User login
Robot pill wins AGA Shark Tank competition
SAN FRANCISCO – No one yet has figured out how to shrink doctors so they can make house calls inside the human blood stream as they did in the science fiction movie “Fantastic Voyage.” But the founders of a gastroenterology startup think they have the next best thing – a remote-controlled robot so small it can be swallowed like a pill.
The concept captured the imagination of a panel of judges earlier this month at the 2023 American Gastroenterological Association Tech Summit where it was named the winner of the annual Shark Tank innovation competition. The AGA Tech Summit and Shark Tank are the flagship events of the AGA Center for GI Innovation and Technology.
“This could be a game-changing investment down the line,” one of the judges, Amrita Sethi, MD, from Columbia University Medical Center in New York, said in an interview.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Hawyard, Calif.–based Endiatx is early in its voyage. , but CEO Torrey Smith, an aerospace engineer, sees future generations of the device operating on any diseased tissues that can be treated with surgery. “We believe teeny robots can go anywhere in the body,” he said.
The company executives envision that one day, robots small enough to enter the human brain will be able to eat away at tumors. “Imagine having your brain surgery while you’re on a ride at Disneyland,” said Endiatx cofounder and chair Alex Luebke. If that sounds fanciful, Mr. Smith cites a case report of a botfly larva that wormed its way into a human skull and ate a golf-ball sized chunk of brain.
Endiatx has raised $3 million and sent 24 of its robots swimming into the stomachs of its founding team. Mr. Smith himself has swallowed 15. Operators can use an external device with a joystick. Engineers have experimented with an Xbox video game controller to navigate around the stomach. The procedure requires no anesthesia.
The company expects to apply for Food and Drug Administration approval in 2025 or 2026. Mr. Smith is hoping the agency will approve it quickly because the robot pills are similar enough to passive camera pills that have been on the market for years.
But he also sees it as a crucial step forward because controlling the robot with three electric motors squirting water in six directions will allow physicians to point it at what they really need to see, not just hope to get a lucky shot of a problem area as the device floats by.
The most immediate technical challenge is improving the quality of the pill’s video. “We’re evaluating different cameras but we know we can’t be inferior on the imaging side,” Mr. Smith said.
Attention from the AGA is crucial because the team of engineers wants physicians to help it improve the robot pill, Mr. Luebeke said. “We can build anything, but we need guidance about what the market needs. Doctors have to say, ‘We need you to tweak it this way or that way.’ ”
The business opportunity is large, Mr. Smith said, with 7.5 million upper endoscopies out of 223 million endoscopic procedures done per year in the United States.
Endiatx figures the gross margin on procedures with the robot pills is 90%-95% because the manufacturing cost is about $50 per pill, but physicians can bill $500 for them using existing CPT codes for passive pill cameras.
Dr. Sethi said the robot pill stood out among other contenders because of the dire need for improved endoscopy technology.
Endiatx will represent AGA at the 2023 Digestive Disease Week® (DDW) Shark Tank pitch competition.
Four other finalists
The choice that received the most votes from the audience was Ezalife’s Button Huggie, a device for securing gastrostomy and cecostomy buttons. It includes a reusable, child-proof lid with a disposable, biodegradable, gauze sponge and a base layer held in place with a long-wearing adhesive. This prevents button movement in the tract, which can delay wound healing and lead to complications. In addition, the Button Huggie is much easier to put in place. “Our device is novel, with no direct competitors,” said CTO/COO Tyler Mironuck.
Currently patients are advised to fasten gastrostomy and cecostomy buttons with tape, but the buttons are dislodged 7% of the time, he said. The company estimates that patients spend an average of $100 a month on tape and gauze. The Button Huggie can be manufactured for $56, and the company envisions selling them for $300.
The device is exempt from needing a 510K FDA approval, so it can get to the market quickly. Nevertheless, the company is conducting a clinical trial with 200 patients at five children’s hospitals, Mr. Mironuck said.
NovaScan was a finalist for nsCanary, a device that uses electrical impedance to detect cancer. The device hinges on the company’s discovery that the Cole relaxation frequency is orders of magnitude different for cancerous and benign tissue, yet not affected by mass. By measuring this frequency, the nsCanary can find cancer in tissue acquired through biopsy forceps, snare polypectomy, mucosal resection, and endoscopic ultrasound-guided fine needle biopsy. It works in seconds without the need to interpret images.
Atlas Endoscopy was recognized for REN, a robotic colonoscopy system. The operator uses an external actuating magnet above the patient to guide a disposable ultracompliant endoscope through the colon. The company says this form of navigation prevents looping, reduces pain, and minimizes tissue stress.
Limaca Medical was recognized for Precision, a motorized, automated, rotational cutting and coring needle for endoscopic ultrasound biopsy. Manual biopsy needles now on the market require repeat passes in and out of the endoscope to obtain fragments of tissue, but Precision obtains larger intact samples of tumor tissue in a single pass.
Dr. Sethi has served as a consultant for Boston Scientific, Medtronic and Olympus; as a board member for EndoSound and has received grant support from FUJIFILM.
SAN FRANCISCO – No one yet has figured out how to shrink doctors so they can make house calls inside the human blood stream as they did in the science fiction movie “Fantastic Voyage.” But the founders of a gastroenterology startup think they have the next best thing – a remote-controlled robot so small it can be swallowed like a pill.
The concept captured the imagination of a panel of judges earlier this month at the 2023 American Gastroenterological Association Tech Summit where it was named the winner of the annual Shark Tank innovation competition. The AGA Tech Summit and Shark Tank are the flagship events of the AGA Center for GI Innovation and Technology.
“This could be a game-changing investment down the line,” one of the judges, Amrita Sethi, MD, from Columbia University Medical Center in New York, said in an interview.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Hawyard, Calif.–based Endiatx is early in its voyage. , but CEO Torrey Smith, an aerospace engineer, sees future generations of the device operating on any diseased tissues that can be treated with surgery. “We believe teeny robots can go anywhere in the body,” he said.
The company executives envision that one day, robots small enough to enter the human brain will be able to eat away at tumors. “Imagine having your brain surgery while you’re on a ride at Disneyland,” said Endiatx cofounder and chair Alex Luebke. If that sounds fanciful, Mr. Smith cites a case report of a botfly larva that wormed its way into a human skull and ate a golf-ball sized chunk of brain.
Endiatx has raised $3 million and sent 24 of its robots swimming into the stomachs of its founding team. Mr. Smith himself has swallowed 15. Operators can use an external device with a joystick. Engineers have experimented with an Xbox video game controller to navigate around the stomach. The procedure requires no anesthesia.
The company expects to apply for Food and Drug Administration approval in 2025 or 2026. Mr. Smith is hoping the agency will approve it quickly because the robot pills are similar enough to passive camera pills that have been on the market for years.
But he also sees it as a crucial step forward because controlling the robot with three electric motors squirting water in six directions will allow physicians to point it at what they really need to see, not just hope to get a lucky shot of a problem area as the device floats by.
The most immediate technical challenge is improving the quality of the pill’s video. “We’re evaluating different cameras but we know we can’t be inferior on the imaging side,” Mr. Smith said.
Attention from the AGA is crucial because the team of engineers wants physicians to help it improve the robot pill, Mr. Luebeke said. “We can build anything, but we need guidance about what the market needs. Doctors have to say, ‘We need you to tweak it this way or that way.’ ”
The business opportunity is large, Mr. Smith said, with 7.5 million upper endoscopies out of 223 million endoscopic procedures done per year in the United States.
Endiatx figures the gross margin on procedures with the robot pills is 90%-95% because the manufacturing cost is about $50 per pill, but physicians can bill $500 for them using existing CPT codes for passive pill cameras.
Dr. Sethi said the robot pill stood out among other contenders because of the dire need for improved endoscopy technology.
Endiatx will represent AGA at the 2023 Digestive Disease Week® (DDW) Shark Tank pitch competition.
Four other finalists
The choice that received the most votes from the audience was Ezalife’s Button Huggie, a device for securing gastrostomy and cecostomy buttons. It includes a reusable, child-proof lid with a disposable, biodegradable, gauze sponge and a base layer held in place with a long-wearing adhesive. This prevents button movement in the tract, which can delay wound healing and lead to complications. In addition, the Button Huggie is much easier to put in place. “Our device is novel, with no direct competitors,” said CTO/COO Tyler Mironuck.
Currently patients are advised to fasten gastrostomy and cecostomy buttons with tape, but the buttons are dislodged 7% of the time, he said. The company estimates that patients spend an average of $100 a month on tape and gauze. The Button Huggie can be manufactured for $56, and the company envisions selling them for $300.
The device is exempt from needing a 510K FDA approval, so it can get to the market quickly. Nevertheless, the company is conducting a clinical trial with 200 patients at five children’s hospitals, Mr. Mironuck said.
NovaScan was a finalist for nsCanary, a device that uses electrical impedance to detect cancer. The device hinges on the company’s discovery that the Cole relaxation frequency is orders of magnitude different for cancerous and benign tissue, yet not affected by mass. By measuring this frequency, the nsCanary can find cancer in tissue acquired through biopsy forceps, snare polypectomy, mucosal resection, and endoscopic ultrasound-guided fine needle biopsy. It works in seconds without the need to interpret images.
Atlas Endoscopy was recognized for REN, a robotic colonoscopy system. The operator uses an external actuating magnet above the patient to guide a disposable ultracompliant endoscope through the colon. The company says this form of navigation prevents looping, reduces pain, and minimizes tissue stress.
Limaca Medical was recognized for Precision, a motorized, automated, rotational cutting and coring needle for endoscopic ultrasound biopsy. Manual biopsy needles now on the market require repeat passes in and out of the endoscope to obtain fragments of tissue, but Precision obtains larger intact samples of tumor tissue in a single pass.
Dr. Sethi has served as a consultant for Boston Scientific, Medtronic and Olympus; as a board member for EndoSound and has received grant support from FUJIFILM.
SAN FRANCISCO – No one yet has figured out how to shrink doctors so they can make house calls inside the human blood stream as they did in the science fiction movie “Fantastic Voyage.” But the founders of a gastroenterology startup think they have the next best thing – a remote-controlled robot so small it can be swallowed like a pill.
The concept captured the imagination of a panel of judges earlier this month at the 2023 American Gastroenterological Association Tech Summit where it was named the winner of the annual Shark Tank innovation competition. The AGA Tech Summit and Shark Tank are the flagship events of the AGA Center for GI Innovation and Technology.
“This could be a game-changing investment down the line,” one of the judges, Amrita Sethi, MD, from Columbia University Medical Center in New York, said in an interview.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Hawyard, Calif.–based Endiatx is early in its voyage. , but CEO Torrey Smith, an aerospace engineer, sees future generations of the device operating on any diseased tissues that can be treated with surgery. “We believe teeny robots can go anywhere in the body,” he said.
The company executives envision that one day, robots small enough to enter the human brain will be able to eat away at tumors. “Imagine having your brain surgery while you’re on a ride at Disneyland,” said Endiatx cofounder and chair Alex Luebke. If that sounds fanciful, Mr. Smith cites a case report of a botfly larva that wormed its way into a human skull and ate a golf-ball sized chunk of brain.
Endiatx has raised $3 million and sent 24 of its robots swimming into the stomachs of its founding team. Mr. Smith himself has swallowed 15. Operators can use an external device with a joystick. Engineers have experimented with an Xbox video game controller to navigate around the stomach. The procedure requires no anesthesia.
The company expects to apply for Food and Drug Administration approval in 2025 or 2026. Mr. Smith is hoping the agency will approve it quickly because the robot pills are similar enough to passive camera pills that have been on the market for years.
But he also sees it as a crucial step forward because controlling the robot with three electric motors squirting water in six directions will allow physicians to point it at what they really need to see, not just hope to get a lucky shot of a problem area as the device floats by.
The most immediate technical challenge is improving the quality of the pill’s video. “We’re evaluating different cameras but we know we can’t be inferior on the imaging side,” Mr. Smith said.
Attention from the AGA is crucial because the team of engineers wants physicians to help it improve the robot pill, Mr. Luebeke said. “We can build anything, but we need guidance about what the market needs. Doctors have to say, ‘We need you to tweak it this way or that way.’ ”
The business opportunity is large, Mr. Smith said, with 7.5 million upper endoscopies out of 223 million endoscopic procedures done per year in the United States.
Endiatx figures the gross margin on procedures with the robot pills is 90%-95% because the manufacturing cost is about $50 per pill, but physicians can bill $500 for them using existing CPT codes for passive pill cameras.
Dr. Sethi said the robot pill stood out among other contenders because of the dire need for improved endoscopy technology.
Endiatx will represent AGA at the 2023 Digestive Disease Week® (DDW) Shark Tank pitch competition.
Four other finalists
The choice that received the most votes from the audience was Ezalife’s Button Huggie, a device for securing gastrostomy and cecostomy buttons. It includes a reusable, child-proof lid with a disposable, biodegradable, gauze sponge and a base layer held in place with a long-wearing adhesive. This prevents button movement in the tract, which can delay wound healing and lead to complications. In addition, the Button Huggie is much easier to put in place. “Our device is novel, with no direct competitors,” said CTO/COO Tyler Mironuck.
Currently patients are advised to fasten gastrostomy and cecostomy buttons with tape, but the buttons are dislodged 7% of the time, he said. The company estimates that patients spend an average of $100 a month on tape and gauze. The Button Huggie can be manufactured for $56, and the company envisions selling them for $300.
The device is exempt from needing a 510K FDA approval, so it can get to the market quickly. Nevertheless, the company is conducting a clinical trial with 200 patients at five children’s hospitals, Mr. Mironuck said.
NovaScan was a finalist for nsCanary, a device that uses electrical impedance to detect cancer. The device hinges on the company’s discovery that the Cole relaxation frequency is orders of magnitude different for cancerous and benign tissue, yet not affected by mass. By measuring this frequency, the nsCanary can find cancer in tissue acquired through biopsy forceps, snare polypectomy, mucosal resection, and endoscopic ultrasound-guided fine needle biopsy. It works in seconds without the need to interpret images.
Atlas Endoscopy was recognized for REN, a robotic colonoscopy system. The operator uses an external actuating magnet above the patient to guide a disposable ultracompliant endoscope through the colon. The company says this form of navigation prevents looping, reduces pain, and minimizes tissue stress.
Limaca Medical was recognized for Precision, a motorized, automated, rotational cutting and coring needle for endoscopic ultrasound biopsy. Manual biopsy needles now on the market require repeat passes in and out of the endoscope to obtain fragments of tissue, but Precision obtains larger intact samples of tumor tissue in a single pass.
Dr. Sethi has served as a consultant for Boston Scientific, Medtronic and Olympus; as a board member for EndoSound and has received grant support from FUJIFILM.
AT THE 2023 AGA TECH SUMMIT
Financial navigators saved about $2,500 per cancer patient
Cancer patients in the United States face complex financial issues in navigating with medical insurance companies to cover their care. This “financial toxicity” has come to be regarded as a side effect of cancer treatment.
Patients with hematologic malignancies may be particularly vulnerable to financial toxicity, owing to the nature of their treatment, which often includes bone marrow transplantation, lengthy hospital stays, and prolonged intensive follow-up, as well as potential treatment-related complications, such as graft vs. host disease.
The results from this small study suggest that using an oncology financial navigator could be helpful. But not all cancer patients have access to such a person, explained lead author Jean S. Edward, PhD, RN, associate professor in the college of nursing at the University of Kentucky, Lexington.
“Unfortunately, it’s not as common as we would like, especially in underserved areas with patient and caregiver populations that need it the most,” she said. Dr. Edward is hopeful that the results from this study, even though it is small, might help to boost use of this intervention. “OFN [oncology financial navigation] is not necessarily a cutting-edge program or ‘novel’ intervention, but the lack of programs and limitations in implementing in cancer centers does make it a gap in practice,” Dr. Edward told this news organization.
“There are gaps in evidence on how to incorporate an oncology financial navigator in current workflows and sustainability of positions, but as our study has shown, the return on investment to the health care system and/or financial benefits to patients/caregivers could help cover the cost of implementing such programs,” she said.
The study was published in JCO Oncology Practice.
The intervention used in this study, Coverage and Cost-of-Care Links (CC Links), was designed specifically to address financial toxicity among patients with hematologic cancers.
The study’s primary outcomes were defined as improvements in financial distress as well as in physical and mental quality of life.
A total of 54 patients and 32 caregivers completed the intervention and pre-/postintervention surveys. More than half of participants were women. The average age was 63 years. Less than a quarter of the patients were employed (23%), about one-third had income that was below the federal poverty level, and almost all had insurance. About 59% of the caregivers were employed.
The navigators’ functions included screening for financial toxicity using FACIT-Comprehensive Score for Financial Toxicity (COST) and the National Comprehensive Cancer Network’s Distress Thermometer and Problem List. They also helped patients to estimate cost of care, assessed health insurance coverage, and connected patients/caregivers with disease-specific resources and other external assistance programs, among other things.
Participants had an average of three in-person meetings and five telephone interactions with the financial navigator. The most common concern was in regard to high out-of-pocket costs. The most frequently provided services from the navigator were helping with financial assistance programs and grant applications. Overall, the navigator was able to obtain $124,600 in financial benefits for 48 participants, as well as money for travel ($24,000), urgent needs ($16,000), patient financial assistance ($9,100), and copay assistance grants ($75,500).
With regard to scores on the screening tools, the only significant change from pre- to postintervention was in the psychological response score, or COST. It decreased by an average of 2.30 points (P = .019; Hedges’ g = 0.33). For caregivers, there was a significant improvement in COST (average decrease, 2.97 points; P = .021; g = 0.43), material condition scores (average decrease, 0.63 points; P = .031; g = 0.39), and total financial toxicity scores (average decrease, 0.13 points; P = .041; g = 0.37).
Most of the participants gave the intervention high ratings for acceptability (89%) and appropriateness (88%).
“Standardized screening for financial toxicity in cancer care settings is essential to support early identification of financial needs that serve as barriers to care,” the authors conclude. “Close collaboration and coordination with existing services and workflows are essential for the seamless integration of OFN interventions within health systems and to help facilitate contact and communication with participants.”
The study was supported by the National Cancer Institute; the University of Kentucky’s Markey Cancer Center; the Research Communications Office of the Patient Oriented and Population Science Shared Resource Facilities; Joan Scales, LCSW, and the Psych-Oncology Program at the University of Kentucky Markey Cancer Center; and UK HealthCare’s Patient Financial Services. Dr. Edward has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer patients in the United States face complex financial issues in navigating with medical insurance companies to cover their care. This “financial toxicity” has come to be regarded as a side effect of cancer treatment.
Patients with hematologic malignancies may be particularly vulnerable to financial toxicity, owing to the nature of their treatment, which often includes bone marrow transplantation, lengthy hospital stays, and prolonged intensive follow-up, as well as potential treatment-related complications, such as graft vs. host disease.
The results from this small study suggest that using an oncology financial navigator could be helpful. But not all cancer patients have access to such a person, explained lead author Jean S. Edward, PhD, RN, associate professor in the college of nursing at the University of Kentucky, Lexington.
“Unfortunately, it’s not as common as we would like, especially in underserved areas with patient and caregiver populations that need it the most,” she said. Dr. Edward is hopeful that the results from this study, even though it is small, might help to boost use of this intervention. “OFN [oncology financial navigation] is not necessarily a cutting-edge program or ‘novel’ intervention, but the lack of programs and limitations in implementing in cancer centers does make it a gap in practice,” Dr. Edward told this news organization.
“There are gaps in evidence on how to incorporate an oncology financial navigator in current workflows and sustainability of positions, but as our study has shown, the return on investment to the health care system and/or financial benefits to patients/caregivers could help cover the cost of implementing such programs,” she said.
The study was published in JCO Oncology Practice.
The intervention used in this study, Coverage and Cost-of-Care Links (CC Links), was designed specifically to address financial toxicity among patients with hematologic cancers.
The study’s primary outcomes were defined as improvements in financial distress as well as in physical and mental quality of life.
A total of 54 patients and 32 caregivers completed the intervention and pre-/postintervention surveys. More than half of participants were women. The average age was 63 years. Less than a quarter of the patients were employed (23%), about one-third had income that was below the federal poverty level, and almost all had insurance. About 59% of the caregivers were employed.
The navigators’ functions included screening for financial toxicity using FACIT-Comprehensive Score for Financial Toxicity (COST) and the National Comprehensive Cancer Network’s Distress Thermometer and Problem List. They also helped patients to estimate cost of care, assessed health insurance coverage, and connected patients/caregivers with disease-specific resources and other external assistance programs, among other things.
Participants had an average of three in-person meetings and five telephone interactions with the financial navigator. The most common concern was in regard to high out-of-pocket costs. The most frequently provided services from the navigator were helping with financial assistance programs and grant applications. Overall, the navigator was able to obtain $124,600 in financial benefits for 48 participants, as well as money for travel ($24,000), urgent needs ($16,000), patient financial assistance ($9,100), and copay assistance grants ($75,500).
With regard to scores on the screening tools, the only significant change from pre- to postintervention was in the psychological response score, or COST. It decreased by an average of 2.30 points (P = .019; Hedges’ g = 0.33). For caregivers, there was a significant improvement in COST (average decrease, 2.97 points; P = .021; g = 0.43), material condition scores (average decrease, 0.63 points; P = .031; g = 0.39), and total financial toxicity scores (average decrease, 0.13 points; P = .041; g = 0.37).
Most of the participants gave the intervention high ratings for acceptability (89%) and appropriateness (88%).
“Standardized screening for financial toxicity in cancer care settings is essential to support early identification of financial needs that serve as barriers to care,” the authors conclude. “Close collaboration and coordination with existing services and workflows are essential for the seamless integration of OFN interventions within health systems and to help facilitate contact and communication with participants.”
The study was supported by the National Cancer Institute; the University of Kentucky’s Markey Cancer Center; the Research Communications Office of the Patient Oriented and Population Science Shared Resource Facilities; Joan Scales, LCSW, and the Psych-Oncology Program at the University of Kentucky Markey Cancer Center; and UK HealthCare’s Patient Financial Services. Dr. Edward has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer patients in the United States face complex financial issues in navigating with medical insurance companies to cover their care. This “financial toxicity” has come to be regarded as a side effect of cancer treatment.
Patients with hematologic malignancies may be particularly vulnerable to financial toxicity, owing to the nature of their treatment, which often includes bone marrow transplantation, lengthy hospital stays, and prolonged intensive follow-up, as well as potential treatment-related complications, such as graft vs. host disease.
The results from this small study suggest that using an oncology financial navigator could be helpful. But not all cancer patients have access to such a person, explained lead author Jean S. Edward, PhD, RN, associate professor in the college of nursing at the University of Kentucky, Lexington.
“Unfortunately, it’s not as common as we would like, especially in underserved areas with patient and caregiver populations that need it the most,” she said. Dr. Edward is hopeful that the results from this study, even though it is small, might help to boost use of this intervention. “OFN [oncology financial navigation] is not necessarily a cutting-edge program or ‘novel’ intervention, but the lack of programs and limitations in implementing in cancer centers does make it a gap in practice,” Dr. Edward told this news organization.
“There are gaps in evidence on how to incorporate an oncology financial navigator in current workflows and sustainability of positions, but as our study has shown, the return on investment to the health care system and/or financial benefits to patients/caregivers could help cover the cost of implementing such programs,” she said.
The study was published in JCO Oncology Practice.
The intervention used in this study, Coverage and Cost-of-Care Links (CC Links), was designed specifically to address financial toxicity among patients with hematologic cancers.
The study’s primary outcomes were defined as improvements in financial distress as well as in physical and mental quality of life.
A total of 54 patients and 32 caregivers completed the intervention and pre-/postintervention surveys. More than half of participants were women. The average age was 63 years. Less than a quarter of the patients were employed (23%), about one-third had income that was below the federal poverty level, and almost all had insurance. About 59% of the caregivers were employed.
The navigators’ functions included screening for financial toxicity using FACIT-Comprehensive Score for Financial Toxicity (COST) and the National Comprehensive Cancer Network’s Distress Thermometer and Problem List. They also helped patients to estimate cost of care, assessed health insurance coverage, and connected patients/caregivers with disease-specific resources and other external assistance programs, among other things.
Participants had an average of three in-person meetings and five telephone interactions with the financial navigator. The most common concern was in regard to high out-of-pocket costs. The most frequently provided services from the navigator were helping with financial assistance programs and grant applications. Overall, the navigator was able to obtain $124,600 in financial benefits for 48 participants, as well as money for travel ($24,000), urgent needs ($16,000), patient financial assistance ($9,100), and copay assistance grants ($75,500).
With regard to scores on the screening tools, the only significant change from pre- to postintervention was in the psychological response score, or COST. It decreased by an average of 2.30 points (P = .019; Hedges’ g = 0.33). For caregivers, there was a significant improvement in COST (average decrease, 2.97 points; P = .021; g = 0.43), material condition scores (average decrease, 0.63 points; P = .031; g = 0.39), and total financial toxicity scores (average decrease, 0.13 points; P = .041; g = 0.37).
Most of the participants gave the intervention high ratings for acceptability (89%) and appropriateness (88%).
“Standardized screening for financial toxicity in cancer care settings is essential to support early identification of financial needs that serve as barriers to care,” the authors conclude. “Close collaboration and coordination with existing services and workflows are essential for the seamless integration of OFN interventions within health systems and to help facilitate contact and communication with participants.”
The study was supported by the National Cancer Institute; the University of Kentucky’s Markey Cancer Center; the Research Communications Office of the Patient Oriented and Population Science Shared Resource Facilities; Joan Scales, LCSW, and the Psych-Oncology Program at the University of Kentucky Markey Cancer Center; and UK HealthCare’s Patient Financial Services. Dr. Edward has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JCO ONCOLOGY PRACTICE
Home-based HPV cervical cancer screening ‘cost effective’
For women who are overdue for cervical cancer screening, mailing self-sampling kits for high-risk human papillomavirus (HPV) is a cost-effective means of increasing screening uptake, reveals an analysis of a large U.S. trial.
The finding comes from a randomized trial in almost 20,000 women, which compared women who received a mailed HPV testing kit with those who did not. The results show that mailing was most cost-effective in women aged 50-64 years and in those who were only recently overdue for cervical screening.
The study was published by JAMA Network Open.
“These results support mailing HPV kits as an efficient outreach strategy for increasing screening rates in U.S. health care systems,” say the authors, led by Rachel L. Winer, PhD, MPH, department of epidemiology, University of Washington, Seattle.
They note that their results are consistent with those from previous studies in other health care contexts, but their analysis “benefited from the randomized clinical trial design and a large sample size,” they write.
However, they point out that the trial was conducted “before the beginning of the COVID-19 pandemic,” and it is “well established” that cancer screening rates “decreased substantially during the pandemic.”
They suggest that mailed HPV self-sampling kits could nevertheless be a “means of overcoming screening barriers among underscreened women,” which may have been exacerbated by the “societal consequences of the pandemic.”
Reducing barriers to screening
Cervical screening is associated with “substantial global reductions” in the incidence and mortality of cervical cancer, the authors point out. Because most cases of the disease are consequently preventable, it now occurs “predominantly in individuals who have never or rarely received screening.”
Home-based HPV-only testing reduces the need for office visits and reduces barriers to screening, such as discomfort, embarrassment, and difficulties with scheduling or attending appointments.
Previous studies have shown that the direct mailing of home-based HPV self-collection kits is associated with increased uptake of screening among underscreened women and is cost-effective, although the researchers point out that these previous studies were conducted in countries with “organized national screening programs.”
For their own study, they focused on home-based HPV screening among underscreened individuals in the United States. The team examined data from the Home-based Options to Make cervical cancer screening Easy trial, which has previously showed that mailing kits to women increased screening uptake, compared with usual care alone.
For the current analysis, they conducted an economic evaluation of data on 19,851 trial participants, who were randomized to receive home-based screening or usual care between February 2014 and August 2016 and were followed up to February 2018.
All of the women were aged 30-64 years and had been enrolled in a health plan from Kaiser Permanente Washington (KPW) for at least 3 years and 5 months. They were also required not have undergone a hysterectomy.
Participant-level economic data were collected between June 2019 and March 2021, with intervention delivery costs calculated from the perspective of both the KPW and Medicare health systems and based on the cost of either a wellness visit or Papanicolaou (Pap) test–only visit.
The mean age of the participants was 50.1 years, and the majority (76.7%) were White; 9.7% were Asian and 4.7% were Black or African American.
There were no significant differences in baseline characteristics between the group assigned to usual care, which comprised patient reminders and ad hoc screening outreach, and those in the intervention group, who received usual care and a mailed HPV self-sampling kit.
The researchers report that 1,206 women in the intervention group sent back a mailed HPV kit, with 1,178 (97.7%) meeting the criteria for completed screening uptake.
Overall, screening uptake was higher in the intervention group than in control participants, at 26.3% vs. 17.4%, respectively (relative risk, 1.51).
Intervention participants were also more likely than controls to have a positive test result (relative risk, 1.49) and to receive treatment (relative risk, 1.70).
The incremental cost-effectiveness ratio for increased screening uptake, defined as the incremental difference in cost between the study groups divided by the difference in the number of participants completing screening within 6 months, ranged from $85.84 per additional completed screening to $146.29, depending on the health system and test considered.
In terms of willingness-to-pay (WTP) thresholds for each additional completed screening, the team found that home-based screening achieved a 90% probability of cost-effectiveness, at a WTP of just $148 if the participant’s last Pap test was between 3.4 and 5.0 years before randomization.
A 90% probability of cost-effectiveness was also achieved at a WTP of $198 among participants aged 50-64 years, a threshold that was lower than that among other age groups.
At a WTP threshold of over $350, the intervention was considered to have 100% probability of being cost-effective in all age groups.
The study was supported by a grant from the National Cancer Institute of the National Institutes of Health. Dr. Winer reports a relationship with the National Cancer Institute outside of the submitted work, as do several other authors.
A version of this article first appeared on Medscape.com.
For women who are overdue for cervical cancer screening, mailing self-sampling kits for high-risk human papillomavirus (HPV) is a cost-effective means of increasing screening uptake, reveals an analysis of a large U.S. trial.
The finding comes from a randomized trial in almost 20,000 women, which compared women who received a mailed HPV testing kit with those who did not. The results show that mailing was most cost-effective in women aged 50-64 years and in those who were only recently overdue for cervical screening.
The study was published by JAMA Network Open.
“These results support mailing HPV kits as an efficient outreach strategy for increasing screening rates in U.S. health care systems,” say the authors, led by Rachel L. Winer, PhD, MPH, department of epidemiology, University of Washington, Seattle.
They note that their results are consistent with those from previous studies in other health care contexts, but their analysis “benefited from the randomized clinical trial design and a large sample size,” they write.
However, they point out that the trial was conducted “before the beginning of the COVID-19 pandemic,” and it is “well established” that cancer screening rates “decreased substantially during the pandemic.”
They suggest that mailed HPV self-sampling kits could nevertheless be a “means of overcoming screening barriers among underscreened women,” which may have been exacerbated by the “societal consequences of the pandemic.”
Reducing barriers to screening
Cervical screening is associated with “substantial global reductions” in the incidence and mortality of cervical cancer, the authors point out. Because most cases of the disease are consequently preventable, it now occurs “predominantly in individuals who have never or rarely received screening.”
Home-based HPV-only testing reduces the need for office visits and reduces barriers to screening, such as discomfort, embarrassment, and difficulties with scheduling or attending appointments.
Previous studies have shown that the direct mailing of home-based HPV self-collection kits is associated with increased uptake of screening among underscreened women and is cost-effective, although the researchers point out that these previous studies were conducted in countries with “organized national screening programs.”
For their own study, they focused on home-based HPV screening among underscreened individuals in the United States. The team examined data from the Home-based Options to Make cervical cancer screening Easy trial, which has previously showed that mailing kits to women increased screening uptake, compared with usual care alone.
For the current analysis, they conducted an economic evaluation of data on 19,851 trial participants, who were randomized to receive home-based screening or usual care between February 2014 and August 2016 and were followed up to February 2018.
All of the women were aged 30-64 years and had been enrolled in a health plan from Kaiser Permanente Washington (KPW) for at least 3 years and 5 months. They were also required not have undergone a hysterectomy.
Participant-level economic data were collected between June 2019 and March 2021, with intervention delivery costs calculated from the perspective of both the KPW and Medicare health systems and based on the cost of either a wellness visit or Papanicolaou (Pap) test–only visit.
The mean age of the participants was 50.1 years, and the majority (76.7%) were White; 9.7% were Asian and 4.7% were Black or African American.
There were no significant differences in baseline characteristics between the group assigned to usual care, which comprised patient reminders and ad hoc screening outreach, and those in the intervention group, who received usual care and a mailed HPV self-sampling kit.
The researchers report that 1,206 women in the intervention group sent back a mailed HPV kit, with 1,178 (97.7%) meeting the criteria for completed screening uptake.
Overall, screening uptake was higher in the intervention group than in control participants, at 26.3% vs. 17.4%, respectively (relative risk, 1.51).
Intervention participants were also more likely than controls to have a positive test result (relative risk, 1.49) and to receive treatment (relative risk, 1.70).
The incremental cost-effectiveness ratio for increased screening uptake, defined as the incremental difference in cost between the study groups divided by the difference in the number of participants completing screening within 6 months, ranged from $85.84 per additional completed screening to $146.29, depending on the health system and test considered.
In terms of willingness-to-pay (WTP) thresholds for each additional completed screening, the team found that home-based screening achieved a 90% probability of cost-effectiveness, at a WTP of just $148 if the participant’s last Pap test was between 3.4 and 5.0 years before randomization.
A 90% probability of cost-effectiveness was also achieved at a WTP of $198 among participants aged 50-64 years, a threshold that was lower than that among other age groups.
At a WTP threshold of over $350, the intervention was considered to have 100% probability of being cost-effective in all age groups.
The study was supported by a grant from the National Cancer Institute of the National Institutes of Health. Dr. Winer reports a relationship with the National Cancer Institute outside of the submitted work, as do several other authors.
A version of this article first appeared on Medscape.com.
For women who are overdue for cervical cancer screening, mailing self-sampling kits for high-risk human papillomavirus (HPV) is a cost-effective means of increasing screening uptake, reveals an analysis of a large U.S. trial.
The finding comes from a randomized trial in almost 20,000 women, which compared women who received a mailed HPV testing kit with those who did not. The results show that mailing was most cost-effective in women aged 50-64 years and in those who were only recently overdue for cervical screening.
The study was published by JAMA Network Open.
“These results support mailing HPV kits as an efficient outreach strategy for increasing screening rates in U.S. health care systems,” say the authors, led by Rachel L. Winer, PhD, MPH, department of epidemiology, University of Washington, Seattle.
They note that their results are consistent with those from previous studies in other health care contexts, but their analysis “benefited from the randomized clinical trial design and a large sample size,” they write.
However, they point out that the trial was conducted “before the beginning of the COVID-19 pandemic,” and it is “well established” that cancer screening rates “decreased substantially during the pandemic.”
They suggest that mailed HPV self-sampling kits could nevertheless be a “means of overcoming screening barriers among underscreened women,” which may have been exacerbated by the “societal consequences of the pandemic.”
Reducing barriers to screening
Cervical screening is associated with “substantial global reductions” in the incidence and mortality of cervical cancer, the authors point out. Because most cases of the disease are consequently preventable, it now occurs “predominantly in individuals who have never or rarely received screening.”
Home-based HPV-only testing reduces the need for office visits and reduces barriers to screening, such as discomfort, embarrassment, and difficulties with scheduling or attending appointments.
Previous studies have shown that the direct mailing of home-based HPV self-collection kits is associated with increased uptake of screening among underscreened women and is cost-effective, although the researchers point out that these previous studies were conducted in countries with “organized national screening programs.”
For their own study, they focused on home-based HPV screening among underscreened individuals in the United States. The team examined data from the Home-based Options to Make cervical cancer screening Easy trial, which has previously showed that mailing kits to women increased screening uptake, compared with usual care alone.
For the current analysis, they conducted an economic evaluation of data on 19,851 trial participants, who were randomized to receive home-based screening or usual care between February 2014 and August 2016 and were followed up to February 2018.
All of the women were aged 30-64 years and had been enrolled in a health plan from Kaiser Permanente Washington (KPW) for at least 3 years and 5 months. They were also required not have undergone a hysterectomy.
Participant-level economic data were collected between June 2019 and March 2021, with intervention delivery costs calculated from the perspective of both the KPW and Medicare health systems and based on the cost of either a wellness visit or Papanicolaou (Pap) test–only visit.
The mean age of the participants was 50.1 years, and the majority (76.7%) were White; 9.7% were Asian and 4.7% were Black or African American.
There were no significant differences in baseline characteristics between the group assigned to usual care, which comprised patient reminders and ad hoc screening outreach, and those in the intervention group, who received usual care and a mailed HPV self-sampling kit.
The researchers report that 1,206 women in the intervention group sent back a mailed HPV kit, with 1,178 (97.7%) meeting the criteria for completed screening uptake.
Overall, screening uptake was higher in the intervention group than in control participants, at 26.3% vs. 17.4%, respectively (relative risk, 1.51).
Intervention participants were also more likely than controls to have a positive test result (relative risk, 1.49) and to receive treatment (relative risk, 1.70).
The incremental cost-effectiveness ratio for increased screening uptake, defined as the incremental difference in cost between the study groups divided by the difference in the number of participants completing screening within 6 months, ranged from $85.84 per additional completed screening to $146.29, depending on the health system and test considered.
In terms of willingness-to-pay (WTP) thresholds for each additional completed screening, the team found that home-based screening achieved a 90% probability of cost-effectiveness, at a WTP of just $148 if the participant’s last Pap test was between 3.4 and 5.0 years before randomization.
A 90% probability of cost-effectiveness was also achieved at a WTP of $198 among participants aged 50-64 years, a threshold that was lower than that among other age groups.
At a WTP threshold of over $350, the intervention was considered to have 100% probability of being cost-effective in all age groups.
The study was supported by a grant from the National Cancer Institute of the National Institutes of Health. Dr. Winer reports a relationship with the National Cancer Institute outside of the submitted work, as do several other authors.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Headache before the revolution: A clinician looks back
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Possible C. difficile–colon cancer connection: Study
C. diff. is a bacterium that infects the large intestine, causing difficult GI symptoms like frequent diarrhea. C. diff. is a widespread infection among patients who have been hospitalized, estimated at almost a half-million cases per year. It’s extremely contagious.
C. diff. has been known to lead to dangerous problems like sepsis if left untreated. Previous research has found there is a higher amount of C. diff. in cancerous lesions than in healthy body tissue, but a recent study published in Cancer Discovery by Johns Hopkins and Vanderbilt University has expanded upon the link between C. diff. and colon cancer. This study, which was conducted in mice, found that C. diff. bacteria may change normal cells to cancer cells.
In colon cancer, the surface of the colon tends to be covered in biofilms – or dense amounts of bacteria. In this study, researchers found that C. diff. was capable of producing colorectal tumors in a cascade.
“Big picture, we’re working to learn what the exact mechanism for this is,” said Julia L. Drewes, PhD, assistant professor of medicine at Johns Hopkins University, Baltimore, and a coauthor of the study.
Anyone can get C. diff., but certain people are more susceptible.
“People who are over 65, have weakened immune systems, live in nursing homes, or work in health care settings are most at risk for C. diff.,” said Lilian Chen, MD, a colon and rectal surgeon at Tufts Medical Centerand assistant professor of surgery at Tufts University, both in Boston. “People with C. diff. can also get it again. One in six patients will end up with recurrent infections.”
Another risk factor: taking antibiotics. “Trillions of microbes are normally found in and on our body, including both good and bad bacteria,” said Caroline Um, PhD, MPH, principal scientist in epidemiology research for the American Cancer Society. “Normally, good bacteria help us fight against bad bacteria such as C. diff. However, you may have a greater chance of C. diff. infection after taking antibiotics, since they usually wipe out both good and bad bacteria in our gut.”
C. diff. is transmitted through stool, often if someone doesn’t wash their hands after using the bathroom. If you touch that person’s skin or a surface that person touched, your body can be “colonized” with the bacteria.
“Once someone is colonized with C. diff., you find it everywhere in their environment. In fact, C. diff. is all around all of us,” said Aasma Shaukat, MD, MPH, a gastroenterologist at the NYU Langone Medical Center and director of GI outcomes research at New York University. “In a healthy person, this kind of exposure doesn’t matter because C. diff. will not make them sick. It’s when someone has a compromised immune system that C. diff. becomes a concern.”
C. diff. may kickstart the process of how cancer begins to form through inflammation
“There are two types of toxins present in C. diff.: toxin A and toxin B,” said Dr. Drewes. “We need to do more work in order to determine an exact mechanism, but toxin B, or TcdB, which is found in a majority of C. diff. infections, appears to drive inflammation in the body. This inflammation contributes to cell damage in the colon, which may then be connected to a mutation that can cause cancer.”
The findings could help researchers understand why so many people under the age of 50 are now being diagnosed with colon cancer.
“We need a better understanding of the potential role of C. diff. in colorectal cancer before we can determine whether this changes current colorectal cancer screening guidelines,” said Dr. Um. “However, it’s a good idea to talk with your health care professional about colorectal cancer screening, regardless of whether you have had C. diff.. Various factors like smoking, poor diet, being overweight, or having a family history of colorectal cancer can affect an individual’s risk.”
A version of this article first appeared on WebMD.com.
C. diff. is a bacterium that infects the large intestine, causing difficult GI symptoms like frequent diarrhea. C. diff. is a widespread infection among patients who have been hospitalized, estimated at almost a half-million cases per year. It’s extremely contagious.
C. diff. has been known to lead to dangerous problems like sepsis if left untreated. Previous research has found there is a higher amount of C. diff. in cancerous lesions than in healthy body tissue, but a recent study published in Cancer Discovery by Johns Hopkins and Vanderbilt University has expanded upon the link between C. diff. and colon cancer. This study, which was conducted in mice, found that C. diff. bacteria may change normal cells to cancer cells.
In colon cancer, the surface of the colon tends to be covered in biofilms – or dense amounts of bacteria. In this study, researchers found that C. diff. was capable of producing colorectal tumors in a cascade.
“Big picture, we’re working to learn what the exact mechanism for this is,” said Julia L. Drewes, PhD, assistant professor of medicine at Johns Hopkins University, Baltimore, and a coauthor of the study.
Anyone can get C. diff., but certain people are more susceptible.
“People who are over 65, have weakened immune systems, live in nursing homes, or work in health care settings are most at risk for C. diff.,” said Lilian Chen, MD, a colon and rectal surgeon at Tufts Medical Centerand assistant professor of surgery at Tufts University, both in Boston. “People with C. diff. can also get it again. One in six patients will end up with recurrent infections.”
Another risk factor: taking antibiotics. “Trillions of microbes are normally found in and on our body, including both good and bad bacteria,” said Caroline Um, PhD, MPH, principal scientist in epidemiology research for the American Cancer Society. “Normally, good bacteria help us fight against bad bacteria such as C. diff. However, you may have a greater chance of C. diff. infection after taking antibiotics, since they usually wipe out both good and bad bacteria in our gut.”
C. diff. is transmitted through stool, often if someone doesn’t wash their hands after using the bathroom. If you touch that person’s skin or a surface that person touched, your body can be “colonized” with the bacteria.
“Once someone is colonized with C. diff., you find it everywhere in their environment. In fact, C. diff. is all around all of us,” said Aasma Shaukat, MD, MPH, a gastroenterologist at the NYU Langone Medical Center and director of GI outcomes research at New York University. “In a healthy person, this kind of exposure doesn’t matter because C. diff. will not make them sick. It’s when someone has a compromised immune system that C. diff. becomes a concern.”
C. diff. may kickstart the process of how cancer begins to form through inflammation
“There are two types of toxins present in C. diff.: toxin A and toxin B,” said Dr. Drewes. “We need to do more work in order to determine an exact mechanism, but toxin B, or TcdB, which is found in a majority of C. diff. infections, appears to drive inflammation in the body. This inflammation contributes to cell damage in the colon, which may then be connected to a mutation that can cause cancer.”
The findings could help researchers understand why so many people under the age of 50 are now being diagnosed with colon cancer.
“We need a better understanding of the potential role of C. diff. in colorectal cancer before we can determine whether this changes current colorectal cancer screening guidelines,” said Dr. Um. “However, it’s a good idea to talk with your health care professional about colorectal cancer screening, regardless of whether you have had C. diff.. Various factors like smoking, poor diet, being overweight, or having a family history of colorectal cancer can affect an individual’s risk.”
A version of this article first appeared on WebMD.com.
C. diff. is a bacterium that infects the large intestine, causing difficult GI symptoms like frequent diarrhea. C. diff. is a widespread infection among patients who have been hospitalized, estimated at almost a half-million cases per year. It’s extremely contagious.
C. diff. has been known to lead to dangerous problems like sepsis if left untreated. Previous research has found there is a higher amount of C. diff. in cancerous lesions than in healthy body tissue, but a recent study published in Cancer Discovery by Johns Hopkins and Vanderbilt University has expanded upon the link between C. diff. and colon cancer. This study, which was conducted in mice, found that C. diff. bacteria may change normal cells to cancer cells.
In colon cancer, the surface of the colon tends to be covered in biofilms – or dense amounts of bacteria. In this study, researchers found that C. diff. was capable of producing colorectal tumors in a cascade.
“Big picture, we’re working to learn what the exact mechanism for this is,” said Julia L. Drewes, PhD, assistant professor of medicine at Johns Hopkins University, Baltimore, and a coauthor of the study.
Anyone can get C. diff., but certain people are more susceptible.
“People who are over 65, have weakened immune systems, live in nursing homes, or work in health care settings are most at risk for C. diff.,” said Lilian Chen, MD, a colon and rectal surgeon at Tufts Medical Centerand assistant professor of surgery at Tufts University, both in Boston. “People with C. diff. can also get it again. One in six patients will end up with recurrent infections.”
Another risk factor: taking antibiotics. “Trillions of microbes are normally found in and on our body, including both good and bad bacteria,” said Caroline Um, PhD, MPH, principal scientist in epidemiology research for the American Cancer Society. “Normally, good bacteria help us fight against bad bacteria such as C. diff. However, you may have a greater chance of C. diff. infection after taking antibiotics, since they usually wipe out both good and bad bacteria in our gut.”
C. diff. is transmitted through stool, often if someone doesn’t wash their hands after using the bathroom. If you touch that person’s skin or a surface that person touched, your body can be “colonized” with the bacteria.
“Once someone is colonized with C. diff., you find it everywhere in their environment. In fact, C. diff. is all around all of us,” said Aasma Shaukat, MD, MPH, a gastroenterologist at the NYU Langone Medical Center and director of GI outcomes research at New York University. “In a healthy person, this kind of exposure doesn’t matter because C. diff. will not make them sick. It’s when someone has a compromised immune system that C. diff. becomes a concern.”
C. diff. may kickstart the process of how cancer begins to form through inflammation
“There are two types of toxins present in C. diff.: toxin A and toxin B,” said Dr. Drewes. “We need to do more work in order to determine an exact mechanism, but toxin B, or TcdB, which is found in a majority of C. diff. infections, appears to drive inflammation in the body. This inflammation contributes to cell damage in the colon, which may then be connected to a mutation that can cause cancer.”
The findings could help researchers understand why so many people under the age of 50 are now being diagnosed with colon cancer.
“We need a better understanding of the potential role of C. diff. in colorectal cancer before we can determine whether this changes current colorectal cancer screening guidelines,” said Dr. Um. “However, it’s a good idea to talk with your health care professional about colorectal cancer screening, regardless of whether you have had C. diff.. Various factors like smoking, poor diet, being overweight, or having a family history of colorectal cancer can affect an individual’s risk.”
A version of this article first appeared on WebMD.com.
FROM CANCER DISCOVERY
Exercise capacity and QOL linked to significant survival benefit with endobronchial valves
according to study results published in Respiratory Medicine. The benefits were independent of reduction in target lobe volume or the presence of a complete lobar atelectasis.
In patients with more severe chronic obstructive pulmonary disease (COPD), the usual treatments of smoking cessation, pharmacological therapy, pulmonary rehabilitation aiming for symptom reduction, minimizing the burden of disease, slowing disease progression, and improving exercise tolerance fall short according to Sharyn A. Roodenburg, PhD candidate in the department of pulmonary diseases, University of Groningen (the Netherlands), and colleagues.
Lung volume reduction is generally reserved for patients with COPD that has a predominantly emphysematous phenotype and severely hyperinflated lungs. While both surgical and bronchoscopic lung volume reduction (BLVR) approaches are in use, bronchoscopic approaches are less invasive and incur lower morbidity. When technically feasible, they are generally preferred over open surgery.
BLVR using endobronchial valves (EBV), the most effective and commonly employed technique, has been shown in randomized controlled trials to improve pulmonary function, exercise capacity, and health-related quality of life.
Noting a survival benefit in prior studies among patients with complete lobar atelectasis following treatment, the authors wrote that their own clinical experience has been that significant treatment responses (pulmonary function and/or exercise capacity) observed in patients with a partial lobar atelectasis may also be associated with a survival benefit. Their aim was to evaluate whether pulmonary function, radiological, health-related quality of life, and/or exercise capacity outcome responders to EBV treatment have a survival benefit over nonresponders.
Their analysis included data collected prospectively out of four clinical trials (CHARTIS, STELVIO, IMPACT, and LIBERATE) from June 2008 to Dec. 2020 at the University Medical Center Groningen. Predetermined potential predictors of survival included change in forced expiratory volume in 1 second (FEV1), change in residual volume (RV), change in RV/total lung capacity (RV/TLC) ratio, change in 6-minute walk distance (6MWD), change in total score on the St. George’s Respiratory Questionnaire (SGRQ), target lobe volume reduction (TLVR), and presence of complete lobar atelectasis (defined as a TLVR of 100%).
Mean age was 61.3 years among the 428 included patients (68% women). Data on both the 6MWD and SGRQ total score at baseline and 1-year follow-up were available for 252 patients. SGRQ decreased by 8.3 points or more, and 6MWD increased by 26 meters or more over baseline. Among these patients, 113 (45%) were responders on both 6MWD and SGRQ, 49 (19%) patients were responders on 6MWD only, 31 (12%) patients on SGRQ only, and 59 (23%) were nonresponders on both. Survival was significantly worse among nonresponders on 6MWD, SGRQ, or on both. 6MWD and SGRQ response were independent predictors for improved survival time (hazard ratio, 0.50; 95% confidence interval, 0.28-0.89; P = .02 and HR, 0.54; 95% confidence interval, 0.30-0.94; P = .03, respectively). Survival was not significantly affected by the presence of complete lobar atelectasis or pulmonary function improvements.
“Especially in patients with a low FEV1 (< 50% predicted), 6-minute walk distance was found to be a better predictor for mortality than pulmonary function. A possible explanation for why change in 6-minute walk distance is a better predictor for survival after EBV treatment than the change in pulmonary function and hyperinflation might be that the 6-minute walk distance not only reflects the pulmonary limitation of these patients, but also captures the extrapulmonary manifestations of COPD, such as cardiac dysfunction, musculoskeletal disorders, fatigue, and psychological symptoms, all of which can impact survival,” the authors noted
The study received no funding, and the authors did not report any disclosures.
This article was updated 3/30/23.
according to study results published in Respiratory Medicine. The benefits were independent of reduction in target lobe volume or the presence of a complete lobar atelectasis.
In patients with more severe chronic obstructive pulmonary disease (COPD), the usual treatments of smoking cessation, pharmacological therapy, pulmonary rehabilitation aiming for symptom reduction, minimizing the burden of disease, slowing disease progression, and improving exercise tolerance fall short according to Sharyn A. Roodenburg, PhD candidate in the department of pulmonary diseases, University of Groningen (the Netherlands), and colleagues.
Lung volume reduction is generally reserved for patients with COPD that has a predominantly emphysematous phenotype and severely hyperinflated lungs. While both surgical and bronchoscopic lung volume reduction (BLVR) approaches are in use, bronchoscopic approaches are less invasive and incur lower morbidity. When technically feasible, they are generally preferred over open surgery.
BLVR using endobronchial valves (EBV), the most effective and commonly employed technique, has been shown in randomized controlled trials to improve pulmonary function, exercise capacity, and health-related quality of life.
Noting a survival benefit in prior studies among patients with complete lobar atelectasis following treatment, the authors wrote that their own clinical experience has been that significant treatment responses (pulmonary function and/or exercise capacity) observed in patients with a partial lobar atelectasis may also be associated with a survival benefit. Their aim was to evaluate whether pulmonary function, radiological, health-related quality of life, and/or exercise capacity outcome responders to EBV treatment have a survival benefit over nonresponders.
Their analysis included data collected prospectively out of four clinical trials (CHARTIS, STELVIO, IMPACT, and LIBERATE) from June 2008 to Dec. 2020 at the University Medical Center Groningen. Predetermined potential predictors of survival included change in forced expiratory volume in 1 second (FEV1), change in residual volume (RV), change in RV/total lung capacity (RV/TLC) ratio, change in 6-minute walk distance (6MWD), change in total score on the St. George’s Respiratory Questionnaire (SGRQ), target lobe volume reduction (TLVR), and presence of complete lobar atelectasis (defined as a TLVR of 100%).
Mean age was 61.3 years among the 428 included patients (68% women). Data on both the 6MWD and SGRQ total score at baseline and 1-year follow-up were available for 252 patients. SGRQ decreased by 8.3 points or more, and 6MWD increased by 26 meters or more over baseline. Among these patients, 113 (45%) were responders on both 6MWD and SGRQ, 49 (19%) patients were responders on 6MWD only, 31 (12%) patients on SGRQ only, and 59 (23%) were nonresponders on both. Survival was significantly worse among nonresponders on 6MWD, SGRQ, or on both. 6MWD and SGRQ response were independent predictors for improved survival time (hazard ratio, 0.50; 95% confidence interval, 0.28-0.89; P = .02 and HR, 0.54; 95% confidence interval, 0.30-0.94; P = .03, respectively). Survival was not significantly affected by the presence of complete lobar atelectasis or pulmonary function improvements.
“Especially in patients with a low FEV1 (< 50% predicted), 6-minute walk distance was found to be a better predictor for mortality than pulmonary function. A possible explanation for why change in 6-minute walk distance is a better predictor for survival after EBV treatment than the change in pulmonary function and hyperinflation might be that the 6-minute walk distance not only reflects the pulmonary limitation of these patients, but also captures the extrapulmonary manifestations of COPD, such as cardiac dysfunction, musculoskeletal disorders, fatigue, and psychological symptoms, all of which can impact survival,” the authors noted
The study received no funding, and the authors did not report any disclosures.
This article was updated 3/30/23.
according to study results published in Respiratory Medicine. The benefits were independent of reduction in target lobe volume or the presence of a complete lobar atelectasis.
In patients with more severe chronic obstructive pulmonary disease (COPD), the usual treatments of smoking cessation, pharmacological therapy, pulmonary rehabilitation aiming for symptom reduction, minimizing the burden of disease, slowing disease progression, and improving exercise tolerance fall short according to Sharyn A. Roodenburg, PhD candidate in the department of pulmonary diseases, University of Groningen (the Netherlands), and colleagues.
Lung volume reduction is generally reserved for patients with COPD that has a predominantly emphysematous phenotype and severely hyperinflated lungs. While both surgical and bronchoscopic lung volume reduction (BLVR) approaches are in use, bronchoscopic approaches are less invasive and incur lower morbidity. When technically feasible, they are generally preferred over open surgery.
BLVR using endobronchial valves (EBV), the most effective and commonly employed technique, has been shown in randomized controlled trials to improve pulmonary function, exercise capacity, and health-related quality of life.
Noting a survival benefit in prior studies among patients with complete lobar atelectasis following treatment, the authors wrote that their own clinical experience has been that significant treatment responses (pulmonary function and/or exercise capacity) observed in patients with a partial lobar atelectasis may also be associated with a survival benefit. Their aim was to evaluate whether pulmonary function, radiological, health-related quality of life, and/or exercise capacity outcome responders to EBV treatment have a survival benefit over nonresponders.
Their analysis included data collected prospectively out of four clinical trials (CHARTIS, STELVIO, IMPACT, and LIBERATE) from June 2008 to Dec. 2020 at the University Medical Center Groningen. Predetermined potential predictors of survival included change in forced expiratory volume in 1 second (FEV1), change in residual volume (RV), change in RV/total lung capacity (RV/TLC) ratio, change in 6-minute walk distance (6MWD), change in total score on the St. George’s Respiratory Questionnaire (SGRQ), target lobe volume reduction (TLVR), and presence of complete lobar atelectasis (defined as a TLVR of 100%).
Mean age was 61.3 years among the 428 included patients (68% women). Data on both the 6MWD and SGRQ total score at baseline and 1-year follow-up were available for 252 patients. SGRQ decreased by 8.3 points or more, and 6MWD increased by 26 meters or more over baseline. Among these patients, 113 (45%) were responders on both 6MWD and SGRQ, 49 (19%) patients were responders on 6MWD only, 31 (12%) patients on SGRQ only, and 59 (23%) were nonresponders on both. Survival was significantly worse among nonresponders on 6MWD, SGRQ, or on both. 6MWD and SGRQ response were independent predictors for improved survival time (hazard ratio, 0.50; 95% confidence interval, 0.28-0.89; P = .02 and HR, 0.54; 95% confidence interval, 0.30-0.94; P = .03, respectively). Survival was not significantly affected by the presence of complete lobar atelectasis or pulmonary function improvements.
“Especially in patients with a low FEV1 (< 50% predicted), 6-minute walk distance was found to be a better predictor for mortality than pulmonary function. A possible explanation for why change in 6-minute walk distance is a better predictor for survival after EBV treatment than the change in pulmonary function and hyperinflation might be that the 6-minute walk distance not only reflects the pulmonary limitation of these patients, but also captures the extrapulmonary manifestations of COPD, such as cardiac dysfunction, musculoskeletal disorders, fatigue, and psychological symptoms, all of which can impact survival,” the authors noted
The study received no funding, and the authors did not report any disclosures.
This article was updated 3/30/23.
FROM RESPIRATORY MEDICINE
Meet the JCOM Author with Dr. Barkoudah: Leading for High Reliability During the COVID-19 Pandemic
Meet the JCOM Author with Dr. Barkoudah: Residence Characteristics and Nursing Home Compare Quality Measures
Implementation of a Multidisciplinary Team–Based Clinical Care Pathway Is Associated With Increased Surgery Rates for Infective Endocarditis
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
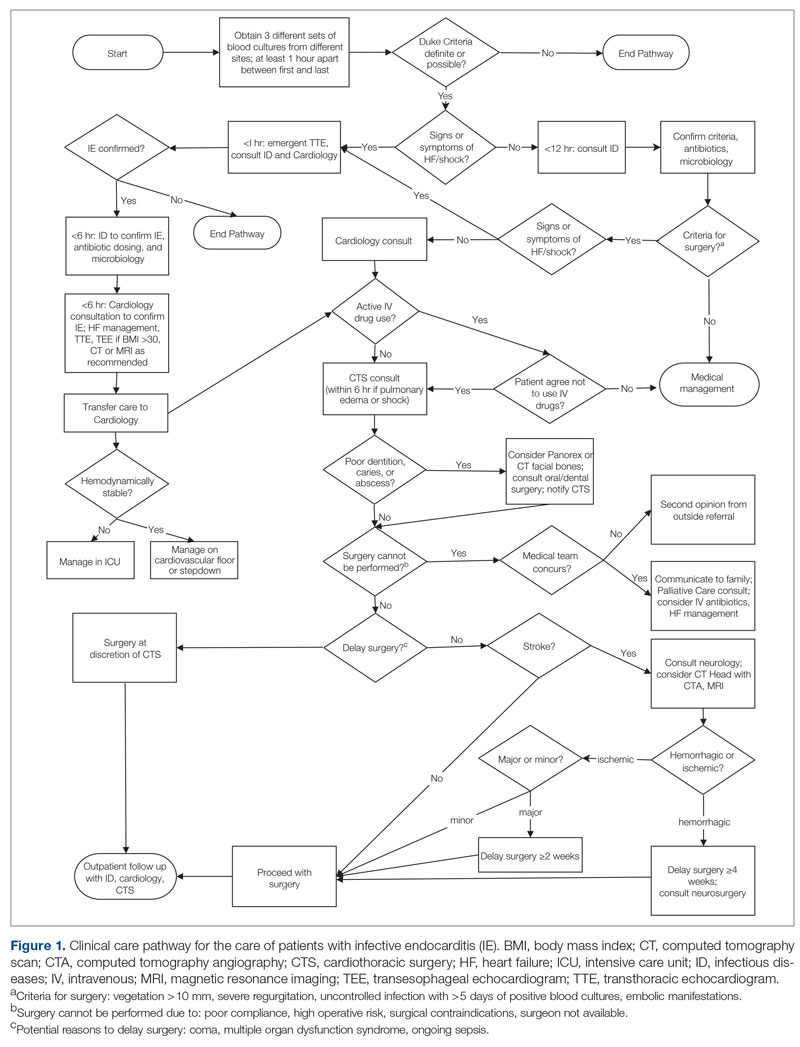
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
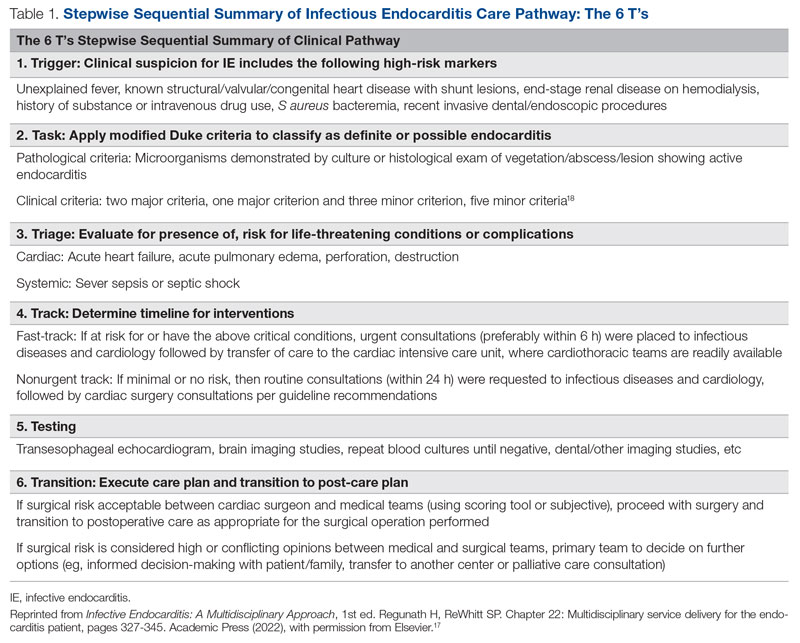
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
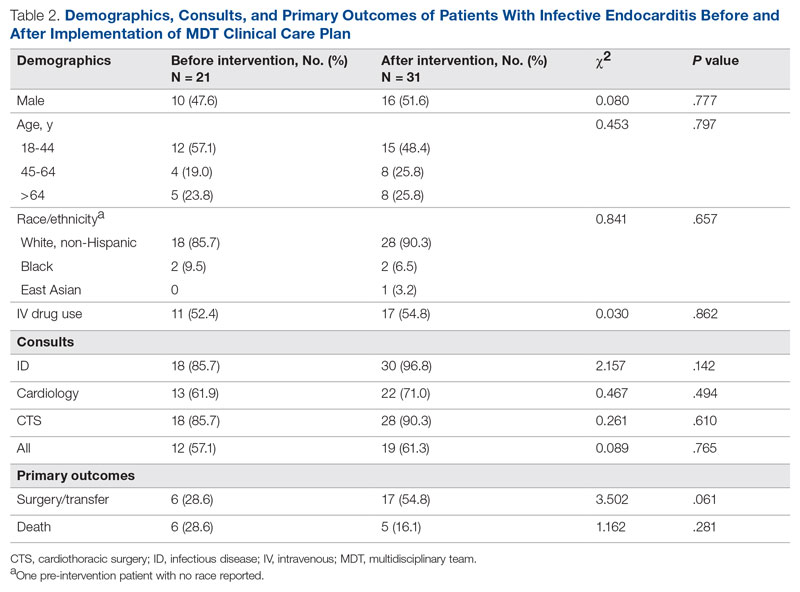
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
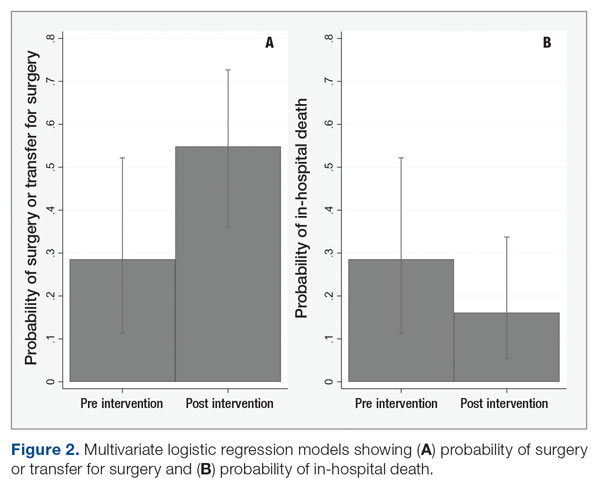
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
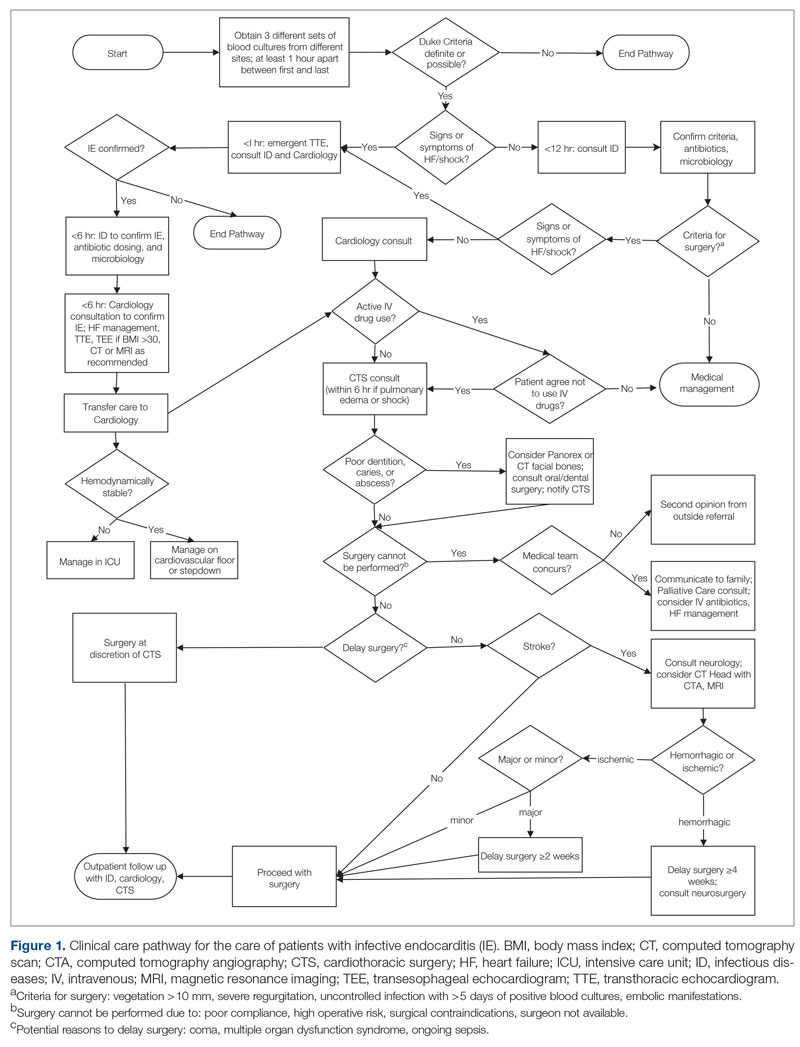
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
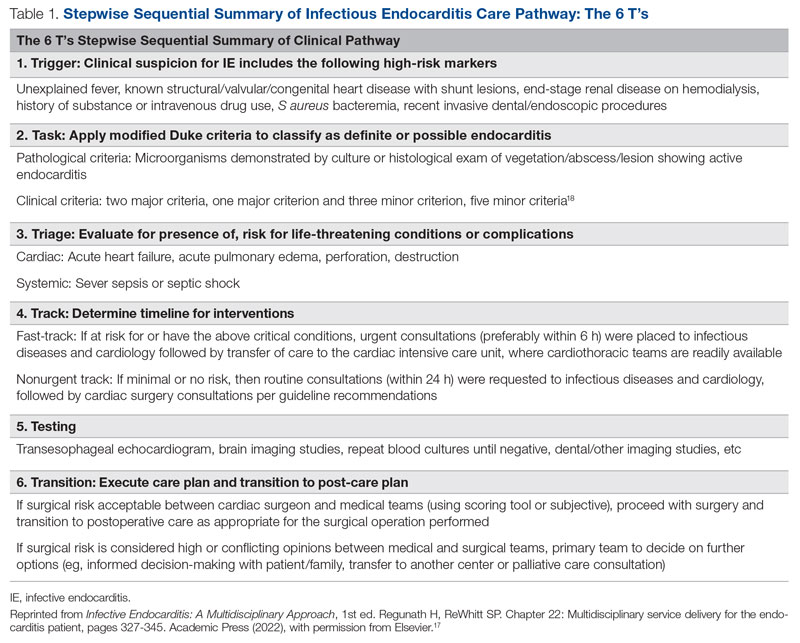
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
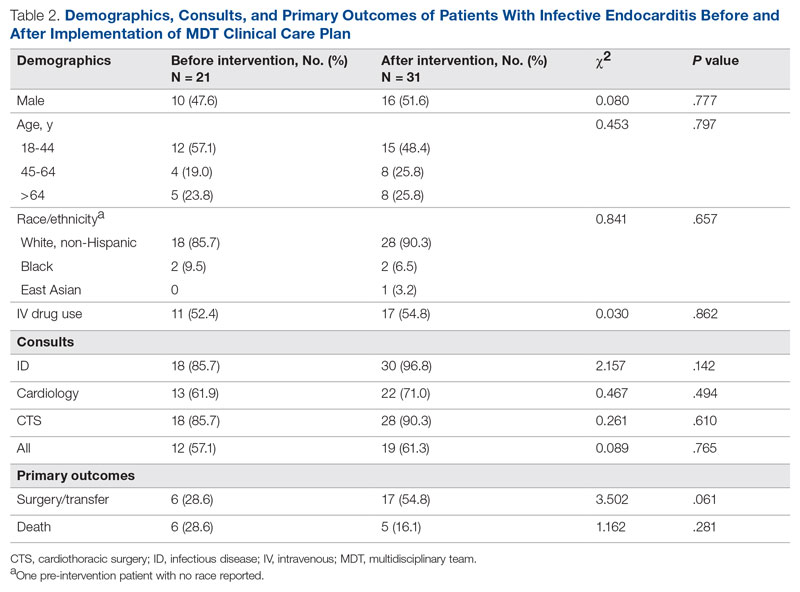
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
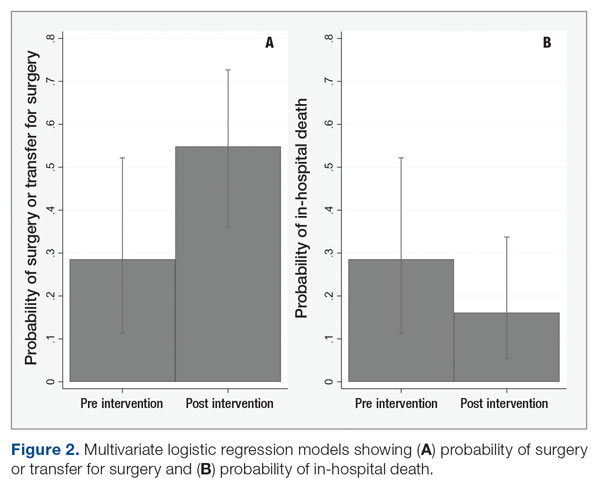
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
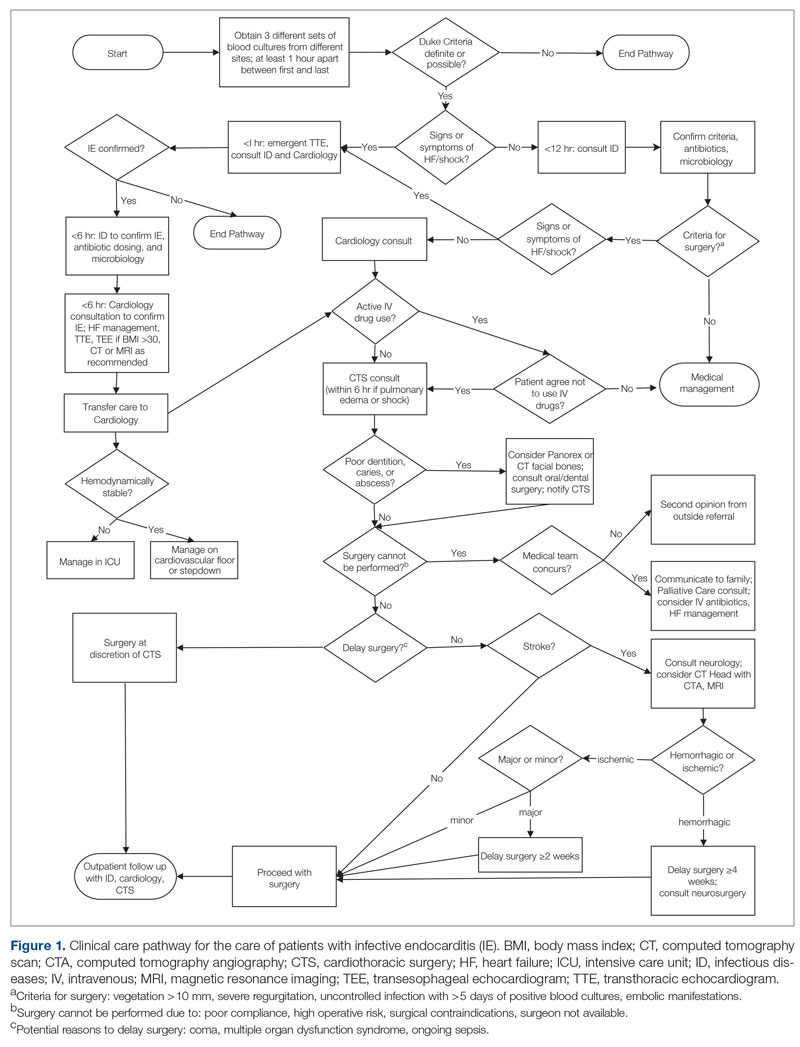
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
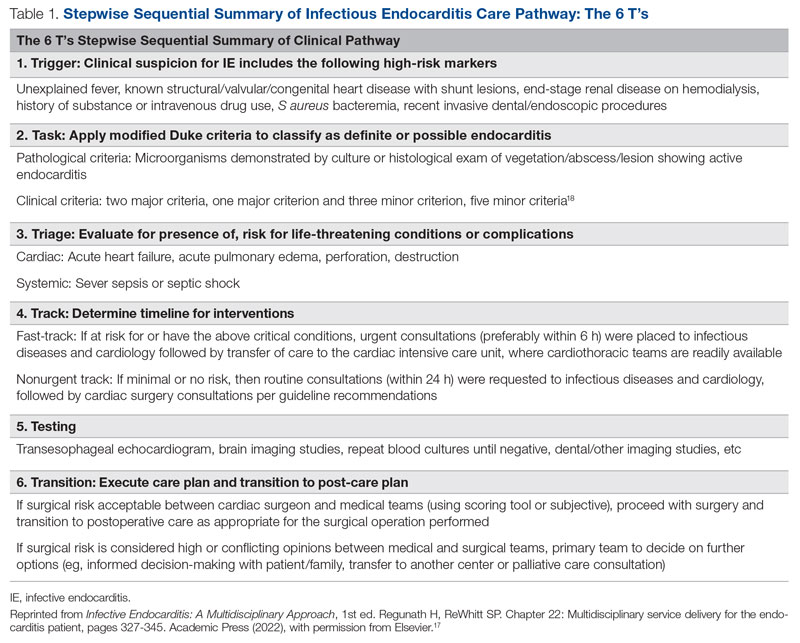
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
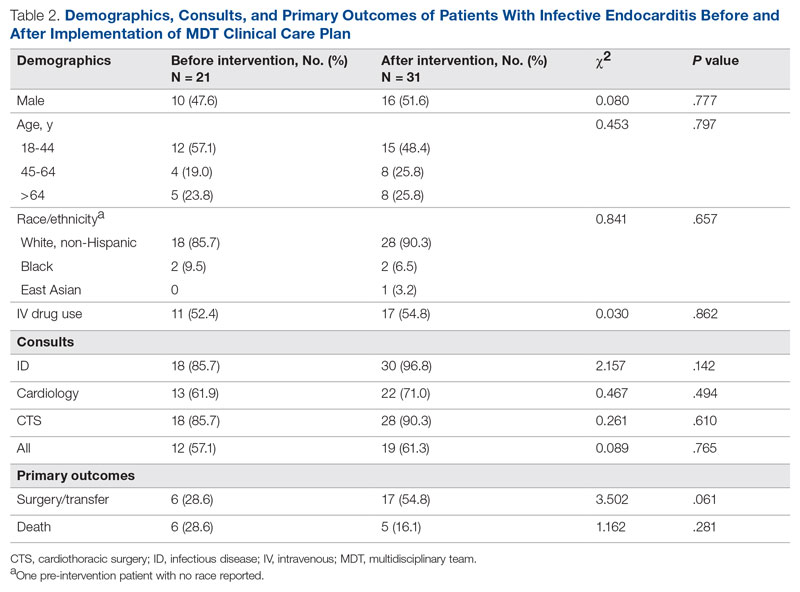
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
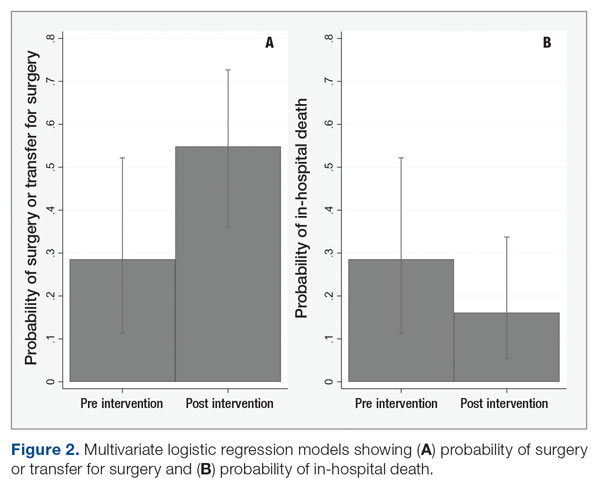
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
Relationships Between Residence Characteristics and Nursing Home Compare Database Quality Measures
From the University of Nebraska, Lincoln (Mr. Puckett and Dr. Ryherd), University of Nebraska Medical Center, Omaha (Dr. Manley), and the University of Nebraska, Omaha (Dr. Ryan).
ABSTRACT
Objective: This study evaluated relationships between physical characteristics of nursing home residences and quality-of-care measures.
Design: This was a cross-sectional ecologic study. The dependent variables were 5 Centers for Medicare & Medicaid Services (CMS) Nursing Home Compare database long-stay quality measures (QMs) during 2019: percentage of residents who displayed depressive symptoms, percentage of residents who were physically restrained, percentage of residents who experienced 1 or more falls resulting in injury, percentage of residents who received antipsychotic medication, and percentage of residents who received anti-anxiety medication. The independent variables were 4 residence characteristics: ownership type, size, occupancy, and region within the United States. We explored how different types of each residence characteristic compare for each QM.
Setting, participants, and measurements: Quality measure values from 15,420 CMS-supported nursing homes across the United States averaged over the 4 quarters of 2019 reporting were used. Welch’s analysis of variance was performed to examine whether the mean QM values for groups within each residential characteristic were statistically different.
Results: Publicly owned and low-occupancy residences had the highest mean QM values, indicating the poorest performance. Nonprofit and high-occupancy residences generally had the lowest (ie, best) mean QM values. There were significant differences in mean QM values among nursing home sizes and regions.
Conclusion: This study suggests that residence characteristics are related to 5 nursing home QMs. Results suggest that physical characteristics may be related to overall quality of life in nursing homes.
Keywords: quality of care, quality measures, residence characteristics, Alzheimer’s disease and related dementias.
More than 55 million people worldwide are living with Alzheimer’s disease and related dementias (ADRD).1 With the aging of the Baby Boomer population, this number is expected to rise to more than 78 million worldwide by 2030.1 Given the growing number of cognitively impaired older adults, there is an increased need for residences designed for the specialized care of this population. Although there are dozens of living options for the elderly, and although most specialized establishments have the resources to meet the immediate needs of their residents, many facilities lack universal design features that support a high quality of life for someone with ADRD or mild cognitive impairment. Previous research has shown relationships between behavioral and psychological symptoms of dementia (BPSD) and environmental characteristics such as acoustics, lighting, and indoor air temperature.2,3 Physical behaviors of BPSD, including aggression and wandering, and psychological symptoms, such as depression, anxiety, and delusions, put residents at risk of injury.4 Additionally, BPSD is correlated with caregiver burden and stress.5-8 Patients with dementia may also experience a lower stress threshold, changes in perception of space, and decreased short-term memory, creating environmental difficulties for those with ADRD9 that lead them to exhibit BPSD due to poor environmental design. Thus, there is a need to learn more about design features that minimize BPSD and promote a high quality of life for those with ADRD.10
Although research has shown relationships between physical environmental characteristics and BPSD, in this work we study relationships between possible BPSD indicators and 4 residence-level characteristics: ownership type, size, occupancy, and region in the United States (determined by location of the Centers for Medicare & Medicaid Services [CMS] regional offices). We analyzed data from the CMS Nursing Home Compare database for the year 2019.11 This database publishes quarterly data and star ratings for quality-of-care measures (QMs), staffing levels, and health inspections for every nursing home supported by CMS. Previous research has investigated the accuracy of QM reporting for resident falls, the impact of residential characteristics on administration of antipsychotic medication, the influence of profit status on resident outcomes and quality of care, and the effect of nursing home size on quality of life.12-16 Additionally, research suggests that residential characteristics such as size and location could be associated with infection control in nursing homes.17
Certain QMs, such as psychotropic drug administration, resident falls, and physical restraint, provide indicators of agitation, disorientation, or aggression, which are often signals of BPSD episodes. We hypothesized that residence types are associated with different QM scores, which could indicate different occurrences of BPSD. We selected 5 QMs for long-stay residents that could potentially be used as indicators of BPSD. Short-stay resident data were not included in this work to control for BPSD that could be a result of sheer unfamiliarity with the environment and confusion from being in a new home.
Methods
Design and Data Collection
This was a cross-sectional ecologic study aimed at exploring relationships between aggregate residential characteristics and QMs. Data were retrieved from the 2019 annual archives found in the CMS provider data catalog on nursing homes, including rehabilitation services.11 The dataset provides general residence information, such as ownership, number of beds, number of residents, and location, as well as residence quality metrics, such as QMs, staffing data, and inspection data. Residence characteristics and 4-quarter averages of QMs were retrieved and used as cross-sectional data. The data used are from 15,420 residences across the United States. Nursing homes located in Guam, the US Pacific Territories, Puerto Rico, and the US Virgin Islands, while supported by CMS and included in the dataset, were excluded from the study due to a severe absence of QM data.
Dependent Variables
We investigated 5 QMs that were averaged across the 4 quarters of 2019. The QMs used as dependent variables were percentage of residents who displayed depressive symptoms (depression), percentage of residents who were physically restrained (restraint), percentage of residents who experienced 1 or more falls resulting in a major injury (falls), percentage of residents who received antipsychotic medication (antipsychotic medication), and percentage of residents who received anti-anxiety or hypnotic medication (anti-anxiety medication).
A total of 2471 QM values were unreported across the 5 QM analyzed: 501 residences did not report depression data; 479 did not report restraint data; 477 did not report falls data; 508 did not report antipsychotic medication data; and 506 did not report anti-anxiety medication data. A residence with a missing QM value was excluded from that respective analysis.
To assess the relationships among the different QMs, a Pearson correlation coefficient r was computed for each unique pair of QMs (Figure). All QMs studied were found to be very weakly or weakly correlated with one another using the Evans classification for very weak and weak correlations (r < 0.20 and 0.20 < r < 0.39, respectively).18
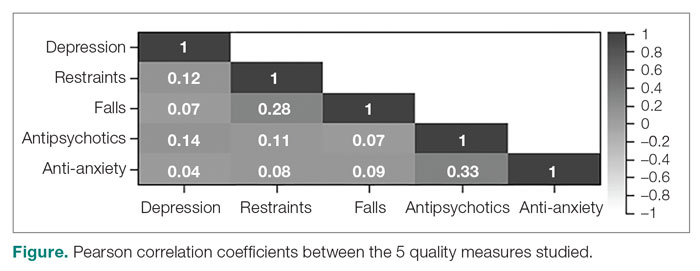
Independent Variables
A total of 15,420 residences were included in the study. Seventy-nine residences did not report occupancy data, however, so those residences were excluded from the occupancy analyses. We categorized the ownership of each nursing home as for-profit, nonprofit, or public. We categorized nursing home size, based on quartiles of the size distribution, as large (> 127 beds), medium (64 to 126 beds), and small (< 64 beds). This method for categorizing the residential characteristics was similar to that used in previous work.19 Similarly, we categorized nursing home occupancy as high (> 92% occupancy), medium (73% to 91% occupancy), and low (< 73% occupancy) based on quartiles of the occupancy distribution. For the regional analysis, we grouped states together based on the CMS regional offices: Atlanta, Georgia; Boston, Massachusetts; Chicago, Illinois; Dallas, Texas; Denver, Colorado; Kansas City, Missouri; New York, New York; Philadelphia, Pennsylvania; San Francisco, California; and Seattle, Washington.20
Analyses
We used Levene’s test to determine whether variances among the residential groups were equal for each QM, using an a priori α = 0.05. For all 20 tests conducted (4 residential characteristics for all 5 QMs), the resulting F-statistics were significant, indicating that the assumption of homogeneity of variance was not met.
We therefore used Welch’s analysis of variance (ANOVA) to evaluate whether the groups within each residential characteristic were the same on their QM means. For example, we tested whether for-profit, nonprofit, and public residences had significantly different mean depression rates. For statistically significant differences, a Games-Howell post-hoc test was conducted to test the difference between all unique pairwise comparisons. An a priori α = 0.05 was used for both Welch’s ANOVA and post-hoc testing. All analyses were conducted in RStudio Version 1.2.5033 (Posit Software, PBC).
Results
Mean Differences
Mean QM scores for the 5 QMs investigated, grouped by residential characteristic for the 2019 year of reporting, are shown in Table 1. It should be noted that the number of residences that reported occupancy data (n = 15,341) does not equal the total number of residences included in the study (N = 15,420) because 79 residences did not report occupancy data. For all QMs reported in Table 1, lower scores are better. Table 2 and Table 3 show results from pairwise comparisons of mean differences for the different residential characteristic and QM groupings. Mean differences and 95% CI are presented along with an indication of statistical significance (when applicable).
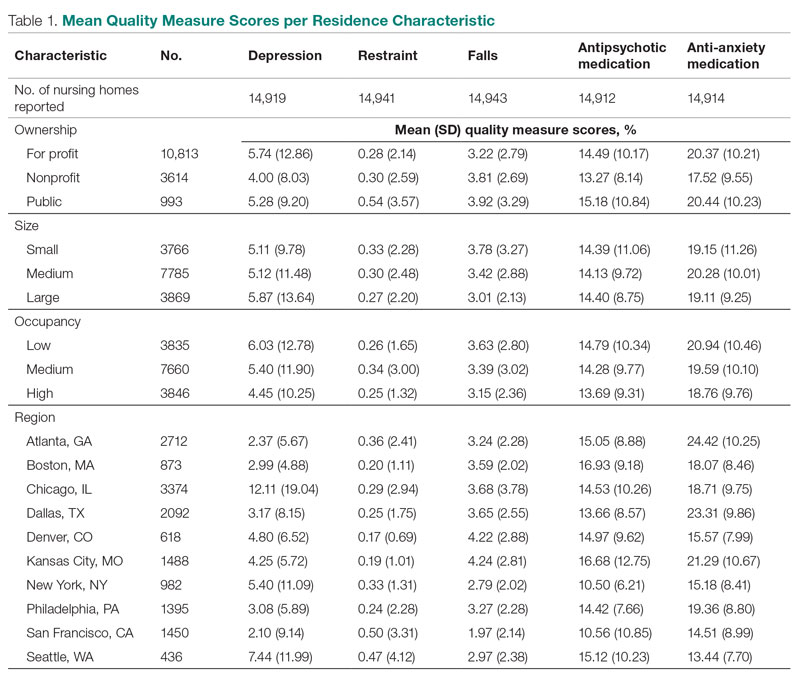
Ownership
Nonprofit residences had significantly lower (ie, better) mean scores than for-profit and public residences for 3 QMs: resident depression, antipsychotic medication use, and anti-anxiety medication use. For-profit and public residences did not significantly differ in their mean values for these QMs. For-profit residences had a significantly lower mean score for resident falls than both nonprofit and public residences, but no significant difference existed between scores for nonprofit and public residence falls. There were no statistically significant differences between mean restraint scores among the ownership types.
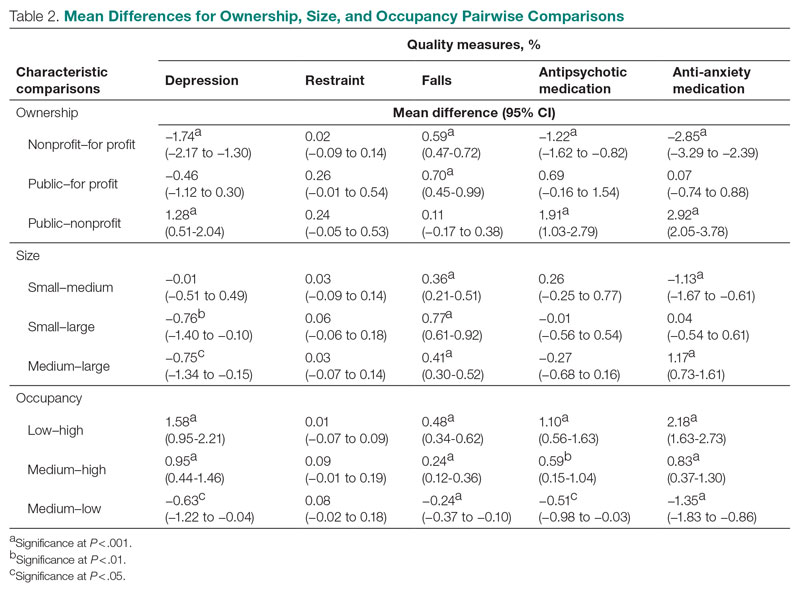
Size
Large (ie, high-capacity) residences had a significantly higher mean depression score than both medium and small residences, but there was not a significant difference between medium and small residences. Large residences had the significantly lowest mean score for resident falls, and medium residences scored significantly lower than small residences. Medium residences had a significantly higher mean score for anti-anxiety medication use than both small and large residences, but there was no significant difference between small and large residences. There were no statistically significant differences between mean scores for restraint and antipsychotic medication use among the nursing home sizes.
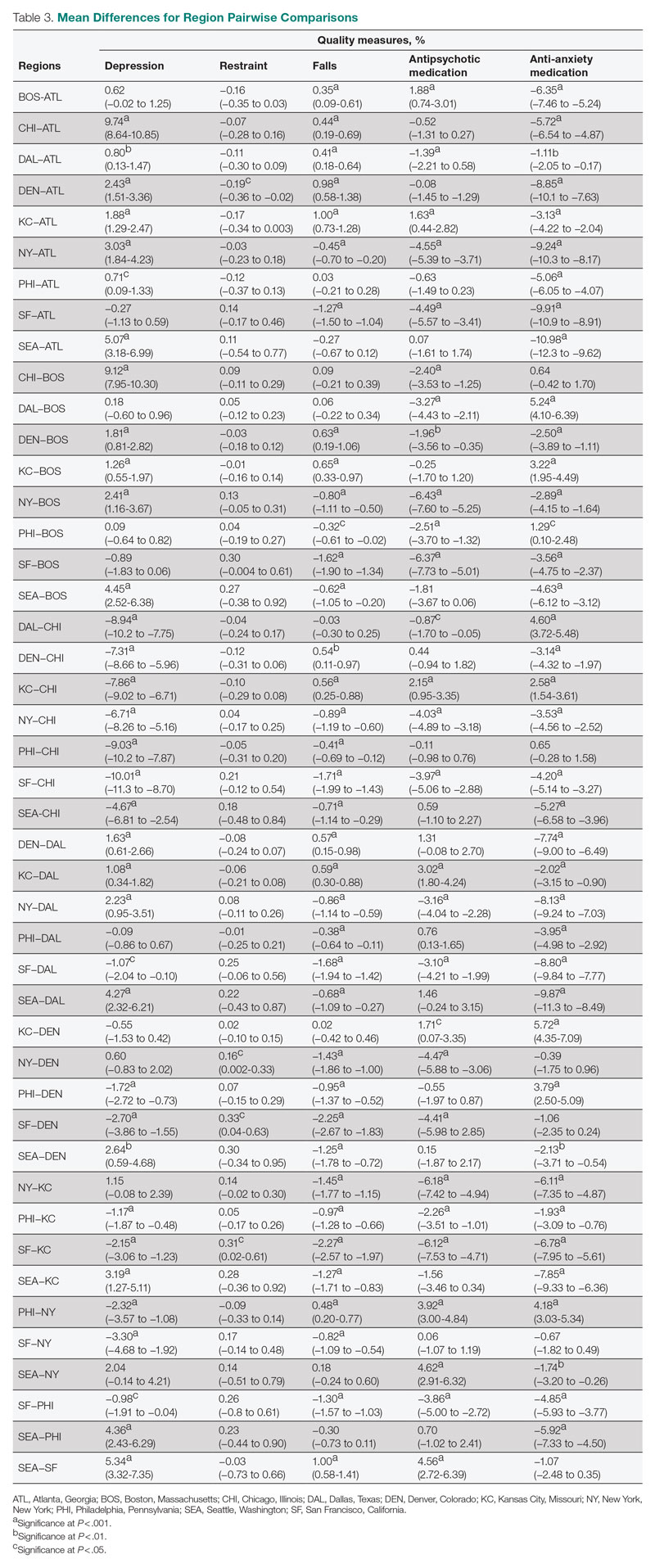
Occupancy
The mean scores for 4 out of the 5 QMs exhibited similar relationships with occupancy rates: resident depression, falls, and antipsychotic and anti-anxiety medication use. Low-occupancy residences consistently scored significantly higher than both medium- and high-occupancy residences, and medium-occupancy residences consistently scored significantly higher than high-occupancy residences. On average, high-occupancy (≥ 92%) residences reported better QM scores than low-occupancy (< 73%) and medium-occupancy (73% to 91%) residences for all the QMs studied except physical restraint, which yielded no significant results. These findings indicate a possible inverse relationship between building occupancy rate and these 4 QMs.
Region
Pairwise comparisons of mean QM scores by region are shown in Table 3. The Chicago region had a significantly higher mean depression score than all other regions, while the San Francisco region’s score was significantly lower than all other regions, except Atlanta and Boston. The Kansas City region had a significantly higher mean score for resident falls than all other regions, with the exception of Denver, and the San Francisco region scored significantly lower than all other regions in falls. The Boston region had a significantly higher mean score for administering antipsychotic medication than all other regions, except for Kansas City and Seattle, and the New York and San Francisco regions both had significantly lower scores than all other regions except for each other. The Atlanta region reported a significantly higher mean score for administering antianxiety medication than all other regions, and the Seattle region’s score for anti-anxiety medication use was significantly lower than all other regions except for San Francisco.
Discussion
This study presented mean percentages for 5 QMs reported in the Nursing Home Compare database for the year 2019: depression, restraint, falls, antipsychotic medication use, and anti-anxiety medication use. We investigated these scores by 4 residential characteristics: ownership type, size, occupancy, and region. In general, publicly owned and low-occupancy residences had the highest scores, and thus the poorest performances, for the 5 chosen QMs during 2019. Nonprofit and high-occupancy residences generally had the lowest (ie, better) scores, and this result agrees with previous findings on long-stay nursing home residents.21 One possible explanation for better performance by high-occupancy buildings could be that increased social interaction is beneficial to nursing home residents as compared with low-occupancy buildings, where less social interaction is probable. It is difficult to draw conclusions regarding nursing home size and region; however, there are significant differences among sizes for 3 out of the 5 QMs and significant differences among regions for all 5 QMs. The analyses suggest that residence-level characteristics are related to QM scores. Although reported QMs are not a direct representation of resident quality of life, this work agrees with previous research that residential characteristics have some impact on the lives of nursing home residents.13-17 Improvements in QM reporting and changes in quality improvement goals since the formation of Nursing Home Compare exist, suggesting that nursing homes’ awareness of their reporting duties may impact quality of care or reporting tendencies.21,22 Future research should consider investigating the impacts of the COVID-19 pandemic on quality-reporting trends and QM scores.
Other physical characteristics of nursing homes, such as noise, lighting levels, and air quality, may also have an impact on QMs and possibly nursing home residents themselves. This type of data exploration could be included in future research. Additionally, future research could include a similar analysis over a longer period, rather than the 1-year period examined here, to investigate which types of residences consistently have high or low scores or how different types of residences have evolved over the years, particularly considering the impact of the COVID-19 pandemic. Information such as staffing levels, building renovations, and inspection data could be accounted for in future studies. Different QMs could also be investigated to better understand the influence of residential characteristics on quality of care.
Conclusion
This study suggests that residence-level characteristics are related to 5 reported nursing home QMs. Overall, nonprofit and high-occupancy residences had the lowest QM scores, indicating the highest performance. Although the results do not necessarily suggest that residence-level characteristics impact individual nursing home residents’ quality of life, they suggest that physical characteristics affect overall quality of life in nursing homes. Future research is needed to determine the specific physical characteristics of these residences that affect QM scores.
Corresponding author: Brian J. Puckett, [email protected].
Disclosures: None reported.
1. Gauthier S, Rosa-Neto P, Morais JA, et al. World Alzheimer report 2021: journey through the diagnosis of dementia. Alzheimer’s Disease International; 2021.
2. Garre-Olmo J, López-Pousa S, Turon-Estrada A, et al. Environmental determinants of quality of life in nursing home residents with severe dementia. J Am Geriatr Soc. 2012;60(7):1230-1236. doi:10.1111/j.1532-5415.2012.04040.x
3. Zeisel J, Silverstein N, Hyde J, et al. Environmental correlates to behavioral health outcomes in Alzheimer’s special care units. Gerontologist. 2003;43(5):697-711. doi:10.1093/geront/43.5.697
4. Brawley E. Environmental design for Alzheimer’s disease: a quality of life issue. Aging Ment Health. 2001;5(1):S79-S83. doi:10.1080/13607860120044846
5. Joosse L. Do sound levels and space contribute to agitation in nursing home residents with dementia? Research Gerontol Nurs. 2012;5(3):174-184. doi:10.3928/19404921-20120605-02
6. Dowling G, Graf C, Hubbard E, et al. Light treatment for neuropsychiatric behaviors in Alzheimer’s disease. Western J Nurs Res. 2007;29(8):961-975. doi:10.1177/0193945907303083
7. Tartarini F, Cooper P, Fleming R, et al. Indoor air temperature and agitation of nursing home residents with dementia. Am J Alzheimers Dis Other Demen. 2017;32(5):272-281. doi:10.1177/1533317517704898
8. Miyamoto Y, Tachimori H, Ito H. Formal caregiver burden in dementia: impact of behavioral and psychological symptoms of dementia and activities of daily living. Geriatr Nurs. 2010;31(4):246-253. doi:10.1016/j.gerinurse.2010.01.002
9. Dementia care and the built environment: position paper 3. Alzheimer’s Australia; 2004.
10. Cloak N, Al Khalili Y. Behavioral and psychological symptoms in dementia. Updated July 21, 2022. In: StatPearls [Internet]. StatPearls Publishing; 2022.
11. Centers for Medicare & Medicaid Services. Nursing homes including rehab services data archive. 2019 annual files. Accessed January 30, 2023. https://data.cms.gov/provider-data/archived-data/nursing-homes
12. Sanghavi P, Pan S, Caudry D. Assessment of nursing home reporting of major injury falls for quality measurement on Nursing Home Compare. Health Serv Res. 2020;55(2):201-210. doi:10.1111/1475-6773.13247
13. Hughes C, Lapane K, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing homes. Med Care. 2000;38(12):1164-1173. doi:10.1097/00005650-200012000-00003
14. Aaronson W, Zinn J, Rosko M. Do for-profit and not-for-profit nursing homes behave differently? Gerontologist. 1994;34(6):775-786. doi:10.1093/geront/34.6.775
15. O’Neill C, Harrington C, Kitchener M, et al. Quality of care in nursing homes: an analysis of relationships among profit, quality, and ownership. Med Care. 2003;41(12):1318-1330. doi:10.1097/01.MLR.0000100586.33970.58
16. Allen PD, Klein WC, Gruman C. Correlates of complaints made to the Connecticut Long-Term Care Ombudsman program: the role of organizational and structural factors. Res Aging. 2003;25(6):631-654. doi:10.1177/0164027503256691
17. Abrams H, Loomer L, Gandhi A, et al. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68(8):1653-1656. doi:10.1111/jgs.16661
18. Evans JD. Straightforward Statistics for the Behavioral Sciences. Thomson Brooks/Cole Publishing Co; 1996.
19. Zinn J, Spector W, Hsieh L, et al. Do trends in the reporting of quality measures on the Nursing Home Compare web site differ by nursing home characteristics? Gerontologist. 2005;45(6):720-730.
20. Centers for Medicare & Medicaid Services. CMS Regional Offices. Accessed January 30, 2023. https://www.cms.gov/Medicare/Coding/ICD10/CMS-Regional-Offices
21. Mukamel DB, Weimer DL, Spector WD, et al. Publication of quality report cards and trends in reported quality measures in nursing homes. Health Serv Res. 2008;43(4):1244-1262. doi:10.1093/geront/45.6.720
22. Harris Y, Clauser SB. Achieving improvement through nursing home quality measurement. Health Care Financ Rev. 2002;23(4):5-18.
From the University of Nebraska, Lincoln (Mr. Puckett and Dr. Ryherd), University of Nebraska Medical Center, Omaha (Dr. Manley), and the University of Nebraska, Omaha (Dr. Ryan).
ABSTRACT
Objective: This study evaluated relationships between physical characteristics of nursing home residences and quality-of-care measures.
Design: This was a cross-sectional ecologic study. The dependent variables were 5 Centers for Medicare & Medicaid Services (CMS) Nursing Home Compare database long-stay quality measures (QMs) during 2019: percentage of residents who displayed depressive symptoms, percentage of residents who were physically restrained, percentage of residents who experienced 1 or more falls resulting in injury, percentage of residents who received antipsychotic medication, and percentage of residents who received anti-anxiety medication. The independent variables were 4 residence characteristics: ownership type, size, occupancy, and region within the United States. We explored how different types of each residence characteristic compare for each QM.
Setting, participants, and measurements: Quality measure values from 15,420 CMS-supported nursing homes across the United States averaged over the 4 quarters of 2019 reporting were used. Welch’s analysis of variance was performed to examine whether the mean QM values for groups within each residential characteristic were statistically different.
Results: Publicly owned and low-occupancy residences had the highest mean QM values, indicating the poorest performance. Nonprofit and high-occupancy residences generally had the lowest (ie, best) mean QM values. There were significant differences in mean QM values among nursing home sizes and regions.
Conclusion: This study suggests that residence characteristics are related to 5 nursing home QMs. Results suggest that physical characteristics may be related to overall quality of life in nursing homes.
Keywords: quality of care, quality measures, residence characteristics, Alzheimer’s disease and related dementias.
More than 55 million people worldwide are living with Alzheimer’s disease and related dementias (ADRD).1 With the aging of the Baby Boomer population, this number is expected to rise to more than 78 million worldwide by 2030.1 Given the growing number of cognitively impaired older adults, there is an increased need for residences designed for the specialized care of this population. Although there are dozens of living options for the elderly, and although most specialized establishments have the resources to meet the immediate needs of their residents, many facilities lack universal design features that support a high quality of life for someone with ADRD or mild cognitive impairment. Previous research has shown relationships between behavioral and psychological symptoms of dementia (BPSD) and environmental characteristics such as acoustics, lighting, and indoor air temperature.2,3 Physical behaviors of BPSD, including aggression and wandering, and psychological symptoms, such as depression, anxiety, and delusions, put residents at risk of injury.4 Additionally, BPSD is correlated with caregiver burden and stress.5-8 Patients with dementia may also experience a lower stress threshold, changes in perception of space, and decreased short-term memory, creating environmental difficulties for those with ADRD9 that lead them to exhibit BPSD due to poor environmental design. Thus, there is a need to learn more about design features that minimize BPSD and promote a high quality of life for those with ADRD.10
Although research has shown relationships between physical environmental characteristics and BPSD, in this work we study relationships between possible BPSD indicators and 4 residence-level characteristics: ownership type, size, occupancy, and region in the United States (determined by location of the Centers for Medicare & Medicaid Services [CMS] regional offices). We analyzed data from the CMS Nursing Home Compare database for the year 2019.11 This database publishes quarterly data and star ratings for quality-of-care measures (QMs), staffing levels, and health inspections for every nursing home supported by CMS. Previous research has investigated the accuracy of QM reporting for resident falls, the impact of residential characteristics on administration of antipsychotic medication, the influence of profit status on resident outcomes and quality of care, and the effect of nursing home size on quality of life.12-16 Additionally, research suggests that residential characteristics such as size and location could be associated with infection control in nursing homes.17
Certain QMs, such as psychotropic drug administration, resident falls, and physical restraint, provide indicators of agitation, disorientation, or aggression, which are often signals of BPSD episodes. We hypothesized that residence types are associated with different QM scores, which could indicate different occurrences of BPSD. We selected 5 QMs for long-stay residents that could potentially be used as indicators of BPSD. Short-stay resident data were not included in this work to control for BPSD that could be a result of sheer unfamiliarity with the environment and confusion from being in a new home.
Methods
Design and Data Collection
This was a cross-sectional ecologic study aimed at exploring relationships between aggregate residential characteristics and QMs. Data were retrieved from the 2019 annual archives found in the CMS provider data catalog on nursing homes, including rehabilitation services.11 The dataset provides general residence information, such as ownership, number of beds, number of residents, and location, as well as residence quality metrics, such as QMs, staffing data, and inspection data. Residence characteristics and 4-quarter averages of QMs were retrieved and used as cross-sectional data. The data used are from 15,420 residences across the United States. Nursing homes located in Guam, the US Pacific Territories, Puerto Rico, and the US Virgin Islands, while supported by CMS and included in the dataset, were excluded from the study due to a severe absence of QM data.
Dependent Variables
We investigated 5 QMs that were averaged across the 4 quarters of 2019. The QMs used as dependent variables were percentage of residents who displayed depressive symptoms (depression), percentage of residents who were physically restrained (restraint), percentage of residents who experienced 1 or more falls resulting in a major injury (falls), percentage of residents who received antipsychotic medication (antipsychotic medication), and percentage of residents who received anti-anxiety or hypnotic medication (anti-anxiety medication).
A total of 2471 QM values were unreported across the 5 QM analyzed: 501 residences did not report depression data; 479 did not report restraint data; 477 did not report falls data; 508 did not report antipsychotic medication data; and 506 did not report anti-anxiety medication data. A residence with a missing QM value was excluded from that respective analysis.
To assess the relationships among the different QMs, a Pearson correlation coefficient r was computed for each unique pair of QMs (Figure). All QMs studied were found to be very weakly or weakly correlated with one another using the Evans classification for very weak and weak correlations (r < 0.20 and 0.20 < r < 0.39, respectively).18
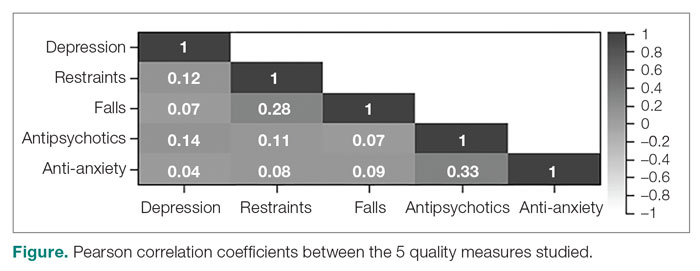
Independent Variables
A total of 15,420 residences were included in the study. Seventy-nine residences did not report occupancy data, however, so those residences were excluded from the occupancy analyses. We categorized the ownership of each nursing home as for-profit, nonprofit, or public. We categorized nursing home size, based on quartiles of the size distribution, as large (> 127 beds), medium (64 to 126 beds), and small (< 64 beds). This method for categorizing the residential characteristics was similar to that used in previous work.19 Similarly, we categorized nursing home occupancy as high (> 92% occupancy), medium (73% to 91% occupancy), and low (< 73% occupancy) based on quartiles of the occupancy distribution. For the regional analysis, we grouped states together based on the CMS regional offices: Atlanta, Georgia; Boston, Massachusetts; Chicago, Illinois; Dallas, Texas; Denver, Colorado; Kansas City, Missouri; New York, New York; Philadelphia, Pennsylvania; San Francisco, California; and Seattle, Washington.20
Analyses
We used Levene’s test to determine whether variances among the residential groups were equal for each QM, using an a priori α = 0.05. For all 20 tests conducted (4 residential characteristics for all 5 QMs), the resulting F-statistics were significant, indicating that the assumption of homogeneity of variance was not met.
We therefore used Welch’s analysis of variance (ANOVA) to evaluate whether the groups within each residential characteristic were the same on their QM means. For example, we tested whether for-profit, nonprofit, and public residences had significantly different mean depression rates. For statistically significant differences, a Games-Howell post-hoc test was conducted to test the difference between all unique pairwise comparisons. An a priori α = 0.05 was used for both Welch’s ANOVA and post-hoc testing. All analyses were conducted in RStudio Version 1.2.5033 (Posit Software, PBC).
Results
Mean Differences
Mean QM scores for the 5 QMs investigated, grouped by residential characteristic for the 2019 year of reporting, are shown in Table 1. It should be noted that the number of residences that reported occupancy data (n = 15,341) does not equal the total number of residences included in the study (N = 15,420) because 79 residences did not report occupancy data. For all QMs reported in Table 1, lower scores are better. Table 2 and Table 3 show results from pairwise comparisons of mean differences for the different residential characteristic and QM groupings. Mean differences and 95% CI are presented along with an indication of statistical significance (when applicable).
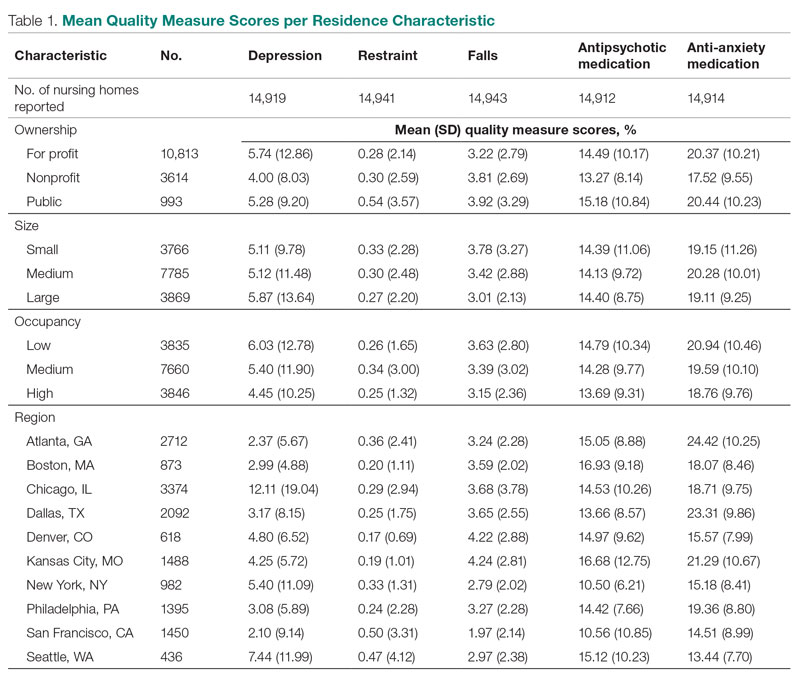
Ownership
Nonprofit residences had significantly lower (ie, better) mean scores than for-profit and public residences for 3 QMs: resident depression, antipsychotic medication use, and anti-anxiety medication use. For-profit and public residences did not significantly differ in their mean values for these QMs. For-profit residences had a significantly lower mean score for resident falls than both nonprofit and public residences, but no significant difference existed between scores for nonprofit and public residence falls. There were no statistically significant differences between mean restraint scores among the ownership types.
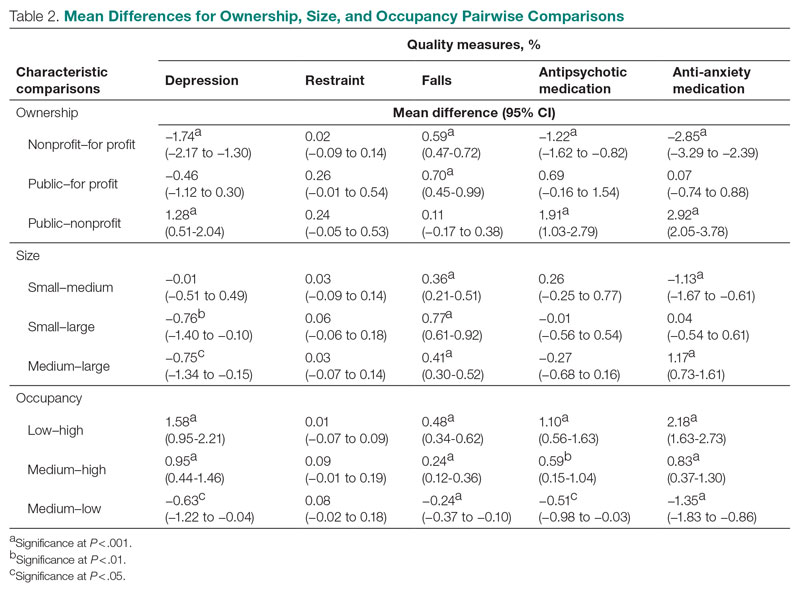
Size
Large (ie, high-capacity) residences had a significantly higher mean depression score than both medium and small residences, but there was not a significant difference between medium and small residences. Large residences had the significantly lowest mean score for resident falls, and medium residences scored significantly lower than small residences. Medium residences had a significantly higher mean score for anti-anxiety medication use than both small and large residences, but there was no significant difference between small and large residences. There were no statistically significant differences between mean scores for restraint and antipsychotic medication use among the nursing home sizes.
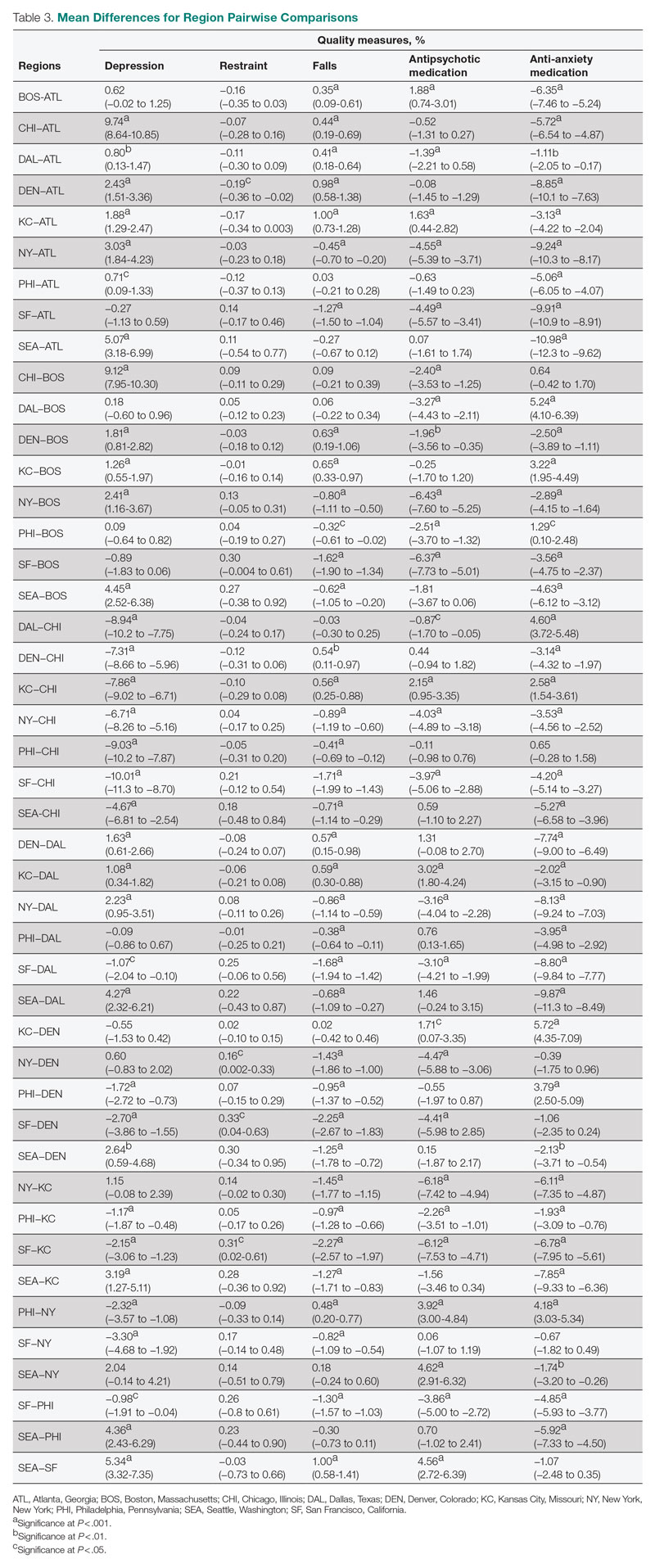
Occupancy
The mean scores for 4 out of the 5 QMs exhibited similar relationships with occupancy rates: resident depression, falls, and antipsychotic and anti-anxiety medication use. Low-occupancy residences consistently scored significantly higher than both medium- and high-occupancy residences, and medium-occupancy residences consistently scored significantly higher than high-occupancy residences. On average, high-occupancy (≥ 92%) residences reported better QM scores than low-occupancy (< 73%) and medium-occupancy (73% to 91%) residences for all the QMs studied except physical restraint, which yielded no significant results. These findings indicate a possible inverse relationship between building occupancy rate and these 4 QMs.
Region
Pairwise comparisons of mean QM scores by region are shown in Table 3. The Chicago region had a significantly higher mean depression score than all other regions, while the San Francisco region’s score was significantly lower than all other regions, except Atlanta and Boston. The Kansas City region had a significantly higher mean score for resident falls than all other regions, with the exception of Denver, and the San Francisco region scored significantly lower than all other regions in falls. The Boston region had a significantly higher mean score for administering antipsychotic medication than all other regions, except for Kansas City and Seattle, and the New York and San Francisco regions both had significantly lower scores than all other regions except for each other. The Atlanta region reported a significantly higher mean score for administering antianxiety medication than all other regions, and the Seattle region’s score for anti-anxiety medication use was significantly lower than all other regions except for San Francisco.
Discussion
This study presented mean percentages for 5 QMs reported in the Nursing Home Compare database for the year 2019: depression, restraint, falls, antipsychotic medication use, and anti-anxiety medication use. We investigated these scores by 4 residential characteristics: ownership type, size, occupancy, and region. In general, publicly owned and low-occupancy residences had the highest scores, and thus the poorest performances, for the 5 chosen QMs during 2019. Nonprofit and high-occupancy residences generally had the lowest (ie, better) scores, and this result agrees with previous findings on long-stay nursing home residents.21 One possible explanation for better performance by high-occupancy buildings could be that increased social interaction is beneficial to nursing home residents as compared with low-occupancy buildings, where less social interaction is probable. It is difficult to draw conclusions regarding nursing home size and region; however, there are significant differences among sizes for 3 out of the 5 QMs and significant differences among regions for all 5 QMs. The analyses suggest that residence-level characteristics are related to QM scores. Although reported QMs are not a direct representation of resident quality of life, this work agrees with previous research that residential characteristics have some impact on the lives of nursing home residents.13-17 Improvements in QM reporting and changes in quality improvement goals since the formation of Nursing Home Compare exist, suggesting that nursing homes’ awareness of their reporting duties may impact quality of care or reporting tendencies.21,22 Future research should consider investigating the impacts of the COVID-19 pandemic on quality-reporting trends and QM scores.
Other physical characteristics of nursing homes, such as noise, lighting levels, and air quality, may also have an impact on QMs and possibly nursing home residents themselves. This type of data exploration could be included in future research. Additionally, future research could include a similar analysis over a longer period, rather than the 1-year period examined here, to investigate which types of residences consistently have high or low scores or how different types of residences have evolved over the years, particularly considering the impact of the COVID-19 pandemic. Information such as staffing levels, building renovations, and inspection data could be accounted for in future studies. Different QMs could also be investigated to better understand the influence of residential characteristics on quality of care.
Conclusion
This study suggests that residence-level characteristics are related to 5 reported nursing home QMs. Overall, nonprofit and high-occupancy residences had the lowest QM scores, indicating the highest performance. Although the results do not necessarily suggest that residence-level characteristics impact individual nursing home residents’ quality of life, they suggest that physical characteristics affect overall quality of life in nursing homes. Future research is needed to determine the specific physical characteristics of these residences that affect QM scores.
Corresponding author: Brian J. Puckett, [email protected].
Disclosures: None reported.
From the University of Nebraska, Lincoln (Mr. Puckett and Dr. Ryherd), University of Nebraska Medical Center, Omaha (Dr. Manley), and the University of Nebraska, Omaha (Dr. Ryan).
ABSTRACT
Objective: This study evaluated relationships between physical characteristics of nursing home residences and quality-of-care measures.
Design: This was a cross-sectional ecologic study. The dependent variables were 5 Centers for Medicare & Medicaid Services (CMS) Nursing Home Compare database long-stay quality measures (QMs) during 2019: percentage of residents who displayed depressive symptoms, percentage of residents who were physically restrained, percentage of residents who experienced 1 or more falls resulting in injury, percentage of residents who received antipsychotic medication, and percentage of residents who received anti-anxiety medication. The independent variables were 4 residence characteristics: ownership type, size, occupancy, and region within the United States. We explored how different types of each residence characteristic compare for each QM.
Setting, participants, and measurements: Quality measure values from 15,420 CMS-supported nursing homes across the United States averaged over the 4 quarters of 2019 reporting were used. Welch’s analysis of variance was performed to examine whether the mean QM values for groups within each residential characteristic were statistically different.
Results: Publicly owned and low-occupancy residences had the highest mean QM values, indicating the poorest performance. Nonprofit and high-occupancy residences generally had the lowest (ie, best) mean QM values. There were significant differences in mean QM values among nursing home sizes and regions.
Conclusion: This study suggests that residence characteristics are related to 5 nursing home QMs. Results suggest that physical characteristics may be related to overall quality of life in nursing homes.
Keywords: quality of care, quality measures, residence characteristics, Alzheimer’s disease and related dementias.
More than 55 million people worldwide are living with Alzheimer’s disease and related dementias (ADRD).1 With the aging of the Baby Boomer population, this number is expected to rise to more than 78 million worldwide by 2030.1 Given the growing number of cognitively impaired older adults, there is an increased need for residences designed for the specialized care of this population. Although there are dozens of living options for the elderly, and although most specialized establishments have the resources to meet the immediate needs of their residents, many facilities lack universal design features that support a high quality of life for someone with ADRD or mild cognitive impairment. Previous research has shown relationships between behavioral and psychological symptoms of dementia (BPSD) and environmental characteristics such as acoustics, lighting, and indoor air temperature.2,3 Physical behaviors of BPSD, including aggression and wandering, and psychological symptoms, such as depression, anxiety, and delusions, put residents at risk of injury.4 Additionally, BPSD is correlated with caregiver burden and stress.5-8 Patients with dementia may also experience a lower stress threshold, changes in perception of space, and decreased short-term memory, creating environmental difficulties for those with ADRD9 that lead them to exhibit BPSD due to poor environmental design. Thus, there is a need to learn more about design features that minimize BPSD and promote a high quality of life for those with ADRD.10
Although research has shown relationships between physical environmental characteristics and BPSD, in this work we study relationships between possible BPSD indicators and 4 residence-level characteristics: ownership type, size, occupancy, and region in the United States (determined by location of the Centers for Medicare & Medicaid Services [CMS] regional offices). We analyzed data from the CMS Nursing Home Compare database for the year 2019.11 This database publishes quarterly data and star ratings for quality-of-care measures (QMs), staffing levels, and health inspections for every nursing home supported by CMS. Previous research has investigated the accuracy of QM reporting for resident falls, the impact of residential characteristics on administration of antipsychotic medication, the influence of profit status on resident outcomes and quality of care, and the effect of nursing home size on quality of life.12-16 Additionally, research suggests that residential characteristics such as size and location could be associated with infection control in nursing homes.17
Certain QMs, such as psychotropic drug administration, resident falls, and physical restraint, provide indicators of agitation, disorientation, or aggression, which are often signals of BPSD episodes. We hypothesized that residence types are associated with different QM scores, which could indicate different occurrences of BPSD. We selected 5 QMs for long-stay residents that could potentially be used as indicators of BPSD. Short-stay resident data were not included in this work to control for BPSD that could be a result of sheer unfamiliarity with the environment and confusion from being in a new home.
Methods
Design and Data Collection
This was a cross-sectional ecologic study aimed at exploring relationships between aggregate residential characteristics and QMs. Data were retrieved from the 2019 annual archives found in the CMS provider data catalog on nursing homes, including rehabilitation services.11 The dataset provides general residence information, such as ownership, number of beds, number of residents, and location, as well as residence quality metrics, such as QMs, staffing data, and inspection data. Residence characteristics and 4-quarter averages of QMs were retrieved and used as cross-sectional data. The data used are from 15,420 residences across the United States. Nursing homes located in Guam, the US Pacific Territories, Puerto Rico, and the US Virgin Islands, while supported by CMS and included in the dataset, were excluded from the study due to a severe absence of QM data.
Dependent Variables
We investigated 5 QMs that were averaged across the 4 quarters of 2019. The QMs used as dependent variables were percentage of residents who displayed depressive symptoms (depression), percentage of residents who were physically restrained (restraint), percentage of residents who experienced 1 or more falls resulting in a major injury (falls), percentage of residents who received antipsychotic medication (antipsychotic medication), and percentage of residents who received anti-anxiety or hypnotic medication (anti-anxiety medication).
A total of 2471 QM values were unreported across the 5 QM analyzed: 501 residences did not report depression data; 479 did not report restraint data; 477 did not report falls data; 508 did not report antipsychotic medication data; and 506 did not report anti-anxiety medication data. A residence with a missing QM value was excluded from that respective analysis.
To assess the relationships among the different QMs, a Pearson correlation coefficient r was computed for each unique pair of QMs (Figure). All QMs studied were found to be very weakly or weakly correlated with one another using the Evans classification for very weak and weak correlations (r < 0.20 and 0.20 < r < 0.39, respectively).18
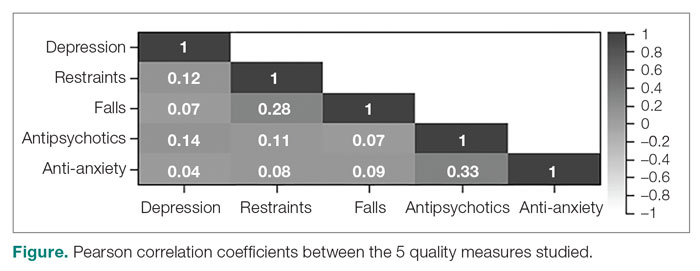
Independent Variables
A total of 15,420 residences were included in the study. Seventy-nine residences did not report occupancy data, however, so those residences were excluded from the occupancy analyses. We categorized the ownership of each nursing home as for-profit, nonprofit, or public. We categorized nursing home size, based on quartiles of the size distribution, as large (> 127 beds), medium (64 to 126 beds), and small (< 64 beds). This method for categorizing the residential characteristics was similar to that used in previous work.19 Similarly, we categorized nursing home occupancy as high (> 92% occupancy), medium (73% to 91% occupancy), and low (< 73% occupancy) based on quartiles of the occupancy distribution. For the regional analysis, we grouped states together based on the CMS regional offices: Atlanta, Georgia; Boston, Massachusetts; Chicago, Illinois; Dallas, Texas; Denver, Colorado; Kansas City, Missouri; New York, New York; Philadelphia, Pennsylvania; San Francisco, California; and Seattle, Washington.20
Analyses
We used Levene’s test to determine whether variances among the residential groups were equal for each QM, using an a priori α = 0.05. For all 20 tests conducted (4 residential characteristics for all 5 QMs), the resulting F-statistics were significant, indicating that the assumption of homogeneity of variance was not met.
We therefore used Welch’s analysis of variance (ANOVA) to evaluate whether the groups within each residential characteristic were the same on their QM means. For example, we tested whether for-profit, nonprofit, and public residences had significantly different mean depression rates. For statistically significant differences, a Games-Howell post-hoc test was conducted to test the difference between all unique pairwise comparisons. An a priori α = 0.05 was used for both Welch’s ANOVA and post-hoc testing. All analyses were conducted in RStudio Version 1.2.5033 (Posit Software, PBC).
Results
Mean Differences
Mean QM scores for the 5 QMs investigated, grouped by residential characteristic for the 2019 year of reporting, are shown in Table 1. It should be noted that the number of residences that reported occupancy data (n = 15,341) does not equal the total number of residences included in the study (N = 15,420) because 79 residences did not report occupancy data. For all QMs reported in Table 1, lower scores are better. Table 2 and Table 3 show results from pairwise comparisons of mean differences for the different residential characteristic and QM groupings. Mean differences and 95% CI are presented along with an indication of statistical significance (when applicable).
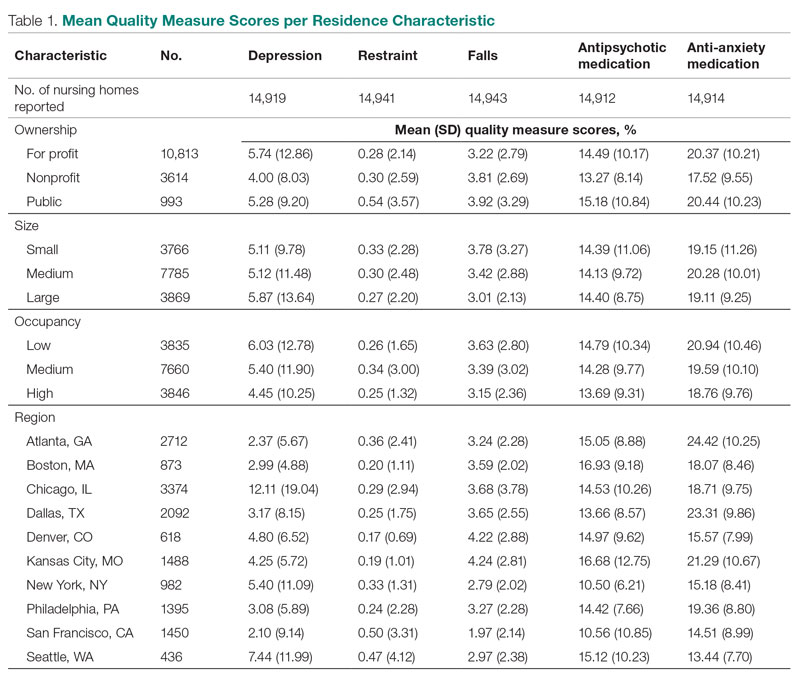
Ownership
Nonprofit residences had significantly lower (ie, better) mean scores than for-profit and public residences for 3 QMs: resident depression, antipsychotic medication use, and anti-anxiety medication use. For-profit and public residences did not significantly differ in their mean values for these QMs. For-profit residences had a significantly lower mean score for resident falls than both nonprofit and public residences, but no significant difference existed between scores for nonprofit and public residence falls. There were no statistically significant differences between mean restraint scores among the ownership types.
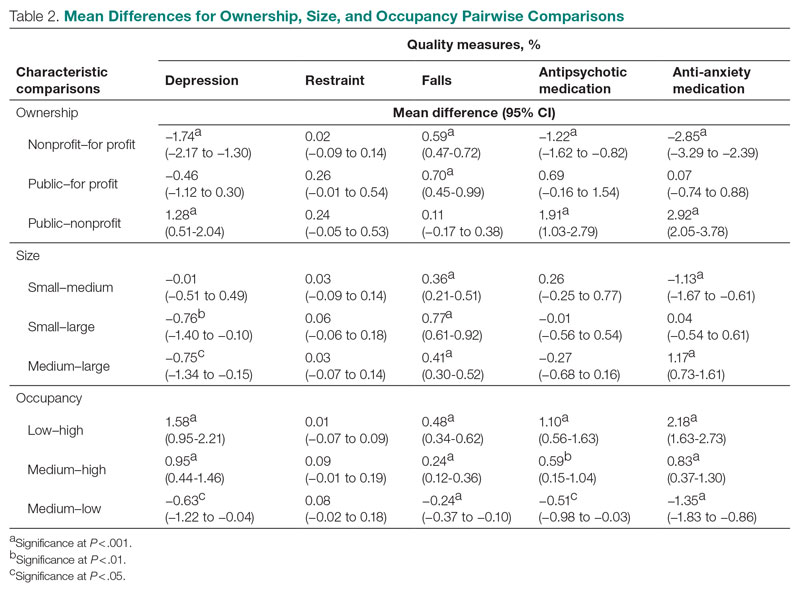
Size
Large (ie, high-capacity) residences had a significantly higher mean depression score than both medium and small residences, but there was not a significant difference between medium and small residences. Large residences had the significantly lowest mean score for resident falls, and medium residences scored significantly lower than small residences. Medium residences had a significantly higher mean score for anti-anxiety medication use than both small and large residences, but there was no significant difference between small and large residences. There were no statistically significant differences between mean scores for restraint and antipsychotic medication use among the nursing home sizes.
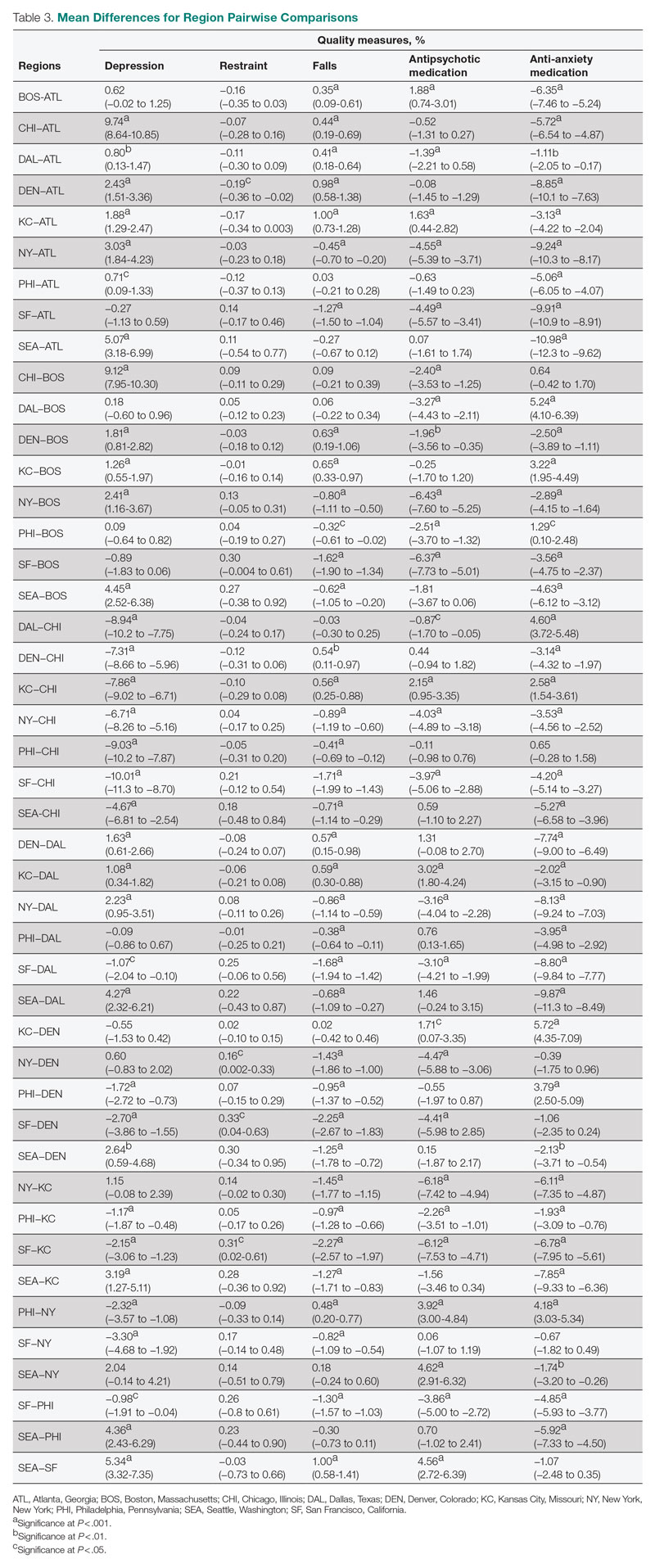
Occupancy
The mean scores for 4 out of the 5 QMs exhibited similar relationships with occupancy rates: resident depression, falls, and antipsychotic and anti-anxiety medication use. Low-occupancy residences consistently scored significantly higher than both medium- and high-occupancy residences, and medium-occupancy residences consistently scored significantly higher than high-occupancy residences. On average, high-occupancy (≥ 92%) residences reported better QM scores than low-occupancy (< 73%) and medium-occupancy (73% to 91%) residences for all the QMs studied except physical restraint, which yielded no significant results. These findings indicate a possible inverse relationship between building occupancy rate and these 4 QMs.
Region
Pairwise comparisons of mean QM scores by region are shown in Table 3. The Chicago region had a significantly higher mean depression score than all other regions, while the San Francisco region’s score was significantly lower than all other regions, except Atlanta and Boston. The Kansas City region had a significantly higher mean score for resident falls than all other regions, with the exception of Denver, and the San Francisco region scored significantly lower than all other regions in falls. The Boston region had a significantly higher mean score for administering antipsychotic medication than all other regions, except for Kansas City and Seattle, and the New York and San Francisco regions both had significantly lower scores than all other regions except for each other. The Atlanta region reported a significantly higher mean score for administering antianxiety medication than all other regions, and the Seattle region’s score for anti-anxiety medication use was significantly lower than all other regions except for San Francisco.
Discussion
This study presented mean percentages for 5 QMs reported in the Nursing Home Compare database for the year 2019: depression, restraint, falls, antipsychotic medication use, and anti-anxiety medication use. We investigated these scores by 4 residential characteristics: ownership type, size, occupancy, and region. In general, publicly owned and low-occupancy residences had the highest scores, and thus the poorest performances, for the 5 chosen QMs during 2019. Nonprofit and high-occupancy residences generally had the lowest (ie, better) scores, and this result agrees with previous findings on long-stay nursing home residents.21 One possible explanation for better performance by high-occupancy buildings could be that increased social interaction is beneficial to nursing home residents as compared with low-occupancy buildings, where less social interaction is probable. It is difficult to draw conclusions regarding nursing home size and region; however, there are significant differences among sizes for 3 out of the 5 QMs and significant differences among regions for all 5 QMs. The analyses suggest that residence-level characteristics are related to QM scores. Although reported QMs are not a direct representation of resident quality of life, this work agrees with previous research that residential characteristics have some impact on the lives of nursing home residents.13-17 Improvements in QM reporting and changes in quality improvement goals since the formation of Nursing Home Compare exist, suggesting that nursing homes’ awareness of their reporting duties may impact quality of care or reporting tendencies.21,22 Future research should consider investigating the impacts of the COVID-19 pandemic on quality-reporting trends and QM scores.
Other physical characteristics of nursing homes, such as noise, lighting levels, and air quality, may also have an impact on QMs and possibly nursing home residents themselves. This type of data exploration could be included in future research. Additionally, future research could include a similar analysis over a longer period, rather than the 1-year period examined here, to investigate which types of residences consistently have high or low scores or how different types of residences have evolved over the years, particularly considering the impact of the COVID-19 pandemic. Information such as staffing levels, building renovations, and inspection data could be accounted for in future studies. Different QMs could also be investigated to better understand the influence of residential characteristics on quality of care.
Conclusion
This study suggests that residence-level characteristics are related to 5 reported nursing home QMs. Overall, nonprofit and high-occupancy residences had the lowest QM scores, indicating the highest performance. Although the results do not necessarily suggest that residence-level characteristics impact individual nursing home residents’ quality of life, they suggest that physical characteristics affect overall quality of life in nursing homes. Future research is needed to determine the specific physical characteristics of these residences that affect QM scores.
Corresponding author: Brian J. Puckett, [email protected].
Disclosures: None reported.
1. Gauthier S, Rosa-Neto P, Morais JA, et al. World Alzheimer report 2021: journey through the diagnosis of dementia. Alzheimer’s Disease International; 2021.
2. Garre-Olmo J, López-Pousa S, Turon-Estrada A, et al. Environmental determinants of quality of life in nursing home residents with severe dementia. J Am Geriatr Soc. 2012;60(7):1230-1236. doi:10.1111/j.1532-5415.2012.04040.x
3. Zeisel J, Silverstein N, Hyde J, et al. Environmental correlates to behavioral health outcomes in Alzheimer’s special care units. Gerontologist. 2003;43(5):697-711. doi:10.1093/geront/43.5.697
4. Brawley E. Environmental design for Alzheimer’s disease: a quality of life issue. Aging Ment Health. 2001;5(1):S79-S83. doi:10.1080/13607860120044846
5. Joosse L. Do sound levels and space contribute to agitation in nursing home residents with dementia? Research Gerontol Nurs. 2012;5(3):174-184. doi:10.3928/19404921-20120605-02
6. Dowling G, Graf C, Hubbard E, et al. Light treatment for neuropsychiatric behaviors in Alzheimer’s disease. Western J Nurs Res. 2007;29(8):961-975. doi:10.1177/0193945907303083
7. Tartarini F, Cooper P, Fleming R, et al. Indoor air temperature and agitation of nursing home residents with dementia. Am J Alzheimers Dis Other Demen. 2017;32(5):272-281. doi:10.1177/1533317517704898
8. Miyamoto Y, Tachimori H, Ito H. Formal caregiver burden in dementia: impact of behavioral and psychological symptoms of dementia and activities of daily living. Geriatr Nurs. 2010;31(4):246-253. doi:10.1016/j.gerinurse.2010.01.002
9. Dementia care and the built environment: position paper 3. Alzheimer’s Australia; 2004.
10. Cloak N, Al Khalili Y. Behavioral and psychological symptoms in dementia. Updated July 21, 2022. In: StatPearls [Internet]. StatPearls Publishing; 2022.
11. Centers for Medicare & Medicaid Services. Nursing homes including rehab services data archive. 2019 annual files. Accessed January 30, 2023. https://data.cms.gov/provider-data/archived-data/nursing-homes
12. Sanghavi P, Pan S, Caudry D. Assessment of nursing home reporting of major injury falls for quality measurement on Nursing Home Compare. Health Serv Res. 2020;55(2):201-210. doi:10.1111/1475-6773.13247
13. Hughes C, Lapane K, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing homes. Med Care. 2000;38(12):1164-1173. doi:10.1097/00005650-200012000-00003
14. Aaronson W, Zinn J, Rosko M. Do for-profit and not-for-profit nursing homes behave differently? Gerontologist. 1994;34(6):775-786. doi:10.1093/geront/34.6.775
15. O’Neill C, Harrington C, Kitchener M, et al. Quality of care in nursing homes: an analysis of relationships among profit, quality, and ownership. Med Care. 2003;41(12):1318-1330. doi:10.1097/01.MLR.0000100586.33970.58
16. Allen PD, Klein WC, Gruman C. Correlates of complaints made to the Connecticut Long-Term Care Ombudsman program: the role of organizational and structural factors. Res Aging. 2003;25(6):631-654. doi:10.1177/0164027503256691
17. Abrams H, Loomer L, Gandhi A, et al. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68(8):1653-1656. doi:10.1111/jgs.16661
18. Evans JD. Straightforward Statistics for the Behavioral Sciences. Thomson Brooks/Cole Publishing Co; 1996.
19. Zinn J, Spector W, Hsieh L, et al. Do trends in the reporting of quality measures on the Nursing Home Compare web site differ by nursing home characteristics? Gerontologist. 2005;45(6):720-730.
20. Centers for Medicare & Medicaid Services. CMS Regional Offices. Accessed January 30, 2023. https://www.cms.gov/Medicare/Coding/ICD10/CMS-Regional-Offices
21. Mukamel DB, Weimer DL, Spector WD, et al. Publication of quality report cards and trends in reported quality measures in nursing homes. Health Serv Res. 2008;43(4):1244-1262. doi:10.1093/geront/45.6.720
22. Harris Y, Clauser SB. Achieving improvement through nursing home quality measurement. Health Care Financ Rev. 2002;23(4):5-18.
1. Gauthier S, Rosa-Neto P, Morais JA, et al. World Alzheimer report 2021: journey through the diagnosis of dementia. Alzheimer’s Disease International; 2021.
2. Garre-Olmo J, López-Pousa S, Turon-Estrada A, et al. Environmental determinants of quality of life in nursing home residents with severe dementia. J Am Geriatr Soc. 2012;60(7):1230-1236. doi:10.1111/j.1532-5415.2012.04040.x
3. Zeisel J, Silverstein N, Hyde J, et al. Environmental correlates to behavioral health outcomes in Alzheimer’s special care units. Gerontologist. 2003;43(5):697-711. doi:10.1093/geront/43.5.697
4. Brawley E. Environmental design for Alzheimer’s disease: a quality of life issue. Aging Ment Health. 2001;5(1):S79-S83. doi:10.1080/13607860120044846
5. Joosse L. Do sound levels and space contribute to agitation in nursing home residents with dementia? Research Gerontol Nurs. 2012;5(3):174-184. doi:10.3928/19404921-20120605-02
6. Dowling G, Graf C, Hubbard E, et al. Light treatment for neuropsychiatric behaviors in Alzheimer’s disease. Western J Nurs Res. 2007;29(8):961-975. doi:10.1177/0193945907303083
7. Tartarini F, Cooper P, Fleming R, et al. Indoor air temperature and agitation of nursing home residents with dementia. Am J Alzheimers Dis Other Demen. 2017;32(5):272-281. doi:10.1177/1533317517704898
8. Miyamoto Y, Tachimori H, Ito H. Formal caregiver burden in dementia: impact of behavioral and psychological symptoms of dementia and activities of daily living. Geriatr Nurs. 2010;31(4):246-253. doi:10.1016/j.gerinurse.2010.01.002
9. Dementia care and the built environment: position paper 3. Alzheimer’s Australia; 2004.
10. Cloak N, Al Khalili Y. Behavioral and psychological symptoms in dementia. Updated July 21, 2022. In: StatPearls [Internet]. StatPearls Publishing; 2022.
11. Centers for Medicare & Medicaid Services. Nursing homes including rehab services data archive. 2019 annual files. Accessed January 30, 2023. https://data.cms.gov/provider-data/archived-data/nursing-homes
12. Sanghavi P, Pan S, Caudry D. Assessment of nursing home reporting of major injury falls for quality measurement on Nursing Home Compare. Health Serv Res. 2020;55(2):201-210. doi:10.1111/1475-6773.13247
13. Hughes C, Lapane K, Mor V. Influence of facility characteristics on use of antipsychotic medications in nursing homes. Med Care. 2000;38(12):1164-1173. doi:10.1097/00005650-200012000-00003
14. Aaronson W, Zinn J, Rosko M. Do for-profit and not-for-profit nursing homes behave differently? Gerontologist. 1994;34(6):775-786. doi:10.1093/geront/34.6.775
15. O’Neill C, Harrington C, Kitchener M, et al. Quality of care in nursing homes: an analysis of relationships among profit, quality, and ownership. Med Care. 2003;41(12):1318-1330. doi:10.1097/01.MLR.0000100586.33970.58
16. Allen PD, Klein WC, Gruman C. Correlates of complaints made to the Connecticut Long-Term Care Ombudsman program: the role of organizational and structural factors. Res Aging. 2003;25(6):631-654. doi:10.1177/0164027503256691
17. Abrams H, Loomer L, Gandhi A, et al. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68(8):1653-1656. doi:10.1111/jgs.16661
18. Evans JD. Straightforward Statistics for the Behavioral Sciences. Thomson Brooks/Cole Publishing Co; 1996.
19. Zinn J, Spector W, Hsieh L, et al. Do trends in the reporting of quality measures on the Nursing Home Compare web site differ by nursing home characteristics? Gerontologist. 2005;45(6):720-730.
20. Centers for Medicare & Medicaid Services. CMS Regional Offices. Accessed January 30, 2023. https://www.cms.gov/Medicare/Coding/ICD10/CMS-Regional-Offices
21. Mukamel DB, Weimer DL, Spector WD, et al. Publication of quality report cards and trends in reported quality measures in nursing homes. Health Serv Res. 2008;43(4):1244-1262. doi:10.1093/geront/45.6.720
22. Harris Y, Clauser SB. Achieving improvement through nursing home quality measurement. Health Care Financ Rev. 2002;23(4):5-18.