists from Vermont and New Mexico notified study authors and AAPOS that they are practicing in the states.
Dr. Bradfield, a board member of AAPOS who also heads the organization’s recruitment task force, said the organization is aware of only one state – Wyoming – without a currently practicing pediatric ophthalmologist.
But based on the March 2022 data, Ms. Walsh and her colleagues found four states – New Mexico, North Dakota, South Dakota, and Vermont – did not have any pediatric ophthalmologists listed in directories for the organizations. Meanwhile, the country’s most populous states – California, New York, Florida, and Texas – had the most pediatric ophthalmologists.
For every million people, the study identified 7.7 pediatric ophthalmologists nationwide.
Julius T. Oatts, MD, the lead author of an accompanying editorial, said the findings are “valuable and sobering.” Even in San Francisco, where Dr. Oatts practices, most pediatric eye specialists have 6-month wait lists, he said.
Not fixing the shortage of children’s eye doctors could carry lifetime consequences, Dr. Oatts and his colleagues warned.
“Vision and eye health represent an important health barrier to learning in children,” Dr. Oatts and his colleagues wrote. “Lack of access to pediatric vision screening and care also contributes to the academic achievement gap and educational disparities.”
Dr. Bradfield said that disparities in pediatric ophthalmology care could leave some children at risk for losing their vision or never being able to see 20/20. Parents living in areas without a specialist may decide to instead visit an optometrist, but they are not trained to treat serious cases, such as strabismus, and only test and diagnose vision changes, according to AAPOS.
“If we don’t get to the kids in time, they can lose vision permanently, even if it’s something as simple as they just need glasses as a toddler,” Dr. Bradfield said.
Dr. Bradfield said AAPOS is recruiting new pediatric ophthalmologists by offering fellowships for medical students to attend the association’s annual conference and creating shadowing opportunities for students. The society also will release a survey of pediatric ophthalmology salaries to dispel rumors that the specialty does not have lucrative wages.
Ms. Walsh said she was interested in looking at disparities in pediatric ophthalmology care, in part, because she was surprised by how few of her classmates attending medical school were interested in the field of study.
“I hope it encourages ophthalmologists to consider pediatric ophthalmology, or to consider volunteering their time, or going to underserved areas to provide care to families that really are in need,” she said.
Coauthor Jayanth Sridhar, MD, reported receiving personal fees from Alcon, Apellis, Allergan, Dutch Ophthalmic Research Center, Genentech, OcuTerra Therapeutics, and Regeneron outside the submitted work. The other authors and the editorialists report no relevant financial relationships.
*This article was updated on 2/2/2023.
A version of this article first appeared on Medscape.com.
More than 2,800 counties in the United States lack a practicing pediatric ophthalmologist, limiting easy access to specialized eye care, a new study found.
The review of public, online pediatric ophthalmology directories found 1,056 pediatric ophthalmologists registered. The majority of these doctors practiced in densely populated areas, leaving many poor and rural residents across the United States without a nearby doctor to visit, and with the burden of spending time and money to get care for their children.
Travel for that care may be out of reach for some, according to Hannah Walsh, a medical student at the University of Miami, who led the study published in JAMA Ophthalmology.
Ms. Walsh’s research found that the median income of families living in a county without a pediatric ophthalmologist was nearly $17,000 lower than that for families with access to such specialists (95% confidence interval, −$18,544 to −$14,389; P < .001). These families were also less likely to own a car.
“We found that counties that didn’t have access to ophthalmic care for pediatrics were already disproportionately affected by lower socioeconomic status,” she said.
Children often receive routine vision screenings through their primary care clinician, but children who fail a routine screening may need to visit a pediatric ophthalmologist for a full eye examination, according to the American Academy of Ophthalmology.
Ms. Walsh and colleagues pulled data in March 2022 on the demographics of pediatric ophthalmologists from online directories hosted by the AAO and the American Association of Pediatric Ophthalmology and Strabismus. Ms. Walsh cautioned that the directories might include eye doctors who are no longer practicing, or there might be specialists who had not registered for the databases.
Yasmin Bradfield, MD, a pediatric ophthalmologist at the University of Wisconsin–Madison, noted that after the study published, pediatric ophthalmologists from Vermont and New Mexico notified study authors and AAPOS that they are practicing in the states.
Dr. Bradfield, a board member of AAPOS who also heads the organization’s recruitment task force, said the organization is aware of only one state – Wyoming – without a currently practicing pediatric ophthalmologist.
But based on the March 2022 data, Ms. Walsh and her colleagues found four states – New Mexico, North Dakota, South Dakota, and Vermont – did not have any pediatric ophthalmologists listed in directories for the organizations. Meanwhile, the country’s most populous states – California, New York, Florida, and Texas – had the most pediatric ophthalmologists.
For every million people, the study identified 7.7 pediatric ophthalmologists nationwide.
Julius T. Oatts, MD, the lead author of an accompanying editorial, said the findings are “valuable and sobering.” Even in San Francisco, where Dr. Oatts practices, most pediatric eye specialists have 6-month wait lists, he said.
Not fixing the shortage of children’s eye doctors could carry lifetime consequences, Dr. Oatts and his colleagues warned.
“Vision and eye health represent an important health barrier to learning in children,” Dr. Oatts and his colleagues wrote. “Lack of access to pediatric vision screening and care also contributes to the academic achievement gap and educational disparities.”
Dr. Bradfield said that disparities in pediatric ophthalmology care could leave some children at risk for losing their vision or never being able to see 20/20. Parents living in areas without a specialist may decide to instead visit an optometrist, but they are not trained to treat serious cases, such as strabismus, and only test and diagnose vision changes, according to AAPOS.
“If we don’t get to the kids in time, they can lose vision permanently, even if it’s something as simple as they just need glasses as a toddler,” Dr. Bradfield said.
Dr. Bradfield said AAPOS is recruiting new pediatric ophthalmologists by offering fellowships for medical students to attend the association’s annual conference and creating shadowing opportunities for students. The society also will release a survey of pediatric ophthalmology salaries to dispel rumors that the specialty does not have lucrative wages.
Ms. Walsh said she was interested in looking at disparities in pediatric ophthalmology care, in part, because she was surprised by how few of her classmates attending medical school were interested in the field of study.
“I hope it encourages ophthalmologists to consider pediatric ophthalmology, or to consider volunteering their time, or going to underserved areas to provide care to families that really are in need,” she said.
Coauthor Jayanth Sridhar, MD, reported receiving personal fees from Alcon, Apellis, Allergan, Dutch Ophthalmic Research Center, Genentech, OcuTerra Therapeutics, and Regeneron outside the submitted work. The other authors and the editorialists report no relevant financial relationships.
*This article was updated on 2/2/2023.
A version of this article first appeared on Medscape.com.
More than 2,800 counties in the United States lack a practicing pediatric ophthalmologist, limiting easy access to specialized eye care, a new study found.
The review of public, online pediatric ophthalmology directories found 1,056 pediatric ophthalmologists registered. The majority of these doctors practiced in densely populated areas, leaving many poor and rural residents across the United States without a nearby doctor to visit, and with the burden of spending time and money to get care for their children.
Travel for that care may be out of reach for some, according to Hannah Walsh, a medical student at the University of Miami, who led the study published in JAMA Ophthalmology.
Ms. Walsh’s research found that the median income of families living in a county without a pediatric ophthalmologist was nearly $17,000 lower than that for families with access to such specialists (95% confidence interval, −$18,544 to −$14,389; P < .001). These families were also less likely to own a car.
“We found that counties that didn’t have access to ophthalmic care for pediatrics were already disproportionately affected by lower socioeconomic status,” she said.
Children often receive routine vision screenings through their primary care clinician, but children who fail a routine screening may need to visit a pediatric ophthalmologist for a full eye examination, according to the American Academy of Ophthalmology.
Ms. Walsh and colleagues pulled data in March 2022 on the demographics of pediatric ophthalmologists from online directories hosted by the AAO and the American Association of Pediatric Ophthalmology and Strabismus. Ms. Walsh cautioned that the directories might include eye doctors who are no longer practicing, or there might be specialists who had not registered for the databases.
Yasmin Bradfield, MD, a pediatric ophthalmologist at the University of Wisconsin–Madison, noted that after the study published, pediatric ophthalmologists from Vermont and New Mexico notified study authors and AAPOS that they are practicing in the states.
Dr. Bradfield, a board member of AAPOS who also heads the organization’s recruitment task force, said the organization is aware of only one state – Wyoming – without a currently practicing pediatric ophthalmologist.
But based on the March 2022 data, Ms. Walsh and her colleagues found four states – New Mexico, North Dakota, South Dakota, and Vermont – did not have any pediatric ophthalmologists listed in directories for the organizations. Meanwhile, the country’s most populous states – California, New York, Florida, and Texas – had the most pediatric ophthalmologists.
For every million people, the study identified 7.7 pediatric ophthalmologists nationwide.
Julius T. Oatts, MD, the lead author of an accompanying editorial, said the findings are “valuable and sobering.” Even in San Francisco, where Dr. Oatts practices, most pediatric eye specialists have 6-month wait lists, he said.
Not fixing the shortage of children’s eye doctors could carry lifetime consequences, Dr. Oatts and his colleagues warned.
“Vision and eye health represent an important health barrier to learning in children,” Dr. Oatts and his colleagues wrote. “Lack of access to pediatric vision screening and care also contributes to the academic achievement gap and educational disparities.”
Dr. Bradfield said that disparities in pediatric ophthalmology care could leave some children at risk for losing their vision or never being able to see 20/20. Parents living in areas without a specialist may decide to instead visit an optometrist, but they are not trained to treat serious cases, such as strabismus, and only test and diagnose vision changes, according to AAPOS.
“If we don’t get to the kids in time, they can lose vision permanently, even if it’s something as simple as they just need glasses as a toddler,” Dr. Bradfield said.
Dr. Bradfield said AAPOS is recruiting new pediatric ophthalmologists by offering fellowships for medical students to attend the association’s annual conference and creating shadowing opportunities for students. The society also will release a survey of pediatric ophthalmology salaries to dispel rumors that the specialty does not have lucrative wages.
Ms. Walsh said she was interested in looking at disparities in pediatric ophthalmology care, in part, because she was surprised by how few of her classmates attending medical school were interested in the field of study.
“I hope it encourages ophthalmologists to consider pediatric ophthalmology, or to consider volunteering their time, or going to underserved areas to provide care to families that really are in need,” she said.
Coauthor Jayanth Sridhar, MD, reported receiving personal fees from Alcon, Apellis, Allergan, Dutch Ophthalmic Research Center, Genentech, OcuTerra Therapeutics, and Regeneron outside the submitted work. The other authors and the editorialists report no relevant financial relationships.
*This article was updated on 2/2/2023.
A version of this article first appeared on Medscape.com.
Similar brain atrophy in obesity and Alzheimer’s disease
Comparisons of MRI scans for more than 1,000 participants indicate correlations between the two conditions, especially in areas of gray matter thinning, suggesting that managing excess weight might slow cognitive decline and lower the risk for AD, according to the researchers.
However, brain maps of obesity did not correlate with maps of amyloid or tau protein accumulation.
“The fact that obesity-related brain atrophy did not correlate with the distribution of amyloid and tau proteins in AD was not what we expected,” study author Filip Morys, PhD, a postdoctoral researcher at McGill University, Montreal, said in an interview. “But it might just show that the specific mechanisms underpinning obesity- and Alzheimer’s disease–related neurodegeneration are different. This remains to be confirmed.”
The study was published in the Journal of Alzheimer’s Disease.
Cortical Thinning
The current study was prompted by the team’s earlier study, which showed that obesity-related neurodegeneration patterns were visually similar to those of AD, said Dr. Morys. “It was known previously that obesity is a risk factor for AD, but we wanted to directly compare brain atrophy patterns in both, which is what we did in this new study.”
The researchers analyzed data from a pooled sample of more than 1,300 participants. From the ADNI database, the researchers selected participants with AD and age- and sex-matched cognitively healthy controls. From the UK Biobank, the researchers drew a sample of lean, overweight, and obese participants without neurologic disease.
To determine how the weight status of patients with AD affects the correspondence between AD and obesity maps, they categorized participants with AD and healthy controls from the ADNI database into lean, overweight, and obese subgroups.
Then, to investigate mechanisms that might drive the similarities between obesity-related brain atrophy and AD-related amyloid-beta accumulation, they looked for overlapping areas in PET brain maps between patients with these outcomes.
The investigations showed that obesity maps were highly correlated with AD maps, but not with amyloid-beta or tau protein maps. The researchers also found significant correlations between obesity and the lean individuals with AD.
Brain regions with the highest similarities between obesity and AD were located mainly in the left temporal and bilateral prefrontal cortices.
“Our research confirms that obesity-related gray matter atrophy resembles that of AD,” the authors concluded. “Excess weight management could lead to improved health outcomes, slow down cognitive decline in aging, and lower the risk for AD.”
Upcoming research “will focus on investigating how weight loss can affect the risk for AD, other dementias, and cognitive decline in general,” said Dr. Morys. “At this point, our study suggests that obesity prevention, weight loss, but also decreasing other metabolic risk factors related to obesity, such as type-2 diabetes or hypertension, might reduce the risk for AD and have beneficial effects on cognition.”
Lifestyle habits
Commenting on the findings, Claire Sexton, DPhil, vice president of scientific programs and outreach at the Alzheimer’s Association, cautioned that a single cross-sectional study isn’t conclusive. “Previous studies have illustrated that the relationship between obesity and dementia is complex. Growing evidence indicates that people can reduce their risk of cognitive decline by adopting key lifestyle habits, like regular exercise, a heart-healthy diet and staying socially and cognitively engaged.”
The Alzheimer’s Association is leading a 2-year clinical trial, U.S. Pointer, to study how targeting these risk factors in combination may reduce risk for cognitive decline in older adults.
The work was supported by a Foundation Scheme award from the Canadian Institutes of Health Research. Dr. Morys received a postdoctoral fellowship from Fonds de Recherche du Quebec – Santé. Data collection and sharing were funded by the Alzheimer’s Disease Neuroimaging Initiative, the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and multiple pharmaceutical companies and other private sector organizations. Dr. Morys and Dr. Sexton reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Comparisons of MRI scans for more than 1,000 participants indicate correlations between the two conditions, especially in areas of gray matter thinning, suggesting that managing excess weight might slow cognitive decline and lower the risk for AD, according to the researchers.
However, brain maps of obesity did not correlate with maps of amyloid or tau protein accumulation.
“The fact that obesity-related brain atrophy did not correlate with the distribution of amyloid and tau proteins in AD was not what we expected,” study author Filip Morys, PhD, a postdoctoral researcher at McGill University, Montreal, said in an interview. “But it might just show that the specific mechanisms underpinning obesity- and Alzheimer’s disease–related neurodegeneration are different. This remains to be confirmed.”
The study was published in the Journal of Alzheimer’s Disease.
Cortical Thinning
The current study was prompted by the team’s earlier study, which showed that obesity-related neurodegeneration patterns were visually similar to those of AD, said Dr. Morys. “It was known previously that obesity is a risk factor for AD, but we wanted to directly compare brain atrophy patterns in both, which is what we did in this new study.”
The researchers analyzed data from a pooled sample of more than 1,300 participants. From the ADNI database, the researchers selected participants with AD and age- and sex-matched cognitively healthy controls. From the UK Biobank, the researchers drew a sample of lean, overweight, and obese participants without neurologic disease.
To determine how the weight status of patients with AD affects the correspondence between AD and obesity maps, they categorized participants with AD and healthy controls from the ADNI database into lean, overweight, and obese subgroups.
Then, to investigate mechanisms that might drive the similarities between obesity-related brain atrophy and AD-related amyloid-beta accumulation, they looked for overlapping areas in PET brain maps between patients with these outcomes.
The investigations showed that obesity maps were highly correlated with AD maps, but not with amyloid-beta or tau protein maps. The researchers also found significant correlations between obesity and the lean individuals with AD.
Brain regions with the highest similarities between obesity and AD were located mainly in the left temporal and bilateral prefrontal cortices.
“Our research confirms that obesity-related gray matter atrophy resembles that of AD,” the authors concluded. “Excess weight management could lead to improved health outcomes, slow down cognitive decline in aging, and lower the risk for AD.”
Upcoming research “will focus on investigating how weight loss can affect the risk for AD, other dementias, and cognitive decline in general,” said Dr. Morys. “At this point, our study suggests that obesity prevention, weight loss, but also decreasing other metabolic risk factors related to obesity, such as type-2 diabetes or hypertension, might reduce the risk for AD and have beneficial effects on cognition.”
Lifestyle habits
Commenting on the findings, Claire Sexton, DPhil, vice president of scientific programs and outreach at the Alzheimer’s Association, cautioned that a single cross-sectional study isn’t conclusive. “Previous studies have illustrated that the relationship between obesity and dementia is complex. Growing evidence indicates that people can reduce their risk of cognitive decline by adopting key lifestyle habits, like regular exercise, a heart-healthy diet and staying socially and cognitively engaged.”
The Alzheimer’s Association is leading a 2-year clinical trial, U.S. Pointer, to study how targeting these risk factors in combination may reduce risk for cognitive decline in older adults.
The work was supported by a Foundation Scheme award from the Canadian Institutes of Health Research. Dr. Morys received a postdoctoral fellowship from Fonds de Recherche du Quebec – Santé. Data collection and sharing were funded by the Alzheimer’s Disease Neuroimaging Initiative, the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and multiple pharmaceutical companies and other private sector organizations. Dr. Morys and Dr. Sexton reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Comparisons of MRI scans for more than 1,000 participants indicate correlations between the two conditions, especially in areas of gray matter thinning, suggesting that managing excess weight might slow cognitive decline and lower the risk for AD, according to the researchers.
However, brain maps of obesity did not correlate with maps of amyloid or tau protein accumulation.
“The fact that obesity-related brain atrophy did not correlate with the distribution of amyloid and tau proteins in AD was not what we expected,” study author Filip Morys, PhD, a postdoctoral researcher at McGill University, Montreal, said in an interview. “But it might just show that the specific mechanisms underpinning obesity- and Alzheimer’s disease–related neurodegeneration are different. This remains to be confirmed.”
The study was published in the Journal of Alzheimer’s Disease.
Cortical Thinning
The current study was prompted by the team’s earlier study, which showed that obesity-related neurodegeneration patterns were visually similar to those of AD, said Dr. Morys. “It was known previously that obesity is a risk factor for AD, but we wanted to directly compare brain atrophy patterns in both, which is what we did in this new study.”
The researchers analyzed data from a pooled sample of more than 1,300 participants. From the ADNI database, the researchers selected participants with AD and age- and sex-matched cognitively healthy controls. From the UK Biobank, the researchers drew a sample of lean, overweight, and obese participants without neurologic disease.
To determine how the weight status of patients with AD affects the correspondence between AD and obesity maps, they categorized participants with AD and healthy controls from the ADNI database into lean, overweight, and obese subgroups.
Then, to investigate mechanisms that might drive the similarities between obesity-related brain atrophy and AD-related amyloid-beta accumulation, they looked for overlapping areas in PET brain maps between patients with these outcomes.
The investigations showed that obesity maps were highly correlated with AD maps, but not with amyloid-beta or tau protein maps. The researchers also found significant correlations between obesity and the lean individuals with AD.
Brain regions with the highest similarities between obesity and AD were located mainly in the left temporal and bilateral prefrontal cortices.
“Our research confirms that obesity-related gray matter atrophy resembles that of AD,” the authors concluded. “Excess weight management could lead to improved health outcomes, slow down cognitive decline in aging, and lower the risk for AD.”
Upcoming research “will focus on investigating how weight loss can affect the risk for AD, other dementias, and cognitive decline in general,” said Dr. Morys. “At this point, our study suggests that obesity prevention, weight loss, but also decreasing other metabolic risk factors related to obesity, such as type-2 diabetes or hypertension, might reduce the risk for AD and have beneficial effects on cognition.”
Lifestyle habits
Commenting on the findings, Claire Sexton, DPhil, vice president of scientific programs and outreach at the Alzheimer’s Association, cautioned that a single cross-sectional study isn’t conclusive. “Previous studies have illustrated that the relationship between obesity and dementia is complex. Growing evidence indicates that people can reduce their risk of cognitive decline by adopting key lifestyle habits, like regular exercise, a heart-healthy diet and staying socially and cognitively engaged.”
The Alzheimer’s Association is leading a 2-year clinical trial, U.S. Pointer, to study how targeting these risk factors in combination may reduce risk for cognitive decline in older adults.
The work was supported by a Foundation Scheme award from the Canadian Institutes of Health Research. Dr. Morys received a postdoctoral fellowship from Fonds de Recherche du Quebec – Santé. Data collection and sharing were funded by the Alzheimer’s Disease Neuroimaging Initiative, the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and multiple pharmaceutical companies and other private sector organizations. Dr. Morys and Dr. Sexton reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ALZHEIMER’S DISEASE
Expert offers insights on pediatric dermatology emergencies
ORLANDO – The eruption spread away from the head and her transaminase levels were “dramatic,” in the 700s, said Kalyani S. Marathe, MD, MPH, associate professor of dermatology and pediatrics at the University of Cincinnati.
Dr. Marathe, director of the division of dermatology at Cincinnati Children’s Hospital, reviewed this case in a presentation on pediatric dermatologic emergencies at the ODAC Dermatology, Aesthetic & Surgery Conference, pointing out potential pitfalls and important aspects that might require swift action.
The patient was diagnosed with drug reaction with eosinophilia and systemic symptoms (DRESS).
Facial involvement is common in pediatric cases of DRESS, but edema of the face is less common in children than adults, Dr. Marathe said.
Antiepileptic medications are the most common cause of DRESS, followed by antibiotics – most often, vancomycin and trimethoprim/sulfamethoxazole, she said. But sometimes the trigger is not clear, she noted, recalling a vexing case she once saw in which IV contrast was eventually identified as the cause.
When DRESS is suspected, she said, lab work should be done during the acute eruption and after resolution. This should include CBC, liver function tests, creatinine, and urinalysis, and human herpesvirus 6 (HHV-6) and thyroid testing.
Treatment typically includes supportive care, unless symptoms are systemic, or if there is impending liver failure, when steroids, cyclosporine, or IVIG can be used.
Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN): Mortality rates when these diseases overlap is 4%, Dr. Marathe said. Clues to diagnosing this other medication-induced condition include involvement of the palms and the soles of the feet; presence of the Nikolsky sign in which the top layers of the skin slip away from the lower layers when rubbed; mucosal involvement, which often precedes cutaneous involvement; and these symptoms occurring within the first 8 weeks of taking a medication, which are most commonly antibiotics and anti-epileptics.
Dr. Marathe underscored how important it is to get ophthalmology involved right away, because of the risk of vision loss. Amniotic membrane transfer to the eye at the time of diagnosis has been found to produce dramatically better outcomes, she said. The membrane has anti-inflammatory and antiscarring properties and can promote wound healing on the surface of the eye.
“I would recommend getting your ophthalmology team on board early because they have to advocate for these patients,” she said.
Corticosteroids and IVIG can improve ocular outcomes, but cyclosporine is associated with better mortality outcomes, she said. Emerging data on etanercept has also led to more use of that drug, she said.
Erythema multiforme (EM): unlike urticaria, multiforme EM can have mucosal involvement, Dr. Marathe said. Clinicians should look for three zones of color: A central duskiness, a rim of pallor, and a ring of erythema.
EM is triggered by a virus, which is usually herpes simplex virus (HSV). But she added that HSV is not always found. “So, there are certainly other triggers out there that we just haven’t identified,” she said.
If HSV is suspected, oral acyclovir is effective, she noted.
Other cases might not be as straightforward. Dr. Marathe said that during her fellowship, she saw a patient with EM that was controlled only by IVIG, so it was administered every 3 months. In that case, the trigger was never found.
Multisystem inflammatory syndrome in children (MIS-C): This syndrome can follow COVID-19 infection, and usually presents with 3-5 days of fever after COVID has resolved. It can include gastrointestinal, cardiorespiratory, and neurocognitive symptoms.
The skin presentation is mainly a morbilliform pattern, but clinicians might also see conjunctival involvement, mucosal involvement, and “COVID toes,” painful red or purple lesions on the toes.
Treatment is usually IVIG and systemic corticosteroids, with the treatment course depending on the severity.
MIS-C was initially thought to be Kawasaki’s disease, another autoinflammatory disorder, which is related but distinct, Dr. Marathe said.
Patients with MIS-C “are usually going to have COVID-positive antibodies,” she said. But since almost everybody may have COVID antibodies, “it’s not usually a helpful test for you now. But early on, that’s what we used as helpful indicator.”
Dr. Marathe reported no relevant financial relationships.
ORLANDO – The eruption spread away from the head and her transaminase levels were “dramatic,” in the 700s, said Kalyani S. Marathe, MD, MPH, associate professor of dermatology and pediatrics at the University of Cincinnati.
Dr. Marathe, director of the division of dermatology at Cincinnati Children’s Hospital, reviewed this case in a presentation on pediatric dermatologic emergencies at the ODAC Dermatology, Aesthetic & Surgery Conference, pointing out potential pitfalls and important aspects that might require swift action.
The patient was diagnosed with drug reaction with eosinophilia and systemic symptoms (DRESS).
Facial involvement is common in pediatric cases of DRESS, but edema of the face is less common in children than adults, Dr. Marathe said.
Antiepileptic medications are the most common cause of DRESS, followed by antibiotics – most often, vancomycin and trimethoprim/sulfamethoxazole, she said. But sometimes the trigger is not clear, she noted, recalling a vexing case she once saw in which IV contrast was eventually identified as the cause.
When DRESS is suspected, she said, lab work should be done during the acute eruption and after resolution. This should include CBC, liver function tests, creatinine, and urinalysis, and human herpesvirus 6 (HHV-6) and thyroid testing.
Treatment typically includes supportive care, unless symptoms are systemic, or if there is impending liver failure, when steroids, cyclosporine, or IVIG can be used.
Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN): Mortality rates when these diseases overlap is 4%, Dr. Marathe said. Clues to diagnosing this other medication-induced condition include involvement of the palms and the soles of the feet; presence of the Nikolsky sign in which the top layers of the skin slip away from the lower layers when rubbed; mucosal involvement, which often precedes cutaneous involvement; and these symptoms occurring within the first 8 weeks of taking a medication, which are most commonly antibiotics and anti-epileptics.
Dr. Marathe underscored how important it is to get ophthalmology involved right away, because of the risk of vision loss. Amniotic membrane transfer to the eye at the time of diagnosis has been found to produce dramatically better outcomes, she said. The membrane has anti-inflammatory and antiscarring properties and can promote wound healing on the surface of the eye.
“I would recommend getting your ophthalmology team on board early because they have to advocate for these patients,” she said.
Corticosteroids and IVIG can improve ocular outcomes, but cyclosporine is associated with better mortality outcomes, she said. Emerging data on etanercept has also led to more use of that drug, she said.
Erythema multiforme (EM): unlike urticaria, multiforme EM can have mucosal involvement, Dr. Marathe said. Clinicians should look for three zones of color: A central duskiness, a rim of pallor, and a ring of erythema.
EM is triggered by a virus, which is usually herpes simplex virus (HSV). But she added that HSV is not always found. “So, there are certainly other triggers out there that we just haven’t identified,” she said.
If HSV is suspected, oral acyclovir is effective, she noted.
Other cases might not be as straightforward. Dr. Marathe said that during her fellowship, she saw a patient with EM that was controlled only by IVIG, so it was administered every 3 months. In that case, the trigger was never found.
Multisystem inflammatory syndrome in children (MIS-C): This syndrome can follow COVID-19 infection, and usually presents with 3-5 days of fever after COVID has resolved. It can include gastrointestinal, cardiorespiratory, and neurocognitive symptoms.
The skin presentation is mainly a morbilliform pattern, but clinicians might also see conjunctival involvement, mucosal involvement, and “COVID toes,” painful red or purple lesions on the toes.
Treatment is usually IVIG and systemic corticosteroids, with the treatment course depending on the severity.
MIS-C was initially thought to be Kawasaki’s disease, another autoinflammatory disorder, which is related but distinct, Dr. Marathe said.
Patients with MIS-C “are usually going to have COVID-positive antibodies,” she said. But since almost everybody may have COVID antibodies, “it’s not usually a helpful test for you now. But early on, that’s what we used as helpful indicator.”
Dr. Marathe reported no relevant financial relationships.
ORLANDO – The eruption spread away from the head and her transaminase levels were “dramatic,” in the 700s, said Kalyani S. Marathe, MD, MPH, associate professor of dermatology and pediatrics at the University of Cincinnati.
Dr. Marathe, director of the division of dermatology at Cincinnati Children’s Hospital, reviewed this case in a presentation on pediatric dermatologic emergencies at the ODAC Dermatology, Aesthetic & Surgery Conference, pointing out potential pitfalls and important aspects that might require swift action.
The patient was diagnosed with drug reaction with eosinophilia and systemic symptoms (DRESS).
Facial involvement is common in pediatric cases of DRESS, but edema of the face is less common in children than adults, Dr. Marathe said.
Antiepileptic medications are the most common cause of DRESS, followed by antibiotics – most often, vancomycin and trimethoprim/sulfamethoxazole, she said. But sometimes the trigger is not clear, she noted, recalling a vexing case she once saw in which IV contrast was eventually identified as the cause.
When DRESS is suspected, she said, lab work should be done during the acute eruption and after resolution. This should include CBC, liver function tests, creatinine, and urinalysis, and human herpesvirus 6 (HHV-6) and thyroid testing.
Treatment typically includes supportive care, unless symptoms are systemic, or if there is impending liver failure, when steroids, cyclosporine, or IVIG can be used.
Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN): Mortality rates when these diseases overlap is 4%, Dr. Marathe said. Clues to diagnosing this other medication-induced condition include involvement of the palms and the soles of the feet; presence of the Nikolsky sign in which the top layers of the skin slip away from the lower layers when rubbed; mucosal involvement, which often precedes cutaneous involvement; and these symptoms occurring within the first 8 weeks of taking a medication, which are most commonly antibiotics and anti-epileptics.
Dr. Marathe underscored how important it is to get ophthalmology involved right away, because of the risk of vision loss. Amniotic membrane transfer to the eye at the time of diagnosis has been found to produce dramatically better outcomes, she said. The membrane has anti-inflammatory and antiscarring properties and can promote wound healing on the surface of the eye.
“I would recommend getting your ophthalmology team on board early because they have to advocate for these patients,” she said.
Corticosteroids and IVIG can improve ocular outcomes, but cyclosporine is associated with better mortality outcomes, she said. Emerging data on etanercept has also led to more use of that drug, she said.
Erythema multiforme (EM): unlike urticaria, multiforme EM can have mucosal involvement, Dr. Marathe said. Clinicians should look for three zones of color: A central duskiness, a rim of pallor, and a ring of erythema.
EM is triggered by a virus, which is usually herpes simplex virus (HSV). But she added that HSV is not always found. “So, there are certainly other triggers out there that we just haven’t identified,” she said.
If HSV is suspected, oral acyclovir is effective, she noted.
Other cases might not be as straightforward. Dr. Marathe said that during her fellowship, she saw a patient with EM that was controlled only by IVIG, so it was administered every 3 months. In that case, the trigger was never found.
Multisystem inflammatory syndrome in children (MIS-C): This syndrome can follow COVID-19 infection, and usually presents with 3-5 days of fever after COVID has resolved. It can include gastrointestinal, cardiorespiratory, and neurocognitive symptoms.
The skin presentation is mainly a morbilliform pattern, but clinicians might also see conjunctival involvement, mucosal involvement, and “COVID toes,” painful red or purple lesions on the toes.
Treatment is usually IVIG and systemic corticosteroids, with the treatment course depending on the severity.
MIS-C was initially thought to be Kawasaki’s disease, another autoinflammatory disorder, which is related but distinct, Dr. Marathe said.
Patients with MIS-C “are usually going to have COVID-positive antibodies,” she said. But since almost everybody may have COVID antibodies, “it’s not usually a helpful test for you now. But early on, that’s what we used as helpful indicator.”
Dr. Marathe reported no relevant financial relationships.
AT ODAC 2023
Poor sleep quality as a teen may up MS risk in adulthood
Too little sleep or poor sleep quality during the teen years can significantly increase the risk for multiple sclerosis (MS) during adulthood, new research suggests.
In a large case-control study, individuals who slept less than 7 hours a night on average during adolescence were 40% more likely to develop MS later on. The risk was even higher for those who rated their sleep quality as bad.
On the other hand, MS was significantly less common among individuals who slept longer as teens – indicating a possible protective benefit.
While sleep duration has been associated with mortality or disease risk for other conditions, sleep quality usually has little to no effect on risk, lead investigator Torbjörn Åkerstedt, PhD, sleep researcher and professor of psychology, department of neuroscience, Karolinska Institutet, Stockholm, told this news organization.
“I hadn’t really expected that, but those results were quite strong, even stronger than sleep duration,” Dr. Åkerstedt said.
“We don’t really know why this is happening in young age, but the most suitable explanation is that the brain in still developing quite a bit, and you’re interfering with it,” he added.
The findings were published online in the Journal of Neurology, Neurosurgery and Psychiatry.
Strong association
Other studies have tied sleep deprivation to increased risk for serious illness, but the link between sleep and MS risk isn’t as well studied.
Previous research by Dr. Åkerstedt showed that the risk for MS was higher among individuals who took part in shift work before the age of 20. However, the impact of sleep duration or quality among teens was unknown.
The current Swedish population-based case-control study included 2,075 patients with MS and 3,164 without the disorder. All participants were asked to recall how many hours on average they slept per night between the ages of 15 and 19 years and to rate their sleep quality during that time.
Results showed that individuals who slept fewer than 7 hours a night during their teen years were 40% more likely to have MS as adults (odds ratio [OR], 1.4; 95% confidence interval [CI], 1.1-1.7).
Poor sleep quality increased MS risk even more (OR, 1.5; 95% CI, 1.3-1.9).
The association remained strong even after adjustment for additional sleep on weekends and breaks and excluding shift workers.
Long sleep ‘apparently good’
The researchers also conducted several sensitivity studies to rule out confounders that might bias the association, such as excluding participants who reported currently experiencing less sleep or poor sleep.
“You would expect that people who are suffering from sleep problems today would be the people who reported sleep problems during their youth,” but that didn’t happen, Dr. Åkerstedt noted.
The investigators also entered data on sleep duration and sleep quality at the same time, thinking the data would cancel each other out. However, the association remained the same.
“Quite often you see that sleep duration would eliminate the effect of sleep complaints in the prediction of disease, but here both remain significant when they are entered at the same time,” Dr. Åkerstedt said. “You get the feeling that this might mean they act together to produce results,” he added.
“One other thing that surprised me is that long sleep was apparently good,” said Dr. Åkerstedt.
The investigators have conducted several studies on sleep duration and mortality. In recent research, they found that both short sleep and long sleep predicted mortality – “and often, long sleep is a stronger predictor than short sleep,” he said.
Underestimated problem?
Commenting on the findings, Kathleen Zackowski, PhD, associate vice president of research for the National Multiple Sclerosis Society in Baltimore, noted that participants were asked to rate their own sleep quality during adolescence, a subjective report that may mean sleep quality has an even larger association with MS risk.
“That they found a result with sleep quality says to me that there probably is a bigger problem, because I don’t know if people over- or underestimate their sleep quality,” said Dr. Zackowski, who was not involved with the research.
“If we could get to that sleep quality question a little more objectively, I bet that we’d find there’s a lot more to the story,” she said.
That’s a story the researchers would like to explore, Dr. Åkerstedt reported. Designing a prospective study that more closely tracks sleeping habits during adolescence and follows individuals through adulthood could provide valuable information about how sleep quality and duration affect immune system development and MS risk, he said.
Dr. Zackowski said clinicians know that MS is not caused just by a genetic abnormality and that other environmental lifestyle factors seem to play a part.
“If we find out that sleep is one of those lifestyle factors, this is very changeable,” she added.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, the Swedish Brain Foundation, AFA Insurance, the European Aviation Safety Authority, the Tercentenary Fund of the Bank of Sweden, the Margaretha af Ugglas Foundation, the Swedish Foundation for MS Research, and NEURO Sweden. Dr. Åkerstadt has been supported by Tercentenary Fund of Bank of Sweden, AFA Insurance, and the European Aviation Safety Authority. Dr. Zackowski reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Too little sleep or poor sleep quality during the teen years can significantly increase the risk for multiple sclerosis (MS) during adulthood, new research suggests.
In a large case-control study, individuals who slept less than 7 hours a night on average during adolescence were 40% more likely to develop MS later on. The risk was even higher for those who rated their sleep quality as bad.
On the other hand, MS was significantly less common among individuals who slept longer as teens – indicating a possible protective benefit.
While sleep duration has been associated with mortality or disease risk for other conditions, sleep quality usually has little to no effect on risk, lead investigator Torbjörn Åkerstedt, PhD, sleep researcher and professor of psychology, department of neuroscience, Karolinska Institutet, Stockholm, told this news organization.
“I hadn’t really expected that, but those results were quite strong, even stronger than sleep duration,” Dr. Åkerstedt said.
“We don’t really know why this is happening in young age, but the most suitable explanation is that the brain in still developing quite a bit, and you’re interfering with it,” he added.
The findings were published online in the Journal of Neurology, Neurosurgery and Psychiatry.
Strong association
Other studies have tied sleep deprivation to increased risk for serious illness, but the link between sleep and MS risk isn’t as well studied.
Previous research by Dr. Åkerstedt showed that the risk for MS was higher among individuals who took part in shift work before the age of 20. However, the impact of sleep duration or quality among teens was unknown.
The current Swedish population-based case-control study included 2,075 patients with MS and 3,164 without the disorder. All participants were asked to recall how many hours on average they slept per night between the ages of 15 and 19 years and to rate their sleep quality during that time.
Results showed that individuals who slept fewer than 7 hours a night during their teen years were 40% more likely to have MS as adults (odds ratio [OR], 1.4; 95% confidence interval [CI], 1.1-1.7).
Poor sleep quality increased MS risk even more (OR, 1.5; 95% CI, 1.3-1.9).
The association remained strong even after adjustment for additional sleep on weekends and breaks and excluding shift workers.
Long sleep ‘apparently good’
The researchers also conducted several sensitivity studies to rule out confounders that might bias the association, such as excluding participants who reported currently experiencing less sleep or poor sleep.
“You would expect that people who are suffering from sleep problems today would be the people who reported sleep problems during their youth,” but that didn’t happen, Dr. Åkerstedt noted.
The investigators also entered data on sleep duration and sleep quality at the same time, thinking the data would cancel each other out. However, the association remained the same.
“Quite often you see that sleep duration would eliminate the effect of sleep complaints in the prediction of disease, but here both remain significant when they are entered at the same time,” Dr. Åkerstedt said. “You get the feeling that this might mean they act together to produce results,” he added.
“One other thing that surprised me is that long sleep was apparently good,” said Dr. Åkerstedt.
The investigators have conducted several studies on sleep duration and mortality. In recent research, they found that both short sleep and long sleep predicted mortality – “and often, long sleep is a stronger predictor than short sleep,” he said.
Underestimated problem?
Commenting on the findings, Kathleen Zackowski, PhD, associate vice president of research for the National Multiple Sclerosis Society in Baltimore, noted that participants were asked to rate their own sleep quality during adolescence, a subjective report that may mean sleep quality has an even larger association with MS risk.
“That they found a result with sleep quality says to me that there probably is a bigger problem, because I don’t know if people over- or underestimate their sleep quality,” said Dr. Zackowski, who was not involved with the research.
“If we could get to that sleep quality question a little more objectively, I bet that we’d find there’s a lot more to the story,” she said.
That’s a story the researchers would like to explore, Dr. Åkerstedt reported. Designing a prospective study that more closely tracks sleeping habits during adolescence and follows individuals through adulthood could provide valuable information about how sleep quality and duration affect immune system development and MS risk, he said.
Dr. Zackowski said clinicians know that MS is not caused just by a genetic abnormality and that other environmental lifestyle factors seem to play a part.
“If we find out that sleep is one of those lifestyle factors, this is very changeable,” she added.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, the Swedish Brain Foundation, AFA Insurance, the European Aviation Safety Authority, the Tercentenary Fund of the Bank of Sweden, the Margaretha af Ugglas Foundation, the Swedish Foundation for MS Research, and NEURO Sweden. Dr. Åkerstadt has been supported by Tercentenary Fund of Bank of Sweden, AFA Insurance, and the European Aviation Safety Authority. Dr. Zackowski reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Too little sleep or poor sleep quality during the teen years can significantly increase the risk for multiple sclerosis (MS) during adulthood, new research suggests.
In a large case-control study, individuals who slept less than 7 hours a night on average during adolescence were 40% more likely to develop MS later on. The risk was even higher for those who rated their sleep quality as bad.
On the other hand, MS was significantly less common among individuals who slept longer as teens – indicating a possible protective benefit.
While sleep duration has been associated with mortality or disease risk for other conditions, sleep quality usually has little to no effect on risk, lead investigator Torbjörn Åkerstedt, PhD, sleep researcher and professor of psychology, department of neuroscience, Karolinska Institutet, Stockholm, told this news organization.
“I hadn’t really expected that, but those results were quite strong, even stronger than sleep duration,” Dr. Åkerstedt said.
“We don’t really know why this is happening in young age, but the most suitable explanation is that the brain in still developing quite a bit, and you’re interfering with it,” he added.
The findings were published online in the Journal of Neurology, Neurosurgery and Psychiatry.
Strong association
Other studies have tied sleep deprivation to increased risk for serious illness, but the link between sleep and MS risk isn’t as well studied.
Previous research by Dr. Åkerstedt showed that the risk for MS was higher among individuals who took part in shift work before the age of 20. However, the impact of sleep duration or quality among teens was unknown.
The current Swedish population-based case-control study included 2,075 patients with MS and 3,164 without the disorder. All participants were asked to recall how many hours on average they slept per night between the ages of 15 and 19 years and to rate their sleep quality during that time.
Results showed that individuals who slept fewer than 7 hours a night during their teen years were 40% more likely to have MS as adults (odds ratio [OR], 1.4; 95% confidence interval [CI], 1.1-1.7).
Poor sleep quality increased MS risk even more (OR, 1.5; 95% CI, 1.3-1.9).
The association remained strong even after adjustment for additional sleep on weekends and breaks and excluding shift workers.
Long sleep ‘apparently good’
The researchers also conducted several sensitivity studies to rule out confounders that might bias the association, such as excluding participants who reported currently experiencing less sleep or poor sleep.
“You would expect that people who are suffering from sleep problems today would be the people who reported sleep problems during their youth,” but that didn’t happen, Dr. Åkerstedt noted.
The investigators also entered data on sleep duration and sleep quality at the same time, thinking the data would cancel each other out. However, the association remained the same.
“Quite often you see that sleep duration would eliminate the effect of sleep complaints in the prediction of disease, but here both remain significant when they are entered at the same time,” Dr. Åkerstedt said. “You get the feeling that this might mean they act together to produce results,” he added.
“One other thing that surprised me is that long sleep was apparently good,” said Dr. Åkerstedt.
The investigators have conducted several studies on sleep duration and mortality. In recent research, they found that both short sleep and long sleep predicted mortality – “and often, long sleep is a stronger predictor than short sleep,” he said.
Underestimated problem?
Commenting on the findings, Kathleen Zackowski, PhD, associate vice president of research for the National Multiple Sclerosis Society in Baltimore, noted that participants were asked to rate their own sleep quality during adolescence, a subjective report that may mean sleep quality has an even larger association with MS risk.
“That they found a result with sleep quality says to me that there probably is a bigger problem, because I don’t know if people over- or underestimate their sleep quality,” said Dr. Zackowski, who was not involved with the research.
“If we could get to that sleep quality question a little more objectively, I bet that we’d find there’s a lot more to the story,” she said.
That’s a story the researchers would like to explore, Dr. Åkerstedt reported. Designing a prospective study that more closely tracks sleeping habits during adolescence and follows individuals through adulthood could provide valuable information about how sleep quality and duration affect immune system development and MS risk, he said.
Dr. Zackowski said clinicians know that MS is not caused just by a genetic abnormality and that other environmental lifestyle factors seem to play a part.
“If we find out that sleep is one of those lifestyle factors, this is very changeable,” she added.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, the Swedish Brain Foundation, AFA Insurance, the European Aviation Safety Authority, the Tercentenary Fund of the Bank of Sweden, the Margaretha af Ugglas Foundation, the Swedish Foundation for MS Research, and NEURO Sweden. Dr. Åkerstadt has been supported by Tercentenary Fund of Bank of Sweden, AFA Insurance, and the European Aviation Safety Authority. Dr. Zackowski reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children and COVID: Weekly cases may have doubled in early January
Although new COVID-19 cases in children, as measured by the American Academy of Pediatrics and the Children’s Hospital Association, have remained fairly steady in recent months, data from the Centers for Diseases Control and Prevention suggest that weekly cases took a big jump in early January.
For the most recent week covered . New cases for the first 2 weeks of the year – 31,000 for the week of Dec. 30 to Jan. 5 and 26,000 during Jan. 6-12 – were consistent with the AAP/CHA assertion that “weekly reported child cases have plateaued at an average of about 32,000 cases ... over the past 4 months.”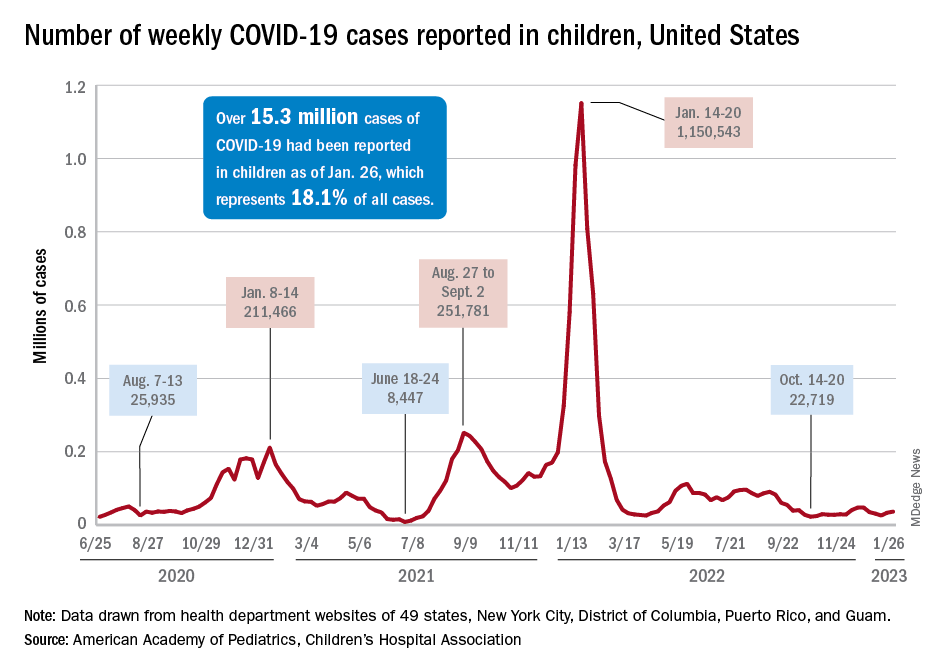
The CDC data, however, show that new cases doubled during the week of Jan. 1-7 to over 65,000, compared with the end of December, and stayed at that level for Jan. 8-14, and since CDC figures are subject to a 6-week reporting delay, the final numbers are likely to be even higher. The composition by age changed somewhat between the 2 weeks, though, as those aged 0-4 years went from almost half of all cases in the first week down to 40% in the second, while cases rose for children aged 5-11 and 12-15, based on data from the COVID-19 response team.
Emergency department visits for January do not show a corresponding increase. ED visits among children aged 0-11 years with COVID-19, measured as a percentage of all ED visits, declined over the course of the month, as did visits for 16- and 17-year-olds, while those aged 12-15 started the month at 1.4% and were at 1.4% on Jan. 27, with a slight dip down to 1.2% in between, the CDC said on its COVID Data Tracker. Daily hospitalizations for children aged 0-17 also declined through mid-January and did not reflect the jump in new cases.
Meanwhile, vaccinated children are still in the minority: 57% of those under age 18 have received no COVID vaccine yet, the AAP said in a separate report. Just 7.4% of children under age 2 years had received at least one dose as of Jan. 25, as had 10.1% of those aged 2-4 years, 39.6% of 5- to 11-year-olds and 71.8% of those 12-17 years old, according to the CDC, with corresponding figures for completion of the primary series at 3.5%, 5.3%, 32.5%, and 61.5%.
Although new COVID-19 cases in children, as measured by the American Academy of Pediatrics and the Children’s Hospital Association, have remained fairly steady in recent months, data from the Centers for Diseases Control and Prevention suggest that weekly cases took a big jump in early January.
For the most recent week covered . New cases for the first 2 weeks of the year – 31,000 for the week of Dec. 30 to Jan. 5 and 26,000 during Jan. 6-12 – were consistent with the AAP/CHA assertion that “weekly reported child cases have plateaued at an average of about 32,000 cases ... over the past 4 months.”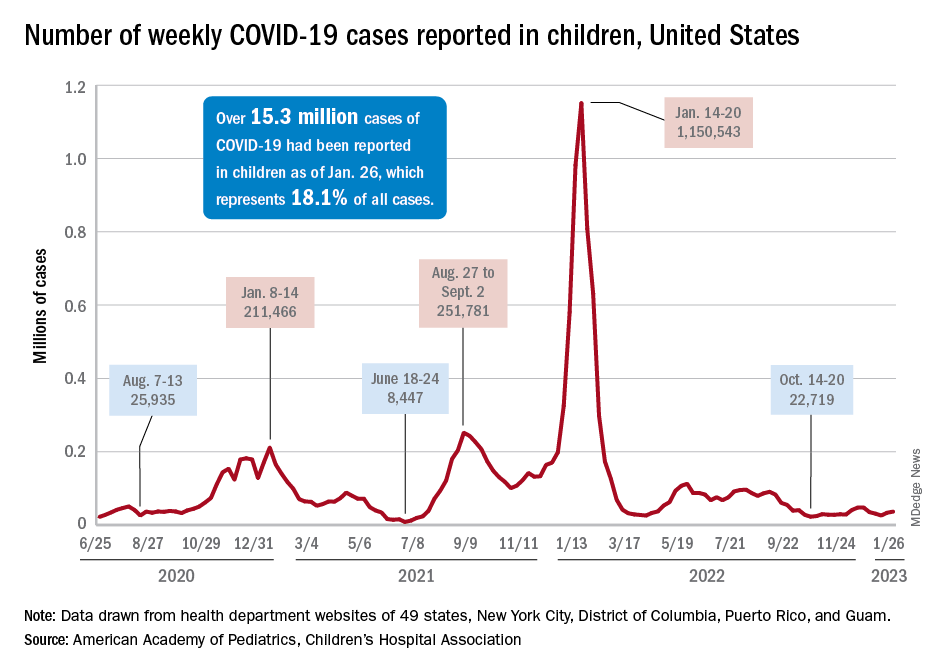
The CDC data, however, show that new cases doubled during the week of Jan. 1-7 to over 65,000, compared with the end of December, and stayed at that level for Jan. 8-14, and since CDC figures are subject to a 6-week reporting delay, the final numbers are likely to be even higher. The composition by age changed somewhat between the 2 weeks, though, as those aged 0-4 years went from almost half of all cases in the first week down to 40% in the second, while cases rose for children aged 5-11 and 12-15, based on data from the COVID-19 response team.
Emergency department visits for January do not show a corresponding increase. ED visits among children aged 0-11 years with COVID-19, measured as a percentage of all ED visits, declined over the course of the month, as did visits for 16- and 17-year-olds, while those aged 12-15 started the month at 1.4% and were at 1.4% on Jan. 27, with a slight dip down to 1.2% in between, the CDC said on its COVID Data Tracker. Daily hospitalizations for children aged 0-17 also declined through mid-January and did not reflect the jump in new cases.
Meanwhile, vaccinated children are still in the minority: 57% of those under age 18 have received no COVID vaccine yet, the AAP said in a separate report. Just 7.4% of children under age 2 years had received at least one dose as of Jan. 25, as had 10.1% of those aged 2-4 years, 39.6% of 5- to 11-year-olds and 71.8% of those 12-17 years old, according to the CDC, with corresponding figures for completion of the primary series at 3.5%, 5.3%, 32.5%, and 61.5%.
Although new COVID-19 cases in children, as measured by the American Academy of Pediatrics and the Children’s Hospital Association, have remained fairly steady in recent months, data from the Centers for Diseases Control and Prevention suggest that weekly cases took a big jump in early January.
For the most recent week covered . New cases for the first 2 weeks of the year – 31,000 for the week of Dec. 30 to Jan. 5 and 26,000 during Jan. 6-12 – were consistent with the AAP/CHA assertion that “weekly reported child cases have plateaued at an average of about 32,000 cases ... over the past 4 months.”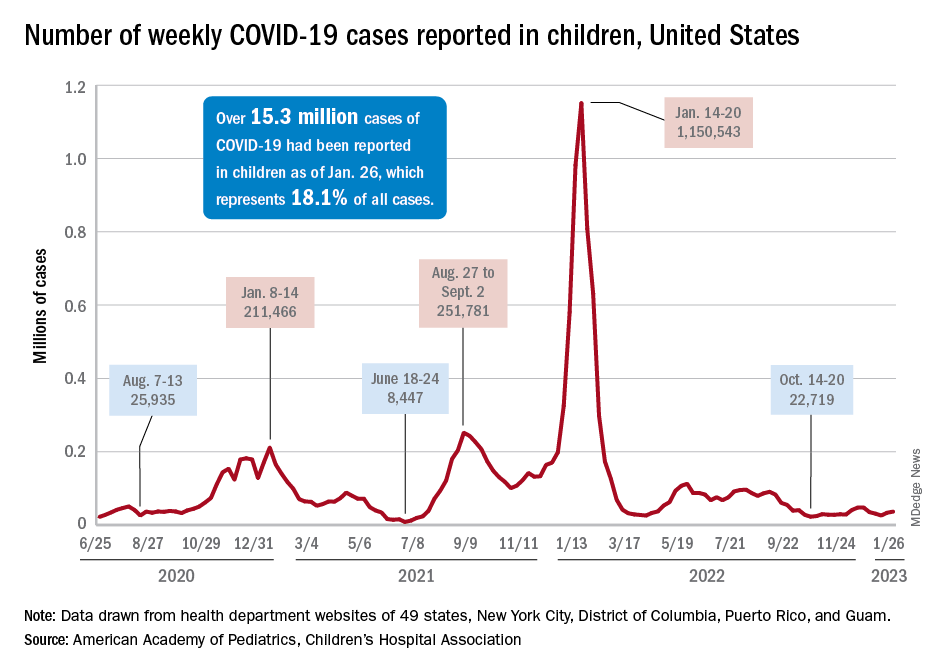
The CDC data, however, show that new cases doubled during the week of Jan. 1-7 to over 65,000, compared with the end of December, and stayed at that level for Jan. 8-14, and since CDC figures are subject to a 6-week reporting delay, the final numbers are likely to be even higher. The composition by age changed somewhat between the 2 weeks, though, as those aged 0-4 years went from almost half of all cases in the first week down to 40% in the second, while cases rose for children aged 5-11 and 12-15, based on data from the COVID-19 response team.
Emergency department visits for January do not show a corresponding increase. ED visits among children aged 0-11 years with COVID-19, measured as a percentage of all ED visits, declined over the course of the month, as did visits for 16- and 17-year-olds, while those aged 12-15 started the month at 1.4% and were at 1.4% on Jan. 27, with a slight dip down to 1.2% in between, the CDC said on its COVID Data Tracker. Daily hospitalizations for children aged 0-17 also declined through mid-January and did not reflect the jump in new cases.
Meanwhile, vaccinated children are still in the minority: 57% of those under age 18 have received no COVID vaccine yet, the AAP said in a separate report. Just 7.4% of children under age 2 years had received at least one dose as of Jan. 25, as had 10.1% of those aged 2-4 years, 39.6% of 5- to 11-year-olds and 71.8% of those 12-17 years old, according to the CDC, with corresponding figures for completion of the primary series at 3.5%, 5.3%, 32.5%, and 61.5%.
Managing respiratory symptoms in the ‘tripledemic’ era
Is it COVID-19, flu, or even RSV? I recently described just such a patient, an obese woman with type 2 diabetes, presenting with fever, cough, myalgia, and fatigue. I asked readers whether they agreed with my management of this patient.
Thank you for your comments as we continue to react to high rates of URIs. Your comments highlight the importance of local resources and practice habits when managing patients with URI.
It was clear that readers value testing to distinguish between infections. However, access to testing is highly variable around the world and is likely to be routinely used only in high-income countries. The Kaiser Family Foundation performed a cost analysis of testing for SARS-CoV-2 in 2020 and found, not surprisingly, wide variability in the cost of testing. Medicare covers tests at rates of $36-$143 per test; a study of list prices for SARS-CoV-2 tests at 93 hospitals found a median cost of $148 per test. And this does not include collection or facility fees. About 20% of tests cost more than $300.
These costs are prohibitive for many health systems. However, more devices have been introduced since that analysis, and competition and evolving technology should drive down prices. Generally, multiplex polymerase chain reaction (PCR) testing for multiple pathogens is less expensive than ordering two or three separate molecular tests and is more convenient for patients and practices alike.
Other reader comments focused on the challenges of getting accurate data on viral epidemiology, and there is certainly a time lag between infection trends and public health reports. This is exacerbated by underreporting of symptoms and more testing at home using antigen tests.
But please do not give up on epidemiology! If a test such as PCR is 90% sensitive for identifying infection, the yield in terms of the number of individuals infected with a particular virus should be high, and that is true when infection is in broad circulation. If 20% of a population of 1,000 has an infection and the test sensitivity is 90%, the yield of testing is 180 true cases versus 20 false positives.
However, if just 2% of the population of 1,000 has the infection in this same scenario, then only 18 true cases are identified. The effect on public health is certainly less, and a lower prevalence rate means that confounding variables, such as how long an individual might shed viral particles and the method of sample collection, have an outsized effect on results. This reduces the validity of diagnostic tests.
Even trends on a national level can provide some insight regarding whom to test. Traditionally, our practice has been to not routinely test patients for influenza or RSV from late spring to early fall unless there was a compelling reason, such as recent travel to an area where these infections were more prevalent. The loss of temporality for these infections since 2020 has altered this approach and made us pay more attention to reports from public health organizations.
I also appreciate the discussion of how to treat Agnes’s symptoms as she waits to improve, and anyone who suffers with or treats a viral URI knows that there are few interventions effective for such symptoms as cough and congestion. A systematic review of 29 randomized controlled trials of over-the-counter medications for cough yielded mixed and largely negative results.
Antihistamines alone do not seem to work, and guaifenesin was successful in only one of three trials. Combinations of different drug classes appeared to be slightly more effective.
My personal favorite for the management of acute cough is something that kids generally love: honey. In a review of 14 studies, 9 of which were limited to pediatric patients, honey was associated with significant reductions in cough frequency, cough severity, and total symptom score. However, there was a moderate risk of bias in the included research, and evidence of honey’s benefit in placebo-controlled trials was limited. Honey used in this research came in a variety of forms, so the best dosage is uncertain.
Clearly, advancements are needed. Better symptom management in viral URI will almost certainly improve productivity across the population and will probably reduce the inappropriate use of antibiotics as well. I have said for years that the scientists who can solve the Gordian knot of pediatric mucus deserve three Nobel prizes. I look forward to that golden day.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported a conflict of interest with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Is it COVID-19, flu, or even RSV? I recently described just such a patient, an obese woman with type 2 diabetes, presenting with fever, cough, myalgia, and fatigue. I asked readers whether they agreed with my management of this patient.
Thank you for your comments as we continue to react to high rates of URIs. Your comments highlight the importance of local resources and practice habits when managing patients with URI.
It was clear that readers value testing to distinguish between infections. However, access to testing is highly variable around the world and is likely to be routinely used only in high-income countries. The Kaiser Family Foundation performed a cost analysis of testing for SARS-CoV-2 in 2020 and found, not surprisingly, wide variability in the cost of testing. Medicare covers tests at rates of $36-$143 per test; a study of list prices for SARS-CoV-2 tests at 93 hospitals found a median cost of $148 per test. And this does not include collection or facility fees. About 20% of tests cost more than $300.
These costs are prohibitive for many health systems. However, more devices have been introduced since that analysis, and competition and evolving technology should drive down prices. Generally, multiplex polymerase chain reaction (PCR) testing for multiple pathogens is less expensive than ordering two or three separate molecular tests and is more convenient for patients and practices alike.
Other reader comments focused on the challenges of getting accurate data on viral epidemiology, and there is certainly a time lag between infection trends and public health reports. This is exacerbated by underreporting of symptoms and more testing at home using antigen tests.
But please do not give up on epidemiology! If a test such as PCR is 90% sensitive for identifying infection, the yield in terms of the number of individuals infected with a particular virus should be high, and that is true when infection is in broad circulation. If 20% of a population of 1,000 has an infection and the test sensitivity is 90%, the yield of testing is 180 true cases versus 20 false positives.
However, if just 2% of the population of 1,000 has the infection in this same scenario, then only 18 true cases are identified. The effect on public health is certainly less, and a lower prevalence rate means that confounding variables, such as how long an individual might shed viral particles and the method of sample collection, have an outsized effect on results. This reduces the validity of diagnostic tests.
Even trends on a national level can provide some insight regarding whom to test. Traditionally, our practice has been to not routinely test patients for influenza or RSV from late spring to early fall unless there was a compelling reason, such as recent travel to an area where these infections were more prevalent. The loss of temporality for these infections since 2020 has altered this approach and made us pay more attention to reports from public health organizations.
I also appreciate the discussion of how to treat Agnes’s symptoms as she waits to improve, and anyone who suffers with or treats a viral URI knows that there are few interventions effective for such symptoms as cough and congestion. A systematic review of 29 randomized controlled trials of over-the-counter medications for cough yielded mixed and largely negative results.
Antihistamines alone do not seem to work, and guaifenesin was successful in only one of three trials. Combinations of different drug classes appeared to be slightly more effective.
My personal favorite for the management of acute cough is something that kids generally love: honey. In a review of 14 studies, 9 of which were limited to pediatric patients, honey was associated with significant reductions in cough frequency, cough severity, and total symptom score. However, there was a moderate risk of bias in the included research, and evidence of honey’s benefit in placebo-controlled trials was limited. Honey used in this research came in a variety of forms, so the best dosage is uncertain.
Clearly, advancements are needed. Better symptom management in viral URI will almost certainly improve productivity across the population and will probably reduce the inappropriate use of antibiotics as well. I have said for years that the scientists who can solve the Gordian knot of pediatric mucus deserve three Nobel prizes. I look forward to that golden day.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported a conflict of interest with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Is it COVID-19, flu, or even RSV? I recently described just such a patient, an obese woman with type 2 diabetes, presenting with fever, cough, myalgia, and fatigue. I asked readers whether they agreed with my management of this patient.
Thank you for your comments as we continue to react to high rates of URIs. Your comments highlight the importance of local resources and practice habits when managing patients with URI.
It was clear that readers value testing to distinguish between infections. However, access to testing is highly variable around the world and is likely to be routinely used only in high-income countries. The Kaiser Family Foundation performed a cost analysis of testing for SARS-CoV-2 in 2020 and found, not surprisingly, wide variability in the cost of testing. Medicare covers tests at rates of $36-$143 per test; a study of list prices for SARS-CoV-2 tests at 93 hospitals found a median cost of $148 per test. And this does not include collection or facility fees. About 20% of tests cost more than $300.
These costs are prohibitive for many health systems. However, more devices have been introduced since that analysis, and competition and evolving technology should drive down prices. Generally, multiplex polymerase chain reaction (PCR) testing for multiple pathogens is less expensive than ordering two or three separate molecular tests and is more convenient for patients and practices alike.
Other reader comments focused on the challenges of getting accurate data on viral epidemiology, and there is certainly a time lag between infection trends and public health reports. This is exacerbated by underreporting of symptoms and more testing at home using antigen tests.
But please do not give up on epidemiology! If a test such as PCR is 90% sensitive for identifying infection, the yield in terms of the number of individuals infected with a particular virus should be high, and that is true when infection is in broad circulation. If 20% of a population of 1,000 has an infection and the test sensitivity is 90%, the yield of testing is 180 true cases versus 20 false positives.
However, if just 2% of the population of 1,000 has the infection in this same scenario, then only 18 true cases are identified. The effect on public health is certainly less, and a lower prevalence rate means that confounding variables, such as how long an individual might shed viral particles and the method of sample collection, have an outsized effect on results. This reduces the validity of diagnostic tests.
Even trends on a national level can provide some insight regarding whom to test. Traditionally, our practice has been to not routinely test patients for influenza or RSV from late spring to early fall unless there was a compelling reason, such as recent travel to an area where these infections were more prevalent. The loss of temporality for these infections since 2020 has altered this approach and made us pay more attention to reports from public health organizations.
I also appreciate the discussion of how to treat Agnes’s symptoms as she waits to improve, and anyone who suffers with or treats a viral URI knows that there are few interventions effective for such symptoms as cough and congestion. A systematic review of 29 randomized controlled trials of over-the-counter medications for cough yielded mixed and largely negative results.
Antihistamines alone do not seem to work, and guaifenesin was successful in only one of three trials. Combinations of different drug classes appeared to be slightly more effective.
My personal favorite for the management of acute cough is something that kids generally love: honey. In a review of 14 studies, 9 of which were limited to pediatric patients, honey was associated with significant reductions in cough frequency, cough severity, and total symptom score. However, there was a moderate risk of bias in the included research, and evidence of honey’s benefit in placebo-controlled trials was limited. Honey used in this research came in a variety of forms, so the best dosage is uncertain.
Clearly, advancements are needed. Better symptom management in viral URI will almost certainly improve productivity across the population and will probably reduce the inappropriate use of antibiotics as well. I have said for years that the scientists who can solve the Gordian knot of pediatric mucus deserve three Nobel prizes. I look forward to that golden day.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported a conflict of interest with McNeil Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Citing workplace violence, one-fourth of critical care workers are ready to quit
A surgeon in Tulsa shot by a disgruntled patient. A doctor in India beaten by a group of bereaved family members. A general practitioner in the United Kingdom threatened with stabbing. A new study identifies this trend and finds that 25% of health care workers polled were willing to quit because of such violence.
“That was pretty appalling,” Rahul Kashyap, MD, MBA, MBBS, recalls. Dr. Kashyap is one of the leaders of the Violence Study of Healthcare Workers and Systems (ViSHWaS), which polled an international sample of physicians, nurses, and hospital staff. This study has worrying implications, Dr. Kashyap says. In a time when hospital staff are reporting burnout in record numbers, further deterrents may be the last thing our health care system needs. But Dr. Kashyap hopes that bringing awareness to these trends may allow physicians, policymakers, and the public to mobilize and intervene before it’s too late.
Previous studies have revealed similar trends. The rate of workplace violence directed at U.S. health care workers is five times that of workers in any other industry, according to the Bureau of Labor Statistics. The same study found that attacks had increased 63% from 2011 to 2018. Other polls that focus on the pandemic show that nearly half of U.S. nurses believe that violence increased since the world shut down. Well before the pandemic, however, a study from the Indian Medical Association found that 75% of doctors experienced workplace violence.
With this history in mind, perhaps it’s not surprising that the idea for the study came from the authors’ personal experiences. They had seen coworkers go through attacks, or they had endured attacks themselves, Dr. Kashyap says. But they couldn’t find any global data to back up these experiences. So Dr. Kashyap and his colleagues formed a web of volunteers dedicated to creating a cross-sectional study.
They got in touch with researchers from countries across Asia, the Middle East, South America, North America, and Africa. The initial group agreed to reach out to their contacts, casting a wide net. Researchers used WhatsApp, LinkedIn, and text messages to distribute the survey. Health care workers in each country completed the brief questionnaire, recalling their prepandemic world and evaluating their current one.
Within 2 months, they had reached health care workers in more than 100 countries. They concluded the study when they received about 5,000 results, according to Dr. Kashyap, and then began the process of stratifying the data. For this report, they focused on critical care, emergency medicine, and anesthesiology, which resulted in 598 responses from 69 countries. Of these, India and the United States had the highest number of participants.
In all, 73% of participants reported facing physical or verbal violence while in the hospital; 48% said they felt less motivated to work because of that violence; 39% of respondents believed that the amount of violence they experienced was the same as before the COVID-19 pandemic; and 36% of respondents believed that violence had increased. Even though they were trained on guidelines from the Occupational Safety and Health Administration, 20% of participants felt unprepared to face violence.
Although the study didn’t analyze the reasons workers felt this way, Dr. Kashyap speculates that it could be related to the medical distrust that grew during the pandemic or the stress patients and health care professionals experienced during its peak.
Regardless, the researchers say their study is a starting point. Now that the trend has been highlighted, it may be acted on.
Moving forward, Dr. Kashyap believes that controlling for different variables could determine whether factors like gender or shift time put a worker at higher risk for violence. He hopes it’s possible to interrupt these patterns and reestablish trust in the hospital environment. “It’s aspirational, but you’re hoping that through studies like ViSHWaS, which means trust in Hindi ... [we could restore] the trust and confidence among health care providers for the patients and family members.”
A version of this article first appeared on Medscape.com.
A surgeon in Tulsa shot by a disgruntled patient. A doctor in India beaten by a group of bereaved family members. A general practitioner in the United Kingdom threatened with stabbing. A new study identifies this trend and finds that 25% of health care workers polled were willing to quit because of such violence.
“That was pretty appalling,” Rahul Kashyap, MD, MBA, MBBS, recalls. Dr. Kashyap is one of the leaders of the Violence Study of Healthcare Workers and Systems (ViSHWaS), which polled an international sample of physicians, nurses, and hospital staff. This study has worrying implications, Dr. Kashyap says. In a time when hospital staff are reporting burnout in record numbers, further deterrents may be the last thing our health care system needs. But Dr. Kashyap hopes that bringing awareness to these trends may allow physicians, policymakers, and the public to mobilize and intervene before it’s too late.
Previous studies have revealed similar trends. The rate of workplace violence directed at U.S. health care workers is five times that of workers in any other industry, according to the Bureau of Labor Statistics. The same study found that attacks had increased 63% from 2011 to 2018. Other polls that focus on the pandemic show that nearly half of U.S. nurses believe that violence increased since the world shut down. Well before the pandemic, however, a study from the Indian Medical Association found that 75% of doctors experienced workplace violence.
With this history in mind, perhaps it’s not surprising that the idea for the study came from the authors’ personal experiences. They had seen coworkers go through attacks, or they had endured attacks themselves, Dr. Kashyap says. But they couldn’t find any global data to back up these experiences. So Dr. Kashyap and his colleagues formed a web of volunteers dedicated to creating a cross-sectional study.
They got in touch with researchers from countries across Asia, the Middle East, South America, North America, and Africa. The initial group agreed to reach out to their contacts, casting a wide net. Researchers used WhatsApp, LinkedIn, and text messages to distribute the survey. Health care workers in each country completed the brief questionnaire, recalling their prepandemic world and evaluating their current one.
Within 2 months, they had reached health care workers in more than 100 countries. They concluded the study when they received about 5,000 results, according to Dr. Kashyap, and then began the process of stratifying the data. For this report, they focused on critical care, emergency medicine, and anesthesiology, which resulted in 598 responses from 69 countries. Of these, India and the United States had the highest number of participants.
In all, 73% of participants reported facing physical or verbal violence while in the hospital; 48% said they felt less motivated to work because of that violence; 39% of respondents believed that the amount of violence they experienced was the same as before the COVID-19 pandemic; and 36% of respondents believed that violence had increased. Even though they were trained on guidelines from the Occupational Safety and Health Administration, 20% of participants felt unprepared to face violence.
Although the study didn’t analyze the reasons workers felt this way, Dr. Kashyap speculates that it could be related to the medical distrust that grew during the pandemic or the stress patients and health care professionals experienced during its peak.
Regardless, the researchers say their study is a starting point. Now that the trend has been highlighted, it may be acted on.
Moving forward, Dr. Kashyap believes that controlling for different variables could determine whether factors like gender or shift time put a worker at higher risk for violence. He hopes it’s possible to interrupt these patterns and reestablish trust in the hospital environment. “It’s aspirational, but you’re hoping that through studies like ViSHWaS, which means trust in Hindi ... [we could restore] the trust and confidence among health care providers for the patients and family members.”
A version of this article first appeared on Medscape.com.
A surgeon in Tulsa shot by a disgruntled patient. A doctor in India beaten by a group of bereaved family members. A general practitioner in the United Kingdom threatened with stabbing. A new study identifies this trend and finds that 25% of health care workers polled were willing to quit because of such violence.
“That was pretty appalling,” Rahul Kashyap, MD, MBA, MBBS, recalls. Dr. Kashyap is one of the leaders of the Violence Study of Healthcare Workers and Systems (ViSHWaS), which polled an international sample of physicians, nurses, and hospital staff. This study has worrying implications, Dr. Kashyap says. In a time when hospital staff are reporting burnout in record numbers, further deterrents may be the last thing our health care system needs. But Dr. Kashyap hopes that bringing awareness to these trends may allow physicians, policymakers, and the public to mobilize and intervene before it’s too late.
Previous studies have revealed similar trends. The rate of workplace violence directed at U.S. health care workers is five times that of workers in any other industry, according to the Bureau of Labor Statistics. The same study found that attacks had increased 63% from 2011 to 2018. Other polls that focus on the pandemic show that nearly half of U.S. nurses believe that violence increased since the world shut down. Well before the pandemic, however, a study from the Indian Medical Association found that 75% of doctors experienced workplace violence.
With this history in mind, perhaps it’s not surprising that the idea for the study came from the authors’ personal experiences. They had seen coworkers go through attacks, or they had endured attacks themselves, Dr. Kashyap says. But they couldn’t find any global data to back up these experiences. So Dr. Kashyap and his colleagues formed a web of volunteers dedicated to creating a cross-sectional study.
They got in touch with researchers from countries across Asia, the Middle East, South America, North America, and Africa. The initial group agreed to reach out to their contacts, casting a wide net. Researchers used WhatsApp, LinkedIn, and text messages to distribute the survey. Health care workers in each country completed the brief questionnaire, recalling their prepandemic world and evaluating their current one.
Within 2 months, they had reached health care workers in more than 100 countries. They concluded the study when they received about 5,000 results, according to Dr. Kashyap, and then began the process of stratifying the data. For this report, they focused on critical care, emergency medicine, and anesthesiology, which resulted in 598 responses from 69 countries. Of these, India and the United States had the highest number of participants.
In all, 73% of participants reported facing physical or verbal violence while in the hospital; 48% said they felt less motivated to work because of that violence; 39% of respondents believed that the amount of violence they experienced was the same as before the COVID-19 pandemic; and 36% of respondents believed that violence had increased. Even though they were trained on guidelines from the Occupational Safety and Health Administration, 20% of participants felt unprepared to face violence.
Although the study didn’t analyze the reasons workers felt this way, Dr. Kashyap speculates that it could be related to the medical distrust that grew during the pandemic or the stress patients and health care professionals experienced during its peak.
Regardless, the researchers say their study is a starting point. Now that the trend has been highlighted, it may be acted on.
Moving forward, Dr. Kashyap believes that controlling for different variables could determine whether factors like gender or shift time put a worker at higher risk for violence. He hopes it’s possible to interrupt these patterns and reestablish trust in the hospital environment. “It’s aspirational, but you’re hoping that through studies like ViSHWaS, which means trust in Hindi ... [we could restore] the trust and confidence among health care providers for the patients and family members.”
A version of this article first appeared on Medscape.com.
Biden to end COVID emergencies in May
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Female doctors have higher infertility rates and riskier pregnancies: What can be done?
In 2021, Eugene Kim, MD, division director of pediatric surgery and vice chair in the department of surgery at Cedars-Sinai Medical Center, Los Angeles, gave his presidential address to the Association for Academic Surgery.
“Presidents tend to give a message of hope or inspiration; I probably took it in a different way,” he said.
Dr. Kim told the story of one of his clinical partners, Eveline Shue, who, after five rounds of in vitro fertilization (IVF), became pregnant with twins. A high-achiever in her field, Ms. Shue continued working the grueling hours required by her job throughout pregnancy until she noticed concerning symptoms – musculoskeletal issues, extreme swelling, and more. She and her group decided that she should step back from work in her third trimester. A few days later, Ms. Shue suffered a stroke. She was rushed to the hospital where her babies were delivered by emergency C-section. Ms. Shue underwent brain surgery but later recovered and is still practicing in Southern California.
“I remember being at her bedside thinking, ‘How could we have let this happen? How could we have prevented this?’ ”
Dr. Kim’s speech kicked off a firestorm of awareness about pregnancy complications among physicians. “I got scores of emails from women around the country, surgeons in particular, who felt like their issues had been seen. The conversation was long overdue,” he said.
Family planning issues, pregnancy complications, infertility, and pregnancy loss are common, pervasive, and often silent issues in medicine. In July 2021, Dr. Kim and a group of other researchers published a study in JAMA Surgery. It revealed staggering truths: When compared to non-surgeons, female surgeons were more likely to delay pregnancy, use assisted reproductive technology such as IVF, have non-elective C-sections, and suffer pregnancy loss. In the study, 42% of surgeons had experienced pregnancy loss – more than double the rate of the general population. Almost half had serious pregnancy complications.
Research has found that female physicians in general have a significantly greater incidence of miscarriage, infertility, and pregnancy complications than the general population. According to a 2016 survey in the Journal of Women’s Health, the infertility rate for physicians is nearly 1 in 4, about double the rate of the general public.
The barriers to starting a family
Physicians face significant professional barriers that impact family planning. Demanding jobs with exhausting and often unpredictable hours contribute to a culture that, traditionally, has been far from family friendly. As a result, many physicians start families later. “For a pediatric surgeon, you finish training at age 35 – minimum,” says Dr. Kim. “Simply being a surgeon makes you a high-risk pregnancy candidate just because of the career.”
In 2020, Ariela L. Marshall, MD, an associate professor of clinical medicine at the University of Pennsylvania’s Perelman school of medicine, co-authored a commentary article in Academic Medicine titled “Physician Fertility: A Call to Action” which was based on her own experiences with infertility. Dr. Marshall was 34 when she and her husband decided to start a family, and she says her infertility diagnosis “came as a shock.”
“I never stopped to think about the consequences of a career path where I’m not going to be established until my 30s,” Dr. Marshall says. “I never thought about how long hours, overnight shifts, or working all the time could impact my fertility.”
It would take four cycles of IVF egg retrieval to create embryos and one failed implantation before Dr. Marshall became pregnant with her son.
When it comes to the timing of pregnancy, medical culture also plays a role. “There’s a lot of messaging around when it’s appropriate to carry a baby – and it’s not until after training is done,” says Arghavan Salles, MD, PhD, a clinical associate professor and special advisor for DEI programs at Stanford (Calif.) University’s department of medicine.
There are always exceptions. Some institutions are more flexible than others about pregnancy during residency. But Dr. Salles notes that this attitude is “not universal,” partly because of the lack of a comprehensive approach to pregnancy or parenthood in the United States. “There’s no federal paid parental leave in this country,” reminds Dr. Salles. “That signals that we don’t value parenting.”
The trickle-down effect of this in medicine is more like a waterfall. Some physicians complain when other physicians are out on leave. There’s an additional burden of work when people take time away, and there are often no support structures in place for backup or fill-in care. Dr. Salles said doctors often tell her that they were responsible for finding coverage for any time off during pregnancy or after becoming a parent. A paper of hers published in JAMA Surgery found that, for physicians, a fear of burdening others was a major barrier to getting pregnant during residency in the first place.
The physical consequences
Although research supports the benefits of physical activity throughout pregnancy, a job such as surgery that requires being on your feet for long periods of time “is not the same as exercise,” explains Erika Lu Rangel, MD, a gastrointestinal surgeon at Brigham and Women’s Hospital, Boston, and Dr. Kim’s lead author on the JAMA Surgery article.
Surgeons operating for more than 12 hours a week are at higher risk for pregnancy complications, the study found. Dr. Rangel also cites data suggesting that night shifts or swing shifts (the hours between day and night) put women at higher risk for pregnancy complications.
Equally alarming: Medical trainees appear to have “almost as high a rate of pregnancy complications as surgeons who have already completed their training,” said Dr. Rangel. It is a concerning finding since, as a younger cohort, they should have lower complication rates based on their age. But doctors in training may be on their feet even more than surgeons during long shifts.
Like Dr. Salles, Dr. Rangel sees these issues as part of a pervasive culture of “presenteeism” in medicine, and she points out that many surgeons don’t even take time off to grieve pregnancy loss or physically recover from it. “We work even when we’re sick and even when it’s not good for our health,” she said. “I think that’s an unhealthy behavior that we cultivate from the time that we’re trainees, and we carry it on through when we’re in practice.”
Penn Medicine’s Dr. Marshall remembers that her own maternity leave was “not an easy process to navigate.” From her hospital room on a magnesium drip for preeclampsia, she still attended Zoom meetings with her colleagues. “Nobody says, ‘Oh, you have to do this,’ ” Dr. Marshall explains, “but you wind up feeling guilty if you’re not there at all moments for everyone. That’s also something that needs to change.”
Dr. Rangel was pregnant with her oldest son as a fourth-year surgery resident. The day she gave birth to him she remembers waking up with a flu-like illness and a fever. She went to work anyway, because “you don’t call in sick as a resident.” She was barely able to complete her rounds and then had to lie down between cases. A co-resident found her and took her to labor and delivery. She had gone into premature labor at 37 weeks, and her son went into the NICU with complications.
“I remember feeling this enormous guilt,” says Dr. Rangel. “I’d been a mom for just a few minutes, and I felt like I had already failed him because I had prioritized what the residency thought of me above what I knew was necessary for his health.”
Hope for the future
Disturbed by the status quo, many physicians are pushing for change. “I think there’s a really important and positive conversation going on in the medical community right now about ways that we need to support new parent physicians,” said Dr. Rangel.
Parental leave is a key part of that support. Last year, The American Board of Medical Specialties enacted a mandate that all specialty boards 2 years or more in duration must provide at least 6 weeks of parental and caregiver leave. In 2023, the Accreditation Council for Graduate Medical Education (ACGME) required that all training programs match that policy. “This sends a message to policymakers and leaders in American medicine that this is a priority,” said Dr. Rangel.
In January 2022, a group from the University of Michigan also published an article in the Annals of Surgery called “Safe and Supported Pregnancy: A Call to Action for Surgery Chairs and Program Directors”. The essay urged leading groups such as the ACGME and the American Board of Surgery to “directly address the health and safety of pregnant trainees” and specifically, to “allow for further flexibility during training for pregnancy and peripartum periods,” calling these “fundamental necessities for cultural progress.”
Others have recommended allowing pregnant trainees more flexibility in their schedules or front-loading certain parts of the training that may be more difficult as a pregnancy progresses. Insurance coverage for fertility preservation and reproductive endocrinology services, and support for reentry (including lactation and childcare) are also issues that must be addressed, says Dr. Salles.
A new paper of Dr. Rangel’s, published in JAMA Surgery, suggests that things like mentorship for residents from faculty can also be important pieces of the puzzle.
Education about reproductive health must start earlier, too – as early as medical school. Research suggests only 8% of physicians receive education on the risks of delaying pregnancy. Those who do are significantly less likely to experience pregnancy loss or seek infertility treatment.
Dr. Salles recalls sitting in a classroom learning about advanced maternal age at a time when age 35 seemed unimaginably distant. “It was never taught – at least to my recollection – in a way that was like, ‘this could be your future,’ ” Dr. Salles says.” It was more like this abstract patient who might have advanced maternal age and what the consequences would be. Maybe some of my colleagues put two and two together, but I definitely didn’t.”
Dr. Marshall is the curriculum chair for the IGNITEMed Initiative, which aims to educate medical students about issues not discussed in traditional medical school curricula. Dr. Marshall and her colleague Julia Files, MD, talk with IGNITEMed students about reproductive life planning.
“Raising awareness is a very big thing. That’s not just true for medical students but for professionals at every level of medicine,” Dr. Marshall said. “Residency and fellowship training program directors, department chairs, and hospital CEOs all need to understand that these issues are very common in the people they oversee – and that they are medical issues, like any other medical issue, where people need time off and support.”
A version of this article first appeared on Medscape.com.
In 2021, Eugene Kim, MD, division director of pediatric surgery and vice chair in the department of surgery at Cedars-Sinai Medical Center, Los Angeles, gave his presidential address to the Association for Academic Surgery.
“Presidents tend to give a message of hope or inspiration; I probably took it in a different way,” he said.
Dr. Kim told the story of one of his clinical partners, Eveline Shue, who, after five rounds of in vitro fertilization (IVF), became pregnant with twins. A high-achiever in her field, Ms. Shue continued working the grueling hours required by her job throughout pregnancy until she noticed concerning symptoms – musculoskeletal issues, extreme swelling, and more. She and her group decided that she should step back from work in her third trimester. A few days later, Ms. Shue suffered a stroke. She was rushed to the hospital where her babies were delivered by emergency C-section. Ms. Shue underwent brain surgery but later recovered and is still practicing in Southern California.
“I remember being at her bedside thinking, ‘How could we have let this happen? How could we have prevented this?’ ”
Dr. Kim’s speech kicked off a firestorm of awareness about pregnancy complications among physicians. “I got scores of emails from women around the country, surgeons in particular, who felt like their issues had been seen. The conversation was long overdue,” he said.
Family planning issues, pregnancy complications, infertility, and pregnancy loss are common, pervasive, and often silent issues in medicine. In July 2021, Dr. Kim and a group of other researchers published a study in JAMA Surgery. It revealed staggering truths: When compared to non-surgeons, female surgeons were more likely to delay pregnancy, use assisted reproductive technology such as IVF, have non-elective C-sections, and suffer pregnancy loss. In the study, 42% of surgeons had experienced pregnancy loss – more than double the rate of the general population. Almost half had serious pregnancy complications.
Research has found that female physicians in general have a significantly greater incidence of miscarriage, infertility, and pregnancy complications than the general population. According to a 2016 survey in the Journal of Women’s Health, the infertility rate for physicians is nearly 1 in 4, about double the rate of the general public.
The barriers to starting a family
Physicians face significant professional barriers that impact family planning. Demanding jobs with exhausting and often unpredictable hours contribute to a culture that, traditionally, has been far from family friendly. As a result, many physicians start families later. “For a pediatric surgeon, you finish training at age 35 – minimum,” says Dr. Kim. “Simply being a surgeon makes you a high-risk pregnancy candidate just because of the career.”
In 2020, Ariela L. Marshall, MD, an associate professor of clinical medicine at the University of Pennsylvania’s Perelman school of medicine, co-authored a commentary article in Academic Medicine titled “Physician Fertility: A Call to Action” which was based on her own experiences with infertility. Dr. Marshall was 34 when she and her husband decided to start a family, and she says her infertility diagnosis “came as a shock.”
“I never stopped to think about the consequences of a career path where I’m not going to be established until my 30s,” Dr. Marshall says. “I never thought about how long hours, overnight shifts, or working all the time could impact my fertility.”
It would take four cycles of IVF egg retrieval to create embryos and one failed implantation before Dr. Marshall became pregnant with her son.
When it comes to the timing of pregnancy, medical culture also plays a role. “There’s a lot of messaging around when it’s appropriate to carry a baby – and it’s not until after training is done,” says Arghavan Salles, MD, PhD, a clinical associate professor and special advisor for DEI programs at Stanford (Calif.) University’s department of medicine.
There are always exceptions. Some institutions are more flexible than others about pregnancy during residency. But Dr. Salles notes that this attitude is “not universal,” partly because of the lack of a comprehensive approach to pregnancy or parenthood in the United States. “There’s no federal paid parental leave in this country,” reminds Dr. Salles. “That signals that we don’t value parenting.”
The trickle-down effect of this in medicine is more like a waterfall. Some physicians complain when other physicians are out on leave. There’s an additional burden of work when people take time away, and there are often no support structures in place for backup or fill-in care. Dr. Salles said doctors often tell her that they were responsible for finding coverage for any time off during pregnancy or after becoming a parent. A paper of hers published in JAMA Surgery found that, for physicians, a fear of burdening others was a major barrier to getting pregnant during residency in the first place.
The physical consequences
Although research supports the benefits of physical activity throughout pregnancy, a job such as surgery that requires being on your feet for long periods of time “is not the same as exercise,” explains Erika Lu Rangel, MD, a gastrointestinal surgeon at Brigham and Women’s Hospital, Boston, and Dr. Kim’s lead author on the JAMA Surgery article.
Surgeons operating for more than 12 hours a week are at higher risk for pregnancy complications, the study found. Dr. Rangel also cites data suggesting that night shifts or swing shifts (the hours between day and night) put women at higher risk for pregnancy complications.
Equally alarming: Medical trainees appear to have “almost as high a rate of pregnancy complications as surgeons who have already completed their training,” said Dr. Rangel. It is a concerning finding since, as a younger cohort, they should have lower complication rates based on their age. But doctors in training may be on their feet even more than surgeons during long shifts.
Like Dr. Salles, Dr. Rangel sees these issues as part of a pervasive culture of “presenteeism” in medicine, and she points out that many surgeons don’t even take time off to grieve pregnancy loss or physically recover from it. “We work even when we’re sick and even when it’s not good for our health,” she said. “I think that’s an unhealthy behavior that we cultivate from the time that we’re trainees, and we carry it on through when we’re in practice.”
Penn Medicine’s Dr. Marshall remembers that her own maternity leave was “not an easy process to navigate.” From her hospital room on a magnesium drip for preeclampsia, she still attended Zoom meetings with her colleagues. “Nobody says, ‘Oh, you have to do this,’ ” Dr. Marshall explains, “but you wind up feeling guilty if you’re not there at all moments for everyone. That’s also something that needs to change.”
Dr. Rangel was pregnant with her oldest son as a fourth-year surgery resident. The day she gave birth to him she remembers waking up with a flu-like illness and a fever. She went to work anyway, because “you don’t call in sick as a resident.” She was barely able to complete her rounds and then had to lie down between cases. A co-resident found her and took her to labor and delivery. She had gone into premature labor at 37 weeks, and her son went into the NICU with complications.
“I remember feeling this enormous guilt,” says Dr. Rangel. “I’d been a mom for just a few minutes, and I felt like I had already failed him because I had prioritized what the residency thought of me above what I knew was necessary for his health.”
Hope for the future
Disturbed by the status quo, many physicians are pushing for change. “I think there’s a really important and positive conversation going on in the medical community right now about ways that we need to support new parent physicians,” said Dr. Rangel.
Parental leave is a key part of that support. Last year, The American Board of Medical Specialties enacted a mandate that all specialty boards 2 years or more in duration must provide at least 6 weeks of parental and caregiver leave. In 2023, the Accreditation Council for Graduate Medical Education (ACGME) required that all training programs match that policy. “This sends a message to policymakers and leaders in American medicine that this is a priority,” said Dr. Rangel.
In January 2022, a group from the University of Michigan also published an article in the Annals of Surgery called “Safe and Supported Pregnancy: A Call to Action for Surgery Chairs and Program Directors”. The essay urged leading groups such as the ACGME and the American Board of Surgery to “directly address the health and safety of pregnant trainees” and specifically, to “allow for further flexibility during training for pregnancy and peripartum periods,” calling these “fundamental necessities for cultural progress.”
Others have recommended allowing pregnant trainees more flexibility in their schedules or front-loading certain parts of the training that may be more difficult as a pregnancy progresses. Insurance coverage for fertility preservation and reproductive endocrinology services, and support for reentry (including lactation and childcare) are also issues that must be addressed, says Dr. Salles.
A new paper of Dr. Rangel’s, published in JAMA Surgery, suggests that things like mentorship for residents from faculty can also be important pieces of the puzzle.
Education about reproductive health must start earlier, too – as early as medical school. Research suggests only 8% of physicians receive education on the risks of delaying pregnancy. Those who do are significantly less likely to experience pregnancy loss or seek infertility treatment.
Dr. Salles recalls sitting in a classroom learning about advanced maternal age at a time when age 35 seemed unimaginably distant. “It was never taught – at least to my recollection – in a way that was like, ‘this could be your future,’ ” Dr. Salles says.” It was more like this abstract patient who might have advanced maternal age and what the consequences would be. Maybe some of my colleagues put two and two together, but I definitely didn’t.”
Dr. Marshall is the curriculum chair for the IGNITEMed Initiative, which aims to educate medical students about issues not discussed in traditional medical school curricula. Dr. Marshall and her colleague Julia Files, MD, talk with IGNITEMed students about reproductive life planning.
“Raising awareness is a very big thing. That’s not just true for medical students but for professionals at every level of medicine,” Dr. Marshall said. “Residency and fellowship training program directors, department chairs, and hospital CEOs all need to understand that these issues are very common in the people they oversee – and that they are medical issues, like any other medical issue, where people need time off and support.”
A version of this article first appeared on Medscape.com.
In 2021, Eugene Kim, MD, division director of pediatric surgery and vice chair in the department of surgery at Cedars-Sinai Medical Center, Los Angeles, gave his presidential address to the Association for Academic Surgery.
“Presidents tend to give a message of hope or inspiration; I probably took it in a different way,” he said.
Dr. Kim told the story of one of his clinical partners, Eveline Shue, who, after five rounds of in vitro fertilization (IVF), became pregnant with twins. A high-achiever in her field, Ms. Shue continued working the grueling hours required by her job throughout pregnancy until she noticed concerning symptoms – musculoskeletal issues, extreme swelling, and more. She and her group decided that she should step back from work in her third trimester. A few days later, Ms. Shue suffered a stroke. She was rushed to the hospital where her babies were delivered by emergency C-section. Ms. Shue underwent brain surgery but later recovered and is still practicing in Southern California.
“I remember being at her bedside thinking, ‘How could we have let this happen? How could we have prevented this?’ ”
Dr. Kim’s speech kicked off a firestorm of awareness about pregnancy complications among physicians. “I got scores of emails from women around the country, surgeons in particular, who felt like their issues had been seen. The conversation was long overdue,” he said.
Family planning issues, pregnancy complications, infertility, and pregnancy loss are common, pervasive, and often silent issues in medicine. In July 2021, Dr. Kim and a group of other researchers published a study in JAMA Surgery. It revealed staggering truths: When compared to non-surgeons, female surgeons were more likely to delay pregnancy, use assisted reproductive technology such as IVF, have non-elective C-sections, and suffer pregnancy loss. In the study, 42% of surgeons had experienced pregnancy loss – more than double the rate of the general population. Almost half had serious pregnancy complications.
Research has found that female physicians in general have a significantly greater incidence of miscarriage, infertility, and pregnancy complications than the general population. According to a 2016 survey in the Journal of Women’s Health, the infertility rate for physicians is nearly 1 in 4, about double the rate of the general public.
The barriers to starting a family
Physicians face significant professional barriers that impact family planning. Demanding jobs with exhausting and often unpredictable hours contribute to a culture that, traditionally, has been far from family friendly. As a result, many physicians start families later. “For a pediatric surgeon, you finish training at age 35 – minimum,” says Dr. Kim. “Simply being a surgeon makes you a high-risk pregnancy candidate just because of the career.”
In 2020, Ariela L. Marshall, MD, an associate professor of clinical medicine at the University of Pennsylvania’s Perelman school of medicine, co-authored a commentary article in Academic Medicine titled “Physician Fertility: A Call to Action” which was based on her own experiences with infertility. Dr. Marshall was 34 when she and her husband decided to start a family, and she says her infertility diagnosis “came as a shock.”
“I never stopped to think about the consequences of a career path where I’m not going to be established until my 30s,” Dr. Marshall says. “I never thought about how long hours, overnight shifts, or working all the time could impact my fertility.”
It would take four cycles of IVF egg retrieval to create embryos and one failed implantation before Dr. Marshall became pregnant with her son.
When it comes to the timing of pregnancy, medical culture also plays a role. “There’s a lot of messaging around when it’s appropriate to carry a baby – and it’s not until after training is done,” says Arghavan Salles, MD, PhD, a clinical associate professor and special advisor for DEI programs at Stanford (Calif.) University’s department of medicine.
There are always exceptions. Some institutions are more flexible than others about pregnancy during residency. But Dr. Salles notes that this attitude is “not universal,” partly because of the lack of a comprehensive approach to pregnancy or parenthood in the United States. “There’s no federal paid parental leave in this country,” reminds Dr. Salles. “That signals that we don’t value parenting.”
The trickle-down effect of this in medicine is more like a waterfall. Some physicians complain when other physicians are out on leave. There’s an additional burden of work when people take time away, and there are often no support structures in place for backup or fill-in care. Dr. Salles said doctors often tell her that they were responsible for finding coverage for any time off during pregnancy or after becoming a parent. A paper of hers published in JAMA Surgery found that, for physicians, a fear of burdening others was a major barrier to getting pregnant during residency in the first place.
The physical consequences
Although research supports the benefits of physical activity throughout pregnancy, a job such as surgery that requires being on your feet for long periods of time “is not the same as exercise,” explains Erika Lu Rangel, MD, a gastrointestinal surgeon at Brigham and Women’s Hospital, Boston, and Dr. Kim’s lead author on the JAMA Surgery article.
Surgeons operating for more than 12 hours a week are at higher risk for pregnancy complications, the study found. Dr. Rangel also cites data suggesting that night shifts or swing shifts (the hours between day and night) put women at higher risk for pregnancy complications.
Equally alarming: Medical trainees appear to have “almost as high a rate of pregnancy complications as surgeons who have already completed their training,” said Dr. Rangel. It is a concerning finding since, as a younger cohort, they should have lower complication rates based on their age. But doctors in training may be on their feet even more than surgeons during long shifts.
Like Dr. Salles, Dr. Rangel sees these issues as part of a pervasive culture of “presenteeism” in medicine, and she points out that many surgeons don’t even take time off to grieve pregnancy loss or physically recover from it. “We work even when we’re sick and even when it’s not good for our health,” she said. “I think that’s an unhealthy behavior that we cultivate from the time that we’re trainees, and we carry it on through when we’re in practice.”
Penn Medicine’s Dr. Marshall remembers that her own maternity leave was “not an easy process to navigate.” From her hospital room on a magnesium drip for preeclampsia, she still attended Zoom meetings with her colleagues. “Nobody says, ‘Oh, you have to do this,’ ” Dr. Marshall explains, “but you wind up feeling guilty if you’re not there at all moments for everyone. That’s also something that needs to change.”
Dr. Rangel was pregnant with her oldest son as a fourth-year surgery resident. The day she gave birth to him she remembers waking up with a flu-like illness and a fever. She went to work anyway, because “you don’t call in sick as a resident.” She was barely able to complete her rounds and then had to lie down between cases. A co-resident found her and took her to labor and delivery. She had gone into premature labor at 37 weeks, and her son went into the NICU with complications.
“I remember feeling this enormous guilt,” says Dr. Rangel. “I’d been a mom for just a few minutes, and I felt like I had already failed him because I had prioritized what the residency thought of me above what I knew was necessary for his health.”
Hope for the future
Disturbed by the status quo, many physicians are pushing for change. “I think there’s a really important and positive conversation going on in the medical community right now about ways that we need to support new parent physicians,” said Dr. Rangel.
Parental leave is a key part of that support. Last year, The American Board of Medical Specialties enacted a mandate that all specialty boards 2 years or more in duration must provide at least 6 weeks of parental and caregiver leave. In 2023, the Accreditation Council for Graduate Medical Education (ACGME) required that all training programs match that policy. “This sends a message to policymakers and leaders in American medicine that this is a priority,” said Dr. Rangel.
In January 2022, a group from the University of Michigan also published an article in the Annals of Surgery called “Safe and Supported Pregnancy: A Call to Action for Surgery Chairs and Program Directors”. The essay urged leading groups such as the ACGME and the American Board of Surgery to “directly address the health and safety of pregnant trainees” and specifically, to “allow for further flexibility during training for pregnancy and peripartum periods,” calling these “fundamental necessities for cultural progress.”
Others have recommended allowing pregnant trainees more flexibility in their schedules or front-loading certain parts of the training that may be more difficult as a pregnancy progresses. Insurance coverage for fertility preservation and reproductive endocrinology services, and support for reentry (including lactation and childcare) are also issues that must be addressed, says Dr. Salles.
A new paper of Dr. Rangel’s, published in JAMA Surgery, suggests that things like mentorship for residents from faculty can also be important pieces of the puzzle.
Education about reproductive health must start earlier, too – as early as medical school. Research suggests only 8% of physicians receive education on the risks of delaying pregnancy. Those who do are significantly less likely to experience pregnancy loss or seek infertility treatment.
Dr. Salles recalls sitting in a classroom learning about advanced maternal age at a time when age 35 seemed unimaginably distant. “It was never taught – at least to my recollection – in a way that was like, ‘this could be your future,’ ” Dr. Salles says.” It was more like this abstract patient who might have advanced maternal age and what the consequences would be. Maybe some of my colleagues put two and two together, but I definitely didn’t.”
Dr. Marshall is the curriculum chair for the IGNITEMed Initiative, which aims to educate medical students about issues not discussed in traditional medical school curricula. Dr. Marshall and her colleague Julia Files, MD, talk with IGNITEMed students about reproductive life planning.
“Raising awareness is a very big thing. That’s not just true for medical students but for professionals at every level of medicine,” Dr. Marshall said. “Residency and fellowship training program directors, department chairs, and hospital CEOs all need to understand that these issues are very common in the people they oversee – and that they are medical issues, like any other medical issue, where people need time off and support.”
A version of this article first appeared on Medscape.com.

